Programmed Death Ligand 1 Regulatory Crosstalk with Ubiquitination and Deubiquitination: Implications in Cancer Immunotherapy
Abstract
1. Introduction
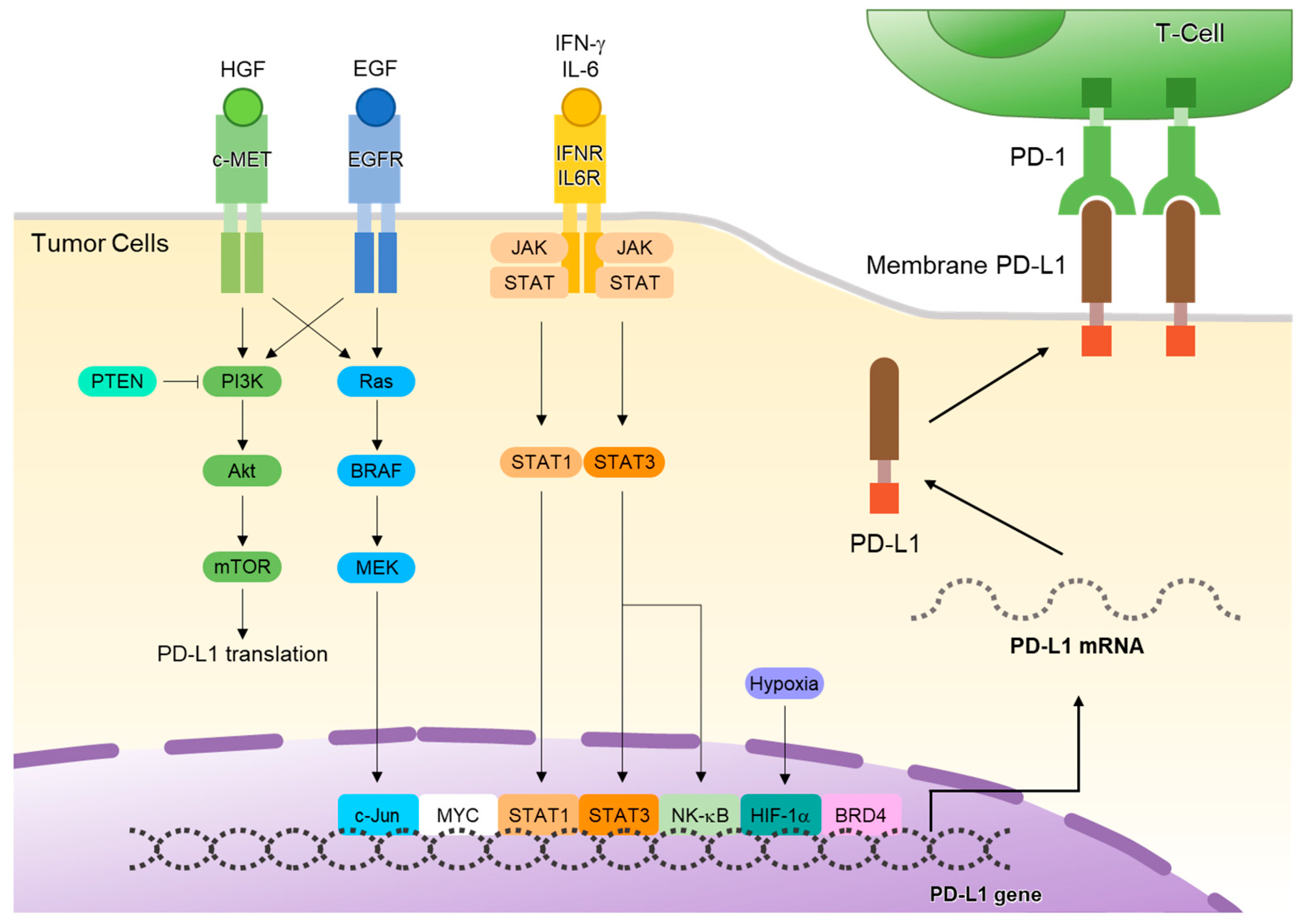
2. PD-L1 and Its Transcriptional Expression
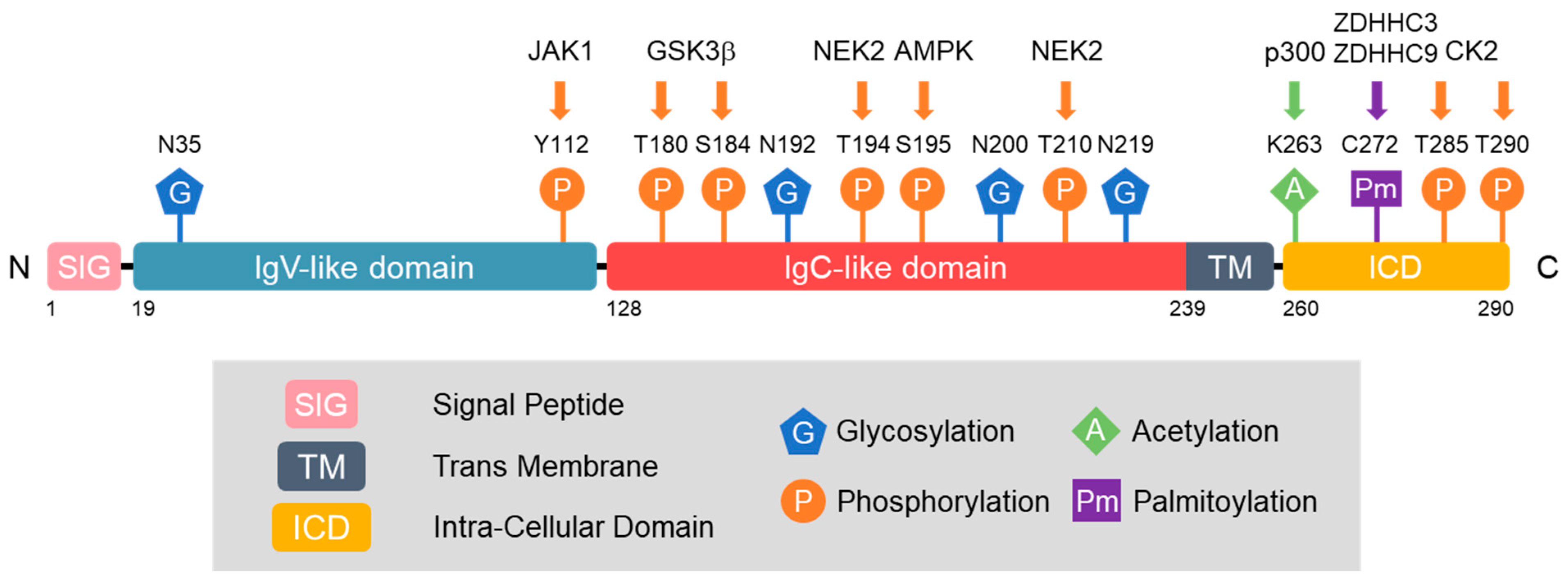
3. Post-Translational Modification (PTM) of PD-L1
3.1. Glycosylation of PD-L1
3.2. Phosphorylation of PD-L1
3.3. Acetylation of PD-L1
3.4. Palmitoylation of PD-L1
3.5. SUMOylation of PD-L1
4. Ubiquitination and Deubiquitination of PD-L1
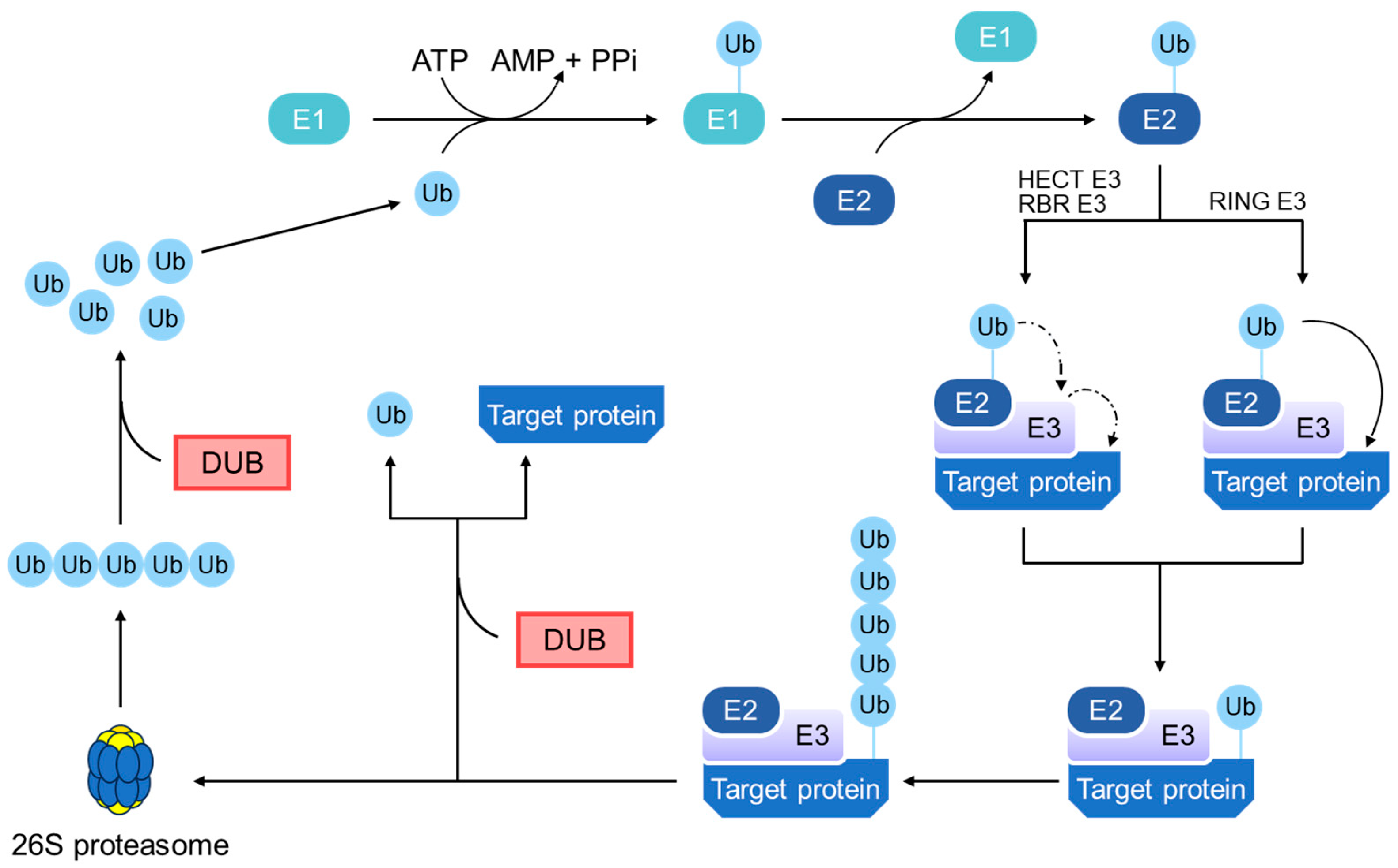
4.1. General Principles of the Ubiquitin–Proteasome Pathway
4.2. E3 Ubiquitin Ligases in PD-L1 Regulation
4.2.1. β-TrCP
4.2.2. STUB1
4.2.3. SPOP
4.2.4. HRD1
4.2.5. RNF144A
4.2.6. NEDD4
4.2.7. FBXO22
4.2.8. TRIM21
| E3 Ligase | Mechanism | Types of Cancer | Effects | References |
|---|---|---|---|---|
| β-TrCP | binds to PD-L1 after GSK3β phosphorylation, leading to PD-L1’s ubiquitination and degradation | Breast cancer | promotes antitumor T-cell immunity and enhances the effectiveness of anti-PD-1 therapy | [28] |
| STUB1 | induces ubiquitination and destabilization of PD-L1 | Lung cancer | negatively modulates immune activity | [57] |
| SPOP | stabilized by CDK4 phosphorylation, downregulates PD-L1 protein, especially during the late G1 and S phases of the cell cycle | Colon cancer Breast cancer | increases T-cell activation | [59,60] |
| HRD1 | HRD1 knockdown diminishes metformin-induced PD-L1 ubiquitination | Breast cancer | enhances antitumor CTL immunity | [32] |
| RNF144A | interacts with PD-L1 and promotes poly-ubiquitination and degradation of PD-L1 | Bladder cancer | Enhances tumor-infiltrating CD8+ T-cell populations | [63] |
| NEDD4 | NEDD4, phosphorylated upon FGFR3 activation, catalyzes the ubiquitination and degradation of PD-L1 | Bladder cancer | Increases the antitumor activity of CD8+ T cells | [65] |
| FBXO22 | FBXO22’s high expression reduces PD-L1 levels, enhancing cancer cell sensitivity to DNA-damaging therapies | NSCLC | enhances the efficacy of immunotherapy | [67] |
| TRIM21 | enhances ubiquitination-mediated proteasomal degradation of PD-L1 | NSCLC | enhances T-cell-induced apoptosis | [70,71] |
4.3. Deubiquitinating Enzymes in PD-L1 Regulation
4.3.1. OTUB1
4.3.2. CSN5
4.3.3. USP2
4.3.4. USP5
4.3.5. USP7
4.3.6. USP8
4.3.7. USP9X
4.3.8. USP18
4.3.9. USP20
4.3.10. USP21
4.3.11. USP22
| DUBs | Mechanism | Types of Cancer | Effects | References |
|---|---|---|---|---|
| OTUB1 | removes K48-linked ubiquitin on PD-L1, thus inhibiting its degradation | lung cancer | decreases CD8+ T-cell infiltration and antitumor immunity | [78,79] |
| CSN5 | removes K48-linked ubiquitin on PD-L1 | breast cancer | promotes immune evasion | [81,82] |
| USP2 | removes K48-linked ubiquitin on PD-L1, leading to increased PD-L1 abundance | colon cancer, prostate cancer | confers resistance to cancer cells against T-cell-mediated killing | [84] |
| USP5 | stabilizes PD-L1 through interaction and deubiquitination | NSCLC | inhibits CD8+ T-cell cytotoxicity | [85] |
| USP7 | stabilizes PD-L1 through interaction and deubiquitination | glioma gastric cancer | inhibits apoptosis and boosts CD8+ T-cell proliferation suppresses M1 macrophages and IFN-γ+ CD8+ T-cell tumor infiltration | [92,93] |
| USP8 | removes K63-linked ubiquitin on PD-L1 stabilizes PD-L1 through deubiquitination | colon cancer lung cancer pancreatic cancer | suppresses activation of CTLs | [96,97] |
| USP9X | stabilizes PD-L1 through interaction and deubiquitination | oral cancer | inhibits T-cell cytotoxicity | [99] |
| USP18 | deconjugates the ubiquitin-like protein ISG15 from PD-L1 | bladder cancer | promotes immune evasion | [100,104] |
| USP20 | stabilizes PD-L1 through deubiquitination. | breast cancer | USP20, stabilized by TINCR, contributes to breast cancer progression | [107] |
| USP21 | stabilizes PD-L1 through interaction and deubiquitination | lung cancer | promotes Treg-cell function | [110,112] |
| USP22 | stabilizes PD-L1 through interaction and deubiquitination | lung cancer liver cancer | inhibits T-cell cytotoxicity | [116,117] |
5. Conclusions and Perspectives
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| PD-L1 | programmed death ligand 1 |
| PD-1 | programmed death 1 |
| DUB | deubiquitinating enzyme |
| IFN | interferon |
| JAK | Janus kinase |
| STAT | signal transducer and activator of the transcription |
| NSCLC | non-small-cell lung cancer |
| PTM | post-translational modification |
| GSK3β | glycogen synthase kinase 3β |
| β-TrCP | β-transducin repeat-containing protein |
| EGF | epidermal growth factor |
| AMPK | AMP-activated protein kinase |
| ERAD | ER-associated degradation |
| SUMO | small-ubiquitin-like modifier |
| CMTM6 | CKLF-like MARVEL transmembrane domain-containing 6 |
| STUB1 | stress-inducible protein-1 (STIP1) homology and U-box containing protein 1 |
| SPOP | speckle-type POZ protein |
| CDK | cyclin-dependent kinase |
| HRD1 | hydroxymethylglutaryl-coenzyme A (HMG-CoA) reductase-degrading protein 1 |
| RNF144A | ring finger 144A |
| NEDD4 | neuronal precursor cell-expressed developmentally downregulated 4 |
| FBXO22 | F-box-only protein 22 |
| TRIM21 | tripartite motif-containing protein 21 |
| OTUB1 | OUT domain-containing ubiquitin aldehyde-binding protein 1 |
| CSN5 | constitutive photomorphogenesis 9 (COP9) signalosome 5 |
| USP | ubiquitin-specific protease |
References
- Qin, S.; Xu, L.; Yi, M.; Yu, S.; Wu, K.; Luo, S. Novel immune checkpoint targets: Moving beyond PD-1 and CTLA-4. Mol. Cancer 2019, 18, 155. [Google Scholar] [CrossRef]
- Sharpe, A.H.; Pauken, K.E. The diverse functions of the PD1 inhibitory pathway. Nat. Rev. Immunol. 2018, 18, 153–167. [Google Scholar] [CrossRef]
- Herbst, R.S.; Baas, P.; Kim, D.W.; Felip, E.; Perez-Gracia, J.L.; Han, J.Y.; Molina, J.; Kim, J.H.; Arvis, C.D.; Ahn, M.J.; et al. Pembrolizumab versus docetaxel for previously treated, PD-L1-positive, advanced non-small-cell lung cancer (KEYNOTE-010): A randomised controlled trial. Lancet 2016, 387, 1540–1550. [Google Scholar] [CrossRef]
- Ishida, Y.; Agata, Y.; Shibahara, K.; Honjo, T. Induced expression of PD-1, a novel member of the immunoglobulin gene superfamily, upon programmed cell death. EMBO J. 1992, 11, 3887–3895. [Google Scholar] [CrossRef] [PubMed]
- Akbay, E.A.; Koyama, S.; Carretero, J.; Altabef, A.; Tchaicha, J.H.; Christensen, C.L.; Mikse, O.R.; Cherniack, A.D.; Beauchamp, E.M.; Pugh, T.J.; et al. Activation of the PD-1 pathway contributes to immune escape in EGFR-driven lung tumors. Cancer Discov. 2013, 3, 1355–1363. [Google Scholar] [CrossRef] [PubMed]
- Keir, M.E.; Butte, M.J.; Freeman, G.J.; Sharpe, A.H. PD-1 and its ligands in tolerance and immunity. Annu. Rev. Immunol. 2008, 26, 677–704. [Google Scholar] [CrossRef]
- Garon, E.B.; Rizvi, N.A.; Hui, R.; Leighl, N.; Balmanoukian, A.S.; Eder, J.P.; Patnaik, A.; Aggarwal, C.; Gubens, M.; Horn, L.; et al. Pembrolizumab for the treatment of non-small-cell lung cancer. N. Engl. J. Med. 2015, 372, 2018–2028. [Google Scholar] [CrossRef] [PubMed]
- Escors, D.; Gato-Canas, M.; Zuazo, M.; Arasanz, H.; Garcia-Granda, M.J.; Vera, R.; Kochan, G. The intracellular signalosome of PD-L1 in cancer cells. Signal Transduct. Target. Ther. 2018, 3, 26. [Google Scholar] [CrossRef] [PubMed]
- Ribas, A.; Wolchok, J.D. Cancer immunotherapy using checkpoint blockade. Science 2018, 359, 1350–1355. [Google Scholar] [CrossRef] [PubMed]
- Hu, X.; Wang, J.; Chu, M.; Liu, Y.; Wang, Z.W.; Zhu, X. Emerging Role of Ubiquitination in the Regulation of PD-1/PD-L1 in Cancer Immunotherapy. Mol. Ther. 2021, 29, 908–919. [Google Scholar] [CrossRef] [PubMed]
- Hou, B.; Chen, T.; Zhang, H.; Li, J.; Wang, P.; Shang, G. The E3 ubiquitin ligases regulate PD-1/PD-L1 protein levels in tumor microenvironment to improve immunotherapy. Front. Immunol. 2023, 14, 1123244. [Google Scholar] [CrossRef]
- Jiang, Y.; Hong, K.; Zhao, Y.; Xu, K. Emerging role of deubiquitination modifications of programmed death-ligand 1 in cancer immunotherapy. Front. Immunol. 2023, 14, 1228200. [Google Scholar] [CrossRef]
- Ding, P.; Ma, Z.; Fan, Y.; Feng, Y.; Shao, C.; Pan, M.; Zhang, Y.; Huang, D.; Han, J.; Hu, Y.; et al. Emerging role of ubiquitination/deubiquitination modification of PD-1/PD-L1 in cancer immunotherapy. Genes Dis. 2023, 10, 848–863. [Google Scholar] [CrossRef] [PubMed]
- Freeman, G.J.; Long, A.J.; Iwai, Y.; Bourque, K.; Chernova, T.; Nishimura, H.; Fitz, L.J.; Malenkovich, N.; Okazaki, T.; Byrne, M.C.; et al. Engagement of the PD-1 immunoinhibitory receptor by a novel B7 family member leads to negative regulation of lymphocyte activation. J. Exp. Med. 2000, 192, 1027–1034. [Google Scholar] [CrossRef] [PubMed]
- He, X.H.; Xu, L.H.; Liu, Y. Identification of a novel splice variant of human PD-L1 mRNA encoding an isoform-lacking Igv-like domain. Acta Pharmacol. Sin. 2005, 26, 462–468. [Google Scholar] [CrossRef] [PubMed]
- Okazaki, T.; Honjo, T. PD-1 and PD-1 ligands: From discovery to clinical application. Int. Immunol. 2007, 19, 813–824. [Google Scholar] [CrossRef] [PubMed]
- Yuan, Y.; Adam, A.; Zhao, C.; Chen, H. Recent Advancements in the Mechanisms Underlying Resistance to PD-1/PD-L1 Blockade Immunotherapy. Cancers 2021, 13, 663. [Google Scholar] [CrossRef] [PubMed]
- Sun, C.; Mezzadra, R.; Schumacher, T.N. Regulation and Function of the PD-L1 Checkpoint. Immunity 2018, 48, 434–452. [Google Scholar] [CrossRef] [PubMed]
- Abiko, K.; Matsumura, N.; Hamanishi, J.; Horikawa, N.; Murakami, R.; Yamaguchi, K.; Yoshioka, Y.; Baba, T.; Konishi, I.; Mandai, M. IFN-γ from lymphocytes induces PD-L1 expression and promotes progression of ovarian cancer. Br. J. Cancer 2015, 112, 1501–1509. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Diaz, A.; Shin, D.S.; Moreno, B.H.; Saco, J.; Escuin-Ordinas, H.; Rodriguez, G.A.; Zaretsky, J.M.; Sun, L.; Hugo, W.; Wang, X.; et al. Interferon Receptor Signaling Pathways Regulating PD-L1 and PD-L2 Expression. Cell Rep. 2017, 19, 1189–1201. [Google Scholar] [CrossRef]
- Kinter, A.L.; Godbout, E.J.; McNally, J.P.; Sereti, I.; Roby, G.A.; O’Shea, M.A.; Fauci, A.S. The common γ-chain cytokines IL-2, IL-7, IL-15, and IL-21 induce the expression of programmed death-1 and its ligands. J. Immunol. 2008, 181, 6738–6746. [Google Scholar] [CrossRef]
- Zhang, N.; Zeng, Y.; Du, W.; Zhu, J.; Shen, D.; Liu, Z.; Huang, J.A. The EGFR pathway is involved in the regulation of PD-L1 expression via the IL-6/JAK/STAT3 signaling pathway in EGFR-mutated non-small cell lung cancer. Int. J. Oncol. 2016, 49, 1360–1368. [Google Scholar] [CrossRef]
- Papaccio, F.; Della Corte, C.M.; Viscardi, G.; Di Liello, R.; Esposito, G.; Sparano, F.; Ciardiello, F.; Morgillo, F. HGF/MET and the Immune System: Relevance for Cancer Immunotherapy. Int. J. Mol. Sci. 2018, 19, 3595. [Google Scholar] [CrossRef]
- Liu, Z.; Yang, J.; Du, M.; Xin, W. Functioning and mechanisms of PTMs in renal diseases. Front. Pharmacol. 2023, 14, 1238706. [Google Scholar] [CrossRef]
- Pinho, S.S.; Reis, C.A. Glycosylation in cancer: Mechanisms and clinical implications. Nat. Rev. Cancer 2015, 15, 540–555. [Google Scholar] [CrossRef]
- Li, C.W.; Lim, S.O.; Xia, W.; Lee, H.H.; Chan, L.C.; Kuo, C.W.; Khoo, K.H.; Chang, S.S.; Cha, J.H.; Kim, T.; et al. Glycosylation and stabilization of programmed death ligand-1 suppresses T-cell activity. Nat. Commun. 2016, 7, 12632. [Google Scholar] [CrossRef]
- Li, C.W.; Lim, S.O.; Chung, E.M.; Kim, Y.S.; Park, A.H.; Yao, J.; Cha, J.H.; Xia, W.; Chan, L.C.; Kim, T.; et al. Eradication of Triple-Negative Breast Cancer Cells by Targeting Glycosylated PD-L1. Cancer Cell 2018, 33, 187–201 e10. [Google Scholar] [CrossRef] [PubMed]
- Hsu, J.M.; Xia, W.; Hsu, Y.H.; Chan, L.C.; Yu, W.H.; Cha, J.H.; Chen, C.T.; Liao, H.W.; Kuo, C.W.; Khoo, K.H.; et al. STT3-dependent PD-L1 accumulation on cancer stem cells promotes immune evasion. Nat. Commun. 2018, 9, 1908. [Google Scholar] [CrossRef] [PubMed]
- Shao, B.; Li, C.W.; Lim, S.O.; Sun, L.; Lai, Y.J.; Hou, J.; Liu, C.; Chang, C.W.; Qiu, Y.; Hsu, J.M.; et al. Deglycosylation of PD-L1 by 2-deoxyglucose reverses PARP inhibitor-induced immunosuppression in triple-negative breast cancer. Am. J. Cancer Res. 2018, 8, 1837–1846. [Google Scholar] [PubMed]
- Cha, J.H.; Yang, W.H.; Xia, W.; Wei, Y.; Chan, L.C.; Lim, S.O.; Li, C.W.; Kim, T.; Chang, S.S.; Lee, H.H.; et al. Metformin Promotes Antitumor Immunity via Endoplasmic-Reticulum-Associated Degradation of PD-L1. Mol. Cell 2018, 71, 606–620 e7. [Google Scholar] [CrossRef] [PubMed]
- Chan, L.C.; Li, C.W.; Xia, W.; Hsu, J.M.; Lee, H.H.; Cha, J.H.; Wang, H.L.; Yang, W.H.; Yen, E.Y.; Chang, W.C.; et al. IL-6/JAK1 pathway drives PD-L1 Y112 phosphorylation to promote cancer immune evasion. J. Clin. Investig. 2019, 129, 3324–3338. [Google Scholar] [CrossRef]
- Zhang, X.; Huang, X.; Xu, J.; Li, E.; Lao, M.; Tang, T.; Zhang, G.; Guo, C.; Zhang, X.; Chen, W.; et al. NEK2 inhibition triggers anti-pancreatic cancer immunity by targeting PD-L1. Nat. Commun. 2021, 12, 4536. [Google Scholar] [CrossRef]
- Zhao, X.; Wei, Y.; Chu, Y.Y.; Li, Y.; Hsu, J.M.; Jiang, Z.; Liu, C.; Hsu, J.L.; Chang, W.C.; Yang, R.; et al. Phosphorylation and Stabilization of PD-L1 by CK2 Suppresses Dendritic Cell Function. Cancer Res. 2022, 82, 2185–2195. [Google Scholar] [CrossRef]
- Drazic, A.; Myklebust, L.M.; Ree, R.; Arnesen, T. The world of protein acetylation. Biochim. Biophys. Acta (BBA) Proteins Proteom. 2016, 1864, 1372–1401. [Google Scholar] [CrossRef]
- Horita, H.; Law, A.; Hong, S.; Middleton, K. Identifying Regulatory Posttranslational Modifications of PD-L1: A Focus on Monoubiquitinaton. Neoplasia 2017, 19, 346–353. [Google Scholar] [CrossRef]
- Gao, Y.; Nihira, N.T.; Bu, X.; Chu, C.; Zhang, J.; Kolodziejczyk, A.; Fan, Y.; Chan, N.T.; Ma, L.; Liu, J.; et al. Acetylation-dependent regulation of PD-L1 nuclear translocation dictates the efficacy of anti-PD-1 immunotherapy. Nat. Cell Biol. 2020, 22, 1064–1075. [Google Scholar] [CrossRef]
- De, I.; Sadhukhan, S. Emerging Roles of DHHC-mediated Protein S-palmitoylation in Physiological and Pathophysiological Context. Eur. J. Cell Biol. 2018, 97, 319–338. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Hsu, J.M.; Sun, L.; Chan, L.C.; Li, C.W.; Hsu, J.L.; Wei, Y.; Xia, W.; Hou, J.; Qiu, Y.; et al. Palmitoylation stabilizes PD-L1 to promote breast tumor growth. Cell Res. 2019, 29, 83–86. [Google Scholar] [CrossRef] [PubMed]
- Yao, H.; Lan, J.; Li, C.; Shi, H.; Brosseau, J.P.; Wang, H.; Lu, H.; Fang, C.; Zhang, Y.; Liang, L.; et al. Inhibiting PD-L1 palmitoylation enhances T-cell immune responses against tumours. Nat. Biomed. Eng. 2019, 3, 306–317. [Google Scholar] [CrossRef]
- Shahid, M.; Kim, M.; Jin, P.; Zhou, B.; Wang, Y.; Yang, W.; You, S.; Kim, J. S-Palmitoylation as a Functional Regulator of Proteins Associated with Cisplatin Resistance in Bladder Cancer. Int. J. Biol. Sci. 2020, 16, 2490–2505. [Google Scholar] [CrossRef] [PubMed]
- Geiss-Friedlander, R.; Melchior, F. Concepts in sumoylation: A decade on. Nat. Rev. Mol. Cell Biol. 2007, 8, 947–956. [Google Scholar] [CrossRef] [PubMed]
- Sarge, K.D. Analysis of Protein Sumoylation. Curr. Protoc. Protein Sci. 2016, 83, 14-8-1–14-8-8. [Google Scholar] [CrossRef] [PubMed]
- Ma, X.; Jia, S.; Wang, G.; Liang, M.; Guo, T.; Du, H.; Li, S.; Li, X.; Huangfu, L.; Guo, J.; et al. TRIM28 promotes the escape of gastric cancer cells from immune surveillance by increasing PD-L1 abundance. Signal Transduct. Target. Ther. 2023, 8, 246. [Google Scholar] [CrossRef] [PubMed]
- Ivanov, A.V.; Peng, H.; Yurchenko, V.; Yap, K.L.; Negorev, D.G.; Schultz, D.C.; Psulkowski, E.; Fredericks, W.J.; White, D.E.; Maul, G.G.; et al. PHD domain-mediated E3 ligase activity directs intramolecular sumoylation of an adjacent bromodomain required for gene silencing. Mol. Cell 2007, 28, 823–837. [Google Scholar] [CrossRef] [PubMed]
- Park, J.; Cho, J.; Song, E.J. Ubiquitin-proteasome system (UPS) as a target for anticancer treatment. Arch. Pharm. Res. 2020, 43, 1144–1161. [Google Scholar] [CrossRef] [PubMed]
- LaPlante, G.; Zhang, W. Targeting the Ubiquitin-Proteasome System for Cancer Therapeutics by Small-Molecule Inhibitors. Cancers 2021, 13, 3079. [Google Scholar] [CrossRef]
- Li, W.; Ye, Y. Polyubiquitin chains: Functions, structures, and mechanisms. Cell Mol. Life Sci. 2008, 65, 2397–2406. [Google Scholar] [CrossRef]
- Komander, D.; Clague, M.J.; Urbe, S. Breaking the chains: Structure and function of the deubiquitinases. Nat. Rev. Mol. Cell Biol. 2009, 10, 550–563. [Google Scholar] [CrossRef]
- Adams, J. The proteasome: Structure, function, and role in the cell. Cancer Treat. Rev. 2003, 29 (Suppl. S1), 3–9. [Google Scholar] [CrossRef]
- Dagar, G.; Kumar, R.; Yadav, K.K.; Singh, M.; Pandita, T.K. Ubiquitination and deubiquitination: Implications on cancer therapy. Biochim. Biophys. Acta (BBA) Gene Regul. Mech. 2023, 1866, 194979. [Google Scholar] [CrossRef]
- Fraile, J.M.; Quesada, V.; Rodriguez, D.; Freije, J.M.; Lopez-Otin, C. Deubiquitinases in cancer: New functions and therapeutic options. Oncogene 2012, 31, 2373–2388. [Google Scholar] [CrossRef]
- Gao, H.; Yin, J.; Ji, C.; Yu, X.; Xue, J.; Guan, X.; Zhang, S.; Liu, X.; Xing, F. Targeting ubiquitin specific proteases (USPs) in cancer immunotherapy: From basic research to preclinical application. J. Exp. Clin. Cancer Res. 2023, 42, 225. [Google Scholar] [CrossRef] [PubMed]
- Fuchs, S.Y.; Spiegelman, V.S.; Kumar, K.G. The many faces of β-TrCP E3 ubiquitin ligases: Reflections in the magic mirror of cancer. Oncogene 2004, 23, 2028–2036. [Google Scholar] [CrossRef] [PubMed]
- Burr, M.L.; Sparbier, C.E.; Chan, Y.C.; Williamson, J.C.; Woods, K.; Beavis, P.A.; Lam, E.Y.N.; Henderson, M.A.; Bell, C.C.; Stolzenburg, S.; et al. CMTM6 maintains the expression of PD-L1 and regulates anti-tumour immunity. Nature 2017, 549, 101–105. [Google Scholar] [CrossRef]
- Mezzadra, R.; Sun, C.; Jae, L.T.; Gomez-Eerland, R.; de Vries, E.; Wu, W.; Logtenberg, M.E.W.; Slagter, M.; Rozeman, E.A.; Hofland, I.; et al. Identification of CMTM6 and CMTM4 as PD-L1 protein regulators. Nature 2017, 549, 106–110. [Google Scholar] [CrossRef] [PubMed]
- Yuan, J.; Li, J.; Shang, M.; Fu, Y.; Wang, T. Identification of vitamin B6 as a PD-L1 suppressor and an adjuvant for cancer immunotherapy. Biochem. Biophys. Res. Commun. 2021, 561, 187–194. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Bu, X.; Wang, H.; Zhu, Y.; Geng, Y.; Nihira, N.T.; Tan, Y.; Ci, Y.; Wu, F.; Dai, X.; et al. Cyclin D-CDK4 kinase destabilizes PD-L1 via cullin 3-SPOP to control cancer immune surveillance. Nature 2018, 553, 91–95. [Google Scholar] [CrossRef] [PubMed]
- Meng, F.; Su, Y.; Xu, B. Rho-associated protein kinase-dependent moesin phosphorylation is required for PD-L1 stabilization in breast cancer. Mol. Oncol. 2020, 14, 2701–2712. [Google Scholar] [CrossRef]
- Xu, Y.; Fang, D. Endoplasmic reticulum-associated degradation and beyond: The multitasking roles for HRD1 in immune regulation and autoimmunity. J. Autoimmun. 2020, 109, 102423. [Google Scholar] [CrossRef]
- Smit, J.J.; Sixma, T.K. RBR E3-ligases at work. EMBO Rep. 2014, 15, 142–154. [Google Scholar] [CrossRef]
- Ho, S.R.; Lee, Y.C.; Ittmann, M.M.; Lin, F.T.; Chan, K.S.; Lin, W.C. RNF144A deficiency promotes PD-L1 protein stabilization and carcinogen-induced bladder tumorigenesis. Cancer Lett. 2021, 520, 344–360. [Google Scholar] [CrossRef] [PubMed]
- Rotin, D.; Kumar, S. Physiological functions of the HECT family of ubiquitin ligases. Nat. Rev. Mol. Cell Biol. 2009, 10, 398–409. [Google Scholar] [CrossRef] [PubMed]
- Jing, W.; Wang, G.; Cui, Z.; Xiong, G.; Jiang, X.; Li, Y.; Li, W.; Han, B.; Chen, S.; Shi, B. FGFR3 Destabilizes PD-L1 via NEDD4 to Control T-cell-Mediated Bladder Cancer Immune Surveillance. Cancer Res. 2022, 82, 114–129. [Google Scholar] [CrossRef] [PubMed]
- Johmura, Y.; Sun, J.; Kitagawa, K.; Nakanishi, K.; Kuno, T.; Naiki-Ito, A.; Sawada, Y.; Miyamoto, T.; Okabe, A.; Aburatani, H.; et al. SCF(Fbxo22)-KDM4A targets methylated p53 for degradation and regulates senescence. Nat. Commun. 2016, 7, 10574. [Google Scholar] [CrossRef] [PubMed]
- De, S.; Holvey-Bates, E.G.; Mahen, K.; Willard, B.; Stark, G.R. The ubiquitin E3 ligase FBXO22 degrades PD-L1 and sensitizes cancer cells to DNA damage. Proc. Natl. Acad. Sci. USA 2021, 118, e2112674118. [Google Scholar] [CrossRef] [PubMed]
- James, L.C.; Keeble, A.H.; Khan, Z.; Rhodes, D.A.; Trowsdale, J. Structural basis for PRYSPRY-mediated tripartite motif (TRIM) protein function. Proc. Natl. Acad. Sci. USA 2007, 104, 6200–6205. [Google Scholar] [CrossRef]
- Zhang, H.; Zhou, F.; Wang, Y.; Xie, H.; Luo, S.; Meng, L.; Su, B.; Ye, Y.; Wu, K.; Xu, Y.; et al. Eliminating Radiation Resistance of Non-Small Cell Lung Cancer by Dihydroartemisinin Through Abrogating Immunity Escaping and Promoting Radiation Sensitivity by Inhibiting PD-L1 Expression. Front. Oncol. 2020, 10, 595466. [Google Scholar] [CrossRef]
- Gao, L.; Xia, L.; Ji, W.; Zhang, Y.; Xia, W.; Lu, S. Knockdown of CDK5 down-regulates PD-L1 via the ubiquitination-proteasome pathway and improves antitumor immunity in lung adenocarcinoma. Transl. Oncol. 2021, 14, 101148. [Google Scholar] [CrossRef]
- Sun, Z.; Mai, H.; Xue, C.; Fan, Z.; Li, J.; Chen, H.; Huo, N.; Kang, X.; Tang, C.; Fang, L.; et al. Hsa-LINC02418/mmu-4930573I07Rik regulated by METTL3 dictates anti-PD-L1 immunotherapeutic efficacy via enhancement of Trim21-mediated PD-L1 ubiquitination. J. Immunother. Cancer 2023, 11, e007415. [Google Scholar] [CrossRef]
- Reyes-Turcu, F.E.; Ventii, K.H.; Wilkinson, K.D. Regulation and cellular roles of ubiquitin-specific deubiquitinating enzymes. Annu. Rev. Biochem. 2009, 78, 363–397. [Google Scholar] [CrossRef]
- Mevissen, T.E.T.; Komander, D. Mechanisms of Deubiquitinase Specificity and Regulation. Annu. Rev. Biochem. 2017, 86, 159–192. [Google Scholar] [CrossRef]
- Ohanna, M.; Biber, P.; Deckert, M. Emerging Role of Deubiquitinating Enzymes (DUBs) in Melanoma Pathogenesis. Cancers 2022, 14, 3371. [Google Scholar] [CrossRef]
- Clague, M.J.; Barsukov, I.; Coulson, J.M.; Liu, H.; Rigden, D.J.; Urbe, S. Deubiquitylases from genes to organism. Physiol. Rev. 2013, 93, 1289–1315. [Google Scholar] [CrossRef]
- Lange, S.M.; Armstrong, L.A.; Kulathu, Y. Deubiquitinases: From mechanisms to their inhibition by small molecules. Mol. Cell 2022, 82, 15–29. [Google Scholar] [CrossRef]
- Wiener, R.; Zhang, X.; Wang, T.; Wolberger, C. The mechanism of OTUB1-mediated inhibition of ubiquitination. Nature 2012, 483, 618–622. [Google Scholar] [CrossRef] [PubMed]
- Zhu, D.; Xu, R.; Huang, X.; Tang, Z.; Tian, Y.; Zhang, J.; Zheng, X. Deubiquitinating enzyme OTUB1 promotes cancer cell immunosuppression via preventing ER-associated degradation of immune checkpoint protein PD-L1. Cell Death Differ. 2021, 28, 1773–1789. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Wang, T.; She, Y.; Wu, K.; Gu, S.; Li, L.; Dong, C.; Chen, C.; Zhou, Y. N6-methyladenosine-modified circIGF2BP3 inhibits CD8+ T-cell responses to facilitate tumor immune evasion by promoting the deubiquitination of PD-L1 in non-small cell lung cancer. Mol. Cancer 2021, 20, 105. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Shah, S.V.; Xiang, X.; Wang, J.; Deng, Z.B.; Liu, C.; Zhang, L.; Wu, J.; Edmonds, T.; Jambor, C.; et al. COP9-associated CSN5 regulates exosomal protein deubiquitination and sorting. Am. J. Pathol. 2009, 174, 1415–1425. [Google Scholar] [CrossRef]
- Lim, S.O.; Li, C.W.; Xia, W.; Cha, J.H.; Chan, L.C.; Wu, Y.; Chang, S.S.; Lin, W.C.; Hsu, J.M.; Hsu, Y.H.; et al. Deubiquitination and Stabilization of PD-L1 by CSN5. Cancer Cell 2016, 30, 925–939. [Google Scholar] [CrossRef]
- Ruan, Z.; Liang, M.; Shang, L.; Lai, M.; Deng, X.; Su, X. Shikonin-mediated PD-L1 degradation suppresses immune evasion in pancreatic cancer by inhibiting NF-κB/STAT3 and NF-κB/CSN5 signaling pathways. Pancreatology 2021, 21, 630–641. [Google Scholar] [CrossRef]
- Kitamura, H.; Hashimoto, M. USP2-Related Cellular Signaling and Consequent Pathophysiological Outcomes. Int. J. Mol. Sci. 2021, 22, 1209. [Google Scholar] [CrossRef]
- Kuang, Z.; Liu, X.; Zhang, N.; Dong, J.; Sun, C.; Yin, M.; Wang, Y.; Liu, L.; Xiao, D.; Zhou, X.; et al. USP2 promotes tumor immune evasion via deubiquitination and stabilization of PD-L1. Cell Death Differ. 2023, 30, 2249–2264. [Google Scholar] [CrossRef]
- Pan, J.; Qiao, Y.; Chen, C.; Zang, H.; Zhang, X.; Qi, F.; Chang, C.; Yang, F.; Sun, M.; Lin, S.; et al. USP5 facilitates non-small cell lung cancer progression through stabilization of PD-L1. Cell Death Dis. 2021, 12, 1051. [Google Scholar] [CrossRef]
- Lou, Y.; Diao, L.; Cuentas, E.R.; Denning, W.L.; Chen, L.; Fan, Y.H.; Byers, L.A.; Wang, J.; Papadimitrakopoulou, V.A.; Behrens, C.; et al. Epithelial-Mesenchymal Transition Is Associated with a Distinct Tumor Microenvironment Including Elevation of Inflammatory Signals and Multiple Immune Checkpoints in Lung Adenocarcinoma. Clin. Cancer Res. 2016, 22, 3630–3642. [Google Scholar] [CrossRef]
- Koh, Y.W.; Han, J.H.; Haam, S. Expression of PD-L1, cancer stem cell and epithelial-mesenchymal transition phenotype in non-small cell lung cancer. Pathology 2021, 53, 239–246. [Google Scholar] [CrossRef] [PubMed]
- Cai, H.; Ke, Z.B.; Chen, J.Y.; Li, X.D.; Zhu, J.M.; Xue, Y.T.; Ruan, Z.T.; Wang, Z.; Lin, F.; Zheng, Q.S.; et al. Ubiquitin-specific protease 5 promotes bladder cancer progression through stabilizing Twist1. Oncogene 2024. [Google Scholar] [CrossRef] [PubMed]
- Bhattacharya, S.; Chakraborty, D.; Basu, M.; Ghosh, M.K. Emerging insights into HAUSP (USP7) in physiology, cancer and other diseases. Signal Transduct. Target. Ther. 2018, 3, 17. [Google Scholar] [CrossRef] [PubMed]
- Al-Eidan, A.; Wang, Y.; Skipp, P.; Ewing, R.M. The USP7 protein interaction network and its roles in tumorigenesis. Genes Dis. 2022, 9, 41–50. [Google Scholar] [CrossRef] [PubMed]
- Schauer, N.J.; Liu, X.; Magin, R.S.; Doherty, L.M.; Chan, W.C.; Ficarro, S.B.; Hu, W.; Roberts, R.M.; Iacob, R.E.; Stolte, B.; et al. Selective USP7 inhibition elicits cancer cell killing through a p53-dependent mechanism. Sci. Rep. 2020, 10, 5324. [Google Scholar] [CrossRef] [PubMed]
- Li, B.; Wang, B. USP7 Enables Immune Escape of Glioma Cells by Regulating PD-L1 Expression. Immunol. Investig. 2022, 51, 1921–1937. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Kang, W.; Li, O.; Qi, F.; Wang, J.; You, Y.; He, P.; Suo, Z.; Zheng, Y.; Liu, H.M. Abrogation of USP7 is an alternative strategy to downregulate PD-L1 and sensitize gastric cancer cells to T cells killing. Acta Pharm. Sin. B 2021, 11, 694–707. [Google Scholar] [CrossRef]
- Dai, X.; Lu, L.; Deng, S.; Meng, J.; Wan, C.; Huang, J.; Sun, Y.; Hu, Y.; Wu, B.; Wu, G.; et al. USP7 targeting modulates anti-tumor immune response by reprogramming Tumor-associated Macrophages in Lung Cancer. Theranostics 2020, 10, 9332–9347. [Google Scholar] [CrossRef]
- Fu, C.; Zhu, X.; Xu, P.; Li, Y. Pharmacological inhibition of USP7 promotes antitumor immunity and contributes to colon cancer therapy. Onco Targets Ther. 2019, 12, 609–617. [Google Scholar] [CrossRef]
- Yang, H.; Zhang, X.; Lao, M.; Sun, K.; He, L.; Xu, J.; Duan, Y.; Chen, Y.; Ying, H.; Li, M.; et al. Targeting ubiquitin-specific protease 8 sensitizes anti-programmed death-ligand 1 immunotherapy of pancreatic cancer. Cell Death Differ. 2023, 30, 560–575. [Google Scholar] [CrossRef]
- Xiong, W.; Gao, X.; Zhang, T.; Jiang, B.; Hu, M.M.; Bu, X.; Gao, Y.; Zhang, L.Z.; Xiao, B.L.; He, C.; et al. USP8 inhibition reshapes an inflamed tumor microenvironment that potentiates the immunotherapy. Nat. Commun. 2022, 13, 1700. [Google Scholar] [CrossRef]
- Meng, Y.; Hong, C.; Yang, S.; Qin, Z.; Yang, L.; Huang, Y. Roles of USP9X in cellular functions and tumorigenesis (Review). Oncol. Lett. 2023, 26, 506. [Google Scholar] [CrossRef] [PubMed]
- Jingjing, W.; Wenzheng, G.; Donghua, W.; Guangyu, H.; Aiping, Z.; Wenjuan, W. Deubiquitination and stabilization of programmed cell death ligand 1 by ubiquitin-specific peptidase 9, X-linked in oral squamous cell carcinoma. Cancer Med. 2018, 7, 4004–4011. [Google Scholar] [CrossRef] [PubMed]
- Malakhov, M.P.; Malakhova, O.A.; Kim, K.I.; Ritchie, K.J.; Zhang, D.E. UBP43 (USP18) specifically removes ISG15 from conjugated proteins. J. Biol. Chem. 2002, 277, 9976–9981. [Google Scholar] [CrossRef] [PubMed]
- Martin-Fernandez, M.; Buta, S.; Le Voyer, T.; Li, Z.; Dynesen, L.T.; Vuillier, F.; Franklin, L.; Ailal, F.; Muglia Amancio, A.; Malle, L.; et al. A partial form of inherited human USP18 deficiency underlies infection and inflammation. J. Exp. Med. 2022, 219, e20211273. [Google Scholar] [CrossRef] [PubMed]
- Song, W.; Yang, K.; Luo, J.; Gao, Z.; Gao, Y. Dysregulation of USP18/FTO/PYCR1 signaling network promotes bladder cancer development and progression. Aging 2021, 13, 3909–3925. [Google Scholar] [CrossRef]
- Kim, Y.H.; Kim, W.T.; Jeong, P.; Ha, Y.S.; Kang, H.W.; Yun, S.J.; Moon, S.K.; Choi, Y.H.; Kim, I.Y.; Kim, W.J. Novel combination markers for predicting survival in patients with muscle invasive bladder cancer: USP18 and DGCR2. J. Korean Med. Sci. 2014, 29, 351–356. [Google Scholar] [CrossRef]
- Zheng, R.; Gao, F.; Mao, Z.; Xiao, Y.; Yuan, L.; Huang, Z.; Lv, Q.; Qin, C.; Du, M.; Zhang, Z.; et al. LncRNA BCCE4 Genetically Enhances the PD-L1/PD-1 Interaction in Smoking-Related Bladder Cancer by Modulating miR-328-3p-USP18 Signaling. Adv. Sci. 2023, 10, e2303473. [Google Scholar] [CrossRef]
- Li, Z.; Wang, D.; Na, X.; Schoen, S.R.; Messing, E.M.; Wu, G. Identification of a deubiquitinating enzyme subfamily as substrates of the von Hippel-Lindau tumor suppressor. Biochem. Biophys. Res. Commun. 2002, 294, 700–709. [Google Scholar] [CrossRef] [PubMed]
- Curcio-Morelli, C.; Zavacki, A.M.; Christofollete, M.; Gereben, B.; de Freitas, B.C.; Harney, J.W.; Li, Z.; Wu, G.; Bianco, A.C. Deubiquitination of type 2 iodothyronine deiodinase by von Hippel-Lindau protein-interacting deubiquitinating enzymes regulates thyroid hormone activation. J. Clin. Investig. 2003, 112, 189–196. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Li, G.; Ma, X.; Liu, L.; Liu, J.; Yin, Y.; Li, H.; Chen, Y.; Zhang, X.; Zhang, L.; et al. LncRNA TINCR impairs the efficacy of immunotherapy against breast cancer by recruiting DNMT1 and downregulating MiR-199a-5p via the STAT1-TINCR-USP20-PD-L1 axis. Cell Death Dis. 2023, 14, 76. [Google Scholar] [CrossRef] [PubMed]
- Xu, P.; Xiao, H.; Yang, Q.; Hu, R.; Jiang, L.; Bi, R.; Jiang, X.; Wang, L.; Mei, J.; Ding, F.; et al. The USP21/YY1/SNHG16 axis contributes to tumor proliferation, migration, and invasion of non-small-cell lung cancer. Exp. Mol. Med. 2020, 52, 41–55. [Google Scholar] [CrossRef] [PubMed]
- An, T.; Lu, Y.; Yan, X.; Hou, J. Insights Into the Properties, Biological Functions, and Regulation of USP21. Front. Pharmacol. 2022, 13, 944089. [Google Scholar] [CrossRef] [PubMed]
- Yang, S.; Yan, H.; Wu, Y.; Shan, B.; Zhou, D.; Liu, X.; Mao, X.; Zhou, S.; Zhao, Q.; Xia, H. Deubiquitination and Stabilization of PD-L1 by USP21. Am. J. Transl. Res. 2021, 13, 12763–12774. [Google Scholar] [PubMed]
- Li, Y.; Lu, Y.; Wang, S.; Han, Z.; Zhu, F.; Ni, Y.; Liang, R.; Zhang, Y.; Leng, Q.; Wei, G.; et al. USP21 prevents the generation of T-helper-1-like Treg cells. Nat. Commun. 2016, 7, 13559. [Google Scholar] [CrossRef]
- Deng, B.; Yang, B.; Chen, J.; Wang, S.; Zhang, W.; Guo, Y.; Han, Y.; Li, H.; Dang, Y.; Yuan, Y.; et al. Gallic acid induces T-helper-1-like T(reg) cells and strengthens immune checkpoint blockade efficacy. J. Immunother. Cancer 2022, 10, e004037. [Google Scholar] [CrossRef]
- Zhang, X.Y.; Varthi, M.; Sykes, S.M.; Phillips, C.; Warzecha, C.; Zhu, W.; Wyce, A.; Thorne, A.W.; Berger, S.L.; McMahon, S.B. The putative cancer stem cell marker USP22 is a subunit of the human SAGA complex required for activated transcription and cell-cycle progression. Mol. Cell 2008, 29, 102–111. [Google Scholar] [CrossRef]
- Schrecengost, R.S.; Dean, J.L.; Goodwin, J.F.; Schiewer, M.J.; Urban, M.W.; Stanek, T.J.; Sussman, R.T.; Hicks, J.L.; Birbe, R.C.; Draganova-Tacheva, R.A.; et al. USP22 regulates oncogenic signaling pathways to drive lethal cancer progression. Cancer Res. 2014, 74, 272–286. [Google Scholar] [CrossRef]
- Hu, J.; Yang, D.; Zhang, H.; Liu, W.; Zhao, Y.; Lu, H.; Meng, Q.; Pang, H.; Chen, X.; Liu, Y.; et al. USP22 promotes tumor progression and induces epithelial-mesenchymal transition in lung adenocarcinoma. Lung Cancer 2015, 88, 239–245. [Google Scholar] [CrossRef]
- Huang, X.; Zhang, Q.; Lou, Y.; Wang, J.; Zhao, X.; Wang, L.; Zhang, X.; Li, S.; Zhao, Y.; Chen, Q.; et al. USP22 Deubiquitinates CD274 to Suppress Anticancer Immunity. Cancer Immunol. Res. 2019, 7, 1580–1590. [Google Scholar] [CrossRef]
- Wang, Y.; Sun, Q.; Mu, N.; Sun, X.; Wang, Y.; Fan, S.; Su, L.; Liu, X. The deubiquitinase USP22 regulates PD-L1 degradation in human cancer cells. Cell Commun. Signal 2020, 18, 112. [Google Scholar] [CrossRef]
- Friebus-Kardash, J.; Christ, T.C.; Dietlein, N.; Elwy, A.; Abdelrahman, H.; Holnsteiner, L.; Hu, Z.; Rodewald, H.R.; Lang, K.S. Usp22 Deficiency Leads to Downregulation of PD-L1 and Pathological Activation of CD8+ T Cells and Causes Immunopathology in Response to Acute LCMV Infection. Vaccines 2023, 11, 1563. [Google Scholar] [CrossRef]
- Chen, S.; Liu, Y.; Zhou, H. Advances in the Development Ubiquitin-Specific Peptidase (USP) Inhibitors. Int. J. Mol. Sci. 2021, 22, 4546. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; Chen, T.; Liu, J.; Zhang, H.; Li, J.; Wang, Z.; Shang, G. PROTACs: Novel tools for improving immunotherapy in cancer. Cancer Lett. 2023, 560, 216128. [Google Scholar] [CrossRef] [PubMed]
- Shi, Y.Y.; Dong, D.R.; Fan, G.; Dai, M.Y.; Liu, M. A cyclic peptide-based PROTAC induces intracellular degradation of palmitoyltransferase and potently decreases PD-L1 expression in human cervical cancer cells. Front. Immunol. 2023, 14, 1237964. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Zheng, M.Z.; Ma, Z.L.; Zhou, Y.R.; Huo, J.F.; Zhang, W.B.; Liu, Y.; Guo, Y.Y.; Zhou, X.C.; Li, H.; et al. Design, synthesis, and evaluation of PD-L1 degraders to enhance T cell killing activity against melanoma. Chin. Chem. Lett. 2023, 34, 107762. [Google Scholar] [CrossRef]
- Cotton, A.D.; Nguyen, D.P.; Gramespacher, J.A.; Seiple, I.B.; Wells, J.A. Development of Antibody-Based PROTACs for the Degradation of the Cell-Surface Immune Checkpoint Protein PD-L1. J. Am. Chem. Soc. 2021, 143, 593–598. [Google Scholar] [CrossRef] [PubMed]
| Drug/Inhibitor | Major Target | Types of Cancer | Action Mechanism | References |
|---|---|---|---|---|
| Pyridoxal | STUB1 | Promotes PD-L1 degradation | [56] | |
| Curcumin | CSN5 | Breast cancer | Promotes ubiquitination and degradation of PD-L1 | [79] |
| Shikonin | CSN5 | Pancreatic cancer | Inhibits CSN5 and promotes PD-L1 degradation | [80] |
| Almac4 | USP7 | Gastric cancer | Downregulates PD-L1 expression and sensitizes cancer cells to T-cell killing | [91] |
| DUB-IN-2 | USP8 | Pancreatic cancer | Downregulates PD-L1 expression and activates antitumor immunity | [94] |
| WP1130 | USP9x | Oral squamous cell carcinoma | Inhibits deubiquitination of PD-L1 and destabilizes its expression | [97] |
| PROTAC BMS-37-C3 | Promotes PD-L1 degradation and enhances the killing ability of T cells | [120] | ||
| AbTAC AC-1 | Induces degradation of PD-L1 | [121] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, S.-B.; Hwang, S.; Cha, J.-Y.; Lee, H.-J. Programmed Death Ligand 1 Regulatory Crosstalk with Ubiquitination and Deubiquitination: Implications in Cancer Immunotherapy. Int. J. Mol. Sci. 2024, 25, 2939. https://doi.org/10.3390/ijms25052939
Kim S-B, Hwang S, Cha J-Y, Lee H-J. Programmed Death Ligand 1 Regulatory Crosstalk with Ubiquitination and Deubiquitination: Implications in Cancer Immunotherapy. International Journal of Molecular Sciences. 2024; 25(5):2939. https://doi.org/10.3390/ijms25052939
Chicago/Turabian StyleKim, Soon-Bin, Soonjae Hwang, Ji-Young Cha, and Ho-Jae Lee. 2024. "Programmed Death Ligand 1 Regulatory Crosstalk with Ubiquitination and Deubiquitination: Implications in Cancer Immunotherapy" International Journal of Molecular Sciences 25, no. 5: 2939. https://doi.org/10.3390/ijms25052939
APA StyleKim, S.-B., Hwang, S., Cha, J.-Y., & Lee, H.-J. (2024). Programmed Death Ligand 1 Regulatory Crosstalk with Ubiquitination and Deubiquitination: Implications in Cancer Immunotherapy. International Journal of Molecular Sciences, 25(5), 2939. https://doi.org/10.3390/ijms25052939





