Traversing through the Mechanistic Event Analysis in IL-6 and IL-17 Signaling for a New Therapeutic Paradigm in NSCLC
Abstract
1. Introduction
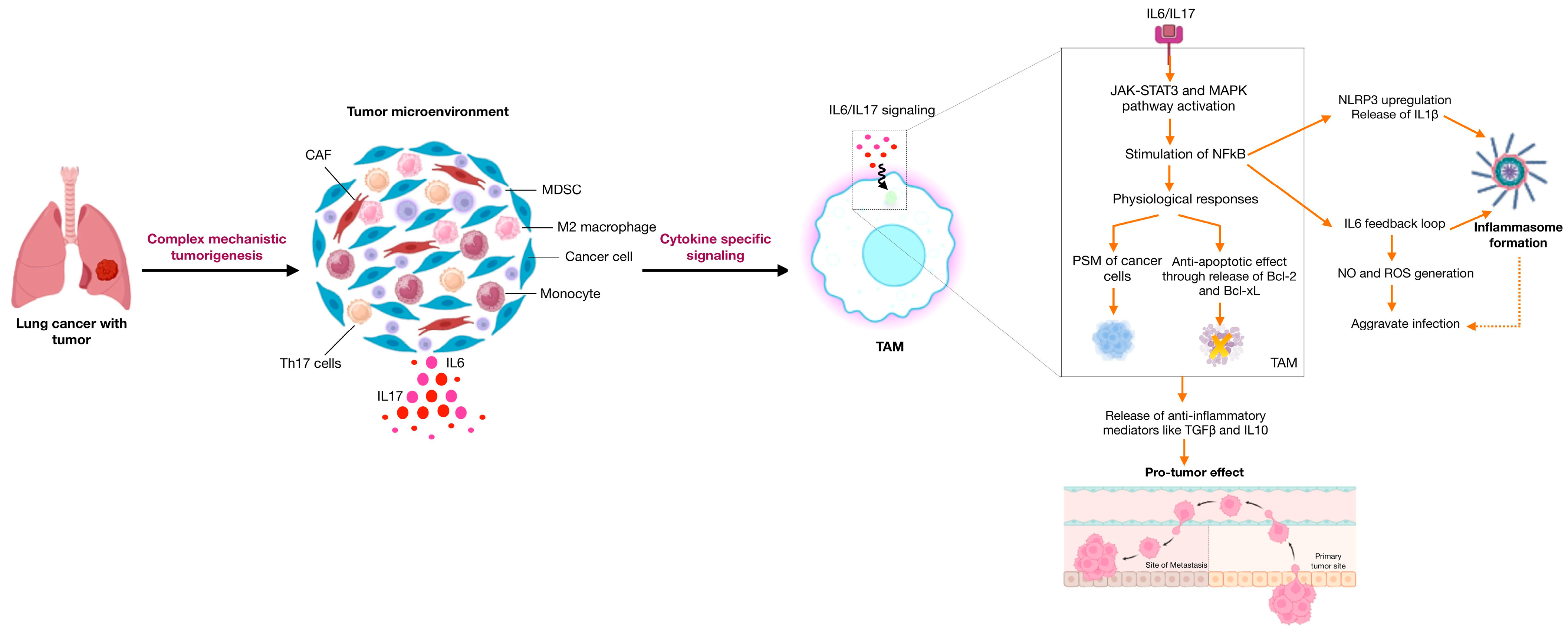
1.1. IL-6 and Signaling Events
1.1.1. The Importance of IL-6 Mediated Regulation in the PSM of Cancer Cells
1.1.2. IL-6 Upregulates NFkB to Address Chronic Inflammation
1.2. IL-17 and Mitogenic Signals
1.2.1. Role of IL-17 in Enhancing Lung Cancer Susceptibility
1.2.2. IL-17 Shapes the TME
1.3. Cellular Crosstalk and Cytokine Implications in Tumor Development
2. Results
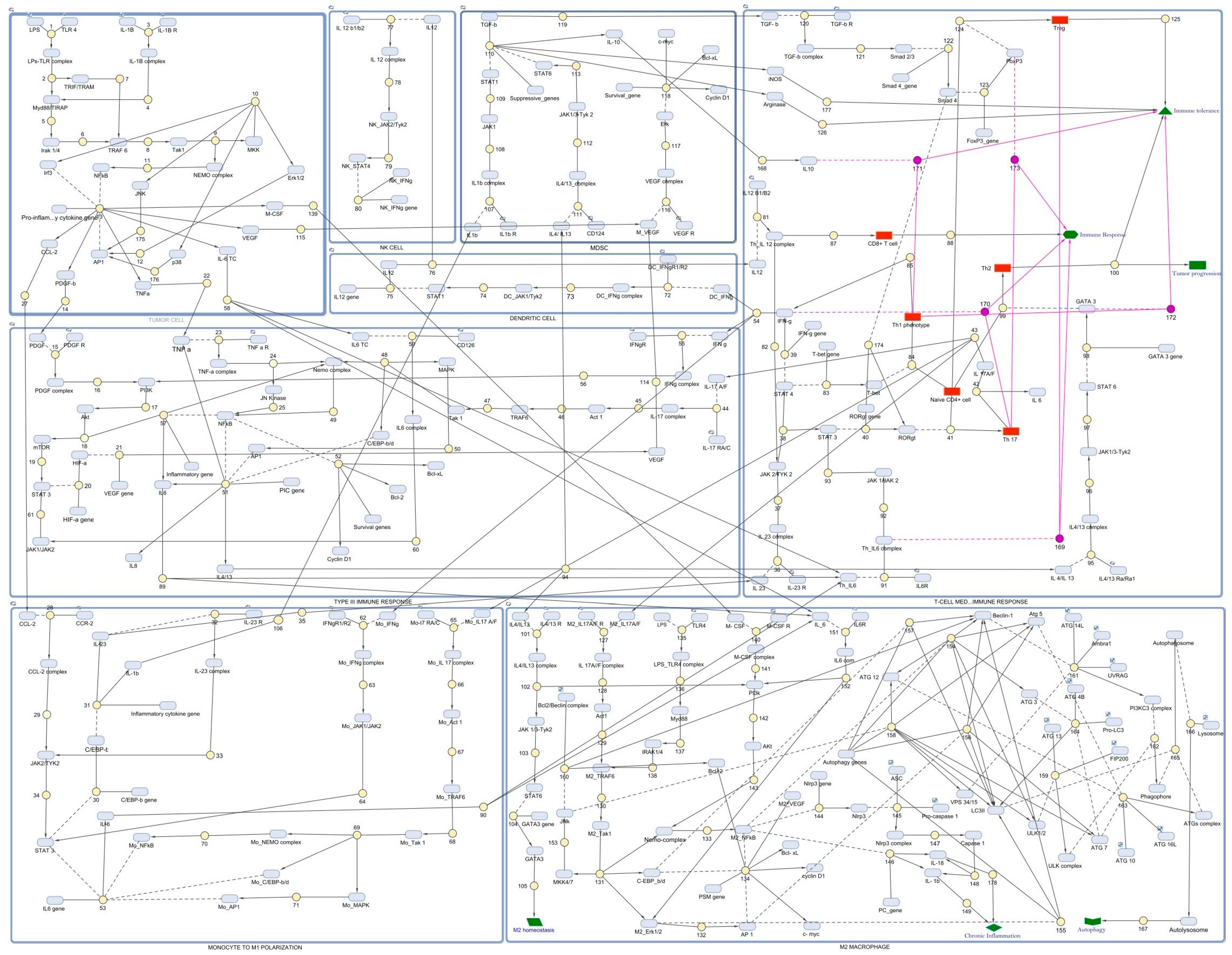
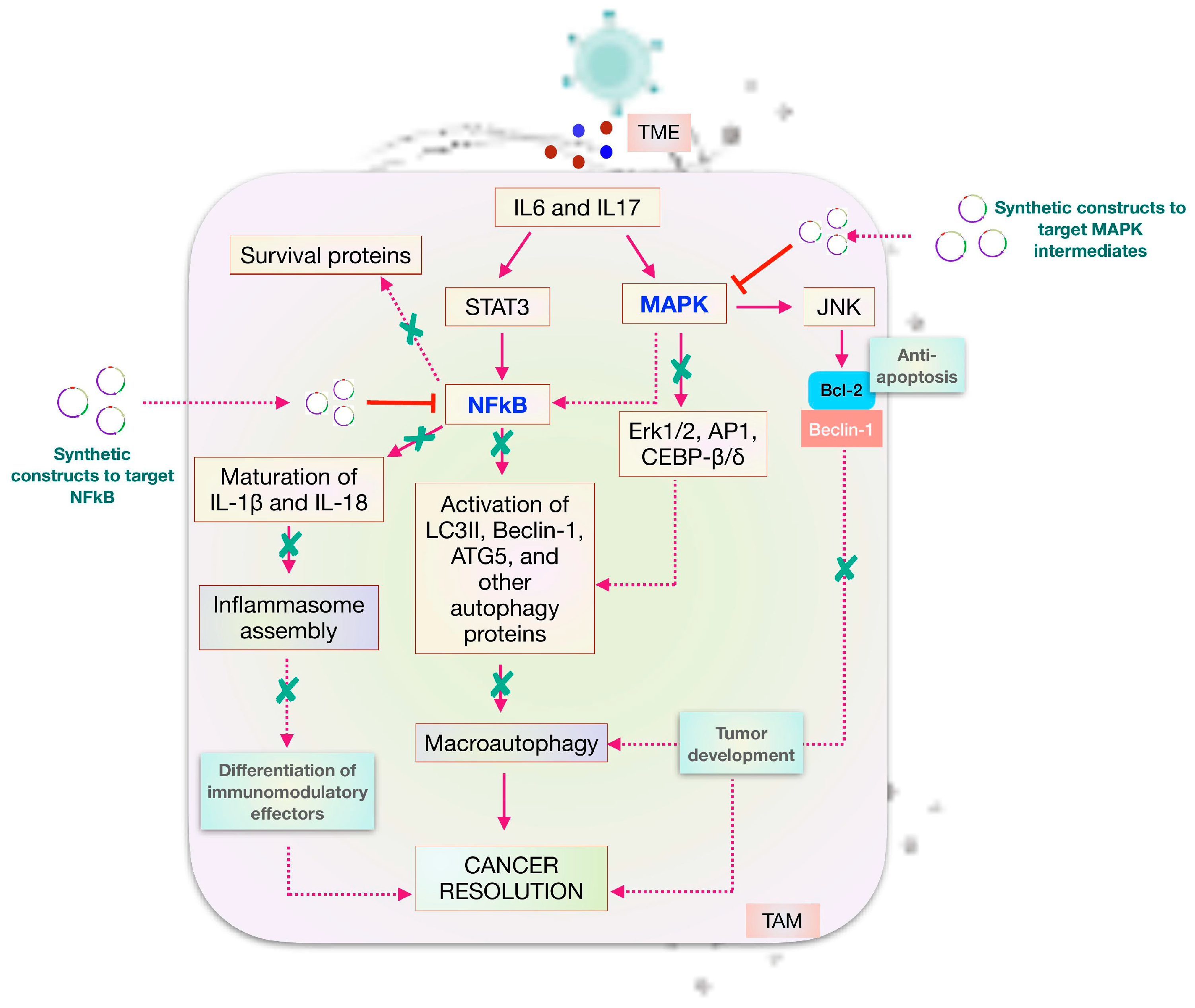
2.1. Reconstructed Mathematical Model and Simulation
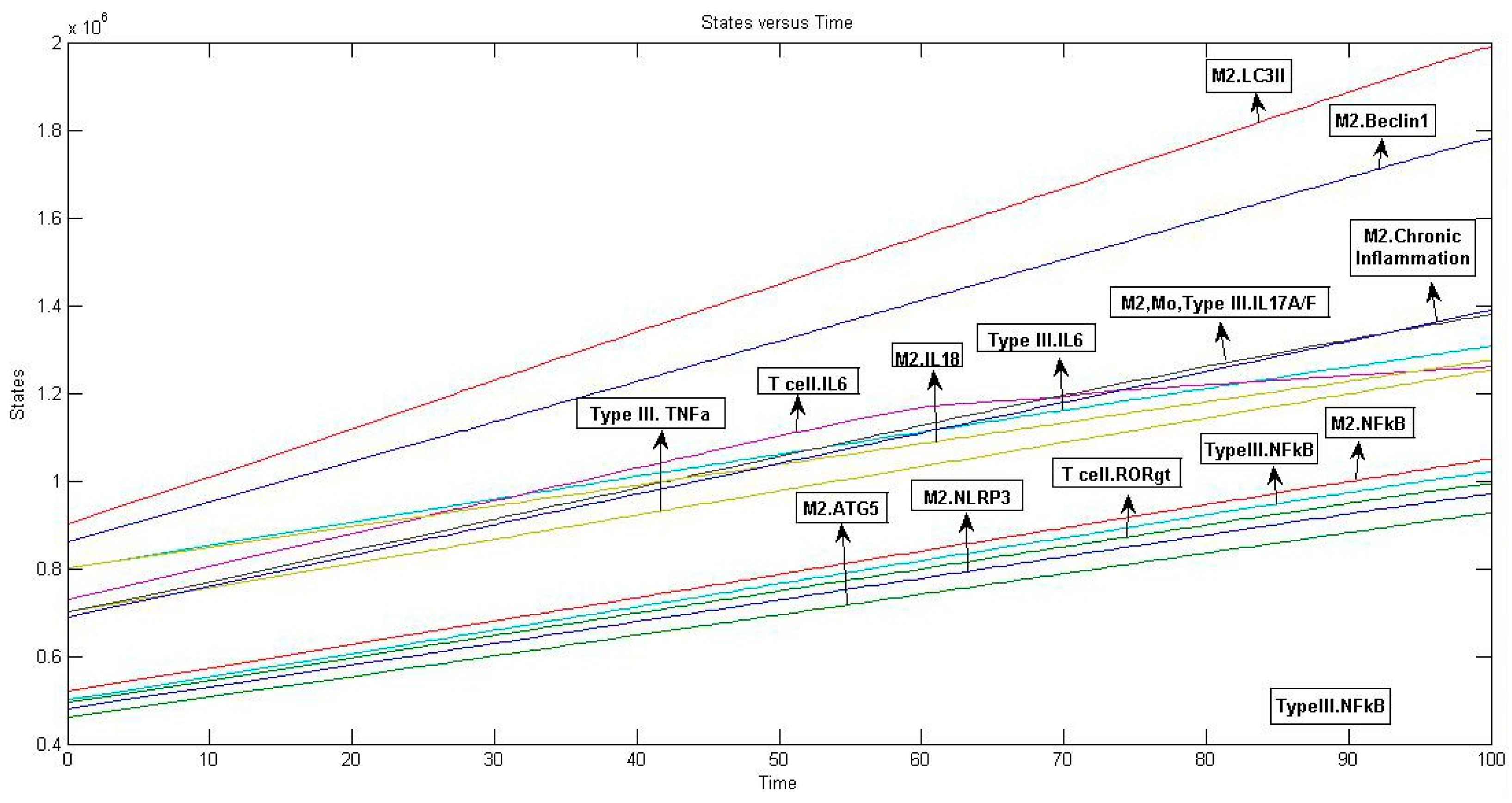
2.2. Triggered Event and Analysis
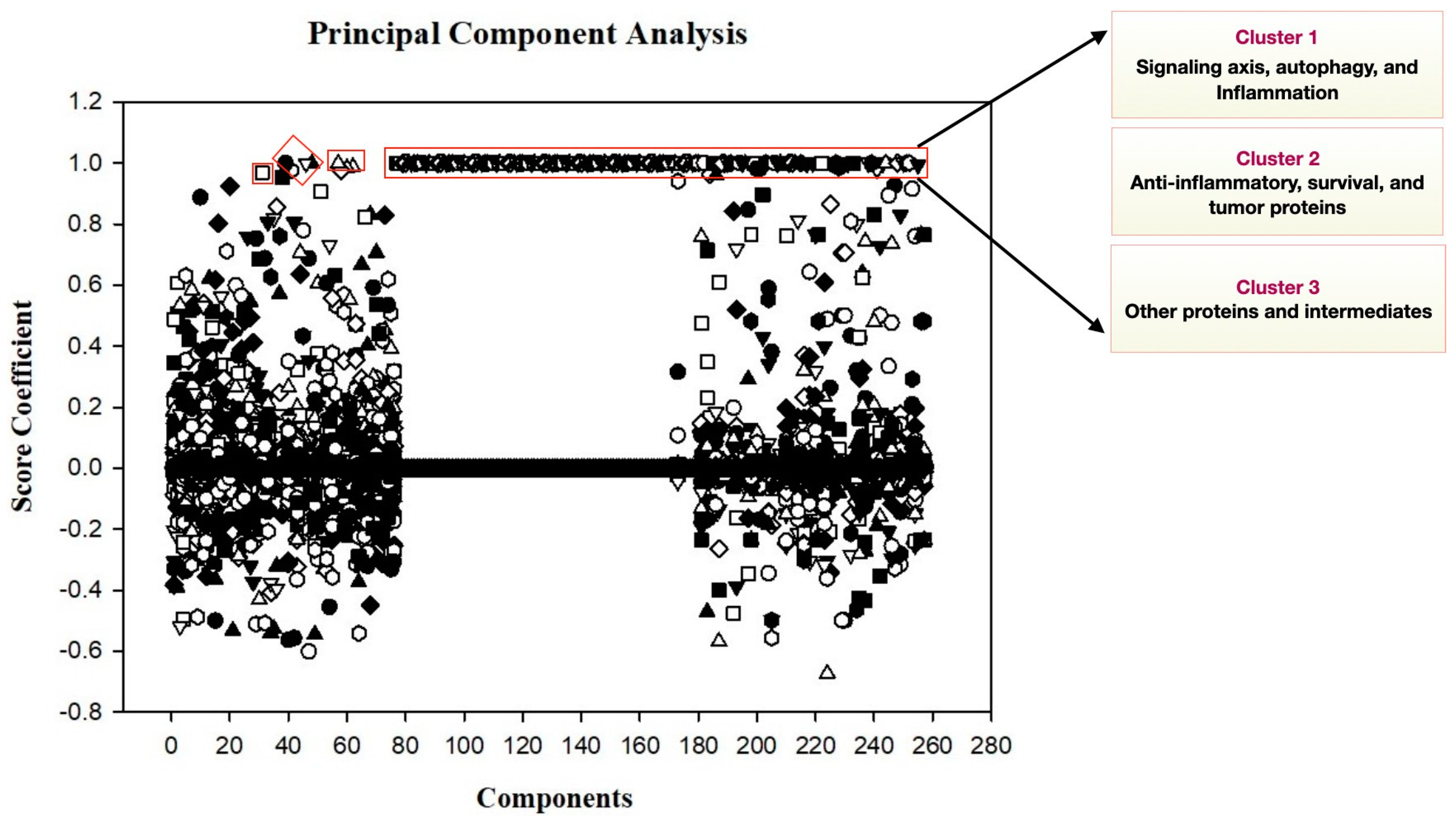
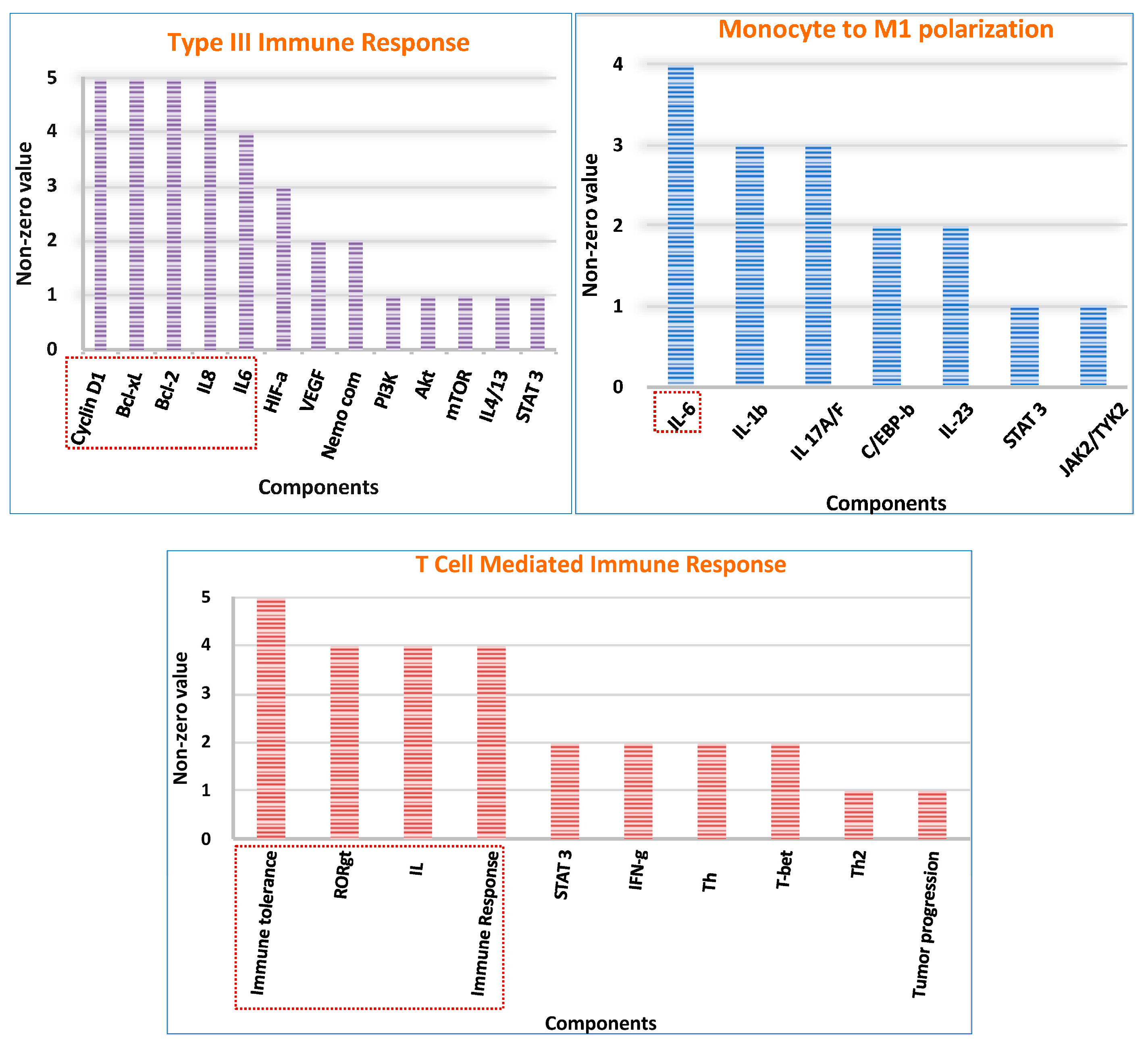
2.3. Principal Components and Analysis to Discern Crucial Elements
2.4. Flux Balance Analysis
2.5. Model Reduction
2.6. Network Crosstalk Score Analysis
3. Discussion
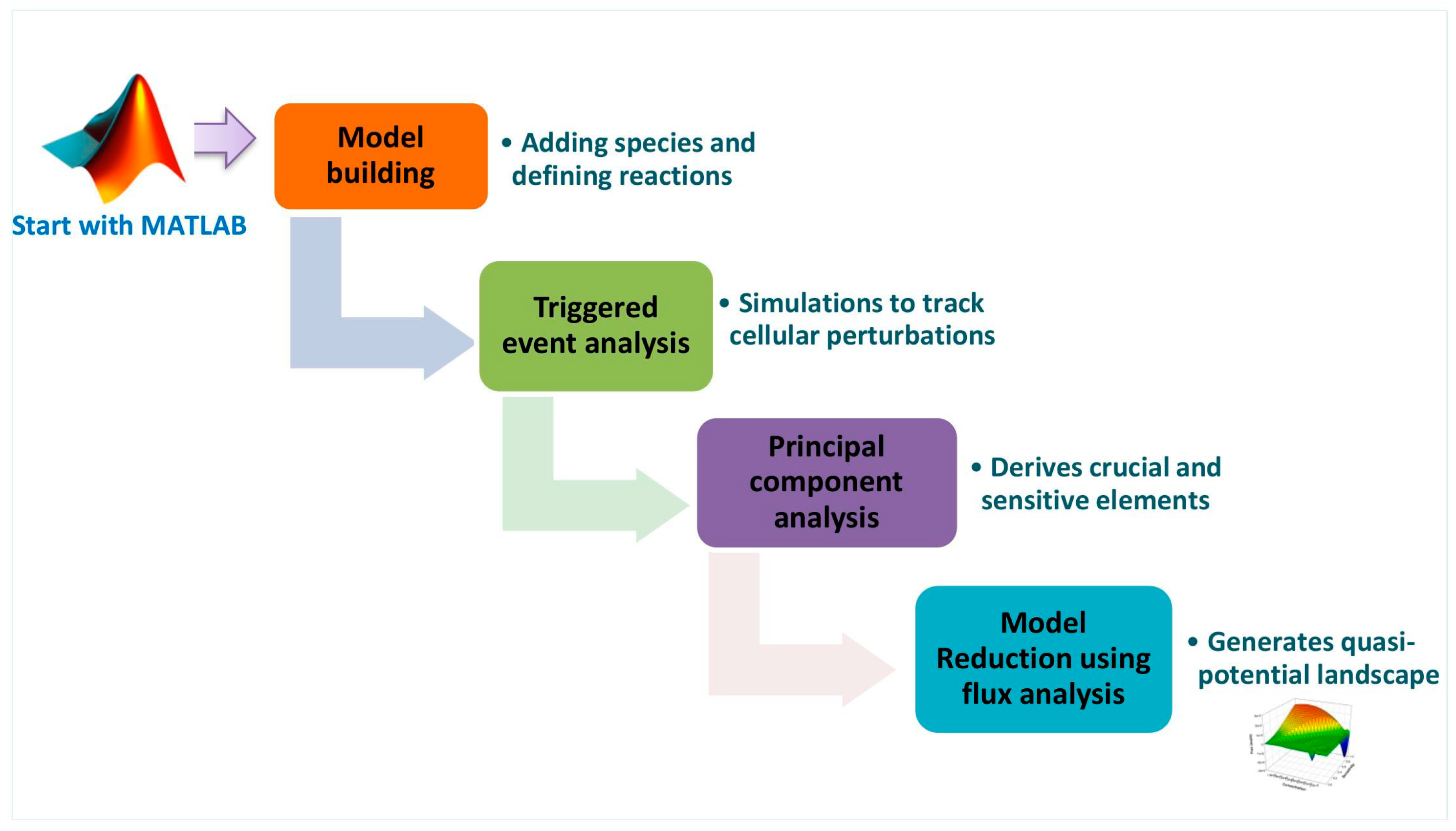
4. Methodology
4.1. Data Collection
4.2. Reconstruction of Mathematical Model for IL-6/IL-17 Axis and Autophagic Pathway
4.3. Event Analysis
4.4. Sensitivity Analysis
4.5. Principal Component Analysis
4.6. Flux Analysis
4.7. Model Reduction
4.8. Network Crosstalk Score
5. Future Perspectives
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AP1 | Activating Protein 1 |
| BSF-2 | B-cell Stimulating Factor-2 |
| CAF | Cancer-Associated Fibroblast |
| CEBP-β/δ | CCAAT/enhancer-binding protein beta/delta |
| CCL2 | Chemokine (C-C motif) ligand 2 |
| CCR2 | C-C chemokine receptor type 2 |
| DC | Dendritic Cell |
| EMT | Epithelial-to-Mesenchymal Transition |
| Erk1/2 | Extracellular signal-regulated protein kinases |
| Hif-1α | Hypoxia-inducible factor-1α |
| HIV | Human Immunodeficiency Virus |
| IFNγ | Interferon-gamma |
| IFNγR | Interferon-gamma Receptor |
| IL | Interleukin |
| iNOS | inducible Nitric Oxide Synthase |
| JNK | Janus Kinase |
| LPS | Lipopolysaccharide |
| MAPK | Mitogen-Activated Protein Kinase |
| MATLAB | MATrix LABoratory |
| MCSF | Macrophage Colony-Stimulating Factor |
| MCSFR | Macrophage Colony-Stimulating Factor Receptor |
| MDSC | Myeloid-Derived suppressor Cell |
| Mo | Monocytes |
| MR | Model Reduction |
| Myd88 | Myeloid Differentiation primary response 88 |
| NDF | Numerical Differentiation Formula |
| NFkB | Nuclear Factor kappa B |
| NK | Natural Killer |
| NLRP3 | Nucleotide-binding domain, leucine-rich containing family, pyrin domain– containing-3 |
| NSCLC | Non-Small Cell Lung Cancer |
| ODE | Ordinary Differential Equation |
| PC | Principal Component |
| PCA | Principal Component Analysis |
| PDGF | Platelet-Derived Growth Factor |
| PDGFR | Platelet-Derived Growth Factor Receptor |
| PIC | Pro-Inflammatory Cytokine gene |
| PSM | Proliferation, Survival, and Migration |
| RORγt | RAR-related orphan receptor gamma t |
| SBML | Systems Biology Markup Language |
| TAM | Tumor-associated Macrophages |
| TC | Tumor Cell |
| TGFβ | Transforming Growth Factor-beta |
| TGFβR | Transforming Growth Factor-beta Receptor |
| Th | T-helper |
| TME | Tumor microenvironment |
| TNFα | Tumor necrosis factor- alpha |
| TNFαR | Tumor necrosis factor- alpha Receptor |
| TLR | Toll-like Receptor |
| Treg | T-regulatory cell |
| VEGF | Vascular Endothelial Growth Factor |
| VEGFR | Vascular Endothelial Growth Factor Receptor |
References
- Ashrafi, A.; Akter, Z.; Modareszadeh, P.; Modareszadeh, P.; Berisha, E.; Alemi, P.S.; Chacon Castro, M.D.C.; Deese, A.R.; Zhang, L. Current Landscape of Therapeutic Resistance in Lung Cancer and Promising Strategies to Overcome Resistance. Cancers 2022, 14, 4562. [Google Scholar] [CrossRef]
- Bel’skaya, L.V.; Loginova, A.I.; Sarf, E.A. Pro-Inflammatory and Anti-Inflammatory Salivary Cytokines in Breast Cancer: Relationship with Clinicopathological Characteristics of the Tumor. Curr. Issues Mol. Biol. 2022, 44, 4676–4691. [Google Scholar] [CrossRef]
- Hirano, T. IL-6 in inflammation, autoimmunity and cancer. Int. Immunol. 2021, 33, 127–148. [Google Scholar] [CrossRef]
- Kuen, D.S.; Kim, B.S.; Chung, Y. IL-17-Producing Cells in Tumor Immunity: Friends or Foes? Immune Netw. 2020, 20, e6. [Google Scholar] [CrossRef]
- Wu, F.; Xu, J.; Huang, Q.; Han, J.; Duan, L.; Fan, J.; Lv, Z.; Guo, M.; Hu, G.; Chen, L.; et al. The Role of Interleukin-17 in Lung Cancer. Mediat. Inflamm. 2016, 2016, 8494079. [Google Scholar] [CrossRef]
- Hu, F.; Song, D.; Yan, Y.; Huang, C.; Shen, C.; Lan, J.; Chen, Y.; Liu, A.; Wu, Q.; Sun, L.; et al. IL-6 regulates autophagy and chemotherapy resistance by promoting BECN1 phosphorylation. Nat. Commun. 2021, 12, 3651. [Google Scholar] [CrossRef]
- Orosz, L.; Papanicolaou, E.G.; Seprényi, G.; Megyeri, K. IL-17A and IL-17F induce autophagy in RAW 264.7 macrophages. Biomed. Pharmacother. 2016, 77, 129–134. [Google Scholar] [CrossRef]
- Khilwani, R.; Singh, S. Systems Biology and Cytokines Potential Role in Lung Cancer Immunotherapy Targeting Autophagic Axis. Biomedicines 2023, 11, 2706. [Google Scholar] [CrossRef]
- Kishimoto, T. Interleukin-6: Discovery of a pleiotropic cytokine. Arthritis Res. Ther. 2006, 8 (Suppl. S2), S2. [Google Scholar] [CrossRef]
- Hirano, T. Interleukin 6 in autoimmune and inflammatory diseases: A personal memoir. Proc. Jpn. Academy. Ser. B Phys. Biol. Sci. 2010, 86, 717–730. [Google Scholar] [CrossRef]
- Kimura, A.; Kishimoto, T. IL-6: Regulator of Treg/Th17 balance. Eur. J. Immunol. 2010, 40, 1830–1835. [Google Scholar] [CrossRef]
- Hunter, C.A.; Jones, S.A. IL-6 as a keystone cytokine in health and disease. Nat. Immunol. 2015, 16, 448–457. [Google Scholar] [CrossRef]
- Aliyu, M.; Zohora, F.T.; Anka, A.U.; Ali, K.; Maleknia, S.; Saffarioun, M.; Azizi, G. Interleukin-6 cytokine: An overview of the immune regulation, immune dysregulation, and therapeutic approach. Int. Immunopharmacol. 2022, 111, 109130. [Google Scholar] [CrossRef]
- Kawano, M.; Hirano, T.; Matsuda, T.; Taga, T.; Horii, Y.; Iwato, K.; Asaoku, H.; Tang, B.; Tanabe, O.; Tanaka, H.; et al. Autocrine generation and requirement of BSF-2/IL-6 for human multiple myelomas. Nature 1988, 332, 83–85. [Google Scholar] [CrossRef]
- Johnson, D.E.; O’Keefe, R.A.; Grandis, J.R. Targeting the IL-6/JAK/STAT3 signalling axis in cancer. Nat. Rev. Clin. Oncol. 2018, 15, 234–248. [Google Scholar] [CrossRef]
- Qu, Z.; Sun, F.; Zhou, J.; Li, L.; Shapiro, S.D.; Xiao, G. Interleukin-6 Prevents the Initiation but Enhances the Progression of Lung Cancer. Cancer Res. 2015, 75, 3209–3215. [Google Scholar] [CrossRef]
- Weber, R.; Groth, C.; Lasser, S.; Arkhypov, I.; Petrova, V.; Altevogt, P.; Utikal, J.; Umansky, V. IL-6 as a major regulator of MDSC activity and possible target for cancer immunotherapy. Cell. Immunol. 2021, 359, 104254. [Google Scholar] [CrossRef]
- Masjedi, A.; Hashemi, V.; Hojjat-Farsangi, M.; Ghalamfarsa, G.; Azizi, G.; Yousefi, M.; Jadidi-Niaragh, F. The significant role of interleukin-6 and its signaling pathway in the immunopathogenesis and treatment of breast cancer. Biomed. Pharmacother. 2018, 108, 1415–1424. [Google Scholar] [CrossRef]
- Kumari, N.; Dwarakanath, B.S.; Das, A.; Bhatt, A.N. Role of interleukin-6 in cancer progression and therapeutic resistance. Tumour Biol. J. Int. Soc. Oncodev. Biol. Med. 2016, 37, 11553–11572. [Google Scholar] [CrossRef]
- Jin, J.O.; Han, X.; Yu, Q. Interleukin-6 induces the generation of IL-10-producing Tr1 cells and suppresses autoimmune tissue inflammation. J. Autoimmun. 2013, 40, 28–44. [Google Scholar] [CrossRef]
- Zhao, C.; Zeng, N.; Zhou, X.; Tan, Y.; Wang, Y.; Zhang, J.; Wu, Y.; Zhang, Q. CAA-derived IL-6 induced M2 macrophage polarization by activating STAT3. BMC Cancer 2023, 23, 392. [Google Scholar] [CrossRef]
- Boaru, S.G.; Borkham-Kamphorst, E.; Van de Leur, E.; Lehnen, E.; Liedtke, C.; Weiskirchen, R. NLRP3 inflammasome expression is driven by NF-κB in cultured hepatocytes. Biochem. Biophys. Res. Commun. 2015, 458, 700–706. [Google Scholar] [CrossRef]
- Zhao, J.; Chen, X.; Herjan, T.; Li, X. The role of interleukin-17 in tumor development and progression. J. Exp. Med. 2020, 217, e20190297. [Google Scholar] [CrossRef]
- Kuwabara, T.; Ishikawa, F.; Kondo, M.; Kakiuchi, T. The Role of IL-17 and Related Cytokines in Inflammatory Autoimmune Diseases. Mediat. Inflamm. 2017, 2017, 3908061. [Google Scholar] [CrossRef]
- Curtis, M.M.; Way, S.S. Interleukin-17 in host defence against bacterial, mycobacterial and fungal pathogens. Immunology 2009, 126, 177–185. [Google Scholar] [CrossRef]
- Wang, Y.H.; Liu, Y.J. The IL-17 cytokine family and their role in allergic inflammation. Curr. Opin. Immunol. 2008, 20, 697–702. [Google Scholar] [CrossRef]
- Yuan, S.; Zhang, S.; Zhuang, Y.; Zhang, H.; Bai, J.; Hou, Q. Interleukin-17 Stimulates STAT3-Mediated Endothelial Cell Activation for Neutrophil Recruitment. Cell. Physiol. Biochem. 2015, 36, 2340–2356. [Google Scholar] [CrossRef]
- Cheng, S.; Shao, Z.; Liu, X.; Guo, L.; Zhang, X.; Na, Q.; Chen, X.; Ma, Y.; Zheng, J.; Song, B.; et al. Interleukin 17A polymorphism elevates gene expression and is associated with increased risk of nonsmall cell lung cancer. DNA Cell Biol. 2015, 34, 63–68. [Google Scholar] [CrossRef]
- Liao, T.; Fan, J.; Lv, Z.; Xu, J.; Wu, F.; Yang, G.; Huang, Q.; Guo, M.; Hu, G.; Zhou, M.; et al. Comprehensive genomic and prognostic analysis of the IL-17 family genes in lung cancer. Mol. Med. Rep. 2019, 19, 4906–4918. [Google Scholar] [CrossRef]
- Xu, B.; Guenther, J.F.; Pociask, D.A.; Wang, Y.; Kolls, J.K.; You, Z.; Chandrasekar, B.; Shan, B.; Sullivan, D.E.; Morris, G.F. Promotion of lung tumor growth by interleukin-17. Am. J. Physiol. Lung Cell. Mol. Physiol. 2014, 307, L497–L508. [Google Scholar] [CrossRef]
- Liu, W.; Xin, M.; Li, Q.; Sun, L.; Han, X.; Wang, J. IL-17A Promotes the Migration, Invasion and the EMT Process of Lung Cancer Accompanied by NLRP3 Activation. BioMed Res. Int. 2022, 2022, 7841279. [Google Scholar] [CrossRef]
- Liu, L.; Liu, R.; Wei, C.; Li, D.; Gao, X. The role of IL-17 in lung cancer growth. Cytokine 2023, 169, 156265. [Google Scholar] [CrossRef]
- Gu, J.; Liu, Y.; Xie, B.; Ye, P.; Huang, J.; Lu, Z. Roles of toll-like receptors: From inflammation to lung cancer progression. Biomed. Rep. 2018, 8, 126–132. [Google Scholar] [CrossRef]
- Kawai, T.; Takeuchi, O.; Fujita, T.; Inoue, J.-I.; Mühlradt, P.F.; Sato, S.; Hoshino, K.; Akira, S. Lipopolysaccharide Stimulates the MyD88-Independent Pathway and Results in Activation of IFN-Regulatory Factor 3 and the Expression of a Subset of Lipopolysaccharide-Inducible Genes. J. Immunol. 2001, 167, 5887–5894. [Google Scholar] [CrossRef]
- Tian, J.; Zhao, Y.; Wang, L.; Li, L. Role of TLR4/MyD88/NF-κB signaling in heart and liver-related complications in a rat model of type 2 diabetes mellitus. J. Int. Med. Res. 2021, 49, 300060521997590. [Google Scholar] [CrossRef]
- Wang, L.; Yu, K.; Zhang, X.; Yu, S. Dual functional roles of the MyD88 signaling in colorectal cancer development. Biomed. Pharmacother. 2018, 107, 177–184. [Google Scholar] [CrossRef]
- Edwardson, D.W.; Boudreau, J.; Mapletoft, J.; Lanner, C.; Kovala, A.T.; Parissenti, A.M. Inflammatory cytokine production in tumor cells upon chemotherapy drug exposure or upon selection for drug resistance. PLoS ONE 2017, 12, e0183662. [Google Scholar] [CrossRef]
- Kadomoto, S.; Izumi, K.; Mizokami, A. Roles of CCL2-CCR2 Axis in the Tumor Microenvironment. Int. J. Mol. Sci. 2021, 22, 8530. [Google Scholar] [CrossRef]
- Chen, Y.; Mathy, N.W.; Lu, H. The role of VEGF in the diagnosis and treatment of malignant pleural effusion in patients with non-small cell lung cancer (Review). Mol. Med. Rep. 2018, 17, 8019–8030. [Google Scholar] [CrossRef]
- Zhang, Y.; Manouchehri Doulabi, E.; Herre, M.; Cedervall, J.; Qiao, Q.; Miao, Z.; Hamidi, A.; Hellman, L.; Kamali-Moghaddam, M.; Olsson, A.K. Platelet-Derived PDGFB Promotes Recruitment of Cancer-Associated Fibroblasts, Deposition of Extracellular Matrix and Tgfβ Signaling in the Tumor Microenvironment. Cancers 2022, 14, 1947. [Google Scholar] [CrossRef]
- Chockalingam, S.; Ghosh, S.S. Macrophage colony-stimulating factor and cancer: A review. Tumour Biol. J. Int. Soc. Oncodev. Biol. Med. 2014, 35, 10635–10644. [Google Scholar] [CrossRef]
- Wang, H.; Yin, Y.; Li, W.; Zhao, X.; Yu, Y.; Zhu, J.; Qin, Z.; Wang, Q.; Wang, K.; Lu, W.; et al. Over-expression of PDGFR-β promotes PDGF-induced proliferation, migration, and angiogenesis of EPCs through PI3K/Akt signaling pathway. PLoS ONE 2012, 7, e30503. [Google Scholar] [CrossRef]
- Turner, M.D.; Nedjai, B.; Hurst, T.; Pennington, D.J. Cytokines and chemokines: At the crossroads of cell signalling and inflammatory disease. Biochim. Biophys. Acta 2014, 1843, 2563–2582. [Google Scholar] [CrossRef]
- Jorgovanovic, D.; Song, M.; Wang, L.; Zhang, Y. Roles of IFN-γ in tumor progression and regression: A review. Biomark. Res. 2020, 8, 49. [Google Scholar] [CrossRef]
- Song, Y.; Yang, J.M. Role of interleukin (IL)-17 and T-helper (Th)17 cells in cancer. Biochem. Biophys. Res. Commun. 2017, 493, 1–8. [Google Scholar] [CrossRef]
- Xu, M.; Wang, Y.; Xia, R.; Wei, Y.; Wei, X. Role of the CCL2-CCR2 signalling axis in cancer: Mechanisms and therapeutic targeting. Cell Prolif. 2021, 54, e13115. [Google Scholar] [CrossRef]
- Briukhovetska, D.; Dörr, J.; Endres, S.; Libby, P.; Dinarello, C.A.; Kobold, S. Interleukins in cancer: From biology to therapy. Nat. Rev. Cancer 2021, 21, 481–499. [Google Scholar] [CrossRef]
- Pastuszak-Lewandoska, D.; Domańska-Senderowska, D.; Antczak, A.; Kordiak, J.; Górski, P.; Czarnecka, K.H.; Migdalska-Sęk, M.; Nawrot, E.; Kiszałkiewicz, J.M.; Brzeziańska-Lasota, E. The Expression Levels of IL-4/IL-13/STAT6 Signaling Pathway Genes and SOCS3 Could Help to Differentiate the Histopathological Subtypes of Non-Small Cell Lung Carcinoma. Mol. Diagn. Ther. 2018, 22, 621–629. [Google Scholar] [CrossRef]
- Liu, Y.; Gao, X.; Miao, Y.; Wang, Y.; Wang, H.; Cheng, Z.; Wang, X.; Jing, X.; Jia, L.; Dai, L.; et al. NLRP3 regulates macrophage M2 polarization through up-regulation of IL-4 in asthma. Biochem. J. 2018, 475, 1995–2008. [Google Scholar] [CrossRef]
- Chen, P.; Cescon, M.; Bonaldo, P. Autophagy-mediated regulation of macrophages and its applications for cancer. Autophagy 2014, 10, 192–200. [Google Scholar] [CrossRef]
- Singh, N.; Baby, D.; Rajguru, J.P.; Patil, P.B.; Thakkannavar, S.S.; Pujari, V.B. Inflammation and cancer. Ann. Afr. Med. 2019, 18, 121–126. [Google Scholar] [CrossRef]
- Peng, L.; Zhong, J.; Xiao, Y.; Wang, B.; Li, S.; Deng, Y.; He, D.; Yuan, J. Therapeutic effects of an anti-IL-6 antibody in fungal keratitis: Macrophage inhibition and T cell subset regulation. Int. Immunopharmacol. 2020, 85, 106649. [Google Scholar] [CrossRef] [PubMed]
- Sahu, U.; Biswas, D.; Prajapati, V.K.; Singh, A.K.; Samant, M.; Khare, P. Interleukin-17—A multifaceted cytokine in viral infections. J. Cell. Physiol. 2021, 236, 8000–8019. [Google Scholar] [CrossRef] [PubMed]
- Grivennikov, S.I.; Greten, F.R.; Karin, M. Immunity, inflammation, and cancer. Cell 2010, 140, 883–899. [Google Scholar] [CrossRef] [PubMed]
- Vijayan, K.K.V.; Karthigeyan, K.P.; Tripathi, S.P.; Hanna, L.E. Pathophysiology of CD4+ T-Cell Depletion in HIV-1 and HIV-2 Infections. Front. Immunol. 2017, 8, 580. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.W.; Zhou, S.F. Inflammation, cytokines, the IL-17/IL-6/STAT3/NF-κB axis, and tumorigenesis. Drug Des. Dev. Ther. 2015, 9, 2941–2946. [Google Scholar] [CrossRef]
- Papin, J.A.; Hunter, T.; Palsson, B.O.; Subramaniam, S. Reconstruction of cellular signalling networks and analysis of their properties. Nat. Rev. Mol. Cell Biol. 2005, 6, 99–111. [Google Scholar] [CrossRef]
- Jawale, D.; Khandibharad, S.; Singh, S. Decoding systems immunological model of sphingolipids with IL-6/IL-17/IL-23 axes in L. major infection. Biochim. Et Biophys. Acta. Mol. Cell Biol. Lipids 2023, 1868, 159261. [Google Scholar] [CrossRef]
- Khandibharad, S.; Singh, S. Computational System Level Approaches for Discerning Reciprocal Regulation of IL10 and IL12 in Leishmaniasis. Front. Genet. 2022, 12, 784664. [Google Scholar] [CrossRef]
- Mol, M.; Patole, M.S.; Singh, S. Immune signal transduction in leishmaniasis from natural to artificial systems: Role of feedback loop insertion. Biochim. Et Biophys. Acta 2014, 1840, 71–79. [Google Scholar] [CrossRef]
- Soni, B.; Singh, S. COVID-19 co-infection mathematical model as guided through signaling structural framework. Comput. Struct. Biotechnol. J. 2021, 19, 1672–1683. [Google Scholar] [CrossRef] [PubMed]
- Zi, Z. Sensitivity analysis approaches applied to systems biology models. IET Syst. Biol. 2011, 5, 336–346. [Google Scholar] [CrossRef] [PubMed]
- Jolliffe, I.T.; Cadima, J. Principal component analysis: A review and recent developments. Philos. Trans. Ser. A Math. Phys. Eng. Sci. 2016, 374, 20150202. [Google Scholar] [CrossRef] [PubMed]
- Elhaik, E. Principal Component Analyses (PCA)-based findings in population genetic studies are highly biased and must be reevaluated. Sci. Rep. 2022, 12, 14683. [Google Scholar] [CrossRef] [PubMed]
- Anand, S.; Mukherjee, K.; Padmanabhan, P. An insight to flux-balance analysis for biochemical networks. Biotechnol. Genet. Eng. Rev. 2020, 36, 32–55. [Google Scholar] [CrossRef] [PubMed]
- Rao, S.; van der Schaft, A.; van Eunen, K.; Bakker, B.M.; Jayawardhana, B. A model reduction method for biochemical reaction networks. BMC Syst. Biol. 2014, 8, 52. [Google Scholar] [CrossRef] [PubMed]
- Liu, G.; Swihart, M.T.; Neelamegham, S. Sensitivity, principal component and flux analysis applied to signal transduction: The case of epidermal growth factor mediated signaling. Bioinformatics 2004, 21, 1194–1202. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ali Eshtewy, N.; Scholz, L. Model reduction for kinetic models of biological systems. Symmetry 2020, 12, 863. [Google Scholar] [CrossRef]
- Vert, G.; Chory, J. Crosstalk in cellular signaling: Background noise or the real thing? Dev. Cell 2011, 21, 985–991. [Google Scholar] [CrossRef]
- Zielinski, R.; Przytycki, P.F.; Zheng, J.; Zhang, D.; Przytycka, T.M.; Capala, J. The crosstalk between EGF, IGF, and Insulin cell signaling pathways-- computational and experimental analysis. BMC Syst. Biol. 2009, 3, 88. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions, and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions, or products referred to in the content. |


| S. No | Model Characteristics | Total Parameters |
|---|---|---|
| 1 | Species | 257 |
| 2 | Reactions involved | 175 |
| 3 | Kinetic rate laws | 335 |
| 4 | Triggered events | 5 |
| S. No. | Reactions | Flux (mol/s) |
|---|---|---|
| 1 | [T-CELL MEDIATED IMMUNE RESPONSE].[Th 17] -> [T-CELL MEDIATED IMMUNE RESPONSE].[IL -17A/F] + [T-CELL MEDIATED IMMUNE RESPONSE].[IL -6] | 7542.65 |
| 2 | [M2 MACROPHAGE].[Caspase 1] -> [M2MACROPHAGE].[IL-1b] + [M2MACROPHAGE].[IL-18] | 7458.54 |
| 3 | [T-CELL MEDIATED IMMUNE RESPONSE].[IL-17A/F] -> [TYPE III IMMUNE RESPONSE].[IL-17 A/F] + [MONOCYTE-TO-M1 POLARIZATION].[Mo_IL-17 A/F] + [M2 MACROPHAGE].[M2_IL-17A/F] | 6885.11 |
| 4 | [M2 MACROPHAGE].[Nlrp3 complex] -> [M2 MACROPHAGE].[Capase 1] | 6748.76 |
| 5 | [M2 MACROPHAGE].[Nemo complex] -> [M2 MACROPHAGE].M2_NFkB | 5357.28 |
| 6 | [TYPE III IMMUNE RESPONSE].[Nemo complex] -> [TYPE III IMMUNE RESPONSE].NFkB | 5155.21 |
| 7 | [T-CELL MEDIATED IMMUNE RESPONSE].[STAT 3] + [T-CELL MEDIATED IMMUNE RESPONSE].[RORgt gene] -> [T-CELL MEDIATED IMMUNE RESPONSE].RORgt + [T-CELL MEDIATED IMMUNE RESPONSE].[STAT 3] | 5078.57 |
| 8 | [M2 MACROPHAGE].M2_NFkB + [M2 MACROPHAGE].[Nlrp3 gene] -> [M2 MACROPHAGE].Nlrp3 + [M2 MACROPHAGE].M2_NFkB | 4979.32 |
| 9 | [M2 MACROPHAGE].PI3k -> [M2 MACROPHAGE].Akt | 4951.11 |
| 10 | [TYPE III IMMUNE RESPONSE].[IL-4/13] -> [T-CELL MEDIATED IMMUNE RESPONSE].[IL- 4/IL- 13] + [M2 MACROPHAGE].[IL-4/IL13] + MDSC.[IL-4/IL-13] | 4885.72 |
| S. No. | Effector Molecules | Modulated Subset | Model Outcome |
|---|---|---|---|
| 1 | IL-6 | Treg | Immune Response |
| 2 | GATA3 | Th1 phenotype | Immune Tolerance |
| 3 | IL-10 | Th1 phenotype | Immune Tolerance |
| 4 | IFNγ | Th17 cell | Immune Response |
| 5 | FoxP3 | Th17 cell | Immune Response |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Khilwani, R.; Singh, S. Traversing through the Mechanistic Event Analysis in IL-6 and IL-17 Signaling for a New Therapeutic Paradigm in NSCLC. Int. J. Mol. Sci. 2024, 25, 1216. https://doi.org/10.3390/ijms25021216
Khilwani R, Singh S. Traversing through the Mechanistic Event Analysis in IL-6 and IL-17 Signaling for a New Therapeutic Paradigm in NSCLC. International Journal of Molecular Sciences. 2024; 25(2):1216. https://doi.org/10.3390/ijms25021216
Chicago/Turabian StyleKhilwani, Riya, and Shailza Singh. 2024. "Traversing through the Mechanistic Event Analysis in IL-6 and IL-17 Signaling for a New Therapeutic Paradigm in NSCLC" International Journal of Molecular Sciences 25, no. 2: 1216. https://doi.org/10.3390/ijms25021216
APA StyleKhilwani, R., & Singh, S. (2024). Traversing through the Mechanistic Event Analysis in IL-6 and IL-17 Signaling for a New Therapeutic Paradigm in NSCLC. International Journal of Molecular Sciences, 25(2), 1216. https://doi.org/10.3390/ijms25021216






