MicroRNA Inhibiting Atheroprotective Proteins in Patients with Unstable Angina Comparing to Chronic Coronary Syndrome
Abstract
1. Introduction
2. Results
2.1. Baseline Characteristics
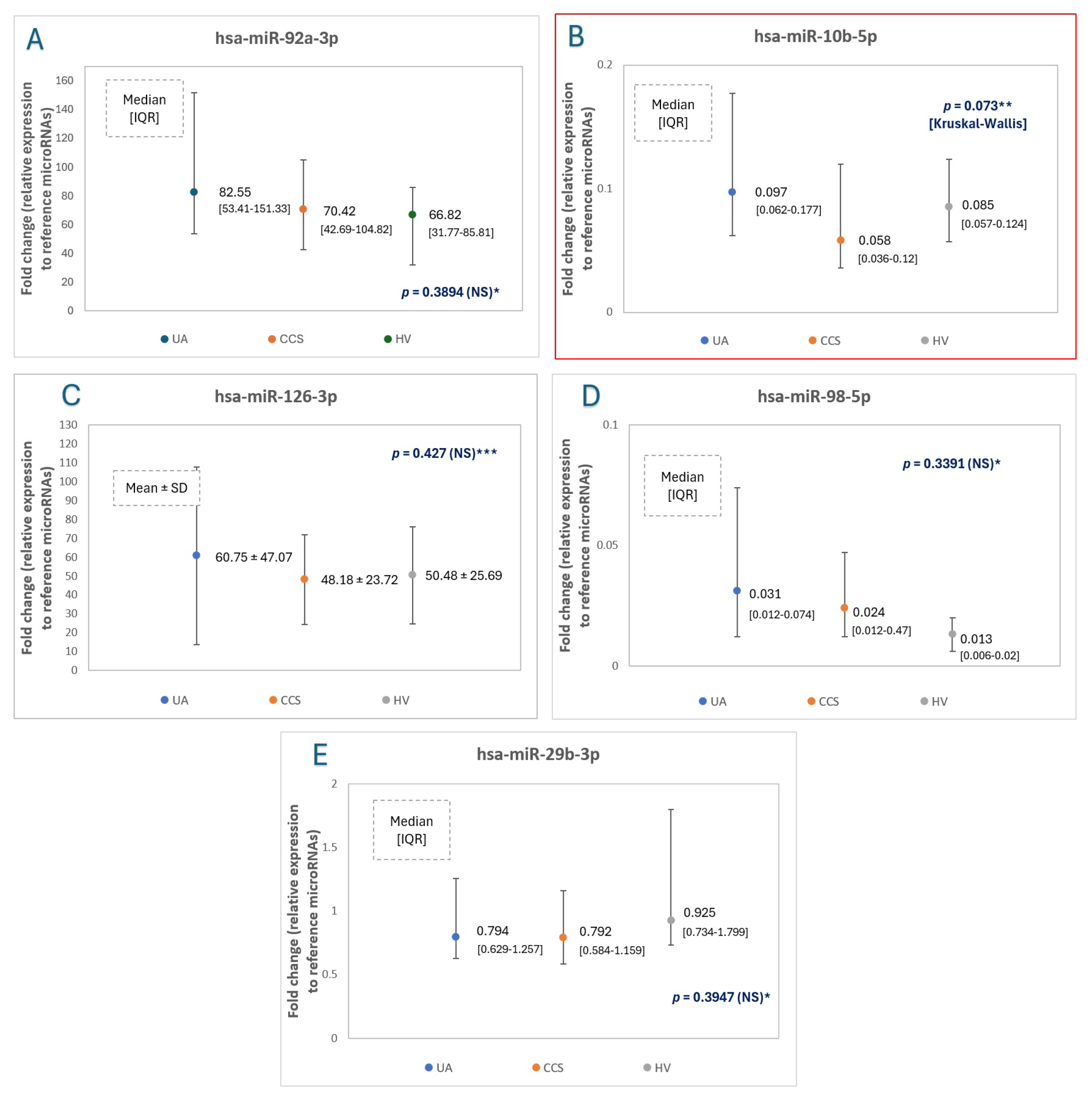
2.2. MicroRNA Expression Levels—The Main Comparison between Study Groups
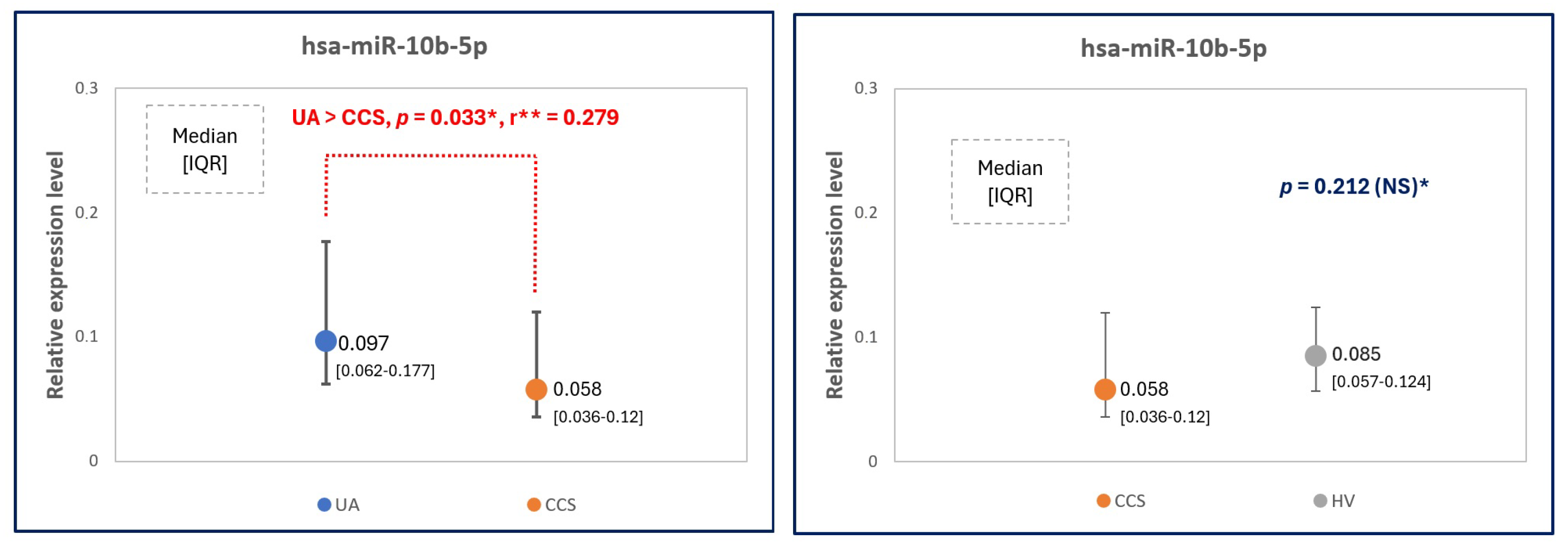
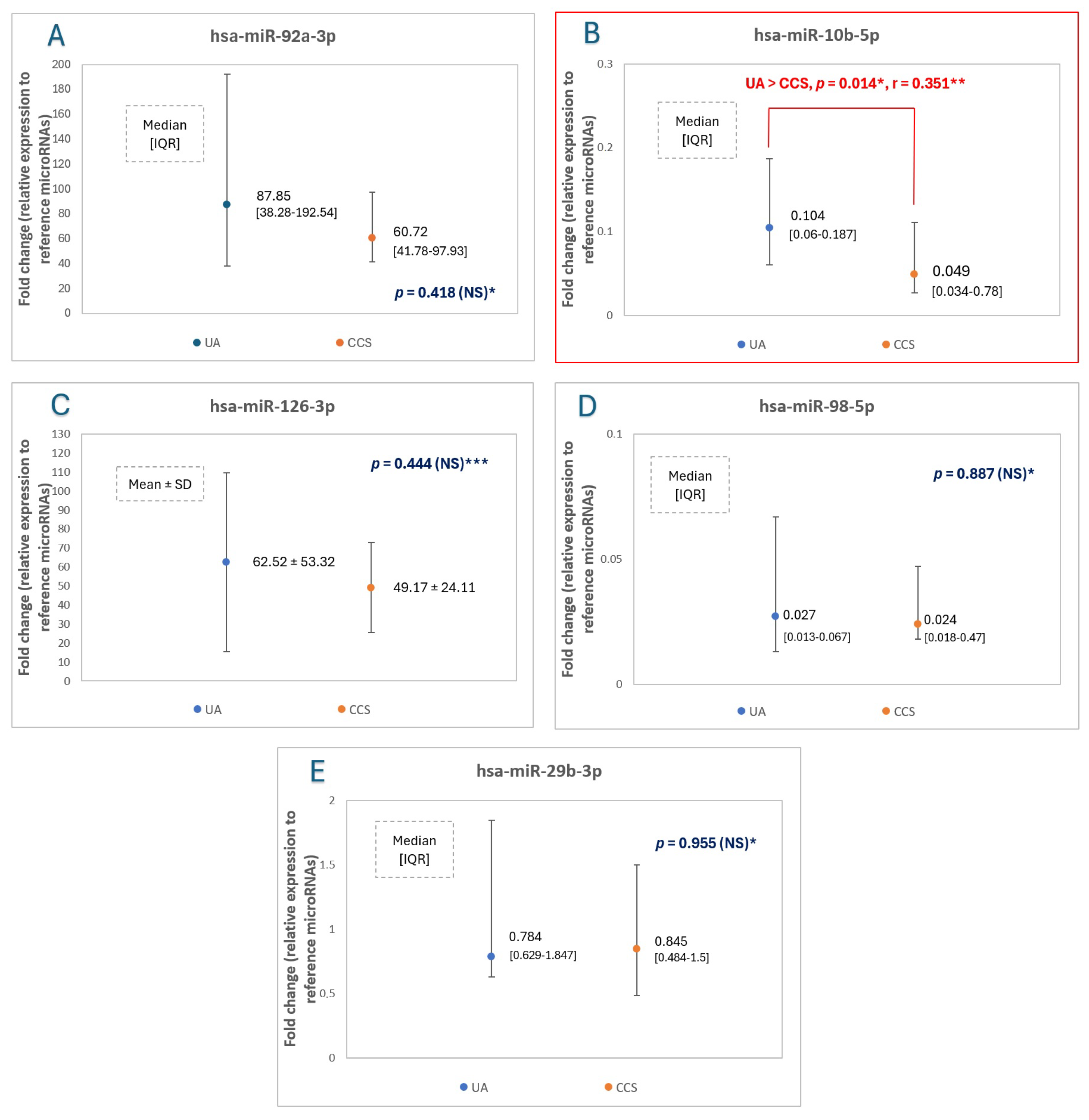
2.3. MicroRNA Expression Levels—Additional Comparison: Only Men Considered
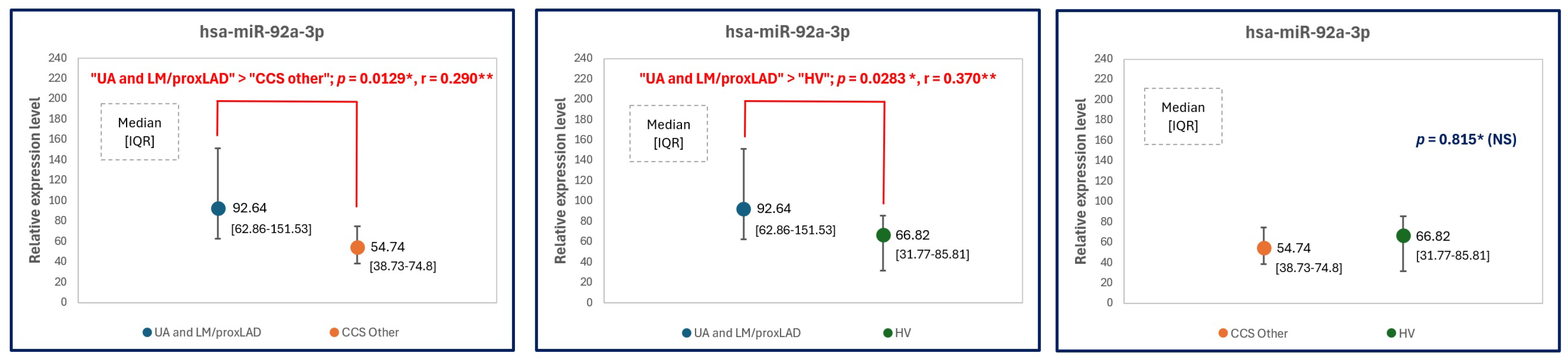
2.4. MicroRNA Expression Levels—Another Approach: Patients with Left Main and Proximal LAD
3. Materials and Methods
3.1. Study microRNAs
3.2. Study Population
3.3. Eligibility Criteria
3.4. Blood Samples
3.5. Micro-RNA
3.6. Statistical Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Khan, M.A.; Hashim, M.J.; Mustafa, H.; Baniyas, M.Y.; Al Suwaidi, S.; AlKatheeri, R.; Alblooshi, F.M.K.; Almatrooshi, M.; Alzaabi, M.E.H.; Al Darmaki, R.S.; et al. Global Epidemiology of Ischemic Heart Disease: Results from the Global Burden of Disease Study. Cureus 2020, 12, e9349. [Google Scholar] [CrossRef] [PubMed]
- Smitherman, T.C. Unstable angina pectoris: The first half century: Natural history, pathophysiology, and treatment. Am. J. Med. Sci. 1986, 292, 395–406. [Google Scholar] [CrossRef] [PubMed]
- Gargiulo, G.; Serino, F.; Esposito, G. Cardiovascular mortality in patients with acute and chronic coronary syndrome: Insights from the clinical evidence on ticagrelor. Eur. Rev. Med. Pharmacol. Sci. 2022, 26, 2524–2542. [Google Scholar] [CrossRef]
- Deckers, J.W. Classification of myocardial infarction and unstable angina: A re-assessment. Int. J. Cardiol. 2013, 167, 2387–2390. [Google Scholar] [CrossRef] [PubMed]
- Katz, D.; Gavin, M.C. Stable Ischemic Heart Disease. Ann. Intern. Med. 2019, 171, ITC17–ITC32. [Google Scholar] [CrossRef] [PubMed]
- Bentzon, J.F.; Otsuka, F.; Virmani, R.; Falk, E. Mechanisms of plaque formation and rupture. Circ. Res. 2014, 114, 1852–1866. [Google Scholar] [CrossRef]
- Jebari-Benslaiman, S.; Galicia-Garcia, U.; Larrea-Sebal, A.; Olaetxea, J.R.; Alloza, I.; Vandenbroeck, K.; Benito-Vicente, A.; Martin, C. Pathophysiology of Atherosclerosis. Int. J. Mol. Sci. 2022, 23, 3346. [Google Scholar] [CrossRef]
- Badimon, L.; Vilahur, G. Thrombosis formation on atherosclerotic lesions and plaque rupture. J. Intern. Med. 2014, 276, 618–632. [Google Scholar] [CrossRef] [PubMed]
- Silvestre-Roig, C.; de Winther, M.P.; Weber, C.; Daemen, M.J.; Lutgens, E.; Soehnlein, O. Atherosclerotic plaque destabilization: Mechanisms, models, and therapeutic strategies. Circ. Res. 2014, 114, 214–226. [Google Scholar] [CrossRef]
- Gimbrone, M.A., Jr.; Garcia-Cardena, G. Endothelial Cell Dysfunction and the Pathobiology of Atherosclerosis. Circ. Res. 2016, 118, 620–636. [Google Scholar] [CrossRef]
- Han, X.; Boisvert, W.A. Interleukin-10 protects against atherosclerosis by modulating multiple atherogenic macrophage function. Thromb. Haemost. 2015, 113, 505–512. [Google Scholar] [CrossRef] [PubMed]
- Cipollone, F.; Fazia, M.; Mincione, G.; Iezzi, A.; Pini, B.; Cuccurullo, C.; Ucchino, S.; Spigonardo, F.; Di Nisio, M.; Cuccurullo, F.; et al. Increased expression of transforming growth factor-beta1 as a stabilizing factor in human atherosclerotic plaques. Stroke 2004, 35, 2253–2257. [Google Scholar] [CrossRef] [PubMed]
- Cai, B.; Thorp, E.B.; Doran, A.C.; Sansbury, B.E.; Daemen, M.J.; Dorweiler, B.; Spite, M.; Fredman, G.; Tabas, I. MerTK receptor cleavage promotes plaque necrosis and defective resolution in atherosclerosis. J. Clin. Investig. 2017, 127, 564–568. [Google Scholar] [CrossRef]
- Dabravolski, S.A.; Sukhorukov, V.N.; Kalmykov, V.A.; Grechko, A.V.; Shakhpazyan, N.K.; Orekhov, A.N. The Role of KLF2 in the Regulation of Atherosclerosis Development and Potential Use of KLF2-Targeted Therapy. Biomedicines 2022, 10, 254. [Google Scholar] [CrossRef] [PubMed]
- Kotlyarov, S.; Kotlyarova, A. Participation of Kruppel-like Factors in Atherogenesis. Metabolites 2023, 13, 448. [Google Scholar] [CrossRef]
- Li, Z.; Martin, M.; Zhang, J.; Huang, H.Y.; Bai, L.; Zhang, J.; Kang, J.; He, M.; Li, J.; Maurya, M.R.; et al. Kruppel-Like Factor 4 Regulation of Cholesterol-25-Hydroxylase and Liver X Receptor Mitigates Atherosclerosis Susceptibility. Circulation 2017, 136, 1315–1330. [Google Scholar] [CrossRef]
- Niu, N.; Xu, S.; Xu, Y.; Little, P.J.; Jin, Z.G. Targeting Mechanosensitive Transcription Factors in Atherosclerosis. Trends Pharmacol. Sci. 2019, 40, 253–266. [Google Scholar] [CrossRef]
- Hammond, S.M. An overview of microRNAs. Adv. Drug Deliv. Rev. 2015, 87, 3–14. [Google Scholar] [CrossRef] [PubMed]
- Colpani, O.; Spinetti, G. MicroRNAs orchestrating senescence of endothelial and vascular smooth muscle cells. Vasc. Biol. 2019, 1, H75–H81. [Google Scholar] [CrossRef]
- Wojciechowska, A.; Braniewska, A.; Kozar-Kaminska, K. MicroRNA in cardiovascular biology and disease. Adv. Clin. Exp. Med. 2017, 26, 865–874. [Google Scholar] [CrossRef]
- Gangwar, R.S.; Rajagopalan, S.; Natarajan, R.; Deiuliis, J.A. Noncoding RNAs in Cardiovascular Disease: Pathological Relevance and Emerging Role as Biomarkers and Therapeutics. Am. J. Hypertens 2018, 31, 150–165. [Google Scholar] [CrossRef] [PubMed]
- Chou, C.H.; Shrestha, S.; Yang, C.D.; Chang, N.W.; Lin, Y.L.; Liao, K.W.; Huang, W.C.; Sun, T.H.; Tu, S.J.; Lee, W.H.; et al. miRTarBase update 2018: A resource for experimentally validated microRNA-target interactions. Nucleic Acids Res. 2018, 46, D296–D302. [Google Scholar] [CrossRef] [PubMed]
- Knuuti, J.; Wijns, W.; Saraste, A.; Capodanno, D.; Barbato, E.; Funck-Brentano, C.; Prescott, E.; Storey, R.F.; Deaton, C.; Cuisset, T.; et al. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. Eur. Heart J. 2020, 41, 407–477. [Google Scholar] [CrossRef] [PubMed]
- Collet, J.P.; Thiele, H.; Barbato, E.; Barthelemy, O.; Bauersachs, J.; Bhatt, D.L.; Dendale, P.; Dorobantu, M.; Edvardsen, T.; Folliguet, T.; et al. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur. Heart J. 2021, 42, 1289–1367. [Google Scholar] [CrossRef] [PubMed]
- Stevens, P.E.; Levin, A.; Kidney Disease: Improving Global Outcomes Chronic Kidney Disease Guideline Development Work Group, M. Evaluation and management of chronic kidney disease: Synopsis of the kidney disease: Improving global outcomes 2012 clinical practice guideline. Ann. Intern. Med. 2013, 158, 825–830. [Google Scholar] [CrossRef]
- American Diabetes, A. Standards of Medical Care in Diabetes-2018 Abridged for Primary Care Providers. Clin. Diabetes 2018, 36, 14–37. [Google Scholar] [CrossRef]
- Li, X.; Lyu, L.; Yang, W.; Pan, J.; Dong, M.; Zhang, M.; Zhang, P. Identification of Flow-Limiting Coronary Stenosis With PCS: A New Cost-Effective Index Derived From the Product of Corrected TIMI Frame Count and Percent Diameter Stenosis. Front. Cardiovasc. Med. 2021, 8, 718935. [Google Scholar] [CrossRef]
- Neumann, F.J.; Sousa-Uva, M.; Ahlsson, A.; Alfonso, F.; Banning, A.P.; Benedetto, U.; Byrne, R.A.; Collet, J.P.; Falk, V.; Head, S.J.; et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. EuroIntervention 2019, 14, 1435–1534. [Google Scholar] [CrossRef]
- Li, S.; Sun, Y.N.; Zhou, Y.T.; Zhang, C.L.; Lu, F.; Liu, J.; Shang, X.M. Screening and identification of microRNA involved in unstable angina using gene-chip analysis. Exp. Ther. Med. 2016, 12, 2716–2722. [Google Scholar] [CrossRef][Green Version]
- D’Alessandra, Y.; Carena, M.C.; Spazzafumo, L.; Martinelli, F.; Bassetti, B.; Devanna, P.; Rubino, M.; Marenzi, G.; Colombo, G.I.; Achilli, F.; et al. Diagnostic potential of plasmatic MicroRNA signatures in stable and unstable angina. PLoS ONE 2013, 8, e80345. [Google Scholar] [CrossRef]
- Shalaby, S.M.; El-Shal, A.S.; Shoukry, A.; Khedr, M.H.; Abdelraheim, N. Serum miRNA-499 and miRNA-210: A potential role in early diagnosis of acute coronary syndrome. IUBMB Life 2016, 68, 673–682. [Google Scholar] [CrossRef] [PubMed]
- Ke-Gang, J.; Zhi-Wei, L.; Xin, Z.; Jing, W.; Ping, S.; Xue-Jing, H.; Hong-Xia, T.; Xin, T.; Xiao-Cheng, L. Evaluating Diagnostic and Prognostic Value of Plasma miRNA133a in Acute Chest Pain Patients Undergoing Coronary Angiography. Medicine 2016, 95, e3412. [Google Scholar] [CrossRef]
- Zeller, T.; Keller, T.; Ojeda, F.; Reichlin, T.; Twerenbold, R.; Tzikas, S.; Wild, P.S.; Reiter, M.; Czyz, E.; Lackner, K.J.; et al. Assessment of microRNAs in patients with unstable angina pectoris. Eur. Heart J. 2014, 35, 2106–2114. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Y.; Lin, Y.; Yan, W.; Sun, Z.; Jiang, Z.; Shen, B.; Jiang, X.; Shi, J. Novel Biomarker MicroRNAs for Subtyping of Acute Coronary Syndrome: A Bioinformatics Approach. Biomed. Res. Int. 2016, 2016, 4618323. [Google Scholar] [CrossRef] [PubMed]
- Yu, X.; Xu, J.F.; Song, M.; Zhang, L.; Li, Y.H.; Han, L.; Tang, M.X.; Zhang, W.; Zhong, M.; Wang, Z.H. Associations of Circulating microRNA-221 and 222 With the Severity of Coronary Artery Lesions in Acute Coronary Syndrome Patients. Angiology 2022, 73, 579–587. [Google Scholar] [CrossRef] [PubMed]
- Masoodi Khabar, P.; Ghydari, M.E.; Vazifeh Shiran, N.; Shirazy, M.; Hamidpour, M. Platelet MicroRNA-484 as a Novel Diagnostic Biomarker for Acute Coronary Syndrome. Lab. Med. 2023, 54, 256–261. [Google Scholar] [CrossRef]
- Navickas, R.; Gal, D.; Laucevicius, A.; Taparauskaite, A.; Zdanyte, M.; Holvoet, P. Identifying circulating microRNAs as biomarkers of cardiovascular disease: A systematic review. Cardiovasc. Res. 2016, 111, 322–337. [Google Scholar] [CrossRef]
- Elgebaly, S.A.; Todd, R.; Kreutzer, D.L.; Christenson, R.; El-Khazragy, N.; Arafa, R.K.; Rabie, M.A.; Mohamed, A.F.; Ahmed, L.A.; El Sayed, N.S. Nourin-Associated miRNAs: Novel Inflammatory Monitoring Markers for Cyclocreatine Phosphate Therapy in Heart Failure. Int. J. Mol. Sci. 2021, 22, 3575. [Google Scholar] [CrossRef]
- Cui, Y.; Song, J.; Li, S.; Lee, C.; Zhang, F.; Chen, H. Plasmatic MicroRNA Signatures in Elderly People with Stable and Unstable Angina. Int. Heart J. 2018, 59, 43–50. [Google Scholar] [CrossRef]
- Tang, Y.; Fan, W.; Zou, B.; Yan, W.; Hou, Y.; Kwabena Agyare, O.; Jiang, Z.; Qu, S. TGF-beta signaling and microRNA cross-talk regulates abdominal aortic aneurysm progression. Clin. Chim. Acta 2021, 515, 90–95. [Google Scholar] [CrossRef]
- Huang, P. Potential new therapeutic targets: Association of microRNA with atherosclerotic plaque stability. Int. J. Immunopathol. Pharmacol. 2023, 37, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Kitahara, S.; Kataoka, Y.; Sugane, H.; Otsuka, F.; Asaumi, Y.; Noguchi, T.; Yasuda, S. In vivo imaging of vulnerable plaque with intravascular modalities: Its advantages and limitations. Cardiovasc. Diagn. Ther. 2020, 10, 1461–1479. [Google Scholar] [CrossRef] [PubMed]
- Chang, M.; Kang, S.J.; Yoon, S.H.; Ahn, J.M.; Park, D.W.; Lee, S.W.; Kim, Y.H.; Lee, C.W.; Park, S.W.; Nakazawa, G.; et al. Plaque composition and morphologic characteristics in significant left main bifurcation disease; virtual histology intravascular ultrasound study. Coron. Artery Dis. 2016, 27, 623–628. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Yoon, Y.E.; Lee, W.; Choi, H.M.; Park, J.B.; Kim, H.L.; Park, H.E.; Lee, S.P.; Kim, H.K.; Choi, S.Y.; et al. Prognosis of anatomic coronary artery disease without myocardial ischemia: Coronary computed tomography angiography detects high-risk patients even in cases of negative single-photon emission computed tomography findings. J. Cardiol. 2018, 72, 162–169. [Google Scholar] [CrossRef]
- Ramadan, R.; Boden, W.E.; Kinlay, S. Management of Left Main Coronary Artery Disease. J. Am. Heart Assoc. 2018, 7, e008151. [Google Scholar] [CrossRef]
- Mao, Q.Q.; Chen, J.J.; Xu, W.J.; Zhao, X.Z.; Sun, X.; Zhong, L. miR-92a-3p promotes the proliferation and invasion of gastric cancer cells by targeting KLF2. J. Biol. Regul. Homeost. Agents 2020, 34, 1333–1341. [Google Scholar] [CrossRef]
- Li, J.; Liu, X.; Hu, X.; Tian, G.G.; Ma, W.; Pei, X.; Wang, Y.; Wu, J. MicroRNA-10b regulates the renewal of spermatogonial stem cells through Kruppel-like factor 4. Cell Biochem. Funct. 2017, 35, 184–191. [Google Scholar] [CrossRef]
- Saenz-Pipaon, G.; Martinez-Aguilar, E.; Orbe, J.; Gonzalez Miqueo, A.; Fernandez-Alonso, L.; Paramo, J.A.; Roncal, C. The Role of Circulating Biomarkers in Peripheral Arterial Disease. Int. J. Mol. Sci. 2021, 22, 3601. [Google Scholar] [CrossRef]


| UA Patients (n = 14) | CCS Patients (n = 38) | HV (n = 10) | p Significance * | |
|---|---|---|---|---|
| Age [years] | 62 ± 8 | 71 ± 11 | 39 ± 10 | Significant between
|
| Sex (woman) ** | 3 (21.43%) | 18 (47.4%) | 6 (60%) | NS (p = 0.13) |
| Hypertension ** | 11 (84.6%) | 30 (81.1%) | NA | NS (p = 0.78) |
| Hyperlipidemia ** | 9 (69.2%) | 26 (68.4%) | NA | NS (p = 0.99) |
| Active smoker ** | 7 (53.9%) | 7 (18.4%) | NA | Significant (p = 0.013) |
| Previous smoker ** | 4 (30.8%) | 9 (23.7%) | NA | NS (p = 0.61) |
| CAD or PAD ** | 5 (35.7%) | 6 (15.8%) | NA | NS (p = 0.12) |
| Baseline statin use ** | 5 (30.8%) | 16 (42.1%) | NA | NS (p = 0.47) |
| Baseline arrythmia ** | 0 (0%) | 6 (15.8%) | NA | NS (p = 0.13) |
| BMI [kg/m2] | 29.5 ± 4.9 | 25.8 ± 4.0 | 24.0 ± 3.6 |
|
| TC [mg/dL] | 196.5 [129–224] | 150.5 [130–190] | 183.5 [173–203] | NS (p = 0.18) |
| LDL [mg/dL] | 93.5 [62–132.5] | 78 [61–108] | 97 [89–117] | NS (p = 0.25) |
| HDL [mg/dL] | 37.8 ± 3.9 | 51.3 ± 11.6 | 65.1 ± 10.5 | Significant between
|
| TG [mg/dL] | 142.5 [94–187] | 103 [80–138] | 76.5 [67–110] |
|
| eGFR [mL/min/1.73 m2] | 74.1 ± 17.5 | 66.1 ± 18.7 | 99.5 [90–113] |
|
| Hgb [g/dL] | 14.9 ± 1.7 | 13.7 ± 1.4 | 13.9 ± 1.5 |
|
| PLT [number] | 243 ± 64 | 228 ± 71 | 241 ± 61 | NS (p = 0.73) |
| TSH [μIU/mL] | 1.41 [0.929–2.39] | 1.39 [0.848–2.42] | 1.34 [0.641–2.06] | NS (p = 0.80) |
| AspAT [U/L] | 24 [19.5–26.5] | 25 [21–30] | NA | NS (p = 0.30) |
| AlAT [U/L] | 35 [24–52] | 24 [17–29] | NA | Significant (p = 0.008) |
| APTT [s] | 30.1 ± 3.6 | 29.4 ± 3.6 | NA | NS (p = 0.57) |
| NEXT STEP AFTER CORONARY ANGIOGRAPHY | ||||
| Indications for invasive treatment *** | 12 (85.7%) | 20 (52.6%) | NA | Significant (p = 0.03) |
| microRNAs | Fold Change in UA Group (n = 14) * | Fold Change in CCS Group (n = 38) * | Fold Change in HV Group (n = 10) * | p ** |
|---|---|---|---|---|
| Hsa-miR-92a-3p | 82.55 [53.41–151.53] | 70.42 [42.69–109.82] | 66.82 [31.77–85.81] | NS (0.389) |
| Hsa-miR-10b-5p | 0.097 [0.062–0.177] | 0.058 [0.036–0.120] | 0.085 [0.057–0.124] | 0.073 (Kruskal-Wallis test) *** |
| Hsa-miR-126-3p | 60.75 ± 47.07 | 48.18 ± 23.72 | 50.48 ± 25.69 | NS (0.427) |
| Hsa-miR-98-5p | 0.031 [0.012–0.074] | 0.024 [0.012–0.047] | 0.013 [0.006–0.020] | NS (0.339) |
| Hsa-miR-29b-3p | 0.794 [0.629–1.257] | 0.792 [0.584–1.159] | 0.925 [0.734–1.799] | NS (0.395) |
| microRNAs | Fold Change in UA Males (n = 11) * | Fold Change in CCS Males (n = 22) * | p ** |
|---|---|---|---|
| Hsa-miR-92a-3p | 87.85 [38.28–192.54] | 60.72 [41.78–97.93] | NS (0.418) |
| Hsa-miR-10b-5p | 0.104 [0.06–0.187] | 0.049 [0.034–0.078] | 0.014 ** |
| Hsa-miR-126-3p | 62.52 ± 53.32 | 49.17 ± 24.11 | NS (0.444) |
| Hsa-miR-98-5p | 0.027 [0.013–0.067] | 0.024 [0.018–0.047] | NS (0.887) |
| Hsa-miR-29b-3p | 0.784 [0.629–1.847] | 0.845 [0.484–1.5] | NS (0.955) |
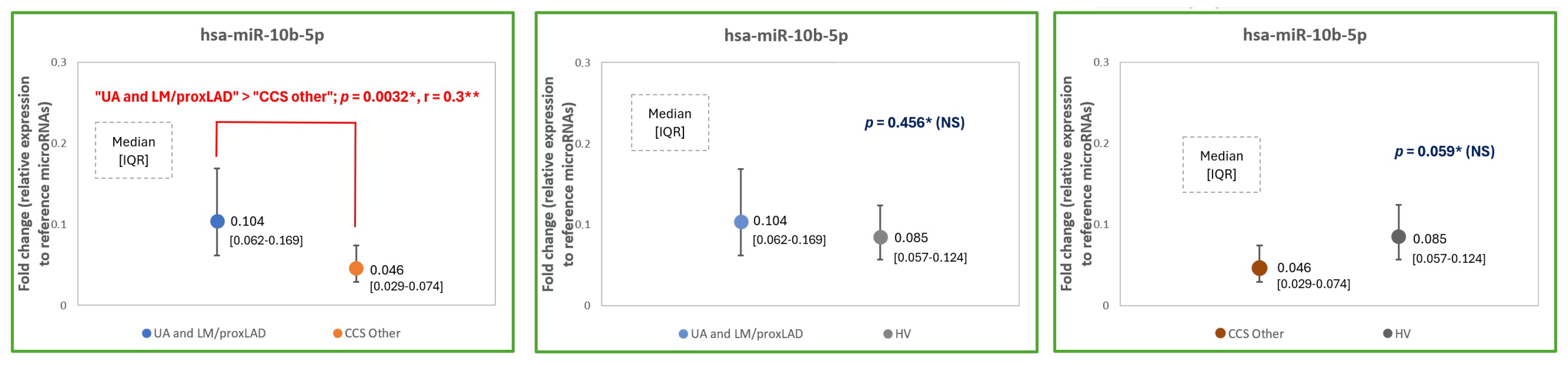
| microRNAs | Fold Change in ”UA and LM/proxLAD” (n = 29) * | Fold Change in ”CCS Other” (n = 25) * | Fold Change in HV (n = 10) * | p ** |
|---|---|---|---|---|
| Hsa-miR-92a-3p | 92.64 [62.86–151.53] | 54.74 [38.73–74.80] | 66.82 [31.77–85.81] | 0.0178 *** |
| Hsa-miR-10b-5p | 0.104 [0.062–0.169] | 0.046 [0.029–0.074] | 0.085 [0.057–0.124] | 0.0089 *** |
| Hsa-miR-126-3p | 45.15 [32.77–65.8] | 48.79 [28.92–61.77] | 43.2 [30.75–60.15] | NS (0.84) |
| Hsa-miR-98-5p | 0.03 [0.012–0.074] | 0.024 [0.014–0.04] | 0.013 [0.006–0.020] | NS (0.239) |
| Hsa-miR-29b-3p | 0.805 [0.629–1.257] | 0.795 [0.612–1.245] | 0.925 [0.734–1.799] | NS (0.551) |
| mRNA of the Protein | Corresponding Downregulating microRNA |
|---|---|
| IL10 | Hsa-miR-98-5p (abbrev. miR-98) |
| MerTK | Hsa-miR-126-3p (abbrev. miR-126) |
| TGFβ1 and TGFβ3 | Hsa-miR-29b-3p (abbrev. miR-29b) |
| KLF2 | Hsa-miR-92a-3p (abbrev. miR-92a) |
| KLF4 | Hsa-miR-10b-5p (abbrev. miR-10b) |
| Exclusion Criteria for Chronic Coronary Syndrome (CCS) Patients |
|---|
|
| Exclusion criteria for unstable angina (UA) patients |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kowara, M.; Kopka, M.; Kopka, K.; Głowczyńska, R.; Mitrzak, K.; Kim, D.-a.; Sadowski, K.A.; Cudnoch-Jędrzejewska, A. MicroRNA Inhibiting Atheroprotective Proteins in Patients with Unstable Angina Comparing to Chronic Coronary Syndrome. Int. J. Mol. Sci. 2024, 25, 10621. https://doi.org/10.3390/ijms251910621
Kowara M, Kopka M, Kopka K, Głowczyńska R, Mitrzak K, Kim D-a, Sadowski KA, Cudnoch-Jędrzejewska A. MicroRNA Inhibiting Atheroprotective Proteins in Patients with Unstable Angina Comparing to Chronic Coronary Syndrome. International Journal of Molecular Sciences. 2024; 25(19):10621. https://doi.org/10.3390/ijms251910621
Chicago/Turabian StyleKowara, Michał, Michał Kopka, Karolina Kopka, Renata Głowczyńska, Karolina Mitrzak, Dan-ae Kim, Karol Artur Sadowski, and Agnieszka Cudnoch-Jędrzejewska. 2024. "MicroRNA Inhibiting Atheroprotective Proteins in Patients with Unstable Angina Comparing to Chronic Coronary Syndrome" International Journal of Molecular Sciences 25, no. 19: 10621. https://doi.org/10.3390/ijms251910621
APA StyleKowara, M., Kopka, M., Kopka, K., Głowczyńska, R., Mitrzak, K., Kim, D.-a., Sadowski, K. A., & Cudnoch-Jędrzejewska, A. (2024). MicroRNA Inhibiting Atheroprotective Proteins in Patients with Unstable Angina Comparing to Chronic Coronary Syndrome. International Journal of Molecular Sciences, 25(19), 10621. https://doi.org/10.3390/ijms251910621






