Effect of Single Session of Swedish Massage on Circulating Levels of Interleukin-6 and Insulin-like Growth Factor 1
Abstract
1. Introduction
2. Results
3. Discussion
4. Materials and Methods
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Salvo, S.G. Massage Techniques, Joint Mobilizations, and Streches. In Massage Therapy, 5th ed.; Elsevier: Amsterdam, The Netherlands, 2015. [Google Scholar]
- Best, T.M.; Hunter, R.; Wilcox, A.; Haq, F. Effectiveness of Sports Massage for Recovery of Skeletal Muscle from Strenuous Exercise. Clin. J. Sport Med. 2008, 18, 446–460. [Google Scholar] [CrossRef] [PubMed]
- Guo, J.; Li, L.; Gong, Y.; Zhu, R.; Xu, J.; Zou, J.; Chen, X. Massage Alleviates Delayed Onset Muscle Soreness after Strenuous Exercise: A Systematic Review and Meta-Analysis. Front. Physiol. 2017, 8, 00747. [Google Scholar] [CrossRef]
- Willison, K.D.; Andrews, G.J.; Cockerham, W.C. Life Chance Characteristics of Older Users of Swedish Massage. Complement. Ther. Clin. Pract. 2005, 11, 232–241. [Google Scholar] [CrossRef]
- Smith, C.A.; Levett, K.M.; Collins, C.T.; Dahlen, H.G.; Ee, C.C.; Suganuma, M. Massage, Reflexology and Other Manual Methods for Pain Management in Labour. Cochrane Database Syst. Rev. 2018, 3, 009290. [Google Scholar] [CrossRef]
- Bayrakdaroğlu, S.; Eken, Ö.; Bayer, R.; Yagin, F.H.; Kızılet, T.; Kayhan, R.F.; Ardigò, L.P. Effects of Swedish Massage at Different Times of the Day on Dynamic and Static Balance in Taekwondo Athletes. Healthcare 2024, 12, 165. [Google Scholar] [CrossRef]
- Mori, H.; Ohsawa, H.; Tanaka, T.H.; Taniwaki, E.; Leisman, G.; Nishijo, K. Effect of Massage on Blood Flow and Muscle Fatigue Following Isometric Lumbar Exercise. Med. Sci. Monit. 2004, 10, CR173–CR178. [Google Scholar]
- Weerapong, P.; Hume, P.A.; Kolt, G.S. The Mechanisms of Massage and Effects on Performance, Muscle Recovery and Injury Prevention. Sport. Med. 2005, 35, 235–256. [Google Scholar] [CrossRef]
- Van Pelt, D.W.; Lawrence, M.M.; Miller, B.F.; Butterfield, T.A.; Dupont-Versteegden, E.E. Massage as a Mechanotherapy for Skeletal Muscle. Exerc. Sport Sci. Rev. 2021, 49, 107–114. [Google Scholar] [CrossRef]
- Crane, J.D.; Ogborn, D.I.; Cupido, C.; Melov, S.; Hubbard, A.; Bourgeois, J.M.; Tarnopolsky, M.A. Massage Therapy Attenuates Inflammatory Signaling after Exercise-Induced Muscle Damage. Sci. Transl. Med. 2012, 4, 119ra13. [Google Scholar] [CrossRef]
- Diego, M.A.; Field, T.; Sanders, C.; Hernandez-Reif, M. Massage Therapy of Moderate and Light Pressure and Vibrator Effects on EEG and Heart Rate. Int. J. Neurosci. 2004, 114, 31–44. [Google Scholar] [CrossRef]
- Do-Jin, K.; Jong-Hyuck, K. Effect of the Muscular Strength Exercise and Massage on Muscle Injury Marker and IGF-1. Indian J. Sci. Technol. 2015, 8, 1–5. [Google Scholar] [CrossRef]
- Drust, B.; Atkinson, G.; Gregson, W.; French, D.; Binningsley, D. The Effects of Massage on Intra Muscular Temperature in the Vastus Lateralis in Humans. Int. J. Sports Med. 2003, 24, 395–399. [Google Scholar] [CrossRef]
- Hernandez-Reif, M.; Field, T.; Krasnegor, J.; Hossain, Z.; Theakston, H.; Burman, I. High Blood Pressure and Associated Symptoms Were Reduced by Massage Therapy. J. Bodyw. Mov. Ther. 2000, 4, 31–38. [Google Scholar] [CrossRef]
- Giudice, J.; Taylor, J.M. Muscle as a Paracrine and Endocrine Organ. Curr. Opin. Pharmacol. 2017, 34, 49–55. [Google Scholar]
- Zunner, B.E.M.; Wachsmuth, N.B.; Eckstein, M.L.; Scherl, L.; Schierbauer, J.R.; Haupt, S.; Stumpf, C.; Reusch, L.; Moser, O. Myokines and Resistance Training: A Narrative Review. Int. J. Mol. Sci. 2022, 23, 3501. [Google Scholar] [CrossRef]
- Pedersen, B.K. Muscles and Their Myokines. J. Exp. Biol. 2011, 214, 337–346. [Google Scholar] [CrossRef] [PubMed]
- Schnyder, S.; Handschin, C. Skeletal Muscle as an Endocrine Organ: PGC-1α, Myokines and Exercise. Bone 2015, 80, 115–125. [Google Scholar] [CrossRef]
- Pedersen, B.K.; Febbraio, M.A. Muscle as an Endocrine Organ: Focus on Muscle-Derived Interleukin-6. Physiol. Rev. 2008, 88, 1379–1406. [Google Scholar] [CrossRef] [PubMed]
- Bakker, A.D.; Jaspers, R.T. IL-6 and IGF-1 Signaling Within and Between Muscle and Bone: How Important Is the MTOR Pathway for Bone Metabolism? Curr. Osteoporos. Rep. 2015, 13, 131–139. [Google Scholar] [CrossRef]
- Balakrishnan, R.; Thurmond, D.C. Mechanisms by Which Skeletal Muscle Myokines Ameliorate Insulin Resistance. Int. J. Mol. Sci. 2022, 23, 4636. [Google Scholar] [CrossRef]
- Kraemer, W.J.; Ratamess, N.A. Hormonal Responses and Adaptations to Resistance Exercise and Training. Sport. Med. 2005, 35, 339–361. [Google Scholar] [CrossRef]
- Carey, A.L.; Steinberg, G.R.; Macaulay, S.L.; Thomas, W.G.; Holmes, A.G.; Ramm, G.; Prelovsek, O.; Hohnen-Behrens, C.; Watt, M.J.; James, D.E.; et al. Interleukin-6 Increases Insulin-Stimulated Glucose Disposal in Humans and Glucose Uptake and Fatty Acid Oxidation in Vitro via AMP-Activated Protein Kinase. Diabetes 2006, 55, 2688–2697. [Google Scholar] [CrossRef] [PubMed]
- Moresi, V.; Adamo, S.; Berghella, L. The JAK/STAT Pathway in Skeletal Muscle Pathophysiology. Front. Physiol. 2019, 10, 00500. [Google Scholar] [CrossRef]
- Rincon, M.; Rudin, E.; Barzilai, N. The Insulin/IGF-1 Signaling in Mammals and Its Relevance to Human Longevity. Exp. Gerontol. 2005, 40, 873–877. [Google Scholar] [CrossRef]
- Hu, X.; Li, J.; Fu, M.; Zhao, X.; Wang, W. The JAK/STAT Signaling Pathway: From Bench to Clinic. Signal Transduct. Target. Ther. 2021, 6, 402. [Google Scholar] [CrossRef]
- Barzilai, N.; Huffman, D.M.; Muzumdar, R.H.; Bartke, A. The Critical Role of Metabolic Pathways in Aging. Diabetes 2012, 61, 1315–1322. [Google Scholar] [CrossRef] [PubMed]
- Huang, X.; Liu, G.; Guo, J.; Su, Z. The PI3K/AKT Pathway in Obesity and Type 2 Diabetes. Int. J. Biol. Sci. 2018, 14, 1483–1496. [Google Scholar] [CrossRef] [PubMed]
- Ersahin, T.; Tuncbag, N.; Cetin-Atalay, R. The PI3K/AKT/MTOR Interactive Pathway. Mol. Biosyst. 2015, 11, 1946–1954. [Google Scholar] [CrossRef]
- Rapaport, M.H.; Schettler, P.; Bresee, C. A Preliminary Study of the Effects of a Single Session of Swedish Massage on Hypothalamic–Pituitary–Adrenal and Immune Function in Normal Individuals. J. Altern. Complement. Med. 2010, 16, 1079–1088. [Google Scholar] [CrossRef]
- Rapaport, M.H.; Schettler, P.; Bresee, C. A Preliminary Study of the Effects of Repeated Massage on Hypothalamic-Pituitary-Adrenal and Immune Function in Healthy Individuals: A Study of Mechanisms of Action and Dosage. J. Altern. Complement. Med. 2012, 18, 789–797. [Google Scholar] [CrossRef]
- Field, T. Massage Therapy Research Review. Complement. Ther. Clin. Pract. 2014, 20, 224–229. [Google Scholar] [CrossRef] [PubMed]
- Field, T.; Diego, M.; Hernandez-Reif, M.; Dieter, J.N.I.; Kumar, A.M.; Schanberg, S.; Kuhn, C. Insulin and Insulin-like Growth Factor-1 Increased in Preterm Neonates Following Massage Therapy. J. Dev. Behav. Pediatr. 2008, 29, 463–466. [Google Scholar] [CrossRef] [PubMed]
- Sudarmi; Sukrama, I.D.M.; Sutirtayasa, I.W.P.; Weta, I.W. Irianto Influence of Baby Massage Stimulation on the Improvement of Nutritional Status, IGF-1, and Cortisol Level on Undernourished Infant. Bali Med. J. 2020, 9, 36–40. [Google Scholar] [CrossRef]
- Duclos, M.; Guinot, M.; Bouc, Y. Le Cortisol and GH: Odd and Controversial Ideas. Appl. Physiol. Nutr. Metab. 2007, 32, 895–903. [Google Scholar] [CrossRef] [PubMed]
- Severinsen, M.C.K.; Pedersen, B.K. Muscle-Organ Crosstalk: The Emerging Roles of Myokines. Endocr. Rev. 2020, 41, 594–609. [Google Scholar] [CrossRef] [PubMed]
- Moyer, C.A.; Rounds, J.; Hannum, J.W. A Meta-Analysis of Massage Therapy Research. Psychol. Bull. 2004, 130, 3–18. [Google Scholar] [CrossRef]
- Morhenn, V.; Beavin, L.E.; Zak, P.J. Massage Increases Oxytocin and Reduces Adrenocorticotropin Hormone in Humans. Altern. Ther. Health Med. 2012, 18, 11–18. [Google Scholar] [PubMed]
- Takayanagi, Y.; Onaka, T. Roles of Oxytocin in Stress Responses, Allostasis and Resilience. Int. J. Mol. Sci. 2021, 23, 150. [Google Scholar] [CrossRef] [PubMed]
- Hannibal, K.E.; Bishop, M.D. Chronic Stress, Cortisol Dysfunction, and Pain: A Psychoneuroendocrine Rationale for Stress Management in Pain Rehabilitation. Phys. Ther. 2014, 94, 1816–1825. [Google Scholar] [CrossRef]
- Hirata, T.; Arai, Y.; Yuasa, S.; Abe, Y.; Takayama, M.; Sasaki, T.; Kunitomi, A.; Inagaki, H.; Endo, M.; Morinaga, J.; et al. Associations of Cardiovascular Biomarkers and Plasma Albumin with Exceptional Survival to the Highest Ages. Nat. Commun. 2020, 11, 3820. [Google Scholar] [CrossRef]
- Krause, M.; Crognale, D.; Cogan, K.; Contarelli, S.; Egan, B.; Newsholme, P.; De Vito, G. The Effects of a Combined Bodyweight-Based and Elastic Bands Resistance Training, with or without Protein Supplementation, on Muscle Mass, Signaling and Heat Shock Response in Healthy Older People. Exp. Gerontol. 2019, 115, 104–113. [Google Scholar] [CrossRef]
| Mean ± Std. | 15 Men, 31 Women | |
|---|---|---|
| SMM (kg) | 29.6 ± 7.2 | 16.7–51.4 |
| BMI | 23.6 ± 2.3 | 19.5–29.4 |
| Weight (kg) | 68.5 ± 12.3 | 47.5–100.6 |
| Height (cm) | 169.8 ± 9.5 | 152.0–190.0 |
| Waist (cm) | 77.5 ± 8.0 | 64.5–94.0 |
| RRSys | 121.3 ± 13.3 | 86.0–155.5 |
| RRDias | 78.7 ± 8.6 | 57.5–98.5 |
| Paired Samples t-Test | ||||||
|---|---|---|---|---|---|---|
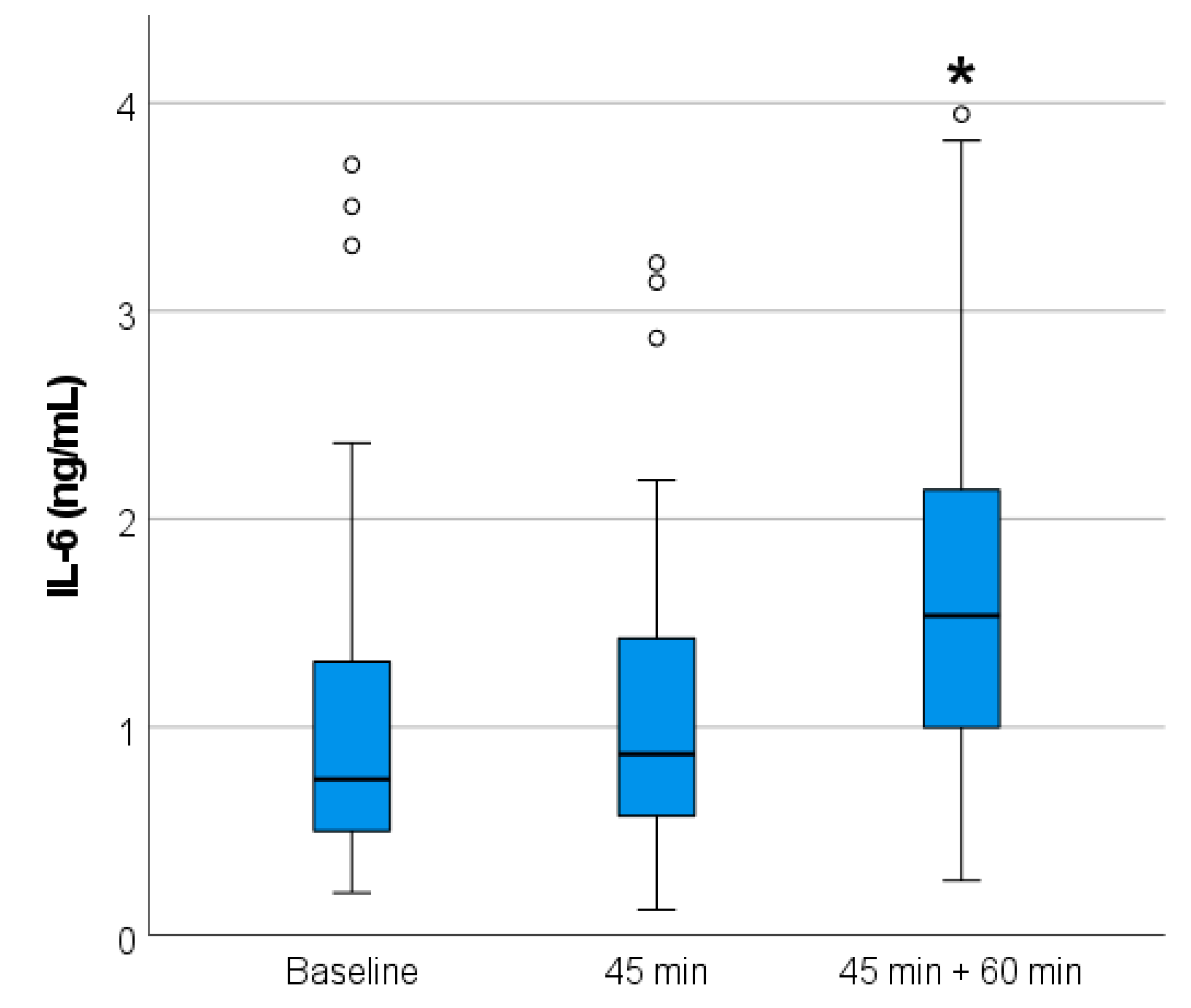
| IL-6 | Mean ± Std. | Upper | Lower | Sig. | ||
| I | 1.10 ± 0.94 | 1–3 | 0.08 | −0.24 | 0.312 | |
| II | 1.20 ± 0.91 | 1–5 | −0.51 | −1.01 | <0.001 | |
| III | 1.85 ± 1.30 | 3–5 | −0.38 | −0.97 | <0.001 | |
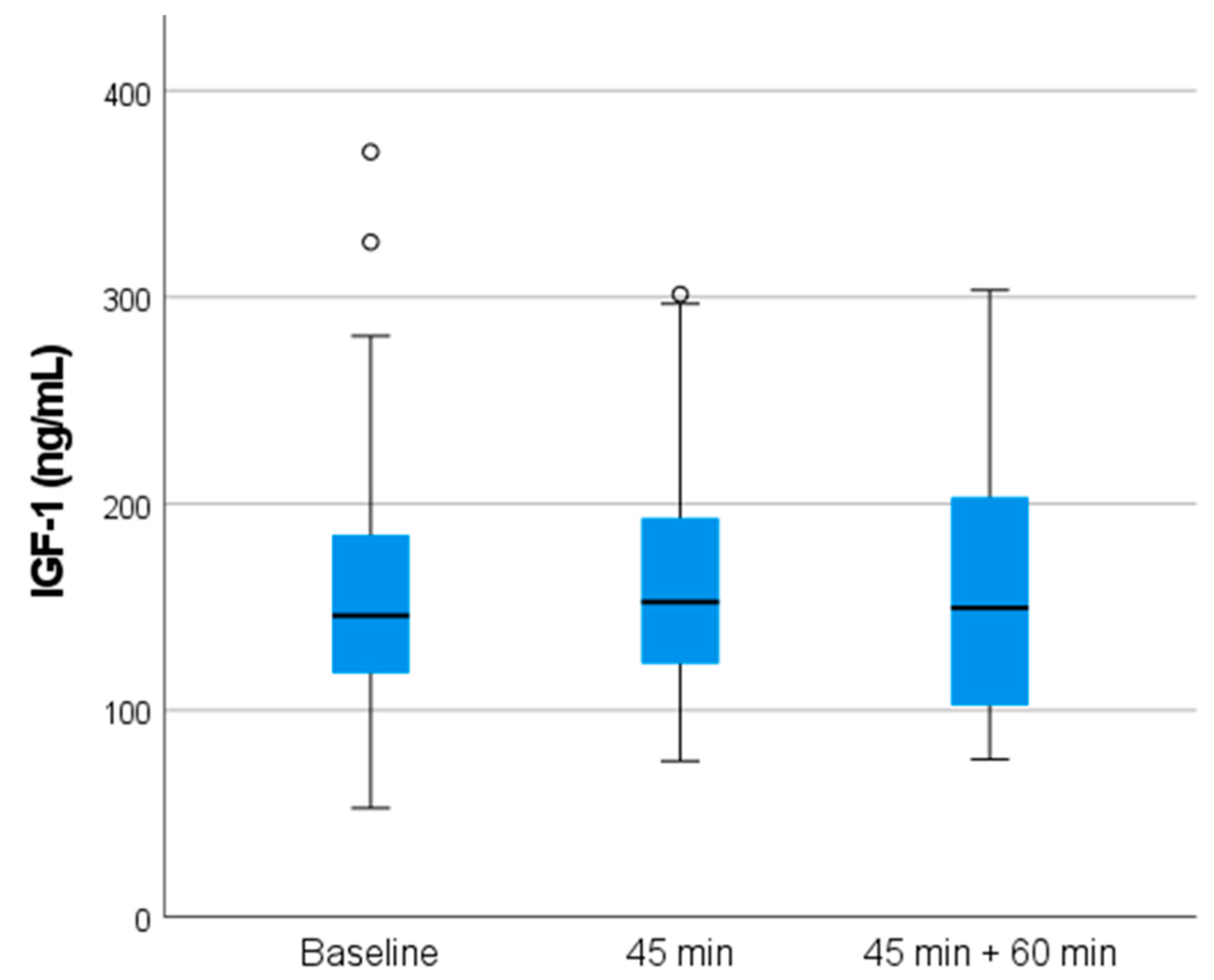
| IGF-1 | Mean ± std. | Upper | Lower | Sig. | ||
| I | 157.3 ± 66.8 | 1–3 | 8.01 | −12.95 | 0.637 | |
| II | 159.8 ± 57.2 | 1–5 | 10.57 | −13.96 | 0.782 | |
| III | 159.0 ± 60.9 | 3–5 | 9.83 | −8.28 | 0.863 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stenbäck, V.; Lehtonen, I.; Mäkelä, K.A.; Raza, G.S.; Ylinen, V.; Valtonen, R.; Hamari, T.; Walkowiak, J.; Tulppo, M.; Herzig, K.-H. Effect of Single Session of Swedish Massage on Circulating Levels of Interleukin-6 and Insulin-like Growth Factor 1. Int. J. Mol. Sci. 2024, 25, 9135. https://doi.org/10.3390/ijms25179135
Stenbäck V, Lehtonen I, Mäkelä KA, Raza GS, Ylinen V, Valtonen R, Hamari T, Walkowiak J, Tulppo M, Herzig K-H. Effect of Single Session of Swedish Massage on Circulating Levels of Interleukin-6 and Insulin-like Growth Factor 1. International Journal of Molecular Sciences. 2024; 25(17):9135. https://doi.org/10.3390/ijms25179135
Chicago/Turabian StyleStenbäck, Ville, Inka Lehtonen, Kari Antero Mäkelä, Ghulam Shere Raza, Venla Ylinen, Rasmus Valtonen, Tuomas Hamari, Jaroslaw Walkowiak, Mikko Tulppo, and Karl-Heinz Herzig. 2024. "Effect of Single Session of Swedish Massage on Circulating Levels of Interleukin-6 and Insulin-like Growth Factor 1" International Journal of Molecular Sciences 25, no. 17: 9135. https://doi.org/10.3390/ijms25179135
APA StyleStenbäck, V., Lehtonen, I., Mäkelä, K. A., Raza, G. S., Ylinen, V., Valtonen, R., Hamari, T., Walkowiak, J., Tulppo, M., & Herzig, K.-H. (2024). Effect of Single Session of Swedish Massage on Circulating Levels of Interleukin-6 and Insulin-like Growth Factor 1. International Journal of Molecular Sciences, 25(17), 9135. https://doi.org/10.3390/ijms25179135







