Gut Microbiota Signatures in Colorectal Cancer as a Potential Diagnostic Biomarker in the Future: A Systematic Review
Abstract
1. Introduction
1.1. Gut Microbiota
1.2. Gut Microbiota Dysbiosis in Colorectal Cancer
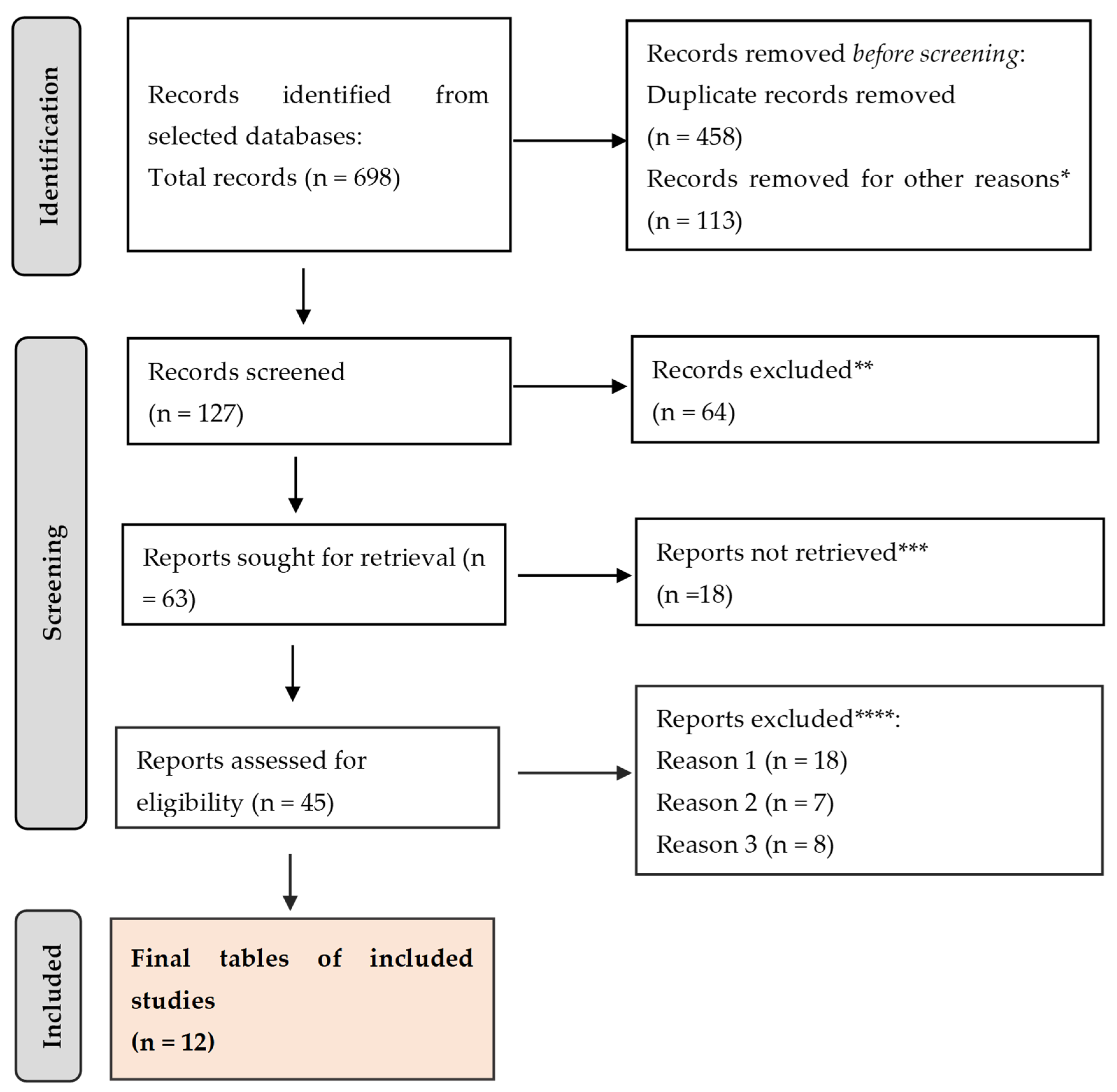
2. Materials and Methods
3. Results
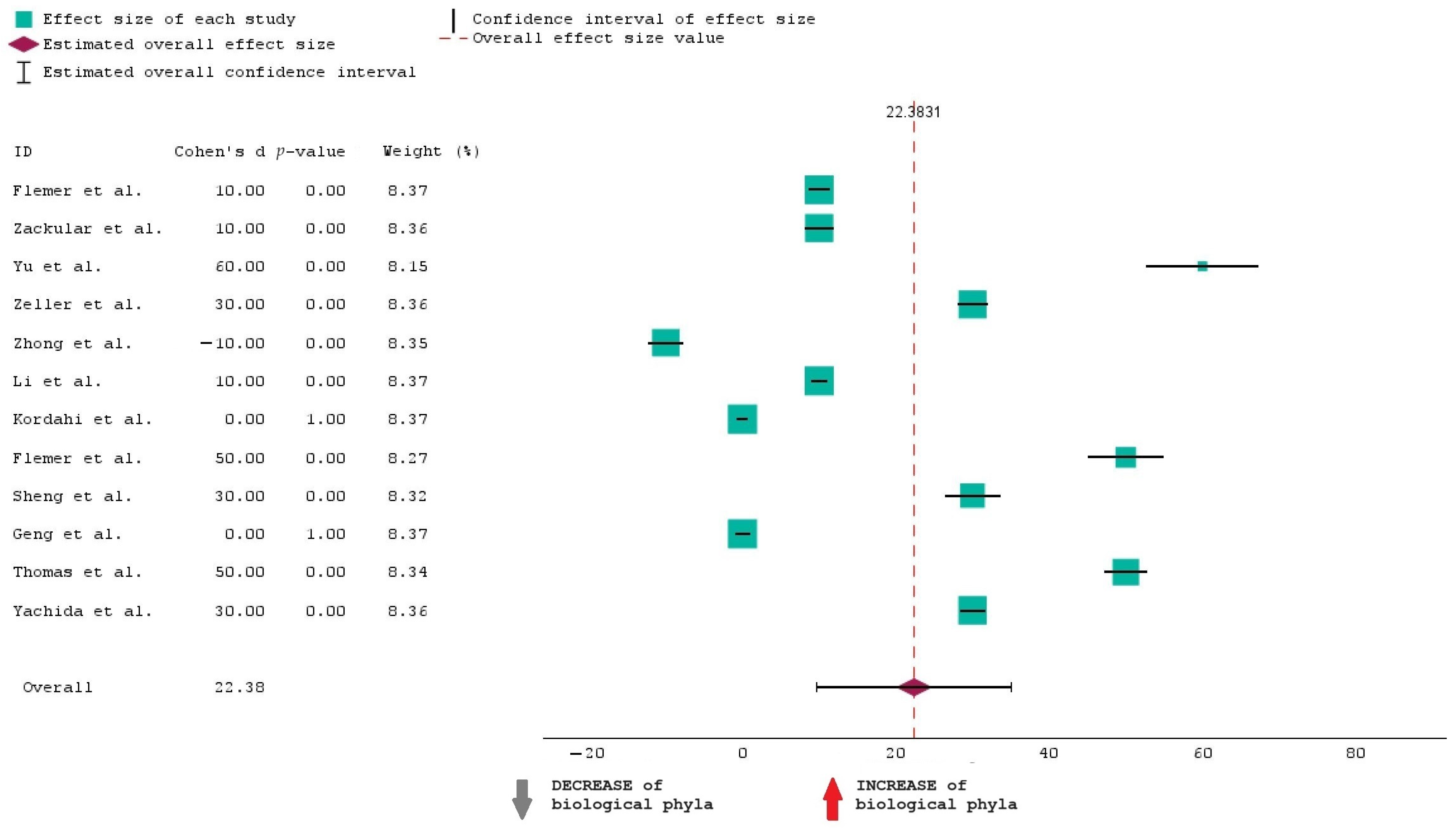
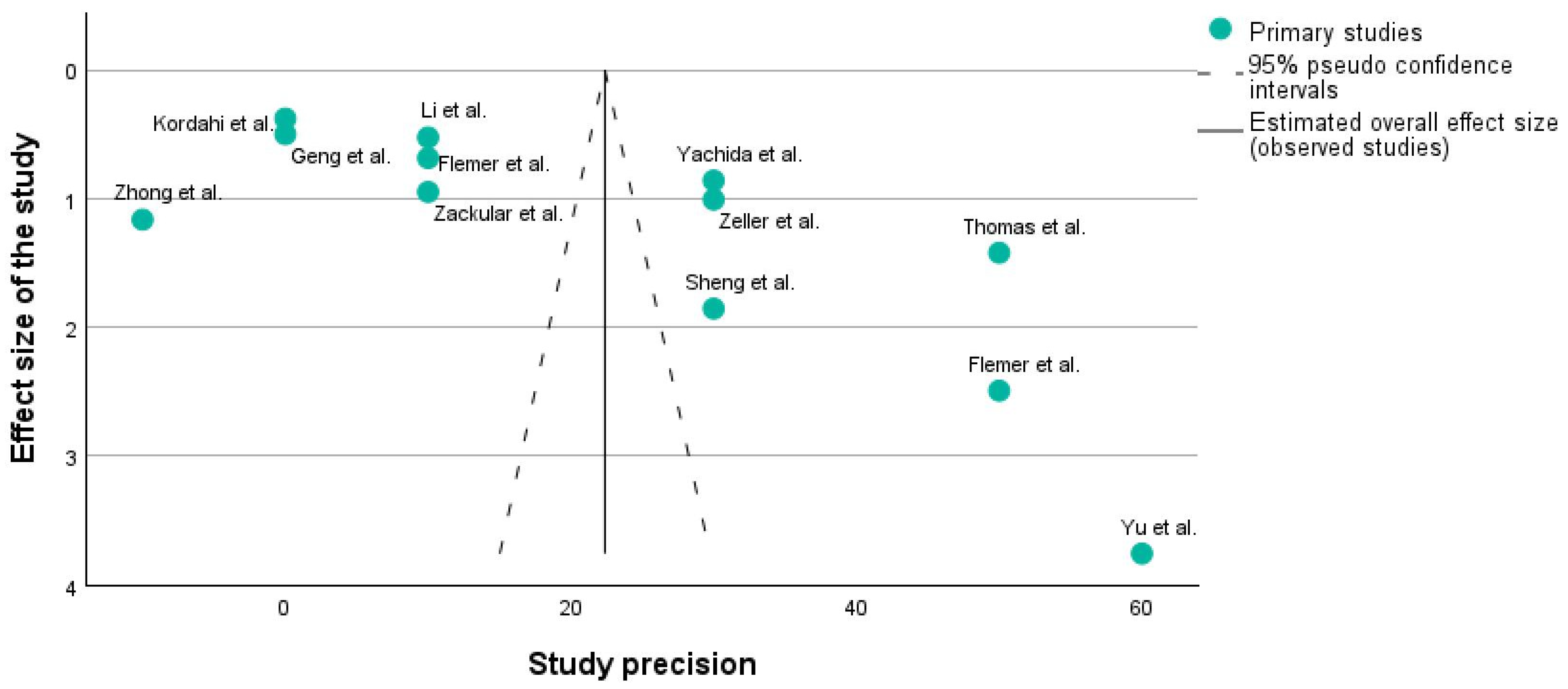
3.1. Statistical Analysis
3.1.1. Forest Plot
3.1.2. Funnel Plot
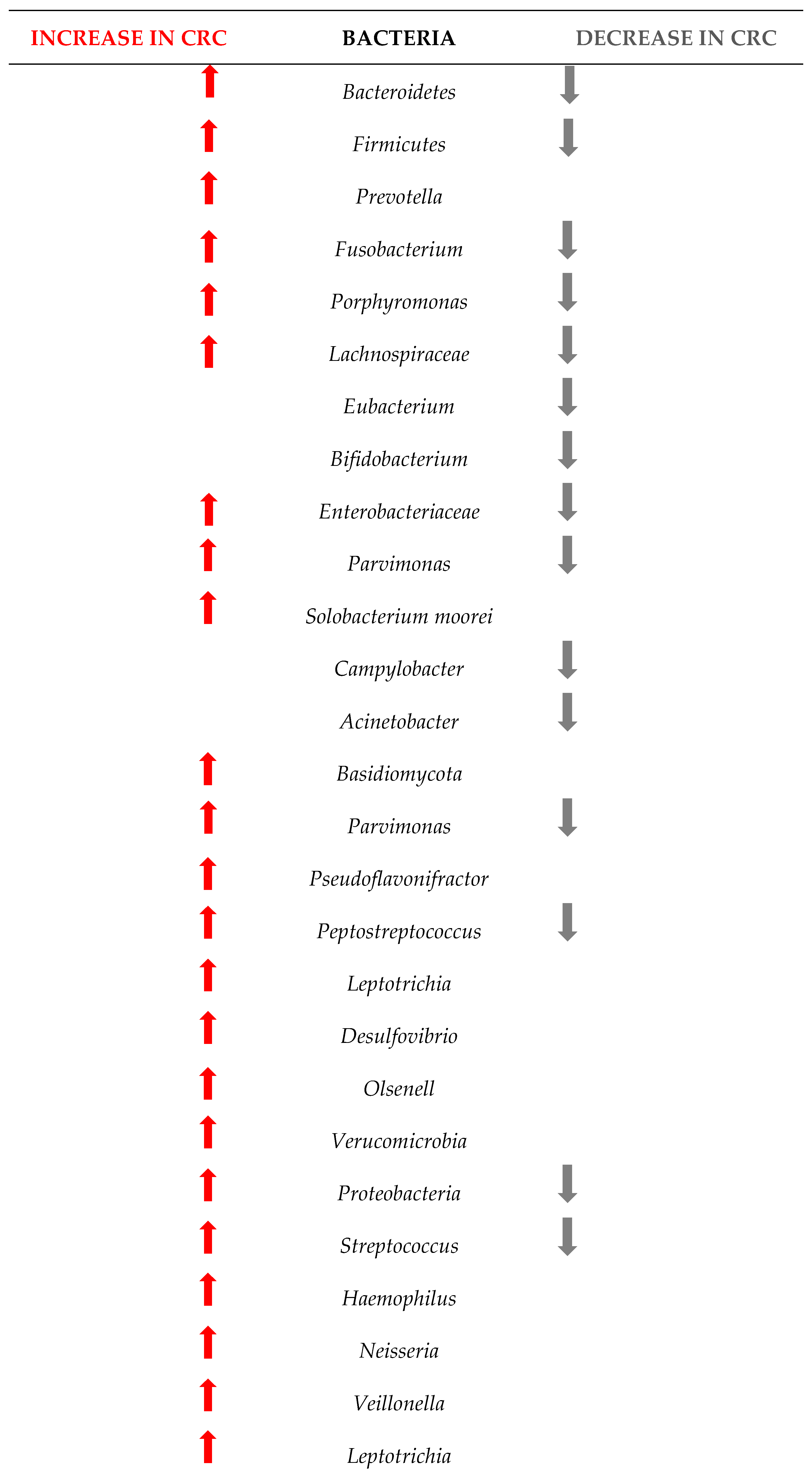
3.2. Potential Biomarkers for the CRC
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- O’Sullivan, D.E.; Sutherland, R.L.; Town, S.; Chow, K.; Fan, J.; Forbes, N.; Heitman, S.J.; Hilsden, R.J.; Brenner, D.R. Risk Factors for Early-Onset Colorectal Cancer: A Systematic Review and Meta-analysis. Clin. Gastroenterol. Hepatol. 2022, 20, 1229–1240.e5. [Google Scholar] [CrossRef] [PubMed]
- Coughlin, S.S. Social determinants of colorectal cancer risk, stage, and survival: A systematic review. Int. J. Colorectal Dis. 2020, 35, 985–995. [Google Scholar] [CrossRef] [PubMed]
- Siegel, R.L.; Wagle, N.S.; Cercek, A.; Smith, R.A.; Jemal, A. Colorectal cancer statistics, 2023. CA Cancer J. Clin. 2023, 73, 233–254. [Google Scholar] [CrossRef] [PubMed]
- Rawla, P.; Sunkara, T.; Barsouk, A. Epidemiology of colorectal cancer: Incidence, mortality, survival, and risk factors. Prz. Gastroenterol. 2019, 14, 89–103. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Pardamean, C.I.; Sudigyo, D.; Budiarto, A.; Mahesworo, B.; Hidayat, A.A.; Baurley, J.W.; Pardamean, B. Changing Colorectal Cancer Trends in Asians: Epidemiology and Risk Factors. Oncol. Rev. 2023, 17, 10576. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hossain, M.S.; Karuniawati, H.; Jairoun, A.A.; Urbi, Z.; Ooi, J.; John, A.; Lim, Y.C.; Kibria, K.M.K.; Mohiuddin, A.K.M.; Ming, L.C.; et al. Colorectal Cancer: A Review of Carcinogenesis, Global Epidemiology, Current Challenges, Risk Factors, Preventive and Treatment Strategies. Cancers 2022, 14, 1732. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Maki, G.; Zervos, M. Health Care-Acquired Infections in Low- and Middle-Income Countries and the Role of Infection Prevention and Control. Infect. Dis. Clin. N. Am. 2021, 35, 827–839. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Toma, M.; Beluşică, L.; Stavarachi, M.; Apostol, P.; Spandole, S.; Radu, I.; Cimponeriu, D. Rating the environmental and genetic risk factors for colorectal cancer. J. Med. Life 2012, 5, 152–159. [Google Scholar] [PubMed] [PubMed Central]
- Tocia, C.; Dumitru, A.; Mateescu, B.; Negreanu, L.; State, M.; Cozaru, G.C.; Mitroi, A.F.; Brinzan, C.; Popescu, R.; Leopa, N.; et al. Tissue and Circulating MicroRNA-31, MicroRNA-200b, and MicroRNA-200c Reflects Disease Activity in Crohn’s Disease Patients: Results from the BIOMIR Study. J. Gastrointest. Liver Dis. 2023, 32, 30–38. [Google Scholar] [CrossRef] [PubMed]
- Durko, L.; Malecka-Panas, E. Lifestyle Modifications and Colorectal Cancer. Curr. Colorectal Cancer Rep. 2014, 10, 45–54. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mindrescu, N.M.; Guja, C.; Jinga, V.; Ispas, S.; Curici, A.; Nelson Twakor, A.; Pantea Stoian, A.M. Interactions between Gut Microbiota and Oral Antihyperglycemic Drugs: A Systematic Review. Int. J. Mol. Sci. 2024, 25, 3540. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Nicolae, M.; Mihai, C.M.; Chisnoiu, T.; Balasa, A.L.; Frecus, C.E.; Mihai, L.; Lupu, V.V.; Ion, I.; Pantazi, A.C.; Nelson Twakor, A.; et al. Immunomodulatory Effects of Vitamin D in Respiratory Tract Infections and COVID-19 in Children. Nutrients 2023, 15, 3430. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Minhajat, R.; Harjianti, T.; Rasyid, H.; Bukhari, A.; Chaidir Islam, I.; Zainal, A.T.F.; Khaliq Gunawan, A.M.A.; Ramadhan, A.C.; Hatta, H.; Syamsu Alam, N.I.; et al. Colorectal cancer patients’ outcome in correlation with dietary and nutritional status: A systematic review. Ann. Med. 2023, 55, 2281662. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bhimani, N.; Wong, G.Y.M.; Molloy, C.; Pavlakis, N.; Diakos, C.I.; Clarke, S.J.; Dieng, M.; Hugh, T.J. Cost of treating metastatic colorectal cancer: A systematic review. Public Health 2022, 211, 97–104. [Google Scholar] [CrossRef] [PubMed]
- Syvyk, S.; Roberts, S.E.; Finn, C.B.; Wirtalla, C.; Kelz, R. Colorectal cancer disparities across the continuum of cancer care: A systematic review and meta-analysis. Am. J. Surg. 2022, 224, 323–331. [Google Scholar] [CrossRef] [PubMed]
- Verma, M.; Kumar, V. Epigenetic Biomarkers in Colorectal Cancer. Mol. Diagn. Ther. 2017, 21, 153–165. [Google Scholar] [CrossRef] [PubMed]
- Ispas, S.; Tuta, L.A.; Botnarciuc, M.; Ispas, V.; Staicovici, S.; Ali, S.; Nelson-Twakor, A.; Cojocaru, C.; Herlo, A.; Petcu, A. Metabolic Disorders, the Microbiome as an Endocrine Organ, and Their Relations with Obesity: A Literature Review. J. Pers. Med. 2023, 13, 1602. [Google Scholar] [CrossRef]
- Feng, Y.L.; Shu, L.; Zheng, P.F.; Zhang, X.Y.; Si, C.J.; Yu, X.L.; Gao, W.; Zhang, L. Dietary patterns and colorectal cancer risk: A meta-analysis. Eur. J. Cancer Prev. 2017, 26, 201–211. [Google Scholar] [CrossRef] [PubMed]
- Sonbol, M.B.; Mountjoy, L.J.; Firwana, B.; Liu, A.J.; Almader-Douglas, D.; Mody, K.; Hubbard, J.; Borad, M.; Ahn, D.H.; Murad, M.H.; et al. The Role of Maintenance Strategies in Metastatic Colorectal Cancer: A Systematic Review and Network Meta-analysis of Randomized Clinical Trials. JAMA Oncol. 2020, 6, e194489. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Tocia, C.; Alexandrescu, L.; Dumitru, E. Sa1892—Nutritional Status Correlates with Quality of Life in Active Crohn’s Disease. Gastroenterology 2019, 156, S-444. [Google Scholar] [CrossRef]
- Puli, A.V.; Lussiez, A.; MacEachern, M.; Hayward, L.; Dualeh, S.; Richburg, C.E.; Capellari, E.; Kwakye, G. Barriers to Colorectal Cancer Screening in US Immigrants: A Scoping Review. J. Surg. Res. 2023, 282, 53–64. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bopanna, S.; Ananthakrishnan, A.N.; Kedia, S.; Yajnik, V.; Ahuja, V. Risk of colorectal cancer in Asian patients with ulcerative colitis: A systematic review and meta-analysis. Lancet Gastroenterol. Hepatol. 2017, 2, 269–276. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Tocia, C.; Iordache, M.M.; Manea, M.; Cozaru, G.C.; Chisoi, A.; Dumitru, A.; Rafti, R.; Cornea, V.; Dina, E.; Alexandrescu, L.; et al. Sa1623: THE LINK BETWEEN PSYCHOLOGICAL STATE AND INTESTINAL PERMEABILITY IN PATIENTS WITH IBD IN REMISSION. Gastroenterology 2022, 162, S-443–S-444. [Google Scholar] [CrossRef]
- Christodoulides, N.; Lami, M.; Malietzis, G.; Rasheed, S.; Tekkis, P.; Kontovounisios, C. Sporadic colorectal cancer in adolescents and young adults: A scoping review of a growing healthcare concern. Int. J. Colorectal Dis. 2020, 35, 1413–1421. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Belkaid, Y.; Hand, T.W. Role of the microbiota in immunity and inflammation. Cell 2014, 157, 121–141. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Nenkov, M.; Ma, Y.; Gaßler, N.; Chen, Y. Metabolic Reprogramming of Colorectal Cancer Cells and the Microenvironment: Implication for Therapy. Int. J. Mol. Sci. 2021, 22, 6262. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zou, S.; Fang, L.; Lee, M.H. Dysbiosis of gut microbiota in promoting the development of colorectal cancer. Gastroenterol. Rep. 2018, 6, 1–12. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Winawer, S.J.; Krabshuis, J.; Lambert, R.; O’Brien, M.; Fried, M.; World Gastroenterology Organization Guidelines Committee. Cascade colorectal cancer screening guidelines: A global conceptual model. J. Clin. Gastroenterol. 2011, 45, 297–300. [Google Scholar] [CrossRef] [PubMed]
- Eriksen, M.B.; Frandsen, T.F. The impact of patient, intervention, comparison, outcome (PICO) as a search strategy tool on literature search quality: A systematic review. J. Med. Libr. Assoc. 2018, 106, 420–431. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Flemer, B.; Lynch, D.B.; Brown, J.M.; Jeffery, I.B.; Ryan, F.J.; Claesson, M.J.; O’Riordain, M.; Shanahan, F.; O.′Toole, P.W. Tumour-associated and non-tumour-associated microbiota in colorectal cancer. Gut 2017, 66, 633–643. [Google Scholar] [CrossRef] [PubMed]
- Zackular, J.P.; Rogers, M.A.; Ruffin, M.T.; Schloss, P.D., 4th. The human gut microbiome as a screening tool for colorectal cancer. Cancer Prev. Res. 2014, 7, 1112–1121. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Yu, J.; Feng, Q.; Wong, S.H.; Zhang, D.; Liang, Q.Y.; Qin, Y.; Tang, L.; Zhao, H.; Stenvang, J.; Li, Y.; et al. Metagenomic analysis of faecal microbiome as a tool towards targeted non-invasive biomarkers for colorectal cancer. Gut 2017, 66, 70–78. [Google Scholar] [CrossRef] [PubMed]
- Zeller, G.; Tap, J.; Voigt, A.Y.; Sunagawa, S.; Kultima, J.R.; Costea, P.I.; Amiot, A.; Böhm, J.; Brunetti, F.; Habermann, N.; et al. Potential of fecal microbiota for early-stage detection of colorectal cancer. Mol. Syst. Biol. 2014, 10, 766. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zhong, X.; Wang, Y.; Xu, J.; Cao, H.; Zhang, F.; Wang, X. Gut microbiota signatures in tissues of the colorectal polyp and normal colorectal mucosa, and faeces. Front. Cell. Infect. Microbiol. 2023, 12, 1054808. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Li, Y.; Cao, H.; Fei, B.; Gao, Q.; Yi, W.; Han, W.; Bao, C.; Xu, J.; Zhao, W.; Zhang, F. Gut Microbiota Signatures in Tumor, Para-Cancerous, Normal Mucosa, and Feces in Colorectal Cancer Patients. Front. Cell Dev. Biol. 2022, 10, 916961. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kordahi, M.C.; Stanaway, I.B.; Avril, M.; Chac, D.; Blanc, M.P.; Ross, B.; Diener, C.; Jain, S.; McCleary, P.; Parker, A.; et al. Genomic and functional characterization of a mucosal symbiont involved in early-stage colorectal cancer. Cell Host Microbe 2021, 29, 1589–1598.e6. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Flemer, B.; Warren, R.D.; Barrett, M.P.; Cisek, K.; Das, A.; Jeffery, I.B.; Hurley, E.; O’Riordain, M.; Shanahan, F.; O’Toole, P.W. The oral microbiota in colorectal cancer is distinctive and predictive. Gut 2018, 67, 1454–1463. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sheng, Q.S.; He, K.X.; Li, J.J.; Zhong, Z.F.; Wang, F.X.; Pan, L.L.; Lin, J.J. Comparison of Gut Microbiome in Human Colorectal Cancer in Paired Tumor and Adjacent Normal Tissues. OncoTargets Ther. 2020, 13, 635–646. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Geng, J.; Fan, H.; Tang, X.; Zhai, H.; Zhang, Z. Diversified pattern of the human colorectal cancer microbiome. Gut Pathog. 2013, 5, 2. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Thomas, A.M.; Manghi, P.; Asnicar, F.; Pasolli, E.; Armanini, F.; Zolfo, M.; Beghini, F.; Manara, S.; Karcher, N.; Pozzi, C.; et al. Metagenomic analysis of colorectal cancer datasets identifies cross-cohort microbial diagnostic signatures and a link with choline degradation. Nat. Med. 2019, 25, 667–678, Erratum in Nat. Med. 2019, 25, 1948. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Yachida, S.; Mizutani, S.; Shiroma, H.; Shiba, S.; Nakajima, T.; Sakamoto, T.; Watanabe, H.; Masuda, K.; Nishimoto, Y.; Kubo, M.; et al. Metagenomic and metabolomic analyses reveal distinct stage-specific phenotypes of the gut microbiota in colorectal cancer. Nat. Med. 2019, 25, 968–976. [Google Scholar] [CrossRef]
- Zepeda-Rivera, M.; Minot, S.S.; Bouzek, H.; Wu, H.; Blanco-Míguez, A.; Manghi, P.; Jones, D.S.; LaCourse, K.D.; Wu, Y.; McMahon, E.F.; et al. A distinct Fusobacterium nucleatum clade dominates the colorectal cancer niche. Nature 2024, 628, 424–432. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Nouri, R.; Hasani, A.; Masnadi Shirazi, K.; Alivand, M.R.; Sepehri, B.; Sotoudeh, S.; Hemmati, F.; Fattahzadeh, A.; Abdinia, B.; Ahangarzadeh Rezaee, M. Mucosa-Associated Escherichia coli in Colorectal Cancer Patients and Control Subjects: Variations in the Prevalence and Attributing Features. Can. J. Infect. Dis. Med. Microbiol. 2021, 2021, 2131787. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Cheng, W.T.; Kantilal, H.K.; Davamani, F. The Mechanism of Bacteroides fragilis Toxin Contributes to Colon Cancer Formation. Malays. J. Med. Sci. 2020, 27, 9–21. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Coleman, O.; Haller, D. Dysbiosis of the Intestinal Microbiota and Colorectal Cancer; Elsevier eBooks; Academic Press: Cambridge, MA, USA, 2020. [Google Scholar] [CrossRef]
- Hou, X.; Zheng, Z.; Wei, J.; Zhao, L. Effects of gut microbiota on immune responses and immunotherapy in colorectal cancer. Front. Immunol. 2022, 13, 1030745. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Tocia, C.; Dumitru, I.M.; Alexandrescu, L.; Petcu, L.C.; Dumitru, E. Does rifaximin offer any promise in Crohn’s disease in remission and concurrent irritable bowel syndrome-like symptoms? Medicine 2021, 100, e24059. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kobiela, J.; Spychalski, P.; Marvaso, G.; Ciardo, D.; Dell′Acqua, V.; Kraja, F.; Błażyńska-Spychalska, A.; Łachiński, A.J.; Surgo, A.; Glynne-Jones, R.; et al. Ablative stereotactic radiotherapy for oligometastatic colorectal cancer: Systematic review. Crit. Rev. Oncol. Hematol. 2018, 129, 91–101. [Google Scholar] [CrossRef] [PubMed]
- Hofmann, B. Ethical issues with colorectal cancer screening-a systematic review. J. Eval. Clin. Pract. 2017, 23, 631–641. [Google Scholar] [CrossRef] [PubMed]
- Cioffi, I.; Imperatore, N.; Di Vincenzo, O.; Santarpia, L.; Rispo, A.; Marra, M.; Testa, A.; Contaldo, F.; Castiglione, F.; Pasanisi, F. Association between Health-Related Quality of Life and Nutritional Status in Adult Patients with Crohn’s Disease. Nutrients 2020, 12, 746. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zhao, H.; He, M.; Zhang, M.; Sun, Q.; Zeng, S.; Chen, L.; Yang, H.; Liu, M.; Ren, S.; Meng, X.; et al. Colorectal Cancer, Gut Microbiota and Traditional Chinese Medicine: A Systematic Review. Am. J. Chin. Med. 2021, 49, 805–828. [Google Scholar] [CrossRef] [PubMed]
- Jaspan, V.; Lin, K.; Popov, V. The impact of anthropometric parameters on colorectal cancer prognosis: A systematic review and meta-analysis. Crit. Rev. Oncol. Hematol. 2021, 159, 103232. [Google Scholar] [CrossRef] [PubMed]
- Dumitru, E.; Alexandrescu, L.; Suceveanu, A.I.; Dumitru, I.M.; Tofolean, I.T. M1255 Fecal Calprotectin in Diagnosis of Complicated Colonic Diverticular Disease. Gastroenterology 2010, 138, S365. [Google Scholar] [CrossRef]
- Dawson, P.A.; Karpen, S.J. Intestinal transport and metabolism of bile acids. J. Lipid Res. 2015, 56, 1085–1099. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wu, Y.; Jiao, N.; Zhu, R.; Zhang, Y.; Wu, D.; Wang, A.J.; Fang, S.; Tao, L.; Li, Y.; Cheng, S.; et al. Identification of microbial markers across populations in early detection of colorectal cancer. Nat. Commun. 2021, 12, 3063. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zhu, X.; Xu, P.; Zhu, R.; Gao, W.; Yin, W.; Lan, P.; Zhu, L.; Jiao, N. Multi-kingdom microbial signatures in excess body weight colorectal cancer based on global metagenomic analysis. Commun. Biol. 2024, 7, 24. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ou, S.; Wang, H.; Tao, Y.; Luo, K.; Ye, J.; Ran, S.; Guan, Z.; Wang, Y.; Hu, H.; Huang, R. Fusobacterium nucleatum and colorectal cancer: From phenomenon to mechanism. Front. Cell. Infect. Microbiol. 2022, 12, 1020583. [Google Scholar] [CrossRef] [PubMed]
- Buc, E.; Dubois, D.; Sauvanet, P.; Raisch, J.; Delmas, J.; Darfeuille-Michaud, A.; Pezet, D.; Bonnet, R. High prevalence of mucosa-associated E. coli producing cyclomodulin and genotoxin in colon cancer. PLoS ONE 2013, 8, e56964. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wang, Y.; Fu, K. Genotoxins: The Mechanistic Links between Escherichia coli and Colorectal Cancer. Cancers 2023, 15, 1152. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sadeghi, M.; Mestivier, D.; Sobhani, I. Contribution of pks+ Escherichia coli (E. coli) to Colon Carcinogenesis. Microorganisms 2024, 12, 1111. [Google Scholar] [CrossRef]
- Jia, W.; Xie, G.; Jia, W. Bile acid-microbiota crosstalk in gastrointestinal inflammation and carcinogenesis. Nat. Rev. Gastroenterol. Hepatol. 2018, 15, 111–128. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Duizer, C.; de Zoete, M.R. The Role of Microbiota-Derived Metabolites in Colorectal Cancer. Int. J. Mol. Sci. 2023, 24, 8024. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ismael, S.; Rodrigues, C.; Santos, G.M.; Castela, I.; Barreiros-Mota, I.; Almeida, M.J.; Calhau, C.; Faria, A.; Araújo, J.R. IPA and its precursors differently modulate the proliferation, differentiation, and integrity of intestinal epithelial cells. Nutr. Res. Pract. 2023, 17, 616–630. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Snezhkina, A.V.; Krasnov, G.S.; Lipatova, A.V.; Sadritdinova, A.F.; Kardymon, O.L.; Fedorova, M.S.; Melnikova, N.V.; Stepanov, O.A.; Zaretsky, A.R.; Kaprin, A.D.; et al. The Dysregulation of Polyamine Metabolism in Colorectal Cancer Is Associated with Overexpression of c-Myc and C/EBPβ rather than Enterotoxigenic Bacteroides fragilis Infection. Oxid. Med. Cell Longev. 2016, 2016, 2353560. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wirbel, J.; Pyl, P.T.; Kartal, E.; Zych, K.; Kashani, A.; Milanese, A.; Fleck, J.S.; Voigt, A.Y.; Palleja, A.; Ponnudurai, R.; et al. Meta-analysis of fecal metagenomes reveals global microbial signatures that are specific for colorectal cancer. Nat. Med. 2019, 25, 679–689. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]

| Study | PICO Framework | Key Results | Microbiota Involvement in CRC |
|---|---|---|---|
| Flemer et al. [30] | Population: total of 136 participants Intervention: microbiota composition was analyzed using 16S rRNA amplicon sequencing, while the expression of host genes related to colorectal cancer development and immune response was measured using real-time quantitative PCR Comparison: 59 patients undergoing surgery for CRC, 21 individuals with polyps and 56 healthy controls Outcome: to assess if the microbiome profiles associated with CRC vary from those in healthy individuals and if they are correlated with certain gene-expression patterns in the mucosa | The microbiota of patients with CRC showed differences compared to the microbiota of healthy individuals. However, these modifications were not limited to the malignant tissue alone. The study identified differences between distal and proximal malignancies and found that the composition of the fecal microbiota only partly matched that of the mucosal microbiome in CRC. Patients with colorectal cancer may be categorized based on higher-level structures of mucosal-associated bacterial co-abundance groups (CAGs) that reflect the enterotypes. The correlation between CRC-associated CAGs and the expression of host immunoinflammatory response genes varied. The presence of Firmicutes Cluster 1 and Bacteroidetes Cluster 1 in the microbiota of CRC patients was significantly lower. On the other hand, the abundance of Firmicutes Cluster 2, Prevotella Cluster, Pathogen Cluster, and Bacteroidetes Cluster 2 was higher in the CRC biopsy microbiota. | INCREASE in:
and DECREASE in:
|
| Zackular et al. [31] | Population: total of 90 participants Intervention: microbiota was analyzed by sequencing the V4 region of the 16S rRNA gene from the feces of each individual using the Illumina MiSeq sequencing platform Comparison: 30 patients with CRC, 30 patients with adenoma, and 30 healthy individuals as control group Outcome: to compare the microbiome of healthy individuals, persons with adenomas, and patients with colorectal carcinomas | Compared to healthy subjects, individuals with carcinomas were found to have higher levels of certain microorganisms, specifically Fusobacterium, Porphyromonas, Lachnospiraceae (OTUs 31, 59, 32, 116, 85), and Enterobacteriaceae. On the other hand, they had lower levels of microorganisms associated with Bacteroides, Lachnospiraceae (OTUs 23, 30, 253, 136), and Clostridiales. | INCREASE in:
and DECREASE in:
|
| Yu et al. [32] | Population: even though the study collects data from multiple countries, we selected only the ones in which feces were analyzed. Thus, for this review, we selected the 128 individuals from China Intervention: metagenomic sequencing on the stool samples Comparison: 74 patients with CRC and 54 control subjects Outcome: to examine taxonomic differences between CRC-associated and control microbiomes, and to identify microbial taxa contributing to the dysbiosis | The findings indicate a disbyosis in the gut microbiota of people with CRC. Leucine promotes both the creation and breakdown of proteins, indicating potential connections between leucine metabolism and cancer. Significant relationships between illness state and various KEGG orthologous groupings were observed at the gene level. The presence of Eubacterium ventriosum was consistently higher in the microbiomes of the control group. However, Parvimonas micra, Solobacterium moorei, Fusobacterium nucleatum, and Peptostreptococcus stomatis were consistently found in higher abundance in the microbiomes of patients with colorectal cancer. At the phylum level, only the Fusobacteria and Basidiomycota were shown to be considerably more abundant in microbiomes linked with colorectal cancer. | INCREASE in:
|
| Zeller et al. [33] | Population: 391 participants from France, Germany, Denmark and Spain Intervention: metagenomic sequencing of fecal samples to identify taxonomic markers that distinguished CRC patients from tumor-free controls Comparison: 358 healthy individuals, 42 patients with adenoma, 91 patients with CRC Outcome: to compare the microbiota from patients with adenomas to neoplasia-free controls and to patients with colorectal cancer | Despite variations in patient country or origin, experimental methodologies, and analytic methodology, there are similarities in the relative abundances of certain species from fecal samples from CRC patients. These findings indicate that analyzing fecal samples may provide insights into the metabolic and functional capabilities of the colonic microbiome in the tumor setting. | INCREASE in:
and DECREASE in:
|
| Zhong et al. [34] | Population: 40 participants Intervention: 16S rRNA gene sequencing of the microbiota present in the normal colorectal mucosa and colorectal polyps Comparison: microbial composition of the colorectal polyp tissue and fecal samples (24 adults) and of the normal intestinal mucosal tissue and fecal samples (16 adults) Outcome: to find out if the microbial structure in feces differs from that in tissues of polyp and normal mucosa | The differential genera seen in the normal colorectal mucosa and the stool sample of individuals with colorectal polyps were similar to those observed between the fecal sample and the polyp tissue. In both groups, the levels of Bacteroides, Prevotella-2, and Agathobacter were higher, while the levels of Haemophilus, Escherichia_Shigella, Fusobacterium, and Streptococcus were lower in feces compared to the normal mucosa in both groups or polyp tissues. There was no notable difference in the presence of Fusobacterium between the typical colorectal mucosa and polyps in individuals with colorectal polyps. However, it was much greater in both the mucosa and polyps compared to the fecal matter. There was a greater presence of Fusobacterium in the normal intestinal mucosa of healthy persons compared to the polyp group. | INCREASE in:
and DECREASE in:
|
| Li et al. [35] | Population: 98 CRC participants Intervention: microbial community genomic DNA was extracted from 200 mg fecal samples or 300 mg tissue samples Comparison: three types of colorectal mucosa (tumor mucosa, para-cancerous mucosa, normal mucosa) and feces Outcome: to find out if there are variations between tumor mucosal microbiota and normal mucosal microbiota | The study found important variations between tumor mucosal microbiota and normal mucosal microbiota, but no notable difference was seen in the microbiota between the tumor and para-tumor mucosa, as well as between the para-tumor and normal mucosa. This suggests that the microbiota in the para-cancerous mucosa serves as an intermediate stage between the microbiota in the tumor and normal mucosa. The significant changes in the composition of the fecal microbiota, when compared to the mucosal microbiota, suggest that utilizing the fecal microbiota as a definition for the mucosal microbiota carries a certain level of risk. A robust link was identified between a positive result on the fecal occult blood test and the presence of Fusobacterium. This suggests that this particular genus, known for its ability to attach to and invade the intestines, is strongly associated with intestinal bleeding. In addition, we have discovered six main types of bacteria, namely Fusobacterium, Gemella, Campylobacter, Peptostreptococcus, Alloprevotella, and Parvimonas, that consistently show higher presence in tumor tissue compared to normal tissue and/or in tissue compared to feces. | INCREASE in:
and DECREASE in:
|
| Kordahi et al. [36] | Population: 40 participants Intervention: two biopsies were collected from CRC patients: one from the area surrounding the polyp or polyp adjacent and another from the macroscopically healthy mucosa situated at least 10 cm distant from the polyp, and one biopsy from the healthy mucosa of control subjects Comparison: 31 patients with CRC and 9 individuals in the control group Outcome: to gain insight into the microbial microenvironment of the pre-neoplastic polyp as compared to the healthy mucosa | There is a clear difference in the types of microorganisms present in the mucosa that is next to pre-neoplastic colonic polyps compared to the mucosa of individuals who are polyp-free. During the first phases of polyp development, it is possible that an imbalanced and inflammatory gut environment enables the growth or establishment of nontoxigenic B. fragilis that possess an abundance of genes responsible for the production of lipopolysaccharides. | INCREASE in:
and DECREASE in:
|
| Flemer et al. [37] | Population: 234 participants Intervention: the microbiota was analyzed from oral swabs, colonic mucosae and stool of the subjects Comparison: 99 CRC patients, 32 colorectal polyps patients and 103 Controls. Outcome: to find out if microbiota alterations are linked with colorectal cancer | The most prevalent bacterial species found in all oral swab samples were Streptococcus (over 30%), Haemophilus (14.2%), Neisseria (almost 9%), Prevotella (6.6%), Fusobacterium and Veillonella (over 5%), Leptotrichia and Rothia (almost 4%), Actinomyces (2.9%), and Porphyromonas (2.4%). | INCREASE in:
and DECREASE in:
|
| Sheng et al. [38] | Population: 66 CRC patients Intervention: all paired tumor and adjacent normal tissue samples were dissected and frozen immediately after collection and stored at −80 °C until DNA extraction Comparison: microbiota of the tumor mucosa with that one of the normal mucosa Outcome: to find out if there are any microbiota linked with colorectal cancer | 7 microbe genus (Fusobacterium, Faecalibacterium, Akkermansia, Ruminococcus, Parabacteroides, Streptococcus, and Ruminococcaceae) were significantly different between tumor and adjacent normal tissues; and 5 microbe genus (Bacteroides, Fusobacterium, Faecalibacterium, Parabacteroides, and Ruminococcus) were also different between distal and proximal CRC segments. | INCREASE in:
and DECREASE in:
|
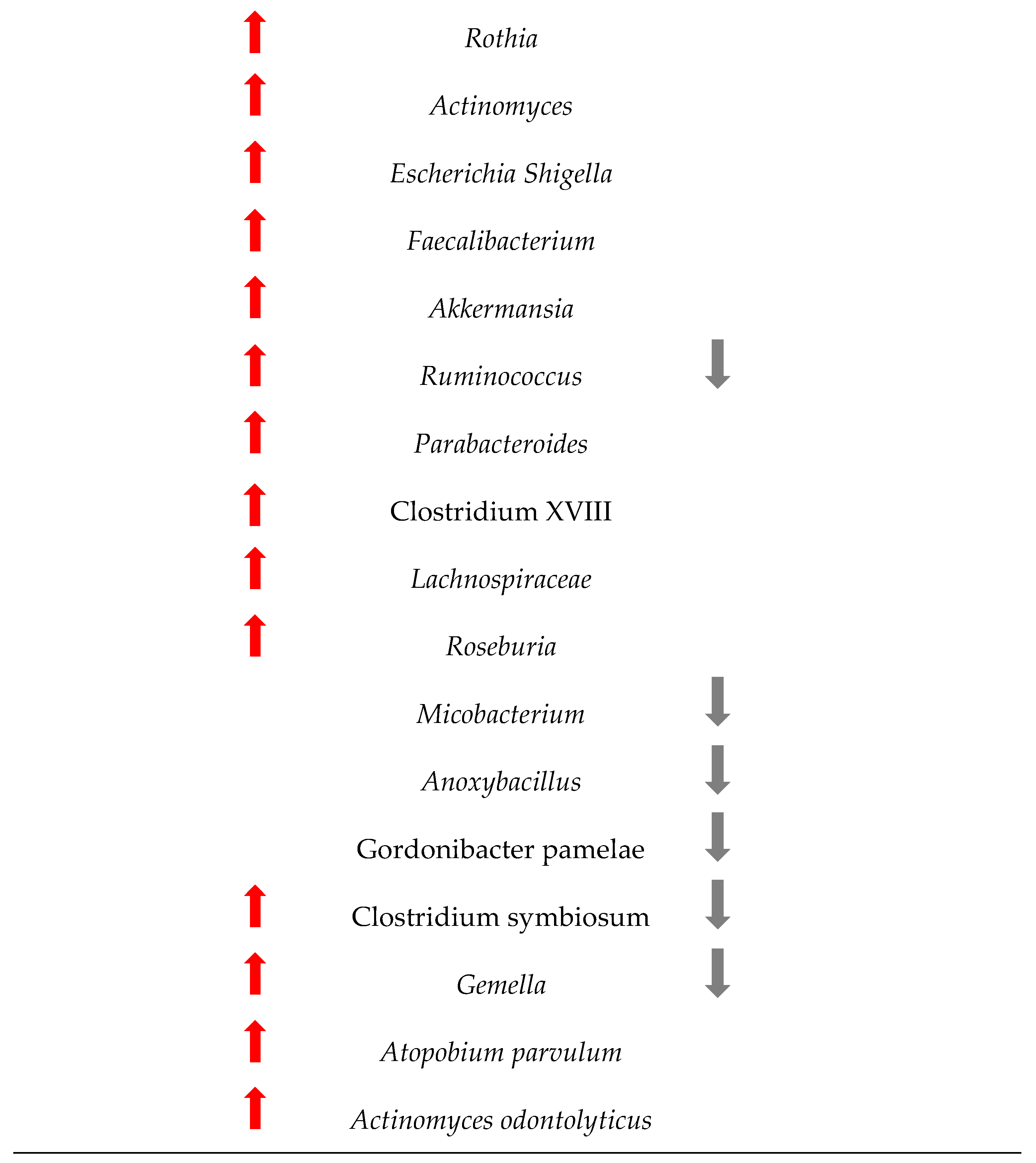
| Geng et al. [39] | Population: 8 patients with CRC Intervention: 16S rRNA gene sequences of biopsy samples taken from both healthy and tumor mucosa Comparison: between microbiota of normal mucosa and tumor mucosa Outcome: to quantitatively evaluate the differences of bacterial communities and compositions between eight tumor/normal pairs | The research identified two distinct patterns of change associated with each of the three major bacterial taxa in the gut (Roseburia, Microbacterium, and Anoxybacillus). | INCREASE in:
and DECREASE in:
|
| Thomas et al. [40] | Population: 764 participants Intervention: participants underwent colonoscopy to diagnose CRC, adenoma, or to confirm the absence of disease, with samples collected before diagnosis or beginning of treatment Comparison: stool microbiome from 313 CRC patients, 143 subjects with adenoma and 303 controls Outcome: to establish consistent correlations between the gut microbiota and colorectal cancer | There is a much greater number of species that are more abundant in individuals with colorectal cancer compared to those without the disease (controls). The functional capacity of the microbiome was shown to be strongly linked to colorectal cancer samples in comparison to healthy subjects. | INCREASE in:
and DECREASE in:
|
| Yachida et al. [41] | Population: 616 patients Intervention: metagenomic and metabolomic markers were identified to separate cases of intramucosal carcinoma from the healthy controls Comparison: 146 healthy subjects and 470 patients with different stages of CRC Outcome: to demonstrate possible associations between the gut microbiota and colorectal cancer | The abundance of certain species belonging to the phyla Firmicutes, Fusobacteria, and Bacteroidetes was consistently higher and correlated with the severity of malignancy. Fusobacteria of higher taxonomic rank were seen in at least two distinct phases, but numerous species from the Firmicutes and Bacteroidetes phyla were exclusive to a particular stage. Within the phylum Proteobacteria, a significant number of species were shown to be increased in patients with colorectal cancer. The population of the Bifidobacterium genus was mostly reduced in early stages of CRC. | INCREASE in:
and DECREASE in:
|
| Study | CRC Mucosa or Stool Samples (n = 1363) | Other Polyps or Adenoma Mucosa or Stool Samples (n = 268) | Healthy Mucosa or Stool Samples (n = 1252) |
|---|---|---|---|
| Flemer et al. [30] | 59 | 21 | 56 |
| Zackular et al. [31] | 30 | 30 | 30 |
| Yu et al. [32] | 74 | N/A | 54 |
| Zeller et al. [33] | 91 | 42 | 358 |
| Zhong et al. [34] | 24 | N/A | 16 |
| Li et al. [35] | 98 | N/A | 98 |
| Kordahi et al. [36] | 31 | N/A | 9 |
| Flemer et al. [37] | 99 | 32 | 103 |
| Sheng et al. [38] | 66 | N/A | 66 |
| Geng et al. [39] | 8 | N/A | 8 |
| Thomas et al. [40] | 313 | 143 | 308 |
| Yachida et al. [41] | 470 | N/A | 146 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Herlo, L.-F.; Salcudean, A.; Sirli, R.; Iurciuc, S.; Herlo, A.; Nelson-Twakor, A.; Alexandrescu, L.; Dumache, R. Gut Microbiota Signatures in Colorectal Cancer as a Potential Diagnostic Biomarker in the Future: A Systematic Review. Int. J. Mol. Sci. 2024, 25, 7937. https://doi.org/10.3390/ijms25147937
Herlo L-F, Salcudean A, Sirli R, Iurciuc S, Herlo A, Nelson-Twakor A, Alexandrescu L, Dumache R. Gut Microbiota Signatures in Colorectal Cancer as a Potential Diagnostic Biomarker in the Future: A Systematic Review. International Journal of Molecular Sciences. 2024; 25(14):7937. https://doi.org/10.3390/ijms25147937
Chicago/Turabian StyleHerlo, Lucian-Flavius, Andreea Salcudean, Roxana Sirli, Stela Iurciuc, Alexandra Herlo, Andreea Nelson-Twakor, Luana Alexandrescu, and Raluca Dumache. 2024. "Gut Microbiota Signatures in Colorectal Cancer as a Potential Diagnostic Biomarker in the Future: A Systematic Review" International Journal of Molecular Sciences 25, no. 14: 7937. https://doi.org/10.3390/ijms25147937
APA StyleHerlo, L.-F., Salcudean, A., Sirli, R., Iurciuc, S., Herlo, A., Nelson-Twakor, A., Alexandrescu, L., & Dumache, R. (2024). Gut Microbiota Signatures in Colorectal Cancer as a Potential Diagnostic Biomarker in the Future: A Systematic Review. International Journal of Molecular Sciences, 25(14), 7937. https://doi.org/10.3390/ijms25147937








