Lysophosphatidic Acid (LPA) and Its Receptors in Mood Regulation: A Systematic Review of the Molecular Mechanisms and Therapeutic Potential
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Chiurchiù, V.; Maccarrone, M. Bioactive lipids as modulators of immunity, inflammation and emotions. Curr. Opin. Pharmacol. 2016, 29, 54–62. [Google Scholar] [CrossRef] [PubMed]
- Twenge, J.M.; Cooper, A.B.; Joiner, T.E.; Duffy, M.E.; Binau, S.G. Age, period, and cohort trends in mood disorder indicators and suicide-related outcomes in a nationally representative dataset, 2005–2017. J. Abnorm. Psychol. 2019, 128, 185–199. [Google Scholar] [CrossRef] [PubMed]
- Akirav, I.; Maroun, M. The role of the medial prefrontal cortex-amygdala circuit in stress effects on the extinction of fear. Neural Plast. 2007, 2007, 30873. [Google Scholar] [CrossRef] [PubMed]
- Nagy, C.; Maitra, M.; Tanti, A.; Suderman, M.; Théroux, J.F.; Davoli, M.A.; Perlman, K.; Yerko, V.; Wang, Y.C.; Tripathy, S.J.; et al. Single-nucleus transcriptomics of the prefrontal cortex in major depressive disorder implicates oligodendrocyte precursor cells and excitatory neurons. Nat. Neurosci. 2020, 23, 771–781. [Google Scholar] [CrossRef] [PubMed]
- Malhi, G.S.; Mann, J.J. Depression. Lancet 2018, 392, 2299–2312. [Google Scholar] [CrossRef] [PubMed]
- Stetler, C.; Miller, G.E. Depression and hypothalamic-pituitary-adrenal activation: A quantitative summary of four decades of research. Psychosom. Med. 2011, 73, 114–126. [Google Scholar] [CrossRef] [PubMed]
- Cui, L.; Li, S.; Wang, S.; Wu, X.; Liu, Y.; Yu, W.; Wang, Y.; Tang, Y.; Xia, M.; Li, B. Major depressive disorder: Hypothesis, mechanism, prevention and treatment. Signal Transduct. Target. Ther. 2024, 9, 30. [Google Scholar] [CrossRef] [PubMed]
- Bandelow, B.; Michaelis, S. Epidemiology of anxiety disorders in the 21st century. Dialogues Clin. Neurosci. 2015, 17, 327–335. [Google Scholar] [CrossRef] [PubMed]
- Kessler, R.C.; Berglund, P.; Demler, O.; Jin, R.; Merikangas, K.R.; Walters, E.E. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch. Gen. Psychiatry 2005, 62, 593–602. [Google Scholar] [CrossRef]
- Goodwin, R.; Olfson, M. Treatment of panic attack and risk of major depressive disorder in the community. Am. J. Psychiatry 2001, 158, 1146–1148. [Google Scholar] [CrossRef]
- Davies, M.R.; Glen, K.; Mundy, J.; Ter Kuile, A.R.; Adey, B.N.; Armour, C.; Assary, E.; Coleman, J.R.I.; Goldsmith, K.A.; Hirsch, C.R.; et al. Factors associated with anxiety disorder comorbidity. J. Affect. Disord. 2023, 323, 280–291. [Google Scholar] [CrossRef] [PubMed]
- Aoki, J.; Taira, A.; Takanezawa, Y.; Kishi, Y.; Hama, K.; Kishimoto, T.; Mizuno, K.; Saku, K.; Taguchi, R.; Arai, H. Serum lysophosphatidic acid is produced through diverse phospholipase pathways. J. Biol. Chem. 2002, 277, 48737–48744. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.W.; Herr, D.R.; Noguchi, K.; Yung, Y.C.; Lee, C.W.; Mutoh, T.; Lin, M.E.; Teo, S.T.; Park, K.E.; Mosley, A.N.; et al. LPA receptors: Subtypes and biological actions. Annu. Rev. Pharmacol. Toxicol. 2010, 50, 157–186. [Google Scholar] [CrossRef] [PubMed]
- Sato, K.; Malchinkhuu, E.; Muraki, T.; Ishikawa, K.; Hayashi, K.; Tosaka, M.; Mochiduki, A.; Inoue, K.; Tomura, H.; Mogi, C.; et al. Identification of autotaxin as a neurite retraction-inducing factor of PC12 cells in cerebrospinal fluid and its possible sources. J. Neurochem. 2005, 92, 904–914. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.W.; Chun, J. Lysophospholipids and their receptors in the central nervous system. Biochim. Biophys. Acta 2013, 1831, 20–32. [Google Scholar] [CrossRef] [PubMed]
- Chun, J.; Hla, T.; Lynch, K.R.; Spiegel, S.; Moolenaar, W.H. International Union of Basic and Clinical Pharmacology. LXXVIII. Lysophospholipid receptor nomenclature. Pharmacol. Rev. 2010, 62, 579–587. [Google Scholar] [CrossRef] [PubMed]
- Noguchi, K.; Herr, D.; Mutoh, T.; Chun, J. Lysophosphatidic acid (LPA) and its receptors. Curr. Opin. Pharmacol. 2009, 9, 15–23. [Google Scholar] [CrossRef] [PubMed]
- Ye, X.; Ishii, I.; Kingsbury, M.A.; Chun, J. Lysophosphatidic acid as a novel cell survival/apoptotic factor. Biochim. Biophys. Acta 2002, 1585, 108–113. [Google Scholar] [CrossRef]
- Choi, S.H.; Jung, S.W.; Lee, B.H.; Kim, H.J.; Hwang, S.H.; Kim, H.K.; Nah, S.Y. Ginseng pharmacology: A new paradigm based on gintonin-lysophosphatidic acid receptor interactions. Front. Pharmacol. 2015, 6, 245. [Google Scholar] [CrossRef]
- Racké, K.; Schwörer, H. Characterization of the role of calcium and sodium channels in the stimulus secretion coupling of 5-hydroxytryptamine release from porcine enterochromaffin cells. Naunyn Schmiedebergs Arch. Pharmacol. 1993, 347, 1–8. [Google Scholar] [CrossRef]
- Andrews, P.L.; Horn, C.C. Signals for nausea and emesis: Implications for models of upper gastrointestinal diseases. Auton. Neurosci. 2006, 125, 100–115. [Google Scholar] [CrossRef] [PubMed]
- Endo, T.; Minami, M.; Hirafuji, M.; Ogawa, T.; Akita, K.; Nemoto, M.; Saito, H.; Yoshioka, M.; Parvez, S.H. Neurochemistry and neuropharmacology of emesis—The role of serotonin. Toxicology 2000, 153, 189–201. [Google Scholar] [CrossRef] [PubMed]
- Almeida-Montes, L.G.; Valles-Sanchez, V.; Moreno-Aguilar, J.; Chavez-Balderas, R.A.; García-Marín, J.A.; Cortés Sotres, J.F.; Hheinze-Martin, G. Relation of serum cholesterol, lipid, serotonin and tryptophan levels to severity of depression and to suicide attempts. J. Psychiatry Neurosci. 2000, 25, 371–377. [Google Scholar] [PubMed]
- Patkar, A.A.; Gopalakrishnan, R.; Naik, P.C.; Murray, H.W.; Vergare, M.J.; Marsden, C.A. Changes in plasma noradrenaline and serotonin levels and craving during alcohol withdrawal. Alcohol. Alcohol. 2003, 38, 224–231. [Google Scholar] [CrossRef] [PubMed]
- Whiting, P.F.; Rutjes, A.W.; Westwood, M.E.; Mallett, S.; Deeks, J.J.; Reitsma, J.B.; Leeflang, M.M.; Sterne, J.A.; Bossuyt, P.M. QUADAS-2: A revised tool for the quality assessment of diagnostic accuracy studies. Ann. Intern. Med. 2011, 155, 529–536. [Google Scholar] [CrossRef] [PubMed]
- Santin, L.J.; Bilbao, A.; Pedraza, C.; Matas-Rico, E.; López-Barroso, D.; Castilla-Ortega, E.; Sánchez-López, J.; Riquelme, R.; Varela-Nieto, I.; de la Villa, P.; et al. Behavioral phenotype of maLPA1-null mice: Increased anxiety-like behavior and spatial memory deficits. Genes. Brain Behav. 2009, 8, 772–784. [Google Scholar] [CrossRef] [PubMed]
- Castilla-Ortega, E.; Sánchez-López, J.; Hoyo-Becerra, C.; Matas-Rico, E.; Zambrana-Infantes, E.; Chun, J.; De Fonseca, F.R.; Pedraza, C.; Estivill-Torrús, G.; Santin, L.J. Exploratory, anxiety and spatial memory impairments are dissociated in mice lacking the LPA1 receptor. Neurobiol. Learn. Mem. 2010, 94, 73–82. [Google Scholar] [CrossRef] [PubMed]
- Callaerts-Vegh, Z.; Leo, S.; Vermaercke, B.; Meert, T.; D’Hooge, R. LPA5 receptor plays a role in pain sensitivity, emotional exploration and reversal learning. Genes. Brain Behav. 2012, 11, 1009–1019. [Google Scholar] [CrossRef]
- Pedraza, C.; Sánchez-López, J.; Castilla-Ortega, E.; Rosell-Valle, C.; Zambrana-Infantes, E.; García-Fernández, M.; Rodriguez de Fonseca, F.; Chun, J.; Santín, L.J.; Estivill-Torrús, G. Fear extinction and acute stress reactivity reveal a role of LPA(1) receptor in regulating emotional-like behaviors. Brain Struct. Funct. 2014, 219, 1659–1672. [Google Scholar] [CrossRef]
- Castilla-Ortega, E.; Escuredo, L.; Bilbao, A.; Pedraza, C.; Orio, L.; Estivill-Torrús, G.; Santín, L.J.; de Fonseca, F.R.; Pavón, F.J. 1-Oleoyl lysophosphatidic acid: A new mediator of emotional behavior in rats. PLoS ONE 2014, 9, e85348. [Google Scholar] [CrossRef]
- Yamada, M.; Tsukagoshi, M.; Hashimoto, T.; Oka, J.; Saitoh, A.; Yamada, M. Lysophosphatidic acid induces anxiety-like behavior via its receptors in mice. J. Neural Transm. 2015, 122, 487–494. [Google Scholar] [CrossRef] [PubMed]
- Castilla-Ortega, E.; Pavón, F.J.; Sánchez-Marín, L.; Estivill-Torrús, G.; Pedraza, C.; Blanco, E.; Suárez, J.; Santín, L.; Rodríguez de Fonseca, F.; Serrano, A. Both genetic deletion and pharmacological blockade of lysophosphatidic acid LPA1 receptor results in increased alcohol consumption. Neuropharmacology 2016, 103, 92–103. [Google Scholar] [CrossRef] [PubMed]
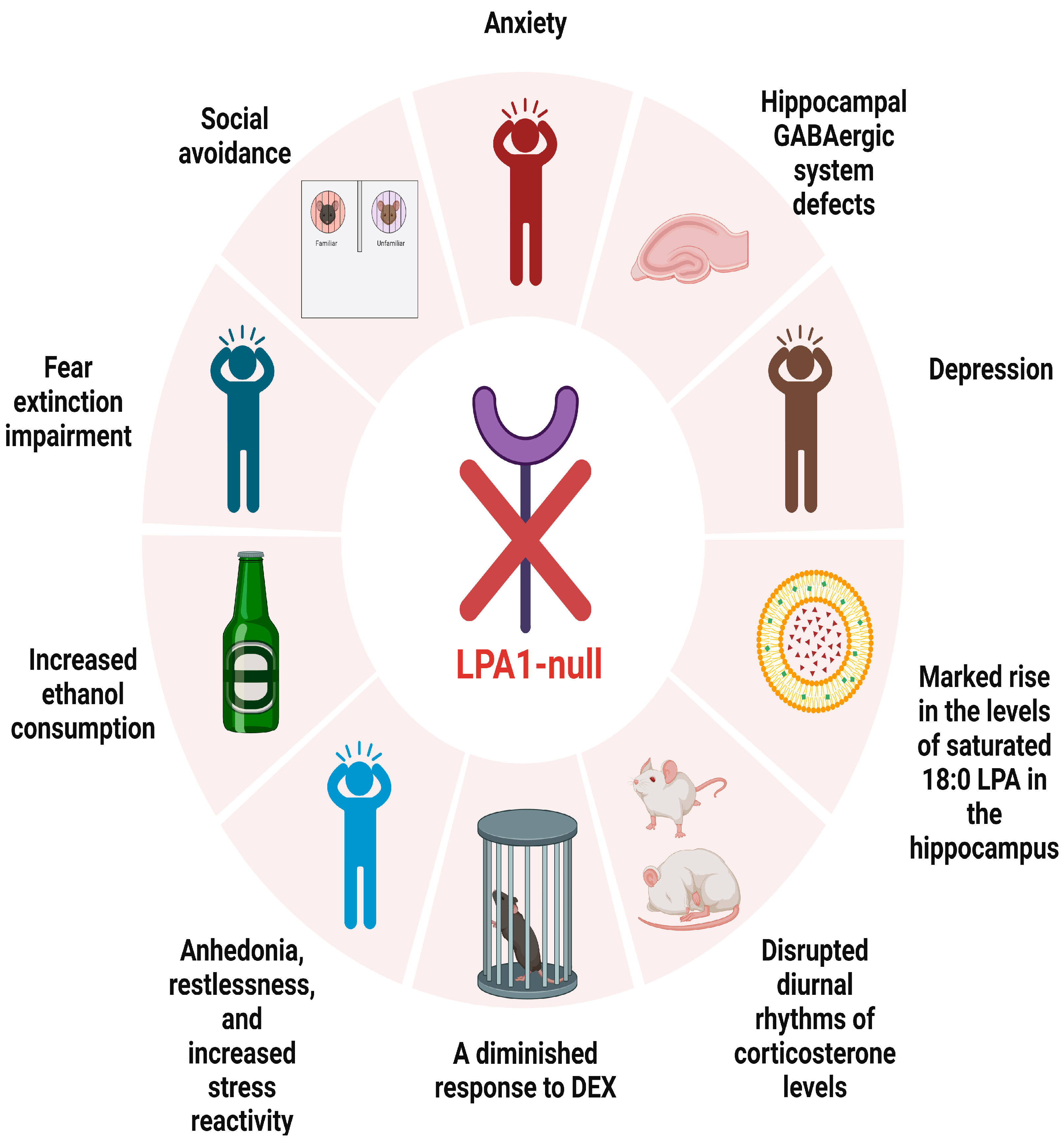
- Moreno-Fernández, R.D.; Pérez-Martín, M.; Castilla-Ortega, E.; Rosell Del Valle, C.; García-Fernández, M.I.; Chun, J.; Estivill-Torrús, G.; Rodríguez de Fonseca, F.; Santín, L.J.; Pedraza, C. maLPA1-null mice as an endophenotype of anxious depression. Transl. Psychiatry 2017, 7, e1077. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.J.; Park, S.D.; Lee, R.M.; Lee, B.H.; Choi, S.H.; Hwang, S.H.; Rhim, H.; Kim, H.C.; Nah, S.Y. Gintonin attenuates depressive-like behaviors associated with alcohol withdrawal in mice. J. Affect. Disord. 2017, 215, 23–29. [Google Scholar] [CrossRef] [PubMed]
- Moreno-Fernández, R.D.; Nieto-Quero, A.; Gómez-Salas, F.J.; Chun, J.; Estivill-Torrús, G.; Rodríguez de Fonseca, F.; Santín, L.J.; Pérez-Martín, M.; Pedraza, C. Effects of genetic deletion versus pharmacological blockade of the LPA(1) receptor on depression-like behaviour and related brain functional activity. Dis. Model. Mech. 2018, 11, dmm035519. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.Y.; Lee, J.W.; Lee, M.Y.; Kim, S.H.; Mok, H.J.; Ha, K.; Ahn, Y.M.; Kim, K.P. Serum lipidomic analysis for the discovery of biomarkers for major depressive disorder in drug-free patients. Psychiatry Res. 2018, 265, 174–182. [Google Scholar] [CrossRef] [PubMed]
- Tabbai, S.; Moreno-Fernández, R.D.; Zambrana-Infantes, E.; Nieto-Quero, A.; Chun, J.; García-Fernández, M.; Estivill-Torrús, G.; Rodríguez de Fonseca, F.; Santín, L.J.; Oliveira, T.G.; et al. Effects of the LPA(1) Receptor Deficiency and Stress on the Hippocampal LPA Species in Mice. Front. Mol. Neurosci. 2019, 12, 146. [Google Scholar] [CrossRef] [PubMed]
- Gotoh, L.; Yamada, M.; Hattori, K.; Sasayama, D.; Noda, T.; Yoshida, S.; Kunugi, H.; Yamada, M. Lysophosphatidic acid levels in cerebrospinal fluid and plasma samples in patients with major depressive disorder. Heliyon 2019, 5, e01699. [Google Scholar] [CrossRef]
- Lin, Y.N.; Audira, G.; Malhotra, N.; Ngoc Anh, N.T.; Siregar, P.; Lu, J.H.; Lee, H.; Hsiao, C.D. A Novel Function of the Lysophosphatidic Acid Receptor 3 (LPAR3) Gene in Zebrafish on Modulating Anxiety, Circadian Rhythm Locomotor Activity, and Short-Term Memory. Int. J. Mol. Sci. 2020, 21, 2837. [Google Scholar] [CrossRef]
- Riya, S.; Sultana, S.; Daria, S.; Proma, M.A.; Bhuiyan, M.A.; Haque, M.A.; Islam, M.R. Evaluation of Serum Lysophosphatidic Acid and Lysophosphatidylcholine Levels in Major Depressive Disorder Patients. Cureus 2020, 12, e12388. [Google Scholar] [CrossRef]
- Rosell-Valle, C.; Pedraza, C.; Manuel, I.; Moreno-Rodríguez, M.; Rodríguez-Puertas, R.; Castilla-Ortega, E.; Caramés, J.M.; Gómez Conde, A.I.; Zambrana-Infantes, E.; Ortega-Pinazo, J.; et al. Chronic central modulation of LPA/LPA receptors-signaling pathway in the mouse brain regulates cognition, emotion, and hippocampal neurogenesis. Prog. Neuropsychopharmacol. Biol. Psychiatry 2021, 108, 110156. [Google Scholar] [CrossRef]
- Rosell-Valle, C.; Martínez-Losa, M.; Matas-Rico, E.; Castilla-Ortega, E.; Zambrana-Infantes, E.; Gómez-Conde, A.I.; Sánchez-Salido, L.; Ladrón de Guevara-Miranda, D.; Pedraza, C.; Serrano-Castro, P.J.; et al. GABAergic deficits in absence of LPA(1) receptor, associated anxiety-like and coping behaviors, and amelioration by interneuron precursor transplants into the dorsal hippocampus. Brain Struct. Funct. 2021, 226, 1479–1495. [Google Scholar] [CrossRef]
- Omori, W.; Kano, K.; Hattori, K.; Kajitani, N.; Okada-Tsuchioka, M.; Boku, S.; Kunugi, H.; Aoki, J.; Takebayashi, M. Reduced Cerebrospinal Fluid Levels of Lysophosphatidic Acid Docosahexaenoic Acid in Patients with Major Depressive Disorder and Schizophrenia. Int. J. Neuropsychopharmacol. 2021, 24, 948–955. [Google Scholar] [CrossRef]
- Moreno-Fernández, R.D.; Sampedro-Piquero, P.; Gómez-Salas, F.J.; Nieto-Quero, A.; Estivill-Torrús, G.; Rodríguez de Fonseca, F.; Santín, L.J.; Pedraza, C. Social avoidance and altered hypothalamic-pituitary-adrenal axis in a mouse model of anxious depression: The role of LPA(1) receptor. Behav. Brain Res. 2023, 455, 114681. [Google Scholar] [CrossRef]
- Nagata, W.; Koizumi, A.; Nakagawa, K.; Takahashi, S.; Gotoh, M.; Satoh, Y.; Ishizuka, T. Treatment with lysophosphatidic acid prevents microglial activation and depression-like behaviours in a murine model of neuropsychiatric systemic lupus erythematosus. Clin. Exp. Immunol. 2023, 212, 81–92. [Google Scholar] [CrossRef] [PubMed]
- Kajitani, N.; Okada-Tsuchioka, M.; Inoue, A.; Miyano, K.; Masuda, T.; Boku, S.; Iwamoto, K.; Ohtsuki, S.; Uezono, Y.; Aoki, J.; et al. G protein-biased LPAR1 agonism of prototypic antidepressants: Implication in the identification of novel therapeutic target for depression. Neuropsychopharmacology 2024, 49, 561–572. [Google Scholar] [CrossRef] [PubMed]
- Wellman, C.L.; Izquierdo, A.; Garrett, J.E.; Martin, K.P.; Carroll, J.; Millstein, R.; Lesch, K.P.; Murphy, D.L.; Holmes, A. Impaired stress-coping and fear extinction and abnormal corticolimbic morphology in serotonin transporter knock-out mice. J. Neurosci. 2007, 27, 684–691. [Google Scholar] [CrossRef]
- Hartley, C.A.; Phelps, E.A. Changing fear: The neurocircuitry of emotion regulation. Neuropsychopharmacology 2010, 35, 136–146. [Google Scholar] [CrossRef] [PubMed]
- Shepard, J.D.; Barron, K.W.; Myers, D.A. Corticosterone delivery to the amygdala increases corticotropin-releasing factor mRNA in the central amygdaloid nucleus and anxiety-like behavior. Brain Res. 2000, 861, 288–295. [Google Scholar] [CrossRef]
- Shepard, J.D.; Barron, K.W.; Myers, D.A. Stereotaxic localization of corticosterone to the amygdala enhances hypothalamo-pituitary-adrenal responses to behavioral stress. Brain Res. 2003, 963, 203–213. [Google Scholar] [CrossRef]
- Davis, M.; Rainnie, D.; Cassell, M. Neurotransmission in the rat amygdala related to fear and anxiety. Trends Neurosci. 1994, 17, 208–214. [Google Scholar] [CrossRef] [PubMed]
- Meyer-Lindenberg, A.; Buckholtz, J.W.; Kolachana, B.; Hariri, A.R.; Pezawas, L.; Blasi, G.; Wabnitz, A.; Honea, R.; Verchinski, B.; Callicott, J.H.; et al. Neural mechanisms of genetic risk for impulsivity and violence in humans. Proc. Natl. Acad. Sci. USA 2006, 103, 6269–6274. [Google Scholar] [CrossRef] [PubMed]
- Yang, R.J.; Mozhui, K.; Karlsson, R.M.; Cameron, H.A.; Williams, R.W.; Holmes, A. Variation in mouse basolateral amygdala volume is associated with differences in stress reactivity and fear learning. Neuropsychopharmacology 2008, 33, 2595–2604. [Google Scholar] [CrossRef]
- Estivill-Torrús, G.; Llebrez-Zayas, P.; Matas-Rico, E.; Santín, L.; Pedraza, C.; De Diego, I.; Del Arco, I.; Fernández-Llebrez, P.; Chun, J.; De Fonseca, F.R. Absence of LPA1 signaling results in defective cortical development. Cereb. Cortex 2008, 18, 938–950. [Google Scholar] [CrossRef]
- Rodríguez Manzanares, P.A.; Isoardi, N.A.; Carrer, H.F.; Molina, V.A. Previous stress facilitates fear memory, attenuates GABAergic inhibition, and increases synaptic plasticity in the rat basolateral amygdala. J. Neurosci. 2005, 25, 8725–8734. [Google Scholar] [CrossRef] [PubMed]
- Ohuchi, H.; Hamada, A.; Matsuda, H.; Takagi, A.; Tanaka, M.; Aoki, J.; Arai, H.; Noji, S. Expression patterns of the lysophospholipid receptor genes during mouse early development. Dev. Dyn. 2008, 237, 3280–3294. [Google Scholar] [CrossRef]
- Li, C.R.; Huang, G.B.; Sui, Z.Y.; Han, E.H.; Chung, Y.C. Effects of 6-hydroxydopamine lesioning of the medial prefrontal cortex on social interactions in adolescent and adult rats. Brain Res. 2010, 1346, 183–189. [Google Scholar] [CrossRef]
- Klimek, V.; Stockmeier, C.; Overholser, J.; Meltzer, H.Y.; Kalka, S.; Dilley, G.; Ordway, G.A. Reduced levels of norepinephrine transporters in the locus coeruleus in major depression. J. Neurosci. 1997, 17, 8451–8458. [Google Scholar] [CrossRef]
- Marrone, R.L.; Pray, S.L.; Bridges, C.C. Norepinephrine elicitation of aggressive display responses in Betta splendens. Psychon. Sci. 1966, 5, 207–208. [Google Scholar] [CrossRef]
- Barton, B.A. Stress in fishes: A diversity of responses with particular reference to changes in circulating corticosteroids. Integr. Comp. Biol. 2002, 42, 517–525. [Google Scholar] [CrossRef]
- Harvey, P.O.; Pruessner, J.; Czechowska, Y.; Lepage, M. Individual differences in trait anhedonia: A structural and functional magnetic resonance imaging study in non-clinical subjects. Mol. Psychiatry 2007, 12, 767–775. [Google Scholar] [CrossRef] [PubMed]
- Der-Avakian, A.; Markou, A. The neurobiology of anhedonia and other reward-related deficits. Trends Neurosci. 2012, 35, 68–77. [Google Scholar] [CrossRef] [PubMed]
- Malkesman, O.; Scattoni, M.L.; Paredes, D.; Tragon, T.; Pearson, B.; Shaltiel, G.; Chen, G.; Crawley, J.N.; Manji, H.K. The female urine sniffing test: A novel approach for assessing reward-seeking behavior in rodents. Biol. Psychiatry 2010, 67, 864–871. [Google Scholar] [CrossRef] [PubMed]
- First, M.B.; Reed, G.M.; Hyman, S.E.; Saxena, S. The development of the ICD-11 Clinical Descriptions and Diagnostic Guidelines for Mental and Behavioural Disorders. World Psychiatry 2015, 14, 82–90. [Google Scholar] [CrossRef] [PubMed]
- Xu, K.; Ma, L.; Li, Y.; Wang, F.; Zheng, G.Y.; Sun, Z.; Jiang, F.; Chen, Y.; Liu, H.; Dang, A.; et al. Genetic and Functional Evidence Supports LPAR1 as a Susceptibility Gene for Hypertension. Hypertension 2015, 66, 641–646. [Google Scholar] [CrossRef] [PubMed]
- Nestler, E.J.; Hyman, S.E. Animal models of neuropsychiatric disorders. Nat. Neurosci. 2010, 13, 1161–1169. [Google Scholar] [CrossRef] [PubMed]
- Matas-Rico, E.; García-Diaz, B.; Llebrez-Zayas, P.; López-Barroso, D.; Santín, L.; Pedraza, C.; Smith-Fernández, A.; Fernández-Llebrez, P.; Tellez, T.; Redondo, M.; et al. Deletion of lysophosphatidic acid receptor LPA1 reduces neurogenesis in the mouse dentate gyrus. Mol. Cell Neurosci. 2008, 39, 342–355. [Google Scholar] [CrossRef] [PubMed]
- Musazzi, L.; Di Daniel, E.; Maycox, P.; Racagni, G.; Popoli, M. Abnormalities in α/β-CaMKII and related mechanisms suggest synaptic dysfunction in hippocampus of LPA1 receptor knockout mice. Int. J. Neuropsychopharmacol. 2011, 14, 941–953. [Google Scholar] [CrossRef]
- Castilla-Ortega, E.; Hoyo-Becerra, C.; Pedraza, C.; Chun, J.; Rodríguez De Fonseca, F.; Estivill-Torrús, G.; Santín, L.J. Aggravation of chronic stress effects on hippocampal neurogenesis and spatial memory in LPA1 receptor knockout mice. PLoS ONE 2011, 6, e25522. [Google Scholar] [CrossRef]
- Alvarez Dolado, M.; Broccoli, V. GABAergic neuronal precursor grafting: Implications in brain regeneration and plasticity. Neural Plast. 2011, 2011, 384216. [Google Scholar] [CrossRef]
- Leussis, M.P.; Bolivar, V.J. Habituation in rodents: A review of behavior, neurobiology, and genetics. Neurosci. Biobehav. Rev. 2006, 30, 1045–1064. [Google Scholar] [CrossRef]
- Takahashi, L.K.; Kalin, N.H.; Vanden Burgt, J.A.; Sherman, J.E. Corticotropin-releasing factor modulates defensive-withdrawal and exploratory behavior in rats. Behav. Neurosci. 1989, 103, 648–654. [Google Scholar] [CrossRef]
- Murph, M.M.; Scaccia, L.A.; Volpicelli, L.A.; Radhakrishna, H. Agonist-induced endocytosis of lysophosphatidic acid-coupled LPA1/EDG-2 receptors via a dynamin2- and Rab5-dependent pathway. J. Cell Sci. 2003, 116, 1969–1980. [Google Scholar] [CrossRef] [PubMed]
- Yung, Y.C.; Stoddard, N.C.; Mirendil, H.; Chun, J. Lysophosphatidic Acid signaling in the nervous system. Neuron 2015, 85, 669–682. [Google Scholar] [CrossRef]
- Ma, L.; Uchida, H.; Nagai, J.; Inoue, M.; Chun, J.; Aoki, J.; Ueda, H. Lysophosphatidic acid-3 receptor-mediated feed-forward production of lysophosphatidic acid: An initiator of nerve injury-induced neuropathic pain. Mol. Pain. 2009, 5, 64. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Tong, J.; He, D.; Pendyala, S.; Evgeny, B.; Chun, J.; Sperling, A.I.; Natarajan, V. Role of lysophosphatidic acid receptor LPA2 in the development of allergic airway inflammation in a murine model of asthma. Respir. Res. 2009, 10, 114. [Google Scholar] [CrossRef]
- Tomás, M.; Lázaro-Diéguez, F.; Durán, J.M.; Marín, P.; Renau-Piqueras, J.; Egea, G. Protective effects of lysophosphatidic acid (LPA) on chronic ethanol-induced injuries to the cytoskeleton and on glucose uptake in rat astrocytes. J. Neurochem. 2003, 87, 220–229. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Z.; Yu, M.; Crabb, D.; Xu, Y.; Liangpunsakul, S. Ethanol-induced alterations in fatty acid-related lipids in serum and tissues in mice. Alcohol. Clin. Exp. Res. 2011, 35, 229–234. [Google Scholar] [CrossRef]
- LeMarquand, D.; Pihl, R.O.; Benkelfat, C. Serotonin and alcohol intake, abuse, and dependence: Findings of animal studies. Biol. Psychiatry 1994, 36, 395–421. [Google Scholar] [CrossRef]
- Pettinati, H.M.; Oslin, D.; Decker, K. Role of serotonin and serotonin-selective pharmacotherapy in alcohol dependence. CNS Spectr. 2000, 5, 33–46. [Google Scholar] [CrossRef]
- Virkkunen, M.; Goldman, D.; Nielsen, D.A.; Linnoila, M. Low brain serotonin turnover rate (low CSF 5-HIAA) and impulsive violence. J. Psychiatry Neurosci. 1995, 20, 271–275. [Google Scholar] [PubMed]
- Lovinger, D.M. Serotonin’s role in alcohol’s effects on the brain. Alcohol. Health Res. World 1997, 21, 114–120. [Google Scholar] [PubMed]
- Lee, N.; Lee, S.H.; Yoo, H.R.; Yoo, H.S. Anti-Fatigue Effects of Enzyme-Modified Ginseng Extract: A Randomized, Double-Blind, Placebo-Controlled Trial. J. Altern. Complement. Med. 2016, 22, 859–864. [Google Scholar] [CrossRef]
- Kim, H.J.; Kim, D.J.; Shin, E.J.; Lee, B.H.; Choi, S.H.; Hwang, S.H.; Rhim, H.; Cho, I.H.; Kim, H.C.; Nah, S.Y. Effects of gintonin-enriched fraction on hippocampal cell proliferation in wild-type mice and an APPswe/PSEN-1 double Tg mouse model of Alzheimer’s disease. Neurochem. Int. 2016, 101, 56–65. [Google Scholar] [CrossRef]
- Nie, X.; Kitaoka, S.; Tanaka, K.; Segi-Nishida, E.; Imoto, Y.; Ogawa, A.; Nakano, F.; Tomohiro, A.; Nakayama, K.; Taniguchi, M.; et al. The Innate Immune Receptors TLR2/4 Mediate Repeated Social Defeat Stress-Induced Social Avoidance through Prefrontal Microglial Activation. Neuron 2018, 99, 464–479.e467. [Google Scholar] [CrossRef]
- Atanasova, D.; Lazarov, N.; Stoyanov, D.S.; Spassov, R.H.; Tonchev, A.B.; Tchekalarova, J. Reduced neuroinflammation and enhanced neurogenesis following chronic agomelatine treatment in rats undergoing chronic constant light. Neuropharmacology 2021, 197, 108706. [Google Scholar] [CrossRef]
- Kappelmann, N.; Lewis, G.; Dantzer, R.; Jones, P.B.; Khandaker, G.M. Antidepressant activity of anti-cytokine treatment: A systematic review and meta-analysis of clinical trials of chronic inflammatory conditions. Mol. Psychiatry 2018, 23, 335–343. [Google Scholar] [CrossRef]
- Mateus-Pinheiro, A.; Pinto, L.; Bessa, J.M.; Morais, M.; Alves, N.D.; Monteiro, S.; Patrício, P.; Almeida, O.F.; Sousa, N. Sustained remission from depressive-like behavior depends on hippocampal neurogenesis. Transl. Psychiatry 2013, 3, e210. [Google Scholar] [CrossRef] [PubMed]
- Nomura, A.; Noto, D.; Murayama, G.; Chiba, A.; Miyake, S. Unique primed status of microglia under the systemic autoimmune condition of lupus-prone mice. Arthritis Res. Ther. 2019, 21, 303. [Google Scholar] [CrossRef]
- Cipriani, A.; Furukawa, T.A.; Salanti, G.; Chaimani, A.; Atkinson, L.Z.; Ogawa, Y.; Leucht, S.; Ruhe, H.G.; Turner, E.H.; Higgins, J.P.T.; et al. Comparative efficacy and acceptability of 21 antidepressant drugs for the acute treatment of adults with major depressive disorder: A systematic review and network meta-analysis. Lancet 2018, 391, 1357–1366. [Google Scholar] [CrossRef]
- Anderson, I.M. Selective serotonin reuptake inhibitors versus tricyclic antidepressants: A meta-analysis of efficacy and tolerability. J. Affect. Disord. 2000, 58, 19–36. [Google Scholar] [CrossRef] [PubMed]
- Salvadore, G.; Quiroz, J.A.; Machado-Vieira, R.; Henter, I.D.; Manji, H.K.; Zarate, C.A., Jr. The neurobiology of the switch process in bipolar disorder: A review. J. Clin. Psychiatry 2010, 71, 1488–1501. [Google Scholar] [CrossRef] [PubMed]
- Rappley, I.; Myers, D.S.; Milne, S.B.; Ivanova, P.T.; Lavoie, M.J.; Brown, H.A.; Selkoe, D.J. Lipidomic profiling in mouse brain reveals differences between ages and genders, with smaller changes associated with alpha-synuclein genotype. J. Neurochem. 2009, 111, 15–25. [Google Scholar] [CrossRef] [PubMed]
- Miranda, A.M.; Bravo, F.V.; Chan, R.B.; Sousa, N.; Di Paolo, G.; Oliveira, T.G. Differential lipid composition and regulation along the hippocampal longitudinal axis. Transl. Psychiatry 2019, 9, 144. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]


| ID | Search Terms | Results |
|---|---|---|
| #1 | (lysophosphatidic acid[Title/Abstract]) AND (mood[Title/Abstract]) | 32 |
| #2 | (lysophosphatidic acid[Title/Abstract]) AND (emotion[Title/Abstract]) | 12 |
| #3 | (lysophosphatidic acid[Title/Abstract]) AND (depression[Title/Abstract]) | 99 |
| #4 | (lysophosphatidic acid[Title/Abstract]) AND (anxiety[Title/Abstract]) | 65 |
| Study | Risk of Bias | Applicability Concerns | |||||
|---|---|---|---|---|---|---|---|
| Patient Selection | Index Text | Reference Standard | Flow and Timing | Patient Selection | Index Text | Reference Standard | |
| L.J. Santin et al. [26] | Low risk | Low risk | Low risk | Unclear risk | Low risk | Low risk | Low risk |
| Estela Castilla-Ortega et al. [27] | Low risk | Low risk | Low risk | Unclear risk | Low risk | Low risk | Low risk |
| Z. Callaerts-Vegh et al. [28] | Low risk | Low risk | Low risk | Unclear risk | Low risk | Low risk | Low risk |
| C. Pedraza et al. [29] | Low risk | Low risk | Low risk | Unclear risk | Low risk | Low risk | Low risk |
| Estela Castilla-Ortega et al. [30] | Low risk | Low risk | Low risk | Unclear risk | Low risk | Low risk | Low risk |
| Misa Yamada et al. [31] | Low risk | Low risk | Low risk | Unclear risk | Low risk | Low risk | Low risk |
| Estela Castilla-Ortega et al. [32] | Low risk | Low risk | Low risk | Unclear risk | Low risk | Low risk | Low risk |
| Moreno-Fernández RD et al. [33] | Low risk | Low risk | Low risk | Unclear risk | Low risk | Low risk | Low risk |
| Hyeon-Joong Kim et al. [34] | Low risk | Low risk | Low risk | Unclear risk | Low risk | Low risk | Low risk |
| Moreno-Fernández RD et al. [35] | Low risk | Low risk | Low risk | Unclear risk | Low risk | Low risk | Low risk |
| Eun Young Kim et al. [36] | Low risk | Low risk | Low risk | Unclear risk | Low risk | Low risk | Low risk |
| Sara Tabbai et al. [37] | Low risk | Low risk | Low risk | Unclear risk | Low risk | Low risk | Low risk |
| Leo Gotoh et al. [38] | Low risk | Low risk | Low risk | Unclear risk | Low risk | Low risk | Low risk |
| Yu-Nung Lin et al. [39] | Unclear risk | Low risk | Low risk | Unclear risk | Low risk | Low risk | Low risk |
| Sumaia Riya et al. [40] | Low risk | Low risk | Low risk | Unclear risk | Low risk | Low risk | Low risk |
| Cristina Rosell-Valle et al. [41] | Low risk | Low risk | Low risk | Unclear risk | Low risk | Low risk | Low risk |
| Cristina Rosell-Valle et al. [42] | Low risk | Low risk | Low risk | Unclear risk | Low risk | Low risk | Low risk |
| Wataru Omori et al. [43] | Low risk | Low risk | Low risk | Unclear risk | Low risk | Low risk | Low risk |
| Moreno-Fernández RD et al. [44] | Low risk | High risk | Unclear risk | Unclear risk | Low risk | High risk | Unclear risk |
| Wataru Nagata et al. [45] | Low risk | Low risk | Low risk | Unclear risk | Low risk | Low risk | Low risk |
| Naoto Kajitani et al. [46] | Low risk | Low risk | Low risk | Unclear risk | Low risk | Low risk | Low risk |
| Authors | Year | Group | Intervention | Results |
|---|---|---|---|---|
| L.J. Santin et al. [26] | 2009 | LPA1-null mice | unknown | anxiety |
| Estela Castilla-Ortega et al. [27] | 2010 | LPA1-null mice | unknown | anxiety |
| Z. Callaerts-Vegh et al. [28] | 2012 | LPA5-null mice | unknown | significantly reduced anxiety levels |
| C. Pedraza et al. [29] | 2013 | LPA1-null mice | unknown | fear extinction impairment |
| wild-type mice | LPA1 antagonist Ki16425 administration | fear extinction impairment | ||
| Estela Castilla-Ortega et al. [30] | 2014 | rats | LPA administration | anxiety and depression |
| Misa Yamada et al. [31] | 2015 | adult mouse | LPA administration | anxiety |
| Estela Castilla-Ortega et al. [32] | 2016 | LPA1-null mice | alcohol withdrawal | anxiety |
| wild-type mice | alcohol withdrawal + LPA1 antagonist Ki16425 administration | increased ethanol consumption | ||
| Moreno-Fernández RD et al. [33] | 2017 | LPA1-null mice | unknown | panic-like responses, anhedonia, restlessness, and increased stress reactivity |
| LPA1-null mice | antidepressant treatment | depressive-like behaviors improved | ||
| Hyeon-Joong Kim et al. [34] | 2017 | enterochromaffin cell line BON cells | gintonin administration | release of 5-hydroxytryptamine |
| C57BL/6 mice | gintonin administration | depressive-like behaviors improved | ||
| Moreno-Fernández RD et al. [35] | 2018 | LPA1-null mice | unknown | anxiety and depression |
| Sara Tabbai et al. [37] | 2019 | LPA1-null mice | unknown | marked rise in the levels of saturated 18:0 LPA in the hippocampus |
| mice | acute stress | changes in hippocampal LPA levels | ||
| Yu-Nung Lin et al. [39] | 2020 | LPAR3 knockout (KO) zebrafish | unknown | anxiety |
| Cristina Rosell-Valle et al. [41] | 2021 | mice | 21-day sustained intracerebroventricular (ICV) infusion of C18:1 LPA and LPA1-3 receptor antagonist Ki16425 | reduced anxious tendencies |
| Cristina Rosell-Valle et al. [42] | 2021 | LPA1-null mice | unknown | hippocampal GABAergic system defects |
| LPA1-null mice | GABAergic precursor cell transplantation | normalize or mitigate hippocampal GABAergic system defects | ||
| Moreno-Fernández RD et al. [44] | 2023 | LPA1-null mice | DEX | diminished response to DEX |
| Wataru Nagata et al. [45] | 2023 | MRL/lpr mice | LPA administration | alleviates depressive-like behaviors |
| Naoto Kajitani et al. [46] | 2023 | LPA1 receptor | tricyclic and tetracyclic antidepressant administration | TCAs directly bind to LPA1 receptor and exhibit G-protein-biased agonism |
| Authors | Year | Group | Intervention | Results |
|---|---|---|---|---|
| Eun Young Kim et al. [36] | 2018 | patients with current MDD (cMDD) | unknown | LPA (16:1), TG (44:0), and TG (54:8) differentiated cMDD from healthy controls with 76% accuracy |
| Leo Gotoh et al. [38] | 2019 | patients with MDD | unknown | no significant differences in LPA levels between MDD patients and healthy controls in either CSF or plasma samples |
| Sumaia Riya et al. [40] | 2020 | patients with MDD | unknown | no significant differences in serum LPA and LPC levels between MDD patients and healthy controls |
| Wataru Omori et al. [43] | 2021 | patients with MDD and SCZ | unknown | significantly lower levels of LPA 22:6 in CSF of patients with MDD and SCZ compared to healthy controls |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, N.; Li, Y. Lysophosphatidic Acid (LPA) and Its Receptors in Mood Regulation: A Systematic Review of the Molecular Mechanisms and Therapeutic Potential. Int. J. Mol. Sci. 2024, 25, 7440. https://doi.org/10.3390/ijms25137440
Li N, Li Y. Lysophosphatidic Acid (LPA) and Its Receptors in Mood Regulation: A Systematic Review of the Molecular Mechanisms and Therapeutic Potential. International Journal of Molecular Sciences. 2024; 25(13):7440. https://doi.org/10.3390/ijms25137440
Chicago/Turabian StyleLi, Nan, and Yanchun Li. 2024. "Lysophosphatidic Acid (LPA) and Its Receptors in Mood Regulation: A Systematic Review of the Molecular Mechanisms and Therapeutic Potential" International Journal of Molecular Sciences 25, no. 13: 7440. https://doi.org/10.3390/ijms25137440
APA StyleLi, N., & Li, Y. (2024). Lysophosphatidic Acid (LPA) and Its Receptors in Mood Regulation: A Systematic Review of the Molecular Mechanisms and Therapeutic Potential. International Journal of Molecular Sciences, 25(13), 7440. https://doi.org/10.3390/ijms25137440






