Inflammatory Cytokine-Induced Muscle Atrophy and Weakness Can Be Ameliorated by an Inhibition of TGF-β-Activated Kinase-1
Abstract
1. Introduction
2. Results
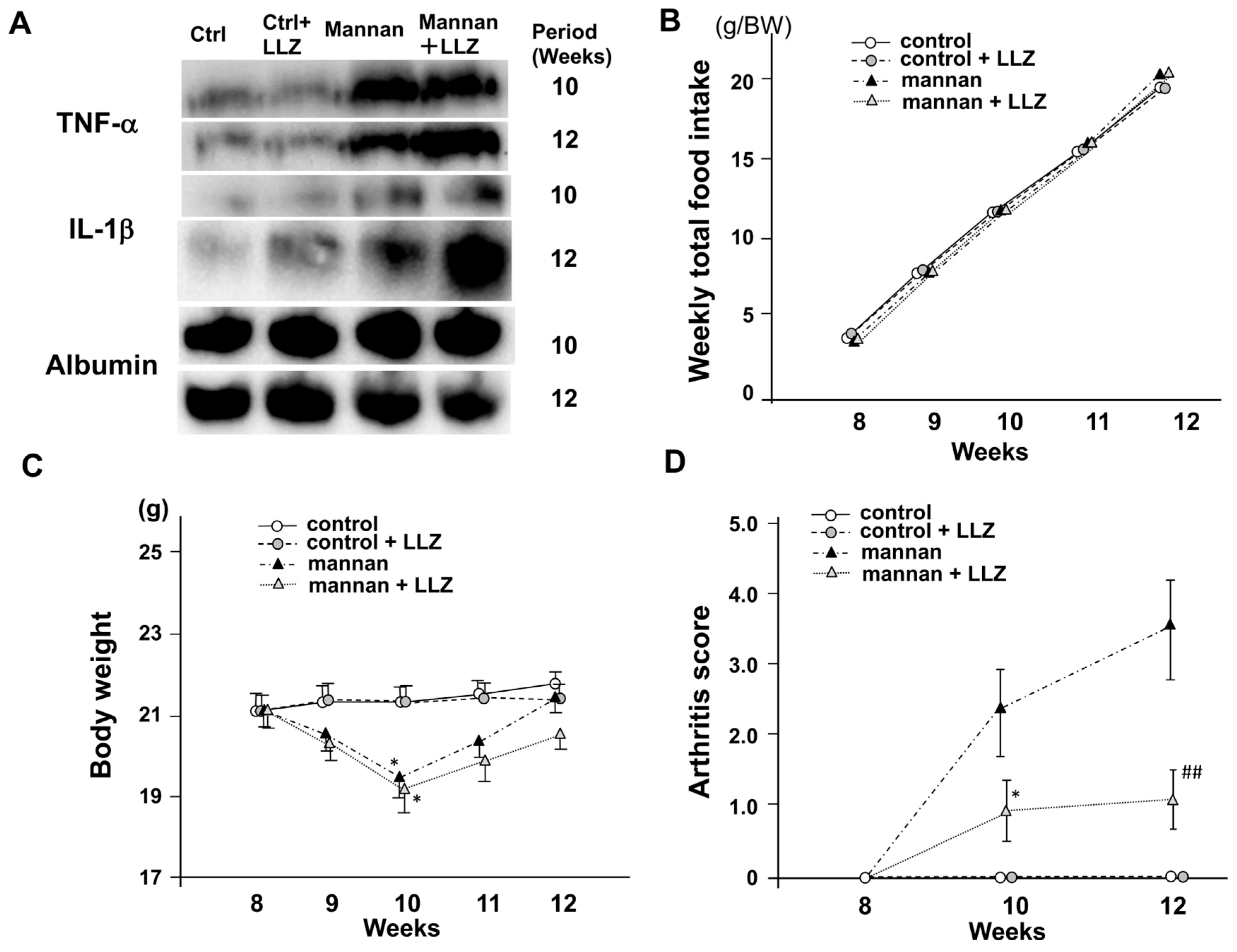
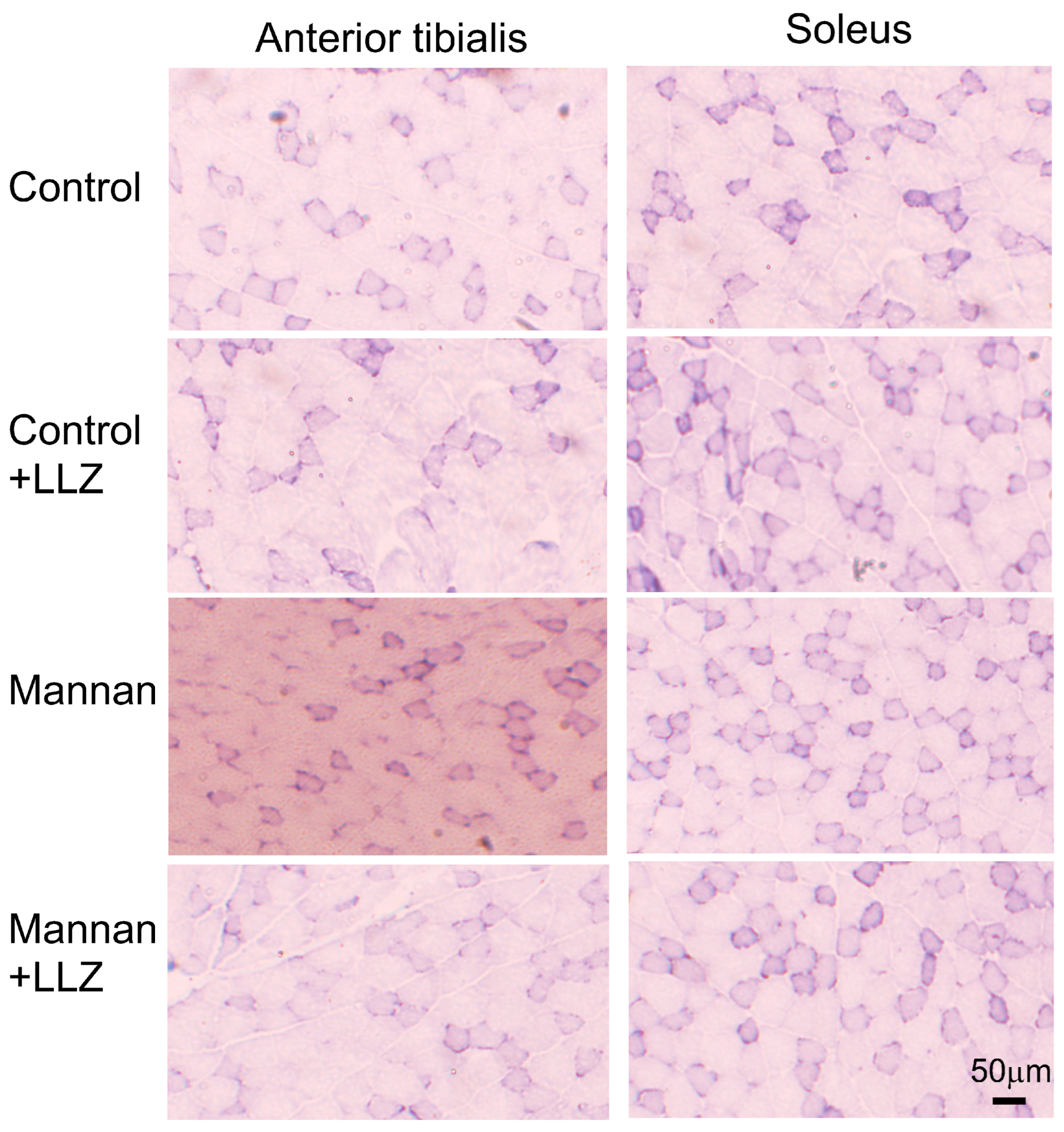
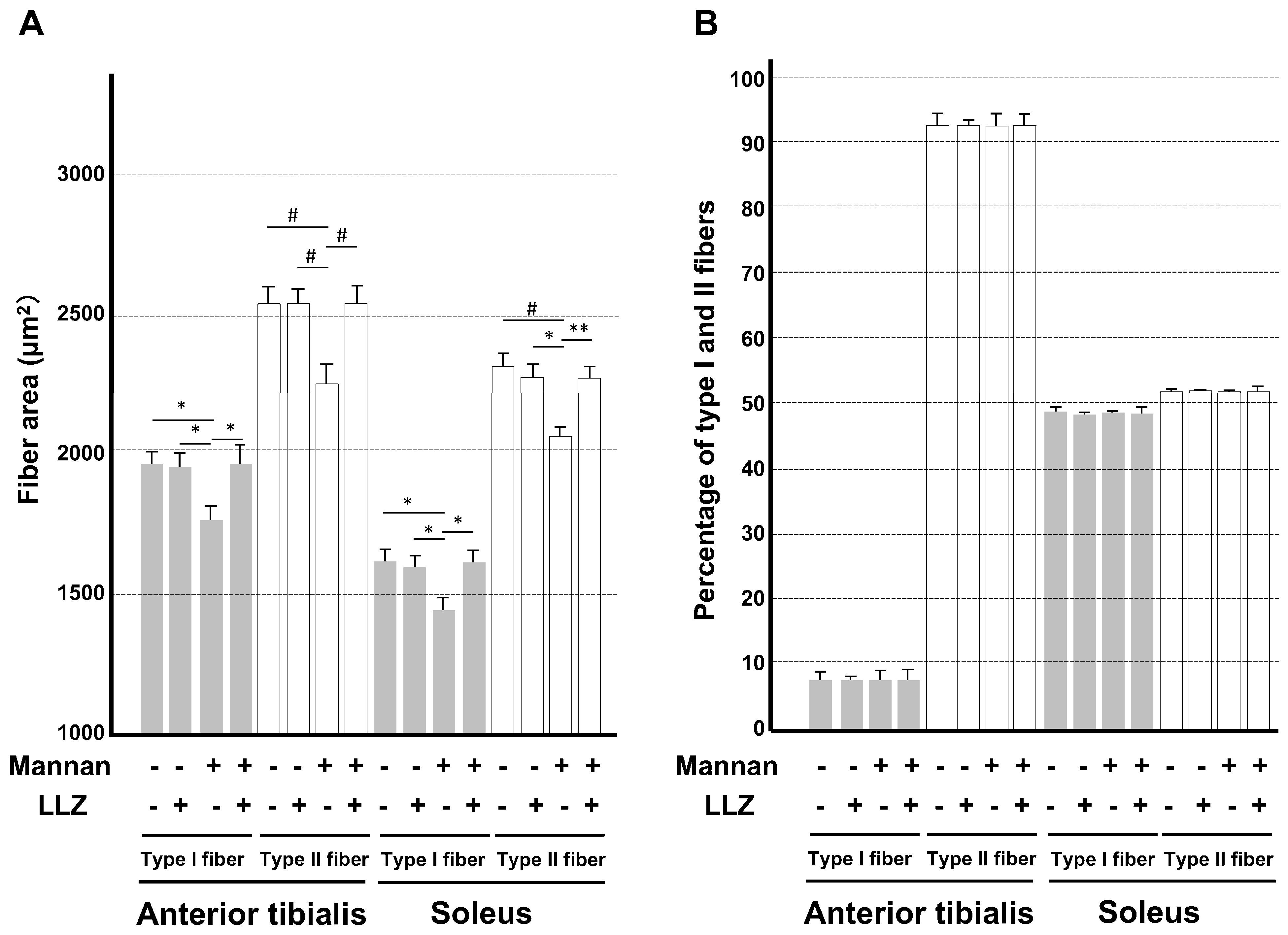
2.1. Inflammatory Cytokine-Induced Myopathy Is Ameliorated by a TAK1 Inhibitor LLZ In Vivo
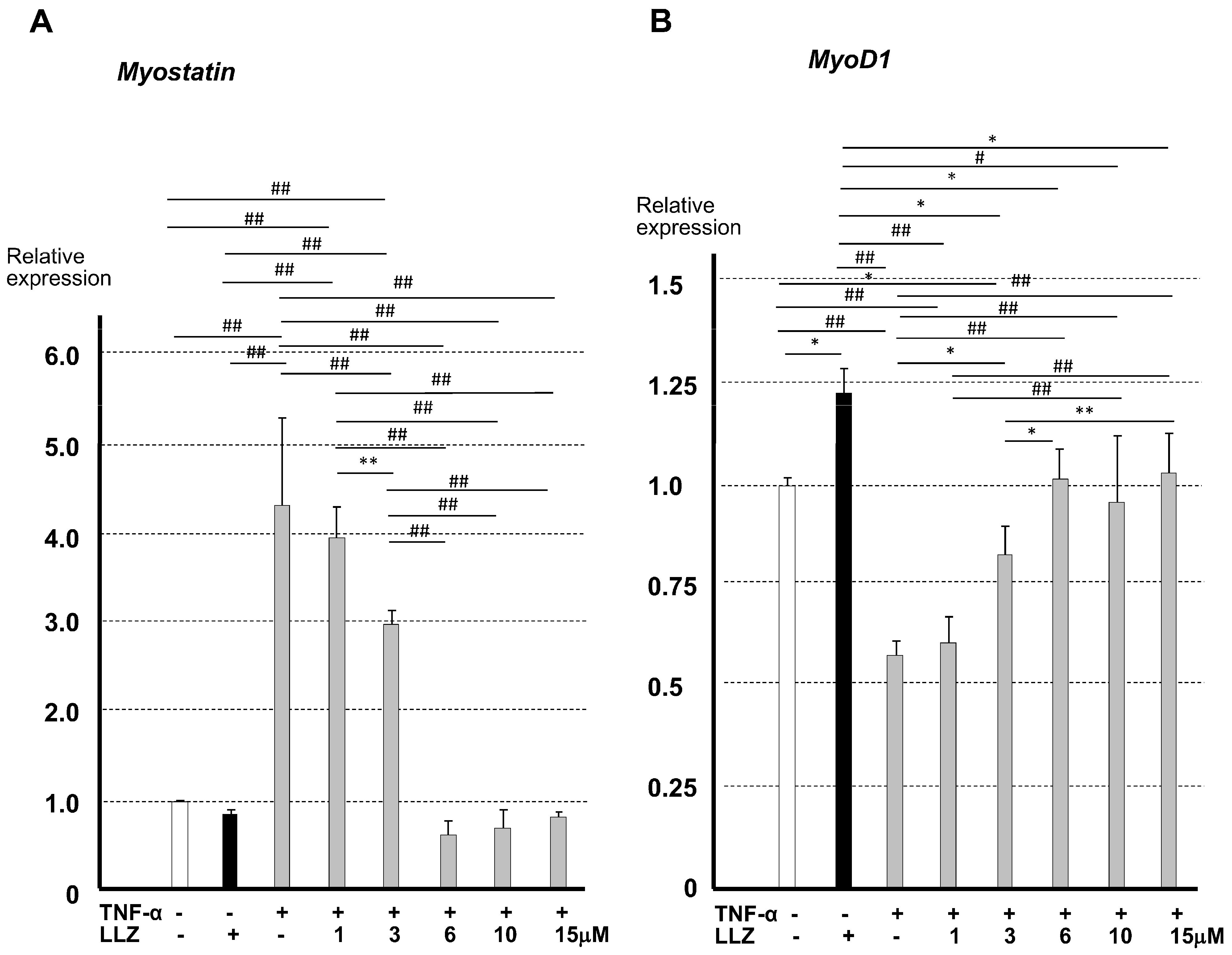
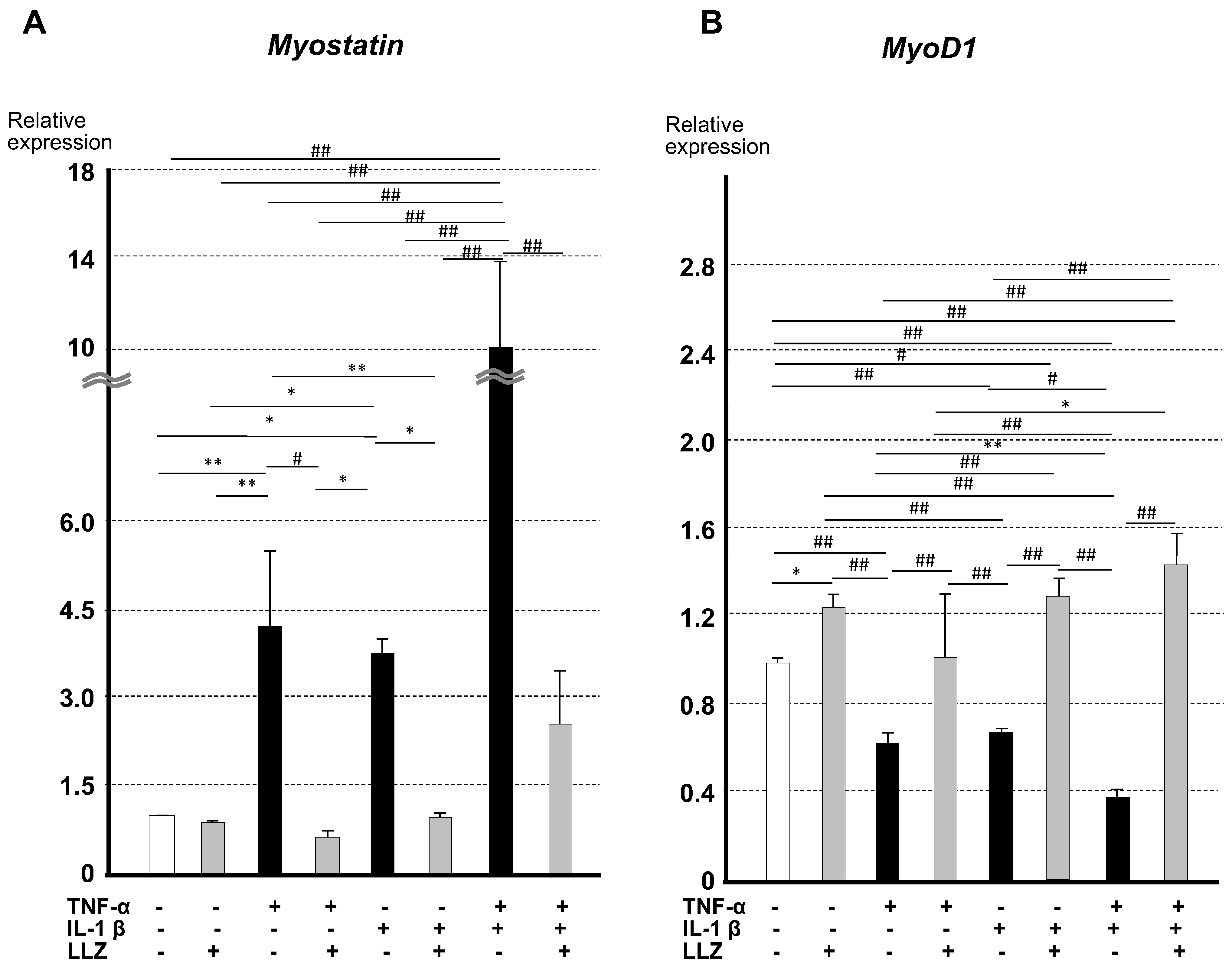
2.2. Effects of TNF-α and IL-1β on Myostatin and MyoD1 Expression Were Reversed by LLZ In Vitro
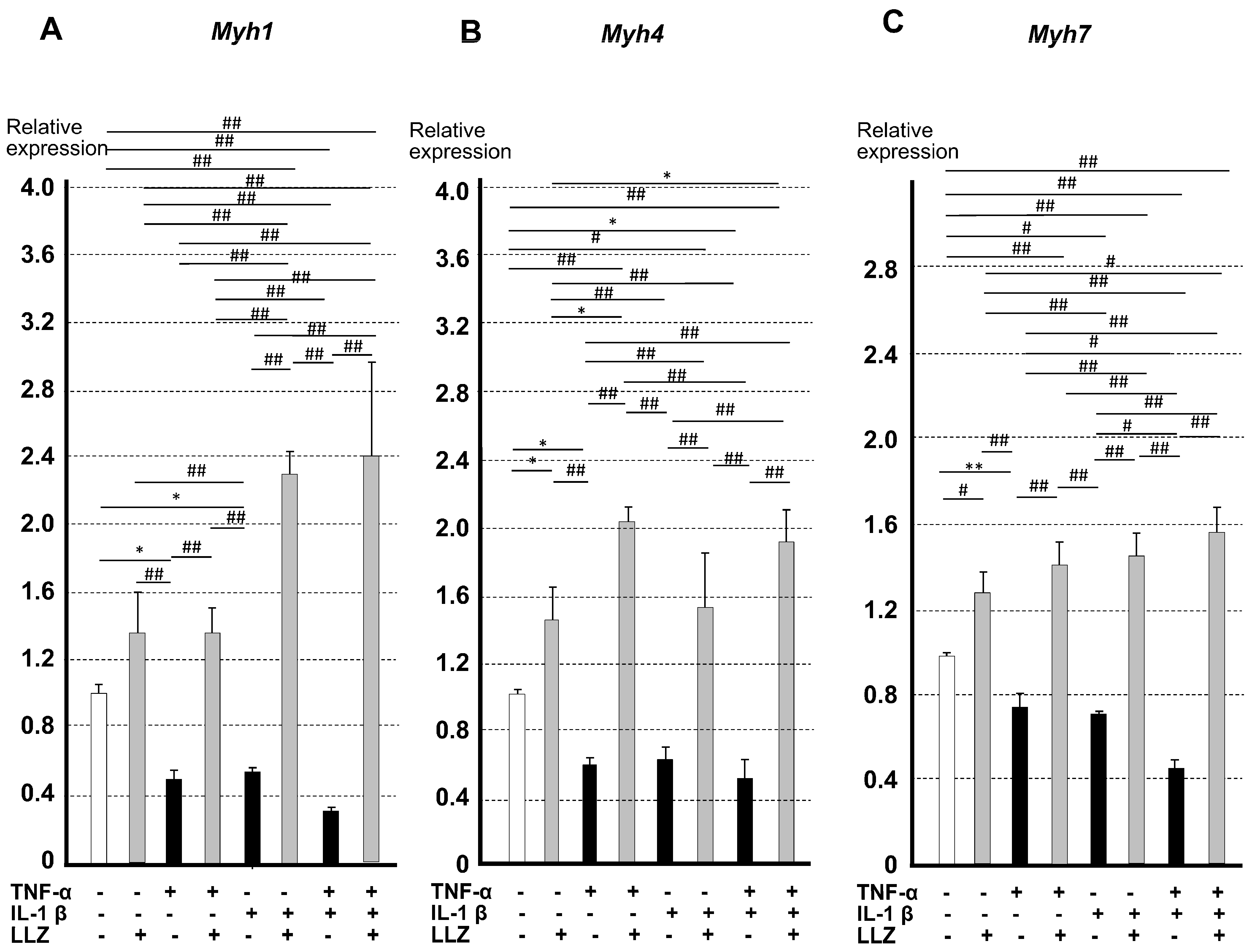
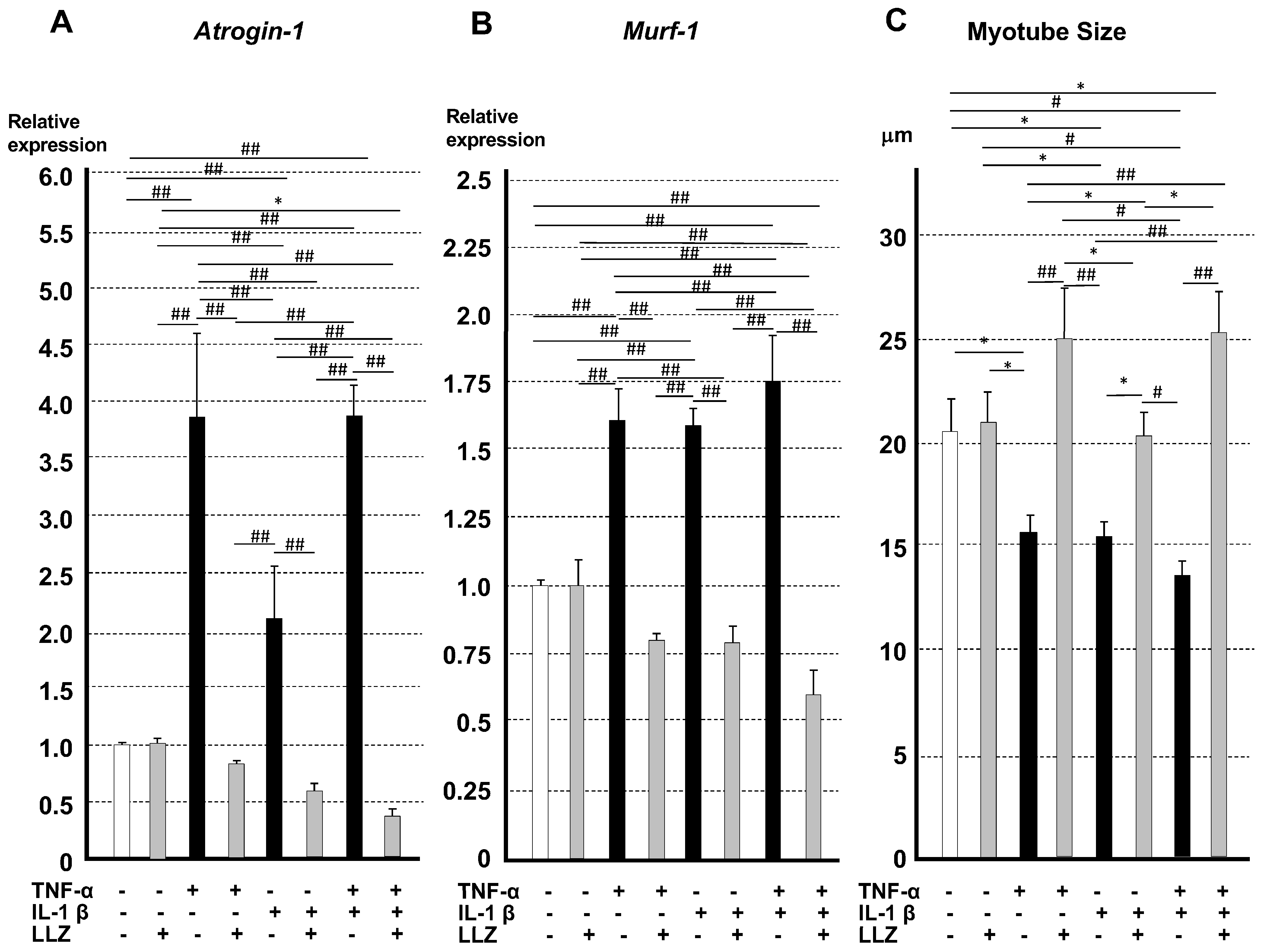
2.3. Reversal of the Effects of TNF-α and IL-1β on the Expression of Muscle-Specific Proteins, Muscle Atrophic Factors, and Myotube Size by LLZ In Vitro
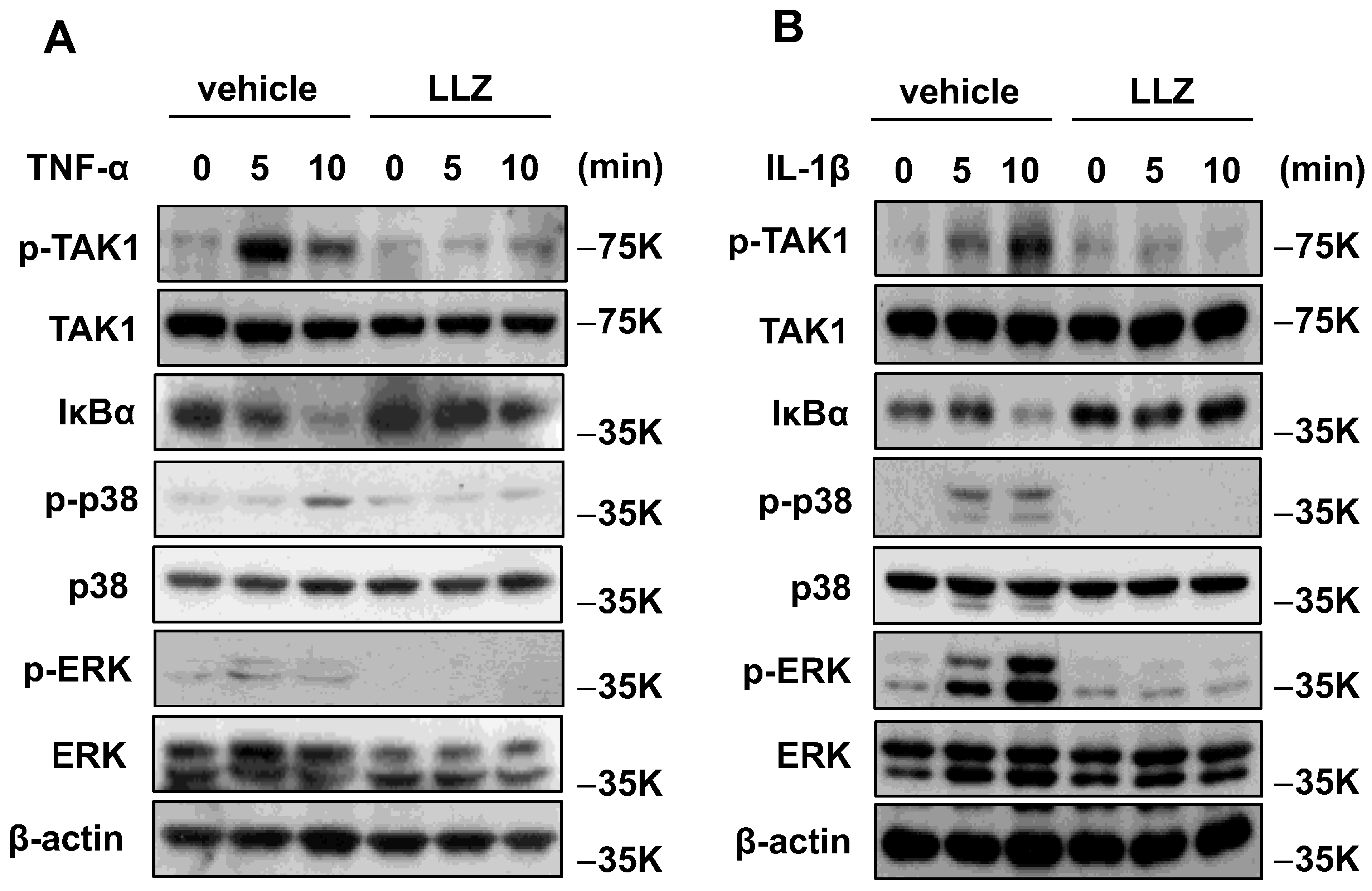
2.4. TNF-α and IL-1β Enhance and LLZ Abrogates TAK1 Signaling In Vitro
3. Discussion
4. Material and Methods
4.1. Reagents
4.2. Animal Experiments
4.3. Western Blot Analysis of Serum TNF-α and IL-1β
4.4. Arthritis Score
4.5. Micro-Computed Tomography (μCT) Analysis
4.6. Measurement of Grip Strength
4.7. Muscle Histology
4.8. Cell Culture
4.9. Immunofluorescence Microscopy and Myotube Analysis
4.10. Real-Time PCR
- mouse Myostatin F: GAGCCCAGGCACTGGTATTT and
- R: AGGGATTCAGCCCATCTTCTC
- mouse Myod1 F: TGCTCTGATGGCATGATGGATT and
- R: TGGAGATGCGCTCCACTATG
- mouse Myh1 F: GGACCCACGGTCGAAGTTG and
- R: CCCGAAAACGGCCATCT
- mouse Myh4 F: CAATCAGGAACCTTCGGAACAC and
- R: GTCCTGGCCTCTGAGAGCAT
- mouse Myh7 F: AGTCCCAGGTCAACAAGCTG and
- R: TTCCACCTAAAGGGCTGTTG
- mouse Atogin1 F: TCTCAGAGAGGCAGATTCGC and
- R: TGAGGGGAAAGTGAGACGGA
- mouse Murf1 F: GGGCTACCTTCCTCTCAAGTG and
- R: GAGCGTGTCTCACTCATCTCC
4.11. Western Blot Analysis of C2C12 Cells
4.12. Statistics
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Brognara, L.; Luna, O.C.; Traina, F.; Cauli, O. Inflammatory Biomarkers and Gait Impairment in Older Adults: A Systematic Review. Int. J. Mol. Sci. 2024, 25, 1368. [Google Scholar] [CrossRef] [PubMed]
- Sakurai, H. Targeting of TAK1 in inflammatory disorders and cancer. Trends Pharmacol. Sci. 2012, 33, 522–530. [Google Scholar] [CrossRef] [PubMed]
- Hata, H.; Sakaguchi, N.; Yoshitomi, H.; Iwakura, Y.; Sekikawa, K.; Azuma, Y.; Kanai, C.; Moriizumi, E.; Nomura, T.; Nakamura, T.; et al. Distinct contribution of IL-6, TNF-alpha, IL-1, and IL-10 to T cell-mediated spontaneous autoimmune arthritis in mice. J. Clin. Investig. 2004, 114, 582–588. [Google Scholar] [CrossRef] [PubMed]
- Hashimoto, M.; Hirota, K.; Yoshitomi, H.; Maeda, S.; Teradaira, S.; Akizuki, S.; Prieto-Martin, P.; Nomura, T.; Sakaguchi, N.; Köhl, J.; et al. Complement drives Th17 cell differentiation and triggers autoimmune arthritis. J. Exp. Med. 2010, 207, 1135–1143. [Google Scholar] [CrossRef]
- Pogostin, B.H.; Saenz, G.; Cole, C.C.; Euliano, E.M.; Hartgerink, J.D.; McHugh, K.J. Dynamic Imine Bonding Facilitates Mannan Release from a Nanofibrous Peptide Hydrogel. Bioconjug. Chem. 2023, 34, 193–203. [Google Scholar] [CrossRef] [PubMed]
- Kishimoto, T.; Akira, S.; Narazaki, M.; Taga, T. Interleukin-6 family of cytokines and gp130. Blood 1995, 86, 1243–1254. [Google Scholar] [CrossRef] [PubMed]
- Waldemer-Streyer, R.J.; Kim, D.; Chen, J. Muscle cell-derived cytokines in skeletal muscle regeneration. FEBS J. 2022, 289, 6463–6483. [Google Scholar] [CrossRef] [PubMed]
- Tenshin, H.; Teramachi, J.; Ashtar, M.; Hiasa, M.; Inoue, Y.; Oda, A.; Tanimoto, K.; Shimizu, S.; Higa, Y.; Harada, T.; et al. TGF-β-activated kinase-1 inhibitor LL-Z1640-2 reduces joint inflammation and bone destruction in mouse models of rheumatoid arthritis by inhibiting NLRP3 inflammasome, TACE, TNF-α and RANKL expression. Clin. Transl. Immunol. 2022, 11, e1371. [Google Scholar] [CrossRef]
- Keller, K.K.; Lindgaard, L.M.; Wogensen, L.; Dagnæs-Hansen, F.; Thomsen, J.S.; Sakaguchi, S.; Stengaard-Pedersen, K.; Hauge, E.M. SKG arthritis as a model for evaluating therapies in rheumatoid arthritis with special focus on bone changes. Rheumatol. Int. 2013, 33, 1127–1133. [Google Scholar] [CrossRef]
- Schiaffino, S. Muscle fiber type diversity revealed by anti-myosin heavy chain antibodies. FEBS J. 2018, 285, 3688–3694. [Google Scholar] [CrossRef] [PubMed]
- Thomas, S.S.; Mitch, W.E. Mechanisms stimulating muscle wasting in chronic kidney disease: The roles of the ubiquitin-proteasome system and myostatin. Clin. Exp. Nephrol. 2013, 17, 174–182. [Google Scholar] [CrossRef] [PubMed]
- Roy, A.; Sharma, A.K.; Nellore, K.; Narkar, V.A.; Kumar, A. TAK1 preserves skeletal muscle mass and mitochondrial function through redox homeostasis. FASEB BioAdv. 2020, 2, 538–553. [Google Scholar] [CrossRef] [PubMed]
- Hindi, S.M.; Sato, S.; Xiong, G.; Bohnert, K.R.; Gibb, A.A.; Gallot, Y.S.; McMillan, J.D.; Hill, B.G.; Uchida, S.; Kumar, A. TAK1 regulates skeletal muscle mass and mitochondrial function. JCI Insight 2018, 3, e98441. [Google Scholar] [CrossRef] [PubMed]
- Ogura, Y.; Hindi, S.M.; Sato, S.; Xiong, G.; Akira, S.; Kumar, A. TAK1 modulates satellite stem cell homeostasis and skeletal muscle repair. Nat. Commun. 2015, 6, 10123. [Google Scholar] [CrossRef] [PubMed]
- Fechtner, S.; Fox, D.A.; Ahmed, S. Transforming growth factor β activated kinase 1: A potential therapeutic target for rheumatic diseases. Rheumatology 2017, 56, 1060–1068. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Yang, W.; Chen, Y.; Zhang, Y.; Wang, X.; Yang, N.; Zhu, D. Extracellular signal-regulated kinase 1/2 mitogen-activated protein kinase pathway is involved in myostatin-regulated differentiation repression. Cancer Res. 2006, 66, 1320–1326. [Google Scholar] [CrossRef] [PubMed]
- Baig, M.H.; Ahmad, K.; Moon, J.S.; Park, S.Y.; Ho Lim, J.; Chun, H.J.; Qadri, A.F.; Hwang, Y.C.; Jan, A.T.; Ahmad, S.S.; et al. Myostatin and its Regulation: A Comprehensive Review of Myostatin Inhibiting Strategies. Front. Physiol. 2022, 13, 876078. [Google Scholar] [CrossRef] [PubMed]
- Sharma, M.; McFarlane, C.; Kambadur, R.; Kukreti, H.; Bonala, S.; Srinivasan, S. Myostatin: Expanding horizons. IUBMB Life 2015, 67, 589–600. [Google Scholar] [CrossRef] [PubMed]
- Huang, Z.; Chen, D.; Zhang, K.; Yu, B.; Chen, X.; Meng, J. Regulation of myostatin signaling by c-Jun N-terminal kinase in C2C12 cells. Cell. Signal. 2007, 19, 2286–2295. [Google Scholar] [CrossRef] [PubMed]
- Sebe, M.; Tsutsumi, R.; Senoura, S.; Kishi, J.; Iuchi, M.; Mishima, Y.; Tsutsumi, Y.M.; Kuroda, M.; Harada, N.; Nakaya, Y.; et al. Saturated fatty acids intake is associated with muscle atrophy in rheumatoid arthritis. JCSM Rapid Commun. 2022, 5, 86–101. [Google Scholar] [CrossRef]
- Zhao, M.; Svensson, M.N.D.; Venken, K.; Chawla, A.; Liang, S.; Engel, I.; Mydel, P.; Day, J.; Elewaut, D.; Bottini, N.; et al. Altered thymic differentiation and modulation of arthritis by invariant NKT cells expressing mutant ZAP70. Nat. Commun. 2018, 9, 2627. [Google Scholar] [CrossRef] [PubMed]
- Ishimoto, S.; Goto, I.; Kuroiwa, Y. Early morphological changes in the striated muscles in normal and dystrophic chickens. J. Comp. Pathol. 1988, 98, 69–79. [Google Scholar] [CrossRef] [PubMed]
- Bonetto, A.; Penna, F.; Minero, V.G.; Reffo, P.; Costamagna, D.; Bonelli, G.; Baccino, F.M.; Costelli, P. Glutamine prevents myostatin hyperexpression and protein hypercatabolism induced in C2C12 myotubes by tumor necrosis factor-α. Amino Acids 2011, 40, 585–594. [Google Scholar] [CrossRef] [PubMed]
- Magee, P.; Pearson, S.; Whittingham-Dowd, J.; Allen, J. PPARγ as a molecular target of EPA anti-inflammatory activity during TNF-α-impaired skeletal muscle cell differentiation. J. Nutr. Biochem. 2012, 23, 1440–1448. [Google Scholar] [CrossRef] [PubMed]
- Dong, B.; Hiasa, M.; Higa, Y.; Ohnishi, Y.; Endo, I.; Kondo, T.; Takashi, Y.; Tsoumpra, M.; Kainuma, R.; Sawatsubashi, S.; et al. Osteoblast/osteocyte-derived interleukin-11 regulates osteogenesis and systemic adipogenesis. Nat. Commun. 2022, 13, 7194. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kanai, M.; Ganbaatar, B.; Endo, I.; Ohnishi, Y.; Teramachi, J.; Tenshin, H.; Higa, Y.; Hiasa, M.; Mitsui, Y.; Hara, T.; et al. Inflammatory Cytokine-Induced Muscle Atrophy and Weakness Can Be Ameliorated by an Inhibition of TGF-β-Activated Kinase-1. Int. J. Mol. Sci. 2024, 25, 5715. https://doi.org/10.3390/ijms25115715
Kanai M, Ganbaatar B, Endo I, Ohnishi Y, Teramachi J, Tenshin H, Higa Y, Hiasa M, Mitsui Y, Hara T, et al. Inflammatory Cytokine-Induced Muscle Atrophy and Weakness Can Be Ameliorated by an Inhibition of TGF-β-Activated Kinase-1. International Journal of Molecular Sciences. 2024; 25(11):5715. https://doi.org/10.3390/ijms25115715
Chicago/Turabian StyleKanai, Mai, Byambasuren Ganbaatar, Itsuro Endo, Yukiyo Ohnishi, Jumpei Teramachi, Hirofumi Tenshin, Yoshiki Higa, Masahiro Hiasa, Yukari Mitsui, Tomoyo Hara, and et al. 2024. "Inflammatory Cytokine-Induced Muscle Atrophy and Weakness Can Be Ameliorated by an Inhibition of TGF-β-Activated Kinase-1" International Journal of Molecular Sciences 25, no. 11: 5715. https://doi.org/10.3390/ijms25115715
APA StyleKanai, M., Ganbaatar, B., Endo, I., Ohnishi, Y., Teramachi, J., Tenshin, H., Higa, Y., Hiasa, M., Mitsui, Y., Hara, T., Masuda, S., Yamagami, H., Yamaguchi, Y., Aihara, K.-i., Sebe, M., Tsutsumi, R., Sakaue, H., Matsumoto, T., & Abe, M. (2024). Inflammatory Cytokine-Induced Muscle Atrophy and Weakness Can Be Ameliorated by an Inhibition of TGF-β-Activated Kinase-1. International Journal of Molecular Sciences, 25(11), 5715. https://doi.org/10.3390/ijms25115715





