CXCL13 in Cerebrospinal Fluid: Clinical Value in a Large Cross-Sectional Study
Abstract
:1. Introduction
2. Results
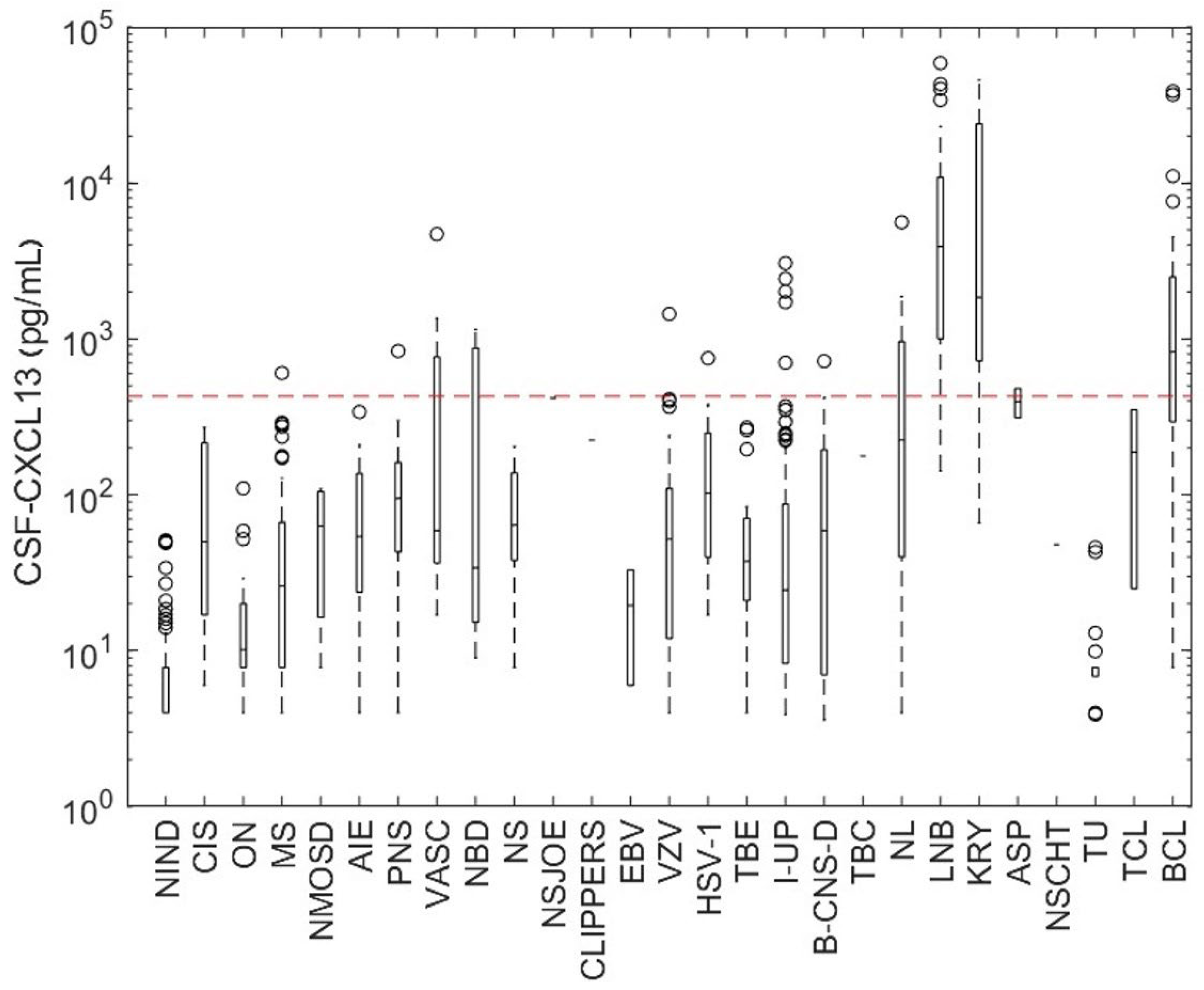
2.1. CSF-CXCL13 in Different Neurological Diseases
2.2. Patient and Demographic Characteristics
2.3. Correlation between CSF-CXCL13 and Other Routine CSF Parameters
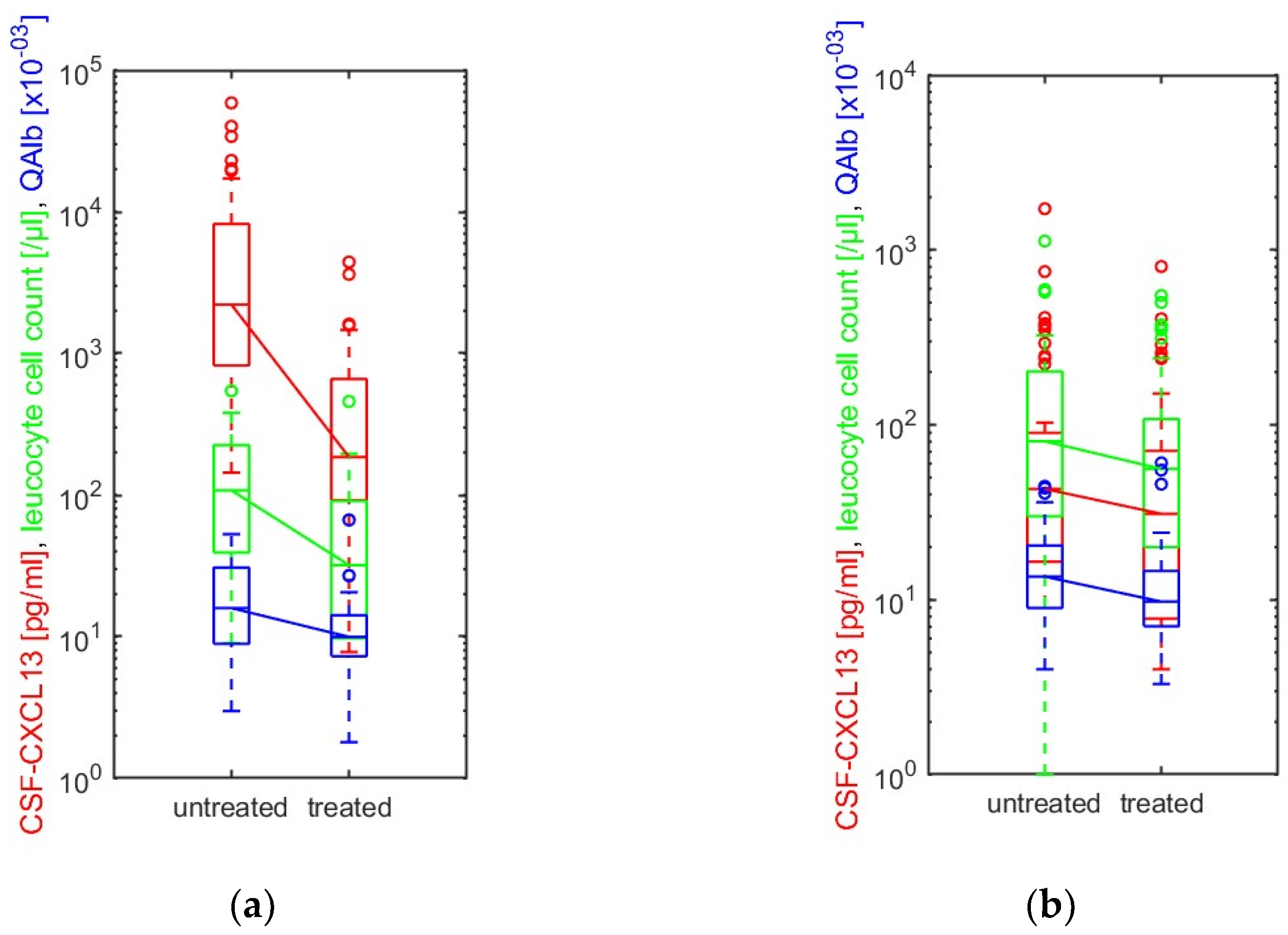
2.4. CSF-CXCL13 as a Treatment Response Marker in LNB and Other Infectious Neurological Diseases
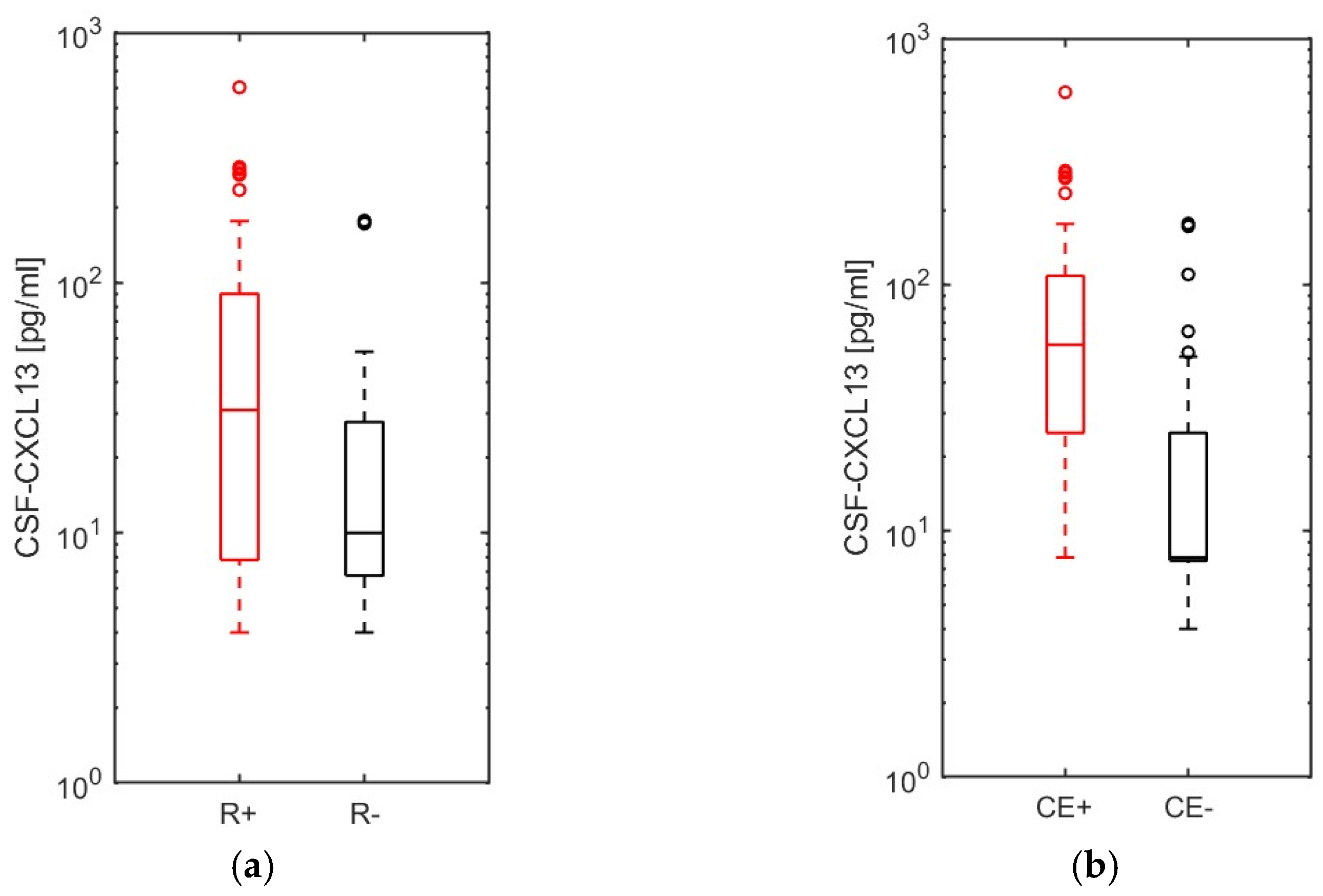
2.5. CSF-CXCL13 as an Activity Parameter in Multiple Sclerosis and Related Diseases
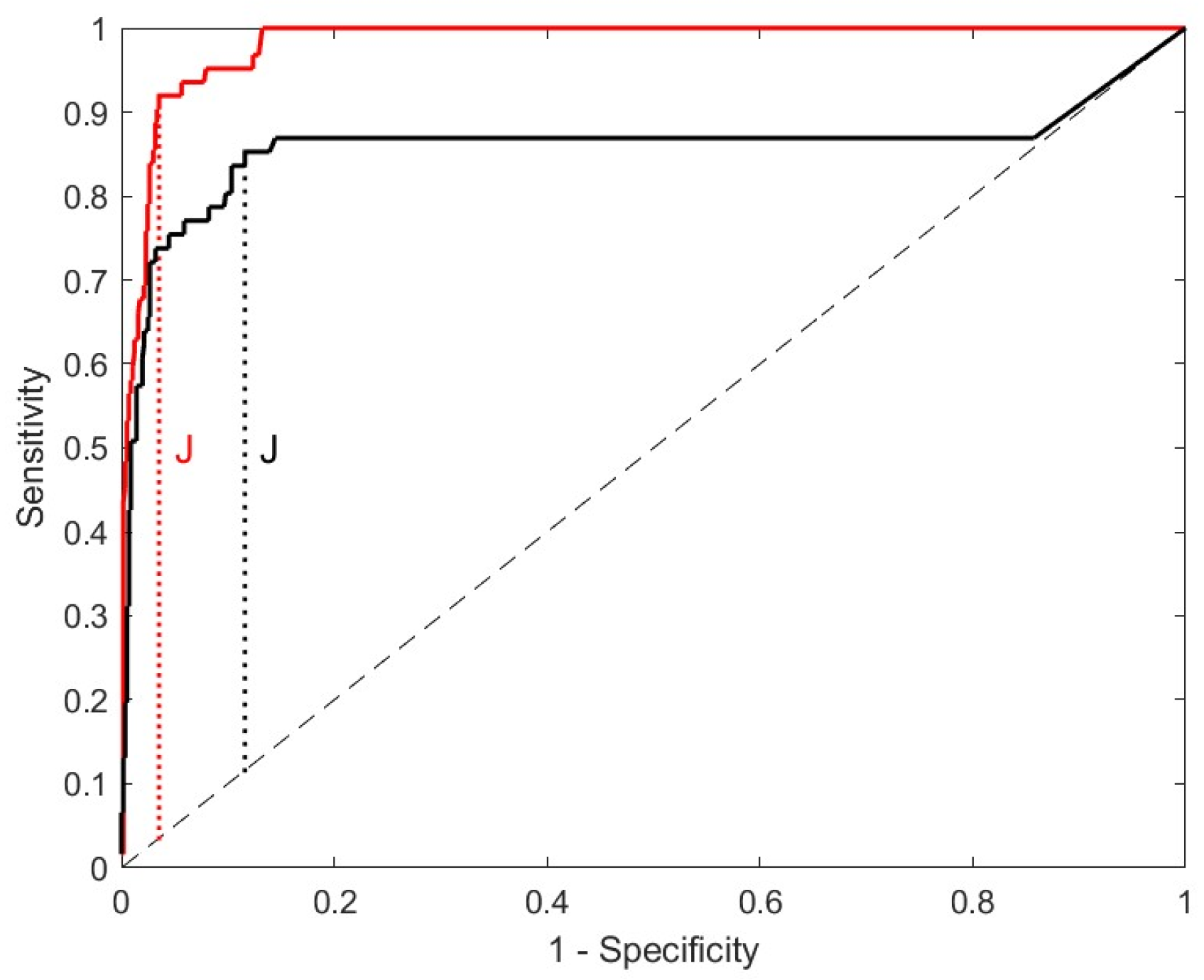
2.6. Differentiation of LNB from Other Neurological Disorders Using CSF-CXCL13–CSF-CXCL13 as a Diagnostic and Differentiation Marker
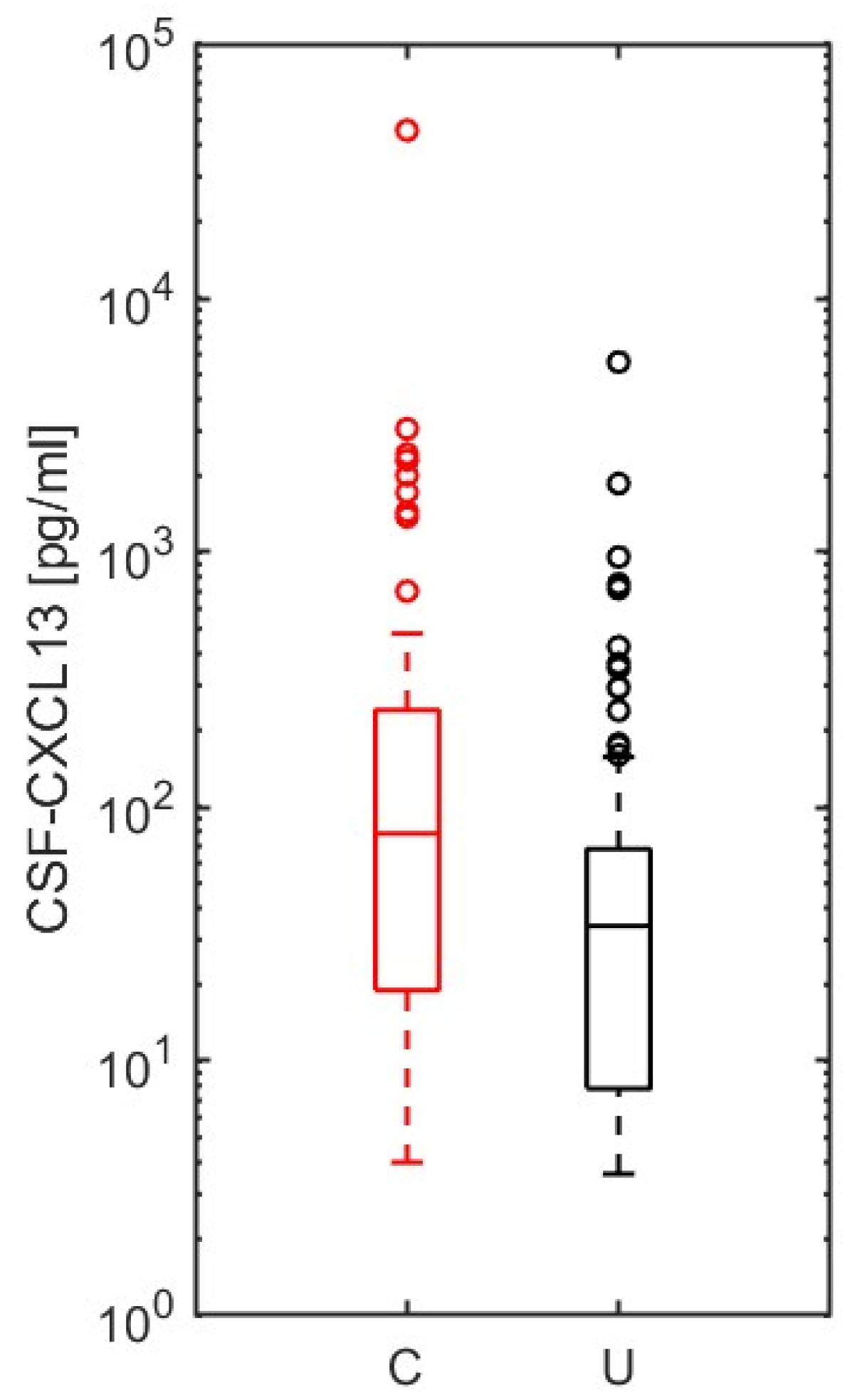
2.7. CSF-CXCL13 as a Possible Marker of Disease Severity to Differentiate an Uncomplicated from a Complicated Course in Neurological Infections of Different Origins
3. Discussion
Strengths and Limitations
4. Materials and Methods
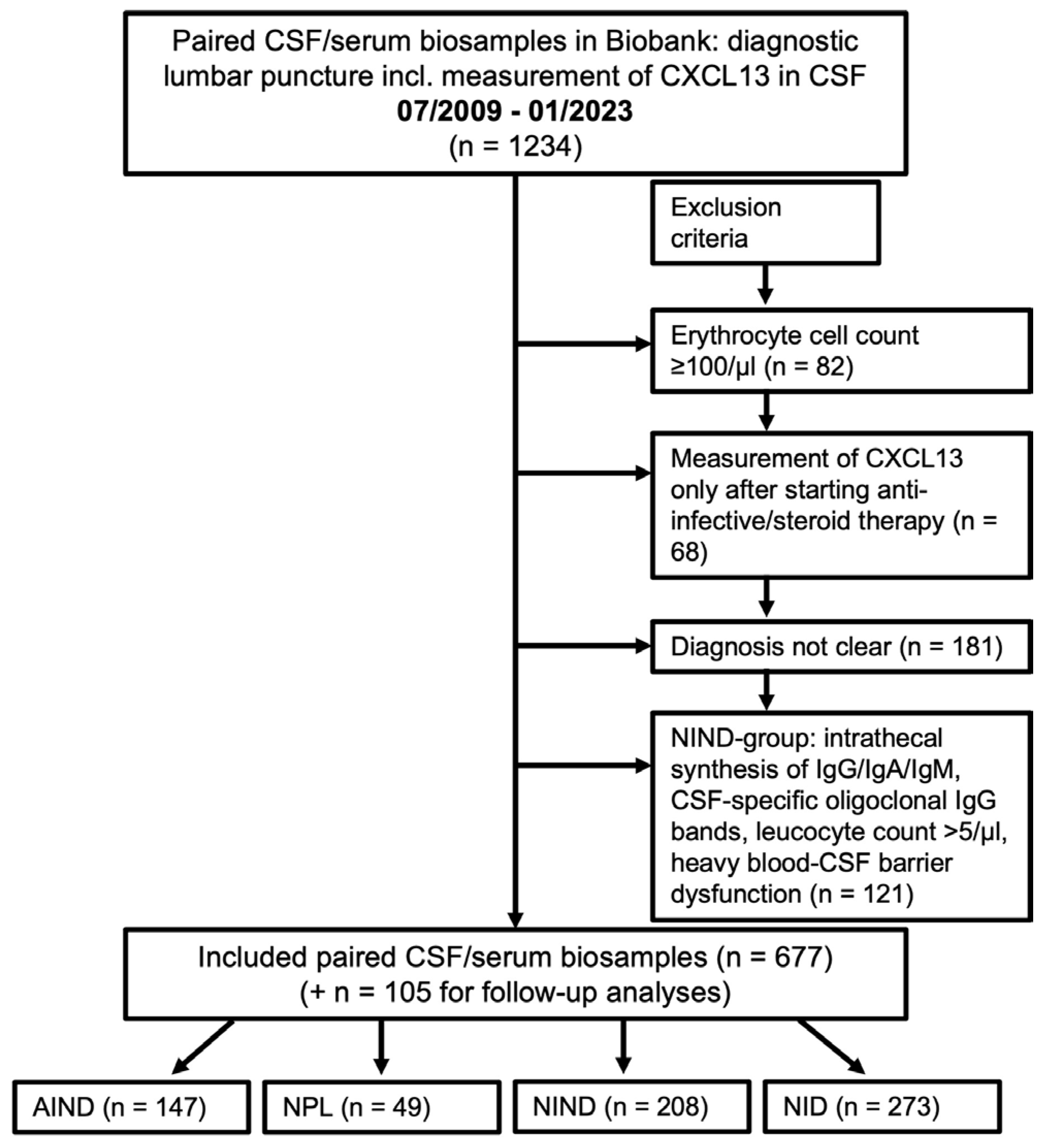
4.1. Patients and Selection Process
4.2. Laboratory CSF Analyses
4.3. Ethics
4.4. Statistics
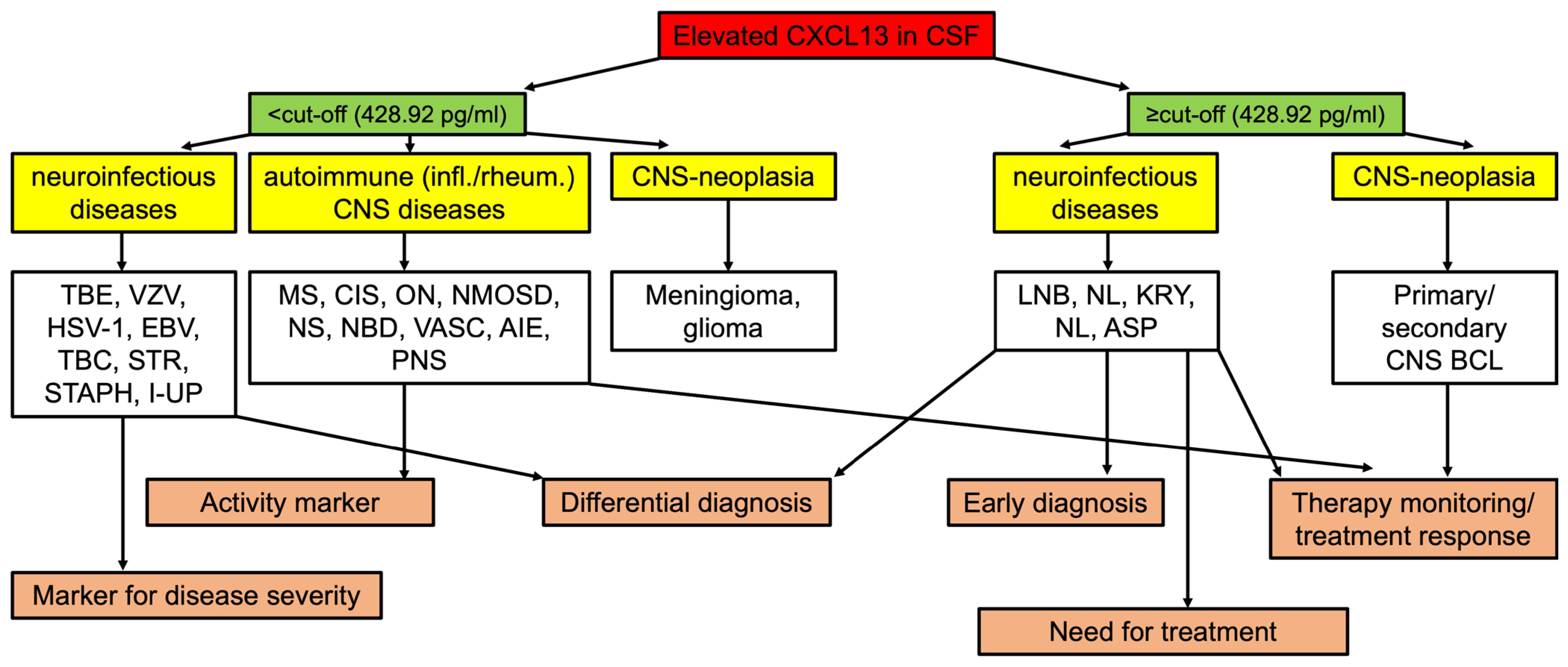
5. Conclusions and Future Perspective
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Allen, C.D.; Ansel, K.M.; Low, C.; Lesley, R.; Tamamura, H.; Fujii, N.; Cyster, J.G. Germinal center dark and light zone organization is mediated by CXCR4 and CXCR5. Nat. Immunol. 2004, 5, 943–952. [Google Scholar] [CrossRef] [PubMed]
- Vissers, J.L.; Hartgers, F.C.; Lindhout, E.; Figdor, C.G.; Adema, G.J. BLC (CXCL13) is expressed by different dendritic cell subsets in vitro and in vivo. Eur. J. Immfunol. 2001, 31, 1544–1549. [Google Scholar] [CrossRef]
- Carlsen, H.S.; Baekkevold, E.S.; Morton, H.C.; Haraldsen, G.; Brandtzaeg, P. Monocyte-like and mature macrophages produce CXCL13 (B cell-attracting chemokine 1) in inflammatory lesions with lymphoid neogenesis. Blood 2004, 104, 3021–3027. [Google Scholar] [CrossRef] [PubMed]
- Harrer, C.; Otto, F.; Pilz, G.; Haschke-Becher, E.; Trinka, E.; Hitzl, W.; Wipfler, P.; Harrer, A. The CXCL13/CXCR5-chemokine axis in neuroinflammation: Evidence of CXCR5 + CD4 T cell recruitment to CSF. Fluids Barriers CNS 2021, 18, 40. [Google Scholar] [CrossRef]
- Narayan, K.; Dail, D.; Li, L.; Cadavid, D.; Amrute, S.; Fitzgerald-Bocarsly, P.; Pachner, A.R. The nervous system as ectopic germinal center: CXCL13 and IgG in lyme neuroborreliosis. Ann. Neurol. 2005, 57, 813–823. [Google Scholar] [CrossRef] [PubMed]
- Rupprecht, T.A.; Plate, A.; Adam, M.; Wick, M.; Kastenbauer, S.; Schmidt, C.; Klein, M.; Pfister, H.-W.; Koedel, U. The chemokine CXCL13 is a key regulator of B cell recruitment to the cerebrospinal fluid in acute Lyme neuroborreliosis. J. Neuroinflammation 2009, 6, 42. [Google Scholar] [CrossRef] [PubMed]
- Rupprecht, T.A.; Kirschning, C.J.; Popp, B.; Kastenbauer, S.; Fingerle, V.; Pfister, H.W.; Koedel, U. Borrelia garinii induces CXCL13 production in human monocytes through Toll-like receptor 2. Infect. Immun. 2007, 75, 4351–4356. [Google Scholar] [CrossRef]
- Schmidt, C.; Plate, A.; Angele, B.; Pfister, H.W.; Wick, M.; Koedel, U.; Rupprecht, T.A. A prospective study on the role of CXCL13 in Lyme neuroborreliosis. Neurology 2011, 76, 1051–1058. [Google Scholar] [CrossRef]
- Senel, M.; Rupprecht, T.A.; Tumani, H.; Pfister, H.W.; Ludolph, A.C.; Brettschneider, J. The chemokine CXCL13 in acute neuroborreliosis. J. Neurol. Neurosurg. Psychiatry 2010, 81, 929–933. [Google Scholar] [CrossRef]
- Wagner, J.N.; Weis, S.; Kubasta, C.; Panholzer, J.; von Oertzen, T.J. CXCL13 as a diagnostic marker of neuroborreliosis and other neuroinflammatory disorders in an unselected group of patients. J. Neurol. 2018, 265, 74–81. [Google Scholar] [CrossRef]
- Strle, F.; Henningsson, A.J.; Strle, K. Diagnostic Utility of CXCL13 in Lyme Neuroborreliosis. Clin. Infect. Dis. 2021, 72, 1727–1729. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Han, X.; Liu, A.; Bao, F.; Peng, Y.; Tao, L.; Ma, M.; Bai, R.; Dai, X. Chemokine CXC Ligand 13 in Cerebrospinal Fluid Can Be Used as an Early Diagnostic Biomarker for Lyme Neuroborreliosis: A Meta-Analysis. J. Interferon. Cytokine Res. 2017, 37, 433–439. [Google Scholar] [CrossRef]
- Hytönen, J.; Kortela, E.; Waris, M.; Puustinen, J.; Salo, J.; Oksi, J. CXCL13 and neopterin concentrations in cerebrospinal fluid of patients with Lyme neuroborreliosis and other diseases that cause neuroinflammation. J. Neuroinflammation 2014, 11, 103. [Google Scholar] [CrossRef] [PubMed]
- Kowarik, M.C.; Cepok, S.; Sellner, J.; Grummel, V.; Weber, M.S.; Korn, T.; Berthele, A.; Hemmer, B. CXCL13 is the major determinant for B cell recruitment to the CSF during neuroinflammation. J. Neuroinflammation 2012, 9, 93. [Google Scholar] [CrossRef] [PubMed]
- Krumbholz, M.; Theil, D.; Cepok, S.; Hemmer, B.; Kivisäkk, P.; Ransohoff, R.M.; Hofbauer, M.; Farina, C.; Derfuss, T.; Hartle, C.; et al. Chemokines in multiple sclerosis: CXCL12 and CXCL13 up-regulation is differentially linked to CNS immune cell recruitment. Brain 2006, 129, 200–211. [Google Scholar] [CrossRef] [PubMed]
- Pilz, G.; Steger, R.; Wipfler, P.; Otto, F.; Afazel, S.; Haschke-Becher, E.; Trinka, E.; Harrer, A.; Beyond, L.N.B. Beyond LNB: Real life data on occurrence and extent of CSF CXCL13 in neuroinflammatory diseases. J. Neuroimmunol 2020, 338, 577087. [Google Scholar] [CrossRef] [PubMed]
- Abu-Rumeileh, S.; Garibashvili, T.; Hagemann, J.B.; Still, V.; Bachhuber, F.; Otto, M.; Tumani, H.; Senel, M. A one-year longitudinal evaluation of cerebrospinal fluid and blood neurochemical markers in a patient with cryptococcal meningitis complicated by ischemic stroke. J. Neurol. Sci. 2022, 432, 120090. [Google Scholar] [CrossRef]
- Dersch, R.; Hottenrott, T.; Senel, M.; Lehmensiek, V.; Tumani, H.; Rauer, S.; Stich, O. The chemokine CXCL13 is elevated in the cerebrospinal fluid of patients with neurosyphilis. Fluids Barriers CNS 2015, 12, 12. [Google Scholar] [CrossRef]
- Fischer, L.; Korfel, A.; Pfeiffer, S.; Kiewe, P.; Volk, H.D.; Cakiroglu, H.; Widmann, T.; Thiel, E. CXCL13 and CXCL12 in central nervous system lymphoma patients. Clin. Cancer Res. 2009, 15, 5968–5973. [Google Scholar] [CrossRef]
- Leypoldt, F.; Höftberger, R.; Titulaer, M.J.; Armangue, T.; Gresa-Arribas, N.; Jahn, H.; Rostásy, K.; Schlumberger, W.; Meyer, T.; Wandinger, K.P.; et al. Investigations on CXCL13 in anti-N-methyl-D-aspartate receptor encephalitis: A potential biomarker of treatment response. JAMA Neurol. 2015, 72, 180–186. [Google Scholar] [CrossRef]
- Rupprecht, T.A.; Manz, K.M.; Fingerle, V.; Lechner, C.; Klein, M.; Pfirrmann, M.; Koedel, U. Diagnostic value of cerebrospinal fluid CXCL13 for acute Lyme neuroborreliosis. A systematic review and meta-analysis. Clin. Microbiol. Infect. 2018, 24, 1234–1240. [Google Scholar] [CrossRef]
- Barstad, B.; Henningsson, A.J.; Tveitnes, D.; Ushakova, A.; Noraas, S.; Ask, I.S.; Bosse, F.J.; Øymar, K. Cerebrospinal fluid cytokines and chemokines in children with Lyme neuroborreliosis; pattern and diagnostic utility. Cytokine 2020, 130, 155023. [Google Scholar] [CrossRef] [PubMed]
- Cerar, T.; Ogrinc, K.; Lotric-Furlan, S.; Kobal, J.; Levicnik-Stezinar, S.; Strle, F.; Ruzić-Sabljic, E. Diagnostic value of cytokines and chemokines in lyme neuroborreliosis. Clin. Vaccine Immunol. 2013, 20, 1578–1584. [Google Scholar] [CrossRef] [PubMed]
- Eckman, E.A.; Clausen, D.M.; Herdt, A.R.; Pacheco-Quinto, J.; Halperin, J.J. Specificity and Diagnostic Utility of Cerebrospinal Fluid CXCL13 in Lyme Neuroborreliosis. Clin. Infect. Dis. 2020, 72, 1719–1726. [Google Scholar] [CrossRef] [PubMed]
- Gorkom, T.; Arkel, G.H.J.; Heron, M.; Voet, W.; Thijsen, S.F.T.; Kremer, K. The Usefulness of Two CXCL13 Assays on Cerebrospinal Fluid for the Diagnosis of Lyme Neuroborreliosis: A Retrospective Study in a Routine Clinical Setting. J. Clin. Microbiol. 2021, 59, e0025521. [Google Scholar] [CrossRef] [PubMed]
- Henningsson, A.J.; Lager, M.; Brännström, R.; Tjernberg, I.; Skogman, B.H. The chemokine CXCL13 in cerebrospinal fluid in children with Lyme neuroborreliosis. Eur. J. Clin. Microbiol. Infect. Dis. 2018, 37, 1983–1991. [Google Scholar] [CrossRef] [PubMed]
- Knudtzen, F.C.; Nilsson, A.C.; Hovius, J.W.; Skarphedinsson, S. The predictive value of CXCL13 in suspected Lyme neuroborreliosis: A retrospective cross-sectional study. Eur. J. Clin. Microbiol. Infect. Dis. 2020, 39, 1461–1470. [Google Scholar] [CrossRef] [PubMed]
- Leth, T.A.; Dessau, R.B.; Møller, J.K. Discriminating between Lyme neuroborreliosis and other central nervous system infections by use of biomarkers CXCL13 and IL-6. Ticks Tick Borne Dis. 2022, 13, 101984. [Google Scholar] [CrossRef]
- Lintner, H.; Hochgatterer-Rechberger, P.; Pischinger, B.; Seier, J.; Vollmann, P.; Haushofer, A.; Rittner, H.; Sommer, C.; Topakian, R. Sensitivity and specificity of cerebrospinal fluid CXCL13 for diagnosing Lyme neuroborreliosis—A study on 1410 patients and review of the literature. J. Neurol. Sci. 2020, 414, 116843. [Google Scholar] [CrossRef]
- Ljøstad, U.; Mygland, A. CSF B—Lymphocyte chemoattractant (CXCL13) in the early diagnosis of acute Lyme neuroborreliosis. J. Neurol. 2008, 255, 732–737. [Google Scholar] [CrossRef]
- Markowicz, M.; Schötta, A.M.; Kundi, M.; Bogovič, P.; Ogrinc, K.; Strle, F.; Stanek, G. CXCL13 concentrations in cerebrospinal fluid of patients with Lyme neuroborreliosis and other neurological disorders determined by Luminex and ELISA. Ticks Tick Borne Dis. 2018, 9, 1137–1142. [Google Scholar] [CrossRef] [PubMed]
- Marra, C.M.; Tantalo, L.C.; Sahi, S.K.; Maxwell, C.L.; Lukehart, S.A. CXCL13 as a cerebrospinal fluid marker for neurosyphilis in HIV-infected patients with syphilis. Sex Transm. Dis. 2010, 37, 283–287. [Google Scholar] [CrossRef] [PubMed]
- Pícha, D.; Moravcová, L.; Smíšková, D. Prospective study on the chemokine CXCL13 in neuroborreliosis and other aseptic neuroinfections. J. Neurol. Sci. 2016, 368, 214–220. [Google Scholar] [CrossRef] [PubMed]
- Remy, M.M.; Schöbi, N.; Kottanattu, L.; Pfister, S.; Duppenthaler, A.; Suter-Riniker, F. Cerebrospinal fluid CXCL13 as a diagnostic marker of neuroborreliosis in children: A retrospective case-control study. J. Neuroinflammation 2017, 14, 173. [Google Scholar] [CrossRef] [PubMed]
- Tjernberg, I.; Henningsson, A.J.; Eliasson, I.; Forsberg, P.; Ernerudh, J. Diagnostic performance of cerebrospinal fluid chemokine CXCL13 and antibodies to the C6-peptide in Lyme neuroborreliosis. J. Infect. 2011, 62, 149–158. [Google Scholar] [CrossRef]
- Van Burgel, N.D.; Bakels, F.; Kroes, A.C.; van Dam, A.P. Discriminating Lyme neuroborreliosis from other neuroinflammatory diseases by levels of CXCL13 in cerebrospinal fluid. J. Clin. Microbiol. 2011, 49, 2027–2030. [Google Scholar] [CrossRef]
- Wutte, N.; Berghold, A.; Löffler, S.; Zenz, W.; Daghofer, E.; Krainberger, I.; Kleinert, G.; Aberer, E. CXCL13 chemokine in pediatric and adult neuroborreliosis. Acta Neurol. Scand. 2011, 124, 321–328. [Google Scholar] [CrossRef]
- Henningsson, A.J.; Gyllemark, P.; Lager, M.; Skogman, B.H.; Tjernberg, I. Evaluation of two assays for CXCL13 analysis in cerebrospinal fluid for laboratory diagnosis of Lyme neuroborreliosis. Apmis 2016, 124, 985–990. [Google Scholar] [CrossRef]
- Erhart, D.K.; Bracknies, V.; Lutz-Schuhbauer, S.; Wigand, S.; Tumani, H. The special role of CXCL13 in Lyme neuroborreliosis: A case report. Neurol. Res. Pract. 2022, 4, 3. [Google Scholar] [CrossRef]
- Fujimori, J.; Nakashima, I.; Kuroda, H.; Fujihara, K.; Aoki, M. Cerebrospinal fluid CXCL13 is a prognostic marker for aseptic meningitis. J. Neuroimmunol. 2014, 273, 77–84. [Google Scholar] [CrossRef]
- Pilz, G.; Wipfler, P.; Otto, F.; Hitzl, W.; Afazel, S.; Haschke-Becher, E.; Trinka, E.; Harrer, A. Cerebrospinal fluid CXLC13 indicates disease course in neuroinfection: An observational study. J. Neuroinflammation 2019, 16, 13. [Google Scholar] [CrossRef]
- Rubenstein, J.L.; Wong, V.S.; Kadoch, C.; Gao, H.X.; Barajas, R.; Chen, L.; Josephson, S.A.; Scott, B.; Douglas, V.; Maiti, M.; et al. CXCL13 plus interleukin 10 is highly specific for the diagnosis of CNS lymphoma. Blood 2013, 121, 4740–4748. [Google Scholar] [CrossRef] [PubMed]
- Zhong, X.; Wang, H.; Dai, Y.; Wu, A.; Bao, J.; Xu, W.; Cheng, C.; Lu, Z.; Qiu, W.; Hu, X. Cerebrospinal fluid levels of CXCL13 are elevated in neuromyelitis optica. J. Neuroimmunol. 2011, 240–241, 104–108. [Google Scholar] [CrossRef] [PubMed]
- Alvarez, E.; Piccio, L.; Mikesell, R.J.; Klawiter, E.C.; Parks, B.J.; Naismith, R.T.; Cross, A.H. CXCL13 is a biomarker of inflammation in multiple sclerosis, neuromyelitis optica, and other neurological conditions. Mult. Scler. J. 2013, 19, 1204–1208. [Google Scholar] [CrossRef]
- Khademi, M.; Kockum, I.; Andersson, M.L.; Iacobaeus, E.; Brundin, L.; Sellebjerg, F.; Hillert, J.; Piehl, F.; Olsson, T. Cerebrospinal fluid CXCL13 in multiple sclerosis: A suggestive prognostic marker for the disease course. Mult. Scler. 2011, 17, 335–343. [Google Scholar] [CrossRef] [PubMed]
- Novakova, L.; Axelsson, M.; Khademi, M.; Zetterberg, H.; Blennow, K.; Malmeström, C.; Piehl, F.; Olsson, T.; Lycke, J. Cerebrospinal fluid biomarkers as a measure of disease activity and treatment efficacy in relapsing-remitting multiple sclerosis. J. Neurochem. 2017, 141, 296–304. [Google Scholar] [CrossRef] [PubMed]
- Sellebjerg, F.; Börnsen, L.; Khademi, M.; Krakauer, M.; Olsson, T.; Frederiksen, J.L.; Sørensen, P.S. Increased cerebrospinal fluid concentrations of the chemokine CXCL13 in active MS. Neurology 2009, 73, 2003–2010. [Google Scholar] [CrossRef] [PubMed]
- Rupprecht, T.A.; Pfister, H.W.; Angele, B.; Kastenbauer, S.; Wilske, B.; Koedel, U. The chemokine CXCL13 (BLC): A putative diagnostic marker for neuroborreliosis. Neurology 2005, 65, 448–450. [Google Scholar] [CrossRef]
- Tumani, H.; Nolker, G.; Reiber, H. Relevance of cerebrospinal fluid variables for early diagnosis of neuroborreliosis. Neurology 1995, 45, 1663. [Google Scholar] [CrossRef]
- Hammers-Berggren, S.; Hansen, K.; Lebech, A.-M.; Karlsson, M. Borrelia burgdorferi-specific intrathecal antibody production in neuroborreliosis. Neurology 1993, 43, 169. [Google Scholar] [CrossRef]
- Smith, J.R.; Braziel, R.M.; Paoletti, S.; Lipp, M.; Uguccioni, M.; Rosenbaum, J.T. Expression of B-cell-attracting chemokine 1 (CXCL13) by malignant lymphocytes and vascular endothelium in primary central nervous system lymphoma. Blood 2003, 101, 815–821. [Google Scholar] [CrossRef]
- Schiffer, L.; Kielstein, J.T.; Haubitz, M.; Lührs, H.; Witte, T.; Haller, H.; Kümpers, P.; Schiffer, M. Elevation of serum CXCL13 in SLE as well as in sepsis. Lupus 2011, 20, 507–511. [Google Scholar] [CrossRef] [PubMed]
- Toczylowski, K.; Grygorczuk, S.; Osada, J.; Wojtkowska, M.; Bojkiewicz, E.; Wozinska-Klepadlo, M.; Potocka, P.; Sulik, A. Evaluation of cerebrospinal fluid CXCL13 concentrations and lymphocyte subsets in tick-borne encephalitis. Int. J. Infect. Dis. 2020, 93, 40–47. [Google Scholar] [CrossRef]
- Cimperman, J.; Maraspin, V.; Lotric-Furlan, S.; Ruzić-Sabljić, E.; Avsic-Zupanc, T.; Strle, F. Double infection with tick borne encephalitis virus and Borrelia burgdorferi sensu lato. Wien Klin Wochenschr 2002, 114, 620–622. [Google Scholar] [PubMed]
- Garcia-Monco, J.C.; Benach, J.L. Lyme Neuroborreliosis: Clinical Outcomes, Controversy, Pathogenesis, and Polymicrobial Infections. Ann. Neurol. 2019, 85, 21–31. [Google Scholar] [CrossRef] [PubMed]
- Holub, M.; Klučková, Z.; Beran, O.; Aster, V.; Lobovská, A. Lymphocyte subset numbers in cerebrospinal fluid: Comparison of tick-borne encephalitis and neuroborreliosis. Acta Neurol. Scand. 2002, 106, 302–308. [Google Scholar] [CrossRef]
- Senel, M.; Rapp, D.; Mayer, B.; Jesse, S.; Süssmuth, S.D.; Otto, M.; Lewerenz, J.; Tumani, H. Tick-Borne Encephalitis: A Differential Pattern of Intrathecal Humoral Immune Response and Inflammatory Cell Composition Compared with Other Viral CNS Infections. Cells 2020, 9, 2169. [Google Scholar] [CrossRef]
- Pietikäinen, A.; Maksimow, M.; Kauko, T.; Hurme, S.; Salmi, M.; Hytönen, J. Cerebrospinal fluid cytokines in Lyme neuroborreliosis. J. Neuroinflammation 2016, 13, 273. [Google Scholar] [CrossRef]
- Mabray, M.C.; Barajas, R.F.; Villanueva-Meyer, J.E.; Zhang, C.A.; Valles, F.E.; Rubenstein, J.L.; Cha, S. The Combined Performance of ADC, CSF CXC Chemokine Ligand 13, and CSF Interleukin 10 in the Diagnosis of Central Nervous System Lymphoma. AJNR Am. J. Neuroradiol. 2016, 37, 74–79. [Google Scholar] [CrossRef]
- Maeyama, M.; Sasayama, T.; Tanaka, K.; Nakamizo, S.; Tanaka, H.; Nishihara, M.; Fujita, Y.; Sekiguchi, K.; Kohta, M.; Mizukawa, K.; et al. Multi-marker algorithms based on CXCL13, IL-10, sIL-2 receptor, and β2-microglobulin in cerebrospinal fluid to diagnose CNS lymphoma. Cancer Med. 2020, 9, 4114–4125. [Google Scholar] [CrossRef]
- Masouris, I.; Manz, K.; Pfirrmann, M.; Dreyling, M.; Angele, B.; Straube, A.; Langer, S.; Huber, M.; Koedel, U.; Von Baumgarten, L. CXCL13 and CXCL9 CSF Levels in Central Nervous System Lymphoma-Diagnostic, Therapeutic, and Prognostic Relevance. Front. Neurol. 2021, 12, 654543. [Google Scholar] [CrossRef] [PubMed]
- Bernard, C.; Maucort-Boulch, D.; Varron, L.; Charlier, C.; Sitbon, K.; Freymond, N.; Bouhour, D.; Hot, A.; Masquelet, A.C.; Valeyre, D.; et al. Cryptococcosis in sarcoidosis: CryptOsarc, a comparative study of 18 cases. QJM Int. J. Med. 2013, 106, 523–539. [Google Scholar] [CrossRef] [PubMed]
- Zajkowska, J.; Moniuszko-Malinowska, A.; Pancewicz, S.A.; Muszyńska-Mazur, A.; Kondrusik, M.; Grygorczuk, S.; Swierzbińska-Pijanowska, R.; Dunaj, J. Czupryna P Evaluation of CXCL10, CXCL11, CXCL12 and CXCL13 chemokines in serum and cerebrospinal fluid in patients with tick borne encephalitis (TBE). Adv. Med. Sci. 2011, 56, 311–317. [Google Scholar] [CrossRef] [PubMed]
- Irani, D.N. Regulated Production of CXCL13 within the Central Nervous System. J. Clin. Cell. Immunol. 2016, 7, 460. [Google Scholar] [CrossRef] [PubMed]
- Brettschneider, J.; Czerwoniak, A.; Senel, M.; Fang, L.; Kassubek, J.; Pinkhardt, E.; Lauda, F.; Kapfer, T.; Jesse, S.; Lehmensiek, V.; et al. The chemokine CXCL13 is a prognostic marker in clinically isolated syndrome (CIS). PLoS ONE 2010, 5, e11986. [Google Scholar] [CrossRef] [PubMed]
- Pilz, G.; Sakic, I.; Wipfler, P.; Kraus, J.; Haschke-Becher, E.; Hitzl, W.; Trinka, E.; Harrer, A. Chemokine CXCL13 in serum, CSF and blood-CSF barrier function: Evidence of compartment restriction. Fluids Barriers CNS 2020, 17, 7. [Google Scholar] [CrossRef]
- Harrer, C.; Otto, F.; Radlberger, R.F.; Moser, T.; Pilz, G.; Wipfler, P.; Harrer, A. The CXCL13/CXCR5 Immune Axis in Health and Disease-Implications for Intrathecal B Cell Activities in Neuroinflammation. Cells 2022, 11, 2649. [Google Scholar] [CrossRef]
- Serafini, B.; Rosicarelli, B.; Magliozzi, R.; Stigliano, E.; Aloisi, F. Detection of ectopic B-cell follicles with germinal centers in the meninges of patients with secondary progressive multiple sclerosis. Brain Pathol. 2004, 14, 164–174. [Google Scholar] [CrossRef]
- Olesen, M.N.; Soelberg, K.; Debrabant, B.; Nilsson, A.C.; Lillevang, S.T.; Grauslund, J.; Brandslund, I.; Madsen, J.S.; Paul, F.; Smith, T.J. Cerebrospinal fluid biomarkers for predicting development of multiple sclerosis in acute optic neuritis: A population-based prospective cohort study. J. Neuroinflammation 2019, 16, 59. [Google Scholar] [CrossRef]
- Olesen, M.N.; Nilsson, A.C.; Pihl-Jensen, G.; Soelberg, K.K.; Olsen, D.A.; Brandslund, I.; Lillevang, S.T.; Madsen, J.S.; Frederiksen, J.L.; Asgari, N. Highly sensitive quantification of optic neuritis intrathecal biomarker CXCL13. Mult. Scler. Relat. Disord. 2020, 44, 102281. [Google Scholar] [CrossRef]
- DiSano, K.D.; Gilli, F.; Pachner, A.R. Intrathecally produced CXCL13: A predictive biomarker in multiple sclerosis. Mult. Scler. J. Exp. Transl. Clin. 2020, 6, 2055217320981396. [Google Scholar] [CrossRef] [PubMed]
- Kosmidis, M.H.; Bozikas, V.P.; Giannouli, V.; Karavatos, A.; Fokas, K. Familial comorbidity of bipolar disorder and multiple sclerosis: Genetic susceptibility, coexistence or causal relationship? Behav. Neurol. 2012, 25, 341–349. [Google Scholar] [CrossRef] [PubMed]
- Coppedè, F.; Lopomo, A.; Spisni, R.; Migliore, L. Genetic and epigenetic biomarkers for diagnosis, prognosis and treatment of colorectal cancer. World J. Gastroenterol. 2014, 20, 943–956. [Google Scholar] [CrossRef]
- Gul, A.; Ohno, S. HLA-B*51 and Behçet Disease. Ocul. Immunol. Inflamm. 2012, 20, 37–43. [Google Scholar] [CrossRef] [PubMed]
- Helliwell, A.M.; Stockwell, P.A.; Edgar, C.D.; Chatterjee, A.; Tate, W.P. Dynamic Epigenetic Changes during a Relapse and Recovery Cycle in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome. Int. J. Mol. Sci. 2022, 23, 11852. [Google Scholar] [CrossRef]
- Moore, L.D.; Le, T.; Fan, G. DNA methylation and its basic function. Neuropsychopharmacology 2013, 38, 23–38. [Google Scholar] [CrossRef]
- Thompson, A.J.; Banwell, B.L.; Barkhof, F.; Carroll, W.M.; Coetzee, T.; Comi, G.; Correale, J.; Fazekas, F.; Filippi, M.; Freedman, M.S.; et al. Diagnosis of multiple sclerosis: 2017 revisions of the McDonald criteria. Lancet Neurol. 2018, 17, 162–173. [Google Scholar] [CrossRef]
- Devine, M.F.; Kothapalli, N.; Elkhooly, M.; Dubey, D. Paraneoplastic neurological syndromes: Clinical presentations and management. Ther. Adv. Neurol. Disord. 2021, 14, 1756286420985323. [Google Scholar] [CrossRef]
- Venkatesan, A.; Tunkel, A.R.; Bloch, K.C.; Lauring, A.S.; Sejvar, J.; Bitnun, A.; Stahl, J.P.; Mailles, A.; Drebot, M.; Rupprecht, C.E.; et al. Case definitions, diagnostic algorithms, and priorities in encephalitis: Consensus statement of the international encephalitis consortium. Clin. Infect. Dis. 2013, 57, 1114–1128. [Google Scholar] [CrossRef]
- Graus, F.; Vogrig, A.; Muñiz-Castrillo, S.; Antoine, J.G.; Desestret, V.; Dubey, D.; Giometto, B.; Irani, S.R.; Joubert, B.; Leypoldt, F.; et al. Updated Diagnostic Criteria for Paraneoplastic Neurologic Syndromes. Neurol. Neuroimmunol. Neuroinflamm. 2021, 8, e1014. [Google Scholar] [CrossRef]
- Davatchi, F.; Assaad-Khalil, S.; Calamia, K.T.; Crook, J.E.; Sadeghi-Abdollahi, B.; Schirmer, M.; Tzellos, T.; Zouboulis, C.C.; Akhlagi, M.; Al-Dalaan, A.; et al. The International Criteria for Behçet’s Disease (ICBD): A collaborative study of 27 countries on the sensitivity and specificity of the new criteria. J. Eur. Aca Dermatol. Venereol. 2014, 28, 338–347. [Google Scholar] [CrossRef]
- Wechsler, B.; Davatchi, I.F.; Mizushima, Y.; Hamza, M.; Dilsen, N.; Kansu, E.; Yazici, H.; Barnes, C.G.; Chamberlain, M.A.; James, D.G.; et al. Evaluation of diagnostic (‘classification’) criteria in Behçet’s disease—Towards internationally agreed criteria. The International Study Group for Behçet’s disease. Br. J. Rheumatol. 1992, 31, 299–308. [Google Scholar] [CrossRef]
- Klein, M.; Angstwurm, K.; Esser, S.; Hahn, K.; Maschke, M.; Scheithauer, S.; Schoefer, H.; Sturzenegger, M.; Wildemann, B.; Weber, J. German guidelines on the diagnosis and treatment of neurosyphilis. Neurol. Res. Pract. 2020, 2, 33. [Google Scholar] [CrossRef] [PubMed]
- Stanek, G.; Fingerle, V.; Hunfeld, K.P.; Jaulhac, B.; Kaiser, R.; Krause, A.; Kristoferitsch, W.; O’Connell, S.; Ornstein, K.; Strle, F.; et al. Lyme borreliosis: Clinical case definitions for diagnosis and management in Europe. Clin. Microbiol. Infect. 2011, 17, 69–79. [Google Scholar] [CrossRef]
- Tumani, H.; Petereit, H.F.; Gerritzen, A.; Gross, C.C.; Huss, A.; Isenmann, S.; Jesse, S.; Khalil, M.; Lewczuk, P.; Lewerenz, J.; et al. S1 guidelines “lumbar puncture and cerebrospinal fluid analysis” (abridged and translated version). Neurol. Res. Pract. 2020, 2, 8. [Google Scholar] [CrossRef] [PubMed]
- Teunissen, C.E.; Tumani, H.; Engelborghs, S.; Mollenhauer, B. Biobanking of CSF: International standardization to optimize biomarker development. Clin. Biochem. 2014, 47, 288–292. [Google Scholar] [CrossRef] [PubMed]
- Reiber, H. Flow rate of cerebrospinal fluid (CSF)—A concept common to normal blood-CSF barrier function and to dysfunction in neurological diseases. J. Neurol. Sci. 1994, 122, 189–203. [Google Scholar] [CrossRef]
- Reiber, H. Cerebrospinal fluid—Physiology, analysis and interpretation of protein patterns for diagnosis of neurological diseases. Mult. Scler. 1998, 4, 99–107. [Google Scholar] [CrossRef]
- Reiber, H.; Peter, J.B. Cerebrospinal fluid analysis: Disease-related data patterns and evaluation programs. J. Neurol. Sci. 2001, 184, 101–122. [Google Scholar] [CrossRef]
- Reiber, H.; Ungefehr, S.; Jacobi, C. The intrathecal, polyspecific and oligoclonal immune response in multiple sclerosis. Mult. Scler. 1998, 4, 111–117. [Google Scholar] [CrossRef]
- Cardillo, G. Dunn’s Test: A Procedure for Multiple, Not Parametric, Comparisons. 2006. Available online: http://www.mathworks.com/matlabcentral/fileexchange/12827 (accessed on 9 July 2023).
- Jones, C.M.; Athanasiou, T. Summary receiver operating characteristic curve analysis techniques in the evaluation of diagnostic tests. Ann. Thorac. Surg. 2005, 79, 16–20. [Google Scholar] [CrossRef] [PubMed]
- Youden, W.J. Index for rating diagnostic tests. Cancer 1950, 3, 32–35. [Google Scholar] [CrossRef] [PubMed]
- Granerod, J.; Ambrose, H.E.; Davies, N.W.; Clewley, J.P.; Walsh, A.L.; Morgan, D.; Cunningham, R.; Zuckerman, M.; Mutton, K.J.; Solomon, T.; et al. Causes of encephalitis and differences in their clinical presentations in England: A multicentre, population-based prospective study. Lancet Infect. Dis. 2010, 10, 835–844. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, P.G.E.; Quan, P.L.; Lipkin, W.I. Viral Encephalitis of Unknown Cause: Current Perspective and Recent Advances. Viruses 2017, 9, 138. [Google Scholar] [CrossRef]
| NIND | NID | AIND | NPL | p-Value | |
|---|---|---|---|---|---|
| n (female/male) | 208 (91/117) (43.8%/46.2%) | 273 (99/174) (36.3%/63.7%) | 147 (87/60) (59.2%/40.8%) | 49 (21/28) (42.3%/57.7%) | <0.001 ** |
| Age (years), median (range) | 54 (3–93) | 56 (14–91) | 45 (4–88) | 66 (34–86) | <0.001 * |
| Leucocyte count (/µL), median (range) | 1 (0–5) | 101 (6–480) | 7 (0–54) | 3 (0–31) | <0.001 * |
| Total protein (mg/L), median (range) | 491 (136–1470) | 957 (179–3268) | 555 (165–1670) | 874 (189–2610) | <0.001 * |
| QAlb (CSF/S), median (range) | 6.3 × 10−3 (1.9 × 10−3–14.7 × 10−3) | 12.5 × 10−3 (2.4 × 10−3–34.6 × 10−3) | 6.2 × 10−3 (2.5 × 10−3–16.2 × 10−3) | 9.3 × 10−3 (3.1 × 10−3–26.6 × 10−3) | <0.001 * |
| CSF-CXCL13 (pg/mL), median (range) | 7.8 (4–13) | 76 (4–1466) | 32 (4–224) | 43 (4–2120) | <0.001 * |
| CSF-specific oligoclonal IgG bands; n (+/−), (+) | 0/208 (0) | 117/156 (42.9%) | 116/31 (78.4%) | 4/45 (8.2%) | <0.001 ** |
| Intrathecal IgM synthesis; n (+/−), (+) | 0/208 (0) | 88/185 (32.2%) | 30/117 (20.3%) | 5/44 (10.2%) | <0.001 ** |
| Parameter | NIND | NID | AIND | NPL |
|---|---|---|---|---|
| n | 208 | 273 | 147 | 49 |
| Leucocyte count (/µL) | r = 0.045 | r = 0.132 | r = 0.560 | r = 0.655 |
| Lymphocyte count (/µL) | r = 0.158 | r = 0.139 | r = 0.495 | r = 0.748 |
| Monocyte count (/µL) | r = 0.120 | r = 0.066 | r = 0.163 | r = 0.358 |
| Plasma cell count (/µL) | - | r = 0.271 | r = 0.311 | - |
| QAlb (CSF/S) | r = 0.135 | r = 0.347 | r = 0.336 | r = 0.674 |
| Unit | Cut-Off | AUC | Youden’s Index | Sensitivity | Specificity |
|---|---|---|---|---|---|
| pg/mL | 428.92 | 0.98 | 0.88 | 92.1% | 96.5% |
| ng/g total protein | 164.15 | 0.86 | 0.74 | 85.2% | 88.4% |
| Neurological Disorder/Disease | Advantages | Limitations |
|---|---|---|
| Neuroborreliosis (LNB) |
|
|
| Neuroinfectious diseases (other than LNB) |
|
|
| MS/ON/CIS/NMOSD |
|
|
| Autoimmune (limbic) encephalitis/paraneoplastic syndrome |
| |
| Primary/secondary B-cell CNS lymphoma |
|
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Erhart, D.K.; Klose, V.; Schäper, T.; Tumani, H.; Senel, M. CXCL13 in Cerebrospinal Fluid: Clinical Value in a Large Cross-Sectional Study. Int. J. Mol. Sci. 2024, 25, 425. https://doi.org/10.3390/ijms25010425
Erhart DK, Klose V, Schäper T, Tumani H, Senel M. CXCL13 in Cerebrospinal Fluid: Clinical Value in a Large Cross-Sectional Study. International Journal of Molecular Sciences. 2024; 25(1):425. https://doi.org/10.3390/ijms25010425
Chicago/Turabian StyleErhart, Deborah Katharina, Veronika Klose, Tatjana Schäper, Hayrettin Tumani, and Makbule Senel. 2024. "CXCL13 in Cerebrospinal Fluid: Clinical Value in a Large Cross-Sectional Study" International Journal of Molecular Sciences 25, no. 1: 425. https://doi.org/10.3390/ijms25010425
APA StyleErhart, D. K., Klose, V., Schäper, T., Tumani, H., & Senel, M. (2024). CXCL13 in Cerebrospinal Fluid: Clinical Value in a Large Cross-Sectional Study. International Journal of Molecular Sciences, 25(1), 425. https://doi.org/10.3390/ijms25010425





