A Tumor and Immune-Related Micro-RNA Signature Predicts Relapse-Free Survival of Melanoma Patients Treated with Ipilimumab
Abstract
1. Introduction
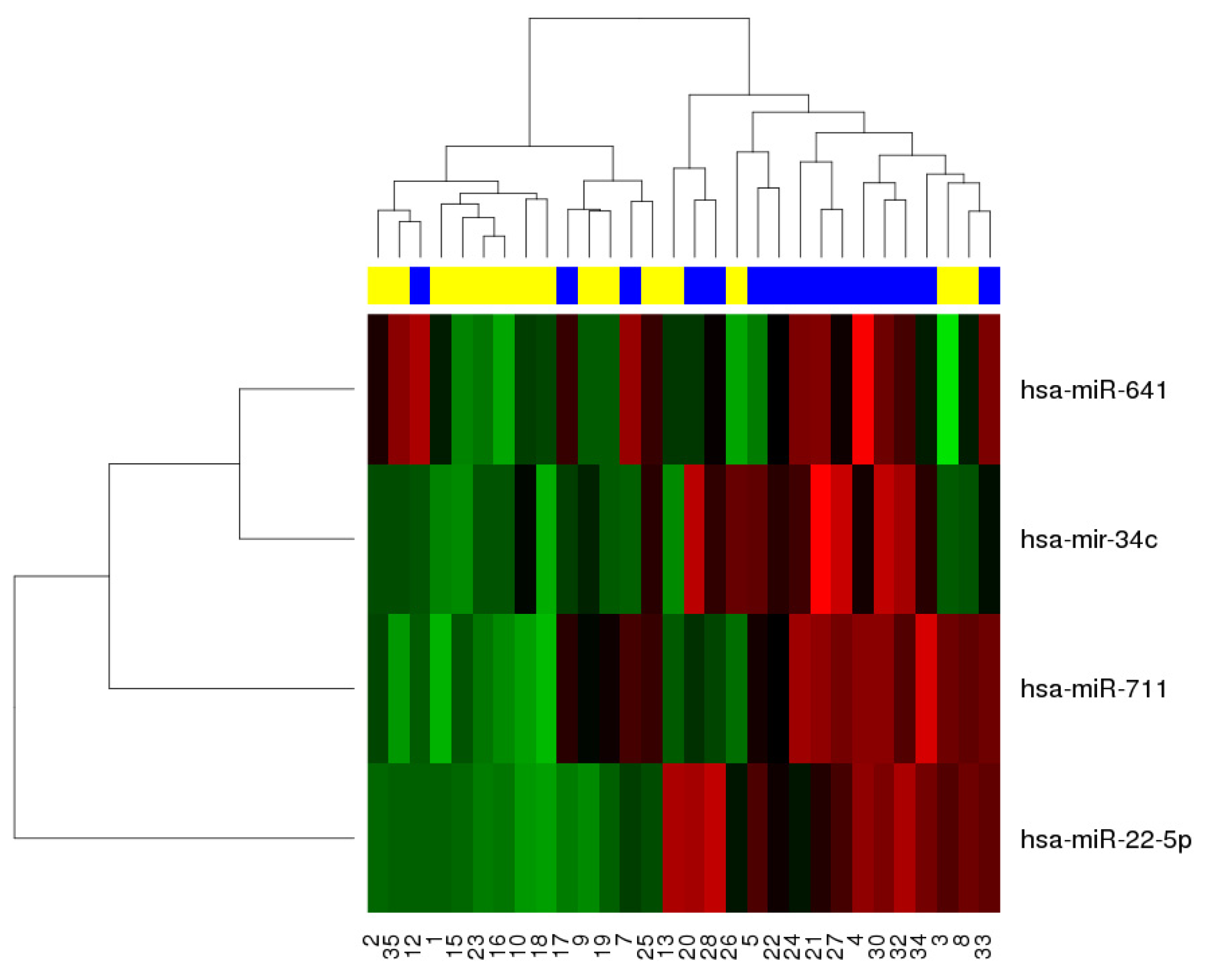
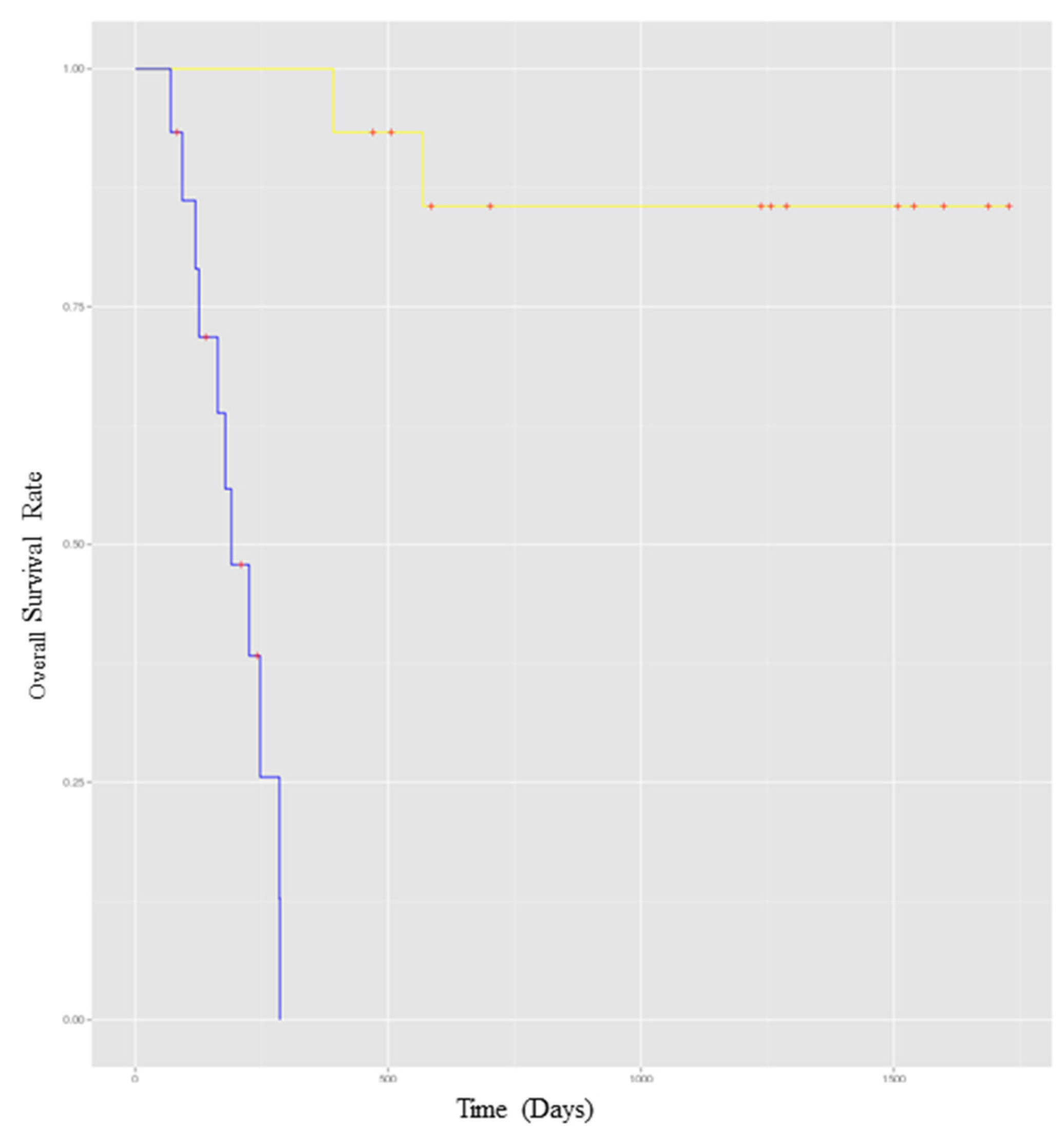
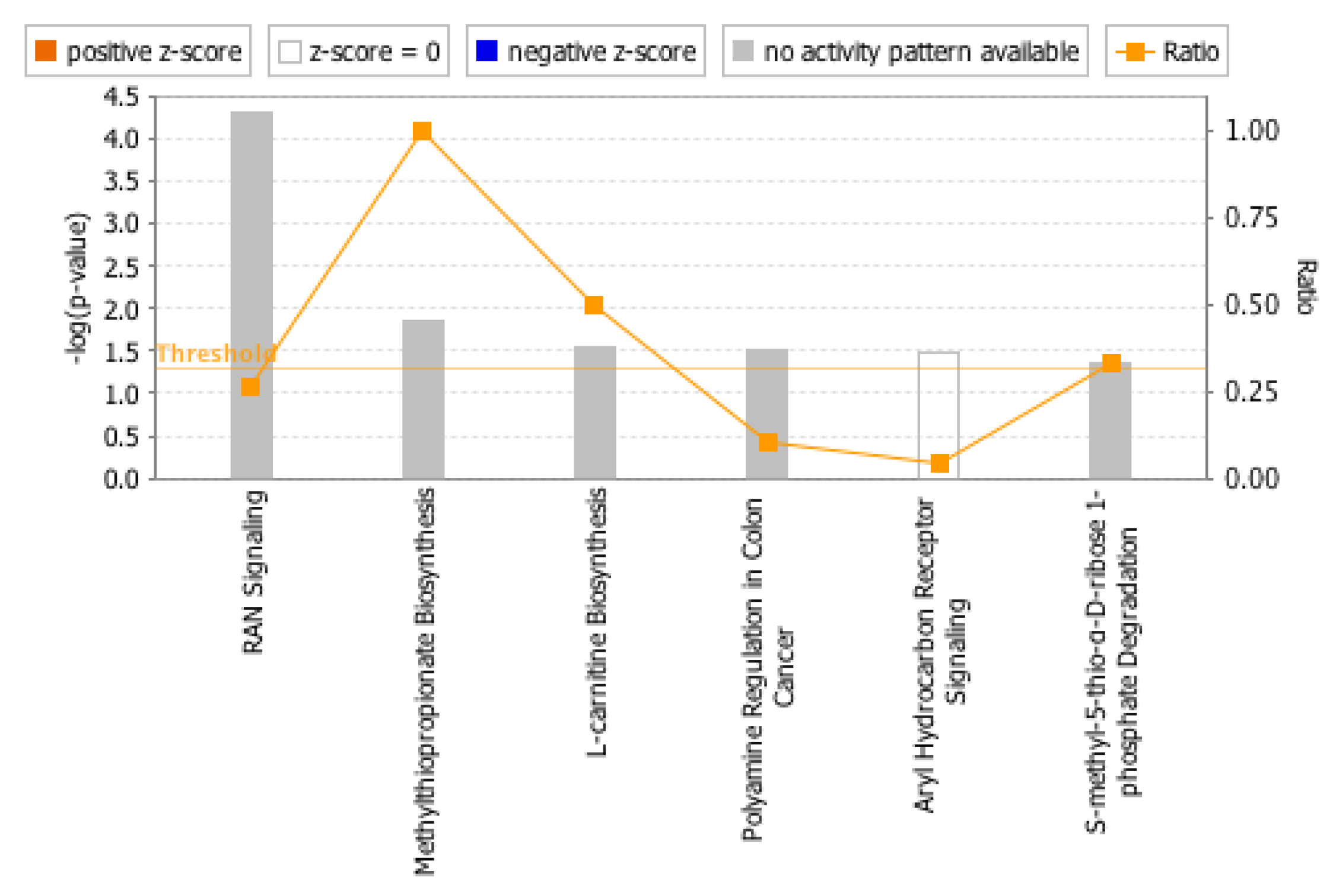
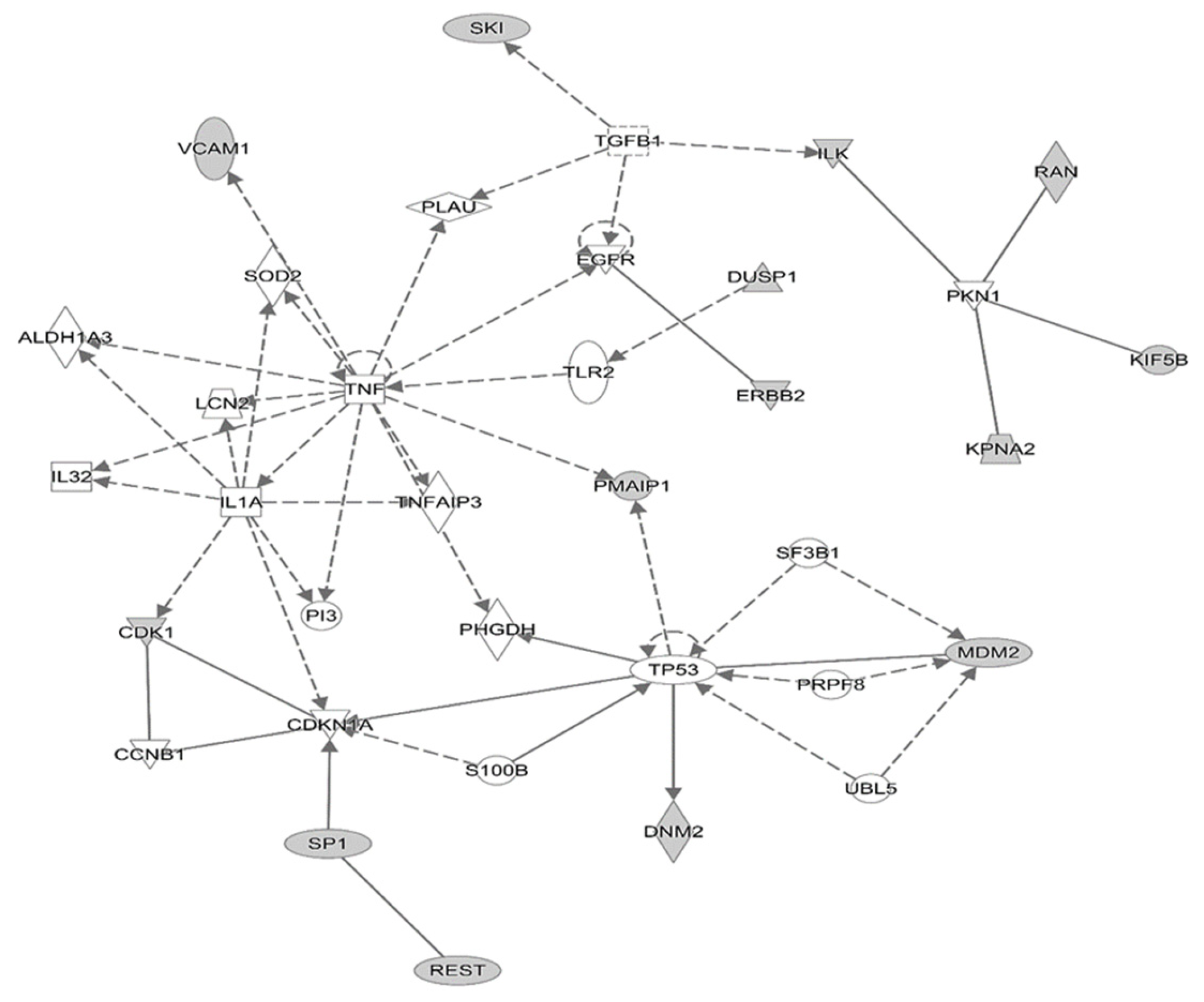
2. Results
3. Discussion
4. Materials and Methods
4.1. Patients
4.2. Laboratory Methods
4.3. Statistical Methods
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Siegel, R.L.; Miller, K.D.; Fuchs, H.E.; Jemal, A. Cancer statistics, 2022. CA Cancer J. Clin. 2022, 72, 7–33. [Google Scholar] [CrossRef]
- American Cancer Society. Cancer Facts & Figures 2023; American Cancer Society: Atlanta, GA, USA, 2023. [Google Scholar]
- Gershenwald, J.E.; Scolyer, R.A.; Hess, K.R.; Sondak, V.K.; Long, G.V.; Ross, M.I.; Lazar, A.J.; Faries, M.B.; Kirkwood, J.M.; McArthur, G.A.; et al. Melanoma staging: Evidence-based changes in the American Joint Committee on Cancer eighth edition cancer staging manual. CA Cancer J. Clin. 2017, 67, 472–492. [Google Scholar] [CrossRef]
- Romano, E.; Scordo, M.; Dusza, S.W.; Coit, D.G.; Chapman, P.B. Site and timing of first relapse in stage III melanoma patients: Implications for follow-up guidelines. J. Clin. Oncol. 2010, 28, 3042–3047. [Google Scholar] [CrossRef] [PubMed]
- Tarhini, A.A.; Lin, Y.; Lin, H.-M.; Vallabhaneni, P.; Sander, C.; LaFramboise, W.; Hamieh, L. Expression profiles of immune-related genes are associated with neoadjuvant ipilimumab clinical benefit. Oncoimmunology 2017, 6, e1231291. [Google Scholar] [CrossRef]
- Tarhini, A.A. The current state of adjuvant therapy of melanoma. Lancet Oncol. 2020, 21, 1394–1395. [Google Scholar] [CrossRef] [PubMed]
- YERVOY. (Ipilimumab) Injection, for Intravenous Use Initial U.S. Approval: 2011. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2020/125377s115lbl.pdf (accessed on 23 February 2023).
- Garg, M.; Couturier, D.L.; Nsengimana, J.; Fonseca, N.A.; Wongchenko, M.; Yan, Y.; Lauss, M.; Jonsson, G.B.; Bishop, J.; Parkinson, C.; et al. Tumour gene expression signature in primary melanoma predicts long-term outcomes. Nat. Commun. 2021, 12, 1137. [Google Scholar] [CrossRef]
- Bartel, D.P. Metazoan MicroRNAs. Cell 2018, 173, 20–51. [Google Scholar] [CrossRef]
- Kent, O.A.; Mendell, J.T. A small piece in the cancer puzzle: MicroRNAs as tumor suppressors and oncogenes. Oncogene 2006, 25, 6188–6196. [Google Scholar] [CrossRef]
- Raue, R.; Frank, A.C.; Syed, S.N.; Brune, B. Therapeutic Targeting of MicroRNAs in the Tumor Microenvironment. Int. J. Mol. Sci. 2021, 22, 2210. [Google Scholar] [CrossRef]
- Iacona, J.R.; Lutz, C.S. miR-146a-5p: Expression, regulation, and functions in cancer. Wiley Interdiscip. Rev. RNA 2019, 10, e1533. [Google Scholar] [CrossRef] [PubMed]
- Esquela-Kerscher, A.; Slack, F.J. Oncomirs-microRNAs with a role in cancer. Nat. Rev. Cancer 2006, 6, 259–269. [Google Scholar] [CrossRef]
- Segura, M.F.; Hanniford, D.; Menendez, S.; Reavie, L.; Zou, X.; Alvarez-Diaz, S.; Zakrewski, J.; Blochin, E.; Rose, A.; Bogunovic, D.; et al. Aberrant miR-182 expression promotes melanoma metastasis by repressing FOXO3 and microphthalmia-associated transcription factor. Proc. Natl. Acad. Sci. USA 2009, 106, 1814–1819. [Google Scholar] [CrossRef]
- Penna, E.; Orso, F.; Taverna, D. miR-214 as a key hub that controls cancer networks: Small player, multiple functions. J. Investig. Dermatol. 2015, 135, 960–969. [Google Scholar] [CrossRef] [PubMed]
- Latchana, N.; Ganju, A.; Howard, J.H.; Carson, W.E., 3rd. MicroRNA dysregulation in melanoma. Surg. Oncol. 2016, 25, 184–189. [Google Scholar] [CrossRef]
- Grignol, V.; Fairchild, E.T.; Zimmerer, J.M.; Lesinski, G.B.; Walker, M.J.; Magro, C.M.; Kacher, J.E.; Karpa, V.I.; Clark, J.; Nuovo, G.; et al. miR-21 and miR-155 are associated with mitotic activity and lesion depth of borderline melanocytic lesions. Br. J. Cancer 2011, 105, 1023–1029. [Google Scholar] [CrossRef] [PubMed]
- Galore-Haskel, G.; Nemlich, Y.; Greenberg, E.; Ashkenazi, S.; Hakim, M.; Itzhaki, O.; Shoshani, N.; Shapira, R.; Ben-Ami, E.; Ofek, E.; et al. A novel immune resistance mechanism of melanoma cells controlled by the ADAR1 enzyme. Oncotarget 2015, 6, 28999–29015. [Google Scholar] [CrossRef] [PubMed]
- Dong, L.; Tian, X.; Zhao, Y.; Tu, H.; Wong, A.; Yang, Y. The Roles of MiRNAs (MicroRNAs) in Melanoma Immunotherapy. Int. J. Mol. Sci. 2022, 23, 14775. [Google Scholar] [CrossRef]
- Edge, S.B.; American Joint Committee on Cancer; American Cancer Society. AJCC Cancer Staging Handbook: From the AJCC Cancer Staging Manual, 7th ed.; Springer: New York, NY, USA, 2010; pp. 19–718. [Google Scholar]
- Brahmer, J.R. Harnessing the immune system for the treatment of non-small-cell lung cancer. J. Clin. Oncol. 2013, 31, 1021–1028. [Google Scholar] [CrossRef]
- Flaherty, L.E.; Othus, M.; Atkins, M.B.; Tuthill, R.J.; Thompson, J.A.; Vetto, J.T.; Haluska, F.G.; Pappo, A.S.; Sosman, J.A. Southwest Oncology Group S0008: A phase III trial of high-dose interferon Alfa-2b versus cisplatin, vinblastine, and dacarbazine, plus interleukin-2 and interferon in patients with high-risk melanoma–An intergroup study of cancer and leukemia Group B, Children’s Oncology Group, Eastern Cooperative Oncology Group, and Southwest Oncology Group. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2014, 32, 3771–3778. [Google Scholar]
- Nguyen, M.T.; Luo, Y.H.; Li, A.L.; Tsai, J.C.; Wu, K.L.; Chung, P.J.; Ma, N. miRNA as a Modulator of Immunotherapy and Immune Response in Melanoma. Biomolecules 2021, 11, 1648. [Google Scholar] [CrossRef]
- Lu, J.; Wu, Z.; Peng, J.; Xu, S.; Zhou, L.; Lin, Y.; Wang, Y.; Yin, W.; Lu, J. Programmed death-ligand 1 single nucleotide polymorphism affects breast cancer chemosensitivity and adverse events in the neoadjuvant setting. Int. J. Biol. Mark. 2020, 35, 38–49. [Google Scholar]
- Wu, J.; Li, W.Z.; Huang, M.L.; Wei, H.L.; Wang, T.; Fan, J.; Li, N.-L.; Ling, R. Regulation of cancerous progression and epithelial-mesenchymal transition by miR-34c-3p via modulation of MAP3K2 signaling in triple-negative breast cancer cells. Biochem. Biophys. Res. Commun. 2017, 483, 10–16. [Google Scholar] [CrossRef]
- Xiao, C.Z.; Wei, W.; Guo, Z.X.; Zhang, M.Y.; Zhang, Y.F.; Wang, J.H.; Shi, M.; Wang, H.-Y.; Guo, R.-P. MicroRNA-34c-3p promotes cell proliferation and invasion in hepatocellular carcinoma by regulation of NCKAP1 expression. J. Cancer Res. Clin. Oncol. 2017, 143, 263–273. [Google Scholar] [CrossRef]
- Sousa, L.O.; Sobral, L.M.; Matsumoto, C.S.; Saggioro, F.P.; Lopez, R.V.; Panepucci, R.A.; Curti, C.; Silva, W.A.; Greene, L.J.; Leopoldino, A.M. Lymph node or perineural invasion is associated with low miR-15a, miR-34c and miR-199b levels in head and neck squamous cell carcinoma. BBA Clin. 2016, 6, 159–164. [Google Scholar] [CrossRef]
- Ralfkiaer, U.; Hagedorn, P.H.; Bangsgaard, N.; Løvendorf, M.B.; Ahler, C.B.; Svensson, L.; Kopp, K.L.; Vennegaard, M.T.; Lauenborg, B.; Zibert, J.R.; et al. Diagnostic microRNA profiling in cutaneous T-cell lymphoma (CTCL). Blood 2011, 118, 5891–5900. [Google Scholar] [CrossRef]
- Hu, J.Y.; Yi, W.; Zhang, M.Y.; Xu, R.; Zeng, L.S.; Long, X.R.; Zhou, X.-M.; Zheng, S.; Kang, Y.; Wang, H.-Y. MicroRNA-711 is a prognostic factor for poor overall survival and has an oncogenic role in breast cancer. Oncol. Lett. 2016, 11, 2155–2163. [Google Scholar] [CrossRef]
- Li, L.; Gao, J.; Li, J.; Wang, J. MiR-711 regulates gastric cancer progression by targeting CD44. Cancer Biomark. 2022, 35, 71–81. [Google Scholar] [CrossRef]
- Zhu, S.X.; Tong, X.Z.; Zhang, S. Expression of miR-711 and mechanism of proliferation and apoptosis in human gastric carcinoma. Oncol. Lett. 2017, 14, 4505–4510. [Google Scholar] [CrossRef] [PubMed]
- Mueller, D.W.; Rehli, M.; Bosserhoff, A.K. miRNA expression profiling in melanocytes and melanoma cell lines reveals miRNAs associated with formation and progression of malignant melanoma. J. Investig. Dermatol. 2009, 129, 1740–1751. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Y.; Liu, B.; Zhang, P.; Zhang, J.; Wang, L. LncRNA TUSC8 inhibits the invasion and migration of cervical cancer cells via miR-641/PTEN axis. Cell Biol. Int. 2019, 43, 781–788. [Google Scholar] [CrossRef]
- Kong, Q.; Shu, N.; Li, J.; Xu, N. miR-641 Functions as a Tumor Suppressor by Targeting MDM2 in Human Lung Cancer. Oncol. Res. 2018, 26, 735–741. [Google Scholar] [CrossRef] [PubMed]
- Tolcher, A.W.; Reeves, J.A.; McKean, M.; Chmielowski, B.; Beck, J.T.; Shaheen, M.F.; Somiah, N.; Wilson, M.; Spira, A.I.; Drabick, J.J.; et al. Preliminary results of a phase II study of alrizomadlin (APG-115), a novel, small-molecule MDM2 inhibitor, in combination with pembrolizumab in patients (pts) with unresectable or metastatic melanoma or advanced solid tumors that have failed immuno-oncologic (I-O) drugs. J. Clin. Oncol. 2021, 39 (Suppl. 15), 2506. [Google Scholar]
- Sand, M.; Skrygan, M.; Sand, D.; Georgas, D.; Gambichler, T.; Hahn, S.A.; Altmeyer, P.; Bechara, F.G. Comparative microarray analysis of microRNA expression profiles in primary cutaneous malignant melanoma, cutaneous malignant melanoma metastases, and benign melanocytic nevi. Cell Tissue Res. 2013, 351, 85–98. [Google Scholar] [CrossRef]
- Xu, M.; Li, J.; Wang, X.; Meng, S.; Shen, J.; Wang, S.; Xu, X.; Xie, B.; Liu, B.; Xie, L. MiR-22 suppresses epithelial–mesenchymal transition in bladder cancer by inhibiting Snail and MAPK1/Slug/vimentin feedback loop. Cell Death Dis. 2018, 9, 209. [Google Scholar] [CrossRef] [PubMed]
- Luo, L.J.; Zhang, L.P.; Duan, C.Y.; Wang, B.; He, N.N.; Abulimiti, P.; Lin, Y. The inhibition role of miR-22 in hepatocellular carcinoma cell migration and invasion via targeting CD147. Cancer Cell Int. 2017, 17, 17. [Google Scholar] [CrossRef]
- Shang, A.Q.X.Y.; Wang, J.; Sun, L.; Wei, J.; Lu, W.Y.; Lan, J.Y.; Wang, W.W.; Wang, L.; Wang, L.L. Predicative values of serum microRNA-22 and microRNA-126 levels for non-small cell lung cancer development and metastasis: A case-control study. Neoplasma 2017, 64, 4149. [Google Scholar] [CrossRef]
- Czarnecka, A.M.; Bartnik, E.; Fiedorowicz, M.; Rutkowski, P. Targeted Therapy in Melanoma and Mechanisms of Resistance. Int. J. Mol. Sci. 2020, 21, 4576. [Google Scholar] [CrossRef]
- Gottesdiener, L.S.; O’Connor, S.; Busam, K.J.; Won, H.; Solit, D.B.; Hyman, D.M.; Shoustari, A.N. Rates of ERBB2 Alterations across Melanoma Subtypes and a Complete Response to Trastuzumab Emtansine in an ERBB2-Amplified Acral Melanoma. Clin. Cancer Res. 2018, 24, 5815–5819. [Google Scholar] [CrossRef]
- Wagner, N.B.; Forschner, A.; Leiter, U.; Garbe, C.; Eigentler, T.K. S100B and LDH as early prognostic markers for response and overall survival in melanoma patients treated with anti-PD-1 or combined anti-PD-1 plus anti-CTLA-4 antibodies. Br. J. Cancer 2018, 119, 339–346. [Google Scholar] [CrossRef]
- Tarhini, A.A.; Stuckert, J.; Lee, S.; Sander, C.; Kirkwood, J.M. Prognostic significance of serum S100B protein in high-risk surgically resected melanoma patients participating in Intergroup Trial ECOG 1694. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2009, 27, 38–44. [Google Scholar] [CrossRef] [PubMed]
- Levati, L.; Pagani, E.; Romani, S.; Castiglia, D.; Piccinni, E.; Covaciu, C.; Caporaso, P.; Bondanza, S.; Antonetti, F.R.; Bonmassar, E.; et al. MicroRNA-155 targets the SKI gene in human melanoma cell lines. Pigment Cell Melanoma Res. 2011, 24, 538–550. [Google Scholar] [CrossRef] [PubMed]
- Guo, W.; Ma, J.; Guo, S.; Wang, H.; Wang, S.; Shi, Q.; Liu, L.; Zhao, T.; Yang, F.; Chen, S.; et al. A20 regulates the therapeutic effect of anti-PD-1 immunotherapy in melanoma. J. Immunother. Cancer 2020, 8, e001866. [Google Scholar] [CrossRef] [PubMed]
- Bertrand, F.; Montfort, A.; Marcheteau, E.; Imbert, C.; Gilhodes, J.; Filleron, T.; Rochaix, P.; Abadie, N.; Levade, T.; Meyer, N.; et al. TNFα blockade overcomes resistance to anti-PD-1 in experimental melanoma. Nat. Commun. 2017, 8, 2256. [Google Scholar] [CrossRef]
- Tarhini, A.A.; Edington, H.; Butterfield, L.H.; Lin, Y.; Shuai, Y.; Tawbi, H.; Sander, C.; Yin, Y.; Holtzman, M.; Johnson, J.; et al. Immune monitoring of the circulation and the tumor microenvironment in patients with regionally advanced melanoma receiving neoadjuvant ipilimumab. PLoS ONE 2014, 9, e87705. [Google Scholar] [CrossRef] [PubMed]
| Variable | Patients (N = 27) |
|---|---|
| Age, years; Median (range) | 53 (40–87) |
| Cutaneous primary, n (%) | 23 (85) |
| Mucosal primary, n (%) | 3 (11) |
| Unknown primary, n (%) | 1 (3) |
| Gender, n (%) | |
| Female | 9 (33) |
| Male | 18 (67) |
| Performance status (ECOG), n (%) | |
| 0 | 19 (70) |
| 1 | 8 (30) |
| Recurrent disease after prior surgery, n (%) | 21 (78) |
| Presence of in-transit metastases, n (%) | 15 (55) |
| Estimated risk stage, n (%) | |
| IIIB | 3 (11) |
| IIIC | 24 (89) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kobeissi, I.; Eljilany, I.; Achkar, T.; LaFramboise, W.A.; Santana-Santos, L.; Tarhini, A.A. A Tumor and Immune-Related Micro-RNA Signature Predicts Relapse-Free Survival of Melanoma Patients Treated with Ipilimumab. Int. J. Mol. Sci. 2023, 24, 8167. https://doi.org/10.3390/ijms24098167
Kobeissi I, Eljilany I, Achkar T, LaFramboise WA, Santana-Santos L, Tarhini AA. A Tumor and Immune-Related Micro-RNA Signature Predicts Relapse-Free Survival of Melanoma Patients Treated with Ipilimumab. International Journal of Molecular Sciences. 2023; 24(9):8167. https://doi.org/10.3390/ijms24098167
Chicago/Turabian StyleKobeissi, Iyad, Islam Eljilany, Tala Achkar, William A. LaFramboise, Lucas Santana-Santos, and Ahmad A. Tarhini. 2023. "A Tumor and Immune-Related Micro-RNA Signature Predicts Relapse-Free Survival of Melanoma Patients Treated with Ipilimumab" International Journal of Molecular Sciences 24, no. 9: 8167. https://doi.org/10.3390/ijms24098167
APA StyleKobeissi, I., Eljilany, I., Achkar, T., LaFramboise, W. A., Santana-Santos, L., & Tarhini, A. A. (2023). A Tumor and Immune-Related Micro-RNA Signature Predicts Relapse-Free Survival of Melanoma Patients Treated with Ipilimumab. International Journal of Molecular Sciences, 24(9), 8167. https://doi.org/10.3390/ijms24098167







