How Staphylococcus aureus and Pseudomonas aeruginosa Hijack the Host Immune Response in the Context of Cystic Fibrosis
Abstract
1. Introduction
2. Modulation of Physical Integrity of Airway Epithelium
3. Modulation of Immune Cell Proliferation and Death
4. Modulation of Cytokine Levels
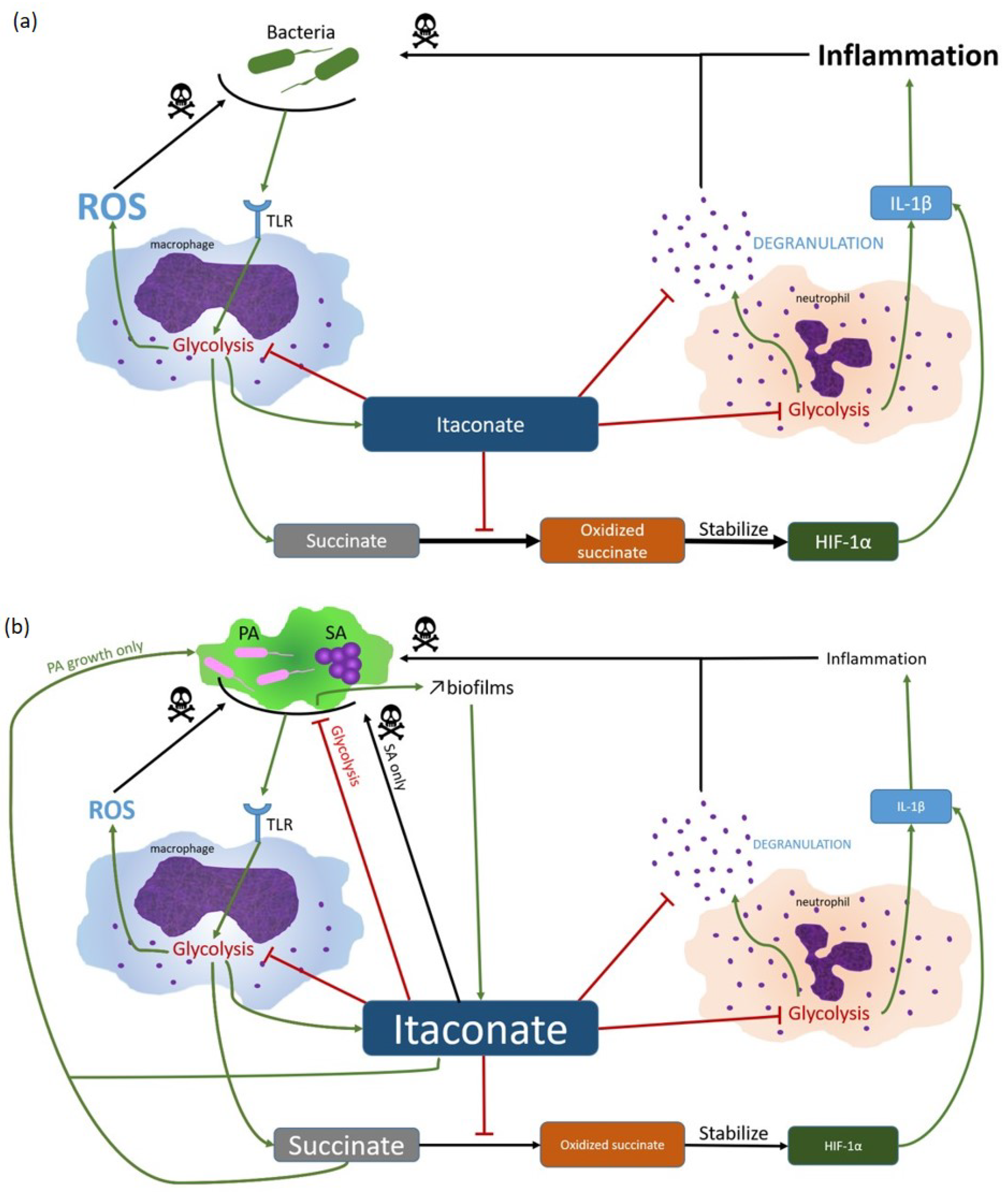
5. Modulation of Itaconate Immune Response
6. Modulation of Nutritional Immunity
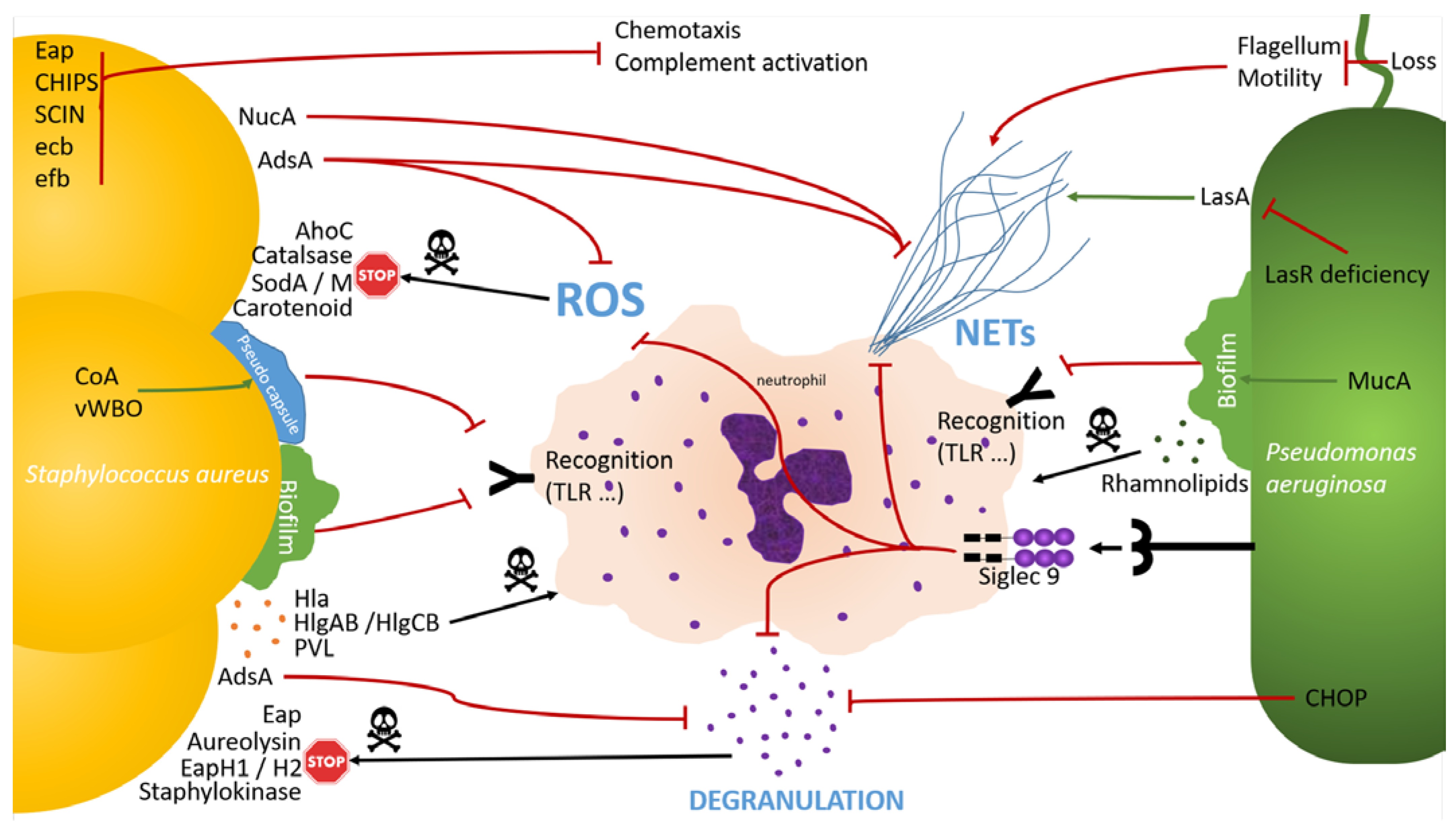
7. Evasion to Neutrophil Activities
7.1. Neutrophil Recognition Evasion
7.2. Degranulation Evasion
7.3. NETosis Evasion
8. Phagocytosis Evasion
9. How Host Immune Response Modulation Promotes SA-PA Coinfection
10. Future Directions
11. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cios, K.; Cohen, B.; Quittell, L.M.; Liu, J.; Larson, E.L. Impact of Colonizing Organism in the Respiratory Tract on the Incidence, Duration, and Time between Subsequent Hospitalizations among Patients with Cystic Fibrosis. Am. J. Infect. Control 2019, 47, 750–754. [Google Scholar] [CrossRef] [PubMed]
- Scotet, V.; L’Hostis, C.; Férec, C. The Changing Epidemiology of Cystic Fibrosis: Incidence, Survival and Impact of the CFTR Gene Discovery. Genes 2020, 11, 589. [Google Scholar] [CrossRef] [PubMed]
- Dehillotte, C.; Lemonnier, L. Registre français de la mucoviscidose—Bilan des données 2021 Vaincre la Mucoviscidose Paris. 2022. [Google Scholar]
- Cystic Fibrosis Foundation Patient Registry. 2021 Annual Data Report Bethesda, Maryland ©2022 Cystic Fibrosis Foundation. 2022. [Google Scholar]
- Cohen, T.S.; Prince, A. Cystic Fibrosis: A Mucosal Immunodeficiency Syndrome. Nat. Med. 2012, 18, 509–519. [Google Scholar] [CrossRef] [PubMed]
- Camus, L.; Briaud, P.; Bastien, S.; Elsen, S.; Doléans-Jordheim, A.; Vandenesch, F.; Moreau, K. Trophic Cooperation Promotes Bacterial Survival of Staphylococcus Aureus and Pseudomonas Aeruginosa. ISME J. 2020, 14, 3093–3105. [Google Scholar] [CrossRef]
- Briaud, P.; Bastien, S.; Camus, L.; Boyadjian, M.; Reix, P.; Mainguy, C.; Vandenesch, F.; Doléans-Jordheim, A.; Moreau, K. Impact of Coexistence Phenotype between Staphylococcus Aureus and Pseudomonas Aeruginosa Isolates on Clinical Outcomes Among Cystic Fibrosis Patients. Front. Cell. Infect. Microbiol. 2020, 10, 266. [Google Scholar] [CrossRef]
- Hubert, D.; Réglier-Poupet, H.; Sermet-Gaudelus, I.; Ferroni, A.; Le Bourgeois, M.; Burgel, P.-R.; Serreau, R.; Dusser, D.; Poyart, C.; Coste, J. Association between Staphylococcus Aureus Alone or Combined with Pseudomonas Aeruginosa and the Clinical Condition of Patients with Cystic Fibrosis. J. Cyst. Fibros. 2013, 12, 497–503. [Google Scholar] [CrossRef]
- Fischer, A.J.; Singh, S.B.; LaMarche, M.M.; Maakestad, L.J.; Kienenberger, Z.E.; Peña, T.A.; Stoltz, D.A.; Limoli, D.H. Sustained Coinfections with Staphylococcus Aureus and Pseudomonas Aeruginosa in Cystic Fibrosis. Am. J. Respir. Crit. Care Med. 2021, 203, 328–338. [Google Scholar] [CrossRef]
- Seilie, E.S.; Wardenburg, J.B. Staphylococcus Aureus Pore-Forming Toxins: The Interface of Pathogen and Host Complexity. Semin. Cell Dev. Biol. 2017, 72, 101–116. [Google Scholar] [CrossRef]
- Chavakis, T.; Hussain, M.; Kanse, S.M.; Peters, G.; Bretzel, R.G.; Flock, J.-I.; Herrmann, M.; Preissner, K.T. Staphylococcus Aureus Extracellular Adherence Protein Serves as Anti-Inflammatory Factor by Inhibiting the Recruitment of Host Leukocytes. Nat. Med. 2002, 8, 687–693. [Google Scholar] [CrossRef]
- de Haas, C.J.C.; Veldkamp, K.E.; Peschel, A.; Weerkamp, F.; Van Wamel, W.J.B.; Heezius, E.C.J.M.; Poppelier, M.J.J.G.; Van Kessel, K.P.M.; van Strijp, J.A.G. Chemotaxis Inhibitory Protein of Staphylococcus Aureus, a Bacterial Antiinflammatory Agent. J. Exp. Med. 2004, 199, 687–695. [Google Scholar] [CrossRef]
- Rooijakkers, S.H.M.; Ruyken, M.; Van Roon, J.; Van Kessel, K.P.M.; Van Strijp, J.A.G.; Van Wamel, W.J.B. Early Expression of SCIN and CHIPS Drives Instant Immune Evasion by Staphylococcus Aureus. Cell. Microbiol. 2006, 8, 1282–1293. [Google Scholar] [CrossRef] [PubMed]
- Rooijakkers, S.H.M.; Ruyken, M.; Roos, A.; Daha, M.R.; Presanis, J.S.; Sim, R.B.; van Wamel, W.J.B.; van Kessel, K.P.M.; van Strijp, J.A.G. Immune Evasion by a Staphylococcal Complement Inhibitor That Acts on C3 Convertases. Nat. Immunol. 2005, 6, 920–927. [Google Scholar] [CrossRef] [PubMed]
- Jongerius, I.; von Köckritz-Blickwede, M.; Horsburgh, M.J.; Ruyken, M.; Nizet, V.; Rooijakkers, S.H.M. Staphylococcus Aureus Virulence Is Enhanced by Secreted Factors That Block Innate Immune Defenses. J. Innate Immun. 2012, 4, 301–311. [Google Scholar] [CrossRef] [PubMed]
- Thammavongsa, V.; Kim, H.K.; Missiakas, D.; Schneewind, O. Staphylococcal Manipulation of Host Immune Responses. Nat. Rev. Microbiol. 2015, 13, 529–543. [Google Scholar] [CrossRef]
- Chekabab, S.M.; Silverman, R.J.; Lafayette, S.L.; Luo, Y.; Rousseau, S.; Nguyen, D. Staphylococcus Aureus Inhibits IL-8 Responses Induced by Pseudomonas Aeruginosa in Airway Epithelial Cells. PLoS ONE 2015, 10, e0137753. [Google Scholar] [CrossRef]
- Tajima, A.; Iwase, T.; Shinji, H.; Seki, K.; Mizunoe, Y. Inhibition of Endothelial Interleukin-8 Production and Neutrophil Transmigration by Staphylococcus Aureus Beta-Hemolysin. Infect. Immun. 2009, 77, 327–334. [Google Scholar] [CrossRef]
- Zurek, O.W.; Pallister, K.B.; Voyich, J.M. Staphylococcus Aureus Inhibits Neutrophil-Derived IL-8 to Promote Cell Death. J. Infect. Dis. 2015, 212, 934–938. [Google Scholar] [CrossRef]
- Guggenberger, C.; Wolz, C.; Morrissey, J.A.; Heesemann, J. Two Distinct Coagulase-Dependent Barriers Protect Staphylococcus Aureus from Neutrophils in a Three Dimensional in Vitro Infection Model. PLoS Pathog. 2012, 8, e1002434. [Google Scholar] [CrossRef]
- Parker, D.; Ahn, D.; Cohen, T.; Prince, A. Innate Immune Signaling Activated by MDR Bacteria in the Airway. Physiol. Rev. 2016, 96, 19–53. [Google Scholar] [CrossRef]
- Thammavongsa, V.; Kern, J.W.; Missiakas, D.M.; Schneewind, O. Staphylococcus Aureus Synthesizes Adenosine to Escape Host Immune Responses. J. Exp. Med. 2009, 206, 2417–2427. [Google Scholar] [CrossRef]
- Stapels, D.A.C.; Ramyar, K.X.; Bischoff, M.; von Köckritz-Blickwede, M.; Milder, F.J.; Ruyken, M.; Eisenbeis, J.; McWhorter, W.J.; Herrmann, M.; van Kessel, K.P.M.; et al. Staphylococcus Aureus Secretes a Unique Class of Neutrophil Serine Protease Inhibitors. Proc. Natl. Acad. Sci. USA 2014, 111, 13187–13192. [Google Scholar] [CrossRef] [PubMed]
- Sieprawska-Lupa, M.; Mydel, P.; Krawczyk, K.; Wójcik, K.; Puklo, M.; Lupa, B.; Suder, P.; Silberring, J.; Reed, M.; Pohl, J.; et al. Degradation of Human Antimicrobial Peptide LL-37 by Staphylococcus Aureus-Derived Proteinases. Antimicrob. Agents Chemother. 2004, 48, 4673–4679. [Google Scholar] [CrossRef] [PubMed]
- Jin, T.; Bokarewa, M.; Foster, T.; Mitchell, J.; Higgins, J.; Tarkowski, A. Staphylococcus Aureus Resists Human Defensins by Production of Staphylokinase, a Novel Bacterial Evasion Mechanism. J. Immunol. 2004, 172, 1169–1176. [Google Scholar] [CrossRef] [PubMed]
- Garcia, Y.M.; Barwinska-Sendra, A.; Tarrant, E.; Skaar, E.P.; Waldron, K.J.; Kehl-Fie, T.E. A Superoxide Dismutase Capable of Functioning with Iron or Manganese Promotes the Resistance of Staphylococcus Aureus to Calprotectin and Nutritional Immunity. PLoS Pathog. 2017, 13, e1006125. [Google Scholar] [CrossRef]
- Treffon, J.; Block, D.; Moche, M.; Reiss, S.; Fuchs, S.; Engelmann, S.; Becher, D.; Langhanki, L.; Mellmann, A.; Peters, G.; et al. Adaptation of Staphylococcus Aureus to Airway Environments in Patients with Cystic Fibrosis by Upregulation of Superoxide Dismutase M and Iron-Scavenging Proteins. J. Infect. Dis. 2018, 217, 1453–1461. [Google Scholar] [CrossRef] [PubMed]
- Treffon, J.; Chaves-Moreno, D.; Niemann, S.; Pieper, D.H.; Vogl, T.; Roth, J.; Kahl, B.C. Importance of Superoxide Dismutases A and M for Protection of Staphylococcus Aureus in the Oxidative Stressful Environment of Cystic Fibrosis Airways. Cell. Microbiol. 2020, 22, e13158. [Google Scholar] [CrossRef] [PubMed]
- Liu, G.Y.; Essex, A.; Buchanan, J.T.; Datta, V.; Hoffman, H.M.; Bastian, J.F.; Fierer, J.; Nizet, V. Staphylococcus Aureus Golden Pigment Impairs Neutrophil Killing and Promotes Virulence through Its Antioxidant Activity. J. Exp. Med. 2005, 202, 209–215. [Google Scholar] [CrossRef]
- Cosgrove, K.; Coutts, G.; Jonsson, I.-M.; Tarkowski, A.; Kokai-Kun, J.F.; Mond, J.J.; Foster, S.J. Catalase (KatA) and Alkyl Hydroperoxide Reductase (AhpC) Have Compensatory Roles in Peroxide Stress Resistance and Are Required for Survival, Persistence, and Nasal Colonization in Staphylococcus Aureus. J. Bacteriol. 2007, 189, 1025–1035. [Google Scholar] [CrossRef]
- Thammavongsa, V.; Missiakas, D.M.; Schneewind, O. Staphylococcus Aureus Degrades Neutrophil Extracellular Traps to Promote Immune Cell Death. Science 2013, 342, 863–866. [Google Scholar] [CrossRef]
- Herzog, S.; Dach, F.; de Buhr, N.; Niemann, S.; Schlagowski, J.; Chaves-Moreno, D.; Neumann, C.; Goretzko, J.; Schwierzeck, V.; Mellmann, A.; et al. High Nuclease Activity of Long Persisting Staphylococcus Aureus Isolates within the Airways of Cystic Fibrosis Patients Protects against NET-Mediated Killing. Front. Immunol. 2019, 10, 2552. [Google Scholar] [CrossRef]
- Berends, E.T.M.; Horswill, A.R.; Haste, N.M.; Monestier, M.; Nizet, V.; von Köckritz-Blickwede, M. Nuclease Expression by Staphylococcus Aureus Facilitates Escape from Neutrophil Extracellular Traps. J. Innate Immun. 2010, 2, 576–586. [Google Scholar] [CrossRef] [PubMed]
- Pernet, E.; Guillemot, L.; Burgel, P.-R.; Martin, C.; Lambeau, G.; Sermet-Gaudelus, I.; Sands, D.; Leduc, D.; Morand, P.C.; Jeammet, L.; et al. Pseudomonas Aeruginosa Eradicates Staphylococcus Aureus by Manipulating the Host Immunity. Nat. Commun. 2014, 5, 5105. [Google Scholar] [CrossRef] [PubMed]
- Pernet, E.; Brunet, J.; Guillemot, L.; Chignard, M.; Touqui, L.; Wu, Y. Staphylococcus Aureus Adenosine Inhibits SPLA2-IIA–Mediated Host Killing in the Airways. J. Immunol. 2015, 194, 5312–5319. [Google Scholar] [CrossRef] [PubMed]
- Falugi, F.; Kim, H.K.; Missiakas, D.M.; Schneewind, O. Role of Protein A in the Evasion of Host Adaptive Immune Responses by Staphylococcus Aureus. mBio 2013, 4, e00575-13. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.K.; Thammavongsa, V.; Schneewind, O.; Missiakas, D. Recurrent Infections and Immune Evasion Strategies of Staphylococcus Aureus. Curr. Opin. Microbiol. 2012, 15, 92–99. [Google Scholar] [CrossRef]
- Foster, T.J. Immune Evasion by Staphylococci. Nat. Rev. Microbiol. 2005, 3, 948–958. [Google Scholar] [CrossRef] [PubMed]
- Winstel, V.; Schneewind, O.; Missiakas, D. Staphylococcus Aureus Exploits the Host Apoptotic Pathway to Persist during Infection. mBio 2019, 10, e02270-19. [Google Scholar] [CrossRef]
- Riquelme, S.A.; Liimatta, K.; Lung, T.W.F.; Fields, B.; Ahn, D.; Chen, D.; Lozano, C.; Sáenz, Y.; Uhlemann, A.-C.; Kahl, B.C.; et al. Pseudomonas Aeruginosa Utilizes Host-Derived Itaconate to Redirect Its Metabolism to Promote Biofilm Formation. Cell Metab. 2020, 31, 1091–1106.e6. [Google Scholar] [CrossRef]
- Tomlinson, K.L.; Lung, T.W.F.; Dach, F.; Annavajhala, M.K.; Gabryszewski, S.J.; Groves, R.A.; Drikic, M.; Francoeur, N.J.; Sridhar, S.H.; Smith, M.L.; et al. Staphylococcus Aureus Induces an Itaconate-Dominated Immunometabolic Response That Drives Biofilm Formation. Nat. Commun. 2021, 12, 1399. [Google Scholar] [CrossRef]
- Grim, K.P.; San Francisco, B.; Radin, J.N.; Brazel, E.B.; Kelliher, J.L.; Párraga Solórzano, P.K.; Kim, P.C.; McDevitt, C.A.; Kehl-Fie, T.E. The Metallophore Staphylopine Enables Staphylococcus Aureus to Compete with the Host for Zinc and Overcome Nutritional Immunity. mBio 2017, 8, e01281-17. [Google Scholar] [CrossRef]
- Skaar, E.P.; Humayun, M.; Bae, T.; DeBord, K.L.; Schneewind, O. Iron-Source Preference of Staphylococcus Aureus Infections. Science 2004, 305, 1626–1628. [Google Scholar] [CrossRef] [PubMed]
- Radin, J.N.; Kelliher, J.L.; Solórzano, P.K.P.; Kehl-Fie, T.E. The Two-Component System ArlRS and Alterations in Metabolism Enable Staphylococcus Aureus to Resist Calprotectin-Induced Manganese Starvation. PLoS Pathog. 2016, 12, e1006040. [Google Scholar] [CrossRef] [PubMed]
- Stanton, B.A. Effects of Pseudomonas Aeruginosa on CFTR Chloride Secretion and the Host Immune Response. Am. J. Physiol.-Cell Physiol. 2017, 312, C357–C366. [Google Scholar] [CrossRef] [PubMed]
- Schwarzer, C.; Ravishankar, B.; Patanwala, M.; Shuai, S.; Fu, Z.; Illek, B.; Fischer, H.; Machen, T.E. Thapsigargin Blocks Pseudomonas Aeruginosa Homoserine Lactone-Induced Apoptosis in Airway Epithelia. Am. J. Physiol.-Cell Physiol. 2014, 306, C844–C855. [Google Scholar] [CrossRef]
- Hauser, A.R. The Type III Secretion System of Pseudomonas Aeruginosa: Infection by Injection. Nat. Rev. Microbiol. 2009, 7, 654–665. [Google Scholar] [CrossRef]
- Hooi, D.S.W.; Bycroft, B.W.; Chhabra, S.R.; Williams, P.; Pritchard, D.I. Differential Immune Modulatory Activity of Pseudomonas Aeruginosa Quorum-Sensing Signal Molecules. Infect Immun. 2004, 72, 8. [Google Scholar] [CrossRef]
- Li, H.; Wang, L.; Ye, L.; Mao, Y.; Xie, X.; Xia, C.; Chen, J.; Lu, Z.; Song, J. Influence of Pseudomonas Aeruginosa Quorum Sensing Signal Molecule N-(3-Oxododecanoyl) Homoserine Lactone on Mast Cells. Med. Microbiol. Immunol. 2009, 198, 113–121. [Google Scholar] [CrossRef]
- Kim, K.; Kim, Y.U.; Koh, B.H.; Hwang, S.S.; Kim, S.-H.; Lépine, F.; Cho, Y.-H.; Lee, G.R. HHQ and PQS, Two Pseudomonas Aeruginosa Quorum-Sensing Molecules, down-Regulate the Innate Immune Responses through the Nuclear Factor-ΚB Pathway. Immunology 2010, 129, 578–588. [Google Scholar] [CrossRef]
- LaFayette, S.L.; Houle, D.; Beaudoin, T.; Wojewodka, G.; Radzioch, D.; Hoffman, L.R.; Burns, J.L.; Dandekar, A.A.; Smalley, N.E.; Chandler, J.R.; et al. Cystic Fibrosis–Adapted Pseudomonas Aeruginosa Quorum Sensing LasR Mutants Cause Hyperinflammatory Responses. Sci. Adv. 2015, 1, e1500199. [Google Scholar] [CrossRef]
- Koeppen, K.; Hampton, T.H.; Jarek, M.; Scharfe, M.; Gerber, S.A.; Mielcarz, D.W.; Demers, E.G.; Dolben, E.L.; Hammond, J.H.; Hogan, D.A.; et al. A Novel Mechanism of Host-Pathogen Interaction through SRNA in Bacterial Outer Membrane Vesicles. PLoS Pathog. 2016, 12, e1005672. [Google Scholar] [CrossRef]
- Glucksam-Galnoy, Y.; Sananes, R.; Silberstein, N.; Krief, P.; Kravchenko, V.V.; Meijler, M.M.; Zor, T. The Bacterial Quorum-Sensing Signal Molecule N -3-Oxo-Dodecanoyl-l-Homoserine Lactone Reciprocally Modulates Pro- and Anti-Inflammatory Cytokines in Activated Macrophages. J. Immunol. 2013, 191, 337–344. [Google Scholar] [CrossRef] [PubMed]
- Bortolotti, D.; LeMaoult, J.; Trapella, C.; Di Luca, D.; Carosella, E.D.; Rizzo, R. Pseudomonas Aeruginosa Quorum Sensing Molecule N-(3-Oxododecanoyl)-l-Homoserine-Lactone Induces HLA-G Expression in Human Immune Cells. Infect. Immun. 2015, 83, 3918–3925. [Google Scholar] [CrossRef] [PubMed]
- Skindersoe, M.E.; Zeuthen, L.H.; Brix, S.; Fink, L.N.; Lazenby, J.; Whittall, C.; Williams, P.; Diggle, S.P.; Froekiaer, H.; Cooley, M.; et al. Pseudomonas Aeruginosa Quorum-Sensing Signal Molecules Interfere with Dendritic Cell-Induced T-Cell Proliferation. FEMS Immunol. Med. Microbiol. 2009, 55, 335–345. [Google Scholar] [CrossRef] [PubMed]
- Telford, G.; Wheeler, D.; Williams, P.; Tomkins, P.T.; Appleby, P.; Sewell, H.; Stewart, G.S.A.B.; Bycroft, B.W.; Pritchard, D.I. The Pseudomonas Aeruginosa Quorum-Sensing Signal Molecule N-(3-Oxododecanoyl)-l-Homoserine Lactone Has Immunomodulatory Activity. Infect. Immun. 1998, 66, 36–42. [Google Scholar] [CrossRef] [PubMed]
- Pedersen, S.S.; Kharazmi, A.; Espersen, F.; Høiby, N. Pseudomonas Aeruginosa Alginate in Cystic Fibrosis Sputum and the Inflammatory Response. Infect. Immun. 1990, 58, 3363–3368. [Google Scholar] [CrossRef] [PubMed]
- Skopelja, S.; Hamilton, B.J.; Jones, J.D.; Yang, M.-L.; Mamula, M.; Ashare, A.; Gifford, A.H.; Rigby, W.F.C. The Role for Neutrophil Extracellular Traps in Cystic Fibrosis Autoimmunity. JCI Insight 2016, 1, e88912. [Google Scholar] [CrossRef]
- Khatua, B.; Bhattacharya, K.; Mandal, C. Sialoglycoproteins Adsorbed by Pseudomonas Aeruginosa Facilitate Their Survival by Impeding Neutrophil Extracellular Trap through Siglec-9. J. Leukoc. Biol. 2012, 91, 641–655. [Google Scholar] [CrossRef]
- Floyd, M.; Winn, M.; Cullen, C.; Sil, P.; Chassaing, B.; Yoo, D.; Gewirtz, A.T.; Goldberg, J.B.; McCarter, L.L.; Rada, B. Swimming Motility Mediates the Formation of Neutrophil Extracellular Traps Induced by Flagellated Pseudomonas Aeruginosa. PLoS Pathog. 2016, 12, e1005987. [Google Scholar] [CrossRef]
- Skopelja-Gardner, S.; Theprungsirikul, J.; Lewis, K.A.; Hammond, J.H.; Carlson, K.M.; Hazlett, H.F.; Nymon, A.; Nguyen, D.; Berwin, B.L.; Hogan, D.A.; et al. Regulation of Pseudomonas Aeruginosa-Mediated Neutrophil Extracellular Traps. Front. Immunol. 2019, 10, 1670. [Google Scholar] [CrossRef]
- Lovewell, R.R.; Collins, R.M.; Acker, J.L.; O’Toole, G.A.; Wargo, M.J.; Berwin, B. Step-Wise Loss of Bacterial Flagellar Torsion Confers Progressive Phagocytic Evasion. PLoS Pathog. 2011, 7, e1002253. [Google Scholar] [CrossRef]
- Mariencheck, W.I.; Alcorn, J.F.; Palmer, S.M.; Wright, J.R. Pseudomonas Aeruginosa Elastase Degrades Surfactant Proteins A and D. Am. J. Respir. Cell Mol. Biol. 2003, 28, 528–537. [Google Scholar] [CrossRef]
- Kuang, Z.; Hao, Y.; Walling, B.E.; Jeffries, J.L.; Ohman, D.E.; Lau, G.W. Pseudomonas Aeruginosa Elastase Provides an Escape from Phagocytosis by Degrading the Pulmonary Surfactant Protein-A. PLoS ONE 2011, 6, e27091. [Google Scholar] [CrossRef]
- Alcorn, J.F.; Wright, J.R. Degradation of Pulmonary Surfactant Protein D by Pseudomonas Aeruginosa Elastase Abrogates Innate Immune Function. J. Biol. Chem. 2004, 279, 30871–30879. [Google Scholar] [CrossRef] [PubMed]
- Moraes, T.J.; Martin, R.; Plumb, J.D.; Vachon, E.; Cameron, C.M.; Danesh, A.; Kelvin, D.J.; Ruf, W.; Downey, G.P. Role of PAR2 in Murine Pulmonary Pseudomonal Infection. Am. J. Physiol.-Lung Cell. Mol. Physiol. 2008, 294, L368–L377. [Google Scholar] [CrossRef] [PubMed]
- Jensen, P.Ø.; Bjarnsholt, T.; Phipps, R.; Rasmussen, T.B.; Calum, H.; Christoffersen, L.; Moser, C.; Williams, P.; Pressler, T.; Givskov, M.; et al. Rapid Necrotic Killing of Polymorphonuclear Leukocytes Is Caused by Quorum-Sensing-Controlled Production of Rhamnolipid by Pseudomonas Aeruginosa. Microbiology 2007, 153, 1329–1338. [Google Scholar] [CrossRef]
- Usher, L.R.; Lawson, R.A.; Geary, I.; Taylor, C.J.; Bingle, C.D.; Taylor, G.W.; Whyte, M.K.B. Induction of Neutrophil Apoptosis by the Pseudomonas Aeruginosa Exotoxin Pyocyanin: A Potential Mechanism of Persistent Infection. J. Immunol. 2002, 168, 1861–1868. [Google Scholar] [CrossRef]
- Reinhart, A.A.; Oglesby-Sherrouse, A.G. Regulation of Pseudomonas Aeruginosa Virulence by Distinct Iron Sources. Genes 2016, 7, 126. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, A.T.; O’Neill, M.J.; Watts, A.M.; Robson, C.L.; Lamont, I.L.; Wilks, A.; Oglesby-Sherrouse, A.G. Adaptation of Iron Homeostasis Pathways by a Pseudomonas Aeruginosa Pyoverdine Mutant in the Cystic Fibrosis Lung. J. Bacteriol. 2014, 196, 2265–2276. [Google Scholar] [CrossRef] [PubMed]
- Avendaño-Ortiz, J.; Llanos-González, E.; Toledano, V.; del Campo, R.; Cubillos-Zapata, C.; Lozano-Rodríguez, R.; Ismail, A.; Prados, C.; Gómez-Campelo, P.; Aguirre, L.A.; et al. Pseudomonas Aeruginosa Colonization Causes PD-L1 Overexpression on Monocytes, Impairing the Adaptive Immune Response in Patients with Cystic Fibrosis. J. Cyst. Fibros. 2019, 18, 630–635. [Google Scholar] [CrossRef]
- Sun, J.; LaRock, D.L.; Skowronski, E.A.; Kimmey, J.M.; Olson, J.; Jiang, Z.; O’Donoghue, A.J.; Nizet, V.; LaRock, C.N. The Pseudomonas Aeruginosa Protease LasB Directly Activates IL-1β. EBioMedicine 2020, 60, 102984. [Google Scholar] [CrossRef]
- Mayer, M.L.; Sheridan, J.A.; Blohmke, C.J.; Turvey, S.E.; Hancock, R.E.W. The Pseudomonas Aeruginosa Autoinducer 3O-C12 Homoserine Lactone Provokes Hyperinflammatory Responses from Cystic Fibrosis Airway Epithelial Cells. PLoS ONE 2011, 6, e16246. [Google Scholar] [CrossRef] [PubMed]
- Shiner, E.K.; Terentyev, D.; Bryan, A.; Sennoune, S.; Martinez-Zaguilan, R.; Li, G.; Gyorke, S.; Williams, S.C.; Rumbaugh, K.P. Pseudomonas Aeruginosa Autoinducer Modulates Host Cell Responses through Calcium Signalling. Cell. Microbiol. 2006, 8, 1601–1610. [Google Scholar] [CrossRef] [PubMed]
- Smith, R.S.; Fedyk, E.R.; Springer, T.A.; Mukaida, N.; Iglewski, B.H.; Phipps, R.P. IL-8 Production in Human Lung Fibroblasts and Epithelial Cells Activated by the Pseudomonas Autoinducer N-3-Oxododecanoyl Homoserine Lactone Is Transcriptionally Regulated by NF-ΚB and Activator Protein-2. J. Immunol. 2001, 167, 366–374. [Google Scholar] [CrossRef] [PubMed]
- Gambello, M.J.; Kaye, S.; Iglewski, B.H. LasR of Pseudomonas Aeruginosa Is a Transcriptional Activator of the Alkaline Protease Gene (Apr) and an Enhancer of Exotoxin a Expression. Infect. Immun. 1993, 61, 1180–1184. [Google Scholar] [CrossRef]
- Férec, C. La mucoviscidose: Du gène à la thérapeutique. Médecine/Sciences 2021, 37, 618–624. [Google Scholar] [CrossRef] [PubMed]
- Welsh, M.J.; Smith, A.E. Molecular Mechanisms of CFTR Chloride Channel Dysfunction in Cystic Fibrosis. Cell 1993, 73, 1251–1254. [Google Scholar] [CrossRef]
- Zheng, M.; Sun, S.; Zhou, J.; Liu, M. Virulence Factors Impair Epithelial Junctions during Bacterial Infection. J. Clin. Lab. Anal. 2021, 35, e23627. [Google Scholar] [CrossRef]
- Crabbé, A.; Sarker, S.F.; Van Houdt, R.; Ott, C.M.; Leys, N.; Cornelis, P.; Nickerson, C.A. Alveolar Epithelium Protects Macrophages from Quorum Sensing-Induced Cytotoxicity in a Three-Dimensional Co-Culture Model. Cell. Microbiol. 2011, 13, 469–481. [Google Scholar] [CrossRef]
- Yamada, K.J.; Kielian, T. Biofilm-Leukocyte Cross-Talk: Impact on Immune Polarization and Immunometabolism. J. Innate Immun. 2019, 11, 280–288. [Google Scholar] [CrossRef]
- Alhede, M.; Bjarnsholt, T.; Jensen, P.O.; Phipps, R.K.; Moser, C.; Christophersen, L.; Christensen, L.D.; van Gennip, M.; Parsek, M.; Hoiby, N.; et al. Pseudomonas Aeruginosa Recognizes and Responds Aggressively to the Presence of Polymorphonuclear Leukocytes. Microbiology 2009, 155, 3500–3508. [Google Scholar] [CrossRef]
- Alhede, M.; Bjarnsholt, T.; Givskov, M.; Alhede, M. Pseudomonas Aeruginosa Biofilms. In Advances in Applied Microbiology; Elsevier: Amsterdam, The Netherlands, 2014; Volume 86, pp. 1–40. ISBN 978-0-12-800262-9. [Google Scholar]
- Walker, T.S.; Tomlin, K.L.; Worthen, G.S.; Poch, K.R.; Lieber, J.G.; Saavedra, M.T.; Fessler, M.B.; Malcolm, K.C.; Vasil, M.L.; Nick, J.A. Enhanced Pseudomonas Aeruginosa Biofilm Development Mediated by Human Neutrophils. Infect. Immun. 2005, 73, 3693–3701. [Google Scholar] [CrossRef] [PubMed]
- Scherr, T.D.; Hanke, M.L.; Huang, O.; James, D.B.A.; Horswill, A.R.; Bayles, K.W.; Fey, P.D.; Torres, V.J.; Kielian, T. Staphylococcus Aureus Biofilms Induce Macrophage Dysfunction Through Leukocidin AB and Alpha-Toxin. mBio 2015, 6, e01021-15. [Google Scholar] [CrossRef] [PubMed]
- Bedi, B.; Lin, K.-C.; Maurice, N.M.; Yuan, Z.; Bijli, K.; Koval, M.; Hart, C.M.; Goldberg, J.B.; Stecenko, A.; Sadikot, R.T. UPR Modulation of Host Immunity by Pseudomonas Aeruginosa in Cystic Fibrosis. Clin. Sci. 2020, 134, 1911–1934. [Google Scholar] [CrossRef]
- Bedi, B.; Maurice, N.M.; Ciavatta, V.T.; Lynn, K.S.; Yuan, Z.; Molina, S.A.; Joo, M.; Tyor, W.R.; Goldberg, J.B.; Koval, M.; et al. Peroxisome Proliferator-Activated Receptor-γ Agonists Attenuate Biofilm Formation by Pseudomonas Aeruginosa. FASEB J. 2017, 31, 3608–3621. [Google Scholar] [CrossRef] [PubMed]
- Bedi, B.; Yuan, Z.; Joo, M.; Zughaier, S.M.; Goldberg, J.B.; Arbiser, J.L.; Hart, C.M.; Sadikot, R.T. Enhanced Clearance of Pseudomonas Aeruginosa by Peroxisome Proliferator-Activated Receptor Gamma. Infect. Immun. 2016, 84, 1975–1985. [Google Scholar] [CrossRef]
- Al Alam, D.; Deslee, G.; Tournois, C.; Lamkhioued, B.; Lebargy, F.; Merten, M.; Belaaouaj, A.; Guenounou, M.; Gangloff, S.C. Impaired Interleukin-8 Chemokine Secretion by Staphylococcus Aureus–Activated Epithelium and T-Cell Chemotaxis in Cystic Fibrosis. Am. J. Respir. Cell Mol. Biol. 2010, 42, 644–650. [Google Scholar] [CrossRef]
- Thammavongsa, V.; Schneewind, O.; Missiakas, D.M. Enzymatic Properties of Staphylococcus Aureus Adenosine Synthase (AdsA). BMC Biochem. 2011, 12, 56. [Google Scholar] [CrossRef]
- Tannahill, G.; Curtis, A.; Adamik, J.; Palsson-McDermott, E.; McGettrick, A.; Goel, G.; Frezza, C.; Bernard, N.; Kelly, B.; Foley, N.; et al. Succinate Is a Danger Signal That Induces IL-1β via HIF-1α. Nature 2013, 496, 238–242. [Google Scholar] [CrossRef]
- Mills, E.; O’Neill, L.A.J. Succinate: A Metabolic Signal in Inflammation. Trends Cell Biol. 2014, 24, 313–320. [Google Scholar] [CrossRef]
- O’Neill, L.A.J.; Artyomov, M.N. Itaconate: The Poster Child of Metabolic Reprogramming in Macrophage Function. Nat. Rev. Immunol. 2019, 19, 273–281. [Google Scholar] [CrossRef]
- Lampropoulou, V.; Sergushichev, A.; Bambouskova, M.; Nair, S.; Vincent, E.E.; Loginicheva, E.; Cervantes-Barragan, L.; Ma, X.; Huang, S.C.-C.; Griss, T.; et al. Itaconate Links Inhibition of Succinate Dehydrogenase with Macrophage Metabolic Remodeling and Regulation of Inflammation. Cell Metab. 2016, 24, 158–166. [Google Scholar] [CrossRef]
- D’Arpa, P.; Karna, S.L.R.; Chen, T.; Leung, K.P. Pseudomonas Aeruginosa Transcriptome Adaptations from Colonization to Biofilm Infection of Skin Wounds. Sci. Rep. 2021, 11, 20632. [Google Scholar] [CrossRef] [PubMed]
- Price, J.V.; Russo, D.; Ji, D.X.; Chavez, R.A.; DiPeso, L.; Lee, A.Y.-F.; Coers, J.; Vance, R.E. IRG1 and Inducible Nitric Oxide Synthase Act Redundantly with Other Interferon-Gamma-Induced Factors to Restrict Intracellular Replication of Legionella Pneumophila. mBio 2019, 10, e02629-19. [Google Scholar] [CrossRef] [PubMed]
- Naujoks, J.; Tabeling, C.; Dill, B.D.; Hoffmann, C.; Brown, A.S.; Kunze, M.; Kempa, S.; Peter, A.; Mollenkopf, H.-J.; Dorhoi, A.; et al. IFNs Modify the Proteome of Legionella-Containing Vacuoles and Restrict Infection Via IRG1-Derived Itaconic Acid. PLoS Pathog. 2016, 12, e1005408. [Google Scholar] [CrossRef]
- Riquelme, S.A.; Lozano, C.; Moustafa, A.M.; Liimatta, K.; Tomlinson, K.L.; Britto, C.; Khanal, S.; Gill, S.K.; Narechania, A.; Azcona-Gutiérrez, J.M.; et al. CFTR-PTEN–Dependent Mitochondrial Metabolic Dysfunction Promotes Pseudomonas Aeruginosa Airway Infection. Sci. Transl. Med. 2019, 11, eaav4634. [Google Scholar] [CrossRef]
- Liao, S.-T.; Han, C.; Xu, D.-Q.; Fu, X.-W.; Wang, J.-S.; Kong, L.-Y. 4-Octyl Itaconate Inhibits Aerobic Glycolysis by Targeting GAPDH to Exert Anti-Inflammatory Effects. Nat. Commun. 2019, 10, 5091. [Google Scholar] [CrossRef] [PubMed]
- Qin, W.; Qin, K.; Zhang, Y.; Jia, W.; Chen, Y.; Cheng, B.; Peng, L.; Chen, N.; Liu, Y.; Zhou, W.; et al. S-Glycosylation-Based Cysteine Profiling Reveals Regulation of Glycolysis by Itaconate. Nat. Chem. Biol. 2019, 15, 983–991. [Google Scholar] [CrossRef] [PubMed]
- Mills, E.L.; Ryan, D.G.; Prag, H.A.; Dikovskaya, D.; Menon, D.; Zaslona, Z.; Jedrychowski, M.P.; Costa, A.S.H.; Higgins, M.; Hams, E.; et al. Itaconate Is an Anti-Inflammatory Metabolite That Activates Nrf2 via Alkylation of KEAP1. Nature 2018, 556, 113–117. [Google Scholar] [CrossRef]
- Zygiel, E.M.; Obisesan, A.O.; Nelson, C.E.; Oglesby, A.G.; Nolan, E.M. Heme Protects Pseudomonas Aeruginosa and Staphylococcus Aureus from Calprotectin-Induced Iron Starvation. J. Biol. Chem. 2021, 296, 100160. [Google Scholar] [CrossRef]
- Lhospice, S.; Gomez, N.O.; Ouerdane, L.; Brutesco, C.; Ghssein, G.; Hajjar, C.; Liratni, A.; Wang, S.; Richaud, P.; Bleves, S.; et al. Pseudomonas Aeruginosa Zinc Uptake in Chelating Environment Is Primarily Mediated by the Metallophore Pseudopaline. Sci. Rep. 2017, 7, 17132. [Google Scholar] [CrossRef]
- Nguyen, A.T.; Jones, J.W.; Ruge, M.A.; Kane, M.A.; Oglesby-Sherrouse, A.G. Iron Depletion Enhances Production of Antimicrobials by Pseudomonas Aeruginosa. J. Bacteriol. 2015, 197, 2265–2275. [Google Scholar] [CrossRef] [PubMed]
- Wakeman, C.A.; Moore, J.L.; Noto, M.J.; Zhang, Y.; Singleton, M.D.; Prentice, B.M.; Gilston, B.A.; Doster, R.S.; Gaddy, J.A.; Chazin, W.J.; et al. The Innate Immune Protein Calprotectin Promotes Pseudomonas Aeruginosa and Staphylococcus Aureus Interaction. Nat. Commun. 2016, 7, 11951. [Google Scholar] [CrossRef] [PubMed]
- Vermilyea, D.M.; Crocker, A.W.; Gifford, A.H.; Hogan, D.A. Calprotectin-Mediated Zinc Chelation Inhibits Pseudomonas Aeruginosa Protease Activity in Cystic Fibrosis Sputum. J. Bacteriol. 2021, 203, 17. [Google Scholar] [CrossRef] [PubMed]
- Cho, H.; Jeong, D.-W.; Liu, Q.; Yeo, W.-S.; Vogl, T.; Skaar, E.P.; Chazin, W.J.; Bae, T. Calprotectin Increases the Activity of the SaeRS Two Component System and Murine Mortality during Staphylococcus Aureus Infections. PLoS Pathog. 2015, 11, e1005026. [Google Scholar] [CrossRef]
- Brinkmann, V.; Reichard, U.; Goosmann, C.; Fauler, B.; Uhlemann, Y.; Weiss, D.S.; Weinrauch, Y.; Zychlinsky, A. Neutrophil Extracellular Traps Kill Bacteria. Science 2004, 303, 1532–1535. [Google Scholar] [CrossRef]
- Urban, C.F.; Ermert, D.; Schmid, M.; Abu-Abed, U.; Goosmann, C.; Nacken, W.; Brinkmann, V.; Jungblut, P.R.; Zychlinsky, A. Neutrophil Extracellular Traps Contain Calprotectin, a Cytosolic Protein Complex Involved in Host Defense against Candida Albicans. PLoS Pathog. 2009, 5, e1000639. [Google Scholar] [CrossRef]
- Gray, R.D.; Hardisty, G.; Regan, K.H.; Smith, M.; Robb, C.T.; Duffin, R.; Mackellar, A.; Felton, J.M.; Paemka, L.; McCullagh, B.N.; et al. Delayed Neutrophil Apoptosis Enhances NET Formation in Cystic Fibrosis. Thorax 2018, 73, 134–144. [Google Scholar] [CrossRef]
- Wieneke, M.K.; Dach, F.; Neumann, C.; Görlich, D.; Kaese, L.; Thißen, T.; Dübbers, A.; Kessler, C.; Große-Onnebrink, J.; Küster, P.; et al. Association of Diverse Staphylococcus Aureus Populations with Pseudomonas Aeruginosa Coinfection and Inflammation in Cystic Fibrosis Airway Infection. mSphere 2021, 6, e00358-21. [Google Scholar] [CrossRef]
- Armbruster, C.R.; Wolter, D.J.; Mishra, M.; Hayden, H.S.; Radey, M.C.; Merrihew, G.; MacCoss, M.J.; Burns, J.; Wozniak, D.J.; Parsek, M.R.; et al. Staphylococcus Aureus Protein A Mediates Interspecies Interactions at the Cell Surface of Pseudomonas Aeruginosa. mBio 2016, 7, e00538-16. [Google Scholar] [CrossRef]
- Amiel, E.; Lovewell, R.R.; O’Toole, G.A.; Hogan, D.A.; Berwin, B. Pseudomonas Aeruginosa Evasion of Phagocytosis Is Mediated by Loss of Swimming Motility and Is Independent of Flagellum Expression. Infect. Immun. 2010, 78, 2937–2945. [Google Scholar] [CrossRef]
- Schwerdt, M.; Neumann, C.; Schwartbeck, B.; Kampmeier, S.; Herzog, S.; Görlich, D.; Dübbers, A.; Große-Onnebrink, J.; Kessler, C.; Küster, P.; et al. Staphylococcus Aureus in the Airways of Cystic Fibrosis Patients—A Retrospective Long-Term Study. Int. J. Med. Microbiol. 2018, 308, 631–639. [Google Scholar] [CrossRef] [PubMed]
- Camus, L.; Vandenesch, F.; Moreau, K. From Genotype to Phenotype: Adaptations of Pseudomonas Aeruginosa to the Cystic Fibrosis Environment. Microb. Genom. 2021, 7, mgen000513. [Google Scholar] [CrossRef] [PubMed]
- Markussen, T.; Marvig, R.L.; Gómez-Lozano, M.; Aanæs, K.; Burleigh, A.E.; Høiby, N.; Johansen, H.K.; Molin, S.; Jelsbak, L. Environmental Heterogeneity Drives within-Host Diversification and Evolution of Pseudomonas Aeruginosa. mBio 2014, 5, e01592-14. [Google Scholar] [CrossRef] [PubMed]
- Marvig, R.L.; Sommer, L.M.; Molin, S.; Johansen, H.K. Convergent Evolution and Adaptation of Pseudomonas Aeruginosa within Patients with Cystic Fibrosis. Nat. Genet. 2015, 47, 57–64. [Google Scholar] [CrossRef] [PubMed]
- Smith, E.E.; Buckley, D.G.; Wu, Z.; Saenphimmachak, C.; Hoffman, L.R.; D’Argenio, D.A.; Miller, S.I.; Ramsey, B.W.; Speert, D.P.; Moskowitz, S.M.; et al. Genetic Adaptation by Pseudomonas Aeruginosa to the Airways of Cystic Fibrosis Patients. Proc. Natl. Acad. Sci. USA 2006, 103, 8487–8492. [Google Scholar] [CrossRef]
- Klockgether, J.; Cramer, N.; Fischer, S.; Wiehlmann, L.; Tümmler, B. Long-Term Microevolution of Pseudomonas Aeruginosa Differs between Mildly and Severely Affected Cystic Fibrosis Lungs. Am. J. Respir. Cell Mol. Biol. 2018, 59, 11. [Google Scholar] [CrossRef]
- Westphal, C.; Görlich, D.; Kampmeier, S.; Herzog, S.; Braun, N.; Hitschke, C.; Mellmann, A.; Peters, G.; Kahl, B.C. Antibiotic Treatment and Age Are Associated with Staphylococcus Aureus Carriage Profiles during Persistence in the Airways of Cystic Fibrosis Patients. Front. Microbiol. 2020, 11, 230. [Google Scholar] [CrossRef]
- Camus, L.; Briaud, P.; Vandenesch, F.; Moreau, K. How Bacterial Adaptation to Cystic Fibrosis Environment Shapes Interactions between Pseudomonas Aeruginosa and Staphylococcus Aureus. Front. Microbiol. 2021, 12, 617784. [Google Scholar] [CrossRef]
- Lennartz, F.E.; Schwartbeck, B.; Dübbers, A.; Große-Onnebrink, J.; Kessler, C.; Küster, P.; Schültingkemper, H.; Peters, G.; Kahl, B.C. The Prevalence of Staphylococcus Aureus with Mucoid Phenotype in the Airways of Patients with Cystic Fibrosis—A Prospective Study. Int. J. Med. Microbiol. 2019, 309, 283–287. [Google Scholar] [CrossRef]
- Tan, X.; Coureuil, M.; Ramond, E.; Euphrasie, D.; Dupuis, M.; Tros, F.; Meyer, J.; Nemazanyy, I.; Chhuon, C.; Guerrera, I.C.; et al. Chronic Staphylococcus Aureus Lung Infection Correlates with Proteogenomic and Metabolic Adaptations Leading to an Increased Intracellular Persistence. Clin. Infect. Dis. 2019, 69, 1937–1945. [Google Scholar] [CrossRef]
- Chatterjee, I.; Kriegeskorte, A.; Fischer, A.; Deiwick, S.; Theimann, N.; Proctor, R.A.; Peters, G.; Herrmann, M.; Kahl, B.C. In Vivo Mutations of Thymidylate Synthase (Encoded by ThyA) Are Responsible for Thymidine Dependency in Clinical Small-Colony Variants of Staphylococcus Aureus. J. Bacteriol. 2008, 190, 834–842. [Google Scholar] [CrossRef] [PubMed]
- Kahl, B.C.; Becker, K.; Löffler, B. Clinical Significance and Pathogenesis of Staphylococcal Small Colony Variants in Persistent Infections. Clin. Microbiol. Rev. 2016, 29, 401–427. [Google Scholar] [CrossRef] [PubMed]
| Effect | Effector | Bibliography |
|---|---|---|
| Anti-inflammatory effect | ||
| Epithelium lysis | Hla | Seilie et al. [9] |
| Chemotaxis and complement activation inhibition | Eap | Chavakis et al. [10] |
| CHIPS | de Haas et al. [11]; Rooijakkers et al. [12] | |
| Complement activation inhibition | SCIN | Rooijakkers et al. [13] |
| ecb | Jongerius et al. [14] | |
| efb | Jongerius et al. [14] | |
| IL-1a inhibition | AdsA | Thammavongsa et al. [15] |
| IL-8 inhibition | Unknown | Chekabab et al. [16] |
| β haemolysin | Tajima et al. [17] | |
| Sae R/S | Zurek et al. [18] | |
| IL-10 inhibition | AdsA | Thammavongsa et al. [15] |
| Neutrophil recognition evasion | CoA | Guggenberger et al. [19] |
| vWBP | Guggenberger et al. [19] | |
| Biofilm | Parker et al. [20] | |
| Neutrophil degranulation inhibition | AdsA | Thammavongsa et al. [15,21] |
| Neutrophil proteases inhibition | Eap, EapH1 and EapH2 | Stapels et al. [22] |
| Neutrophil products degradation | Aureolysin | Sieprawska-Lupa et al. [23] |
| Neutrophil products protection | Staphylokinase | Jin et al. [24] |
| Oxidative burst inhibition | AdsA | Thammavongsa et al. [18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91] |
| ROS inhibition | SodA and SodM | Garcia et al. [25]; Treffon et al. [26,27] |
| Carotenoid | Liu et al. [28] | |
| KatG | Cosgrove et al. [29] | |
| NETs degradation | AdsA | Thammavongsa et al. [30] |
| Nuclease | Herzog et al. [31]; Berends et al. [32] | |
| Phagocytosis inhibition | AdsA | Pernet et al. [33,34] |
| SpA | Falugi et al. [35] | |
| Sbi | Kim et al. [36] | |
| Phagocytic cells killing | Hla HlgAB HlgCB | Seilie et al. [9] Foster et al. [37]; Seilie et al. [9] Seilie et al. [9] |
| PVL | Foster et al. [37] | |
| AdsA | Winstel et al. [38] | |
| T-cell activation inhibition through adenosine accumulation | AdsA | Thammavongsa et al. [15] |
| B-Lymphocytes apoptosis | SpA | Kim et al. [36] |
| sPLA2-IIA inhibition | AdsA | Pernet et al. [33,34] |
| Itaconate induction | Biofilm | Riquelme et al. [39]; Tomlinson et al. [40] |
| Nutritional immunity resistance | Staphylopine | Grim et al. [41] |
| Heme intake | Skaar et al. [42] | |
| Increased growth in presence of calprotectin | ArlRS | Radin et al. [43] |
| Activated in presence of calprotectin | Sae R/S | Rooijakkers et al. [13]; Jin et al. [24] |
| Pro inflammatory effect | ||
| NETs formation | Unknown | Herzog et al. [31] |
| Effect | Effector/Pathway | Bibliography |
|---|---|---|
| Anti-inflammatory effect | ||
| Mucus thickening and mucociliary clearance impairing | Cif | Stanton et al. [44] |
| Epithelium lysis | 3O-C12-HSL | Schwarzer et al. [45] |
| Exo U | Hauser et al. [46] | |
| IL-2 inhibition | 3O-C12-HSL | Hooi et al. [47] |
| IL-6 inhibition | 3O-C12-HSL | Li et al. [48] |
| HHQ | Kim et al. [49] | |
| PQS | Kim et al. [49] | |
| IL-6 destruction | LasB | LaFayette et al. [50] |
| IL-8 inhibition | OMVs | Koeppen et al. [51] |
| UPR/CHOP/PPARγ pathway | Bedi et al. [39,40,41] | |
| IL-8 destruction | LasB | LaFayette et al. [50] |
| IL-10 induction | 3O-C12-HSL | Glucksam-Galnoy et al. [52], Bortolotti et al. [53] |
| IL-12 inhibition | PQS | Skindersoe et al. [54] |
| 3O-C12-HSL | Skindersoe et al. [54], Telford et al. [55] | |
| TNFα inhibition | HHQ | Kim et al. [49] |
| PQS | Kim et al. [49] | |
| 3O-C12-HSL | Hooi et al. [47] | |
| Neutrophil recognition evasion | Biofilm | Pedersen et al. [56]; Parker et al. [20] |
| Neutrophil products degradation | LasB | Skopelja et al. [57] |
| Neutrophil protease inhibition | siglec-9 binding | Khatua et al. [58] |
| ROS inhibition | siglec-9 binding | Khatua et al. [58] |
| UPR/CHOP/PPARγ pathway | Bedi et al. [39,40,41] | |
| NETs inhibition | siglec-9 binding | Khatua et al. [58] |
| LasR deficiency | Floyd et al. [59]; Skopelja-Gardner et al. [60] | |
| Phagocytosis inhibition | Loss of motility | Lovewell et al. [61] |
| Exo T | Hauser et al. [46] | |
| Exo S | Hauser et al. [46] | |
| LasB | Mariencheck et al. [62]; Kuang et al. [63]; Alcorn et al. [64]; Moraes et al. [65] | |
| PBMC, mast cells and lymphocyte proliferation inhibition | 3O-C12-HSL | Hooi et al. [47]; Li et al. [48]; Skindersoe et al. [54] |
| PQS | Hooi et al. [47]; Li et al. [48] | |
| Phagocytic cells killing | Exo U | Hauser, [46] |
| Rhamnolipids | Jensen et al. [66] | |
| Pyocyanin | Usher et al. [67] | |
| Itaconate induction | Biofilm | Riquelme et al. [39] |
| Nutritional immunity resistance | Heme intake | Reinhart et al. [68]; Nguyen et al. [69] |
| QS molecule accumulation | Paraoxoanse-2 | Bedi et al. [39,40,41] |
| Endotoxin tolerance | Unknown | Avendaño-Ortiz et al. [70] |
| Pro inflammatory effect | ||
| IL-1B induction | LasB | Sun et al. [71] |
| IL-6 induction | 3O-C12-HSL low concentration | Mayer et al. [72]; Li et al. [48] |
| IL-8 induction | 3O-C12-HSL low concentration | Shiner et al. [73]; Smith et al. [74] |
| NETs formation | LasA | Gambello et al. [75] |
| Motility | Floyd et al. [59] | |
| Flagellum | Floyd et al. [59] | |
| sPLA2-IIA induction | ExoS | Pernet et al. [33] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Souche, A.; Vandenesch, F.; Doléans-Jordheim, A.; Moreau, K. How Staphylococcus aureus and Pseudomonas aeruginosa Hijack the Host Immune Response in the Context of Cystic Fibrosis. Int. J. Mol. Sci. 2023, 24, 6609. https://doi.org/10.3390/ijms24076609
Souche A, Vandenesch F, Doléans-Jordheim A, Moreau K. How Staphylococcus aureus and Pseudomonas aeruginosa Hijack the Host Immune Response in the Context of Cystic Fibrosis. International Journal of Molecular Sciences. 2023; 24(7):6609. https://doi.org/10.3390/ijms24076609
Chicago/Turabian StyleSouche, Aubin, François Vandenesch, Anne Doléans-Jordheim, and Karen Moreau. 2023. "How Staphylococcus aureus and Pseudomonas aeruginosa Hijack the Host Immune Response in the Context of Cystic Fibrosis" International Journal of Molecular Sciences 24, no. 7: 6609. https://doi.org/10.3390/ijms24076609
APA StyleSouche, A., Vandenesch, F., Doléans-Jordheim, A., & Moreau, K. (2023). How Staphylococcus aureus and Pseudomonas aeruginosa Hijack the Host Immune Response in the Context of Cystic Fibrosis. International Journal of Molecular Sciences, 24(7), 6609. https://doi.org/10.3390/ijms24076609








