Preventing Disused Bone Loss through Inhibition of Advanced Glycation End Products
Abstract
1. Introduction
2. Results
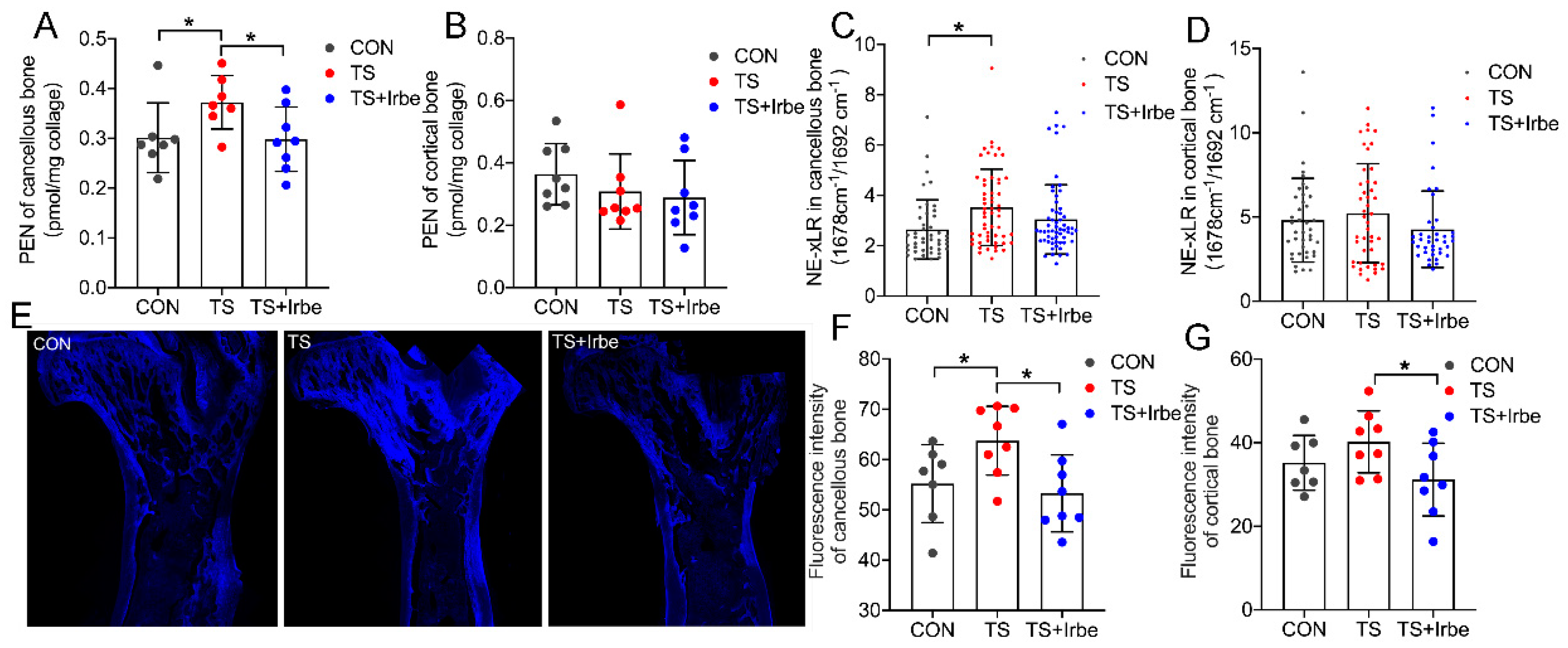
2.1. Irbesartan Inhibited AGEs Accumulation in Bone Matrix after Tail Suspension
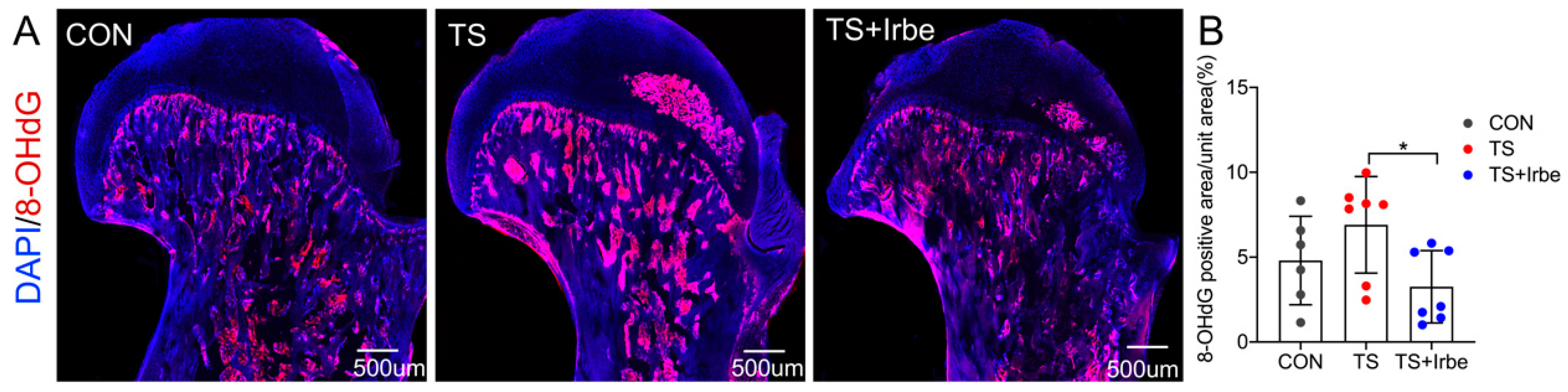
2.2. Irbesartan Can Inhibit Reactive Oxygen Species in Bone Matrix after Tail Suspension
2.3. Inhibition of AGEs Partially Improved Bone Microstructure after Tail Suspension
2.4. PEN Content Was Related to Bone Microstructure of Cancellous Bone
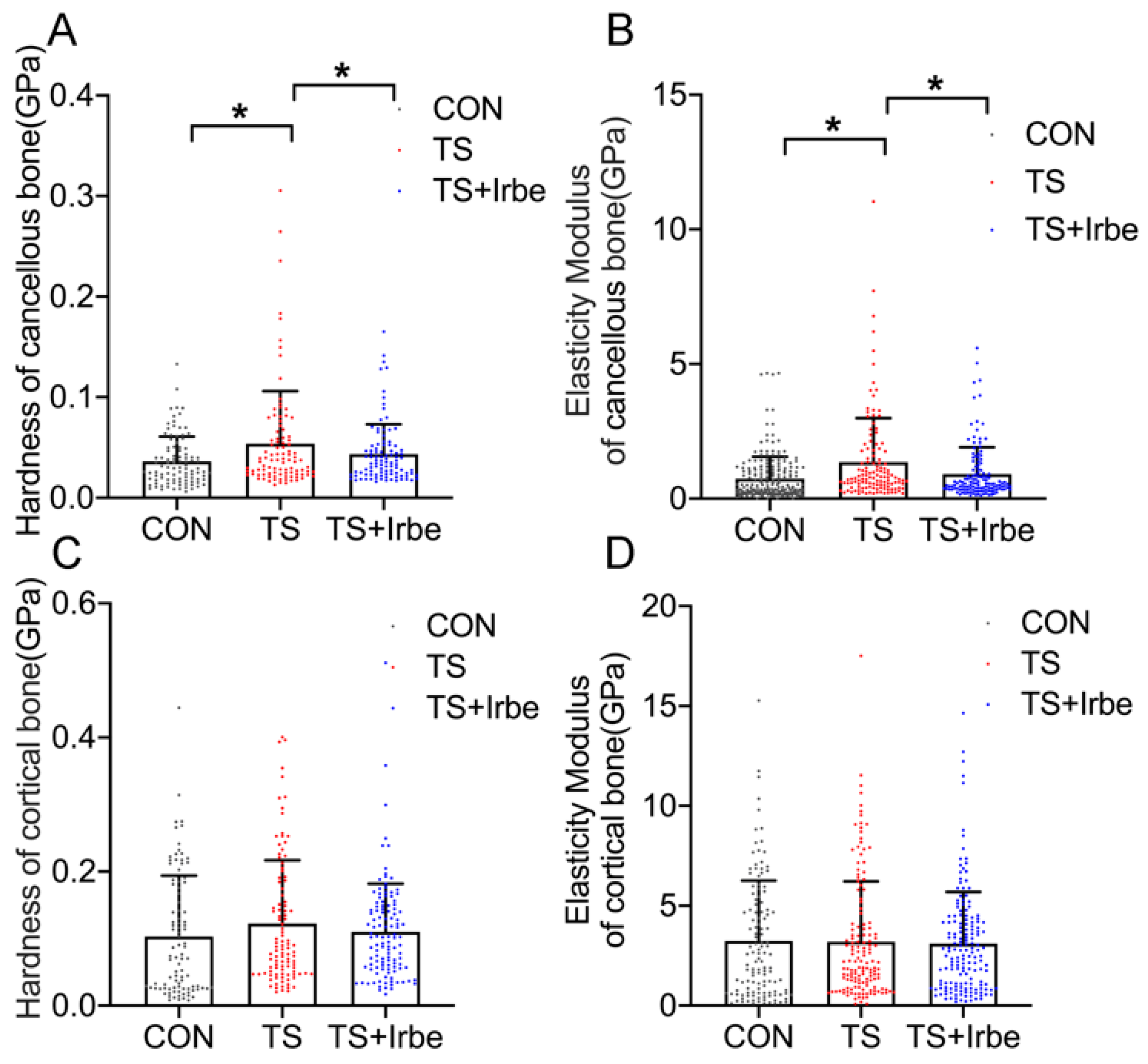
2.5. Inhibition of AGEs Improved Bone Micromechanical Properties after Tail Suspension
2.6. NE−xLR Was Related to Bone Micromechanical Properties in Cancellous Bone
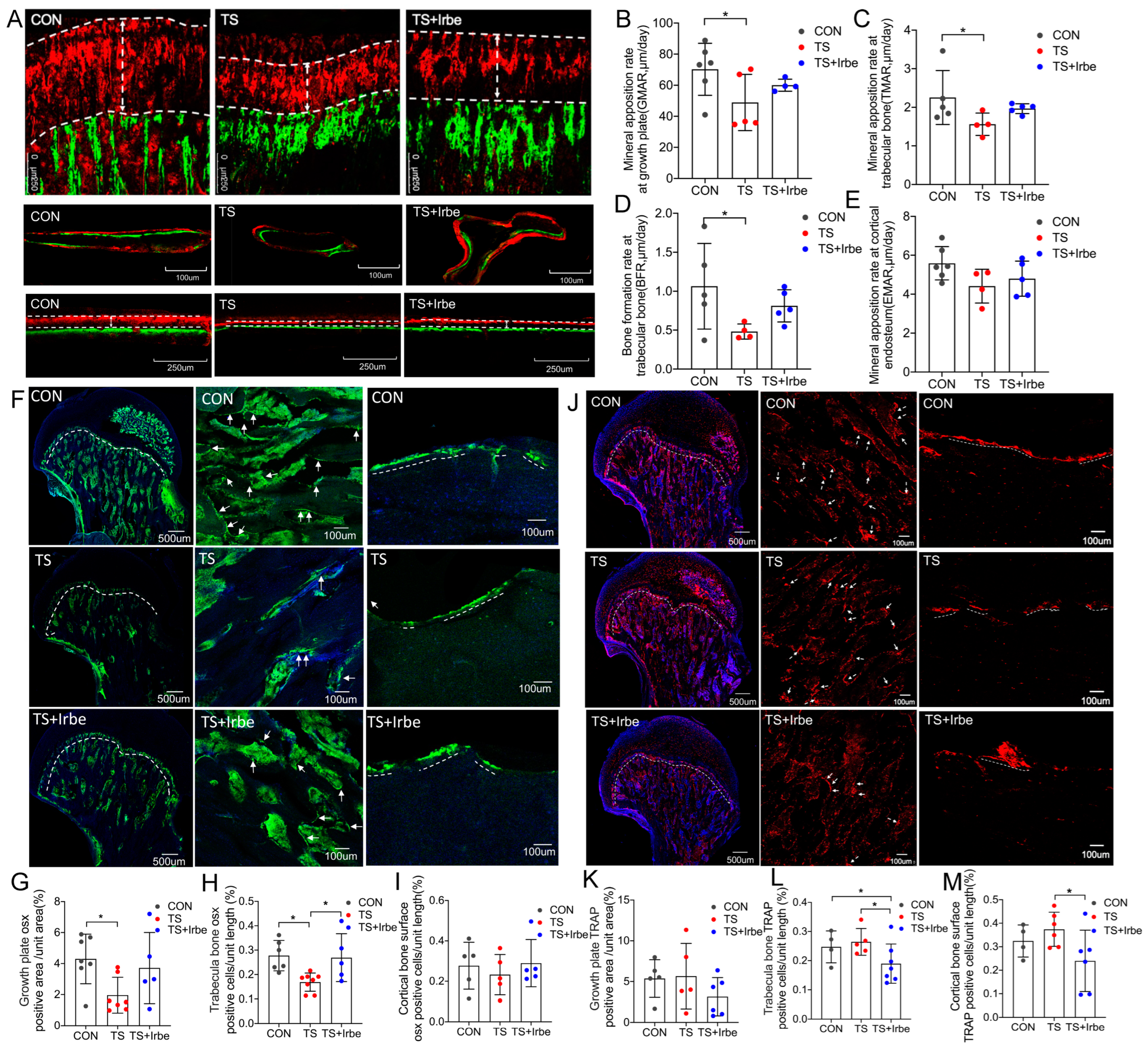
2.7. Inhibition of AGEs Partially Improved Bone Metabolism after Tail Suspension
2.8. Fluorescent AGEs in Bone Matrix Was Related to Bone Metabolism Biomarkers
3. Discussion
4. Materials and Methods
4.1. Animal Care and Experimental Designs
4.2. Sample Preparation
4.3. Non-Enzymatic Cross-Links in Bone Matrix Determination by FTIR
4.4. Bone Micromechanical Properties Determination by Nanoindentation
4.5. Fluorescent AGEs Observation by Autofluorescence Microscopy
4.6. Bone Metabolism Biomarkers Analysis by Immunofluorescence Staining
4.7. Pentosidine (PEN) Content of Bone Determination by High Performance Liquid Chromatography (HPLC)
4.8. Bone Microstructure Determination by Micro-CT Analysis
4.9. Dynamic Histomorphometric Analysis of Bone
4.10. Statistical Analysis
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Vico, L.; Collet, P.; Guignandon, A.; Lafage-Proust, M.-H.; Thomas, T.; Rehailia, M.; Alexandre, C. Effects of long-term microgravity exposure on cancellous and cortical weight-bearing bones of cosmonauts. Lancet 2000, 355, 1607–1611. [Google Scholar] [CrossRef]
- Leblanc, A.; Schneider, V.; Shackelford, L.; West, S.; Oganov, V.; Bakulin, A.; Voronin, L. Bone mineral and lean tissue loss after long duration space flight. J. Musculoskelet. Neuronal Interact. 2000, 1, 157–160. [Google Scholar]
- LeBlanc, A.; Shackelford, L.; Schneider, V. Future Human Bone Research in Space. Bone 1998, 22, 113S–116S. [Google Scholar] [CrossRef]
- Lang, T.F.; Leblanc, A.D.; Evans, H.J.; Lu, Y. Adaptation of the Proximal Femur to Skeletal Reloading after Long-Duration Spaceflight. J. Bone Miner. Res. 2006, 21, 1224–1230. [Google Scholar] [CrossRef]
- Gabel, L.; Liphardt, A.-M.; Hulme, P.A.; Heer, M.; Zwart, S.R.; Sibonga, J.D.; Smith, S.M.; Boyd, S.K. Incomplete recovery of bone strength and trabecular microarchitecture at the distal tibia 1 year after return from long duration spaceflight. Sci. Rep. 2022, 12, 1–13. [Google Scholar] [CrossRef]
- Sibonga, J.; Matsumoto, T.; Jones, J.; Shapiro, J.; Lang, T.; Shackelford, L.; Smith, S.; Young, M.; Keyak, J.; Kohri, K.; et al. Resistive exercise in astronauts on prolonged spaceflights provides partial protection against spaceflight-induced bone loss. Bone 2019, 128, 112037. [Google Scholar] [CrossRef]
- Scheuring, R.A.; Mathers, C.H.; Jones, J.A.; Wear, M.L. Musculoskeletal Injuries and Minor Trauma in Space: Incidence and Injury Mechanisms in U.S. Astronauts. Aviat. Space Environ. Med. 2009, 80, 117–124. [Google Scholar] [CrossRef]
- Liu, C.-J.; Yang, X.; Mao, Y.; Zhang, X.-X.; Wu, X.-T.; Wang, S.-H.; Fan, Y.-B.; Sun, L.-W. The alteration of advanced glycation end products and its potential role on bone loss under microgravity. Acta Astronaut. 2023, 206, 114–122. [Google Scholar] [CrossRef]
- Vistoli, G.; De Maddis, D.; Cipak, A.; Zarkovic, N.; Carini, M.; Aldini, G. Advanced glycoxidation and lipoxidation end products (AGEs and ALEs): An overview of their mechanisms of formation. Free Radic. Res. 2013, 47 (Suppl. 1), 3–27. [Google Scholar] [CrossRef]
- Lamb, L.S.; Alfonso, H.; E Norman, P.; E Davis, T.M.; Forbes, J.; Müench, G.; Irrgang, F.; Almeida, O.P.; Golledge, J.; Hankey, G.J.; et al. Advanced Glycation End Products and esRAGE Are Associated with Bone Turnover and Incidence of Hip Fracture in Older Men. J. Clin. Endocrinol. Metab. 2018, 103, 4224–4231. [Google Scholar] [CrossRef]
- Choi, D.-H.; Lee, S.-M.; Lim, S.-A.; Choi, Y.-S. Feasibility of Serum Pentosidine Level as a Potential Risk Factor for Osteoporotic Vertebral Compression Fracture. Asian Spine J. 2018, 12, 992–997. [Google Scholar] [CrossRef]
- Neumann, T.; Lodes, S.; Kästner, B.; Franke, S.; Kiehntopf, M.; Lehmann, T.; Müller, U.A.; Wolf, G.; Sämann, A. High serum pentosidine but not esRAGE is associated with prevalent fractures in type 1 diabetes independent of bone mineral density and glycaemic control. Osteoporos. Int. 2014, 25, 1527–1533. [Google Scholar] [CrossRef]
- Dhaliwal, R.; Ewing, S.K.; Vashishth, D.; Semba, R.D.; Schwartz, A.V. Greater Carboxy-Methyl-Lysine Is Associated With Increased Fracture Risk in Type 2 Diabetes. J. Bone Miner. Res. 2021, 37, 265–272. [Google Scholar] [CrossRef]
- Tang, S.; Zeenath, U.; Vashishth, D. Effects of non-enzymatic glycation on cancellous bone fragility. Bone 2007, 40, 1144–1151. [Google Scholar] [CrossRef]
- Wang, X.; Shen, X.; Li, X.; Agrawal, C.M. Age-related changes in the collagen network and toughness of bone. Bone 2002, 31, 1–7. [Google Scholar] [CrossRef]
- Hernandez, C.J.; Tang, S.; Baumbach, B.M.; Hwu, P.B.; Sakkee, A.N.; van der Ham, F.; DeGroot, J.; Bank, R.A.; Keaveny, T.M. Trabecular microfracture and the influence of pyridinium and non-enzymatic glycation-mediated collagen cross-links. Bone 2005, 37, 825–832. [Google Scholar] [CrossRef]
- Viguet-Carrin, S.; Follet, H.; Gineyts, E.; Roux, J.; Munoz, F.; Chapurlat, R.; Delmas, P.; Bouxsein, M. Association between collagen cross-links and trabecular microarchitecture properties of human vertebral bone. Bone 2010, 46, 342–347. [Google Scholar] [CrossRef]
- Rubin, M.R.; Paschalis, E.P.; Poundarik, A.; Sroga, G.E.; McMahon, D.J.; Gamsjaeger, S.; Klaushofer, K.; Vashishth, D. Advanced Glycation Endproducts and Bone Material Properties in Type 1 Diabetic Mice. PLoS ONE 2016, 11, e0154700. [Google Scholar] [CrossRef]
- Hunt, H.B.; Torres, A.M.; Palomino, P.M.; Marty, E.; Saiyed, R.; Cohn, M.; Jo, J.; Warner, S.; E Sroga, G.; King, K.B.; et al. Altered Tissue Composition, Microarchitecture, and Mechanical Performance in Cancellous Bone From Men with Type 2 Diabetes Mellitus. J. Bone Miner. Res. 2019, 34, 1191–1206. [Google Scholar] [CrossRef]
- Campbell, G.; Tiwari, S.; Hofbauer, C.; Picke, A.-K.; Rauner, M.; Huber, G.; Peña, J.; Damm, T.; Barkmann, R.; Morlock, M.; et al. Effects of parathyroid hormone on cortical porosity, non-enzymatic glycation and bone tissue mechanics in rats with type 2 diabetes mellitus. Bone 2016, 82, 116–121. [Google Scholar] [CrossRef]
- Piccoli, A.; Cannata, F.; Strollo, R.; Pedone, C.; Leanza, G.; Russo, F.; Greto, V.; Isgrò, C.; Quattrocchi, C.C.; Massaroni, C.; et al. Sclerostin Regulation, Microarchitecture, and Advanced Glycation End-Products in the Bone of Elderly Women with Type 2 Diabetes. J. Bone Miner. Res. 2020, 35, 2415–2422. [Google Scholar] [CrossRef]
- Notsu, M.; Yamaguchi, T.; Okazaki, K.; Tanaka, K.-I.; Ogawa, N.; Kanazawa, I.; Sugimoto, T. Advanced Glycation End Product 3 (AGE3) Suppresses the Mineralization of Mouse Stromal ST2 Cells and Human Mesenchymal Stem Cells by Increasing TGF-β Expression and Secretion. Endocrinology 2014, 155, 2402–2410. [Google Scholar] [CrossRef]
- Alikhani, M.; Alikhani, Z.; Boyd, C.; MacLellan, C.M.; Raptis, M.; Liu, R.; Pischon, N.; Trackman, P.C.; Gerstenfeld, L.; Graves, D.T. Advanced glycation end products stimulate osteoblast apoptosis via the MAP kinase and cytosolic apoptotic pathways. Bone 2007, 40, 345–353. [Google Scholar] [CrossRef]
- Franke, S.; Rüster, C.; Pester, J.; Hofmann, G.; Oelzner, P.; Wolf, G. Advanced glycation end products affect growth and function of osteoblasts. Ann. Rheum. Dis. 2011, 29, 650–660. [Google Scholar]
- Sanguineti, R.; Storace, D.; Monacelli, F.; Federici, A.; Odetti, P. Pentosidine Effects on Human Osteoblasts In Vitro. Ann. N. Y. Acad. Sci. 2008, 1126, 166–172. [Google Scholar] [CrossRef]
- Valcourt, U.; Merle, B.; Gineyts, E.; Viguet-Carrin, S.; Delmas, P.D.; Garnero, P. Non-enzymatic Glycation of Bone Collagen Modifies Osteoclastic Activity and Differentiation. J. Biol. Chem. 2007, 282, 5691–5703. [Google Scholar] [CrossRef]
- Franke, S.; Sommer, M.; Rüster, C.; Bondeva, T.; Marticke, J.; Hofmann, G.; Hein, G.; Wolf, G. Advanced glycation end products induce cell cycle arrest and proinflammatory changes in osteoarthritic fibroblast-like synovial cells. Thromb. Haemost. 2009, 11, R136. [Google Scholar] [CrossRef]
- Dong, X.N.; Qin, A.; Xu, J.; Wang, X. In situ accumulation of advanced glycation endproducts (AGEs) in bone matrix and its correlation with osteoclastic bone resorption. Bone 2011, 49, 174–183. [Google Scholar] [CrossRef]
- Hein, G.; Wiegand, R.; Lehmann, G.; Stein, G.; Franke, S. Advanced glycation end-products pentosidine and N-carboxymethyllysine are elevated in serum of patients with osteoporosis. Rheumatology 2003, 42, 1242–1246. [Google Scholar] [CrossRef]
- Li, Z.; Li, C.; Zhou, Y.; Chen, W.; Luo, G.; Zhang, Z.; Xu, D.; Sheng, P. Advanced glycation end products biphasically modulate bone resorption in osteoclast-like cells. Am. J. Physiol. Endocrinol. Metab. 2016, 310, E355–E366. [Google Scholar] [CrossRef]
- Bradke, B.S.; Vashishth, D. N-Phenacylthiazolium Bromide Reduces Bone Fragility Induced by Nonenzymatic Glycation. PLoS ONE 2014, 9, e103199. [Google Scholar] [CrossRef]
- Llabre, J.E.; Sroga, G.E.; Tice, M.J.; Vashishth, D. Induction and rescue of skeletal fragility in a high-fat diet mouse model of type 2 diabetes: An in vivo and in vitro approach. Bone 2022, 156, 116302. [Google Scholar] [CrossRef]
- Zhang, M.; Li, Y.; Rao, P.; Huang, K.; Luo, D.; Cai, X.; Xiao, J. Blockade of receptors of advanced glycation end products ameliorates diabetic osteogenesis of adipose-derived stem cells through DNA methylation and Wnt signalling pathway. Cell Prolif. 2018, 51, e12471. [Google Scholar] [CrossRef]
- Davis, H.M.; Essex, A.L.; Valdez, S.; Deosthale, P.J.; Aref, M.W.; Allen, M.R.; Bonetto, A.; Plotkin, L.I. Short-term pharmacologic RAGE inhibition differentially affects bone and skeletal muscle in middle-aged mice. Bone 2019, 124, 89–102. [Google Scholar] [CrossRef]
- Abar, O.; Dharmar, S.; Tang, S.Y. The effect of aminoguanidine (AG) and pyridoxamine (PM) on ageing human cortical bone. Bone Jt. Res. 2018, 7, 105–110. [Google Scholar] [CrossRef]
- Cheng, Y.-Z.; Yang, S.-L.; Wang, J.-Y.; Ye, M.; Zhuo, X.-Y.; Wang, L.T.; Chen, H.; Zhang, H.; Yang, L. Irbesartan attenuates advanced glycation end products-mediated damage in diabetes-associated osteoporosis through the AGEs/RAGE pathway. Life Sci. 2018, 205, 184–192. [Google Scholar] [CrossRef]
- Miyata, T.; Strihou, C.V.Y.D.; Ueda, Y.; Ichimori, K.; Inagi, R.; Onogi, H.; Ishikawa, N.; Nangaku, M.; Kurokawa, K. Angiotensin II Receptor Antagonists and Angiotensin-Converting Enzyme Inhibitors Lower In Vitro the Formation of Advanced Glycation End Products. J. Am. Soc. Nephrol. 2002, 13, 2478–2487. [Google Scholar] [CrossRef]
- Karim, L.; Tang, S.Y.; Sroga, G.E.; Vashishth, D. Differences in non-enzymatic glycation and collagen cross-links between human cortical and cancellous bone. Osteoporos. Int. 2013, 24, 2441–2447. [Google Scholar] [CrossRef]
- Saito, M.; Marumo, K. Effects of Collagen Crosslinking on Bone Material Properties in Health and Disease. Calcif. Tissue Int. 2015, 97, 242–261. [Google Scholar] [CrossRef]
- Tian, X.; Jee, W.S.; Li, X.; Paszty, C.; Ke, H.Z. Sclerostin antibody increases bone mass by stimulating bone formation and inhibiting bone resorption in a hindlimb-immobilization rat model. Bone 2011, 48, 197–201. [Google Scholar] [CrossRef]
- Macias, B.R.; Swift, J.M.; Nilsson, M.I.; Hogan, H.A.; Bouse, S.D.; Bloomfield, S.A. Simulated resistance training, but not alendronate, increases cortical bone formation and suppresses sclerostin during disuse. J. Appl. Physiol. 2012, 112, 918–925. [Google Scholar] [CrossRef]
- Wronski, T.J.; Morey-Holton, E.R.; Doty, S.B.; Maese, A.C.; Walsh, C.C. Histomorphometric analysis of rat skeleton following spaceflight. Am. J. Physiol. Integr. Comp. Physiol. 1987, 252, R252–R255. [Google Scholar] [CrossRef]
- Wronski, T.J.; Li, M.; Shen, Y.; Miller, S.; Bowman, B.M.; Kostenuik, P.; Halloran, B.P. Lack of effect of spaceflight on bone mass and bone formation in group-housed rats. J. Appl. Physiol. 1998, 85, 279–285. [Google Scholar] [CrossRef]
- Turner, R.T.; Evans, G.L.; Wakley, G.K. Spaceflight results in depressed cancellous bone formation in rat humeri. Aviat. Space, Environ. Med. 1995, 66, 770–774. [Google Scholar]
- Buckwalter, J.A.; Cooper, R.R. Bone structure and function. Instr. Course Lect. 1987, 36, 27–48. [Google Scholar]
- Sroga, G.E.; Siddula, A.; Vashishth, D. Glycation of Human Cortical and Cancellous Bone Captures Differences in the Formation of Maillard Reaction Products between Glucose and Ribose. PLoS ONE 2015, 10, e0117240. [Google Scholar] [CrossRef]
- Vashishth, D.; Gibson, G.; Khoury, J.; Schaffler, M.; Kimura, J.; Fyhrie, D. Influence of nonenzymatic glycation on biomechanical properties of cortical bone. Bone 2001, 28, 195–201. [Google Scholar] [CrossRef]
- Moshtagh, P.R.; Korthagen, N.M.; van Rijen, M.H.; Castelein, R.M.; Zadpoor, A.A.; Weinans, H. Effects of non-enzymatic glycation on the micro- and nano-mechanics of articular cartilage. J. Mech. Behav. Biomed. Mater. 2018, 77, 551–556. [Google Scholar] [CrossRef]
- Vaidya, R.; Rezaee, T.; Edwards, T.; Bender, R.; Vickneswaran, A.; Chalivendra, V.; Karim, L. Accumulation of fluorescent advanced glycation end products and carboxymethyl-lysine in human cortical and trabecular bone. Bone Rep. 2022, 17. [Google Scholar] [CrossRef]
- Yang, X.; Mostafa, A.J.; Appleford, M.; Sun, L.-W.; Wang, X. Bone Formation is Affected by Matrix Advanced Glycation End Products (AGEs) In Vivo. Calcif. Tissue Int. 2016, 99, 373–383. [Google Scholar] [CrossRef]
- Wei, Q.; Ren, X.; Jiang, Y.; Jin, H.; Liu, N.; Li, J. Advanced glycation end products accelerate rat vascular calcification through RAGE/oxidative stress. BMC Cardiovasc. Disord. 2013, 13, 13. [Google Scholar] [CrossRef]
- Knott, L.; Bailey, A. Collagen cross-links in mineralizing tissues: A review of their chemistry, function, and clinical relevance. Bone 1998, 22, 181–187. [Google Scholar] [CrossRef]
- Asaba, Y.; Ito, M.; Fumoto, T.; Watanabe, K.; Fukuhara, R.; Takeshita, S.; Nimura, Y.; Ishida, J.; Fukamizu, A.; Ikeda, K. Activation of Renin–Angiotensin System Induces Osteoporosis Independently of Hypertension. J. Bone Miner. Res. 2009, 24, 241–250. [Google Scholar] [CrossRef] [PubMed]
- Abuohashish, H.M.; Ahmed, M.M.; Sabry, D.; Khattab, M.M.; Al-Rejaie, S.S. The ACE-2/Ang1-7/Mas cascade enhances bone structure and metabolism following angiotensin-II type 1 receptor blockade. Eur. J. Pharmacol. 2017, 807, 44–55. [Google Scholar] [CrossRef] [PubMed]
- Sun, L.-W.; Huang, Y.-F.; Wang, Y.; Luan, H.-Q.; Fan, Y.-B. Comparison of bone histomorphometry and μCT for evaluating bone quality in tail-suspended rats. Life Sci. Space Res. 2014, 3, 18–23. [Google Scholar] [CrossRef]
- Camacho, N.P.; West, P.; Torzilli, P.A.; Mendelsohn, R. FTIR microscopic imaging of collagen and proteoglycan in bovine cartilage. Biopolymers 2001, 62, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, F.; Zimmermann, E.; Campbell, G.; Sroga, G.; Püschel, K.; Amling, M.; Tang, S.; Vashishth, D.; Busse, B. Assessment of collagen quality associated with non-enzymatic cross-links in human bone using Fourier-transform infrared imaging. Bone 2017, 97, 243–251. [Google Scholar] [CrossRef] [PubMed]
- Rabotyagova, O.S.; Cebe, P.; Kaplan, D.L. Collagen structural hierarchy and susceptibility to degradation by ultraviolet radiation. Mater. Sci. Eng. C 2008, 28, 1420–1429. [Google Scholar] [CrossRef]
- Oliver, W.C.; Pharr, G.M. An improved technique for determining hardness and elastic modulus using load and displacement sensing indentation experiments. J. Mater. Res. 1992, 7, 1564–1583. [Google Scholar] [CrossRef]
- Luo, C.; Liao, J.; Zhu, Z.; Wang, X.; Lin, X.; Huang, W. Analysis of Mechanical Properties and Mechanical Anisotropy in Canine Bone Tissues of Various Ages. BioMed Res. Int. 2019, 2019, 3503152. [Google Scholar] [CrossRef]
- Kusumbe, A.P.; Ramasamy, S.; Starsichova, A.; Adams, R.H. Sample preparation for high-resolution 3D confocal imaging of mouse skeletal tissue. Nat. Protoc. 2015, 10, 1904–1914. [Google Scholar] [CrossRef]
- Viguet-Carrin, S.; Gineyts, E.; Bertholon, C.; Delmas, P. Simple and sensitive method for quantification of fluorescent enzymatic mature and senescent crosslinks of collagen in bone hydrolysate using single-column high performance liquid chromatography. J. Chromatogr. B 2009, 877, 1–7. [Google Scholar] [CrossRef]


| PEN of Cancellous Bone | ||
|---|---|---|
| R | p | |
| BMD | −0.485 | 0.041 * |
| BV/TV | −0.482 | 0.050 |
| Tb.Th | −0.367 | 0.148 |
| Tb.N | −0.519 | 0.028 * |
| Tb.Sp | 0.365 | 0.137 |
| BS/BV | 0.277 | 0.263 |
| BS/TV | −0.609 | 0.009 * |
| SMI | 0.505 | 0.032 * |
| NE−xLR in Cancellous Bone | NE−xLR in Cortical Bone | |||
|---|---|---|---|---|
| R | p | R | p | |
| Hardness | 0.686 | <0.0001 * | 0.135 | 0.548 |
| Elastic modulus | 0.547 | 0.0031 * | 0.273 | 0.218 |
| fAGEs in Cancellous Bone | fAGEs in Cortical Bone | |||
|---|---|---|---|---|
| R | p | R | p | |
| Osterix (+) cells | −0.611 | 0.005 * | −0.187 | 0.5055 |
| TRAP (+) cells | 0.4414 | 0.0996 | 0.554 | 0.0260 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, C.-J.; Yang, X.; Wang, S.-H.; Wu, X.-T.; Mao, Y.; Shi, J.-W.; Fan, Y.-B.; Sun, L.-W. Preventing Disused Bone Loss through Inhibition of Advanced Glycation End Products. Int. J. Mol. Sci. 2023, 24, 4953. https://doi.org/10.3390/ijms24054953
Liu C-J, Yang X, Wang S-H, Wu X-T, Mao Y, Shi J-W, Fan Y-B, Sun L-W. Preventing Disused Bone Loss through Inhibition of Advanced Glycation End Products. International Journal of Molecular Sciences. 2023; 24(5):4953. https://doi.org/10.3390/ijms24054953
Chicago/Turabian StyleLiu, Cong-Jin, Xiao Yang, Shou-Hui Wang, Xin-Tong Wu, Yan Mao, Jing-Wen Shi, Yu-Bo Fan, and Lian-Wen Sun. 2023. "Preventing Disused Bone Loss through Inhibition of Advanced Glycation End Products" International Journal of Molecular Sciences 24, no. 5: 4953. https://doi.org/10.3390/ijms24054953
APA StyleLiu, C.-J., Yang, X., Wang, S.-H., Wu, X.-T., Mao, Y., Shi, J.-W., Fan, Y.-B., & Sun, L.-W. (2023). Preventing Disused Bone Loss through Inhibition of Advanced Glycation End Products. International Journal of Molecular Sciences, 24(5), 4953. https://doi.org/10.3390/ijms24054953







