Prediction Model with HLA-A*33:03 Reveals Number of Days to Develop Liver Cancer from Blood Test
Abstract
1. Introduction
2. Results
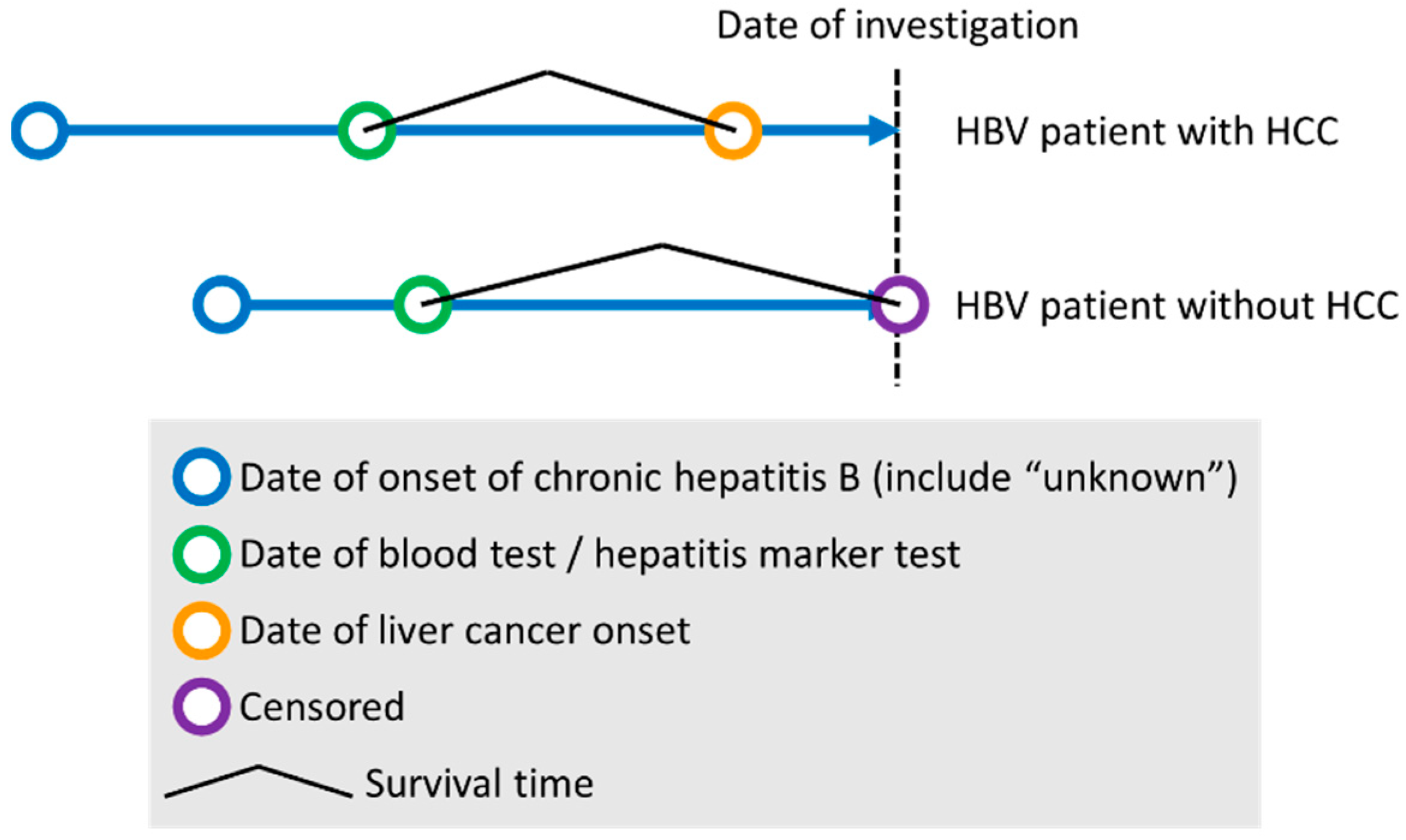
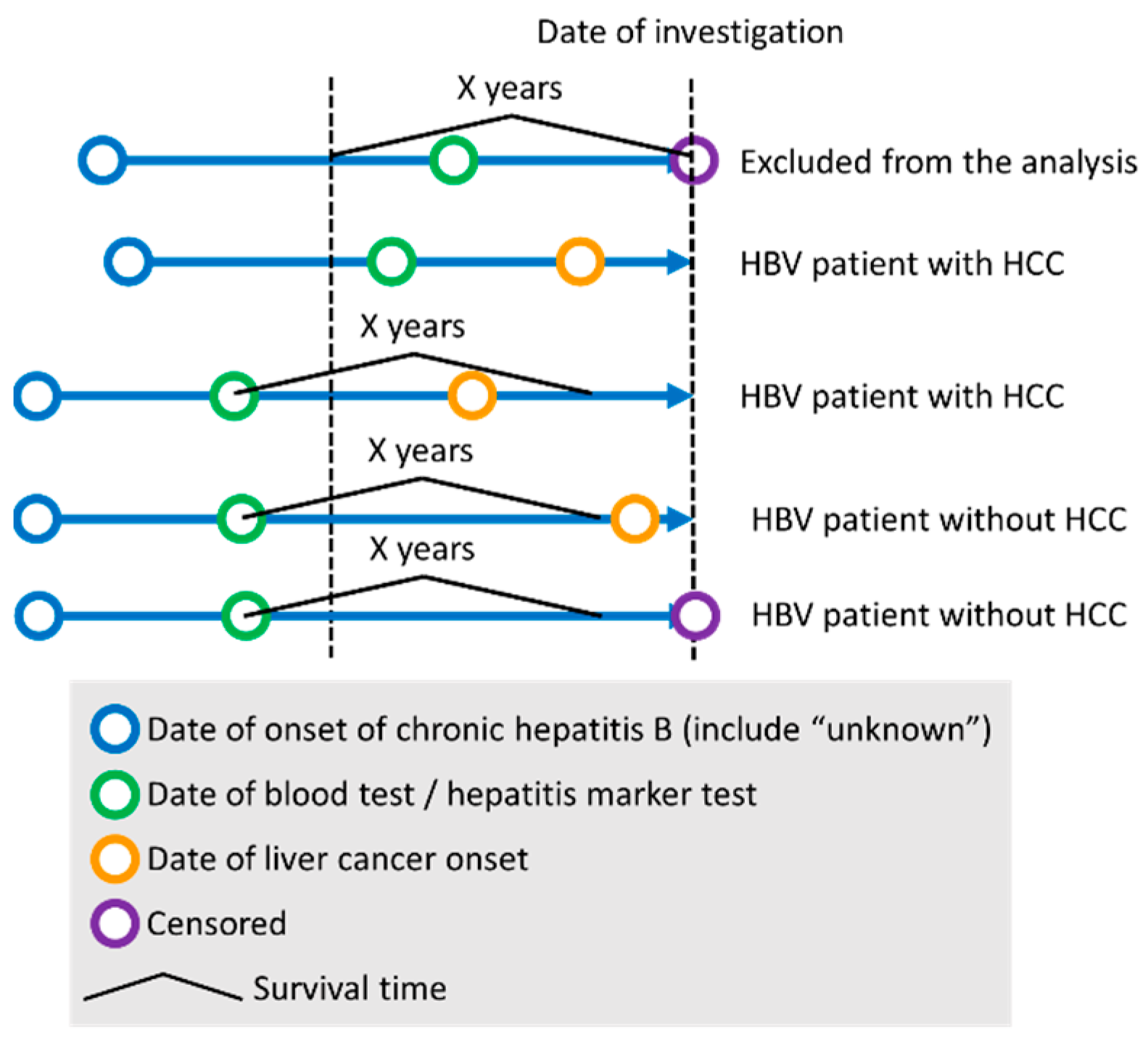
2.1. Clinical Characteristics of Studied Individuals and Study Design
2.2. The Cox Proportional-Hazards Regression Model to Predict the Early Onset of HCC
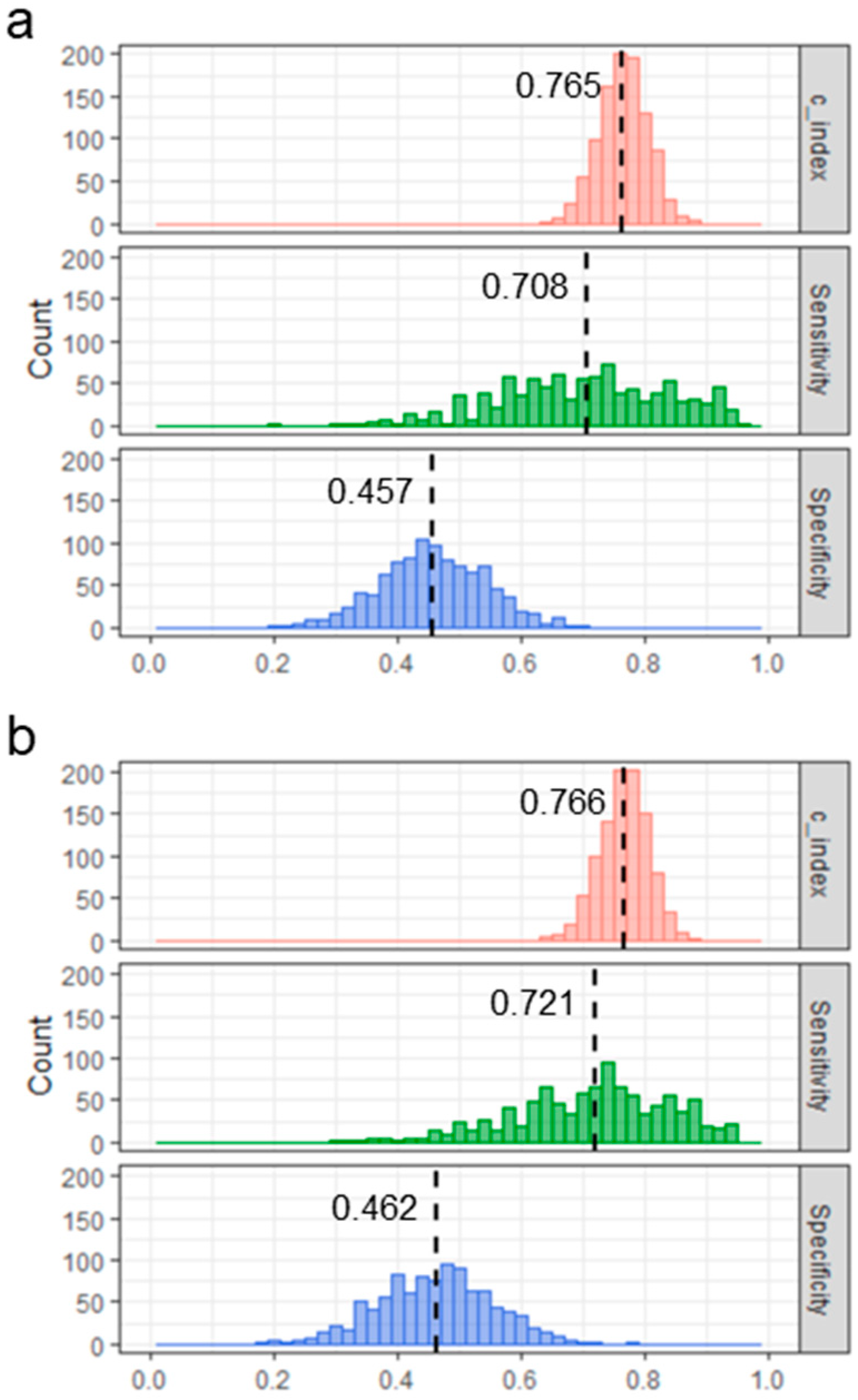
2.3. Validation of the Model
3. Discussion
4. Materials and Methods
4.1. Study Population
4.2. Data Curation of Clinical Items
4.3. HLA Imputation Using Genome-Wide SNP Typing Data
4.4. Constructing the Cox Proportional-Hazards Regression Model to Predict the Onset of HCC
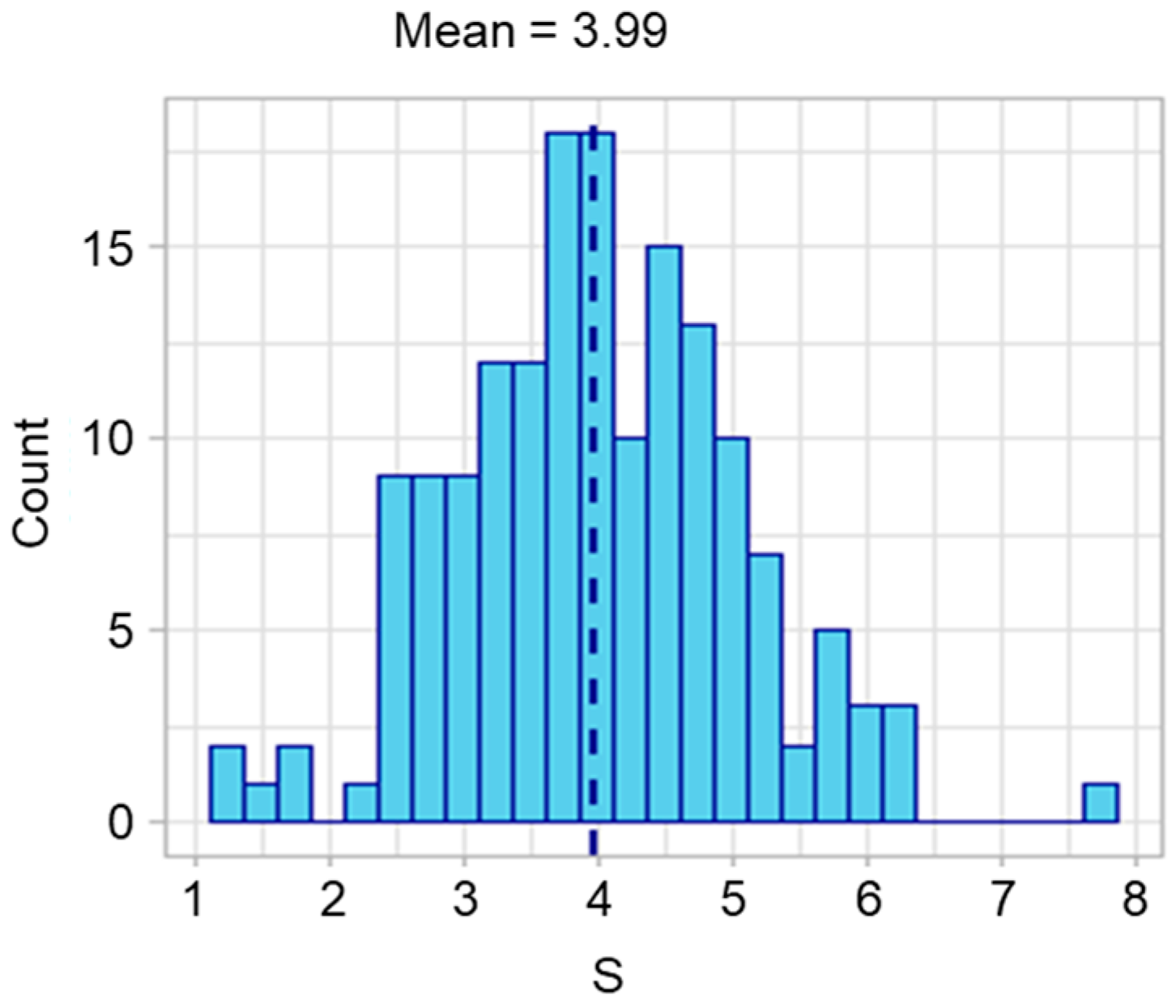
4.5. Validation of the HBV-HCC Model by Computer Simulation
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ishiguro, S.; Inoue, M.; Tanaka, Y.; Mizokami, M.; Iwasaki, M.; Tsugane, S.; Group, J.S. Impact of viral load of hepatitis C on the incidence of hepatocellular carcinoma: A population-based cohort study (JPHC Study). Cancer Lett. 2011, 300, 173–179. [Google Scholar] [CrossRef]
- Yang, H.I.; Yuen, M.F.; Chan, H.L.; Han, K.H.; Chen, P.J.; Kim, D.Y.; Ahn, S.H.; Chen, C.J.; Wong, V.W.; Seto, W.K.; et al. Risk estimation for hepatocellular carcinoma in chronic hepatitis B (REACH-B): Development and validation of a predictive score. Lancet Oncol. 2011, 12, 568–574. [Google Scholar] [CrossRef]
- Papatheodoridis, G.; Dalekos, G.; Sypsa, V.; Yurdaydin, C.; Buti, M.; Goulis, J.; Calleja, J.L.; Chi, H.; Manolakopoulos, S.; Mangia, G.; et al. PAGE-B predicts the risk of developing hepatocellular carcinoma in Caucasians with chronic hepatitis B on 5-year antiviral therapy. J. Hepatol. 2016, 64, 800–806. [Google Scholar] [CrossRef]
- Kim, J.H.; Kim, Y.D.; Lee, M.; Jun, B.G.; Kim, T.S.; Suk, K.T.; Kang, S.H.; Kim, M.Y.; Cheon, G.J.; Kim, D.J.; et al. Modified PAGE-B score predicts the risk of hepatocellular carcinoma in Asians with chronic hepatitis B on antiviral therapy. J. Hepatol. 2018, 69, 1066–1073. [Google Scholar] [CrossRef] [PubMed]
- Yuen, M.F.; Tanaka, Y.; Fong, D.Y.; Fung, J.; Wong, D.K.; Yuen, J.C.; But, D.Y.; Chan, A.O.; Wong, B.C.; Mizokami, M.; et al. Independent risk factors and predictive score for the development of hepatocellular carcinoma in chronic hepatitis B. J. Hepatol. 2009, 50, 80–88. [Google Scholar] [CrossRef]
- Chen, C.H.; Lee, C.M.; Lai, H.C.; Hu, T.H.; Su, W.P.; Lu, S.N.; Lin, C.H.; Hung, C.H.; Wang, J.H.; Lee, M.H.; et al. Prediction model of hepatocellular carcinoma risk in Asian patients with chronic hepatitis B treated with entecavir. Oncotarget 2017, 8, 92431–92441. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.S.; Yu, X.; Kramer, J.; Thrift, A.P.; Richardson, P.; Hsu, Y.C.; Flores, A.; El-Serag, H.B.; Kanwal, F. Comparative performance of risk prediction models for hepatitis B-related hepatocellular carcinoma in the United States. J. Hepatol. 2022, 76, 294–301. [Google Scholar] [CrossRef] [PubMed]
- Kamatani, Y.; Wattanapokayakit, S.; Ochi, H.; Kawaguchi, T.; Takahashi, A.; Hosono, N.; Kubo, M.; Tsunoda, T.; Kamatani, N.; Kumada, H.; et al. A genome-wide association study identifies variants in the HLA-DP locus associated with chronic hepatitis B in Asians. Nat. Genet. 2009, 41, 591–595. [Google Scholar] [CrossRef] [PubMed]
- Mbarek, H.; Ochi, H.; Urabe, Y.; Kumar, V.; Kubo, M.; Hosono, N.; Takahashi, A.; Kamatani, Y.; Miki, D.; Abe, H.; et al. A genome-wide association study of chronic hepatitis B identified novel risk locus in a Japanese population. Hum. Mol. Genet. 2011, 20, 3884–3892. [Google Scholar] [CrossRef]
- Nishida, N.; Sawai, H.; Kashiwase, K.; Minami, M.; Sugiyama, M.; Seto, W.K.; Yuen, M.F.; Posuwan, N.; Poovorawan, Y.; Ahn, S.H.; et al. New susceptibility and resistance HLA-DP alleles to HBV-related diseases identified by a trans-ethnic association study in Asia. PLoS ONE 2014, 9, e86449. [Google Scholar] [CrossRef]
- Sawai, H.; Nishida, N.; Khor, S.S.; Honda, M.; Sugiyama, M.; Baba, N.; Yamada, K.; Sawada, N.; Tsugane, S.; Koike, K.; et al. Genome-wide association study identified new susceptible genetic variants in HLA class I region for hepatitis B virus-related hepatocellular carcinoma. Sci. Rep. 2018, 8, 7958. [Google Scholar] [CrossRef]
- Nagai, A.; Hirata, M.; Kamatani, Y.; Muto, K.; Matsuda, K.; Kiyohara, Y.; Ninomiya, T.; Tamakoshi, A.; Yamagata, Z.; Mushiroda, T.; et al. Overview of the BioBank Japan Project: Study design and profile. J. Epidemiol. 2017, 27, S2–S8. [Google Scholar] [CrossRef] [PubMed]
- Hirata, M.; Kamatani, Y.; Nagai, A.; Kiyohara, Y.; Ninomiya, T.; Tamakoshi, A.; Yamagata, Z.; Kubo, M.; Muto, K.; Mushiroda, T.; et al. Cross-sectional analysis of BioBank Japan clinical data: A large cohort of 200,000 patients with 47 common diseases. J. Epidemiol. 2017, 27, S9–S21. [Google Scholar] [CrossRef] [PubMed]
- Cox, D.R. Regression Models and Life Tables (with Discussion). J. R. Stat. Soc. 1972, 34, 187–220. [Google Scholar]
- Harrell, F.E., Jr.; Califf, R.M.; Pryor, D.B.; Lee, K.L.; Rosati, R.A. Evaluating the yield of medical tests. JAMA 1982, 247, 2543–2546. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.I.; Yeh, M.L.; Wong, G.L.; Peng, C.Y.; Chen, C.H.; Trinh, H.N.; Cheung, K.S.; Xie, Q.; Su, T.H.; Kozuka, R.; et al. Real-World Effectiveness from the Asia Pacific Rim Liver Consortium for HBV Risk Score for the Prediction of Hepatocellular Carcinoma in Chronic Hepatitis B Patients Treated with Oral Antiviral Therapy. J. Infect. Dis. 2020, 221, 389–399. [Google Scholar] [CrossRef]
- Poh, Z.; Shen, L.; Yang, H.I.; Seto, W.K.; Wong, V.W.; Lin, C.Y.; Goh, B.B.; Chang, P.E.; Chan, H.L.; Yuen, M.F.; et al. Real-world risk score for hepatocellular carcinoma (RWS-HCC): A clinically practical risk predictor for HCC in chronic hepatitis B. Gut 2016, 65, 887–888. [Google Scholar] [CrossRef]
- Khor, S.S.; Yang, W.; Kawashima, M.; Kamitsuji, S.; Zheng, X.; Nishida, N.; Sawai, H.; Toyoda, H.; Miyagawa, T.; Honda, M.; et al. High-accuracy imputation for HLA class I and II genes based on high-resolution SNP data of population-specific references. Pharm. J. 2015, 15, 530–537. [Google Scholar] [CrossRef]
- Wang, Y.Y.; Mimori, T.; Khor, S.S.; Gervais, O.; Kawai, Y.; Hitomi, Y.; Tokunaga, K.; Nagasaki, M. HLA-VBSeq v2: Improved HLA calling accuracy with full-length Japanese class-I panel. Hum. Genome Var. 2019, 6, 29. [Google Scholar] [CrossRef]
- Nariai, N.; Kojima, K.; Saito, S.; Mimori, T.; Sato, Y.; Kawai, Y.; Yamaguchi-Kabata, Y.; Yasuda, J.; Nagasaki, M. HLA-VBSeq: Accurate HLA typing at full resolution from whole-genome sequencing data. BMC Genom. 2015, 16 (Suppl. 2), S7. [Google Scholar] [CrossRef]
- Li, H.; Durbin, R. Fast and accurate short read alignment with Burrows-Wheeler transform. Bioinformatics 2009, 25, 1754–1760. [Google Scholar] [CrossRef] [PubMed]
- Robinson, J.; Halliwell, J.A.; Hayhurst, J.D.; Flicek, P.; Parham, P.; Marsh, S.G. The IPD and IMGT/HLA database: Allele variant databases. Nucleic Acids Res. 2015, 43, D423–D431. [Google Scholar] [CrossRef] [PubMed]


| HBV Patients with HCC (n = 83) | HBV Patients without HCC (n = 79) | |
|---|---|---|
| Age at blood test (average (min, max)) | 57.1 (32–83) | 48.7 (21–78) |
| Average number of days from blood test to diagnosis of HCC | 1274 | - |
| Average number of days between blood test date and censored date | - | 1189 |
| Sex (Male/Female) | 65/18 | 34/45 |
| Presence of LC at blood test (%) | 12.0 | 5.1 |
| AFP at blood test (median log10AFP) | 1.16 | 0.55 |
| HLA-A*33:03 carrier frequency | 0.11 | 0.08 |
| HLA-A*31:01 carrier frequency | 0.24 | 0.28 |
| HLA-DPB1*02:01 carrier frequency | 0.33 | 0.38 |
| Variable | Beta | HR | HR Lower | HR Upper | z | p Value |
|---|---|---|---|---|---|---|
| age | 0.057 | 1.058 | 1.036 | 1.081 | 5.313 | 1.08 × 10−7 |
| sex | 0.601 | 1.825 | 1.069 | 3.114 | 2.206 | 2.74 × 10−2 |
| log10AFP | 0.642 | 1.900 | 1.467 | 2.462 | 4.859 | 1.18 × 10−6 |
| A*33:03 | 0.714 | 2.042 | 0.987 | 4.225 | 1.924 | 5.44 × 10−2 |
| HBV Patients with HCC (n = 291) | HBV Patients without HCC (n = 361) | |
|---|---|---|
| Age at blood test (average (min, max)) | 58.4 (37–83) | 53.9 (18–82) |
| Average number of days from blood test to diagnosis of HCC | 1130 | - |
| Average number of days between blood test date and censored date | - | 2826 |
| Sex (Male/Female) | 233/58 | 169/192 |
| Presence of LC at blood test (%) | 26.8 | 4.71 |
| AFP at blood test (median log10AFP) | 1.33 | 0.57 |
| HLA-A*33:03 carrier frequency | 0.10 | 0.08 |
| HLA-A*31:01 carrier frequency | 0.228 | 0.20 |
| HLA-DPB1*02:01 carrier frequency | 0.398 | 0.336 |
| Variable | Beta | HR | HR Lower | HR Upper | z | p Value |
|---|---|---|---|---|---|---|
| age | 0.059 | 1.061 | 1.038 | 1.084 | 5.404 | 6.52 × 10−8 |
| sex | 0.704 | 2.022 | 1.145 | 3.570 | 2.428 | 1.52 × 10−2 |
| LC | 0.167 | 1.181 | 0.583 | 2.391 | 0.463 | 6.44 × 10−1 |
| log10AFP | 0.650 | 1.916 | 1.477 | 2.486 | 4.892 | 1.00 × 10−6 |
| HLA-A*33:03 | 0.740 | 2.096 | 1.006 | 4.364 | 1.977 | 4.81 × 10−2 |
| HLA-A*31:01 | 0.277 | 1.319 | 0.772 | 2.253 | 1.012 | 3.11 × 10−1 |
| HLA-DPB1*02:01 | −0.256 | 0.774 | 0.479 | 1.252 | −1.043 | 2.97 × 10−1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nishida, N.; Ohashi, J.; Suda, G.; Chiyoda, T.; Tamaki, N.; Tomiyama, T.; Ogasawara, S.; Sugiyama, M.; Kawai, Y.; Khor, S.-S.; et al. Prediction Model with HLA-A*33:03 Reveals Number of Days to Develop Liver Cancer from Blood Test. Int. J. Mol. Sci. 2023, 24, 4761. https://doi.org/10.3390/ijms24054761
Nishida N, Ohashi J, Suda G, Chiyoda T, Tamaki N, Tomiyama T, Ogasawara S, Sugiyama M, Kawai Y, Khor S-S, et al. Prediction Model with HLA-A*33:03 Reveals Number of Days to Develop Liver Cancer from Blood Test. International Journal of Molecular Sciences. 2023; 24(5):4761. https://doi.org/10.3390/ijms24054761
Chicago/Turabian StyleNishida, Nao, Jun Ohashi, Goki Suda, Takehiro Chiyoda, Nobuharu Tamaki, Takahiro Tomiyama, Sachiko Ogasawara, Masaya Sugiyama, Yosuke Kawai, Seik-Soon Khor, and et al. 2023. "Prediction Model with HLA-A*33:03 Reveals Number of Days to Develop Liver Cancer from Blood Test" International Journal of Molecular Sciences 24, no. 5: 4761. https://doi.org/10.3390/ijms24054761
APA StyleNishida, N., Ohashi, J., Suda, G., Chiyoda, T., Tamaki, N., Tomiyama, T., Ogasawara, S., Sugiyama, M., Kawai, Y., Khor, S.-S., Nagasaki, M., Fujimoto, A., Tsuchiura, T., Ishikawa, M., Matsuda, K., Yano, H., Yoshizumi, T., Izumi, N., Hasegawa, K., ... Tokunaga, K. (2023). Prediction Model with HLA-A*33:03 Reveals Number of Days to Develop Liver Cancer from Blood Test. International Journal of Molecular Sciences, 24(5), 4761. https://doi.org/10.3390/ijms24054761








