The Effect of Mice Adaptation Process on the Pathogenicity of Influenza A/South Africa/3626/2013 (H1N1)pdm09 Model Strain
Abstract
:1. Introduction
2. Results
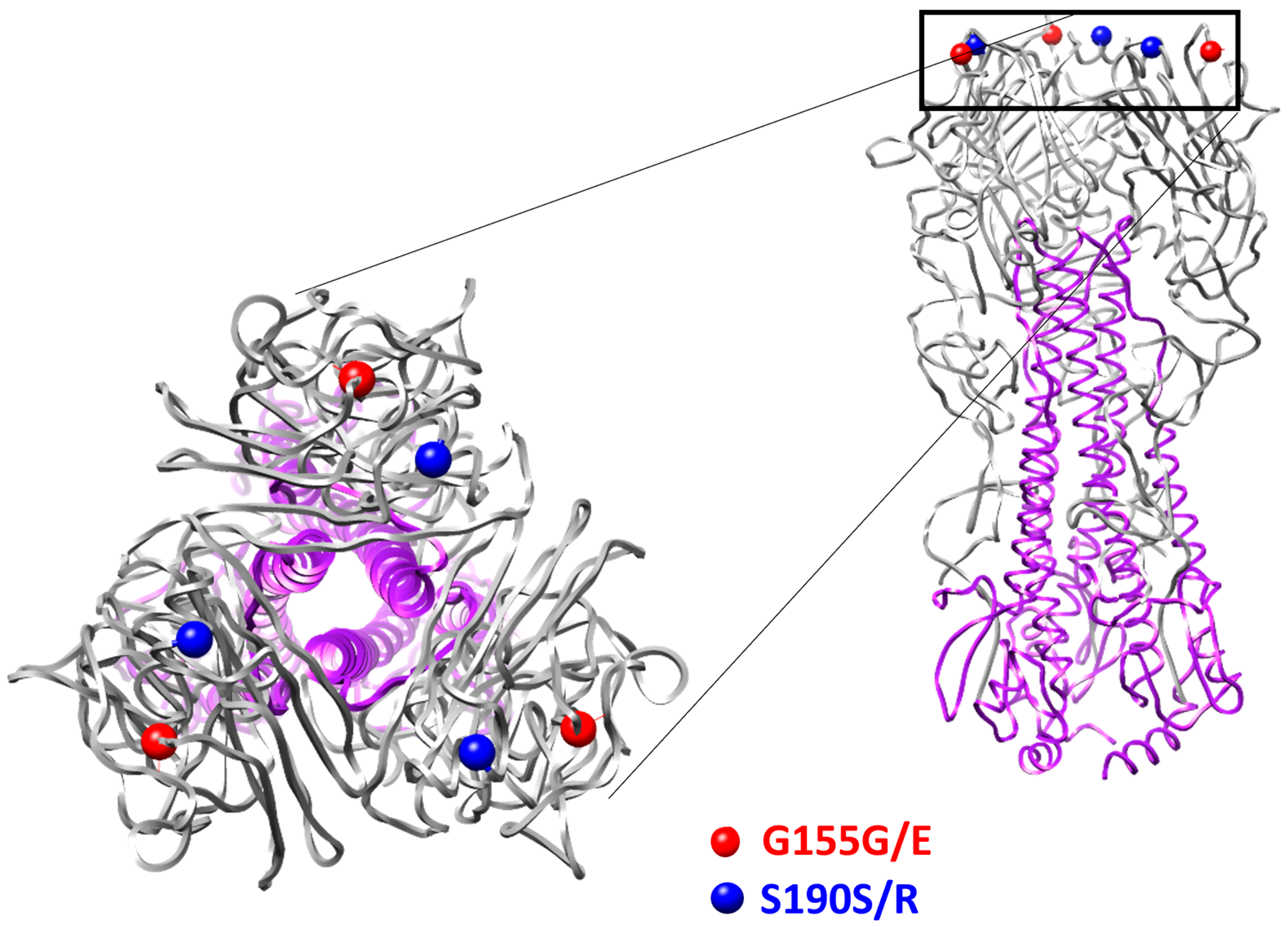
2.1. Sequencing Analysis of SA-M5
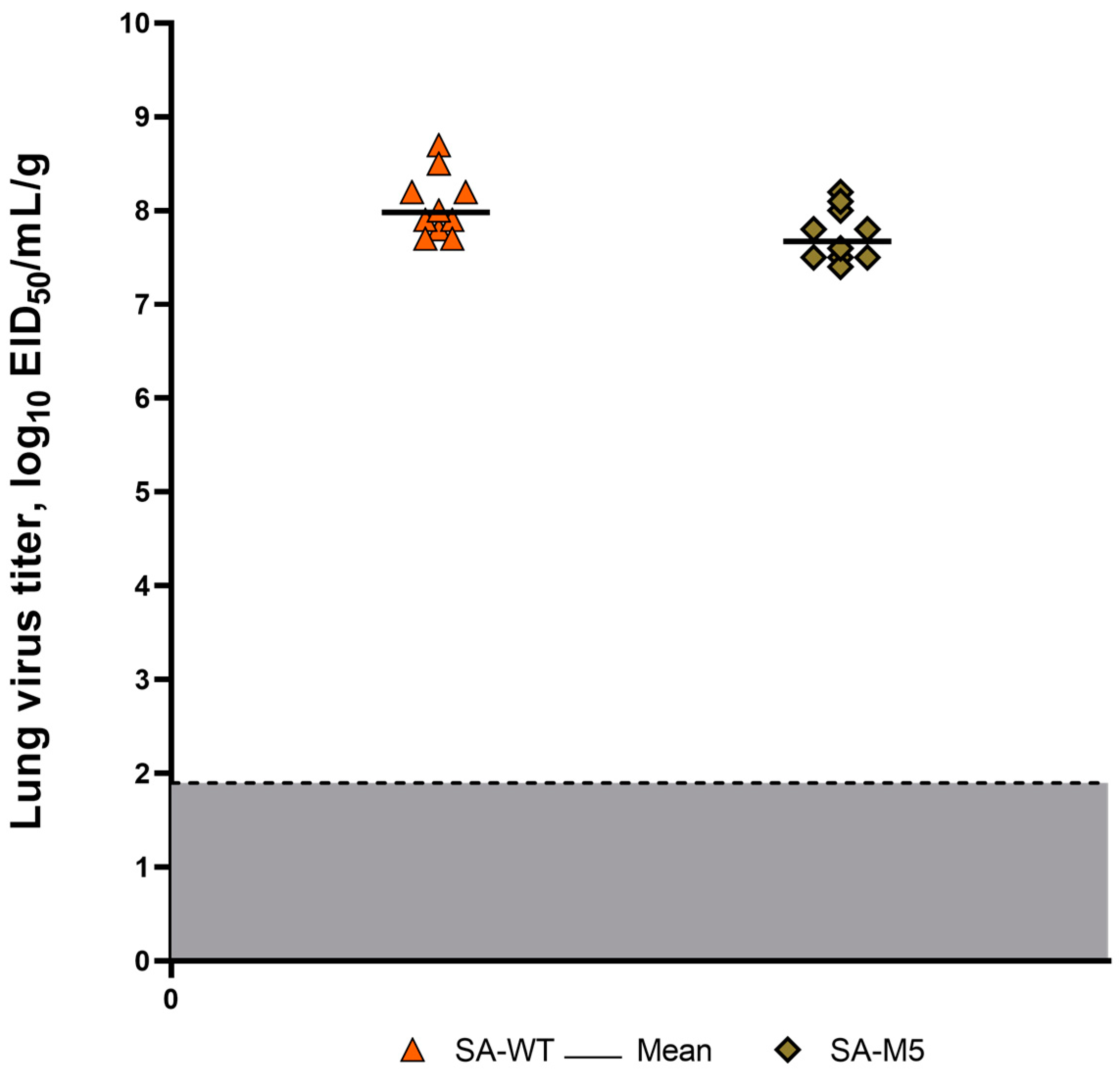
2.2. Viral Replication in Lung Tissue
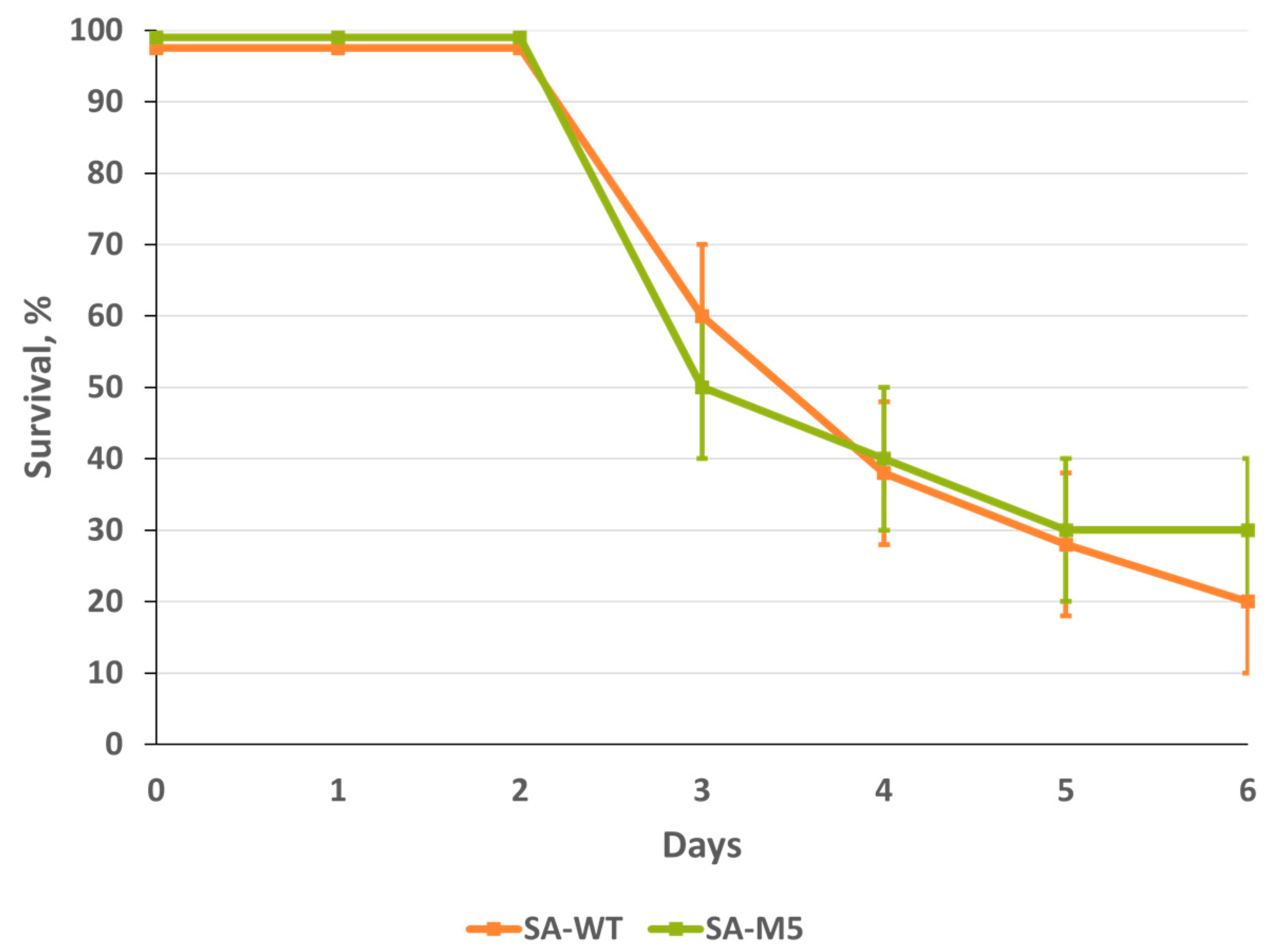
2.3. SA-WT and SA-M5 Toxicity in Mice
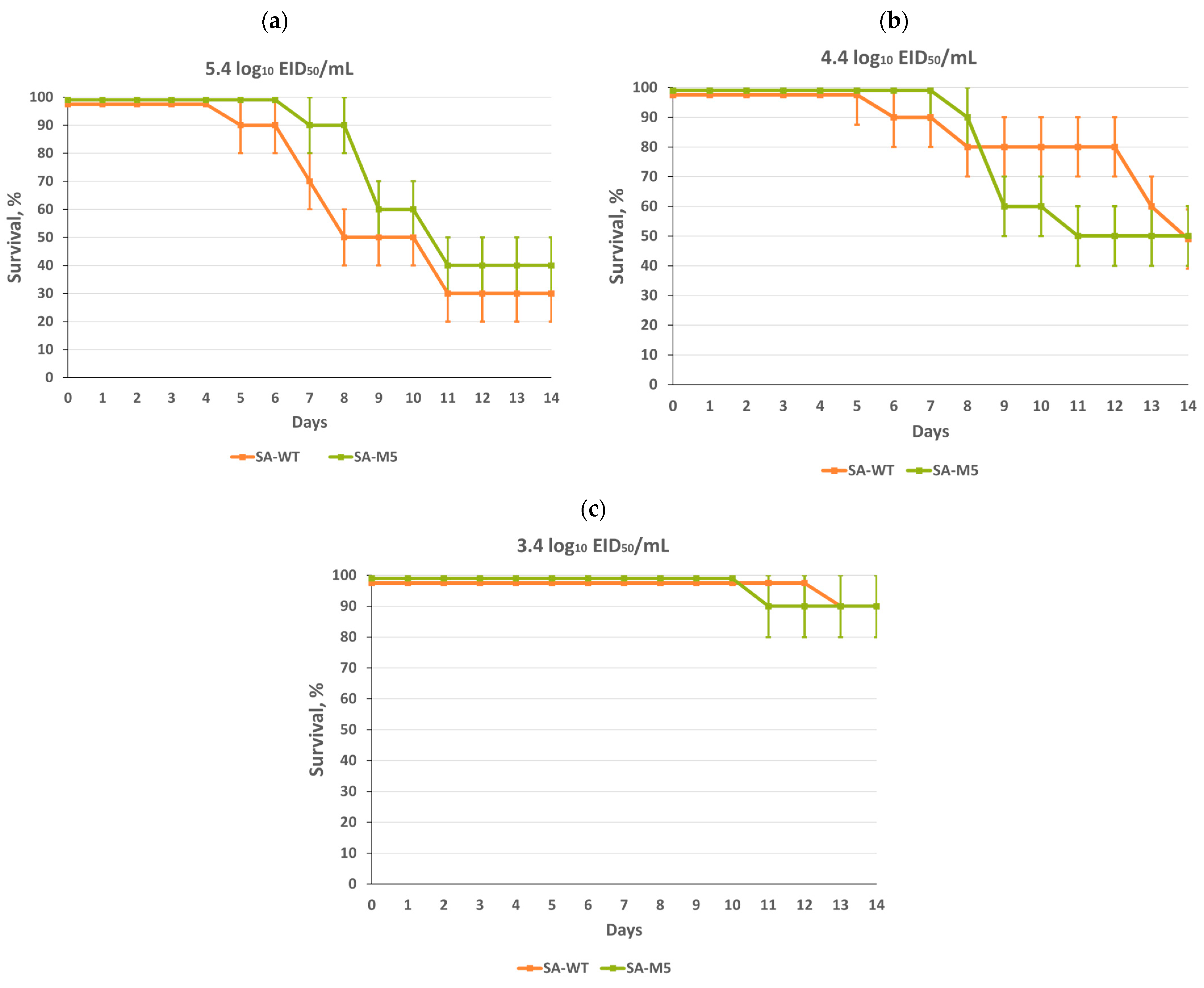
2.4. SA-WT and SA-M5 Pathogenicity in Mice
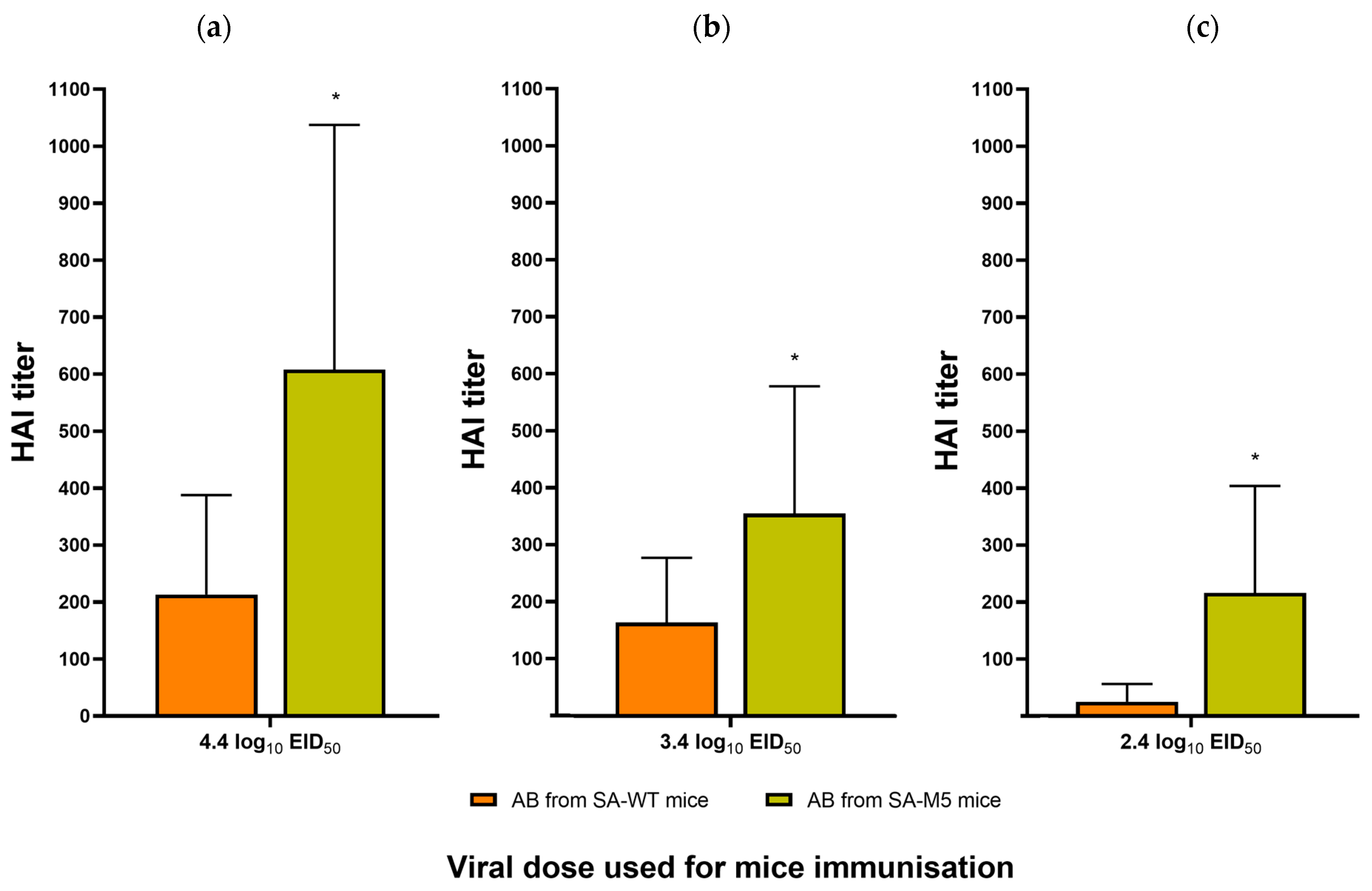
2.5. SA-WT and SA-M5 Immunogenicity
3. Discussion
4. Materials and Methods
4.1. Viruses
4.2. Mice
4.3. Virus Adaptation to Mice
4.4. Viral Replication in Lung Tissue
4.5. Viral Genome Sequencing
4.6. Toxicity in Mice
4.7. Pathogenicity in Mice
4.8. Hemagglutination Inhibition Test
4.9. 3D Structure
4.10. Ethics Statement
4.11. Statistics
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Estimating Disease Burden of Influenza. Available online: https://www.who.int/europe/activities/estimating-disease-burden-of-influenza (accessed on 22 October 2023).
- Shao, W.; Li, X.; Goraya, M.U.; Wang, S.; Chen, J.-L. Evolution of Influenza A Virus by Mutation and Re-Assortment. Int. J. Mol. Sci. 2017, 18, 1650. [Google Scholar] [CrossRef]
- Tosh, P.K.; Jacobson, R.M.; Poland, G.A. Influenza Vaccines: From Surveillance Through Production to Protection. Mayo Clin. Proc. 2010, 85, 257–273. [Google Scholar] [CrossRef] [PubMed]
- Lampejo, T. Influenza and Antiviral Resistance: An Overview. Eur. J. Clin. Microbiol. Infect. Dis. Off. Publ. Eur. Soc. Clin. Microbiol. 2020, 39, 1201–1208. [Google Scholar] [CrossRef] [PubMed]
- Dadonaite, B.; Gilbertson, B.; Knight, M.L.; Trifkovic, S.; Rockman, S.; Laederach, A.; Brown, L.E.; Fodor, E.; Bauer, D.L.V. The Structure of the Influenza A Virus Genome. Nat. Microbiol. 2019, 4, 1781–1789. [Google Scholar] [CrossRef] [PubMed]
- Kiseleva, I.; Rekstin, A.; Al Farroukh, M.; Bazhenova, E.; Katelnikova, A.; Puchkova, L.; Rudenko, L. Non-Mouse-Adapted H1N1pdm09 Virus as a Model for Influenza Research. Viruses 2020, 12, 590. [Google Scholar] [CrossRef] [PubMed]
- Al Farroukh, M.; Kiseleva, I.; Bazhenova, E.; Stepanova, E.; Puchkova, L.; Rudenko, L. Understanding the Variability of Certain Biological Properties of H1N1pdm09 Influenza Viruses. Vaccines 2022, 10, 395. [Google Scholar] [CrossRef] [PubMed]
- Bouvier, N.M.; Palese, P. The biology of influenza viruses. Vaccine 2008, 26, D49–D53. [Google Scholar] [CrossRef]
- Cox, N.J.; Kitame, F.; Kendal, A.P.; Maassab, H.F.; Naeve, C. Identification of Sequence Changes in the Cold-Adapted, Live Attenuated Influenza Vaccine Strain, A/Ann Arbor/6/60 (H2N2). Virology 1988, 167, 554–567. [Google Scholar] [CrossRef]
- Massin, P.; van der Werf, S.; Naffakh, N. Residue 627 of PB2 Is a Determinant of Cold Sensitivity in RNA Replication of Avian Influenza Viruses. J. Virol. 2001, 75, 5398–5404. [Google Scholar] [CrossRef]
- McCauley, J.W.; Penn, C.R. The Critical Cut-off Temperature of Avian Influenza Viruses. Virus Res. 1990, 17, 191–198. [Google Scholar] [CrossRef]
- Reed, L.J.; Muench, H. A simple method of estimating fifty per cent endpoints. Am. J. Epidemiol. 1938, 27, 493–497. [Google Scholar] [CrossRef]
- Sugiyama, K.; Obayashi, E.; Kawaguchi, A.; Suzuki, Y.; Tame, J.R.H.; Nagata, K.; Park, S.-Y. Structural Insight into the Essential PB1–PB2 Subunit Contact of the Influenza Virus RNA Polymerase. EMBO J. 2009, 28, 1803–1811. [Google Scholar] [CrossRef] [PubMed]
- Pflug, A.; Guilligay, D.; Reich, S.; Cusack, S. Structure of Influenza A Polymerase Bound to the Viral RNA Promoter. Nature 2014, 516, 355–360. [Google Scholar] [CrossRef] [PubMed]
- Isakova-Sivak, I.; Stepanova, E.; Mezhenskaya, D.; Matyushenko, V.; Prokopenko, P.; Sychev, I.; Wong, P.-F.; Rudenko, L. Influenza Vaccine: Progress in a Vaccine That Elicits a Broad Immune Response. Expert Rev. Vaccines 2021, 20, 1097–1112. [Google Scholar] [CrossRef] [PubMed]
- Kamal, R.P.; Katz, J.M.; York, I.A. Molecular Determinants of Influenza Virus Pathogenesis in Mice. Curr. Top. Microbiol. Immunol. 2014, 385, 243–274. [Google Scholar] [CrossRef]
- Hirst, G.K. Studies on the mechanism of adaptation of influenza virus to mice. J. Exp. Med. 1947, 86, 357–366. [Google Scholar] [CrossRef]
- Sriwilaijaroen, N.; Suzuki, Y. Molecular Basis of the Structure and Function of H1 Hemagglutinin of Influenza Virus. Proc. Jpn. Acad. Ser. B 2012, 88, 226–249. [Google Scholar] [CrossRef]
- Zhu, R.; Xu, S.; Sun, W.; Li, Q.; Wang, S.; Shi, H.; Liu, X. HA Gene Amino Acid Mutations Contribute to Antigenic Variation and Immune Escape of H9N2 Influenza Virus. Vet. Res. 2022, 53, 43. [Google Scholar] [CrossRef]
- Ilyushina, N.A.; Komatsu, T.E.; Ince, W.L.; Donaldson, E.F.; Lee, N.; O’Rear, J.J.; Donnelly, R.P. Influenza A Virus Hemagglutinin Mutations Associated with Use of Neuraminidase Inhibitors Correlate with Decreased Inhibition by Anti-Influenza Antibodies. Virol. J. 2019, 16, 149. [Google Scholar] [CrossRef]
- Chen, Y.; Bai, T.; Zhu, W.; Gao, R.; Deng, Z.; Shi, Y.; Zou, S.; Huang, Y.; Li, X.; Li, F.; et al. The S190R Mutation in the Hemagglutinin Protein of Pandemic H1N1 2009 Influenza Virus Increased Its Pathogenicity in Mice. Sci. China Life Sci. 2018, 61, 836–843. [Google Scholar] [CrossRef]
- Nicolson, C.; Harvey, R.; Engelhardt, O.G.; Robertson, J.S. The Ability of a Non-Egg Adapted (Cell-Like) A(H1N1)Pdm09 Virus to Egg-Adapt at HA Loci Other than 222 and 223 and Its Effect on the Yield of Viral Protein. PLoS ONE 2016, 11, e0166761. [Google Scholar] [CrossRef] [PubMed]
- Matyushenko, V.; Isakova-Sivak, I.; Smolonogina, T.; Dubrovina, I.; Tretiak, T.; Rudenko, L. Genotyping Assay for Differentiation of Wild-Type and Vaccine Viruses in Subjects Immunized with Live Attenuated Influenza Vaccine. PLoS ONE 2017, 12, e0180497. [Google Scholar] [CrossRef] [PubMed]
- Deng, Y.-M.; Caldwell, N.; Barr, I.G. Rapid Detection and Subtyping of Human Influenza A Viruses and Reassortants by Pyrosequencing. PLoS ONE 2011, 6, e23400. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, E.; Stech, J.; Guan, Y.; Webster, R.G.; Perez, D.R. Universal Primer Set for the Full-Length Amplification of All Influenza A Viruses. Arch. Virol. 2001, 146, 2275–2289. [Google Scholar] [CrossRef]
- Manual for the Laboratory Diagnosis and Virological Surveillance of Influenza. Available online: https://www.who.int/publications-detail-redirect/manual-for-the-laboratory-diagnosis-and-virological-surveillance-of-influenza (accessed on 22 October 2023).
- Klimov, A.; Balish, A.; Veguilla, V.; Sun, H.; Schiffer, J.; Lu, X.; Katz, J.M.; Hancock, K. Influenza Virus Titration, Antigenic Characterization, and Serological Methods for Antibody Detection. In Influenza Virus: Methods and Protocols; Kawaoka, Y., Neumann, G., Eds.; Methods in Molecular Biology; Humana Press: Totowa, NJ, USA, 2012; pp. 25–51. ISBN 978-1-61779-621-0. [Google Scholar]
- Directive 2010/63/EU of the European Parliament and of the Council of 22 September 2010 on the Protection of Animals Used for Scientific Purposes Text with EEA Relevance; 2010; Volume 276. Available online: https://eur-lex.europa.eu/legal-content/EN/TXT/?uri=celex%3A32010L0063 (accessed on 9 December 2023).

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al Farroukh, M.; Kiseleva, I.; Stepanova, E.; Bazhenova, E.; Krutikova, E.; Tkachev, A.; Chistyakova, A.; Rekstin, A.; Puchkova, L.; Rudenko, L. The Effect of Mice Adaptation Process on the Pathogenicity of Influenza A/South Africa/3626/2013 (H1N1)pdm09 Model Strain. Int. J. Mol. Sci. 2023, 24, 17386. https://doi.org/10.3390/ijms242417386
Al Farroukh M, Kiseleva I, Stepanova E, Bazhenova E, Krutikova E, Tkachev A, Chistyakova A, Rekstin A, Puchkova L, Rudenko L. The Effect of Mice Adaptation Process on the Pathogenicity of Influenza A/South Africa/3626/2013 (H1N1)pdm09 Model Strain. International Journal of Molecular Sciences. 2023; 24(24):17386. https://doi.org/10.3390/ijms242417386
Chicago/Turabian StyleAl Farroukh, Mohammad, Irina Kiseleva, Ekaterina Stepanova, Ekaterina Bazhenova, Elena Krutikova, Artem Tkachev, Anna Chistyakova, Andrey Rekstin, Ludmila Puchkova, and Larisa Rudenko. 2023. "The Effect of Mice Adaptation Process on the Pathogenicity of Influenza A/South Africa/3626/2013 (H1N1)pdm09 Model Strain" International Journal of Molecular Sciences 24, no. 24: 17386. https://doi.org/10.3390/ijms242417386
APA StyleAl Farroukh, M., Kiseleva, I., Stepanova, E., Bazhenova, E., Krutikova, E., Tkachev, A., Chistyakova, A., Rekstin, A., Puchkova, L., & Rudenko, L. (2023). The Effect of Mice Adaptation Process on the Pathogenicity of Influenza A/South Africa/3626/2013 (H1N1)pdm09 Model Strain. International Journal of Molecular Sciences, 24(24), 17386. https://doi.org/10.3390/ijms242417386






