Upregulation in Inflammation and Collagen Expression in Perirenal but Not in Mesenteric Adipose Tissue from Diabetic Munich Wistar Frömter Rats
Abstract
1. Introduction
2. Results
2.1. MWF-D Showed an Increase in Body Weight and Adiposity after Treatment
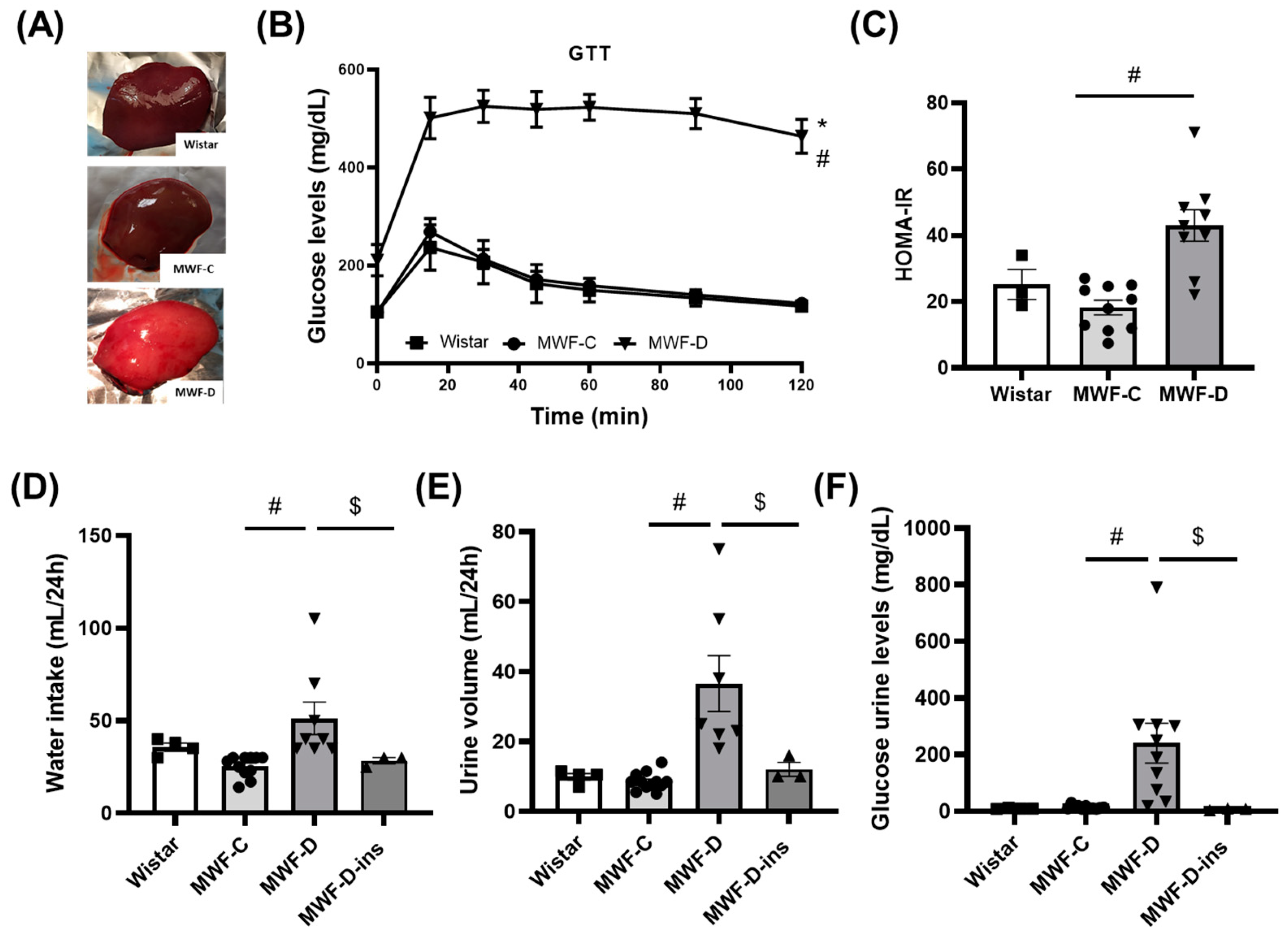
2.2. MWF-D Developed Hyperglycemia, Glucose Intolerance, Insulin Resistance, Polydipsia, and Polyuria
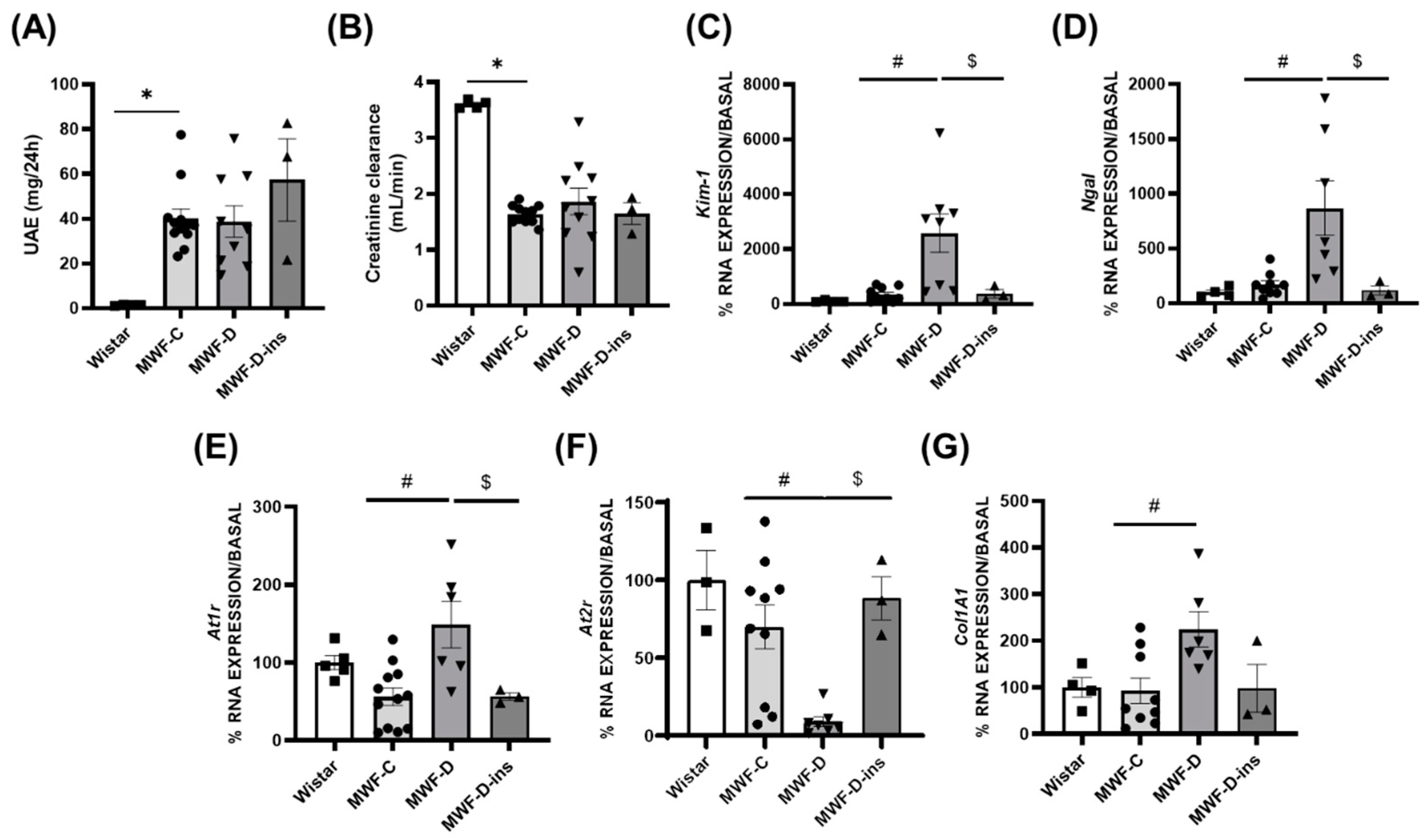
2.3. MWF-D Exhibited a Worsening in Kidney Damage
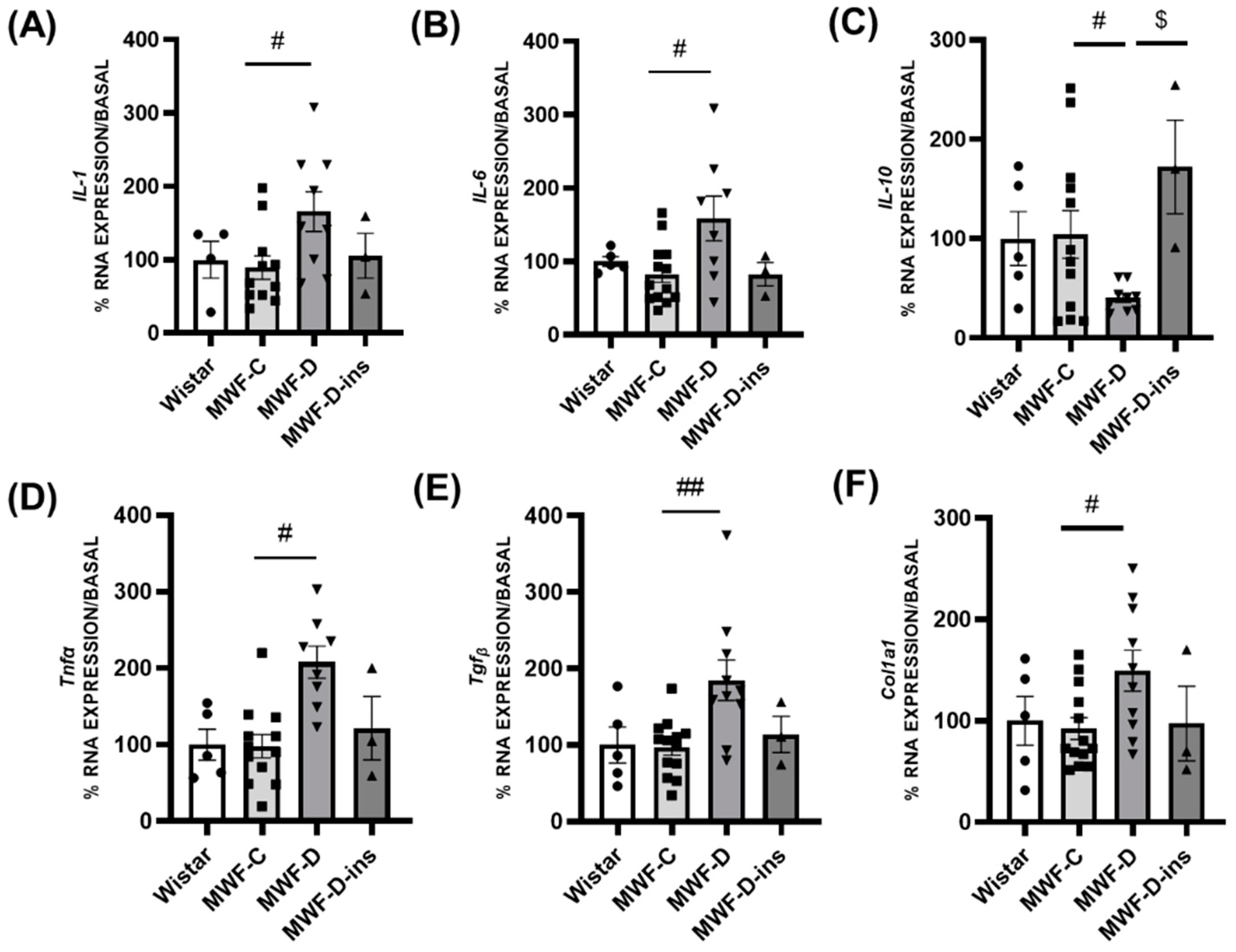
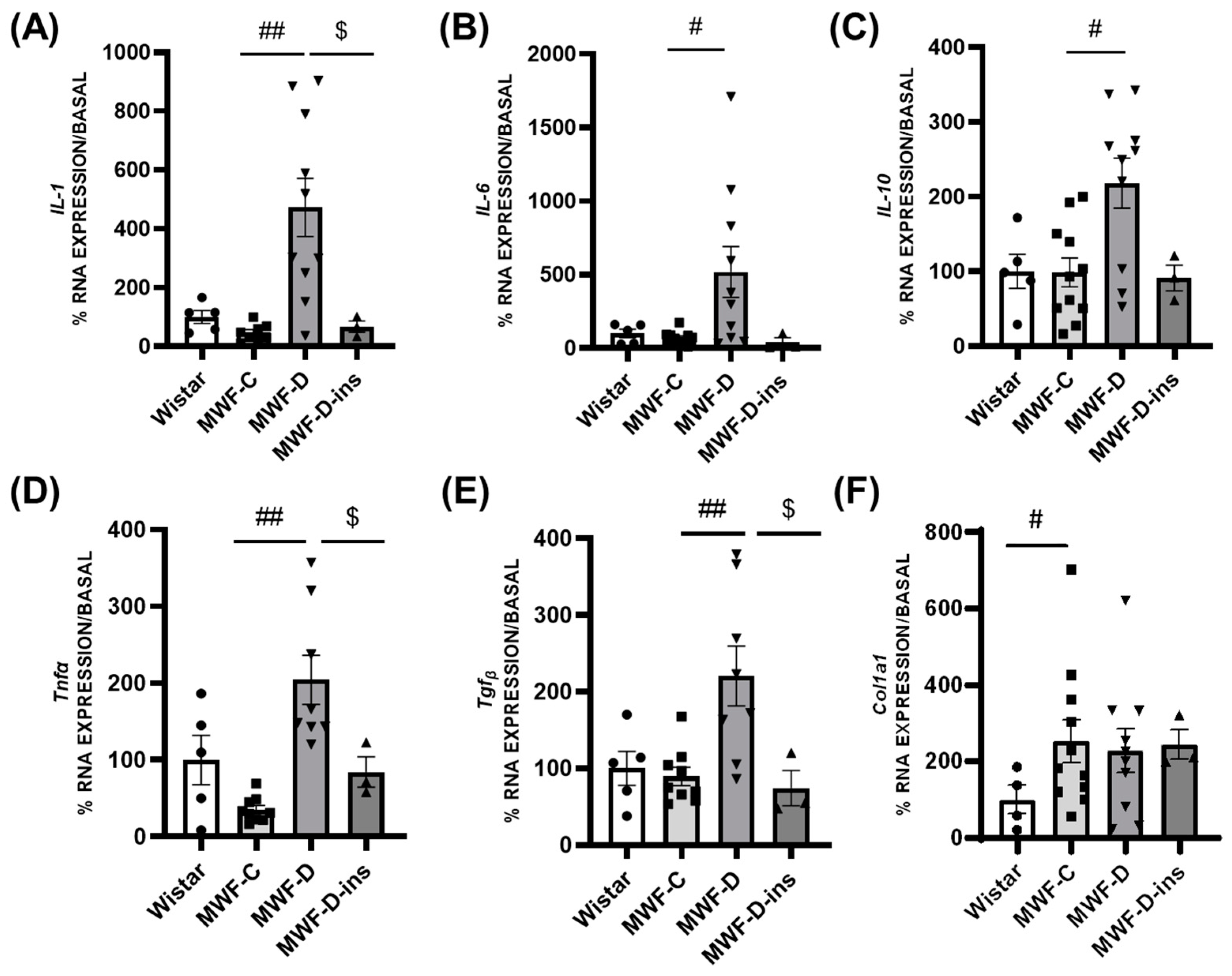
2.4. Expression of Inflammatory and Profibrotic Factors in PRAT and MAT
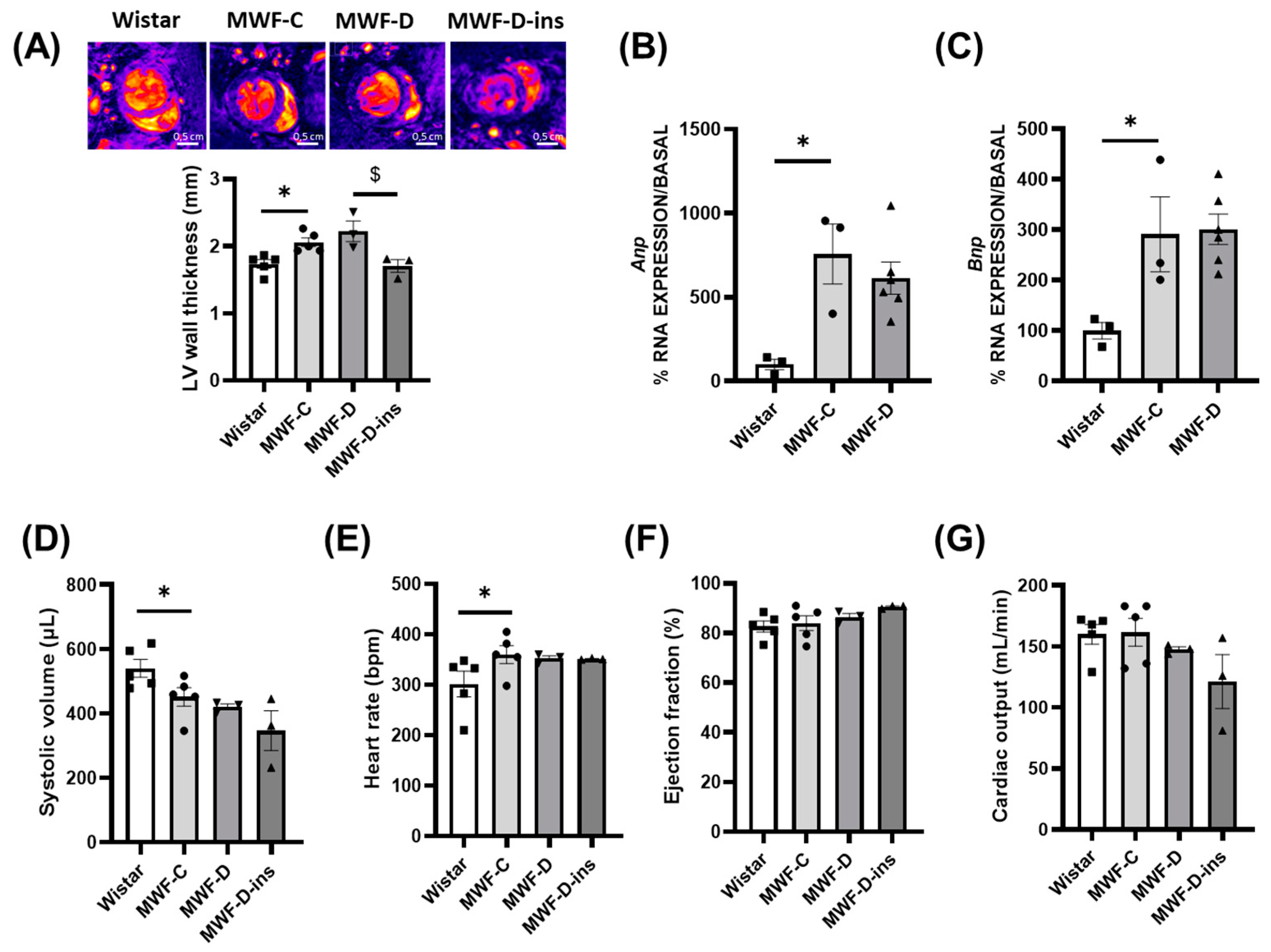
2.5. Hemodynamic and Cardiac Parameters in MWF-D
3. Discussion
4. Material and Methods
4.1. Animals and Diabetes Induction
4.2. Glucose Determination and Intraperitoneal Glucose Tolerance Test (GTT)
4.3. Determination of Urinary Albumin Excretion and Hemodynamic Parameters
4.4. Acquisition and Analysis of Cardiac Structure and Function by Magnetic Resonance Imaging
4.5. RNA Extraction and Real-Time PCR (RT-qPCR)
4.6. Statistical Analysis
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Mortality and Global Health Estimates: Causes of Death; Projections for 2015–2030; Projection of Death Rates. Available online: http://apps.who.int/gho/data/node.main.PROJRATEWORLD?lang=en (accessed on 13 September 2022).
- GBD Chronic Kidney Disease Collaboration; Bikbov, B.; Purcell, C.A.; Levey, A.S.; Smith, M.; Abdoli, A.; Abebe, M.; Adebayo, O.M.; Afarideh, M.; Agarwal, S.K.; et al. Global, regional, and national burden of chronic kidney disease, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2020, 395, 709–733. [Google Scholar] [CrossRef] [PubMed]
- Sundström, J.; Bodegard, J.; Bollmann, A.; Vervloet, M.G.; Mark, P.B.; Karasik, A.; Taveira-Gomes, T.; Botana, M.; Birkeland, K.I.; Thuresson, M.; et al. Prevalence, outcomes, and cost of chronic kidney disease in a contemporary population of 2·4 million patients from 11 countries: The CaReMe CKD study. Lancet Reg. Health Eur. 2022, 20, 100438. [Google Scholar] [CrossRef]
- International Diabetes Federation IDF Diabetes Atlas 2022 Reports. Available online: https://diabetesatlas.org/resources/?gclid=Cj0KCQiAgqGrBhDtARIsAM5s0_l-b1g1jVD7YBsY1G8c3K_sB9suyDCI8X5Mm62mfkRKAXsUGkICIyMaAoTzEALw_wcB (accessed on 10 September 2023).
- Blacher, J.; Guerin, A.P.; Pannier, B.; Marchais, S.J.; Safar, M.E.; London, G.M. Impact of aortic stiffness on survival in end-stage renal disease. Circulation 1999, 99, 2434–2439. [Google Scholar] [CrossRef] [PubMed]
- Zanoli, L.; Lentini, P.; Briet, M.; Castellino, P.; House, A.A.; London, G.M.; Malatino, L.; McCullough, P.A.; Mikhailidis, D.P.; Boutouyrie, P. Arterial Stiffness in the Heart Disease of CKD. J. Am. Soc. Nephrol. 2019, 30, 918–928. [Google Scholar] [CrossRef]
- Navaneethan, S.D.; Schold, J.D.; Jolly, S.E.; Arrigain, S.; Winkelmayer, W.C.; Nally, J.V., Jr. Diabetes control and the risks of ESRD and mortality in patients with CKD. Am. J. Kidney Dis. 2017, 70, 191–198. [Google Scholar] [CrossRef] [PubMed]
- Anders, H.J.; Huber, T.B.; Isermann, B.; Schiffer, M. CKD in diabetes: Diabetic kidney disease versus nondiabetic kidney disease. Nat. Rev. Nephrol. 2018, 14, 361–377. [Google Scholar] [CrossRef] [PubMed]
- Favre, G.; Grangeon-Chapon, C.; Raffaellim, C.; François-Chalmin, F.; Iannelli, A.; Esnault, V. Perirenal fat thickness measured with computed tomography is a reliable estimate of perirenal fat mass. PLoS ONE 2017, 12, e0175561. [Google Scholar] [CrossRef]
- Geraci, G.; Zammuto, M.M.; Mattina, A.; Zanoli, L.; Geraci, C.; Granata, A.; Nardi, E.; Fatuzzo, P.M.; Cottone, S.; Mulè, G. Para-perirenal distribution of body fat is associated with reduced glomerular filtration rate regardless of other indices of adiposity in hypertensive patients. J. Clin. Hypertens. 2018, 20, 1438–1446. [Google Scholar] [CrossRef]
- Sun, X.; Han, F.; Miao, W.; Hou, N.; Cao, Z.; Zhang, G. Sonographic evaluation of para- and perirenal fat thickness is an independent predictor of early kidney damage in obese patients. Int. Urol. Nephrol. 2013, 45, 1589–1595. [Google Scholar] [CrossRef]
- Lamacchia, O.; Nicastro, V.; Camarchio, D.; Valente, U.; Grisorio, R.; Gesualdo, L.; Cignarelli, M. Para- and perirenal fat thickness is an independent predictor of chronic kidney disease, increased renal resistance index and hyperuricaemia in type-2 diabetic patients. Nephrol. Dial. Transplant. 2011, 26, 892–898. [Google Scholar] [CrossRef]
- Fang, Y.; Xu, Y.; Yang, Y.; Liu, C.; Zhao, D.; Ke, J. The relationship between perirenal fat thickness and reduced glomerular filtration rate in patients with type 2 diabetes. J. Diabetes Res. 2020, 2020, 6076145. [Google Scholar] [CrossRef]
- Chen, X.; Mao, Y.; Hu, J.; Han, S.; Gong, L.; Luo, T.; Yang, S.; Qing, H.; Wang, Y.; Du, Z.; et al. Perirenal Fat Thickness Is Significantly Associated With the Risk for Development of Chronic Kidney Disease in Patients With Diabetes. Diabetes 2021, 70, 2322–2332. [Google Scholar] [CrossRef] [PubMed]
- Shen, F.C.; Cheng, B.C.; Chen, J.F. Peri-renal fat thickness is positively associated with the urine albumin excretion rate in patients with type 2 diabetes. Obes. Res. Clin. Pract. 2020, 14, 345–349. [Google Scholar] [CrossRef] [PubMed]
- D’Marco, L. Perirenal fat thickness is associated with metabolic risk factors in patients with chronic kidney disease. Kidney Res. Clin. Pract. 2019, 38, 365–372. [Google Scholar] [CrossRef] [PubMed]
- Mahabadi, A.A.; Massaro, J.M.; Rosito, G.A.; Levy, D.; Murabito, J.M.; Wolf, P.A.; O’Donnell, C.J.; Fox, C.S.; Hoffmann, U. Association of pericardial fat, intrathoracic fat, and visceral abdominal fat with cardiovascular disease burden: The Framingham Heart Study. Eur. Heart J. 2009, 30, 850–856. [Google Scholar] [CrossRef] [PubMed]
- Liu, B.X.; Sun, W.; Kong, X.Q. Perirenal fat: A unique fat pad and potential target for cardiovascular disease. Angiology 2019, 70, 584–593. [Google Scholar] [CrossRef] [PubMed]
- Hammoud, S.H.; AlZaim, I.; Al-Dhaheri, Y.; Eid, A.H.; El-Yazbi, A.F. Perirenal Adipose Tissue Inflammation: Novel Insights Linking Metabolic Dysfunction to Renal Diseases. Front. Endocrinol. 2021, 12, 707126. [Google Scholar] [CrossRef]
- Pulido-Olmo, H.; García-Prieto, C.F.; Álvarez-Llamas, G.; Barderas, M.G.; Vivanco, F.; Aranguez, I.; Somoza, B.; Segura, J.; Kreutz, R.; Fernández-Alfonso, M.S.; et al. Role of matrix metalloproteinase-9 in chronic kidney disease: A new biomarker of resistant albuminuria. Clin. Sci. 2016, 130, 525–538. [Google Scholar] [CrossRef]
- Manzano-Lista, F.J.; Sanz-Gómez, M.; González-Moreno, D.; Vega-Martín, E.; Gil-Ortega, M.; Schulz, A.; Rubio, M.Á.; Ruiz-Hurtado, G.; Ruilope, L.M.; Aránguez, I.; et al. Imbalance in Bone Morphogenic Proteins 2 and 7 Is Associated with Renal and Cardiovascular Damage in Chronic Kidney Disease. Int. J. Mol. Sci. 2022, 24, 40. [Google Scholar] [CrossRef]
- Gil-Ortega, M.; García-Prieto, C.F.; Ruiz-Hurtado, G.; Steireif, C.; González, M.C.; Schulz, A.; Kreutz, R.; Fernández-Alfonso, M.S.; Arribas, S.; Somoza, B. Genetic predisposition to albuminuria is associated with increased arterial stiffness: Role of elastin. Br. J. Pharmacol. 2015, 172, 4406–4418. [Google Scholar] [CrossRef]
- Gil-Ortega, M.; Vega-Martín, E.; Martín-Ramos, M.; González-Blázquez, R.; Pulido-Olmo, H.; Ruiz-Hurtado, G.; Schulz, A.; Ruilope, L.M.; Kolkhof, P.; Somoza, B.; et al. Finerenone Reduces Intrinsic Arterial Stiffness in Munich Wistar Frömter Rats, a Genetic Model of Chronic Kidney Disease. Am. J. Nephrol. 2020, 51, 294–303. [Google Scholar] [CrossRef]
- González-Blázquez, R.; Somoza, B.; Gil-Ortega, M.; Martín Ramos, M.; Ramiro-Cortijo, D.; Vega-Martín, E.; Schulz, A.; Ruilope, L.M.; Kolkhof, P.; Kreutz, R.; et al. Finerenone Attenuates Endothelial Dysfunction and Albuminuria in a Chronic Kidney Disease Model by a Reduction in Oxidative Stress. Front. Pharmacol. 2018, 9, 1131. [Google Scholar] [CrossRef]
- Gschwend, S.; Pinto-Sietsma, S.J.; Buikema, H.; Pinto, Y.M.; Van Gilst, W.H.; Schulz, A.; Kreutz, R. Impaired coronary endothelial function in a rat model of spontaneous albuminuria. Kidney Int. 2002, 62, 181–191. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Steireif, C.; García-Prieto, C.F.; Ruiz-Hurtado, G.; Pulido-Olmo, H.; Aranguez, I.; Gil-Ortega, M.; Somoza, B.; Schönfelder, G.; Schulz, A.; Fernández-Alfonso, M.S.; et al. Dissecting the genetic predisposition to albuminuria and endothelial dysfunction in a genetic rat model. J. Hypertens. 2013, 31, 2203–2212. [Google Scholar] [CrossRef]
- Herlan, L.; Unland, J.; Langer, S.; Schulte, L.; Schütten, S.; García-Prieto, C.F.; Kossmehl, P.; Fernández-Alfonso, M.S.; Schulz, A.; Kreutz, R. Development of progressive albuminuria in male Munich Wistar Frömter rats is androgen dependent. Physiol. Genom. 2015, 47, 281–289. [Google Scholar] [CrossRef] [PubMed]
- Skovsø, S. Modeling type 2 diabetes in rats using high fat diet and streptozotocin. J. Diabetes Investig. 2014, 5, 349–358. [Google Scholar] [CrossRef]
- Parilla, J.H.; Willard, J.R.; Barrow, B.M.; Zraika, S. A Mouse Model of Beta-Cell Dysfunction as Seen in Human Type 2 Diabetes. J. Diabetes Res. 2018, 30, 6106051. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Li, G.; Zhang, F. Identification of variations of gene expression of visceral adipose and renal tissue in type 2 diabetic rats using cDNA representational difference analysis. Chin. Med. J. 2003, 116, 529–533. [Google Scholar] [PubMed]
- Zhang, F.; Ye, C.; Li, G.; Ding, W.; Zhou, W.; Zhu, H.; Chen, G.; Luo, T.; Guang, M.; Liu, Y.; et al. The rat model of type 2 diabetic 2mellitus and its glycometabolism characters. Exp. Anim. 2003, 52, 401–407. [Google Scholar] [CrossRef]
- Gao, L.; Niu, Y.; Liu, W.; Xie, M.; Liu, X.; Chen, Z.; Li, L. The antilipolytic action of bis(alpha-furancarboxylato) oxovanadium (IV) in adipocytes. Clin. Chim. Acta. 2008, 388, 89–94. [Google Scholar] [CrossRef]
- Hou, L.; Lian, K.; Yao, M.; Shi, Y.; Lu, X.; Fang, L.; He, T.; Jiang, L. Reduction of n-3 PUFAs, specifically DHA and EPA, and enhancement of peroxisomal beta-oxidation in type 2 diabetic rat heart. Cardiovasc. Diabetol. 2012, 11, 126. [Google Scholar] [CrossRef] [PubMed]
- Zhang, T.; Pan, B.S.; Zhao, B.; Zhang, L.M.; Huang, Y.L.; Sun, F.Y. Exacerbation of poststroke dementia by type 2 diabetes is associated with synergistic increases of beta-secretase activation and beta-amyloid generation in rat brains. Neuroscience 2009, 161, 1045–1056. [Google Scholar] [CrossRef]
- Zou, F.; Mao, X.Q.; Wang, N.; Liu, J.; Ou-Yang, J.P. Astragalus polysaccharides alleviates glucose toxicity and restores glucose homeostasis in diabetic states via activation of AMPK. Acta Pharmacol. Sin. 2009, 30, 1607–1615. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M.; Lv, X.Y.; Li, J.; Xu, Z.G.; Chen, L. The characterization of high-fat diet and multiple low-dose streptozotocin induced type 2 diabetes rat model. Exp. Diabetes Res. 2008, 2008, 704045. [Google Scholar] [CrossRef] [PubMed]
- Guo, Z.; Zheng, C.; Qin, Z.; Wei, P. Effect of telmisartan on the expression of cardiac adiponectin and its receptor 1 in type 2 diabetic rats. J. Pharm. Pharmacol. 2011, 63, 87–94. [Google Scholar] [CrossRef] [PubMed]
- Guo, Z.; Zhang, R.; Li, J.; Xu, G. Effect of telmisartan on the expression of adiponectin receptors and nicotinamide adenine dinucleotide phosphate oxidase in the heart and aorta in type 2 diabetic rats. Cardiovasc. Diabetol. 2012, 11, 94. [Google Scholar] [CrossRef]
- Ma, C.; Long, H. Protective effect of betulin on cognitive decline in streptozotocin (STZ)-induced diabetic rats. Neurotoxicology 2016, 57, 104–111. [Google Scholar] [CrossRef]
- Lu, H.E.; Jian, C.H.; Chen, S.F.; Chen, T.M.; Lee, S.T.; Chang, C.S.; Weng, C.F. Hypoglycaemic effects of fermented mycelium of Paecilomyces farinosus (G30801) on high-fat fed rats with streptozotocin-induced diabetes. Indian J. Med. Res. 2010, 131, 696–701. [Google Scholar]
- Ren, Z.; Li, W.; Zhao, Q.; Ma, L.; Zhu, J. The impact of 1,25-dihydroxy vitamin D3 on the expressions of vascular endothelial growth factor and transforming growth factor-β1 in the retinas of rats with diabetes. Diabetes Res. Clin. Pract. 2012, 98, 474–480. [Google Scholar] [CrossRef]
- Albersen, M.; Lin, G.; Fandel, T.M.; Zhang, H.; Qiu, X.; Lin, C.S.; Lue, T.F. Functional, metabolic, and morphologic characteristics of a novel rat model of type 2 diabetes-associated erectile dysfunction. Urology 2011, 78, 476.e1–476.e8. [Google Scholar] [CrossRef]
- Reed, M.J.; Meszaros, K.; Entes, L.J.; Claypool, M.D.; Pinkett, J.G.; Gadbois, T.M.; Reaven, G.M. A new rat model of type 2 diabetes: The fat-fed, streptozotocin-treated rat. Metabolism 2000, 49, 1390–1394. [Google Scholar] [CrossRef] [PubMed]
- Srinivasan, K.; Viswanad, B.; Asrat, L.; Kaul, C.L.; Ramarao, P. Combination of high-fat diet-fed and low-dose streptozotocin-treated rat: A model for type 2 diabetes and pharmacological screening. Pharmacol. Res. 2005, 52, 313–320. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.; Sohn, S.; Lee, M.; Jung, J.; Kineman, R.D.; Park, S. Differential responses of the growth hormone axis in two rat models of streptozotocin-induced insulinopenic diabetes. J. Endocrinol. 2006, 188, 263–270. [Google Scholar] [CrossRef]
- Ravussin, E.; Smith, S.R. Increased fat intake, impaired fat oxidation, and failure of fat cell proliferation result in ectopic fat storage, insulin resistance, and type 2 diabetes mellitus. Ann. N. Y. Acad. Sci. 2002, 967, 363–378. [Google Scholar] [CrossRef] [PubMed]
- Acheson, K.J.; Schutz, Y.; Bessard, T.; Anantharaman, K.; Flatt, J.P.; Jéquier, E. Glycogen storage capacity and de novo lipogenesis during massive carbohydrate overfeeding in man. Am. J. Clin. Nutr. 1988, 48, 240–247. [Google Scholar] [CrossRef]
- de Vries, M.; Westerink, J.; Kaasjager, K.H.A.H.; de Valk, H.W. Prevalence of nonalcoholic fatty liver disease (nafld) in patients with type 1 diabetes mellitus: A systematic review and meta-analysis. J. Clin. Endocrinol. Metab. 2020, 105, 3842–3853. [Google Scholar] [CrossRef]
- Stenvinkel, P.; Ketteler, M.; Johnson, R.J.; Lindholm, B.; Pecoits-Filho, R.; Riella, M.; Heimbürger, O.; Cederholm, T.; Girndt, M. IL-10, IL-6, and TNF-alpha: Central factors in the altered cytokine network of uremia--the good, the bad, and the ugly. Kidney Int. 2005, 67, 1216–1233. [Google Scholar] [CrossRef]
- Biernacka, A.; Dobaczewski, M.; Frangogiannis, N.G. TGF-β signaling in fibrosis. Growth Factors 2011, 29, 196–202. [Google Scholar] [CrossRef]
- Eddy, A.A. Progression in chronic kidney disease. Adv. Chronic Kidney Dis. 2005, 12, 353–365. [Google Scholar] [CrossRef]
- Gao, X.; He, X.; Luo, B.; Peng, L.; Lin, J.; Zuo, Z. Angiotensin II increases collagen I expression via transforming growth factor-beta1 and extracellular signal-regulated kinase in cardiac fibroblasts. Eur. J. Pharmacol. 2009, 606, 115–120. [Google Scholar] [CrossRef]
- Wang, Y.; Del Borgo, M.; Lee, H.W.; Baraldi, D.; Hirmiz, B.; Gaspari, T.A.; Denton, K.M.; Aguilar, M.I.; Samuel, C.S.; Widdop, R.E. Anti-fibrotic Potential of AT2 Receptor Agonists. Front. Pharmacol. 2017, 8, 564. [Google Scholar] [CrossRef] [PubMed]
- Gil-Ortega, M.; Somoza, B.; Huang, Y.; Gollasch, M.; Fernández-Alfonso, M.S. Regional differences in perivascular adipose tissue impacting vascular homeostasis. Trends Endocrinol. Metab. 2015, 26, 367–375. [Google Scholar] [CrossRef] [PubMed]
- Percie du Sert, N.; Hurst, V.; Ahluwalia, A.; Alam, S.; Avey, M.T.; Baker, M.; Browne, W.J.; Clark, A.; Cuthill, I.C.; Dirnagl, U.; et al. The ARRIVE guidelines 2.0: Updated guidelines for reporting animal research. PLoS Biol. 2020, 18, e3000410. [Google Scholar]
- Mancia Chairperson, G.; Kreutz Co-Chair, R.; Brunström, M.; Burnier, M.; Grassi, G.; Januszewicz, A.; Muiesan, M.L.; Tsioufis, K.; Agabiti-Rosei, E.; Algharably, E.A.E.; et al. Authors/Task Force Members: 2023 ESH Guidelines for the management of arterial hypertension the Task Force for the management of arterial hypertension of the European Society of Hypertension Endorsed by the European Renal Association (ERA) and the International Society of Hypertension (ISH). J. Hypertens. 2023, 41, 1874–2071. [Google Scholar] [CrossRef]
- Wu, Y.; Ouyang, J.P.; Zhou, Y.F.; Wu, K.; Zhao, D.H.; Wen, C.Y. Mechanism of improving effect of losartan on insulin sensitivity of non-insulin-dependent diabetes mellitus rats. Sheng Li Xue Bao 2004, 56, 539–549. [Google Scholar]
- Nørgaard, S.A.; Søndergaard, H.; Sørensen, D.B.; Galsgaard, E.D.; Hess, C.; Sand, F.W. Optimising streptozotocin dosing to minimise renal toxicity and impairment of stomach emptying in male 129/Sv mice. Lab. Anim. 2020, 54, 341–352. [Google Scholar] [CrossRef]
- Pellicer-Valero, Ó.J.; Massaro, G.A.; Casanova, A.G.; Paniagua-Sancho, M.; Fuentes-Calvo, I.; Harvat, M.; Martín-Guerrero, J.D.; Martínez-Salgado, C.; López-Hernández, F.J. Neural Network-Based Calculator for Rat Glomerular Filtration Rate. Biomedicines 2023, 10, 610. [Google Scholar] [CrossRef]
| Wistar | MWF-C | MWF-D | |
|---|---|---|---|
| Final weight (g) | 557.4 ± 20.5 | 400.3 ± 9.6 * | 433.0 ± 4.4 # |
| Food intake (kcal/day) | 44.15 ± 2.4 | 47.95 ± 2.0 | 68.7 ± 6.8 # |
| PRAT weight/tibia length (g/mm) | 0.18 ± 0.02 | 0.09 ± 0.01 * | 0.15 ± 0.01 # |
| MAT weight/tibia length (g/mm) | 0.13 ± 0.02 | 0.07 ± 0.01 | 0.12 ± 0.01 # |
| Fasting glucose (mg/dL) | 130.5 ± 11.1 | 124.6 ± 3.9 | 243.0 ± 28.4 # |
| Post-prandrial glucose (mg/dL) | 291.8 ± 49.6 | 302.3 ± 24.7 | 481.2 ± 33.1 # |
| Fasting insulin (ng/mL) | 3.3 ± 0.3 | 2.6 ± 0.4 | 3.4 ± 0.4 |
| Post-prandrial insulin (ng/mL) | 8.3 ± 0.9 | 5.8 ± 0.3 * | 3.4 ± 0.4 # |
| Wistar | MWF-C | MWF-D | |
|---|---|---|---|
| SBP (mmHg) | 97.3 ± 5.6 | 146.2 ± 6.3 * | 147.6 ± 11.3 * |
| DBP (mmHg) | 71.16 ± 4.9 | 106.1 ± 4.8 * | 114.7 ± 10.1 * |
| PWV (m/s) | 5.9 ± 0.2 | 8.1 ± 0.5 * | 8.2 ± 0.8 * |
| Standard Chow (C) | High-Fat, High-Sucrose (HF/HS) Diet | |||
|---|---|---|---|---|
| Composition (%) | % kcal | Composition (%) | % kcal | |
| Fat of animal origin | 10 | 12 | 23 | 45 |
| Carbohydrate | 70 | 68 | 48 | 40 |
| Protein | 20 | 20 | 17 | 15 |
| Other | - | - | 20 | 3 |
| Gene | Accession Number | Forward (5′-3′) | Reverse (5′-3′) |
|---|---|---|---|
| Rn Kim-1 | NM_173149.2 | ATTGTTGCCGAGTGGAGAT | TGTGGTTGTGGGTCTTGTAGT |
| Rn Ngal | NM_130741.1 | GGCCGACACTGACTACGACC | GCCCCTTGGTTCTTCCGTAC |
| Rn At1r | NM_030985.4 | GTTGGGAGGGACTGGATGATGC | TGATCGGGTGGAACAGGACTCA |
| Rn At2r | NM_012494.4 | CCTCTGGAAAGCTGGCAAGTGT | TATTCGCTCTGTCCACTGGGGA |
| Rn Col1a1 | NM_053304.1 | GGATGCCATCAAGGTCTACTGC | TGAGTGGGGAACACACAGGTCT |
| Rn IL-1β | NM_031512.2 | TGACAGACCCCAAAAGATTAAGGA | CGAGATGCTGCTGTGAGATTTG |
| Rn IL-6 | NM_012589.2 | CCTGGAGTTTGTGAAGAACAACTT | TGGAAGGTGGGGTAGGAAGGAC |
| Rn IL-10 | NM_012854.2 | CAGTGGAGCAGGTGAAGAATGA | CATTCATGGCCTTGTAGACACC |
| Rn Tnf-α | NM_012675.3 | CTACTGAACTTCGGGGTGATCG | GGCTTGTCACTCGAGTTTTGAGA |
| Rn Tgf-β | NM_021578.2 | ATGGTGGACCGCAACAAC | CAGCAATGGGGGTTCTGG |
| Rn Anp | NM_012612.2 | ATACAGTGCGGTGTCCAACA | CGAGAGCACCTCCATCTCTC |
| Rn Bnp | NM_031545.1 | TCCTTAATCTGTCGCCGCTG | TTTTCTCTTATCAGCTCCAGCA |
| Rn Gapdh | NM_017008.4 | AAGGCTGAGAAATGGGAAGCTC | CCATTTGATGTTAGCGGGATCT |
| Rn Atpaf-1 | NM_001107959.1 | GATCTCTCCAAGAAGCTGCAAG | AAGATGACCCCAAGGCATTTTT |
| Rn Tbp | NM_001004198.1 | GACCCACCAGCAGTTCAGTAGC | CAATTCTGGGTTTGATCATTCTG |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vega-Martín, E.; González-Moreno, D.; Sanz-Gómez, M.; Guzmán-Aguayo, A.K.; Manzano-Lista, F.J.; Schulz, A.; Aránguez, I.; Kreutz, R.; Fernández-Alfonso, M.S. Upregulation in Inflammation and Collagen Expression in Perirenal but Not in Mesenteric Adipose Tissue from Diabetic Munich Wistar Frömter Rats. Int. J. Mol. Sci. 2023, 24, 17008. https://doi.org/10.3390/ijms242317008
Vega-Martín E, González-Moreno D, Sanz-Gómez M, Guzmán-Aguayo AK, Manzano-Lista FJ, Schulz A, Aránguez I, Kreutz R, Fernández-Alfonso MS. Upregulation in Inflammation and Collagen Expression in Perirenal but Not in Mesenteric Adipose Tissue from Diabetic Munich Wistar Frömter Rats. International Journal of Molecular Sciences. 2023; 24(23):17008. https://doi.org/10.3390/ijms242317008
Chicago/Turabian StyleVega-Martín, Elena, Daniel González-Moreno, Marta Sanz-Gómez, Ana Karen Guzmán-Aguayo, Francisco Javier Manzano-Lista, Angela Schulz, Isabel Aránguez, Reinhold Kreutz, and María S. Fernández-Alfonso. 2023. "Upregulation in Inflammation and Collagen Expression in Perirenal but Not in Mesenteric Adipose Tissue from Diabetic Munich Wistar Frömter Rats" International Journal of Molecular Sciences 24, no. 23: 17008. https://doi.org/10.3390/ijms242317008
APA StyleVega-Martín, E., González-Moreno, D., Sanz-Gómez, M., Guzmán-Aguayo, A. K., Manzano-Lista, F. J., Schulz, A., Aránguez, I., Kreutz, R., & Fernández-Alfonso, M. S. (2023). Upregulation in Inflammation and Collagen Expression in Perirenal but Not in Mesenteric Adipose Tissue from Diabetic Munich Wistar Frömter Rats. International Journal of Molecular Sciences, 24(23), 17008. https://doi.org/10.3390/ijms242317008






