Expression of Matrix Metalloproteinases in the Circulating Immune Cells in Children with Helicobacter pylori Infection—Correlation with Clinical Factors
Abstract
:1. Introduction
2. Results
2.1. Plasma Levels of MMPs and TIMP in Hp+, Hp- and Control Children
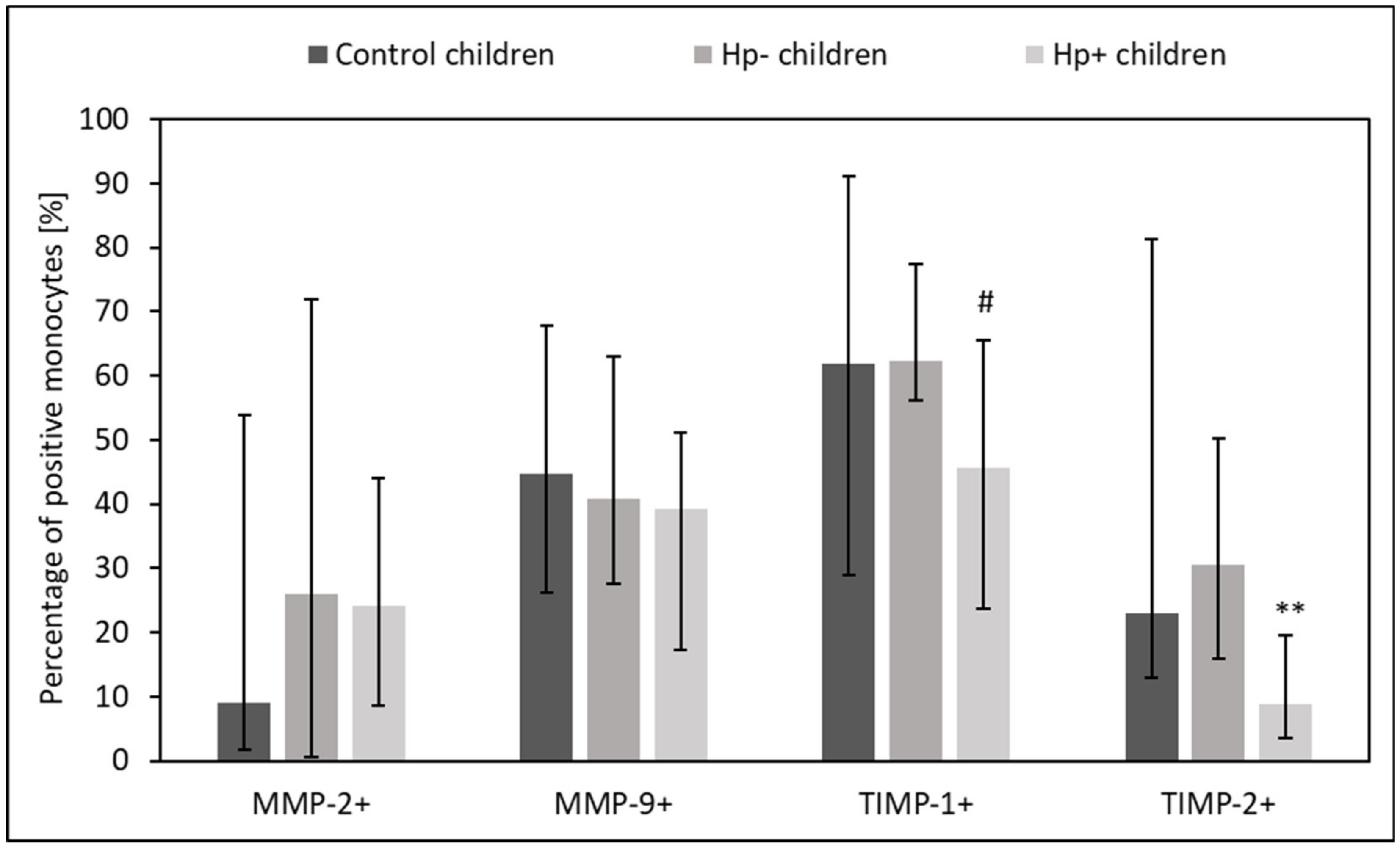
2.2. MMPs and TIMPs Expression in Circulating Lymphocytes, Monocytes, and Neutrophils from Hp+, Hp-, and Control Children
2.3. Evaluation of mRNA for MMPs and TIMP-1 in the Gastric Mucosa in Hp-+, Hp- and Control Children
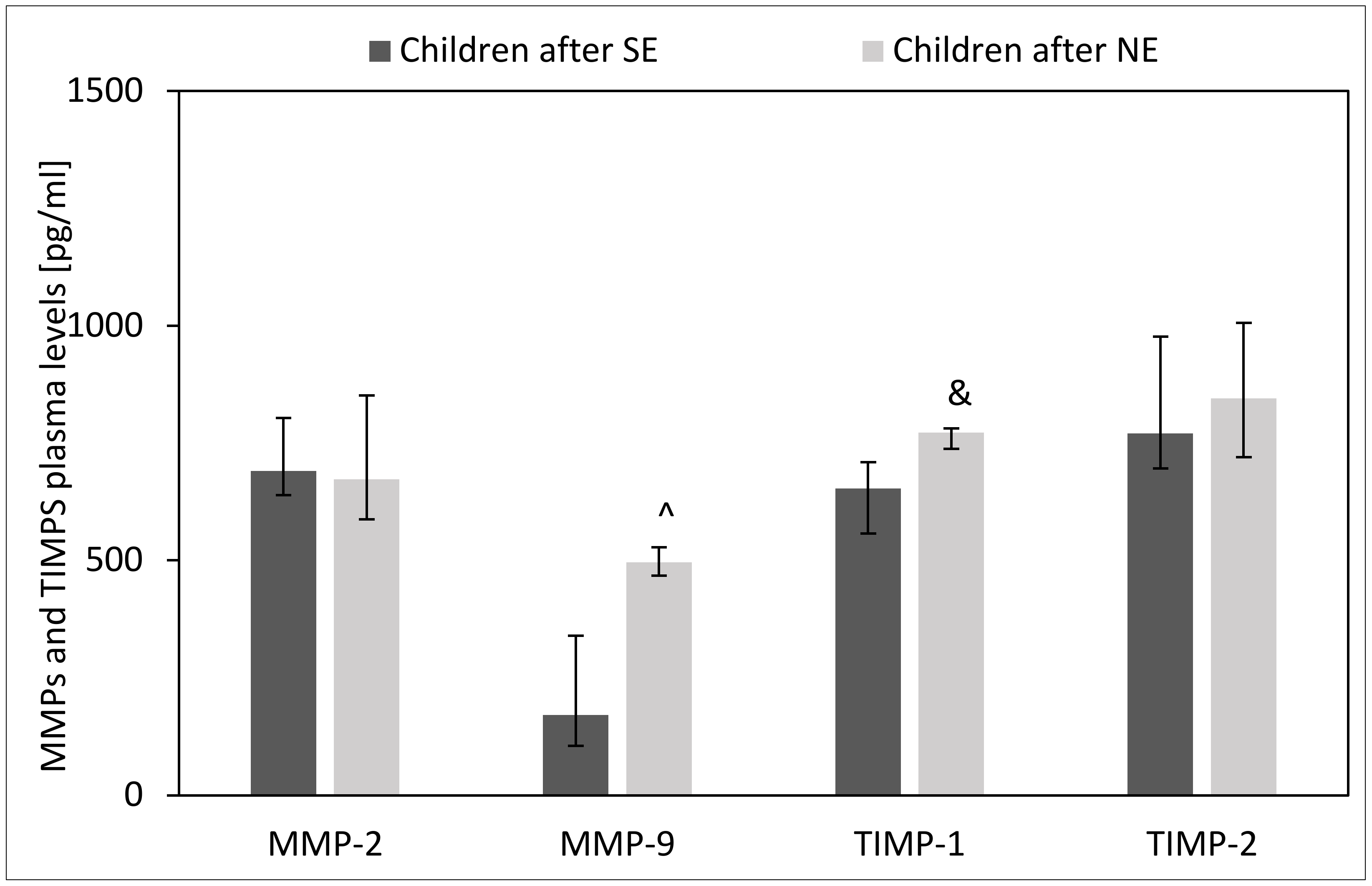
2.4. Effect of H. pylori Eradication Therapy on Plasma Levels of MMPs and TIMPs
2.5. Effect of H. pylori Eradication Therapy on the Intracellular Expression of MMPs and TIMPs in Circulating Lymphocytes, Monocytes and Neutrophils
2.6. Effect of H. pylori Eradication Therapy on the Expression of mRNA for MMPs and TIMP-1 in the Gastric Mucosa
2.7. The Association of MMPs and TIMPs with the Inflammation, Activity and Density of H. pylori in Gastric Mucosa
3. Discussion
4. Materials and Methods
4.1. Patients
4.2. Flow Cytometry Technique
4.3. Real-Time PCR
4.4. ELISA
4.5. Statistical Analyses
4.6. Ethical Considerations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kato, S.; Gold, B.D.; Kato, A. Helicobacter pylori-Associated Iron Deficiency Anemia in Childhood and Adolescence-Pathogenesis and Clinical Management Strategy. J. Clin. Med. 2022, 11, 7351. [Google Scholar] [CrossRef] [PubMed]
- Marginean, C.M.; Cioboata, R.; Olteanu, M.; Vasile, C.M.; Popescu, M.; Popescu, A.I.S.; Bondari, S.; Pirscoveanu, D.; Marginean, I.C.; Iacob, G.A.; et al. The Importance of Accurate Early Diagnosis and Eradication in Helicobacter pylori Infection: Pictorial Summary Review in Children and Adults. Antibiotics 2022, 12, 60. [Google Scholar] [CrossRef]
- Xu, C.; Wu, Y.; Xu, S. Association between Helicobacter pylori infection and growth outcomes in children: A meta-analysis. Helicobacter 2022, 27, e12861. [Google Scholar] [CrossRef] [PubMed]
- Yuan, C.; Adeloye, D.; Luk, T.T.; Huang, L.; He, Y.; Xu, Y.; Ye, X.; Yi, Q.; Song, P.; Rudan, I. The global prevalence of and factors associated with Helicobacter pylori infection in children: A systematic review and meta-analysis. Lancet Child. Adolesc. Health 2022, 6, 185–194. [Google Scholar] [CrossRef] [PubMed]
- Borka Balas, R.; Meliț, L.E.; Mărginean, C.O. Worldwide Prevalence and Risk Factors of Helicobacter pylori Infection in Children. Children 2022, 9, 1359. [Google Scholar] [CrossRef] [PubMed]
- Spee, L.A.A.; Madderom, M.B.; Pijpers, M.; van Leeuwen, Y.; Berger, M.Y. Association between Helicobacter pylori and gastrointestinal symptoms in children. Pediatrics 2010, 125, e651–e669. [Google Scholar] [CrossRef] [PubMed]
- Jones, N.L.; Koletzko, S.; Goodman, K.; Bontmes, P.; Cadranel, S.; Casswall, T.; Czinn, S.; Gold, B.D.; Guarner, J.; Elitsur, Y.; et al. Joint ESPGHAN/NASPGHAN Guidelines for the Management of Helicobacter pylori in children and adolescents (Update 2016). JPGN 2017, 64, 991–1003. [Google Scholar] [CrossRef] [PubMed]
- Schweitzer, K.; Sokolova, O.; Bozko, P.M.; Naumann, M. Helicobacter pylori induces NF-kappaB independent of CagA. EMBO Rep. 2010, 11, 10–11. [Google Scholar] [CrossRef] [PubMed]
- Sokolova, O.; Borgmann, M.; Rieke, C.; Schweitzer, K.; Rothkötter, H.J.; Naumann, M. Helicobacter pylori induces type 4 secretion system-dependent, but CagA-independent activation of IκBs and NF-κB/RelA at early time points. Int. J. Med. Microbiol. 2013, 303, 548–552. [Google Scholar] [CrossRef]
- Sokolova, O.; Vieth, M.; Naumann, M. Protein kinase C isozymes regulate matrix metalloproteinase-1 expression and cell invasion in Helicobacter pylori infection. Gut 2013, 62, 358–367. [Google Scholar] [CrossRef]
- Sokolova, O.; Maubach, G.; Naumann, M. Helicobacter pylori regulates TIFA turnover in gastric epithelial cells. Eur. J. Cell Biol. 2023, 102, 151307. [Google Scholar] [CrossRef]
- Koyama, S. Significance of cell-surface expression of matrix metalloproteinases and their inhibitors on gastric epithelium and infiltrating mucosal lymphocytes in progression of Helicobacter pylori-associated gastritis. Scand. J. Gastroenterol. 2004, 39, 1046–1053. [Google Scholar] [CrossRef]
- Rautelin, H.; Tervahartiala, T.; Lauhio, A.; Sorsa, T.; Kolho, K.L. Assessment of systemic matrix metalloproteinase and their regulator response in children with Helicobacter pylori gastritis. Scand. J. Clin. Lab. Investig. 2010, 70, 492–496. [Google Scholar] [CrossRef]
- Rautelin, H.I.; Oksanen, A.M.; Veijola, L.I.; Sipponen, P.I.; Tervahartiala, T.I.; Sorsa, T.A.; Lauhio, A. Enhanced systemic matrix metalloproteinase response in Helicobacter pylori gastritis. Ann. Med. 2009, 41, 208–215. [Google Scholar] [CrossRef] [PubMed]
- Chakraborti, S.; Mandal, M.; Das, S.; Mandal, A.; Chakraborti, T. Regulation of matrix metalloproteinases: An overview. Mol. Cell Biochem. 2003, 253, 269–285. [Google Scholar] [CrossRef] [PubMed]
- Itoh, Y. Membrane-type matrix metalloproteinases: Their functions and regulations. Matrix Biol. 2015, 44–46, 207–223. [Google Scholar] [CrossRef]
- Jobin, P.G.; Butler, G.S.; Overall, C.M. New intracellular activities of matrix metalloproteinases shine in the moonlight. Biochim. Biophys. Acta BBA Mol. Cell Res. 2017, 1864, 2043–2055. [Google Scholar]
- Bassiouni, W.; Ali, M.A.M.; Schulz, R. Multifunctional intracellular matrix metalloproteinases: Implications in disease. FEBS J. 2021, 288, 7162–7182. [Google Scholar] [CrossRef] [PubMed]
- Yeh, Y.C.; Sheu, B.S.; Cheng, H.C.; Wang, Y.L.; Yang, H.B.; Wu, J.J. Elevated Serum Matrix Metalloproteinase-3 and -7 in H. pylori-Related Gastric Cancer Can Be Biomarkers Correlating with a Poor Survival. Dig. Dis. Sci. 2010, 55, 1649–1657. [Google Scholar] [CrossRef]
- Weeks, B.S.; Schnaper, H.W.; Handy, M.; Holloway, E.; Kleinman, H.K. Human T lymphocytes synthesize the 92 kDa type IV collagenase (gelatinase B). J. Cell Physiol. 1993, 157, 644–649. [Google Scholar] [CrossRef]
- Leppert, D.; Waubant, E.; Galardy, R.; Bunnett, N.W.; Hauser, S.L. T cell gelatinases mediate basement membrane transmigration in vitro. J. Immunol. Baltim. Md. 1995, 154, 4379–4389. [Google Scholar] [CrossRef]
- Opdenakker, G. New insights in the regulation of leukocytosis and the role played by leukocytes in septic shock. Verh—K. Acad. Voor Geneeskd. Van. Belg. 2001, 63, 531–538; discussion 538–541. [Google Scholar]
- Stein, S.C.; Faber, E.; Bats, S.H.; Murillo, T.; Speidel, Y.; Coombs, N.; Josenhans, C. Helicobacter pylori modulates host cell responses by CagT4SS-dependent translocation of an intermediate metabolite of LPS inner core heptose biosynthesis. Monack DM, editor. PLoS Pathog. 2017, 13, e1006514. [Google Scholar] [CrossRef] [PubMed]
- Pfannkuch, L.; Hurwitz, R.; Traulsen, J.; Sigulla, J.; Poeschke, M.; Matzner, L.; Kosma, P.; Schmid, M.; Meyer, T.F. ADP heptose, a novel pathogen-associated molecular pattern identified in Helicobacter pylori. FASEB J. 2019, 33, 9087–9099. [Google Scholar] [CrossRef]
- Sokolova, O.; Naumann, M. Matrix Metalloproteinases in Helicobacter pylori–Associated Gastritis and Gastric Cancer. Int. J. Mol. Sci. 2022, 23, 1883. [Google Scholar] [CrossRef]
- Posselt, G.; Crabtree, J.; Wessler, S. Proteolysis in Helicobacter pylori-Induced Gastric Cancer. Toxins 2017, 9, 134. [Google Scholar] [CrossRef] [PubMed]
- Stetler-Stevenson, M.; Mansoor, A.; Lim, M.; Fukushima, P.; Kehrl, J.; Marti, G.; Ptaszynski, K.; Wang, J.; Stetler-Stevenson, W.G. Expression of matrix metalloproteinases and tissue inhibitors of metalloproteinases in reactive and neoplastic lymphoid cells. Blood 1997, 89, 1708–1715. [Google Scholar] [CrossRef]
- Ashutosh Chao, C.; Borgmann, K.; Brew, K.; Ghorpade, A. Tissue inhibitor of metalloproteinases-1 protects human neurons from staurosporine and HIV-1-induced apoptosis: Mechanisms and relevance to HIV-1-associated dementia. Cell Death Dis. 2012, 3, e332. [Google Scholar] [CrossRef] [PubMed]
- Kazachkov, E.L.; Kazimirova, A.A. [Role of matrix metalloproteinases and their tissue inhibitor in the morphogenesis of chronic Helicobacter pylori-associated gastritis in children]. Arkh Patol. 2009, 71, 43–45. [Google Scholar]
- Mori, N.; Sato, H.; Hayashibara, T.; Senba, M.; Geleziunas, R.; Wada, A.; Hirayama, T.; Yamamoto, N. Helicobacter pylori induces matrix metalloproteinase-9 through activation of nuclear factor κB. Gastroenterology 2003, 124, 983–992. [Google Scholar] [CrossRef]
- Bergin, P.J.; Anders, E.; Sicheng, W.; Erik, J.; Jennie, A.; Hans, L.; Pierre, M.; Qiang, P.-H.; Marianne, Q.-J. Increased Production of Matrix Metalloproteinases in Helicobacter pylori-Associated Human Gastritis. Helicobacter 2004, 9, 201–210. [Google Scholar] [CrossRef]
- Li, S.L. Increased expression of matrix metalloproteinase-9 associated with gastric ulcer recurrence. World J. Gastroenterol. 2013, 19, 4590. [Google Scholar] [CrossRef] [PubMed]
- Negaresh, M.; Safarzadeh, E.; Fouladi, N.; Matin, S.; Pourfarzi, S. The evaluation of the MMP-2/TIMP-1 ratio in peptic ulcer and its association with refractory helicobacter pylori infection. BMC Gastroenterol. 2023, 23, 287. [Google Scholar] [CrossRef] [PubMed]
- Kubben, F.J.G.M.; Sier, C.F.M.; Schram, M.T.; Witte, A.M.C.; Veenendaal, R.A.; van Duijn, W.; Verheijen, J.H.; Hanemaaijer, R.; Lamers, C.B.H.W.; Verspaget, H.W. Eradication of Helicobacter pylori Infection Favourably Affects Altered Gastric Mucosal MMP-9 Levels. Helicobacter 2007, 12, 498–504. [Google Scholar] [CrossRef] [PubMed]
- Helmin-Basa, A.; Michalkiewicz, J.; Gackowska, L.; Kubiszewska, I.; Eljaszewicz, A.; Mierzwa, G.; Bala, G.; Czerwionka-Szaflarska, M.; Prokurat, A.; Marszalek, A. Pediatric Helicobacter pylori Infection and Circulating T-Lymphocyte Activation and Differentiation: H. pylori, T-Cell Activation and Differentiation. Helicobacter 2011, 16, 27–35. [Google Scholar] [CrossRef]










| Variable | Inflammation | Activity | H. pylori |
|---|---|---|---|
| Activity | 0.19 | 1.00 | 0.02 |
| Inflammation | 1.00 | 0.19 | 0.60 |
| H. pylori | 0.60 | 0.02 | 1.00 |
| Total lymphocytes [%] | 0.11 | 0.18 | 0.18 |
| MMP-2+ lymphocytes [%] | 0.07 | 0.32 | −0.04 |
| MFI for MMP-2 in lymphocytes | −0.42 | −0.23 | −0.49 |
| MMP-9+ lymphocytes [%] | 0.00 | 0.24 | −0.19 |
| MFI for MMP-9 in lymphocytes | 0.14 | −0.05 | 0.36 |
| TIMP-1+ lymphocytes [%] | −0.17 | −0.09 | 0.55 |
| MFI for TIMP-1 in lymphocytes | 0.16 | 0.09 | 0.63 |
| TIMP-2+ lymphocytes [%] | 0.22 | −0.20 | −0.11 |
| MFI for TIMP-2 in lymphocytes | −0.76 | −0.48 | −0.58 |
| Total monocytes [%] | 0.51 | 0.46 | 0.16 |
| MMP-2+ monocytes [%] | 0.00 | 0.15 | −0.33 |
| MFI for MMP-2 in monocytes | −0.01 | −0.31 | 0.17 |
| MMP-9+ monocytes [%] | 0.02 | −0.05 | −0.22 |
| MFI for MMP-9 in monocytes | 0.22 | −0.25 | 0.16 |
| TIMP-1+ monocytes [%] | −0.03 | 0.02 | 0.40 |
| MFI for TIMP-1 in monocytes | −0.02 | −0.11 | 0.59 |
| TIMP-2+ monocytes [%] | 0.22 | −0.48 | 0.16 |
| MFI for TIMP-2 in monocytes | 0.08 | −0.45 | −0.21 |
| Total neutrophils [%] | −0.11 | −0.22 | −0.11 |
| MMP-2+ neutrophils [%] | −0.02 | −0.53 | −0.09 |
| MFI for MMP-2 in neutrophils | −0.38 | −0.30 | −0.53 |
| MMP-9+ neutrophils [%] | 0.13 | 0.17 | 0.18 |
| MFI for MMP-9 in neutrophils | 0.15 | −0.59 | −0.05 |
| TIMP-1+ neutrophils % | 0.06 | 0.00 | 0.32 |
| MFI for TIMP-1 in neutrophils | −0.43 | −0.05 | 0.06 |
| TIMP-2+ neutrophils [%] | 0.02 | −0.45 | −0.26 |
| MFI for TIMP-2 in neutrophils | −0.41 | −0.45 | −0.78 |
| TIMP-1 pg/mL | 0.42 | 0.22 | 0.46 |
| MMP-9 pg/mL | 0.28 | 0.22 | 0.73 |
| MMP-2 pg/mL | 0.32 | −0.09 | 0.02 |
| TIMP-2 pg/mL | 0.53 | −0.22 | 0.09 |
| TIMP1 mRNA | 0.57 | −0.04 | 0.32 |
| MMP2 mRNA | 0.20 | −0.20 | −0.05 |
| MMP9 mRNA | 0.71 | −0.16 | 0.66 |
| Gene Symbol | Gene Name | Ensembl ID/Entrez ID | Bio-Rad Unique Assay ID |
|---|---|---|---|
| TIMP1 | Tissue metalloproteinase inhibitor 1 | ENSG00000102265/7076 | qHsaCID0007434 |
| MMP2 | Matrix metalloproteinase 2 | ENSG00000087245/4313 | qHsaCID0015623 |
| MMP9 | Matrix metallopeptidase 9 | ENSG00000100985/4318 | qHsaCID0011597 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Helmin-Basa, A.; Kubiszewska, I.; Wiese-Szadkowska, M.; Strzyżewska, E.; Skalska-Bugała, A.; Balcerowska, S.; Rasmus, M.; Balcerczyk, D.; Pokrywczyńska, M.; Michałkiewicz, J.; et al. Expression of Matrix Metalloproteinases in the Circulating Immune Cells in Children with Helicobacter pylori Infection—Correlation with Clinical Factors. Int. J. Mol. Sci. 2023, 24, 15660. https://doi.org/10.3390/ijms242115660
Helmin-Basa A, Kubiszewska I, Wiese-Szadkowska M, Strzyżewska E, Skalska-Bugała A, Balcerowska S, Rasmus M, Balcerczyk D, Pokrywczyńska M, Michałkiewicz J, et al. Expression of Matrix Metalloproteinases in the Circulating Immune Cells in Children with Helicobacter pylori Infection—Correlation with Clinical Factors. International Journal of Molecular Sciences. 2023; 24(21):15660. https://doi.org/10.3390/ijms242115660
Chicago/Turabian StyleHelmin-Basa, Anna, Izabela Kubiszewska, Małgorzata Wiese-Szadkowska, Edyta Strzyżewska, Aleksandra Skalska-Bugała, Sara Balcerowska, Marta Rasmus, Daria Balcerczyk, Marta Pokrywczyńska, Jacek Michałkiewicz, and et al. 2023. "Expression of Matrix Metalloproteinases in the Circulating Immune Cells in Children with Helicobacter pylori Infection—Correlation with Clinical Factors" International Journal of Molecular Sciences 24, no. 21: 15660. https://doi.org/10.3390/ijms242115660
APA StyleHelmin-Basa, A., Kubiszewska, I., Wiese-Szadkowska, M., Strzyżewska, E., Skalska-Bugała, A., Balcerowska, S., Rasmus, M., Balcerczyk, D., Pokrywczyńska, M., Michałkiewicz, J., Krogulska, A., Główczewski, A., & Szaflarska-Popławska, A. (2023). Expression of Matrix Metalloproteinases in the Circulating Immune Cells in Children with Helicobacter pylori Infection—Correlation with Clinical Factors. International Journal of Molecular Sciences, 24(21), 15660. https://doi.org/10.3390/ijms242115660






