Consensus Gene Network Analysis Identifies the Key Similarities and Differences in Endothelial and Epithelial Cell Dynamics after Candida albicans Infection
Abstract
1. Introduction
2. Results
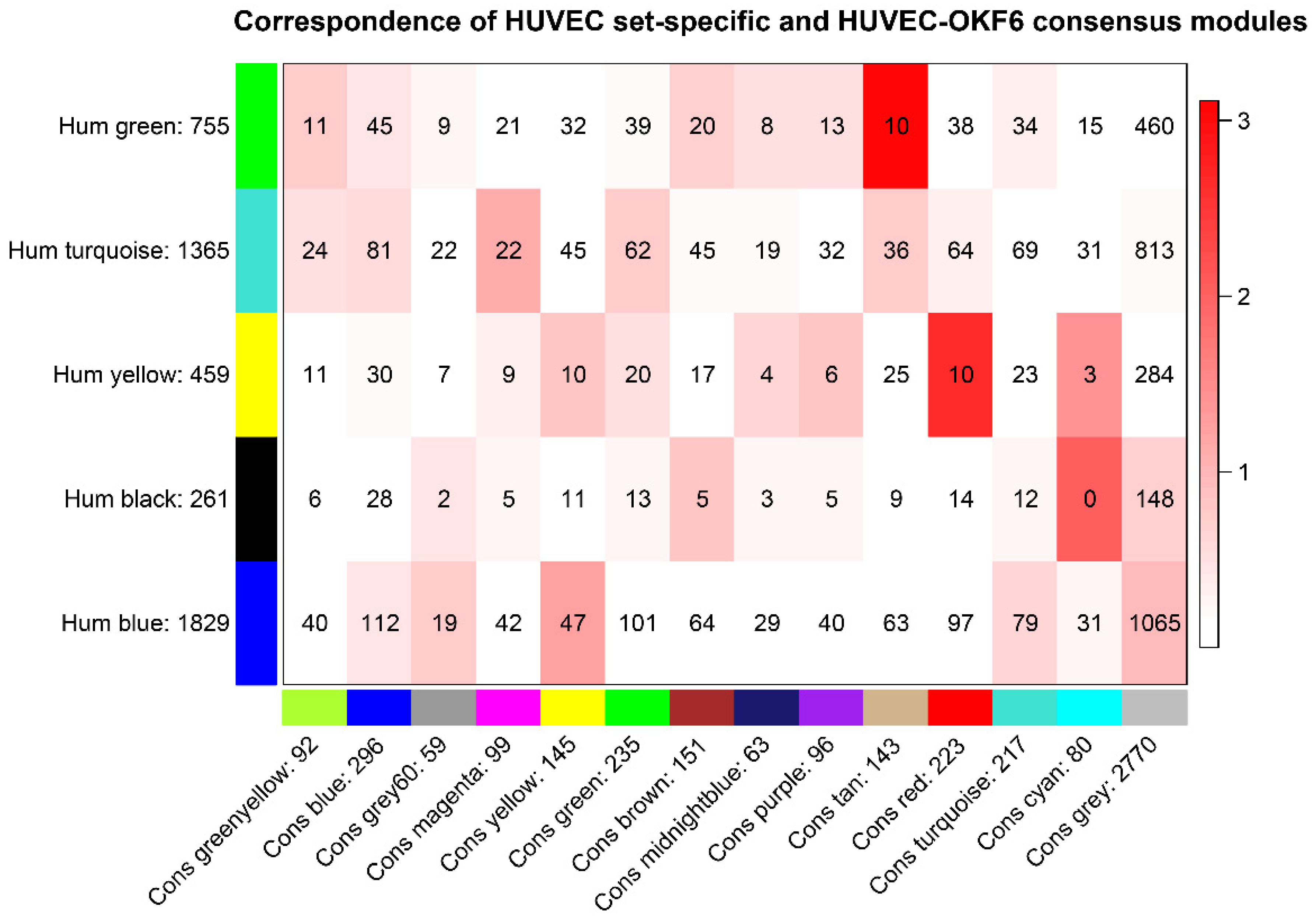
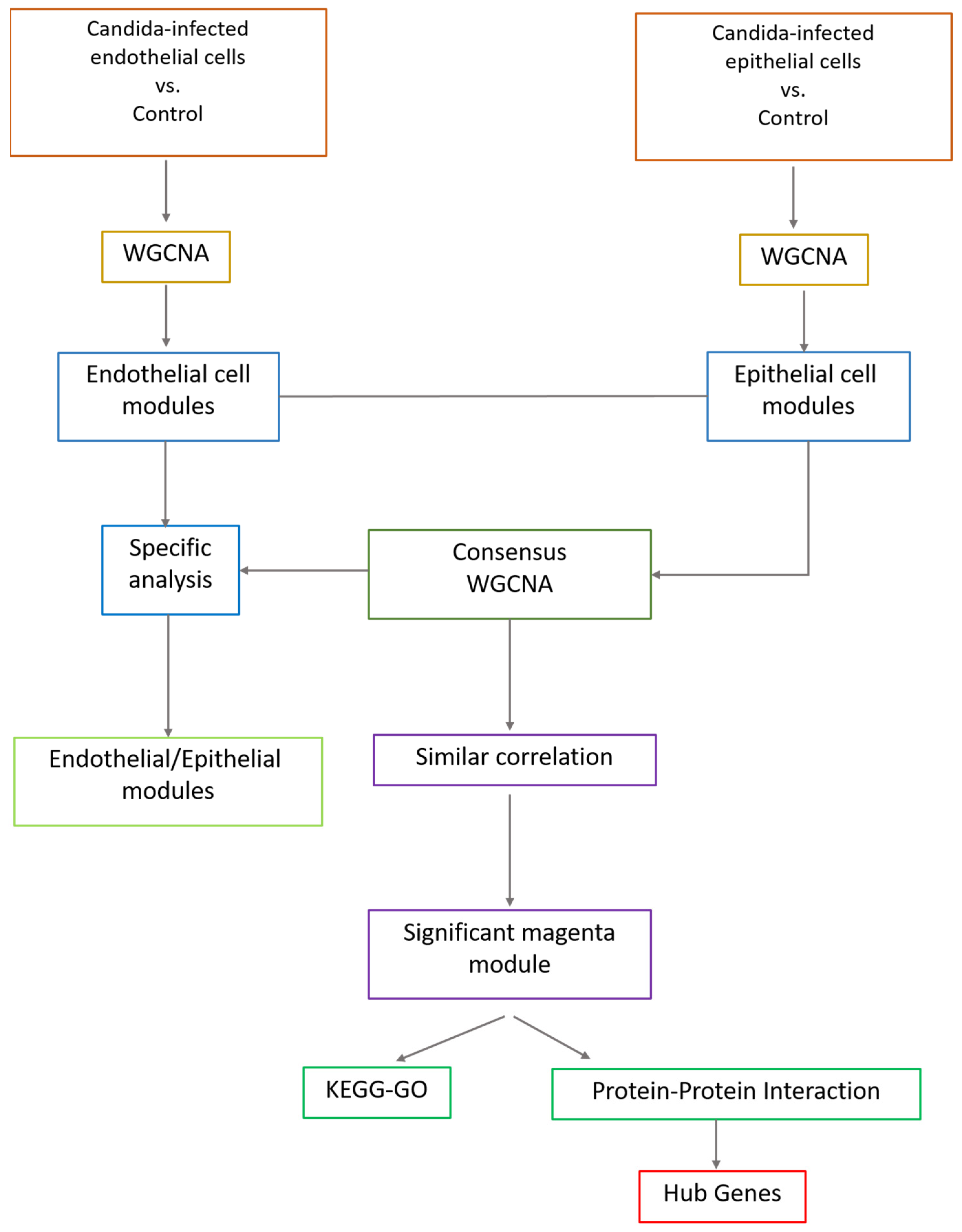
2.1. Identification of Consensus Gene Modules between Endothelial and Epithelial Cells
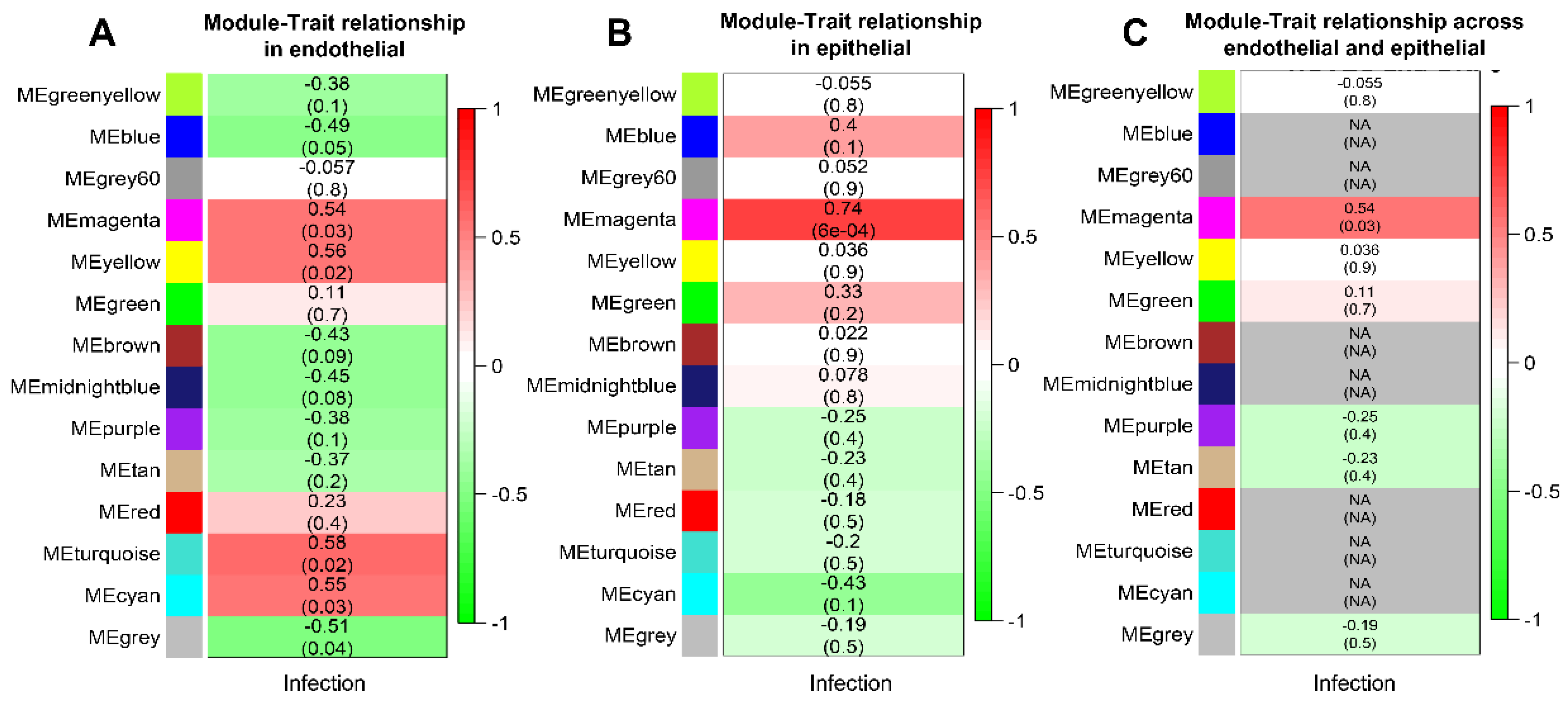
2.2. Module Association with External Trait
2.3. Differential Consensus Eigengene Network Analysis Reveals a Preserved Network Structure
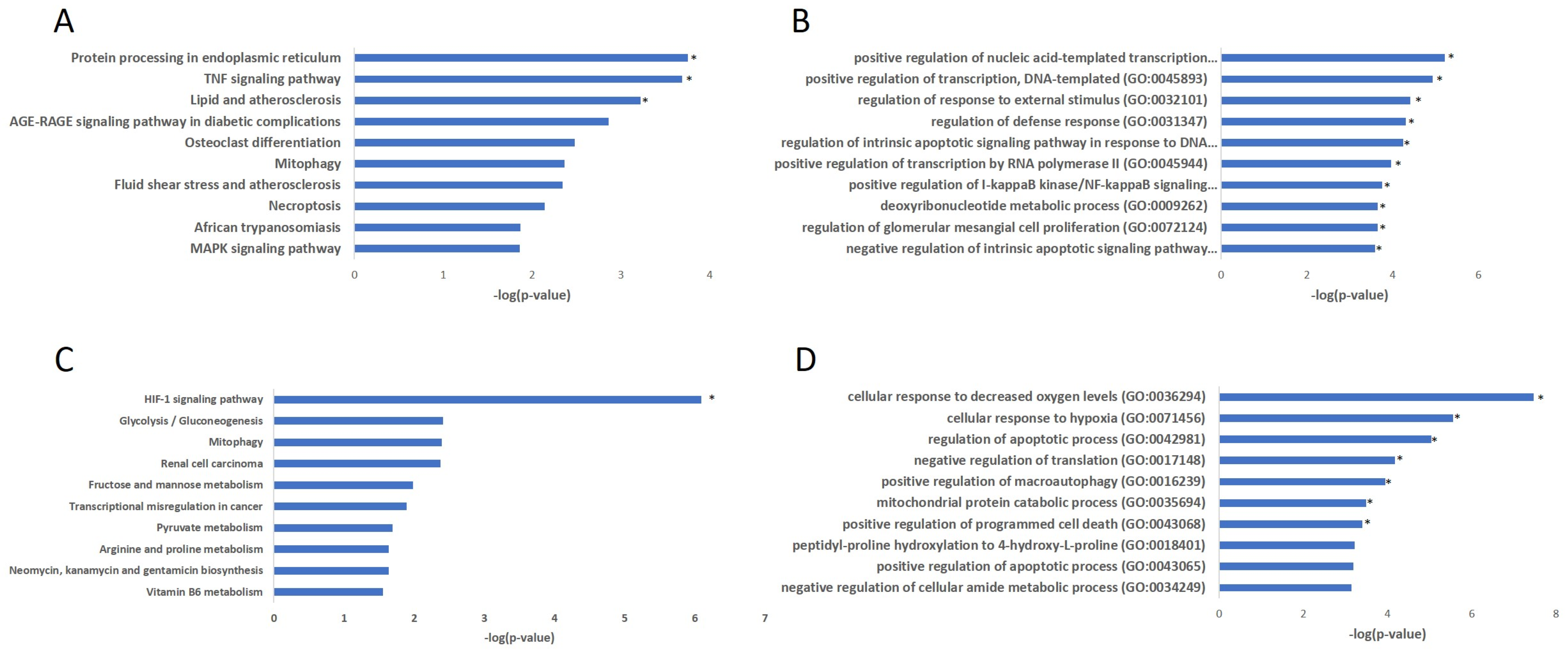
2.4. Functional Enrichment Analyses for Correlated Consensus Modules from Endothelial and Epithelial Cells
3. Discussion
4. Materials and Methods
4.1. Data Collection and Quality Control
4.2. Consensus Weighted Gene Correlation Network Analysis
4.3. Functional Enrichment Analysis of Genes
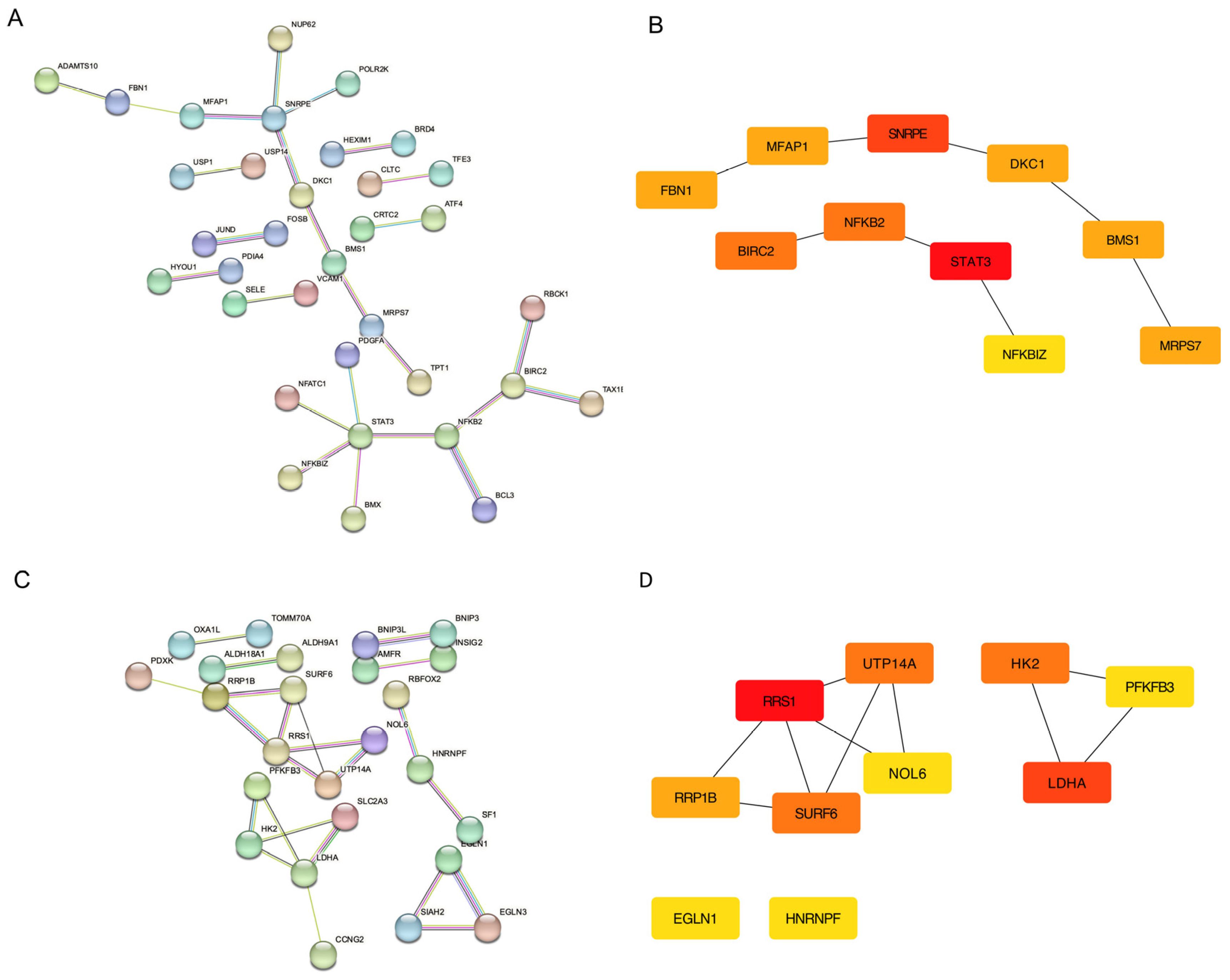
4.4. Protein–Protein Interaction
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Alonso-Monge, R.; Gresnigt, M.S.; Román, E.; Hube, B.; Pla, J. Candida albicans Colonization of the Gastrointestinal Tract: A Double-Edged Sword. PLoS Pathog. 2021, 17, e1009710. [Google Scholar] [CrossRef] [PubMed]
- Candida Infections of the Mouth, Throat, and Esophagus |Fungal Diseases| CDC. Available online: https://www.cdc.gov/fungal/diseases/candidiasis/thrush/index.html (accessed on 20 February 2023).
- Roselletti, E.; Perito, S.; Sabbatini, S.; Monari, C.; Vecchiarelli, A. Vaginal Epithelial Cells Discriminate Between Yeast and Hyphae of Candida in Women Who Are Colonized or Have Vaginal Candidiasis. J. Infect. Dis. 2019, 220, 1645–1654. [Google Scholar] [CrossRef] [PubMed]
- Pendleton, K.M.; Huffnagle, G.B.; Dickson, R.P. The Significance of Candida in the Human Respiratory Tract: Our Evolving Understanding. Pathog. Dis. 2017, 75, 29. [Google Scholar] [CrossRef] [PubMed]
- About Invasive Candidiasis |Invasive Candidiasis| Candidiasis |Types of Diseases|Fungal Diseases| CDC. Available online: https://www.cdc.gov/fungal/diseases/candidiasis/invasive/definition.html (accessed on 20 February 2023).
- Pappas, P.G.; Lionakis, M.S.; Arendrup, M.C.; Ostrosky-Zeichner, L.; Kullberg, B.J. Invasive Candidiasis. Nat. Rev. Dis. Prim. 2018, 4, 18026. [Google Scholar] [CrossRef] [PubMed]
- Nishimoto, A.T.; Sharma, C.; Rogers, P.D. Molecular and Genetic Basis of Azole Antifungal Resistance in the Opportunistic Pathogenic Fungus Candida albicans. J. Antimicrob. Chemother. 2020, 75, 257–270. [Google Scholar] [CrossRef] [PubMed]
- Klepser, M.E. Candida Resistance and Its Clinical Relevance. Pharmacotherapy 2006, 26, 68S–75S. [Google Scholar] [CrossRef]
- Liu, Y.; Shetty, A.C.; Schwartz, J.A.; Bradford, L.L.; Xu, W.; Phan, Q.T.; Kumari, P.; Mahurkar, A.; Mitchell, A.P.; Ravel, J.; et al. New Signaling Pathways Govern the Host Response to C. albicans Infection in Various Niches. Genome Res. 2015, 125, 679–689. [Google Scholar] [CrossRef]
- Wächtler, B.; Citiulo, F.; Jablonowski, N.; Förster, S.; Dalle, F.; Schaller, M.; Wilson, D.; Hube, B. Candida albicans-Epithelial Interactions: Dissecting the Roles of Active Penetration, Induced Endocytosis and Host Factors on the Infection Process. PLoS ONE 2012, 7, e36952. [Google Scholar] [CrossRef]
- Barker, K.S.; Park, H.; Phan, Q.T.; Xu, L.; Homayouni, R.; Rogers, P.D.; Filler, S.G. Transcriptome Profile of the Vascular Endothelial Cell Response to Candida albicans. J. Infect. Dis. 2008, 198, 193–202. [Google Scholar] [CrossRef]
- Grubb, S.E.W.; Murdoch, C.; Sudbery, P.E.; Saville, S.P.; Lopez-Ribot, J.L.; Thornhill, M.H. Candida albicans-Endothelial Cell Interactions: A Key Step in the Pathogenesis of Systemic Candidiasis. Infect. Immun. 2008, 76, 4370. [Google Scholar] [CrossRef]
- Dragoni, S.; Hudson, N.; Kenny, B.-A.; Burgoyne, T.; McKenzie, J.A.; Gill, Y.; Blaber, R.; Futter, C.E.; Adamson, P.; Greenwood, J.; et al. Endothelial MAPKs Direct ICAM-1 Signaling to Divergent Inflammatory Functions. J. Immunol. 2017, 198, 4074–4085. [Google Scholar] [CrossRef]
- Kong, D.H.; Kim, Y.K.; Kim, M.R.; Jang, J.H.; Lee, S. Emerging Roles of Vascular Cell Adhesion Molecule-1 (VCAM-1) in Immunological Disorders and Cancer. Int. J. Mol. Sci. 2018, 19, 1057. [Google Scholar] [CrossRef]
- Filler, S.G.; Swerdloff, J.N.; Hobbs, C.; Luckett, P.M. Penetration and Damage of Endothelial Cells by Candida albicans. Infect. Immun. 1995, 63, 976–983. [Google Scholar] [CrossRef]
- Allert, S.; Förster, T.M.; Svensson, C.M.; Richardson, J.P.; Pawlik, T.; Hebecker, B.; Rudolphi, S.; Juraschitz, M.; Schaller, M.; Blagojevic, M.; et al. Candida albicans-Induced Epithelial Damage Mediates Translocation through Intestinal Barriers. mBio 2018, 9, e00915-18. [Google Scholar] [CrossRef]
- Johnstone, K.F.; Herzberg, M.C. Antimicrobial Peptides: Defending the Mucosal Epithelial Barrier. Front. Oral Health 2022, 3, 958480. [Google Scholar] [CrossRef]
- Moyes, D.L.; Richardson, J.P.; Naglik, J.R. Candida albicans-Epithelial Interactions and Pathogenicity Mechanisms: Scratching the Surface. Virulence 2015, 6, 338. [Google Scholar] [CrossRef]
- Fusco, A.; Savio, V.; Donniacuo, M.; Perfetto, B.; Donnarumma, G. Antimicrobial Peptides Human Beta-Defensin-2 and -3 Protect the Gut During Candida albicans Infections Enhancing the Intestinal Barrier Integrity: In Vitro Study. Front. Cell. Infect. Microbiol. 2021, 11, 486. [Google Scholar] [CrossRef]
- Teijaro, J.R.; Walsh, K.B.; Cahalan, S.; Fremgen, D.M.; Roberts, E.; Scott, F.; Martinborough, E.; Peach, R.; Oldstone, M.B.A.; Rosen, H. Endothelial Cells Are Central Orchestrators of Cytokine Amplification during Influenza Virus Infection. Cell 2011, 146, 980. [Google Scholar] [CrossRef]
- Villar, C.C.; Kashleva, H.; Mitchell, A.P.; Dongari-Bagtzoglou, A. Invasive Phenotype of Candida albicans Affects the Host Proinflammatory Response to Infection. Infect. Immun. 2005, 73, 4588. [Google Scholar] [CrossRef]
- Shoham, S.; Marr, K.A. Invasive Fungal Infections in Solid Organ Transplant Recipients. Future Microbiol. 2012, 7, 639. [Google Scholar] [CrossRef]
- Aslam, S.; Rotstein, C. Candida Infections in Solid Organ Transplantation: Guidelines from the American Society of Transplantation Infectious Diseases Community of Practice. Clin. Transplant. 2019, 33, e13623. [Google Scholar] [CrossRef] [PubMed]
- Barros, N.; Mansour, M.K. Candida Infections in Solid Organ Transplantation. In Emerging Transplant Infections; Springer: Cham, Switzerland, 2021; pp. 1045–1075. [Google Scholar] [CrossRef]
- Naik, S.; Mohammed, A. Coexpression Network Analysis of Human Candida Infection Reveals Key Modules and Hub Genes Responsible for Host-Pathogen Interactions. Front. Genet. 2022, 13, 917636. [Google Scholar] [CrossRef] [PubMed]
- Obradovic, R.; Igic, M.; Mitic, A.; Pejcic, A.; Boskovic, M.; Todorovic, K. Diabetes Mellitus as a Risk Factor for Periodontal Disease Development. J. Environ. Prot. Ecol. 2019, 20, 1487–1495. [Google Scholar]
- Ángel González-Moles, M.; Ramos-García, P. Oral Health Problems in Diabetic Patients: A Critical Review of the Literature. J. Clin. Med. 2021, 10, 5383. [Google Scholar] [CrossRef]
- Sehnert, B.; Burkhardt, H.; Wessels, J.T.; Schröder, A.; May, M.J.; Vestweber, D.; Zwerina, J.; Warnatz, K.; Nimmerjahn, F.; Schett, G.; et al. NF-ΚB Inhibitor Targeted to Activated Endothelium Demonstrates a Critical Role of Endothelial NF-ΚB in Immune-Mediated Diseases. Proc. Natl. Acad. Sci. USA 2013, 110, 16556–16561. [Google Scholar] [CrossRef]
- Ben-Abdallah, M.; Sturny-Leclère, A.; Avé, P.; Louise, A.; Moyrand, F.; Weih, F.; Janbon, G.; Mémet, S. Fungal-Induced Cell Cycle Impairment, Chromosome Instability and Apoptosis via Differential Activation of NF-ΚB. PLoS Pathog. 2012, 8, e1002555. [Google Scholar] [CrossRef]
- Correia, I.; Prieto, D.; Román, E.; Wilson, D.; Hube, B.; Alonso-Monge, R.; Pla, J. Cooperative Role of MAPK Pathways in the Interaction of Candida albicans with the Host Epithelium. Microorganisms 2020, 8, 48. [Google Scholar] [CrossRef]
- Nikou, S.A.; Zhou, C.; Griffiths, J.S.; Kotowicz, N.K.; Coleman, B.M.; Green, M.J.; Moyes, D.L.; Gaffen, S.L.; Naglik, J.R.; Parker, P.J. The Candida albicans Toxin Candidalysin Mediates Distinct Epithelial Inflammatory Responses through P38 and EGFR-ERK Pathways. Sci. Signal. 2022, 15, 6915. [Google Scholar] [CrossRef]
- Nurgeldiyeva, M.J.; Hojakuliyev, B.G.; Muhammedov, M.B. Correlation of Atherogenesis with an Infection of Candida albicans. Int. J. Clin. Exp. Med. 2014, 7, 2137. [Google Scholar]
- Belanger, P.H.; Johnston, D.A.; Fratti, R.A.; Zhang, M.; Filler, S.G. Endocytosis of Candida albicans by Vascular Endothelial Cells Is Associated with Tyrosine Phosphorylation of Specific Host Cell Proteins. Cell. Microbiol. 2002, 4, 805–812. [Google Scholar] [CrossRef]
- Klotz, S.A.; Drutz, D.; Harrison, J.L.; Huppert, M. Adherence and Penetration of Vascular Endothelium by Candida Yeasts. Infect. Immun. 1983, 42, 374–384. [Google Scholar] [CrossRef]
- Kalliolias, G.D.; Ivashkiv, L.B. TNF Biology, Pathogenic Mechanisms and Emerging Therapeutic Strategies. Nat. Rev. Rheumatol. 2016, 12, 49–62. [Google Scholar] [CrossRef]
- Hennigs, J.K.; Matuszcak, C.; Trepel, M.; Körbelin, J. Vascular Endothelial Cells: Heterogeneity and Targeting Approaches. Cells 2021, 10, 2712. [Google Scholar] [CrossRef] [PubMed]
- Pober, J.S. Endothelial Activation: Intracellular Signaling Pathways. Arthritis Res. 2002, 4, S109. [Google Scholar] [CrossRef] [PubMed]
- Bradford, E.M.; Ryu, S.H.; Singh, A.P.; Lee, G.; Goretsky, T.; Sinh, P.; Williams, D.B.; Cloud, A.L.; Gounaris, E.; Patel, V.; et al. Epithelial TNF Receptor Signaling Promotes Mucosal Repair in IBD. J. Immunol. 2017, 199, 1886. [Google Scholar] [CrossRef] [PubMed]
- Rungratanawanich, W.; Qu, Y.; Wang, X.; Essa, M.M.; Song, B.J. Advanced Glycation End Products (AGEs) and Other Adducts in Aging-Related Diseases and Alcohol-Mediated Tissue Injury. Exp. Mol. Med. 2021, 53, 168–188. [Google Scholar] [CrossRef] [PubMed]
- Nowotny, K.; Jung, T.; Höhn, A.; Weber, D.; Grune, T. Advanced Glycation End Products and Oxidative Stress in Type 2 Diabetes Mellitus. Biomolecules 2015, 5, 194. [Google Scholar] [CrossRef]
- Calviño, J.; Cigarran, S.; Gonzalez-Tabares, L.; Menendez, N.; Latorre, J.; Cillero, S.; Millan, B.; Cobelo, C.; Sanjurjo-Amado, A.; Quispe, J.; et al. Advanced Glycation End Products (AGEs) Estimated by Skin Autofluorescence Are Related with Cardiovascular Risk in Renal Transplant. PLoS ONE 2018, 13, e0201118. [Google Scholar] [CrossRef]
- Radić, J.; Vučković, M.; Gelemanović, A.; Kolak, E.; Bučan Nenadić, D.; Begović, M.; Radić, M. Associations between Advanced Glycation End Products, Body Composition and Mediterranean Diet Adherence in Kidney Transplant Recipients. Int. J. Environ. Res. Public Health 2022, 19, 11060. [Google Scholar] [CrossRef]
- Moser, B.; Szabolcs, M.J.; Ankersmit, H.J.; Lu, Y.; Qu, W.; Weinberg, A.; Herold, K.C.; Schmidt, A.M. Blockade of RAGE Suppresses Alloimmune Reactions in Vitro and Delays Allograft Rejection in Murine Heart Transplantation. Am. J. Transplant. 2007, 7, 293–302. [Google Scholar] [CrossRef]
- Shu, H.B.; Agranoff, A.B.; Nabel, E.G.; Leung, K.; Duckett, C.S.; Neish, A.S.; Collins, T.; Nabel, G.J. Differential Regulation of Vascular Cell Adhesion Molecule 1 Gene Expression by Specific NF-Kappa B Subunits in Endothelial and Epithelial Cells. Mol. Cell. Biol. 1993, 13, 6283–6289. [Google Scholar] [CrossRef]
- Zhai, Z.; Boquete, J.-P.; Correspondence, B.L. Cell-Specific Imd-NF-κB Responses Enable Simultaneous Antibacterial Immunity and Intestinal Epithelial Cell Shedding upon Bacterial Infection. Immunity 2018, 48, 897–910. [Google Scholar] [CrossRef]
- Netea, M.G.; Joosten, L.A.B.; Van Der Meer, J.W.M.; Kullberg, B.J.; Van De Veerdonk, F.L. Immune Defence against Candida Fungal Infections. Nat. Rev. Immunol. 2015, 15, 630–642. [Google Scholar] [CrossRef]
- Serban, D.; Leng, J.; Cheresh, D. H-Ras Regulates Angiogenesis and Vascular Permeability by Activation of Distinct Downstream Effectors. Circ. Res. 2008, 102, 1350–1358. [Google Scholar] [CrossRef]
- Abumrad, N.A.; Cabodevilla, A.G.; Samovski, D.; Pietka, T.; Basu, D.; Goldberg, I.J. Endothelial Cell Receptors in Tissue Lipid Uptake and Metabolism. Circ. Res. 2021, 128, 433–450. [Google Scholar] [CrossRef]
- Nakamura, Y.; Shimizu, Y. Cellular and Molecular Control of Lipid Metabolism in Idiopathic Pulmonary Fibrosis: Clinical Application of the Lysophosphatidic Acid Pathway. Cells 2023, 12, 548. [Google Scholar] [CrossRef]
- Basante-Bedoya, M.A.; Bogliolo, S.; Garcia-Rodas, R.; Zaragoza, O.; Arkowitz, R.A.; Bassilana, M. Two Distinct Lipid Transporters Together Regulate Invasive Filamentous Growth in the Human Fungal Pathogen Candida albicans. PLoS Genet. 2022, 18, e1010549. [Google Scholar] [CrossRef]
- Otunla, A.A.; Shanmugarajah, K.; Madariaga, M.L.; Davies, A.H.; Shalhoub, J. Chronic Rejection and Atherosclerosis in Post-Transplant Cardiovascular Mortality: Two Sides of the Same Coin. Heart Lung Circ. 2022, 31, 162–166. [Google Scholar] [CrossRef]
- Hruban, R.H.; Beschorner, W.E.; Baumgartner, W.A.; Augustine, S.M.; Ren, H.; Reitz, B.A.; Hutchins, G.M. Accelerated Arteriosclerosis in Heart Transplant Recipients Is Associated with a T-Lymphocyte-Mediated Endothelialitis. Am. J. Pathol. 1990, 137, 871. [Google Scholar]
- Davignon, J.; Ganz, P. Role of Endothelial Dysfunction in Atherosclerosis. Circulation 2004, 109, III-27. [Google Scholar] [CrossRef]
- Pellon, A.; Begum, N.; Nasab, S.D.S.; Harzandi, A.; Shoaie, S.; Moyes, D.L. Role of Cellular Metabolism during Candida-Host Interactions. Pathogens 2022, 11, 184. [Google Scholar] [CrossRef] [PubMed]
- Drummond, R.; Leibundgut-Landmann, S.; Peters, B.M.; Moyes, D.L.; Pellon, A.; Dokht, S.; Nasab, S. New Insights in Candida albicans Innate Immunity at the Mucosa: Toxins, Epithelium, Metabolism, and Beyond. Front. Cell. Infect. Microbiol. 2020, 10, 81. [Google Scholar] [CrossRef]
- Brown, A.J.P.; Brown, G.D.; Netea, M.G.; Gow, N.A.R. Metabolism Impacts upon Candida Immunogenicity and Pathogenicity at Multiple Levels. Trends Microbiol. 2014, 22, 614–622. [Google Scholar] [CrossRef] [PubMed]
- Silao, F.G.S.; Ljungdahl, P.O. Amino Acid Sensing and Assimilation by the Fungal Pathogen Candida albicans in the Human Host. Pathogens 2022, 11, 5. [Google Scholar] [CrossRef] [PubMed]
- Kumrungsee, T.; Zhang, P.; Chartkul, M.; Yanaka, N.; Kato, N. Potential Role of Vitamin B6 in Ameliorating the Severity of COVID-19 and Its Complications. Front. Nutr. 2020, 7, 562051. [Google Scholar] [CrossRef]
- Parra, M.; Stahl, S.; Hellmann, H. Vitamin B6 and Its Role in Cell Metabolism and Physiology. Cells 2018, 7, 84. [Google Scholar] [CrossRef]
- Nagi, M.; Tanabe, K.; Nakayama, H.; Ueno, K.; Yamagoe, S.; Umeyama, T.; Ohno, H.; Miyazaki, Y. Iron-Depletion Promotes Mitophagy to Maintain Mitochondrial Integrity in Pathogenic Yeast Candida glabrata. Autophagy 2016, 12, 1259–1271. [Google Scholar] [CrossRef]
- Cho, D.H.; Kim, J.K.; Jo, E.K. Mitophagy and Innate Immunity in Infection. Mol. Cells 2020, 43, 10. [Google Scholar] [CrossRef]
- Majno, G.; Joris, I. Apoptosis, Oncosis, and Necrosis. An Overview of Cell Death. Am. J. Pathol. 1995, 146, 3. [Google Scholar]
- Choi, M.E.; Price, D.R.; Ryter, S.W.; Choi, A.M.K. Necroptosis: A Crucial Pathogenic Mediator of Human Disease. JCI Insight 2019, 4, e128834. [Google Scholar] [CrossRef]
- Nagata, S.; Nagase, H.; Kawane, K.; Mukae, N.; Fukuyama, H. Degradation of Chromosomal DNA during Apoptosis. Cell Death Differ. 2003, 10, 108–116. [Google Scholar] [CrossRef]
- Nagata, S. DNA Degradation during Apoptotic Cell Death. Arthritis Res. Ther. 2003, 5, 1. [Google Scholar] [CrossRef]
- Lukenaite, B.; Griciune, E.; Leber, B.; Strupas, K.; Stiegler, P.; Schemmer, P. Necroptosis in Solid Organ Transplantation: A Literature Overview. Int. J. Mol. Sci. 2022, 23, 3677. [Google Scholar] [CrossRef]
- Zhao, H.; Jaffer, T.; Eguchi, S.; Wang, Z.; Linkermann, A.; Ma, D. Role of Necroptosis in the Pathogenesis of Solid Organ Injury. Cell Death Dis. 2015, 6, e1975. [Google Scholar] [CrossRef]
- Pavlosky, A.; Lau, A.; Su, Y.; Lian, D.; Huang, X.; Yin, Z.; Haig, A.; Jevnikar, A.M.; Zhang, Z.X. RIPK3-Mediated Necroptosis Regulates Cardiac Allograft Rejection. Am. J. Transplant. 2014, 14, 1778–1790. [Google Scholar] [CrossRef]
- Yeaman, M.R.; Büttner, S.; Thevissen, K. Review Article Regulated Cell Death as a Therapeutic Target for Novel Antifungal Peptides and Biologics. Oxidative Med. Cell. Longev. 2018, 2018, 5473817. [Google Scholar] [CrossRef]
- Bassetti, M.; Peghin, M.; Carnelutti, A.; Righi, E.; Merelli, M.; Ansaldi, F.; Trucchi, C.; Alicino, C.; Sartor, A.; Wauters, J.; et al. Invasive Candida Infections in Liver Transplant Recipients: Clinical Features and Risk Factors for Mortality. Transplant. Direct 2017, 3, e156. [Google Scholar] [CrossRef]
- Pradhan, A.; Avelar, G.M.; Bain, J.M.; Childers, D.S.; Larcombe, D.E.; Netea, M.G.; Shekhova, E.; Munro, C.A.; Brown, G.D.; Erwig, L.P.; et al. Hypoxia Promotes Immune Evasion by Triggering β-Glucan Masking on the Candida albicans Cell Surface via Mitochondrial and CAMP-Protein Kinase A Signaling. mBio 2018, 9, e01318-18. [Google Scholar] [CrossRef]
- Griffiths, J.S.; Camilli, G.; Kotowicz, N.K.; Ho, J.; Richardson, J.P.; Naglik, J.R. Role for IL-1 Family Cytokines in Fungal Infections. Front. Microbiol. 2021, 12, 132. [Google Scholar] [CrossRef]
- Cottier, F.; Hall, R.A. Face/Off: The Interchangeable Side of Candida albicans. Front. Cell. Infect. Microbiol. 2020, 9, 471. [Google Scholar] [CrossRef]
- Zhou, Y.; Cheng, L.; Lei, Y.L.; Ren, B.; Zhou, X. The Interactions Between Candida albicans and Mucosal Immunity. Front. Microbiol. 2021, 12, 1694. [Google Scholar] [CrossRef] [PubMed]
- Friedrich, D.; Fecher, R.A.; Rupp, J.; Deepe, G.S. Impact of HIF-1α and Hypoxia on Fungal Growth Characteristics and Fungal Immunity. Microbes Infect. 2017, 19, 204. [Google Scholar] [CrossRef] [PubMed]
- Gautier, L.; Cope, L.; Bolstad, B.M.; Irizarry, R.A. Affy-Analysis of Affymetrix GeneChip Data at the Probe Level. Bioinformatics 2004, 20, 307–315. [Google Scholar] [CrossRef] [PubMed]
- Langfelder, P.; Horvath, S. WGCNA: An R Package for Weighted Correlation Network Analysis. BMC Bioinform. 2008, 9, 559. [Google Scholar] [CrossRef]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Naik, S.; Mohammed, A. Consensus Gene Network Analysis Identifies the Key Similarities and Differences in Endothelial and Epithelial Cell Dynamics after Candida albicans Infection. Int. J. Mol. Sci. 2023, 24, 11748. https://doi.org/10.3390/ijms241411748
Naik S, Mohammed A. Consensus Gene Network Analysis Identifies the Key Similarities and Differences in Endothelial and Epithelial Cell Dynamics after Candida albicans Infection. International Journal of Molecular Sciences. 2023; 24(14):11748. https://doi.org/10.3390/ijms241411748
Chicago/Turabian StyleNaik, Surabhi, and Akram Mohammed. 2023. "Consensus Gene Network Analysis Identifies the Key Similarities and Differences in Endothelial and Epithelial Cell Dynamics after Candida albicans Infection" International Journal of Molecular Sciences 24, no. 14: 11748. https://doi.org/10.3390/ijms241411748
APA StyleNaik, S., & Mohammed, A. (2023). Consensus Gene Network Analysis Identifies the Key Similarities and Differences in Endothelial and Epithelial Cell Dynamics after Candida albicans Infection. International Journal of Molecular Sciences, 24(14), 11748. https://doi.org/10.3390/ijms241411748





