Calcium/P53/Ninjurin 1 Signaling Mediates Plasma Membrane Rupture of Acinar Cells in Severe Acute Pancreatitis
Abstract
1. Introduction
2. Results
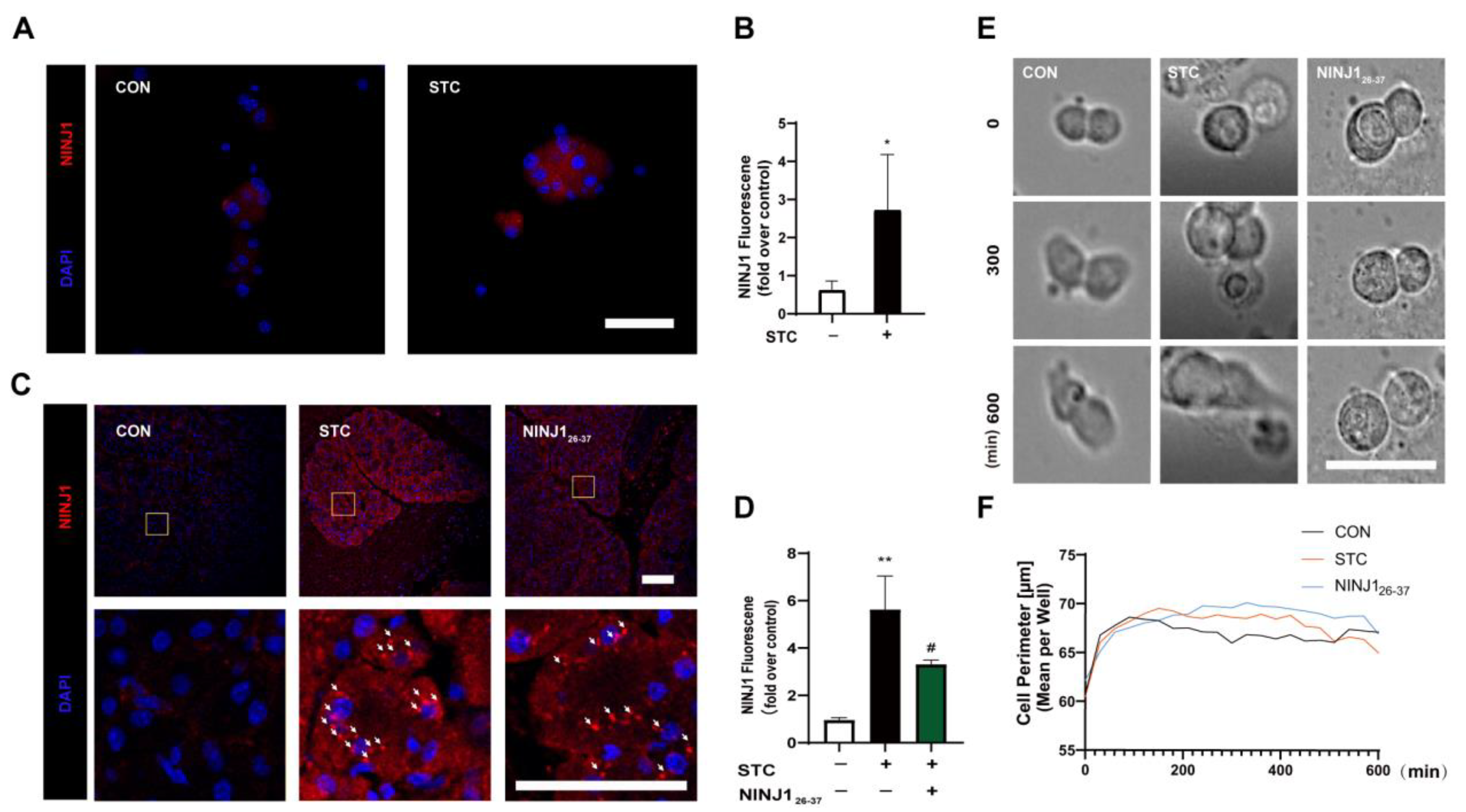
2.1. NINJ1 Is Expressed and Activated in SAP Acinar Cells
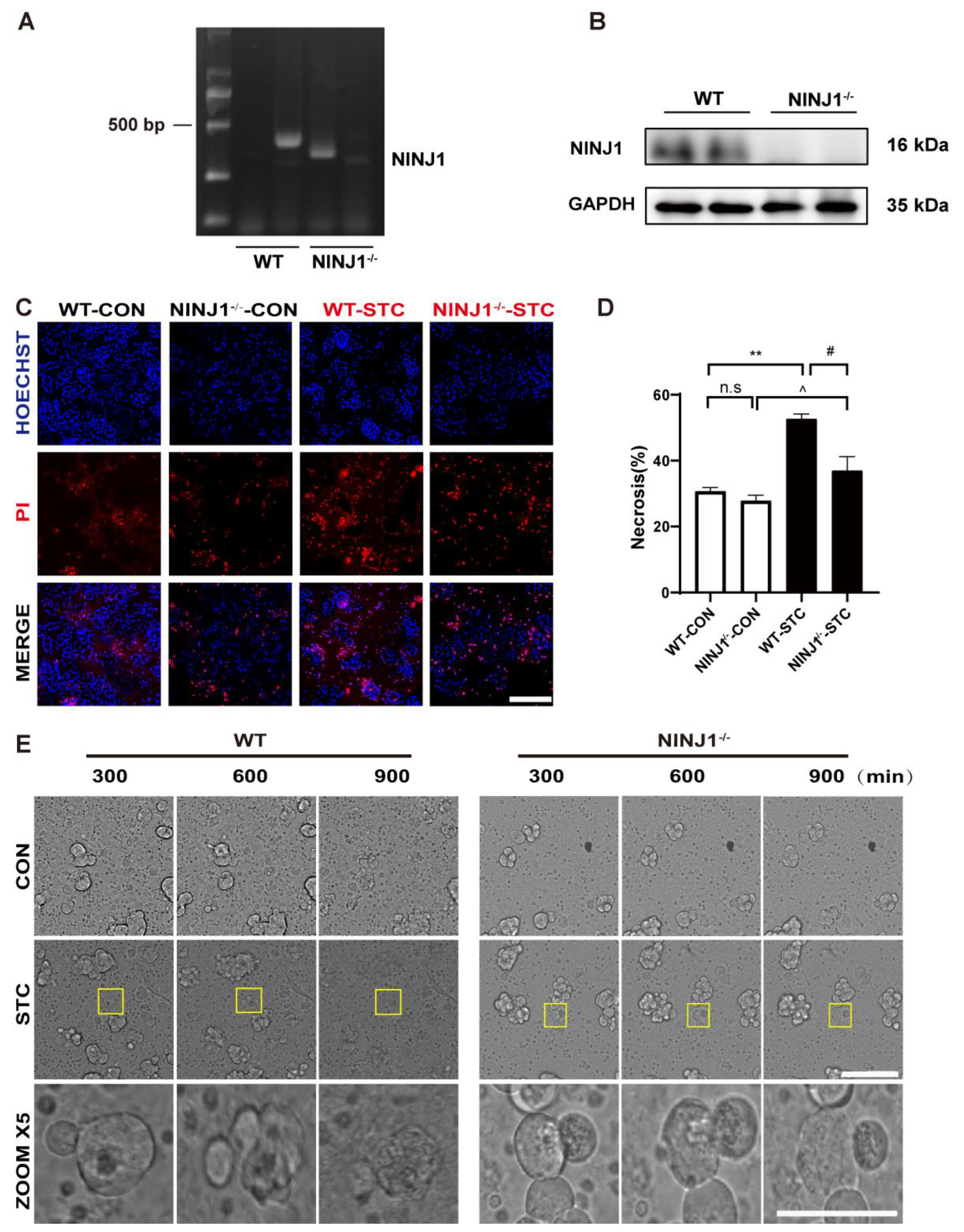
2.2. NINJ1 Knockout Inhibits PMR of Acinar Cells and Ameliorated SAP
2.3. NINJ1 Expression Is Mediated by Ca2+
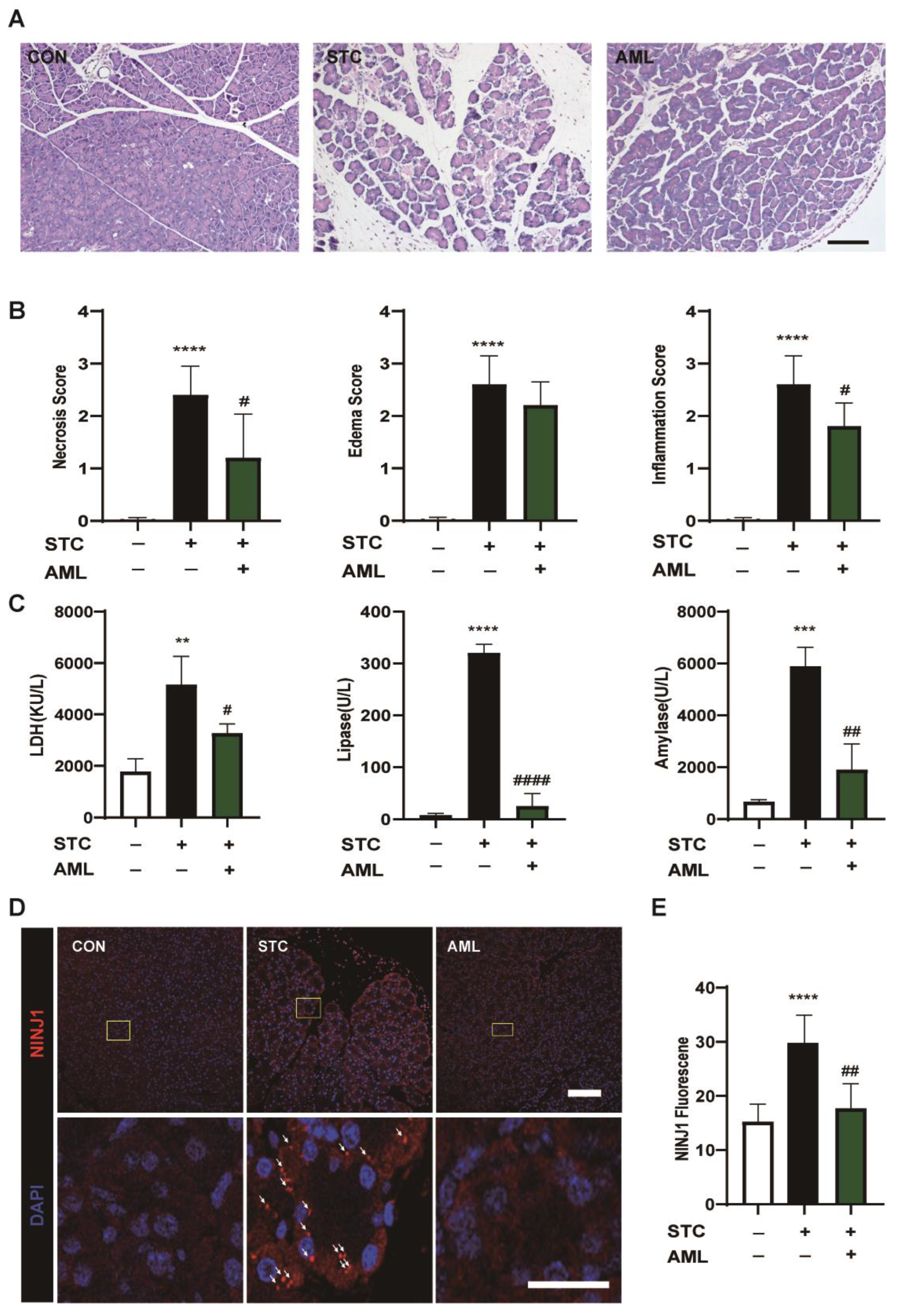
2.4. NINJ1 Inhibition by AML Improves SAP in Mice
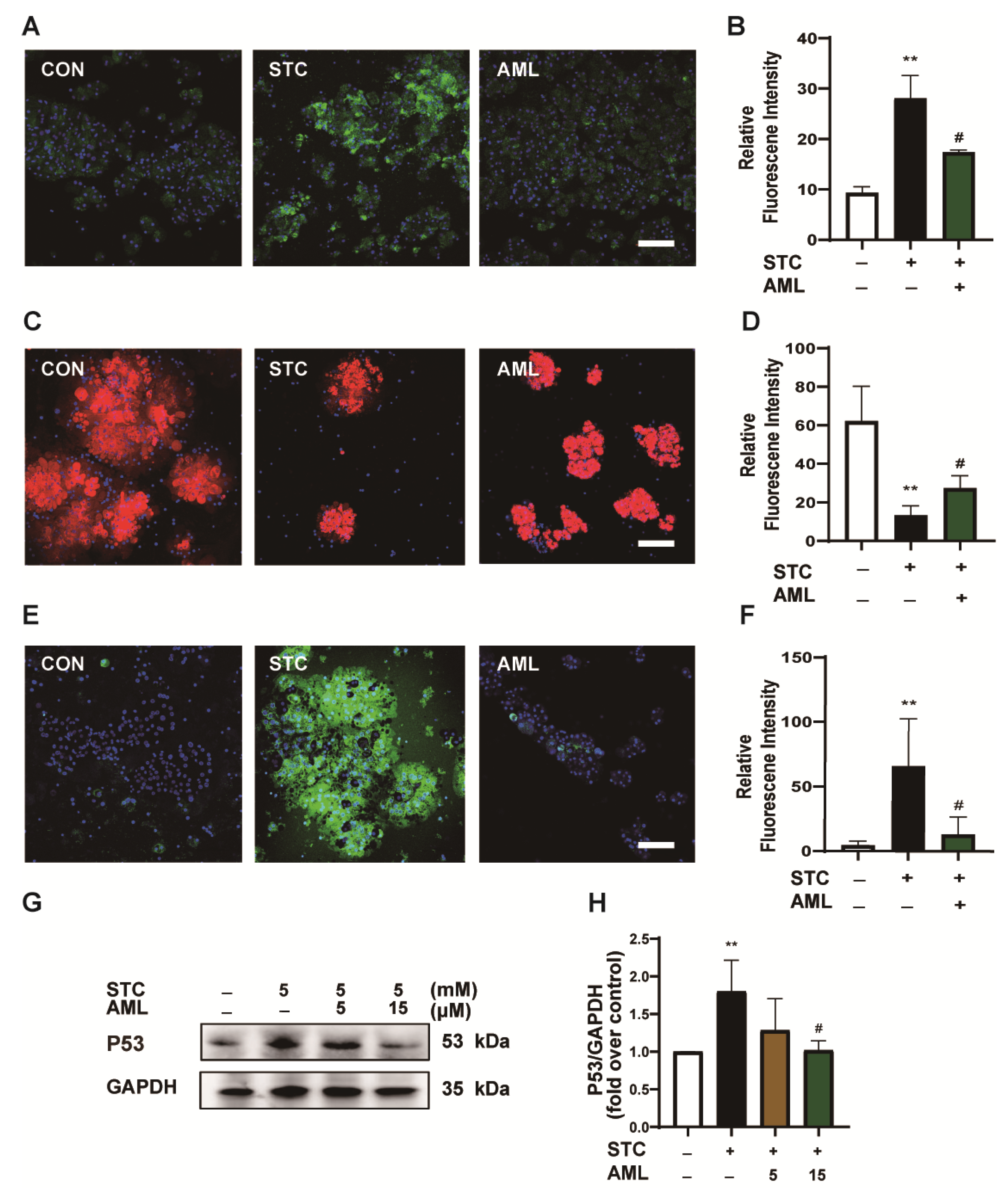
2.5. Inhibition of Ca2+Channels Protects ΔΨm and Decreases P53 Expression
2.6. P53 Upregulates NINJ1 to Induce PMR
3. Discussion
4. Materials and Methods
4.1. Animals
4.2. Materials
4.3. Animal Model of SAP and Treatments
4.4. Histopathology
4.5. Immunofluorescence Staining
4.6. Preparation of Pancreatic Acinar Cells
4.7. STC-Induced Acinar Cell Death Measurement In Vitro
4.8. Detection of ROS
4.9. ΔΨm Measurement
4.10. Detection of Intracellular Calcium Content
4.11. Detection of Serum Amylase and Lipase
4.12. Western Blot Analysis
4.13. Cell Culture
4.14. Cell Viability Assay
4.15. HCS Real-Time Imaging
4.16. Statistical Analysis
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AP | Acute pancreatitis |
| SAP | Severe acute pancreatitis |
| PMR | Plasma membrane rupture |
| DAMPs | Damage-associated molecular pattern |
| NINJ1 | Ninjurin 1 |
| ER | endoplasmic reticulum |
| IP3R | inositol 1,4,5-trisphosphate receptor |
| ΔΨm | mitochondrial membrane potential |
| MCU | mitochondrial calcium uniporter |
| AML | Amlodipine |
| STC | sodium taurocholate |
| HCS | High-content screening |
| SOD | superoxide dismutase |
| MDA | malondialdehyde |
References
- Hines, O.J.; Pandol, S.J. Management of severe acute pancreatitis. BMJ 2019, 367, l6227. [Google Scholar] [CrossRef]
- Boxhoorn, L.; Voermans, R.P.; Bouwense, S.A.; Bruno, M.J.; Verdonk, R.C.; Boermeester, M.A.; van Santvoort, H.C.; Besselink, M.G. Acute pancreatitis. Lancet 2020, 396, 726–734. [Google Scholar] [CrossRef]
- Banks, P.A.; Bollen, T.L.; Dervenis, C.; Gooszen, H.G.; Johnson, C.D.; Sarr, M.G.; Tsiotos, G.G.; Vege, S.S. Classification of acute pancreatitis--2012: Revision of the Atlanta classification and definitions by international consensus. Gut 2013, 62, 102–111. [Google Scholar] [CrossRef]
- Iannuzzi, J.P.; King, J.A.; Leong, J.H.; Quan, J.; Windsor, J.W.; Tanyingoh, D.; Coward, S.; Forbes, N.; Heitman, S.J.; Shaheen, A.-A. Global incidence of acute pancreatitis is increasing over time: A systematic review and meta-analysis. Gastroenterology 2022, 162, 122–134. [Google Scholar] [CrossRef]
- Xiao, A.Y.; Tan, M.L.Y.; Wu, L.M.; Asrani, V.M.; Windsor, J.A.; Yadav, D.; Petrov, M.S. Global incidence and mortality of pancreatic diseases: A systematic review, meta-analysis, and meta-regression of population-based cohort studies. Lancet Gastroenterol. Hepatol. 2016, 1, 45–55. [Google Scholar] [CrossRef]
- Pagliari, D.; Brizi, M.G.; Saviano, A.; Mancarella, F.A.; Dal Lago, A.A.; Serricchio, M.L.; Newton, E.E.; Attili, F.; Manfredi, R.; Gasbarrini, A. Clinical assessment and management of severe acute pancreatitis: A multi-disciplinary approach in the XXI century. Eur. Rev. Med. Pharmacol. Sci. 2019, 23, 771–787. [Google Scholar] [CrossRef]
- Jabłońska, B.; Mrowiec, S. Nutritional support in patients with severe acute pancreatitis-current standards. Nutrients 2021, 13, 1498. [Google Scholar] [CrossRef]
- Lee, P.J.; Papachristou, G.I. New insights into acute pancreatitis. Nat. Rev. Gastroenterol. Hepatol. 2019, 16, 479–496. [Google Scholar] [CrossRef]
- Leppäniemi, A.; Tolonen, M.; Tarasconi, A.; Segovia-Lohse, H.; Gamberini, E.; Kirkpatrick, A.W.; Ball, C.G.; Parry, N.; Sartelli, M.; Wolbrink, D.; et al. 2019 WSES guidelines for the management of severe acute pancreatitis. World J. Emerg. Surg. 2019, 14, 27. [Google Scholar] [CrossRef]
- Araki, T.; Milbrandt, J. Ninjurin, a novel adhesion molecule, is induced by nerve injury and promotes axonal growth. Neuron 1996, 17, 353–361. [Google Scholar] [CrossRef]
- Lee, H.J.; Ahn, B.J.; Shin, M.W.; Choi, J.-H.; Kim, K.-W. Ninjurin1: A potential adhesion molecule and its role in inflammation and tissue remodeling. Mol. Cells 2010, 29, 223–227. [Google Scholar] [CrossRef] [PubMed]
- Kayagaki, N.; Kornfeld, O.S.; Lee, B.L.; Stowe, I.B.; O’Rourke, K.; Li, Q.; Sandoval, W.; Yan, D.; Kang, J.; Xu, M.; et al. NINJ1 mediates plasma membrane rupture during lytic cell death. Nature 2021, 591, 131–136. [Google Scholar] [CrossRef] [PubMed]
- Petersen, O.H.; Gerasimenko, J.V.; Gerasimenko, O.V.; Gryshchenko, O.; Peng, S. The roles of calcium and ATP in the physiology and pathology of the exocrine pancreas. Physiol. Rev. 2021, 101, 1691–1744. [Google Scholar] [CrossRef] [PubMed]
- Biczo, G.; Vegh, E.T.; Shalbueva, N.; Mareninova, O.A.; Elperin, J.; Lotshaw, E.; Gretler, S.; Lugea, A.; Malla, S.R.; Dawson, D.; et al. Mitochondrial dysfunction, through impaired autophagy, leads to endoplasmic reticulum stress, deregulated lipid metabolism, and pancreatitis in animal models. Gastroenterology 2018, 154, 689–703. [Google Scholar] [CrossRef]
- Criddle, D.N.; McLaughlin, E.; Murphy, J.A.; Petersen, O.H.; Sutton, R. The pancreas misled: Signals to pancreatitis. Pancreatology 2007, 7, 436–446. [Google Scholar]
- Marolt, U.; Paradiž Leitgeb, E.; Pohorec, V.; Lipovšek, S.; Venglovecz, V.; Gál, E.; Ébert, A.; Menyhárt, I.; Potrč, S.; Gosak, M.; et al. Calcium imaging in intact mouse acinar cells in acute pancreas tissue slices. PLoS ONE 2022, 17, e0268644. [Google Scholar] [CrossRef]
- Niwa-Kawakita, M.; Ferhi, O.; Soilihi, H.; Le Bras, M.; Lallemand-Breitenbach, V.; de Thé, H. PML is a ROS sensor activating p53 upon oxidative stress. J. Exp. Med. 2017, 214, 3197–3206. [Google Scholar] [CrossRef]
- Shi, T.; Dansen, T.B. Reactive oxygen species induced p53 activation: DNA damage, redox signaling, or Both? Antioxid. Redox Signal. 2020, 33, 839–859. [Google Scholar] [CrossRef]
- Rius-Pérez, S.; Pérez, S.; Toledano, M.B.; Sastre, J. P53 drives necroptosis via downregulation of sulfiredoxin and peroxiredoxin 3. Redox Biol. 2022, 56, 102423. [Google Scholar] [CrossRef]
- Napoletano, F.; Gibert, B.; Yacobi-Sharon, K.; Vincent, S.; Favrot, C.; Mehlen, P.; Girard, V.; Teil, M.; Chatelain, G.; Walter, L.; et al. P53-dependent programmed necrosis controls germ cell homeostasis during spermatogenesis. PLoS Genet. 2017, 13, e1007024. [Google Scholar] [CrossRef]
- Cho, S.-J.; Rossi, A.; Jung, Y.-S.; Yan, W.; Liu, G.; Zhang, J.; Zhang, M.; Chen, X. Ninjurin1, a target of p53, regulates p53 expression and p53-dependent cell survival, senescence, and radiation-induced mortality. Proc. Natl. Acad. Sci. USA 2013, 110, 9362–9367. [Google Scholar] [CrossRef]
- Li, Y.; Zhao, D.; Qian, M.; Liu, J.; Pan, C.; Zhang, X.; Duan, X.; Zhang, Y.; Jia, W.; Wang, L. Amlodipine, an anti-hypertensive drug, alleviates non-alcoholic fatty liver disease by modulating gut microbiota. Br. J. Pharmacol. 2022, 179, 2054–2077. [Google Scholar] [CrossRef]
- Toma, L.; Sanda, G.M.; Raileanu, M.; Stancu, C.S.; Niculescu, L.S.; Sima, A.V. Ninjurin-1 upregulated by TNFα receptor 1 stimulates monocyte adhesion to human TNFα-activated endothelial cells; benefic effects of amlodipine. Life Sci. 2020, 249, 117518. [Google Scholar] [CrossRef] [PubMed]
- Jennewein, C.; Sowa, R.; Faber, A.C.; Dildey, M.; von Knethen, A.; Meybohm, P.; Scheller, B.; Dröse, S.; Zacharowski, K. Contribution of Ninjurin1 to Toll-like receptor 4 signaling and systemic inflammation. Am. J. Respir. Cell Mol. Biol. 2015, 53, 656–663. [Google Scholar] [CrossRef] [PubMed]
- Zhou, X.; Yu, X.; Wan, C.; Li, F.; Wang, Y.; Zhang, K.; Feng, L.; Wen, A.; Deng, J.; Li, S.; et al. NINJ1 regulates platelet activation and PANoptosis in septic disseminated intravascular coagulation. Int. J. Mol. Sci. 2023, 24, 4168. [Google Scholar] [CrossRef]
- Wang, X.; An, P.; Gu, Z.; Luo, Y.; Luo, J. Mitochondrial metal ion transport in cell metabolism and disease. Int. J. Mol. Sci. 2021, 22, 7525. [Google Scholar] [CrossRef]
- Jomova, K.; Makova, M.; Alomar, S.Y.; Alwasel, S.H.; Nepovimova, E.; Kuca, K.; Rhodes, C.J.; Valko, M. Essential metals in health and disease. Chem. Biol. Interact. 2022, 367, 110173. [Google Scholar] [CrossRef]
- Kokilambigai, K.S.; Kavitha, J.; Seetharaman, R.; Lakshmi, K.S.; Sai Susmitha, A. Analytical and bioanalytical techniques for the quantification of the calcium channel blocker—Amlodipine: A critical review. Crit. Rev. Anal. Chem. 2021, 51, 754–786. [Google Scholar] [CrossRef]
- Trikudanathan, G.; Wolbrink, D.R.J.; van Santvoort, H.C.; Mallery, S.; Freeman, M.; Besselink, M.G. Current concepts in severe acute and necrotizing pancreatitis: An evidence-based approach. Gastroenterology 2019, 156, 1994–2007. [Google Scholar] [CrossRef]
- Agupitan, A.D.; Neeson, P.; Williams, S.; Howitt, J.; Haupt, S.; Haupt, Y. P53: A guardian of immunity becomes its saboteur through mutation. Int. J. Mol. Sci. 2020, 21, 3452. [Google Scholar] [CrossRef]
- Chen, Q.; Xin, G.; Li, S.; Dong, Y.; Yu, X.; Wan, C.; Wei, Z.; Zhu, Y.; Zhang, K.; Wang, Y.; et al. Berberine-mediated REDD1 down-regulation ameliorates senescence of retinal pigment epithelium by interrupting the ROS-DDR positive feedback loop. Phytomedicine 2022, 104, 154181. [Google Scholar] [CrossRef]
- Jeon, S.; Kim, T.K.; Jeong, S.J.; Jung, I.-H.; Kim, N.; Lee, M.-N.; Sonn, S.-K.; Seo, S.; Jin, J.; Kweon, H.Y.; et al. Anti-inflammatory actions of soluble Ninjurin-1 ameliorate atherosclerosis. Circulation 2020, 142, 1736–1751. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Ren, H.; Gao, X.; Cai, D.; Shan, H.; Bai, J.; Sheng, L.; Jin, Y.; Zhou, X. Amlodipine improves spinal cord injury repair by inhibiting motoneuronal apoptosis through autophagy upregulation. Spine 2022, 47, E570–E578. [Google Scholar] [CrossRef] [PubMed]
- Haria, M.; Wagstaff, A.J. Amlodipine. A reappraisal of its pharmacological properties and therapeutic use in cardiovascular disease. Drugs 1995, 50, 560–586. [Google Scholar] [CrossRef] [PubMed]
- Perides, G.; van Acker, G.J.D.; Laukkarinen, J.M.; Steer, M.L. Experimental acute biliary pancreatitis induced by retrograde infusion of bile acids into the mouse pancreatic duct. Nat. Protoc. 2010, 5, 335–341. [Google Scholar] [CrossRef]
- Shen, Y.; Wen, L.; Zhang, R.; Wei, Z.; Shi, N.; Xiong, Q.; Xia, Q.; Xing, Z.; Zeng, Z.; Niu, H.; et al. Dihydrodiosgenin protects against experimental acute pancreatitis and associated lung injury through mitochondrial protection and PI3Kγ/Akt inhibition. Br. J. Pharmacol. 2018, 175, 1621–1636. [Google Scholar] [CrossRef]
- Zhang, X.; Xin, G.; Li, S.; Wei, Z.; Ming, Y.; Yuan, J.; Wen, E.; Xing, Z.; Yu, K.; Li, Y.; et al. Dehydrocholic acid ameliorates sodium taurocholate-induced acute biliary pancreatitis in mice. Biol. Pharm. Bull. 2020, 43, 985–993. [Google Scholar] [CrossRef]
- Qiao, Y.; Wang, L.; Hu, T.; Yin, D.; He, H.; He, M. Capsaicin protects cardiomyocytes against lipopolysaccharide-induced damage via 14-3-3γ-mediated autophagy augmentation. Front. Pharmacol. 2021, 12, 659015. [Google Scholar] [CrossRef]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, C.; Xin, G.; Li, F.; Wan, C.; Yu, X.; Feng, L.; Wen, A.; Cao, Y.; Huang, W. Calcium/P53/Ninjurin 1 Signaling Mediates Plasma Membrane Rupture of Acinar Cells in Severe Acute Pancreatitis. Int. J. Mol. Sci. 2023, 24, 11554. https://doi.org/10.3390/ijms241411554
Lee C, Xin G, Li F, Wan C, Yu X, Feng L, Wen A, Cao Y, Huang W. Calcium/P53/Ninjurin 1 Signaling Mediates Plasma Membrane Rupture of Acinar Cells in Severe Acute Pancreatitis. International Journal of Molecular Sciences. 2023; 24(14):11554. https://doi.org/10.3390/ijms241411554
Chicago/Turabian StyleLee, Chehao, Guang Xin, Fan Li, Chengyu Wan, Xiuxian Yu, Lijuan Feng, Ao Wen, Yu Cao, and Wen Huang. 2023. "Calcium/P53/Ninjurin 1 Signaling Mediates Plasma Membrane Rupture of Acinar Cells in Severe Acute Pancreatitis" International Journal of Molecular Sciences 24, no. 14: 11554. https://doi.org/10.3390/ijms241411554
APA StyleLee, C., Xin, G., Li, F., Wan, C., Yu, X., Feng, L., Wen, A., Cao, Y., & Huang, W. (2023). Calcium/P53/Ninjurin 1 Signaling Mediates Plasma Membrane Rupture of Acinar Cells in Severe Acute Pancreatitis. International Journal of Molecular Sciences, 24(14), 11554. https://doi.org/10.3390/ijms241411554




