Abstract
Calcific aortic valve stenosis (CAVS) is among the most common causes of cardiovascular mortality in an aging population worldwide. The pathomechanisms of CAVS are such a complex and multifactorial process that researchers are still making progress to understand its physiopathology as well as the complex players involved in CAVS pathogenesis. Currently, there is no successful and effective treatment to prevent or slow down the disease. Surgical and transcatheter valve replacement represents the only option available for treating CAVS. Insufficient oxygen availability (hypoxia) has a critical role in the pathogenesis of almost all CVDs. This process is orchestrated by the hallmark transcription factor, hypoxia-inducible factor 1 alpha subunit (HIF-1α), which plays a pivotal role in regulating various target hypoxic genes and metabolic adaptations. Recent studies have shown a great deal of interest in understanding the contribution of HIF-1α in the pathogenesis of CAVS. However, it is deeply intertwined with other major contributors, including sustained inflammation and mitochondrial impairments, which are attributed primarily to CAVS. The present review aims to cover the latest understanding of the complex interplay effect of hypoxia signaling pathways, mitochondrial dysfunction, and inflammation in CAVS. We propose further hypotheses and interconnections on the complexity of these impacts in a perspective of better understanding the pathophysiology. These interplays will be examined considering recent studies that shall help us better dissect the molecular mechanism to enable the design and development of potential future therapeutic approaches that can prevent or slow down CAVS processes.
1. Introduction
Heart valve diseases are a major contributor to cardiovascular morbidity and mortality worldwide. They affect more than 13% of the population aged over 75 years old and occur when any type of the four heart valves (tricuspid, pulmonic, mitral, and aortic valves) is damaged. Calcific aortic valve disease (CAVD) is defined as a slowly progressing condition that ranges from mild valve aortic sclerosis to severe calcifying aortic valve stenosis. This progression manifests in approximately 2% of individuals over 65 years old annually [1,2,3].
Calcific aortic valve stenosis (CAVS) remains one of the most rapidly increasing and common forms of heart valve disorders, prevailing in over 3.4% of the aged population, making it a major predominant and critical public health care and economic burden [4], and it entails 80% of the risk to develop heart failure (HF) or mortality by approximately 25% annually [5].
Despite the growing amount of evidence to better understand the factors underlying CAVS progression, today it remains unclear in terms of molecular and cellular mechanisms. Currently, no drug strategies exist to prevent or treat CAVS once symptoms occur and the only clinical option available is a surgical or transcatheter valve replacement. Since CAVS incidence increases with age, it becomes critically urgent to identify and emphasize the pathophysiological causes to ameliorate the current therapy. CAVS is a multifactorial and active process, with aging being the principal risk factor. Other relevant factors in CAVS have been reported including gender “male”, obesity, smoking, hypertension, increased triglyceride levels (TG), and high oxidative stress [6]. The aortic valve (AV) is largely an avascular tissue, where oxygen (O2) and nutrients within the AV occur via passive diffusion. With aging and the early phases of CAVD, the significant O2 demand of the inflammatory cells with the further thickening process of AV reduces and impedes O2 levels progressively, which turns the AV region hypoxic. Hypoxia-inducible factor 1 alpha subunit α (HIF-1α) is the primary sensor of hypoxia, and it mediates numerous responses and acts as a central modulator of several target genes in the human organism [7,8]. Studies have identified the expression of HIF-1α, a pro-angiogenic transcription factor, in the calcific leaflet nodule of aortic stenosis (AS) [9,10]. However, the further impact of HIF-1α at the onset of AV disorders is still to be explored. Hypoxia is reported as a promoter of angiogenesis. Indeed, it has been suggested that the involvement of HIF-1α induces the expression of vascular endothelial growth factor (VEGF), thereby stimulating neo-angiogenesis, a feature of valvular disorders, and increasing metabolic adaptation, affecting in return the valve phenotype [10,11]. Importantly, numerous pieces of evidence have documented the appearance of neovascularization throughout the progression of the calcification process [12,13]. The presence of neovessels exhibits an increased expression of vascular and intercellular adhesion molecules that have also been linked to the inflammatory response, bone development, and calcification progression [14,15].
Today, inflammation is still considered the main active player in the phases that precede calcification. It is deeply entwined among other major contributors such as mitochondrial dysfunctions, which have recently been identified as the main contributor to CAVS; however, cause–effect relationships are difficult to address.
This review aims to cover the most recent understanding of the impact of the hypoxia signaling pathways, mitochondrial dysfunction, and inflammation on a key condition of cardiovascular disease, which is “calcific aortic valve stenosis”. We will discuss the new molecular and cellular mechanisms involved in CAVS and will propose further critical hypotheses and interconnections on the complexity of these impacts with a perspective of better understanding the pathophysiology that shall help us to design further future potential therapeutic strategies in CAVS processes and research methodology. The following keywords were used to search the PubMed database: “inflammation and CAVS”, “mitochondria and CAVS”, and “Hypoxia signaling”. We also reviewed articles on the concepts of “inflammation and mitochondria” and “inflammation and hypoxia signaling”. Most recent original articles and review articles published and reported in the last four years were included.
2. Overview of the Calcific Aortic Valve Disease
Epidemiology and Histological Structure
Calcific aortic valve disease (CAVD) is a progressive heart valve disorder defined by an active process of remodeling with an uncontrolled formation of calcium nodules, valve mineralization, which leads to the consequent narrowing of the valve, to the restriction of the valvular area, and to serious problems in the correct blood flow.
CAVD is an important clinical problem because it is the most common heart valve disease; its frequency increases with age, and men are more affected than women. According to epidemiological studies, 2.8% of adults over 75 years old have some degree of CAVS, and one adult over 65 out of four presented valvular sclerosis [16].
A very recent study focused on the epidemiology of CAVD during the past 30 years by taking full advantage of estimates from the Global Burden of Diseases, Injuries, and Risk Factors 2019 [17,18]. The results obtained confirmed that the global number of incident cases of CAVD has increased continuously over the past 30 years and the prevalence is higher in men than in women. CAVD mortality is associated with three primary causes: high systolic blood pressure, a diet high in sodium, lead exposure, and age are all fundamental factors in CAVD incidence [19].
To note, the most common congenital heart disease is bicuspid AV, affecting 0.5% to 1.4% of the population [20,21]. Most of these patients develop stenosis and valvular calcification early in their lifetime with a faster progression [22]; an event that might be linked to genetic, mechanical, and biological factors [23]. Given the previous data, the clinical approaches against CAVD have received enhanced interest over the last decade, but, right now, the gold standard intervention for CAVD patients is valve replacement or the percutaneous implantation of valve prostheses, such as mechanical prostheses and bioprostheses [24]. This approach is common, life-saving, and certainly improves the patient’s quality of life but might have some side effects, such as the necessity for long-term anticoagulation therapy or failure of bioprostheses due to tissue degeneration and mineralization [25]. The one-way blood flow from the left ventricle to the aorta goes through the aortic heart valve without regurgitation. The AV possesses three leaflets with a trilaminar conformation covered by endothelium: a layer named fibrosa, on the aorta side, a central layer named spongiosa, and a layer named ventricularis, on the left ventricle side [26] (Figure 1). Each layer is important for the mechanical feature of the AV and has a different tissue composition. Fibrosa is rich in collagen fibers indispensable for strength and support, the most present cell type is valvular interstitial cells (VICs). The spongiosa layer consists of glycosaminoglycans and is responsible for absorbing shear stress; it also presents smooth muscle cells (SMC) with contractile function. Ventricularis is made of collagen and elastin fibers, which provide the dynamism of the valve. The valve leaflets are attached to the annulus, a fibrous ring, fundamental for their connection to the aortic root and the dissipation of mechanical energy [27].
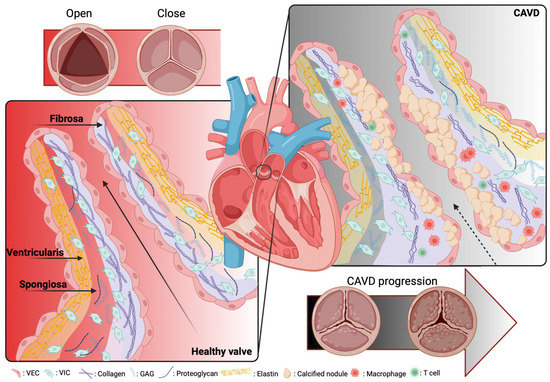
Figure 1.
Schematic representation of a native healthy and calcific aortic valve. The healthy aortic valve contains 3 layers of extracellular matrix termed fibrosa that consist of collagen, on the aorta side, a central layer named spongiosa contains proteoglycan and glycosaminoglycans, and a layer named ventricularis consists of elastin fiber, on the left ventricle side. The main cells in the aortic valve cusp core are the endothelial and the interstitial cells (the left) Therefore, in the pathological case, the valve cusp becomes thick and calcified on the surface of the fibrosa, with further fragmentation in the elastin fibers and the enhanced collagens (the right).
The main cellular components localized in the AV are VICs, present in all the layers, valvular endothelial cells (VECs) are on the surface of the leaflets, and there are a few SMCs, but only in the ventricularis layer [23]. VICs control matrix remodeling, they synthesize the extracellular matrix (ECM) and remodel collagen, maintaining normal valve structure; VECs are involved with VICs in the maintenance of the integrity of valve tissues [14,15].
CAVD is a multistep process that starts at the early stage with aortic sclerosis, characterized firstly by endothelial dysfunction, then by mechanical stress, lipid accumulation in the tissue and their subsequent oxidation, and then by initiating an inflammatory response with the infiltration of inflammatory cells, T cells, and macrophages [28]. A second phase is characterized by fibrosis and accelerated calcification; in fact, the inflammation process in stenotic valves leads VICs to differentiate myofibroblasts, which actuate matrix remodeling through the activation of matrix metalloproteinase (MMP) enzymes [29,30].
Along with stenosis, a key feature of this pathological condition is the calcification process, resulting from the activation of several osteogenesis pathways [31]. The increased lipid deposition induces VICs to change their phenotype through osteogenic differentiation, producing spheroid calcium phosphate particles, leading irreversibly to leaflet stiffening [32,33,34].
3. The Complex Interplay of Hypoxia Signaling, Mitochondrial Dysfunction, and Inflammation
3.1. Hypoxia Signaling and Molecular Regulation of HIF-1
Hypoxia plays a critical role in CVDs and is orchestrated by a hallmark heterodimer trans-acting DNA-binding hypoxia-inducible transcription factors (HIFs), which are key regulators mediating adaptation to hypoxic conditions and are modulated by an O2-sensitive-expressed alpha subunit (HIF-1α) (or its analogs HIF-2α and HIF-3α). In normal conditions, HIF-1α is continuously synthesized and hydroxylated through HIF prolyl-4-hydroxylases, leading to its rapid ubiquitination and proteasomal degradation (ubiquitin proteasome 26S), the von Hippel–Lindau (pVHL) function as a tumor suppressor binds to the ubiquitin ligase complex E3 targeting the HIF-1α subunit destruction in the O2 degradation domain, causing its short life. In contrast, under hypoxia, HIF-1α hydroxylation is suppressed through the inhibition of the O2-dependent propyl-hydroxylase-1, -2, and -3 enzyme activity (PHD1, -2, and -3), leading to the stabilization of HIF-1α in the cytosol, and migrates to the nucleus, where it forms a heterodimer with the beta subunits (HIF-1β, aryl hydrocarbon receptor nuclear translocator, ARNT) that bind to a core putative regulatory sequence called hypoxia response elements (HRE) with a consensus sequence (5′-RCGTG-3′) in the promoter or enhancer of target genes to enhance a concerted transcriptional response during a hypoxic condition [35] (Figure 2). Both α and β subunits have basic helix-loop-helix (bHLH) motifs, a DNA-binding domain that can bind HREs to target specific genes [8,36]. The transcription activity of the target genes requires not only the transfer of HIF-1α to the nucleus but also the complex HIF-1 requires the recruitment of multiple cofactors such as CREB-binding protein (CBP)/p300 and transcription intermediary factor 2 steroid-receptor activator that binds to the CTAD domain, and another cofactor that increases the HIF-1/HRE complex binding the M2 isoform of pyruvate kinase (PKM2) [37]. The canonical sensor of hypoxia, HIF-1α, mediates a cellular response during hypoxic conditions through the regulation of the transcription activity of enormous target genes, termed hypoxia-inducible genes encoding proteins, as examples: the lactate dehydrogenase-A (LDH-A) or pyruvate dehydrogenase kinase isoform 1 (PDK) [38,39]; VEGF-A [40]; erythropoietin (EPO) [41]; and inducible nitric oxide synthase (iNOS) [42], which are needed for improving tissue O2 homeostasis, energy metabolism, and efficient management of hypoxia-induced toxic stress, and elicit a crucial impact in various CVDs, such as ischemic heart disease (IHD) and HF [7,43]. HIF-2α, the analog of HIF-1α, is also termed endothelial PAS domain protein-1 (EPAS-1), and is predominantly enriched within endothelial cells and in highly vascularized tissues [44]. These two subunits (HIF-1α and HIF-2α) contain different spatial expressions in IHD, for example, and various effects in response to hypoxia [45]. Despite the recent interest in studying hypoxia and HIF-1 in CVDs, their role at the onset of CAVS remains unclear and requires deep further investigation.
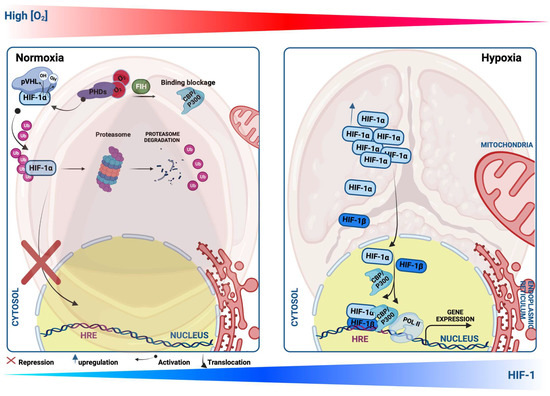
Figure 2.
Schematic illustration showing Hypoxia-inducible factor-1 α (HIF-1α) protein regulation during normoxia and hypoxia. Under the normoxic condition, HIF-1α protein is hydroxylated by propyl-hydroxylases (PHDs) and factor-inhibiting HIF (FIH), which facilitate the binding of HIF-1α with the von Hippel–Lindau protein (pVHL), leading to its ubiquitination, and thus proteasomal degradation. Upon the PHD inhibition or hypoxic condition, HIF-1α translocates to the nucleus, where it heterodimerizes with HIF-1β and binds to a core putative sequences of target genes termed hypoxia response element (HRE) and stimulates their transcriptional activity.
3.2. Hypoxia Signaling and Inflammation in CAVD
The heart AV is an avascular tissue able to sustain metabolic activity, nutrition, and oxygenation through passive diffusion. Nevertheless, with age, the initiation of CAVS is exhibited by endothelial injury triggered by shear stress, lipid deposition, and inflammation [46]. In these early stages of CAVS, the thickening of the valve process compromises the diffusion of O2, resulting in tissue hypoxia, while the CAVS progression occurs through the abnormal remodeling of the ECM, which is modulated by the valve interstitial cells [47,48]. Sustained stimulation of hypoxia maintains HIF-1α signaling, leading to the upregulation of inflammation and fibrosis, but these effects are counterbalanced by sustained HIF-2α signaling, potentially linked to mitochondrial and peroxisomal abnormalities [49]. It is demonstrated that during hypoxia, HIF-1α and HIF-2α are activated and both can transactivate VEGF expression [50,51,52]. HIF-1α is reported to initiate the process of angiogenesis, while HIF-2α is required for vascular network maturation [53,54,55]. Nevertheless, it is not yet established whether HIF-2α contributes to the angiogenesis maturation and regenerative process in CAVS.
Hypoxia has been recently identified in both the aortic and mitral valves [56,57]. Moreover, diseased valvular interstitial cells in regions surrounding calcific nodules have been found to express HIF-1α, which is a pro-angiogenic transcription factor [9,10]. Additionally, in human aortic endothelial cells (HAVEC), the level of HIF-1α mRNA and protein expression are identified as elevated in response to disturbed flow as opposed to stable flow [58]. A study has demonstrated the significant upregulation of HIF-1α in the stenotic valves and its colocalization with angiogenesis in areas calcified [10]. These findings suggest a further key role of HIF-1α in influencing the valve phenotype through the induction of VEGF expression, thereby activating neo-angiogenesis, a feature of valvular disorders, to increase metabolic adaptation [10,59]. In contrast to the upregulation of pro-angiogenic factors, anti-angiogenic factors have been identified as suppressed [60,61,62]. Furthermore, there are five VEGF family growth factors that bind to specific tyrosine kinase receptors and play important roles in the formation of new blood vessels and lymphatic vessels [63,64]. Among the VEGF receptors is the soluble fms-like tyrosine kinase 1 (sFlt1), an anti-angiogenic component that sustains AV avascularity [65].
A recent study by Lewis and colleagues has shown that sFlt1 is expressed in the native normal AV, but its expression level is significantly downregulated in patients with CAVS [65]. The authors demonstrated for the first time the dual roles of hypoxia in stimulating angiogenesis in CAVS, as the classical way by inducing VEGF-A and by inhibiting the sFlt1 expression, which could elevate inflammation, thus contributing to CAVS progression [65]. Sphingosine 1-phosphate (SP1) is a bioactive lipid signaling mediator shown to inhibit angiogenesis via the activation of sFlt1 expression in CAVS patients [65]. However, the link between HIFs (HIF-1α and HIF-2α) and sFlt1 has not been studied yet in CAVS, and its mechanism of action in response to hypoxia is not clear. To our knowledge, the relationship between sFlt1 and HIFs in response to hypoxia has been studied only in the pathogenesis of Preeclampsia, the onset of hypertension during pregnancy [66,67]. The relationship between HIF-1 and sFlt1 needs to be studied to understand further the molecular mechanisms behind this process in CAVS. Prior studies have shown that sFlt1 induces inflammation in VICs when it synergizes with lipopolysaccharide (LPS), which is a major component of the outer membrane of Gram-negative bacteria [68]. LPS drives the activation of Toll-like receptor 4 (TLR4), a key receptor of innate and adaptive immunity, stimulating the inflammatory (interleukin 6 and 8 (IL-6, IL-8), and intercellular adhesion molecule-1 (ICAM-1)) and osteogenic responses (bone morphogenetic protein-2 (BMP-2) and runt-related transcription factor 2 (RUNX2) in CAVS patients [69,70]. IL-37 is a novel cytokine member of the IL-1 family and plays a potential role in suppressing inflammatory responses, identified as downregulated in CAVS [71,72]. The lower levels of IL-37 observed in CAVS patients have been explained by M1 macrophage infiltration in pathological AV stenosis (AVs). IL-37 inhibits the macrophages polarization M1 (reduction in IL-6, MCP-1, iNOS, and the surface marker of M1 (CD11c)) via the suppression of nuclear factor kappa B (NF-κB) and Notch homolog 1, translocation-associated (Notch1) signaling pathways [73]. Along with that, IL-37 is reported as a potent anti-osteogenic in AVICs from patients, through the suppression of the NF-κB and extracellular signal-regulated kinase (ERK1/2) [72]. The anti-inflammatory response of IL-37 is associated with NF-κB, suppressing the TLR4 ligand LPS-mediated IL-6, IL-8, monocyte chemoattractant protein-1 (MCP-1), and ICAM-1 stimulation in AVICs from patients [74], thus playing a critical role in CAVS physiopathology. Noteworthy, IL-37 is capable of inducing other anti-inflammatory pathways including the AMP-activated protein kinase (AMPK) and Phosphatase and tensin homolog, which may impact NF-κB stimulation in CAVS [71]. Morciano and colleagues have shown the correlation of both pro-inflammatory cytokine levels of IL-18 and IL-1β—which both belong to the IL-1 family—in CAVS [46]. Furthermore, IL-1β has been found to stimulate mTORC1, and, downstream, it enhances HIF-1α activity in several diseases [75]. The expression of the HIF-1α protein is induced by IL-1β in normoxia in multiple cell types [76,77,78]. For instance, HIF-2α is one among the different signaling pathways that are involved in M1 infiltration [79], but is yet to be studied in macrophages of AVICs. Previous studies have shed light on better understanding the further relationship between HIF-1, Signal Transducer and Activator of Transcription 3 (STAT3), and IL-37 in cancer disorders [80]. This would increase further interest in a deep understanding of the crosstalk of the IL-37 and HIF-1 in the pathogenesis of CAVS. Evidence has confirmed the upregulation of HIF-1α and its analog HIF-2α in valve stenosis. Interestingly, HIF-2α co-localizes with NF-κB in regions of calcified lesions of AS of patients [52]. These findings have been correlated positively with the enhanced levels of VEGF and the formation of neovessels [52]. On the other hand, it is well known that the expression of VEGF can also be increased by inflammatory cytokines [81]. The findings indicate further convergence between hypoxia and inflammatory mechanisms involved in the remodeling of the valve ECM, which contributes to VIC stimulation and calcification. It has been shown that the HIF-1α activates the expression of various proteins involved in ECM remodeling including the Neutrophil Gelatinase-Associated Lipocalin [82,83] and the MMP2 and MMP9, suggesting the key impact of hypoxia in ECM remodeling.
In light of the previous findings, a novel immune non-hypoxic process entailing the combination between LPS and interferon-γ (IFN-γ) has been explored to stimulate calcification in AVICs from patients, through the STAT1/HIF-1α signaling pathway [84]. Interestingly, this response to HIF-1α stimulation mediated by LPS is sex-dependent, as it is more robust in VICs from male donors compared to females [84]. The Janus kinases (JAK)-STAT signaling pathways are hallmark regulatory routes contributing to several cytokine responses activating mineralization and calcification of AV interstitial tissues, including IL-6 and IFN-γ [84,85,86]. Notably, the study of Parra-Izquierdo and colleagues also suggests further a relationship between JAK-STAT and HIF-1α-dependent sex differences in the context of CAVS [84]. However, females display lower responses and tend to be more protective compared with males due to the activation of the phosphatidylinositol 3-kinase (PI3K)-AKT signaling survival pathways [87]. Nevertheless, more research is needed to fully understand these relationships.
These findings propose the further potential involvement of HIF-1α in normoxia and in the early phases of CAVS when the hypoxic event is not yet activated; however, it is not known how LPS and/or IFN-γ could stabilize HIF-1α. Since the stabilization of HIF-1α is regulated by prolyl-4-hydroxylases under normoxic conditions, it is therefore possible that LPS and/or IFN-γ treatment could cause a decrease in hydroxylation, leading to the activation of HIF-1α. Other pioneer evidence supports the upregulation of HIF-1α in normoxic conditions—mediating the calcification process in AVICs. The ubiquitin E2 ligase C (UBE2C) is a member of the Anaphase Promoting Complex/Cyclosome (APC/C), which has been reported to also bind pVHL [88]. UBE2C upregulates the endothelial–mesenchymal transition (EndMT) and endothelial AV inflammation via the stimulation of HIF-1α levels through further ubiquitination and degradation of its upstream modulator pVHL, and this was accompanied by the reduction in microRNA-483–3p (miR-483) in HAECs [58]. In addition, the miR-483 mimics and the pharmacological suppressor of HIF-1α (PX478) significantly downregulate the porcine AV calcification through UBE2C reduction [58]. Other evidence supports the involvement of HIF-1α in valve calcification: PX478 significantly blocked the deposition of calcium resulting from distributed flow, and the response was more effective in male valve interstitial cells [10,11]. Other in vitro studies have identified the increased expression levels of HIF-1 signaling pathways including IL-6, HIF-1α, and Heme Oxygenase 1 (HMOX1) in CAVS-related ferroptosis signaling pathways [89]. Hence, one of the causes of ferroptosis is an iron overload that is involved in CAVS by enhancing calcium deposition and calcification in endothelial cells (HUVEC) [90]. It is identified that the endothelial cells play crucial impacts in the calcification process through the EndMT [91]. Multiple pathways are involved in this process including the signaling pathways involved in hypoxia and inflammation, such as the transforming growth factor beta (TGF-β) signaling pathway [92], and the Wnt signaling pathway [93,94].
In the same regard, inflammation is also triggered by fetuin-A (alpha2-Heremans Schmid glycoprotein); a 59 kDa glycoprotein synthesized in the liver, emerges as a potent circulating inhibitor of the calcification process, modulates macrophage polarization, and attenuates inflammation and fibrosis [95]. Intracellular fetuin-A suppresses calcification stimulated by transforming growth factor-β and bone morphogenetic proteins [96,97]. In addition, previous works have conflicting results on circulating fetuin-A as a biomarker for CAVD. Nevertheless, a meta-analysis demonstrated significantly lower levels of fetuin-A in AS patients compared to healthy conditions; also, fetuin-A levels have been significantly identified as being associated with CVD risk factors including age, male gender, smoking, low-density lipoprotein (LDL) and TG, hypertension, and diabetes [98]. Studies have shown an inverse correlation between fetuin-A levels and the progression of calcific AV and underlined diminished fetuin-A levels in AV sclerosis patients, the early asymptomatic phase of CAVD, suggesting that fetuin-A is an early calcification biomarker [99,100]. These studies suggest further involvement of fetuin-A in the initiation of AV calcification, hence raising the concept that fetuin-A, as an inhibitor of calcification, may prevent valvular calcifications when the calcium phosphate is disrupted, suggesting its correlation to calcium tissue deposition [101], and its levels, is also associated with inflammation and other comorbidities such as chronic kidney disease and diabetes [102]. In a very recent study, Chen et al. demonstrated the involvement of Fetuin-A in calcific osteogenic environment-induced VICs calcification, and in parallel, its level reported the decreased inhibition of miR-101 taking place [103]. However, the role of fetuin-A in the progression of CAVD has not been clearly investigated. Therefore, relationships of fetuin-A with tissue calcification and cardiovascular diseases in general are divergent, reflecting its diverse action. Notably, beyond the role of fetuin-A as a calcification suppressor in the serum phase, it acts as a potent calcium mineral scavenger, preventing the ectopic pathological calcification of the tissue especially in response to hypoxic stress in renal tissue remodeling upon IH injury [95]. Recently, fetuin-A has been identified as an evolutionary target gene of HIF-1 [104]; however, the correlation between HIF-1 and fetuin-A is still unclear in CAVS. Further understanding the complex interplay between HIF-1, fetuin-A, and pro-inflammatory cytokine in CAVS patients would pave the way to better predict the presence of CAVS and may provide further molecular targeting strategies.
3.3. Mitochondrial Impairment in CAVD
Mitochondria have key roles in eukaryotic cells, as they control several cellular mechanisms such as bioenergetics, signal transduction, and energy metabolism. Furthermore, these organelles are major regulators and executioners of cell death mechanisms, in particular autophagy and apoptosis [105]. To regulate these processes, cells have to preserve a functional mitochondrial population, a fundamental aspect allowed by the mitochondrial quality control system, in which mitochondrial dynamics, mitochondrial biogenesis, and mitochondrial autophagy (named mitophagy) are the main events [106]. Fusion and fission help to keep mitochondrial structure integrity and are necessary steps to improve metabolism and facilitate cooperation and communication between mitochondria [107]. At the same time, erroneous fission and fusion events may provoke the formation of a nonfunctional mitochondria population, which can induce the production of damaged elements (such as mitochondrial reactive oxygen species) that are harmful for the entire mitochondria population and for the cell. Injured mitochondria can be removed by the degradative process, mitophagy, which recognizes and sequesters the damaged organelle into autophagy vesicles, which are then delivered to the lysosome for degradation [108]. Finally, preserving the adequate mitochondrial number of the cell may intervene in mitochondrial biogenesis that is responsible for generating new mitochondrial offspring [109]. Decline and/or sustained activation of these molecular mechanisms deputed to control the mitochondrial amount and quality has been associated with several human diseases, in particular, mitochondrial diseases [110], genetic disorders [111], neurodegeneration [112,113], cancer [114], and cardiovascular disorders [46].
For instance, immunostained calcified human AVs revealed high levels of the mitochondrial fission initiator protein dynamin-related protein 1 (DRP1). Inhibition of DRP1 via RNA interference promotes a reduction in the osteogenic differentiation process and inhibits oxidative stress [115]. A more recent study highlighted the overexpression of protein tyrosine phosphatase 1B (PTP1B) in CAVD [116]. PTP1B is a negative regulator of the leptin and insulin signaling pathways, which are involved in the regulation of mitochondrial dynamics and biogenesis [117,118]. The authors demonstrate the decreased osteogenic differentiation of interstitial valvular cells by the pharmacological inhibition of PTPB1. This effect is accompanied by an upregulation of mitochondrial biogenesis, which has been observed to be downregulated during the progression of valvular calcification [116]. Morciano et al. revealed the presence of aged mitochondria together with reduced PGC-1α expression, a key mitochondrial biogenesis protein, in interstitial cells isolated from human patients [46]. Impairment of mitochondrial biogenesis in CAVS is associated with increased cell death and the presence of aged mitochondria, despite an increase in mitophagy and autophagy fluxes, suggesting an insufficient turnover of mitochondria in CAVD samples. Moreover, the authors revealed for the first time the presence of other mitochondrial impairments in CAVD patients, such as calcium dysregulation, reduced respiratory capacity, and lack of ATP production [46].
The gene expression profile of AV tissue identified several novel genes associated with mitochondrial functions variations that are involved in the pathogenesis of CAVD, such as an increase in reactive oxygen species (ROS) production and reduced mitochondrial membrane potential, metabolic imbalance, and mitochondrial fragmentation [119]. Moreover, the authors suggest that integrated miRNA/mRNA analyses might be used as diagnostic biomarkers for CAVD [119]. Interestingly, they later identified matrix metalloproteinase 9 expression (MMP9), a mitochondrial-related gene, as being extremely high in AS samples, which would be a useful biomarker for aortic stenosis [120].
Inside the cell, Calcium (Ca2+) is one of the major second messengers and regulates a plethora of biological processes, such as metabolism, antioxidant defense, apoptosis, muscle contraction, neurotransmitter release, and also mitochondrial functioning [121]. Therefore, it is not surprising that dysregulations of Ca2+ dynamics are involved in different pathologies [122]. In the context of aortic calcification, evidence that connects aortic stenosis and Ca2+ dysregulation goes back to a genome-wide association study [123], where calcified valves reveal the upregulation of mRNA levels of RUNX2 concomitant with an increased calcium voltage-gated channel subunit alpha 1 C (CACNA1C) gene [123], which encodes the CaV1.2 L-type voltage-gated Ca2+ channel. Later, these data were confirmed by another study, which demonstrated a higher Ca2+ influx in CAVD patients through the CaV1.2 channel [124].
VEGF is a target gene of HIF-1α that regulates several cellular processes including proliferation, cell survival, differentiation, and migration [125]. Xu et al. have demonstrated the impact of VEGF in sustaining the mitochondrial fission and fusion balance, mitigating the mitochondrial apoptotic pathway; thereby, VEGF could play a critical role in repairing the AS transition from compensatory cardiac hypertrophy to HF in mouse animal models [125].
It is important to note that patients with AS exhibit a metabolic shift from fatty acid to glucose metabolism, which is characterized by a decreased expression of fatty acid translocase (FAT/CD36) protein, together with a downregulation of other fatty acid transporters, such as plasma membrane and heart-type cytosolic fatty acid binding proteins (FABPpm and H-FABP), β-oxidation, Krebs cycle, and oxidative phosphorylation proteins. On the contrary, the same cardiac biopsy exhibits an increased expression of glucose transporter 1 and 4 (Glut 1, 4). This study suggests a downregulation of fatty acid oxidation proportionally to a more severe outcome in patients with aortic stenosis [126]. Nonetheless, whether this metabolic shift in CAVS patients results from the involvement of mitochondrial ROS (mtROS) in instigating AV calcification or whether another mediator contributes to this process remains unknown.
Notably, such a metabolic shift to glycolysis is well demonstrated in various CVDs orchestrated by HIF-1α; however, its effect on the metabolism adaptation in CAVD is yet to be explored. HIF-1α regulates multiple genes influencing mitochondrial activity and is crucial for the metabolic shift, such as LDH-A and phosphoglycerate kinase-1 (PGK1) [127], thus elevating anaerobic glycolysis by enhancing the generation of glycolysis enzymes, increasing glucose transporters expression (e.g., Glut 1, 4), and inhibiting mitochondrial energy metabolism [128,129], while impeding fatty acid oxidation [7,130]. Several studies have supported the notion that HIF-1α plays a significant role in oxidative stress, as its expression level is intrinsically associated with mtROS in response to O2 deprivation [7,131].
Furthermore, it has been reported that human calcified valves are enriched in oxidative stress, worsening the progression of calcification [132]. The increased oxidative stress levels seem to be inversely proportional to antioxidant enzyme expression and functionality, as well as the uncoupling nitric oxide synthase (NOS) activation [133,134]. Together these data illustrate the crucial role of mitochondria in the pathophysiology of CAVD.
3.4. Relationship between Inflammation and Mitochondria in CAVD
As we reviewed in the previous paragraphs, the inflammatory response has been the only known mediator of CAVD in the past [135,136], and its connection with the onset and progression of the disease that resulted in either surgical valve replacement or transcatheter AV implantation has been extensively reported [26,137]. Indeed, a significant amount of clinical data, extrapolated from patients affected by AS, showed with different techniques, high levels of inflammation. In the 1990s, aortic valvular lesions from this cohort of patients were carefully analyzed through popular biochemical approaches; the native tissue appeared as being characterized by thickening, by a large amount of lipids deposition, and by the presence of mineralization and calcium accumulation into the leaflet (Figure 3). Concurrently, a high grade of inflammatory infiltrate with foam cell macrophages was present in the lesions [138]. From plasma samples of AS patients, IL-1β and IL-18 were the main circulating cytokines to be overexpressed [46]; however, IL-6 and TNF have also been reported to play a role in osteogenic differentiation with a significant pool of M1 polarized macrophages [139]. In 2012, Dweck MR and co-workers used for the first time the positron emission tomography (PET) and two common PET tracers, 18F-Flurodeoxyglucose (18F-FDG) and 18F-Sodium fluoride (18F-NaF), which were able to target calcification and inflammation into the same patient [140]. They found the inflammatory response increased by 91% in AS patients compared to healthy subjects [140].
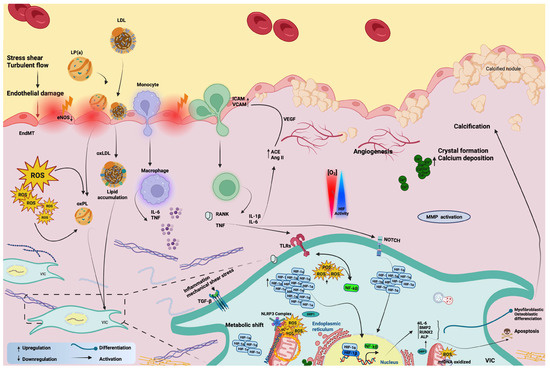
Figure 3.
A diagram representing the contribution of inflammation, mitochondrial dysfunction, and hypoxia signaling in the pathophysiology of the calcific aortic valve.
Today, inflammation is still considered to be the main active player in the phases that precede calcification, but it is deeply nestled among other major contributors such as mitochondrial dysfunctions for which cause–effect relationships are difficult to address [26,46,141,142].
The link between mitochondria and inflammation is very close. A seminal paper by Zhong Z. and co-workers showed how mitochondria directly orchestrate signals from TLR to produce oxidized mtDNA fragments, needed to activate NLRP3 inflammasomes once they have moved into the cytosol [143]. Basically, according to this evidence, mitochondria constitute a reservoir of many signaling substances. A pool of these, once released into the cytosol, becomes harmful and can trigger mitochondria-mediated inflammation through multiple receptor-dependent responses [144]. These are the so-called mitochondrial danger-associated molecular patterns (mtDAMPS) and include, for example, ATP, mtDNA, and mtROS.
NLRP3 is a multiprotein platform that is activated by mtDAMPS; it relocalizes to mitochondria and associated membranes and plays a crucial role in CAVD through the production of the mature form of IL-1β [145]. This cytokine is consistently upregulated in CAVD patients, is highly expressed in situ in calcified areas, and further sustains inflammation, stimulating IL-6 and IL-8 production and activating the NF-kB pathway [146]. It is documented that IL-1β activates HIF-1α to stimulate a metabolic shift from oxidative phosphorylation (OXPHOS) to glycolysis, which is crucial in adaptive immunity [147]. The exacerbation of the inflammatory phenotype is also given by the enhancement of the MPP1 function with drastic changes in the extracellular matrix composition [148]. Accordingly, the antagonization of the IL-1 receptor by the IL-1 receptor antagonist (Ra) has been shown to block the proinflammatory pathway [149], conferring on the receptor properties targeted for cardioprotection. Moreover, its genetic depletion in animal models of CAVD has definitively shown its crucial contribution to the calcification process of the AV [149].
Additionally, to the aforementioned studies in the previous sections, HIF-1α upregulates mtROS levels, stimulates the NF-kB transcription factor, and activates inflammasome genes expression, including NOD-, LRR-, and pyrin domain-containing protein (NLRC)4, NLRP3, and the IL-1β genes. Thereby, leading to mitochondrial oxidative stress, affecting in return mitochondrial membrane permeability, lipid peroxidation, and mtDNA, as a consequence of mitochondrial abnormalities [7].
Mitochondria are also a place where ROS are produced in great amounts, mainly as end-products from OXPHOS [150]. ROS are usually culprits of mitochondrial damage in cardiovascular diseases, especially when an overproduction of free radicals or impairment of the ROS-scavenging enzyme system occurs [151,152,153,154]; moreover, ROS further sustain inflammation [155]. In the last few years, evidence involving mtROS in CAVD has become manifold. First studies carried out on isolated ex vivo cultures from human valve samples demonstrated how the presence of lipoprotein a (Lp(a)) selectively triggered acute superoxide production from mitochondria, [156] and through it, Lp(a) chronically lead to cell calcification. Lp(a) induces significant calcium deposition in vitro, and patients with CAVD have higher plasma levels of Lp(a) [157,158]. mtROS reached high levels in a few hours after Lp(a) exposure, but the calcification followed in several days. This evidence ascribes a role for mtROS generation in the acute stages of the disease, but it is still in doubt if they can be targeted to revert the pathological phenotype once the CAVD condition is established.
In addition to Lp(a), another apolipoprotein named ApoC-III was found to be involved in functions far from their primary role in metabolism [141]. Similarly, ApoC-III was detected in large amounts around the calcific regions of human AV leaflets and was directly related to the calcification grade [141]. The process was further monitored in vitro through the chronic treatment of normal noncalcified interstitial cells with ApoC-III, which led to calcification in a few days. The pathological process was accompanied by an increase in several mitochondrial proteins involved in oxidative stress and in the inflammatory cascade with the upregulation of IL-6 and BMP-2 expression [141]. Among the signs of mitochondrial stress during calcification, the expression of superoxide dismutase 2 (SOD2), HSP60, HtrA Serine Peptidase 2 (HTRA2), and Caseinolytic Mitochondrial Matrix Peptidase Proteolytic Subunit (CLPP) are the most affected proteins. They usually participate in apoptotic and mitophagic pathways [159]. Inflammation in CAVD also acts via TNF-α. There was an acute increase in the number of cytokines at 30 min and chronically, at 21 days, associated with a significant induction of mtROS [160]. These results were only observational without any correlation to the calcific phenotype. Besides the involvement of HSP60, the downregulated expression of HSP90 has also been revealed in a proteomic analysis of CAVD, leading to ROS generation and endothelial alterations [161].
The organized interplay between mtROS and inflammation also participates in the calcification process by regulating the osteogenic differentiation of vascular smooth muscle cells (VSMC) through the fine-tuning of RUNX2 expression [162]. Furthermore, mtROS are generated by mitochondrial carbonic anhydrases, enzymes that result in upregulation in calcified aortic tissues [163]. The inhibition of their function alleviates both inflammation and the calcification process to which VSMCs are subjected [163].
Besides this partially direct evidence of the contribution of mitochondria to inflammation through mtROS release and linked to mitochondrial stress, a study by Smyrnias, in 2019, described the presence of a dysfunctional mitochondrial unfolded protein response (mtUPR) in patients affected by AS. The role of mtUPR in heart and cardiac diseases is unclear, but this work showed how patients having a higher activation of mtUPR also have a lower rate of myocyte death and fibrosis/calcification levels [164].
4. Novel Insights on the Therapeutic Strategies of CAVS
Despite the increasing amount of evidence to better comprehend the factors underlying CAVS progression. Nowadays, this disorder is a major growing challenge, and it remains unclear in terms of molecular and cellular mechanisms, and presently no therapeutic strategies successfully exist to prevent or treat CAVS. Only surgical intervention or transcatheter valve replacement is an efficient treatment option for CAVS. Nevertheless, it is well recognized that these types of therapeutic options are highly complicated, in which the surgical implantation of an artificial valve requires lifelong antithrombotic therapy, and the bioprosthetic valves are prone to deterioration over time, requiring patients to have a further operation, as well as a higher risk of thromboembolism due to the reduced flow and pressure [165,166]. To the best of our knowledge, at present, no therapeutic strategies successfully exist yet to prevent or treat CAVS; therefore, the development of a potent medical therapy for CAVS becomes a major urgent necessity to reverse the development of the disease and ameliorate the clinical outcomes. To attain this noble purpose, it is highly necessary to deeply focus and target the molecular/cellular mechanisms for a better understanding of the etiopathology. In Table 1, we report an updated list of the most promising therapeutic options for CAVS.
In recent years, so much has been learned about novel promising pharmacotherapy for CVDs. From the pool of molecules, one favorable molecule is HIF-1α, which has been shown to act as a cardio-protectant in different aspects of CVDs. However, very little has been explored regarding its role in CAVS. A few studies showing the involvement of HIF-1α in CAVS are addressed in the earlier sections of this review but none have demonstrated HIF-1α’s role in the staging of calcification. It has been very recently discovered that HIF-1α expression can be blocked by PX-478 and miR-483 mimics, which are novel stretch-sensitive and flow-sensitive disease molecules, respectively. Thus, they convey a novel potent target to develop an innovative therapeutic strategy to alleviate CAVD [58,167]. Further studies are required to study the different members of the HIF family in CAVS.
Dimethylloxetane, an inhibitor of HIF-1α, downregulates osteogenic transcription factors including RUNX2 and BMP-2, thereby reducing vascular calcification in ovariectomized rats. In addition, estrogen drug therapy alleviates HIF-1α expression and vascular calcification [168]. Indeed, studies have also documented the role of estrogen as a negative modulator of several mechanisms, such as inhibiting NFκB signaling and the receptor–activator of nuclear factor κB ligand (RANKL) [71,130], blocking p53 activity [169], inhibiting the activity of NADPH oxidase, and causing inflammation [24,153]. Moreover, regarding its role mentioned previously, as a negative modulator, estrogen can direct the activation of antioxidant enzymes in mitochondria, in the lysosome, and in the cytosol to enhance NOX expression and contribute to the protective impact in calcification [170,171]. Another inhibitor of HIF-1α that still needs to be better investigated in cardiovascular calcification is the HIF-1α mRNA antagonist EZN-2968, [172]. Studies are necessary to unveil whether it could be a therapeutic alternative to treat vascular calcifications in the future.
Hypoxia has been reported to contribute to the early development of the disorder and stimulate HAVIC proliferation. Hypoxia is a canonical stimulator of the angiogenesis process through HIF-1 transcription activity. A novel correlation between hypoxia and pro-angiogenic conditions has been recently demonstrated in CAVS [65]. Furthermore, hypoxia modulates angiogenesis in CAVS through the activation of VEGF receptor sFlt1 expression, which is an anti-angiogenic component where its released mechanism action is still unknown [65]. Inhibiting the angiogenesis process has demonstrated a potential target to treat various disorders, such as cancer [173,174], and CVD including myocardial infarction [175]. In a recent study, S1P is identified to halt the formation of neo-vessels by targeting sFlt1 in CAVS [65], suggesting further future therapeutic approaches to stimulate the S1P receptors in CAVS to limit the progression of the disorder. Treatments used for vascular problems have been suggested to ameliorate CAVS outcomes; however, it is well-known that the molecular mechanisms of CAVS are different from vascular disorders [176].
Angiotensin-II (Ang-II) plays a crucial role in CAVS progression. It upregulates IL-6 generation to stimulate cardiac fibrosis and to stimulate the osteogenic differentiation of valve interstitial cells [177,178]. Inhibitors of Angiotensin-converting enzyme (ACE-I) or Ang-II receptors have been widely used for hypertension treatment and have been explored in CAVS progression and the multiple severities of CAVS [179,180]. ACE-I therapy is correlated with reduced CAVS and a slowdown in mild CAVS development [181,182]. Indeed, ACE-I therapy has shown amelioration in the hemodynamic and left ventricular (LV) hypertrophy in patients with moderate and severe CAVS in randomized clinical trials, for example, the RIAS [183,184]. In the same regard, potent blockers of Ang-II such as fimasartan and losartan have shown a beneficial impact in severe CAVS patients with hypertension (clinicaltrials.gov/NCT03666351). Moreover, the targeting of renin–angiotensin–angiotensinogen system (RAAS) inhibitor therapy may impede CAVS progression and reduce the mortality risk in CAVS patients [185]. Thus, large-scale trials are needed to dissect this further therapy in delaying the development of CAVS.
KPT-330 is a potent selective exportin-1 (XPO1) inhibitor, widely involved in cancer disorders, which regulates the expression of cyclin D1 [186]. KPT-330 has shown an effective impact in vitro to mitigate calcific nodule formation protecting against CAVS through a novel CCAAT/enhancing-binding protein (C/EBPβ) signaling pathway, suggesting KPT-330 as an alternative pharmaco-based therapy to treat CAVS [187].
Melatonin (N-acetyl-5-methoxytryptamine) is a pleiotropic molecule with cardioprotective effects, maintains mitochondrial function via its antioxidant activities, and impedes the opening of the permeability transition pore complex (PTPC) [188]. Notably, PTPC is a mitochondrial supramolecular entity [189] that initiates mitochondrial permeability transition, an event characterized by a sudden and irreversible augmentation of the permeability of mitochondrial membranes, which causes the dissipation of the mitochondrial transmembrane potential, osmotic breakdown of the organelle, and, finally, cell death [190]. In addition, melatonin targets and shields the mitochondrial fission protein DRP1 in diabetic hearts [191], and blocks DRP1 in HUVEC through the stimulation of the AMPK/Sarco-Endoplasmic Reticulum Calcium ATPase (SERCA) signaling pathway [192]. Besides its effective roles in mitochondria, melatonin plays an important role as an anti-inflammatory effect [193]. Recently researchers have shown much interest in studying the cardioprotective capabilities of melatonin in CAVS. Melatonin has been shown to improve CAV in valve interstitial cells via RNA CircRIC3/miR-204-5p/DPP4 signaling [194], and it targets melatonin receptor (MT1)/NF-κB/RUNX2 signaling to reduce the calcification in valve interstitial-mediated osteogenic stimulation [195]. Another significant study shows the crucial protective impact of melatonin in inhibiting calcification through the AMPK/DRP1 pathway in vascular smooth muscle cells (VSMCs) [196].
The enzyme carnitine O-octanoyltransferase (CROT) is responsible for the transport of medium and long-chain acyl-CoA molecules out of the peroxisome to the cytosol and mitochondria. antiCROT has been discovered as a novel recent candidate that contributes to valve fibrocalcification. The inhibition of CROT corrects mitochondrial abnormalities in VICs by blocking mitochondrial fragmentation, restoring mitochondrial proteome changes in the osteogenic environment, and promoting fatty acid metabolism [197].
Recently, microarray technologies have been used to identify newly discovered functional genes that can also be adopted for ultimate diagnosis and prognostics in various diseases [198]. Among these, microarray profiling identified the proprotein convertase subtilisin/kexin type 9 (PCSK9), an enzyme mainly secreted in the liver that targets the LDL receptor for further lysosomal destruction, which is involved in the inflammatory gene’s expression, cell cycle, and stress condition responses [199]. Additional studies demonstrated the impact of PCSK9 in promoting the inflammatory response, which is the main contributor to valve calcification, through the stimulation of T cells infiltrating calcified AVs and promoting inflammation; besides its role in activating the T cells, PCSK9 can also stimulate directly macrophages to secrete proinflammatory cytokines including, IL-6, IL-1β, and TNFα [200,201]. Ongoing clinical trials are presently testing whether blocking PCSK9 may mitigate the micro/macro-calcification of AVs using computed tomography and 18F-NaF positron-emission tomography/computed tomography, respectively, in CAVS patients (clinicaltrials.gov/NCT03051360). Indeed, PCSK9 inhibitors, such as evolocumab, in the explorative analysis of the “FOURIER” trial (Further Cardiovascular Outcomes Research with PCSK9 Inhibition in Subjects with Elevated Risk) [202], demonstrated positive outcomes in reducing CAVS events after the first year of the therapy [143].
Other crucial genes that have been recently discovered in CAVS pathogenesis through advanced gene chip technology are the Secretogranin II (SCG2) and C-C motif chemokine ligand 19 (CCL19), which are involved in inflammatory responses; however, their exact correlation and mechanism with the CAVS are still to be elucidated. As previously reported by Fang and colleagues, SCG2 alters angiogenesis and tumor growth by HIF-1α destruction [203] and is able to stimulate wound healing in response to fasting [204]. These findings suggest a further impact of SCG2 in tissue remodeling and provide further insights for future research into immunotherapy strategies for CAVS progression.
On the other hand, MSI-1436, a pharmacological inhibitor of PTPB prevents fibrocalcification of the AV and protects the mitochondrial biogenesis and performances through the optic atrophy 1 (OPA1) regulation [116].
Recent studies by Liu et al. demonstrate that MMP-9i, an inhibitor of MMP9, reveals its significant effectiveness in attenuating mitochondrial impairments and repressing oxidative stress, and thereby VIC calcification in CAVS patients [120].
Rapamycin is a potent inducer of autophagy, and it has been shown by Morciano and colleagues to revert calcification by attenuating cell death and restoring calcium dysregulation in CAVS patients [46]. It is, however, required to be studied in animal models in combination with an anti-inflammatory.

Table 1.
A representative table on the therapeutic strategies of CAVS.
Table 1.
A representative table on the therapeutic strategies of CAVS.
| Therapeutic Target | Treatment | Mechanism of Action and Effect | References |
|---|---|---|---|
| HIF-1α inhibitors | Dimethylloxetane | Downregulates osteogenic transcription factors (RUNX2 and BMP-2), reduces vascular calcification | [168,205] |
| PX-478 | Downregulates porcine AV (PAV) calcification, and significantly blocks the deposition of calcium, thereby alleviating CAVD | [58,167] | |
| EZN-2968 | Possible to mitigate the calcification | [172] | |
| Estrogen drug therapy | - | Alleviates HIF-1α expression and vascular calcification, inhibits NFκB signaling and RNKL, blocks p53 activity and NADPH oxidase, as well as inflammation. Activates antioxidant enzymes including in mitochondria and lysosomes, as well as the cytosol | [168,169,170,206,207,208,209] |
| Angiogenesis repressor | S1P | Halts neo-vessels formation via sFlt1 activation | [65] |
| RAAS inhibitors (ACE-I therapy Ang-II blockers) | Fimasartan and losartan | Reduces CAV and a slowdown in mild CAVS development. Improves hemodynamic and left ventricular (LV) hypertrophy in patients with moderate and severe CAVS | [179,180,181,182], https://clinicaltrials.gov/show/nct01589380, https://clinicaltrials.gov/ct2/show/NCT03666351 (accessed on 30 March 2023) |
| Exportin-1 (XPO1) inhibitor | KPT-330 | Mitigates calcific nodule formation via CCAAT/enhancing-binding protein (C/EBPβ) signaling pathway, protecting against CAVS | [187] |
| Melatonine (N-acetyl-5-methoxytryptamine) | Melatonine | Improves CAV in VICs via RNA CircRIC3/miR-204-5p/DPP4 signaling and targets MT1/NF-κB/RUNX2 signaling, reducing VIC calcification-mediated osteogenic stimulation. Inhibits calcification via the AMPK/DRP1 pathway in VSMCs | [194,195,196] |
| CROT inhibitor | - | Blocks mitochondrial fragmentation, restores mitochondrial proteome changes in the osteogenic environment, and promotes fatty acid metabolism, and reduces fibrocalcification | [197] |
| PCSK9 inhibitors | Evolocumab | Reduces CAVS events | [143,202] |
| PTPB inhibitor | MSI-1436 | Prevents AV fibrocalcification, protects mitochondrial biogenesis, and performances via OPA1 | [116] |
| MMP9 inhibitor | MMP-9i | Attenuates mitochondrial impairments, represses oxidative stress, and VIC calcification | [120] |
| Autophagy activator | Rapamycin | Reverts calcification through cell death downregulation and restores calcium dysregulation in CAVS patients | [46] |
5. Conclusions and Future Perspective
CAVS is a complex and progressive heart valvular disease. Extensive research has led to the identification of several risk factors underlying CAVS progression. The early insidious nature and etiology of CAVS have made it challenging to explore and unravel the cellular and molecular mechanisms underlying its complex etiology. This has left us with only surgical and transcatheter valve replacement as the only possible option to treat CAVS, which is very likely a costly procedure that is expected to double by 2050 [6]. At present, no therapeutic approaches have been successfully developed yet to prevent or treat the disease. Therefore, the development of a potent therapy for CAVS has become a major urgent and critical necessity. To attain this noble purpose, it is highly essential for scientists to dive deep into understanding the molecular and cellular mechanisms of CAVS initiation and progression.
Inflammatory pathways are one of the major molecular mediators in both the initiation and progression of CAVS. Recent insights demonstrate that impairments in the functioning of mitochondria are involved in the pathogenesis of this disorder through both the processes of oxidative stress and inflammation. Furthermore, discoveries have identified the hypoxia signaling pathway as a critical contributor in the early and evolution stages of CAVS. However, extended investigations are required to better dissect the hypoxia-related pathways in CAVS and their interconnections with mitochondria and inflammation. Another important point to inspect is how members of the HIF1 family can regulate the hypoxic levels to modulate the different processes of autophagy and mitophagy in CAVS, taking into account of the important role of these pathways in controlling mitochondrial homeostasis and inflammation.
Understanding how elements related to the HIF1 family contribute to CAVS disease could help to solve another great issue in the study of CAVS, which is the lack of established elements for an early diagnosis and prognosis. Furthermore, assessing whether the markers of hypoxia can influence the calcification score in calcific AV areas of patients by applying artificial intelligence would be an innovative approach to predict the severity and extent of calcification, and to be used for further prognosis.
The identification of the close relationship between hypoxia signaling, mitochondrial dysfunction, and inflammation in CAVS could be also essential to develop new therapeutic approaches that target factors of these signaling pathways at the early phases of the disease rather than at the end stage where patients exhibit severe aortic stenosis.
Author Contributions
E.B. conceived and planned the manuscript with input from S.P., C.G., P.P., E.B., G.M., G.P. and D.R. wrote the manuscript with input from P.P., S.P., C.G. and E.B. prepared the display items (with https://biorender.com (accessed on 30 March 2023)). The figures are original and have not been published before. E.T., C.G., P.P., S.P. and E.B. reviewed the manuscript before submission. All authors have read and agreed to the published version of the manuscript.
Funding
The Signal Transduction Laboratory is supported by the Italian Association for Cancer Research grants IG-23670 (to P.P.) and IG-19803 (to C.G.), A-ROSE (Associazione Ricerca Oncologica Sperimentale Estense); Progetti di Rilevante Interesse Nazionale grants PRIN2017E5L5P3 (to P.P.) and PRIN20177E9EPY (to C.G.); Italian Ministry of Health grants GR-2018-12367114 (to C.G.) and GR-2019-12369862 (to G.M.); European Research Council grant 853057-InflaPML (to C.G.); and local funds from the University of Ferrara (to P.P. and C.G.); FISM—Fondazione Italiana Sclerosi Multipla—cod.2022/R-Multi/050 and financed or co-financed with the ‘5 per mille’ public funding (to S.P.).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Acknowledgments
P.P. is grateful to Camilla Degli Scrovegni for his continuous support.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
| 18F-FDG | 18F-Flurodeoxyglucose |
| ACE-I | Angiotensin-converting enzyme |
| Ang-II | Angiotensin-II |
| APC/C | Complex/Cyclosome |
| AS | aortic stenosis |
| AV | Aortic valve |
| BMP-2 | Bone morphogenetic protein-2 |
| C/EBPβ | CCAAT/enhancing-binding protein |
| CACNA1C | Calcium voltage-gated channel subunit alpha 1 C |
| CAVD | Calcific aortic valve disease |
| CAVS | Calcific aortic valve stenosis |
| CBP | CREB-binding protein |
| CCL19 | C-C motif chemokine ligand 19 |
| CD11 | Surface marker of M1 |
| CLPP | Caseinolytic Mitochondrial Matrix Peptidase Proteolytic Subunit |
| CROT | Carnitine O-octanoyltransferase |
| CTB | Cytotrophoblast |
| CVD | Cardiovascular disease |
| DRP1 | Dynamin-related protein 1 |
| ECM | Extracellular matrix |
| EPAS-1 | Endothelial PAS domain protein-1 |
| EPO | Erythropoietin |
| ERK1/2 | Extracellular signal-regulated kinase |
| FAT/CD36 | Fatty acid translocase |
| FOURIER | Further Cardiovascular Outcomes Research with PCSK9 Inhibition in Subjects with Elevated Risk |
| Glut 1, 4 | Glucose transporter 1 and 4 |
| HAVEC | Human aortic endothelial cells |
| HC-OA | Human osteoarthritic |
| HF | Heart failure |
| HIF-1α | Hypoxia-inducible factor 1 alpha subunit |
| HIFs | Hypoxia-inducible transcription factors |
| HMOX1 | Heme Oxygenase 1 |
| HTRA2 | HtrA Serine Peptidase 2 |
| HUVEC | Human umbilical endothelial cells |
| ICAM-1 | Intracellular adhesion molecule-1 |
| IFN-γ | Interferon-γ |
| IHD | ischemic heart disease |
| IL- | Interleukin |
| iNOS | Inducible nitric oxide synthase |
| LDH-A | Lactate dehydrogenase-A |
| LDL | Low-density lipoprotein |
| Lp(a) | Lipoprotein a |
| LV | Left ventricular |
| MCP-1 | Monocyte chemoattractant protein-1 |
| MMP9 | Matrix metalloproteinase 9 expression |
| MMPs | Matrix metalloproteinases |
| MMP-9i | Matrix metalloproteinase 9 inhibitor |
| MT1 | Melatonin receptor |
| mtDNA | Mitochondrial DNA |
| mtROS | Mitochondrial ROS |
| mtUPR | Mitochondrial unfolded protein response |
| N-acetyl-5-methoxytryptamine | Melatonine |
| NF-κB | Nuclear factor kappa B |
| NLRC4 | Pyrin domain-containing protein |
| NOS | Nitric oxide synthase |
| O2 | Oxygen |
| OPA1 | Optic atrophy 1 |
| OXPHOS | Oxidative phosphorylation |
| PAV | Porcine AV |
| PCSK9 | Proprotein convertase subtilisin/kexin type 9 |
| PDK | Dehydrogenase kinase isoform 1 |
| PET | Positron emission tomography |
| PGK1 | Phosphoglycerate kinase-1 |
| PHD1, -2, -3 | Propyl-hydroxylase-1, -2, and -3 enzyme activity |
| PI3K/Akt | P hosphatidylinositol 3-kinase (PI3K)-Akt (protein kinase B) |
| PKM2 | M2 isoform of pyruvate kinase |
| PTP1B | Protein tyrosine phosphatase 1B |
| pVHL | von Hippel–Lindau |
| RANKL | Receptor-activator of nuclear factor κB ligand |
| SCG2 | Secretogranin II |
| sFlt1 | Soluble fms-like tyrosine kinase 1 |
| SMC | Smooth muscle cells |
| SOD2 | Superoxide dismutase 2 |
| STAT3 | Signal Transducer and Activator of Transcription 3 |
| TG | Triglyceride levels |
| TGF-β | Transforming growth factor-beta |
| TLR | Toll-like receptor |
| UBE2C | Ubiquitin E2 ligase C |
| VECs | Valvular endothelial cells |
| VEGF | Vascular endothelial growth factor |
| VICs | valvular interstitial cells |
| VSMC | Vascular smooth muscle cells |
| XPO1 | Exportin-1 |
References
- Aisagbonhi, O.; Rai, M.; Ryzhov, S.; Atria, N.; Feoktistov, I.; Hatzopoulos, A.K. Experimental myocardial infarction triggers canonical Wnt signaling and endothelial-to-mesenchymal transition. Dis. Model. Mech. 2011, 4, 469–483. [Google Scholar] [CrossRef]
- Akahori, H.; Tsujino, T.; Naito, Y.; Sawada, H.; Sugahara, M.; Fukui, M.; Ohyanagi, M.; Mitsuno, M.; Miyamoto, Y.; Masuyama, T. Nuclear factor-kappaB-hypoxia-inducible factor-2 pathway in aortic valve stenosis. J. Heart Valve Dis. 2014, 23, 558–566. [Google Scholar]
- Andersson, C.; Abdulla, J. Is the use of renin-angiotensin system inhibitors in patients with aortic valve stenosis safe and of prognostic benefit? A systematic review and meta-analysis. Eur. Heart J. Cardiovasc. Pharmacother. 2017, 3, 21–27. [Google Scholar] [CrossRef] [PubMed]
- Angelo, L.S.; Kurzrock, R. Vascular endothelial growth factor and its relationship to inflammatory mediators. Clin. Cancer Res. 2007, 13, 2825–2830. [Google Scholar] [CrossRef] [PubMed]
- Bai, C.G.; Liu, X.H.; Liu, W.Q.; Ma, D.L. Regional expression of the hypoxia-inducible factor (HIF) system and association with cardiomyocyte cell cycle re-entry after myocardial infarction in rats. Heart Vessels 2008, 23, 193–200. [Google Scholar] [CrossRef]
- Bergmark, B.A.; O’Donoghue, M.L.; Murphy, S.A.; Kuder, J.F.; Ezhov, M.V.; Ceska, R.; Gouni-Berthold, I.; Jensen, H.K.; Tokgozoglu, S.L.; Mach, F.; et al. An Exploratory Analysis of Proprotein Convertase Subtilisin/Kexin Type 9 Inhibition and Aortic Stenosis in the FOURIER Trial. JAMA Cardiol. 2020, 5, 709–713. [Google Scholar] [CrossRef]
- Bertazzo, S.; Gentleman, E.; Cloyd, K.L.; Chester, A.H.; Yacoub, M.H.; Stevens, M.M. Nano-analytical electron microscopy reveals fundamental insights into human cardiovascular tissue calcification. Nat. Mater. 2013, 12, 576–583. [Google Scholar] [CrossRef]
- Bonora, M.; Giorgi, C.; Pinton, P. Molecular mechanisms and consequences of mitochondrial permeability transition. Nat. Rev. Mol. Cell Biol. 2022, 23, 266–285. [Google Scholar] [CrossRef]
- Bonora, M.; Pinton, P. A New Current for the Mitochondrial Permeability Transition. Trends Biochem. Sci. 2019, 44, 559–561. [Google Scholar] [CrossRef] [PubMed]
- Borchi, E.; Bargelli, V.; Stillitano, F.; Giordano, C.; Sebastiani, M.; Nassi, P.A.; d’Amati, G.; Cerbai, E.; Nediani, C. Enhanced ROS production by NADPH oxidase is correlated to changes in antioxidant enzyme activity in human heart failure. Biochim. Biophys. Acta 2010, 1802, 331–338. [Google Scholar] [CrossRef] [PubMed]
- Bouchareb, R.; Boulanger, M.C.; Fournier, D.; Pibarot, P.; Messaddeq, Y.; Mathieu, P. Mechanical strain induces the production of spheroid mineralized microparticles in the aortic valve through a RhoA/ROCK-dependent mechanism. J. Mol. Cell. Cardiol. 2014, 67, 49–59. [Google Scholar] [CrossRef]
- Bouhamida, E.; Morciano, G.; Perrone, M.; Kahsay, A.E.; Della Sala, M.; Wieckowski, M.R.; Fiorica, F.; Pinton, P.; Giorgi, C.; Patergnani, S. The Interplay of Hypoxia Signaling on Mitochondrial Dysfunction and Inflammation in Cardiovascular Diseases and Cancer: From Molecular Mechanisms to Therapeutic Approaches. Biology 2022, 11, 300. [Google Scholar] [CrossRef] [PubMed]
- Bull, S.; Loudon, M.; Francis, J.M.; Joseph, J.; Gerry, S.; Karamitsos, T.D.; Prendergast, B.D.; Banning, A.P.; Neubauer, S.; Myerson, S.G. A prospective, double-blind, randomized controlled trial of the angiotensin-converting enzyme inhibitor Ramipril In Aortic Stenosis (RIAS trial). Eur. Heart J. Cardiovasc. Imaging 2015, 16, 834–841. [Google Scholar] [CrossRef]
- Butcher, J.T.; Nerem, R.M. Valvular endothelial cells regulate the phenotype of interstitial cells in co-culture: Effects of steady shear stress. Tissue Eng. 2006, 12, 905–915. [Google Scholar] [CrossRef] [PubMed]
- Butcher, J.T.; Penrod, A.M.; Garcia, A.J.; Nerem, R.M. Unique morphology and focal adhesion development of valvular endothelial cells in static and fluid flow environments. Arterioscler. Thromb. Vasc. Biol. 2004, 24, 1429–1434. [Google Scholar] [CrossRef]
- Byon, C.H.; Javed, A.; Dai, Q.; Kappes, J.C.; Clemens, T.L.; Darley-Usmar, V.M.; McDonald, J.M.; Chen, Y. Oxidative stress induces vascular calcification through modulation of the osteogenic transcription factor Runx2 by AKT signaling. J. Biol. Chem. 2008, 283, 15319–15327. [Google Scholar] [CrossRef] [PubMed]
- Carracedo, M.; Back, M. Fetuin A in aortic stenosis and valve calcification: Not crystal clear. Int. J. Cardiol. 2018, 265, 77–78. [Google Scholar] [CrossRef] [PubMed]
- Castardo-de-Paula, J.C.; de Campos, B.H.; Amorim, E.D.T.; da Silva, R.V.; de Farias, C.C.; Higachi, L.; Pinge-Filho, P.; Barbosa, D.S.; Martins-Pinge, M.C. Cardiovascular risk and the effect of nitric oxide synthase inhibition in female rats: The role of estrogen. Exp. Gerontol. 2017, 97, 38–48. [Google Scholar] [CrossRef]
- Castellazzi, M.; Patergnani, S.; Donadio, M.; Giorgi, C.; Bonora, M.; Fainardi, E.; Casetta, I.; Granieri, E.; Pugliatti, M.; Pinton, P. Correlation between auto/mitophagic processes and magnetic resonance imaging activity in multiple sclerosis patients. J. Neuroinflamm. 2019, 16, 131. [Google Scholar] [CrossRef]
- Chen, J.; Lin, Y.; Sun, Z. Inhibition of miR-101-3p prevents human aortic valve interstitial cell calcification through regulation of CDH11/SOX9 expression. Mol. Med. 2023, 29, 24. [Google Scholar] [CrossRef]
- Chen, J.H.; Simmons, C.A. Cell-matrix interactions in the pathobiology of calcific aortic valve disease: Critical roles for matricellular, matricrine, and matrix mechanics cues. Circ. Res. 2011, 108, 1510–1524. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.R.; Liu, H.B.; Chen, Y.D.; Sha, Y.; Ma, Q.; Zhu, P.J.; Mu, Y. Melatonin Attenuates Myocardial Ischemia/Reperfusion Injury by Inhibiting Autophagy Via an AMPK/mTOR Signaling Pathway. Cell. Physiol. Biochem. 2018, 47, 2067–2076. [Google Scholar] [CrossRef]
- Chen, W.R.; Zhou, Y.J.; Sha, Y.; Wu, X.P.; Yang, J.Q.; Liu, F. Melatonin attenuates vascular calcification by inhibiting mitochondria fission via an AMPK/Drp1 signalling pathway. J. Cell. Mol. Med. 2020, 24, 6043–6054. [Google Scholar] [CrossRef]
- Chignalia, A.Z.; Oliveira, M.A.; Debbas, V.; Dull, R.O.; Laurindo, F.R.; Touyz, R.M.; Carvalho, M.H.; Fortes, Z.B.; Tostes, R.C. Testosterone induces leucocyte migration by NADPH oxidase-driven ROS- and COX2-dependent mechanisms. Clin. Sci. 2015, 129, 39–48. [Google Scholar] [CrossRef] [PubMed]
- Chockalingam, A.; Venkatesan, S.; Subramaniam, T.; Jagannathan, V.; Elangovan, S.; Alagesan, R.; Gnanavelu, G.; Dorairajan, S.; Krishna, B.P.; Chockalingam, V.; et al. Safety and efficacy of angiotensin-converting enzyme inhibitors in symptomatic severe aortic stenosis: Symptomatic Cardiac Obstruction-Pilot Study of Enalapril in Aortic Stenosis (SCOPE-AS). Am. Heart J. 2004, 147, E19. [Google Scholar] [CrossRef]
- Chowdhury, A.; Aich, A.; Jain, G.; Wozny, K.; Luchtenborg, C.; Hartmann, M.; Bernhard, O.; Balleiniger, M.; Alfar, E.A.; Zieseniss, A.; et al. Defective Mitochondrial Cardiolipin Remodeling Dampens HIF-1alpha Expression in Hypoxia. Cell Rep. 2018, 25, 561–570.e566. [Google Scholar] [CrossRef]
- Coffey, S.; Cox, B.; Williams, M.J. The prevalence, incidence, progression, and risks of aortic valve sclerosis: A systematic review and meta-analysis. J. Am. Coll. Cardiol. 2014, 63, 2852–2861. [Google Scholar] [CrossRef] [PubMed]
- Crouzier, L.; Danese, A.; Yasui, Y.; Richard, E.M.; Lievens, J.C.; Patergnani, S.; Couly, S.; Diez, C.; Denus, M.; Cubedo, N.; et al. Activation of the sigma-1 receptor chaperone alleviates symptoms of Wolfram syndrome in preclinical models. Sci. Transl. Med. 2022, 14, eabh3763. [Google Scholar] [CrossRef]
- Cui, J.; Li, Z.; Zhuang, S.; Qi, S.; Li, L.; Zhou, J.; Zhang, W.; Zhao, Y. Melatonin alleviates inflammation-induced apoptosis in human umbilical vein endothelial cells via suppression of Ca2+-XO-ROS-Drp1-mitochondrial fission axis by activation of AMPK/SERCA2a pathway. Cell Stress Chaperones 2018, 23, 281–293. [Google Scholar] [CrossRef]
- Dachs, G.U.; Tozer, G.M. Hypoxia modulated gene expression: Angiogenesis, metastasis and therapeutic exploitation. Eur. J. Cancer 2000, 36, 1649–1660. [Google Scholar] [CrossRef]
- Dalsgaard, M.; Iversen, K.; Kjaergaard, J.; Grande, P.; Goetze, J.P.; Clemmensen, P.; Hassager, C. Short-term hemodynamic effect of angiotensin-converting enzyme inhibition in patients with severe aortic stenosis: A placebo-controlled, randomized study. Am. Heart J. 2014, 167, 226–234. [Google Scholar] [CrossRef]
- Danese, A.; Patergnani, S.; Maresca, A.; Peron, C.; Raimondi, A.; Caporali, L.; Marchi, S.; La Morgia, C.; Del Dotto, V.; Zanna, C.; et al. Pathological mitophagy disrupts mitochondrial homeostasis in Leber’s hereditary optic neuropathy. Cell Rep. 2022, 40, 111124. [Google Scholar] [CrossRef]
- Dhalla, A.K.; Hill, M.F.; Singal, P.K. Role of oxidative stress in transition of hypertrophy to heart failure. J. Am. Coll. Cardiol. 1996, 28, 506–514. [Google Scholar] [CrossRef]
- Di Minno, A.; Zanobini, M.; Myasoedova, V.A.; Valerio, V.; Songia, P.; Saccocci, M.; Di Minno, M.N.D.; Tremoli, E.; Poggio, P. Could circulating fetuin A be a biomarker of aortic valve stenosis? Int. J. Cardiol. 2017, 249, 426–430. [Google Scholar] [CrossRef]
- Dinarello, C.A.; Nold-Petry, C.; Nold, M.; Fujita, M.; Li, S.; Kim, S.; Bufler, P. Suppression of innate inflammation and immunity by interleukin-37. Eur. J. Immunol. 2016, 46, 1067–1081. [Google Scholar] [CrossRef]
- Ding, M.; Feng, N.; Tang, D.; Feng, J.; Li, Z.; Jia, M.; Liu, Z.; Gu, X.; Wang, Y.; Fu, F.; et al. Melatonin prevents Drp1-mediated mitochondrial fission in diabetic hearts through SIRT1-PGC1alpha pathway. J. Pineal Res. 2018, 65, e12491. [Google Scholar] [CrossRef]
- GBD 2019 Risk Factors Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222. [Google Scholar] [CrossRef]
- Dodd, M.S.; Sousa Fialho, M.D.L.; Montes Aparicio, C.N.; Kerr, M.; Timm, K.N.; Griffin, J.L.; Luiken, J.; Glatz, J.F.C.; Tyler, D.J.; Heather, L.C. Fatty Acids Prevent Hypoxia-Inducible Factor-1alpha Signaling Through Decreased Succinate in Diabetes. JACC Basic Transl. Sci. 2018, 3, 485–498. [Google Scholar] [CrossRef] [PubMed]
- Duan, C.; Cao, Z.; Tang, F.; Jian, Z.; Liang, C.; Liu, H.; Xiao, Y.; Liu, L.; Ma, R. miRNA-mRNA crosstalk in myocardial ischemia induced by calcified aortic valve stenosis. Aging 2019, 11, 448–466. [Google Scholar] [CrossRef] [PubMed]
- Dutta, P.; Kodigepalli, K.M.; LaHaye, S.; Thompson, J.W.; Rains, S.; Nagel, C.; Thatcher, K.; Hinton, R.B.; Lincoln, J. KPT-330 Prevents Aortic Valve Calcification via a Novel C/EBPbeta Signaling Pathway. Circ. Res. 2021, 128, 1300–1316. [Google Scholar] [CrossRef]
- Dweck, M.R.; Boon, N.A.; Newby, D.E. Calcific aortic stenosis: A disease of the valve and the myocardium. J. Am. Coll. Cardiol. 2012, 60, 1854–1863. [Google Scholar] [CrossRef] [PubMed]
- Dweck, M.R.; Jones, C.; Joshi, N.V.; Fletcher, A.M.; Richardson, H.; White, A.; Marsden, M.; Pessotto, R.; Clark, J.C.; Wallace, W.A.; et al. Assessment of valvular calcification and inflammation by positron emission tomography in patients with aortic stenosis. Circulation 2012, 125, 76–86. [Google Scholar] [CrossRef] [PubMed]
- Dweck, M.R.; Khaw, H.J.; Sng, G.K.; Luo, E.L.; Baird, A.; Williams, M.C.; Makiello, P.; Mirsadraee, S.; Joshi, N.V.; van Beek, E.J.; et al. Aortic stenosis, atherosclerosis, and skeletal bone: Is there a common link with calcification and inflammation? Eur. Heart J. 2013, 34, 1567–1574. [Google Scholar] [CrossRef] [PubMed]
- El Husseini, D.; Boulanger, M.C.; Mahmut, A.; Bouchareb, R.; Laflamme, M.H.; Fournier, D.; Pibarot, P.; Bosse, Y.; Mathieu, P. P2Y2 receptor represses IL-6 expression by valve interstitial cells through Akt: Implication for calcific aortic valve disease. J. Mol. Cell. Cardiol. 2014, 72, 146–156. [Google Scholar] [CrossRef]
- Engberding, N.; Spiekermann, S.; Schaefer, A.; Heineke, A.; Wiencke, A.; Muller, M.; Fuchs, M.; Hilfiker-Kleiner, D.; Hornig, B.; Drexler, H.; et al. Allopurinol attenuates left ventricular remodeling and dysfunction after experimental myocardial infarction: A new action for an old drug? Circulation 2004, 110, 2175–2179. [Google Scholar] [CrossRef]
- Fang, C.; Dai, L.; Wang, C.; Fan, C.; Yu, Y.; Yang, L.; Deng, H.; Zhou, Z. Secretogranin II impairs tumor growth and angiogenesis by promoting degradation of hypoxia-inducible factor-1alpha in colorectal cancer. Mol. Oncol. 2021, 15, 3513–3526. [Google Scholar] [CrossRef]
- GBD 2019 Risk Factors Collaborators. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1223–1249. [Google Scholar] [CrossRef]
- Farrar, E.J.; Huntley, G.D.; Butcher, J. Endothelial-derived oxidative stress drives myofibroblastic activation and calcification of the aortic valve. PLoS ONE 2015, 10, e0123257. [Google Scholar] [CrossRef]
- Feldhoff, L.M.; Rueda, C.M.; Moreno-Fernandez, M.E.; Sauer, J.; Jackson, C.M.; Chougnet, C.A.; Rupp, J. IL-1beta induced HIF-1alpha inhibits the differentiation of human FOXP3+ T cells. Sci. Rep. 2017, 7, 465. [Google Scholar] [CrossRef]
- Fernandez-Pisonero, I.; Lopez, J.; Onecha, E.; Duenas, A.I.; Maeso, P.; Crespo, M.S.; San Roman, J.A.; Garcia-Rodriguez, C. Synergy between sphingosine 1-phosphate and lipopolysaccharide signaling promotes an inflammatory, angiogenic and osteogenic response in human aortic valve interstitial cells. PLoS ONE 2014, 9, e109081. [Google Scholar] [CrossRef]
- Fernandez Esmerats, J.; Villa-Roel, N.; Kumar, S.; Gu, L.; Salim, M.T.; Ohh, M.; Taylor, W.R.; Nerem, R.M.; Yoganathan, A.P.; Jo, H. Disturbed Flow Increases UBE2C (Ubiquitin E2 Ligase C) via Loss of miR-483-3p, Inducing Aortic Valve Calcification by the pVHL (von Hippel-Lindau Protein) and HIF-1alpha (Hypoxia-Inducible Factor-1alpha) Pathway in Endothelial Cells. Arterioscler. Thromb. Vasc. Biol. 2019, 39, 467–481. [Google Scholar] [CrossRef]
- Ferrara, N.; Gerber, H.P.; LeCouter, J. The biology of VEGF and its receptors. Nat. Med. 2003, 9, 669–676. [Google Scholar] [CrossRef] [PubMed]
- Ferrari, S.; Pesce, M. The Complex Interplay of Inflammation, Metabolism, Epigenetics, and Sex in Calcific Disease of the Aortic Valve. Front. Cardiovasc. Med. 2021, 8, 791646. [Google Scholar] [CrossRef] [PubMed]
- Ferreira-Gonzalez, I.; Pinar-Sopena, J.; Ribera, A.; Marsal, J.R.; Cascant, P.; Gonzalez-Alujas, T.; Evangelista, A.; Brotons, C.; Moral, I.; Permanyer-Miralda, G.; et al. Prevalence of calcific aortic valve disease in the elderly and associated risk factors: A population-based study in a Mediterranean area. Eur. J. Prev. Cardiol. 2013, 20, 1022–1030. [Google Scholar] [CrossRef] [PubMed]
- Forsythe, J.A.; Jiang, B.H.; Iyer, N.V.; Agani, F.; Leung, S.W.; Koos, R.D.; Semenza, G.L. Activation of vascular endothelial growth factor gene transcription by hypoxia-inducible factor 1. Mol. Cell. Biol. 1996, 16, 4604–4613. [Google Scholar] [CrossRef]
- Gendron, N.; Rosa, M.; Blandinieres, A.; Sottejeau, Y.; Rossi, E.; Van Belle, E.; Idelcadi, S.; Lecourt, S.; Vincentelli, A.; Cras, A.; et al. Human Aortic Valve Interstitial Cells Display Proangiogenic Properties During Calcific Aortic Valve Disease. Arterioscler. Thromb. Vasc. Biol. 2021, 41, 415–429. [Google Scholar] [CrossRef] [PubMed]
- Ghaisas, N.K.; Foley, J.B.; O’Briain, D.S.; Crean, P.; Kelleher, D.; Walsh, M. Adhesion molecules in nonrheumatic aortic valve disease: Endothelial expression, serum levels and effects of valve replacement. J. Am. Coll. Cardiol. 2000, 36, 2257–2262. [Google Scholar] [CrossRef] [PubMed]
- Gil-Gil, M.J.; Mesia, C.; Rey, M.; Bruna, J. Bevacizumab for the treatment of glioblastoma. Clin. Med. Insights Oncol. 2013, 7, 123–135. [Google Scholar] [CrossRef] [PubMed]
- Giorgi, C.; Bouhamida, E.; Danese, A.; Previati, M.; Pinton, P.; Patergnani, S. Relevance of Autophagy and Mitophagy Dynamics and Markers in Neurodegenerative Diseases. Biomedicines 2021, 9, 149. [Google Scholar] [CrossRef]
- Giorgi, C.; Danese, A.; Missiroli, S.; Patergnani, S.; Pinton, P. Calcium Dynamics as a Machine for Decoding Signals. Trends Cell Biol. 2018, 28, 258–273. [Google Scholar] [CrossRef]
- Giorgi, C.; Marchi, S.; Pinton, P. The machineries, regulation and cellular functions of mitochondrial calcium. Nat. Rev. Mol. Cell Biol. 2018, 19, 713–730. [Google Scholar] [CrossRef] [PubMed]
- Gravina, G.L.; Mancini, A.; Sanita, P.; Vitale, F.; Marampon, F.; Ventura, L.; Landesman, Y.; McCauley, D.; Kauffman, M.; Shacham, S.; et al. KPT-330, a potent and selective exportin-1 (XPO-1) inhibitor, shows antitumor effects modulating the expression of cyclin D1 and survivin [corrected] in prostate cancer models. BMC Cancer 2015, 15, 941. [Google Scholar] [CrossRef] [PubMed]
- Greenberg, H.Z.E.; Zhao, G.; Shah, A.M.; Zhang, M. Role of oxidative stress in calcific aortic valve disease and its therapeutic implications. Cardiovasc. Res. 2022, 118, 1433–1451. [Google Scholar] [CrossRef] [PubMed]
- Greene, A.W.; Grenier, K.; Aguileta, M.A.; Muise, S.; Farazifard, R.; Haque, M.E.; McBride, H.M.; Park, D.S.; Fon, E.A. Mitochondrial processing peptidase regulates PINK1 processing, import and Parkin recruitment. EMBO Rep. 2012, 13, 378–385. [Google Scholar] [CrossRef]
- Guauque-Olarte, S.; Messika-Zeitoun, D.; Droit, A.; Lamontagne, M.; Tremblay-Marchand, J.; Lavoie-Charland, E.; Gaudreault, N.; Arsenault, B.J.; Dube, M.P.; Tardif, J.C.; et al. Calcium Signaling Pathway Genes RUNX2 and CACNA1C Are Associated With Calcific Aortic Valve Disease. Circ. Cardiovasc. Genet. 2015, 8, 812–822. [Google Scholar] [CrossRef]
- Hakuno, D.; Kimura, N.; Yoshioka, M.; Fukuda, K. Molecular mechanisms underlying the onset of degenerative aortic valve disease. J. Mol. Med. 2009, 87, 17–24. [Google Scholar] [CrossRef]
- Head, S.J.; Celik, M.; Kappetein, A.P. Mechanical versus bioprosthetic aortic valve replacement. Eur. Heart J. 2017, 38, 2183–2191. [Google Scholar] [CrossRef]
- Heather, L.C.; Howell, N.J.; Emmanuel, Y.; Cole, M.A.; Frenneaux, M.P.; Pagano, D.; Clarke, K. Changes in cardiac substrate transporters and metabolic proteins mirror the metabolic shift in patients with aortic stenosis. PLoS ONE 2011, 6, e26326. [Google Scholar] [CrossRef]
- Hutcheson, J.D.; Aikawa, E.; Merryman, W.D. Potential drug targets for calcific aortic valve disease. Nat. Rev. Cardiol. 2014, 11, 218–231. [Google Scholar] [CrossRef]
- Isoda, K.; Matsuki, T.; Kondo, H.; Iwakura, Y.; Ohsuzu, F. Deficiency of interleukin-1 receptor antagonist induces aortic valve disease in BALB/c mice. Arterioscler. Thromb. Vasc. Biol. 2010, 30, 708–715. [Google Scholar] [CrossRef]
- Jansen, F.; Xiang, X.; Werner, N. Role and function of extracellular vesicles in calcific aortic valve disease. Eur. Heart J. 2017, 38, 2714–2716. [Google Scholar] [CrossRef] [PubMed]
- Jaskiewicz, M.; Moszynska, A.; Kroliczewski, J.; Cabaj, A.; Bartoszewska, S.; Charzynska, A.; Gebert, M.; Dabrowski, M.; Collawn, J.F.; Bartoszewski, R. The transition from HIF-1 to HIF-2 during prolonged hypoxia results from reactivation of PHDs and HIF1A mRNA instability. Cell Mol. Biol. Lett. 2022, 27, 109. [Google Scholar] [CrossRef] [PubMed]
- Jeong, W.; Rapisarda, A.; Park, S.R.; Kinders, R.J.; Chen, A.; Melillo, G.; Turkbey, B.; Steinberg, S.M.; Choyke, P.; Doroshow, J.H.; et al. Pilot trial of EZN-2968, an antisense oligonucleotide inhibitor of hypoxia-inducible factor-1 alpha (HIF-1alpha), in patients with refractory solid tumors. Cancer Chemother. Pharmacol. 2014, 73, 343–348. [Google Scholar] [CrossRef]
- Jersmann, H.P.; Dransfield, I.; Hart, S.P. Fetuin/alpha2-HS glycoprotein enhances phagocytosis of apoptotic cells and macropinocytosis by human macrophages. Clin. Sci. 2003, 105, 273–278. [Google Scholar] [CrossRef]
- Jiang, B.H.; Rue, E.; Wang, G.L.; Roe, R.; Semenza, G.L. Dimerization, DNA binding, and transactivation properties of hypoxia-inducible factor 1. J. Biol. Chem. 1996, 271, 17771–17778. [Google Scholar] [CrossRef]
- Jiang, X.; Tian, W.; Tu, A.B.; Pasupneti, S.; Shuffle, E.; Dahms, P.; Zhang, P.; Cai, H.; Dinh, T.T.; Liu, B.; et al. Endothelial Hypoxia-Inducible Factor-2alpha Is Required for the Maintenance of Airway Microvasculature. Circulation 2019, 139, 502–517. [Google Scholar] [CrossRef]
- Jimenez-Candil, J.; Bermejo, J.; Yotti, R.; Cortina, C.; Moreno, M.; Cantalapiedra, J.L.; Garcia-Fernandez, M.A. Effects of angiotensin converting enzyme inhibitors in hypertensive patients with aortic valve stenosis: A drug withdrawal study. Heart 2005, 91, 1311–1318. [Google Scholar] [CrossRef]
- Jung, Y.J.; Isaacs, J.S.; Lee, S.; Trepel, J.; Neckers, L. IL-1beta-mediated up-regulation of HIF-1alpha via an NFkappaB/COX-2 pathway identifies HIF-1 as a critical link between inflammation and oncogenesis. FASEB J. 2003, 17, 2115–2117. [Google Scholar] [CrossRef] [PubMed]
- Kaden, J.J.; Dempfle, C.E.; Grobholz, R.; Fischer, C.S.; Vocke, D.C.; Kilic, R.; Sarikoc, A.; Pinol, R.; Hagl, S.; Lang, S.; et al. Inflammatory regulation of extracellular matrix remodeling in calcific aortic valve stenosis. Cardiovasc. Pathol. 2005, 14, 80–87. [Google Scholar] [CrossRef] [PubMed]
- Kaden, J.J.; Dempfle, C.E.; Grobholz, R.; Tran, H.T.; Kilic, R.; Sarikoc, A.; Brueckmann, M.; Vahl, C.; Hagl, S.; Haase, K.K.; et al. Interleukin-1 beta promotes matrix metalloproteinase expression and cell proliferation in calcific aortic valve stenosis. Atherosclerosis 2003, 170, 205–211. [Google Scholar] [CrossRef]
- Kim, J.W.; Tchernyshyov, I.; Semenza, G.L.; Dang, C.V. HIF-1-mediated expression of pyruvate dehydrogenase kinase: A metabolic switch required for cellular adaptation to hypoxia. Cell Metab. 2006, 3, 177–185. [Google Scholar] [CrossRef]
- Kobayashi, K.; Maeda, K.; Takefuji, M.; Kikuchi, R.; Morishita, Y.; Hirashima, M.; Murohara, T. Dynamics of angiogenesis in ischemic areas of the infarcted heart. Sci. Rep. 2017, 7, 7156. [Google Scholar] [CrossRef] [PubMed]
- Kokudo, T.; Suzuki, Y.; Yoshimatsu, Y.; Yamazaki, T.; Watabe, T.; Miyazono, K. Snail is required for TGFbeta-induced endothelial-mesenchymal transition of embryonic stem cell-derived endothelial cells. J. Cell Sci. 2008, 121, 3317–3324. [Google Scholar] [CrossRef] [PubMed]
- Koos, R.; Brandenburg, V.; Mahnken, A.H.; Muhlenbruch, G.; Stanzel, S.; Gunther, R.W.; Floege, J.; Jahnen-Dechent, W.; Kelm, M.; Kuhl, H.P. Association of fetuin-A levels with the progression of aortic valve calcification in non-dialyzed patients. Eur. Heart J. 2009, 30, 2054–2061. [Google Scholar] [CrossRef]
- Kornicka-Garbowska, K.; Bourebaba, L.; Rocken, M.; Marycz, K. Inhibition of protein tyrosine phosphatase improves mitochondrial bioenergetics and dynamics, reduces oxidative stress, and enhances adipogenic differentiation potential in metabolically impaired progenitor stem cells. Cell Commun. Signal. 2021, 19, 106. [Google Scholar] [CrossRef]
- Kronenberg, F.; Mora, S.; Stroes, E.S.G.; Ference, B.A.; Arsenault, B.J.; Berglund, L.; Dweck, M.R.; Koschinsky, M.; Lambert, G.; Mach, F.; et al. Lipoprotein(a) in atherosclerotic cardiovascular disease and aortic stenosis: A European Atherosclerosis Society consensus statement. Eur. Heart J. 2022, 43, 3925–3946. [Google Scholar] [CrossRef]
- Lagace, T.A.; Curtis, D.E.; Garuti, R.; McNutt, M.C.; Park, S.W.; Prather, H.B.; Anderson, N.N.; Ho, Y.K.; Hammer, R.E.; Horton, J.D. Secreted PCSK9 decreases the number of LDL receptors in hepatocytes and in livers of parabiotic mice. J. Clin. Investig. 2006, 116, 2995–3005. [Google Scholar] [CrossRef]
- Leopold, J.A. PCSK9 and Calcific Aortic Valve Stenosis: Moving Beyond Lipids. JACC Basic Transl. Sci. 2020, 5, 662–664. [Google Scholar] [CrossRef]
- Lewis, C.T.A.; Mascall, K.S.; Wilson, H.M.; Murray, F.; Kerr, K.M.; Gibson, G.; Buchan, K.; Small, G.R.; Nixon, G.F. An endogenous inhibitor of angiogenesis downregulated by hypoxia in human aortic valve stenosis promotes disease pathogenesis. J. Mol. Cell. Cardiol. 2023, 174, 25–37. [Google Scholar] [CrossRef] [PubMed]
- Li, G.; Qiao, W.; Zhang, W.; Li, F.; Shi, J.; Dong, N. The shift of macrophages toward M1 phenotype promotes aortic valvular calcification. J. Thorac. Cardiovasc. Surg. 2017, 153, 1318–1327.e1311. [Google Scholar] [CrossRef]
- Li, S.J.; Cheng, W.L.; Kao, Y.H.; Chung, C.C.; Trang, N.N.; Chen, Y.J. Melatonin Inhibits NF-kappaB/CREB/Runx2 Signaling and Alleviates Aortic Valve Calcification. Front. Cardiovasc. Med. 2022, 9, 885293. [Google Scholar] [CrossRef]
- Li, X.Z.; Xiong, Z.C.; Zhang, S.L.; Hao, Q.Y.; Gao, M.; Wang, J.F.; Gao, J.W.; Liu, P.M. Potential ferroptosis key genes in calcific aortic valve disease. Front. Cardiovasc. Med. 2022, 9, 916841. [Google Scholar] [CrossRef] [PubMed]
- Liberman, M.; Bassi, E.; Martinatti, M.K.; Lario, F.C.; Wosniak, J., Jr.; Pomerantzeff, P.M.; Laurindo, F.R. Oxidant generation predominates around calcifying foci and enhances progression of aortic valve calcification. Arterioscler. Thromb. Vasc. Biol. 2008, 28, 463–470. [Google Scholar] [CrossRef] [PubMed]
- Lindman, B.R.; Clavel, M.A.; Mathieu, P.; Iung, B.; Lancellotti, P.; Otto, C.M.; Pibarot, P. Calcific aortic stenosis. Nat. Rev. Dis. Primers 2016, 2, 16006. [Google Scholar] [CrossRef]
- Liu, C.; Liu, R.; Cao, Z.; Guo, Q.; Huang, H.; Liu, L.; Xiao, Y.; Duan, C.; Ma, R. Identification of MMP9 as a Novel Biomarker to Mitochondrial Metabolism Disorder and Oxidative Stress in Calcific Aortic Valve Stenosis. Oxidat. Med. Cell. Longev. 2022, 2022, 3858871. [Google Scholar] [CrossRef]
- Liu, D.; Iruthayanathan, M.; Homan, L.L.; Wang, Y.; Yang, L.; Wang, Y.; Dillon, J.S. Dehydroepiandrosterone stimulates endothelial proliferation and angiogenesis through extracellular signal-regulated kinase 1/2-mediated mechanisms. Endocrinology 2008, 149, 889–898. [Google Scholar] [CrossRef]
- Liu, F.; Chen, J.; Hu, W.; Gao, C.; Zeng, Z.; Cheng, S.; Yu, K.; Qian, Y.; Xu, D.; Zhu, G.; et al. PTP1B Inhibition Improves Mitochondrial Dynamics to Alleviate Calcific Aortic Valve Disease Via Regulating OPA1 Homeostasis. JACC Basic Transl. Sci. 2022, 7, 697–712. [Google Scholar] [CrossRef]
- Liu, W.; Xin, H.; Eckert, D.T.; Brown, J.A.; Gnarra, J.R. Hypoxia and cell cycle regulation of the von Hippel-Lindau tumor suppressor. Oncogene 2011, 30, 21–31. [Google Scholar] [CrossRef] [PubMed]
- Losenno, K.L.; Goodman, R.L.; Chu, M.W. Bicuspid aortic valve disease and ascending aortic aneurysms: Gaps in knowledge. Cardiol. Res. Pract. 2012, 2012, 145202. [Google Scholar] [CrossRef]
- Luo, M.J.; Rao, S.S.; Tan, Y.J.; Yin, H.; Hu, X.K.; Zhang, Y.; Liu, Y.W.; Yue, T.; Chen, L.J.; Li, L.; et al. Fasting before or after wound injury accelerates wound healing through the activation of pro-angiogenic SMOC1 and SCG2. Theranostics 2020, 10, 3779–3792. [Google Scholar] [CrossRef]
- Luo, W.; Hu, H.; Chang, R.; Zhong, J.; Knabel, M.; O’Meally, R.; Cole, R.N.; Pandey, A.; Semenza, G.L. Pyruvate kinase M2 is a PHD3-stimulated coactivator for hypoxia-inducible factor 1. Cell 2011, 145, 732–744. [Google Scholar] [CrossRef] [PubMed]
- Ma, F.; Li, Y.; Jia, L.; Han, Y.; Cheng, J.; Li, H.; Qi, Y.; Du, J. Macrophage-stimulated cardiac fibroblast production of IL-6 is essential for TGF beta/Smad activation and cardiac fibrosis induced by angiotensin II. PLoS ONE 2012, 7, e35144. [Google Scholar]
- Maeda, K.; Ma, X.; Chalajour, F.; Hanley, F.L.; Riemer, R.K. Critical Role of Coaptive Strain in Aortic Valve Leaflet Homeostasis: Use of a Novel Flow Culture Bioreactor to Explore Heart Valve Mechanobiology. J. Am. Heart Assoc. 2016, 5, e003506. [Google Scholar] [CrossRef] [PubMed]
- Maemura, K.; Hsieh, C.M.; Jain, M.K.; Fukumoto, S.; Layne, M.D.; Liu, Y.; Kourembanas, S.; Yet, S.F.; Perrella, M.A.; Lee, M.E. Generation of a dominant-negative mutant of endothelial PAS domain protein 1 by deletion of a potent C-terminal transactivation domain. J. Biol. Chem. 1999, 274, 31565–31570. [Google Scholar] [CrossRef] [PubMed]
- Marchi, S.; Giorgi, C.; Galluzzi, L.; Pinton, P. Ca2+ Fluxes and Cancer. Mol. Cell 2020, 78, 1055–1069. [Google Scholar] [CrossRef]
- Masri, A.; Svensson, L.G.; Griffin, B.P.; Desai, M.Y. Contemporary natural history of bicuspid aortic valve disease: A systematic review. Heart 2017, 103, 1323–1330. [Google Scholar] [CrossRef]
- Matsui, M.; Bouchareb, R.; Storto, M.; Hussain, Y.; Gregg, A.; Marx, S.O.; Pitt, G.S. Increased Ca2+ influx through CaV1.2 drives aortic valve calcification. JCI Insight 2022, 7, e155569. [Google Scholar] [CrossRef]
- Mazzone, A.; Epistolato, M.C.; De Caterina, R.; Storti, S.; Vittorini, S.; Sbrana, S.; Gianetti, J.; Bevilacqua, S.; Glauber, M.; Biagini, A.; et al. Neoangiogenesis, T-lymphocyte infiltration, and heat shock protein-60 are biological hallmarks of an immunomediated inflammatory process in end-stage calcified aortic valve stenosis. J. Am. Coll. Cardiol. 2004, 43, 1670–1676. [Google Scholar] [CrossRef]
- McClelland, G.B.; Brooks, G.A. Changes in MCT 1, MCT 4, and LDH expression are tissue specific in rats after long-term hypobaric hypoxia. J. Appl. Physiol. 2002, 92, 1573–1584. [Google Scholar] [CrossRef]
- Melillo, G.; Musso, T.; Sica, A.; Taylor, L.S.; Cox, G.W.; Varesio, L. A hypoxia-responsive element mediates a novel pathway of activation of the inducible nitric oxide synthase promoter. J. Exp. Med. 1995, 182, 1683–1693. [Google Scholar] [CrossRef]
- Meng, X.; Ao, L.; Song, Y.; Babu, A.; Yang, X.; Wang, M.; Weyant, M.J.; Dinarello, C.A.; Cleveland, J.C., Jr.; Fullerton, D.A. Expression of functional Toll-like receptors 2 and 4 in human aortic valve interstitial cells: Potential roles in aortic valve inflammation and stenosis. Am. J. Physiol. Cell Physiol. 2008, 294, C29–C35. [Google Scholar] [CrossRef] [PubMed]
- Metry, G.; Stenvinkel, P.; Qureshi, A.R.; Carrero, J.J.; Yilmaz, M.I.; Barany, P.; Snaedal, S.; Heimburger, O.; Lindholm, B.; Suliman, M.E. Low serum fetuin-A concentration predicts poor outcome only in the presence of inflammation in prevalent haemodialysis patients. Eur. J. Clin. Investig. 2008, 38, 804–811. [Google Scholar] [CrossRef] [PubMed]
- Miller, J.D.; Chu, Y.; Brooks, R.M.; Richenbacher, W.E.; Pena-Silva, R.; Heistad, D.D. Dysregulation of antioxidant mechanisms contributes to increased oxidative stress in calcific aortic valvular stenosis in humans. J. Am. Coll. Cardiol. 2008, 52, 843–850. [Google Scholar] [CrossRef] [PubMed]
- Miller, J.D.; Weiss, R.M.; Heistad, D.D. Calcific aortic valve stenosis: Methods, models, and mechanisms. Circ. Res. 2011, 108, 1392–1412. [Google Scholar] [CrossRef] [PubMed]
- Missiroli, S.; Bonora, M.; Patergnani, S.; Poletti, F.; Perrone, M.; Gafa, R.; Magri, E.; Raimondi, A.; Lanza, G.; Tacchetti, C.; et al. PML at Mitochondria-Associated Membranes Is Critical for the Repression of Autophagy and Cancer Development. Cell Rep. 2016, 16, 2415–2427. [Google Scholar] [CrossRef]
- Missiroli, S.; Perrone, M.; Gafa, R.; Nicoli, F.; Bonora, M.; Morciano, G.; Boncompagni, C.; Marchi, S.; Lebiedzinska-Arciszewska, M.; Vezzani, B.; et al. PML at mitochondria-associated membranes governs a trimeric complex with NLRP3 and P2X7R that modulates the tumor immune microenvironment. Cell Death Differ. 2023, 30, 429–441. [Google Scholar] [CrossRef]
- Moorlag, S.; Roring, R.J.; Joosten, L.A.B.; Netea, M.G. The role of the interleukin-1 family in trained immunity. Immunol. Rev. 2018, 281, 28–39. [Google Scholar] [CrossRef]
- Morciano, G.; Patergnani, S.; Pedriali, G.; Cimaglia, P.; Mikus, E.; Calvi, S.; Albertini, A.; Giorgi, C.; Campo, G.; Ferrari, R.; et al. Impairment of mitophagy and autophagy accompanies calcific aortic valve stenosis favouring cell death and the severity of disease. Cardiovasc. Res. 2022, 118, 2548–2559. [Google Scholar] [CrossRef]
- Mosch, J.; Gleissner, C.A.; Body, S.; Aikawa, E. Histopathological assessment of calcification and inflammation of calcific aortic valves from patients with and without diabetes mellitus. Histol. Histopathol. 2017, 32, 293–306. [Google Scholar]
- Nadlonek, N.; Lee, J.H.; Reece, T.B.; Weyant, M.J.; Cleveland, J.C., Jr.; Meng, X.; Fullerton, D.A. Interleukin-1 Beta induces an inflammatory phenotype in human aortic valve interstitial cells through nuclear factor kappa Beta. Ann. Thorac. Surg. 2013, 96, 155–162. [Google Scholar] [CrossRef]
- Nagy, E.; Lei, Y.; Martinez-Martinez, E.; Body, S.C.; Schlotter, F.; Creager, M.; Assmann, A.; Khabbaz, K.; Libby, P.; Hansson, G.K.; et al. Interferon-gamma Released by Activated CD8+ T Lymphocytes Impairs the Calcium Resorption Potential of Osteoclasts in Calcified Human Aortic Valves. Am. J. Pathol. 2017, 187, 1413–1425. [Google Scholar] [CrossRef]
- Naldini, A.; Filippi, I.; Miglietta, D.; Moschetta, M.; Giavazzi, R.; Carraro, F. Interleukin-1beta regulates the migratory potential of MDAMB231 breast cancer cells through the hypoxia-inducible factor-1alpha. Eur. J. Cancer 2010, 46, 3400–3408. [Google Scholar] [CrossRef] [PubMed]
- Negri, A.L. Role of prolyl hydroxylase/HIF-1 signaling in vascular calcification. Clin. Kidney J. 2023, 16, 205–209. [Google Scholar] [CrossRef] [PubMed]
- Ng, M.Y.W.; Wai, T.; Simonsen, A. Quality control of the mitochondrion. Dev. Cell 2021, 56, 881–905. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, T.D.; Schwarzer, M.; Schrepper, A.; Amorim, P.A.; Blum, D.; Hain, C.; Faerber, G.; Haendeler, J.; Altschmied, J.; Doenst, T. Increased Protein Tyrosine Phosphatase 1B (PTP1B) Activity and Cardiac Insulin Resistance Precede Mitochondrial and Contractile Dysfunction in Pressure-Overloaded Hearts. J. Am. Heart Assoc. 2018, 7, e008865. [Google Scholar] [CrossRef]
- Nkomo, V.T.; Gardin, J.M.; Skelton, T.N.; Gottdiener, J.S.; Scott, C.G.; Enriquez-Sarano, M. Burden of valvular heart diseases: A population-based study. Lancet 2006, 368, 1005–1011. [Google Scholar] [CrossRef]
- Nsaibia, M.J.; Mahmut, A.; Boulanger, M.C.; Arsenault, B.J.; Bouchareb, R.; Simard, S.; Witztum, J.L.; Clavel, M.A.; Pibarot, P.; Bosse, Y.; et al. Autotaxin interacts with lipoprotein(a) and oxidized phospholipids in predicting the risk of calcific aortic valve stenosis in patients with coronary artery disease. J. Internal Med. 2016, 280, 509–517. [Google Scholar] [CrossRef]
- O’Brien, K.D.; Zhao, X.Q.; Shavelle, D.M.; Caulfield, M.T.; Letterer, R.A.; Kapadia, S.R.; Probstfield, J.L.; Otto, C.M. Hemodynamic effects of the angiotensin-converting enzyme inhibitor, ramipril, in patients with mild to moderate aortic stenosis and preserved left ventricular function. J. Investig. Med. 2004, 52, 185–191. [Google Scholar] [CrossRef]
- Okui, T.; Iwashita, M.; Rogers, M.A.; Halu, A.; Atkins, S.K.; Kuraoka, S.; Abdelhamid, I.; Higashi, H.; Ramsaroop, A.; Aikawa, M.; et al. CROT (Carnitine O-Octanoyltransferase) Is a Novel Contributing Factor in Vascular Calcification via Promoting Fatty Acid Metabolism and Mitochondrial Dysfunction. Arterioscler. Thromb. Vasc. Biol. 2021, 41, 755–768. [Google Scholar] [CrossRef]
- Osako, M.K.; Nakagami, H.; Koibuchi, N.; Shimizu, H.; Nakagami, F.; Koriyama, H.; Shimamura, M.; Miyake, T.; Rakugi, H.; Morishita, R. Estrogen inhibits vascular calcification via vascular RANKL system: Common mechanism of osteoporosis and vascular calcification. Circ. Res. 2010, 107, 466–475. [Google Scholar] [CrossRef]
- Osnabrugge, R.L.; Mylotte, D.; Head, S.J.; Van Mieghem, N.M.; Nkomo, V.T.; LeReun, C.M.; Bogers, A.J.; Piazza, N.; Kappetein, A.P. Aortic stenosis in the elderly: Disease prevalence and number of candidates for transcatheter aortic valve replacement: A meta-analysis and modeling study. J. Am. Coll. Cardiol. 2013, 62, 1002–1012. [Google Scholar] [CrossRef] [PubMed]
- Otto, C.M.; Burwash, I.G.; Legget, M.E.; Munt, B.I.; Fujioka, M.; Healy, N.L.; Kraft, C.D.; Miyake-Hull, C.Y.; Schwaegler, R.G. Prospective study of asymptomatic valvular aortic stenosis. Clinical, echocardiographic, and exercise predictors of outcome. Circulation 1997, 95, 2262–2270. [Google Scholar] [CrossRef]
- Otto, C.M.; Kuusisto, J.; Reichenbach, D.D.; Gown, A.M.; O’Brien, K.D. Characterization of the early lesion of ‘degenerative’ valvular aortic stenosis. Histological and immunohistochemical studies. Circulation 1994, 90, 844–853. [Google Scholar] [CrossRef] [PubMed]
- Packer, M. Mutual Antagonism of Hypoxia-Inducible Factor Isoforms in Cardiac, Vascular, and Renal Disorders. JACC Basic Transl. Sci. 2020, 5, 961–968. [Google Scholar] [CrossRef] [PubMed]
- Parra-Izquierdo, I.; Castanos-Mollor, I.; Lopez, J.; Gomez, C.; San Roman, J.A.; Sanchez Crespo, M.; Garcia-Rodriguez, C. Calcification Induced by Type I Interferon in Human Aortic Valve Interstitial Cells Is Larger in Males and Blunted by a Janus Kinase Inhibitor. Arterioscler. Thromb. Vasc. Biol. 2018, 38, 2148–2159. [Google Scholar] [CrossRef] [PubMed]
- Parra-Izquierdo, I.; Castanos-Mollor, I.; Lopez, J.; Gomez, C.; San Roman, J.A.; Sanchez Crespo, M.; Garcia-Rodriguez, C. Lipopolysaccharide and interferon-gamma team up to activate HIF-1alpha via STAT1 in normoxia and exhibit sex differences in human aortic valve interstitial cells. Biochim. Biophys. Acta Mol. Basis Dis. 2019, 1865, 2168–2179. [Google Scholar] [CrossRef] [PubMed]
- Patergnani, S.; Bonora, M.; Ingusci, S.; Previati, M.; Marchi, S.; Zucchini, S.; Perrone, M.; Wieckowski, M.R.; Castellazzi, M.; Pugliatti, M.; et al. Antipsychotic drugs counteract autophagy and mitophagy in multiple sclerosis. Proc. Natl. Acad. Sci. USA 2021, 118, e2020078118. [Google Scholar] [CrossRef]
- Patergnani, S.; Bouhamida, E.; Leo, S.; Pinton, P.; Rimessi, A. Mitochondrial Oxidative Stress and “Mito-Inflammation”: Actors in the Diseases. Biomedicines 2021, 9, 216. [Google Scholar] [CrossRef]
- Pedriali, G.; Morciano, G.; Patergnani, S.; Cimaglia, P.; Morelli, C.; Mikus, E.; Ferrari, R.; Gasbarro, V.; Giorgi, C.; Wieckowski, M.R.; et al. Aortic Valve Stenosis and Mitochondrial Dysfunctions: Clinical and Molecular Perspectives. Int. J. Mol. Sci. 2020, 21, 4899. [Google Scholar] [CrossRef]
- Perrotta, I.; Moraca, F.M.; Sciangula, A.; Aquila, S.; Mazzulla, S. HIF-1alpha and VEGF: Immunohistochemical Profile and Possible Function in Human Aortic Valve Stenosis. Ultrastruct. Pathol. 2015, 39, 198–206. [Google Scholar] [CrossRef]
- Pickles, S.; Vigie, P.; Youle, R.J. Mitophagy and Quality Control Mechanisms in Mitochondrial Maintenance. Curr. Biol. 2018, 28, R170–R185. [Google Scholar] [CrossRef]
- Qian, D.; Lin, H.Y.; Wang, H.M.; Zhang, X.; Liu, D.L.; Li, Q.L.; Zhu, C. Normoxic induction of the hypoxic-inducible factor-1 alpha by interleukin-1 beta involves the extracellular signal-regulated kinase 1/2 pathway in normal human cytotrophoblast cells. Biol. Reprod. 2004, 70, 1822–1827. [Google Scholar] [CrossRef] [PubMed]
- Zhong, Z.; Liang, S.; Sanchez-Lopez, E.; He, F.; Shalapour, S.; Lin, X.J.; Wong, J.; Ding, S.; Seki, E.; Schnabl, B.; et al. New mitochondrial DNA synthesis enables NLRP3 inflammasome activation. Nature 2018, 560, 198–203. [Google Scholar] [CrossRef] [PubMed]
- Rajamannan, N.M.; Nealis, T.B.; Subramaniam, M.; Pandya, S.; Stock, S.R.; Ignatiev, C.I.; Sebo, T.J.; Rosengart, T.K.; Edwards, W.D.; McCarthy, P.M.; et al. Calcified rheumatic valve neoangiogenesis is associated with vascular endothelial growth factor expression and osteoblast-like bone formation. Circulation 2005, 111, 3296–3301. [Google Scholar] [CrossRef]
- Rajamannan, N.M.; Subramaniam, M.; Rickard, D.; Stock, S.R.; Donovan, J.; Springett, M.; Orszulak, T.; Fullerton, D.A.; Tajik, A.J.; Bonow, R.O.; et al. Human aortic valve calcification is associated with an osteoblast phenotype. Circulation 2003, 107, 2181–2184. [Google Scholar] [CrossRef]
- Richards, J.; El-Hamamsy, I.; Chen, S.; Sarang, Z.; Sarathchandra, P.; Yacoub, M.H.; Chester, A.H.; Butcher, J.T. Side-specific endothelial-dependent regulation of aortic valve calcification: Interplay of hemodynamics and nitric oxide signaling. Am. J. Pathol. 2013, 182, 1922–1931. [Google Scholar] [CrossRef] [PubMed]
- Roberts, W.C.; Ko, J.M. Frequency by decades of unicuspid, bicuspid, and tricuspid aortic valves in adults having isolated aortic valve replacement for aortic stenosis, with or without associated aortic regurgitation. Circulation 2005, 111, 920–925. [Google Scholar] [CrossRef]
- Rogers, M.A.; Maldonado, N.; Hutcheson, J.D.; Goettsch, C.; Goto, S.; Yamada, I.; Faits, T.; Sesaki, H.; Aikawa, M.; Aikawa, E. Dynamin-Related Protein 1 Inhibition Attenuates Cardiovascular Calcification in the Presence of Oxidative Stress. Circ. Res. 2017, 121, 220–233. [Google Scholar] [CrossRef]
- Roos, C.M.; Zhang, B.; Hagler, M.A.; Verzosa, G.C.; Huang, R.; Oehler, E.A.; Arghami, A.; Miller, J.D. Effects of Altering Mitochondrial Antioxidant Capacity on Molecular and Phenotypic Drivers of Fibrocalcific Aortic Valve Stenosis. Front. Cardiovasc. Med. 2021, 8, 694881. [Google Scholar] [CrossRef]
- Rudloff, S.; Jahnen-Dechent, W.; Huynh-Do, U. Tissue chaperoning-the expanded functions of fetuin-A beyond inhibition of systemic calcification. Pflugers Arch. 2022, 474, 949–962. [Google Scholar] [CrossRef]
- Rudloff, S.; Janot, M.; Rodriguez, S.; Dessalle, K.; Jahnen-Dechent, W.; Huynh-Do, U. Fetuin-A is a HIF target that safeguards tissue integrity during hypoxic stress. Nat. Commun. 2021, 12, 549. [Google Scholar] [CrossRef]
- Sabatine, M.S.; Giugliano, R.P.; Keech, A.C.; Honarpour, N.; Wiviott, S.D.; Murphy, S.A.; Kuder, J.F.; Wang, H.; Liu, T.; Wasserman, S.M.; et al. Evolocumab and Clinical Outcomes in Patients with Cardiovascular Disease. N. Engl. J. Med. 2017, 376, 1713–1722. [Google Scholar] [CrossRef]
- Sahoo, S.; Meijles, D.N.; Pagano, P.J. NADPH oxidases: Key modulators in aging and age-related cardiovascular diseases? Clin. Sci. 2016, 130, 317–335. [Google Scholar] [CrossRef]
- Sainger, R.; Grau, J.B.; Branchetti, E.; Poggio, P.; Lai, E.; Koka, E.; Vernick, W.J.; Gorman, R.C.; Bavaria, J.E.; Ferrari, G. Comparison of transesophageal echocardiographic analysis and circulating biomarker expression profile in calcific aortic valve disease. J. Heart Valve Dis. 2013, 22, 156–165. [Google Scholar]
- Salhiyyah, K.; Sarathchandra, P.; Latif, N.; Yacoub, M.H.; Chester, A.H. Hypoxia-mediated regulation of the secretory properties of mitral valve interstitial cells. Am. J. Physiol. Heart Circ. Physiol. 2017, 313, H14–H23. [Google Scholar] [CrossRef] [PubMed]
- Salim, M.T.; Villa-Roel, N.; Vogel, B.; Jo, H.; Yoganathan, A.P. HIF1A inhibitor PX-478 reduces pathological stretch-induced calcification and collagen turnover in aortic valve. Front. Cardiovasc. Med. 2022, 9, 1002067. [Google Scholar] [CrossRef]
- Sanchez-Duffhues, G.; Garcia de Vinuesa, A.; van de Pol, V.; Geerts, M.E.; de Vries, M.R.; Janson, S.G.; van Dam, H.; Lindeman, J.H.; Goumans, M.J.; Ten Dijke, P. Inflammation induces endothelial-to-mesenchymal transition and promotes vascular calcification through downregulation of BMPR2. J. Pathol. 2019, 247, 333–346. [Google Scholar] [CrossRef]
- Sanjuan-Pla, A.; Cervera, A.M.; Apostolova, N.; Garcia-Bou, R.; Victor, V.M.; Murphy, M.P.; McCreath, K.J. A targeted antioxidant reveals the importance of mitochondrial reactive oxygen species in the hypoxic signaling of HIF-1alpha. FEBS Lett. 2005, 579, 2669–2674. [Google Scholar] [CrossRef] [PubMed]
- Sapp, M.C.; Krishnamurthy, V.K.; Puperi, D.S.; Bhatnagar, S.; Fatora, G.; Mutyala, N.; Grande-Allen, K.J. Differential cell-matrix responses in hypoxia-stimulated aortic versus mitral valves. J. R. Soc. Interface 2016, 13, 20160449. [Google Scholar] [CrossRef]
- Sasagawa, T.; Nagamatsu, T.; Morita, K.; Mimura, N.; Iriyama, T.; Fujii, T.; Shibuya, M. HIF-2alpha, but not HIF-1alpha, mediates hypoxia-induced up-regulation of Flt-1 gene expression in placental trophoblasts. Sci. Rep. 2018, 8, 17375. [Google Scholar] [CrossRef] [PubMed]
- Schlotter, F.; de Freitas, R.C.C.; Rogers, M.A.; Blaser, M.C.; Wu, P.J.; Higashi, H.; Halu, A.; Iqbal, F.; Andraski, A.B.; Rodia, C.N.; et al. ApoC-III is a novel inducer of calcification in human aortic valves. J. Biol. Chem. 2021, 296, 100193. [Google Scholar] [CrossRef]
- Schoen, F.J. Evolving concepts of cardiac valve dynamics: The continuum of development, functional structure, pathobiology, and tissue engineering. Circulation 2008, 118, 1864–1880. [Google Scholar] [CrossRef]
- Schoen, F.J.; Levy, R.J. Calcification of tissue heart valve substitutes: Progress toward understanding and prevention. Ann. Thorac. Surg. 2005, 79, 1072–1080. [Google Scholar] [CrossRef] [PubMed]
- Semenza, G.L. Hypoxia-inducible factor 1: Regulator of mitochondrial metabolism and mediator of ischemic preconditioning. Biochim. Biophys. Acta 2011, 1813, 1263–1268. [Google Scholar] [CrossRef] [PubMed]
- Semenza, G.L.; Wang, G.L. A nuclear factor induced by hypoxia via de novo protein synthesis binds to the human erythropoietin gene enhancer at a site required for transcriptional activation. Mol. Cell. Biol. 1992, 12, 5447–5454. [Google Scholar] [PubMed]
- Shin, M.; Beane, T.J.; Quillien, A.; Male, I.; Zhu, L.J.; Lawson, N.D. Vegfa signals through ERK to promote angiogenesis, but not artery differentiation. Development 2016, 143, 3796–3805. [Google Scholar] [CrossRef] [PubMed]
- Shworak, N.W. Angiogenic modulators in valve development and disease: Does valvular disease recapitulate developmental signaling pathways? Curr. Opin. Cardiol. 2004, 19, 140–146. [Google Scholar] [CrossRef]
- Simon, M.C.; Liu, L.; Barnhart, B.C.; Young, R.M. Hypoxia-induced signaling in the cardiovascular system. Annu. Rev. Physiol. 2008, 70, 51–71. [Google Scholar] [CrossRef]
- Souilhol, C.; Harmsen, M.C.; Evans, P.C.; Krenning, G. Endothelial-mesenchymal transition in atherosclerosis. Cardiovasc. Res. 2018, 114, 565–577. [Google Scholar] [CrossRef]
- Stiehl, D.P.; Jelkmann, W.; Wenger, R.H.; Hellwig-Burgel, T. Normoxic induction of the hypoxia-inducible factor 1alpha by insulin and interleukin-1beta involves the phosphatidylinositol 3-kinase pathway. FEBS Lett. 2002, 512, 157–162. [Google Scholar] [CrossRef]
- Sun, Y.; Wang, W.; Tang, Y.; Wang, D.; Li, L.; Na, M.; Jiang, G.; Li, Q.; Chen, S.; Zhou, J. Microarray profiling and functional analysis of differentially expressed plasma exosomal circular RNAs in Graves’ disease. Biol. Res. 2020, 53, 32. [Google Scholar] [CrossRef] [PubMed]
- Swaminathan, G.; Krishnamurthy, V.K.; Sridhar, S.; Robson, D.C.; Ning, Y.; Grande-Allen, K.J. Hypoxia Stimulates Synthesis of Neutrophil Gelatinase-Associated Lipocalin in Aortic Valve Disease. Front. Cardiovasc. Med. 2019, 6, 156. [Google Scholar] [CrossRef] [PubMed]
- Szweras, M.; Liu, D.; Partridge, E.A.; Pawling, J.; Sukhu, B.; Clokie, C.; Jahnen-Dechent, W.; Tenenbaum, H.C.; Swallow, C.J.; Grynpas, M.D.; et al. alpha 2-HS glycoprotein/fetuin, a transforming growth factor-beta/bone morphogenetic protein antagonist, regulates postnatal bone growth and remodeling. J. Biol. Chem. 2002, 277, 19991–19997. [Google Scholar] [CrossRef] [PubMed]
- Tan, D.X.; Manchester, L.C.; Qin, L.; Reiter, R.J. Melatonin: A Mitochondrial Targeting Molecule Involving Mitochondrial Protection and Dynamics. Int. J. Mol. Sci. 2016, 17, 2124. [Google Scholar] [CrossRef] [PubMed]
- Thanassoulis, G. Lipoprotein (a) in calcific aortic valve disease: From genomics to novel drug target for aortic stenosis. J. Lipid Res. 2016, 57, 917–924. [Google Scholar] [CrossRef]
- Tian, H.; McKnight, S.L.; Russell, D.W. Endothelial PAS domain protein 1 (EPAS1), a transcription factor selectively expressed in endothelial cells. Genes Dev. 1997, 11, 72–82. [Google Scholar] [CrossRef]
- Tian, X.; Zhou, N.; Yuan, J.; Lu, L.; Zhang, Q.; Wei, M.; Zou, Y.; Yuan, L. Heat shock transcription factor 1 regulates exercise-induced myocardial angiogenesis after pressure overload via HIF-1alpha/VEGF pathway. J. Cell. Mol. Med. 2020, 24, 2178–2188. [Google Scholar] [CrossRef]
- Tuder, R.M.; Flook, B.E.; Voelkel, N.F. Increased gene expression for VEGF and the VEGF receptors KDR/Flk and Flt in lungs exposed to acute or to chronic hypoxia. Modulation of gene expression by nitric oxide. J. Clin. Investig. 1995, 95, 1798–1807. [Google Scholar] [CrossRef]
- Verstraete, A.; Herregods, M.C.; Verbrugghe, P.; Lamberigts, M.; Vanassche, T.; Meyns, B.; Oosterlinck, W.; Rega, F.; Adriaenssens, T.; Van Hoof, L.; et al. Antithrombotic Treatment After Surgical and Transcatheter Heart Valve Repair and Replacement. Front. Cardiovasc. Med. 2021, 8, 702780. [Google Scholar] [CrossRef]
- Viau, A.; El Karoui, K.; Laouari, D.; Burtin, M.; Nguyen, C.; Mori, K.; Pillebout, E.; Berger, T.; Mak, T.W.; Knebelmann, B.; et al. Lipocalin 2 is essential for chronic kidney disease progression in mice and humans. J. Clin. Investig. 2010, 120, 4065–4076. [Google Scholar] [CrossRef]
- Wakabayashi, K.; Tsujino, T.; Naito, Y.; Ezumi, A.; Lee-Kawabata, M.; Nakao, S.; Goda, A.; Sakata, Y.; Yamamoto, K.; Daimon, T.; et al. Administration of angiotensin-converting enzyme inhibitors is associated with slow progression of mild aortic stenosis in Japanese patients. Heart Vessels 2011, 26, 252–257. [Google Scholar] [CrossRef]
- Wang, A.; Rana, S.; Karumanchi, S.A. Preeclampsia: The role of angiogenic factors in its pathogenesis. Physiology 2009, 24, 147–158. [Google Scholar] [CrossRef] [PubMed]
- Wang, G.L.; Jiang, B.H.; Rue, E.A.; Semenza, G.L. Hypoxia-inducible factor 1 is a basic-helix-loop-helix-PAS heterodimer regulated by cellular O2 tension. Proc. Natl. Acad. Sci. USA 1995, 92, 5510–5514. [Google Scholar] [CrossRef] [PubMed]
- Wang, K.; Klionsky, D.J. Mitochondria removal by autophagy. Autophagy 2011, 7, 297–300. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Fang, D.; Yang, Q.; You, J.; Wang, L.; Wu, J.; Zeng, M.; Luo, M. Interactions between PCSK9 and NLRP3 inflammasome signaling in atherosclerosis. Front. Immunol. 2023, 14, 1126823. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Han, D.; Zhou, T.; Zhang, J.; Liu, C.; Cao, F.; Dong, N. Melatonin ameliorates aortic valve calcification via the regulation of circular RNA CircRIC3/miR-204-5p/DPP4 signaling in valvular interstitial cells. J. Pineal Res. 2020, 69, e12666. [Google Scholar] [CrossRef]
- Weisell, J.; Ohukainen, P.; Napankangas, J.; Ohlmeier, S.; Bergmann, U.; Peltonen, T.; Taskinen, P.; Ruskoaho, H.; Rysa, J. Heat shock protein 90 is downregulated in calcific aortic valve disease. BMC Cardiovasc. Disord. 2019, 19, 306. [Google Scholar] [CrossRef]
- Wu, X.; Zhao, Q.; Chen, Z.; Geng, Y.J.; Zhang, W.; Zhou, Q.; Yang, W.; Liu, Q.; Liu, H. Estrogen inhibits vascular calcification in rats via hypoxia-induced factor-1alpha signaling. Vascular 2020, 28, 465–474. [Google Scholar] [CrossRef]
- Xie, C.; Shen, Y.; Hu, W.; Chen, Z.; Li, Y. Angiotensin II promotes an osteoblast-like phenotype in porcine aortic valve myofibroblasts. Aging Clin. Exp. Res. 2016, 28, 181–187. [Google Scholar] [CrossRef]
- Xu, X.H.; Xu, J.; Xue, L.; Cao, H.L.; Liu, X.; Chen, Y.J. VEGF attenuates development from cardiac hypertrophy to heart failure after aortic stenosis through mitochondrial mediated apoptosis and cardiomyocyte proliferation. J. Cardiothorac. Surg. 2011, 6, 54. [Google Scholar] [CrossRef]
- Yan, H.F.; Liu, Z.Y.; Guan, Z.A.; Guo, C. Deferoxamine ameliorates adipocyte dysfunction by modulating iron metabolism in ob/ob mice. Endocr. Connect. 2018, 7, 604–616. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.; Fullerton, D.A.; Su, X.; Ao, L.; Cleveland, J.C., Jr.; Meng, X. Pro-osteogenic phenotype of human aortic valve interstitial cells is associated with higher levels of Toll-like receptors 2 and 4 and enhanced expression of bone morphogenetic protein 2. J. Am. Coll. Cardiol. 2009, 53, 491–500. [Google Scholar] [CrossRef] [PubMed]
- Yi, B.; Zeng, W.; Lv, L.; Hua, P. Changing epidemiology of calcific aortic valve disease: 30-year trends of incidence, prevalence, and deaths across 204 countries and territories. Aging 2021, 13, 12710–12732. [Google Scholar] [CrossRef] [PubMed]
- Yip, C.Y.; Chen, J.H.; Zhao, R.; Simmons, C.A. Calcification by valve interstitial cells is regulated by the stiffness of the extracellular matrix. Arterioscler. Thromb. Vasc. Biol. 2009, 29, 936–942. [Google Scholar] [CrossRef] [PubMed]
- Youle, R.J.; van der Bliek, A.M. Mitochondrial fission, fusion, and stress. Science 2012, 337, 1062–1065. [Google Scholar] [CrossRef]
- Yu, B.; Khan, K.; Hamid, Q.; Mardini, A.; Siddique, A.; Aguilar-Gonzalez, L.P.; Makhoul, G.; Alaws, H.; Genest, J.; Thanassoulis, G.; et al. Pathological significance of lipoprotein(a) in aortic valve stenosis. Atherosclerosis 2018, 272, 168–174. [Google Scholar] [CrossRef]
- Yuan, L.; Wang, M.; Liu, T.; Lei, Y.; Miao, Q.; Li, Q.; Wang, H.; Zhang, G.; Hou, Y.; Chang, X. Carbonic Anhydrase 1-Mediated Calcification Is Associated With Atherosclerosis, and Methazolamide Alleviates Its Pathogenesis. Front. Pharmacol. 2019, 10, 766. [Google Scholar] [CrossRef]
- Zeng, Q.; Song, R.; Fullerton, D.A.; Ao, L.; Zhai, Y.; Li, S.; Ballak, D.B.; Cleveland, J.C., Jr.; Reece, T.B.; McKinsey, T.A.; et al. Interleukin-37 suppresses the osteogenic responses of human aortic valve interstitial cells in vitro and alleviates valve lesions in mice. Proc. Natl. Acad. Sci. USA 2017, 114, 1631–1636. [Google Scholar] [CrossRef]
- Zhan, Q.; Zeng, Q.; Song, R.; Zhai, Y.; Xu, D.; Fullerton, D.A.; Dinarello, C.A.; Meng, X. IL-37 suppresses MyD88-mediated inflammatory responses in human aortic valve interstitial cells. Mol. Med. 2017, 23, 83–91. [Google Scholar] [CrossRef]
- Zhao, L.; Yang, N.; Song, Y.; Si, H.; Qin, Q.; Guo, Z. Effect of iron overload on endothelial cell calcification and its mechanism. Ann. Transl. Med. 2021, 9, 1658. [Google Scholar] [CrossRef]
- Zhao, T.; Jin, F.; Xiao, D.; Wang, H.; Huang, C.; Wang, X.; Gao, S.; Liu, J.; Yang, S.; Hao, J. IL-37/ STAT3/ HIF-1alpha negative feedback signaling drives gemcitabine resistance in pancreatic cancer. Theranostics 2020, 10, 4088–4100. [Google Scholar] [CrossRef]
- Zhao, W.; Zhao, D.; Yan, R.; Sun, Y. Cardiac oxidative stress and remodeling following infarction: Role of NADPH oxidase. Cardiovasc. Pathol. 2009, 18, 156–166. [Google Scholar] [CrossRef]
- Zhou, P.; Li, Q.; Su, S.; Dong, W.; Zong, S.; Ma, Q.; Yang, X.; Zuo, D.; Zheng, S.; Meng, X.; et al. Interleukin 37 Suppresses M1 Macrophage Polarization Through Inhibition of the Notch1 and Nuclear Factor Kappa B Pathways. Front. Cell Dev. Biol. 2020, 8, 56. [Google Scholar] [CrossRef] [PubMed]
- Zimna, A.; Kurpisz, M. Hypoxia-Inducible Factor-1 in Physiological and Pathophysiological Angiogenesis: Applications and Therapies. BioMed Res. Int. 2015, 2015, 549412. [Google Scholar] [CrossRef]
- Zorov, D.B.; Juhaszova, M.; Sollott, S.J. Mitochondrial reactive oxygen species (ROS) and ROS-induced ROS release. Physiol. Rev. 2014, 94, 909–950. [Google Scholar] [CrossRef] [PubMed]
- Smyrnias, I.; Gray, S.P.; Okonko, D.O.; Sawyer, G.; Zoccarato, A.; Catibog, N.; Lopez, B.; Gonzalez, A.; Ravassa, S.; Diez, J.; et al. Cardioprotective Effect of the Mitochondrial Unfolded Protein Response During Chronic Pressure Overload. J. Am. Coll. Cardiol. 2019, 73, 1795–1806. [Google Scholar] [CrossRef] [PubMed]
- Soini, Y.; Salo, T.; Satta, J. Angiogenesis is involved in the pathogenesis of nonrheumatic aortic valve stenosis. Human Pathol. 2003, 34, 756–763. [Google Scholar] [CrossRef]
- Stephens, E.H.; Saltarrelli, J.G., Jr.; Balaoing, L.R.; Baggett, L.S.; Nandi, I.; Anderson, K.M.; Morrisett, J.D.; Reardon, M.J.; Simpson, M.A.; Weigel, P.H.; et al. Hyaluronan turnover and hypoxic brown adipocytic differentiation are co-localized with ossification in calcified human aortic valves. Pathol. Res. Pract. 2012, 208, 642–650. [Google Scholar] [CrossRef]
- Stewart, B.F.; Siscovick, D.; Lind, B.K.; Gardin, J.M.; Gottdiener, J.S.; Smith, V.E.; Kitzman, D.W.; Otto, C.M. Clinical factors associated with calcific aortic valve disease. Cardiovascular Health Study. J. Am. Coll. Cardiol. 1997, 29, 630–634. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).