Different Kinetics of Serum ADAMTS13, GDF-15, and Neutrophil Gelatinase-Associated Lipocalin in the Early Phase of Aneurysmal Subarachnoid Hemorrhage
Abstract
1. Introduction
2. Results
2.1. Patients’ Characteristics
2.2. Levels of ADAMTS13, GDF-15, and NGAL in Different SAH Severity Groups
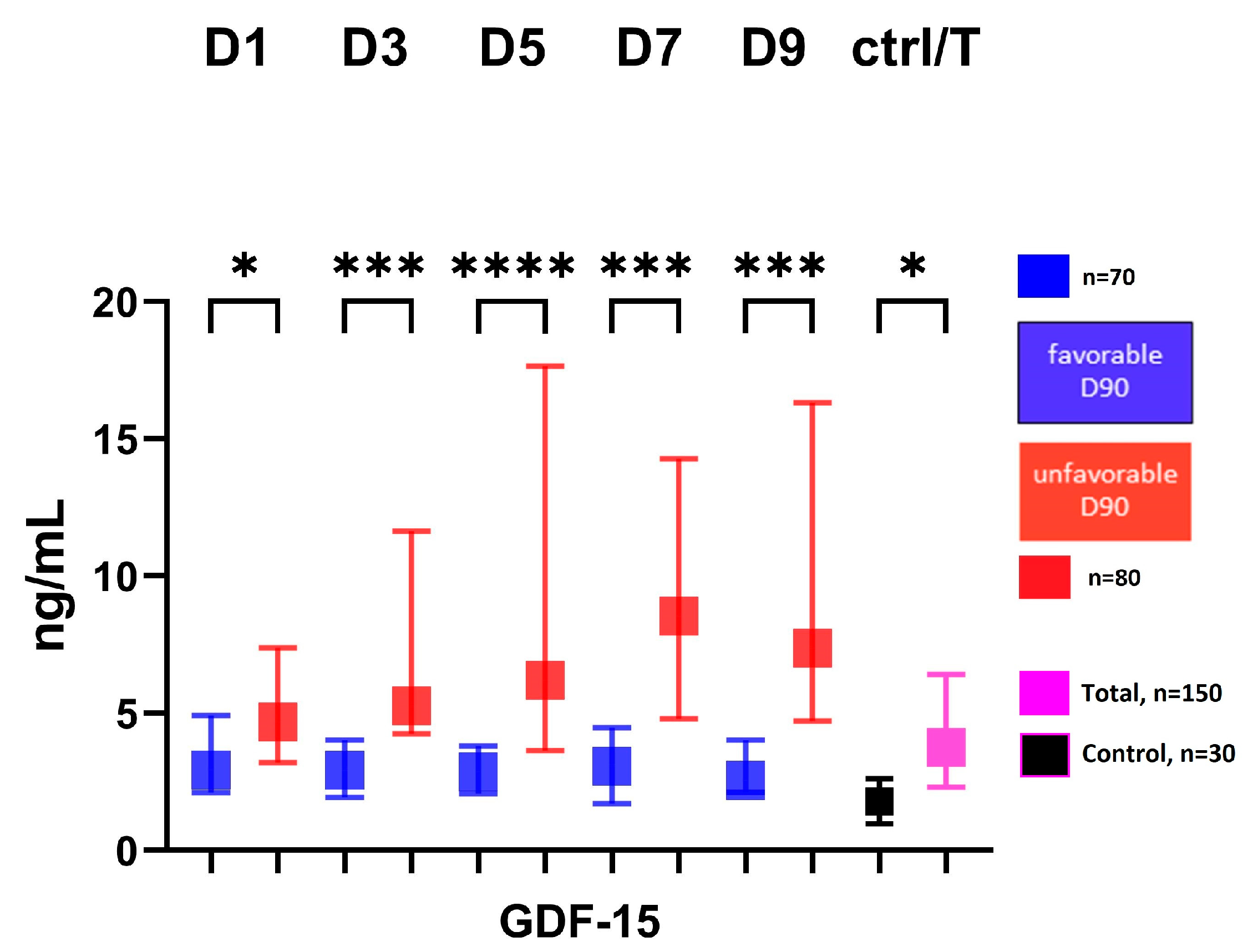
2.3. Association of ADAMTS13, NGAL, and GDF-15 with 3-Month Outcome
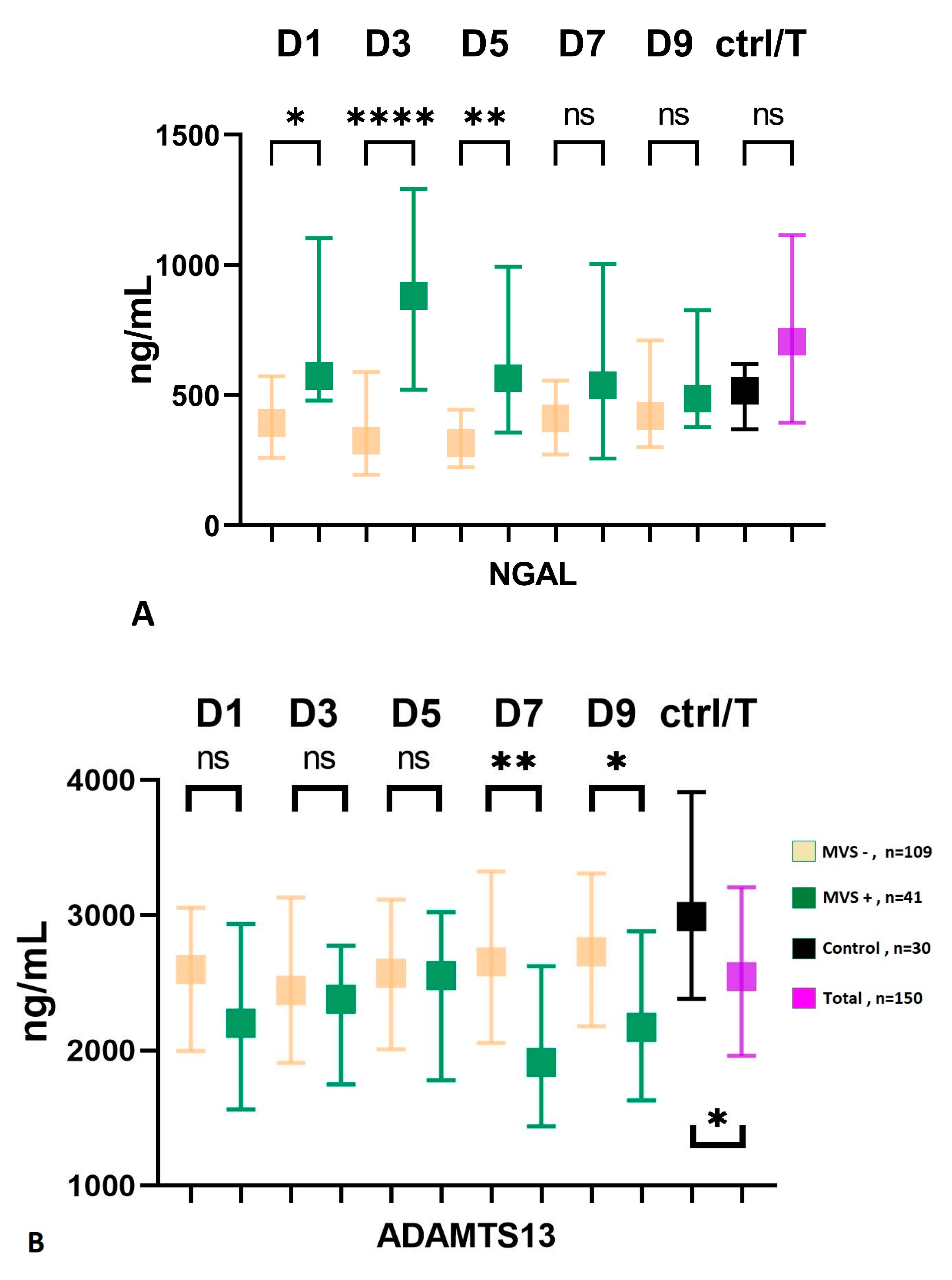
2.4. NGAL and ADAMTS13 in Patients with and without Macrovascular Vasospasm
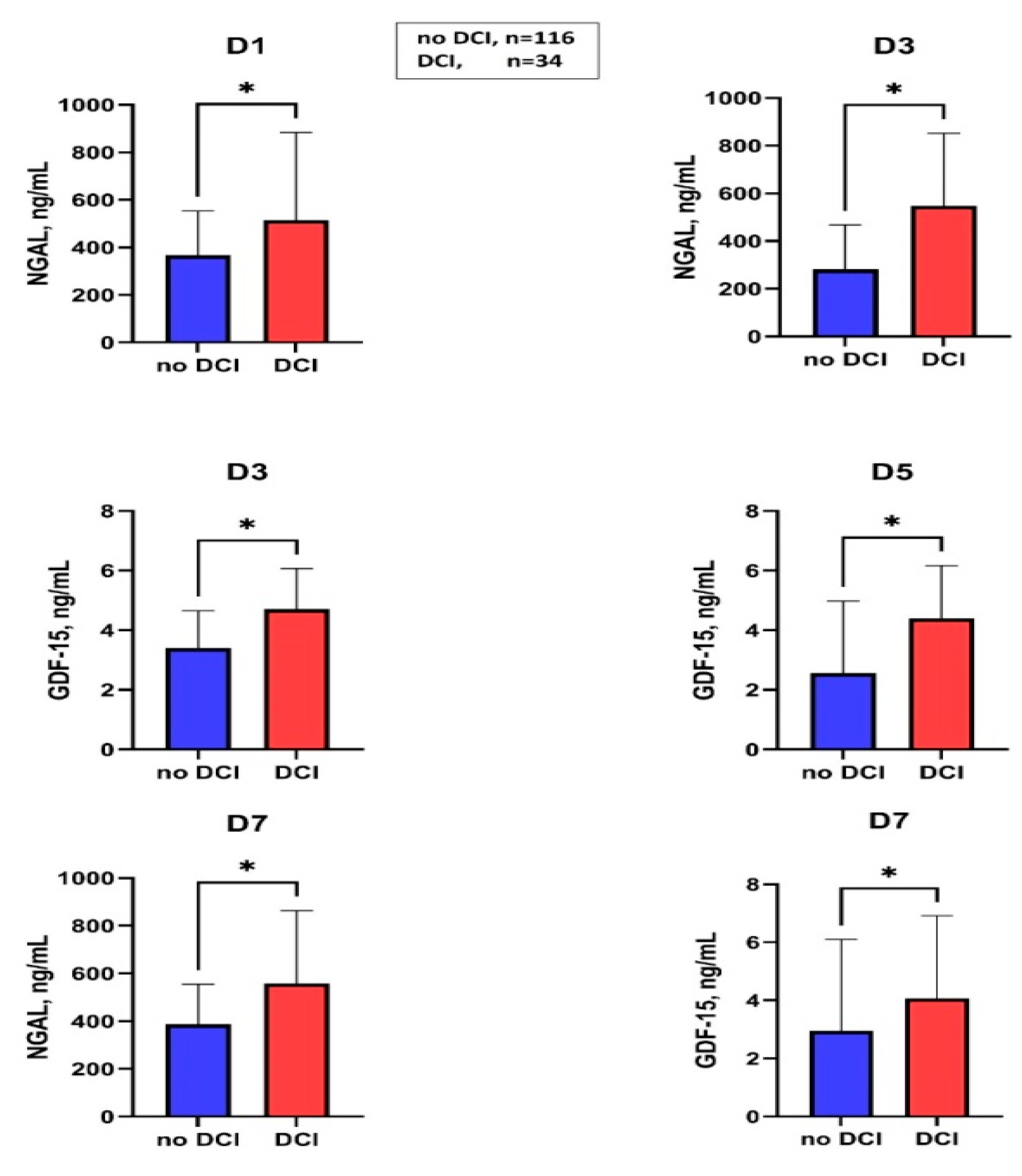
2.5. Association of Serum Levels of NGAL and GDF-15 in Patients with and without DCI
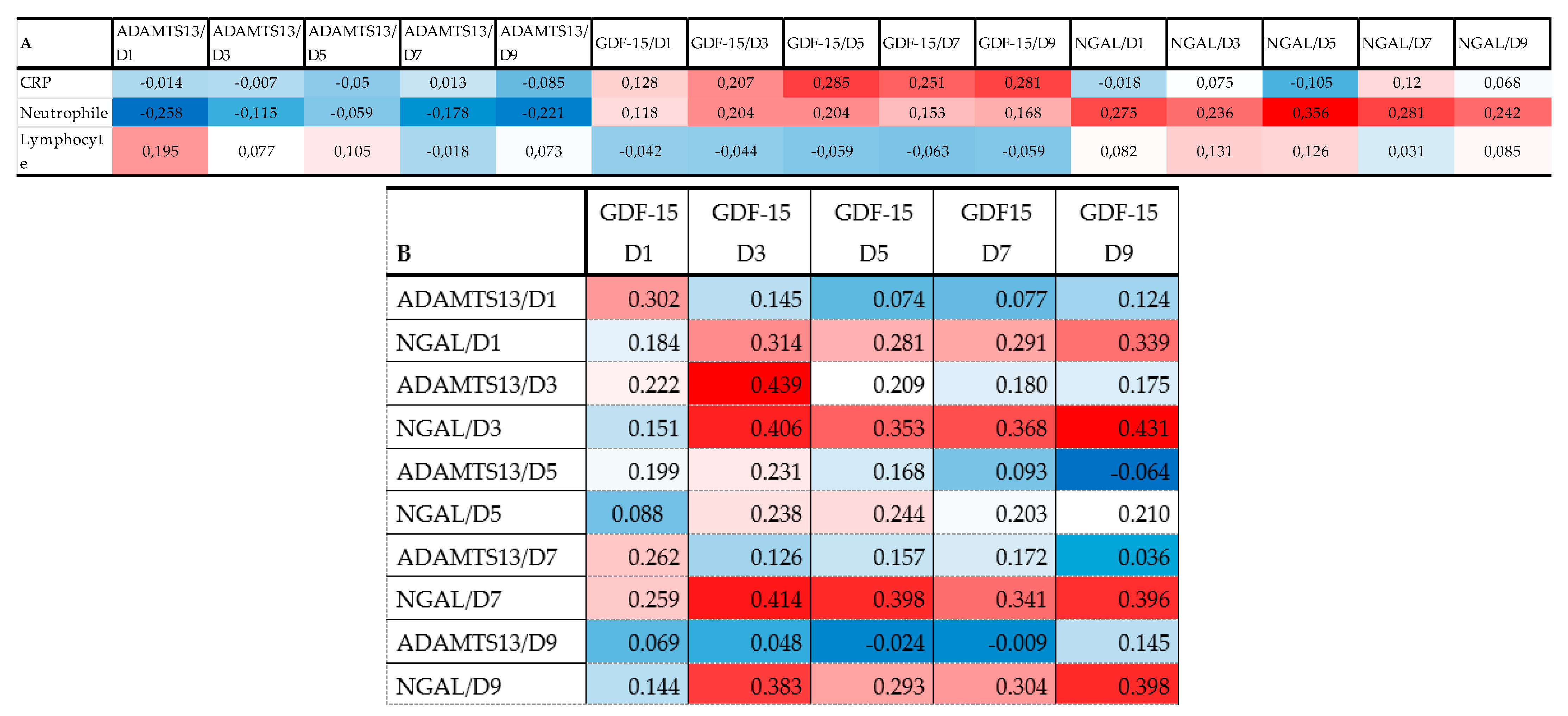
2.6. Correlation of Biomarkers with Each Other and Admission Inflammatory Parameters
3. Discussion
3.1. GDF-15 and Outcome
3.2. NGAL and ADAMTS13 in Macrovascular Vasospasm
3.3. Limitations
4. Materials and Methods
4.1. Subjects and Study Design
4.2. Clinical Definitions Data Collections and Outcome Measures
4.3. Sample Collection and Processing Protocol
4.4. Statistical Analysis
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Nieuwkamp, D.J.; Setz, L.E.; Algra, A.; Linn, F.H.; de Rooij, N.K.; Rinkel, G.J. Changes in case fatality of aneurysmal subarachnoid haemorrhage over time, according to age, sex, and region: A meta-analysis. Lancet Neurol. 2009, 8, 635–642. [Google Scholar] [CrossRef] [PubMed]
- Sehba, F.A.; Pluta, R.M.; Zhang, J.H. Metamorphosis of subarachnoid hemorrhage research: From delayed vasospasm to early brain injury. Mol. Neurobiol. 2011, 43, 27–40. [Google Scholar] [CrossRef] [PubMed]
- Lantigua, H.; Ortega-Gutierrez, S.; Schmidt, J.M.; Lee, K.; Badjatia, N.; Agarwal, S.; Claassen, J.; Connolly, E.S.; Mayer, S.A. Subarachnoid hemorrhage: Who dies, and why? Crit. Care 2015, 19, 309. [Google Scholar] [CrossRef] [PubMed]
- Negishi, K.; Hoshide, S.; Shimpo, M.; Kanegae, H.; Kario, K. Growth Differentiation Factor-15 Predicts Death and Stroke Event in Outpatients With Cardiovascular Risk Factors: The J-HOP Study. J. Am. Heart Assoc. 2021, 10, e022601. [Google Scholar] [CrossRef]
- Luan, H.H.; Wang, A.; Hilliard, B.K.; Carvalho, F.; Rosen, C.E.; Ahasic, A.M.; Herzog, E.L.; Kang, I.; Pisani, M.A.; Yu, S.; et al. GDF15 Is an Inflammation-Induced Central Mediator of Tissue Tolerance. Cell 2019, 178, 1231–1244.e11. [Google Scholar] [CrossRef] [PubMed]
- Worthmann, H.; Kempf, T.; Widera, C.; Tryc, A.B.; Goldbecker, A.; Ma, Y.T.; Deb, M.; Tountopoulou, A.; Lambrecht, J.; Heeren, M.; et al. Growth differentiation factor 15 plasma levels and outcome after ischemic stroke. Cerebrovasc. Dis. 2011, 32, 72–78. [Google Scholar] [CrossRef]
- Gröschel, K.; Schnaudigel, S.; Edelmann, F.; Niehaus, C.F.; Weber-Krüger, M.; Haase, B.; Lahno, R.; Seegers, J.; Wasser, K.; Wohlfahrt, J.; et al. Growth-differentiation factor-15 and functional outcome after acute ischemic stroke. J. Neurol. 2012, 259, 1574–1579. [Google Scholar] [CrossRef]
- Andersson, C.; Preis, S.R.; Beiser, A.; DeCarli, C.; Wollert, K.C.; Wang, T.J. Associations of Circulating Growth Differentiation Factor-15 and ST2 Concentrations With Subclinical Vascular Brain Injury and Incident Stroke. Stroke 2015, 46, 2568–2575. [Google Scholar] [CrossRef]
- Jeong, H.S.; Shin, J.W.; Jeong, J.Y.; Kwon, H.J.; Koh, H.S.; Kim, J.J.; Na, K.-R.; Lee, K.W.; Choi, D.E. Association of plasma level of growth differentiation factor-15 and clinical outcome after intraarterial thrombectomy. J. Stroke Cerebrovasc. Dis. 2020, 29, 104973. [Google Scholar] [CrossRef]
- McGrath, E.R.; Himali, J.J.; Levy, D.; Conner, S.C.; DeCarli, C.; Pase, M.P.; Ninomiya, T.; Ohara, T.; Courchesne, P.; Satizabal, C.L.; et al. Growth Differentiation Factor 15 and NT-proBNP as Blood-Based Markers of Vascular Brain Injury and Dementia. J. Am. Heart Assoc. 2020, 9, e014659. [Google Scholar] [CrossRef]
- Song, L.; Söderholm, M.; Svensson, E.H.; Borné, Y.; Engström, G. Circulating Growth Differentiation Factor 15 Levels Are Associated With Risk of Both Intracerebral and Subarachnoid Hemorrhage. Front. Neurol. 2021, 9, 664010. [Google Scholar] [CrossRef] [PubMed]
- Dong, X.; Nao, J. Association of serum growth differentiation factor 15 level with acute ischemic stroke in a Chinese population. Int. J. Neurosci. 2019, 129, 1247–1255. [Google Scholar] [CrossRef] [PubMed]
- Jin, M.; Kim, J.H.; Jang, E.; Lee, Y.M.; Soo Han, H.; Woo, D.K.; Park, D.H.; Kook, H.; Suk, K. Lipocalin-2 deficiency attenuates neuroinflammation and brain injury after transient middle cerebral artery occlusion in mice. J. Cereb. Blood Flow Metab. 2014, 34, 1306–1314. [Google Scholar] [CrossRef] [PubMed]
- Yu, F.; Saand, A.; Xing, C.; Lee, J.W.; Hsu, L.; Palmer, O.P.; Jackson, V.; Tang, L.; Ning, M.; Du, R.; et al. CSF lipocalin-2 increases early in subarachnoid hemorrhage are associated with neuroinflammation and unfavorable outcome. J. Cereb. Blood Flow Metab. 2021, 41, 2524–2533. [Google Scholar] [CrossRef]
- Chauhan, A.K.; Kisucka, J.; Brill, A.; Walsh, M.T.; Scheiflinger, F.; Wagner, D.D. ADAMTS13: A new link between thrombosis and inflammation. J. Exp. Med. 2008, 205, 2065–2074. [Google Scholar] [CrossRef]
- Muroi, C.; Fujioka, M.; Mishima, K.; Irie, K.; Fujimura, Y.; Nakano, T.; Fandino, J.; Keller, E.; Iwasaki, K.; Fujiwara, M. Effect of ADAMTS-13 on cerebrovascular microthrombosis and neuronal injury after experimental subarachnoid hemorrhage. J. Thromb. Haemost. 2014, 12, 505–514. [Google Scholar] [CrossRef]
- Friedrich, V.; Flores, R.; Muller, A.; Sehba, F.A. Luminal platelet aggregates in functional deficits in parenchymal vessels after subarachnoid hemorrhage. Brain Res. 2010, 1, 179–187. [Google Scholar] [CrossRef]
- Vergouwen, M.D.; Bakhtiari, K.; van Geloven, N.; Vermeulen, M.; Roos, Y.B.; Meijers, J.C. Reduced ADAMTS13 activity in delayed cerebral ischemia after aneurysmal subarachnoid hemorrhage. J. Cereb. Blood Flow Metab. 2009, 29, 1734–1741. [Google Scholar] [CrossRef]
- Dorhout Mees, S.M.; Algra, A.; Vandertop, W.P.; van Kooten, F.; Kuijsten, H.A.; Boiten, J.; van Oostenbrugge, R.J.; Salman, R.A.-S.; Lavados, P.M.; Rinkel, G.J.E.; et al. MASH-2 Study Group. Magnesium for aneurysmal subarachnoid haemorrhage (MASH-2): A randomised placebo-controlled trial. Lancet 2012, 380, 44–49. [Google Scholar] [CrossRef]
- Kirkpatrick, P.J.; Turner, C.L.; Smith, C.; Hutchinson, P.J.; Murray, G.D. STASH Collaborators. Simvastatin in aneurysmal subarachnoid haemorrhage (STASH): A multicentre randomised phase 3 trial. Lancet Neurol. 2014, 13, 666–675. [Google Scholar] [CrossRef]
- Ago, T.; Sadoshima, J. GDF15, a cardioprotective TGF-beta superfamily protein. Circ. Res. 2006, 98, 294–297. [Google Scholar] [CrossRef]
- Yang, L.; Chang, C.C.; Sun, Z.; Madsen, D.; Zhu, H.; Padkjær, S.B.; Wu, X.; Huang, T.; Hultman, K.; Paulsen, S.J.; et al. GFRAL is the receptor for GDF15 and is required for the anti-obesity effects of the ligand. Nat. Med. 2017, 23, 1158–1166. [Google Scholar] [CrossRef]
- Corre, J.; Hébraud, B.; Bourin, P. Concise review: Growth differentiation factor 15 in pathology: A clinical role? Stem Cells Transl. Med. 2013, 2, 946–952. [Google Scholar] [CrossRef] [PubMed]
- Reyes, J.; Yap, G.S. Emerging Roles of Growth Differentiation Factor 15 in Immunoregulation and Pathogenesis. J. Immunol. 2023, 210, 5–11. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Noren Hooten, N.; Evans, M.K. CRP Stimulates GDF15 Expression in Endothelial Cells through p53. Mediat. Inflamm. 2018, 3, 8278039. [Google Scholar] [CrossRef] [PubMed]
- Adela, R.; Banerjee, S.K. GDF-15 as a Target and Biomarker for Diabetes and Cardiovascular Diseases: A Translational Prospective. J. Diabetes Res. 2015, 2015, 490842. [Google Scholar] [CrossRef]
- Wischhusen, J.; Melero, I.; Fridman, W.H. Growth/Differentiation Factor-15 (GDF-15): From Biomarker to Novel Targetable Immune Checkpoint. Front. Immunol. 2020, 19, 951. [Google Scholar] [CrossRef]
- Schroll, A.; Eller, K.; Feistritzer, C.; Nairz, M.; Sonnweber, T.; Moser, P.A.; Rosenkranz, A.R.; Theurl, I.; Weiss, G. Lipocalin-2 ameliorates granulocyte functionality. Eur. J. Immunol. 2012, 42, 3346–3357. [Google Scholar] [CrossRef]
- Xu, X.; Jackson, P.L.; Tanner, S.; Hardison, M.T.; Abdul Roda, M.; Blalock, J.E.; Gaggar, A. A self-propagating matrix metalloprotease-9 (MMP-9) dependent cycle of chronic neutrophilic inflammation. PLoS ONE 2011, 6, e15781. [Google Scholar] [CrossRef]
- Dong, M.; Xi, G.; Keep, R.F.; Hua, Y. Role of iron in brain lipocalin 2 upregulation after intracerebral hemorrhage in rats. Brain Res. 2013, 10, 86–92. [Google Scholar] [CrossRef]
- Shishido, H.; Toyota, Y.; Hua, Y.; Keep, R.F.; Xi, G. Role of lipocalin 2 in intraventricular haemoglobin-induced brain injury. Stroke Vasc. Neurol. 2016, 1, 37–43. [Google Scholar] [CrossRef] [PubMed]
- Marques, F.; Mesquita, S.D.; Sousa, J.C.; Coppola, G.; Gao, F.; Geschwind, D.H.; Columba-Cabezas, S.; Aloisi, F.; Degn, M.; Cerqueira, J.J.; et al. Lipocalin 2 is present in the EAE brain and is modulated by natalizumab. Front. Cell. Neurosci. 2012, 9, 33. [Google Scholar] [CrossRef] [PubMed]
- Mårtensson, J.; Bell, M.; Xu, S.; Bottai, M.; Ravn, B.; Venge, P.; Martling, C.R. Association of plasma neutrophil gelatinase-associated lipocalin (NGAL) with sepsis and acute kidney dysfunction. Biomarkers 2013, 18, 349–356. [Google Scholar] [CrossRef]
- Egashira, Y.; Zhao, H.; Hua, Y.; Keep, R.F.; Xi, G. White Matter Injury After Subarachnoid Hemorrhage: Role of Blood-Brain Barrier Disruption and Matrix Metalloproteinase-9. Stroke 2015, 46, 2909–2915. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.R.; Li, Y.P.; Gao, S.; Xia, W.; Gao, K.; Kong, Q.-H.; Qi, H.; Wu, L.; Qu, J.-M.; Bai, C.; et al. Increased serum levels of lipocalin-1 and -2 in patients with stable chronic obstructive pulmonary disease. Int. J. Chronic Obs. Pulm. Dis. 2014, 9, 543–549. [Google Scholar] [CrossRef] [PubMed]
- Ni, W.; Zheng, M.; Xi, G.; Keep, R.F.; Hua, Y. Role of lipocalin-2 in brain injury after intracerebral hemorrhage. J. Cereb. Blood Flow Metab. 2015, 35, 1454–1461. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Fang, Q.; Dang, B.Q.; Shen, X.M.; Shu, Z.; Zuo, G.; He, W.-C.; Chen, G. Potential contribution of matrix metalloproteinase-9 (mmp-9) to cerebral vasospasm after experimental subarachnoid hemorrhage in rats. Ann. Clin. Lab. Sci. 2012, 42, 14–20. [Google Scholar]
- Akpinar, A.; Ucler, N.; Erdogan, U.; Baydin, S.S.; Gungor, A.; Tugcu, B. Measuring serum matrix metalloproteinase-9 levels in peripheral blood after subarachnoid hemorrhage to predict cerebral vasospasm. Springerplus 2016, 5, 1153. [Google Scholar] [CrossRef]
- Mehta, V.; Russin, J.; Spirtos, A.; He, S.; Adamczyk, P.; Amar, A.P.; Mack, W.J. Matrix Metalloproteinases in Cerebral Vasospasm following Aneurysmal Subarachnoid Hemorrhage. Neurol. Res. Int. 2013, 2013, 943761. [Google Scholar] [CrossRef]
- Lucke-Wold, B.; Hosaka, K.; Dodd, W.; Motwani, K.; Laurent, D.; Martinez, M.; Hoh, B. Interleukin-6: Important Mediator of Vasospasm Following Subarachnoid Hemorrhage. Curr. Neurovasc. Res. 2021, 18, 364–369. [Google Scholar] [CrossRef]
- Vecchione, C.; Frati, A.; Di Pardo, A.; Cifelli, G.; Carnevale, D.; Gentile, M.T.; Carangi, R.; Landolfi, A.; Carullo, P.; Bettarini, U.; et al. Tumor necrosis factor-alpha mediates hemolysis-induced vasoconstriction and the cerebral vasospasm evoked by subarachnoid hemorrhage. Hypertension 2009, 54, 150–156. [Google Scholar] [CrossRef] [PubMed]
- Sadler, J.E. Von Willebrand factor, ADAMTS13, and thrombotic thrombocytopenic purpura. Blood 2008, 112, 11–18. [Google Scholar] [CrossRef] [PubMed]
- Dodd, W.S.; Laurent, D.; Dumont, A.S.; Hasan, D.M.; Jabbour, P.M.; Starke, R.M.; Hosaka, K.; Polifka, A.J.; Hoh, B.L.; Chalouhi, N. Pathophysiology of Delayed Cerebral Ischemia After Subarachnoid Hemorrhage: A Review. J. Am. Heart Assoc. 2021, 10, e021845. [Google Scholar] [CrossRef] [PubMed]
- Matsumoto, H.; Takeba, J.; Umakoshi, K.; Kikuchi, S.; Ohshita, M.; Annen, S.; Moriyama, N.; Nakabayashi, Y.; Sato, N.; Aibiki, M. ADAMTS13 activity decreases in the early phase of trauma associated with coagulopathy and systemic inflammation: A prospective observational study. Thromb. J. 2021, 19, 17. [Google Scholar] [CrossRef]
- Lauzier, D.C.; Jayaraman, K.; Yuan, J.Y.; Diwan, D.; Vellimana, A.K.; Osbun, J.W.; Chatterjee, A.R.; Athiraman, U.; Dhar, R.; Zipfel, G.J. Early Brain Injury After Subarachnoid Hemorrhage: Incidence and Mechanisms. Stroke 2023, 54, 1426–1440. [Google Scholar] [CrossRef]
- Kramer, D.R.; Winer, J.L.; Pease, B.A.; Amar, A.P.; Mack, W.J. Cerebral vasospasm in traumatic brain injury. Neurol. Res. Int. 2013, 2013, 415813. [Google Scholar] [CrossRef]
- Vergouwen, M.D.; Vermeulen, M.; van Gijn, J.; Rinkel, G.J.; Wijdicks, E.F.; Muizelaar, J.P.; Mendelow, A.D.; Juvela, S.; Yonas, H.; Terbrugge, K.G.; et al. Definition of delayed cerebral ischemia after aneurysmal subarachnoid hemorrhage as an outcome event in clinical trials and observational studies: Proposal of a multidisciplinary research group. Stroke 2010, 41, 2391–2395. [Google Scholar] [CrossRef]
- Mandrekar, J.N. Receiver operating characteristic curve in diagnostic test assessment. J. Thorac. Oncol. 2010, 5, 1315–1316. [Google Scholar] [CrossRef]
| Variable | Patients with SAH |
|---|---|
| N | 150 |
| Age (years), mean ± SD | 55 ± 12 |
| Gender, female, numbers (% of total) | 104 (69) |
| Hypertension, numbers (% of total) | 71 (47) |
| NIDDM, numbers (% of total) | 16 (11) |
| Smoking, numbers (% of total) | 28 (19) |
| modified Fischer score, median, IQR | 3 (2–3) |
| WFNS score, numbers (% of total) | |
| I | 59 (39) |
| II | 33 (22) |
| III | 11 (7.3) |
| IV | 10 (6.7) |
| V | 37 (25) |
| Multiple aneurysms, numbers (% of total) | 43 (29) |
| Aneurysm location, numbers (% of total) | |
| ICA | 18 (12) |
| MCA | 39 (26) |
| ACoA | 51 (34) |
| PCom | 12 (8) |
| ACA | 11 (7) |
| VB | 19 (13) |
| Ventricular drain, numbers (% of total) | 68 (45) |
| Lumbar drain, numbers (% of total) | 57 (38) |
| Decompressive craniotomy, numbers (% of total) | 18 (12) |
| Mechanical ventilation, numbers (% of total) | 66 (44) |
| CSF infection, numbers (% of total) | 14 (9) |
| Systemic infection, numbers (% of total) | 33 (22) |
| Sonologic vasospasm, numbers (% of total) | 56 (37) |
| Onset time of sonologic vasospasm, days, median (IQR) | 6.5 (4–9) |
| Macrovascular vasospasm, numbers (% of total) | 41 (27) |
| Onset time of macrovascular vasospasm, day, median (IQR) | 8 (6–9) |
| Delayed cerebral ischemia, numbers (% of total) | 34 (23) |
| Onset time of DCI, day, median (IQR) | 8 (5–11) |
| Favorable outcome (Day 90), numbers (% of total) | 70 (47) |
| Marker/Time Points | WFNS I-III, n = 102 | WFNS IV-V, n = 48 | |||||
|---|---|---|---|---|---|---|---|
| Median, ng/mL | Interquartile Range | Median, ng/mL | Interquartile Range | p-Value | |||
| ADAMTS13/D1 | 2589.68 | 1798.74 | 3078.70 | 2383.22 | 1918.90 | 2871.88 | 0.206 |
| ADAMTS13/D3 | 2530.23 | 1920.05 | 3154.64 | 2190.62 | 1834.78 | 2660.88 | 0.184 |
| ADAMTS13/D5 | 2573.34 | 1965.41 | 3026.97 | 2480.44 | 1837.69 | 3135.82 | 0.622 |
| ADAMTS13/D7 | 2632.80 | 2019.50 | 3209.94 | 2198.12 | 1598.33 | 2730.10 | 0.038 |
| ADAMTS13/D9 | 2660.20 | 2162.93 | 3319.75 | 2224.08 | 1695.33 | 3077.56 | 0.091 |
| Ptrend = 0.747 | Ptrend = 0.867 | ||||||
| GDF15/D1 | 2.99 | 1.93 | 4.85 | 4.64 | 3.45 | 7.40 | 0.001 |
| GDF15/D3 | 2.92 | 1.62 | 4.68 | 4.35 | 3.94 | 6.29 | <0.001 |
| GDF15/D5 | 2.54 | 1.84 | 3.86 | 6.04 | 3.77 | 16.04 | <0.001 |
| GDF15/D7 | 2.41 | 1.63 | 3.92 | 7.33 | 5.10 | 14.26 | <0.001 |
| GDF15/D9 | 2.74 | 1.66 | 3.87 | 6.28 | 4.60 | 13.53 | <0.001 |
| Ptrend = 0.919 | Ptrend = 0.208 | ||||||
| NGAL/D1 | 462.23 | 266.20 | 721.58 | 534.41 | 373.04 | 719.52 | 0.230 |
| NGAL/D3 | 350.13 | 229.53 | 708.22 | 496.44 | 251.35 | 768.72 | 0.315 |
| NGAL/D5 | 331.34 | 235.64 | 557.28 | 389.24 | 288.07 | 705.22 | 0.180 |
| NGAL/D7 | 407.84 | 249.49 | 581.54 | 490.46 | 368.16 | 788.13 | 0.068 |
| NGAL/D9 | 420.86 | 302.60 | 754.04 | 494.53 | 360.65 | 724.72 | 0.543 |
| Ptrend = 0.284 | Ptrend = 0.799 | ||||||
| mFisher score I-II, n = 51 | mFisher score III-IV, n = 99 | ||||||
| ADAMTS13/D1 | 1988.69 | 1601.32 | 2589.68 | 2823.11 | 1941.26 | 3008.73 | 0.014 |
| ADAMTS13/D3 | 1972.90 | 1608.09 | 2565.11 | 2633.11 | 1921.11 | 3218.44 | 0.018 |
| ADAMTS13/D5 | 2310.33 | 1824.31 | 2693.09 | 2563.74 | 1911.39 | 3116.20 | 0.162 |
| ADAMTS13/D7 | 2144.63 | 1742.80 | 2613.93 | 2576.12 | 1820.17 | 3209.94 | 0.252 |
| ADAMTS13/D9 | 2367.95 | 2084.82 | 3204.92 | 2422.68 | 1705.39 | 3296.32 | 0.755 |
| Ptrend = 0.057 | Ptrend = 0.949 | ||||||
| GDF15/D1 | 2.43 | 1.76 | 3.90 | 3.79 | 2.28 | 6.82 | 0.004 |
| GDF15/D3 | 3.00 | 1.39 | 3.97 | 4.09 | 2.56 | 5.50 | 0.012 |
| GDF15/D5 | 2.13 | 1.39 | 3.18 | 3.77 | 2.65 | 10.32 | <0.001 |
| GDF15/D7 | 1.76 | 1.20 | 2.67 | 5.11 | 3.07 | 9.74 | <0.001 |
| GDF15/D9 | 2.38 | 1.61 | 3.62 | 4.37 | 2.48 | 10.78 | <0.001 |
| Ptrend = 0.436 | Ptrend = 0.376 | ||||||
| NGAL/D1 | 309.04 | 188.97 | 462.23 | 566.08 | 380.50 | 877.28 | <0.001 |
| NGAL/D3 | 252.36 | 149.78 | 342.94 | 505.36 | 280.46 | 1176.92 | 0.001 |
| NGAL/D5 | 298.72 | 216.70 | 410.36 | 374.22 | 245.35 | 705.22 | 0.072 |
| NGAL/D7 | 340.73 | 253.22 | 538.52 | 434.01 | 287.65 | 612.29 | 0.097 |
| NGAL/D9 | 398.80 | 272.03 | 668.35 | 477.61 | 299.67 | 672.98 | 0.738 |
| Ptrend = 0.750 | Ptrend = 0.106 | ||||||
| Parameter | p Value | Unadjusted OR (95% CI) | p Value | Adjusted OR (95% CI) † |
|---|---|---|---|---|
| GDF-15/D1 | 0.001 | 1.456 (1.159–1.830) | 0.015 | 1.895 (1.132–3.172) |
| GDF-15/D3 | <0.001 | 1.848 (1.339–2.549) | 0.008 | 1.599 (1.129–2.267) |
| GDF-15/D5 | <0.001 | 1.802 (1.326–2.449) | 0.005 | 1.778 (1.195–2.645) |
| GDF-15/D7 | <0.001 | 1.806 (1.362–2.394) | 0.007 | 1.587 (1.137–2.216) |
| GDF-15/D9 | 0.001 | 1.681 (1.237–2.283) | 0.042 | 1.512 (1.016–2.251) |
| Cut-Off Value * | AUC | p-Value | 95% CI | Sensitivity (%) | Specificity (%) | Power | ||
|---|---|---|---|---|---|---|---|---|
| Lower Limit Upper Limit | ||||||||
| Total cohort | ||||||||
| GDF-15 D1 | 3.16 | 0.728 | <0.001 | 0.627 | 0.830 | 76.1 | 61.7 | acceptable |
| GDF-15 D3 | 3.93 | 0.844 | <0.001 | 0.765 | 0.924 | 78.6 | 81.2 | excellent |
| GDF-15 D5 | 2.77 | 0.865 | <0.001 | 0.790 | 0.940 | 89.1 | 70.8 | excellent |
| GDF-15 D7 | 3.59 | 0.847 | <0.001 | 0.764 | 0.930 | 82.2 | 82.6 | excellent |
| GDF-15 D9 | 3.06 | 0.809 | <0.001 | 0.711 | 0.907 | 78.4 | 66.7 | excellent |
| WFNS I-II-III | ||||||||
| GDF-15 D1 | 3.31 | 0.669 | 0.037 | 0.519 | 0.819 | 66.7 | 64.4 | poor |
| GDF-15 D3 | 3.97 | 0.833 | <0.001 | 0.728 | 0.938 | 73.7 | 82.6 | excellent |
| GDF-15 D5 | 3.06 | 0.783 | <0.001 | 0.657 | 0.909 | 75 | 78.7 | acceptable |
| GDF-15 D7 | 2.41 | 0.699 | 0.015 | 0.538 | 0.859 | 66.7 | 56.8 | poor |
| GDF-15 D9 | 3.06 | 0.696 | 0.017 | 0.542 | 0.851 | 66.7 | 65.9 | poor |
| Cut-Off Value * | AUC | p-Value | 95% CI | Sensitivity (%) | Specificity (%) | Power | ||
|---|---|---|---|---|---|---|---|---|
| Lower Limit Upper Limit | ||||||||
| NGAL/D1 | 453 | 0.709 | 0.001 | 0.590 | 0.829 | 82.1 | 56.9 | acceptable |
| NGAL/D3 | 518 | 0.776 | <0.001 | 0.665 | 0.887 | 78.3 | 73.1 | acceptable |
| NGAL/D5 | 368 | 0.719 | 0.001 | 0.601 | 0.838 | 74.1 | 61.2 | acceptable |
| ADAMTS13/D7 | 2236 | 0.701 | 0.003 | 0.574 | 0.827 | 68.2 | 64 | acceptable |
| ADAMTS13/D9 | 2276 | 0.676 | 0.024 | 0.525 | 0.827 | 68.9 | 72.2 | poor |
| Parameter | p Value | Unadjusted OR (95% CI) | p Value | Adjusted OR (95% CI) † |
|---|---|---|---|---|
| NGAL/D1 | 0.002 | 1.002 (1.001–1.003) | 0.088 | 1.002 (1.000–1.003) |
| NGAL/D3 | 0.006 | 1.001 (1.000–1.002) | 0.056 | 1.002 (1.000–1.004) |
| NGAL/D5 | 0.007 | 1.002 (1.000–1.003) | 0.808 | 1.000 (0.997–1.004) |
| ADAMTS13/D7 | 0.004 | 0.999 (0.998–1.000) | 0.036 | 0.999 (0.997–1.000) |
| ADAMTS13/D9 | 0.032 | 0.999 (0.999–1.000) | 0.059 | 0.999 (0.998–1.000) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Csecsei, P.; Olah, C.; Varnai, R.; Simon, D.; Erdo-Bonyar, S.; Berki, T.; Czabajszki, M.; Zavori, L.; Schwarcz, A.; Molnar, T. Different Kinetics of Serum ADAMTS13, GDF-15, and Neutrophil Gelatinase-Associated Lipocalin in the Early Phase of Aneurysmal Subarachnoid Hemorrhage. Int. J. Mol. Sci. 2023, 24, 11005. https://doi.org/10.3390/ijms241311005
Csecsei P, Olah C, Varnai R, Simon D, Erdo-Bonyar S, Berki T, Czabajszki M, Zavori L, Schwarcz A, Molnar T. Different Kinetics of Serum ADAMTS13, GDF-15, and Neutrophil Gelatinase-Associated Lipocalin in the Early Phase of Aneurysmal Subarachnoid Hemorrhage. International Journal of Molecular Sciences. 2023; 24(13):11005. https://doi.org/10.3390/ijms241311005
Chicago/Turabian StyleCsecsei, Peter, Csaba Olah, Reka Varnai, Diana Simon, Szabina Erdo-Bonyar, Timea Berki, Mate Czabajszki, Laszlo Zavori, Attila Schwarcz, and Tihamer Molnar. 2023. "Different Kinetics of Serum ADAMTS13, GDF-15, and Neutrophil Gelatinase-Associated Lipocalin in the Early Phase of Aneurysmal Subarachnoid Hemorrhage" International Journal of Molecular Sciences 24, no. 13: 11005. https://doi.org/10.3390/ijms241311005
APA StyleCsecsei, P., Olah, C., Varnai, R., Simon, D., Erdo-Bonyar, S., Berki, T., Czabajszki, M., Zavori, L., Schwarcz, A., & Molnar, T. (2023). Different Kinetics of Serum ADAMTS13, GDF-15, and Neutrophil Gelatinase-Associated Lipocalin in the Early Phase of Aneurysmal Subarachnoid Hemorrhage. International Journal of Molecular Sciences, 24(13), 11005. https://doi.org/10.3390/ijms241311005








