Relative Humidity and Its Impact on the Immune System and Infections
Abstract
1. Introduction
2. Mechanisms
3. RH Alteration and Its Direct Effects on Health
4. Interaction among Climate Change, Pollutants and RH
5. Allergic Diseases and RH Influencing Effects
6. Infections and RH Influencing Effects
7. Unhealthy Environment and Interventions
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sterling, E.M.; Arundel, A.; Sterling, T.D. Criteria for Human Exposure to Humidity in occupied buildings. ASHRAE Trans. 1985, 91, 611–622. [Google Scholar]
- Wise, S.K.; Laury, A.M.; Katz, E.H.; Beste, K.A.; Parkos, C.A.; Nusrat, A. Interleukin-4 and interleukin-13 comprise the sinonasal epithelial barrier and perturb intercellular junction protein expression. Int. Forum Allergy Rhinol. 2014, 4, 361–370. [Google Scholar] [CrossRef] [PubMed]
- Schleimer, R.P. Immunopathogenesis of chronic rhinosinusitis and nasal polyposis. Annu. Rev. Pathol. 2017, 12, 331–357. [Google Scholar] [CrossRef] [PubMed]
- Schleimer, R.P.; Berdnikovs, S. Etiology of epithelial barrier dysfunction in patients with type 2 inflammatory diseases. J. Allergy Clin. Immunol. 2017, 139, 1752–1761. [Google Scholar] [CrossRef] [PubMed]
- Lowen, A.C.; Mubareka, S.; Steel, J.; Palese, P. Influenza virus transmission is dependent on relative humidity and temperatures. PLoS Pathog. 2007, 3, 1470–1476. [Google Scholar] [CrossRef]
- Ludwig, S.; Jimenez-Bush, I.; Brigham, E.; Bose, S.; Diette, G.; McCormack, M.; Matsui, E.C.; Davis, M.F. Analysis of home dust for Staphylococcus aureus and staphylococcal enteroxin gene using quantitative PCR. Sci. Total Environ. 2017, 582, 750–755. [Google Scholar] [CrossRef] [PubMed]
- Wolkoff, P.; Azuma, K.; Carrer, P. Health, work performance, and risk of infection in office-like environments: The role of indoor temperature, air humidity, and ventilation. Int. J. Hyg. Environ. Health 2021, 233, 113709. [Google Scholar] [CrossRef]
- Gui, S.Y.; Qiao, J.C.; Wang, X.C.; Yang, F.; Hu, C.Y.; Tao, F.B.; Yi, X.-L.; Jiang, Z.X. Long-term effects of meteorological factors and extreme weather on daily outpatient visits for conjunctivitis from 2013 to 2020: A time-series study in Urumqi, China. Environ. Sci. Pollut. Res. Int. 2023, 30, 1–17. [Google Scholar] [CrossRef]
- Mekjavic, P.J.; Tipton, M.J.; Mekjavic, I.B. The eye in extreme environments. Exp. Physiol. 2021, 106, 52–64. [Google Scholar] [CrossRef]
- Tan, B.K.; Peters, A.T.; Schleimer, R.P.; Hulse, K.E. Pathogenic and protective roles of B cells and antibodies in chronic rhinosinusitis. J. Allergy Clin. Immunol. 2018, 141, 1553–1560. [Google Scholar] [CrossRef]
- Rowe, S.M.; Miller, S.; Sorscher, E.J. Cystis Fibrosis. N. Engl. J. Med. 2005, 352, 1992–2001. [Google Scholar] [CrossRef]
- Welp, A.L.; Bomberger, M. Bacterial Community Interactions during Chronic Respiratory Disease. Front. Cell. Infect. Microbiol. 2020, 10, 213. [Google Scholar] [CrossRef]
- Prapamontol, T.; Thongjan, N.; Suwannarin, N. Asthma and rhinitis in wet and dry season among students in upper Northen Thailand: The role of building dampness and household air pollution. Int. J. Environ. Health Res. 2022, 5, 1–13. [Google Scholar] [CrossRef]
- Vilen, L.; Atosuo, J.; Putus, T. Prevalence of hoarseness in primary health care and hospitals-association with different work tasks and environmental factors among nurses. J. Voice 2022. [Google Scholar] [CrossRef] [PubMed]
- Beaker, R.; Hoie, A.H.; Bakke, J.V.; Holos, S.B.; Ovrevik, J. Dampness and moisture problems in Norwegian homes. Int. J. Environ. Res. Public Health 2017, 14, 1241. [Google Scholar] [CrossRef]
- Park, J.-H.; Cho, S.J.; White, S.K.; Cox-Ganser, J.M. Changes in respiratory and non-respiratory symptoms in occupants of a large office building over a period of moisture damage remediation attempts. PLoS ONE 2018, 13, e0191165. [Google Scholar] [CrossRef] [PubMed]
- Fang, L.; Wyon, D.P.; Clausen, C.; Fanger, P.O. Impact of indoor air temperature and humidity in an office on perceived air quality, SBS symptoms and performance. Indoor Air 2004, 14, 74–81. [Google Scholar] [CrossRef] [PubMed]
- Goad, N.; Gawkrodger, D.J. Ambient humidity and the skin: The impact of air humidity in healthy and diseased states. JEADV 2016, 30, 1285–1294. [Google Scholar] [CrossRef]
- Cheng, X.; Zhang, H.; Pan, W.; Liu, S.; Zhang, M.; Long, Z.; Zhang, T.; Chen, Q. Field study of infiltration rate and its influence on indoor air quality in an apartment. Procedia Eng. 2017, 205, 3954–3961. [Google Scholar] [CrossRef]
- Wang, Z.; Tian, X.; Li, J.; Wang, F.; Liang, W.; Zhao, H.; Huang, B.; Wang, Z.; Feng, Y.; Shi, G. Quantitative evidence from VOCs source apportionment reveals O3 control strategies in northern and southern China. Environ. Int. 2023, 172, 107786. [Google Scholar] [CrossRef]
- Wang, F.; Wang, W.; Wang, Z.; Zhang, Z.; Feng, Y.; Russell, A.; Shi, G. Drivers of PM2.5-O3 co-pollution: From the perspective of reactive nitrogen conversion pathways in atmospheric nitrogen cycling. Sci. Bull. 2022, 67, 1833–1836. [Google Scholar] [CrossRef] [PubMed]
- Fadeyi, M.O. Ozone in indoor environments: Research progress in the past 15 years. Sustain. Cities Soc. 2015, 18, 78–94. [Google Scholar] [CrossRef]
- Lee, W.C.; Shen, L.; Catalano, P.J.; Mickley, L.J.; Koutrakis, P. Effects of future temperature change on PM2.5 infiltration in the Greater Boston area. Atmos. Environ. 2017, 150, 98–105. [Google Scholar] [CrossRef]
- Nazaroff, W.W. Exploring the consequences of climate change for indoor air quality. Environ. Res. Lett. 2013, 8, 015022. [Google Scholar] [CrossRef]
- D’Amato, G.; Cecchi, L. Effects of climate change on environmental factors in respiratory allergic diseases. Clin. Exp. Allergy 2008, 38, 1264–1274. [Google Scholar] [CrossRef]
- Bodaghkhani, E.; Mahdavian, M.; MacLellan, M.; Farrell, A.; Asghari, S. Effects of Meteorological Factors on Hospitalizations in Adult Patients with Asthma: A Systematic Review. Can. Respir. J. 2019, 11, 3435103. [Google Scholar] [CrossRef]
- Feng, Y.; Wang, Y.; Wu, L.; Shu, Q.; Li, H.; Yang, X. Causal relationship between outdoor atmospheric quality and pediatric visits in Hangzhou. Heliyon 2023, 9, e14271. [Google Scholar] [CrossRef]
- Available online: https://www.ginasthma.com (accessed on 3 May 2023).
- Deng, R.; Ma, P.; Li, B.; Wu, Y.; Yang, X. Development of allergic asthma and changes of intestinal microbiota in mice under high humidity and/or carbon black nanoparticles. Ecotoxicol. Environ. Saf. 2022, 241, 113786. [Google Scholar] [CrossRef]
- Pelegrino, F.S.A.; Pflugfelder, S.C.; De Paiva, C.S. Low humidity environmental challenge causes barrier disruption and cornification of the mouse corneal epithelium via c-jun N-terminal kinase 2 (JNK2) pathway. Exp. Eye Res. 2012, 94, 150–156. [Google Scholar] [CrossRef]
- Bolger, C.; Tufvesson, E.; Sue-Chu, M.; Devereux, G.; Ayres, J.G.; Bjermer, L.; Kippen, P. Hyperpnea-induced bronchoconstriction and urinary CC16 levels in athletes. Med. Sci. Sports Exerc. 2011, 43, 1207–1213. [Google Scholar] [CrossRef]
- Shaaban, R.; Zureik, M.; Soussan, D.; Neukirch, C.; Heinrich, J.; Sunyer, J.; Wjst, M.; Cerveri, I.; Pin, I.; Bousquet, J.; et al. Rhinitis and onset of asthma: A longitudinal population-based study. Lancet 2008, 372, 1049–1057. [Google Scholar] [CrossRef]
- Bousquet, J.; Gaugris, S.; Sazonov Kocevar, V.; Zhang, Q.; Yin, D.D.; Polos, P.G.; Bjermer, L. Increased risk of asthma attacks and emergency visits among asthma patients with allergic rhinitis: A subgroup analysis of the investigation of montelukast as a partner agent for complementary therapy. Clin. Exp. Allergy 2005, 35, 723–727, Erratum in Clin. Exp. Allergy 2006, 36, 249. [Google Scholar] [CrossRef]
- Tsuge, M.; Ikeda, M.; Matsumoto, N.; Yorifuji, T.; Tsukahara, H. Current Insights into Atopic March. Children 2021, 8, 1067. [Google Scholar] [CrossRef]
- Gao, W.; Gong, J.; Mu, M.; Zhu, Y.; Wang, W.; Chen, W.; Han, G.; Hu, H.; Bao, P. The pathogenesis of eosinophilic asthma: A positive feedback mechanism that promotes Th2 Immune response via filaggrin deficiency. Front. Immunol. 2021, 12, 672312. [Google Scholar] [CrossRef]
- Caminati, M.; Vianello, A.; Ricci, G.; Festi, G.; Bellamoli, R.; Longhi, S.; Crivellaro, M.; Marcer, G.; Monai, M.; Andretta, M.; et al. Trends and determinants of emergency room admissions for asthma: A retrospective evaluation in Northeast Italy. World Allergy Organ. J. 2019, 12, 100046. [Google Scholar] [CrossRef]
- D’Amato, G.; Chong-Neto, H.J.; Monge Ortega, O.P. The effects of climate change on respiratory allergy and asthma induced by pollen and mold allergens. Allergy 2020, 75, 2219–2228. [Google Scholar] [CrossRef] [PubMed]
- Tiotiu, A.I.; Novakova, P.; Nedeva, D.; Chong, H.J. Impact of air pollution on asthma outcomes 2022. Int. J. Environ. Res. Public Health 2020, 17, 6212. [Google Scholar] [CrossRef] [PubMed]
- Vianello, A.; Caminati, M.; Crivellaro, M.; El Mazloum, R.; Snenghi, R.; Schiappoli, M.; Dama, A.; Rossi, A.; Festi, G.; Marchi, M.R.; et al. Fatal asthma; is it still an epidemic? World Allergy Organ. J. 2016, 9, 42. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Wang, J.; Song, G.; Xie, H.; Lin, X.; Chai, R.; Zhu, R.; He, Y.; Tang, J.; Wang, J.; et al. Environmental and sensitization variations among asthma and/or rhinitis patients between 2008 and 2018 in China. Clin. Transl. Allergy 2022, 12, e12116. [Google Scholar] [CrossRef]
- Novaes, P.; Saldiva, P.H.; Matsuda, M.; Macchione, M.; Rangel, M.P.; Kara-Jose, N.; Berra, A. The effects of chronic exposure to traffic derived air pollution on the ocular surface. Environ. Res. 2010, 110, 372–374. [Google Scholar] [CrossRef]
- Ceylan, E.; Doruk, S.; Genc, S.; Ozkutuk, A.A.; Karadag, F.; Ergor, G.; Itil, B.O.; Cimrin, A.H. The role of molds in the relation between indoor environment and atopy in asthma patients. J. Res. Med. Sci. 2013, 18, 1067–1073. [Google Scholar]
- Moses, L.; Morrissey, K.; Sharpe, R.A.; Taylor, T. Exposure to Indoor Mouldy Odour Increases the Risk of Asthma in Older Adults Living in Social Housing. Int. J. Environ. Res. Public Health 2019, 16, 2600. [Google Scholar] [CrossRef] [PubMed]
- Acevedo, N.; Zakzuk, J.; Caraballo, L. House dust mite allergy under changing environments. Allergy Asthma Immunol. Res. 2019, 11, 450–469. [Google Scholar] [CrossRef] [PubMed]
- Shen, C.-Y.; Yen, C.-Y.; Chein, D.-K.; Tsai, J.-J.; Yu, S.-J.; Liao, E.-C. Influence of storage conditions on the infestation of Tyrophagus putrescentiae and prevalence of mite hypersensitivity in Taiwan. Exp. Appl. Acarol. 2020, 80, 381–398. [Google Scholar] [CrossRef]
- Vandenborght, L.-E.; Enaud, R.; Urien, C.; Coron, N.; Girodet, P.-O.; Ferreira, S.; Berger, P.; Delhaes, L. Type 2-high asthma is associated with a specific indoor mycobiome and microbiome. J. Allergy Clin. Immunol. 2021, 147, 1296–1305.e6. [Google Scholar] [CrossRef] [PubMed]
- Alsmo, T.; Alsmo, C. A comparison of relative humidity between two swedish buildings with different ventilation solutions. J. Environ. Prot. 2016, 7, 855–873. [Google Scholar] [CrossRef]
- Noti, J.D.; Blachere, F.M.; McMillen, C.M.; Lindsley, W.G.; Kashon, M.L.; Slaughter, D.R.; Beezhold, D.H. High Humidity leads to loss of infectious influenza virus from simulated coughs. PLoS ONE 2013, 8, e57485. [Google Scholar] [CrossRef]
- Li, Z.; Liu, Q.; Zhan, M.; Tao, B.; Wang, J.; Lu, W. Meteorological factors contribute to the risk of pulmonary tuberculosis: A multicenter study in eastern China. Sci. Total Environ. 2021, 793, 148621. [Google Scholar] [CrossRef]
- Ward, M.P.; Liu, Y.; Xiao, S.; Zhang, Z. Challenges in the control of COVID-19 outbreaks caused by the delta variant during period of low humidity: An observational study in Sydney, Australia. Infect. Dis Poverty 2021, 10, 139. [Google Scholar] [CrossRef]
- Aune, K.T.; Davis, M.F.; Smith, G.S. Extreme Precipitation Events and Infectious Disease Risk: A Scoping Review and Framework for Infectious Respiratory Viruses. Int. J. Environ. Res. Public Health 2022, 19, 165. [Google Scholar] [CrossRef]
- Lofgren, E.; Fefferman, N.H.; Naumova, E.N.; Gorski, J.; Naumov, Y.N. Influenza Seasonality: Underlying Causes and Modeling Theories. J. Virol. 2006, 81, 5429–5436. [Google Scholar] [CrossRef]
- Qian, H.; Zheng, X.; Zhang, M.; Weschler, L.; Sundell, J. Associations between parent’s perceived air quality in homes and health among children in Nanjing, China. PLoS ONE 2016, 11, e0155742. [Google Scholar] [CrossRef] [PubMed]
- Ngu, F.F.; Kelman, I.; Chambers, J.; Ayeb-Karlsson, S. Correlating heatwaves and relative humidity with suicide (fatal intentional self-harm). Sci. Rep. 2021, 11, 22175. [Google Scholar] [CrossRef] [PubMed]
- Ammari, W.G.; Mohammad, M.K.; Tayyem, R.F. The impact of patients’ real-life environmental temperature and humidity use conditions of tiotropium dry powder inhaler on its aerosol emission characteristics. Eur. J. Pharm. Sci. 2019, 133, 137–144. [Google Scholar] [CrossRef] [PubMed]
- Byber, K.; Radtke, T.; Norbäck, D.; Hitzke, C.; Imo, D.; Schwenkglenks, M.; Puhan, M.A.; Dressel, H.; Mutsch, M. Humidification of indoor air for preventing or reducing dryness symptoms or upper respiratory infections in educational settings and at the workplace. Cochrane Database Syst. Rev. 2021, 12, CD012219. [Google Scholar] [CrossRef] [PubMed]
- Myatt, T.A.; Kaufman, M.H.; Allen, J.G.; Macintosh, D.L.; Fabian, M.P.; McDevitt, J.J. Modeling the airbone survival of influenza virus in a residential setting: The impacts of home humidification. Environ. Health 2010, 9, 55. [Google Scholar] [CrossRef]
- Manuyakorn, W.; Padungpak, S.; Luecha, O.; Kamchaisatian, E. Assessing the efficacy of a novel temperature and humidity machine to minimize house dust mite allergen exposure and clinical symptoms in allergic rhinitis children sensitized to dust mites: A pilot study 2014. Asian Pac. J. Allergy Immunol. 2015, 33, 129–135. [Google Scholar]
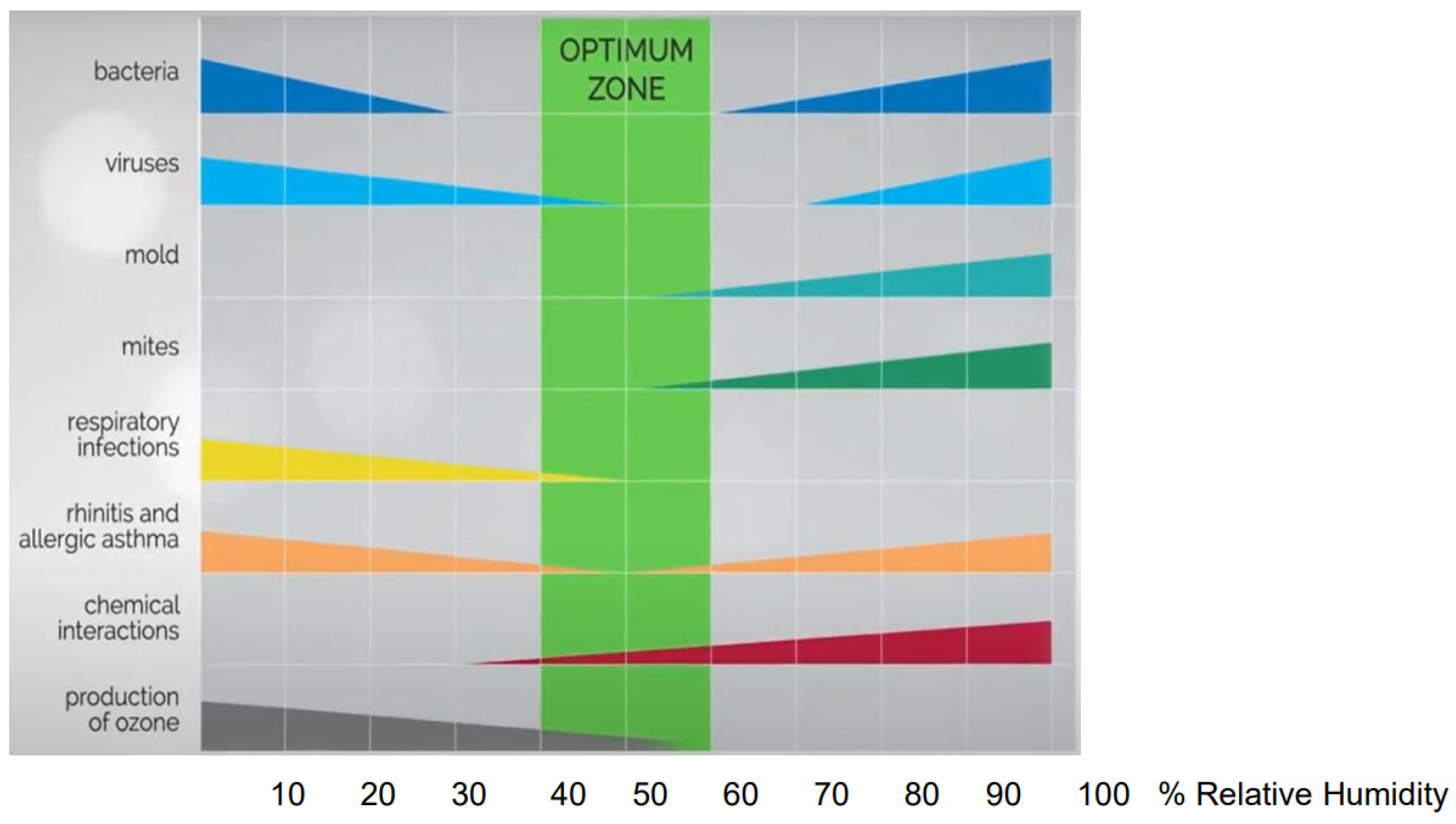
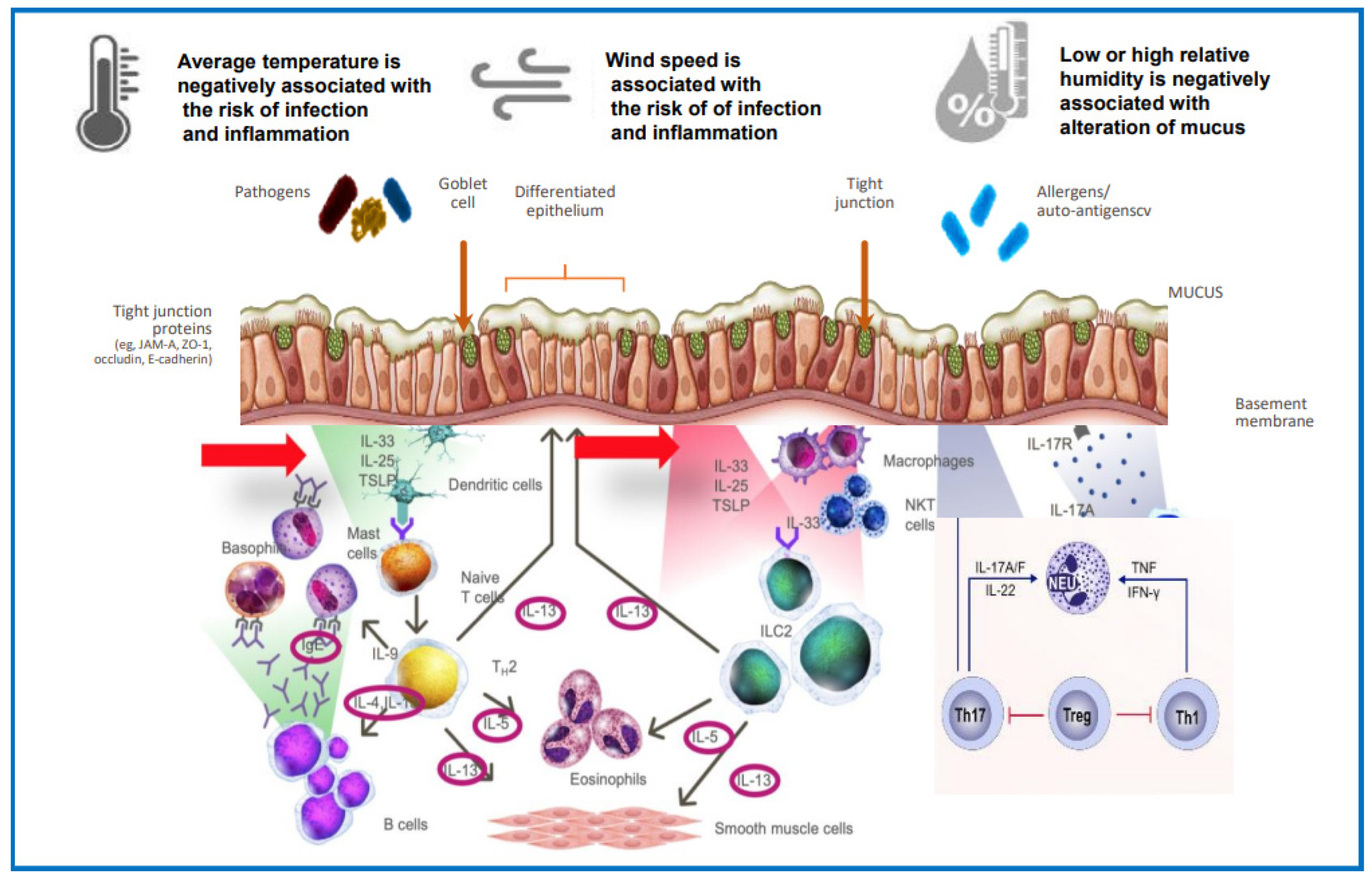
| Relative Humidity Effects | Mechanisms | Citations |
|---|---|---|
| Increased infections |
| [1,5] |
| Increased allergen burden | Excess humidity in the indoor environment is associated with the growth of allergens, such as moulds and mites. | [6] |
| Reduced mucociliary clearance |
| [2,3,4] |
| Mucosal impairment |
| [2,3,4,7,8,9] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Guarnieri, G.; Olivieri, B.; Senna, G.; Vianello, A. Relative Humidity and Its Impact on the Immune System and Infections. Int. J. Mol. Sci. 2023, 24, 9456. https://doi.org/10.3390/ijms24119456
Guarnieri G, Olivieri B, Senna G, Vianello A. Relative Humidity and Its Impact on the Immune System and Infections. International Journal of Molecular Sciences. 2023; 24(11):9456. https://doi.org/10.3390/ijms24119456
Chicago/Turabian StyleGuarnieri, Gabriella, Bianca Olivieri, Gianenrico Senna, and Andrea Vianello. 2023. "Relative Humidity and Its Impact on the Immune System and Infections" International Journal of Molecular Sciences 24, no. 11: 9456. https://doi.org/10.3390/ijms24119456
APA StyleGuarnieri, G., Olivieri, B., Senna, G., & Vianello, A. (2023). Relative Humidity and Its Impact on the Immune System and Infections. International Journal of Molecular Sciences, 24(11), 9456. https://doi.org/10.3390/ijms24119456







