The Role of hsa-miR-125b-5p Interaction with S1P/Ceramide Axis in the Potential Development of Inflammation-Associated Colon Cancer in Primary Sclerosing Cholangitis
Abstract
1. Introduction
2. Results
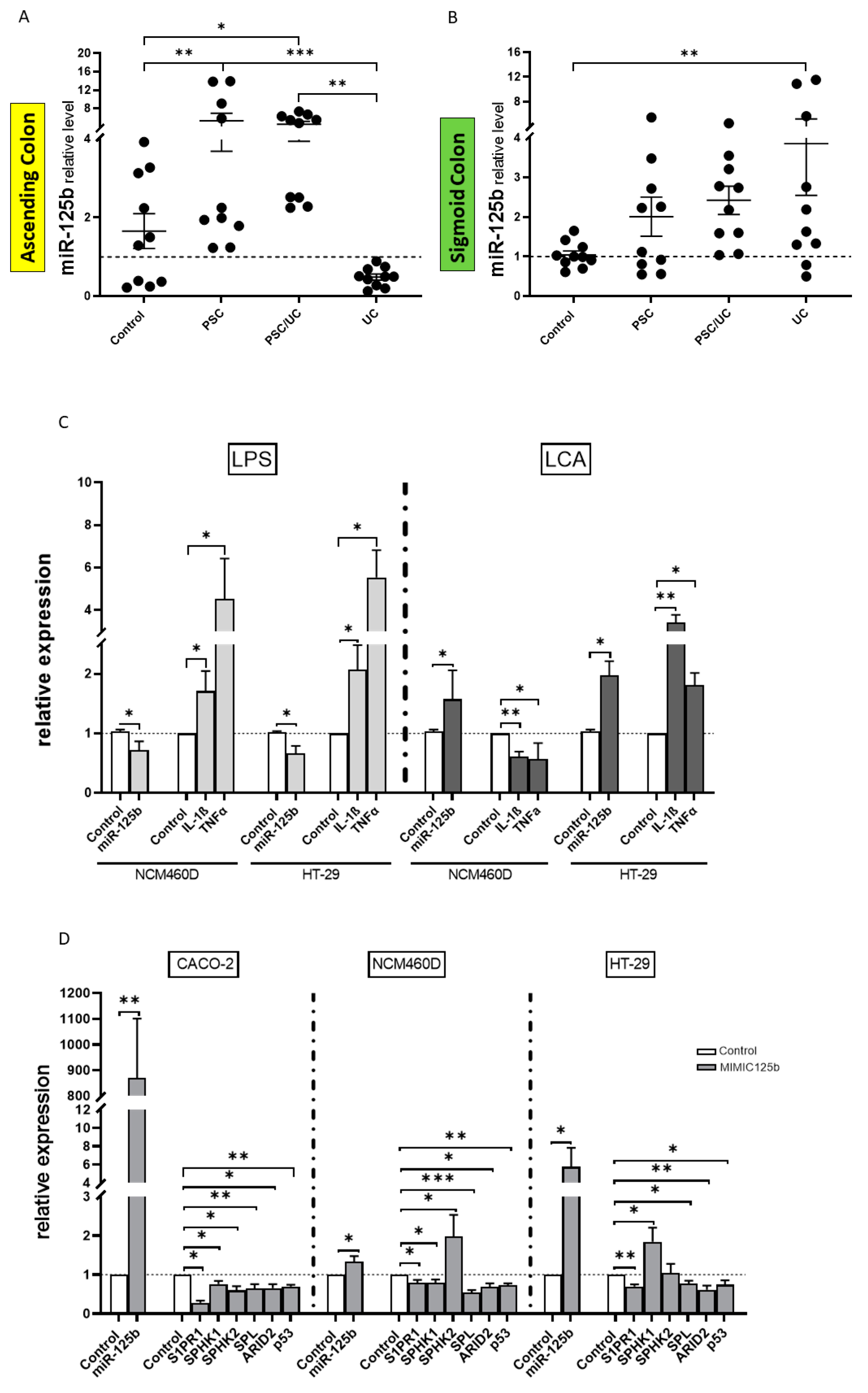
2.1. miR-125b-Related Signalling Pathways
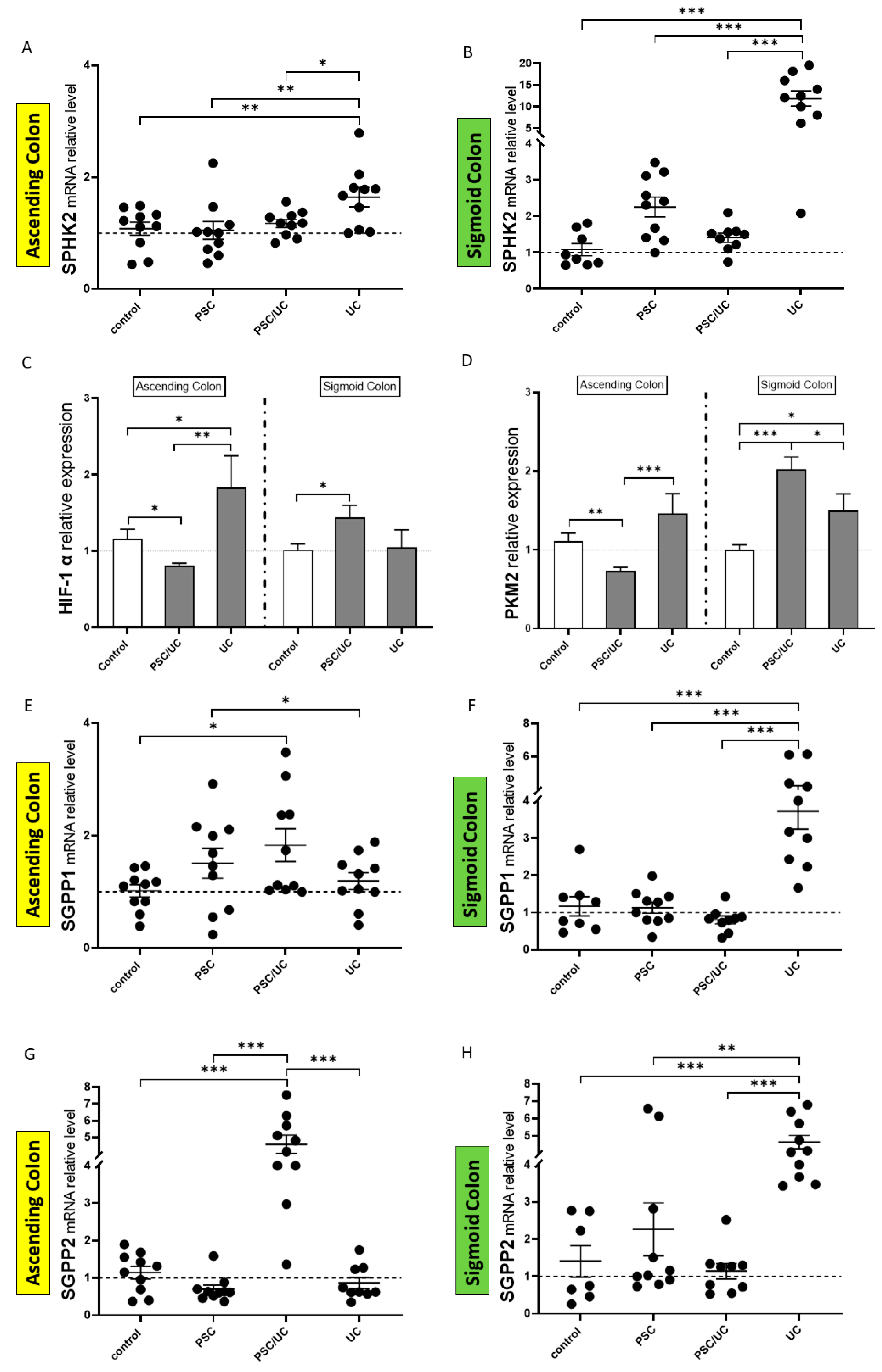
2.2. SPHKs/S1P Signalling Axis in Inflammation
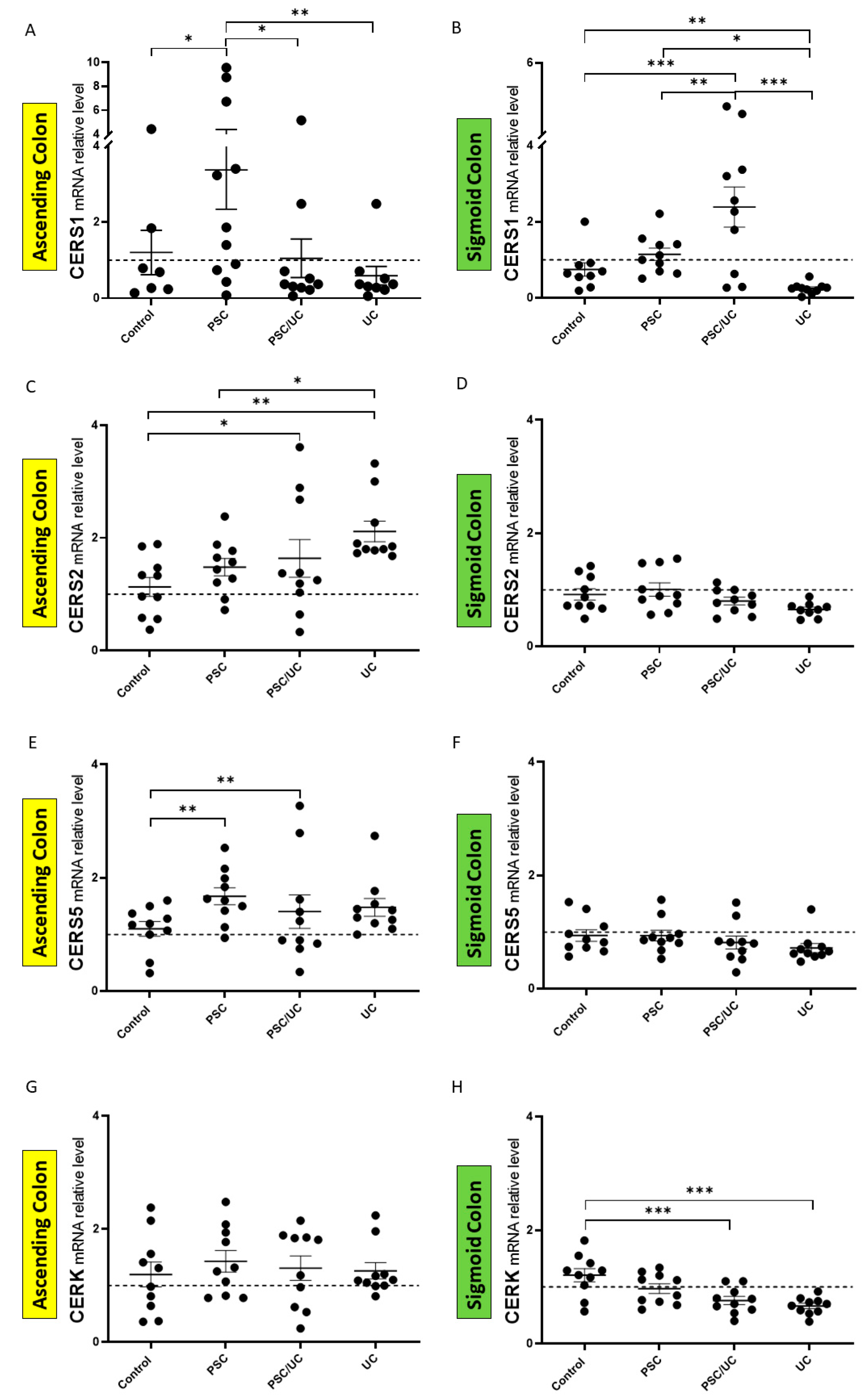
2.3. The Expression of Enzymes Involved in the Ceramide Pathway
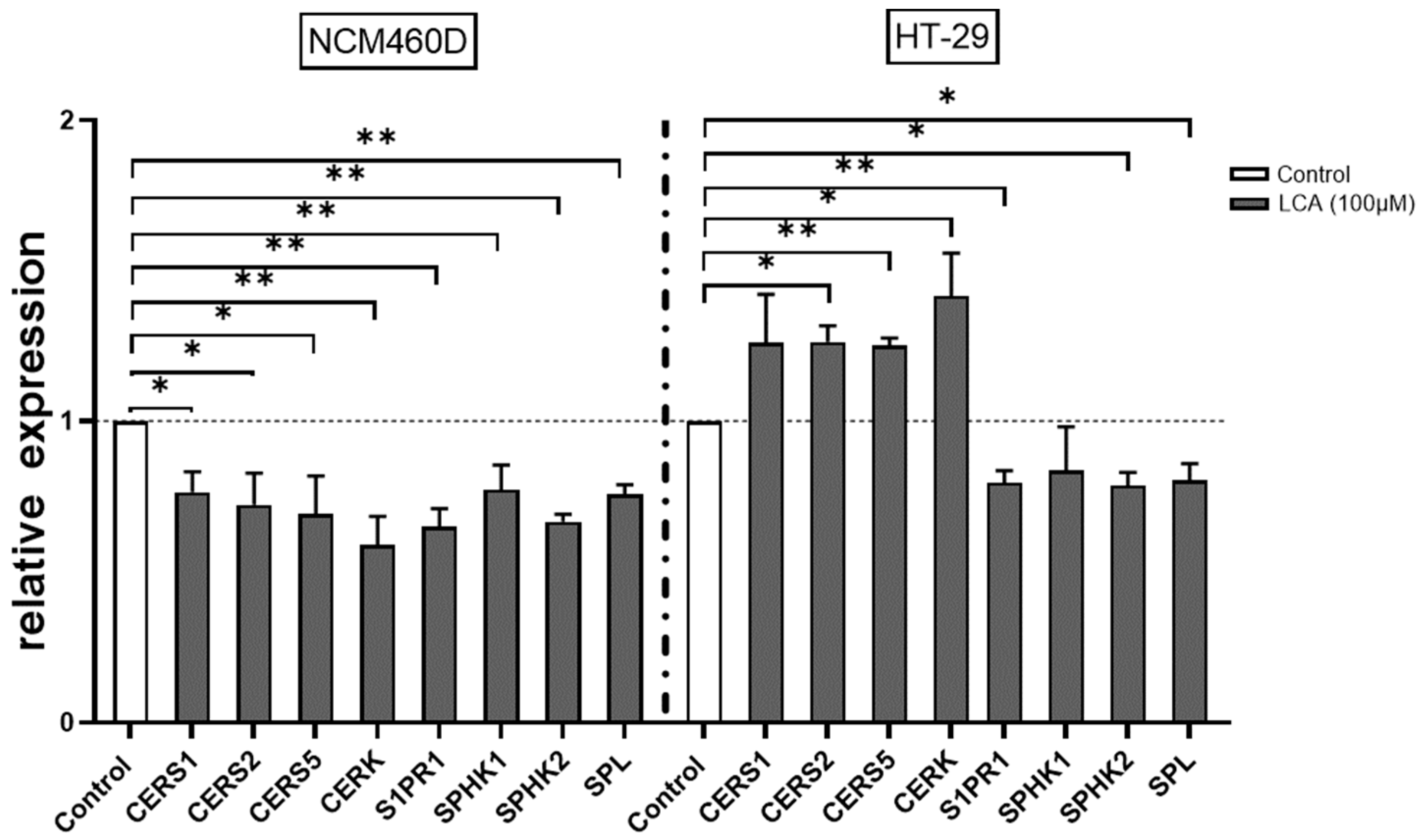
2.4. LCA-Induced Regulation of the Ceramide Pathway
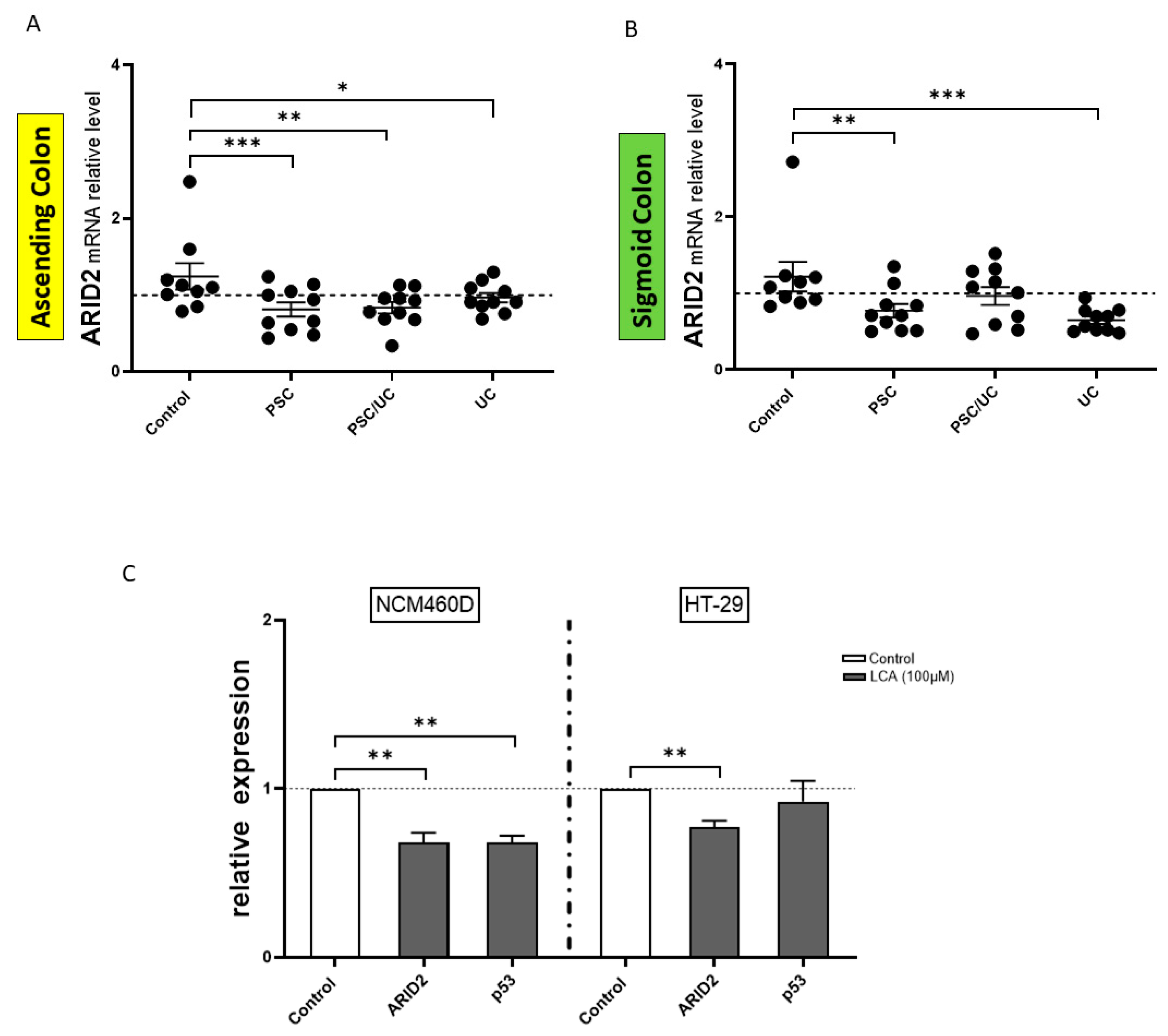
2.5. ARID2 in Microsatellite-Unstable (MSI) Colorectal Cancer
3. Discussion
4. Materials and Methods
4.1. Subjects
4.2. Cell Culture Transfection and Treatments
4.3. RNA and miRNA Expression Analysis
4.4. Statistics
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hirschfield, G.M.; Heathcote, E.J.; Gershwin, M.E. Pathogenesis of Cholestatic Liver Disease and Therapeutic Approaches. Gastroenterology 2010, 139, 1481–1496. [Google Scholar] [CrossRef] [PubMed]
- Weismuller, T.J.; Trivedi, P.J.; Bergquist, A.; Imam, M.; Lenzen, H.; Ponsioen, C.Y.; Holm, K.; Gotthardt, D.; Farkkila, M.A.; Marschall, H.U.; et al. Patient Age, Sex, and Inflammatory Bowel Disease Phenotype Associate with Course of Primary Sclerosing Cholangitis. Gastroenterology 2017, 152, 1975–1984.e8. [Google Scholar] [CrossRef]
- Eaden, J.A.; Abrams, K.R.; Mayberry, J.F. The Risk of Colorectal Cancer in Ulcerative Colitis: A Meta-Analysis. Gut 2001, 48, 526–535. [Google Scholar] [CrossRef]
- Hanse, R.J.; Pritchard, C.C.; Shendure, J.; Salipante, S.J. Classification and Characterization of Microsatellite Instability across 18 Cancer Types. Nat. Med. 2016, 22, 1342–1350. [Google Scholar]
- Patsialou, A.; Wilsker, D.; Moran, E. DNA-Binding Properties of Arid Family Proteins. Nucleic Acids Res. 2005, 33, 66–80. [Google Scholar] [CrossRef] [PubMed]
- Mohammadi, A.; Mansoori, B.; Baradaran, B. The Role of Micrornas in Colorectal Cancer. Biomed. Pharmacother. 2016, 84, 705–713. [Google Scholar] [CrossRef]
- Svoronos, A.A.; Engelman, D.M.; Slack, F.J. Oncomir or Tumor Suppressor? The Duplicity of Micrornas in Cancer. Cancer Res. 2016, 76, 3666–3670. [Google Scholar] [CrossRef]
- Liu, G.; Abraham, E. Micrornas in Immune Response and Macrophage Polarization. Arterioscler. Thromb. Vasc. Biol. 2013, 33, 170–177. [Google Scholar] [CrossRef]
- Valmiki, S. PWE-066 Microrna Signatures Can Differentiate between Inflamed and Non Inflamed Colonic Mucosa of Ulcerative Colitis Patients. Gut 2018, 67, A100–A100. [Google Scholar]
- Banzhaf-Strathmann, J.; Edbauer, D. Good Guy or Bad Guy: The Opposing Roles of Microrna 125b in Cancer. Cell Commun. Signal. 2014, 12, 30. [Google Scholar] [CrossRef]
- Sun, Y.M.; Lin, K.Y.; Chen, Y.Q. Diverse Functions of miR-125 Family in Different Cell Contexts. J. Hematol. Oncol. 2013, 6, 6–8. [Google Scholar] [CrossRef] [PubMed]
- Shaham, L.; Binder, V.; Gefen, N.; Borkhardt, A.; Izraeli, S. miR-125 in Normal and Malignant Hematopoiesis. Leukemia 2012, 26, 2011–2018. [Google Scholar] [CrossRef] [PubMed]
- del Solar, V.; Lizardo, D.Y.; Li, N.S.; Hurst, J.J.; Brais, C.J.; Atilla-Gokcumen, G.E. Differential Regulation of Specific Sphingolipids in Colon Cancer Cells During Staurosporine-Induced Apoptosis. Chem. Biol. 2015, 22, 1662–1670. [Google Scholar] [CrossRef] [PubMed]
- Olivera, A.; Spiegel, S. Sphingosine-1-Phosphate as 2nd Messenger in Cell-Proliferation Induced by Pdgf and Fcs Mitogens. Nature 1993, 365, 557–560. [Google Scholar] [CrossRef] [PubMed]
- Reynolds, C.P.; Maurer, B.J.; Kolesnick, R.N. Ceramide Synthesis and Metabolism as a Target for Cancer Therapy. Cancer Lett. 2004, 206, 169–180. [Google Scholar] [CrossRef]
- Machala, M.; Prochazkova, J.; Hofmanova, J.; Kralikova, L.; Slavik, J.; Tylichova, Z.; Ovesna, P.; Kozubik, A.; Vondracek, J. Colon Cancer and Perturbations of the Sphingolipid Metabolism. Int. J. Mol. Sci. 2019, 20, 6051. [Google Scholar] [CrossRef]
- Blom, T.; Bergelin, N.; Meinander, A.; Lof, C.; Slotte, J.P.; Eriksson, J.E.; Tornquist, K. An Autocrine Sphingosine-1-Phosphate Signaling Loop Enhances Nf-Kappab-Activation and Survival. BMC Cell Biol. 2010, 11, 45. [Google Scholar] [CrossRef]
- Karuppuchamy, T.; Behrens, E.H.; Gonzalez-Cabrera, P.; Sarkisyan, G.; Gima, L.; Boyer, J.D.; Bamias, G.; Jedlicka, P.; Veny, M.; Clark, D.; et al. Sphingosine-1-Phosphate Receptor-1 (S1p(1)) Is Expressed by Lymphocytes, Dendritic Cells, and Endothelium and Modulated During Inflammatory Bowel Disease. Mucosal Immunol. 2017, 10, 162–171. [Google Scholar] [CrossRef]
- Rivera, J.; Proia, R.L.; Olivera, A. The Alliance of Sphingosine-1-Phosphate and Its Receptors in Immunity. Nat. Rev. Immunol. 2008, 8, 753–763. [Google Scholar] [CrossRef]
- Pyne, N.J.; Pyne, S. Sphingosine 1-Phosphate and Cancer. Nat. Rev. Cancer 2010, 10, 489–503. [Google Scholar] [CrossRef]
- Mullen, T.D.; Jenkins, R.W.; Clarke, C.J.; Bielawski, J.; Hannun, Y.A.; Obeid, L.M. Ceramide Synthase-Dependent Ceramide Generation and Programmed Cell Death Involvement of Salvage Pathway in Regulating Postmitochondrial Events. J. Biol. Chem. 2011, 286, 15929–15942. [Google Scholar] [CrossRef] [PubMed]
- Payne, A.W.; Pant, D.K.; Pan, T.C.; Chodosh, L.A. Ceramide Kinase Promotes Tumor Cell Survival and Mammary Tumor Recurrence. Cancer Res. 2014, 74, 6352–6363. [Google Scholar] [CrossRef] [PubMed]
- Gomez-Munoz, A. Ceramide 1-Phosphate/Ceramide, a Switch between Life and Death. Biochim. Biophys. Acta-Biomembr. 2006, 1758, 2049–2056. [Google Scholar] [CrossRef] [PubMed]
- Granado, M.H.; Gangoiti, P.; Ouro, A.; Arana, L.; González, M.; Trueba, M.; Gómez-Muñoz, A. Ceramide 1-Phosphate (C1p) Promotes Cell Migration Involvement of a Specific C1p Receptor. Cell Signal. 2009, 21, 405–412. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Liu, Y.; Huang, W.-C.; Zheng, L.-C. miR-125b-1-3p Exerts Antitumor Functions in Lung Carcinoma Cells by Targeting S1pr1. Chin. Med. J. 2018, 131, 1909–1916. [Google Scholar] [CrossRef]
- Zhao, X.; He, W.; Li, J.L.; Huang, S.; Wan, X.; Luo, H.; Wu, D. Mirna-125b Inhibits Proliferation and Migration by Targeting Sphk1 in Bladder Cancer. Am. J. Transl. Res. 2015, 7, 2346–2354. [Google Scholar]
- Yang, W.W.; Wang, A.N.; Zhao, C.L.; Li, Q.H.; Pan, Z.F.; Han, X.F.; Zhang, C.J.; Wang, G.H.; Ji, C.; Wang, G.L.; et al. miR-125b Enhances Il-8 Production in Early-Onset Severe Preeclampsia by Targeting Sphingosine-1-Phosphate Lyase 1. PLoS ONE 2016, 11, e0166940. [Google Scholar] [CrossRef]
- Barra, G.; Lepore, A.; Gagliardi, M.; Somma, D.; Matarazzo, M.R.; Costabile, F.; Pasquale, G.; Mazzoni, A.; Gallo, C.; Nuzzo, G.; et al. Sphingosine Kinases Promote Il-17 Expression in Human T Lymphocytes. Sci. Rep. 2018, 8, 13233. [Google Scholar] [CrossRef]
- Adamowicz, M.; Stukan, I.; Milkiewicz, P.; Bialek, A.; Milkiewicz, M.; Kempinska-Podhorodecka, A. Modulation of Mismatch Repair and the Socs1/P53 Axis by Microrna-155 in the Colon of Patients with Primary Sclerosing Cholangitis. Int. J. Mol. Sci. 2022, 23, 4905. [Google Scholar] [CrossRef]
- Fajgenbaum, D.C.; June, C.H. Cytokine Storm. N. Engl. J. Med. 2020, 383, 2255–2273. [Google Scholar] [CrossRef]
- Owen, R.W.; Thompson, M.H.; Hill, M.J.; Wilpart, M.; Mainguet, P.; Roberfroid, M. The Importance of the Ratio of Lithocholic to Deoxycholic Acid in Large Bowel Carcinogenesis. Nutr. Cancer 1987, 9, 67–71. [Google Scholar] [CrossRef] [PubMed]
- Katona, B.W.; Anant, S.; Covey, D.F.; Stenson, W.F. Characterization of Enantiomeric Bile Acid-Induced Apoptosis in Colon Cancer Cell Lines. J. Biol. Chem. 2009, 284, 3354–3364. [Google Scholar] [CrossRef]
- Coskun, M.; Bjerrum, J.T.; Seidelin, J.B.; Troelsen, J.T.; Olsen, J.; Nielsen, O.H. miR-20b, miR-98, miR-125b-1*, and Let-7e* as New Potential Diagnostic Biomarkers in Ulcerative Colitis. World J. Gastroenterol. 2013, 19, 4289–4299. [Google Scholar] [CrossRef] [PubMed]
- Huang, W.C.; Liang, J.; Nagahashi, M.; Avni, D.; Yamada, A.; Maceyka, M.; Wolen, A.R.; Kordula, T.; Milstien, S.; Takabe, K.; et al. Sphingosine-1-Phosphate Phosphatase 2 Promotes Disruption of Mucosal Integrity, and Contributes to Ulcerative Colitis in Mice and Humans. FASEB J. 2016, 30, 2945–2958. [Google Scholar] [CrossRef] [PubMed]
- Warburg, O.; Wind, F.; Negelein, E. The Metabolism of Tumors in the Body. J. Gen. Physiol. 1927, 8, 519–530. [Google Scholar] [CrossRef]
- Li, J.; Wang, R.; Zhou, X.; Wang, W.; Gao, S.; Mao, Y.; Wu, X.; Guo, L.; Liu, H.; Wen, L.; et al. Genomic and Transcriptomic Profiling of Carcinogenesis in Patients with Familial Adenomatous Polyposis. Gut 2019, 69, 1283–1293. [Google Scholar] [CrossRef]
- Jeffery, J.; Lewis, S.J.; Ayling, R.M. Fecal Dimeric M2-Pyruvate Kinase (Tumor M2-Pk) in the Differential Diagnosis of Functional and Organic Bowel Disorders. Inflamm. Bowel Dis. 2009, 15, 1630–1634. [Google Scholar] [CrossRef]
- Almousa, A.A.; Morris, M.; Fowler, S.; Jones, J.; Alcorn, J. Elevation of Serum Pyruvate Kinase M2 (Pkm2) in Ibd and Its Relationship to Ibd Indices. Clin. Biochem. 2018, 53, 19–24. [Google Scholar] [CrossRef]
- Spiegel, S.; Milstien, S. Sphingosine-1-Phosphate: An Enigmatic Signalling Lipid. Nat. Rev. Mol. Cell Biol. 2003, 4, 397–407. [Google Scholar] [CrossRef]
- Kunkel, G.T.; Maceyka, M.; Milstien, S.; Spiegel, S. Targeting the Sphingosine-1-Phosphate Axis in Cancer, Inflammation and Beyond. Nat. Rev. Drug Discov. 2013, 12, 688–702. [Google Scholar] [CrossRef]
- Schneider, G.; Sellers, Z.P.; Bujko, K.; Kakar, S.S.; Kucia, M.; Ratajczak, M.Z. Novel Pleiotropic Effects of Bioactive Phospholipids in Human Lung Cancer Metastasis. Oncotarget 2017, 8, 58247–58263. [Google Scholar] [CrossRef] [PubMed]
- Hartmann, D.; Lucks, J.; Fuchs, S.; Schiffmann, S.; Schreiber, Y.; Ferreirós, N.; Merkens, J.; Marschalek, R.; Geisslinger, G.; Grösch, S. Long Chain Ceramides and Very Long Chain Ceramides Have Opposite Effects on Human Breast and Colon Cancer Cell Growth. Int. J. Biochem. Cell Biol. 2012, 44, 620–628. [Google Scholar] [CrossRef] [PubMed]
- Fitzgerald, S.; Sheehan, K.M.; Espina, V.; O’Grady, A.; Cummins, R.; Kenny, D.; Liotta, L.; O’Kennedy, R.; Kay, E.W.; Kijanka, G.S. High Cers5 Expression Levels Associate with Reduced Patient Survival and Transition from Apoptotic to Autophagy Signalling Pathways in Colorectal Cancer. J. Pathol. Clin. Res. 2014, 1, 54–65. [Google Scholar] [CrossRef] [PubMed]
- Kolesnick, R.N.; Krönke, M. Regulation of Ceramide Production and Apoptosis. Annu. Rev. Physiol. 1998, 60, 643–665. [Google Scholar] [CrossRef]
- Nishida, N.; Yokobori, T.; Mimori, K.; Sudo, T.; Tanaka, F.; Shibata, K.; Ishii, H.; Doki, Y.; Kuwano, H.; Mori, M. Microrna miR-125b Is a Prognostic Marker in Human Colorectal Cancer. Int. J. Oncol. 2011, 38, 1437–1443. [Google Scholar] [PubMed]
- Kempinska-Podhorodecka, A.; Adamowicz, M.; Ostrycharz, E.; Chmielarz, M.; Wójcicki, M.; Milkiewicz, P.; Milkiewicz, M. Role of miR-506 in Ulcerative Colitis Associated with Primary Sclerosing Cholangitis. Sci. Rep. 2021, 11, 10134. [Google Scholar] [CrossRef]
- Alhopuro, P.; Sammalkorpi, H.; Niittymäki, I.; Biström, M.; Raitila, A.; Saharinen, J.; Nousiainen, K.; Lehtonen, H.J.; Heliövaara, E.; Puhakka, J.; et al. Candidate Driver Genes in Microsatellite-Unstable Colorectal Cancer. Int. J. Cancer 2011, 130, 1558–1566. [Google Scholar] [CrossRef]
- Xie, C.Y.; Fu, L.; Han, Y.; Li, Q.C.; Wang, E.H. Decreased Arid1a Expression Facilitates Cell Proliferation and Inhibits 5-Fluorouracil-Induced Apoptosis in Colorectal Carcinoma. Tumor Biol. 2014, 35, 7921–7927. [Google Scholar] [CrossRef]
- Chou, A.; Toon, C.W.; Clarkson, A.; Sioson, L.; Houang, M.; Watson, N.; DeSilva, K.; Gill, A.J. Loss of Arid1a Expression in Colorectal Carcinoma Is Strongly Associated with Mismatch Repair Deficiency. Hum. Pathol. 2014, 45, 1697–1703. [Google Scholar] [CrossRef]
- Agaimy, A.; Daum, O.; Markl, B.; Lichtmannegger, I.; Michal, M.; Hartmann, A. Swi/Snf Complex-Deficient Undifferentiated/Rhabdoid Carcinomas of the Gastrointestinal Tract a Series of 13 Cases Highlighting Mutually Exclusive Loss of Smarca4 and Smarca2 and Frequent Co-Inactivation of Smarcb1 and Smarca2. Am. J. Surg. Pathol. 2016, 40, 544–553. [Google Scholar] [CrossRef]
- Zhang, Y.-L.; Li, Z.-J.; Gou, H.-Z.; Song, X.-J.; Zhang, L. The Gut Microbiota-Bile Acid Axis: A Potential Therapeutic Target for Liver Fibrosis. Front. Cell. Infect. Microbiol. 2022, 12, 945368. [Google Scholar] [CrossRef] [PubMed]
- Barrasa, J.I.; Olmo, N.; Lizarbe, M.A.; Turnay, J. Bile Acids in the Colon, from Healthy to Cytotoxic Molecules. Toxicol. Vitr. 2013, 27, 964–977. [Google Scholar] [CrossRef] [PubMed]
- Bernstein, H.; Bernstein, C.; Payne, C.M.; Dvorakova, K.; Garewal, H. Bile Acids as Carcinogens in Human Gastrointestinal Cancers. Mutat. Res. Mutat. Res. 2005, 589, 47–65. [Google Scholar] [CrossRef] [PubMed]

| Control (n = 10) | PSC (n = 10) | PSC/UC (n = 10) | UC (n = 10) | |
|---|---|---|---|---|
| Gender (Male/Female) | 6/4 | 8/2 | 8/2 | 2/8 |
| Age (years) | 58 ± 4 | 44 ± 7 | 54 ± 15 | 43 ± 17 |
| Hb (mg/dL, normal F: 12–16, M: 14–18) | ND | 14 ± 1.5 | 13 ± 2.2 | ND |
| Bilirubin (mg/dL, normal < 1.1) | ND | 1.08 ± 0.83 | 1.4 ± 1.07 | 0.4 ± 0.16 |
| ALP (IU/L, normal 30–120) | ND | 149 ± 68 | 433 ± 209 | 82 ± 23 |
| GGTP (IU/L, normal F < 66, M < 100) | ND | 238 ± 116 | 444 ± 275 | 18 ± 13 |
| ALT (IU/L, normal < 40) | ND | 193 ± 45 | 158 ± 42 | 15 ± 8.4 |
| Cirrhosis (yes/no) | N/A | 0/10 | 2/10 | N/A |
| Duration of the disease (months) | N/A | 32 ± 12 | 44 ± 11 | ND |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abramczyk, J.; Milkiewicz, M.; Hula, B.; Milkiewicz, P.; Kempinska-Podhorodecka, A. The Role of hsa-miR-125b-5p Interaction with S1P/Ceramide Axis in the Potential Development of Inflammation-Associated Colon Cancer in Primary Sclerosing Cholangitis. Int. J. Mol. Sci. 2023, 24, 9175. https://doi.org/10.3390/ijms24119175
Abramczyk J, Milkiewicz M, Hula B, Milkiewicz P, Kempinska-Podhorodecka A. The Role of hsa-miR-125b-5p Interaction with S1P/Ceramide Axis in the Potential Development of Inflammation-Associated Colon Cancer in Primary Sclerosing Cholangitis. International Journal of Molecular Sciences. 2023; 24(11):9175. https://doi.org/10.3390/ijms24119175
Chicago/Turabian StyleAbramczyk, Joanna, Malgorzata Milkiewicz, Bartosz Hula, Piotr Milkiewicz, and Agnieszka Kempinska-Podhorodecka. 2023. "The Role of hsa-miR-125b-5p Interaction with S1P/Ceramide Axis in the Potential Development of Inflammation-Associated Colon Cancer in Primary Sclerosing Cholangitis" International Journal of Molecular Sciences 24, no. 11: 9175. https://doi.org/10.3390/ijms24119175
APA StyleAbramczyk, J., Milkiewicz, M., Hula, B., Milkiewicz, P., & Kempinska-Podhorodecka, A. (2023). The Role of hsa-miR-125b-5p Interaction with S1P/Ceramide Axis in the Potential Development of Inflammation-Associated Colon Cancer in Primary Sclerosing Cholangitis. International Journal of Molecular Sciences, 24(11), 9175. https://doi.org/10.3390/ijms24119175






