Comparison between Capillary and Serum Lactate Levels in Predicting Short-Term Mortality of Septic Patients at the Emergency Department
Abstract
1. Introduction
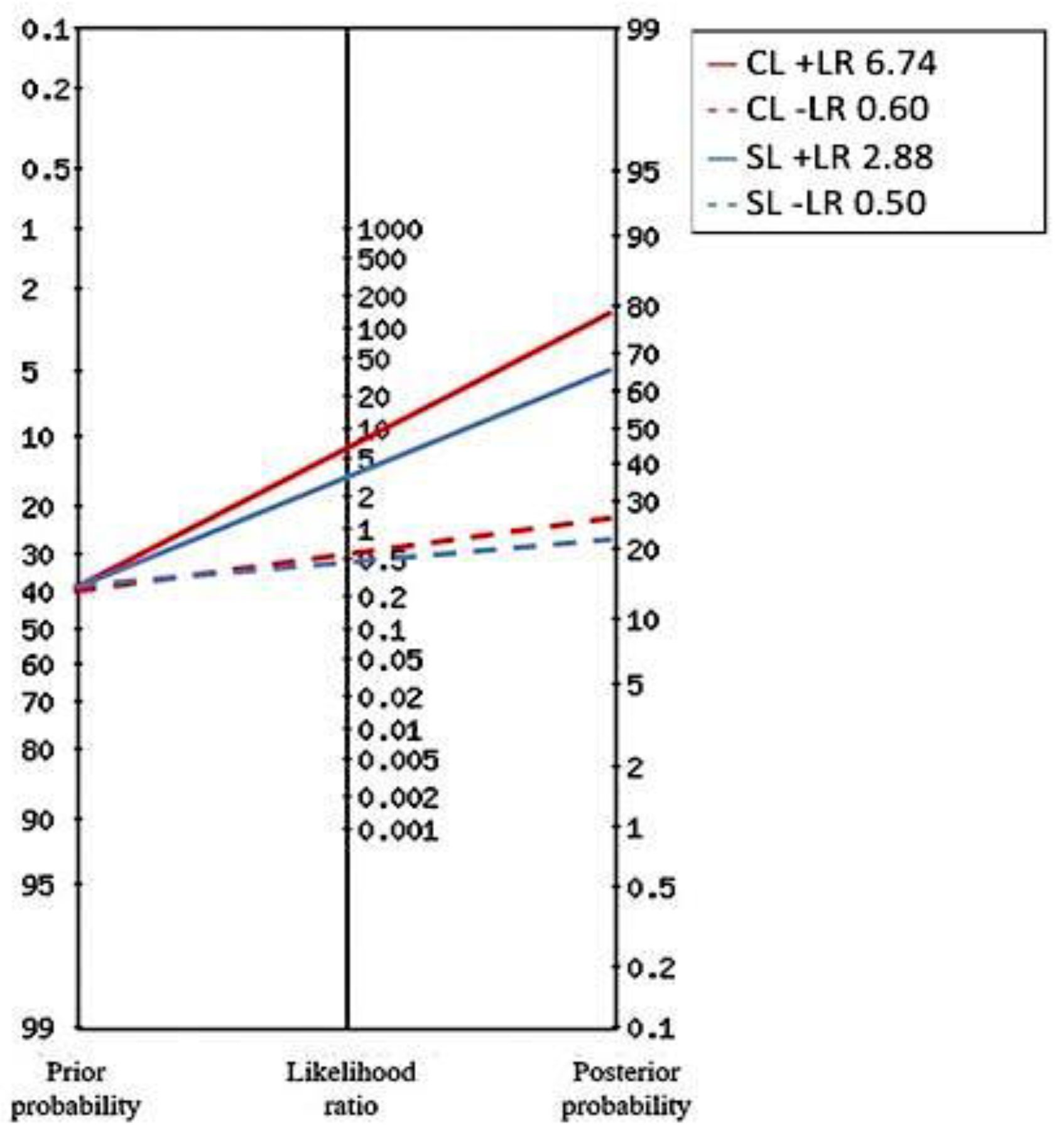
2. Results
3. Discussion
4. Materials and Methods
Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviation
References
- Singer, M.; Deutschman, C.S.; Seymour, C.W.; Shankar-Hari, M.; Annane, D.; Bauer, M.; Bellomo, R.; Bernard, G.R.; Chiche, J.-D.; Coopersmith, C.M.; et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA 2016, 315, 801–810. [Google Scholar] [CrossRef] [PubMed]
- Evans, L.; Rhodes, A.; Alhazzani, W.; Antonelli, M.; Coopersmith, C.M.; French, C.; Machado, F.R.; Mcintyre, L.; Ostermann, M.; Prescott, H.C.; et al. Surviving sepsis campaign: International guidelines for management of sepsis and septic shock 2021. Intensive Care Med. 2021, 47, 1181–1247. [Google Scholar] [CrossRef] [PubMed]
- Chiu, C.; Legrand, M. Epidemiology of sepsis and septic shock. Curr. Opin. Anaesthesiol. 2021, 34, 71–76. [Google Scholar] [CrossRef] [PubMed]
- Global Report on the Epidemiology and Burden of Sepsis: Current Evidence, Identifying Gaps and Future Directions; World Health Organization: Geneva, Switzerland, 2020.
- Font, M.D.; Thyagarajan, B.; Khanna, A.K. Sepsis and Septic Shock—Basics of diagnosis, pathophysiology and clinical decision making. Med. Clin. N. Am. 2020, 104, 573–585. [Google Scholar] [CrossRef]
- Piechota, M.; Banach, M.; Irzmanski, R.; Barylski, M.; Piechota-Urbanska, M.; Kowalski, J.; Pawlicki, L. Plasma endothelin-1 levels in septic patients. J. Intensive Care Med. 2007, 22, 232–239. [Google Scholar] [CrossRef]
- Angus, D.C.; van der Poll, T. Severe sepsis and septic shock. N. Engl. J. Med. 2013, 369, 840–851. [Google Scholar] [CrossRef]
- Bakker, J.; Postelnicu, R.; Mukherjee, V. Lactate: Where Are We Now? Crit. Care Clin. 2020, 36, 115–124. [Google Scholar] [CrossRef]
- Vincent, J.L.; De Backer, D. Circulatory shock. N. Engl. J. Med. 2013, 369, 1726–1734. [Google Scholar] [CrossRef]
- Levy, B. Lactate and shock state: The metabolic view. Curr. Opin. Crit. Care. 2006, 12, 315–321. [Google Scholar] [CrossRef]
- Liu, Z.; Meng, Z.; Li, Y.; Zhao, J.; Wu, S.; Gou, S.; Wu, H. Prognostic accuracy of the serum lactate level, the SOFA score and the qSOFA score for mortality among adults with Sepsis. Scand. J. Trauma Resusc. Emerg. Med. 2019, 27, 51. [Google Scholar] [CrossRef]
- Garcia-Alvarez, M.; Marik, P.; Bellomo, R. Sepsis-associated hyperlactatemia. Crit. Care 2014, 18, 503. [Google Scholar] [CrossRef] [PubMed]
- Innocenti, F.; Meo, F.; Giacomelli, I.; Tozzi, C.; Ralli, M.L.; Donnini, C.; Tassinari, I.; Caldi, F.; Zanobetti, M.; Pini, R. Prognostic value of serial lactate levels in septic patients with and without shock. Intern. Emerg. Med. 2019, 14, 1321–1330. [Google Scholar] [CrossRef] [PubMed]
- Van den Nouland, D.P.A.; Brouwers, M.C.G.J.; Stassen, P.M. Prognostic value of plasma lactate levels in a retrospective cohort presenting at a university hospital emergency department. BMJ Open 2017, 7, e011450. [Google Scholar] [CrossRef]
- Guarino, M.; Perna, B.; De Giorgi, A.; Gambuti, E.; Alfano, F.; Catanese, E.M.; Volpato, S.; Strada, A.; Caio, G.; Contini, C.; et al. A 2-year retrospective analysis of the prognostic value of MqSOFA compared to lactate, NEWS and qSOFA in patients with sepsis. Infection 2022, 50, 941–948. [Google Scholar] [CrossRef]
- Rhodes, A.; Evans, L.E.; Alhazzani, W.; Levy, M.M.; Antonelli, M.; Ferrer, R.; Kumar, A.; Sevransky, J.E.; Sprung, C.L.; Nunnally, M.E.; et al. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock: 2016. Intensive Care Med. 2017, 43, 304–377. [Google Scholar] [CrossRef] [PubMed]
- Pan, J.; Peng, M.; Liao, C.; Hu, X.; Wang, A.; Li, X. Relative efficacy and safety of early lactate clearance-guided therapy resuscitation in patients with sepsis: A meta-analysis. Medicine 2019, 98, e14453. [Google Scholar] [CrossRef] [PubMed]
- Theerawit, P.; Na Petvicharn, C.; Tangsujaritvijit, V.; Sutherasan, Y. The Correlation Between Arterial Lactate and Venous Lactate in Patients With Sepsis and Septic Shock. J. Intensive Care Med. 2018, 33, 116–120. [Google Scholar] [CrossRef]
- Mahmoodpoor, A.; Shadvar, K.; Sanaie, S.; Golzari, S.E.J.; Parthvi, R.; Hamishehkar, H.; Nader, N.D. Arterial vs venous lactate: Correlation and predictive value of mortality of patients with sepsis during early resuscitation phase. J. Crit. Care 2020, 58, 118–124. [Google Scholar] [CrossRef]
- Jedlicka, J.; Becker, B.F.; Chappell, D. Endothelial Glycocalyx. Crit. Care Clin. 2020, 36, 217–232. [Google Scholar] [CrossRef]
- Ilyina, Y.; Fot, E.; Kuzkov, V.; Kirov, M. The Glycocalyx Shedding Influences Hemodynamic and Metabolic Response to Fluid Load in Septic Shock. Turk. J. Anaesthesiol. Reanim. 2022, 50, 94–100. [Google Scholar] [CrossRef]
- Joffre, J.; Hellman, J.; Ince, C.; Ait-Oufella, H. Endothelial Responses in Sepsis. Am. J. Respir. Crit. Care Med. 2020, 202, 361–370. [Google Scholar] [CrossRef] [PubMed]
- Wardi, G.; Brice, J.; Correia, M.; Liu, D.; Self, M.; Tainter, C. Demystifying Lactate in the Emergency Department. Ann. Emerg. Med. 2020, 75, 287–298. [Google Scholar] [CrossRef] [PubMed]
- Mok, G.; Hendin, A.; Reardon, P.; Hickey, M.; Gray, S.; Yadav, K. Macrocirculatory and Microcirculatory Endpoints in Sepsis Resuscitation. J. Intensive Care Med. 2021, 36, 1385–1391. [Google Scholar] [CrossRef] [PubMed]
- De Backer, D.; Ricottilli, F.; Ospina-Tascón, G.A. Septic shock: A microcirculation disease. Curr. Opin. Anaesthesiol. 2021, 34, 85–91. [Google Scholar] [CrossRef]
- Bakker, J.; Kattan, E.; Annane, D.; Castro, R.; Cecconi, M.; De Backer, D.; Dubin, A.; Evans, L.; Gong, M.N.; Hamzaoui, O.; et al. Current practice and evolving concepts in septic shock resuscitation. Intensive Care Med. 2022, 48, 148–163. [Google Scholar] [CrossRef] [PubMed]
- Raa, A.; Sunde, G.A.; Bolann, B.; Kvåle, R.; Bjerkvig, C.; Eliassen, H.S.; Wentzel-Larsen, T.; Heltne, J.-K. Validation of a point-of-care capillary lactate measuring device (Lactate Pro 2). Scand. J. Trauma Resusc. Emerg. Med. 2020, 28, 83. [Google Scholar] [CrossRef]
- Viana, M.V.; Pantet, O.; Bagnoud, G.; Martinez, A.; Favre, E.; Charrière, M.; Favre, D.; Eckert, P.; Berger, M.M. Metabolic and Nutritional Characteristics of Long-Stay Critically Ill Patients. J. Clin. Med. 2019, 8, 985. [Google Scholar] [CrossRef]
- Gaieski, D.F.; Drumheller, B.C.; Goyal, M.; Fuchs, B.D.; Shofer, F.S.; Zogby, K. Accuracy of Handheld Point-of-Care Fingertip Lactate Measurement in the Emergency Department. West J. Emerg. Med. 2013, 14, 58–62. [Google Scholar] [CrossRef]
- Hariri, G.; Joffre, J.; Leblanc, G.; Bonsey, M.; Lavillegrand, J.R.; Urbina, T.; Guidet, B.; Maury, E.; Bakker, J.; Ait-Oufella, H. Narrative review: Clinical assessment of peripheral tissue perfusion in septic shock. Ann. Intensive Care 2019, 9, 37. [Google Scholar] [CrossRef]
- Collange, O.; Garcia, V.; Kindo, M.; Meyer, N.; Lavaux, T.; Mertes, P.M.; Joshi, G.P.; Diemunsch, P. Comparison of capillary and arterial lactate levels in patients with shock. Anaesth. Crit. Care Pain Med. 2017, 36, 157–162. [Google Scholar] [CrossRef]
- A Graham, C.; Leung, L.Y.; Lo, R.S.; Lee, K.H.; Yeung, C.Y.; Chan, S.Y.; Cattermole, G.; Hung, K.K. Agreement between capillary and venous lactate in emergency department patients: Prospective observational study. BMJ Open 2019, 9, e026109. [Google Scholar] [CrossRef] [PubMed]
- Purcarea, A.; Bourgarit, A.; Sovaila, A.; Ghiura, C.; Diemunsch, P.; Andres, E. Brief report: Serial capillary lactate measurement predict the evolution of early sepsis. J. Med. Life 2016, 9, 74–78. [Google Scholar] [PubMed]
- Pattharanitima, P.; Tongyoo, S.; Ratanarat, R.; Wilachone, W.; Poompichet, A.; Permpikul, C. Correlation of arterial, central venous and capillary lactate levels in septic shock patients. J. Med. Assoc. Thai. 2011, 94 (Suppl. S1), S175–S180. [Google Scholar] [PubMed]
- Léguillier, T.; Jouffroy, R.; Boisson, M.; Boussaroque, A.; Chenevier-Gobeaux, C.; Chaabouni, T.; Vivien, B.; Nivet-Antoine, V.; Beaudeux, J.-L. Lactate POCT in mobile intensive care units for septic patients? A comparison of capillary blood method versus venous blood and plasma-based reference methods. Clin. Biochem. 2018, 55, 9–14. [Google Scholar] [CrossRef]
- Yajnik, V.; Maarouf, R. Sepsis and the microcirculation: The impact on outcomes. Curr. Opin. Anaesthesiol. 2022, 35, 230–235. [Google Scholar] [CrossRef] [PubMed]
- López-Izquierdo, R.; Martín-Rodríguez, F.; Pastor, J.C.S.; Criado, J.G.; Millán, L.N.F.; Rodríguez, V.C.; Ibáñez, P.D.B.; Vegas, C.D.P. Can capillary lactate improve early warning scores in emergency department? An observational, prospective, multicentre study. Int. J. Clin. Pract. 2021, 75, e13779. [Google Scholar] [CrossRef]
- Morris, E.; McCartney, D.; Lasserson, D.; Van Den Bruel, A.; Fisher, R.; Hayward, G. Point-of-care lactate testing for sepsis at presentation to health care: A systematic review of patient outcomes. Br. J. Gen. Pract. 2017, 67, e859–e870. [Google Scholar] [CrossRef]
- Mullen, M.; Cerri, G.; Murray, R.; Talbot, A.; Sanseverino, A.; McCahill, P.; Mangolds, V.; Volturo, J.; Darling, C.; Restuccia, M. Use of point-of-care lactate in the prehospital aeromedical environment. Prehospital Disaster Med. 2014, 29, 200–203. [Google Scholar] [CrossRef]
- Contenti, J.; Corraze, H.; Lemoël, F.; Levraut, J. Effectiveness of arterial, venous, and capillary blood lactate as a sepsis triage tool in ED patients. Am. J. Emerg. Med. 2015, 33, 167–172. [Google Scholar] [CrossRef]
- Singer, A.J.; Taylor, M.; LeBlanc, D.; Williams, J.; Thode, H.C., Jr. ED bedside point-of-care lactate in patients with suspected sepsis is associated with reduced time to iv fluids and mortality. Am. J. Emerg. Med. 2014, 32, 1120–1124. [Google Scholar] [CrossRef]
- Maung, L.H.; Ng, X.H.; Ong, Z.Y.; See, K.C. Early lactate measurement triggers early treatment and improves outcomes in critically ill patients. Acad. Med. Singap. 2014, 1, S327. [Google Scholar]
- See, K.C.; Dizon, J.; Mahadevan, M.; Lim, T.K.; Phua, J. Impact of point-of-care lactate measurement on mortality in critically-ill patients requiring mechanical ventilation. European Respiratory Society Annual Congress. Eur. Respir. J. 2014, 44, P2062. [Google Scholar]
- Manzon, C.; Barrot, L.; Besch, G.; Barbot, O.; Desmettre, T.; Capellier, G.; Piton, G. Capillary lactate as a tool for the triage nurse among patients with SIRS at emergency department presentation: A preliminary report. Ann. Intensive Care 2015, 5, 7. [Google Scholar] [CrossRef] [PubMed]
- Houston, M.C.; Thompson, W.L.; Robertson, D. Shock. Diagnosis and management. Arch. Intern. Med. 1984, 144, 1433–1439. [Google Scholar] [CrossRef]
- Guven, G.; Hilty, M.P.; Ince, C. Microcirculation: Physiology, Pathophysiology, and Clinical Application. Blood Purif. 2020, 49, 143–150. [Google Scholar] [CrossRef] [PubMed]
- Zampieri, F.G.; Damiani, L.P.; Bakker, J.; Ospina-Tascón, G.A.; Castro, R.; Cavalcanti, A.B.; Hernandez, G. Effects of a Resuscitation Strategy Targeting Peripheral Perfusion Status versus Serum Lactate Levels among Patients with Septic Shock. A Bayesian Reanalysis of the ANDROMEDA-SHOCK Trial. Am. J. Respir. Crit. Care Med. 2020, 201, 423–429. [Google Scholar] [CrossRef]
- Hernández, G.; Ospina-Tascón, G.A.; Damiani, L.P.; Estenssoro, E.; Dubin, A.; Hurtado, J.; Friedman, G.; Castro, R.; Alegría, L.; Teboul, J.L.; et al. Effect of a Resuscitation Strategy Targeting Peripheral Perfusion Status vs. Serum Lactate Levels on 28-Day Mortality Among Patients With Septic Shock: The ANDROMEDA-SHOCK Randomized Clinical Trial. JAMA 2019, 321, 654–664. [Google Scholar] [CrossRef]
- Ait-Oufella, H.; Bige, N.; Boelle, P.Y.; Pichereau, C.; Alves, M.; Bertinchamp, R.; Baudel, J.L.; Galbois, A.; Maury, E.; Guidet, B. Capillary refill time exploration during septic shock. Intensive Care Med. 2014, 40, 958–964. [Google Scholar] [CrossRef]
- Ait-Oufella, H.; Lemoinne, S.; Boelle, P.Y.; Galbois, A.; Baudel, J.L.; Lemant, J.; Joffre, J.; Margetis, D.; Guidet, B.; Maury, E.; et al. Mottling score predicts survival in septic shock. Intensive Care Med. 2011, 37, 801–807. [Google Scholar] [CrossRef]
- Lara, B.; Enberg, L.; Ortega, M.; Leon, P.; Kripper, C.; Aguilera, P.; Kattan, E.; Castro, R.; Bakker, J.; Hernandez, G. Capillary refill time during fluid resuscitation in patients with sepsis-related hyperlactatemia at the emergency department is related to mortality. PLoS ONE 2017, 12, e0188548. [Google Scholar] [CrossRef]
- Dépret, F.; Legrand, M. Are capillary and arterial lactates interchangeable? Anaesth. Crit. Care Pain Med. 2017, 36, 149. [Google Scholar] [CrossRef] [PubMed]
- La Via, L.; Sanfilippo, F.; Continella, C.; Triolo, T.; Messina, A.; Robba, C.; Astuto, M.; Hernandez, G.; Noto, A. Agreement between Capillary Refill Time measured at Finger and Earlobe sites in different positions: A pilot prospective study on healthy volunteers. BMC Anesthesiol. 2023, 23, 30. [Google Scholar] [CrossRef] [PubMed]
- Jacquet-Lagrèze, M.; Wiart, C.; Schweizer, R.; Didier, L.; Ruste, M.; Coutrot, M.; Legrand, M.; Baudin, F.; Javouhey, E.; Dépret, F.; et al. Capillary refill time for the management of acute circulatory failure: A survey among pediatric and adult intensivists. BMC Emerg. Med. 2022, 22, 131. [Google Scholar] [CrossRef] [PubMed]
- Guarino, M.; Gambuti, E.; Alfano, F.; De Giorgi, A.; Maietti, E.; Strada, A.; Ursini, F.; Volpato, S.; Caio, G.; Contini, C.; et al. Predicting in-hospital mortality for sepsis: A comparison between qSOFA and modified qSOFA in a 2-year single-centre retrospective analysis. Eur. J. Clin. Microbiol. Infect. Dis. 2021, 40, 825–831. [Google Scholar] [CrossRef]
- Guarino, M.; Perna, B.; Cesaro, A.E.; Maritati, M.; Spampinato, M.D.; Contini, C.; De Giorgio, R. 2023 Update on Sepsis and Septic Shock in Adult Patients: Management in the Emergency Department. J. Clin. Med. 2023, 12, 3188. [Google Scholar] [CrossRef]
- Myles, P.; Cui, J.I. Using the Bland–Altman method to measure agreement with repeated measures. Br. J. Anaesth. 2007, 99, 309–311. [Google Scholar] [CrossRef]
- DeLong, E.R.; DeLong, D.M.; Clarke-Pearson, D.L. Comparing the areas under two or more correlated receiver operating characteristic curves: A nonparametric approach. Biometrics 1988, 44, 837–845. [Google Scholar] [CrossRef]

| Clinical/Lab Features | 48-h Mortality | 7-Day Mortality | ||||
|---|---|---|---|---|---|---|
| Survived | Deceased | Survived | Deceased | |||
| n = 184 (90.7%) | n = 19 (9.3%) | p | n = 175 (86.2%) | n = 28 (13.8%) | p | |
| Male | 79 (42.9) | 10 (52.6) | 0.395 | 76 (43.4) | 11 (39.3) | 0.68 |
| Age, years | 85 (79–89) | 85 (73–90) | 0.74 | 85 (79–90) | 84 (71–88) | 0.91 |
| CCI > 4 | 36 (19.4) | 5 (26.3) | 0.47 | 34 (19.4) | 6 (21.4) | 0.8 |
| Admission to the ED | ||||||
| MAP | 76 (60–92) | 78 (55–92) | 0.55 | 77 (62–92) | 75 (56–90) | 0.51 |
| Altered mental status | 152 (82.6) | 18 (94.7) | 0.54 | 142 (82.1) | 27 (96.4) | 0.06 |
| GCS | 13 (11–14) | 9 (7.5–13) | 0.001 | 13 (10.5–14) | 8 (6–11) | 0.01 |
| Laboratory data | ||||||
| Hb g/dL | 11.5 (9.65–13.3) | 11 (9.5–13) | <0.001 | 11.5 (9.65–13.3) | 10.9 (8.3–13) | 0.23 |
| PLT (×1000/mmc) | 224 (165–281) | 230.5 (150–320) | 0.84 | 230 (170–286) | 187 (144–287) | 0.47 |
| Bilirubin mg/dL | 0.8 (0.52–1.19) | 0.79 (0.56–1.06) | 0.93 | 0.795 (0.52–1.18) | 0.87 (0.51–1.06) | 0.94 |
| INR | 1.15 (1.07–1.26) | 1.32 (1.15–1.69) | 0.01 | 1.16 (1.07–1.27) | 1.34 (1.2–1.8) | 0.03 |
| C-reactive protein mg/dL | 10.1 (3.17–16.17) | 13.47 (2.82–22.07) | 0.46 | 10. (3.17–15.98)1 | 14.39 (2.28–23.47) | 0.78 |
| Urea mg/dL | 65 (40–110) | 95 (53–173) | 0.06 | 64 (40–110) | 121 (73.5–244.5) | 0.02 |
| Creatinine mg/dL | 1.24 (0.83–1.92) | 1.92 (0.96–3.63) | 0.12 | 1.24 (0.83–1.92) | 2.86 (1.32–4.57) | 0.02 |
| DTX mg/dL | 128 (109–166.5) | 163 (123–326) | 0.06 | 128 (110–170) | 170.5 (123.5–276) | 0.17 |
| Blood Gas Analysis | ||||||
| pH | 7.45 (7.4–7.48) | 7.37 (7.18–7.40) | <0.001 | 7.45 (7.4–7.48) | 7.26 (7.16–7.37) | <0.001 |
| pO2 mmHg | 74.3 (66–87.75) | 86 (68–168) | 0.18 | 74.5 (66–88) | 91.35 (66.5–127) | 0.44 |
| pCO2 mmHg | 35.7 (32–41) | 35.5 (30.6–40) | 0.93 | 35.8 (32.4–41) | 32 (24.6–38) | 0.5 |
| HCO3 mmol/L | 25.8 (22.5–28.5) | 19 (12.7–26.3) | 0.12 | 25.8 (22.4–28.6) | 15.25 (11–19) | 0.01 |
| P/F | 334.5 (269–389) | 374 (210–446) | 0.61 | 339.5 (274–393) | 231 (113–446) | 0.65 |
| Severity scores | ||||||
| SIRS ≥ 2 | 124 (67.8) | 16 (84.2) | 0.14 | 116 (67.4) | 23 (82.1) | 0.12 |
| NEWS ≥ 7 | 111 (59.7) | 17 (89.5) | 0.11 | 103 (58.9) | 23 (82.1) | 0.02 |
| NEWS | 8 (5–10) | 10.5 (9–12) | <0.001 | 8 (5–10) | 10 (9–13) | 0.001 |
| SOFA ≥ 2 | 154 (82.8) | 17 (89.5) | 0.45 | 146 (83.4) | 24 (85.7) | 0.76 |
| SOFA | 4 (3–6) | 7 (5–8) | <0.001 | 4 (3–6) | 8 (7–9) | 0.001 |
| Treatments in the ED | ||||||
| O2 supplementation | 78 (42.2) | 13 (72.2) | 0.01 | 73 (42) | 17 (63) | 0.04 |
| Optimal fluid replacement | 127 (68.6) | 16 (84.2) | 0.16 | 119 (68.4) | 22 (78.6) | 0.27 |
| Antibiotics administration | 95 (51.9) | 12 (66.7) | 0.23 | 89 (51.7) | 17 (63) | 0.28 |
| Vasopressors administration | 4 (2.2) | 3 (15.8) | 0.01 | 4 (2.3) | 3 (10.7) | 0.02 |
| Serum and Capillary Lactate | ||||||
| SLs mmol/L | 1.1 (0.7–2) | 2.75 (1.55–8.1) | <0.001 | 1.1 (0.7–2) | 6.5 (2.4–11.1) | 0.001 |
| SLs ≥ 2 mmol/L | 47 (25.3) | 15 (78.9) | <0.001 | 43 (24.6) | 18 (64.3) | <0.001 |
| CLs mmol/L | 5 (3.1–9.1) | 11.15 (3.7–22.95) | <0.001 | 5 (3–9.05) | 19.3 (10.8–25) | <0.001 |
| CLs ≥ 16.8 mmol/L | 11 (5.9) | 13 (68.4) | <0.001 | 11 (6.3) | 12 (42.9) | <0.001 |
| 48-h Mortality | 7-Day Mortality | |||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p | OR | 95% CI | p | |
| CLs ≥ 16.8mmol/L | 22.960 | 4.72–111.53 | <0.001 | 6.090 | 1.78–20.87 | 0.004 |
| SLs ≥ 2 mmol/L | 13.790 | 1.43–132.9 | 0.020 | 3.880 | 1.25–12.05 | 0.020 |
| SOFA | 1.460 | 0.98–2.18 | 0.060 | 1.160 | 0.91–1.48 | 0.210 |
| NEWS | 1.030 | 0.77–1.38 | 0.830 | 1.130 | 0.94–1.36 | 0.160 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Guarino, M.; Perna, B.; Cesaro, A.E.; Spampinato, M.D.; Previati, R.; Costanzini, A.; Maritati, M.; Contini, C.; De Giorgio, R. Comparison between Capillary and Serum Lactate Levels in Predicting Short-Term Mortality of Septic Patients at the Emergency Department. Int. J. Mol. Sci. 2023, 24, 9121. https://doi.org/10.3390/ijms24119121
Guarino M, Perna B, Cesaro AE, Spampinato MD, Previati R, Costanzini A, Maritati M, Contini C, De Giorgio R. Comparison between Capillary and Serum Lactate Levels in Predicting Short-Term Mortality of Septic Patients at the Emergency Department. International Journal of Molecular Sciences. 2023; 24(11):9121. https://doi.org/10.3390/ijms24119121
Chicago/Turabian StyleGuarino, Matteo, Benedetta Perna, Alice Eleonora Cesaro, Michele Domenico Spampinato, Rita Previati, Anna Costanzini, Martina Maritati, Carlo Contini, and Roberto De Giorgio. 2023. "Comparison between Capillary and Serum Lactate Levels in Predicting Short-Term Mortality of Septic Patients at the Emergency Department" International Journal of Molecular Sciences 24, no. 11: 9121. https://doi.org/10.3390/ijms24119121
APA StyleGuarino, M., Perna, B., Cesaro, A. E., Spampinato, M. D., Previati, R., Costanzini, A., Maritati, M., Contini, C., & De Giorgio, R. (2023). Comparison between Capillary and Serum Lactate Levels in Predicting Short-Term Mortality of Septic Patients at the Emergency Department. International Journal of Molecular Sciences, 24(11), 9121. https://doi.org/10.3390/ijms24119121









