A Highly Sensitive Biomarker of Type II Collagen C-Terminal Pro-Peptide Associated with Cartilage Formation
Abstract
1. Introduction
2. Results
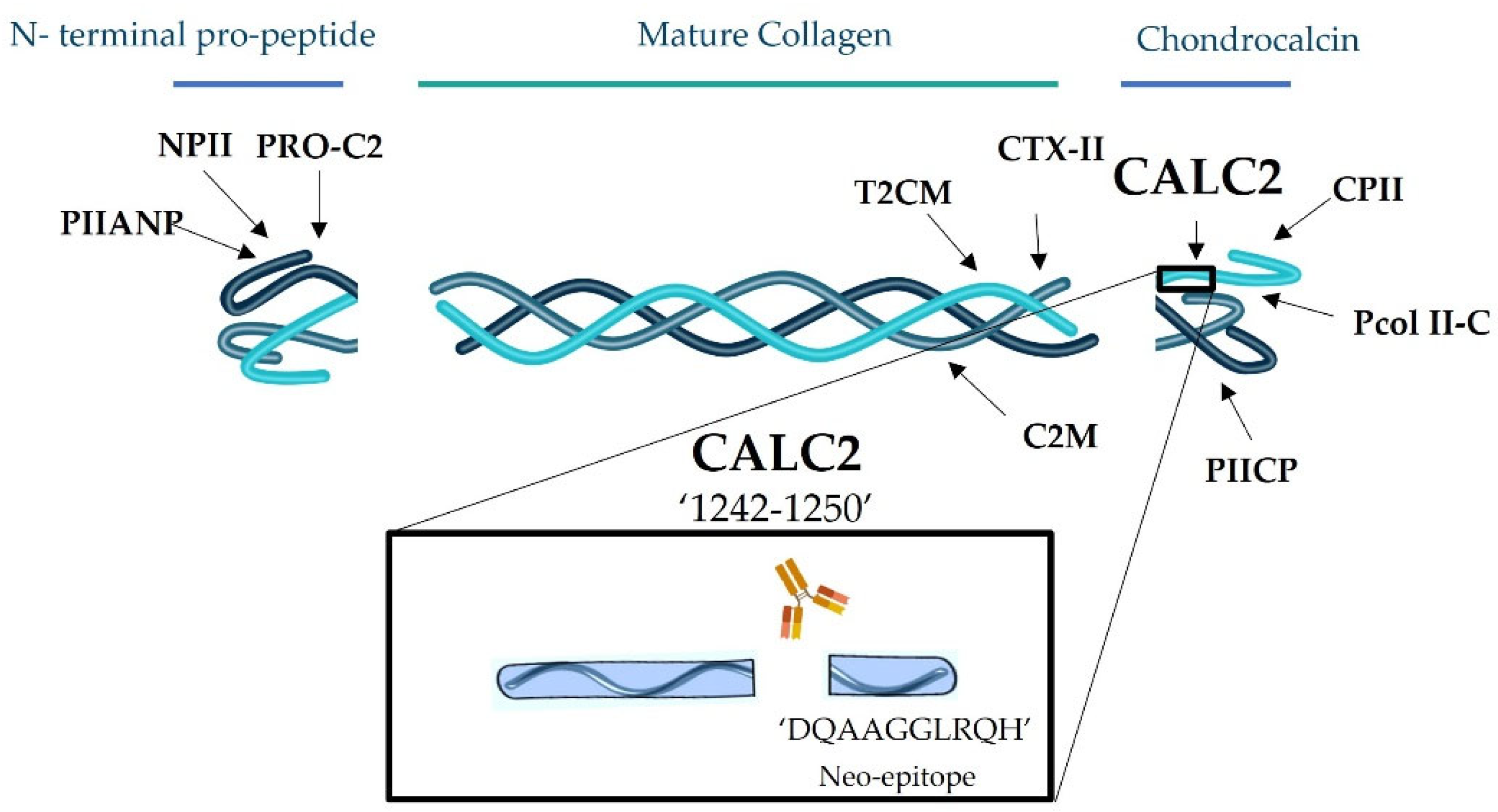
2.1. CALC2 Neoepitope Identification and Monoclonal Antibody Characterisation
2.2. Development and Technical Evaluation of the CALC2 Assay
2.3. Biological and Clinical Evaluations of the CALC2 Assay
3. Discussion
4. Materials and Methods
4.1. Materials
4.2. Immunogen Selection, Immunisation, and Fusion
4.3. Assay Protocol for CALC2 CLIA
4.4. Technical Evaluation of CALC2
4.5. Human Cartilage Explant Model
4.6. In Vitro Protease Cleavage
4.7. Western Blot of HEX Supernatant
4.8. Clinical Profiling of CALC2
4.9. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sophia Fox, A.J.; Bedi, A.; Rodeo, S.A. The basic science of articular cartilage: Structure, composition, and function. Sports Health 2009, 1, 461. [Google Scholar] [CrossRef] [PubMed]
- Gudmann, N.S.; Wang, J.; Hoielt, S.; Chen, P.; Siebuhr, A.S.; He, Y.; Christiansen, T.G.; Karsdal, M.A.; Bay-Jensen, A.C. Cartilage turnover reflected by metabolic processing of type II collagen: A novel marker of anabolic function in chondrocytes. Int. J. Mol. Sci. 2014, 15, 18789–18803. [Google Scholar] [CrossRef] [PubMed]
- Van Der Rest, M.; Rosenberg, L.C.; Olsen, B.R.; Pooletii, A.R. Chondrocalcin is identical with the C-propeptide of type II procollagen. Biochem. J. 1986, 237, 923–925. [Google Scholar] [CrossRef] [PubMed]
- Lian, W.; Liu, H.; Sun, L.Y.; Liu, Y.Q.; Cui, S.L.; Wang, Y.; Song, Q.Q.; Deng, Q.; Wang, S.P.; Cao, Y.H.; et al. Serum levels of PIICP, PIIANP, and PIIBNP are decreased in patients with an endemic osteochondropathy, Kashin-Beck disease. J. Orthop. Surg. Res. 2018, 13, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Broder, C.; Arnold, P.; Goff, S.V.L.; Konerding, M.A.; Bahr, K.; Müller, S.; Overall, C.M.; Bond, J.S.; Koudelka, T.; Tholey, A.; et al. Metalloproteases meprin α and meprin β are C- and N-procollagen proteinases important for collagen assembly and tensile strength. Proc. Natl. Acad. Sci. USA 2013, 110, 14219–14224. [Google Scholar] [CrossRef] [PubMed]
- Luo, Y.; He, Y.; Reker, D.; Gudmann, N.S.; Henriksen, K.; Simonsen, O.; Ladel, C.; Michaelis, M.; Mobasheri, A.; Karsdal, M.; et al. A novel high sensitivity type II collagen blood-based biomarker, PRO-C2, for assessment of cartilage formation. Int. J. Mol. Sci. 2018, 19, 3485. [Google Scholar] [CrossRef] [PubMed]
- Bay-Jensen, A.C.; Liu, Q.; Byrjalsen, I.; Li, Y.; Wang, J.; Pedersen, C.; Leeming, D.J.; Dam, E.B.; Zheng, Q.; Qvist, P.; et al. Enzyme-linked immunosorbent assay (ELISAs) for metalloproteinase derived type II collagen neoepitope, CIIM-increased serum CIIM in subjects with severe radiographic osteoarthritis. Clin. Biochem. 2011, 44, 423–429. [Google Scholar] [CrossRef] [PubMed]
- Christgau, S.; Garnero, P.; Fledelius, C.; Moniz, C.; Ensig, M.; Gineyts, E.; Rosenquist, C.; Qvist, P. Collagen Type II C-telopeptide fragments as an index of cartilage degradation. Bone 2001, 29, 209–215. [Google Scholar] [CrossRef] [PubMed]
- Groen, S.S.; Sinkeviciute, D.; Bay-Jensen, A.-C.; Thudium, C.S.; Karsdal, M.A.; Thomsen, S.F.; Lindemann, S.; Werkmann, D.; Blair, J.; Staunstrup, L.M.; et al. A serological type II collagen neoepitope biomarker reflects cartilage breakdown in patients with osteoarthritis. Osteoarthr. Cartil. Open 2021, 3, 100207. [Google Scholar] [CrossRef] [PubMed]
- Nemirovskiy, O.V.; Sunyer, T.; Aggarwal, P.; Abrams, M.; Hellio, M.P.; Graverand, L.; Mathews, W.R. Discovery and development of the N-terminal procollagen type II (NPII) biomarker: A tool for measuring collagen type II synthesis. Osteoarthr. Cartil. 2008, 16, 1494–1500. [Google Scholar] [CrossRef] [PubMed]
- Shinmei, M.; Ito, K.; Matsuyama, S.; Yoshihara, Y.; Matsuzawa, K. Joint fluid carboxy-terminal type ii procollagen peptide as a marker of cartilage collagen biosynthesis. Osteoarthr. Cartil. 1993, 1, 121–128. [Google Scholar] [CrossRef] [PubMed]
- Rousseau, J.C.; Zhu, Y.; Miossec, P.; Vignon, E.; Sandell, L.J.; Garnero, P.; Delmas, P.D. Serum levels of type IIA procollagen amino terminal propeptide (PIIANP) are decreased in patients with knee osteoarthritis and rheumatoid arthritis. Osteoarthr. Cartil. 2004, 12, 440–447. [Google Scholar] [CrossRef] [PubMed]
- Nelson, F.; Dahlberg, L.; Laverty, S.; Reiner, A.; Pidoux, I.; Ionescu, M.; Fraser, G.L.; Brooks, E.; Tanzer, M.; Rosenberg, L.C.; et al. Evidence for altered synthesis of type II collagen in patients with osteoarthritis. J. Clin. Investig. 1998, 102, 2115–2125. [Google Scholar] [CrossRef] [PubMed]
- Committee for Medicinal Products for Human Use. Guideline on Bioanalytical Method Validation; European Medicines Agency: London, UK, 2021; pp. 1–23. [Google Scholar]
- Bihlet, A.R.; Byrjalsen, I.; Bay-Jensen, A.C.; Andersen, J.R.; Christiansen, C.; Riis, B.J.; Karsdal, M.A. Associations between biomarkers of bone and cartilage turnover, gender, pain categories and radiographic severity in knee osteoarthritis. Arthritis Res. Ther. 2019, 21, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Chung, H.J.; Steplewski, A.; Chung, K.Y.; Uitto, J.; Fertala, A. Collagen fibril formation: A new target to limit fibrosis. J. Biol. Chem. 2008, 283, 25879–25886. [Google Scholar] [CrossRef] [PubMed]
- Kim, T.H.; Stone, M.; Payne, U.; Zhang, X.; Ionescu, M.; Lobanok, T.; King, L.; Robin, A.P.; Inman, R.D. Cartilage biomarkers in ankylosing spondylitis: Relationship to clinical variables and treatment response. Arthr. Rheum. 2005, 52, 885–891. [Google Scholar] [CrossRef] [PubMed]
- Gefter, M.L.; Margulies, D.H.; Scharff, M.D. A simple method for polyethylene glycol-promoted hybridization of mouse myeloma cells. Somat. Cell Genet. 1977, 3, 231–236. [Google Scholar] [CrossRef]
- Reker, D.; Siebuhr, A.S.; Thudium, C.S.; Gantzel, T.; Ladel, C.; Michaelis, M.; Aspberg, A.; Berchtold, M.W.; Karsdal, M.A.; Gigout, A.; et al. Sprifermin (RhFGF18) versus vehicle induces a biphasic process of extracellular matrix remodeling in human knee OA articular cartilage ex vivo. Sci. Rep. 2020, 10, 6011. [Google Scholar] [CrossRef] [PubMed]




| Assay Parameter | Result |
| IC50 | 1.63 ng/mL |
| Measurement range (LLOQ–ULOQ) | 0.44–44 ng/mL |
| Inter-assay variation * | 12% (6.19–21.11%) |
| Intra-assay variation * | 7% (4.91–11.47%) |
| Dilution recovery of human serum (n = 4) * | 106% (102–113%) |
| Spiking recovery (serum in serum) (n = 3) * | 83% (76–95%) |
| Analyte stability * | |
| 98.9–113%/101–128.3% 95.6–110.5%/92.7–110.2% 100.6–115.8%/101.4–106.4% 98.5–101.5%/100.8–115.1% |
| Analyte recovery, 4 freeze/thaw cycles * | 93.8% (62.4–113.8) |
| Haemoglobin recovery low/high * | 109.6%/110.7% |
| Lipid recovery low/high * | 99%/93% |
| Biotin recovery low/high * | 93.1%/102.5% |
| Patients with RA (n = 18) | Patients with AS (n = 19) | Healthy Donors (n = 18) | p Value | |
|---|---|---|---|---|
| Age, years | 35.7 (3.3) | 35.8 (3.2) | 35.8 (3.8) | 0.981 |
| Sex, male | 9 (50.0%) | 10 (52.6%) | 9 (50.0%) | 0.983 |
| BMI, kg/m2 | 24.1 (1.8) | 22.9 (1.9) * | 25.6 (3.0) | 0.034 |
| CALC2, ng/mL | 0.6 (0.2) | 0.6 (0.3) | 1.2 (0.6) | <0.001 |
| Patients with OA (n = 8) | Healthy Donors (n = 14) | p Value | |
|---|---|---|---|
| Age, years | 69.8 (4.1) | 70.6 (1.2) | 0.683 |
| Sex, male | 4 (50.0%) | 7 (50.0%) | 0.375 |
| BMI, kg/m2 | 29.5 (3.0) | 25.9 (2.0) | 0.038 |
| CALC2, ng/mL | 0.6 (0.2) | 0.8 (0.4) | 0.729 |
| Peptide Type | Sequence |
|---|---|
| Immunogenic peptide | DQAAGGLRQH-GGC-KLH * |
| Standard peptide | DQAAGGLRQH |
| Screening peptide | DQAAGGLRQH{LYS(Biotin)} |
| Elongated peptide | ADQAAGGLRQH |
| Truncated peptide | QAAGGLRQH |
| Non-sense coating peptide | MSAFAGLGPRK-Biotin |
| Non-sense standard peptide | MSAFAGLGPR |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Port, H.; Bay-Jensen, A.-C.; He, Y.; Karsdal, M.A.; Gantzel, T.; Thudium, C.S.; Holm Nielsen, S. A Highly Sensitive Biomarker of Type II Collagen C-Terminal Pro-Peptide Associated with Cartilage Formation. Int. J. Mol. Sci. 2023, 24, 454. https://doi.org/10.3390/ijms24010454
Port H, Bay-Jensen A-C, He Y, Karsdal MA, Gantzel T, Thudium CS, Holm Nielsen S. A Highly Sensitive Biomarker of Type II Collagen C-Terminal Pro-Peptide Associated with Cartilage Formation. International Journal of Molecular Sciences. 2023; 24(1):454. https://doi.org/10.3390/ijms24010454
Chicago/Turabian StylePort, Helena, Anne-Christine Bay-Jensen, Yi He, Morten A. Karsdal, Thorbjørn Gantzel, Christian S. Thudium, and Signe Holm Nielsen. 2023. "A Highly Sensitive Biomarker of Type II Collagen C-Terminal Pro-Peptide Associated with Cartilage Formation" International Journal of Molecular Sciences 24, no. 1: 454. https://doi.org/10.3390/ijms24010454
APA StylePort, H., Bay-Jensen, A.-C., He, Y., Karsdal, M. A., Gantzel, T., Thudium, C. S., & Holm Nielsen, S. (2023). A Highly Sensitive Biomarker of Type II Collagen C-Terminal Pro-Peptide Associated with Cartilage Formation. International Journal of Molecular Sciences, 24(1), 454. https://doi.org/10.3390/ijms24010454







