Evaluation of a Gel Containing a Propionibacterium Extract in an In Vivo Model of Wound Healing
Abstract
:1. Introduction
2. Materials and Methods
2.1. The Tested Formulation
2.2. Study Design
2.3. Antioxidant Activity
2.4. Franz Cell Diffusion Study
2.5. In Vitro Study
2.5.1. Cell Culture
2.5.2. In Vitro Model Induction
2.5.3. Experimental Design
2.5.4. Malondialdehyde (MDA) and Nitrite Evaluation by Biochemical Assay
2.6. In Vivo Study
2.6.1. Materials
2.6.2. Animals
2.6.3. Wound Healing Induction Model
2.6.4. Experimental Groups
2.6.5. Immunohistochemical Localization of TNF-α, IL-1β TGF-β, VEGF, ICAM-1, and P-Selectin
2.6.6. Toluidine Blue Staining
2.6.7. Pruritogen-Induced Scratching Behaviors
2.6.8. Skin Irritation
2.6.9. Histopathological Analysis
2.7. Malondialdehyde (MDA) Assay
2.8. Nitrite/Nitrate Measurement
2.9. Statistical Analysis
3. Results
3.1. Antioxidant Activity of Bacterial Extract
3.2. Effect of Emorsan® Gel Diffusion through Mice Epidermal Mucosa over 24 h
3.3. Effect of Propionibacterium Extract on Oxidative Stress
3.4. Effect of Emorsan® Gel Administration on Proinflammatory Cytokines after Wound Induction
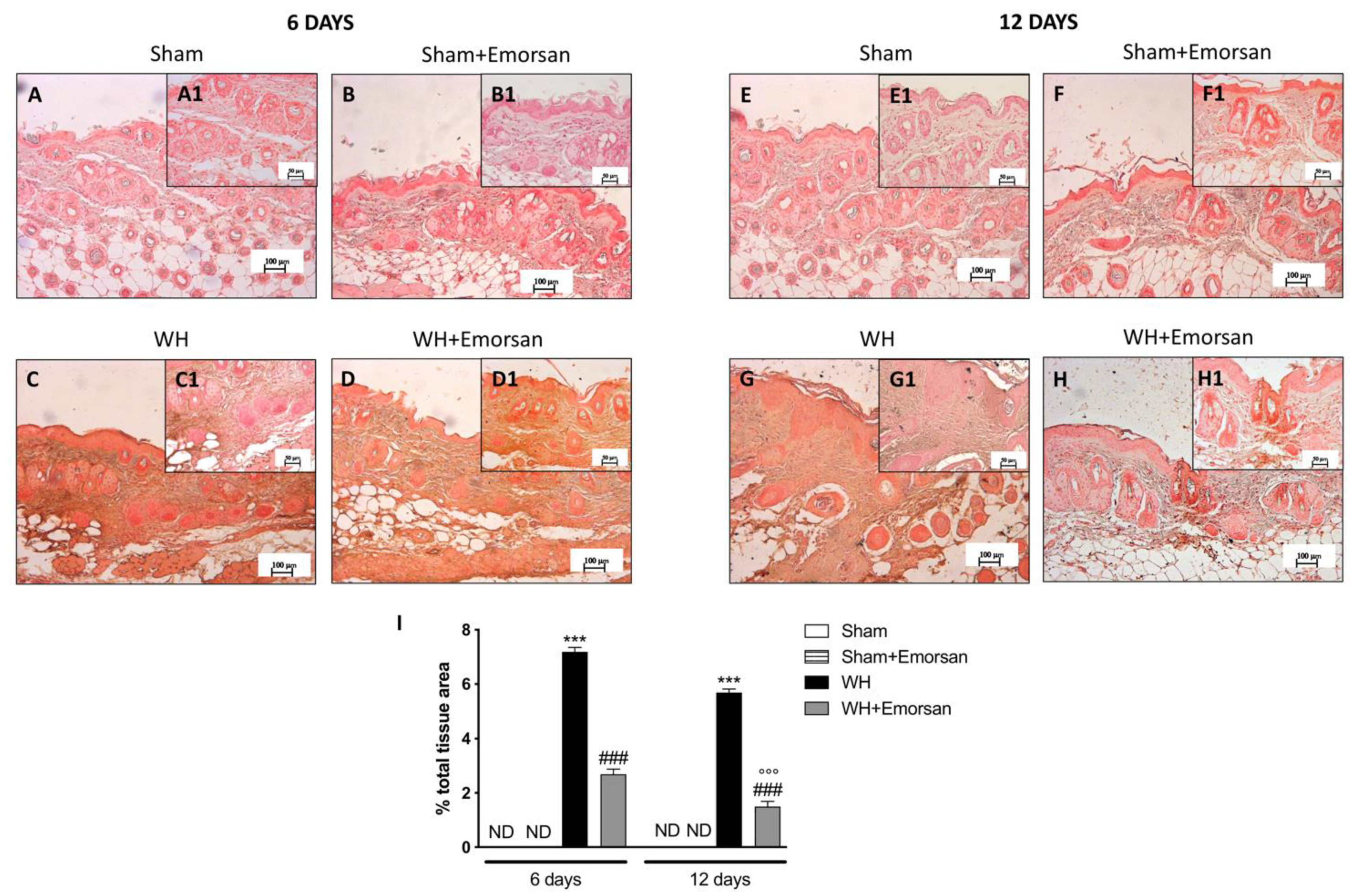
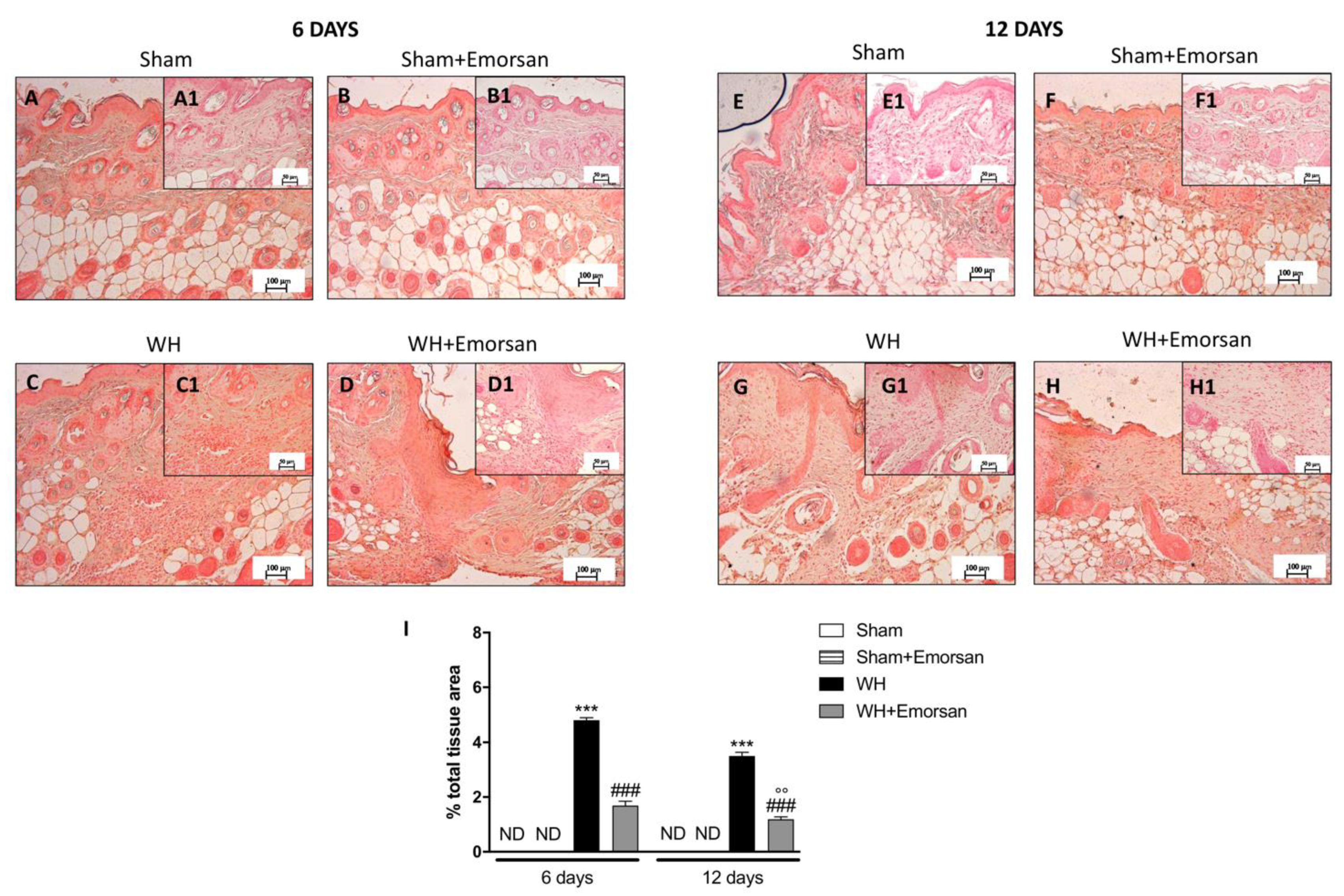
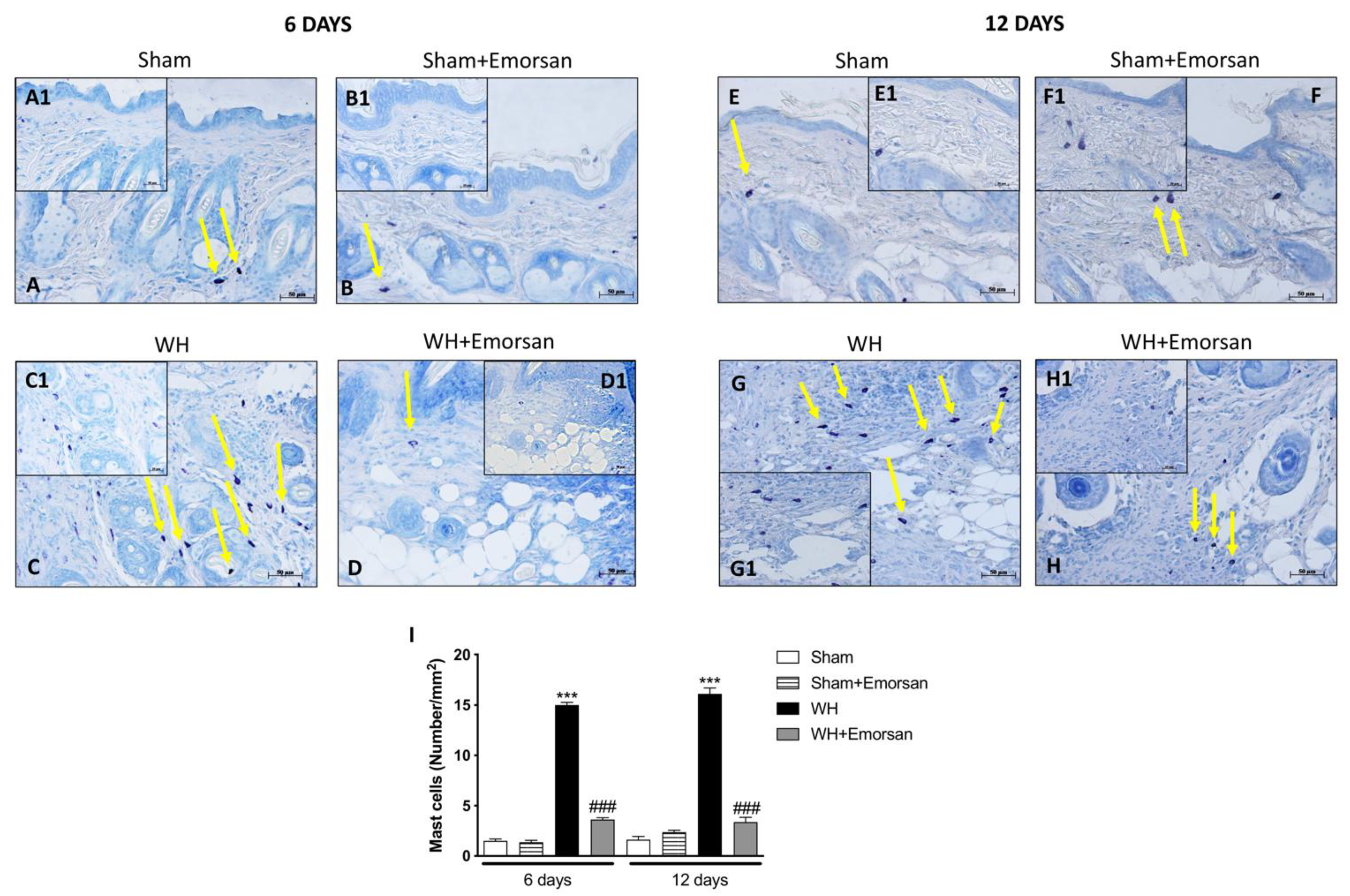
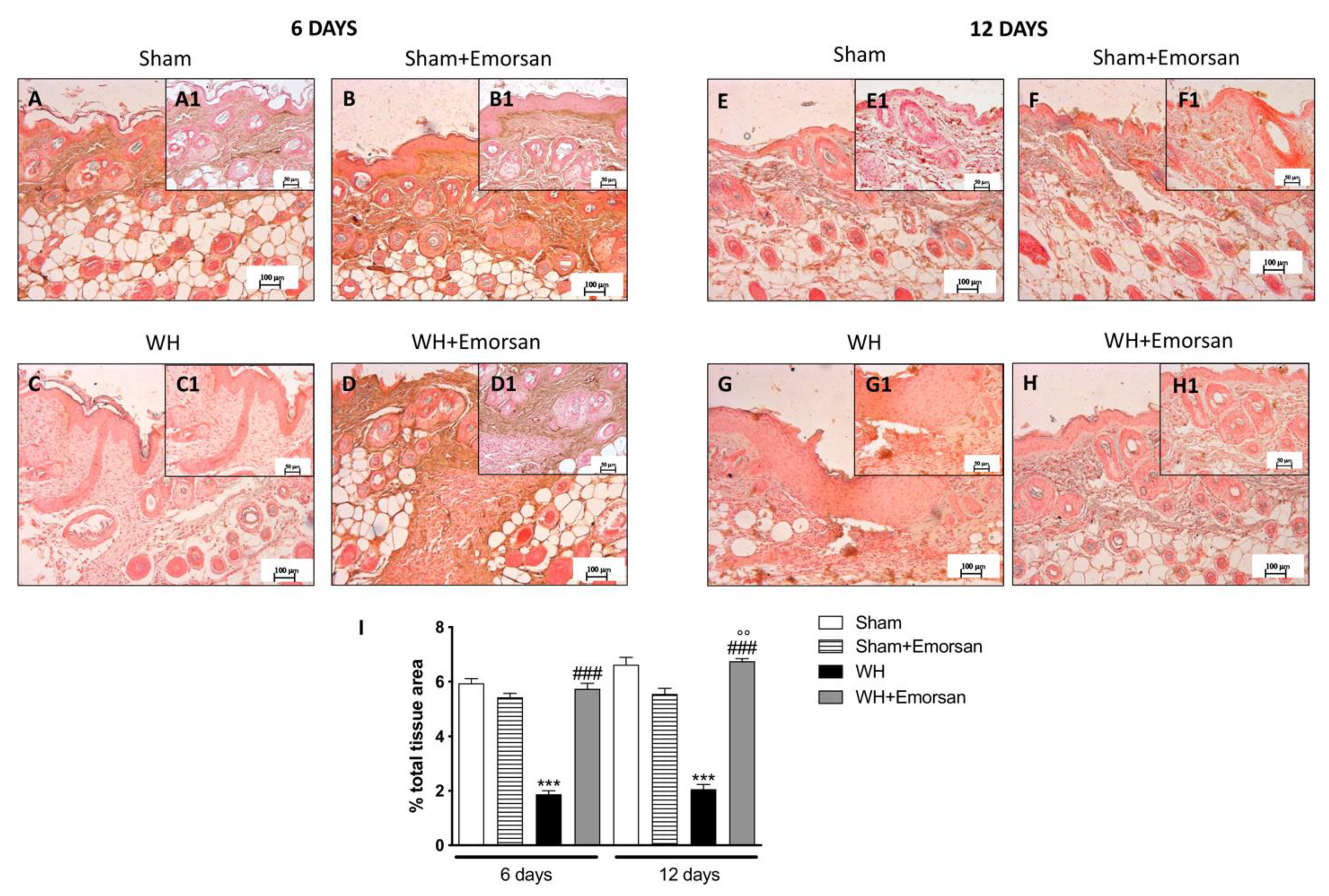
3.5. Effect of Emorsan® Gel Administration on Mast Cells Infiltration after Wound Induction
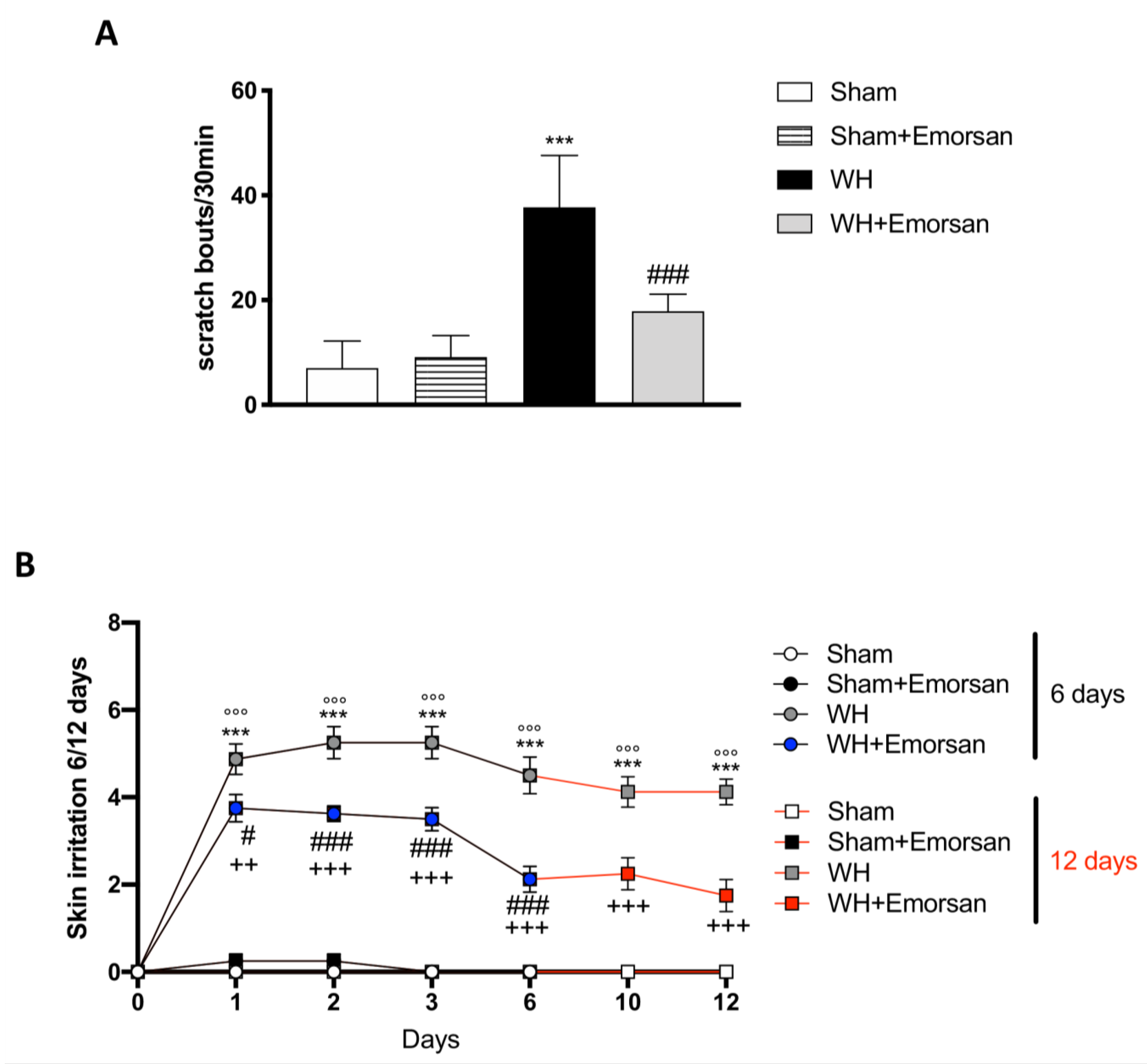
3.6. Effect of Emorsan® Gel Administration on Itch-Induced Scratching and Skin Irritation
3.7. Effect of Emorsan® Gel Administration on TGF-β Expression
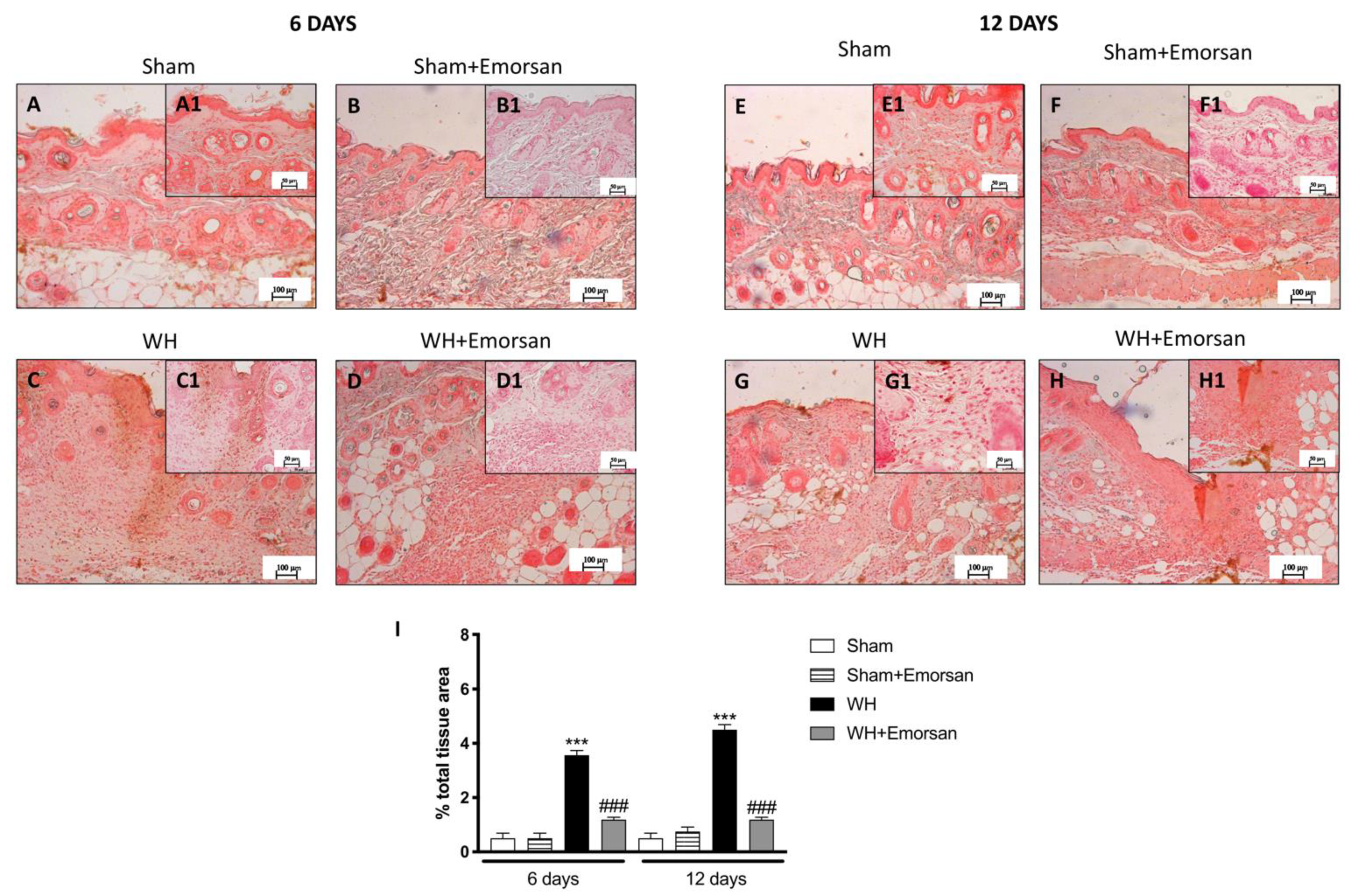
3.8. Effect of Emorsan® Gel Administration on VEGF Expression after Wound Induction
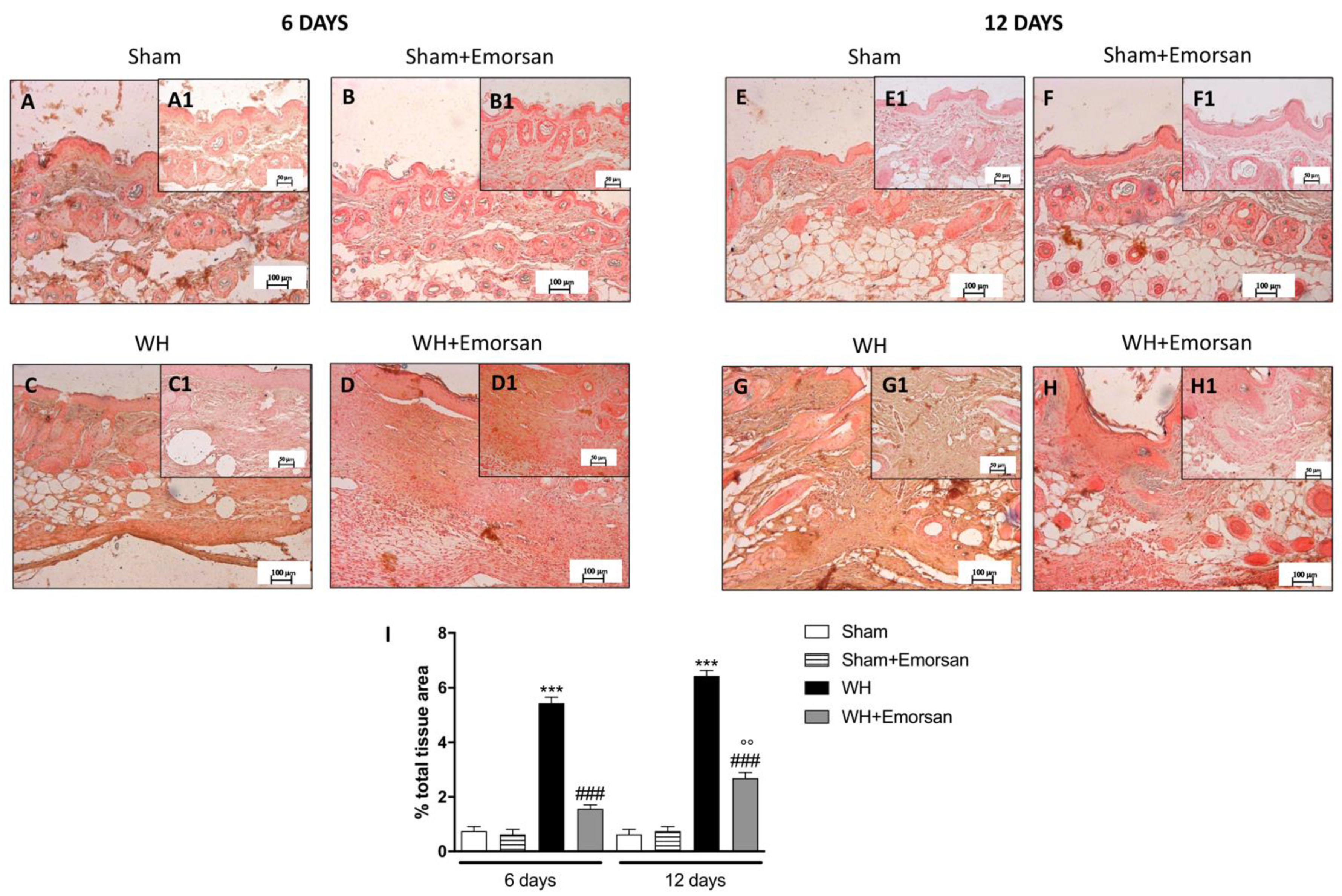
3.9. Effect of Emorsan® Gel Administration on ICAM-1 and P-Selectin Expression after Wound Induction
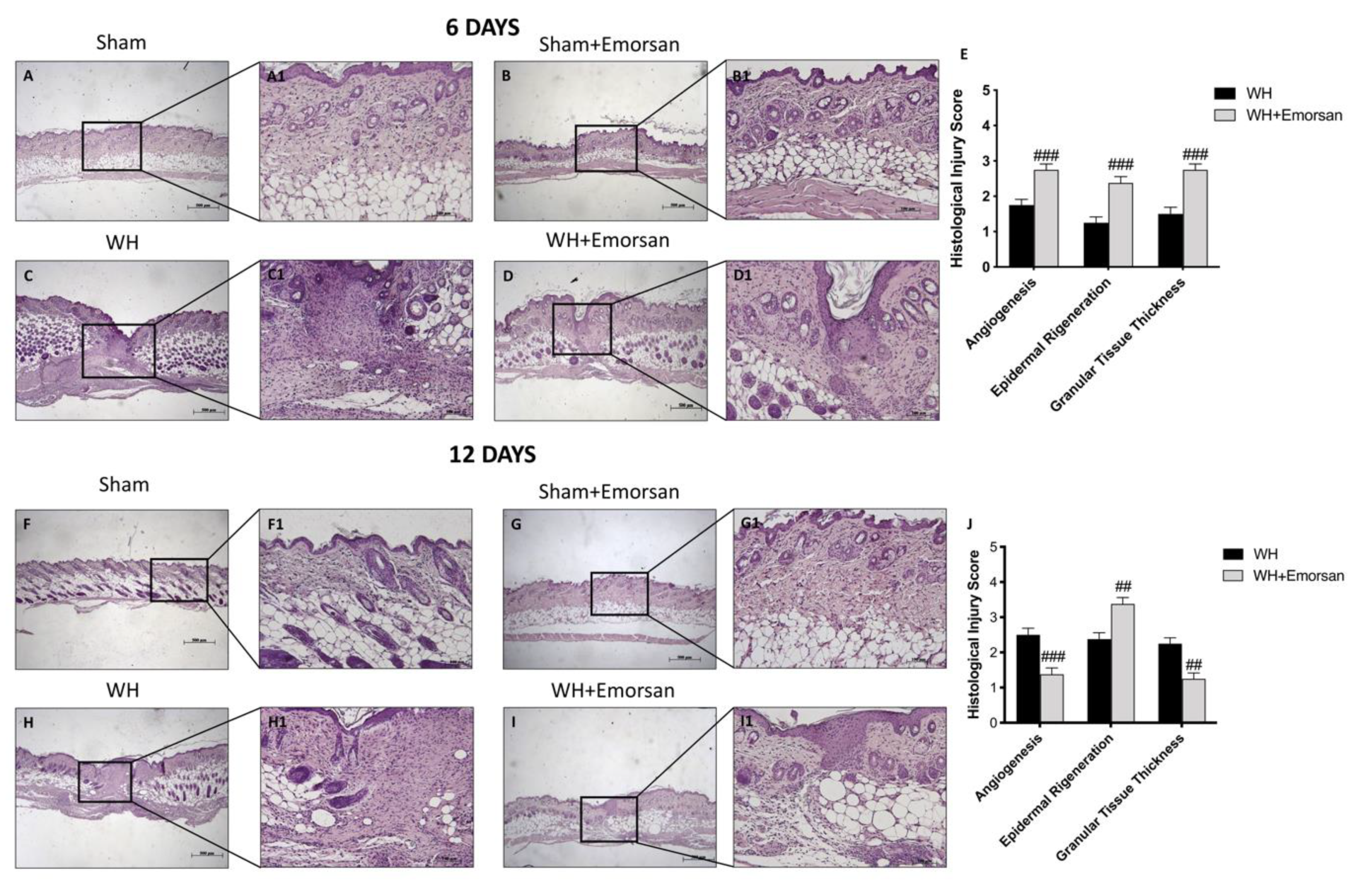
3.10. Effect of Emorsan® Gel Administration on Epidermal Tissue Repair
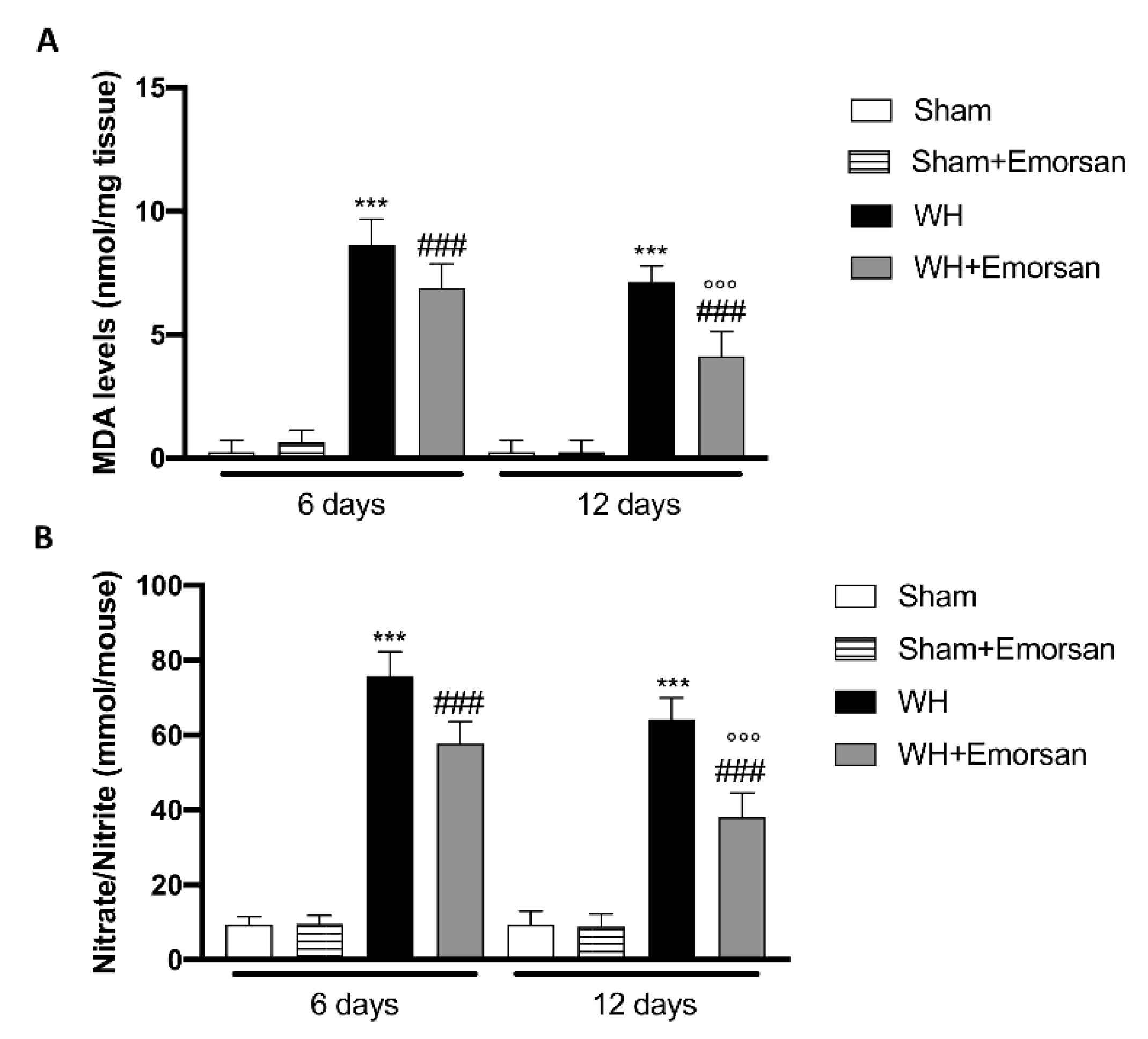
3.11. Effect of Emorsan® Gel Administration on Oxidative Stress Markers after Wound Induction
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wilkins, R.G.; Unverdorben, M. Wound cleaning and wound healing: A concise review. Adv. Ski. Wound Care 2013, 26, 160–163. [Google Scholar] [CrossRef] [PubMed]
- Dunn, L.; Prosser, H.C.; Tan, J.T.; Vanags, L.Z.; Ng, M.K.; Bursill, C.A. Murine model of wound healing. J. Vis. Exp. 2013, 75, e50265. [Google Scholar] [CrossRef] [Green Version]
- Zarchi, K.; Martinussen, T.; Jemec, G.B. Wound healing and all-cause mortality in 958 wound patients treated in home care. Wound Repair Regen. 2015, 23, 753–758. [Google Scholar] [CrossRef] [PubMed]
- McLafferty, E.; Hendry, C.; Farley, A. The integumentary system: Anatomy, physiology and function of skin. Nurs. Stand. 2012, 27, 35. [Google Scholar] [CrossRef] [PubMed]
- Bootun, R. Effects of immunosuppressive therapy on wound healing. Int. Wound J. 2013, 10, 98–104. [Google Scholar] [CrossRef] [PubMed]
- Siracusa, R.; Impellizzeri, D.; Cordaro, M.; Gugliandolo, E.; Peritore, A.F.; Di Paola, R.; Cuzzocrea, S. Topical Application of Adelmidrol + Trans-Traumatic Acid Enhances Skin Wound Healing in a Streptozotocin-Induced Diabetic Mouse Model. Front. Pharmacol. 2018, 9, 871. [Google Scholar] [CrossRef] [PubMed]
- Reinke, J.M.; Sorg, H. Wound repair and regeneration. Eur. Surg. Res. 2012, 49, 35–43. [Google Scholar] [CrossRef]
- Yang, F.; Qin, X.; Zhang, T.; Lin, H.; Zhang, C. Evaluation of Small Molecular Polypeptides from the Mantle of Pinctada Martensii on Promoting Skin Wound Healing in Mice. Molecules 2019, 24, 4231. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ustuner, O.; Anlas, C.; Bakirel, T.; Ustun-Alkan, F.; Diren Sigirci, B.; Ak, S.; Akpulat, H.A.; Donmez, C.; Koca-Caliskan, U. In vitro evaluation of antioxidant, anti-inflammatory, antimicrobial and wound healing potential of thymus sipyleus boiss. subsp. rosulans (borbas) jalas. Molecules 2019, 24, 3353. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Deng, L.; Du, C.; Song, P.; Chen, T.; Rui, S.; Armstrong, D.G.; Deng, W. The Role of Oxidative Stress and Antioxidants in Diabetic Wound Healing. Oxid. Med. Cell Longev. 2021, 2021, 8852759. [Google Scholar] [CrossRef]
- Bilgen, F.; Ural, A.; Kurutas, E.B.; Bekerecioglu, M. The effect of oxidative stress and Raftlin levels on wound healing. Int. Wound J. 2019, 16, 1178–1184. [Google Scholar] [CrossRef]
- Dunnill, C.; Patton, T.; Brennan, J.; Barrett, J.; Dryden, M.; Cooke, J.; Leaper, D.; Georgopoulos, N.T. Reactive oxygen species (ROS) and wound healing: The functional role of ROS and emerging ROS-modulating technologies for augmentation of the healing process. Int. Wound J. 2017, 14, 89–96. [Google Scholar] [CrossRef]
- Dissemond, J.; Goos, M.; Wagner, S. The role of oxidative stress in the pathogenesis and therapy of chronic wounds. Der Hautarzt Z. Fur Dermatol. Venerol. Und Verwandte Geb. 2002, 53, 718–723. [Google Scholar] [CrossRef] [PubMed]
- Triantafillou, V.; Workman, A.D.; Patel, N.N.; Maina, I.W.; Tong, C.C.L.; Kuan, E.C.; Kennedy, D.W.; Palmer, J.N.; Adappa, N.D.; Waizel-Haiat, S.; et al. Broncho-Vaxom(R) (OM-85 BV) soluble components stimulate sinonasal innate immunity. Int. Forum. Allergy Rhinol. 2019, 9, 370–377. [Google Scholar] [CrossRef]
- Jurkiewicz, D.; Zielnik-Jurkiewicz, B. Bacterial lysates in the prevention of respiratory tract infections. Otolaryngol. Pol. 2018, 72, 1–8. [Google Scholar] [CrossRef]
- Melis, G.B.; Piras, B.; Marotto, M.F.; Neri, M.; Corda, V.; Vallerino, V.; Saba, A.; Lello, S.; Pilloni, M.; Zedda, P.; et al. The stimulation of the vaginal immune system with short-term administration of a vaginal gel containing fraction of Propionibacterium acnes, hyaluronic acid and polycarbophil is efficacious in vaginal infections dependent on disorders in the vaginal ecosystem. Gynecol. Endocrinol. 2018, 34, 880–883. [Google Scholar] [CrossRef] [PubMed]
- Mangano, K.; Vergalito, F.; Mammana, S.; Mariano, A.; De Pasquale, R.; Meloscia, A.; Bartollino, S.; Guerra, G.; Nicoletti, F.; Di Marco, R. Evaluation of hyaluronic acid-P40 conjugated cream in a mouse model of dermatitis induced by oxazolone. Exp. Ther. Med. 2017, 14, 2439–2444. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Allhorn, M.; Arve, S.; Brüggemann, H.; Lood, R. A novel enzyme with antioxidant capacity produced by the ubiquitous skin colonizer Propionibacterium acnes. Sci. Rep. 2016, 6, 36412. [Google Scholar] [CrossRef] [Green Version]
- Gallo, G.; Grossi, U.; Di Tanna, G.L.; Santoro, G.A.; De Paola, G.; Clerico, G.; Realis Luc, A.; Trompetto, M.; Sammarco, G. Short-Term Outcomes of Polycarbophil and Propionibacterium acnes Lysate Gel after Open Hemorrhoidectomy: A Prospective Cohort Study. J. Clin. Med. 2020, 9, 3996. [Google Scholar] [CrossRef] [PubMed]
- Proksch, E. pH in nature, humans and skin. J. Dermatol. 2018, 45, 1044–1052. [Google Scholar] [CrossRef] [PubMed]
- Boniakowski, A.E.; Kimball, A.S.; Jacobs, B.N.; Kunkel, S.L.; Gallagher, K.A. Macrophage-Mediated Inflammation in Normal and Diabetic Wound Healing. J. Immunol. 2017, 199, 17–24. [Google Scholar] [CrossRef] [Green Version]
- Yu, L.; Perret, J.; Harris, M.; Wilson, J.; Haley, S. Antioxidant properties of bran extracts from “Akron” wheat grown at different locations. J. Agric. Food Chem. 2003, 51, 1566–1570. [Google Scholar] [CrossRef] [PubMed]
- Re, R.; Pellegrini, N.; Proteggente, A.; Pannala, A.; Yang, M.; Rice-Evans, C. Antioxidant activity applying an improved ABTS radical cation decolorization assay. Free Radic. Biol. Med. 1999, 26, 1231–1237. [Google Scholar] [CrossRef]
- Ayala, A.; Munoz, M.F.; Arguelles, S. Lipid peroxidation: Production, metabolism, and signaling mechanisms of malondialdehyde and 4-hydroxy-2-nonenal. Oxid. Med. Cell Longev. 2014, 2014, 360438. [Google Scholar] [CrossRef]
- Lanza, M.; Casili, G.; Torre, G.L.; Giuffrida, D.; Rotondo, A.; Esposito, E.; Ardizzone, A.; Rando, R.; Bartolomeo, G.; Albergamo, A.; et al. Properties of a New Food Supplement Containing Actinia equina Extract. Antioxidants 2020, 9, 945. [Google Scholar] [CrossRef]
- Calabrese, G.; Ardizzone, A.; Campolo, M.; Conoci, S.; Esposito, E.; Paterniti, I. Beneficial Effect of Tempol, a Membrane-Permeable Radical Scavenger, on Inflammation and Osteoarthritis in In Vitro Models. Biomolecules 2021, 11, 352. [Google Scholar] [CrossRef] [PubMed]
- Campolo, M.; Crupi, R.; Cordaro, M.; Cardali, S.M.; Ardizzone, A.; Casili, G.; Scuderi, S.A.; Siracusa, R.; Esposito, E.; Conti, A.; et al. Co-Ultra PEALut Enhances Endogenous Repair Response Following Moderate Traumatic Brain Injury. Int. J. Mol. Sci. 2021, 22, 8717. [Google Scholar] [CrossRef] [PubMed]
- Campolo, M.; Casili, G.; Paterniti, I.; Filippone, A.; Lanza, M.; Ardizzone, A.; Scuderi, S.A.; Cuzzocrea, S.; Esposito, E. Effect of a Product Containing Xyloglucan and Pea Protein on a Murine Model of Atopic Dermatitis. Int. J. Mol. Sci. 2020, 21, 3596. [Google Scholar] [CrossRef] [PubMed]
- Song, J.; Xian, D.; Yang, L.; Xiong, X.; Lai, R.; Zhong, J. Pruritus: Progress toward Pathogenesis and Treatment. Biomed. Res. Int. 2018, 2018, 9625936. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Upton, D.; Richardson, C.; Andrews, A.; Rippon, M. Wound pruritus: Prevalence, aetiology and treatment. J. Wound Care 2013, 22, 501–508. [Google Scholar] [CrossRef]
- Proksch, E.; de Bony, R.; Trapp, S.; Boudon, S. Topical use of dexpanthenol: A 70th anniversary article. J. Dermatolog. Treat 2017, 28, 766–773. [Google Scholar] [CrossRef]
- Scuderi, S.A.; Casili, G.; Lanza, M.; Filippone, A.; Paterniti, I.; Esposito, E.; Campolo, M. Modulation of NLRP3 Inflammasome Attenuated Inflammatory Response Associated to Diarrhea-Predominant Irritable Bowel Syndrome. Biomedicines 2020, 8, 519. [Google Scholar] [CrossRef]
- Genovese, T.; Duranti, A.; D’Amico, R.; Fusco, R.; Impellizzeri, D.; Peritore, A.F.; Crupi, R.; Gugliandolo, E.; Cuzzocrea, S.; Di Paola, R.; et al. Fatty Acid Amide Hydrolase (FAAH) Inhibition Plays a Key Role in Counteracting Acute Lung Injury. Int. J. Mol. Sci. 2022, 23, 2781. [Google Scholar] [CrossRef]
- Mareček, V.; Mikyška, A.; Hampel, D.; Čejka, P.; Neuwirthová, J.; Malachová, A.; Cerkal, R. ABTS and DPPH methods as a tool for studying antioxidant capacity of spring barley and malt. J. Cereal Sci. 2017, 73, 40–45. [Google Scholar] [CrossRef]
- Kaleci, B.; Koyuturk, M. Efficacy of resveratrol in the wound healing process by reducing oxidative stress and promoting fibroblast cell proliferation and migration. Dermatol. Ther. 2020, 33, e14357. [Google Scholar] [CrossRef]
- Ng, M.F. The role of mast cells in wound healing. Int. Wound J. 2010, 7, 55–61. [Google Scholar] [CrossRef] [PubMed]
- Sutthammikorn, N.; Supajatura, V.; Yue, H.; Takahashi, M.; Chansakaow, S.; Nakano, N.; Song, P.; Ogawa, T.; Ikeda, S.; Okumura, K.; et al. Topical Gynura procumbens as a Novel Therapeutic Improves Wound Healing in Diabetic Mice. Plants 2021, 10, 1122. [Google Scholar] [CrossRef] [PubMed]
- Ud-Din, S.; Wilgus, T.A.; Bayat, A. Mast Cells in Skin Scarring: A Review of Animal and Human Research. Front. Immunol. 2020, 11, 552205. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Yu, H.; Pan, H.; Zhou, X.; Ruan, Q.; Kong, D.; Chu, Z.; Li, H.; Huang, J.; Huang, X. Nrf2 suppression delays diabetic wound healing through sustained oxidative stress and inflammation. Front. Pharmacol. 2019, 10, 1099. [Google Scholar] [CrossRef] [PubMed]
- Ashcroft, G.S.; Jeong, M.J.; Ashworth, J.J.; Hardman, M.; Jin, W.; Moutsopoulos, N.; Wild, T.; McCartney-Francis, N.; Sim, D.; McGrady, G. Tumor necrosis factor-alpha (TNF-α) is a therapeutic target for impaired cutaneous wound healing. Wound Repair Regen. 2012, 20, 38–49. [Google Scholar] [CrossRef] [Green Version]
- Mirza, R.E.; Fang, M.M.; Ennis, W.J.; Koh, T.J. Blocking interleukin-1β induces a healing-associated wound macrophage phenotype and improves healing in type 2 diabetes. Diabetes 2013, 62, 2579–2587. [Google Scholar] [CrossRef] [Green Version]
- Parnell, L.K.S. Itching for Knowledge About Wound and Scar Pruritus. Wounds 2018, 30, 17–36. [Google Scholar] [PubMed]
- Golpanian, R.S.; Smith, P.; Yosipovitch, G. Itch in organs beyond the skin. Curr. Allergy Asthma Rep. 2020, 20, 49. [Google Scholar] [CrossRef]
- Lichtman, M.K.; Otero-Vinas, M.; Falanga, V. Transforming growth factor beta (TGF-β) isoforms in wound healing and fibrosis. Wound Repair Regen. 2016, 24, 215–222. [Google Scholar] [CrossRef] [PubMed]
- Honnegowda, T.M.; Kumar, P.; Udupa, E.G.P.; Kumar, S.; Kumar, U.; Rao, P. Role of angiogenesis and angiogenic factors in acute and chronic wound healing. Plast. Aesthetic Res. 2015, 2, 243–249. [Google Scholar]
- Bao, P.; Kodra, A.; Tomic-Canic, M.; Golinko, M.S.; Ehrlich, H.P.; Brem, H. The role of vascular endothelial growth factor in wound healing. J. Surg. Res. 2009, 153, 347–358. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Koivisto, L.; Heino, J.; Häkkinen, L.; Larjava, H. Integrins in wound healing. Adv. Wound Care 2014, 3, 762–783. [Google Scholar] [CrossRef] [Green Version]
- Groves, R.; Allen, M.; Ross, E.; Barker, J.; MacDonald, D. Tumour necrosis factor alpha is pro-inflammatory in normal human skin and modulates cutaneous adhesion molecule expression. Br. J. Dermatol. 1995, 132, 345–352. [Google Scholar] [CrossRef] [PubMed]
- Ley, K. The role of selectins in inflammation and disease. Trends Mol. Med. 2003, 9, 263–268. [Google Scholar] [CrossRef] [Green Version]
- Pardo, A.; Gómez-Florit, M.; Barbosa, S.; Taboada, P.; Domingues, R.M.A.; Gomes, M.E. Magnetic Nanocomposite Hydrogels for Tissue Engineering: Design Concepts and Remote Actuation Strategies to Control Cell Fate. ACS Nano 2021, 15, 175–209. [Google Scholar] [CrossRef] [PubMed]
- Ziai, Y.; Petronella, F.; Rinoldi, C.; Nakielski, P.; Zakrzewska, A.A.; Kowalewski, T.A.; Augustyniak, W.; Li, X.; Calogero, A.; Sabała, I.; et al. Chameleon-inspired multifunctional plasmonic nanoplatforms for biosensing applications. NPG Asia Mater. 2022, 14, 14–18. [Google Scholar] [CrossRef]
- Gallo, G.; Martellucci, J.; Sturiale, A.; Clerico, G.; Milito, G.; Marino, F.; Cocorullo, G.; Giordano, P.; Mistrangelo, M.; Trompetto, M. Consensus statement of the Italian society of colorectal surgery (SICCR): Management and treatment of hemorrhoidal disease. Tech. Coloproctol. 2020, 24, 145–164. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pata, F.; Sgro, A.; Ferrara, F.; Vigorita, V.; Gallo, G.; Pellino, G. Anatomy, Physiology and Pathophysiology of Haemorrhoids. Rev. Recent Clin. Trials 2021, 16, 75–80. [Google Scholar] [CrossRef] [PubMed]


| Treatment | Days of Treatment | Number of Animals |
|---|---|---|
| SHAM | ||
| Vehicle | 6 | 8 |
| Vehicle | 12 | 8 |
| Emorsan® Gel | 6 | 8 |
| Emorsan® Gel | 12 | 8 |
| WH | ||
| Vehicle | 6 | 8 |
| Vehicle | 12 | 8 |
| Emorsan® Gel | 6 | 8 |
| Emorsan® Gel | 12 | 8 |
| Reaction | Irritation Score |
|---|---|
| Erythema and eschar formation | |
| No erythema | 0 |
| Very slight erythema (barely perceptible) | 1 |
| Well-defined erythema | 2 |
| Moderate erythema | 3 |
| Severe erythema (beet-redness) | 4 |
| Oedema formation | |
| No oedema | 0 |
| Very slight oedema (barely perceptible) | 1 |
| Well-defined oedema (edges of area well-defined by definite raising) | 2 |
| Moderate oedema (raised approximately 1 mm) | 3 |
| Severe oedema (raised more than 1 mm an extending beyond exposure area) | 4 |
| Maximal possible score for irritation | 8 |
| Method | Trolox Equivalent/kg Bacterial Extract ± Standard Deviation |
|---|---|
| ABTS | 19.95 ± 2.08 |
| DPPH | 7.88 ± 1.93 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
M., C.; G., G.; F., R.; A., A.; M., L.T.; A., F.; M., L.; S., C.; L., S.; E., E. Evaluation of a Gel Containing a Propionibacterium Extract in an In Vivo Model of Wound Healing. Int. J. Mol. Sci. 2022, 23, 4708. https://doi.org/10.3390/ijms23094708
M. C, G. G, F. R, A. A, M. LT, A. F, M. L, S. C, L. S, E. E. Evaluation of a Gel Containing a Propionibacterium Extract in an In Vivo Model of Wound Healing. International Journal of Molecular Sciences. 2022; 23(9):4708. https://doi.org/10.3390/ijms23094708
Chicago/Turabian StyleM., Campolo, Gallo G., Roviello F., Ardizzone A., La Torre M., Filippone A., Lanza M., Cuzzocrea S., Siroli L., and Esposito E. 2022. "Evaluation of a Gel Containing a Propionibacterium Extract in an In Vivo Model of Wound Healing" International Journal of Molecular Sciences 23, no. 9: 4708. https://doi.org/10.3390/ijms23094708
APA StyleM., C., G., G., F., R., A., A., M., L. T., A., F., M., L., S., C., L., S., & E., E. (2022). Evaluation of a Gel Containing a Propionibacterium Extract in an In Vivo Model of Wound Healing. International Journal of Molecular Sciences, 23(9), 4708. https://doi.org/10.3390/ijms23094708













