Membrane Interactivity of Capsaicin Antagonized by Capsazepine
Abstract
1. Introduction
2. Results
2.1. Interaction with Phosphatidylcholine Liposomal Membranes
2.2. Interaction with Neuro-Mimetic Membranes
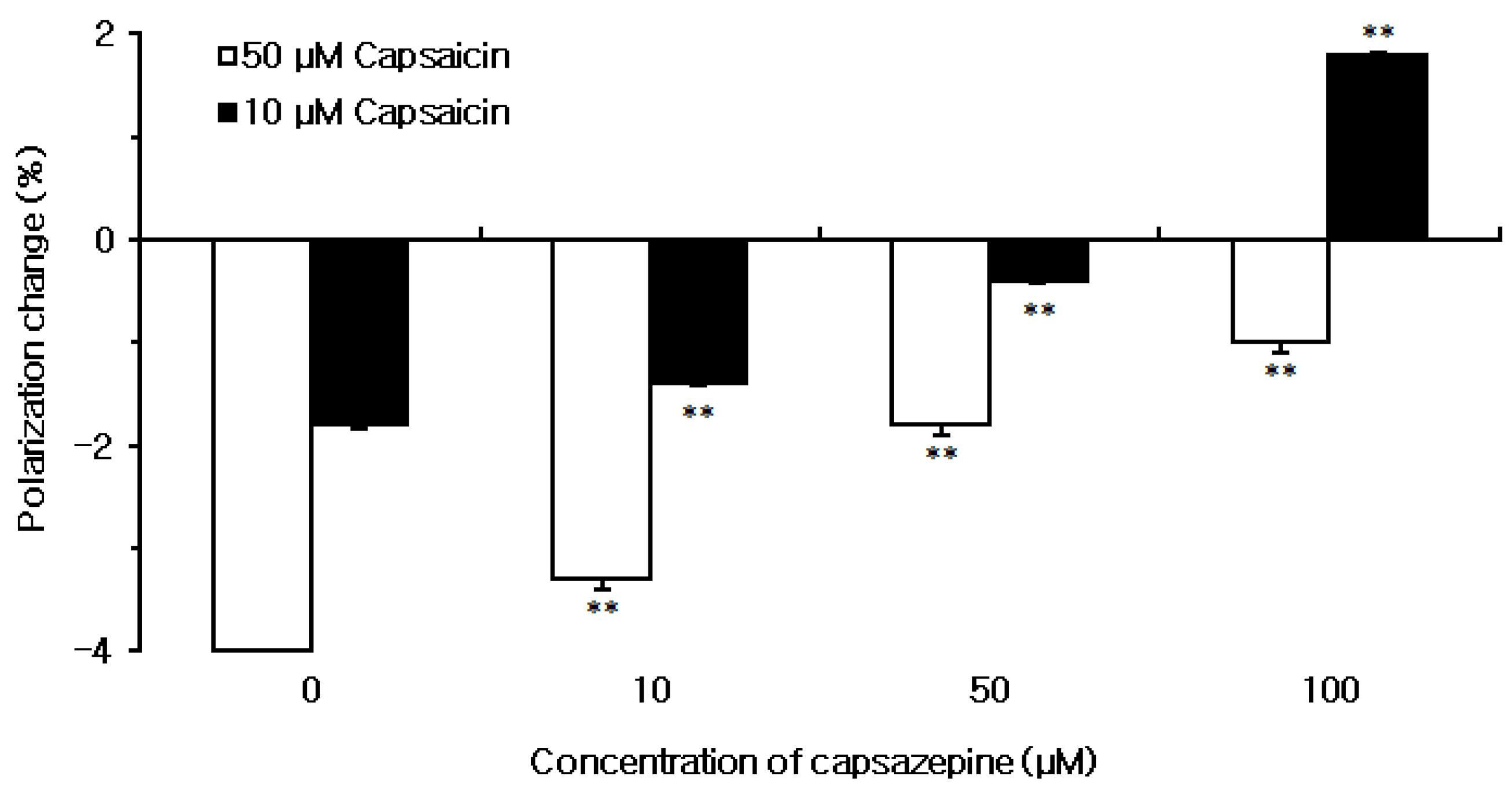
2.3. Effect of Capsaicin on Neuro-Mimetic Membranes and Inhibition by Capsazepine
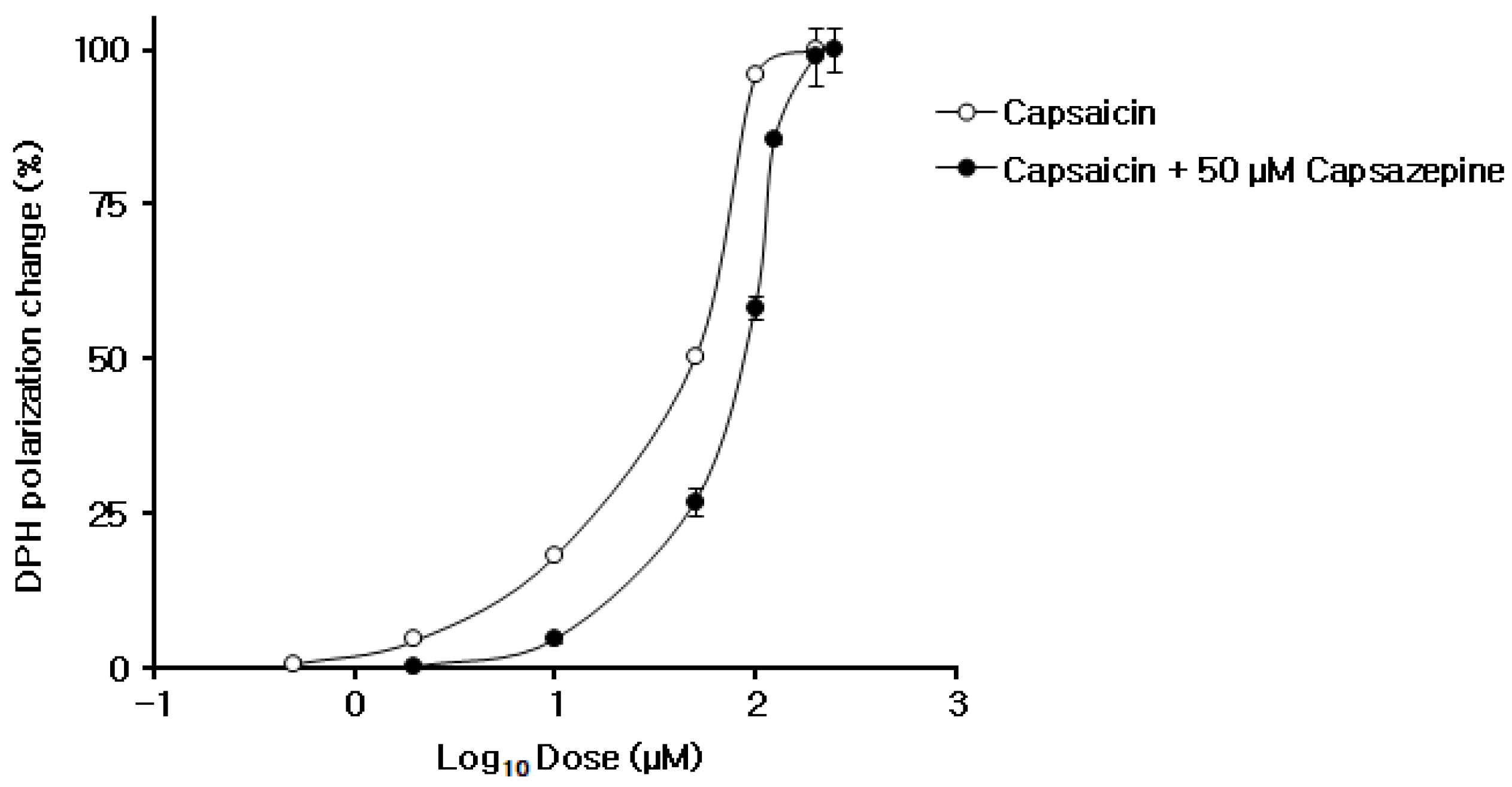
2.4. Membrane Interaction Antagonism between Capsaicin and Capsazepine
3. Discussion
4. Materials and Methods
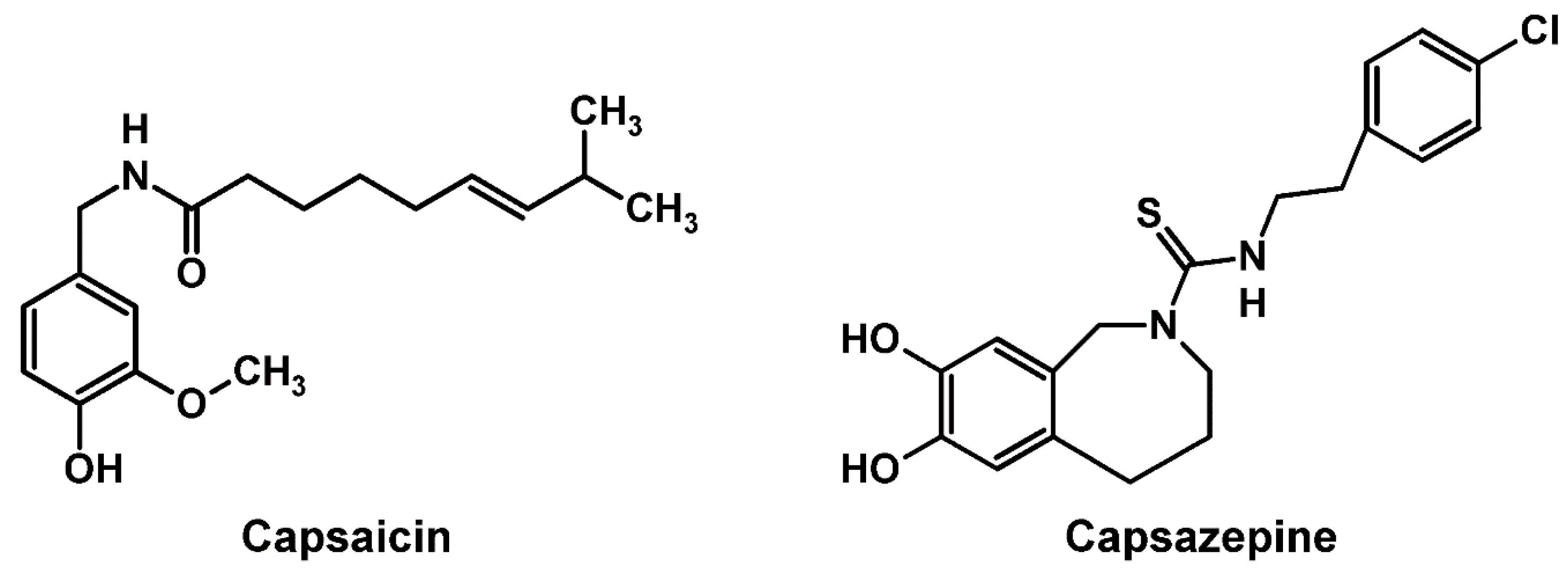
4.1. Chemicals
4.2. Membrane Preparation
4.3. Determination of Membrane Interactivity
4.4. Estimation of Antagonism between Capsaicin and Capsazepine
4.5. Statistical Analysis
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| DMSO | dimethyl sulfoxide |
| DOPC | 1,2-dioleoylphosphatidylcholine |
| DPH | diphenyl-1,3,5-hexatriene |
| DPPC | 1,2-dipalmitoylphosphatidylcholine |
| EGCG | (−)-epigallocatechin-3-gallate |
| POPC | 1-palmitoyl-2-oleoylphosphatidylcholine |
| TMA-DPH | 1-(4-trimethylammoniumphenyl)-6-phenyl-1,3,5-hexatriene |
| TRP | transient receptor potential |
| TRPV1 | transient receptor potential vanilloid type 1 |
References
- Young, A.; Buvanendran, A. Recent advances in multimodal analgesia. Anesthesiol. Clin. 2012, 30, 91–100. [Google Scholar] [CrossRef] [PubMed]
- Giménez-Milà, M.; Videla, S.; Navarro, M.A.; Faulí, A.; Ojeda, A.; Bogdanovich, A.; Moreno, L.A.; Hernández-Cera, C.; Busquets, C. Assessment of the feasibility of high-concentration capsaicin patches in the pain unit of a tertiary hospital for a population of mixed refractory peripheral neuropathic pain syndromes in non-diabetic patients. BMC Anesthesiol. 2014, 14, 120. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Couto, V.M.; Oliveira-Nascimento, L.; Cabeça, L.F.; Geraldes, D.C.; Costa, J.; Riske, K.A.; Franz-Montan, M.; Yokaychiya, F.; Franco, M.; Paula, E. Capsaicin-cyclodextrin complex enhances mepivacaine targeting and improves local anesthesia in inflamed tissues. Int. J. Mol. Sci. 2020, 21, 5741. [Google Scholar] [CrossRef] [PubMed]
- Fattori, V.; Hohmann, M.S.; Rossaneis, A.C.; Pinho-Ribeiro, F.A.; Verri, W.A. Capsaicin: Current understanding of its mechanisms and therapy of pain and other pre-clinical and clinical uses. Molecules 2016, 21, 844. [Google Scholar] [CrossRef]
- Juárez-Contreras, R.; Méndez-Reséndiz, K.A.; Rosenbaum, T.; González-Ramírez, R.; Morales-Lázaro, S.L. TRPV1 channel: A noxious signal transducer that affects mitochondrial function. Int. J. Mol. Sci. 2020, 21, 8882. [Google Scholar] [CrossRef]
- Sharma, S.K.; Vij, A.S.; Sharma, M. Mechanisms and clinical uses of capsaicin. Eur. J. Pharmacol. 2013, 720, 55–62. [Google Scholar] [CrossRef]
- Lundbæk, J.A.; Birn, P.; Tape, S.E.; Toombes, G.E.; Søgaard, R.; Koeppe, R.E., II; Gruner, S.M.; Hansen, A.J.; Andersen, O.S. Capsaicin regulates voltage-dependent sodium channels by altering lipid bilayer elasticity. Mol. Pharmacol. 2005, 68, 680–689. [Google Scholar] [CrossRef]
- Tsuchiya, H. Membrane interactions of phytochemicals as their molecular mechanism applicable to the discovery of drug leads from plants. Molecules 2015, 20, 18923–18966. [Google Scholar] [CrossRef]
- Neupane, S.; Cordoyiannis, G.; Renner, F.U.; Losada-Pérez, P. Real-time monitoring of interactions between solid-supported lipid vesicle layers and short- and medium-chain length alcohols: Ethanol and 1-pentanol. Biomimetics 2019, 4, 8. [Google Scholar] [CrossRef]
- Lundbæk, J.A.; Koeppe, R.E., II; Andersen, O.S. Amphiphile regulation of ion channel function by changes in the bilayer spring constant. Proc. Natl. Acad. Sci. USA 2010, 107, 15427–15430. [Google Scholar] [CrossRef]
- Lichtenberger, L.M.; Zhou, Y.; Jayaraman, V.; Doyen, J.R.; O’Neil, R.G.; Dial, E.J.; Volk, D.E.; Gorenstein, D.G.; Boggara, M.B.; Krishnamoorti, R. Insight into NSAID-induced membrane alterations, pathogenesis and therapeutics: Characterization of interaction of NSAIDs with phosphatidylcholine. Biochim. Biophys. Acta 2012, 1821, 994–1002. [Google Scholar] [CrossRef] [PubMed]
- Græsbøll, K.; Sasse-Middelhoff, H.; Heimburg, T. The thermodynamics of general and local anesthesia. Biophys. J. 2014, 106, 2143–2156. [Google Scholar] [CrossRef]
- Tsuchiya, H.; Mizogami, M. Interaction of drugs with lipid raft membrane domains as a possible target. Drug Target Insights 2020, 14, 34–47. [Google Scholar] [CrossRef] [PubMed]
- Startek, J.B.; Boonen, B.; Talavera, K.; Meseguer, V. TRP channels as sensors of chemically-induced changes in cell membrane mechanical properties. Int. J. Mol. Sci. 2019, 20, 371. [Google Scholar] [CrossRef] [PubMed]
- Startek, J.B.; Boonen, B.; López-Requena, A.; Talavera, A.; Alpizar, Y.A.; Ghosh, D.; Van Ranst, N.; Nilius, B.; Voets, T.; Talavera, K. Mouse TRPA1 function and membrane localization are modulated by direct interactions with cholesterol. Elife 2019, 8, e46084. [Google Scholar] [CrossRef] [PubMed]
- Hanson, S.M.; Newstead, S.; Swartz, K.J.; Sansom, M.S. Capsaicin interaction with TRPV1 channels in a lipid bilayer: Molecular dynamics simulation. Biophys. J. 2015, 108, 1425–1434. [Google Scholar] [CrossRef] [PubMed]
- Ciardo, M.G.; Ferrer-Montiel, A. Lipids as central modulators of sensory TRP channels. Biochim. Biophys. Acta Biomembr. 2017, 1859, 1615–1628. [Google Scholar] [CrossRef]
- Aranda, F.J.; Villalaín, J.; Gómez-Fernández, J.C. Capsaicin affects the structure and phase organization of phospholipid membranes. Biochim. Biophys. Acta 1995, 1234, 225–234. [Google Scholar] [CrossRef]
- Tsuchiya, H. Biphasic membrane effects of capsaicin, an active component in Capsicum species. J. Ethnopharmacol. 2001, 75, 295–299, Erratum in J. Ethnopharmacol. 2001, 76, 313. [Google Scholar] [CrossRef]
- Torrecillas, A.; Schneider, M.; Fernández-Martínez, A.M.; Ausili, A.; de Godos, A.M.; Corbalán-García, S.; Gómez-Fernández, J.C. Capsaicin fluidifies the membrane and localizes itself near the lipid-water interface. ACS Chem. Neurosci. 2015, 6, 1741–1750. [Google Scholar] [CrossRef]
- Sharma, N.; Phan, H.T.; Yoda, T.; Shimokawa, N.; Vestergaard, M.C.; Takagi, M. Effects of capsaicin on biomimetic membranes. Biomimetics 2019, 4, 17. [Google Scholar] [CrossRef] [PubMed]
- Dickenson, A.H.; Dray, A. Selective antagonism of capsaicin by capsazepine: Evidence for a spinal receptor site in capsaicin-induced antinociception. Br. J. Pharmacol. 1991, 104, 1045–1049. [Google Scholar] [CrossRef] [PubMed]
- Bevan, S.; Hothi, S.; Hughes, G.; James, I.F.; Rang, H.P.; Shah, K.; Walpole, C.S.; Yeats, J.C. Capsazepine: A competitive antagonist of the sensory neurone excitant capsaicin. Br. J. Pharmacol. 1992, 107, 544–552. [Google Scholar] [CrossRef] [PubMed]
- Perkins, M.N.; Campbell, E.A. Capsazepine reversal of the antinociceptive action of capsaicin in vivo. Br. J. Pharmacol. 1992, 107, 329–333. [Google Scholar] [CrossRef] [PubMed]
- Phillips, E.; Reeve, A.; Bevan, S.; McIntyre, P. Identification of species-specific determinants of the action of the antagonist capsazepine and the agonist PPAHV on TRPV1. J. Biol. Chem. 2004, 279, 17165–17172. [Google Scholar] [CrossRef]
- Brandt, M.R.; Beyer, C.E.; Stahl, S.M. TRPV1 antagonists and chronic pain: Beyond thermal perception. Pharmaceuticals 2012, 5, 114–132. [Google Scholar] [CrossRef]
- Lambert, D.G. Drugs and receptors. Anesth. Crit. Care Pain 2004, 6, 181–184. [Google Scholar] [CrossRef]
- Chaiyasit, K.; Khovidhunkit, W.; Wittayalertpanya, S. Pharmacokinetic and the effect of capsaicin in Capsicum frutescens on decreasing plasma glucose level. J. Med. Assoc. Thai. 2009, 92, 108–113. [Google Scholar]
- Suresh, D.; Srinivasan, K. Tissue distribution & elimination of capsaicin, piperine & curcumin following oral intake in rats. Indian J. Med. Res. 2010, 131, 682–691. [Google Scholar]
- Swain, J.; Kumar Mishra, A. Location, partitioning behavior, and interaction of capsaicin with lipid bilayer membrane: Study using its intrinsic fluorescence. J. Phys. Chem. B 2015, 119, 12086–12093. [Google Scholar] [CrossRef]
- M’Baye, G.; Mély, Y.; Duportail, G.; Klymchenko, A.S. Liquid ordered and gel phases of lipid bilayers: Fluorescent probes reveal close fluidity but different hydration. Biophys. J. 2008, 95, 217–225. [Google Scholar] [CrossRef] [PubMed]
- Ingólfsson, H.I.; Thakur, P.; Herold, K.F.; Hobart, E.A.; Ramsey, N.B.; Periole, X.; de Jong, D.H.; Zwama, M.; Yilmaz, D.; Hall, K.; et al. Phytochemicals perturb membranes and promiscuously alter protein function. ACS Chem. Biol. 2014, 9, 1788–1798. [Google Scholar] [CrossRef] [PubMed]
- Okamoto, Y.; Kishi, Y.; Ishigami, T.; Suga, K.; Umakoshi, H. Chiral selective adsorption of ibuprofen on a liposome membrane. J. Phys. Chem. B 2016, 120, 2790–2795. [Google Scholar] [CrossRef] [PubMed]
- Tsuchiya, H.; Mizogami, M. Discrimination of stereoisomers by their enantioselective interactions with chiral cholesterol membranes. Molecules 2017, 23, 49. [Google Scholar] [CrossRef]
- Do Canto, A.M.T.M.; Robalo, J.R.; Santos, P.D.; Carvalho, A.J.P.; Ramalho, J.P.P.; Loura, L.M.S. Diphenylhexatriene membrane probes DPH and TMA-DPH: A comparative molecular dynamics simulation study. Biochim. Biophys. Acta 2016, 1858, 2647–2661. [Google Scholar] [CrossRef]
- Yun, I.; Kang, J.S. Transbllayer effects of n-alkanols on the fluidity of phospholipid model membranes. Arch. Pharm. Res. 1992, 15, 152–161. [Google Scholar] [CrossRef]
- Prakash, U.N.; Srinivasan, K. Beneficial influence of dietary spices on the ultrastructure and fluidity of the intestinal brush border in rats. Br. J. Nutr. 2010, 104, 31–39. [Google Scholar] [CrossRef]
- Liu, M.; Huang, W.; Wu, D.; Priestley, J.V. TRPV1, but not P2X3, requires cholesterol for its function and membrane expression in rat nociceptors. Eur. J. Neurosci. 2006, 24, 1–6. [Google Scholar] [CrossRef]
- Gouda, A.; Sakr, O.S.; Nasr, M.; Sammour, O. Ethanol injection technique for liposomes formulation: An insight into development, influencing factors, challenges and applications. J. Drug Deliv. Sci. Technol. 2021, 61, 102174. [Google Scholar] [CrossRef]
- Okimoto, Y.; Watanabe, A.; Niki, E.; Yamashita, T.; Noguchi, N. A novel fluorescent probe diphenyl-1-pyrenylphosphine to follow lipid peroxidation in cell membranes. FEBS Lett. 2000, 474, 137–140. [Google Scholar] [CrossRef]
- Shaker, S.; Gardouh, A.R.; Ghorab, M.M. Factors affecting liposomes particle size prepared by ethanol injection method. Res. Pharm. Sci. 2017, 12, 346–352. [Google Scholar] [CrossRef] [PubMed]
- Ushijima, H.; Tanaka, K.; Takeda, M.; Katsu, T.; Mima, S.; Mizushima, T. Geranylgeranylacetone protects membranes against nonsteroidal anti-inflammatory drugs. Mol. Pharmacol. 2005, 68, 1156–1161. [Google Scholar] [CrossRef] [PubMed]
- Pubplus.Org—A Pubmed Search Engine (the University of British Columbia, Vancouver, Canada). Science Gateway—Cell Biology Protocols. Available online: https://www.sciencegateway.org/protocols/cellbio/drug/hcic50.htm (accessed on 7 October 2021).
- Ishikawa, N.; Ichikawa, T.; Tsuru, H.; Shigei, T. An extension of pA principle to the potentiation of drug effects, and its application to the biological assay of some anticholinesterases and cardenolides. Jpn. J. Pharmacol. 1980, 30, 49–58. [Google Scholar] [CrossRef] [PubMed]


| Relative DPH Polarization Change (%) | ||||
|---|---|---|---|---|
| Concentration (μM) | Capsaicin | Capsazepine | ||
| DPPC Membrane | Neuro-Mimetic Membrane | DPPC Membrane | Neuro-Mimetic Membrane | |
| 50 | −2.4 ± 0.5 ** | −4.1 ± 0.0 ** | 2.6 ± 0.1 ** | 1.8 ± 0.1 ** |
| 100 | −8.5 ± 0.4 ** | −7.8 ± 0.0 ** | 4.5 ± 0.1 ** | 3.2 ± 0.1 ** |
| 200 | −20.0 ± 0.2 ** | −8.1 ± 0.0 ** | 17.9 ± 0.1 ** | 5.7 ± 0.1 ** |
| 250 | −25.4 ± 0.5 ** | 5.5 ± 0.1 ** | 46.7 ± 0.3 ** | 9.7 ± 0.2 ** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mizogami, M.; Tsuchiya, H. Membrane Interactivity of Capsaicin Antagonized by Capsazepine. Int. J. Mol. Sci. 2022, 23, 3971. https://doi.org/10.3390/ijms23073971
Mizogami M, Tsuchiya H. Membrane Interactivity of Capsaicin Antagonized by Capsazepine. International Journal of Molecular Sciences. 2022; 23(7):3971. https://doi.org/10.3390/ijms23073971
Chicago/Turabian StyleMizogami, Maki, and Hironori Tsuchiya. 2022. "Membrane Interactivity of Capsaicin Antagonized by Capsazepine" International Journal of Molecular Sciences 23, no. 7: 3971. https://doi.org/10.3390/ijms23073971
APA StyleMizogami, M., & Tsuchiya, H. (2022). Membrane Interactivity of Capsaicin Antagonized by Capsazepine. International Journal of Molecular Sciences, 23(7), 3971. https://doi.org/10.3390/ijms23073971





