Abstract
Vascular remodeling is a typical feature of vascular diseases, such as atherosclerosis, aneurysms or restenosis. Excessive inflammation is a key mechanism underlying vascular remodeling via the modulation of vascular fibrosis, phenotype and function. Recent evidence suggests that not only augmented inflammation but unresolved inflammation might also contribute to different aspects of vascular diseases. Resolution of inflammation is mediated by a family of specialized pro-resolving mediators (SPMs) that limit immune cell infiltration and initiate tissue repair mechanisms. SPMs (lipoxins, resolvins, protectins, maresins) are generated from essential polyunsaturated fatty acids. Synthases and receptors for SPMs were initially described in immune cells, but they are also present in endothelial cells (ECs) and vascular smooth muscle cells (VSMCs), where they regulate processes important for vascular physiology, such as EC activation and VSMC phenotype. Evidence from genetic models targeting SPM pathways and pharmacological supplementation with SPMs have demonstrated that these mediators may play a protective role against the development of vascular remodeling in atherosclerosis, aneurysms and restenosis. This review focuses on the latest advances in understanding the role of SPMs in vascular cells and their therapeutic effects in the vascular remodeling associated with different cardiovascular diseases.
1. Introduction
Cardiovascular diseases are the leading cause of death worldwide, resulting in around 18 million deaths per year (WHO, 2020).
Endothelial dysfunction is a key early step in the development of several cardiovascular pathologies, including atherosclerosis, coronary artery disease and hypertension among others [1,2,3]. Although the main functional feature of endothelial dysfunction is the impairment of endothelium-dependent vasodilation and vascular hypercontractility, endothelial dysfunction is also characterized by the overexpression of proinflammatory, proliferative and procoagulant molecules that promote vascular remodeling, which, ultimately, affects vessel wall function [4]. Both endothelial dysfunction and vascular remodeling are key events in cardiovascular diseases; therefore, a complete understanding of the underlying mechanisms is fundamental.
Inflammation plays a central role in the pathogenesis of cardiovascular diseases, such as atherosclerosis, aortic aneurysm, balloon angioplasty or intravascular stenting [5,6,7,8,9]. After a vascular insult (mechanical, hemodynamic or metabolic), activated endothelial cells (ECs) promote the recruitment and infiltration of inflammatory circulating cells, including leukocytes, monocytes and T-lymphocytes to the intima. Both inflammatory cells and activated ECs release inflammatory cytokines, chemokines, proliferative growth factors and reactive oxygen species (ROS) that activate vascular smooth muscle cell (VMSC) proliferation and migration. Moreover, this inflammatory milieu promotes the synthesis and accumulation of extracellular matrix (ECM) by activated VMSCs, resident fibroblasts and infiltrated macrophages, which also contributes to vascular remodeling [10]. Termination of inflammation, known as resolution of inflammation, is a critical process in the restoration of tissue homeostasis [11]. Anti-inflammation is not equivalent to resolution. While anti-inflammation limits the actions of proinflammatory mediators, resolution activates specific mechanisms to return to homeostasis. Resolution is mediated by a family of specialized pro-resolving mediators (SPMs) that limit immune cell infiltration and initiate tissue repair mechanisms [12]. Therefore, failure to resolve inflammation will provoke prolonged inflammation and profound changes in the affected tissues. In this regard, increasing evidence indicates that lack of resolution might be a major cause of the pathophysiology of commonly occurring vascular diseases, including atherosclerosis, aortic aneurysm and neointimal hyperplasia [13]. Therefore, addressing specific biochemical and cellular mechanisms involved in the resolution of inflammation at the vascular level would provide a framework for investigating resolution-based pharmacology and disease mechanisms. This review summarizes current knowledge of SPM actions in vascular cells and their role in vascular remodeling.
2. Vascular Remodeling
Vascular remodeling refers to changes in vascular structure to maintain adequate blood flow to the tissues [14]. Usually, vascular remodeling is a response to hemodynamic changes, such as pregnancy or ageing. However, vascular remodeling can become maladaptative, as in atherosclerosis, restenosis, aneurysm, hypertension or obesity. Underlying mechanisms involved in vascular remodeling include alterations in phenotype, migratory capacity or death of VSMCs, as well as changes in the synthesis, reorganisation or degradation of ECM proteins [6,15].
Vascular remodeling may involve an increase (outward), a decrease (inward) or no change (compensated) in vessel size. It can also be classified as hypertrophic, hypotrophic or eutrophic when associated with an increase, a decrease or no change in vessel wall material, respectively [16,17] (Figure 1). Hypertrophic remodeling is observed in large arteries with aging and hypertension [18,19], atherosclerosis and restenosis and predominates in secondary hypertension [20]. This type of remodeling is typically characterized by an increased cross-sectional area and/or media thickness due to increased proliferation and/or migration of VSMCs [16]. Hypotrophic remodeling has been found in the small arteries of some animal models of hypertension [21,22] and is due to apoptosis or a rearrangement of the material of the vascular wall [23]. Finally, eutrophic remodeling is observed in small arteries of patients with hypertension and in animal models of hypertension, diabetes or obesity [18,19]. A combination of inward vascular wall growth and apoptosis in the peripheral area or prolonged vasoconstriction are the main mechanisms described for this type of remodeling [18]. Likewise, outward remodeling occurs in aneurysms, obesity, in large arteries during hypertension and in uterine arteries during pregnancy, while inward remodeling can be observed in obesity, atherosclerosis, restenosis or resistance arteries in hypertension [19,24] (Figure 1).
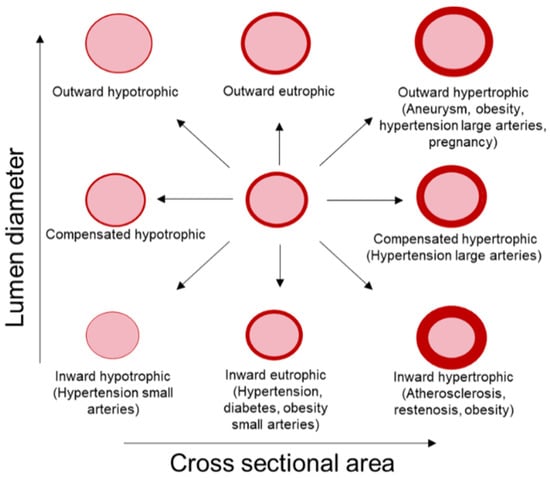
Figure 1.
Types of vascular remodeling. Vascular remodeling includes changes in lumen diameter and/or vessel cross-sectional area (CSA). Remodeling can be inward (smaller lumen diameter), outward (greater lumen diameter) or compensated (unaltered lumen diameter). According to changes in vessel CSA, remodeling can be classified as eutrophic (unaltered CSA), hypotrophic (decreased CSA) or hypertrophic (augmented CSA). Modified from [16].
Underlying mechanisms involved in vascular remodeling include hemodynamic, metabolic and inflammatory factors, though it is not the aim of this study to review this aspect in detail. Although vascular remodeling observed in atherosclerosis, aneurysms and restenosis is clearly different, common mechanisms include as activation of the endothelium, phenotypical changes in VSMCs, alteration in ECM deposition and infiltration of immune cells. In general, in response to a variety of stimuli, including ROS, inflammatory cytokines, LDL accumulation, mechanical forces and catecholamines, ECs express chemokines, selectins and adhesion molecules that facilitate the adhesion, rolling and transmigration of immune cells, such as macrophages and T-lymphocytes [7,9,25]. In this context, ECs can also secrete proinflammatory mediators, such as IL-6, IL1β or TNF-α, and thus contribute to the proinflammatory microenvironment in the vascular wall. Interactions between ECM and vascular cells are crucial for normal vessel function. Inflammation or alteration in ECM content affects the plasticity of VSMCs by changing their quiescent phenotype to a pathological (synthetic, osteogenic, macrophage or senescent) phenotype [26]. Both VSMC phenotype switching and macrophage infiltration induce the aberrant deposition of ECM that perpetuates the cycle. Interestingly, not only vascular cells contribute to vascular inflammation; perivascular adipose tissue (PVAT) can release different factors, such as interleukins, cytokines, ROS or angiotensin II (Ang II), which impact vascular structure. In fact, in atherosclerosis or aneurysms, dysregulated PVAT contributes to the infiltration of immune cells and to the maintenance of vascular inflammation [27,28,29]. Therefore, decreasing vascular inflammation might have beneficial effects in vascular remodeling in different cardiovascular pathologies.
3. Specialized Pro-Resolving Lipid Mediators (SPMs)
Transition from inflammation to resolution is marked by a temporal “lipid mediator class switch”. The early phase of an acute inflammatory response is characterized by biosynthesis of pro-inflammatory mediators, such as leukotriene B4 (LTB4), which is a potent chemoattractant for neutrophils [30,31], or prostaglandin E2 (PGE2), which increases vascular permeability, and both are key mediators of vascular remodeling in different cardiovascular diseases [32,33,34,35]. These proinflammatory mediators reach a peak at approximately 4 h post injury. Subsequently, they are replaced by SPMs, which limit further polymorphonuclear cell (PMN) infiltration and initiate resolution [12,36,37] (Figure 2). These potent bioactive mediators were first identified by lipidomic analysis in self-resolving inflammatory exudates in mice [38].
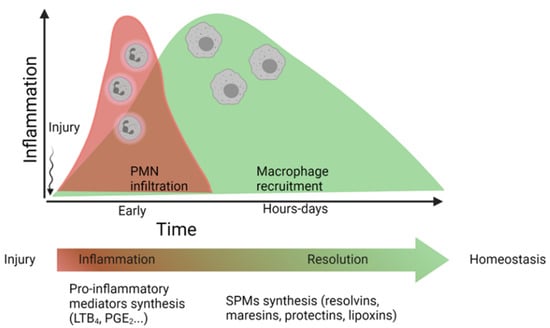
Figure 2.
Simplified timeline of the “lipid mediator class switch”. During the first hours after injury, there is an increase in the production of pro-inflammatory mediators (like leukotriene B4, (LTB4), which act as polymorphonuclear cell (PMN) chemoattractants, as well as factors that increase vascular permeability (i.e., prostaglandin E2, PGE2). Subsequently, these inflammatory mediators will be replaced by specialized pro-resolving lipid mediators (SPMs) that terminate the inflammatory process and restore tissue homeostasis. Modified from [11].
SPMs include four structurally unique different families: lipoxins, resolvins, protectins and maresins. The biosynthesis and vascular actions of these families are overviewed herein.
3.1. Biosynthesis of SPMs
SPMs are generated from different essential omega-6 and omega-3 polyunsaturated fatty acids (PUFAs): arachidonic acid (AA), eicosapentaenoic acid (EPA), docosahexaenoic acid (DHA) and docosapentaenoic (n-3DPA) acid.
Lipoxins were the first SPM family to be characterized with a dual profile: anti-inflammatory and pro-resolutive. In humans, they are biosynthesized from omega-6 PUFA AA and oxygenated via 15-lipoxygenase (LOX), resulting in 15-hydroxyeicosatetraenoic acid (15S-HpETE), which is subsequently rapidly converted via 5-LOX in neutrophils into two different regioisomers: lipoxin A4 (LXA4) and LXB4 [39] (Figure 3). Alternatively, lipoxins can also be biosynthesized in the leukocyte:platelet interaction, where LTA4 is converted via 12-LOX into lipoxins [39].
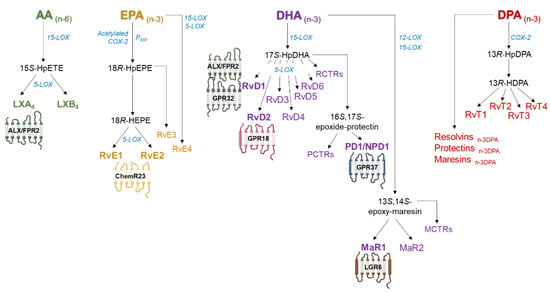
Figure 3.
Simplified scheme of the synthesis of specialized pro-resolvin lipid mediators (SPMs) from n-6 and n-3 polyunsaturated fatty acids and the main receptors involved in SPM actions. AA: arachidonic acid, EPA: eicosapentaenoic acid, DHA: docosahexaenoic acid, DPA: docosapentaenoic acid. LX: lipoxin, Rv: resolvin, PD/NPD: protectin/neuroprotectin, MaR: maresin, RvT: 13-series resolvins. GPR: G protein-coupled receptors, LGR6: leucine-rich repeat containing GPR 6, ChemR23: chemerin receptor 23, MCTR: maresin conjugates in tissue regeneration, RCTR: resolvin conjugates in tissue regeneration, PCTR: protectin conjugates in tissue regeneration.
The rest of the SPM families are derived from omega-3 PUFA DHA, EPA and DPA. Resolvins are divided into two series depending on the PUFA from which they are biosynthesized. E-series resolvins are biosynthesized from EPA via acetylated cyclooxygenase-2 (COX-2) or cytochrome P450, which synthesizes an 18-hydroperoxide intermediate, 18(R)-HpEPE, subsequently converted into 18R-hydroxyeicosapentaenoic acid (18R-HEPE), which is also a bioactive metabolite. This compound will be finally transformed via 5-LOX to the members resolvin E1 (RvE1) or E2 (RvE2) through leukocyte–endothelial interactions [11]. The 18(R)-HpEPE intermediate is also the precursor to RvE3, which does not require 5-LOX for its conversion (Figure 3) [40]. A new E-series resolvin member, termed RvE4, has been recently discovered. This novel bioactive molecule is biosynthesized in physiological hypoxia by human neutrophils and macrophages via 15- or 5-LOX [40].
DHA is the precursor for a 17-hydroperoxide product, 17S-HpDHA, that is subsequently converted to resolvins D1–D6 in the presence of 5-LOX by human PMNs and macrophages (Figure 3). Specifically, RvD1 and RvD2, the main members of this family, are biosynthesized from a 7S,8S epoxide which is then hydrolyzed to produce RvD1 or D2 [11]. Apart from being the precursor of D-series resolvins, 17S-HpDHA intermediate is also a precursor to 16S,17S-expoxide-protectin, which is transformed to protectin D1 (PD1) by neutrophils, macrophages, eosinophils and T-cells. When produced by neural cells and retinal-pigmented epithelial cells, this mediator is termed neuroprotectin D1 (NPD1/PD1) (Figure 3) [41]. Maresins are also biosynthesized from DHA, but via 12-LOX by macrophages. Subsequently, a 13S,14S-epoxide intermediate (13,14-epoxy maresin) is enzymatically converted to maresin 1 and 2 (MaR1, MaR2) (Figure 3) [41].
Aspirin acetylation of COX-2 leads to 15R-HETE, 18R-HEPE and 17R-HDHA, intermediates of the AA, EPA and DHA pathways respectively, which produce 17R epimers coined as aspirin-triggered (AT) lipoxins, AT resolvins and AT protectins [11].
n-3 DPA is less well studied compared to EPA and DHA but is also a substrate and precursor for three families of SPMs: resolvinsn-3 DPA, protectinsn-3 DPA and maresinsn-3 DPA, with potent pro-resolving effects in human physiology [41,42]. Other studies have shown that during neutrophil–endothelial cell interactions, 13-series resolvins (RvTs) are biosynthesized from n-3 DPA via COX-2 S-nitrosylation [43] (Figure 3).
Along with the SPMs mentioned above, three families of sulphido-conjugated mediators and their biosynthetic pathways have been identified, named maresin conjugates in tissue regeneration (MCTR), protectin conjugates in tissue regeneration (PCTR) and resolvin conjugates in tissue regeneration (RTCR). These SPMs are specifically relevant in tissue regeneration and repair [44]. DHA is the common precursor of these three new families, 15-LOX being the initiating enzyme in the RCTR and PCTR biosynthetic pathways and 14-LOX the initiating enzyme in MCTR biosynthesis [44].
Biosynthesis and transformation into the final lipid mediator can take place within a single cell (e.g., macrophages, PMNs) or during cell–cell interactions, such as leukocyte–endothelium, leukocyte–epithelium or PMN–macrophage interactions. For instance, the intermediate 18-HEPE is generated in ECs and subsequently transformed by leukocytes via 5-LOX to generate RvE1 [38]. MaR1 is produced by circulating neutrophil–platelet aggregates via DHA conversion into 13S, 14S-MaR by the platelet 12-LOX [45]. LXs are generated by PMNs from 15-HETE donated by lung, oral and gastrointestinal epithelial cells [46].
3.2. Receptors for SPMs
SPMs produce their biological actions through binding to G protein-coupled transmembrane superfamily receptors (GPCR) (Figure 3). So far, seven receptors for SPMs have been identified: ALX–FPR2 for lipoxin A4 and RvD1; DRV1/GPR32 for RvD1; DRV2/GPR18 for RvD2; ERV1/ChemR23 mainly for RvE1 but also for RvE2 [5,47]; GPR37, the potential receptor for NPD1/PD1 [48]; and LGR6, which binds MaR1 [49]. Finally, it has been reported that GPR101 mediates the leukocyte-directed actions of RvD5n-3DPA [50]. In addition, the DRV1/GPR32 receptor is also activated by other D-series resolvin members, such as RvD3 and RvD5, and AT resolvins [51,52]. Moreover, RvE1 and E2 and MaR1 can bind the LTB4 receptor 1 (BLT1) with lower affinity, inducing anti-inflammatory responses [5,53,54,55,56].
SPM receptors are expressed in different cell types, leading to tissue selectivity (Figure 4 and Figure 5). The GPR32 receptor is expressed in human PMNs, macrophages, T-cells, VSMCs and ECs. ALX–FPR2 is expressed in immune and vascular cells and also in adipocytes and bone marrow cells [54]. GPR18 has been found mainly in immune cells but also in isolated arteries [57] and in EC [58]. ChemR23 is expressed in NK cells, dendritic cells and macrophages [53,59], murine cardiomyocytes [60], human epithelial cells [36] and ECs and VSMCs [61,62,63]. In addition to PMNs and macrophages, BLT1 is also expressed in eosinophils, differentiated T-cells and osteoclasts [64]. GPR37 is expressed in macrophages [48].
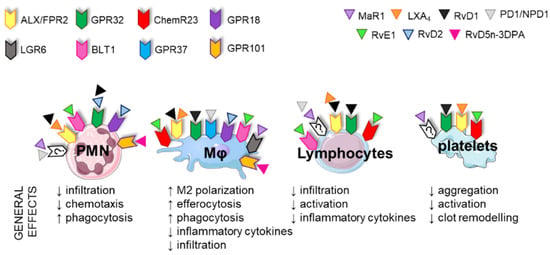
Figure 4.
Main receptors for specialized pro-resolving lipid mediators (SPMs) in immune cells and platelets. The key effects of SPMs in immune cells are to decrease inflammation, chemotaxis and infiltration and increase phagocytic activity. SPMs also affect platelet function, decreasing aggregation, activation and clot remodeling. PMNs: polymorphonuclear cells, MΦ: macrophage, LX: lipoxin, Rv: resolvin, MaR: maresin.
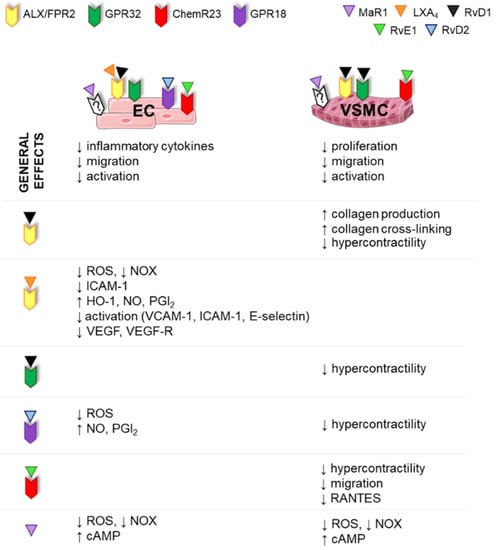
Figure 5.
SPM receptors in endothelial cells (ECs) and vascular smooth muscle cells (VSMCs) and key effects of specialized pro-resolving lipid mediators (SPMs) in vascular cells. In general, SPMs decrease activation, migration and inflammatory cytokine release and reactive oxygen species (ROS) production by ECs and VSMCs and increase collagen production by VSMCs. In addition, SPMs act on vascular function decreasing hypercontractility. LX: lipoxin, Rv: resolvin, MaR: maresin, NOX: NADPH oxidase, ICAM-1: intercellular adhesion molecule 1, VCAM-1: vascular cell adhesion molecule, HO-1: hemooxygenase 1, NO: nitric oxide, PGI2: prostacyclin, VEGF: vascular endothelial grow factor.
3.3. Immune Functions of SPMs
SPMs have dual actions, as they possess broad pro-resolving and anti-inflammatory actions in immune cells at the transcriptional and translational levels. In general, these mediators play pivotal roles in different immune responses, including augmented macrophage phagocytosis and efferocytosis, promotion of M2 or “resolutive” macrophage phenotypes, limitation of further leukocyte infiltration and counter-regulation of pro-inflammatory chemical mediators [65,66] (Figure 4). These events will finally lead to resolution of inflammation, reduced organ fibrosis, enhanced wound healing and restored homeostasis. As has already been mentioned, immune cells express several SPM receptors, making the effects of specific SPMs very complex and sometimes overlapping (Figure 4). For example, GPR18 activation reduces infiltration of PMNs, decreases inflammation and increases M2 polarization, efferocytosis and phagocytosis [67]. RvE1, through ChemR23, reduces levels of proinflammatory cytokines and immune cell infiltration and stimulates phagocytosis/efferocytosis in NK cells, dendritic cells and macrophages [53]. GPR37 is expressed in macrophages and its activation by NPD1 enhances macrophage phagocytic activity and resolution of inflammatory pain [48]. Moreover, exogenous SPMs have been found to reduce T-cell recruitment and infiltration into target organs and decrease activation and inflammatory cytokine production [68,69]. Interestingly, human platelets also express the SPM receptors GPR32, ALX–FPR2 and ChemR23, which modulate aggregation, clot remodeling and platelet–PMN interactions. Thus, in general, SPMs have beneficial antithrombotic properties, inhibit inflammatory responses induced by platelet-activating factor and avoid aggregation [70,71,72,73] (Figure 4). These findings suggest that, in principle, any clinical condition that is characterized by immune cell infiltration or altered platelet reactivity might benefit from the effects of SPMs.
3.4. Vascular Functions of SPMs
Although the effects of SPMs have been more extensively studied in immune cells, recent evidence demonstrates that vascular cells express SPM receptors, and a range of direct effects of SPMs have been found in the vasculature which ultimately lead to a reduction in their inflammatory state and restore their quiescent state (Figure 5).
3.4.1. SPM Effects in ECs
The endothelium is directly involved in the passage of macromolecules and immune cells and thereby plays a central role in the early inflammatory response. In addition, ECs regulate blood flow, control leukocyte and platelet interaction with the vessel wall and modulate vascular tone by releasing vasodilator and vasoconstrictor factors. Morphological or functional endothelial abnormalities lead to decreased vasodilation and proinflammatory and prothrombic states. Indeed, permanently activated ECs are characterized by expressing cell surface adhesion molecules, such as E-selectin or VCAM-1 (vascular cell adhesion molecule), and secretion of procoagulant molecules and chemokines, and these are found in different chronic inflammatory diseases, such as atherosclerosis and hypertension [74]. In general, it is accepted that endothelial cell dysfunction is a hallmark of a wide range of cardiovascular diseases [2].
Regarding the effects of SPMs in ECs, in vitro studies show that certain SPMs, such as LXA4, MaR1, RvE1, RvD1 and RvD2, attenuate the expression of adhesion molecules, decrease the release of proinflammatory cytokines, such as IL-12 (involved in leukocyte recruitment), and regulate leukocyte–endothelial interactions [13,75,76,77]. In addition, RvD2 enhances endothelial cell migration, but not proliferation, in a Rac-dependent manner [78] and stimulates the production of the vasodilators nitric oxide (NO) and prostacyclin (PGI2) [79] (Figure 5). Similarly, AT LXA4 directly increases plasma NO levels and decreases the number of leukocyte–endothelial interactions. Of note, evidence suggests that this NO production underlies some of the beneficial effects of aspirin in the management of cardiovascular diseases [80]. Lipoxins and AT LXs increase PGI2 production and block ROS generation in human ECs by downregulating NADPH oxidase [81,82]. In addition, lipoxins and their derivatives upregulate the expression of the stress-response protein heme oxygenase-1 in human ECs, suggesting a new mechanism for the anti-inflammatory effect of these mediators [83]. Lipoxins and AT LXs have further effects in ECs, such as downregulation of the endothelial activation markers VCAM-1, ICAM-1 and E-selectin [84,85]. Moreover, LXA4, 15-epi-LXA4 and other analogs limit endothelial migration and proliferation by inhibiting vascular endothelial growth factor (VEGF) and VEGF receptor expression, supporting a novel role for these mediators as angiogenesis modulators [86,87] (Figure 5). Other mechanisms responsible for the beneficial effects of SPMs on ECs are attenuation of NF-κB activation, upregulation of cAMP, which is involved in anti-inflammatory and anti-oxidant pathways [76], and activation of the GSK-3β–C/EBPβ axis, which ultimately leads to upregulation of Del-1, an endothelial cell-secreted anti-inflammatory protein [88].
3.4.2. SPM Effects in VSMCs
In response to vascular injury, VSMCs switch from a contractile to a synthetic phenotype and become more proliferative and chemotactic. In this sense, acute vessel injury is characterized by inflammation, cytokine production and VSMC proliferation and migration, which ultimately lead to neointima formation and reduction in lumen diameter. Treatment with certain SPMs, such as MaR1, RvD1, RvD2, 15-epi-LXA4 or RvE1, attenuated VSMC proliferation both in vitro and in vivo [89,90,91,92,93] and decreased migration, cytoskeletal changes, expression of adhesion molecules (e.g., VCAM-1, ICAM-1), ROS production and release of proinflammatory mediators in several animal models [76,90,92,94] (Figure 5). In addition, the expression of ALX–FPR2 seems to be related to collagen accumulation in VSMCs, as VSMCs derived from Ldlr−/− × FPR2−/− double-knockout mice exhibited decreased collagen production and increased collagenase pathways [95]. Therefore, in general, SPMs have the potential to regulate vascular remodeling in different conditions (Figure 5). These anti-proliferative and anti-inflammatory effects can be explained by downregulation of NF-κB or activation of cAMP–PKA pathways [13].
The above-mentioned effects of SPMs in vascular cells clearly affect vascular structure. However, vascular function can be also modulated by these molecules, and this has been particularly explored in the pulmonary vasculature. Thus, RvE1, RvD1 and RvD2 inhibited vasoconstrictor responses induced by U46619, a TP agonist, in human pulmonary arteries (HPA) and also in rat aorta [96]. Moreover, RvE1 and RvD1 attenuated pulmonary hypertension-induced hypercontractility and Ca2+ hypersensitivity in cultured HPA SMCs [61,97]. A recent study showed that RvE1 also suppresses vasoconstriction of rat pulmonary arteries and HPAs, probably via inhibition of Src family kinases [98]. On the other hand, the involvement of LXA4 in vascular function is controversial. Both vasodilator effects through NO production [99] and vasoconstriction and endothelial dysfunction via RhoA/Rhokinase and oxidative stress production have been described [100]. In this sense, it has been suggested that LXA4 could participate in the development of post-angioplasty complications, such as vasospasm, in patients treated with aspirin [101].
4. SPMs in Cardiovascular Diseases
Vascular remodeling is a typical feature of several cardiovascular diseases. Most of the studies analyzing the effect of SPM pathways in vascular remodeling have been performed in the context of atherosclerosis, aneurysms and neointima hyperplasia (Table 1).
4.1. SPMs in Atherosclerosis
Atherosclerosis is widely viewed as a chronic immunoinflammatory disease, affecting vascular and peripheral blood mononuclear cells, the major players contributing to the development of this disease [102,103]. However, emerging evidence suggests that advanced atherosclerosis could also be a result of deficient resolution of inflammation [104,105], although the mechanisms that prevent resolution of inflammation in atherosclerosis remain unclear. An imbalance between proinflammatory and anti-inflammatory mediators during atheroprogression has been found [106,107]. For example, Fredman et al. [107] showed that the RvD1/LTB4 ratio is significantly decreased in human vulnerable atherosclerotic plaques. SPMs are also reduced in plaques of high-fat diet-fed Ldlr−/− mice and the plasma of atherosclerotic patients [62,71]. Therefore, different studies have evaluated the potential anti-atherosclerotic effects of SPMs as novel approaches to current lipid lowering strategies.
In general, SPM administration promotes plaque stability by inducing a switch of macrophage phenotypes to M2-like phenotypes and by decreasing local inflammatory cytokines, ROS production and the activation of matrix metalloproteinases that break atherosclerotic plaque [108] (Table 1). For instance, exogenous administration of RvD1 to Ldlr−/− mice suppressed ROS and necrosis in murine lesions, enhanced efferocytosis and fibrous caps and decreased collagenase and metalloproteinases [107]. RvD2 and MaR1 delivery prevented atheroprogression in a model of apolipoprotein E-deficient (ApoE−/−) mice by polarizing macrophages to a reparative phenotype and stimulating collagen synthesis in VMSCs [106]. Similar results were described with RvE1, which displays protective effects in several atherosclerosis settings, even when administered on top of statins, by mechanisms that seem to be independent of cholesterol lowering and include the reduction of inflammatory cell infiltration and pro-inflammatory cytokine secretion [109,110], inhibition of vascular calcification of smooth muscle cells and the reduction of macrophage-derived foam cell formation [111,112]. In addition, AT LXA4 administration blocked atheroprogression in ApoE−/− mice via FPR2 receptors [91].
Genetic models of SPM pathways have provided important information on the protective effects of endogenous molecules in atherosclerosis progression. Thus, targeted deletion of the RvE1 receptor, ChemR23, is associated with atheroprogression and mediates RvE1 protective effects by modifying oxidized LDL uptake and phagocytosis in two independent hyperlipidemic murine models [113]. Interestingly, even though ALX–FPR2 expression has been identified in macrophages, endothelial cells and VMSCs in human atherosclerotic lesions [54], no consensus has yet been reached on the contribution of this receptor in different hyperlipidemic murine models. On the one hand, deletion of the murine homologue of human ALX–FPR2 decreased atherosclerosis development in Ldlr−/− × Fpr2−/− double-knockout mice by reducing macrophage infiltration [95]. On the other hand, Fpr2 deletion seems to promote a less stable plaque phenotype with decreased collagen content in VSMCs [95], suggesting that ALX–FPR2 signaling has a dual role in atherosclerosis development and plaque stability. In addition, other authors have shown that atherosclerotic lesions are enhanced in Fpr2 × ApoE double-knockout mice [114]. Moreover, administration of AT LXA4 was atheroprotective in ApoE−/− mice via the FPR2 receptor [91]. More recently, it has been found that human GPR32 expression in a Fpr2×ApoE double-knockout background is associated with decreased atherosclerotic lesions and necrotic core via reduced aortic inflammation [115].
4.2. SPMs in Aneurysm
Aortic aneurysms are defined as focused dilations 1.5-times greater than normal aortic size [116] and are characterized by adventitial and medial inflammatory cell infiltration, ECM degradation, VMSC apoptosis and oxidative stress that leads to vascular remodeling characterized by adventitial thickening and media degradation [8,117,118,119,120].
Although abdominal aortic aneurysm (AAA) has been classically associated with atherosclerosis [121], increasing evidence indicates that the developing mechanisms for both diseases are different [8,120]. It has been proposed that aneurysm formation starts with the infiltration of inflammatory cells, including macrophages, T- and B-lymphocytes and neutrophils, among others, into the adventitia layer which subsequently migrate towards media layer. In the media, activated macrophages secrete matrix metalloproteinases (MMPs) and cytokines that ultimately lead to ECM degradation and VSMC apoptosis, thereby causing aortic layer degradation, which leads to progressive aortic dilatation and, ultimately, rupture [8,120].
As in atherosclerosis, some evidence suggests that in AAA there might be an imbalance between proinflammatory mediators and SPMs. A study carried out in patients undergoing AAA surgery, where lipid mediators were evaluated in plasma obtained from the surgical area, revealed two different profiles. One group of patients presented a pro-inflammatory profile characterized by increased levels of leukotrienes and prostaglandins and their precursors, while another group displayed a pro-resolving profile with increased levels of RvE1 and RvE2 and the RvD1 and MaR1 precursors 17-HDHA and 14-HDHA, respectively. However, they did not investigate the correlation between lipid mediator profiles and AAA progression or patient recovery [122]. Another study evaluated human aortic aneurysm samples from patients undergoing elective open surgery and aortic samples from non-aneurysmatic organ donors. The authors found lower gene expression levels of ALX–FPR2, which is the receptor for LXA4 and RvD1, in the adventitial layer of the aneurysmal patients compared with healthy donors [123]. This prompted investigators to determine the consequences of deleting the FPR2 gene in an experimental model of AAA. They found that ApoE−/− mice lacking the Fpr2 receptor (ApoE−/−Fpr2−/− mice), exhibited an exaggerated aortic dilation after Ang II infusion compared with ApoE−/−Fpr2+/+ mice, with elastin disruption and MMP9 expression and a decrease in collagen deposition, accompanied by an increased infiltration of neutrophils and macrophages [123]. Similar results were observed in mice lacking the enzyme involved in LXA4 and RvD1 synthesis, 12/15-LOX [123], indicating a possible protective role of endogenous lipid mediators in AAA development.
Administration of different SPMs has been beneficial in several models of AAA. This is relevant, since currently there is no efficient pharmacological treatment for AAA disease. RvD1 and RvD2 inhibit AAA development in murine experimental models [124,125]. Specifically, in the model of AAA induced by Ang II administration in ApoE−/− mice, RvD2 treatment decreased AAA formation by reducing local pro-inflammatory molecules, including MCP-1, IL-6, IL-1β and RANTES, and MMP2 and MMP9 activity and increased anti-inflammatory cytokines, such as IL-10. This reduction in AAA formation was attributed to macrophage M2 polarization, as no changes in T-cell or neutrophil infiltration were observed [124]. Analogous results were described with RvD1 and RvD2 treatments in the AAA experimental model of local elastase perfusion [124]. More importantly, RvD2 administration after small AAAs had formed caused a reduction in later aortic enlargement [124], thus demonstrating its potential to slow AAA progression. More recently, the same group reported that in the same models of AAA, RvD1 administration decreased AAA formation by decreasing neutrophils and neutrophil extracellular traps release (NETosis) [125]. Of note, other SPMs also showed beneficial effects with respect to AAA formation. For example, in the experimental model of AAA using elastase infusion, MaR1 upregulated the macrophage-dependent efferocytosis of apoptotic VSMCs via LGR6 receptors [126]. Together, these results likely suggest common underlying mechanisms of SPMs to improve AAA homeostasis and integrity (Table 1).
4.3. SPMs in Hyperplasia
Vascular hyperplasia and restenosis are important side effects associated with endovascular interventional procedures, such as balloon angioplasty or intravascular stenting intended for revascularization, in which the endothelium is mechanically damaged. Neointimal hyperplasia is characterized by an uncontrolled proliferation of VSMCs and fibroblasts and an increase in ECM deposition in the intima layer that leads to hypertrophic inward remodeling of arteries and veins, with a thickened intima and narrowed lumen [127]. As in atherosclerosis and AAA, neointimal hyperplasia starts with infiltration of circulating inflammatory cells, including monocytes and T-lymphocytes [128], that release cytokines and chemokines that activate the differentiation of VSMCs into a proliferative phenotype and induce their migration towards the lumen, leading to vascular stenosis [129].
Evidence of the beneficial effects of SPM administration in this type of vascular remodeling have been provided in different experimental models [127] (Table 1). In balloon-injured rabbit arteries, RvD series decreased vascular remodeling by diminishing VSMC proliferation and leukocyte recruitment, probably due to a local increase in RvD1 receptor (FPR2 and GPR32) expression and endogenous biosynthesis of other SPMs [90], demonstrating the existence of positive feedforward mechanisms. Similarly, RvD2 and MaR1 decreased vascular hyperplasia and reduced VSMC proliferation and neutrophil and macrophage recruitment in the arterial wall in a mouse model of carotid artery ligation [89]. In the same experimental model, administration of AT-LXA4 also reduced the intima area and the intima/media ratio in wildtype mice but not in FPR2/ALX-deficient mice [130], demonstrating that these effects are due to SPM receptor signaling. Moreover, mice lacking ChemR23 presented increased intimal hyperplasia 28 days after ligation of the left common carotid artery compared with ChemR23+/+ mice [131]. Conversely, RvE1 administration inhibited vascular remodeling after wire-induced injury in mice femoral arteries by hindering VSMCs migration, neutrophil infiltration and T-cell trafficking and promoting macrophage polarization toward an M2-like phenotype [94]. Furthermore, not only systemic delivery of RvD1 prevented vascular damage but locally administered biodegradable gels also ameliorated vascular hyperplasia in a rat model of carotid angioplasty and in a rabbit carotid bypass model [92,93], suggesting that local, lesion-inherent effects are likely taking place in VSMC and immune-infiltrated cells. Moreover, intravenous injection of both RvD1 and PD1 improved vascular remodeling in the rat carotid artery balloon injury model through NF-κB pathway inhibition [132]. Interestingly, in a rat model of carotid angioplasty, oral administration of RvD1 ameliorated inflammation but not intimal hyperplasia, highlighting the importance of administration routes [133].

Table 1.
Summary of in vivo experimental approaches to test the effects of SPMs in vascular remodeling. The effects of exogenous SPM administration or genetic modification of SPM receptors in macrophages (MØs) and/or vascular smooth muscle cells (VSMCs) are shown. In general, SPM administration promotes beneficial effects in vascular remodeling, whereas deletion of SPM receptors aggravates vascular disease. AT: aspirin-triggered, oxLDL: oxidized low-density lipoprotein. hGPR32 × Fpr2−/− indicates overexpression of the human GPR32 in a Fpr2−/− mice. M2 indicates “resolutive” macrophage phenotype.
Table 1.
Summary of in vivo experimental approaches to test the effects of SPMs in vascular remodeling. The effects of exogenous SPM administration or genetic modification of SPM receptors in macrophages (MØs) and/or vascular smooth muscle cells (VSMCs) are shown. In general, SPM administration promotes beneficial effects in vascular remodeling, whereas deletion of SPM receptors aggravates vascular disease. AT: aspirin-triggered, oxLDL: oxidized low-density lipoprotein. hGPR32 × Fpr2−/− indicates overexpression of the human GPR32 in a Fpr2−/− mice. M2 indicates “resolutive” macrophage phenotype.
| Disease | Approach | Target Cell and Action | Main Effects | Ref. | ||
|---|---|---|---|---|---|---|
| SPM Admin. | Genetic Modification | |||||
| Atherosclerosis | RvD1 | - | MØ | ↑ efferocytosis | Promoted plaque stability, suppressed plaque progression | [107] |
| VSMCs | unaltered No. | |||||
| RvD2, MaR1 | - | MØ | polarization to M2 | Reduced atheroprogression and promoted plaque stability | [106] | |
| VSMCs | ↑ collagen synthesis, ↑ No. | |||||
| RvE1 | - | MØ | ↓ foam cell infiltration | Reduced atheroprogression | [109] [110] | |
| - | ChemR23−/− | MØ | ↓ phagocytosis, ↑ oxLDL uptake | Increased atherosclerotic plaque size and necrotic core formation | [113] | |
| VSMCs | ↓ collagen ↓ proliferation | |||||
| Frp2−/− | MØ | ↓ infiltration | Reduced atheroprogression Impaired plaque stability | [95] | ||
| VSMCs | ↓ collagen synthesis | |||||
| - | Frp2−/− | Leukocytes | ↑recruitment | Enhanced atheroprogression | [114] | |
| AT-LXA4 | - | MØ | ↓ infiltration | Reduced atheroprogression ↓ systemic inflammation | [91] | |
| - | hGPR32 × Fpr2−/− | MØ, neutrophils, monocytes | ↓ aortic infiltration | Reduced atheroprogression, necrotic core, aortic inflammation | [115] | |
| Aneurysms | - | Frp2−/− | MØ, neutrophils | ↑ aortic infiltration | ↑ aortic dilation, elastin disruption and ↓ collagen deposition | [123] |
| RvD1, RvD2 | - | MØ | polarization to M2, ↓ pro-inflammatory cytokines | Decreased AAA formation | [124] | |
| Neutrophils | ↓ infiltration, ↓ NETosis | [125] | ||||
| MaR1 | - | MØ | ↑ efferocytosis | Decreased AAA formation | [126] | |
| Hyperplasia | RvD1, RvD2, RvE1, MaR1, PD1 | - | MØ, neutrophils | ↓ infiltration, polarization to M2 | Decreased neointima formation | [89] [90] [92,93,94] [132] |
| VSMCs | ↓ proliferation, ↓ migration | |||||
| AT-LXA4 | - | VSMCs | ↓ migration | Decreased neointima formation | [130] | |
| - | ChemR23−/− | Peritoneal MØ | ↑ inflammatory cytokines | Increased intimal hyperplasia | [131] | |
| VSMCs | ↓ proliferation | |||||
5. Conclusions
Inflammation contributes to vascular damage in different cardiovascular diseases by activating ECs, inducing phenotypic switching of VSMCs and stimulating aberrant ECM production. This chronic inflammatory state may be caused by both an excess of proinflammatory mediators and/or by a defect or disbalance in the mechanisms of resolution, and this seems to occur in several vascular pathologies, including atherosclerosis, aneurysms and restenosis. Deletion of enzymes or receptors involved in SPM synthesis or signaling in mice has provided evidence of the beneficial effects of endogenous SPMs in vessel homeostasis, particularly in pathological situations. Moreover, exogenous administration of different SPMs improved vascular remodeling associated with disease. Notably, in general, beneficial effects are observed for different members of the SPM families, such as D or E resolvins, maresins and lipoxins, pointing to common underlying mechanisms that explain these positive effects of SPMs at the vascular level. In this sense, ECs and VSMCs express several SPM receptors that modulate fundamental processes of vascular biology, such as VSMC phenotype, the production of vasoprotective mediators and the regulation of inflammatory responses, although more research is needed to identify the molecular mechanisms involved in direct SPM actions in vascular cells. Moreover, there is no doubt that the beneficial effects of these molecules in vascular remodeling can be explained, at least in part, by effects in infiltrating immune cells. In any case, these results suggest that SPMs may offer a novel therapeutic strategy for the treatment of cardiovascular diseases associated with vascular remodeling by different mechanisms (Figure 6).
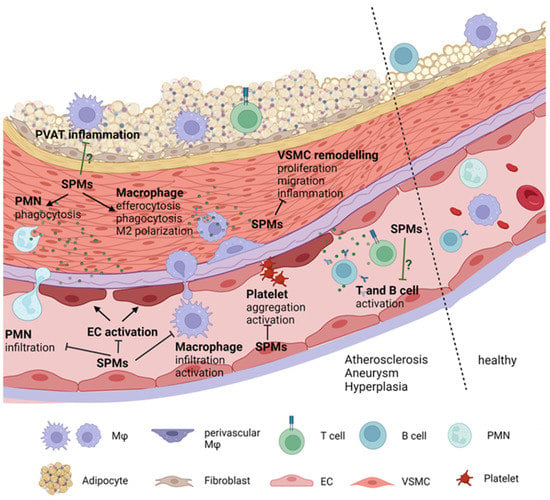
Figure 6.
Effects of SPMs in pathological vascular remodeling. Vascular remodeling in pathological conditions, such as atherosclerosis, aneurysm and hyperplasia includes activation of endothelial cells (ECs), phenotype switching of vascular smooth muscle cells (VSMCs), immune cell (polymorphonuclear cell (PMNs), macrophage and lymphocyte) infiltration and activation, and platelet aggregation. SPMs reduce EC activation and proliferation, and migration and inflammation in VSMCs. SPMs also reduce immune cell activation and infiltration, promote macrophages M2 phenotype polarization, facilitate macrophage and PMN efferocytosis and inhibit platelet activation and aggregation.
The relationship between SPMs and vascular remodeling at the clinical level has not been explored in depth, although some evidence points to impaired resolution of inflammation in some vascular pathologies. Some clinical trials using SPM precursors, such as EPA (JELIS and REDUCE-IT trials), showed cardiovascular risk reduction in patients with high triglyceride levels and high cardiovascular risk [134,135]. However, other studies found no improvement on cardiovascular events after treatment with a carboxylic acid formulation of EPA and DHA [136]. Future studies will confirm or dismiss the beneficial effects of SPMs in cardiovascular diseases and in vascular damage, either as pharmacological treatments or as predictive biomarkers of vascular disease.
Author Contributions
L.S.D.d.C., R.R.-D. and A.B.G.-R. contributed to the writing of the manuscript. M.S., A.M.B. and A.B.G.-R. contributed to the review of the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
Supported by Ministerio de Ciencia e Innovación and Fondo Europeo de Desarrollo Regional (FEDER)/FSE (SAF2016-80305P; PID2020-116498RB-I00), Comunidad de Madrid (CM) (AORTASANA B2017/BMD-3676) and CM-Universidad Autónoma de Madrid (SI1-PJI-2019-00321). LSDC was supported by a FPI-UAM fellowship and RRD by a Juan de la Cierva contract (IJCI-2017-31399). The study has received funding from the European Union’s Horizon 2020 research and innovation programme under the Marie Sklodowska-Curie grant agreement no. 954798.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Simionescu, M. Implications of early structural-functional changes in the endothelium for vascular disease. Arterioscler. Thromb. Vasc. Biol. 2007, 27, 266–274. [Google Scholar] [CrossRef] [PubMed]
- Godo, S.; Shimokawa, H. Endothelial functions. Arterioscler. Thromb. Vasc. Biol. 2017, 37, 108–114. [Google Scholar] [CrossRef] [PubMed]
- Harrison, D.G.; Coffman, T.M.; Wilcox, C.S. Pathophysiology of Hypertension: The Mosaic Theory and Beyond. Circ. Res. 2021, 128, 847–863. [Google Scholar] [CrossRef] [PubMed]
- Watson, T.; Goon, P.K.; Lip, G.Y. Endothelial progenitor cells, endothelial dysfunction, inflammation, and oxidative stress in hypertension. Antioxid. Redox Signal. 2008, 10, 1079–1088. [Google Scholar] [CrossRef]
- Kim, A.S.; Conte, M.S. Specialized pro-resolving lipid mediators in cardiovascular disease, diagnosis, and therapy. Adv. Drug Deliv. Rev. 2020, 159, 170–179. [Google Scholar] [CrossRef]
- Libby, P. Inflammation during the life cycle of the atherosclerotic plaque. Cardiovasc. Res. 2021, 117, 2525–2536. [Google Scholar] [CrossRef]
- Soehnlein, O.; Libby, P. Targeting inflammation in atherosclerosis—From experimental insights to the clinic. Nat. Rev. Drug Discov. 2021, 20, 589–610. [Google Scholar] [CrossRef]
- Yuan, Z.; Lu, Y.; Wei, J.; Wu, J.; Yang, J.; Cai, Z. Abdominal Aortic Aneurysm: Roles of Inflammatory Cells. Front. Immunol. 2021, 11, 609161. [Google Scholar] [CrossRef]
- Shimizu, K.; Mitchell, R.N.; Libby, P. Inflammation and cellular immune responses in abdominal aortic aneurysms. Arterioscler. Thromb. Vasc. Biol. 2006, 26, 987–994. [Google Scholar] [CrossRef]
- Whiteford, J.R.; De Rossi, G.; Woodfin, A. Mutually Supportive Mechanisms of Inflammation and Vascular Remodeling. Int. Rev. Cell Mol. Biol. 2016, 326, 201–278. [Google Scholar]
- Serhan, C.N. Pro-resolving lipid mediators are leads for resolution physiology. Nature 2014, 510, 92–101. [Google Scholar] [CrossRef] [PubMed]
- Levy, B.D.; Clish, C.B.; Schmidt, B.; Gronert, K.; Serhan, C.N. Lipid mediator class switching during acute inflammation: Signals in resolution. Nat. Immunol. 2001, 2, 612–619. [Google Scholar] [CrossRef] [PubMed]
- Conte, M.S.; Desai, T.A.; Wu, B.; Schaller, M.; Werlin, E. Pro-resolving lipid mediators in vascular disease. J. Clin. Investig. 2018, 128, 3727–3735. [Google Scholar] [CrossRef] [PubMed]
- Gibbons, G.H.; Dzau, V.J. The emerging concept of vascular remodeling. N. Engl. J. Med. 1994, 330, 1431–1438. [Google Scholar] [CrossRef]
- Gurung, R.; Choong, A.M.; Woo, C.C.; Foo, R.; Sorokin, V. Genetic and Epigenetic Mechanisms Underlying Vascular Smooth Muscle Cell Phenotypic Modulation in Abdominal Aortic Aneurysm. Int. J. Mol. Sci. 2020, 21, 6334. [Google Scholar] [CrossRef]
- Mulvany, M.J. Small artery remodeling in hypertension. Curr. Hypertens. Rep. 2002, 4, 49–55. [Google Scholar] [CrossRef]
- Van Varik, B.J.; Rennenberg, R.J.; Reutelingsperger, C.P.; Kroon, A.A.; de Leeuw, P.W.; Schurgers, L.J. Mechanisms of arterial remodeling: Lessons from genetic diseases. Front. Genet. 2012, 3, 290. [Google Scholar] [CrossRef]
- Schiffrin, E.L. Vascular remodeling in hypertension: Mechanisms and treatment. Hypertension 2012, 59, 367–374. [Google Scholar] [CrossRef]
- Briones, A.M.; Aras-López, R.; Alonso, M.J.; Salaices, M. Small artery remodeling in obesity and insulin resistance. Curr. Vasc. Pharmacol. 2014, 12, 427–437. [Google Scholar] [CrossRef]
- Mulvany, M.J. Small artery remodeling in hypertension: Causes, consequences and therapeutic implications. Med. Biol. Eng. Comput. 2008, 46, 461–467. [Google Scholar] [CrossRef]
- Nørrelund, H.; Christensen, K.L.; Samani, N.J.; Kimber, P.; Mulvany, M.J.; Korsgaard, N. Early narrowed afferent arteriole is a contributor to the development of hypertension. Hypertension 1994, 24, 301–308. [Google Scholar] [CrossRef] [PubMed]
- Briones, A.M.; Xavier, F.E.; Arribas, S.M.; González, M.C.; Rossoni, L.V.; Alonso, M.J.; Salaices, M. Alterations in structure and mechanics of resistance arteries from ouabain-induced hypertensive rats. Am. J. Physiol. Heart Circ. Physiol. 2006, 291, H193–H201. [Google Scholar] [CrossRef] [PubMed]
- Intengan, H.D.; Schiffrin, E.L. Vascular remodeling in hypertension: Roles of apoptosis, inflammation, and fibrosis. Hypertension 2001, 38 (3 Pt 2), 581–587. [Google Scholar] [CrossRef]
- Dorrance, A.M.; Matin, N.; Pires, P.W. The effects of obesity on the cerebral vasculature. Curr. Vasc. Pharmacol. 2014, 12, 462–472. [Google Scholar] [CrossRef]
- Cahill, P.A.; Redmond, E.M. Vascular endothelium—Gatekeeper of vessel health. Atherosclerosis 2016, 248, 97–109. [Google Scholar] [CrossRef] [PubMed]
- Sorokin, V.; Vickneson, K.; Kofidis, T.; Woo, C.C.; Lin, X.Y.; Foo, R.; Shanahan, C.M. Role of Vascular Smooth Muscle Cell Plasticity and Interactions in Vessel Wall Inflammation. Front. Immunol. 2020, 11, 599415. [Google Scholar] [CrossRef] [PubMed]
- Nosalski, R.; Guzik, T.J. Perivascular adipose tissue inflammation in vascular disease. Br. J. Pharmacol. 2017, 174, 3496–3513. [Google Scholar] [CrossRef] [PubMed]
- Villacorta, L.; Chang, L. The role of perivascular adipose tissue in vasoconstriction, arterial stiffness, and aneurysm. Horm. Mol. Biol. Clin. Investig. 2015, 21, 137–147. [Google Scholar] [CrossRef]
- Hu, H.; Garcia-Barrio, M.; Jiang, Z.-S.; Chen, Y.E.; Chang, L. Roles of Perivascular Adipose Tissue in Hypertension and Atherosclerosis. Antioxid. Redox Signal. 2021, 34, 736–749. [Google Scholar] [CrossRef]
- Canetti, C.; Leung, B.P.; Culshaw, S.; McInnes, I.; Cunha, F.; Liew, F. IL-18 enhances collagen-induced arthritis by recruiting neutrophils via TNF-alpha and leukotriene B4. J. Immunol. 2003, 171, 1009–1015. [Google Scholar] [CrossRef]
- Chou, R.; Kim, N.D.; Sadik, C.D.; Seung, E.; Lan, Y.; Byme, M.H.; Haribabu, B.; Iwakura, Y.; Luster, A.D. Lipid-Cytokine-Chemokine Cascade Drives Neutrophil Recruitment in a Murine Model of Inflammatory Arthritis. Immunity 2011, 33, 266–278. [Google Scholar] [CrossRef]
- Bäck, M.; Bu, D.X.; Bränström, R.; Sheikine, Y.; Yan, Z.Q.; Hansson, G.K. Leukotriene B4 signaling through NF-kappaB-dependent BLT1 receptors on vascular smooth muscle cells in atherosclerosis and intimal hyperplasia. Proc. Natl. Acad. Sci. USA 2005, 102, 17501–17506. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.; Zukas, A.M.; Hui, Y.; Ricciotti, E.; Puré, E.; Fitzgerald, G.A. Deletion of microsomal prostaglandin E synthase-1 augments prostacyclin and retards atherogenesis. Proc. Natl. Acad. Sci. USA 2006, 103, 14507–14512. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.; Lee, E.; Song, W.; Ricciotti, E.; Rader, D.J.; Lawson, J.A.; Puré, E.; FitzGerald, G.A. Microsomal prostaglandin E synthase-1 deletion suppresses oxidative stress and angiotensin II-induced abdominal aortic aneurysm formation. Circulation 2008, 117, 1302–1309. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.; Ihida-Stansbury, K.; Kothapalli, D.; Tamby, M.C.; Yu, Z.; Chen, L.; Grant, G.; Cheng, Y.; Lawson, J.A.; Assoian, R.K.; et al. Microsomal prostaglandin E2 synthase-1 modulates the response to vascular injury. Circulation 2011, 123, 631–639. [Google Scholar] [CrossRef]
- Motwani, M.P.; Colas, R.A.; George, M.J.; Flint, J.D.; Dalli, J.; Richard-Loendt, A.; De Maeyer, R.P.; Serhan, C.N.; Gilroy, D.W. Pro-resolving mediators promote resolution in a human skin model of UV-killed Escherichia coli-driven acute inflammation. JCI Insight 2018, 3, e94463. [Google Scholar] [CrossRef]
- Sansbury, B.E.; Spite, M. Resolution of Acute Inflammation and the Role of Resolvins in Immunity, Thrombosis, and Vascular Biology. Circ. Res. 2016, 119, 113–130. [Google Scholar] [CrossRef]
- Serhan, C.N.; Clish, C.B.; Brannon, J.; Colgan, S.P.; Chiang, N.; Gronert, K. Novel functional sets of lipid-derived mediators with antiinflammatory actions generated from omega-3 fatty acids via cyclooxygenase 2-nonsteroidal antiinflammatory drugs and transcellular processing. J. Exp. Med. 2000, 192, 1197–1204. [Google Scholar] [CrossRef]
- Spite, M.; Serhan, C.N. Novel lipid mediators promote resolution of acute inflammation: Impact of aspirin and statins. Circ. Res. 2010, 107, 1170–1184. [Google Scholar] [CrossRef]
- Serhan, C.N.; Libreros, S.; Nshimiyimana, R. E-series resolvin metabolome, biosynthesis and critical role of stereochemistry of specialized pro-resolving mediators (SPMs) in inflammation-resolution: Preparing SPMs for long COVID-19, human clinical trials, and targeted precision nutrition. Semin. Immunol. 2022, 101597. [Google Scholar] [CrossRef]
- Serhan, C.N.; Levy, B.D. Resolvins in inflammation: Emergence of the pro-resolving superfamily of mediators. J. Clin. Investig. 2018, 128, 2657–2669. [Google Scholar] [CrossRef]
- Markworth, J.F.; Kaur, G.; Miller, E.G.; Larsen, A.E.; Sinclair, A.J.; Maddipati, K.R.; Cameron-Smith, D. Divergent shifts in lipid mediator profile following supplementation with n-3 docosapentaenoic acid and eicosapentaenoic acid. FASEB J. 2016, 30, 3714–3725. [Google Scholar] [CrossRef]
- Dalli, J.; Chiang, N.; Serhan, C.N. Elucidation of novel 13-series resolvins that increase with atorvastatin and clear infections. Nat. Med. 2015, 21, 1071–1075. [Google Scholar] [CrossRef]
- Serhan, C.N.; Chiang, N.; Dalli, J. New pro-resolving n-3 mediators bridge resolution of infectious inflammation to tissue regeneration. Mol. Asp. Med. 2018, 64, 1–17. [Google Scholar] [CrossRef]
- Abdulnour, R.E.; Dalli, J.; Colby, J.K.; Krishnamoorthy, N.; Timmons, J.Y.; Tan, S.H.; Colas, R.A.; Petasis, N.A.; Serhan, C.N.; Levy, B.D. Maresin 1 biosynthesis during platelet-neutrophil interactions is organ-protective. Proc. Natl. Acad. Sci. USA 2014, 111, 16526–16531. [Google Scholar] [CrossRef]
- Serhan, C.N.; Yacoubian, S.; Yang, R. Anti-inflammatory and proresolving lipid mediators. Annu. Rev. Pathol. Mech. Dis. 2008, 3, 279–312. [Google Scholar] [CrossRef]
- Oh, S.F.; Dona, M.; Fredman, G.; Krishnamoorthy, S.; Irimia, D.; Serhan, C.N. Resolvin E2 formation and impact in inflammation resolution. J. Immunol. 2012, 188, 4527–4534. [Google Scholar] [CrossRef]
- Bang, S.; Xie, Y.K.; Zhang, Z.J.; Wang, Z.; Xu, Z.Z.; Ji, R.R. GPR37 regulates macrophage phagocytosis and resolution of inflammatory pain. J. Clin. Investig. 2018, 128, 3568–3582. [Google Scholar] [CrossRef]
- Chiang, N.; Libreros, S.; Norris, P.C.; De La Rosa, X.; Serhan, C.N. Maresin 1 activates LGR6 receptor promoting phagocyte immunoresolvent functions. J. Clin. Investig. 2019, 129, 5294–5311. [Google Scholar] [CrossRef]
- Flak, M.B.; Koenis, D.S.; Sobrino, A.; Smith, J.; Pistorius, K.; Palmas, F.; Dalli, J. GPR101 mediates the pro-resolving actions of RvD5n-3 DPA in arthritis and infections. J. Clin. Investig. 2020, 30, 359–373. [Google Scholar] [CrossRef]
- Chiang, N.; Fredman, G.; Bäckhed, F.; Oh, S.F.; Vickery, T.; Schmidt, B.A.; Serhan, C.N. Infection regulates pro-resolving mediators that lower antibiotic requirements. Nature 2012, 484, 524–528. [Google Scholar] [CrossRef]
- Dalli, J.; Winkler, J.W.; Colas, R.A.; Arnardottir, H.; Cheng, C.Y.C.; Chiang, N.; Petasis, N.A.; Serhan, C.N. Resolvin D3 and aspirin-triggered resolvin D3 are potent immunoresolvents. Chem. Biol. 2013, 20, 188–201. [Google Scholar] [CrossRef]
- Arita, M.; Ohira, T.; Sun, Y.-P.; Elangovan, S.; Chiang, N.; Serhan, C.N. Resolvin E1 selectively interacts with leukotriene B4 receptor BLT1 and ChemR23 to regulate inflammation. J. Immunol. 2007, 178, 3912–3917. [Google Scholar] [CrossRef]
- Pirault, J.; Bäck, M. Lipoxin and resolvin receptors transducing the resolution of inflammation in cardiovascular disease. Front. Pharmacol. 2018, 9, 1273. [Google Scholar] [CrossRef]
- Colas, R.A.; Dalli, J.; Chiang, N.; Vlasakov, I.; Sanger, J.M.; Riley, I.R.; Serhan, C.N. Identification and Actions of the Maresin 1 Metabolome in Infectious Inflammation. J. Immunol. 2016, 197, 4444–4452. [Google Scholar] [CrossRef]
- Tulowiecka, N.; Kotlęga, D.; Prowans, P.; Szczuko, M. The role of resolvins: EPA and DHA derivatives can be useful in the prevention and treatment of ischemic stroke. Int. J. Mol. Sci. 2020, 21, 7628. [Google Scholar] [CrossRef]
- Kozłowska, H.; Malinowska, B.; Baranowska-Kuczko, M.; Kusaczuk, M.; Nesterowicz, M.; Kozłowski, M.; Müller, C.E.; Kieć-Kononowicz, K.; Schlicker, E. GPR18-Mediated Relaxation of Human Isolated Pulmonary Arteries. Int. J. Mol. Sci. 2022, 23, 1427. [Google Scholar] [CrossRef]
- Zuo, G.; Zhang, D.; Mu, R.; Shen, H.; Li, X.; Wang, Z.; Li, H.; Chen, G. Resolvin D2 protects against cerebral ischemia/reperfusion injury in rats. Mol. Brain 2018, 11, 9. [Google Scholar] [CrossRef]
- De Palma, G.; Castellano, G.; Del Prete, A.; Sozzani, S.; Fiore, N.; Loverre, A.; Parmentier, M.; Gesualdo, L.; Grandaliano, G.; Schena, F. The possible role of ChemR23/Chemerin axis in the recruitment of dendritic cells in lupus nephritis. Kidney Int. 2011, 79, 1228–1235. [Google Scholar] [CrossRef]
- Rodríguez-Penas, D.; Feijóo-Bandín, S.; García-Rúa, V.; Mosquera-Leal, A.; Durán, D.; Varela, A.; Portolés, M.; Roselló-Lletí, E.; Rivera, M.; Diéguez, C.; et al. The Adipokine Chemerin Induces Apoptosis in Cardiomyocytes. Cell. Physiol. Biochem. 2015, 37, 176–192. [Google Scholar] [CrossRef]
- Hiram, R.; Rizcallah, E.; Marouan, S.; Sirois, C.; Sirois, M.; Morin, C.; Fortin, S.; Rousseau, E. Resolvin E1 normalizes contractility, Ca2+ sensitivity and smooth muscle cell migration rate in TNF-α- and IL-6-pretreated human pulmonary arteries. Am. J. Physiol. Lung Cell. Mol. Physiol. 2015, 309, L776–L788. [Google Scholar] [CrossRef]
- Ho, K.J.; Spite, M.; Owens, C.D.; Lancero, H.; Kroemer, A.H.K.; Pande, R.; Creager, M.A.; Serhan, C.N.; Conte, M.S. Aspirin-triggered lipoxin and resolvin E1 modulate vascular smooth muscle phenotype and correlate with peripheral atherosclerosis. Am. J. Pathol. 2010, 177, 2116–2123. [Google Scholar] [CrossRef]
- Jun, L.; Lin-Lin, S.; Hui, S. Chemerin promotes microangiopathy in diabetic retinopathy via activation of ChemR23 in rat primary microvascular endothelial cells. Mol. Vis. 2021, 27, 575–587. [Google Scholar]
- Yokomizo, T. Two distinct leukotriene B4 receptors, BLT1 and BLT2. J. Biochem. 2015, 157, 65–71. [Google Scholar] [CrossRef]
- Serhan, C.N.; Chiang, N.; Dalli, J. The resolution code of acute inflammation: Novel pro-resolving lipid mediators in resolution. Semin. Immunol. 2015, 27, 200–215. [Google Scholar] [CrossRef]
- Dalli, J.; Serhan, C.N. Identification and structure elucidation of the pro-resolving mediators provides novel leads for resolution pharmacology. Br. J. Pharmacol. 2019, 176, 1024–1037. [Google Scholar] [CrossRef]
- Chiang, N.; Dalli, J.; Colas, R.A.; Serhan, C.N. Identification of resolvin D2 receptor mediating resolution of infections and organ protection. J. Exp. Med. 2015, 212, 1203–1217. [Google Scholar] [CrossRef]
- Chiurchiù, V.; Leuti, A.; Dalli, J.; Jacobsson, A.; Battistini, L.; Maccarrone, M.; Serhan, C.N. Proresolving lipid mediators resolvin D1, resolvin D2, and maresin 1 are critical in modulating T cell responses. Sci. Transl. Med. 2016, 8, 353ra111. [Google Scholar] [CrossRef]
- Perez-Hernandez, J.; Chiurchiù, V.; Perruche, S.; You, S. Regulation of T-Cell Immune Responses by Pro-Resolving Lipid Mediators. Front. Immunol. 2021, 12, 768133. [Google Scholar] [CrossRef]
- Lannan, K.L.; Spinelli, S.L.; Blumberg, N.; Phipps, R.P. Maresin 1 induces a novel pro-resolving phenotype in human platelets. J. Thromb. Haemost. 2017, 15, 802–813. [Google Scholar] [CrossRef]
- Elajami, T.K.; Colas, R.A.; Dalli, J.; Chiang, N.; Serhan, C.N.; Welty, F.K. Specialized proresolving lipid mediators in patients with coronary artery disease and their potential for clot remodeling. FASEB J. 2016, 30, 2792–2801. [Google Scholar] [CrossRef]
- Börgeson, E.; Lönn, J.; Bergström, I.; Brodin, V.P.; Ramström, S.; Nayeri, F.; Särndahl, E.; Bengtsson, T. Lipoxin A4 inhibits porphyromonas gingivalis-induced aggregation and reactive oxygen species production by modulating neutrophil-platelet interaction and CD11b expression. Infect. Immun. 2011, 79, 1489–1497. [Google Scholar] [CrossRef]
- Chen, P.; Fenet, B.; Michaud, S.; Tomczyk, N.; Véricel, E.; Lagarde, M.; Guichardant, M. Full characterization of PDX, a neuroprotectin/protectin D1 isomer, which inhibits blood platelet aggregation. FEBS Lett. 2009, 583, 3478–3484. [Google Scholar] [CrossRef]
- Gimbrone, M.A., Jr.; García-Cardeña, G. Endothelial Cell Dysfunction and the Pathobiology of Atherosclerosis. Circ. Res. 2016, 118, 620–636. [Google Scholar] [CrossRef]
- Filep, J.G.; Zouki, C.; Petasis, N.A.; Hachicha, M.; Serhan, C.N. Anti-inflammatory actions of lipoxin A(4) stable analogs are demonstrable in human whole blood: Modulation of leukocyte adhesion molecules and inhibition of neutrophil-endothelial interactions. Blood 1999, 94, 4132–4142. [Google Scholar] [CrossRef]
- Chatterjee, A.; Sharma, A.; Chen, M.; Toy, R.; Mottola, G.; Conte, M.S. The pro-resolving lipid mediator maresin 1 (MaR1) attenuates inflammatory signaling pathways in vascular smooth muscle and endothelial cells. PLoS ONE 2014, 9, e113480. [Google Scholar] [CrossRef]
- Chattopadhyay, R.; Raghavan, S.; Rao, G.N. Resolvin D1 via prevention of ROS-mediated SHP2 inactivation protects endothelial adherens junction integrity and barrier function. Redox Biol. 2017, 12, 438–455. [Google Scholar] [CrossRef]
- Zhang, M.J.; Sansbury, B.E.; Hellmann, J.; Baker, J.F.; Guo, L.; Parmer, C.M.; Prenner, J.C.; Conklin, D.J.; Bhatnagar, A.; Creager, M.A.; et al. Resolvin D2 enhances postischemic revascularization while resolving inflammation. Circulation 2016, 134, 666–680. [Google Scholar] [CrossRef]
- Spite, M.; Norling, L.V.; Summers, L.; Yang, R.; Cooper, D.; Petasis, N.A.; Flower, R.J.; Perretti, M.; Serhan, C.N. Resolvin D2 is a potent regulator of leukocytes and controls microbial sepsis. Nature 2009, 461, 1287–1291. [Google Scholar] [CrossRef]
- Paul-Clark, M.J.; van Cao, T.; Moradi-Bidhendi, N.; Cooper, D.; Gilroy, D.W. 15-epi-lipoxin A4–mediated Induction of Nitric Oxide Explains How Aspirin Inhibits Acute Inflammation. J. Exp. Med. 2004, 200, 69–78. [Google Scholar] [CrossRef]
- Brezinski, M.; Gimbrone, M.A.; Nicolau, K.; Serhan, C.N. Lipoxins stimulate prostacyclin generation by human endothelial cells. FEBS Lett. 1989, 245, 167–172. [Google Scholar] [CrossRef]
- Nascimento-Silva, V.; Arruda, M.A.; Barja-Fidalgo, C.; Fierro, I.M. Aspirin-triggered lipoxin A4 blocks reactive oxygen species generation in endothelial cells: A novel antioxidative mechanism. Thromb. Haemost. 2007, 97, 88–98. [Google Scholar] [PubMed]
- Nascimento-Silva, V.; Arruda, M.A.; Barja-Fidalgo, C.; Villela, C.G.; Fierro, I.M. Novel lipid mediator aspirin-triggered lipoxin A4 induces heme oxygenase-1 in endothelial cells. American journal of physiology. Cell Physiol. 2005, 289, C557–C563. [Google Scholar] [CrossRef]
- Souza, M.C.; Pádua, T.A.; Torres, N.D.; Souza Costa, M.F.; Candéa, A.P.; Maramaldo, T.; Seito, L.N.; Penido, C.; Estato, V.; Antunes, B.; et al. Lipoxin A4 attenuates endothelial dysfunction during experimental cerebral malaria. Int. Immunopharmacol. 2015, 24, 400–407. [Google Scholar] [CrossRef]
- Baker, N.; O’Meara, S.J.; Scannell, M.; Maderna, P.; Godson, C. Lipoxin A4: Anti-inflammatory and anti-angiogenic impact on endothelial cells. J. Immunol. 2009, 182, 3819–3826. [Google Scholar] [CrossRef]
- Cezar-de-Mello, P.F.; Nascimento-Silva, V.; Villela, C.G.; Fierro, I.M. Aspirin-triggered Lipoxin A4 inhibition of VEGF-induced endothelial cell migration involves actin polymerization and focal adhesion assembly. Oncogene 2006, 25, 122–129. [Google Scholar] [CrossRef][Green Version]
- Fierro, I.M.; Kutok, J.L.; Serhan, C.N. Novel lipid mediator regulators of endothelial cell proliferation and migration: Aspirin-triggered-15R-lipoxin A(4) and lipoxin A(4). J. Pharmacol. Exp. Ther. 2002, 300, 385–392. [Google Scholar] [CrossRef]
- Maekawa, T.; Hosur, K.; Abe, T.; Kantarci, A.; Ziogas, A.; Wang, B.; Van Dyke, T.E.; Chavakis, T.; Hajishengallis, G. Antagonistic effects of IL-17 and D-resolvins on endothelial Del-1 expression through a GSK-3β-C/EBPβ pathway. Nat. Commun. 2015, 6, 8272. [Google Scholar] [CrossRef]
- Akagi, D.; Chen, M.; Toy, R.; Chatterjee, A.; Conte, M.S. Systemic delivery of proresolving lipid mediators resolvin D2 and maresin 1 attenuates intimal hyperplasia in mice. FASEB J. 2015, 29, 2504–2513. [Google Scholar] [CrossRef]
- Miyahara, T.; Runge, S.; Chatterjee, A.; Chen, M.; Mottola, G.; Fitzgerald, J.M.; Serhan, C.N.; Conte, M.S. D-series resolvin attenuates vascular smooth muscle cell activation and neointimal hyperplasia following vascular injury. FASEB J. 2013, 27, 2220–2232. [Google Scholar] [CrossRef]
- Petri, M.H.; Laguna-Fernandez, A.; Arnardottir, H.; Wheelock, C.E.; Perretti, M.; Hansson, G.K.; Bäck, M. Aspirin-triggered lipoxin A4 inhibits atherosclerosis progression in apolipoprotein E-/- mice. Br. J. Pharmacol. 2017, 174, 4043–4054. [Google Scholar] [CrossRef] [PubMed]
- Wu, B.; Mottola, G.; Chatterjee, A.; Lance, K.D.; Chen, M.; Siguenza, I.; Desai, T.A.; Conte, M.S. Perivascular delivery of Resolvin D1 inhibits neointimal hyperplasia in a rat model of arterial injury. J. Vasc. Surg. 2017, 65, 207–217. [Google Scholar] [CrossRef] [PubMed]
- Wu, B.; Werlin, E.C.; Chen, M.; Mottola, G.; Chatterjee, A.; Lance, K.D.; Bernards, D.A.; Sansbury, B.E.; Spite, M.; Desai, T.A.; et al. Perivascular delivery of resolvin D1 inhibits neointimal hyperplasia in a rabbit vein graft model. J. Vasc. Surg. 2018, 68, 188S–200S.e4. [Google Scholar] [CrossRef] [PubMed]
- Liu, G.; Gong, Y.; Zhang, R.; Piao, L.; Li, X.; Liu, Q.; Yan, S.; Shen, Y. Resolvin E1 attenuates injury-induced vascular neointimal formation by inhibition of inflammatory responses and vascular smooth muscle cell migration. FASEB J. 2018, 32, 5413–5425. [Google Scholar] [CrossRef] [PubMed]
- Petri, M.H.; Laguna-Fernández, A.; Gonzalez-Diez, M.; Paulsson-Berne, G.; Hansson, G.K.; Bäck, M. The role of the FPR2/ALX receptor in atherosclerosis development and plaque stability. Cardiovasc. Res. 2015, 105, 65–74. [Google Scholar] [CrossRef] [PubMed]
- Jannaway, M.; Torrens, C.; Warner, J.A.; Sampson, A.P. Resolvin E1, resolvin D1 and resolvin D2 inhibit constriction of rat thoracic aorta and human pulmonary artery induced by the thromboxane mimetic U46619. Br. J. Pharmacol. 2018, 175, 1100–1108. [Google Scholar] [CrossRef]
- Hiram, R.; Rizcallah, E.; Sirois, C.; Sirois, M.; Morin, C.; Fortin, S.; Rousseau, E. Resolvin D1 reverses reactivity and Ca2+ sensitivity induced by ET-1, TNF-α, and IL-6 in the human pulmonary artery. Am. J. Physiol. Heart Circ. Physiol. 2014, 307, H1547–H1558. [Google Scholar] [CrossRef][Green Version]
- Kurahara, L.H.; Hiraishi, K.; Yamamura, A.; Zhang, Y.; Abe, K.; Yahiro, E.; Aoki, M.; Koga, K.; Yokomise, H.; Go, T.; et al. Eicosapentaenoic acid ameliorates pulmonary hypertension via inhibition of tyrosine kinase Fyn. J. Mol. Cell. Cardiol. 2020, 148, 50–62. [Google Scholar] [CrossRef]
- von der Weid, P.Y.; Hollenberg, M.D.; Fiorucci, S.; Wallace, J.L. Aspirin-triggered, cyclooxygenase-2-dependent lipoxin synthesis modulates vascular tone. Circulation 2004, 110, 1320–1325. [Google Scholar] [CrossRef]
- Brezinski, D.A.; Nesto, R.W.; Serhan, C.N. Angioplasty triggers intracoronary leukotrienes and lipoxin A4. Impact of aspirin therapy. Circulation 1992, 86, 56–63. [Google Scholar] [CrossRef]
- Wenceslau, C.F.; McCarthy, C.G.; Szasz, T.; Webb, R.C. Lipoxin A4 mediates aortic contraction via RhoA/Rho kinase, endothelial dysfunction and reactive oxygen species. J. Vasc. Res. 2014, 51, 407–417. [Google Scholar] [CrossRef] [PubMed]
- Falk, E. Pathogenesis of atherosclerosis. J. Am. Coll. Cardiol. 2006, 47 (Suppl. S8), C7–C12. [Google Scholar] [CrossRef] [PubMed]
- Tabas, I.; Bornfeldt, K.E. Macrophage Phenotype and Function in Different Stages of Atherosclerosis. Circ. Res. 2016, 118, 653–667. [Google Scholar] [CrossRef] [PubMed]
- Tabas, I. Macrophage death and defective inflammation resolution in atherosclerosis. Nat. Rev. Immunol. 2010, 10, 36–46. [Google Scholar] [CrossRef]
- Merched, A.J.; Ko, K.; Gotlinger, K.H.; Serhan, C.N.; Chan, L. Atherosclerosis: Evidence for impairment of resolution of vascular inflammation governed by specific lipid mediators. FASEB J. 2008, 22, 3595–3606. [Google Scholar] [CrossRef]
- Viola, J.R.; Lemnitzer, P.; Jansen, Y.; Csaba, G.; Winter, C.; Neideck, C.; Silvestre-Roig, C.; Dittmar, G.; Döring, Y.; Drechsler, M.; et al. Resolving Lipid Mediators Maresin 1 and Resolvin D2 Prevent Atheroprogression in Mice. Circ. Res. 2016, 119, 1030–1038. [Google Scholar] [CrossRef]
- Fredman, G.; Hellmann, J.; Proto, J.D.; Kuriakose, G.; Colas, R.A.; Dorweiler, B.; Connolly, E.S.; Solomon, R.; Jones, D.M.; Heyer, E.J.; et al. An imbalance between specialized pro-resolving lipid mediators and pro-inflammatory leukotrienes promotes instability of atherosclerotic plaques. Nat. Commun. 2016, 7, 12859. [Google Scholar] [CrossRef]
- Bäck, M.; Yurdagul, A., Jr.; Tabas, I.; Öörni, K.; Kovanen, P.T. Inflammation and its resolution in atherosclerosis: Mediators and therapeutic opportunities. Nat. Rev. Cardiol. 2019, 16, 389–406. [Google Scholar] [CrossRef]
- Hasturk, H.; Abdallah, R.; Kantarci, A.; Nguyen, D.; Giordano, N.; Hamilton, J.; Van Dyke, T.E. Resolvin E1 (RvE1) Attenuates Atherosclerotic Plaque Formation in Diet and Inflammation-Induced atherogenesis. Arterioscler. Thromb. Vasc. Biol. 2015, 35, 1123–1133. [Google Scholar] [CrossRef]
- Salic, K.; Morrison, M.C.; Verschuren, L.; Wielinga, P.Y.; Wu, L.; Kleemann, R.; Gjorstrup, P.; Kooistra, T. Resolvin E1 attenuates atherosclerosis in absence of cholesterol-lowering effects and on top of atorvastatin. Atherosclerosis 2016, 250, 158–165. [Google Scholar] [CrossRef]
- Carracedo, M.; Artiach, G.; Witasp, A.; Clària, J.; Carlstrom, M.; Laguna-Fernandez, A.; Stenvinkel, P.; Bäck, M. The G-protein coupled receptor ChemR23 determines smooth muscle cell phenotypic switching to enhance high phosphate-induced vascular calcification. Cardiovasc. Res. 2019, 115, 1557–1566. [Google Scholar] [CrossRef] [PubMed]
- Xu, F.; Zhang, J.; Zhou, X.; Hao, H. Lipoxin A4 and its analog attenuate high fat diet-induced atherosclerosis via Keap1/Nrf2 pathway. Exp. Cell Res. 2022, 412, 113025. [Google Scholar] [CrossRef] [PubMed]
- Laguna-Fernandez, A.; Checa, A.; Carracedo, M.; Artiach, G.; Petri, M.H.; Baumgartner, R.; Forteza, M.J.; Jiang, X.; Andonova, T.; Walker, M.E.; et al. ERV1/ChemR23 Signaling Protects against Atherosclerosis by Modifying Oxidized Low-Density Lipoprotein Uptake and Phagocytosis in Macrophages. Circulation 2018, 138, 1693–1705. [Google Scholar] [CrossRef]
- Drechsler, M.; de Jong, R.; Rossaint, J.; Viola, J.R.; Leoni, G.; Wang, J.M.; Grommes, J.; Hinkel, R.; Kupatt, C.; Weber, C.; et al. Annexin A1 counteracts chemokine-induced arterial myeloid cell recruitment. Circ. Res. 2015, 116, 827–835. [Google Scholar] [CrossRef]
- Arnardottir, H.; Thul, S.; Pawelzik, S.-C.; Karadimou, G.; Artiach, G.; Gallina, A.L.; Mysdotter, V.; Carracedo, M.; Tarnawski, L.; Caravaca, A.S.; et al. The resolvin D1 receptor GPR32 transduces inflammation resolution and atheroprotection. J. Clin. Investig. 2021, 131, e142883. [Google Scholar] [CrossRef] [PubMed]
- Johnston, K.; Rutherford, R.B.; Tilson, M.; Shah, D.M.; Hollier, L.; Stanley, J.C. Suggested standards for reporting on arterial aneurysms. Subcommittee on Reporting Standards for Arterial Aneurysms, Ad Hoc Committee on Reporting Standards, Society for Vascular Surgery and North Am Chapter, International Society for Cardiovascular Surgery. J. Vasc. Surg. 1991, 13, 452–458. [Google Scholar] [CrossRef] [PubMed]
- Dua, A.; Kuy, S.; Lee, C.J.; Upchurch, G.R., Jr.; Desai, S.S. Epidemiology of aortic aneurysm repair in the United States from 2000 to 2010. J. Vasc. Surg. 2014, 59, 1512–1517. [Google Scholar] [CrossRef] [PubMed]
- Skotsimara, G.; Antonopoulos, A.; Oikonomou, E.; Papastamos, C.; Siasos, G.; Tousoulis, D. Aortic Wall Inflammation in the Pathogenesis, Diagnosis and Treatment of Aortic Aneurysms. Inflammation 2022. [Google Scholar] [CrossRef]
- Meital, L.T.; Sandow, S.L.; Calder, P.C.; Russell, F.D. Abdominal aortic aneurysm and omega-3 polyunsaturated fatty acids: Mechanisms, animal models, and potential treatment. Prostaglandins Leukot. Essent. Fat. Acids 2017, 118, 1–9. [Google Scholar] [CrossRef]
- Quintana, R.A.; Taylor, W.R. Cellular Mechanisms of Aortic Aneurysm Formation. Circ. Res. 2019, 124, 607–618. [Google Scholar] [CrossRef]
- Reed, D.; Reed, C.; Stemmermann, G.; Hayashi, T. Are aortic aneurysms caused by atherosclerosis? Circulation 1992, 85, 205–211. [Google Scholar] [CrossRef] [PubMed]
- Pillai, P.S.; Leeson, S.; Porter, T.F.; Owens, C.D.; Kim, J.M.; Conte, M.S.; Serhan, C.N.; Gelman, S. Chemical mediators of inflammation and resolution in post-operative abdominal aortic aneurysm patients. Inflammation 2012, 35, 98–113. [Google Scholar] [CrossRef] [PubMed]
- Petri, M.H.; Thul, S.; Andonova, T.; Lindquist-Liljeqvist, M.; Jin, H.; Skenteris, N.T.; Arnardottir, H.; Maegdefessel, L.; Caidahl, K.; Perretti, M.; et al. Resolution of Inflammation Through the Lipoxin and ALX–FPR2 Receptor Pathway Protects against Abdominal Aortic Aneurysms. JACC Basic Transl. Sci. 2018, 3, 719–727. [Google Scholar] [CrossRef] [PubMed]
- Pope, N.H.; Salmon, M.; Davis, J.P.; Chatterjee, A.; Su, G.; Conte, M.S.; Ailawadi, G.; Upchurch, G.R., Jr. D-series resolvins inhibit murine abdominal aortic aneurysm formation and increase M2 macrophage polarization. FASEB J. 2016, 30, 4192–4201. [Google Scholar] [CrossRef]
- Spinosa, M.; Su, G.; Salmon, M.D.; Lu, G.; Cullen, J.M.; Fashandi, A.Z.; Hawkins, R.B.; Montgomery, W.; Meher, A.K.; Conte, M.S.; et al. Resolvin D1 decreases abdominal aortic aneurysm formation by inhibiting NETosis in a mouse model. J. Vasc. Surg. 2018, 68, 93S–103S. [Google Scholar] [CrossRef]
- Elder, C.T.; Filiberto, A.C.; Su, G.; Ladd, Z.; Leroy, V.; Pruitt, E.Y.; Lu, G.; Jiang, Z.; Sharma, A.K.; Upchurch, G.R., Jr. Maresin 1 activates LGR6 signaling to inhibit smooth muscle cell activation and attenuate murine abdominal aortic aneurysm formation. FASEB J. 2021, 35, e21780. [Google Scholar] [CrossRef]
- Satish, M.; Agrawal, D.K. Pro-resolving lipid mediators in the resolution of neointimal hyperplasia pathogenesis in atherosclerotic diseases. Expert Rev. Cardiovasc. Ther. 2019, 17, 177–184. [Google Scholar] [CrossRef]
- Collins, M.J.; Li, X.; Lv, W.; Yang, C.; Protack, C.D.; Muto, A.; Jadlowiec, C.C.; Shu, C.; Dardik, A. Therapeutic strategies to combat neointimal hyperplasia in vascular grafts. Expert Rev. Cardiovasc. Ther. 2012, 10, 635–647. [Google Scholar] [CrossRef]
- Muto, A.; Fitzgerald, T.N.; Pimiento, J.M.; Maloney, S.P.; Teso, D.; Paszkowiak, J.J.; Westvik, T.S.; Kudo, F.A.; Nishibe, T.; Dardik, A. Smooth muscle cell signal transduction: Implications of vascular biology for vascular surgeons. J. Vasc. Surg. 2007, 45 (Suppl. A(6S)), A15–A24. [Google Scholar] [CrossRef]
- Petri, M.H.; Laguna-Fernandez, A.; Tseng, C.N.; Hedin, U.; Perretti, M.; Bäck, M. Aspirin-triggered 15-epi-lipoxin A4 signals through FPR2/ALX in vascular smooth muscle cells and protects against intimal hyperplasia after carotid ligation. Int. J. Cardiol. 2015, 179, 370–372. [Google Scholar] [CrossRef]
- Artiach, G.; Carracedo, M.; Clària, J.; Laguna-Fernandez, A.; Bäck, M. Opposing Effects on Vascular Smooth Muscle Cell Proliferation and Macrophage-induced Inflammation Reveal a Protective Role for the Proresolving Lipid Mediator Receptor ChemR23 in Intimal Hyperplasia. Front. Pharmacol. 2018, 9, 1327. [Google Scholar] [CrossRef] [PubMed]
- Makino, Y.; Miyahara, T.; Nitta, J.; Miyahara, K.; Seo, A.; Kimura, M.; Suhara, M.; Akai, A.; Akagi, D.; Yamamoto, K.; et al. Proresolving Lipid Mediators Resolvin D1 and Protectin D1 Isomer Attenuate Neointimal Hyperplasia in the Rat Carotid Artery Balloon Injury Model. J. Surg. Res. 2019, 233, 104–110. [Google Scholar] [CrossRef] [PubMed]
- Mottola, G.; Werlin, E.C.; Wu, B.; Chen, M.; Chatterjee, A.; Schaller, M.S.; Conte, M.S. Oral Resolvin D1 attenuates early inflammation but not intimal hyperplasia in a rat carotid angioplasty model. Prostaglandins Other Lipid Mediat. 2020, 146, 106401. [Google Scholar] [CrossRef] [PubMed]
- Yokoyama, M.; Origasa, H.; Matsuzaki, M.; Matsuzawa, Y.; Saito, Y.; Ishikawa, Y.; Oikawa, S.; Sasaki, J.; Hishida, H.; Itakura, H.; et al. Effects of eicosapentaenoic acid on major coronary events in hypercholesterolaemic patients (JELIS): A randomised open-label, blinded endpoint analysis. Lancet 2007, 369, 1090–1098. [Google Scholar] [CrossRef]
- Bhatt, D.L.; Steg, P.G.; Miller, M.; Brinton, E.A.; Jacobson, T.A.; Ketchum, S.B.; Doyle, R.T., Jr.; Juliano, R.A.; Jiao, L.; Granowitz, C.; et al. Cardiovascular Risk Reduction with Icosapent Ethyl for Hypertriglyceridemia. N. Engl. J. Med. 2019, 380, 11–22. [Google Scholar] [CrossRef] [PubMed]
- Nicholls, S.J.; Lincoff, A.M.; Garcia, M.; Bash, D.; Ballantyne, C.M.; Barter, P.J.; Davidson, M.H.; Kastelein, J.J.P.; Koenig, W.; McGuire, D.K.; et al. Effect of High-Dose Omega-3 Fatty Acids vs Corn Oil on Major Adverse Cardiovascular Events in Patients at High Cardiovascular Risk: The STRENGTH Randomized Clinical Trial. JAMA 2020, 324, 2268–2280. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).