A Novel Xeno-Free Method to Isolate Human Endometrial Mesenchymal Stromal Cells (E-MSCs) in Good Manufacturing Practice (GMP) Conditions
Abstract
:1. Introduction
2. Results
2.1. Isolation of E-MSCs
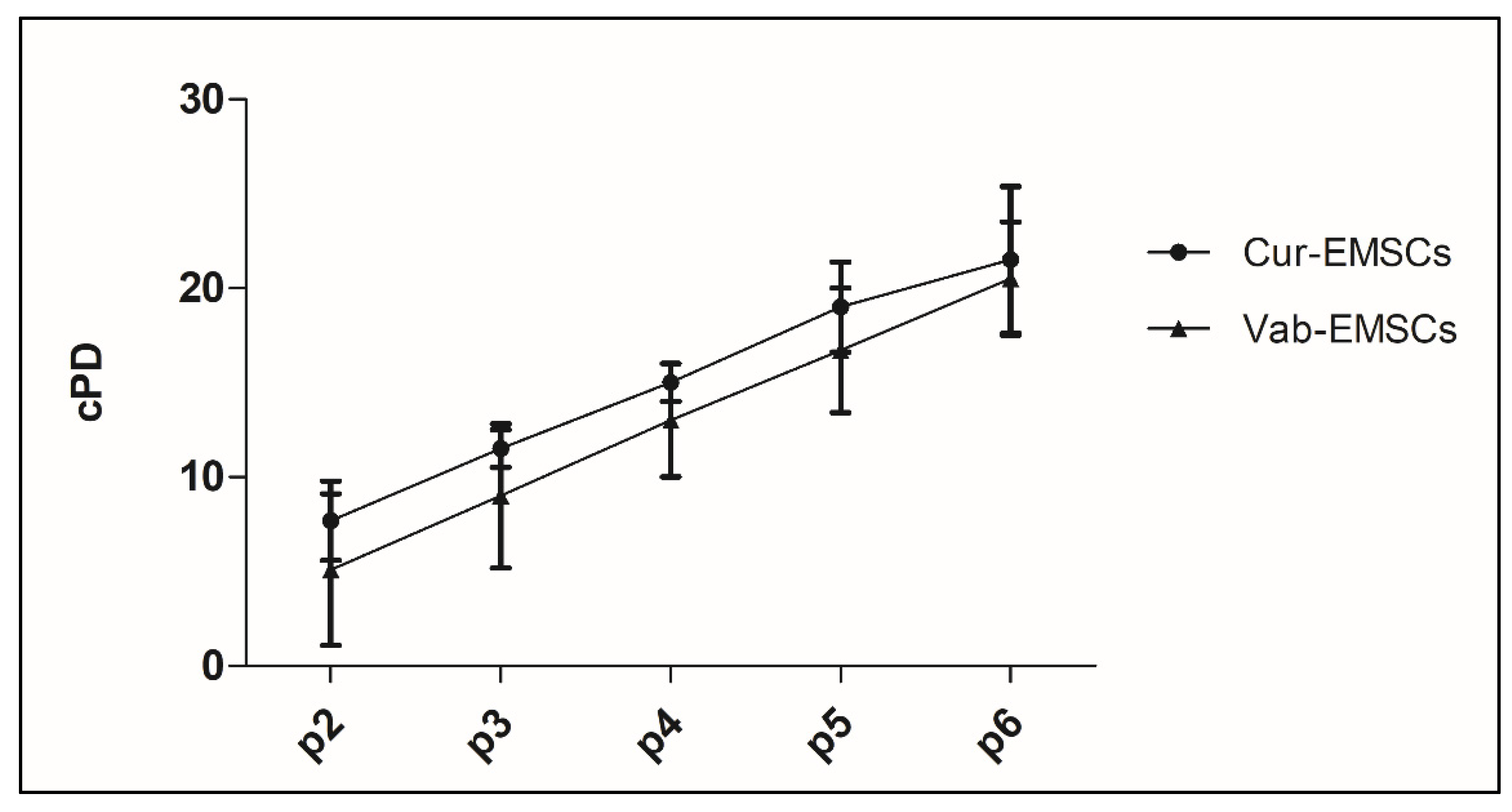
2.2. Colony Formation and Cellular Expansion Analysis
2.3. Cytofluorimetric Analysis
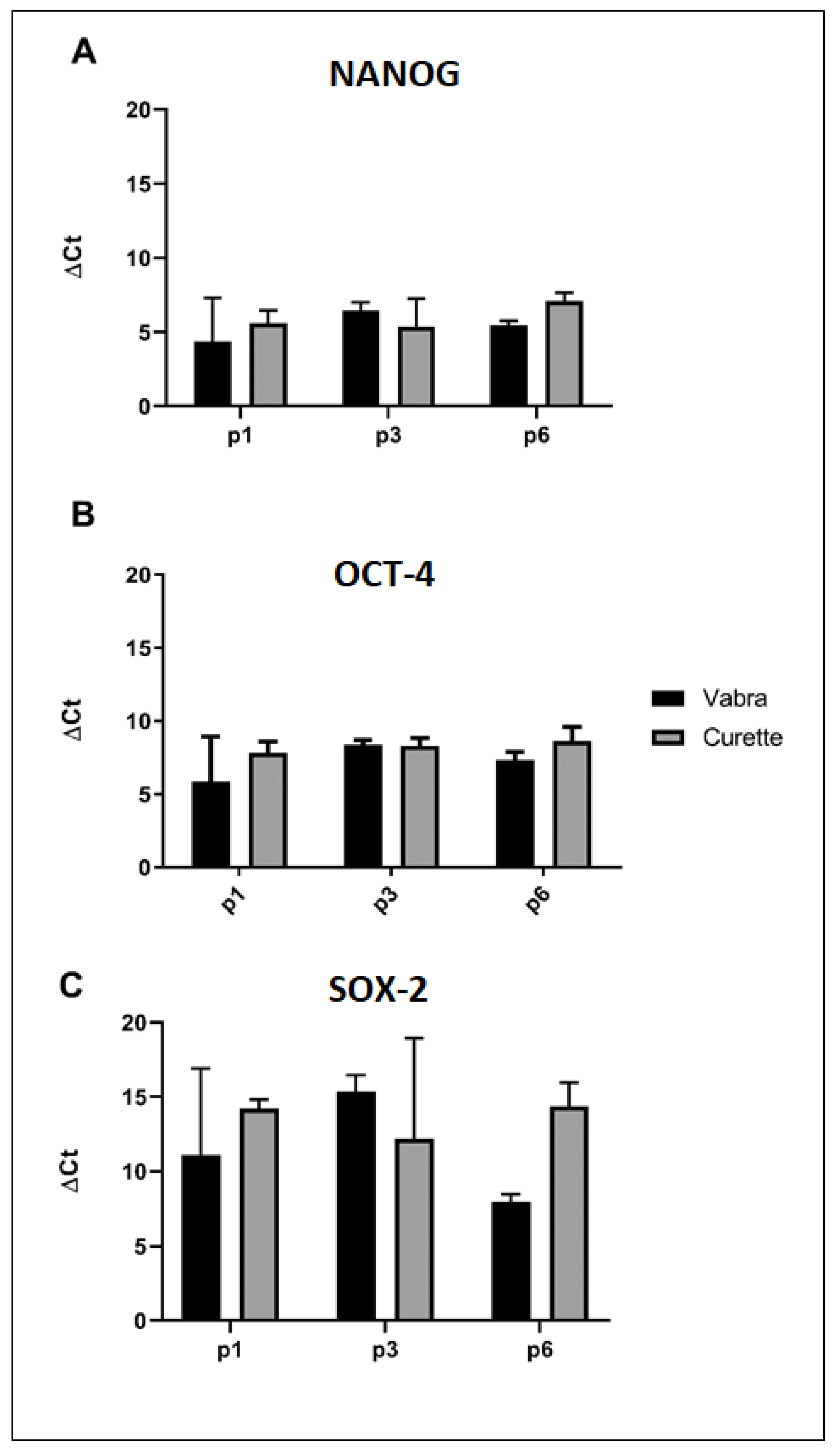
2.4. Stemness Evaluation
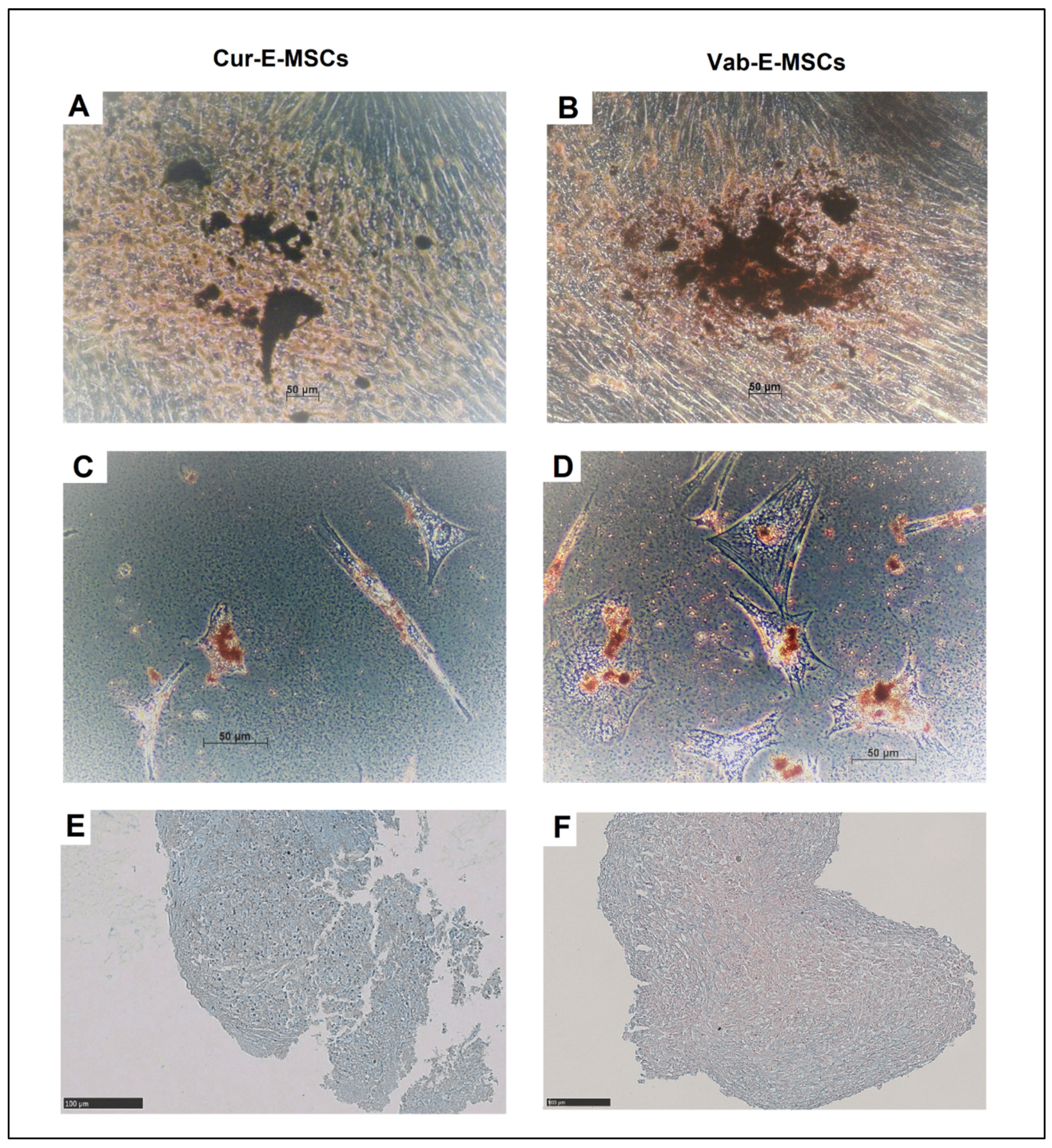
2.5. In Vitro Differentiation
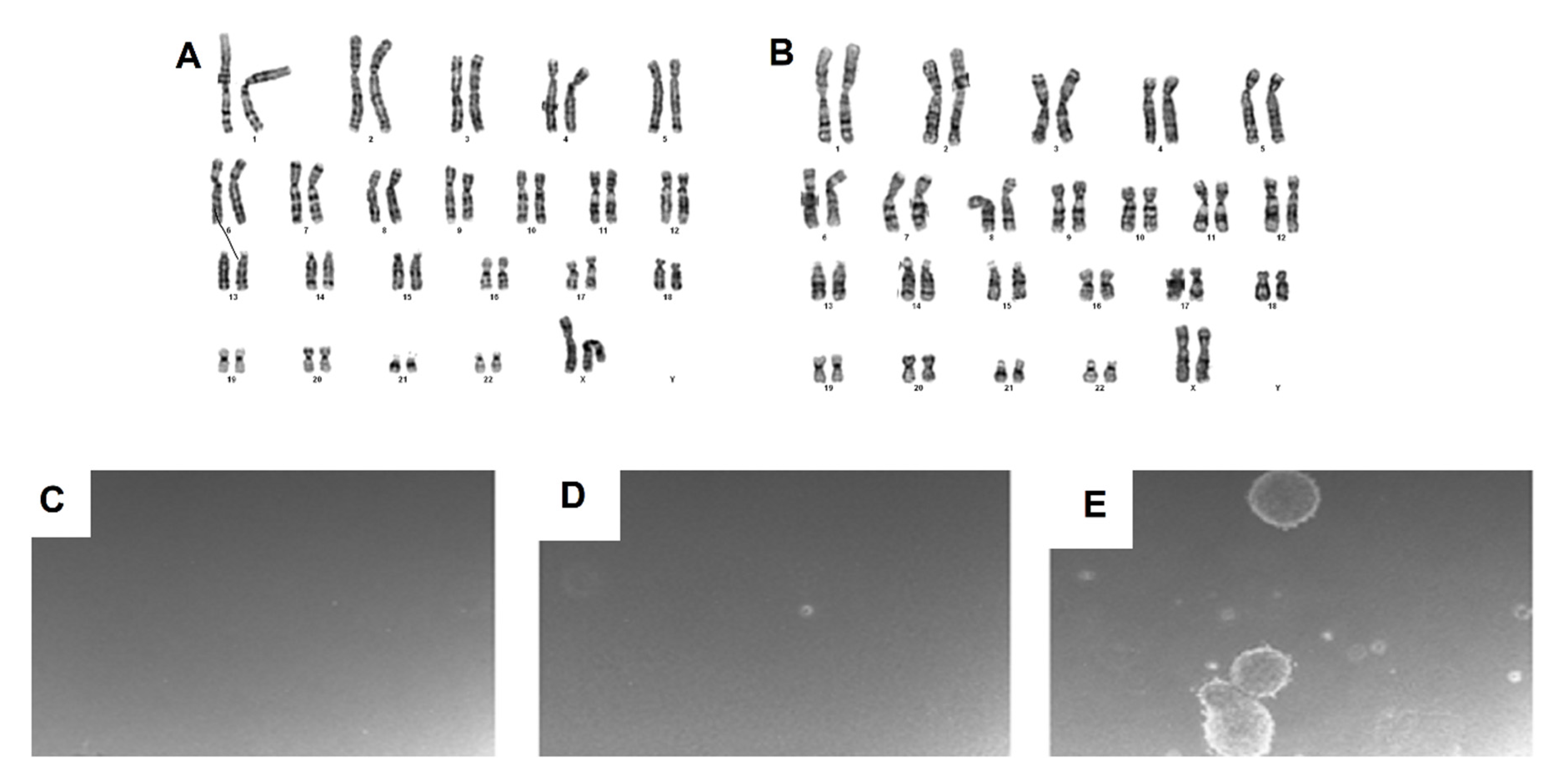
2.6. Karyotype Analysis
2.7. Invasion Assay
3. Discussion
4. Materials and Methods
4.1. Patients
4.2. E-MSC Isolation and Culture
4.3. Colony Formation Assay, Cell Viability and Proliferative Capacity
4.4. Flow Cytometric Analysis
4.5. Real-Time PCR Analysis
4.6. Karyotype Analysis
4.7. Differentiation Potential Assay
4.8. Soft Agar Assay
4.9. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AS | Asherman syndrome |
| APC | Allophycocyanin |
| ATMP | Advanced therapy medicinal products |
| BMDSCs | Bone marrow-derived stem cells |
| CD | Cluster of differentiation |
| CFU-F | Colony forming units-fibroblast |
| Cur-E-MSCs | Endometrial mesenchymal stromal cells isolated by curette |
| E-MSCs | Endometrial mesenchymal stromal cells |
| EPCAM | Epithelial cell adhesion molecule |
| FACS | Fluorescence-activated cell sorting |
| FITC | Fluorescein isothiocyanate |
| FBS | Fetal bovine serum |
| GMP | Good Manufacturing Practice |
| HLA-DR | Human leukocyte antigen–DR isotype |
| HPL | Human platelet lysate |
| ISCT | International Society for Cellular Stem Cells International Therapy |
| IVF | In vitro fertilization |
| MenSCs | Menstrual blood-derived endometrial stromal cells |
| NANOG | Nanog homeobox |
| OCT4 | Octamer-binding transcription factor 4 |
| PE | Phycoerythrin |
| PCR | Polymerase chain reaction |
| PD | Population doubling |
| SOX2 | SRY (sex determining region Y)-box 2 |
| SRY | Sex Determining region Y |
| SUSD2 (W5C5 | Sushi domain containing 2 |
| Vab-E-MSCs | Endometrial mesenchymal stromal cells isolated by VABRA |
| VABRA | Vacuum aspiration biopsy random assay |
References
- Chan, R.W.S.; Schwab, K.E.; Gargett, C.E. Clonogenicity of Human Endometrial Epithelial and Stromal Cells. Biol. Reprod. 2004, 70, 1738–1750. [Google Scholar] [CrossRef]
- Chan, R.W.S.; Gargett, C.E. Identification of Label-Retaining Cells in Mouse Endometrium. Stem Cells 2006, 24, 1529–1538. [Google Scholar] [CrossRef] [PubMed]
- Gargett, C.E. Identification and Characterisation of Human Endometrial Stem/Progenitor Cells. Aust. N. Z. J. Obstet. Gynaecol. 2006, 46, 250–253. [Google Scholar] [CrossRef]
- Gargett, C.E.; Schwab, K.E.; Zillwood, R.M.; Nguyen, H.P.T.; Wu, D. Isolation and Culture of Epithelial Progenitors and Mesenchymal Stem Cells from Human Endometrium. Biol. Reprod. 2009, 80, 1136–1145. [Google Scholar] [CrossRef] [Green Version]
- Queckbörner, S.; Davies, L.C.; von Grothusen, C.; Santamaria, X.; Simón, C.; Gemzell-Danielsson, K. Cellular Therapies for the Endometrium: An Update. Acta Obstet. Gynecol. Scand. 2019, 98, 672–677. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schwab, K.E.; Gargett, C.E. Co-Expression of Two Perivascular Cell Markers Isolates Mesenchymal Stem-like Cells from Human Endometrium. Hum. Reprod. 2007, 22, 2903–2911. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Berger, M.; Bergers, G.; Arnold, B.; Hämmerling, G.J.; Ganss, R. Regulator of G-Protein Signaling-5 Induction in Pericytes Coincides with Active Vessel Remodeling during Neovascularization. Blood 2005, 105, 1094–1101. [Google Scholar] [CrossRef]
- Spitzer, T.L.B.; Rojas, A.; Zelenko, Z.; Aghajanova, L.; Erikson, D.W.; Barragan, F.; Meyer, M.; Tamaresis, J.S.; Hamilton, A.E.; Irwin, J.C.; et al. Perivascular Human Endometrial Mesenchymal Stem Cells Express Pathways Relevant to Self-Renewal, Lineage Specification, and Functional Phenotype. Biol. Reprod. 2012, 86, 58. [Google Scholar] [CrossRef]
- Moggio, A.; Pittatore, G.; Cassoni, P.; Marchino, G.L.; Revelli, A.; Bussolati, B. Sorafenib Inhibits Growth, Migration, and Angiogenic Potential of Ectopic Endometrial Mesenchymal Stem Cells Derived from Patients with Endometriosis. Fertil. Steril. 2012, 98, 1521–1530.e2. [Google Scholar] [CrossRef] [PubMed]
- Canosa, S.; Moggio, A.; Brossa, A.; Pittatore, G.; Marchino, G.L.; Leoncini, S.; Benedetto, C.; Revelli, A.; Bussolati, B. Angiogenic Properties of Endometrial Mesenchymal Stromal Cells in Endothelial Co-Culture: An in Vitro Model of Endometriosis. Mol. Hum. Reprod. 2017, 23, 187–198. [Google Scholar] [CrossRef]
- Queckbörner, S.; Syk Lundberg, E.; Gemzell-Danielsson, K.; Davies, L.C. Endometrial Stromal Cells Exhibit a Distinct Phenotypic and Immunomodulatory Profile. Stem Cell Res. Ther. 2020, 11, 15. [Google Scholar] [CrossRef] [PubMed]
- Ocansey, D.K.W.; Pei, B.; Yan, Y.; Qian, H.; Zhang, X.; Xu, W.; Mao, F. Improved Therapeutics of Modified Mesenchymal Stem Cells: An Update. J. Transl. Med. 2020, 18, 42. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, X.; Man, G.C.W.; Liu, Y.; Wu, F.; Huang, J.; Li, T.C.; Wang, C.C. Physiological and Pathological Angiogenesis in Endometrium at the Time of Embryo Implantation. Am. J. Reprod. Immunol. 2017, 78, e12693. [Google Scholar] [CrossRef]
- Yu, D.; Wong, Y.-M.; Cheong, Y.; Xia, E.; Li, T.-C. Asherman Syndrome--One Century Later. Fertil. Steril. 2008, 89, 759–779. [Google Scholar] [CrossRef]
- Cervelló, I.; Gil-Sanchis, C.; Santamaría, X.; Cabanillas, S.; Díaz, A.; Faus, A.; Pellicer, A.; Simón, C. Human CD133(+) Bone Marrow-Derived Stem Cells Promote Endometrial Proliferation in a Murine Model of Asherman Syndrome. Fertil. Steril. 2015, 104, 1552–1560.e3. [Google Scholar] [CrossRef] [Green Version]
- Santamaria, X.; Cabanillas, S.; Cervelló, I.; Arbona, C.; Raga, F.; Ferro, J.; Palmero, J.; Remohí, J.; Pellicer, A.; Simón, C. Autologous Cell Therapy with CD133+ Bone Marrow-Derived Stem Cells for Refractory Asherman’s Syndrome and Endometrial Atrophy: A Pilot Cohort Study. Hum. Reprod. 2016, 31, 1087–1096. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tan, J.; Li, P.; Wang, Q.; Li, Y.; Li, X.; Zhao, D.; Xu, X.; Kong, L. Autologous Menstrual Blood-Derived Stromal Cells Transplantation for Severe Asherman’s Syndrome. Hum. Reprod. 2016, 31, 2723–2729. [Google Scholar] [CrossRef] [Green Version]
- Domnina, A.; Novikova, P.; Obidina, J.; Fridlyanskaya, I.; Alekseenko, L.; Kozhukharova, I.; Lyublinskaya, O.; Zenin, V.; Nikolsky, N. Human Mesenchymal Stem Cells in Spheroids Improve Fertility in Model Animals with Damaged Endometrium. Stem Cell Res. Ther. 2018, 9, 50. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zuo, W.; Xie, B.; Li, C.; Yan, Y.; Zhang, Y.; Liu, W.; Huang, J.; Chen, D. The Clinical Applications of Endometrial Mesenchymal Stem Cells. Biopreserv. Biobank. 2018, 16, 158–164. [Google Scholar] [CrossRef]
- EudraLex—Volume 4. Available online: https://ec.europa.eu/health/medicinal-products/eudralex/eudralex-volume-4_en (accessed on 28 January 2022).
- Castiglia, S.; Mareschi, K.; Labanca, L.; Lucania, G.; Leone, M.; Sanavio, F.; Castello, L.; Rustichelli, D.; Signorino, E.; Gunetti, M.; et al. Inactivated Human Platelet Lysate with Psoralen: A New Perspective for Mesenchymal Stromal Cell Production in Good Manufacturing Practice Conditions. Cytotherapy 2014, 16, 750–763. [Google Scholar] [CrossRef]
- Horwitz, E.M.; Gordon, P.L.; Koo, W.K.K.; Marx, J.C.; Neel, M.D.; McNall, R.Y.; Muul, L.; Hofmann, T. Isolated Allogeneic Bone Marrow-Derived Mesenchymal Cells Engraft and Stimulate Growth in Children with Osteogenesis Imperfecta: Implications for Cell Therapy of Bone. Proc. Natl. Acad. Sci. USA 2002, 99, 8932–8937. [Google Scholar] [CrossRef] [Green Version]
- Spees, J.L.; Gregory, C.A.; Singh, H.; Tucker, H.A.; Peister, A.; Lynch, P.J.; Hsu, S.-C.; Smith, J.; Prockop, D.J. Internalized Antigens Must Be Removed to Prepare Hypoimmunogenic Mesenchymal Stem Cells for Cell and Gene Therapy. Mol. Ther. 2004, 9, 747–756. [Google Scholar] [CrossRef]
- Sundin, M.; Ringdén, O.; Sundberg, B.; Nava, S.; Götherström, C.; Le Blanc, K. No Alloantibodies against Mesenchymal Stromal Cells, but Presence of Anti-Fetal Calf Serum Antibodies, after Transplantation in Allogeneic Hematopoietic Stem Cell Recipients. Haematologica 2007, 92, 1208–1215. [Google Scholar] [CrossRef] [PubMed]
- Müller, I.; Kordowich, S.; Holzwarth, C.; Spano, C.; Isensee, G.; Staiber, A.; Viebahn, S.; Gieseke, F.; Langer, H.; Gawaz, M.P.; et al. Animal Serum-Free Culture Conditions for Isolation and Expansion of Multipotent Mesenchymal Stromal Cells from Human BM. Cytotherapy 2006, 8, 437–444. [Google Scholar] [CrossRef]
- Halme, D.G.; Kessler, D.A. FDA Regulation of Stem-Cell-Based Therapies. N. Engl. J. Med. 2006, 355, 1730–1735. [Google Scholar] [CrossRef] [Green Version]
- Mareschi, K.; Rustichelli, D.; Calabrese, R.; Gunetti, M.; Sanavio, F.; Castiglia, S.; Risso, A.; Ferrero, I.; Tarella, C.; Fagioli, F. Multipotent Mesenchymal Stromal Stem Cell Expansion by Plating Whole Bone Marrow at a Low Cellular Density: A More Advantageous Method for Clinical Use. Stem Cells Int. 2012, 2012, 920581. [Google Scholar] [CrossRef] [PubMed]
- Dominici, M.; Le Blanc, K.; Mueller, I.; Slaper-Cortenbach, I.; Marini, F.; Krause, D.; Deans, R.; Keating, A.; Prockop, D.; Horwitz, E. Minimal Criteria for Defining Multipotent Mesenchymal Stromal Cells. The International Society for Cellular Therapy Position Statement. Cytotherapy 2006, 8, 315–317. [Google Scholar] [CrossRef]
- Torre, M.L.; Lucarelli, E.; Guidi, S.; Ferrari, M.; Alessandri, G.; De Girolamo, L.; Pessina, A.; Ferrero, I.; Gruppo Italiano Staminali Mesenchimali (GISM). Ex Vivo Expanded Mesenchymal Stromal Cell Minimal Quality Requirements for Clinical Application. Stem Cells Dev. 2015, 24, 677–685. [Google Scholar] [CrossRef] [Green Version]
- Masuda, H.; Anwar, S.S.; Bühring, H.-J.; Rao, J.R.; Gargett, C.E. A Novel Marker of Human Endometrial Mesenchymal Stem-like Cells. Cell Transplant. 2012, 21, 2201–2214. [Google Scholar] [CrossRef]
- Cervelló, I.; Gil-Sanchis, C.; Mas, A.; Delgado-Rosas, F.; Martínez-Conejero, J.A.; Galán, A.; Martínez-Romero, A.; Martínez, S.; Navarro, I.; Ferro, J.; et al. Human Endometrial Side Population Cells Exhibit Genotypic, Phenotypic and Functional Features of Somatic Stem Cells. PLoS ONE 2010, 5, e10964. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- EMA Guidelines Relevant for Advanced Therapy Medicinal Products. Available online: https://www.ema.europa.eu/en/human-regulatory/research-development/advanced-therapies/guidelines-relevant-advanced-therapy-medicinal-products (accessed on 28 January 2022).
- EU GMP Annex 15: Qualification and Validation—ECA Academy. Available online: https://www.gmp-compliance.org/guidelines/gmp-guideline/eu-gmp-annex-15-qualification-and-validation (accessed on 28 January 2022).
- Kasius, A.; Smit, J.G.; Torrance, H.L.; Eijkemans, M.J.C.; Mol, B.W.; Opmeer, B.C.; Broekmans, F.J.M. Endometrial Thickness and Pregnancy Rates after IVF: A Systematic Review and Meta-Analysis. Hum. Reprod. Update 2014, 20, 530–541. [Google Scholar] [CrossRef]
- Craciunas, L.; Gallos, I.; Chu, J.; Bourne, T.; Quenby, S.; Brosens, J.J.; Coomarasamy, A. Conventional and Modern Markers of Endometrial Receptivity: A Systematic Review and Meta-Analysis. Hum. Reprod. Update 2019, 25, 202–223. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Velasco, J.A.; Acevedo, B.; Alvarez, C.; Alvarez, M.; Bellver, J.; Fontes, J.; Landeras, J.; Manau, D.; Martinez, F.; Muñoz, E.; et al. Strategies to Manage Refractory Endometrium: State of the Art in 2016. Reprod. Biomed. Online 2016, 32, 474–489. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Salazar, C.A.; Isaacson, K.; Morris, S. A Comprehensive Review of Asherman’s Syndrome: Causes, Symptoms and Treatment Options. Curr. Opin. Obstet. Gynecol. 2017, 29, 249–256. [Google Scholar] [CrossRef]
- Deane, J.A.; Gualano, R.C.; Gargett, C.E. Regenerating Endometrium from Stem/Progenitor Cells: Is It Abnormal in Endometriosis, Asherman’s Syndrome and Infertility? Curr. Opin. Obstet. Gynecol. 2013, 25, 193–200. [Google Scholar] [CrossRef]
- Benor, A.; Gay, S.; DeCherney, A. An Update on Stem Cell Therapy for Asherman Syndrome. J. Assist. Reprod. Genet. 2020, 37, 1511–1529. [Google Scholar] [CrossRef]
- Li, Z.; Yan, G.; Diao, Q.; Yu, F.; Li, X.; Sheng, X.; Liu, Y.; Dai, Y.; Zhou, H.; Zhen, X.; et al. Transplantation of Human Endometrial Perivascular Cells with Elevated CYR61 Expression Induces Angiogenesis and Promotes Repair of a Full-Thickness Uterine Injury in Rat. Stem Cell Res. Ther. 2019, 10. [Google Scholar] [CrossRef] [PubMed]
- Marinaro, F.; Gómez-Serrano, M.; Jorge, I.; Silla-Castro, J.C.; Vázquez, J.; Sánchez-Margallo, F.M.; Blázquez, R.; López, E.; Álvarez, V.; Casado, J.G. Unraveling the Molecular Signature of Extracellular Vesicles From Endometrial-Derived Mesenchymal Stem Cells: Potential Modulatory Effects and Therapeutic Applications. Front. Bioeng. Biotechnol. 2019, 7, 431. [Google Scholar] [CrossRef] [Green Version]

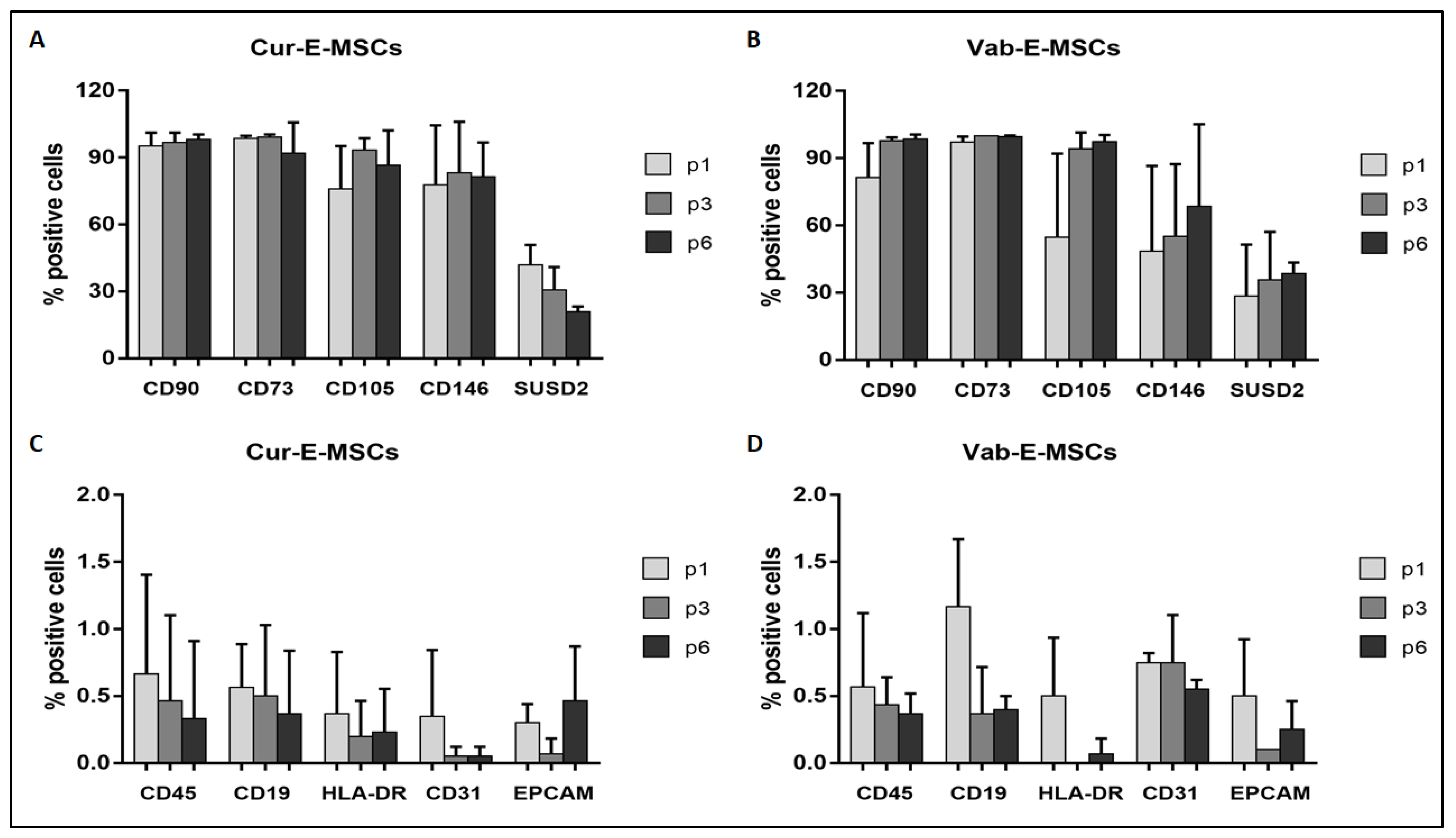
| Marker | Cur-E-MSCs (n = 3) (%) | Vab-E-MSCs (n = 3) (%) | p Value |
|---|---|---|---|
| CD90 | 97.2 ± 2.7 | 93.2 ± 7.9 | ns |
| CD73 | 97.5 ± 4.7 | 99.2 ± 0.8 | ns |
| CD105 | 82.2 ± 20.5 | 70.3 ± 27.3 | ns |
| CD146 | 80.6 ± 27.6 | 62.8 ± 20.2 | ns |
| SUSD2 | 30.5 ± 9.8 | 32.0 ± 24.7 | ns |
| CD45 | 0.6 ± 0.5 | 2.2 ± 0.7 | ns |
| CD19 | 0.6 ± 0.2 | 0.7 ± 0.4 | ns |
| HLA-DR | 0.3 ± 0.3 | 0.3 ± 0.4 | ns |
| CD31 | 2.2 ± 2.5 | 2.8 ± 2.0 | ns |
| EPCAM | 0.3 ± 0.3 | 0.5 ± 0.4 | ns |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Canosa, S.; Mareschi, K.; Marini, E.; Carosso, A.R.; Castiglia, S.; Rustichelli, D.; Ferrero, I.; Gennarelli, G.; Bussolati, B.; Nocifora, A.; et al. A Novel Xeno-Free Method to Isolate Human Endometrial Mesenchymal Stromal Cells (E-MSCs) in Good Manufacturing Practice (GMP) Conditions. Int. J. Mol. Sci. 2022, 23, 1931. https://doi.org/10.3390/ijms23041931
Canosa S, Mareschi K, Marini E, Carosso AR, Castiglia S, Rustichelli D, Ferrero I, Gennarelli G, Bussolati B, Nocifora A, et al. A Novel Xeno-Free Method to Isolate Human Endometrial Mesenchymal Stromal Cells (E-MSCs) in Good Manufacturing Practice (GMP) Conditions. International Journal of Molecular Sciences. 2022; 23(4):1931. https://doi.org/10.3390/ijms23041931
Chicago/Turabian StyleCanosa, Stefano, Katia Mareschi, Elena Marini, Andrea Roberto Carosso, Sara Castiglia, Deborah Rustichelli, Ivana Ferrero, Gianluca Gennarelli, Benedetta Bussolati, Alberto Nocifora, and et al. 2022. "A Novel Xeno-Free Method to Isolate Human Endometrial Mesenchymal Stromal Cells (E-MSCs) in Good Manufacturing Practice (GMP) Conditions" International Journal of Molecular Sciences 23, no. 4: 1931. https://doi.org/10.3390/ijms23041931
APA StyleCanosa, S., Mareschi, K., Marini, E., Carosso, A. R., Castiglia, S., Rustichelli, D., Ferrero, I., Gennarelli, G., Bussolati, B., Nocifora, A., Asnaghi, V., Bergallo, M., Isidoro, C., Benedetto, C., Revelli, A., & Fagioli, F. (2022). A Novel Xeno-Free Method to Isolate Human Endometrial Mesenchymal Stromal Cells (E-MSCs) in Good Manufacturing Practice (GMP) Conditions. International Journal of Molecular Sciences, 23(4), 1931. https://doi.org/10.3390/ijms23041931











