The Potential Role of Spermine and Its Acetylated Derivative in Human Malignancies
Abstract
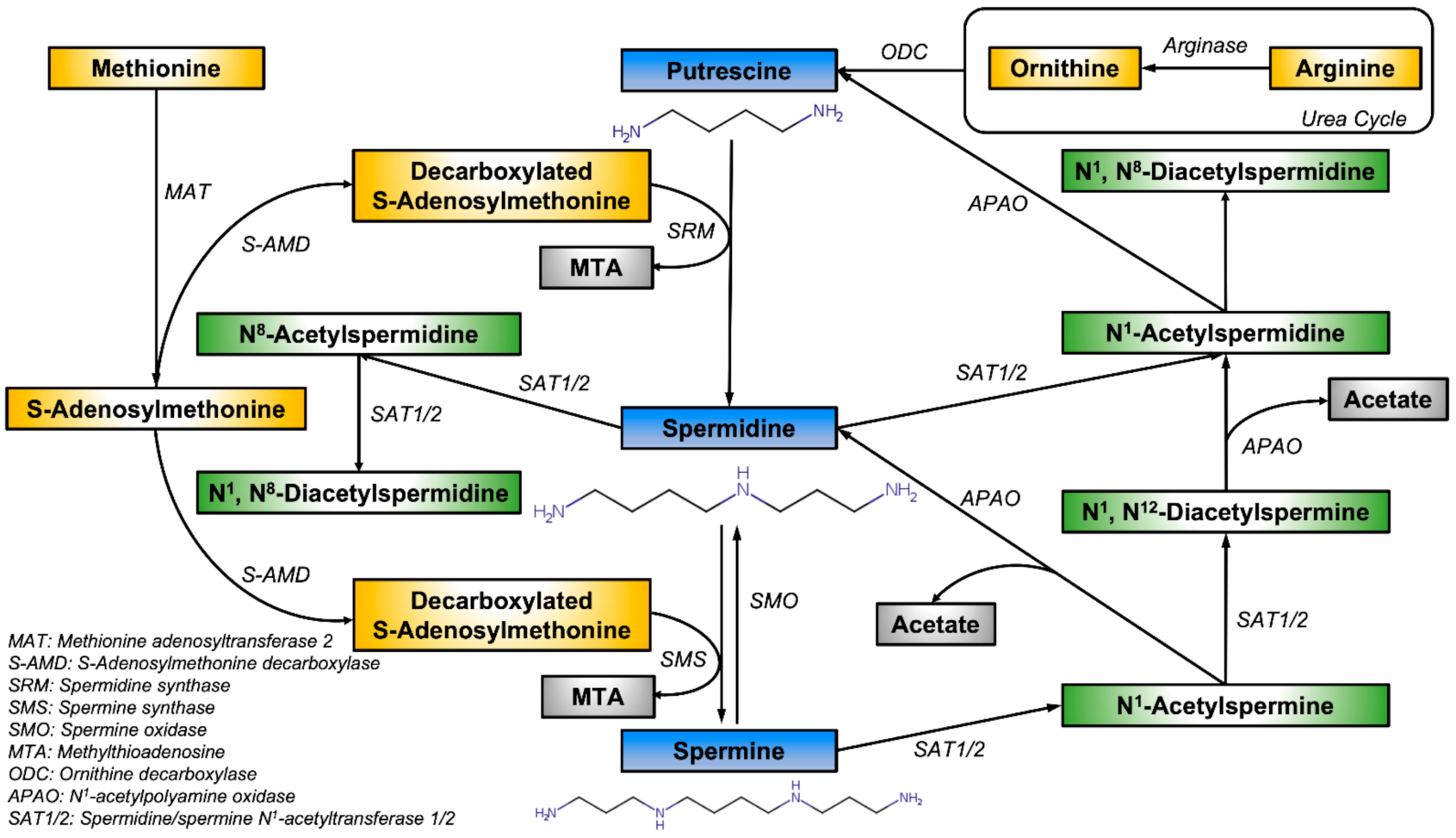
1. Introduction
2. Roles of Spermine in Cancers
2.1. Lung Cancer
2.2. Liver Cancer
2.3. Breast Cancer
2.4. Colorectal Cancer
2.5. Urological Cancers
2.6. Gynaecological Cancers
3. Applications and Prospects
3.1. Detection and Prognosis
3.2. Novel Therapeutic Agents
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bae, D.H.; Lane, D.J.R.; Jansson, P.J.; Richardson, D.R. The old and new biochemistry of polyamines. Biochim. Biophys. Acta Gen. Subj. 2018, 1862, 2053–2068. [Google Scholar] [CrossRef] [PubMed]
- Corral, M.; Wallace, H.M. Upregulation of Polyamine Transport in Human Colorectal Cancer Cells. Biomolecules 2020, 10. [Google Scholar] [CrossRef] [PubMed]
- Madeo, F.; Eisenberg, T.; Pietrocola, F.; Kroemer, G. Spermidine in health and disease. Science 2018, 359. [Google Scholar] [CrossRef] [PubMed]
- Wallace, H.M.; Fraser, A.V.; Hughes, A. A perspective of polyamine metabolism. Biochem. J. 2003, 376, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Casero, R.A., Jr.; Murray Stewart, T.; Pegg, A.E. Polyamine metabolism and cancer: Treatments, challenges and opportunities. Nat. Rev. Cancer 2018, 18, 681–695. [Google Scholar] [CrossRef]
- Cervelli, M.; Pietropaoli, S.; Signore, F.; Amendola, R.; Mariottini, P. Polyamines metabolism and breast cancer: State of the art and perspectives. Breast. Cancer Res. Treat. 2014, 148, 233–248. [Google Scholar] [CrossRef]
- Pegg, A.E. The function of spermine. IUBMB Life 2014, 66, 8–18. [Google Scholar] [CrossRef]
- Durie, B.G.; Salmon, S.E.; Russell, D.H. Polyamines as markers of response and disease activity in cancer chemotherapy. Cancer Res. 1977, 37, 214–221. [Google Scholar]
- Tsoi, T.H.; Chan, C.F.; Chan, W.L.; Chiu, K.F.; Wong, W.T.; Ng, C.F.; Wong, K.L. Urinary Polyamines: A Pilot Study on Their Roles as Prostate Cancer Detection Biomarkers. PLoS ONE 2016, 11, e0162217. [Google Scholar] [CrossRef]
- Liu, R.; Li, Q.; Ma, R.; Lin, X.; Xu, H.; Bi, K. Determination of polyamine metabolome in plasma and urine by ultrahigh performance liquid chromatography-tandem mass spectrometry method: Application to identify potential markers for human hepatic cancer. Anal. Chim. Acta 2013, 791, 36–45. [Google Scholar] [CrossRef]
- Bartos, D.; Campbell, R.A.; Bartos, F.; Grettie, D.P. Direct determination of polyamines in human serum by radioimmunoassay. Cancer Res. 1975, 35, 2056–2060. [Google Scholar] [PubMed]
- Samarra, I.; Ramos-Molina, B.; Queipo-Ortuno, M.I.; Tinahones, F.J.; Arola, L.; Delpino-Rius, A.; Herrero, P.; Canela, N. Gender-Related Differences on Polyamine Metabolome in Liquid Biopsies by a Simple and Sensitive Two-Step Liquid-Liquid Extraction and LC-MS/MS. Biomolecules 2019, 9. [Google Scholar] [CrossRef] [PubMed]
- Damiani, E.; Wallace, H.M. Polyamines and Cancer. Methods Mol. Biol. 2018, 1694, 469–488. [Google Scholar] [CrossRef] [PubMed]
- Mu, T.; Chu, T.; Li, W.; Dong, Q.; Liu, Y. N1, N12-Diacetylspermine Is Elevated in Colorectal Cancer and Promotes Proliferation through the miR-559/CBS Axis in Cancer Cell Lines. J. Oncol. 2021, 2021, 6665704. [Google Scholar] [CrossRef] [PubMed]
- Fahrmann, J.F.; Vykoukal, J.; Fleury, A.; Tripathi, S.; Dennison, J.B.; Murage, E.; Wang, P.; Yu, C.Y.; Capello, M.; Creighton, C.J.; et al. Association Between Plasma Diacetylspermine and Tumor Spermine Synthase With Outcome in Triple-Negative Breast Cancer. J. Natl. Cancer Inst. 2020, 112, 607–616. [Google Scholar] [CrossRef] [PubMed]
- Wikoff, W.R.; Hanash, S.; DeFelice, B.; Miyamoto, S.; Barnett, M.; Zhao, Y.; Goodman, G.; Feng, Z.; Gandara, D.; Fiehn, O.; et al. Diacetylspermine Is a Novel Prediagnostic Serum Biomarker for Non-Small-Cell Lung Cancer and Has Additive Performance With Pro-Surfactant Protein, B. J. Clin. Oncol. 2015, 33, 3880–3886. [Google Scholar] [CrossRef]
- Min, J.Z.; Matsumoto, A.; Li, G.; Jiang, Y.Z.; Yu, H.F.; Todoroki, K.; Inoue, K.; Toyo’oka, T. A quantitative analysis of the polyamine in lung cancer patient fingernails by LC-ESI-MS/MS. Biomed. Chromatogr. 2014, 28, 492–499. [Google Scholar] [CrossRef]
- Xu, H.; Liu, R.; He, B.; Bi, C.W.; Bi, K.; Li, Q. Polyamine Metabolites Profiling for Characterization of Lung and Liver Cancer Using an LC-Tandem MS Method with Multiple Statistical Data Mining Strategies: Discovering Potential Cancer Biomarkers in Human Plasma and Urine. Molecules 2016, 21. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, Y.; Sakaguchi, K.; Horio, H.; Hiramatsu, K.; Moriya, S.; Takahashi, K.; Kawakita, M. Urinary N1, N12-diacetylspermine is a non-invasive marker for the diagnosis and prognosis of non-small-cell lung cancer. Br. J. Cancer 2015, 113, 1493–1501. [Google Scholar] [CrossRef]
- Enjoji, M.; Nakamuta, M.; Arimura, E.; Morizono, S.; Kuniyoshi, M.; Fukushima, M.; Kotoh, K.; Nawata, H. Clinical significance of urinary N1,N12-diacetylspermine levels in patients with hepatocellular carcinoma. Int. J. Biol. Markers 2004, 19, 322–327. [Google Scholar] [CrossRef]
- Stabellini, G.; Calastrini, C.; Gagliano, N.; Dellavia, C.; Moscheni, C.; Vizzotto, L.; Occhionorelli, S.; Gioia, M. Polyamine levels and ornithine decarboxylase activity in blood and erythrocytes in human diseases. Int. J. Clin. Pharm. Res. 2003, 23, 17–22. [Google Scholar]
- Venalainen, M.K.; Roine, A.N.; Hakkinen, M.R.; Vepsalainen, J.J.; Kumpulainen, P.S.; Kiviniemi, M.S.; Lehtimaki, T.; Oksala, N.K.; Rantanen, T.K. Altered Polyamine Profiles in Colorectal Cancer. Anticancer Res. 2018, 38, 3601–3607. [Google Scholar] [CrossRef] [PubMed]
- Bentrad, V.V.; Gogol, S.V.; Zaletok, S.P.; Vitruk, Y.V.; Stakhovskyi, E.O.; Grechko, B.O. P1-114-Urinary spermine level as novel additional diagnostic marker of prostate cancer. Ann. Oncol. 2019, 30, vi123. [Google Scholar] [CrossRef]
- Serkova, N.J.; Gamito, E.J.; Jones, R.H.; O’Donnell, C.; Brown, J.L.; Green, S.; Sullivan, H.; Hedlund, T.; Crawford, E.D. The metabolites citrate, myo-inositol, and spermine are potential age-independent markers of prostate cancer in human expressed prostatic secretions. Prostate 2008, 68, 620–628. [Google Scholar] [CrossRef]
- Giskeodegard, G.F.; Bertilsson, H.; Selnaes, K.M.; Wright, A.J.; Bathen, T.F.; Viset, T.; Halgunset, J.; Angelsen, A.; Gribbestad, I.S.; Tessem, M.B. Spermine and citrate as metabolic biomarkers for assessing prostate cancer aggressiveness. PLoS ONE 2013, 8, e62375. [Google Scholar] [CrossRef]
- Dunzendorfer, U.; Russell, D.H. Altered polyamine profiles in prostatic hyperplasia and in kidney tumors. Cancer Res. 1978, 38, 2321–2324. [Google Scholar]
- Stejskal, D.; Humenanska, V.; Hanulova, Z.; Fiala, R.; Vrtal, R.; Solichova, P.; Karpisek, M. Evaluation of urine N1,N12-Diacetylspermine as potential tumor marker for urinary bladder cancer. Biomed. Pap. Med. Fac. Univ. Palacky Olomouc. Czech Repub. 2006, 150, 235–237. [Google Scholar] [CrossRef]
- Niemi, R.J.; Roine, A.N.; Hakkinen, M.R.; Kumpulainen, P.S.; Keinanen, T.A.; Vepsalainen, J.J.; Lehtimaki, T.; Oksala, N.K.; Maenpaa, J.U. Urinary Polyamines as Biomarkers for Ovarian Cancer. Int. J. Gynecol. Cancer 2017, 27, 1360–1366. [Google Scholar] [CrossRef]
- Cooper, K.D.; Shukla, J.B.; Rennert, O.M. Polyamine compartmentalization in various human disease states. Clin. Chim. Acta 1978, 82, 1–7. [Google Scholar] [CrossRef]
- Zhe Min, J. Development of a highly sensitive separation method for the analysis of metabolites in human nails and applications in the diagnosis of chronic disease. Yakugaku Zasshi 2014, 134, 1191–1198. [Google Scholar] [CrossRef][Green Version]
- Schipper, R.G.; Romijn, J.C.; Cuijpers, V.M.; Verhofstad, A.A. Polyamines and prostatic cancer. Biochem. Soc. Trans. 2003, 31, 375–380. [Google Scholar] [CrossRef] [PubMed]
- Cheng, L.L.; Wu, C.; Smith, M.R.; Gonzalez, R.G. Non-destructive quantitation of spermine in human prostate tissue samples using HRMAS 1H NMR spectroscopy at 9.4 T. FEBS Lett. 2001, 494, 112–116. [Google Scholar] [CrossRef]
- Swanson, M.G.; Zektzer, A.S.; Tabatabai, Z.L.; Simko, J.; Jarso, S.; Keshari, K.R.; Schmitt, L.; Carroll, P.R.; Shinohara, K.; Vigneron, D.B.; et al. Quantitative analysis of prostate metabolites using 1H HR-MAS spectroscopy. Magn. Reson. Med. 2006, 55, 1257–1264. [Google Scholar] [CrossRef] [PubMed]
- Huang, W.; Eickhoff, J.C.; Mehraein-Ghomi, F.; Church, D.R.; Wilding, G.; Basu, H.S. Expression of spermidine/spermine N(1) -acetyl transferase (SSAT) in human prostate tissues is related to prostate cancer progression and metastasis. Prostate 2015, 75, 1150–1159. [Google Scholar] [CrossRef] [PubMed]
- Peng, Q.; Wong, C.Y.; Cheuk, I.W.; Teoh, J.Y.; Chiu, P.K.; Ng, C.F. The Emerging Clinical Role of Spermine in Prostate Cancer. Int. J. Mol. Sci. 2021, 22. [Google Scholar] [CrossRef]
- Maksymiuk, A.W.; Sitar, D.S.; Ahmed, R.; Cheng, B.; Bach, H.; Bagchi, R.A.; Aroutiounova, N.; Tappia, P.S.; Ramjiawan, B. Spermidine/spermine N1-acetyltransferase-1 as a diagnostic biomarker in human cancer. Future Sci. OA 2018, 4, FSO345. [Google Scholar] [CrossRef]
- Tan, G.H.; Nason, G.; Ajib, K.; Woon, D.T.S.; Herrera-Caceres, J.; Alhunaidi, O.; Perlis, N. Smarter screening for prostate cancer. World J. Urol. 2019, 37, 991–999. [Google Scholar] [CrossRef]
- Chiu, P.K.; Fung, Y.H.; Teoh, J.Y.; Chan, C.H.; Lo, K.L.; Li, K.M.; Tse, R.T.; Leung, C.H.; Wong, Y.P.; Roobol, M.J.; et al. Urine spermine and multivariable Spermine Risk Score predict high-grade prostate cancer. Prostate Cancer Prostatic Dis. 2021, 24, 542–548. [Google Scholar] [CrossRef]
- Amin, M.; Tang, S.; Shalamanova, L.; Taylor, R.L.; Wylie, S.; Abdullah, B.M.; Whitehead, K.A. Polyamine biomarkers as indicators of human disease. Biomarkers 2021, 26, 77–94. [Google Scholar] [CrossRef]
- Redman, C.; Xu, M.J.; Peng, Y.M.; Scott, J.A.; Payne, C.; Clark, L.C.; Nelson, M.A. Involvement of polyamines in selenomethionine induced apoptosis and mitotic alterations in human tumor cells. Carcinogenesis 1997, 18, 1195–1202. [Google Scholar] [CrossRef][Green Version]
- Du, X.; Li, D.; Wang, G.; Fan, Y.; Li, N.; Chai, L.; Li, G.; Li, J. Chemoprotective effect of atorvastatin against benzo(a)pyrene-induced lung cancer via the inhibition of oxidative stress and inflammatory parameters. Ann. Transl. Med. 2021, 9, 355. [Google Scholar] [CrossRef] [PubMed]
- Hacker, A.; Marton, L.J.; Sobolewski, M.; Casero, R.A., Jr. In vitro and in vivo effects of the conformationally restricted polyamine analogue CGC-11047 on small cell and non-small cell lung cancer cells. Cancer Chemother. Pharm. 2008, 63, 45–53. [Google Scholar] [CrossRef] [PubMed]
- Lopez-Contreras, F.; Munoz-Uribe, M.; Perez-Laines, J.; Ascencio-Leal, L.; Rivera-Dictter, A.; Martin-Martin, A.; Burgos, R.A.; Alarcon, P.; Lopez-Munoz, R. Searching for Drug Synergy Against Cancer Through Polyamine Metabolism Impairment: Insight Into the Metabolic Effect of Indomethacin on Lung Cancer Cells. Front. Pharm. 2019, 10, 1670. [Google Scholar] [CrossRef] [PubMed]
- Lu, B.; Liang, X.; Scott, G.K.; Chang, C.H.; Baldwin, M.A.; Thomas, T.; Benz, C.C. Polyamine inhibition of estrogen receptor (ER) DNA-binding and ligand-binding functions. Breast Cancer Res. Treat. 1998, 48, 243–257. [Google Scholar] [CrossRef] [PubMed]
- Chow, L.W.C.; Wong, K.L.; Shiao, L.R.; Wu, K.C.; Leung, Y.M. Polyamine stimulation perturbs intracellular Ca2+ homeostasis and decreases viability of breast cancer BT474 cells. Z. Nat. C J. Biosci. 2020, 75, 65–73. [Google Scholar] [CrossRef] [PubMed]
- Alexiou, G.A.; Lianos, G.D.; Ragos, V.; Galani, V.; Kyritsis, A.P. Difluoromethylornithine in cancer: New advances. Future Oncol. 2017, 13, 809–819. [Google Scholar] [CrossRef] [PubMed]
- Gutierrez, L.G.; Hernandez-Morales, M.; Nunez, L.; Villalobos, C. Inhibition of Polyamine Biosynthesis Reverses Ca(2+) Channel Remodeling in Colon Cancer Cells. Cancers 2019, 11. [Google Scholar] [CrossRef]
- Khan, A.; Gamble, L.D.; Upton, D.H.; Ung, C.; Yu, D.M.T.; Ehteda, A.; Pandher, R.; Mayoh, C.; Hebert, S.; Jabado, N.; et al. Dual targeting of polyamine synthesis and uptake in diffuse intrinsic pontine gliomas. Nat. Commun. 2021, 12, 971. [Google Scholar] [CrossRef]
- Fan, J.; Feng, Z.; Chen, N. Spermidine as a target for cancer therapy. Pharm. Res. 2020, 159, 104943. [Google Scholar] [CrossRef]
- Darmostuk, M.; Jurasek, M.; Lengyel, K.; Zelenka, J.; Rumlova, M.; Drasar, P.; Ruml, T. Conjugation of chlorins with spermine enhances phototoxicity to cancer cells in vitro. J. Photochem. Photobiol. B 2017, 168, 175–184. [Google Scholar] [CrossRef]
| Cancer of Origin | Method | Major Outcome | Polyamine Levels ^ | Statistical Significance | AUC | Reference |
|---|---|---|---|---|---|---|
| Lung | LC-ESI-MS/MS | Increased fingernail Spm level | NR | p < 0.05 a | NR | [17] |
| UHPLC-MS/MS | Increased urinary Spm level | 0.30 ± 0.36 ‡; 0.80 ± 0.86 ‡; 2.67 | p < 0.01 a | NR | [18] | |
| UHPLC-MS/MS | Decreased plasma Spm level | 12.61 ± 12.02 †; 6.78 ± 3.87 †; 0.54 | p > 0.05 a | NR | ||
| Colloidal gold aggregation | Increased urinary DiAcSpm level in NSCLC | 0.0005 (0.485–0.847) ‡; 0.0008 (0.605–1.28) ‡; 1.60 | p < 2.2 × 10−6 a | 0.75 | [19] | |
| Liver | UHPLC-MS/MS | Increased urinary Spm level | 0.30 ± 0.36 ‡; 1.88 ± 2.34 ‡; 6.27 | p < 0.01 a | NR | [18] |
| UHPLC-MS/MS | Increased plasma Spm level | 12.61 ± 12.02 †; 14.24 ± 10.73 †; 0.89 | p > 0.05 a | NR | ||
| ELISA | Increased urinary DiAcSpm level in advanced HCC | Threshold set at 325 nM/g creatinine | p < 0.0001 a,b | NR | [20] | |
| Breast | NR | Increased serum Spm level and Spm/Put ratio | NR | NR b | NR | [21] |
| LC-MS | Increased plasma DiAcSpm level in TNBC | 0.98 ± 0.05; 1.11 ± 0.30; 1.13 | p < 0.001 a | 0.64 | [15] | |
| Colorectal | LC-MS/MS | Increased urinary DiAcSpm level | 0.0855 (0.15) ‡; 0.182 (0.20) ‡; 2.13 | p = 0.00049 a,b p = 0.042 b | 0.72 | [22] |
| Prostate | UHPLC-MS/MS | Decreased urinary Spm level | 5.43 ± 1.17; 1.47 ± 0.22; 0.27 | p < 0.0001 a,b | 0.83 ± 0.03 | [9] |
| HPLC | Decreased urinary Spm level | NR | NR | NR | [23] | |
| 1H-NMRS | Decreased prostatic secretion Spm level | NR | p < 0.002 a | 0.79 | [24] | |
| HR-MAS | Decreased tissue Spm level in PCa | 1.92 (0.86–3.13) #; 1.22 (0.66–2.00) #; 0.635 | p = 0.022 a | 0.86 * | [25] | |
| Kidney | Amino acid analyzer | Decreased tissue Spm level | 6.85 ± 6.97; 4.05 ± 2.23; 0.59 | p = 0.1 a | NR | [26] |
| Urinary Bladder | ELISA | No significant urinary DiAcSpm level change | NR | p = 0.64 a | <0.7 | [27] |
| Ovary | LC-MS/MS | Increased urinary DiAcSpm level | 0.10 ± 0.04 ‡; 0.54 ± 0.62 ‡; 5.4 | p < 0.001 a,b | 0.83 | [28] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tse, R.T.-H.; Wong, C.Y.-P.; Chiu, P.K.-F.; Ng, C.-F. The Potential Role of Spermine and Its Acetylated Derivative in Human Malignancies. Int. J. Mol. Sci. 2022, 23, 1258. https://doi.org/10.3390/ijms23031258
Tse RT-H, Wong CY-P, Chiu PK-F, Ng C-F. The Potential Role of Spermine and Its Acetylated Derivative in Human Malignancies. International Journal of Molecular Sciences. 2022; 23(3):1258. https://doi.org/10.3390/ijms23031258
Chicago/Turabian StyleTse, Ryan Tsz-Hei, Christine Yim-Ping Wong, Peter Ka-Fung Chiu, and Chi-Fai Ng. 2022. "The Potential Role of Spermine and Its Acetylated Derivative in Human Malignancies" International Journal of Molecular Sciences 23, no. 3: 1258. https://doi.org/10.3390/ijms23031258
APA StyleTse, R. T.-H., Wong, C. Y.-P., Chiu, P. K.-F., & Ng, C.-F. (2022). The Potential Role of Spermine and Its Acetylated Derivative in Human Malignancies. International Journal of Molecular Sciences, 23(3), 1258. https://doi.org/10.3390/ijms23031258






