Molecular Insights and Clinical Outcomes of Drugs of Abuse Adulteration: New Trends and New Psychoactive Substances
Abstract
:1. Introduction
2. Results
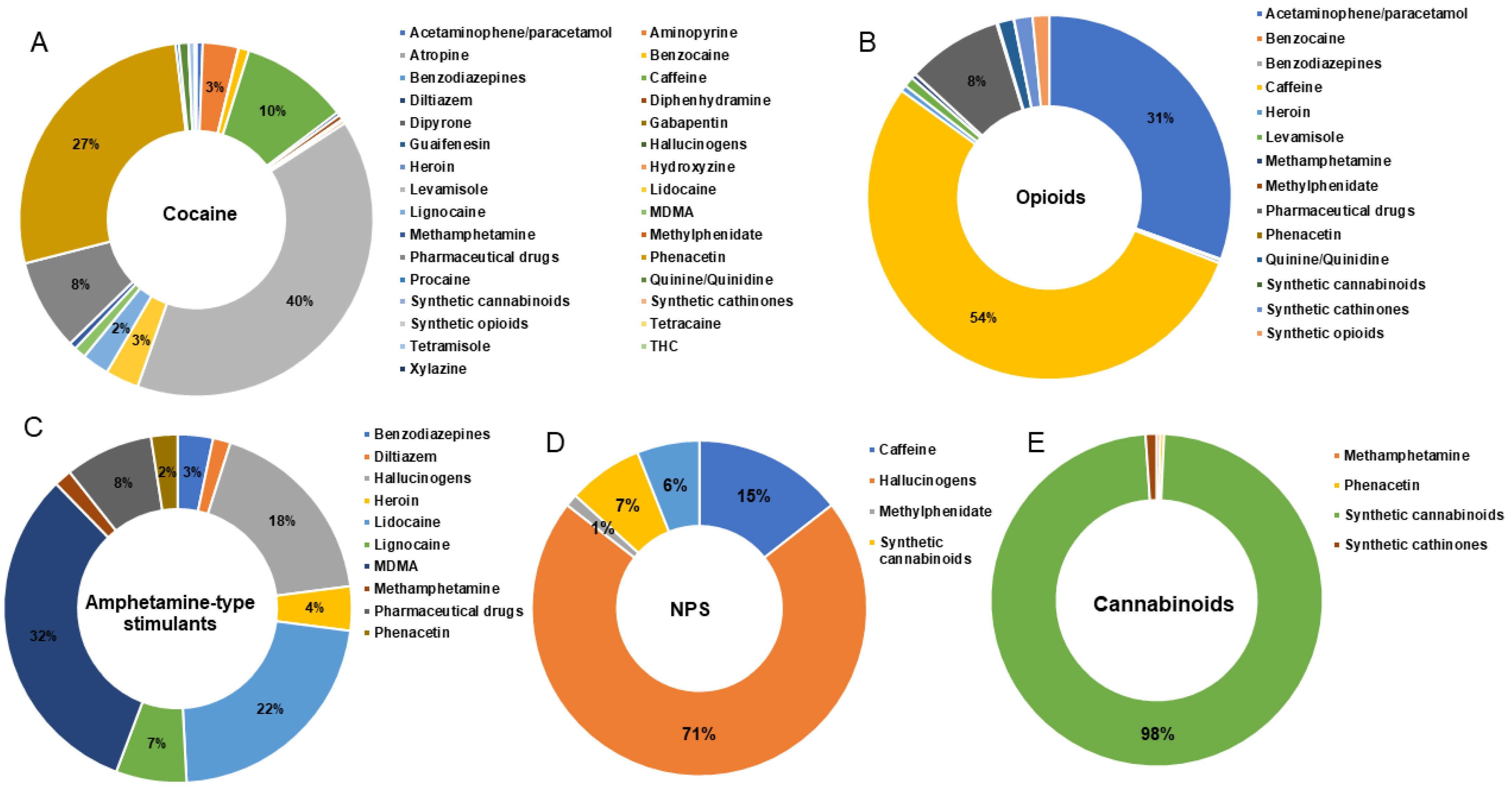
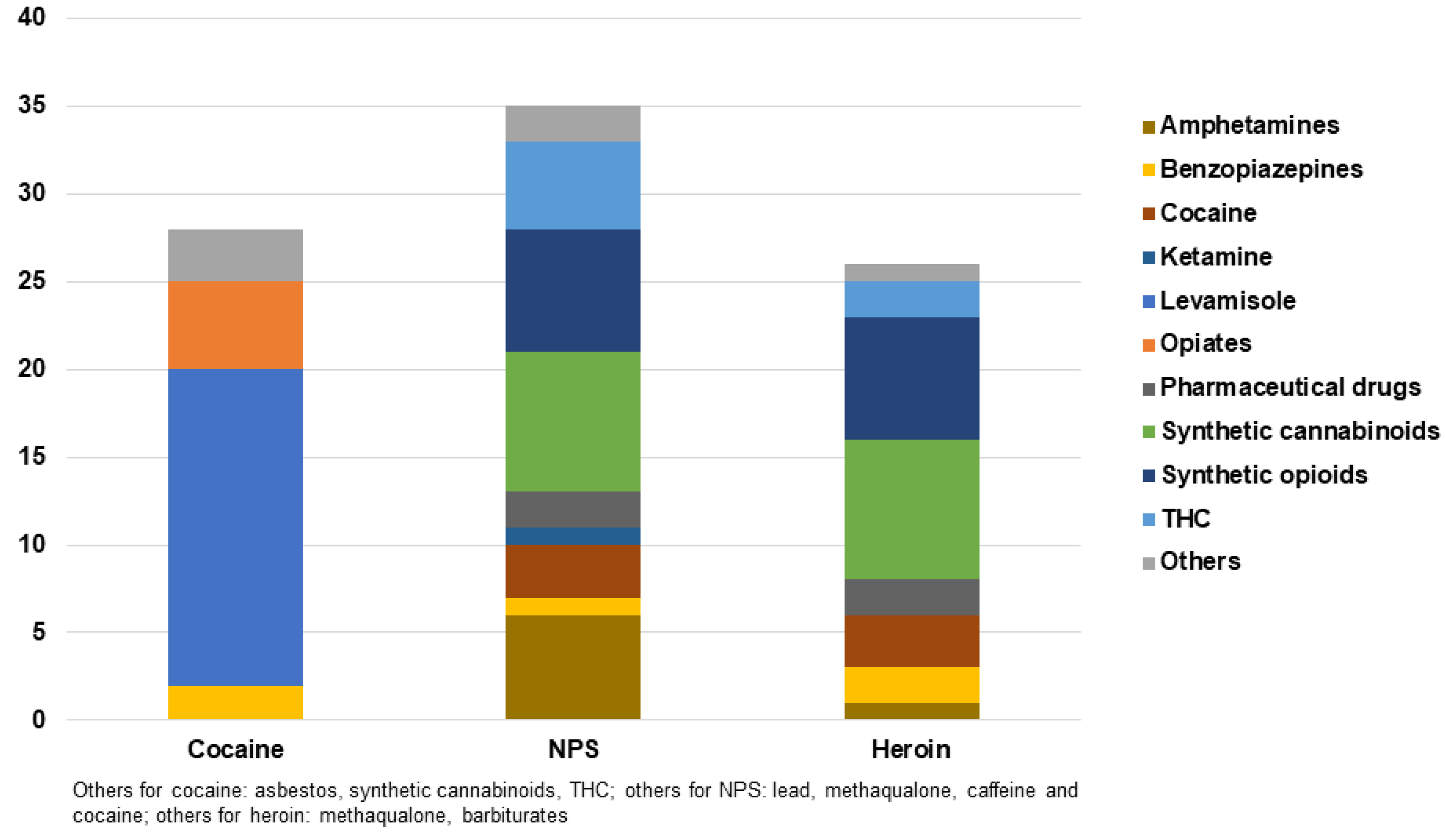
2.1. Non-Biological Samples
2.2. Biological Samples
2.3. Case Series Reports
| Drug Class #Cases | Adulterant #Cases | Analysis | Seizure Yrs Country | Ref. | Drug Class #Cases | Adulterant # Cases | Analysis | Seizure Yrs Country | Ref. | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Cocaine | Opioids | ||||||||||
| 1 | 7841 | Levamisole; phenacetin; caffeine; lidocaine | GC-MS | 2006–2015 Switzerland | [20] | 33 | Fentanyl 2 | U-47700; lidocaine; heroin; 6-AM; methoxyacetyl fentanyl; phenyl fentanyl; codeine; methacryl fentanyl; caffeine | GEMBE | 2019 USA | [27] |
| 2 | 728 | Levamisole 433; phenacetin 323; aminopyrine 60; benzocaine 29; lidocaine 22; caffeine 21 | FTIR-MCR-ALSGC-FID | 2009–2015 Brazil | [21] | 34 | Fentanyl 46 | Xylazine 46 | GC-MS LC-HRMS/MS | 2020 Australia | [28] |
| 3 | 24 | Tetramisole 23; levamisole 1 | LC-MS/MS | 2013–2016 Switzerland | [43] | 35 | Heroin 4 | Ocfentanil 4; caffeine 4; paracetamol 4 | GC-MS LC-MS/ MS | 2015 Spain | [30] |
| 4 | 351 | Levamisole 214; lignocaine 103; meth 13; MDMA 10; phenacetin 7; benzocaine 6; THC 4; amphetamine 1; heroin 2 | GC-MS | 2015–2016 Canada | [12] | 36 | Heroin 217; cocaine 19; amphetamine 367 | Caffeine 852; nicotine 244; acetaminophen 261; levamisole 8 | GC-MS | 2015–2016 Hungary | [44] |
| 5 | 292 | Levamisole 292 | SVM-DA GC-FID | 2015 Belgium | [37] | 37 | Heroin 11 | Meth 7; dextromethorphan 3; cocaine 2; diazepam 1 | GC-MS | 2015–2016 Canada | [12] |
| 6 | 97 | Levamisole 92; phenacetin 22; caffeine 14; hydroxyzine 10; benzocaine 6 | GC-MS GC-TMS UPLC-MS/MS | 2016–2017 USA | [17] | 38 | Heroin 10 | Lead 10; caffeine 8; chloroquine 3; methadone 3; phenobarbital 2; tramadol 2; acetaminophen 1; meth 2 | HPLC-MS GC-MS FAAS | 2016–2017 Iran | [15] |
| 7 | 17 | Caffeine 11; lidocaine 10; acetaminophen 9; phenacetin 7; diltiazem 4 | HPLC-DAD | 2017 Brazil | [22] | 39 | Heroin 198 | Quinine/quinidine 44; fentanyl 31; lidocaine 24; caffeine 21; levamisole 20; phenacetin 12 | GC-MS LC-Q-ToF | 2017 USA | [13] |
| 8 | 96 | Levamisole 30; lidocaine 26; phenacetin 13; caffeine 11; quinine/quinidine 12 | GC-MS LC-Q-ToF | 2017 USA | [13] | 40 | Heroin 7 | Acetaminophen 4; caffeine 4; fentanyl 1 | GC-MS | 2018 UK | [29] |
| 9 | 3 | Caffeine 3 | Colorimetric GC-FID | 2018 Brazil | [21] | 41 | Heroin 30 | Caffeine 30; noscapine 26; papaverine 22; paracetamol 16; lidocaine 2; dextromethorphan 5 | GC-MS GC-FID SWV | 2018 Belgium | [72] |
| 10 | 50 | Levamisole 17; lidocaine 16 | CE-C4D | 2018 Brazil | [23] | 42 | Heroin 3 | Caffeine 1 | GC-MS GC-VUV | 2019 USA | [38] |
| 11 | 3 | Levamisole 3 | SWV HPLC-MS GC-MS GC-FID NMR | 2018 Belgium | [36] | 43 | Heroin 59 Meth 26 Oxycodone | Caffeine 7 | GC-MS | 2019 Australia | [39] |
| 12 | 3 | Levamisole 3 | CV | 2018 Belgium | [14] | 44 | Heroin 659 | Paracetamol 656; caffeine 656 | GC-MS HPLC-UV LC-Q-ToF | 2019–2020 Luxembourg | [16] |
| 13 | 7 | Levamisole 5; Phenacetin 3; caffeine 2; procaine 1; tetracaine 1 | GC-MS NMR | 2018 France | [24] | 45 | Heroin 1 | 4-AP-t-BOC (tert-butyl-4-anilinopiperidine-1-carboxylate) | GC-MS LC-MS | 2019–2020 Ireland | [40] |
| 14 | 156 | Levamisole 58; caffeine 39; quinine/quinidine 27; diphenhydramine 20; phenacetin 17; acetaminophen 17; lidocaine 16; procaine 13; diltiazem 10; xylazine 4; atropine 2; aminopyrine 4; hydroxyzine 3; dipyrone 2; guaifenesin 1; gabapentin 1 | GC-MS LC-Q-ToF | 2018 USA | [25] | 46 | Opium 10 | Lead 10; acetaminophen 8; chloroquine 4; tramadol 2 | HPLC-MS GC-MS FAAS | 2016–2017 Iran | [15] |
| 15 | 47 | Levamisole; phenacetin; lidocaine; caffeine | DART-HRMS | 2019 China | [18] | 47 | Opium 10 | Lead 10 | AAS | 2015–2016 Iran | [31] |
| 16 | 1078 | Levamisole 584; phenacetin 386; caffeine 113; lidocaine; ketamine; hydroxyzine | GC-MS HPLC-UVLC-Q-ToF | 2019–2020 Luxembourg | [16] | 48 | Morphine 6 | Codeine 4; thebaine 2; papaverine 2; noscapine 2; 6-AM 1; heroin 1; oxycodone 1; acetylcodeine 1; fentanyl 1; alprazolam 1 | GC-MS | 2015–2016 Canada | [12] |
| 17 | 169 | Phenacetin 169 | GC-EA-IRMS | 6 yrs France | [41] | 49 | Fentanyl 100 | Caffeine 96; etizolam 50; carfentanil 8; cocaine 7; heroin 6; acetyl fentanyl 1 | IR SERS PS-MS | 2018–2022 Canada | [73] |
| 18 | 306 | Phenacetin 231; caffeine 196; aminopyrine 82; levamisole 16; lidocaine 5; benzocaine 1 | GC-MS-QP HPLC-DAD | 2019 Uruguay | [19] | NPS | |||||
| 19 | 45 | Caffeine 32; phenacetin 30; levamisole 27; lidocaine 15 | GC-MS | 2020 Colombia | [42] | 50 | 3-MEC | 3-MeO-PCP; 4F-α-PVP; DiPT; ketamine | LC-Q-ToF NMR | 2010–2014 Sweden | [33] |
| Amphetamines stimulants | 51 | 4-Aco-DMT | DPT | LC-Q-ToF NMR | 2010–2014 Sweden | [33] | |||||
| 20 | Amphetamine 28 | Meth 25; DMA 14; MDMA 2; cocaine 1; methylphenidate 1; lignocaine 1 | GC-MS | 2015–2016 Canada | [12] | 52 | 4-Meo-PCP | 3-MeO-PCP | LC-Q-ToF NMR | 2010–2014 Sweden | [33] |
| 21 | Ecstasy 10 | Lead 10; meth 4; heroin 2 | HPLC-MSGC-MS FAAS | 2016–2017 Iran | [15] | 52 | 4-MeO-PCP 2 | AB-FUBINACA 2; nicotine 2; ketamine 2; amitriptyline 2 | LC-Q-ToF NMR | 2010–2014 Sweden | [33] |
| 22 | MDMA 211 | Unspecified 104; methylone 35; synthetic cathinones 21; methamphetamine 13; benzylpiperazine 8; dextromethorphan 8; mephedrone 5; Amphetamine 4 butylone 4; cocaine 4; ketamine 1; MeO-amphetamine 3; LSD 1 | Colorimetric | 2010–2015 USA | [32] | 53 | 4-OH-MET | Methoxetamine | LC-Q-ToF NMR | 2010–2014 Sweden | [33] |
| 23 | MDMA 122 | Ethylone 189; meth 34; MDA 16; cocaine 10; 5-Meo-DALT 8; phenethylamine 7; 2C-T-2 6; DMA 5; dibutylone 3; DMT 2; amphetamine 2; methylone 2 sildenafil 2; THC 1 methoxetamine 1; 2C-B 1; MDDM 1; | GC-MS | 2015–2016 Canada | [12] | 54 | α-MT | MDPBP; 25B-NBOME | LC-Q-ToF NMR | 2010–2014 Sweden | [33] |
| 24 | MDMA 6 | Caffeine; lidocaine | GC-MS Raman Spectroscopy | 2020 Brazil | [74] | 55 | Butyrylfentanyl 2 | Fentanyl 2; acetylfentanyl 2; 4-ANPP 2 | LC-Q-ToF NMR | 2010–2014 Sweden | [33] |
| 25 | MDMA 302 | Unknown 259; dimethylsulfone 36; dimethylsulfone and Caffeine 2; ketamine 2; MDEA 1; cocaine and ketamine 1; N-Moc-MDMA and T-Boc-MDMA 1 | GC-MS/MS | 2019–2020 Australia | 56 | Ethylphenidate | 5-Meo-DALT; caffeine; phenacetin; lidocaine | LC-Q-ToF NMR | 2010–2014 Sweden | [33] | |
| 26 | Methamphetamine 181 | N-isopropyl benzylamine 37; DMA 30; amphetamine 24; cocaine 15; α-PHP 1; DMMA 1; N-Me-2AI 1; ethylphenidate 1; phenethylamine 1; praziquantel 1; 25C-NBOME 1; 25I-NBOME 1; ketamine 1; methoxetamine 1; MDMA 36; THC 36; heroin 3; diazepam 3; alprazolam 1; quetiapine 5; lignocaine 7 | GC-MS | 2015–2016 Canada | [12] | 57 | Isopropylphenidate | Methylphenidate | LC-Q-ToF NMR | 2010–2014 Sweden | [33] |
| 27 | Methamphetamine 10 | Lead 10; phenmetrazin e 6; pseudoephedrine 5; caffeine 3; dextromethorphan 3; ketamine 1; MDMA 1 | HPLC-MSGC-MS FAAS | 2016–2017 Iran | [15] | 58 | MDMB-CHMICA | AMB-FUBINACA; 1-(cyclohexylmethyl)-1H-indole-3-carbonyl)valine | LC-Q-ToF NMR | 2010–2014 Sweden | [33] |
| 28 | Methamphetamine 219 | Phenacetin 3; caffeine 2; diltiazem 2 | GC-MS LC-Q-ToF | 2017 USA | [13] | 59 | MET | 3-MeO-PCP/ 4-MeO-PCP; 4-AcO-DMT; 3-MEC; 4F-α-PVP; Ketamine | LC-Q-ToF NMR | 2010–2014 Sweden | [33] |
| Cannabinoids | 60 | Mitragynine | Caffeine | LC-MS/ MS | 2010–2014 Sweden | [33] | |||||
| 29 | ∆9-THC 9 | Cocaine 4; 4-F-AMB 3; MDMA 1; methamphetamine 1; 5-UR-144 1; 5F-AKB48 1; desvenlafaxine 1 | GC-MS | 2015–2016 Canada | [12] | 61 | NM2201 and THJ-018 | MDMB-CHMICA | LC-Q-ToF NMR | 2010–2014 Sweden | [33] |
| 30 | ∆9-THC 1142 | MDMB-4en-PINACA 270 | GC-MS HPLC-MS UPLC-QToF TLC UPLC-MS3 UPLC-DAD FTIR MALDI-HRMS | 2020–2021 Europe | 62 | THJ-018 | MDMB-BB-22 | LC-Q-ToF NMR | 2010–2014 Sweden | [33] | |
| Opioids | 63 | 2C-B 46 | 5-MeO-DALT 46; MDMA 1 | GC-MS | 2015–2016 Canada | [12] | |||||
| 31 | Crack heroin 10 | Lead 10 | AAS | 2015–2016 Iran | [31] | 64 | NEP 10 | Caffeine 10 | GC-MS Raman spectroscopy | 2020 Brazil | [31] |
| 32 | Fentanyl and analogs 26 Heroin 5 | Caffeine 33; AMB-FUBINACA 29; heroin 17; phencetin 10; etizolam 6 AB-FUBINACA 5; fentanyl analogs 6 benzocaine 3; 5F-MDMB-PINACA 3 metformin 2; meth 3 lidocaine 1; acetaminophen 3; dextromethorphan 2; 4Cl-α-PVP 1; UF-17 1; furanyl 5F-MDMB-PICA 1; hydromorphone 1; flubromazolam 1 | FTIR Fentanyl immunoassay GC-MS LC-HRMS/MS LC-MS | 2018–2019 Canada | [42] | ||||||
| Clinical Description | Adulterant | Adulterant Analysis | Matrix | Drug Analysis ng/mL | Ref. |
|---|---|---|---|---|---|
| Cocaine | |||||
| Hx: 52 y F chronic cocaine user admitted with ulcers on extremities; pustule, rash on arms/axilla/temple; longstanding perforation hard palate Lab: c-ANCA+; LA+ Skin biopsy: superficial neutrophil-rich dermal infiltrate, papillary derma edema Dx: pyoderma gangrenosum associated with LAC Tx: prednisone, topical betamethasone | Levamisole * | NA | U | Cocaine + | [54] |
| Hx: 31 y F cocaine user admitted with facial pain, chronic fronto-maxillary sinus pain, yellow/green discharge, rhinorrhea, crusting, rash legs Lab: ESR 2 mm/h; CRP 24 mg/L; WCC 7.7; p-ANCA+; c-ANCA-; anti-PR3+; anti-MPO Nasal biopsy: ulceration, necrosis surrounded macrophages and fibrotic stroma; chronic inflammatory infiltrate, no vasculitis Dx: CIMDLs, systemic levamisole vasculitis Tx: abstinence, mycophenolate, azathioprine, rituximab, surgical debridement | Levamisole * | NA | U | Cocaine + | [44] |
| Hx: 30 y F cocaine user, chronic sinusitis, left deviated septum, rhinitis, purulent rhinorrhea, macular rash on hands; Lab: ESR 5 mm/h; CPR 30 mg/L; WCC 11.1; p-ANCA+; c-ANCA-; anti-MPO-; anti-PR3- Nasal biopsy: ulceration, acute/chronic inflammation, fibrotic stroma, vessels permeated by inflammatory cells, no fibrinoid necrosis Dx: CIMDLs and systemic levamisole vasculitis Tx: abstinence, drug rehabilitation, surgical debridement | Levamisole * | NA | U | Cocaine + | [44] |
| Hx: 36 y M cocaine user, severe facial pain, epistaxis, crusting, rhinorrhoea, rash/livedo in thighs; hematuria, proteinuria Lab: ESR 36 mm/h; CPR 44 mg/L; WCC 8.0; p-ANCA+; c-ANCA-; anti-MPO-; anti-PR3-; IgG4 increase Nasal biopsy (n = 3): extensive ulceration, fibrin, proliferative fibrosis; acute/chronic inflammatory cells; no vasculitis (1st); geographic necrosis, fibrinoid necrosis foci (2nd); ulcerated mucosa and granulation; no vasculitis (3rd); Dx: CIMDLs and systemic levamisole vasculitis Tx: abstinence, steroids; methotrexate; mycophenolate; rituximab, surgical debridement | Levamisole | NA | U | Cocaine +; levamisole + | [44] |
| Hx: 48 y F, severe facial pain, epistaxis, septal perforation with fistula from skin to intra-nasal cavity, soft palate ulceration; hematuria Lab: ESR 80 mm/h; CPR 48 mg/L; WCC 7,6; p-ANCA+; c-ANCA-; anti-MPO-; anti-PR3 + Dx: CIMDLs and systemic levamisole vasculitis Tx: abstinence, steroids, methotrexate, surgical debridement | Levamisole | NA | U | Cocaine +; levamisole + | [44] |
| Hx: 48 y M, previous Chron’s disease and pneumonia, admitted with purpuric rash worsening in four limbsLab: c-ANCA+; ANA+; anti-MPO- Skin biopsy: leukocytoclastic vasculitis and multiple fibrin thrombi; Dx: levamisole adulterated cocaine-associated vasculitis Tx: supportive therapy | Levamisole * | NA | U | Cocaine + | [60] |
| Hx: 53 y F cannabis/cocaine user, admitted with extensive, painful retiform symmetric purpura patches in limbs, buttocks/abdomen with necrosis evolution Lab: neutropenia, thrombocytopenia, CPR 13 mg/L; LA-; anticardiolipin antibody-; cryoglobulins-; c-ANCA+ Skin biopsy: thrombotic vasculopathy Dx: levamisole-induced vasculitis Tx: corticosteroids, surgical debridement of necrotic tissue | Levamisole * | NA | U | Cocaine +; THC + | [61] |
| Hx 46 y M, increased cocaine use last 3 months, admitted with weakness/fatigue, blood-tinged sputum, cough Lab (n = 2) creatinine 9.61; GFR 7 mL/min; K+ 7 meq/L (1st); AST 196; ALT 235; total bilirubin 13; A-phosphatase 520 (2nd); ANA+; p-ANCA+; c-ANCA+; anti-α-SME+; anti-HCV+; HCV-RNA- CT chest: cavitary lesions Renal biopsy: fibrous glomerular crescents, few cellular crescents (severe kidney damage) Liver biopsy: isolated intrahepatic bile duct with onion skinning and foci injury, canalicular cholestasis, periportal ductal reaction Dx: intrahepatic duct injury associated with LAC-induced glomerulonephritis Tx: dialysis for AKI; ursodeoxycholic/cholestyramine for duct damage | Levamisole * | NA | U | Cocaine + | [62] |
| Hx: 29 y M, 3 months cocaine abuse, admitted with severe head-pain, incomprehensible vocalization, amnesia, aggressiveness, agitation, sleep inversion, space/time disoriented; MRI brain (n = 2): ubiquitous white matter small lesions (1–14 d after adm); additional punctate lesions in corpus callosum, abn meningeal enhancement, contrast agent in CSF (15–31 d after adm); CSF: protein 224 mg/dL; albumin 37.9; RFA: multiple segmental occlusion in central retinal artery Audiogram: bilateral sensorineural hearing loss; Dx: acute SS associated to LAC; Tx: methylprenisolone, mycophenolate (at brain damage relapse) | Levamisole | UPLC-ESI+-MS/MS | H segments (n = 6) | Cocaine >5; BE > 5; EME 0.07–0.11; norcocaine 0.58–1; levamisole 0.07–1.14; tramadol 1.38–2.16 | [45] |
| Hx: 33 y M cocaine abuse history, admitted with 4 weeks of nasal obstruction, dysphagia, otalgia, nasal bridge deformity; Endoscopy: nasal corridor necrosis; CT head/chest: nasal cavity extensive bone destruction, multiple small pulmonary nodules; Lab: leukocytosis, high CRP, high ESR; c-ANCA+; Nasal biopsy: no vasculitis signs; Dx: CIMDL; Tx: counseling on cocaine cessation | Levamisole * | NA | U | Cocaine +; metabolites + | [57] |
| Hx: 59 y M active cocaine use, anamnestic febrile syndrome with neutropenia/agranulocytosis treated and recovered; new ED admission with 4 days abdominal pain/bloody diarrhea probably due to rectal cocaine administration CT abdomen: rectum/sigmoid/descending colon/caecum/appendix with increased bowel wall thickness Flexible sigmoidoscopy: sigmoid colon/rectum edema, severe ulceration; bowel ischemia/necrosis Lab: normal ENA and ANCA+ Dx: neutropenia agranulocytosis induced by levamisole complicated by bowel necrosis Tx: surgery sigmoid colectomy, ileocecectomy with end ileostomy and descending mucus fistula | Levamisole * | NA | U | Cocaine + | [46] |
| Hx: 53 y M crack cocaine user, anamnestic hypertension/dyslipidemia/chronic pain syndrome, developed 2 wks limb rash/hematuria/creatinine increase (150 µmol/L); ED admission with abdomen/thighs/legs purpura and ear necrosis Lab: urea 24.8 mmol/L; cr 449; PCR 186.8 mg/mmol; Na = 137 mmol/L; K+ = 4.9 mmol/L; ANA -; ENA -; c-ANCA -; p-ANCA +; HCV/HBV/HIV neg; Renal biopsy: active focal crescentic and necrotizing GN, glomerular capillary wall thickening; tubular epithelial injury; no active vasculitis Dx: concurrent AAV secondary to LAC and associated MN Tx: corticosteroids, ACE inhibitor | Levamisole * | CEDIA | U | Cocaine metabolites (s) + | [58] |
| Hx: 35 y M tobacco/cannabis smoker, intranasal cocaine use, inhaled crack use; admitted to ED with hemoptysis, iron deficiency anemia CT chest: bilateral ground glass opacities; Lab: urea 7.1 mmol/L; Cr 150 µmol/L; Na 136 mmol/L; K+ 4 mmol/L; ANA -; c-ANCA -; p-ANCA +; cryoglobulinus -; HBV/HCV/HIV neg; Renal biopsy: active segmental fibrinoid necrosis, no arteries vasculitis, diffuse epithelial cell foot process effacement and deposit of immune complex; Dx: concurrent AAV secondary to LAC and associated MN; Tx: prednisone, cyclophosphamide | Levamisole | CEDIA and LC-MS | U | Cocaine metabolite (s) +; cannabinoids, opiates, benzodiazepines, levamisole (c) + | [58] |
| Hx: 34 y M cocaine user; anamnestic obesity, hyperpigmented lesions, leukocitoclastic vasculitis due to levamisole; recently admitted to ED with proteinuria associated with fatigue/arthralgias Lab: urea 4.6 mmol/L; Cr 71 µmol/L; PCR 449.9mg/mmol; Na+ 140 mmol/L; K+ 4.4 mmol/L; ANA-; ENA-; c-ANCA-; p-ANCA+; HBV/HCV/HIV neg Renal biopsy: no glomerular crescentic or necrotizing injury, glomerular artery wall normal, no artery vasculitis Dx: development of MN after AAV secondary to LAC | Levamisole | CEDIA and LC-MS | U | Cocaine metabolites (s) +;opiates +; benzodiazepines +; levamisole (c) + | [58] |
| Hx: 68 y M cocaine user, recent haemorrhagic lesions on forearms/face, anamnestic analogous vasculitis 6 months prior Lab: pancytopenia/neutropenia; ANA+; p-ANCA+; anti-PR3+; anti-MPO+ Skin biopsy: leukocytoclastic vasculitis with subepidermal bullae Dx: levamisole-induced vasculitis Tx: 6 months cocaine abstinence | Levamisole * | NA | U | Cocaine + | [47] |
| Hx: 58 y M polysubstance user presented 4 d after last cocaine use with painful pruritic rash/polyarthralgyas Lab: high CRP, leukopenia; p-ANCA-; c-ANCA-; ANA-; RA-; HCV/HIV neg Skin biopsy:acute/chronic inflammation of superficial derma, acute perivascular inflammation in deeper derma; acute leukocytoclastic vasculitis; eosinophilic infiltrate Dx: cutaneous levamisole induced vasculitis Tx: steroids | Levamisole | LC-MS/MS | U | Cocaine +; levamisole (c)+ | [33] |
| Hx: 40 y F tobacco and cocaine smoker, methadone and hydroxyzine user; anamnestic HCV+, previous septic shock; admitted with extensive retiform purpura/ bullous necrotic lesion legs/nose/ear/cheeks Lab: lactate elevated; PCR 180 mg/L; p-ANCA+; ANA+; LA+; cryoglubulinaemia+; RF+; HBV/HIV neg; HCV pos Skin biopsy: vasculitis, microthrombi/fibrinoid degeneration of vascular walls Dx: transient renal failure, extensive levamisole induced vasculitis | Levamisole | LC-MS/MS | U | Opiates; cocaine; methadone + | [59] |
| H segments (n = 2) | Levamisole 1–1.78 ng/mg | ||||
| Hx: 39 y F intravenous cocaine user dead in bathroom with recent needle marks Autopsy: pulmonary edema, brain/heart/coronary vessels/aorta/kidneys moderately congested COD: cardiorespiratory arrest due to intravenous cocaine and foreign body pulmonary granuloma Histology: foreign bodies (asbestos fibers) in pulmonary parenchyma associated with non-necrotising granulomas in lung Dx: pulmonary granulomatosis due to asbestos fibers related to intravenous cocaine | Asbestos fibers in lung | Histology | VH | Cocaine 40 | [53] |
| B | BE 300 | ||||
| Hx: about 20 y M after white drug insufflation (sold as cocaine); presented at ED with hypertension; combative/delirious behaviour; decreased level of consciousness; Clinical: GCS = 7/15–13/15; pin-pupils; systolic pressure = 123 mmHg; HR = 85; Dx: poisonings with LSD after nasal insufflation of a white powder sold as cocaine; Tx: intravenous droperidol; midazolam; intubation (for 12 h). | LSD | UHPLC-Q-ToF | U | Cannabis; benzodiazepine +; ketamine +; | [48] |
| UHPLC-MS/MS | B | LSD 60; THC-COOH 38 | |||
| Hx: about 20 y M history of cocaine and THC as recreational use; after white drug insufflation (as cocaine); his thoughts were “foggy”; sedation; Clinical: GCS = 13/15; pin-pupils; BP = 130/70 mmHg; HR = 64; vomiting develops hypokalaemia (K 2.9 mmol/L). Dx: poisonings with LSD after nasal insufflation of a white powder sold as cocaine; Tx: anti-emetics; anticonvulsant | LSD | UHPLC-Q-ToF | U | Cannabis +; amphetamines +; | [48] |
| UHPLC-MS/MS | S | LSD 60; MDMA 20 | |||
| Hx: about 20 y M past recreational use of cocaine/LSD; before white drug insufflation (sold as cocaine); smoked THC; drunk alcohol; reported thoughts-clouding; sensation of dying; vivid hallucinations; sedation; Clinical: HR = 97; BP = 227/145 mmHg; pin-pupils; GCS = 14/15; vomiting developing hypokalaemia (K 2.8 mmol/L); Dx: poisonings with LSD after nasal insufflation of a white powder sold as cocaine; Tx: diazepam; droperidol | LSD | UHPLC-Q-ToF | U | THC +; amphetamines + | [48] |
| UHPLC-MS/MS | B | LSD 40; MDMA 10; THC-COOH 22; | |||
| Hx: about 20 y M 10–15 min after white drug insufflation (sold as cocaine) developed hypersalivation; palpitations; nausea; dissociative state; Clinical: pin-pupils; Dx: poisonings with LSD after nasal insufflation of a white powder sold as cocaine Tx: diazepam | LSD | UHPLC-MS/MS | B | LSD < 5; MDMA < 30; THC-COOH < 3 | [48] |
| Heroin | |||||
| Hx: 28 y M 7 yrs cannabis/tobacco use disorders; 2 yrs inhaled heroin use; Due to reduced heroin supply and high cost used “CUT” heroin to save money and discover new drug; ED admission with time/space disorientation, confused; outburst at minimal provocation; pupils constricted/symmetrical; slurring speech, saliva drooling; wide-based gait, staggering/stumbling; unable to perform a tandem walk; Brain MRI: no detectable lesions Lab: ALT 271 U/L; ASL 148 U/L; urea 34 mg/dL; Cr 0.86 mg/dL; anti-HCV-; HCV-RNA 7.27000/mm3; HIV/HBV neg Dx: cognitive–behavioural and neurological symptoms due to CUT agent; Tx: sublingual buprenorphine–naloxone for 7 months | Methaqualone, caffeine, oxazepam, Ketazolam, nordazepa, pinazepam, alprazolam, acetaminophen | GC-MS | U | Morphine; benzodiazepines | [55] |
| CD | acetaminophen; caffeine; methaqualone; Oxazepam; ketazolam; nordiazepam; pinazepam, alprazolam | ||||
| Hx: 28 y M anamnestic with treated bipolar disorder, polysubstance abuse including intravenous heroin, found unresponsive at home with packets of “Santa Muerte”; on arrival typical initial opioid toxidrome Clinical: SpO2 78%; tachycardia, flushing, dry mucous membranes, mydriasis Chest X-ray chest: pneumonia and ARDS CT brain: negative Dx: anticholinergic toxicity after heroin containing 5F-MDMB-PINACA, pneumonia/ARDS Tx: after 2 doses of naloxone, became agitated and combative; OI for 12 d | 5F-MDMB-PINACA | LC-MSMS | S | Cocaine +; 6-MAM +; heroin +; fentanyl +; THC +; alprazolam + | [52] |
| Immunoassay | U | Cocaine; opiates; fentanyl; THC; benzodiazepines | |||
| GC-MS and LC-Q-ToF | CD | 5F-MDMB-PINACA; Heroin; Fentanyl | |||
| Hx: 25 y M intravenous heroin abuse; admitted at ED for typical opioid toxidrome after intravenous ‘heroin’ injection; Clinical: HR = 102 b/m; BP = 146/89 mm Hg, RR = 24 breaths/min; SpO2 = 98%, flushing, tachycardia, agitation; Dx: anticholinergic toxicity after heroin containing 5F-MDMB-PINACA; Tx: 2 doses of naloxone, became anxious and tachycardic so EV lorazepam was added; intravenous fluids, supportive care. He confirmed Santa Muerte use. | 5F-MDMB-PINACA | Immunoassay | U | Opiates+; amphetamine+; barbiturates +; cocaine+ | [52] |
| GC-MS/LC-Q-ToF-MS | CD | 5F-MDMB-PINACA; Heroin; fentanyl | |||
| Hx: 31 y M history of intravenous heroine abuse; admitted at ED after intravenous “heroin” injection associated to typical opioids overdose symptoms; Clinical: HR = 163 b/m; BP = 131/81 mmHg, RR = 29 breaths/minute, SpO2 99%; tachycardic, flushed, dilated pupils; full bladder; Dx: anticholinergic toxicity after heroin containing 5F-MDMB-PINACA, and ARDS; Tx: after naloxone, became combative, anxious, agitated, so intravenous lorazepam was added; intubated for airway protection | 5F-MDMB- PINACA | Immunoassay | U | Opiates | [52] |
| LC-MS-MS | S | Heroin; 6-MAM, fentanyl | |||
| GC-MS/LC-Q-ToF-MS | CD | 5F-MDMB-PINACA; heroin; fentanyl | |||
| Hx: 25 y M admitted at ED after intravenous heroin (found a drug packet labeled “Santa Muerte”); Clinical: HR = 158 b/m; BP = 215/158 mm Hg; RR = 26 breaths/minute; SpO2 = 99%; urinary retention; anhidrosis; Dx: anticholinergic toxicity after heroin containing 5F-MDMB-PINACA; Tx: naloxone; afterwards tachycardia/agitation; so lorazepam and physostigmine to calm him down; | 5F-MDMB- PINACA | Immunoassay | U | Cocaine; opiates; THC | [52] |
| LC-MS/MS | S | 5F-MDMB-PICA (5F-ADB); heroin; 6-MAM; fentanyl; | |||
| GC-MS LC-Q-ToF/MS | CD | 5F-MDMB-PINACA; heroin; fentanyl | |||
| Hx: 45 y M presented at ED with tachycardia; pinpoint pupils; flushing of skin; drug packet “50 CAL” found in his pocket; Clinical: HR = 124 b/m; BP = 140/82 mmHg; RR = 22 breaths/minute; SpO2 = 99%; pinpoint pupils; flushing of skin; Dx: anticholinergic toxicity after heroin containing 5F-MDMB-PINACA; Tx: midazolam/olanzepine to calm; afterward intravenous diazepam; dexmedetomidine infusion in case of agitation returning; 24 hrs in hospital | 5F-MDMB-PINACA | Immunoassay | U | Opiates; fentanyl | [52] |
| GC-MS LC-Q-ToF/MS | CD | 5F-MDMB-PINACA; heroin; fentanyl | |||
| Hx: 36 y M found unresponsive in the street; after naloxone; agitation; benzo/physostigmine with improvement in agitation behaviour. Clinical: HR = 130 b/M; BP = 160/100 mm Hg; RR = 24 breaths/minute; oxygen saturation 95%; Dx: anticholinergic toxicity after heroin containing 5F-MDMB-PINACA; Tx: naloxone; benzo/physostigmine; intubated to avoid to risk of aspiration from vomiting; found blue packet (“50 CAL”). | 5F-MDMB- PINACA | Immunoassay | U | Opiates; fentanyl | [52] |
| GC-MS and LC-Q-ToF | CD | Fentanyl; heroin; 5F-MDMB-PINACA | |||
| Hx: 23 y F admitted at ED for severe agitation/combative behavior; Clinical: HR = 156 b/m; BP = 147/64 mm Hg; RR = 20 breaths/minute; Dx: anticholinergic toxicity after heroin containing 5F-MDMB-PINACA; Tx: lorazepam/physostigmine. The patient reported consuming a substance named “50 CAL.” | 5F-MDMB- PINACA * | Immunoassay | U | Opiates; fentanyl | [52] |
| Hx: 27 y M presented at ED after intravenous heroin use; he was admitted with respiratory and CNS depression; Clinical: HR = 130 b/M; BP = 130–94 mm Hg; RR = 22 breaths/minute; sPO2 = 95%; dilated pupils; dry oral mucous membrane Tx: lorazepam; physostigmine. Dx: anticholinergic toxicity after heroin containing 5F-MDMB-PINACA | 5F-MDMB- PINACA * | Immunoassay | U | Opiates; fentanyl | [52] |
| Hx: 36 y F 3 yrs oral opium abuse (dose = 0.3 gr/day); presented at ED with nausea; acute/severe abdominal pain; vomiting; pleuritic chest pain; Clinical: severe hypochromic-microcytic anemia; CT abdomen: multiple radiopaque flakes in intestinal lumen and in its wall due to metal deposition; Dx: lead poisoning in oral opium user; Tx: intravenous chelators (Ca Na2 EDTA) | lead | NA | B | Lead 780; lead (7 day after) 460 | [49] |
| Γ-hydroxybutyrate (GHB) | |||||
| Hx: 29 y M and 34 y M bought two GHB doses that were dissolved in 200 mL of alcohol each; 1st case drunk the whole drink in 10 min; 2nd case drunk 2/3 of his drink; Clinical: after 20 min 29 y began to accuse chest pain; tachycardia; short of breath; 34 y accused just headache. Dx: acute intoxication GHB and SLD | SDF | B | GHB 55–100 (case 1); 37–800 ng/mL (case 2); SDF 340 (case 1), SDF< LOQ; desMe-SDF < LOQ; desMe-SDF < LOQ | [50] | |
| U | GHB: 35;700 and 15;500; SDF = 1;270 and SDF 1;220 desMe-SDF = 810 and 1;210 | ||||
| Drink | GHB 7460;7 μg/mL; SDF 521;2 μg/mL | ||||
| Alprazolam | |||||
| Hx: 49 y M past substance abuse; found dead in his bed; nearby the corpse; a glass with dried; white; crystalline substance; on a shelf/living room; 2 plastic-bags containing white tablets (imprint XANAX); Autopsy: heart; lungs; liver; kidney: sign of decomposition; COD: acute intoxication of caffeine and etizolam. | Etizolam and caffeine | GC-MS and HPLC-DAD | FB | Etizolam = 770; caffeine = 190 Etoh 24 mg/mL | [51] |
| CB | Caffeine 426 mg/mL | ||||
| U | THC-COOH 192 | ||||
| H segments (n = 4) | Etizolam 0.05–0.11; THC 0.06–0.19; amphetamine 0.42–2;568; cocaine 0.03–0.22. BEG 0.04–0.07 | ||||
| Stomach content | Etizolam + | ||||
| Drug | Caffeine; etizolam | ||||
| Kratom | |||||
| Hx: 54 y M past history of HCV treated; alcohol use disorder; OUD; admitted at ED with altered mental status after 1 spoon of “Kratom crazy®®” taken for an entire year; in morning he added a table spoon of “Vivazen Botanical De Kratom®®”; headache; vomit; fall asleep; when he woke up; he had incomprehensible speech. Clinical: BP = 120/70 mmHg; HR = 70; RR 18; sPo2 = 98%; Lab: glucose = 124 mg/dL; leukocytosis; troponin T = 91 ng/L; CT brain: large right frontal intraparenchymal haemorrhage with extension to ventricles (40 cm3) and mass effect; MRI brain: intraparenchymal hemmorrhage with 7 mm midline shift. Dx: PEA-adulterated kratom intoxicationTx: surgical craniotomy | PEA | LC-MS/MS | S | Mitragynine 340 | [56] |
| LC-HRMS/MS | CD | PEA | |||
| Number of Cases | Adulterant | Analytical Technique | Matrices | LOD (ng/mL) | LOQ (ng/mL) | Quantification (ng/mL) | Reference |
|---|---|---|---|---|---|---|---|
| DUID (n = 724) | Levamisole; PTHIT | LC-MS/MS | H | 2.5 pg/mg | 10 pg/mg | Cocaine 500–800.000 pg/mg (n = 627); PTHIT 3.5–61,000 pg/mg; levamisole/dexamisole 0.71–1.34 | [43] |
| DUID (n = 55) | Caffeine DZ; hydroxyzine; levamisole; lidocaine; benzocaine; diphenhydramine; phenazone; procaine | SWATH LC-HRMS | U | __ | __ | THC + (n = 19) THC, cocaine + (n = 19); cocaine + (n = 17) | [65] |
| U (n = 100) PL (n = 8) | Levamisole Aminorex | LC-HRMS | U PL | ___ | 1 0.1 | U: levamisole (n = 72) average conc.= 565 (4–72,970 µg/L); BE (n = 100) averange conc. = 13,510 (174–251,000 µg/mL); Aminorex not detected U: metabolites: 4-OH-LEV; LEV sulfoxide; LEV glucuronide; OH-LEV glucuronide; PL (n = 8): LEV average conc. = 10.6 (0.9–64.1 µg/L); U (n = 8) average conc. =144.50 (50–10,050); aminorex not detected | [66] |
| H (n= 100) CRATOD admission | THC; lidocaine; phenacetin; levamisole; benzocaine; procaine hydroxyzine | LC-MS/MS | H | ___ | ___ | Cocaine (n = 100), BE + (n = 100); CE + (n = 94) THC + (n = 23); lidocaine (n = 92) +; phenacetin + (n = 69); levamisole + (n = 31) benzocaine + (n = 19); procaine + (n = 5); hydroxyzine (n = 2) | [67] |
| Brain tissue (n = 10) Blood (n = 5) U (n = 1) | DZ; hydroxyzine; levamisole; lidocaine; phenacetin; procaine; cetirizine | GC-MS | Brain tissue; U; BL | Cocaine 3.6 BE 27 EME 67 CET 71 DZ 26 HYD 9 LEV 14 LID 38 PHE 21 PRO 16 | Cocaine 30 BE 93 EME 105 CET 363 DZ 101 HYD 152 LEV 66 LID 81 PHE 132 PRO 121 | Cocaine 530.8 ng/g; benzodiazepine 423.1 ng/g; EME 548.7 ng/g; LEV 128.1 ng/mg; LID 73.5 ng/mg; HYD 170.5 ng/g; ALC (BL) 0.86‰; ALC (brain) 0;54‰; ALC (U) 4;97‰ | [65] |
| U (n = 3665) | Levamisole | Immunoassay LC-Q-ToF | U | ___ | ___ | Cocaine + (n = 51); levamisole + (n = 27); methamphetamine/MDMA + (n = 23); cannabis metabolites + (n = 12); heroin or metabolite + (n = 2). | [69] |
| H (n = 55) | Levamisole | LC-MS/MS | H | ___ | Levamisole 0.002 pg/mg; Cocaine 0.005 pg/mg | H [cocaine + samples > 500 pg/mg]: 4265.4 pg/mg (levamisole); 322.9 pg/mg (MDMA); 253.9 g/week (alcohol); H [cocaine—samples]: 0 (levamisole); 0.99 pg/mg (MDMA); 56.5 g/week (alcohol) | [68] |
| Heroin | |||||||
| H (n = 40) | Fentanyl; acetylfentanyl; furanylfentanyl; U-47700 | UHPLC-MS/MS | H | 0.1–0.3 pg/mg | 0.3–0.9 pg/mg | Fentanyl 2.3–8600 pg/mg (mean = 860 pg/mg; median = 440 pg/mg); acetylfentanyl = 2.1–3200 pg/mg (mean = 160 pg/mg; median = 26 pg/mg); furanylfentanyl = 0.7–42 pg/mg (mean = 8.0 pg/mg; median = 1.6 pg/mg); U-47700 (n = 3/40): 1.4–4.5 pg/mg | [70] |
| OF (n = 30) U (n = 30) | Fentanyl; norfentanyl; acetylfentanyl; U-47700 | LC-Q-ToF-MS | OF U | Fentanyl 1; norfentanyl 2; acetylfentanyl 1; carfentanil 1; U-47700 1 | ___ | U (n = 29 fentanyl +); OF (n = 27 fentanyl +); norfentanyl; acetylfentanyl; U-47700 | [71] |
3. Discussion
4. Method
- (1)
- Articles not written in English
- (2)
- Commentary; editorial letters; and surveys
- (3)
- Duplicates were removed
- (4)
- Irrelevant studies
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- United Nations Office on Drugs and Crime (UNODC). Global Overview: Drug Demand; United Nations Office on Drugs and Crime: Vienna, Austria, 2022; ISBN 9789211483611. [Google Scholar]
- Di Trana, A.; Carlier, J.; Berretta, P.; Zaami, S.; Ricci, G. Consequences of COVID-19 Lockdown on the Misuse and Marketing of Addictive Substances and New Psychoactive Substances. Front. Psychiatry 2020, 11, 584462. [Google Scholar] [CrossRef]
- European Monitoring Centre for Drugs and Drug Addiction. European Drug Report 2022:Trends and Developments; Publications Office of the European Union: Luxembourg, 2022; ISBN 9789294977694.
- Solimini, R.; CRotolo, M.; Pellegrini, M.; Minutillo, A.; Pacifici, R.; Busardò, F.P.; Zaami, S. Adulteration Practices of Psychoactive Illicit Drugs: An Updated Review. Curr. Pharm. Biotechnol. 2017, 18, 524–530. [Google Scholar] [CrossRef]
- Tittarelli, R.; Di Luca, N.M.; Pacifici, R.; Pichini, S.; Del Rio, A.; Busardò, F.P. Commentary—Heroin purity and adulteration: An updated snapshot from the Italian Early Warning System. Eur. Rev. Med. Pharmacol. Sci. 2020, 24, 4461–4466. [Google Scholar] [CrossRef]
- Di Trana, A.; Montanari, E. Adulterants in drugs of abuse: A recent focus of a changing phenomenon. Clin. Ter. 2022, 173, 54–55. [Google Scholar] [CrossRef]
- UNODC. Going Beyond Drug Seizures Cocaine: A Spectrum of Products 2; United Nations Office on Drugs and Crime: Vienna, Austria, 2021.
- UNODC. Booklet 4—Drug Market Trends of Cocaine, Amphetamine-Type Stimulants and New Psychoactive Substances. In World Drug Report 2022 (United Nations Publication, 2022); United Nations: Vienna, Austria, 2022; ISBN 9789211483758. [Google Scholar]
- Di Trana, A.; Pichini, S.; Pacifici, R.; Giorgetti, R.; Busardò, F.P. Synthetic Benzimidazole Opioids: The Emerging Health Challenge for European Drug Users. Front. Psychiatry 2022, 13, 858234. [Google Scholar] [CrossRef]
- Montanari, E.; Madeo, G.; Pichini, S.; Busardò, F.P.; Carlier, J. Acute Intoxications and Fatalities Associated With Benzimidazole Opioid (Nitazene Analog) Use: A Systematic Review. Ther. Drug Monit. 2022, 44, 494–510. [Google Scholar] [CrossRef]
- Page, M.J.; Moher, D.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. PRISMA 2020 explanation and elaboration: Updated guidance and exemplars for reporting systematic reviews. BMJ 2021, 372, n160. [Google Scholar] [CrossRef]
- Peck, Y.; Clough, A.R.; Culshaw, P.N.; Liddell, M.J. Multi-drug cocktails: Impurities in commonly used illicit drugs seized by police in Queensland, Australia. Drug Alcohol Depend. 2019, 201, 49–57. [Google Scholar] [CrossRef]
- Fiorentin, T.R.; Logan, B.K. Analytical findings in used syringes from a syringe exchange program. Int. J. Drug Policy 2020, 81, 102770. [Google Scholar] [CrossRef]
- Florea, A.; Cowen, T.; Piletsky, S.; De Wael, K. Polymer platforms for selective detection of cocaine in street samples adulterated with levamisole. Talanta 2018, 186, 362–367. [Google Scholar] [CrossRef]
- Akhgari, M.; Moradi, F.; Ziarati, P. The Texture of Psychoactive Illicit Drugs in Iran: Adulteration with Lead and other Active Pharmaceutical Ingredients. J. Psychoact. Drugs 2018, 50, 451–459. [Google Scholar] [CrossRef]
- Bourmaud, A.; Dahm, G.; Meys, F.; Gengler, N.; Origer, A.; Schneider, S. Investigation on heroin and cocaine quality in Luxembourg. Harm Reduct. J. 2021, 18, 97. [Google Scholar] [CrossRef] [PubMed]
- Fiorentin, T.R.; Krotulski, A.J.; Martin, D.M.; Browne, T.; Triplett, J.; Conti, T.; Logan, B.K. Detection of Cutting Agents in Drug-Positive Seized Exhibits within the United States. J. Forensic Sci. 2019, 64, 888–896. [Google Scholar] [CrossRef] [PubMed]
- Cui, X.; Wang, R.; Lian, R.; Liang, C.; Chen, G.; Zhang, Y. Correlation analysis between cocaine samples seized in China by the rapid detection of organic impurities using direct analysis in real time coupled with high-resolution mass spectrometry. Int. J. Mass Spectrom. 2019, 444, 116188. [Google Scholar] [CrossRef]
- Abin-Carriquiry, J.A.; Martínez-Busi, M.; Galvalisi, M.; Minteguiaga, M.; Prieto, J.P.; Scorza, M.C. Identification and Quantification of Cocaine and Active Adulterants in Coca-Paste Seized Samples: Useful Scientific Support to Health Care. Neurotox. Res. 2018, 34, 295–304. [Google Scholar] [CrossRef]
- Morelato, M.; Franscella, D.; Esseiva, P.; Broséus, J. When does the cutting of cocaine and heroin occur? The first large-scale study based on the chemical analysis of cocaine and heroin seizures in Switzerland. Int. J. Drug Policy 2019, 73, 7–15. [Google Scholar] [CrossRef] [PubMed]
- da Silva, A.F.; Grobério, T.S.; Zacca, J.J.; Maldaner, A.O.; Braga, J.W.B. Cocaine and adulterants analysis in seized drug samples by infrared spectroscopy and MCR-ALS. Forensic Sci. Int. 2018, 290, 169–177. [Google Scholar] [CrossRef]
- Pacheco, W.F.; Almeida, V.G.K.; Cassella, R.J.; Lepri, F.G. Development of an analytical methodology for chemical profile of cocaine seized in rio de janeiro, brazil. Brazilian J. Anal. Chem. 2018, 5, 28–39. [Google Scholar] [CrossRef]
- Barreto, D.N.; Ribeiro, M.M.A.C.; Sudo, J.T.C.; Richter, E.M.; Muñoz, R.A.A.; Silva, S.G. High-throughput screening of cocaine, adulterants, and diluents in seized samples using capillary electrophoresis with capacitively coupled contactless conductivity detection. Talanta 2020, 217, 120987. [Google Scholar] [CrossRef]
- Yemloul, M.; Adyatmika, I.M.; Caldarelli, S.; Ollivier, D.; Campredon, M. Rapid characterization of cocaine in illicit drug samples by 1D and 2D NMR spectroscopy. Anal. Bioanal. Chem. 2018, 410, 5237–5244. [Google Scholar] [CrossRef]
- Fiorentin, T.R.; Scherer, J.N.; Marcelo, M.C.A.; Sousa, T.R.V.; Pechansky, F.; Ferrão, M.F.; Limberger, R.P. Comparison of Cocaine/Crack Biomarkers Concentrations in Oral Fluid, Urine and Plasma Simultaneously Collected From Drug Users. J. Anal. Toxicol. 2018, 42, 69–76. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- CFSRE. Drug Supply Assessment: Q1 2021; CFSRE: Willow Grove, PA, USA, 2021. [Google Scholar]
- Krauss, S.T.; Ross, D.; Forbes, T.P. Separation and Detection of Trace Fentanyl from Complex Mixtures Using Gradient Elution Moving Boundary Electrophoresis. Anal. Chem. 2019, 91, 13014–13021. [Google Scholar] [CrossRef] [PubMed]
- Bowles, J.M.; McDonald, K.; Maghsoudi, N.; Thompson, H.; Stefan, C.; Beriault, D.R.; Delaney, S.; Wong, E.; Werb, D. Xylazine detected in unregulated opioids and drug administration equipment in Toronto, Canada: Clinical and social implications. Harm Reduct. J. 2021, 18, 104. [Google Scholar] [CrossRef]
- Gilbert, N.; Antonides, L.H.; Schofield, C.J.; Costello, A.; Kilkelly, B.; Cain, A.R.; Dalziel, P.R.V.; Horner, K.; Mewis, R.E.; Sutcliffe, O.B. Hitting the Jackpot—Development of gas chromatography–mass spectrometry (GC–MS) and other rapid screening methods for the analysis of 18 fentanyl-derived synthetic opioids. Drug Test. Anal. 2020, 12, 798–811. [Google Scholar] [CrossRef]
- Quintana, P.; Ventura, M.; Grifell, M.; Palma, A.; Galindo, L.; Fornís, I.; Gil, C.; Carbón, X.; Caudevilla, F.; Farré, M.; et al. The hidden web and the fentanyl problem: Detection of ocfentanil as an adulterant in heroin. Int. J. Drug Policy 2017, 40, 78–83. [Google Scholar] [CrossRef] [Green Version]
- Aghababaei, R.; Javadi, I.; Nili-Ahmadabadi, A.; Parsafar, S.; Ahmadimoghaddam, D. Occurrence of bacterial and toxic metals contamination in illegal opioid-like drugs in Iran: A significant health challenge in drug abusers. DARU J. Pharm. Sci. 2018, 26, 77–83. [Google Scholar] [CrossRef]
- Saleemi, S.; Pennybaker, S.J.; Wooldridge, M.; Johnson, M.W. Who is “Molly”? MDMA adulterants by product name and the impact of harm-reduction services at raves. J. Psychopharmacol. 2017, 31, 1056–1060. [Google Scholar] [CrossRef] [PubMed]
- Salehi, M.; Morgan, M.P.; Gabriel, A. Levamisole-Induced Leukocytoclastic Vasculitis with Negative Serology in a Cocaine User. Am. J. Case Rep. 2017, 18, 641–643. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Oomen, P.E.; Schori, D.; Tögel-Lins, K.; Acreman, D.; Chenorhokian, S.; Luf, A.; Karden, A.; Paulos, C.; Fornero, E.; Gerace, E.; et al. Cannabis adulterated with the synthetic cannabinoid receptor agonist MDMB-4en-PINACA and the role of European drug checking services. Int. J. Drug Policy 2022, 100, 103493. [Google Scholar] [CrossRef]
- da Silva, G.O.; de Araujo, W.R.; Paixão, T.R.L.C. Portable and low-cost colorimetric office paper-based device for phenacetin detection in seized cocaine samples. Talanta 2018, 176, 674–678. [Google Scholar] [CrossRef]
- De Jong, M.; Florea, A.; De Vries, A.M.; Van Nuijs, A.L.N.; Covaci, A.; Van Durme, F.; Martins, J.C.; Samyn, N.; De Wael, K. Levamisole: A Common Adulterant in Cocaine Street Samples Hindering Electrochemical Detection of Cocaine. Anal. Chem. 2018, 90, 5290–5297. [Google Scholar] [CrossRef] [PubMed]
- Eliaerts, J.; Meert, N.; Van Durme, F.; Dardenne, P.; Charles, S.; De Wael, K.; Samyn, N. Challenges for cocaine detection in smuggling samples. Forensic Sci. Int. 2021, 319, 110534. [Google Scholar] [CrossRef]
- Roberson, Z.R.; Gordon, H.C.; Goodpaster, J.V. Instrumental and chemometric analysis of opiates via gas chromatography–vacuum ultraviolet spectrophotometry (GC-VUV). Anal. Bioanal. Chem. 2020, 412, 1123–1128. [Google Scholar] [CrossRef] [PubMed]
- Lefrancois, E.; Belackova, V.; Silins, E.; Latimer, J.; Jauncey, M.; Shimmon, R.; Mozaner Bordin, D.; Augsburger, M.; Esseiva, P.; Roux, C.; et al. Substances injected at the Sydney supervised injecting facility: A chemical analysis of used injecting equipment and comparison with self-reported drug type. Drug Alcohol Depend. 2020, 209, 107909. [Google Scholar] [CrossRef] [PubMed]
- May, C.; Downey, C.; Power, J.D.; Kavanagh, P.V. An unusual detection of tert-butyl-4-anilinopiperidine-1-carboxylate in seizures of falsified “Xanax” tablets and in items in a suspected heroin seizure submitted by Irish law enforcement. Drug Test. Anal. 2020, 12, 1387–1392. [Google Scholar] [CrossRef]
- Ladroue, V.; Dujourdy, L.; Besacier, F.; Jame, P. IRMS to study a common cocaine cutting agent: Phenacetin. Drug Test. Anal. 2017, 9, 479–484. [Google Scholar] [CrossRef]
- Urzola-Ortega, J.; Mendoza-Goez, L.; Acevedo, D. Personal Doses of Cocaine and Coca Paste are Adulterated in Cartagena de Indias (Colombia). Sci. World J. 2021, 2021, 5562315. [Google Scholar] [CrossRef]
- Madry, M.M.; Kraemer, T.; Baumgartner, M.R. Cocaine adulteration with the anthelminthic tetramisole (levamisole/dexamisole): Long-term monitoring of its intake by chiral LC–MS/MS analysis of cocaine-positive hair samples. Drug Test. Anal. 2019, 11, 472–478. [Google Scholar] [CrossRef]
- Phillips, R.; King, M.; McGilligan, J.A.; Hajela, V.; Allan, K. A retrospective review of four patients with severe nasal destruction secondary to cocaine adulterated with levamisole. Clin. Otolaryngol. 2021, 46, 673–678. [Google Scholar] [CrossRef] [PubMed]
- De Baerdemaeker, K.; Mabiglia, C.; Hantson, P.; Di Fazio, V.; Duprez, T.; Kozyreff, A.; Van Pesch, V.; Sellimi, A. Acute Susac Syndrome in a Recent User of Adulterated Cocaine: Levamisole as a Triggering Factor? Case Rep. Neurol. 2020, 12, 78–83. [Google Scholar] [CrossRef]
- Saud Khan, M.; Khan, Z.; Khateeb, F.; Moustafa, A.; Taleb, M.; Yoon, Y. Recurrent Levamisole-Induced Agranulocytosis Complicated by Bowel Ischemia in a Cocaine User. Am. J. Case Rep. 2018, 19, 630–633. [Google Scholar] [CrossRef]
- Mohan, V.; Maiti, A.; Swaby, M.G.; Cherian, S.V. Vasculitis due to levamisole-adulterated cocaine. Postgrad. Med. J. 2018, 94, 61. [Google Scholar] [CrossRef] [PubMed]
- Roberts, D.M.; Premachandra, K.H.; Chan, B.S.; Auld, R.; Jiranantakan, T.; Ewers, C.; McDonald, C.; Shaw, V.; Brown, J.A. A cluster of lysergic acid diethylamide (LSD) poisonings following insufflation of a white powder sold as cocaine. Clin. Toxicol. 2021, 59, 969–974. [Google Scholar] [CrossRef]
- Aghabiklooei, A.; Saboori, H.; Ameri, M. Lead poisoning with presentation of acute abdomen and narcotic bowel syndrome in opium user woman CASE REPORT. Gulhane Med. J. 2018, 60, 116–118. [Google Scholar] [CrossRef] [Green Version]
- Pichini, S.; Marchei, E.; Pacifici, R.; Marinelli, E.; Busardò, F.P. Chemsex intoxication involving sildenafil as an adulterant of GHB. Drug Test. Anal. 2017, 9, 956–959. [Google Scholar] [CrossRef] [PubMed]
- Kolbe, V.; Rentsch, D.; Boy, D.; Schmidt, B.; Kegler, R.; Büttner, A. The adulterated XANAX pill: A fatal intoxication with etizolam and caffeine. Int. J. Legal Med. 2020, 134, 1727–1731. [Google Scholar] [CrossRef] [PubMed]
- Ershad, M.; Dela Cruz, M.; Mostafa, A.; Khalid, M.; Arnold, R.; Hamilton, R. Heroin Adulterated with the Novel Synthetic Cannabinoid, 5F-MDMB-PINACA: A Case Series. Clin. Pract. Cases Emerg. Med. 2020, 4, 121–125. [Google Scholar] [CrossRef] [PubMed]
- Lazzaro, M.C.; Romanò, S.; Santoro, S.; Camuto, C.; Carbone, A.; Casamassima, R.; Abate, S.; De-Giorgio, F. A potential cause of asbestos-related granulomatosis due to adulterant contamination in a drug abuser. Virchows Arch. 2021, 478, 361–366. [Google Scholar] [CrossRef] [PubMed]
- Gadarowski, M.B.; Agnihothri, R.; Scott, G.; Plovanich, M. Pyoderma gangrenosum associated with levamisole-adulterated cocaine in a c-ANCA positive patient. Dermatol. Online J. 2021, 27, 11. [Google Scholar] [CrossRef]
- Mahintamani, T.; Ghosh, A.; Jain, R. Serious health threats of novel adulterants of the street heroin: A report from India during the COVID-19 pandemic. BMJ Case Rep. 2021, 14, e242239. [Google Scholar] [CrossRef]
- Nacca, N.; Schult, R.F.; Li, L.; Spink, D.C.; Ginsberg, G.; Navarette, K.; Marraffa, J. Kratom Adulterated with Phenylethylamine and Associated Intracerebral Hemorrhage: Linking Toxicologists and Public Health Officials to Identify Dangerous Adulterants. J. Med. Toxicol. 2020, 16, 71–74. [Google Scholar] [CrossRef] [PubMed]
- Hussaini, A.S.; Black, C.K.; Malekzadeh, S.; Milmoe, G.J. Extensive Sinonasal and Oropharyngeal Necrosis as a Consequence of Adulterated Cocaine with Mimicry of ANCA-Positive Vasculitis. OTO Open 2019, 3, 2473974X19894239. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Collister, D.; Sathianathan, C.; Ryz, K.; Karpinski, M.; Bernstein, K.; Gibson, I.W. ANCA Associated Vasculitis Secondary to Levamisole-Adultered Cocaine with Associated Membranous Nephropathy: A Case Series. Am. J. Nephrol. 2017, 45, 209–216. [Google Scholar] [CrossRef] [PubMed]
- Desvignes, C.; Becquart, C.; Launay, D.; Terriou, L.; Patenotre, P.; Deheul, S.; Peytavin, G.; Dupin, N.; Delaporte, E.; Staumont-Sallé, D. Extensive levamisole-induced vasculitis. Clin. Exp. Dermatol. 2017, 42, 413–415. [Google Scholar] [CrossRef] [PubMed]
- Gill, H.; Trinh, D.; Anderson, D.J.; Li, N.; Madenberg, D. Cocaine and Levamisole Induced Vasculitis. Cureus 2021, 13. [Google Scholar] [CrossRef]
- Sánchez-Velázquez, A.; Calleja-Algarra, A.; Velasco-Tamariz, V.; Zarco-Olivo, C.; Sánchez-Velázquez, A.; Calleja-Algarra, A.; Velasco-Tamariz, V.; Zarco-Olivo, C. Widespread cutaneous vasculopathy associated with levamisole-adulterated cocaine. Indian J. Dermatol. Venereol. Leprol. 2021, 87, 540–542. [Google Scholar] [CrossRef]
- Salabei, J.K.; Khan, S.; Khan, A.; Asnake, Z.T.; Fishman, T.J.; Stromas, J.D.; Ismail, Z.H.; Leibach, J.R. ANCA-Associated Intrahepatic Duct Injury Associated with Levamisole-Adulterated Cocaine. Case reports Hepatol. 2020, 2020, 8867183. [Google Scholar] [CrossRef]
- Schulte-Pelkum, J.; Radice, A.; Norman, G.L.; Lpez Hoyos, M.; Lakos, G.; Buchner, C.; Musset, L.; Miyara, M.; Stinton, L.; Mahler, M. Novel clinical and diagnostic aspects of antineutrophil cytoplasmic antibodies. J. Immunol. Res. 2014, 2014, 185416. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Whitacre, C.C. Sex differences in autoimmune disease. Nat. Immunol. 2001, 2, 777–780. [Google Scholar] [CrossRef] [PubMed]
- Klont, F.; Jahn, S.; Grivet, C.; König, S.; Bonner, R.; Hopfgartner, G. SWATH data independent acquisition mass spectrometry for screening of xenobiotics in biological fluids: Opportunities and challenges for data processing. Talanta 2020, 211, 120747. [Google Scholar] [CrossRef]
- Handley, S.A.; Belsey, S.L.; Couchman, L.; Flanagan, R.J. Plasma and Urine Levamisole in Clinical Samples Containing Benzoylecgonine: Absence of Aminorex. J. Anal. Toxicol. 2019, 43, 299–306. [Google Scholar] [CrossRef]
- Ribeiro, M.; Trevizol, A.P.; Frajzinger, R.; Ribeiro, A.; Speierl, H.; Pires, L.; Andraus, M.; Tsanaclis, L.; Alonso, A.L.S.; Cordeiro, Q.; et al. Adulterants in crack cocaine in Brazil. Trends Psychiatry Psychother. 2019, 41, 186–190. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Michels, L.; Moisa, M.; Stämpfli, P.; Hirsiger, S.; Baumgartner, M.R.; Surbeck, W.; Seifritz, E.; Quednow, B.B. The impact of levamisole and alcohol on white matter microstructure in adult chronic cocaine users. Addict. Biol. 2022, 27, e13149. [Google Scholar] [CrossRef] [PubMed]
- Pope, J.D.; Drummer, O.H.; Schneider, H.G. The cocaine cutting agent levamisole is frequently detected in cocaine users. Pathology 2018, 50, 536–539. [Google Scholar] [CrossRef] [PubMed]
- Palamar, J.J.; Salomone, A.; Bigiarini, R.; Vincenti, M.; Acosta, P.; Tofighi, B. Testing hair for fentanyl exposure: A method to inform harm reduction behavior among individuals who use heroin. Am. J. Drug Alcohol Abus. 2019, 45, 90–96. [Google Scholar] [CrossRef] [PubMed]
- Griswold, M.K.; Chai, P.R.; Krotulski, A.J.; Friscia, M.; Chapman, B.P.; Varma, N.; Boyer, E.W.; Logan, B.K.; Babu, K.M. A Novel Oral Fluid Assay (LC-QTOF-MS) for the Detection of Fentanyl and Clandestine Opioids in Oral Fluid After Reported Heroin Overdose. J. Med. Toxicol. 2017, 13, 287–292. [Google Scholar] [CrossRef]
- Florea, A.; Schram, J.; De Jong, M.; Eliaerts, J.; Van Durme, F.; Kaur, B.; Samyn, N.; De Wael, K. Electrochemical Strategies for Adulterated Heroin Samples. Anal. Chem. 2019, 91, 7920–7928. [Google Scholar] [CrossRef] [PubMed]
- Gozdzialski, L.; Rowley, A.; Borden, S.A.; Saatchi, A.; Gill, C.G.; Wallace, B.; Hore, D.K. Rapid and accurate etizolam detection using surface-enhanced Raman spectroscopy for community drug checking. Int. J. Drug Policy 2022, 102, 103611. [Google Scholar] [CrossRef]
- Braz, A.; Santos Silva, C.; Peixoto, A.C.; Pimentel, M.F.; Pereira, G.; Caixeta Castro Souza Braga, P.; Martini, A.L.; Lino Fernandes Alcântara, T. Preliminary study on the identification of synthetic cathinones in street seized samples by Raman spectroscopy and chemometrics. J. Raman Spectrosc. 2021, 52, 901–913. [Google Scholar] [CrossRef]
- Barbera, N.; Busardò, F.P.; Indorato, F.; Romano, G. The pathogenetic role of adulterants in 5 cases of drug addicts with a fatal outcome. Forensic Sci. Int. 2013, 227, 74–76. [Google Scholar] [CrossRef] [PubMed]
- CFSRE. Quinine and Quinidine: Toxic Adulterants Found in Illicit Street Drugs; CFSRE: Willow Grove, PA, USA, 2022. [Google Scholar]
- Scott, T.M.; Yeakel, J.K.; Logan, B.K. Identification of mitragynine and O-desmethyltramadol in Kratom and legal high products sold online. Drug Test. Anal. 2014, 6, 959–963. [Google Scholar] [CrossRef] [PubMed]
- Ujvary, I. Kratom and Other Mitragynines: The Chemistry and Pharmacology of Opioids from a Non-Opium Source. J. Addict. Res. Ther. 2015, 6. [Google Scholar] [CrossRef]
- Arndt, T.; Claussen, U.; Güssregen, B.; Schröfel, S.; Stürzer, B.; Werle, A.; Wolf, G. Kratom alkaloids and O-desmethyltramadol in urine of a “Krypton” herbal mixture consumer. Forensic Sci. Int. 2011, 208, 47–52. [Google Scholar] [CrossRef] [PubMed]
- Lydecker, A.G.; Sharma, A.; McCurdy, C.R.; Avery, B.A.; Babu, K.M.; Boyer, E.W. Suspected Adulteration of Commercial Kratom Products with 7-Hydroxymitragynine. J. Med. Toxicol. 2016, 12, 341–349. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xylazine, W.I. CCENDU Drug Alert Xylazine; CCENDU: Ottawa, ON, Canada, 2022; pp. 1–5.
- Kacinko, S.L.; Mohr, A.L.A.; Logan, B.K.; Barbieri, E.J. Xylazine: Pharmacology Review and Prevalence and Drug Combinations in Forensic Toxicology Casework. J. Anal. Toxicol. 2022, 46, 911–917. [Google Scholar] [CrossRef]
- Karch, S.B.; Busardò, F.P.; Vaiano, F.; Portelli, F.; Zaami, S.; Bertol, E. Levamisole adulterated cocaine and pulmonary vasculitis: Presentation of two lethal cases and brief literature review. Forensic Sci. Int. 2016, 265, 96–102. [Google Scholar] [CrossRef]
- Tollens, N.; Post, P.; Martins Dos Santos, M.; Niggemann, P.; Warken, M.; Wolf, J. Multifocal leukoencephalopathy associated with intensive use of cocaine and the adulterant levamisole in a 29-year old patient. Neurol. Res. Pract. 2022, 4, 38. [Google Scholar] [CrossRef]
- Madry, M.M.; Kraemer, T.; Baumgartner, M.R. Large scale consumption monitoring of benzodiazepines and z-drugs by hair analysis. J. Pharm. Biomed. Anal. 2020, 183, 113151. [Google Scholar] [CrossRef]
- Knuth, M.; Temme, O.; Daldrup, T.; Pawlik, E. Analysis of cocaine adulterants in human brain in cases of drug-related death. Forensic Sci. Int. 2018, 285, 86–92. [Google Scholar] [CrossRef]
- Conrad, F.; Hirsiger, S.; Winklhofer, S.; Baumgartner, M.R.; Stämpfli, P.; Seifritz, E.; Wegener, S.; Quednow, B.B. Use of levamisole-adulterated cocaine is associated with increased load of white matter lesions. J. Psychiatry Neurosci. 2021, 46, E281–E291. [Google Scholar] [CrossRef]
- UNODC. World Drug Report 2022 Global Overview: Drug Demand Drug Supply; UNODC: Vienna, Austria, 2022. [Google Scholar]
- Huhn, C.; Neusüß, C.; Pelzing, M.; Pyell, U.; Mannhardt, J.; Pütz, M. Capillary electrophoresis-laser induced fluorescence-electrospray ionization-mass spectrometry: A case study. Electrophoresis 2005, 26, 1389–1397. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Di Trana, A.; Berardinelli, D.; Montanari, E.; Berretta, P.; Basile, G.; Huestis, M.A.; Busardò, F.P. Molecular Insights and Clinical Outcomes of Drugs of Abuse Adulteration: New Trends and New Psychoactive Substances. Int. J. Mol. Sci. 2022, 23, 14619. https://doi.org/10.3390/ijms232314619
Di Trana A, Berardinelli D, Montanari E, Berretta P, Basile G, Huestis MA, Busardò FP. Molecular Insights and Clinical Outcomes of Drugs of Abuse Adulteration: New Trends and New Psychoactive Substances. International Journal of Molecular Sciences. 2022; 23(23):14619. https://doi.org/10.3390/ijms232314619
Chicago/Turabian StyleDi Trana, Annagiulia, Diletta Berardinelli, Eva Montanari, Paolo Berretta, Giuseppe Basile, Marilyn A. Huestis, and Francesco Paolo Busardò. 2022. "Molecular Insights and Clinical Outcomes of Drugs of Abuse Adulteration: New Trends and New Psychoactive Substances" International Journal of Molecular Sciences 23, no. 23: 14619. https://doi.org/10.3390/ijms232314619
APA StyleDi Trana, A., Berardinelli, D., Montanari, E., Berretta, P., Basile, G., Huestis, M. A., & Busardò, F. P. (2022). Molecular Insights and Clinical Outcomes of Drugs of Abuse Adulteration: New Trends and New Psychoactive Substances. International Journal of Molecular Sciences, 23(23), 14619. https://doi.org/10.3390/ijms232314619









