Myocardial Protection and Current Cancer Therapy: Two Opposite Targets with Inevitable Cost
Abstract
1. Introduction
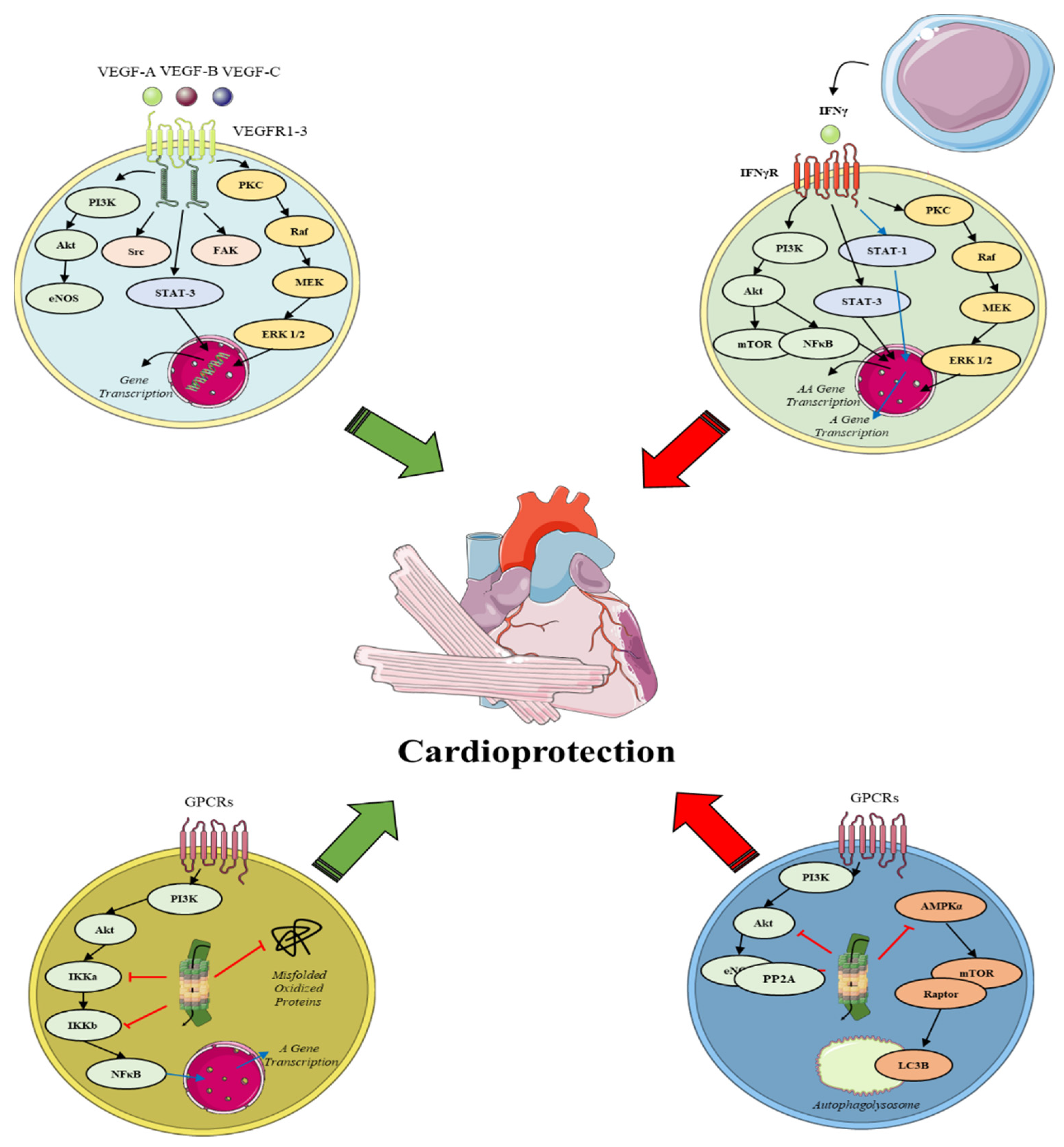
1.1. Endogenous Cardioprotection
1.2. Direct Drug Cardiotoxicity and/or Neutralization of Cardioprotection
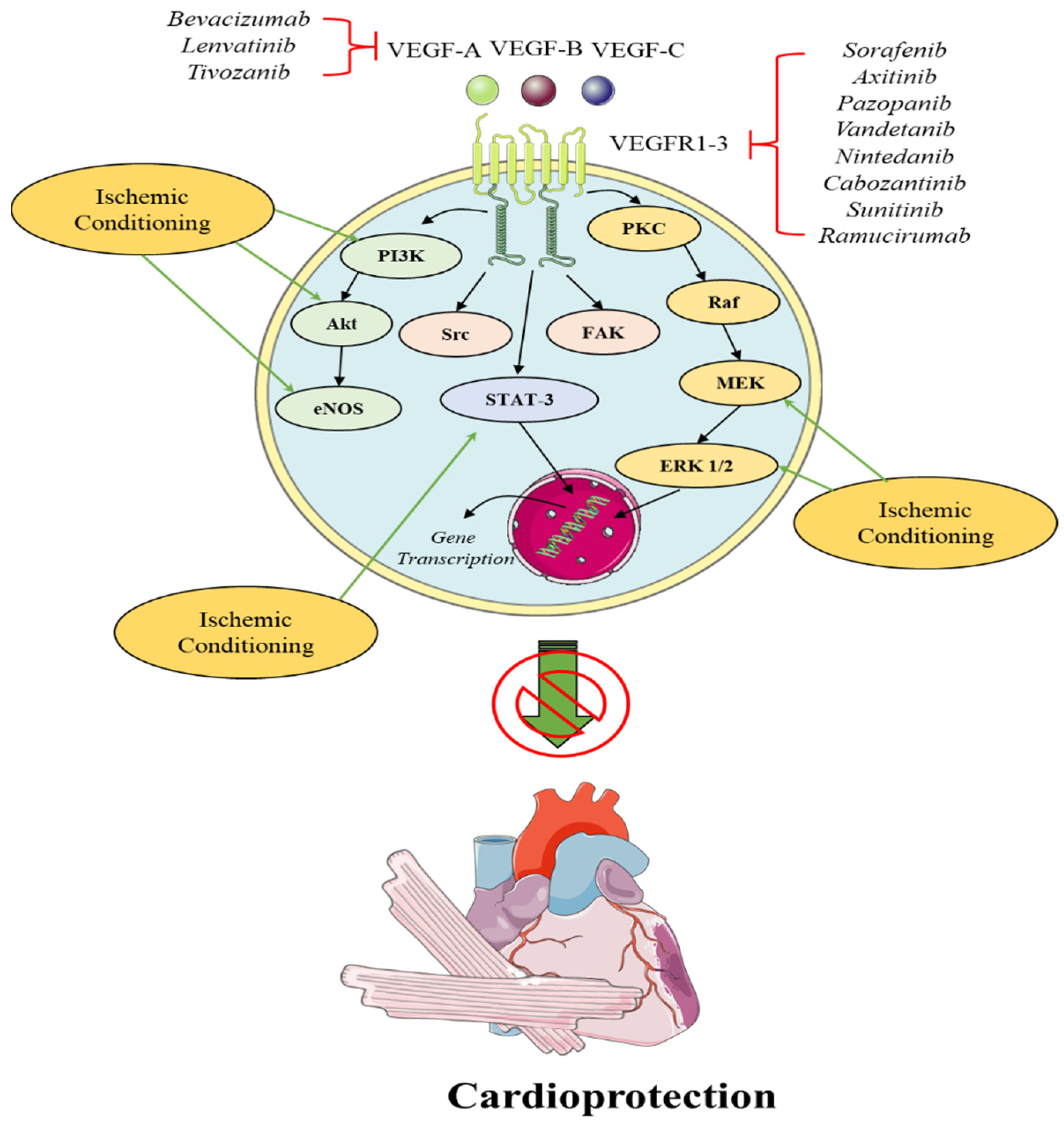
2. VEGF Inhibitors
2.1. Angiogenesis in Cardioprotection and Tumor Growth
2.2. Angiogenesis, Angiogenic Factors and Cardioprotection
2.2.1. The Role of VEGF in IRI
2.2.2. The Role of VEGF in Cardioprotection
2.3. Antitumor Effects of Anti-Angiogenetic Drugs
2.4. Cardiotoxic Effects of Anti-Angiogenetic Drugs
2.5. Breakthroughs and Perspectives
3. Proteasome Inhibitors
3.1. Proteasome in Cardioprotection and Tumor Growth
3.1.1. The Cardiac UPS System and Cardioprotection
3.1.2. The Role of Proteasome in IRI
3.1.3. The Role of Proteasome in Cardioprotection
3.2. Proteasome Inhibitors and IRI
3.3. Cardiotoxic Effects of Proteasome Inhibitors
3.4. Breakthroughs and Perspectives
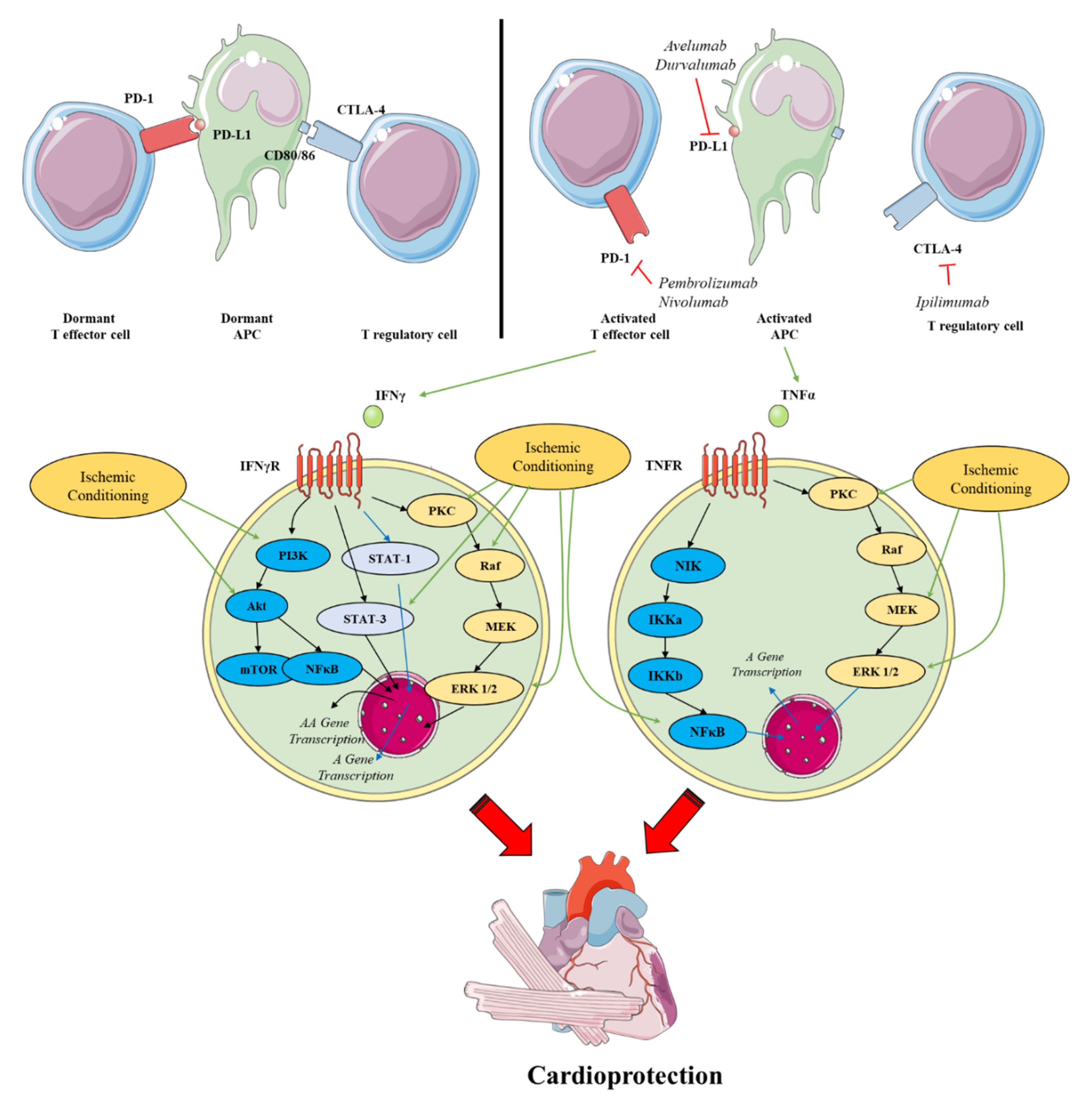
4. Immune Checkpoint Inhibitors
4.1. Immune Checkpoints in Cardioprotection and Tumor Growth
4.2. The role of Immune Checkpoints in IRI
4.3. The Role of Immune Checkpoints in Cardioprotection
4.4. Cardiotoxicity of Immune Check Point Inhibitors
4.5. Breakthroughs and Perspectives
5. Diagnostic Modalities of Anti-Neoplastic Drugs CAEs
5.1. Arrhythmogenesis
5.2. Cardiometabolic Cofounders and Cancer Therapy-Related Cardiovascular Toxicity
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- De Wit, S.; de Boer, R.A. From Studying Heart Disease and Cancer Simultaneously to Reverse Cardio-Oncology. Circulation 2021, 144, 93–95. [Google Scholar] [CrossRef] [PubMed]
- Lyon, A.R.; Lopez-Fernandez, T.; Couch, L.S.; Asteggiano, R.; Aznar, M.C.; Bergler-Klein, J.; Boriani, G.; Cardinale, D.; Cordoba, R.; Cosyns, B.; et al. 2022 ESC Guidelines on cardio-oncology developed in collaboration with the European Hematology Association (EHA), the European Society for Therapeutic Radiology and Oncology (ESTRO) and the International Cardio-Oncology Society (IC-OS). Eur. Heart J. 2022, 43, 4229–4361. [Google Scholar] [CrossRef] [PubMed]
- Daiber, A.; Andreadou, I.; Oelze, M.; Davidson, S.M.; Hausenloy, D.J. Discovery of new therapeutic redox targets for cardioprotection against ischemia/reperfusion injury and heart failure. Free Radic. Biol. Med. 2021, 163, 325–343. [Google Scholar] [CrossRef] [PubMed]
- Iliodromitis, E.K.; Kremastinos, D.T.; Katritsis, D.G.; Papadopoulos, C.C.; Hearse, D.J. Multiple cycles of preconditioning cause loss of protection in open-chest rabbits. J. Mol. Cell. Cardiol. 1997, 29, 915–920. [Google Scholar] [CrossRef] [PubMed]
- Iliodromitis, E.K.; Aggeli, I.K.; Gaitanaki, C.; Tsiafoutis, I.; Zoga, A.; Beis, I.; Kremastinos, D.T. p38-MAPK is involved in restoration of the lost protection of preconditioning by nicorandil in vivo. Eur. J. Pharmacol. 2008, 579, 289–297. [Google Scholar] [CrossRef]
- Davidson, S.M.; Ferdinandy, P.; Andreadou, I.; Botker, H.E.; Heusch, G.; Ibanez, B.; Ovize, M.; Schulz, R.; Yellon, D.M.; Hausenloy, D.J.; et al. Multitarget Strategies to Reduce Myocardial Ischemia/Reperfusion Injury: JACC Review Topic of the Week. J. Am. Coll. Cardiol. 2019, 73, 89–99. [Google Scholar] [CrossRef]
- Iliodromitis, E.K.; Cohen, M.V.; Dagres, N.; Andreadou, I.; Kremastinos, D.T.; Downey, J.M. What is Wrong With Cardiac Conditioning? We May be Shooting at Moving Targets. J. Cardiovasc. Pharmacol. Ther. 2015, 20, 357–369. [Google Scholar] [CrossRef]
- Ferdinandy, P.; Hausenloy, D.J.; Heusch, G.; Baxter, G.F.; Schulz, R. Interaction of risk factors, comorbidities, and comedications with ischemia/reperfusion injury and cardioprotection by preconditioning, postconditioning, and remote conditioning. Pharmacol. Rev. 2014, 66, 1142–1174. [Google Scholar] [CrossRef]
- Ferdinandy, P.; Andreadou, I.; Baxter, G.F.; Bøtker, H.E.; Davidson, S.M.; Dobrev, D.; Gersh, B.J.; Heusch, G.; Lecour, S.; Ruiz-Meana, M.; et al. Interaction of cardiovascular non-modifiable risk factors, comorbidities and comedications with ischemia/reperfusion injury and cardioprotection by pharmacological treatments and ischemic conditioning. Pharmacol. Rev. 2022, in press.
- Inserte, J.; Hernando, V.; Vilardosa, U.; Abad, E.; Poncelas-Nozal, M.; Garcia-Dorado, D. Activation of cGMP/protein kinase G pathway in postconditioned myocardium depends on reduced oxidative stress and preserved endothelial nitric oxide synthase coupling. J. Am. Heart Assoc. 2013, 2, e005975. [Google Scholar] [CrossRef]
- Alburquerque-Bejar, J.J.; Barba, I.; Inserte, J.; Miro-Casas, E.; Ruiz-Meana, M.; Poncelas, M.; Vilardosa, U.; Valls-Lacalle, L.; Rodriguez-Sinovas, A.; Garcia-Dorado, D. Combination therapy with remote ischaemic conditioning and insulin or exenatide enhances infarct size limitation in pigs. Cardiovasc. Res. 2015, 107, 246–254. [Google Scholar] [CrossRef] [PubMed]
- Heusch, G. Molecular basis of cardioprotection: Signal transduction in ischemic pre-, post-, and remote conditioning. Circ. Res. 2015, 116, 674–699. [Google Scholar] [CrossRef] [PubMed]
- Kleinbongard, P.; Skyschally, A.; Heusch, G. Cardioprotection by remote ischemic conditioning and its signal transduction. Pflugers Arch. 2017, 469, 159–181. [Google Scholar] [CrossRef] [PubMed]
- Hausenloy, D.J.; Schulz, R.; Girao, H.; Kwak, B.R.; De Stefani, D.; Rizzuto, R.; Bernardi, P.; Di Lisa, F. Mitochondrial ion channels as targets for cardioprotection. J. Cell. Mol. Med. 2020, 24, 7102–7114. [Google Scholar] [CrossRef] [PubMed]
- Heusch, G. Critical Issues for the Translation of Cardioprotection. Circ. Res. 2017, 120, 1477–1486. [Google Scholar] [CrossRef]
- Iliodromitis, E.K.; Kyrzopoulos, S.; Paraskevaidis, I.A.; Kolocassides, K.G.; Adamopoulos, S.; Karavolias, G.; Kremastinos, D.T. Increased C reactive protein and cardiac enzyme levels after coronary stent implantation. Is there protection by remote ischaemic preconditioning? Heart 2006, 92, 1821–1826. [Google Scholar] [CrossRef][Green Version]
- Alfi, E.; Thairi, C.; Femmino, S.; Alloatti, G.; Moccia, F.; Brizzi, M.F.; Pagliaro, P.; Penna, C. Extracellular vesicles (EVs) in ischemic conditioning and angiogenesis: Focus on endothelial derived EVs. Vasc. Pharmacol. 2021, 140, 106873. [Google Scholar] [CrossRef]
- Cross, M.J.; Dixelius, J.; Matsumoto, T.; Claesson-Welsh, L. VEGF-receptor signal transduction. Trends Biochem. Sci. 2003, 28, 488–494. [Google Scholar] [CrossRef]
- Andreadou, I.; Cabrera-Fuentes, H.A.; Devaux, Y.; Frangogiannis, N.G.; Frantz, S.; Guzik, T.; Liehn, E.A.; Gomes, C.P.C.; Schulz, R.; Hausenloy, D.J. Immune cells as targets for cardioprotection: New players and novel therapeutic opportunities. Cardiovasc. Res. 2019, 115, 1117–1130. [Google Scholar] [CrossRef]
- Ferdinandy, P.; Baczko, I.; Bencsik, P.; Giricz, Z.; Gorbe, A.; Pacher, P.; Varga, Z.V.; Varro, A.; Schulz, R. Definition of hidden drug cardiotoxicity: Paradigm change in cardiac safety testing and its clinical implications. Eur. Heart J. 2019, 40, 1771–1777. [Google Scholar] [CrossRef]
- Tocchetti, C.G.; Ameri, P.; de Boer, R.A.; D’Alessandra, Y.; Russo, M.; Sorriento, D.; Ciccarelli, M.; Kiss, B.; Bertrand, L.; Dawson, D.; et al. Cardiac dysfunction in cancer patients: Beyond direct cardiomyocyte damage of anticancer drugs: Novel cardio-oncology insights from the joint 2019 meeting of the ESC Working Groups of Myocardial Function and Cellular Biology of the Heart. Cardiovasc. Res. 2020, 116, 1820–1834. [Google Scholar] [CrossRef] [PubMed]
- Zamorano, J.L.; Gottfridsson, C.; Asteggiano, R.; Atar, D.; Badimon, L.; Bax, J.J.; Cardinale, D.; Cardone, A.; Feijen, E.A.M.; Ferdinandy, P.; et al. The cancer patient and cardiology. Eur. J. Heart Fail. 2020, 22, 2290–2309. [Google Scholar] [CrossRef]
- Vanhoutte, P.M.; Shimokawa, H.; Feletou, M.; Tang, E.H. Endothelial dysfunction and vascular disease—A 30th anniversary update. Acta Physiol. 2017, 219, 22–96. [Google Scholar] [CrossRef] [PubMed]
- Aslam, M.; Gunduz, D.; Troidl, C.; Heger, J.; Hamm, C.W.; Schulz, R. Purinergic Regulation of Endothelial Barrier Function. Int. J. Mol. Sci. 2021, 22, 1207. [Google Scholar] [CrossRef] [PubMed]
- Barton, M. Prevention and endothelial therapy of coronary artery disease. Curr. Opin. Pharmacol. 2013, 13, 226–241. [Google Scholar] [CrossRef]
- Maas, A.; Rosano, G.; Cifkova, R.; Chieffo, A.; van Dijken, D.; Hamoda, H.; Kunadian, V.; Laan, E.; Lambrinoudaki, I.; Maclaran, K.; et al. Cardiovascular health after menopause transition, pregnancy disorders, and other gynaecologic conditions: A consensus document from European cardiologists, gynaecologists, and endocrinologists. Eur. Heart J. 2021, 42, 967–984. [Google Scholar] [CrossRef]
- Barton, M.; Traupe, T.; Haudenschild, C.C. Endothelin, hypercholesterolemia and atherosclerosis. Coron. Artery Dis. 2003, 14, 477–490. [Google Scholar] [CrossRef]
- Schwartz, S.M. Smooth muscle migration in atherosclerosis and restenosis. J. Clin. Investig. 1997, 100, S87–S89. [Google Scholar]
- Pasquier, J.; Ghiabi, P.; Chouchane, L.; Razzouk, K.; Rafii, S.; Rafii, A. Angiocrine endothelium: From physiology to cancer. J. Transl. Med. 2020, 18, 52. [Google Scholar] [CrossRef]
- Singhal, M.; Augustin, H.G. Beyond Angiogenesis: Exploiting Angiocrine Factors to Restrict Tumor Progression and Metastasis. Cancer Res. 2020, 80, 659–662. [Google Scholar] [CrossRef]
- Felmeden, D.C.; Blann, A.D.; Lip, G.Y. Angiogenesis: Basic pathophysiology and implications for disease. Eur. Heart J. 2003, 24, 586–603. [Google Scholar] [CrossRef]
- Ferrara, N.; Gerber, H.P.; LeCouter, J. The biology of VEGF and its receptors. Nat. Med. 2003, 9, 669–676. [Google Scholar] [CrossRef] [PubMed]
- Luttun, A.; Tjwa, M.; Carmeliet, P. Placental growth factor (PlGF) and its receptor Flt-1 (VEGFR-1): Novel therapeutic targets for angiogenic disorders. Ann. N. Y. Acad. Sci. 2002, 979, 80–93. [Google Scholar] [CrossRef]
- Mac Gabhann, F.; Popel, A.S. Systems biology of vascular endothelial growth factors. Microcirculation 2008, 15, 715–738. [Google Scholar] [CrossRef] [PubMed]
- Folkman, J.; Haudenschild, C. Angiogenesis in vitro. Nature 1980, 288, 551–556. [Google Scholar] [CrossRef] [PubMed]
- Pepe, M.; Mamdani, M.; Zentilin, L.; Csiszar, A.; Qanud, K.; Zacchigna, S.; Ungvari, Z.; Puligadda, U.; Moimas, S.; Xu, X.; et al. Intramyocardial VEGF-B167 gene delivery delays the progression towards congestive failure in dogs with pacing-induced dilated cardiomyopathy. Circ. Res. 2010, 106, 1893–1903. [Google Scholar] [CrossRef] [PubMed]
- Woitek, F.; Zentilin, L.; Hoffman, N.E.; Powers, J.C.; Ottiger, I.; Parikh, S.; Kulczycki, A.M.; Hurst, M.; Ring, N.; Wang, T.; et al. Intracoronary Cytoprotective Gene Therapy: A Study of VEGF-B167 in a Pre-Clinical Animal Model of Dilated Cardiomyopathy. J. Am. Coll. Cardiol. 2015, 66, 139–153. [Google Scholar] [CrossRef] [PubMed]
- Callera, G.; Tostes, R.; Savoia, C.; Muscara, M.N.; Touyz, R.M. Vasoactive peptides in cardiovascular (patho)physiology. Expert Rev. Cardiovasc. Ther. 2007, 5, 531–552. [Google Scholar] [CrossRef]
- Davis, G.E.; Senger, D.R. Endothelial extracellular matrix: Biosynthesis, remodeling, and functions during vascular morphogenesis and neovessel stabilization. Circ. Res. 2005, 97, 1093–1107. [Google Scholar] [CrossRef]
- Drummond, G.R.; Vinh, A.; Guzik, T.J.; Sobey, C.G. Immune mechanisms of hypertension. Nat. Rev. Immunol. 2019, 19, 517–532. [Google Scholar] [CrossRef]
- Norlander, A.E.; Madhur, M.S.; Harrison, D.G. The immunology of hypertension. J. Exp. Med. 2018, 215, 21–33. [Google Scholar] [CrossRef] [PubMed]
- Carnevale, D.; Pallante, F.; Fardella, V.; Fardella, S.; Iacobucci, R.; Federici, M.; Cifelli, G.; De Lucia, M.; Lembo, G. The angiogenic factor PlGF mediates a neuroimmune interaction in the spleen to allow the onset of hypertension. Immunity 2014, 41, 737–752. [Google Scholar] [CrossRef] [PubMed]
- Khurana, R.; Moons, L.; Shafi, S.; Luttun, A.; Collen, D.; Martin, J.F.; Carmeliet, P.; Zachary, I.C. Placental growth factor promotes atherosclerotic intimal thickening and macrophage accumulation. Circulation 2005, 111, 2828–2836. [Google Scholar] [CrossRef] [PubMed]
- Perrotta, M.; Lori, A.; Carnevale, L.; Fardella, S.; Cifelli, G.; Iacobucci, R.; Mastroiacovo, F.; Iodice, D.; Pallante, F.; Storto, M.; et al. Deoxycorticosterone acetate-salt hypertension activates placental growth factor in the spleen to couple sympathetic drive and immune system activation. Cardiovasc. Res. 2018, 114, 456–467. [Google Scholar] [CrossRef]
- Hausenloy, D.J.; Yellon, D.M. Cardioprotective growth factors. Cardiovasc. Res. 2009, 83, 179–194. [Google Scholar] [CrossRef]
- Hausenloy, D.J.; Yellon, D.M. New directions for protecting the heart against ischaemia-reperfusion injury: Targeting the Reperfusion Injury Salvage Kinase (RISK)-pathway. Cardiovasc. Res. 2004, 61, 448–460. [Google Scholar] [CrossRef]
- Hausenloy, D.J.; Yellon, D.M. Survival kinases in ischemic preconditioning and postconditioning. Cardiovasc. Res. 2006, 70, 240–253. [Google Scholar] [CrossRef]
- Messadi, E.; Aloui, Z.; Belaidi, E.; Vincent, M.P.; Couture-Lepetit, E.; Waeckel, L.; Decorps, J.; Bouby, N.; Gasmi, A.; Karoui, H.; et al. Cardioprotective effect of VEGF and venom VEGF-like protein in acute myocardial ischemia in mice: Effect on mitochondrial function. J. Cardiovasc. Pharmacol. 2014, 63, 274–281. [Google Scholar] [CrossRef]
- Markel, T.A.; Wang, Y.; Herrmann, J.L.; Crisostomo, P.R.; Wang, M.; Novotny, N.M.; Herring, C.M.; Tan, J.; Lahm, T.; Meldrum, D.R. VEGF is critical for stem cell-mediated cardioprotection and a crucial paracrine factor for defining the age threshold in adult and neonatal stem cell function. Am. J. Physiol. Heart Circ. Physiol. 2008, 295, H2308–H2314. [Google Scholar] [CrossRef]
- Madonna, R.; Petrov, L.; Teberino, M.A.; Manzoli, L.; Karam, J.P.; Renna, F.V.; Ferdinandy, P.; Montero-Menei, C.N.; Yla-Herttuala, S.; De Caterina, R. Transplantation of adipose tissue mesenchymal cells conjugated with VEGF-releasing microcarriers promotes repair in murine myocardial infarction. Cardiovasc. Res. 2015, 108, 39–49. [Google Scholar] [CrossRef]
- Addya, S.; Shiroto, K.; Turoczi, T.; Zhan, L.; Kaga, S.; Fukuda, S.; Surrey, S.; Duan, L.J.; Fong, G.H.; Yamamoto, F.; et al. Ischemic preconditioning-mediated cardioprotection is disrupted in heterozygous Flt-1 (VEGFR-1) knockout mice. J. Mol. Cell. Cardiol. 2005, 38, 345–351. [Google Scholar] [CrossRef]
- Ueno, K.; Samura, M.; Nakamura, T.; Tanaka, Y.; Takeuchi, Y.; Kawamura, D.; Takahashi, M.; Hosoyama, T.; Morikage, N.; Hamano, K. Increased plasma VEGF levels following ischemic preconditioning are associated with downregulation of miRNA-762 and miR-3072-5p. Sci. Rep. 2016, 6, 36758. [Google Scholar] [CrossRef] [PubMed]
- Zheng, Y.; Lu, X.; Li, J.; Zhang, Q.; Reinhardt, J.D. Impact of remote physiological ischemic training on vascular endothelial growth factor, endothelial progenitor cells and coronary angiogenesis after myocardial ischemia. Int. J. Cardiol. 2014, 177, 894–901. [Google Scholar] [CrossRef] [PubMed]
- Qian, B.; Yang, Y.; Yao, Y.; Liao, Y.; Lin, Y. Upregulation of vascular endothelial growth factor receptor-1 contributes to sevoflurane preconditioning-mediated cardioprotection. Drug Des. Devel. Ther. 2018, 12, 769–776. [Google Scholar] [CrossRef] [PubMed]
- Henry, T.D.; Annex, B.H.; McKendall, G.R.; Azrin, M.A.; Lopez, J.J.; Giordano, F.J.; Shah, P.K.; Willerson, J.T.; Benza, R.L.; Berman, D.S.; et al. The VIVA trial: Vascular endothelial growth factor in Ischemia for Vascular Angiogenesis. Circulation 2003, 107, 1359–1365. [Google Scholar] [CrossRef]
- Simons, M.; Annex, B.H.; Laham, R.J.; Kleiman, N.; Henry, T.; Dauerman, H.; Udelson, J.E.; Gervino, E.V.; Pike, M.; Whitehouse, M.J.; et al. Pharmacological treatment of coronary artery disease with recombinant fibroblast growth factor-2: Double-blind, randomized, controlled clinical trial. Circulation 2002, 105, 788–793. [Google Scholar] [CrossRef]
- Sabra, M.; Karbasiafshar, C.; Aboulgheit, A.; Raj, S.; Abid, M.R.; Sellke, F.W. Clinical Application of Novel Therapies for Coronary Angiogenesis: Overview, Challenges, and Prospects. Int. J. Mol. Sci. 2021, 22, 3722. [Google Scholar] [CrossRef]
- McLornan, D.P.; List, A.; Mufti, G.J. Applying synthetic lethality for the selective targeting of cancer. N. Engl. J. Med. 2014, 371, 1725–1735. [Google Scholar] [CrossRef] [PubMed]
- Jayson, G.C.; Kerbel, R.; Ellis, L.M.; Harris, A.L. Antiangiogenic therapy in oncology: Current status and future directions. Lancet 2016, 388, 518–529. [Google Scholar] [CrossRef]
- Ho, Y.J.; Wang, T.C.; Fan, C.H.; Yeh, C.K. Current progress in antivascular tumor therapy. Drug Discov. Today 2017, 22, 1503–1515. [Google Scholar] [CrossRef] [PubMed]
- Kerbel, R.S. Antiangiogenic therapy: A universal chemosensitization strategy for cancer? Science 2006, 312, 1171–1175. [Google Scholar] [CrossRef] [PubMed]
- Ferrarotto, R.; Hoff, P.M. Antiangiogenic drugs for colorectal cancer: Exploring new possibilities. Clin. Colorectal. Cancer 2013, 12, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Nagy, J.A.; Dvorak, A.M.; Dvorak, H.F. VEGF-A and the induction of pathological angiogenesis. Annu. Rev. Pathol. 2007, 2, 251–275. [Google Scholar] [CrossRef] [PubMed]
- Qin, S.; Li, A.; Yi, M.; Yu, S.; Zhang, M.; Wu, K. Recent advances on anti-angiogenesis receptor tyrosine kinase inhibitors in cancer therapy. J. Hematol. Oncol. 2019, 12, 27. [Google Scholar] [CrossRef] [PubMed]
- Hasskarl, J. Sorafenib: Targeting multiple tyrosine kinases in cancer. Recent Results Cancer Res. 2014, 201, 145–164. [Google Scholar] [CrossRef]
- Tocchetti, C.G.; Gallucci, G.; Coppola, C.; Piscopo, G.; Cipresso, C.; Maurea, C.; Giudice, A.; Iaffaioli, R.V.; Arra, C.; Maurea, N. The emerging issue of cardiac dysfunction induced by antineoplastic angiogenesis inhibitors. Eur. J. Heart Fail. 2013, 15, 482–489. [Google Scholar] [CrossRef]
- Cignarella, A.; Fadini, G.P.; Bolego, C.; Trevisi, L.; Boscaro, C.; Sanga, V.; Seccia, T.M.; Rosato, A.; Rossi, G.P.; Barton, M. Clinical efficacy and safety of angiogenesis inhibitors: Sex differences and current challenges. Cardiovasc. Res. 2022, 118, 988–1003. [Google Scholar] [CrossRef]
- Totzeck, M.; Mincu, R.I.; Rassaf, T. Cardiovascular Adverse Events in Patients With Cancer Treated With Bevacizumab: A Meta-Analysis of More than 20,000 Patients. J. Am. Heart Assoc. 2017, 6, e006278. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Gao, Z.H.; Qu, X.J. The adverse effects of sorafenib in patients with advanced cancers. Basic Clin. Pharmacol. Toxicol. 2015, 116, 216–221. [Google Scholar] [CrossRef]
- Justice, C.N.; Derbala, M.H.; Baich, T.M.; Kempton, A.N.; Guo, A.S.; Ho, T.H.; Smith, S.A. The Impact of Pazopanib on the Cardiovascular System. J. Cardiovasc. Pharmacol. Ther. 2018, 23, 387–398. [Google Scholar] [CrossRef]
- Grande, E.; Kreissl, M.C.; Filetti, S.; Newbold, K.; Reinisch, W.; Robert, C.; Schlumberger, M.; Tolstrup, L.K.; Zamorano, J.L.; Capdevila, J. Vandetanib in advanced medullary thyroid cancer: Review of adverse event management strategies. Adv. Ther. 2013, 30, 945–966. [Google Scholar] [CrossRef] [PubMed]
- Tanriverdi, O.; Ates, S.; Sandal, K.K.; Uylas, S.; Bosna, I.C.; Alkan, A. Left ventricular dysfunction associated with axitinib and nivolumab experience in an advanced renal cell carcinoma. J. Oncol. Pharm. Pract. 2020, 26, 1765–1768. [Google Scholar] [CrossRef] [PubMed]
- Richter, M.J.; Ewert, J.; Grimminger, F.; Ghofrani, H.A.; Kojonazarov, B.; Petrovic, A.; Seeger, W.; Schermuly, R.T.; Tello, K.; Gall, H. Nintedanib in Severe Pulmonary Arterial Hypertension. Am. J. Respir. Crit. Care Med. 2018, 198, 808–810. [Google Scholar] [CrossRef] [PubMed]
- Cabanillas, M.E.; Takahashi, S. Managing the adverse events associated with lenvatinib therapy in radioiodine-refractory differentiated thyroid cancer. Semin. Oncol. 2019, 46, 57–64. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, G.; Darling, J.O.; Mindo, M.; Damicis, L. Management of Adverse Events Associated with Cabozantinib Treatment in Patients with Advanced Hepatocellular Carcinoma. Target Oncol. 2020, 15, 549–565. [Google Scholar] [CrossRef]
- Joensuu, H. Cardiac toxicity of sunitinib. Lancet 2007, 370, 1978–1980. [Google Scholar] [CrossRef]
- Molina, A.M.; Hutson, T.E.; Nosov, D.; Tomczak, P.; Lipatov, O.; Sternberg, C.N.; Motzer, R.; Eisen, T. Efficacy of tivozanib treatment after sorafenib in patients with advanced renal cell carcinoma: Crossover of a phase 3 study. Eur. J. Cancer 2018, 94, 87–94. [Google Scholar] [CrossRef]
- Casavecchia, G.; Galderisi, M.; Novo, G.; Gravina, M.; Santoro, C.; Agricola, E.; Capalbo, S.; Zicchino, S.; Cameli, M.; De Gennaro, L.; et al. Early diagnosis, clinical management, and follow-up of cardiovascular events with ponatinib. Heart Fail. Rev. 2020, 25, 447–456. [Google Scholar] [CrossRef]
- Abdel-Rahman, O.; ElHalawani, H. Risk of cardiovascular adverse events in patients with solid tumors treated with ramucirumab: A meta analysis and summary of other VEGF targeted agents. Crit. Rev. Oncol. Hematol. 2016, 102, 89–100. [Google Scholar] [CrossRef]
- Pandey, A.K.; Singhi, E.K.; Arroyo, J.P.; Ikizler, T.A.; Gould, E.R.; Brown, J.; Beckman, J.A.; Harrison, D.G.; Moslehi, J. Mechanisms of VEGF (Vascular Endothelial Growth Factor) Inhibitor-Associated Hypertension and Vascular Disease. Hypertension 2018, 71, e1–e8. [Google Scholar] [CrossRef]
- Chen, H.X.; Cleck, J.N. Adverse effects of anticancer agents that target the VEGF pathway. Nat. Rev. Clin. Oncol. 2009, 6, 465–477. [Google Scholar] [CrossRef] [PubMed]
- Dobbin, S.J.H.; Cameron, A.C.; Petrie, M.C.; Jones, R.J.; Touyz, R.M.; Lang, N.N. Toxicity of cancer therapy: What the cardiologist needs to know about angiogenesis inhibitors. Heart 2018, 104, 1995–2002. [Google Scholar] [CrossRef] [PubMed]
- Touyz, R.M.; Herrmann, S.M.S.; Herrmann, J. Vascular toxicities with VEGF inhibitor therapies-focus on hypertension and arterial thrombotic events. J. Am. Soc. Hypertens. 2018, 12, 409–425. [Google Scholar] [CrossRef] [PubMed]
- Versmissen, J.; Mirabito Colafella, K.M.; Koolen, S.L.W.; Danser, A.H.J. Vascular Cardio-Oncology: Vascular Endothelial Growth Factor inhibitors and hypertension. Cardiovasc. Res. 2019, 115, 904–914. [Google Scholar] [CrossRef]
- Fukumura, D.; Kloepper, J.; Amoozgar, Z.; Duda, D.G.; Jain, R.K. Enhancing cancer immunotherapy using antiangiogenics: Opportunities and challenges. Nat. Rev. Clin. Oncol. 2018, 15, 325–340. [Google Scholar] [CrossRef]
- Drobni, Z.D.; Alvi, R.M.; Taron, J.; Zafar, A.; Murphy, S.P.; Rambarat, P.K.; Mosarla, R.C.; Lee, C.; Zlotoff, D.A.; Raghu, V.K.; et al. Association Between Immune Checkpoint Inhibitors With Cardiovascular Events and Atherosclerotic Plaque. Circulation 2020, 142, 2299–2311. [Google Scholar] [CrossRef]
- Poels, K.; van Leent, M.M.T.; Boutros, C.; Tissot, H.; Roy, S.; Meerwaldt, A.E.; Toner, Y.C.A.; Reiche, M.E.; Kusters, P.J.H.; Malinova, T.; et al. Immune Checkpoint Inhibitor Therapy Aggravates T Cell-Driven Plaque Inflammation in Atherosclerosis. JACC CardioOncol. 2020, 2, 599–610. [Google Scholar] [CrossRef]
- Li, J.L.; Harris, A.L. Crosstalk of VEGF and Notch pathways in tumour angiogenesis: Therapeutic implications. Front. Biosci. (Landmark Ed) 2009, 14, 3094–3110. [Google Scholar] [CrossRef]
- Benedito, R.; Rocha, S.F.; Woeste, M.; Zamykal, M.; Radtke, F.; Casanovas, O.; Duarte, A.; Pytowski, B.; Adams, R.H. Notch-dependent VEGFR3 upregulation allows angiogenesis without VEGF-VEGFR2 signalling. Nature 2012, 484, 110–114. [Google Scholar] [CrossRef]
- Jaszai, J.; Schmidt, M.H.H. Trends and Challenges in Tumor Anti-Angiogenic Therapies. Cells 2019, 8, 1102. [Google Scholar] [CrossRef]
- Leroyer, A.S.; Blin, M.G.; Bachelier, R.; Bardin, N.; Blot-Chabaud, M.; Dignat-George, F. CD146 (Cluster of Differentiation 146). Arterioscler. Thromb. Vasc. Biol. 2019, 39, 1026–1033. [Google Scholar] [CrossRef] [PubMed]
- Stalin, J.; Nollet, M.; Garigue, P.; Fernandez, S.; Vivancos, L.; Essaadi, A.; Muller, A.; Bachelier, R.; Foucault-Bertaud, A.; Fugazza, L.; et al. Targeting soluble CD146 with a neutralizing antibody inhibits vascularization, growth and survival of CD146-positive tumors. Oncogene 2016, 35, 5489–5500. [Google Scholar] [CrossRef] [PubMed]
- Luo, Y.; Teng, X.; Zhang, L.; Chen, J.; Liu, Z.; Chen, X.; Zhao, S.; Yang, S.; Feng, J.; Yan, X. CD146-HIF-1alpha hypoxic reprogramming drives vascular remodeling and pulmonary arterial hypertension. Nat. Commun. 2019, 10, 3551. [Google Scholar] [CrossRef] [PubMed]
- Krause, D.S.; Van Etten, R.A. Tyrosine kinases as targets for cancer therapy. N. Engl. J. Med. 2005, 353, 172–187. [Google Scholar] [CrossRef] [PubMed]
- Lacal, P.M.; Graziani, G. Therapeutic implication of vascular endothelial growth factor receptor-1 (VEGFR-1) targeting in cancer cells and tumor microenvironment by competitive and non-competitive inhibitors. Pharmacol. Res. 2018, 136, 97–107. [Google Scholar] [CrossRef]
- Schmidt, K.T.; Chau, C.H.; Price, D.K.; Figg, W.D. Precision Oncology Medicine: The Clinical Relevance of Patient-Specific Biomarkers Used to Optimize Cancer Treatment. J. Clin. Pharmacol. 2016, 56, 1484–1499. [Google Scholar] [CrossRef]
- Herrmann, J. Adverse cardiac effects of cancer therapies: Cardiotoxicity and arrhythmia. Nat. Rev. Cardiol. 2020, 17, 474–502. [Google Scholar] [CrossRef]
- Herrmann, J. Vascular toxic effects of cancer therapies. Nat. Rev. Cardiol. 2020, 17, 503–522. [Google Scholar] [CrossRef]
- Neves, K.B.; Montezano, A.C.; Lang, N.N.; Touyz, R.M. Vascular toxicity associated with anti-angiogenic drugs. Clin. Sci. 2020, 134, 2503–2520. [Google Scholar] [CrossRef]
- Rossi, G.P.; Seccia, T.M.; Maniero, C.; Pessina, A.C. Drug-related hypertension and resistance to antihypertensive treatment: A call for action. J. Hypertens. 2011, 29, 2295–2309. [Google Scholar] [CrossRef]
- Carmeliet, P.; Jain, R.K. Molecular mechanisms and clinical applications of angiogenesis. Nature 2011, 473, 298–307. [Google Scholar] [CrossRef] [PubMed]
- Fadini, G.P.; Albiero, M.; Bonora, B.M.; Avogaro, A. Angiogenic Abnormalities in Diabetes Mellitus: Mechanistic and Clinical Aspects. J. Clin. Endocrinol. Metab. 2019, 104, 5431–5444. [Google Scholar] [CrossRef] [PubMed]
- Almond, J.B.; Cohen, G.M. The proteasome: A novel target for cancer chemotherapy. Leukemia 2002, 16, 433–443. [Google Scholar] [CrossRef] [PubMed]
- Yu, X.; Kem, D.C. Proteasome inhibition during myocardial infarction. Cardiovasc. Res. 2010, 85, 312–320. [Google Scholar] [CrossRef] [PubMed]
- Drews, O.; Wildgruber, R.; Zong, C.; Sukop, U.; Nissum, M.; Weber, G.; Gomes, A.V.; Ping, P. Mammalian proteasome subpopulations with distinct molecular compositions and proteolytic activities. Mol. Cell. Proteom. 2007, 6, 2021–2031. [Google Scholar] [CrossRef] [PubMed]
- Gomes, A.V.; Young, G.W.; Wang, Y.; Zong, C.; Eghbali, M.; Drews, O.; Lu, H.; Stefani, E.; Ping, P. Contrasting proteome biology and functional heterogeneity of the 20 S proteasome complexes in mammalian tissues. Mol. Cell. Proteom. 2009, 8, 302–315. [Google Scholar] [CrossRef] [PubMed]
- Young, G.W.; Wang, Y.; Ping, P. Understanding proteasome assembly and regulation: Importance to cardiovascular medicine. Trends Cardiovasc. Med. 2008, 18, 93–98. [Google Scholar] [CrossRef][Green Version]
- Mearini, G.; Schlossarek, S.; Willis, M.S.; Carrier, L. The ubiquitin-proteasome system in cardiac dysfunction. Biochim. Biophys. Acta 2008, 1782, 749–763. [Google Scholar] [CrossRef]
- Bulteau, A.L.; Szweda, L.I.; Friguet, B. Age-dependent declines in proteasome activity in the heart. Arch. Biochem. Biophys. 2002, 397, 298–304. [Google Scholar] [CrossRef]
- Li, Y.F.; Wang, X. The role of the proteasome in heart disease. Biochim. Biophys. Acta 2011, 1809, 141–149. [Google Scholar] [CrossRef]
- Cai, Z.P.; Shen, Z.; Van Kaer, L.; Becker, L.C. Ischemic preconditioning-induced cardioprotection is lost in mice with immunoproteasome subunit low molecular mass polypeptide-2 deficiency. FASEB J. 2008, 22, 4248–4257. [Google Scholar] [CrossRef] [PubMed]
- Gomes, A.V.; Zong, C.; Edmondson, R.D.; Li, X.; Stefani, E.; Zhang, J.; Jones, R.C.; Thyparambil, S.; Wang, G.W.; Qiao, X.; et al. Mapping the murine cardiac 26S proteasome complexes. Circ. Res. 2006, 99, 362–371. [Google Scholar] [CrossRef] [PubMed]
- Rechsteiner, M.; Hill, C.P. Mobilizing the proteolytic machine: Cell biological roles of proteasome activators and inhibitors. Trends Cell Biol. 2005, 15, 27–33. [Google Scholar] [CrossRef] [PubMed]
- Powell, S.R.; Samuel, S.M.; Wang, P.; Divald, A.; Thirunavukkarasu, M.; Koneru, S.; Wang, X.; Maulik, N. Upregulation of myocardial 11S-activated proteasome in experimental hyperglycemia. J. Mol. Cell. Cardiol. 2008, 44, 618–621. [Google Scholar] [CrossRef] [PubMed]
- Kirk, R.; Laman, H.; Knowles, P.P.; Murray-Rust, J.; Lomonosov, M.; Meziane, E.K.; McDonald, N.Q. Structure of a conserved dimerization domain within the F-box protein Fbxo7 and the PI31 proteasome inhibitor. J. Biol. Chem. 2008, 283, 22325–22335. [Google Scholar] [CrossRef] [PubMed]
- Efentakis, P.; Kremastiotis, G.; Varela, A.; Nikolaou, P.E.; Papanagnou, E.D.; Davos, C.H.; Tsoumani, M.; Agrogiannis, G.; Konstantinidou, A.; Kastritis, E.; et al. Molecular mechanisms of carfilzomib-induced cardiotoxicity in mice and the emerging cardioprotective role of metformin. Blood 2019, 133, 710–723. [Google Scholar] [CrossRef]
- Bulteau, A.L.; Lundberg, K.C.; Humphries, K.M.; Sadek, H.A.; Szweda, P.A.; Friguet, B.; Szweda, L.I. Oxidative modification and inactivation of the proteasome during coronary occlusion/reperfusion. J. Biol. Chem. 2001, 276, 30057–30063. [Google Scholar] [CrossRef]
- Powell, S.R.; Wang, P.; Katzeff, H.; Shringarpure, R.; Teoh, C.; Khaliulin, I.; Das, D.K.; Davies, K.J.; Schwalb, H. Oxidized and ubiquitinated proteins may predict recovery of postischemic cardiac function: Essential role of the proteasome. Antioxid. Redox Signal. 2005, 7, 538–546. [Google Scholar] [CrossRef]
- Gurusamy, N.; Goswami, S.; Malik, G.; Das, D.K. Oxidative injury induces selective rather than global inhibition of proteasomal activity. J. Mol. Cell. Cardiol. 2008, 44, 419–428. [Google Scholar] [CrossRef]
- Asai, M.; Tsukamoto, O.; Minamino, T.; Asanuma, H.; Fujita, M.; Asano, Y.; Takahama, H.; Sasaki, H.; Higo, S.; Asakura, M.; et al. PKA rapidly enhances proteasome assembly and activity in in vivo canine hearts. J. Mol. Cell. Cardiol. 2009, 46, 452–462. [Google Scholar] [CrossRef]
- Adams, V.; Linke, A.; Gielen, S.; Erbs, S.; Hambrecht, R.; Schuler, G. Modulation of Murf-1 and MAFbx expression in the myocardium by physical exercise training. Eur. J. Cardiovasc. Prev. Rehabil. 2008, 15, 293–299. [Google Scholar] [CrossRef] [PubMed]
- Hedhli, N.; Lizano, P.; Hong, C.; Fritzky, L.F.; Dhar, S.K.; Liu, H.; Tian, Y.; Gao, S.; Madura, K.; Vatner, S.F.; et al. Proteasome inhibition decreases cardiac remodeling after initiation of pressure overload. Am. J. Physiol. Heart Circ. Physiol. 2008, 295, H1385–H1393. [Google Scholar] [CrossRef] [PubMed]
- Taegtmeyer, H.; King, L.M.; Jones, B.E. Energy substrate metabolism, myocardial ischemia, and targets for pharmacotherapy. Am. J. Cardiol. 1998, 82, 54K–60K. [Google Scholar] [CrossRef]
- Powell, S.R.; Davies, K.J.; Divald, A. Optimal determination of heart tissue 26S-proteasome activity requires maximal stimulating ATP concentrations. J. Mol. Cell. Cardiol. 2007, 42, 265–269. [Google Scholar] [CrossRef] [PubMed]
- Sohns, W.; van Veen, T.A.; van der Heyden, M.A. Regulatory roles of the ubiquitin-proteasome system in cardiomyocyte apoptosis. Curr. Mol. Med. 2010, 10, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Naito, A.T.; Okada, S.; Minamino, T.; Iwanaga, K.; Liu, M.L.; Sumida, T.; Nomura, S.; Sahara, N.; Mizoroki, T.; Takashima, A.; et al. Promotion of CHIP-mediated p53 degradation protects the heart from ischemic injury. Circ. Res. 2010, 106, 1692–1702. [Google Scholar] [CrossRef]
- Tsukamoto, O.; Minamino, T.; Okada, K.; Shintani, Y.; Takashima, S.; Kato, H.; Liao, Y.; Okazaki, H.; Asai, M.; Hirata, A.; et al. Depression of proteasome activities during the progression of cardiac dysfunction in pressure-overloaded heart of mice. Biochem. Biophys. Res. Commun. 2006, 340, 1125–1133. [Google Scholar] [CrossRef]
- Churchill, E.N.; Mochly-Rosen, D. The roles of PKCdelta and epsilon isoenzymes in the regulation of myocardial ischaemia/reperfusion injury. Biochem. Soc. Trans. 2007, 35 Pt 5, 1040–1042. [Google Scholar] [CrossRef]
- Powell, S.R.; Gurzenda, E.M.; Teichberg, S.; Mantell, L.L.; Maulik, D. Association of increased ubiquitinated proteins with cardiac apoptosis. Antioxid. Redox Signal. 2000, 2, 103–112. [Google Scholar] [CrossRef]
- Campbell, B.; Adams, J.; Shin, Y.K.; Lefer, A.M. Cardioprotective effects of a novel proteasome inhibitor following ischemia and reperfusion in the isolated perfused rat heart. J. Mol. Cell. Cardiol. 1999, 31, 467–476. [Google Scholar] [CrossRef]
- Yu, X.; Patterson, E.; Kem, D.C. Targeting proteasomes for cardioprotection. Curr. Opin. Pharmacol. 2009, 9, 167–172. [Google Scholar] [CrossRef] [PubMed]
- Bao, J.; Sato, K.; Li, M.; Gao, Y.; Abid, R.; Aird, W.; Simons, M.; Post, M.J. PR-39 and PR-11 peptides inhibit ischemia-reperfusion injury by blocking proteasome-mediated I kappa B alpha degradation. Am. J. Physiol. Heart Circ. Physiol. 2001, 281, H2612–H2618. [Google Scholar] [CrossRef] [PubMed]
- Frangogiannis, N.G.; Smith, C.W.; Entman, M.L. The inflammatory response in myocardial infarction. Cardiovasc. Res. 2002, 53, 31–47. [Google Scholar] [CrossRef]
- Wang, J.; Maldonado, M.A. The ubiquitin-proteasome system and its role in inflammatory and autoimmune diseases. Cell. Mol. Immunol. 2006, 3, 255–261. [Google Scholar] [PubMed]
- Kis, A.; Yellon, D.M.; Baxter, G.F. Role of nuclear factor-kappa B activation in acute ischaemia-reperfusion injury in myocardium. Br. J. Pharmacol. 2003, 138, 894–900. [Google Scholar] [CrossRef]
- Morishita, R.; Sugimoto, T.; Aoki, M.; Kida, I.; Tomita, N.; Moriguchi, A.; Maeda, K.; Sawa, Y.; Kaneda, Y.; Higaki, J.; et al. In vivo transfection of cis element "decoy" against nuclear factor-kappaB binding site prevents myocardial infarction. Nat. Med. 1997, 3, 894–899. [Google Scholar] [CrossRef]
- Moss, N.C.; Stansfield, W.E.; Willis, M.S.; Tang, R.H.; Selzman, C.H. IKKbeta inhibition attenuates myocardial injury and dysfunction following acute ischemia-reperfusion injury. Am. J. Physiol. Heart Circ. Physiol. 2007, 293, H2248–H2253. [Google Scholar] [CrossRef]
- Moss, N.C.; Tang, R.H.; Willis, M.; Stansfield, W.E.; Baldwin, A.S.; Selzman, C.H. Inhibitory kappa B kinase-beta is a target for specific nuclear factor kappa B-mediated delayed cardioprotection. J. Thorac. Cardiovasc. Surg. 2008, 136, 1274–1279. [Google Scholar] [CrossRef]
- Jurado-Pueyo, M.; Campos, P.M.; Mayor, F.; Murga, C. GRK2-dependent desensitization downstream of G proteins. J. Recept. Signal Transduct. Res. 2008, 28, 59–70. [Google Scholar] [CrossRef]
- Penela, P.; Murga, C.; Ribas, C.; Tutor, A.S.; Peregrin, S.; Mayor, F., Jr. Mechanisms of regulation of G protein-coupled receptor kinases (GRKs) and cardiovascular disease. Cardiovasc. Res. 2006, 69, 46–56. [Google Scholar] [CrossRef]
- Metaye, T.; Gibelin, H.; Perdrisot, R.; Kraimps, J.L. Pathophysiological roles of G-protein-coupled receptor kinases. Cell Signal. 2005, 17, 917–928. [Google Scholar] [CrossRef] [PubMed]
- Tevaearai, H.T.; Koch, W.J. Molecular restoration of beta-adrenergic receptor signaling improves contractile function of failing hearts. Trends Cardiovasc. Med. 2004, 14, 252–256. [Google Scholar] [CrossRef] [PubMed]
- Yu, X.; Zhang, M.; Kyker, K.; Patterson, E.; Benovic, J.L.; Kem, D.C. Ischemic inactivation of G protein-coupled receptor kinase and altered desensitization of canine cardiac beta-adrenergic receptors. Circulation 2000, 102, 2535–2540. [Google Scholar] [CrossRef] [PubMed]
- Theilade, J.; Strom, C.; Christiansen, T.; Haunso, S.; Sheikh, S.P. Differential G protein receptor kinase 2 expression in compensated hypertrophy and heart failure after myocardial infarction in the rat. Basic Res. Cardiol. 2003, 98, 97–103. [Google Scholar] [CrossRef] [PubMed]
- Penela, P.; Ruiz-Gomez, A.; Castano, J.G.; Mayor, F., Jr. Degradation of the G protein-coupled receptor kinase 2 by the proteasome pathway. J. Biol. Chem. 1998, 273, 35238–35244. [Google Scholar] [CrossRef]
- Elorza, A.; Penela, P.; Sarnago, S.; Mayor, F., Jr. MAPK-dependent degradation of G protein-coupled receptor kinase 2. J. Biol. Chem. 2003, 278, 29164–29173. [Google Scholar] [CrossRef]
- Penela, P.; Elorza, A.; Sarnago, S.; Mayor, F., Jr. Beta-arrestin- and c-Src-dependent degradation of G-protein-coupled receptor kinase 2. EMBO J. 2001, 20, 5129–5138. [Google Scholar] [CrossRef]
- Salcedo, A.; Mayor, F., Jr.; Penela, P. Mdm2 is involved in the ubiquitination and degradation of G-protein-coupled receptor kinase 2. EMBO J. 2006, 25, 4752–4762. [Google Scholar] [CrossRef]
- Divald, A.; Kivity, S.; Wang, P.; Hochhauser, E.; Roberts, B.; Teichberg, S.; Gomes, A.V.; Powell, S.R. Myocardial ischemic preconditioning preserves postischemic function of the 26S proteasome through diminished oxidative damage to 19S regulatory particle subunits. Circ. Res. 2010, 106, 1829–1838. [Google Scholar] [CrossRef]
- Liu, C.; Chen, S.; Kamme, F.; Hu, B.R. Ischemic preconditioning prevents protein aggregation after transient cerebral ischemia. Neuroscience 2005, 134, 69–80. [Google Scholar] [CrossRef]
- Meller, R.; Cameron, J.A.; Torrey, D.J.; Clayton, C.E.; Ordonez, A.N.; Henshall, D.C.; Minami, M.; Schindler, C.K.; Saugstad, J.A.; Simon, R.P. Rapid degradation of Bim by the ubiquitin-proteasome pathway mediates short-term ischemic tolerance in cultured neurons. J. Biol. Chem. 2006, 281, 7429–7436. [Google Scholar] [CrossRef] [PubMed]
- Pradillo, J.M.; Romera, C.; Hurtado, O.; Cardenas, A.; Moro, M.A.; Leza, J.C.; Davalos, A.; Castillo, J.; Lorenzo, P.; Lizasoain, I. TNFR1 upregulation mediates tolerance after brain ischemic preconditioning. J. Cereb. Blood Flow Metab. 2005, 25, 193–203. [Google Scholar] [CrossRef] [PubMed]
- Calise, J.; Powell, S.R. The ubiquitin proteasome system and myocardial ischemia. Am. J. Physiol. Heart Circ. Physiol. 2013, 304, H337–H349. [Google Scholar] [CrossRef] [PubMed]
- Inagaki, K.; Chen, L.; Ikeno, F.; Lee, F.H.; Imahashi, K.; Bouley, D.M.; Rezaee, M.; Yock, P.G.; Murphy, E.; Mochly-Rosen, D. Inhibition of delta-protein kinase C protects against reperfusion injury of the ischemic heart in vivo. Circulation 2003, 108, 2304–2307. [Google Scholar] [CrossRef] [PubMed]
- Baines, C.P.; Song, C.X.; Zheng, Y.T.; Wang, G.W.; Zhang, J.; Wang, O.L.; Guo, Y.; Bolli, R.; Cardwell, E.M.; Ping, P. Protein kinase Cepsilon interacts with and inhibits the permeability transition pore in cardiac mitochondria. Circ. Res. 2003, 92, 873–880. [Google Scholar] [CrossRef]
- Tian, Z.; Zheng, H.; Li, J.; Li, Y.; Su, H.; Wang, X. Genetically induced moderate inhibition of the proteasome in cardiomyocytes exacerbates myocardial ischemia-reperfusion injury in mice. Circ. Res. 2012, 111, 532–542. [Google Scholar] [CrossRef]
- Yu, X.; Huang, S.; Patterson, E.; Garrett, M.W.; Kaufman, K.M.; Metcalf, J.P.; Zhu, M.; Dunn, S.T.; Kem, D.C. Proteasome degradation of GRK2 during ischemia and ventricular tachyarrhythmias in a canine model of myocardial infarction. Am. J. Physiol. Heart Circ. Physiol. 2005, 289, H1960–H1967. [Google Scholar] [CrossRef]
- Takagi, H.; Hsu, C.P.; Kajimoto, K.; Shao, D.; Yang, Y.; Maejima, Y.; Zhai, P.; Yehia, G.; Yamada, C.; Zablocki, D.; et al. Activation of PKN mediates survival of cardiac myocytes in the heart during ischemia/reperfusion. Circ. Res. 2010, 107, 642–649. [Google Scholar] [CrossRef]
- Dosenko, V.E.; Nagibin, V.S.; Tumanovskaya, L.V.; Zagoriy, V.Y.; Moibenko, A.A.; Vaage, J. Proteasomal proteolysis in anoxia-reoxygenation, preconditioning and postconditioning of isolated cardiomyocytes. Pathophysiology 2006, 13, 119–125. [Google Scholar] [CrossRef]
- Bennett, M.K.; Kirk, C.J. Development of proteasome inhibitors in oncology and autoimmune diseases. Curr. Opin. Drug Discov. Dev. 2008, 11, 616–625. [Google Scholar]
- Huang, S.; Patterson, E.; Yu, X.; Garrett, M.W.; De Aos, I.; Kem, D.C. Proteasome inhibition 1 h following ischemia protects GRK2 and prevents malignant ventricular tachyarrhythmias and SCD in a model of myocardial infarction. Am. J. Physiol. Heart Circ. Physiol. 2008, 294, H1298–H1303. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Pye, J.; Ardeshirpour, F.; McCain, A.; Bellinger, D.A.; Merricks, E.; Adams, J.; Elliott, P.J.; Pien, C.; Fischer, T.H.; Baldwin, A.S., Jr.; et al. Proteasome inhibition ablates activation of NF-kappa B in myocardial reperfusion and reduces reperfusion injury. Am. J. Physiol. Heart Circ. Physiol. 2003, 284, H919–H926. [Google Scholar] [CrossRef] [PubMed]
- Stansfield, W.E.; Moss, N.C.; Willis, M.S.; Tang, R.; Selzman, C.H. Proteasome inhibition attenuates infarct size and preserves cardiac function in a murine model of myocardial ischemia-reperfusion injury. Ann. Thorac. Surg. 2007, 84, 120–125. [Google Scholar] [CrossRef] [PubMed]
- Hoffmeyer, M.R.; Scalia, R.; Ross, C.R.; Jones, S.P.; Lefer, D.J. PR-39, a potent neutrophil inhibitor, attenuates myocardial ischemia-reperfusion injury in mice. Am. J. Physiol. Heart Circ. Physiol. 2000, 279, H2824–H2828. [Google Scholar] [CrossRef]
- Gao, Y.; Lecker, S.; Post, M.J.; Hietaranta, A.J.; Li, J.; Volk, R.; Li, M.; Sato, K.; Saluja, A.K.; Steer, M.L.; et al. Inhibition of ubiquitin-proteasome pathway-mediated I kappa B alpha degradation by a naturally occurring antibacterial peptide. J. Clin. Investig. 2000, 106, 439–448. [Google Scholar] [CrossRef]
- Spinale, F.G. Matrix metalloproteinases: Regulation and dysregulation in the failing heart. Circ. Res. 2002, 90, 520–530. [Google Scholar] [CrossRef]
- Enrico, O.; Gabriele, B.; Nadia, C.; Sara, G.; Daniele, V.; Giulia, C.; Antonio, S.; Mario, P. Unexpected cardiotoxicity in haematological bortezomib treated patients. Br. J. Haematol. 2007, 138, 396–397. [Google Scholar] [CrossRef]
- Hacihanefioglu, A.; Tarkun, P.; Gonullu, E. Acute severe cardiac failure in a myeloma patient due to proteasome inhibitor bortezomib. Int. J. Hematol. 2008, 88, 219–222. [Google Scholar] [CrossRef]
- Mikhail, P.; Rogers, J.; Forsyth, C.; Ford, T.J. Proteasome inhibitor-induced coronary vasospasm in multiple myeloma: A case report. Eur. Heart J. Case Rep. 2021, 5, ytab076. [Google Scholar] [CrossRef]
- Efentakis, P.; Doerschmann, H.; Witzler, C.; Siemer, S.; Nikolaou, P.E.; Kastritis, E.; Stauber, R.; Dimopoulos, M.A.; Wenzel, P.; Andreadou, I.; et al. Investigating the Vascular Toxicity Outcomes of the Irreversible Proteasome Inhibitor Carfilzomib. Int. J. Mol. Sci. 2020, 21, 5185. [Google Scholar] [CrossRef]
- Dimopoulos, M.A.; Moreau, P.; Palumbo, A.; Joshua, D.; Pour, L.; Hajek, R.; Facon, T.; Ludwig, H.; Oriol, A.; Goldschmidt, H.; et al. Carfilzomib and dexamethasone versus bortezomib and dexamethasone for patients with relapsed or refractory multiple myeloma (ENDEAVOR): A randomised, phase 3, open-label, multicentre study. Lancet Oncol. 2016, 17, 27–38. [Google Scholar] [CrossRef]
- Ling, Y.; Li, R.; Zhong, J.; Zhao, Y.; Chen, Z. Ixazomib-associated cardiovascular adverse events in multiple myeloma: A systematic review and meta-analysis. Drug Chem. Toxicol. 2020, 45, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Heckmann, M.B.; Doroudgar, S.; Katus, H.A.; Lehmann, L.H. Cardiovascular adverse events in multiple myeloma patients. J. Thorac. Dis. 2018, 10 (Suppl. 35), S4296–S4305. [Google Scholar] [CrossRef] [PubMed]
- Kloss, A.; Meiners, S.; Ludwig, A.; Dahlmann, B. Multiple cardiac proteasome subtypes differ in their susceptibility to proteasome inhibitors. Cardiovasc. Res. 2010, 85, 367–375. [Google Scholar] [CrossRef] [PubMed]
- Xie, P.; Guo, S.; Fan, Y.; Zhang, H.; Gu, D.; Li, H. Atrogin-1/MAFbx enhances simulated ischemia/reperfusion-induced apoptosis in cardiomyocytes through degradation of MAPK phosphatase-1 and sustained JNK activation. J. Biol. Chem. 2009, 284, 5488–5496. [Google Scholar] [CrossRef] [PubMed]
- Ostrowska, H. The ubiquitin-proteasome system: A novel target for anticancer and anti-inflammatory drug research. Cell. Mol. Biol. Lett. 2008, 13, 353–365. [Google Scholar] [CrossRef]
- Gustafsson, A.B.; Gottlieb, R.A. Eat your heart out: Role of autophagy in myocardial ischemia/reperfusion. Autophagy 2008, 4, 416–421. [Google Scholar] [CrossRef]
- La, J.; Cheng, D.; Brophy, M.T.; Do, N.V.; Lee, J.S.H.; Tuck, D.; Fillmore, N.R. Real-World Outcomes for Patients Treated With Immune Checkpoint Inhibitors in the Veterans Affairs System. JCO Clin. Cancer Inform. 2020, 4, 918–928. [Google Scholar] [CrossRef]
- Patel, R.P.; Parikh, R.; Gunturu, K.S.; Tariq, R.Z.; Dani, S.S.; Ganatra, S.; Nohria, A. Cardiotoxicity of Immune Checkpoint Inhibitors. Curr. Oncol. Rep. 2021, 23, 79. [Google Scholar] [CrossRef]
- Thuny, F.; Naidoo, J.; Neilan, T.G. Cardiovascular complications of immune checkpoint inhibitors for cancer. Eur. Heart J. 2022, 43, 4458–4468. [Google Scholar] [CrossRef]
- Matsumoto, T.; Sasaki, N.; Yamashita, T.; Emoto, T.; Kasahara, K.; Mizoguchi, T.; Hayashi, T.; Yodoi, K.; Kitano, N.; Saito, T.; et al. Overexpression of Cytotoxic T-Lymphocyte-Associated Antigen-4 Prevents Atherosclerosis in Mice. Arterioscler. Thromb. Vasc. Biol. 2016, 36, 1141–1151. [Google Scholar] [CrossRef] [PubMed]
- Ma, K.; Lv, S.; Liu, B.; Liu, Z.; Luo, Y.; Kong, W.; Xu, Q.; Feng, J.; Wang, X. CTLA4-IgG ameliorates homocysteine-accelerated atherosclerosis by inhibiting T-cell overactivation in apoE(-/-) mice. Cardiovasc. Res. 2013, 97, 349–359. [Google Scholar] [CrossRef] [PubMed]
- Bu, D.X.; Tarrio, M.; Maganto-Garcia, E.; Stavrakis, G.; Tajima, G.; Lederer, J.; Jarolim, P.; Freeman, G.J.; Sharpe, A.H.; Lichtman, A.H. Impairment of the programmed cell death-1 pathway increases atherosclerotic lesion development and inflammation. Arterioscler. Thromb. Vasc. Biol. 2011, 31, 1100–1107. [Google Scholar] [CrossRef] [PubMed]
- Lyon, A.R.; Yousaf, N.; Battisti, N.M.L.; Moslehi, J.; Larkin, J. Immune checkpoint inhibitors and cardiovascular toxicity. Lancet Oncol. 2018, 19, e447–e458. [Google Scholar] [CrossRef]
- Xia, W.; Zou, C.; Chen, H.; Xie, C.; Hou, M. Immune checkpoint inhibitor induces cardiac injury through polarizing macrophages via modulating microRNA-34a/Kruppel-like factor 4 signaling. Cell Death Dis. 2020, 11, 575. [Google Scholar] [CrossRef] [PubMed]
- Michel, L.; Rassaf, T.; Totzeck, M. Cardiotoxicity from immune checkpoint inhibitors. Int. J. Cardiol. Heart Vasc. 2019, 25, 100420. [Google Scholar] [CrossRef] [PubMed]
- Geisler, B.P.; Raad, R.A.; Esaian, D.; Sharon, E.; Schwartz, D.R. Apical ballooning and cardiomyopathy in a melanoma patient treated with ipilimumab: A case of takotsubo-like syndrome. J. Immunother. Cancer 2015, 3, 4. [Google Scholar] [CrossRef]
- Roth, M.E.; Muluneh, B.; Jensen, B.C.; Madamanchi, C.; Lee, C.B. Left Ventricular Dysfunction After Treatment With Ipilimumab for Metastatic Melanoma. Am. J. Ther. 2016, 23, e1925–e1928. [Google Scholar] [CrossRef]
- Voskens, C.J.; Goldinger, S.M.; Loquai, C.; Robert, C.; Kaehler, K.C.; Berking, C.; Bergmann, T.; Bockmeyer, C.L.; Eigentler, T.; Fluck, M.; et al. The price of tumor control: An analysis of rare side effects of anti-CTLA-4 therapy in metastatic melanoma from the ipilimumab network. PLoS ONE 2013, 8, e53745. [Google Scholar] [CrossRef]
- Yun, S.; Vincelette, N.D.; Mansour, I.; Hariri, D.; Motamed, S. Late onset ipilimumab-induced pericarditis and pericardial effusion: A rare but life threatening complication. Case Rep. Oncol. Med. 2015, 2015, 794842. [Google Scholar] [CrossRef]
- Laubli, H.; Balmelli, C.; Bossard, M.; Pfister, O.; Glatz, K.; Zippelius, A. Acute heart failure due to autoimmune myocarditis under pembrolizumab treatment for metastatic melanoma. J. Immunother. Cancer 2015, 3, 11. [Google Scholar] [CrossRef] [PubMed]
- Zimmer, L.; Goldinger, S.M.; Hofmann, L.; Loquai, C.; Ugurel, S.; Thomas, I.; Schmidgen, M.I.; Gutzmer, R.; Utikal, J.S.; Goppner, D.; et al. Neurological, respiratory, musculoskeletal, cardiac and ocular side-effects of anti-PD-1 therapy. Eur. J. Cancer 2016, 60, 210–225. [Google Scholar] [CrossRef] [PubMed]
- Heinzerling, L.; Ott, P.A.; Hodi, F.S.; Husain, A.N.; Tajmir-Riahi, A.; Tawbi, H.; Pauschinger, M.; Gajewski, T.F.; Lipson, E.J.; Luke, J.J. Cardiotoxicity associated with CTLA4 and PD1 blocking immunotherapy. J. Immunother. Cancer 2016, 4, 50. [Google Scholar] [CrossRef] [PubMed]
- Johnson, D.B.; Balko, J.M.; Compton, M.L.; Chalkias, S.; Gorham, J.; Xu, Y.; Hicks, M.; Puzanov, I.; Alexander, M.R.; Bloomer, T.L.; et al. Fulminant Myocarditis with Combination Immune Checkpoint Blockade. N. Engl. J. Med. 2016, 375, 1749–1755. [Google Scholar] [CrossRef]
- Barlesi, F.; Vansteenkiste, J.; Spigel, D.; Ishii, H.; Garassino, M.; de Marinis, F.; Ozguroglu, M.; Szczesna, A.; Polychronis, A.; Uslu, R.; et al. Avelumab versus docetaxel in patients with platinum-treated advanced non-small-cell lung cancer (JAVELIN Lung 200): An open-label, randomised, phase 3 study. Lancet Oncol. 2018, 19, 1468–1479. [Google Scholar] [CrossRef]
- Cham, J.; Ng, D.; Nicholson, L. Durvalumab-induced myocarditis, myositis, and myasthenia gravis: A case report. J. Med. Case Rep. 2021, 15, 278. [Google Scholar] [CrossRef]
- Hoyer, F.F.; Nahrendorf, M. Neutrophil contributions to ischaemic heart disease. Eur. Heart J. 2017, 38, 465–472. [Google Scholar] [CrossRef]
- Nahrendorf, M. Myeloid cell contributions to cardiovascular health and disease. Nat. Med. 2018, 24, 711–720. [Google Scholar] [CrossRef]
- King, K.R.; Aguirre, A.D.; Ye, Y.X.; Sun, Y.; Roh, J.D.; Ng, R.P., Jr.; Kohler, R.H.; Arlauckas, S.P.; Iwamoto, Y.; Savol, A.; et al. IRF3 and type I interferons fuel a fatal response to myocardial infarction. Nat. Med. 2017, 23, 1481–1487. [Google Scholar] [CrossRef]
- Finger, S.; Knorr, M.; Molitor, M.; Schuler, R.; Garlapati, V.; Waisman, A.; Brandt, M.; Munzel, T.; Bopp, T.; Kossmann, S.; et al. A sequential interferon gamma directed chemotactic cellular immune response determines survival and cardiac function post-myocardial infarction. Cardiovasc. Res. 2019, 115, 1907–1917. [Google Scholar] [CrossRef]
- Horckmans, M.; Ring, L.; Duchene, J.; Santovito, D.; Schloss, M.J.; Drechsler, M.; Weber, C.; Soehnlein, O.; Steffens, S. Neutrophils orchestrate post-myocardial infarction healing by polarizing macrophages towards a reparative phenotype. Eur. Heart J. 2017, 38, 187–197. [Google Scholar] [CrossRef] [PubMed]
- Hoyer, F.F.; Nahrendorf, M. Interferon-gamma regulates cardiac myeloid cells in myocardial infarction. Cardiovasc. Res. 2019, 115, 1815–1816. [Google Scholar] [CrossRef] [PubMed]
- Nikolaou, P.E.; Mylonas, N.; Makridakis, M.; Makrecka-Kuka, M.; Iliou, A.; Zerikiotis, S.; Efentakis, P.; Kampoukos, S.; Kostomitsopoulos, N.; Vilskersts, R.; et al. Cardioprotection by selective SGLT-2 inhibitors in a non-diabetic mouse model of myocardial ischemia/reperfusion injury: A class or a drug effect? Basic Res. Cardiol. 2022, 117, 27. [Google Scholar] [CrossRef] [PubMed]
- Gordon, J.W.; Shaw, J.A.; Kirshenbaum, L.A. Multiple facets of NF-kappaB in the heart: To be or not to NF-kappaB. Circ. Res. 2011, 108, 1122–1132. [Google Scholar] [CrossRef]
- Rathi, S.S.; Xu, Y.J.; Dhalla, N.S. Mechanism of cardioprotective action of TNF-alpha in the isolated rat heart. Exp. Clin. Cardiol. 2002, 7, 146–150. [Google Scholar]
- Rolski, F.; Blyszczuk, P. Complexity of TNF-alpha Signaling in Heart Disease. J. Clin. Med. 2020, 9, 3267. [Google Scholar] [CrossRef]
- Irwin, M.W.; Mak, S.; Mann, D.L.; Qu, R.; Penninger, J.M.; Yan, A.; Dawood, F.; Wen, W.H.; Shou, Z.; Liu, P. Tissue expression and immunolocalization of tumor necrosis factor-alpha in postinfarction dysfunctional myocardium. Circulation 1999, 99, 1492–1498. [Google Scholar] [CrossRef]
- Sato, T.; Suzuki, H.; Shibata, M.; Kusuyama, T.; Omori, Y.; Soda, T.; Shoji, M.; Iso, Y.; Koba, S.; Geshi, E.; et al. Tumor-necrosis-factor-alpha-gene-deficient mice have improved cardiac function through reduction of intercellular adhesion molecule-1 in myocardial infarction. Circ. J. 2006, 70, 1635–1642. [Google Scholar] [CrossRef]
- Kurrelmeyer, K.M.; Michael, L.H.; Baumgarten, G.; Taffet, G.E.; Peschon, J.J.; Sivasubramanian, N.; Entman, M.L.; Mann, D.L. Endogenous tumor necrosis factor protects the adult cardiac myocyte against ischemic-induced apoptosis in a murine model of acute myocardial infarction. Proc. Natl. Acad. Sci. USA 2000, 97, 5456–5461. [Google Scholar] [CrossRef]
- Maekawa, N.; Wada, H.; Kanda, T.; Niwa, T.; Yamada, Y.; Saito, K.; Fujiwara, H.; Sekikawa, K.; Seishima, M. Improved myocardial ischemia/reperfusion injury in mice lacking tumor necrosis factor-alpha. J. Am. Coll. Cardiol. 2002, 39, 1229–1235. [Google Scholar] [CrossRef]
- Gao, C.; Liu, Y.; Yu, Q.; Yang, Q.; Li, B.; Sun, L.; Yan, W.; Cai, X.; Gao, E.; Xiong, L.; et al. TNF-alpha antagonism ameliorates myocardial ischemia-reperfusion injury in mice by upregulating adiponectin. Am. J. Physiol. Heart Circ. Physiol. 2015, 308, H1583–H1591. [Google Scholar] [CrossRef] [PubMed]
- Berry, M.F.; Woo, Y.J.; Pirolli, T.J.; Bish, L.T.; Moise, M.A.; Burdick, J.W.; Morine, K.J.; Jayasankar, V.; Gardner, T.J.; Sweeney, H.L. Administration of a tumor necrosis factor inhibitor at the time of myocardial infarction attenuates subsequent ventricular remodeling. J. Heart Lung Transplant. 2004, 23, 1061–1068. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Guo, Z.; Ding, Z.; Mehta, J.L. Inflammation, Autophagy, and Apoptosis After Myocardial Infarction. J. Am. Heart Assoc. 2018, 7, e008024. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.; Xu, X.; Potter, B.J.; Wang, W.; Kuo, L.; Michael, L.; Bagby, G.J.; Chilian, W.M. TNF-alpha contributes to endothelial dysfunction in ischemia/reperfusion injury. Arterioscler. Thromb. Vasc. Biol. 2006, 26, 475–480. [Google Scholar] [CrossRef]
- Monden, Y.; Kubota, T.; Inoue, T.; Tsutsumi, T.; Kawano, S.; Ide, T.; Tsutsui, H.; Sunagawa, K. Tumor necrosis factor-alpha is toxic via receptor 1 and protective via receptor 2 in a murine model of myocardial infarction. Am. J. Physiol. Heart Circ. Physiol. 2007, 293, H743–H753. [Google Scholar] [CrossRef]
- Achim, A.; Liblik, K.; Gevaert, S. Immune checkpoint inhibitors—The revolutionary cancer immunotherapy comes with a cardiotoxic price. Trends Cardiovasc. Med. 2022. [Google Scholar] [CrossRef]
- Mahmood, S.S.; Fradley, M.G.; Cohen, J.V.; Nohria, A.; Reynolds, K.L.; Heinzerling, L.M.; Sullivan, R.J.; Damrongwatanasuk, R.; Chen, C.L.; Gupta, D.; et al. Myocarditis in Patients Treated With Immune Checkpoint Inhibitors. J. Am. Coll. Cardiol. 2018, 71, 1755–1764. [Google Scholar] [CrossRef]
- Hu, J.R.; Florido, R.; Lipson, E.J.; Naidoo, J.; Ardehali, R.; Tocchetti, C.G.; Lyon, A.R.; Padera, R.F.; Johnson, D.B.; Moslehi, J. Cardiovascular toxicities associated with immune checkpoint inhibitors. Cardiovasc. Res. 2019, 115, 854–868. [Google Scholar] [CrossRef]
- Pradhan, R.; Nautiyal, A.; Singh, S. Diagnosis of immune checkpoint inhibitor-associated myocarditis: A systematic review. Int. J. Cardiol. 2019, 296, 113–121. [Google Scholar] [CrossRef]
- Darvin, P.; Toor, S.M.; Sasidharan Nair, V.; Elkord, E. Immune checkpoint inhibitors: Recent progress and potential biomarkers. Exp. Mol. Med. 2018, 50, 1–11. [Google Scholar] [CrossRef]
- Postow, M.A.; Sidlow, R.; Hellmann, M.D. Immune-Related Adverse Events Associated with Immune Checkpoint Blockade. N. Engl. J. Med. 2018, 378, 158–168. [Google Scholar] [CrossRef] [PubMed]
- Sanmamed, M.F.; Chester, C.; Melero, I.; Kohrt, H. Defining the optimal murine models to investigate immune checkpoint blockers and their combination with other immunotherapies. Ann. Oncol. 2016, 27, 1190–1198. [Google Scholar] [CrossRef] [PubMed]
- Michel, L.; Rassaf, T.; Totzeck, M. Biomarkers for the detection of apparent and subclinical cancer therapy-related cardiotoxicity. J. Thorac. Dis. 2018, 10, S4282–S4295. [Google Scholar] [CrossRef] [PubMed]
- Lopez-Fernandez, T.; Lyon, A.R.; Herrmann, J. 2022 ESC Guidelines on cardio-oncology: How can we improve the cardiovascular health of patients with cancer and cancer survivors? Eur. Heart J. Cardiovasc. Pharmacother. 2022. [Google Scholar] [CrossRef]
- Teske, A.J. The ESC cardio-oncology 2022 guidelines; the ball is in our court. Eur. Heart J. Cardiovasc. Imaging 2022. [Google Scholar] [CrossRef]
- Ahmed, T.; Marmagkiolis, K.; Ploch, M.; Irizarry-Caro, J.A.; Amatullah, A.; Desai, S.; Aziz, M.K.; Yarrabothula, A.; Fossas-Espinosa, J.; Koutroumpakis, E.; et al. The Year in Cardio-oncology 2022. Curr. Probl. Cardiol. 2022, 48, 101435. [Google Scholar] [CrossRef]
- Chapman, P.B.; Hauschild, A.; Robert, C.; Haanen, J.B.; Ascierto, P.; Larkin, J.; Dummer, R.; Garbe, C.; Testori, A.; Maio, M.; et al. Improved survival with vemurafenib in melanoma with BRAF V600E mutation. N. Engl. J. Med. 2011, 364, 2507–2516. [Google Scholar] [CrossRef]
- Solit, D.B.; Rosen, N. Resistance to BRAF inhibition in melanomas. N. Engl. J. Med. 2011, 364, 772–774. [Google Scholar] [CrossRef]
- Corcoran, R.B.; Andre, T.; Atreya, C.E.; Schellens, J.H.M.; Yoshino, T.; Bendell, J.C.; Hollebecque, A.; McRee, A.J.; Siena, S.; Middleton, G.; et al. Combined BRAF, EGFR, and MEK Inhibition in Patients with BRAF(V600E)-Mutant Colorectal Cancer. Cancer Discov. 2018, 8, 428–443. [Google Scholar] [CrossRef]
- Planchard, D.; Besse, B.; Groen, H.J.M.; Souquet, P.J.; Quoix, E.; Baik, C.S.; Barlesi, F.; Kim, T.M.; Mazieres, J.; Novello, S.; et al. Dabrafenib plus trametinib in patients with previously treated BRAF(V600E)-mutant metastatic non-small cell lung cancer: An open-label, multicentre phase 2 trial. Lancet Oncol. 2016, 17, 984–993. [Google Scholar] [CrossRef]
- Glen, C.; Tan, Y.Y.; Waterston, A.; Evans, T.R.J.; Jones, R.J.; Petrie, M.C.; Lang, N.N. Mechanistic and Clinical Overview Cardiovascular Toxicity of BRAF and MEK Inhibitors: JACC: CardioOncology State-of-the-Art Review. JACC CardioOncol. 2022, 4, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Mincu, R.I.; Mahabadi, A.A.; Michel, L.; Mrotzek, S.M.; Schadendorf, D.; Rassaf, T.; Totzeck, M. Cardiovascular Adverse Events Associated with BRAF and MEK Inhibitors: A Systematic Review and Meta-analysis. JAMA Netw. Open 2019, 2, e198890. [Google Scholar] [CrossRef] [PubMed]
- Lips, D.J.; Bueno, O.F.; Wilkins, B.J.; Purcell, N.H.; Kaiser, R.A.; Lorenz, J.N.; Voisin, L.; Saba-El-Leil, M.K.; Meloche, S.; Pouyssegur, J.; et al. MEK1-ERK2 signaling pathway protects myocardium from ischemic injury in vivo. Circulation 2004, 109, 1938–1941. [Google Scholar] [CrossRef] [PubMed]
- Zullig, L.L.; Sung, A.D.; Khouri, M.G.; Jazowski, S.; Shah, N.P.; Sitlinger, A.; Blalock, D.V.; Whitney, C.; Kikuchi, R.; Bosworth, H.B.; et al. Cardiometabolic Comorbidities in Cancer Survivors: JACC: CardioOncology State-of-the-Art Review. JACC CardioOncol. 2022, 4, 149–165. [Google Scholar] [CrossRef]
- Tsao, C.W.; Aday, A.W.; Almarzooq, Z.I.; Alonso, A.; Beaton, A.Z.; Bittencourt, M.S.; Boehme, A.K.; Buxton, A.E.; Carson, A.P.; Commodore-Mensah, Y.; et al. Heart Disease and Stroke Statistics-2022 Update: A Report From the American Heart Association. Circulation 2022, 145, e153–e639. [Google Scholar] [CrossRef]
- Buford, T.W. Hypertension and aging. Ageing Res. Rev. 2016, 26, 96–111. [Google Scholar] [CrossRef]
- Whelton, P.K.; Carey, R.M.; Aronow, W.S.; Casey, D.E., Jr.; Collins, K.J.; Dennison Himmelfarb, C.; DePalma, S.M.; Gidding, S.; Jamerson, K.A.; Jones, D.W.; et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2018, 138, e426–e483. [Google Scholar] [CrossRef]
- Murai, T. Cholesterol lowering: Role in cancer prevention and treatment. Biol. Chem. 2015, 396, 1–11. [Google Scholar] [CrossRef]
- Ding, X.; Zhang, W.; Li, S.; Yang, H. The role of cholesterol metabolism in cancer. Am. J. Cancer Res. 2019, 9, 219–227. [Google Scholar]
- Grundy, S.M.; Stone, N.J.; Bailey, A.L.; Beam, C.; Birtcher, K.K.; Blumenthal, R.S.; Braun, L.T.; de Ferranti, S.; Faiella-Tommasino, J.; Forman, D.E.; et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 2019, 73, e285–e350. [Google Scholar] [CrossRef]
- Ederer, F.; Leren, P.; Turpeinen, O.; Frantz, I. Cancer among men on cholesterol-lowering diets: Experience from Five Clinical Trials. Lancet 1971, 298, 203–206. [Google Scholar] [CrossRef]
- Dale, K.M.; Coleman, C.I.; Henyan, N.N.; Kluger, J.; White, C.M. Statins and cancer risk: A meta-analysis. JAMA 2006, 295, 74–80. [Google Scholar] [CrossRef] [PubMed]
- Rosch, P.J.; McCully, K. Statin use and reduced cancer-related mortality. N. Engl. J. Med. 2013, 368, 576. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control Prevention. National Diabetes Statistics Report; Centers for Disease Control Prevention, U.S. Dept of Health and Human Services: Atlanta, GA, USA, 2020. [Google Scholar]
- Edgington, A.; Morgan, M.A. Looking beyond recurrence: Comorbidities in cancer survivors. Clin. J. Oncol. Nurs. 2011, 15, E3–E12. [Google Scholar] [CrossRef]
- Weaver, K.E.; Foraker, R.E.; Alfano, C.M.; Rowland, J.H.; Arora, N.K.; Bellizzi, K.M.; Hamilton, A.S.; Oakley-Girvan, I.; Keel, G.; Aziz, N.M. Cardiovascular risk factors among long-term survivors of breast, prostate, colorectal, and gynecologic cancers: A gap in survivorship care? J. Cancer Surviv. 2013, 7, 253–261. [Google Scholar] [CrossRef]
- Arreskov, A.B.; Olsen, M.A.; Pouplier, S.S.; Siersma, V.; Andersen, C.L.; Friis, S.; de Fine Olivarius, N. The impact of cancer on diabetes outcomes. BMC Endocr. Disord. 2019, 19, 60. [Google Scholar] [CrossRef]
- Barone, B.B.; Yeh, H.C.; Snyder, C.F.; Peairs, K.S.; Stein, K.B.; Derr, R.L.; Wolff, A.C.; Brancati, F.L. Long-term all-cause mortality in cancer patients with preexisting diabetes mellitus: A systematic review and meta-analysis. JAMA 2008, 300, 2754–2764. [Google Scholar] [CrossRef]
- van Spronsen, D.J.; Janssen-Heijnen, M.L.; Breed, W.P.; Coebergh, J.W. Prevalence of co-morbidity and its relationship to treatment among unselected patients with Hodgkin’s disease and non-Hodgkin’s lymphoma, 1993–1996. Ann. Hematol. 1999, 78, 315–319. [Google Scholar] [CrossRef]
- Barroso-Sousa, R.; Barry, W.T.; Garrido-Castro, A.C.; Hodi, F.S.; Min, L.; Krop, I.E.; Tolaney, S.M. Incidence of endocrine dysfunction following the use of different immune checkpoint inhibitor regimens: A systematic review and meta-analysis. JAMA Oncol. 2018, 4, 173–182. [Google Scholar] [CrossRef]
- Norwood Toro, L.E.; Hader, S.N.; Didier, D.; McIntosh, J.J.; Freed, J.K.; Kong, A.; Beyer, A.M. Effects of Anti-Cancer Therapy on Human Microvascular Function—A Longitudinal Study. FASEB J. 2020, 34, 1. [Google Scholar] [CrossRef]
- Galan-Arriola, C.; Vilchez-Tschischke, J.P.; Lobo, M.; Lopez, G.J.; de Molina-Iracheta, A.; Perez-Martinez, C.; Villena-Gutierrez, R.; Macias, A.; Diaz-Rengifo, I.A.; Oliver, E.; et al. Coronary microcirculation damage in anthracycline cardiotoxicity. Cardiovasc. Res. 2022, 118, 531–541. [Google Scholar] [CrossRef] [PubMed]
- Strain, W.D.; Paldanius, P.M. Diabetes, cardiovascular disease and the microcirculation. Cardiovasc. Diabetol. 2018, 17, 57, Erratum in Cardiovasc. Diabetol. 2021, 20, 120. [Google Scholar] [CrossRef] [PubMed]
- Zaha, V.G.; Hayek, S.S.; Alexander, K.M.; Beckie, T.M.; Hundley, W.G.; Kondapalli, L.; Ky, B.; Leger, K.J.; Meijers, W.C.; Moslehi, J.J.; et al. Future Perspectives of Cardiovascular Biomarker Utilization in Cancer Survivors: A Scientific Statement From the American Heart Association. Circulation 2021, 144, e551–e563. [Google Scholar] [CrossRef] [PubMed]

| Drug Name | First Approval | Mechanism of Action | Clinical Use | Cardiovascular Adverse Events and Toxicity | Reference |
|---|---|---|---|---|---|
| Bevacizumab | 2004 | Monoclonal antibody that binds and inhibits VEGF | Metastatic colorectal cancer; breast cancer; non-small cell lung cancer; renal cell carcinoma; cancer of the ovary and the cervix | Arterial hypertension; bleeding; arterial thromboembolism | [68] |
| Sorafenib | 2005 | Multikinase inhibitor of CRAF (RAF proto-oncogene serine/threonine-protein kinase, also known as proto-oncogene c-RAF), VEGFR-2, VEGFR-3 and PDGFR-β expressed in tumor vasculature | Hepatocellular carcinoma; advanced renal cell carcinoma; differentiated thyroid carcinoma | Myocardial infarction or ischemia; bleeding; arterial hypertension; hypertensive crisis | [69] |
| Pazopanib | 2009 | Small molecule tyrosine kinase inhibitor of VEGF, PDGF and KIT receptors | Advanced renal cell carcinoma | Arterial hypertension | [70] |
| Vandetanib | 2011 | Small molecule tyrosine kinase inhibitor of VEGF, EGF and glial cell-line derived neurotrophic factor (RET) receptors | Medullary thyroid cancer | Arterial hypertension; pro-arrhythmic effects (QTc interval prolongation) | [71] |
| Axitinib | 2012 | Small molecule tyrosine kinase inhibitor of VEGF receptors | Advanced renal cell carcinoma | Arterial hypertension; bleeding; congestive heart failure/cardiomyopathy | [72] |
| Nintedanib | 2014 | Small molecule tyrosine kinase inhibitor of VEGF, FGF and PDGF receptors | Non-small cell lung adenocarcinoma | Venous thromboembolism; bleeding; arterial hypertension | [73] |
| Lenvatinib | 2015 | Small molecule tyrosine kinase inhibitor of VEGF, fibroblast growth factor receptor (FGFR), platelet-derived growth factor receptor (PDGFR), stem cell factor receptor (KIT) and glial cell-line derived neurotrophic factor (RET) receptors | Advanced renal cell carcinoma; differentiated thyroid carcinoma | Arterial hypertension; peripheral oedema (swelling, especially of the ankles and feet); heart failure | [74] |
| Cabozantinib | 2017 | Small molecule tyrosine kinase inhibitor of VEGF receptor, MET, MET receptor tyrosine kinase (RTK) and its ligand hepatocyte growth factor (HGF) | Medullary thyroid cancer | Arterial hypertension; venous thrombosis; bleeding; pulmonary embolism | [75] |
| Sunitinib | 2017 | Small molecule tyrosine kinase inhibitor of platelet-derived growth factor receptors (PDGFRα and PDGFRβ), VEGF receptors (VEGFR1, VEGFR2, and VEGFR3), stem cell factor receptor (KIT), Fms-like tyrosine kinase-3 (FLT3), colony-stimulating factor receptor (CSF-1R) and the glial cell-line derived neurotrophic factor receptor (RET) | Gastrointestinal stromal tumor; metastatic renal cell carcinoma; pancreatic neuroendocrine tumors | Arterial hypertension; thrombocytopenia; anemia; leucopenia; heart and kidney failure; venous thrombosis; pulmonary embolism; pericardial events; myocardial infarction | [76] |
| Tivozanib | 2017 | Small molecule tyrosine kinase inhibitor of VEGF-ligand-induced phosphorylation of all VEGF receptors 1, 2, and 3 | Advanced renal cell carcinoma | Arterial hypertension (in 50% of the patients) | [77] |
| Ponatinib | 2020 | Small molecule tyrosine kinase inhibitor of Bcr-Abl | Chronic myeloid leukemia and acute lymphoblastic leukemia | Myocardial injury; myocardial infarction; atrial fibrillation; peripheral arterial occlusive disease; anemia; angina pectoris; decreased platelet counts; arterial hypertension; coronary artery disease; heart failure; venous thromboembolism | [78] |
| Ramucirumab | 2020 | Monoclonal antibody to VEGF receptor 2 (VEGFR2) | Gastric cancer; metastatic colorectal cancer; non-small cell lung cancer with mutated EGFR; hepatocellular carcinoma | Peripheral edema; arterial hypertension; thrombocytopenia; arterial thromboembolic events | [79] |
| Myocardial I/R Model | I/R Protocol | Effects on Proteasome Function | Reference |
|---|---|---|---|
| Rat | 30 min of ischemia/60 min reperfusion | Increased ubiquitinated proteins; decreased 20S proteasome activity; oxidative modification of 20S subcomplex | [117] |
| Langendorff perfused Isolated Rat heart | 30 min of ischemia/60 min reperfusion | Increased ubiquitinated proteins; decreased 20S/26S proteasome activities | [118] |
| Rat | 30 min of ischemia/60, 120, 240 min reperfusion | Selective inhibition of proteasome activity | [119] |
| Canine | 90 min of ischemia/360 min reperfusion | Increased ubiquitinated proteins; decreased 26S proteasome activities | [120] |
| Rat | Permanent LAD ligation followed by six weeks period | Increased ubiquitinated proteins; increased E3 ligase (MuRF-1/MAFbx) | [121] |
| Mouse | Aortic banding followed by three weeks period | Increased proteasome activity; increased 11S/19S/20S sub-complexes | [122] |
| Drug Name | First Approval | Mechanism of Action | Clinical Use | Cardiovascular Adverse Events and Toxicity and Effect on Myocardial I/R | Reference |
|---|---|---|---|---|---|
| Bortezomib | 2003 | Reversible β5, β1 subunits inhibitor | Antibody-mediated rejection in cardiac transplantation, Multiple myeloma, T cell and follicular lymphomas, systemic light-chain amyloidosis, Relapsed/Refractory Waldenstrom macroglobulinemia | Administration prior to or after ischemia in a canine in vivo model of myocardial infarction prevented ischemic loss of GRK2 and ventricular tachyarrhythmias | [104,161] |
| Carfilzomib | 2012 | Irreversible β5 subunit inhibitor | Relapsed/Refractory Multiple Myeloma | Acute cardiotoxicity, acute coronary syndrome, hypertension, pulmonary hypertension | [171] |
| Ixazomib | 2015 | Reversible β5 subunit inhibitor | Multiple Myeloma (oral proteasome inhibitor) | Heart failure, hypertension, ischemia and arrhythmia | [172] |
| Marizomib | Pending | Irreversible β5, β2 subunits inhibitor | Not applicable | Not applicable | [173] |
| Oprozomib | Pending | Irreversible β5 subunit inhibitor | Not applicable | Hypotension | [173] |
| Epoxomicin | Not approved | Not applicable | Not applicable | Administration prior to ischemia in a canine in vivo model of myocardial infarction led to no change in IS | [120] |
| Administration 2 weeks postischemia in a mouse in vivo model of myocardial infarction decreased cardiac remodeling and improved LV function | [122] | ||||
| Lactacystin | Not approved | Not applicable | Not applicable | Administration prior to ischemia in a rat ex vivo model of myocardial infarction exerted no effect on postischemic hemodynamic recovery, whereas protein carbonylation is increased | [149] |
| MG132 | Not approved | Not applicable | Not applicable | Administration prior to ischemia in a rat ex vivo model of myocardial infarction impaired postischemic recovery of hemodynamic function | [118] |
| PR-39 | Not approved | Not applicable | Not applicable | Administration 7 days postischemia in a mouse in vivo model of myocardial infarction increased vascular density in infarct border zone | [110] |
| Administration 7 days postischemia in a mouse in vivo model of myocardial infarction reduced IS | [165] | ||||
| Administration prior to ischemia in a mouse in vivo model of myocardial infarction decreased leucocyte recruitment and IS | [164] | ||||
| Administration at reperfusion in a rat in vivo model of myocardial infarction decreased neutrophils recruitment and IS and improved LV function | [132] | ||||
| PS-519 | Not approved | Not applicable | Administration prior to ischemia in a mouse in vivo model of myocardial infarction decreased myocardial inflammation and IS and improved LV function | [163] | |
| Administration prior to reperfusion in a mouse in vivo model of myocardial infarction decreased IS and improved LV function | [137] | ||||
| Administration prior to reperfusion in a porcine in vivo model of myocardial infarction decreased IS and improved LV function and inhibited NF-κB activation | [162] | ||||
| Administration during I/R in a rat ex vivo model of myocardial infarction improved cardiac function and abrogated IC infiltration | [130] | ||||
| Drug Name | First Approval | Mechanism of Action | Clinical Use | Cardiovascular Adverse Events and Toxicity | Reference |
|---|---|---|---|---|---|
| Ipilimumab | 2011 | anti-CTLA-4 IgG1κ moAb | Unresectable or metastatic melanoma in adult and juvenile patients; melanoma stage III after complete resection as adjuvant therapy. | Myocarditis, paroxysmal atrial fibrillation, left BBB, left ventricular dysfunction, ischemia, pericarditis, pericardial effusion, subacute “Takotsubo-like” cardiomyopathy, transient supraventricular/ventricular tachycardia | [187,188,189,190] |
| Pembrolizumab | 2014 (September) | anti-PD-1 IgG1κ moAb | Unresectable or metastatic melanoma; metastatic NSCLC; recurrent or metastatic HNSCC with progression; relapsed classical Hodgkin lymphoma; advanced or metastatic urothelial carcinoma; microsatellite instability-high or mismatch repair deficient tumors; recurrent local or metastatic gastric cancer; recurrent or metastatic cervical cancer. | Acute heart failure, myocarditis (in combination with Nivolumab), stable angina, sinus tachycardia, ventricular arrhythmia, asystole, hypertension, atrial flutter, myocarditis, cardiomyopathy, LV systolic dysfunction | [191,192] |
| Nivolumab | 2014 (December) | anti-PD-1 IgG1κ moAb | Unresectable or metastatic melanoma as monotherapy or in combination with ipilimumab; melanoma stage III-IV; metastatic NSCLC refractory to platins; renal cell carcinoma as monotherapy or in combination with ipilimumab; relapsed classical Hodgkin lymphoma after HSCT; recurrent or metastatic HNSCC; microsatellite instability-high or mismatch repair deficient metastatic colorectal cancer. | Myocarditis (in combination with Pembrolizumab), stable angina, sinus tachycardia, ventricular arrhythmia, asystole, hypertension, atrial flutter, myocarditis, cardiomyopathy, LV systolic dysfunction (in combination with Ipilimumab) Myocarditis, myositis, intraventricular conduction delay, complete heart block, refractory ventricular tachycardia | [192,193,194] |
| Avelumab | 2017 (March) | anti-PD-L1 IgG1κ moAb | Metastatic Merkel cell carcinoma; advanced or metastatic urothelial carcinoma. | Autoimmune myocarditis, acute cardiac failure (rare) | [195] |
| Durvalumab | 2017 (May) | anti-PD-L1 IgG1κ moAb | Advanced or metastatic urothelial carcinoma; NSCLC stage III with stable disease or remission. | Autoimmune myocarditis | [196] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Efentakis, P.; Andreadou, I.; Iliodromitis, K.E.; Triposkiadis, F.; Ferdinandy, P.; Schulz, R.; Iliodromitis, E.K. Myocardial Protection and Current Cancer Therapy: Two Opposite Targets with Inevitable Cost. Int. J. Mol. Sci. 2022, 23, 14121. https://doi.org/10.3390/ijms232214121
Efentakis P, Andreadou I, Iliodromitis KE, Triposkiadis F, Ferdinandy P, Schulz R, Iliodromitis EK. Myocardial Protection and Current Cancer Therapy: Two Opposite Targets with Inevitable Cost. International Journal of Molecular Sciences. 2022; 23(22):14121. https://doi.org/10.3390/ijms232214121
Chicago/Turabian StyleEfentakis, Panagiotis, Ioanna Andreadou, Konstantinos E. Iliodromitis, Filippos Triposkiadis, Péter Ferdinandy, Rainer Schulz, and Efstathios K. Iliodromitis. 2022. "Myocardial Protection and Current Cancer Therapy: Two Opposite Targets with Inevitable Cost" International Journal of Molecular Sciences 23, no. 22: 14121. https://doi.org/10.3390/ijms232214121
APA StyleEfentakis, P., Andreadou, I., Iliodromitis, K. E., Triposkiadis, F., Ferdinandy, P., Schulz, R., & Iliodromitis, E. K. (2022). Myocardial Protection and Current Cancer Therapy: Two Opposite Targets with Inevitable Cost. International Journal of Molecular Sciences, 23(22), 14121. https://doi.org/10.3390/ijms232214121







