Abstract
Signal peptide (SP) mutations are an infrequent cause of inherited retinal diseases (IRDs). We report the genes currently associated with an IRD that possess an SP sequence and assess the prevalence of these variants in a multi-institutional retrospective review of clinical genetic testing records. The online databases, RetNet and UniProt, were used to determine which IRD genes possess a SP. A multicenter retrospective review was performed to retrieve cases of patients with a confirmed diagnosis of an IRD and a concurrent SP variant. In silico evaluations were performed with MutPred, MutationTaster, and the signal peptide prediction tool, SignalP 6.0. SignalP 6.0 was further used to determine the locations of the three SP regions in each gene: the N-terminal region, hydrophobic core, and C-terminal region. Fifty-six (56) genes currently associated with an IRD possess a SP sequence. Based on the records review, a total of 505 variants were present in the 56 SP-possessing genes. Six (1.18%) of these variants were within the SP sequence and likely associated with the patients’ disease based on in silico predictions and clinical correlation. These six SP variants were in the CRB1 (early-onset retinal dystrophy), NDP (familial exudative vitreoretinopathy) (FEVR), FZD4 (FEVR), EYS (retinitis pigmentosa), and RS1 (X-linked juvenile retinoschisis) genes. It is important to be aware of SP mutations as an exceedingly rare cause of IRDs. Future studies will help refine our understanding of their role in each disease process and assess therapeutic approaches.
1. Introduction
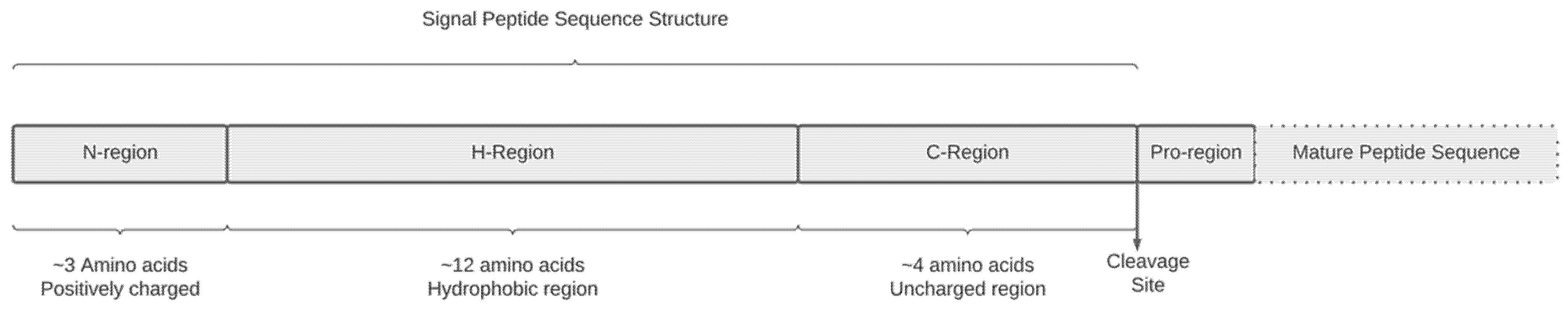
Signal peptides (SP) are N-terminal extensions of newly synthesized polypeptide chains whose primary function is to target secretory or membrane-bound proteins to and across the endoplasmic reticulum (ER) membrane [1]. Roughly 18% of human proteins in the UniProt (Universal Protein Service) database contain an SP sequence [2]. Characteristically, SP sequences consist of 16 to 30 amino acids (AA) grouped into three chemically well-defined regions: a hydrophilic N-region, a hydrophobic core, and a polar C-region (Figure 1) [1,3]. Each one fulfills an essential role in preprotein processing, including initial interaction with the ER membrane receptors, SP cleavage, and exit from the ER membrane to the cell membrane. SP sequences also contain a cleavage site where the SP is removed from the mature protein once processing is complete. Mutations in the SP sequence can alter the biochemical properties of SPs and result in defects in the co-translational processing of newly synthesized proteins. SP mutations have been found in association with human diseases. In a systematic review, Jarjanzani, et al. identified 26 SP sequence mutations in 21 different genes associated with various human genetic disorders [3].
Figure 1.
Characteristic SP sequence structure. Classically, the positively charged N-terminal region is composed of 1–5 residues, the hydrophobic core of 7–15 residues, and the uncharged C-region, which contains 3–7 residues. The cleavage site borders the C-region and the pro region.
Inherited retinal dystrophies (IRDs) comprise a heterogenic group of genetically inherited disorders that result in progressive retinal degeneration leading to partial or complete vision loss [4]. The estimated prevalence of IRDs is approximately 1 in 2000 individuals, affecting more than two million individuals worldwide [5]. They commonly display significant variability in genotype, phenotype, and mode of inheritance [4]. The prevalence of SP signal mutations in IRDs is likely very small as there are only a few descriptions of IRD-associated SP mutations in the scientific literature. In one study, Hiroaka, et al. identified a heterozygous 3-bp insertion in the CTG repeat region of exon 1 of the LRP5 gene in a patient with advanced retinopathy of prematurity (ROP) [6]. Vijayasarathy, et al. analyzed the biochemical consequences of several RS1 SP variants caused by missense mutations in four different subjects with X-linked juvenile retinoschisis (XLRS), and concluded that the mutations affected protein biosynthesis, and resulted in a null RS1 phenotype [7].
In this study, we herein identify which genes currently implicated in IRDs contain an SP sequence. We then perform a multi-institutional review of genetic testing results to investigate the occurrence of SP variants. We also describe a series of patients with an IRD in whom genetic testing revealed at least one SP sequence variant that was likely contributing to their disease.
2. Results
Fifty-six (21%) of the 271 genes currently implicated in IRDs on RetNet possessed an SP sequence (Supplementary Table S1). A total of 505 variants were present in the 56 SP-possessing genes, of which six (1.19%) were located within the SP coding sequence and considered disease causing based on our criteria. The SP sequences of the CRB1 (early-onset retinal dystrophy), NDP (familial exudative vitreoretinopathy) (FEVR), FZD4 (FEVR), EYS (RP), and RS1 (XLRS) genes were affected. Based on SignalP 6.0, one mutation was located within the N-terminal region, three within the hydrophobic core, and two affecting the C-terminal region. Clinical summaries of these six patients are provided in Appendix A. The variants, affected genes, and related IRDs are shown in Table 1.

Table 1.
Disease-causing SP Variants in Our Patient Population.
The SignalP 6.0 likelihood score, MutationTaster, MutPred, and in silico pathogenicity prediction scores are shown in Table 1. MutationTaster and MutPred classified all six variants as deleterious or pathogenic, respectively. The two exceptions were the EYS variant, which could not be evaluated by MutPred because the resulting peptide sequence was shorter than the required 30 residues, and the RS1 c.52+1 variant, as MutPred cannot evaluate intronic mutations. All six variants had a population frequency of <0.01% in the GnomAD database.
The three frameshift mutations in EYS, FZD4, and RS1 resulted in a SignalP 6.0 likelihood score of 0, reduced from 0.998 in the respective WT sequence. The 21-basepair deletion in the H-region of the NDP gene SP sequence also reduced the predicted SP likelihood from 0.991 to zero. The CRB1 SP variant was not evaluated by SignalP due to the program not being able to readily assess the effects of start codon mutations. The RS1 c. 52+1 G>C splice site mutation, although classified as deleterious by MutationTaster, did not cause a change in SP likelihood, as it did not result in a peptide sequence change, and the program may not be able to assess the effects of splice site mutations. Cleavage site prediction was lost in all four of the evaluated variants. The EYS p.W32L mutation in the non-SP allele obtained a pathogenic score from one predictor, and a likely harmless from the second predictor, while the CRB1 p.R686C non-SP variant did not achieve disease causing scores from neither predictor.
3. Discussion
Signal peptide mutations are an exceedingly uncommon cause of IRDs. There is a paucity of reports of IRDs caused by SP variants. In this study, we identified the 56 genes associated with IRDs that possess an SP sequence and presented six cases of patients with an SP variant implicated in their disease. The unfavorable effects of SP variants depend on the affected region, and the resulting effects on the processing of proteins destined for the secretory pathway.
The N-region is responsible for the initial interaction with the signal recognition particle (SRP) in the ER membrane and plays a role in SP orientation, favoring or preventing translocation across membranes [12]. Positively charged residues, such as lysine and arginine, give this region its characteristically hydrophilic and ionic properties [13]. Missense mutations in these highly conserved positively charged residues can significantly impair the targeting/translocation process to varying degrees due to dysfunctional recognition of the SP sequence by ER membrane receptors [14]. It has also been reported that when the SRP fails to interact with an anomalous SP sequence, the mutated protein is targeted for degradation via activation of the ribosome-associated protein quality control (RAPP) pathway [15,16]. In our study, two compound heterozygous missense mutations in the CRB1 gene, p.Met1* and p.Arg686Cys, were present in a patient with early-onset retinal dystrophy (EORD). The p.Arg686Cys variant has been previously reported in a compound heterozygous patient with RP [17]. The c.2T>C p.Met1* variant has been previously reported in a Japanese patient with LCA and results in a substitution of the initial methionine residue for threonine [8]. In most cases, mutations affecting the start codon (AUG) are deleterious and result in a null allele [15]. However, translation can rarely initiate in alternate start codons such as those that code for leucine (CUG), although studies show they typically perform at a markedly reduced efficiency compared to AUG codons [16]. In rare cases, downstream AUG codons can also be used for translation initiation. However, this can result in the SP possessing protein accumulating intracellularly, which has been reported as disease causing [18]. A similar RS1 p.Met1Leu mutation was reported in a patient with XLRS. Cells transfected with mutant cDNA failed to express a mutated RS1 protein due to a blocked translation initiation at the mutant start codon [7]. Although the mutation affects the SP, the role of this variant in our patient’s disease is likely secondary to a near-complete loss of protein production from the affected allele, rather than a loss of SP function alone.
The hydrophobic region is integral to proper SP function as it is involved in conformation and orientation toward the cell membrane, SP cleavage, rate and efficiency of protein translocation, secretion pathway function, and protein processing [19]. We present a 21 base pair deletion in the NDP gene, which removed seven amino acids within the hydrophobic core of the SP in a patient with FEVR. SignalP 6.0 likelihood and cleavage site prediction scores for this variant decreased to 0. A similar 18-base-pair deletion eliminating six leucine residues within the LRP5 SP hydrophobic core was reported in a patient with Osteoporosis-Pseudoglioma Syndrome (OPPG) [20]. Functional assays suggested that the mutant LRP5 polypeptide had impaired ER entry and post-translational processing [20]. Mutations that cause changes in SP hydrophobicity have been shown to reduce protein expression up to 70–90% due to defective targeting to the endoplasmic reticulum, and failed protein translocation [21,22,23]. H-region mutations have also been reported in association with IRDs. Vijasajarthy, et al. evaluated two RS1 mutations, p.Leu12His and p.Leu13Pro, found in two patients with XLRS in vitro. Both histidine and proline have hydrophilic properties, which may disrupt the hydrophobic properties of the SP’s hydrophobic core [24]. In their study, the level of RS1 protein was nondetectable in the cellular and secreted fractions [7]. However, the study also found that a mutation exchanging one hydrophobic residue for another did not impair SP function. A cell line transfected with an RS1 p.Leu13Phe plasmid expressed the same RS1 levels in the culture medium as WT cells [7]. We can postulate that our patient’s disease process involved similar mechanisms of impaired protein ER entry and post-translational processing due to loss of the hydrophobic core region. We also describe two EYS p.Met12Aspfs*14 and FZD4 p.Pro8Argfs*53 frameshift variants found in patients with RP and FEVR, respectively. Although the SP function is likely completely lost, which is supported by the complete loss of SP likelihood prediction in both cases, the entire peptide sequence of the protein is likely affected. Thus, it is more likely that the deleterious effects of the mutation are primarily due to the frameshift mutation. Furthermore, the SP mutations result in truncated EYS and FZD4 proteins, which can also be targeted for rapid degradation by the nonsense-mediated decay (NMD) pathway [25].
Additionally, we found two mutations in the RS1 gene located within the 5′ donor splice site of intron 1, affecting the SP’s hydrophobic core and C-terminal region. The c.53-859_78+276 variant in case three results in the deletion of exon 2, which contains the AA for the C-terminal region of the SP, leading to a frameshift mutation with a premature stop codon at position 108 (submitted elsewhere as a case report). There was a complete loss of SP likelihood in this variant. As in the EYS and FZD4 mutants, the truncated protein may also undergo degradation via the NMD pathway. RS1 frameshift mutations that result in truncated proteins have been reported in multiple patients with XLRS [7]. In case five, RS1 c.52+1 G>C was predicted to be deleterious by one of the in silico predictors. The SignalP 6.0 likelihood score of this variant was unaffected, as the program evaluates the biochemical properties of the entered amino acid sequences, which does not reflect the possible effects of intronic splice site mutations. A similar mutation, c.52+1 G>A, was identified in a Chinese family with XLRS [7]. In vitro analysis of this variant showed an absolute lack of RS1 protein in transfected cells. This mutation resulted in skipping exon 2, leading to a frameshift at the resulting exon 1 and exon 3 junction and a premature stop codon [7], which may similarly occur in our patient. Deletion of exon 2 removes the C-terminal region, which is responsible for the final cleavage of the SP sequence from the mature protein. Small nonpolar amino acids at positions −1 and −3 from the cleavage site conferred this region an extended beta conformation that provided the peptidase binding site [4,23]. Loss or substitutions of these amino acids are thought to cause failed recognition or cleavage by the signal peptidase. This lead to mutant chains remaining anchored to the microsomal membranes, with eventual removal from the ER by retrograde translocation and degradation, through the endoplasmic-reticulum-associated protein degradation (ERAD) and proteasome pathways [26]. Accumulation of unfolded proteins in the ER can also lead to activation of the unfolded protein response (UPR), which in the presence of continued ER stress can shift from a protective to a proapoptotic pathway, thus causing disease [27,28]. The role of ER stress in IRDs has also been previously established [29,30].
Currently, there are no therapeutic approaches designed specifically for SP sequence mutations. One proposed mechanism is the use of chemical chaperones, which are molecules that bind to the active site of the mutant protein and stabilize or destabilize the folding transition state to compensate for the mutation [31]. In vitro studies have shown that chemical chaperones could potentially correct the abnormal intracellular accumulation of proteins caused by SP mutations, as evidenced by improved clearance of intracellularly trapped hormones, alleviation of ER stress, and reduced cell death [31]. In vitro studies evaluating this approach have shown promising results in diseases such as RP and Fabry disease [26,32,33]. In the absence of a dominant-negative effect caused by an SP variant, where the mutant protein interacts with the WT inside the ER and prevents proper folding and translocation, a gene augmentation approach in which the WT gene is introduced into the cell, or gene editing, could also confer a therapeutic benefit [7].
There are some limitations to our study. Functional in vitro studies were not performed, and the study is retrospective in nature. Therefore, protein processing, secretion, and function could not be assessed. These tests will be helpful in future studies to elucidate the disease mechanisms. Additionally, genetic testing technology has drastically improved over the past decade [34]. Consequently, the development of genomic databases and other resources that are publicly accessible revolutionized our ability to interpret genetic testing data. Therefore, signal peptide mutations may not have been identified in individuals who received testing several years ago due to limitations in technology and reporting. Regarding Signal 6.0, it does not provide a cut-off score for its SP likelihood prediction, which could be helpful in the future in cases where there is a milder loss of likelihood probability. Although SignalP 6.0 can be a useful tool to evaluate SP variants, it may not be able to assess certain types of mutations such as start codon or splice-site mutations, as seen in two of our cases.
4. Materials and Methods
4.1. Identification of Signal Peptide Possessing Genes and Cases of Interest
This study was approved by the Wills Eye Hospital (IRB #2021-74) IRB and ethics committee in accordance with the tenants of the Declaration of Helsinki. Genes implicated in IRDs were retrieved from the hereditary retinal disease online database RetNet (https://sph.uth.edu/retnet/ (accessed on 15 April 2021)). The protein sequence database UniProt (https://www.uniprot.org/ (accessed on 16 April 2021)) was then queried to determine which IRD-associated genes contain SP sequences and to identify the positions of the amino acids composing the SP sequences. The most likely locations of the three SP regions (N-terminal, hydrophobic core, and C-terminal) and the cleavage site were then identified using the online signal peptide analysis tool, Signal 6.0 (https://services.healthtech.predcitortu.dk/service.php?SignalP-6.0 (accessed on 20 April 2021)).
Patient genetic results databases from three separate institutions, Wills Eye Hospital, Children’s Hospital of Los Angeles, and Casey Eye Institute, were reviewed to identify cases of patients with both a confirmed IRD diagnosis and a variant located within the SP sequence from June 2011–August 2021.
4.2. In Silico Bioinformatic Evaluation of Signal Peptide Variants
In silico analyses of SP variants were performed using SignalP 6.0, MutationTaster, and MutPred. These freely available online software packages assess the structural and functional biochemical consequences of genetic mutations on proteins.
The SignalP 6.0 (https://services.healthtech.predcitortu.dk/service.php?SignalP-6.0 (accessed on 20 April 2021)) server uses protein language models containing an extensive list of proteins to predict the presence of SP sequences across all organisms [35]. SignalP 6.0 offers a likelihood score (0–1) of whether an input nucleotide sequence contains an SP based on the biological and structural properties of the amino acid sequence. A 0-likelihood score indicates a 0% chance likelihood that the input sequence contains an SP, whereas a 1-likelihood score indicates a 100% chance of the presence of an SP. Wildtype (WT) sequence retrieved from UniProt and variant amino acid sequences of the identified genes with SP mutations in our patient population were input to SignalP 6.0. Differences in their likelihood scores were expressed as a percentage (%) change.
MutationTaster (https://www.mutationtaster.org/ (accessed on 1 August 2021)) uses a Random Forest method to predict the disease potential of a mutation and classifies it as either disease-causing or polymorphism. The MutPred suite (http://mutpred.mutdb.org/ (accessed on 1 August 2021)) encompasses a group of web-based tools including MutPred2, MutPred INDEL, and MutPred-Loss of Function. These are sequence-based machine learning models that integrate genetic and molecular information to predict the pathogenicity of amino acid substitutions [36]. All three tools generate a continuous pathogenicity prediction value of 0–1 for a given mutation. Values above 0.70 indicate pathogenicity for missense mutations and values above 0.50 indicate pathogenicity for both in-frame insertion/deletion and frameshift mutations.
The SP variants that were considered as contributing to the disease burden of IRDs in this patient population were those that met all of the following criteria: they were (1) identified in the SP coding sequence, (2) present in genes that have previously been associated with an IRD, (3) present in IRD patients with genetic testing and a clinical phenotype consistent with mutations in the specific gene containing the SP mutation (genotype-phenotype correlation), (4) present in patients without genetic evidence of further mutational burden in the SP-mutated gene in cis outside of the SP region, (5) present in patients without genetic evidence that their IRD may be caused by mutations in other genes, and (6) considered pathogenic or deleterious by at least one of the in silico algorithms.
5. Conclusions
In conclusion, we have described several cases of distinct IRDs associated with mutations in the SP of the affected proteins. Previous reports have demonstrated how mutations in the different regions of the SP will impact protein processing and secretion, leading to disease. We hope this information will further expand the awareness of these extremely rare types of genetic mutations and help lay further groundwork for research into the prevalence and role of SP mutations in hereditary ophthalmic diseases and the development of possible therapies for these patients.
Supplementary Materials
The following supporting information can be downloaded at: www.mdpi.com/article/10.3390/ijms232113361/s1.
Author Contributions
Conceptualization, A.N., M.E.P. and J.S.P.; Funding acquisition, T.B.T.T.; Investigation, H.J.J. and J.S.P.; Methodology, H.J.J., R.A.P., M.H.M., M.A.K., A.N., M.E.P. and J.S.P.; Project administration, J.S.P.; Supervision, M.A.K. and J.S.P.; Visualization, H.J.J., R.A.P., T.B.T.T., M.H.M., N.I., M.A.K., A.N., M.E.P. and J.S.P.; Writing—original draft, H.J.J., R.A.P., T.B.T.T., M.H.M., M.A.K., A.N. and J.S.P.; Writing—review & editing, H.J.J., R.A.P., T.B.T.T., M.H.M., N.I., M.A.K., A.N., M.E.P. and J.S.P. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported in part by the National Institute for Health Research under Grant R24 EY027285.
Institutional Review Board Statement
This study was approved by the Wills Eye Hospital (IRB #2021-74) IRB and ethics committee in accordance with the tenants of the Declaration of Helsinki.
Informed Consent Statement
Patient consent was waived by the Wills Eye Hospital IRD due to the retrospective nature of the study and the use of deidentified patient data.
Data Availability Statement
Not applicable.
Acknowledgments
We express our gratitude to the J. Arch McNamara Fund, Wills Eye Hospital, and MidAtlantic Retina for their support of this research.
Conflicts of Interest
The authors declare no conflict of interest.
Appendix A. Clinical Summaries of Cases in Our Patient Cohort
- Case 1
A 5-year-old male was evaluated due to nyctalopia, which started at 2 years of age. Past medical history and review of systems were otherwise unremarkable. On exam, visual acuity was 20/200 OU. Intraocular pressure (IOP) and slit-lamp examination (SLE) were unremarkable in both eyes. Fundus autofluorescence revealed no abnormal findings. OCT of the macula was remarkable for cystoid macular edema. ERG demonstrated an essentially absent scotopic response OU. Photopic responses were severely attenuated OU. OCT showed stable cystoid macular edema. These findings were consistent with early childhood-onset retinal dystrophy (EORD). Genetic testing performed via Blueprint Retinal Dystrophy panel identified two disease-causing or pathogenic, genetic variants in the CRB1 gene, c.2T>C (p.Met1*) and c.2056C>T (p.R686C). Segregation analysis revealed the father was a carrier of the c.2T>C variant, who was not affected.
- Case 2
A 2-month-old male was evaluated due to concern for familial exudative vitreoretinopathy (FEVR). The patient had a history of iris contact against the posterior cornea with the lens directly behind the iris almost in contact with the cornea and a fibrotic posterior plaque of dysplastic retina was noted in contact with the back of the lens in both eyes confirmed by ultrasound biomicroscopy. No clear blood vessels were seen at the posterior lens in either eye. Upon fundus examination, no clear persistent vasculature stalk was appreciated although there was a retina attached to the optic nerve in both eyes. A brain MRI revealed bilateral retinal detachments which were determined to be posterior persistent hyperplastic primary vitreous. Visual evoked potentials were performed and showed no reproducible evoked potentials with monocular stimulation in either eye. The Blueprint Vitreoretinopathy gene panel was ordered for molecular diagnosis and revealed a hemizygous likely pathogenic variant, c.37_57del21 (p.L13_M19del), in the NDP gene. Subsequent segregation analysis revealed that the mother and sister were both carriers of the variant. Due to the absence of systemic symptoms or developmental delay associated with Norrie disease, a diagnosis of isolated FEVR was made.
- Case 3
An 11-year-old male patient was first evaluated at 2 years old. The most recent clinical examination was remarkable for visual acuity of CF OD and 20/60 OS. The patient had a spherical equivalent error of approximately -5D OU. Upon fundus examination, inferotemporal traction with retinal fold OD and temporal traction with dragged macula OS. No laser therapy was performed given minimal avascular retina and no active neo-vascularization. There is no pertinent family history, and segregation analysis was not performed. Genetic testing found an FZD4 c.23delC (p.P8Rfs*53) variant resulting in a frameshift and a premature stop codon at position 53.
- Case 4
A 64-year-old male presented at age 48 with nyctalopia, visual field defects, photophobia, and dyschromatopsia. ERG showed moderate to severe decreases in both rod and cone-driven responses consistent with a mixed rod/cone dystrophy. He was diagnosed with RP. Genetic testing was positive for two heterozygous EYS c.32_33insT (p. M12Dfs*14) and c.9036delT (p.W32L) variants. Although segregation analysis was not performed, an autosomal inheritance pattern is suspected. Both variants have been previously reported in different patients with autosomal recessive RP (39,40).
- Case 5
A male patient was diagnosed with XLRS at the age of 11. Multiple surgeries had been performed on his right eye, and the fundus could not be viewed with fundoscopy or tested by ERG. His left eye has retinoschisis with inner retinal holes inferiorly and temporally, and scarring medially; the vessels were attenuated, and a cataract was present. ERG of the left eye showed abnormal amplitudes and implicit time of rod and cone-dependent responses. Consistent with the clinical phenotype, a hemizygous frameshift c.53-859_78+276 (p.A18Pfs*108) deletion was detected in the RS1 gene. This mutation removes the entire exon 2 of the RS1 gene (This case is submitted elsewhere as a case report).
- Case 6
A 12-year-old was referred for ophthalmology evaluation due to problems with vision in low light settings. VA was 20/40 OD and 20/50 OS. IOP was within normal limits and SLE was unremarkable. Dilated fundus exam was remarkable for radial stria of his perifoveal in the superficial retina and small intraretinal cystoid spaces. OCT of the macula showed inner retinoschisis with septa with a normal photoreceptor layer and no surface gliosis. No vitreoretinal attraction. Goldmann visual fields were normal. Fundus autofluorescence was normal except for abnormally placed fluorescence in the perifovea with a stellate pattern. Full-field ERG was normal with borderline cone responses. Multi-focal ERG showed depression centrally more than peripherally and no electronegative B waves. IV fluorescein angiography has abnormal fluorescence in the perifovea but no leakage, thus ruling out cystoid macular edema. Based on findings, the patient was sent for genetic testing, which was positive for a hemizygous RS1 c.52+1 G>C mutation which was also present in his mother and sister.
References
- Von Heijne, G. The signal peptide. J. Membr. Biol. 1990, 115, 195–201. [Google Scholar] [CrossRef] [PubMed]
- UniProt. Available online: https://www.uniprot.org/ (accessed on 14 July 2021).
- Jarjanazi, H.; Savas, S.; Pabalan, N.; Dennis, J.; Ozelik, H. Biological implications of SNPs in signal peptide domains of human proteins. Proteins 2008, 70, 394–403. [Google Scholar] [CrossRef] [PubMed]
- Inglehearn, C.F. Molecular genetics of human retinal dystrophies. Eye 1998, 12, 571–579. [Google Scholar] [CrossRef] [PubMed]
- Berger, W.; Kloeckener-Gruissem, B.; Neidhardt, J. The molecular basis of human retinal and vitreoretinal diseases. Prog. Retin. Eye Res. 2010, 29, 335–375. [Google Scholar] [CrossRef]
- Hiraoka, M.; Takahashi, H.; Orimo, H.; Hiraoka, M.; Ogata, T.; Azuma, N. Genetic screening of Wnt signaling factors in advanced retinopathy of prematurity. Mol. Vis. 2010, 16, 2572–2577. [Google Scholar]
- Vijayasarathy, C.; Sui, R.; Zeng, Y.; Yang, G.; Xu, F.; Caruso, R.C.; Lewis, R.A.; Ziccardi, L.; Sieving, P.A. Molecular mechanisms leading to null-protein product from retinoschisin (RS1) signal-sequence mutants in X-Linked Retinoschisis (XLRS) disease. Hum. Mutat. 2010, 31, 1251–1260. [Google Scholar] [CrossRef]
- Hosono, K.; Nishina, S.; Yokoi, T.; Katagiri, S.; Saitsu, H.; Kurata, K.; Miyamichi, D.; Hikoya, A.; Mizobuchi, K.; Nakano, T.; et al. Molecular diagnosis of 34 Japanese families with leber congenital amaurosis using targeted next generation sequencing. Sci. Rep. 2018, 8, 8279. [Google Scholar] [CrossRef]
- Glöckle, N.; Kohl, S.; Mohr, J.; Scheurenbrand, T.; Sprecher, A.; Weisschuh, N.; Bernd, A.; Rudolph, G.; Schubach, M.; Poloschek, C.; et al. Panel-based next generation sequencing as a reliable and efficient technique to detect mutations in unselected patients with retinal dystrophies. Eur. J. Hum. Genet. 2014, 22, 99–104. [Google Scholar] [CrossRef]
- McGuigan, D.B.; Heon, E.; Cideciyan, A.V.; Ratnapriya, R.; Lu, M.; Sumaroka, A.; Roman, A.J.; Batmanabane, V.; Garafalo, A.V.; Stone, E.M.; et al. EYS mutations causing autosomal recessive retinitis pigmentosa: Changes of retinal structure and function with disease progression. Genes 2017, 8, 178. [Google Scholar] [CrossRef]
- Stone, E.M.; Andorf, J.L.; Whitmore, S.S.; DeLuca, A.P.; Giacalone, J.C.; Streb, L.M.; Braun, T.A.; Mullins, R.F.; Scheetz, T.E.; Sheffield, V.C.; et al. Clinically Focused Molecular Investigation of 1000 Consecutive Families with Inherited Retinal Disease. Ophthalmology 2017, 124, 1314–1331. [Google Scholar] [CrossRef]
- Andrew, D.W.; Young, J.C.; Mirelsq, L.F.; Czarnota, G.J. The Role of the N Region in Signal Sequence and Signal-anchor Function*. J. Biol. Chem. 1992, 267, 7761–7769. [Google Scholar] [CrossRef]
- Guo, H.; Sun, J.; Li, X.; Xiong, Y.; Wang, H.; Shu, H.; Zhu, R.; Liu, Q.; Huang, Y.; Madley, R.; et al. Positive charge in the n-region of the signal peptide contributes to efficient post-translational translocation of small secretory preproteins. J. Biol. Chem. 2018, 293, 1899–1907. [Google Scholar] [CrossRef] [PubMed]
- Liu, M.; Sun, J.; Cui, J.; Chen, W.; Guo, H.; Barbetti, F.; Arvan, P. INS-gene mutations: From genetics and beta cell biology to clinical disease. Mol. Asp. Med. 2016, 176, 139–148. [Google Scholar] [CrossRef] [PubMed]
- Abad-Navarro, F.; De La Morena-Barrio, M.E.; Fernández-Breis, J.T.; Corral, J. Lost in translation: Bioinformatic analysis of variations affecting the translation initiation codon in the human genome. Bioinformatics 2018, 34, 3788–3794. [Google Scholar] [CrossRef]
- Kearse, M.G.; Wilusz, J.E. Non-AUG translation: A new start for protein synthesis in eukaryotes. Genes Dev. 2017, 31, 1717–1731. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Zhang, J.; Chen, N.; Wang, L.; Zhang, F.; Ma, Z.; Li, G.; Yang, L. Application of whole exome and targeted panel sequencing in the clinical molecular diagnosis of 319 Chinese families with inherited retinal dystrophy and comparison study. Genes 2018, 9, 360. [Google Scholar] [CrossRef]
- Navarro-Fernández, J.; Dybedal, I.; Águila, S.; Bohdam, N.; Corrales, F.; Miqueo, C.; Andresen, M.; Ferrer, F.; Tjønnfjord, G.E.; Martínez-Martínez, I.; et al. C0380: Clinical and Biochemical Consequences of Met1Ileu Mutation in Serpinc1 Gene: Generation of a Small Non-Inhibitory Antithrombin Variant without the N-Terminal Region by Use of an Alternative Initiation Codon that Has a Strong Gain-Of-Function Associ. Thromb. Res. 2014, 133, S11. [Google Scholar] [CrossRef]
- Owji, H.; Nezafat, N.; Negahdaripour, M.; Hajiebrahimi, A.; Ghasemi, Y. A comprehensive review of signal peptides: Structure, roles, and applications. Eur. J. Cell Biol. 2018, 97, 422–441. [Google Scholar] [CrossRef]
- Chung, B.D.; Kayserili, H.; Ai, M.; Freudenberg, J.; Üzümcü, A.; Uyguner, O.; Bartels, C.F.; Höning, S.; Ramirez, A.; Hanisch, F.G.; et al. A mutation in the signal sequence of LRP5 in a family with an osteoporosis-pseudoglioma syndrome(OPPG)-like phenotype indicates a novel disease mechanism for trinucleotide repeats. Hum. Mutat. 2009, 30, 641–648. [Google Scholar] [CrossRef]
- Hughes, A.E.; Ralston, S.H.; Marken, J.; Bell, C.; MacPherson, H.; Wallace, R.G.H.; Van Hul, W.; Whyte, M.P.; Nakatsuka, K.; Hovy, L.; et al. Mutations in TNFRSF11A, affecting the signal peptide of RANK, cause familial expansile osteolysis. Nat. Genet. 2000, 24, 45–48. [Google Scholar] [CrossRef]
- Seppen, J.; Steenken, E.; Lindhout, D.; Bosma, P.J.; Oude Elferink, R.P.J. A mutation which disrupts the hydrophobic core of the signal peptide of bilirubin UDP-glucuronosyltransferase, an endoplasmic reticulum membrane protein, causes Crigler-Najjar type II. FEBS Lett. 1996, 390, 294–298. [Google Scholar] [CrossRef]
- Vezzoli, V.; Duminuco, P.; Vottero, A.; Kleinau, G.; Schülein, R.; Minari, R.; Bassi, I.; Bernasconi, S.; Persani, L.; Bonomi, M. A newvariant in signal peptide of the human luteinizing hormone receptor (LHCGR) affects receptor biogenesis causing leydig cell hypoplasia. Hum. Mol. Genet. 2015, 24, 6003–6012. [Google Scholar] [CrossRef] [PubMed]
- Kyte, J.; Doolittle, R.F. A simple method for displaying the hydropathic character of a protein. J. Mol. Biol. 1982, 157, 105–132. [Google Scholar] [CrossRef]
- Karamyshev, A.L.; Karamysheva, Z.N. Lost in translation: Ribosome-associated mRNA and protein quality controls. Front. Genet. 2018, 9, 431. [Google Scholar] [CrossRef]
- Noorwez, S.M.; Kuksa, V.; Imanishi, Y.; Zhu, L.; Filipek, S.; Palczewski, K.; Kaushal, S. Pharmacological chaperone-mediated in vivo folding and stabilization of the P23H-opsin mutant associated with autosomal dominant retinitis pigmentosa. J. Biol. Chem. 2003, 278, 14442–14450. [Google Scholar] [CrossRef]
- Walter, P.; Ron, D. The unfolded protein response: From stress pathway to homeostatic regulation. Science 2011, 334, 1081–1086. [Google Scholar] [CrossRef]
- Guerriero, C.J.; Brodsky, J.L. The delicate balance between secreted protein folding and endoplasmic reticulum-associated degradation in human physiology. Physiol. Rev. 2012, 92, 537–576. [Google Scholar] [CrossRef]
- Zhang, S.X.; Sanders, E.; Fliesler, S.J.; Wang, J.J. Endoplasmic reticulum stress and the unfolded protein responses in retinal degeneration. Exp. Eye Res. 2014, 125, 30–40. [Google Scholar] [CrossRef]
- Kroeger, H.; Lavail, M.M.; Lin, J.H. Endoplasmic reticulum stress in vertebrate mutant rhodopsin models of retinal degeneration. In Advances in Experimental Medicine and Biology; NIH Public Access: Bethesda, MD, USA, 2014; Volume 801, pp. 585–592. [Google Scholar]
- Datta, R.; Waheed, A.; Shah, G.N.; Sly, W.S. Signal sequence mutation in autosomal dominant form of hypoparathyroidism induces apoptosis that is corrected by a chemical chaperone. Proc. Natl. Acad. Sci. USA 2007, 104, 19989–19994. [Google Scholar] [CrossRef]
- Kosmaoglou, M.; Schwarz, N.; Bett, J.S.; Cheetham, M.E. Molecular chaperones and photoreceptor function. Prog. Retin. Eye Res. 2008, 27, 434–449. [Google Scholar] [CrossRef]
- Fan, J.Q.; Ishii, S.; Asano, N.; Suzuki, Y. Accelerated transport and maturation of lysosomal α-galactosidase A in fabry lymphoblasts by an enzyme inhibitor. Nat. Med. 1999, 5, 112–115. [Google Scholar] [CrossRef] [PubMed]
- Lam, B.L.; Leroy, B.P.; Black, G.; Ong, T.; Yoon, D.; Trzupek, K. Genetic testing and diagnosis of inherited retinal diseases. Orphanet J. Rare Dis. 2021, 16, 514. [Google Scholar] [CrossRef] [PubMed]
- Teufel, F.; Juan, J.; Armenteros, A.; Johansen, A.R.; Gíslason, M.H.; Pihl, S.I.; Tsirigos, K.D.; Winther, O.; Brunak, S.; Von Heijne, G.; et al. SignalP 6.0 achieves signal peptide prediction across all types using protein language models. Nat. Biotechnol. 2021, 40, 1023–1025. [Google Scholar] [CrossRef] [PubMed]
- Pejaver, V.; Urresti, J.; Lugo-Martinez, J.; Pagel, K.A.; Lin, G.N.; Nam, H.J.; Mort, M.; Cooper, D.N.; Sebat, J.; Iakoucheva, L.M.; et al. Inferring the molecular and phenotypic impact of amino acid variants with MutPred2. Nat. Commun. 2020, 11, 5918. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).