GSTT1/GSTM1 Genotype and Anti-Tuberculosis Drug-Induced Hepatotoxicity in Peruvian Patients
Abstract
1. Introduction
2. Results
3. Discussion
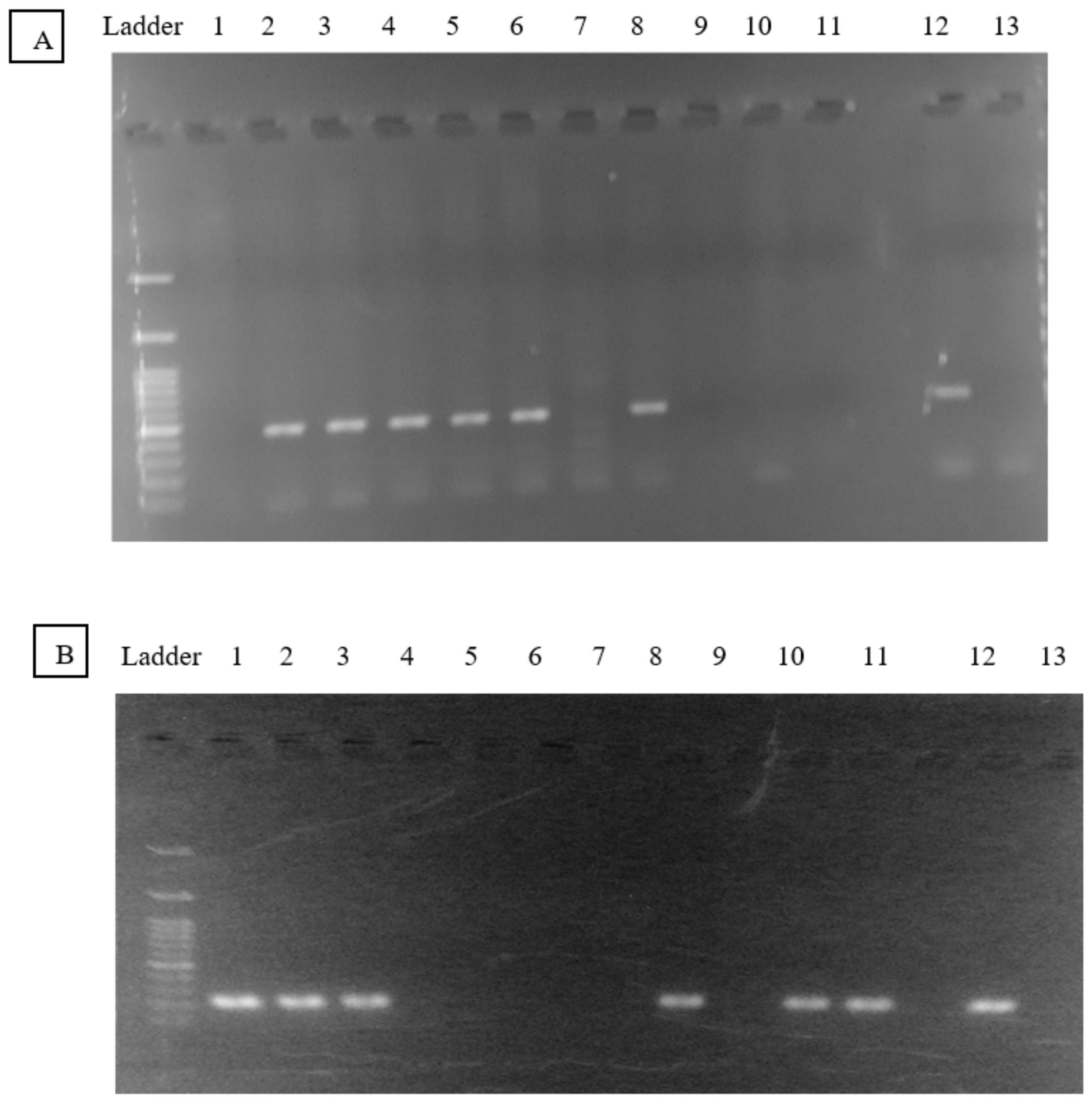
4. Methods and Materials
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Chamorro, J.G.; Castagnino, J.P.; Musella, R.M.; Nogueras, M.; Aranda, F.M.; Frías, A.; Visca, M.; Aidar, O.; Perés, S.; de Larrañaga, G.F. Sex, ethnicity, and slow acetylator profile are the major causes of hepatotoxicity induced by antituberculosis drugs. J. Gastroenterol. Hepatol. 2013, 28, 323–328. Available online: http://www.ncbi.nlm.nih.gov/pubmed/23190413 (accessed on 20 August 2019). [CrossRef] [PubMed]
- Possuelo, L.G.; Castelan, J.A.; de Brito, T.C.; Ribeiro, A.W.; Cafrune, P.I.; Picon, P.D.; Santos, A.R.; Teixeira, R.L.F.; Gregianini, T.S.; Hutz, M.H.; et al. Association of slow N-acetyltransferase 2 profile and anti-TB drug-induced hepatotoxicity in patients from Southern Brazil. Eur. J. Clin. Pharmacol. 2008, 64, 673–681. [Google Scholar] [CrossRef] [PubMed]
- Yimer, G.; Ueda, N.; Habtewold, A.; Amogne, W.; Suda, A.; Riedel, K.-D.; Burhenne, J.; Aderaye, G.; Lindquist, L.; Makonnen, E.; et al. Pharmacogenetic & pharmacokinetic biomarker for efavirenz based ARV and rifampicin based anti-TB drug induced liver injury in TB-HIV infected patients. PLoS ONE 2011, 6, e27810. [Google Scholar]
- Simon, T.; Becquemont, L.; Mary-Krause, M.; de Waziers, I.; Beaune, P.; Funck-Brentano, C.; Jaillon, P. Combined glutathione-S-transferase M1 and T1 genetic polymorphism and tacrine hepatotoxicity. Clin. Pharmacol. Ther. 2000, 67, 432–437. [Google Scholar] [CrossRef]
- Gupta, V.H.; Singh, M.; Amarapurkar, D.N.; Sasi, P.; Joshi, J.M.; Baijal, R.; Kumar, H.R.P.; Amarapurkar, A.D.; Joshi, K.; Wangikar, P.P. Association of GST null genotypes with anti-tuberculosis drug induced hepatotoxicity in Western Indian population. Ann. Hepatol. 2013, 12, 959–965. Available online: https://www.elsevier.es/en-revista-annals-hepatology-16-articulo-association-gst-null-genotypes-with-S166526811931302X (accessed on 31 May 2022). [CrossRef]
- De Teixeira, R.L.F.; Morato, R.G.; Cabello, P.H.; Muniz, L.M.K.; Moreira, A.d.S.R.; Kritski, A.L.; Mello, F.C.Q.; Suffys, P.N.; de Miranda, A.B. Genetic polymorphisms of NAT2, CYP2E1 and GST enzymes and the occurrence of antituberculosis drug-induced hepatitis in Brazilian TB patients. Mem. Inst. Oswaldo Cruz. 2011, 106, 716–724. [Google Scholar] [CrossRef]
- Lv, X.; Tang, S.; Xia, Y.; Zhang, Y.; Wu, S.; Yang, Z.; Li, X.; Tu, D.; Chen, Y.; Deng, P.; et al. NAT2 genetic polymorphisms and anti-tuberculosis drug-induced hepatotoxicity in Chinese community population. Ann. Hepatol. 2012, 11, 700–707. [Google Scholar] [CrossRef]
- Strange, R.C.; Jones, P.W.; Fryer, A.A. Glutathione S-transferase: Genetics and role in toxicology. Toxicol. Lett. 2000, 112–113, 357–363. [Google Scholar] [CrossRef]
- Meister, A. Selective modification of glutathione metabolism. Science 1983, 220, 472–477. [Google Scholar] [CrossRef]
- Meyer, D.J.; Coles, B.; Pemble, S.E.; Gilmore, K.S.; Fraser, G.M.; Ketterer, B. Theta, a new class of glutathione transferases purified from rat and man. Biochem. J. 1991, 274, 409–414. [Google Scholar] [CrossRef]
- Pemble, S.; Schroeder, K.R.; Spencer, S.R.; Meyer, D.J.; Hallier, E.; Bolt, H.M.; Ketterer, B.; Taylor, J.B. Human glutathione S-transferase theta (GSTT1): cDNA cloning and the characterization of a genetic polymorphism. Biochem. J. 1994, 300 Pt 1, 271–276. [Google Scholar] [CrossRef]
- Roy, B.; Chowdhury, A.; Kundu, S.; Santra, A.; Dey, B.; Chakraborty, M.; Majumder, P.P. Increased risk of antituberculosis drug-induced hepatotoxicity in individuals with glutathione S-transferase M1 “null” mutation. J. Gastroenterol. Hepatol. 2001, 16, 1033–1037. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.-S.; Su, W.-J.; Huang, Y.-H.; Chen, C.-Y.; Chang, F.-Y.; Lin, H.-C.; Lee, S.D. Genetic polymorphisms of manganese superoxide dismutase, NAD(P)H:quinone oxidoreductase, glutathione S-transferase M1 and T1, and the susceptibility to drug-induced liver injury. J. Hepatol. 2007, 47, 128–134. [Google Scholar] [CrossRef] [PubMed]
- Chatterjee, S.; Lyle, N.; Mandal, A.; Kundu, S. GSTT1 and GSTM1 gene deletions are not associated with hepatotoxicity caused by antitubercular drugs. J. Clin. Pharm. Ther. 2010, 35, 465–470. [Google Scholar] [CrossRef]
- Leiro, V.; Fernández-Villar, A.; Valverde, D.; Constenla, L.; Vázquez, R.; Piñeiro, L.; González-Quintela, A. Influence of glutathione S-transferase M1 and T1 homozygous null mutations on the risk of antituberculosis drug-induced hepatotoxicity in a Caucasian population. Liver Int. 2008, 28, 835–839. [Google Scholar] [CrossRef] [PubMed]
- Tang, S.-W.; Lv, X.-Z.; Zhang, Y.; Wu, S.-S.; Yang, Z.-R.; Xia, Y.-Y.; Tu, D.-H.; Deng, P.-Y.; Ma, Y.; Chen, D.-F.; et al. CYP2E1, GSTM1 and GSTT1 genetic polymorphisms and susceptibility to antituberculosis drug-induced hepatotoxicity: A nested case-control study. J. Clin. Pharm. Ther. 2012, 37, 588–593. [Google Scholar] [CrossRef]
- Lu, Y.-F.; Goldstein, D.B.; Angrist, M.; Cavalleri, G. Personalized medicine and human genetic diversity. Cold Spring Harb. Perspect. Med. 2014, 4, a008581. Available online: http://www.ncbi.nlm.nih.gov/pubmed/25059740 (accessed on 1 August 2019). [CrossRef]
- Suarez-Kurtz, G.; Pena, S.D.J. Pharmacogenomics in the Americas: The impact of genetic admixture. Curr. Drug Targets 2006, 7, 1649–1658. [Google Scholar] [CrossRef]
- Guio, H.; Poterico, J.A.; Levano, K.S.; Cornejo-Olivas, M.; Mazzetti, P.; Manassero-Morales, G.; Ugarte-Gil, M.F.; Acevedo-Vásquez, E.; Dueñas-Roque, M.; Piscoya, A. Genetics and genomics in Peru: Clinical and research perspective. Mol. Genet. Genomic Med. 2018, 6, 873–886. Available online: http://www.ncbi.nlm.nih.gov/pubmed/30584990 (accessed on 1 August 2019). [CrossRef]
- Rohrer Vitek, C.R.; Nicholson, W.T.; Schultz, C.; Caraballo, P.J. Evaluation of the use of clinical decision support and online resources for pharmacogenomics education. Pharmacogenomics 2015, 16, 1595–1603. Available online: http://www.ncbi.nlm.nih.gov/pubmed/26419532 (accessed on 1 August 2019). [CrossRef]
- Weinshilboum, R.; Wang, L. Pharmacogenomics: Bench to bedside. Nat. Rev. Drug. Discov. 2004, 3, 739–748. Available online: http://www.ncbi.nlm.nih.gov/pubmed/15340384 (accessed on 1 August 2019). [CrossRef] [PubMed]
- Fuselli, S.; Gilman, R.H.; Chanock, S.J.; Bonatto, S.L.; De Stefano, G.; Evans, C.A.; Labuda, D.; Luiselli, D.; Salzano, F.M.; Soto, G.; et al. Analysis of nucleotide diversity of NAT2 coding region reveals homogeneity across Native American populations and high intra-population diversity. Pharm. J. 2007, 7, 144–152. Available online: http://www.ncbi.nlm.nih.gov/pubmed/16847467 (accessed on 15 April 2018). [CrossRef] [PubMed]
- Bisso-Machado, R.; Ramallo, V.; Paixão-Côrtes, V.R.; Acuña-Alonzo, V.; Demarchi, D.A.; Sandoval, J.R.S.; Granara, A.A.S.; Salzano, F.M.; Hünemeier, T.; Bortolini, M.C. NAT2 gene diversity and its evolutionary trajectory in the Americas. Pharm. J. 2016, 16, 559–565. Available online: https://pubmed.ncbi.nlm.nih.gov/26503810/ (accessed on 12 March 2021). [CrossRef]
- Levano, K.S.; Jaramillo-Valverde, L.; Tarazona, D.D.; Sanchez, C.; Capristano, S.; Solari, L.; Mendoza-Ticona, A.; Soto, A.; Rojas, C.; Zegarra-Chapoñan, R.; et al. Allelic and Genotypic Frequencies of NAT2, CYP2E1 and AADAC genes in a cohort of Peruvian Tuberculosis Patients. bioRxiv 2021, 9, e1764. [Google Scholar] [CrossRef] [PubMed]
- Harris, D.N.; Song, W.; Shetty, A.C.; Levano, K.S.; Cáceres, O.; Padilla, C.; Borda, V.; Tarazona, D.; Trujillo, O.; Sanchez, C.; et al. Evolutionary genomic dynamics of Peruvians before, during, and after the Inca Empire. Proc. Natl. Acad. Sci. USA 2018, 115, E6526–E6535. Available online: http://www.ncbi.nlm.nih.gov/pubmed/29946025 (accessed on 27 February 2019). [CrossRef]
- Bolt, H.; Thier, R. Relevance of the Deletion Polymorphisms of the Glutathione S-Transferases GSTT1 and GSTM1 in Pharmacology and Toxicology. Curr. Drug. Metab. 2006, 7, 613–628. [Google Scholar] [CrossRef]
- Metabolic Gene Polymorphism Frequencies in Control Populations1|Cancer Epidemiology, Biomarkers & Prevention|American Association for Cancer Research. Available online: https://aacrjournals.org/cebp/article/10/12/1239/164217/Metabolic-Gene-Polymorphism-Frequencies-in-Control (accessed on 31 May 2022).
- Chanhom, N.; Udomsinprasert, W.; Chaikledkaew, U.S.A.; Mahasirimongkol, S.; Wattanapokayakit, S.; Jittikoon, J. GSTM1 and GSTT1 genetic polymorphisms and their association with antituberculosis drug-induced liver injury. Biomed Rep. 2020, 12, 153. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7054707/ (accessed on 25 July 2022). [CrossRef]
- Kim, S.H.; Kim, S.H.; Yoon, H.J.; Shin, D.H.; Park, S.S.; Kim, Y.S.; Jae-Seuk, P.; Young Koo, J. GSTT1 and GSTM1 null mutations and adverse reactions induced by antituberculosis drugs in Koreans. Tuberculosis 2010, 90, 39–43. [Google Scholar] [CrossRef]
- Voso, M.T.; D’Alo’, F.; Putzulu, R.; Mele, L.; Scardocci, A.; Chiusolo, P.; Latagliata, R.; Lo-Coco, F.; Rutella, S.; Pagano, L.; et al. Negative prognostic value of glutathione S-transferase (GSTM1 and GSTT1) deletions in adult acute myeloid leukemia. Blood 2002, 100, 2703–2707. Available online: https://pubmed.ncbi.nlm.nih.gov/12351375/ (accessed on 31 May 2022). [CrossRef]
- Haase, D.; Binder, C.; Bünger, J.; Fonatsch, C.; Streubel, B.; Schnittger, S.; Griesinger, F.; Westphal, G.; Schoch, C.; Knopp, A.; et al. Increased risk for therapy-associated hematologic malignancies in patients with carcinoma of the breast and combined homozygous gene deletions of glutathione transferases M1 and T1. Leuk. Res. 2002, 26, 249–254. Available online: https://europepmc.org/article/med/11792413 (accessed on 31 May 2022). [CrossRef]
- Huang, C.C.; Chien, W.P.; Wong, R.H.; Cheng, Y.W.; Chen, M.C.; Chou, M.C.; Lee, H. NAT2 Fast Acetylator Genotype is Associated with an Increased Risk of Colorectal Cancer in Taiwan. Dis. Colon. Rectum. 2007, 50, 981–989. [Google Scholar] [CrossRef]
- Guio, H.; Levano, K.S.; Sanchez, C.; Tarazona, D. The role of pharmacogenomics in the tuberculosis treatment regime. Rev. Peru Med. Exp. Salud. Publica 2015, 32, 794–800. [Google Scholar] [CrossRef]
- Shaikh, R.S.; Amir, M.; Masood, A.I.; Sohail, A.; Athar, H.U.R.; Siraj, S.; Ali, M.; Anjam, M.S. Frequency distribution of GSTM1 and GSTT1 null allele in Pakistani population and risk of disease incidence. Environ. Toxicol. Pharmacol. 2010, 30, 76–79. [Google Scholar] [CrossRef] [PubMed]
- Li, C.; Long, J.; Hu, X.; Zhou, Y. GSTM1 and GSTT1 genetic polymorphisms and risk of anti-tuberculosis drug-induced hepatotoxicity: An updated meta-analysis. Eur. J. Clin. Microbiol. Infect. Dis. 2013, 32, 859–868. [Google Scholar] [CrossRef] [PubMed]
- Tang, N.; Deng, R.; Wang, Y.; Lin, M.; Li, H.; Qiu, Y.; Hong, M.; Zhou, G. GSTM1 and GSTT1 null polymorphisms and susceptibility to anti-tuberculosis drug-induced liver injury: A meta-analysis. Int. J. Tuberc. Lung Dis. 2013, 17, 17–25. [Google Scholar] [CrossRef] [PubMed]
- MINSA. Norma Técnica de Salud Para la Atención Integral de las Personas Afectadas por Tuberculosis. 2013. Available online: http://www.minsa.gob.pe (accessed on 21 November 2021).
- Ramappa, V.; Aithal, G.P. Hepatotoxicity Related to Anti-tuberculosis Drugs: Mechanisms and Management. J. Clin. Exp. Hepatol. 2013, 3, 37–49. Available online: http://www.ncbi.nlm.nih.gov/pubmed/25755470 (accessed on 12 October 2019). [CrossRef]
- Araujo-Mariz, C.; Militão de Albuquerque, M.F.P.; Lopes, E.P.; Ximenes, R.A.A.; Lacerda, H.R.; Miranda-Filho, D.B.; Lustosa-Martins, B.B.; Pastor, A.F.P.; Acioli-Santos, B. Hepatotoxicity during TB treatment in people with HIV/AIDS related to NAT2 polymorphisms in Pernambuco, Northeast Brazil. Ann. Hepatol. 2020, 19, 153–160. [Google Scholar] [CrossRef]
- Jaramillo-Valverde, L.; Levano, K.S.; Tarazona, D.D.; Capristano, S.; Zegarra-Chapoñan, R.; Sanchez, C.; Yufra-Picardo, V.M.; Tarazona-Santos, E.; Ugarte-Gil, C.; Guio, H. NAT2 and CYP2E1 polymorphisms and antituberculosis drug-induced hepatotoxicity in Peruvian patients. Mol. Genet. Genomic Med. 2022, 10, e1987. [Google Scholar] [CrossRef]
- Schiaffino, A.; Rodríguez, M.; Pasarín, M.I.; Regidor, E.; Borrell, C.; Fernández, E. ¿Odds ratio o razón de proporciones? Su utilización en estudios transversales. Gac. Sanit. 2003, 17, 70–74. [Google Scholar] [CrossRef]
| Total | Adverse Reaction (DILI) | ||||||
|---|---|---|---|---|---|---|---|
| Variables | Yes | No | p-Value | ||||
| N | % | N | % | N | % | ||
| Sex | |||||||
| Male | 207 | 54.91 | 10 | 62.50 | 197 | 54.57 | |
| Female | 170 | 45.09 | 6 | 37.50 | 164 | 45.43 | 0.533 a |
| Age (years) | - | - | 24.3 * | (20.3–30.8) † | 24.2 * | (20.9–29.6) † | 0.995 b |
| Alcohol consumption | |||||||
| No | 49 | 13.00 | 3 | 18.75 | 46 | 12.74 | |
| Yes | 328 | 87.00 | 13 | 81.25 | 315 | 87.26 | 0.346 c |
| Cholesterol (mg/dL) | - | - | 154.0 * | (141.2–185.0) † | 169 * | (149.0–189.0) † | 0.214 b |
| Hemoglobin (g/dL) | - | - | 13.9 * | (12.2–15.6) † | 13.6 * | (12.4–14.9) † | 0.769 b |
| Glucose (mg/dL) | - | - | 89.5 * | (80.0–95.0) † | 83.1 * | (77.9–91.1) † | 0.084 b |
| BMI (kg/m2) | - | - | 21.1 * | (19.7–22.5) † | 22 * | (20.3–23.6) † | 0.182 b |
| GSTM1 genotype | |||||||
| Present | 199 | 52.79 | 6 | 3.02 | 193 | 96.98 | |
| Null | 178 | 47.21 | 10 | 5.62 | 168 | 94.38 | 0.160 c |
| GSTT1 genotype | |||||||
| Present | 263 | 69.76 | 10 | 3.8 | 253 | 96.20 | |
| Null | 114 | 30.24 | 6 | 5.26 | 108 | 94.74 | 0.346 c |
| Adverse Reaction (DILI) | ||||
|---|---|---|---|---|
| Yes = 16 (%) | No = 361 (%) | OR (CI 95%) | p-Value | |
| GSTM1 | ||||
| Present (M+) | 6 (3.02) | 193 (96.98) | - | |
| Null (M−) | 10 (5.62) | 168 (94.38) | 1.915 (0.61–6.54) | 0.211 |
| GSTT1 | ||||
| Present (T+) | 10 (3.80) | 253 (96.20) | - | |
| Null (T−) | 6 (5.26) | 108 (94.74) | 1.406 (0.41–4.39) | 0.518 |
| Both GSTM1 and T1 | - | |||
| M+/T+ | 13 (3.96) | 314 (96.04) | ||
| M+/T− | 7 (5.47) | 121 (94.53) | 1.397 (0.46–3.87) | 0.485 |
| M−/T+ | 3 (4.92) | 61 (95.08) | 1.188 (0.21–4.50) | 0.793 |
| M−/T− | 3 (6.00) | 47 (96.00) | 1.542 (0.27–5.90) | 0.508 |
| Adverse Reaction (DILI) | |||||||
|---|---|---|---|---|---|---|---|
| GSTM1 | GSTT1 | CYP2E1 | NAT2 | Yes = 16 (%) | No = 361 (%) | OR (IC 95%) | p-Value |
| Present | Present | C1/C1 | Slow | 3 | 33 | Reference | |
| Null | Present | C1/C1 | Slow | 3 | 33 | 1 (0.12–8.02) | 1 |
| Present | Null | C1/C1 | Slow | 0 | 20 | 0 (0–2.28) | 0.185 |
| Null | Null | C1/C1 | Slow | 1 | 15 | 0.73 (0.01–10.09) | 0.795 |
| Present | Present | C1/C2 or C2/C2 | Slow | 0 | 27 | 0 (0–1.67) | 0.124 |
| Null | Present | C1/C2 or C2/C2 | Slow | 0 | 19 | 0 (0–2.4) | 0.196 |
| Present | Null | C1/C2 or C2/C2 | Slow | 0 | 14 | 0 (0–3.31) | 0.265 |
| Null | Null | C1/C2 or C2/C2 | Slow | 2 | 5 | 4.4 (0.28–47.68) | 0.126 |
| Present | Present | C1/C1 | Intermediate | 0 | 29 | 0 (0–1.55) | 0.111 |
| Null | Present | C1/C1 | Intermediate | 1 | 34 | 0.32 (0.01–4.33) | 0.317 |
| Present | Null | C1/C1 | Intermediate | 0 | 16 | 0 (0–2.86) | 0.234 |
| Null | Null | C1/C1 | Intermediate | 0 | 13 | 0 (0–3.58) | 0.283 |
| Present | Present | C1/C2 or C2/C2 | Intermediate | 0 | 15 | 0 (0–3.08) | 0.249 |
| Null | Present | C1/C2 or C2/C2 | Intermediate | 0 | 21 | 0 (0–2.16) | 0.174 |
| Present | Null | C1/C2 or C2/C2 | Intermediate | 0 | 7 | 0 (0–7.04) | 0.428 |
| Null | Null | C1/C2 or C2/C2 | Intermediate | 0 | 6 | 0 (0–8.36) | 0.463 |
| Present | Present | C1/C1 | Rapid | 0 | 14 | 0 (0–3.31) | 0.265 |
| Null | Present | C1/C1 | Rapid | 2 | 10 | 2.2 (0.16–21.78) | 0.413 |
| Present | Null | C1/C1 | Rapid | 2 | 2 | 11 (0.54–186.35) | 0.017 |
| Null | Null | C1/C1 | Rapid | 0 | 6 | 0 (0–8.36) | 0.463 |
| Present | Present | C1/C2 or C2/C2 | Rapid | 0 | 10 | 0 (0–4.75) | 0.345 |
| Null | Present | C1/C2 or C2/C2 | Rapid | 1 | 3 | 3.67 (0.05–65.57) | 0.292 |
| Present | Null | C1/C2 or C2/C2 | Rapid | 1 | 2 | 5.5 (0.07–129.91) | 0.17 |
| Null | Null | C1/C2 or C2/C2 | Rapid | 0 | 2 | 0 (0–28.51) | 0.671 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jaramillo-Valverde, L.; Levano, K.S.; Tarazona, D.D.; Vasquez-Dominguez, A.; Toledo-Nauto, A.; Capristano, S.; Sanchez, C.; Tarazona-Santos, E.; Ugarte-Gil, C.; Guio, H. GSTT1/GSTM1 Genotype and Anti-Tuberculosis Drug-Induced Hepatotoxicity in Peruvian Patients. Int. J. Mol. Sci. 2022, 23, 11028. https://doi.org/10.3390/ijms231911028
Jaramillo-Valverde L, Levano KS, Tarazona DD, Vasquez-Dominguez A, Toledo-Nauto A, Capristano S, Sanchez C, Tarazona-Santos E, Ugarte-Gil C, Guio H. GSTT1/GSTM1 Genotype and Anti-Tuberculosis Drug-Induced Hepatotoxicity in Peruvian Patients. International Journal of Molecular Sciences. 2022; 23(19):11028. https://doi.org/10.3390/ijms231911028
Chicago/Turabian StyleJaramillo-Valverde, Luis, Kelly S. Levano, David D. Tarazona, Andres Vasquez-Dominguez, Anel Toledo-Nauto, Silvia Capristano, Cesar Sanchez, Eduardo Tarazona-Santos, Cesar Ugarte-Gil, and Heinner Guio. 2022. "GSTT1/GSTM1 Genotype and Anti-Tuberculosis Drug-Induced Hepatotoxicity in Peruvian Patients" International Journal of Molecular Sciences 23, no. 19: 11028. https://doi.org/10.3390/ijms231911028
APA StyleJaramillo-Valverde, L., Levano, K. S., Tarazona, D. D., Vasquez-Dominguez, A., Toledo-Nauto, A., Capristano, S., Sanchez, C., Tarazona-Santos, E., Ugarte-Gil, C., & Guio, H. (2022). GSTT1/GSTM1 Genotype and Anti-Tuberculosis Drug-Induced Hepatotoxicity in Peruvian Patients. International Journal of Molecular Sciences, 23(19), 11028. https://doi.org/10.3390/ijms231911028






