Abstract
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), causing the coronavirus disease 2019 (COVID-19), has provoked more than six million deaths worldwide and continues to pose a major threat to global health. Enormous efforts have been made by researchers around the world to elucidate COVID-19 pathophysiology, design efficacious therapy and develop new vaccines to control the pandemic. To this end, experimental models are essential. While animal models and conventional cell cultures have been widely utilized during these research endeavors, they often do not adequately reflect the human responses to SARS-CoV-2 infection. Therefore, models that emulate with high fidelity the SARS-CoV-2 infection in human organs are needed for discovering new antiviral drugs and vaccines against COVID-19. Three-dimensional (3D) cell cultures, such as lung organoids and bioengineered organs-on-chips, are emerging as crucial tools for research on respiratory diseases. The lung airway, small airway and alveolus organ chips have been successfully used for studies on lung response to infection by various pathogens, including corona and influenza A viruses. In this review, we provide an overview of these new tools and their use in studies on COVID-19 pathogenesis and drug testing. We also discuss the limitations of the existing models and indicate some improvements for their use in research against COVID-19 as well as future emerging epidemics.
Keywords:
SARS-CoV-2; 3D cultures; organ-on-a-chip; organoids; lung models; airways; alveolus; viruses 1. Introduction
Coronavirus disease 2019 (COVID-19), caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), is one of the most serious pandemics in human history. In addition to the respiratory system, this virus can impair the function of multiple organs, leading to death, particularly of older people with co-morbidities, such as cardiovascular diseases, chronic kidney and lung disease and diabetes [1]. Soon after the start of the pandemic, investigators from both academia and industry have been tirelessly seeking vaccines and treatments to combat COVID-19 [2,3,4,5,6,7,8]. However, the capability of the SARS-CoV-2 spike protein to mutate and therefore to increase viral transmission rate and escape immunosurveillance has raised additional challenges for the vaccination strategy. A key aspect in this battle against COVID-19 is the need for appropriate experimental models that reproduce human disease with high fidelity in order to generate data that can be rapidly translated to the clinic. In this respect, cell lines have been useful to elucidate mechanisms of viral invasion and infection [9], allowing the identification of the host receptor Angiotensin-converting enzyme 2 (ACE2), Neuropilin-1 (NRP1) and transmembrane serine proteinase 2 (TMPRSS2) as the main proteins involved in SARS-CoV-2 binding and entry into the host cells [10,11,12,13]. However, these 2D cultures revealed major limitations for antiviral drug testing. For example, while chloroquine (or its derivative hydroxychloroquine) showed an antiviral effect in the Vero E6 or Huh-7 cell lines [14,15,16], it failed to inhibit SARS-CoV-2 entry into human cells as well as demonstrate efficacy in clinical trials [17]. On the other hand, animal models, including primates, are not fully representative of human disease and often fail to predict the efficacy of antivirals in humans [14,18,19].
To fill this gap, 3D cultures that recapitulate human lung structure and physiology have been developed. In 2005, Fulcher et al. [20] reported that primary airway epithelial cells (HAE) can be grown on transwells under an air–liquid interface (ALI) and differentiated into a pseudostratified epithelium composed of the main airway cell types, i.e., basal, goblet, club and ciliated cells. Airway cells can be isolated from patients and used for studies of epithelial–stroma interaction when organized as organoids. These are self-organized 3D multicellular structures where the pseudostratified airway epithelium interacts with the extracellular matrix and maintains its main functions, i.e., mucus production and ciliary beating. Thus, these structures can reproduce in vitro the features of the human airway epithelium in vivo [21,22]. The respiratory epithelium organoid culture has been successfully used for research on cystic fibrosis (CF) and other pulmonary diseases [23,24], including viral infections [25,26,27]. However, a main limitation of the organoid models is the absence of vascularization and, therefore, the impossibility to study interactions between the viruses and cells of the immune system [28].
To overcome this limitation, more complex in vitro multicellular cultures have been developed. Today, the respiratory organ-on-a-chip technology represents the in vitro system with the highest structural and functional complexity. In addition to the 3D culture of lung cells under ALI, it includes vascular structures, allowing perfusion of drugs and immune cells under controlled shear, and it can be subjected to mechanical strain to mimic the respiratory cycle. This technology has been successfully applied to studies on COVID-19 [14,29], leading to significant advances in our knowledge of viral pneumonia and its treatment.
The main goal of the present work is to provide an updated review of the organoid and the organs-on-chip technologies, focusing on COVID-19 research. Challenges and improvements of these systems will be also discussed.
2. Lung 3D Cultures
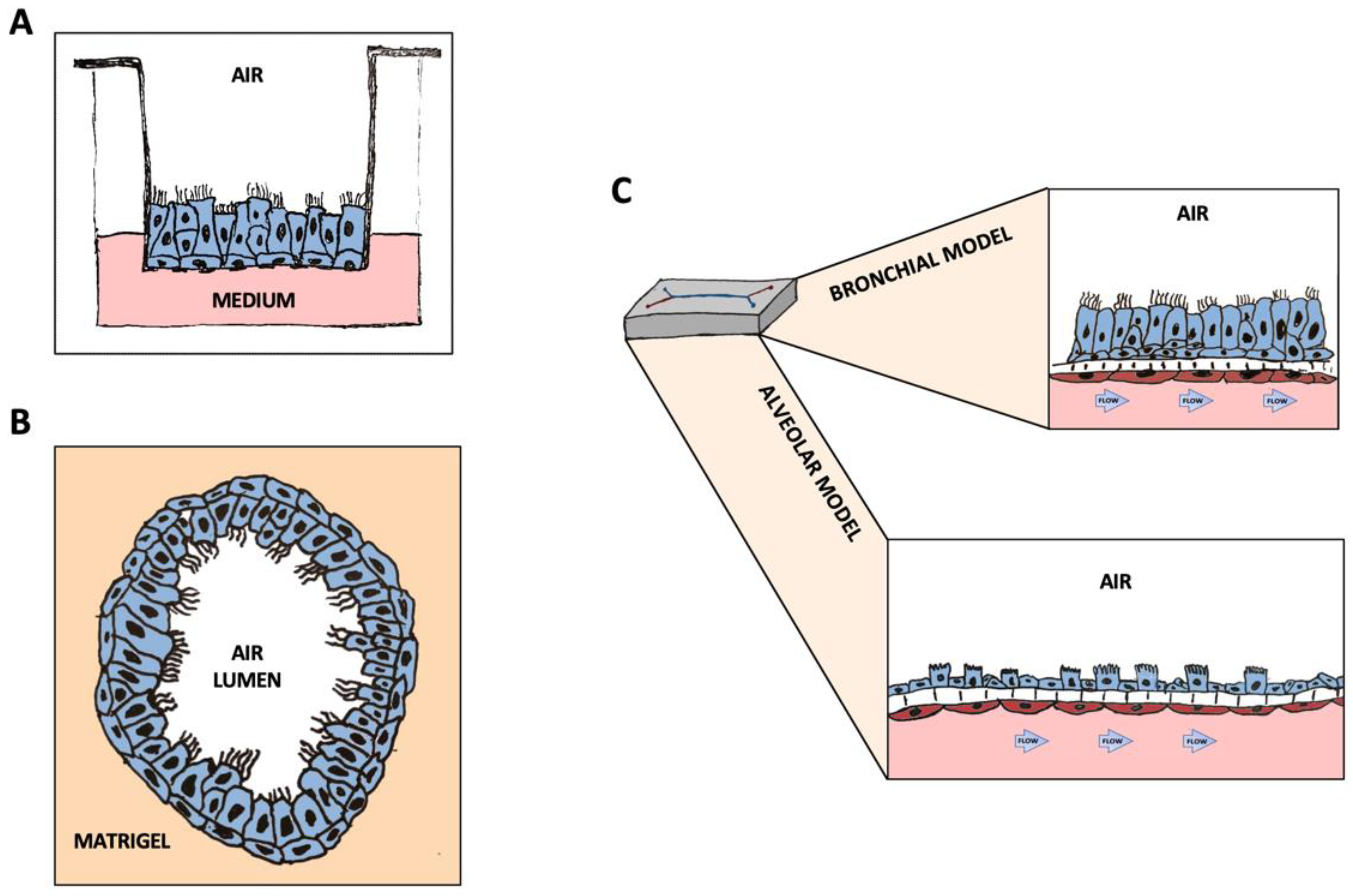
The advent of porous membrane supports, such as transwells, has enabled the development of ALI cultures that reproduce in vitro with high fidelity the structure of the airway epithelium (Figure 1A). Indeed, all cell types found in the human airway in vivo, including ciliated, goblet, basal and club cells, as well as ionocytes can be observed in these cultures [20,21,22]. In addition, transwell cultures allow the investigation of the interactions among cell and tissue types, pathogens and the immune system [30,31,32]. These models have been extensively exploited to study CF, chronic obstructive pulmonary disease (COPD) and airway infections by bacterial and viral pathogens [33,34,35,36].
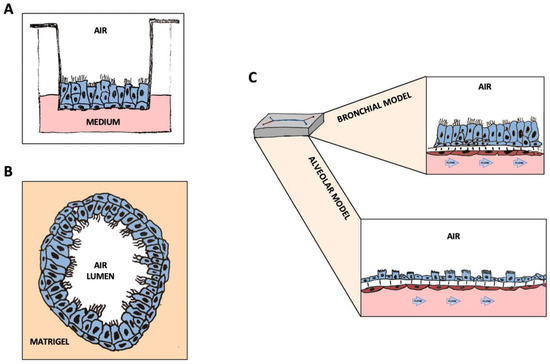
Figure 1.
Graphic representation of the 3D structures discussed in this manuscript: (A) Airway Epithelial cells in ALI culture on transwells. (B) Airway organoids composed of all cell types, differentiated and oriented towards the inner lumen. (C) Differentiated lung-airway (top) and lung-alveolus (bottom) chips. The differentiated Airway-on-a-Chip is composed of ciliate, basal, goblet and club cells in the top channel, interfaced with pulmonary microvascular endothelial cells perfused using a microfluidic device. The differentiated alveolus chip is composed of ~45% type II and ~55% type I lung alveolar cells, forming together an in vitro surfactant-producing human alveolar structure.
Compared to transwell cultures of airway epithelial cells, the culture of primary alveolar epithelial cells is less explored, partly because of limited cell availability. Primary alveolar type II cells (ATII) can only be cultured under 2D conditions for a limited period (3–7 days) before differentiation into alveolar type I (ATI)-like cells [37]. In addition, unlike airway epithelial cells, a consistent method to passage and expand primary ATII cells under 2D conditions has not yet been established. A few studies have investigated the culture of alveolar epithelial cell lines (such as A549 and NCI-H441) or inducible pluripotent stem cells (iPSC)-derived ATII cells under ALI, showing increased cell polarization, barrier formation, ion transport, and cell maturation [38,39,40]. However, none of these models supports both the maintenance of the ATII phenotype and the differentiation into ATI cells. Other efforts by coculturing alveolar epithelial cells with other cell types present in the lung alveolus, such as fibroblast and microvascular endothelial cells (MVEC), have obtained limited success [41,42,43]. Lung 3D cultures have also been used to study the immune response, monitored as cytokine production and lymph/monocyte, neutrophil migration [43,44].
Another 3D culture model that has attracted great interest in the field of lung biology and respiratory medicine is represented by lung organoids. These are 3D structures that can derive from pluripotent stem cells or adult stem cells undergoing spontaneous self-organization and differentiation in sphere structures with the apical side oriented toward the lumen or outward the medium [45,46,47] (Figure 1B). Organoids have been used to model the upper respiratory tract and even the distal alveoli in various lung diseases, including viral infections [48,49,50]. These 3D structures offer the advantage of allowing the study of the relationships between the epithelial tissue and the stromal component [51]. Furthermore, an organoid model that combines proximal and distal organoids, thus simulating in a certain way the crosstalk between the bronchi and the distal lungs has been recently developed [50,52]. Moreover, the inclusion of vascular networks by the incorporation of mesodermal progenitor cells has been recently described [53].
A further step towards the in vitro reconstitution of a human respiratory unit is represented by organ-on-chip technology. Ingber and his team pioneered the development of the lung-on-a-chip by growing lung epithelial cells and microvascular endothelial cells (MVEC) in two parallel microfluidic channels made of polydimethylsiloxane (PDMS), separated by a porous membrane [54,55]. Fluid shear stress and other mechanical forces, such as lung rhythmic breathing motions, can be introduced. Moreover, immune cells can be perfused through the vascular channel [29,56] (Figure 1C). This model has been optimized and utilized for studies on respiratory diseases, including CF, COPD, and lung infections [14,29,57,58]. Additional respiratory organ-on-chips with slightly different structures have been built by other groups. These are based on varying microfluidics platforms, mostly in PDMS, and composed of one or more channels or supports where to grow cells for differentiation into mature tissues [59,60,61,62]. These chips have been used for modeling viral infections and lung cancer or for studies on nanoparticle toxicity/transport in the lungs [59,60,61,62].
3. Three-Dimensional Systems in COVID-19 Research
Since the beginning of the COVID-19 pandemic, 3D in vitro cultures including airway organoids, static 3D co-cultures and organs-on-chip have been used for mechanistic studies on SARS-CoV-2 infection, as well as for drug repurposing, and testing of novel antiviral therapeutics. Compared to animal models, these systems demonstrated a higher fidelity to human disease and a high prediction rate of drug efficacy [14,63].
3.1. Lung Organoids
Organoids have been a reference model during the fight against COVID-19. It has been reported that both airway and alveolar organoids can be successfully infected with influenza and SARS-CoV-2 viruses [64,65]. Primary cell-based organoids provided a useful system for understanding SARS-CoV-2 pathogenesis and identifying effective antiviral drugs. Indeed, several SARS-CoV-2 inhibitors have been identified using the organoid model. Han et al. reported the efficacy of imatinib, mycophenolic acid and quinacrine dihydrochloride, against SARS-CoV-2 in a human physiologically relevant setting [66]. The in vivo antiviral efficacy of these drugs has been explored and confirmed, leading to the conclusion that hPSC-organoids can be useful to study SARS-CoV-2 infection and provide a valuable model for the identification of anti-COVID-19 molecules. This work and other studies have led to clinical trials to evaluate the efficacy of imatinib against COVID-19 [67]. Another study by Sano et al. [68] describes the anti-SARS-CoV-2 efficacy of camostat, remdesivir and EIDD-2801 in bronchial organoids. The organoid models also allowed the study of airway regeneration after SARS-CoV-2 infection by monitoring the replacement of ciliated cells destroyed by the virus with new ciliated cells differentiated from basal cells [68]. Of note, remdesivir is currently administered to patients with COVID-19. Spitalieri et al. [69] developed 3D complex lung organoid structures (hLORGs) starting from human iPSCs. Using the hiPSC-derived hLORGs, they identified two immunotherapeutic candidates for COVID-19 treatment, a tetravalent neutralizing antibody (15033-7) targeting the spike protein, and a synthetic peptide homologous to the dipeptidyl peptidase-4 (DPP4) receptor on host cells. Both Ab15033-7 and DPP4 significantly inhibited infection by SARS-CoV-2 S pseudovirus in hLORGs. Although the efficacy of these molecules against native SARS-CoV-2 needs further exploration, this study demonstrates that hiPSC-derived hLORGs could provide an alternative system for testing therapeutics against COVID-19. Tindle et al. [50] created adult lung organoids (ALOs) that are composed of both proximal airway and distal alveolar epithelium for modeling the SARS-CoV-2 infection and associated host immune responses. They demonstrated that the ALO model of the SARS-CoV-2 infection better recapitulates the transcriptomic signatures of respiratory samples from diverse cohorts of COVID-19 patients, compared with other existing SARS-CoV-2-infected lung models, due to the fact that this model contains both proximal and distal alveolar signatures. In this respect, this model could serve as a preclinical screening system for the identification of drugs that target both local and immune responses. Along these lines, Lamers et al. [49] described a human 2D ALI culture system wherein alveolar, basal and rare neuroendocrine cells are derived from 3D self-renewing fetal lung bud tip organoids. They showed that SARS-CoV-2 can readily infect these cultures mainly targeting surfactant protein C-positive alveolar type II-like cells and that it can be inhibited by a low dose of interferon lambda 1. Distal lungs were also successfully infected by SARS-CoV-2, indicating that this model can be useful to study alveolar pathogenetic processes. On the other hand, Salahudeen et al. [48] developed a long-term feeder-free culture system of human distal lung organoids derived from single adult human alveolar epithelial type II (AT2) or KRT5+ basal cells. They demonstrated that the organoids enabled the analysis of SARS-CoV-2 infection of the distal lung and revealed that SCGB1A1+ club cells are targeted by SARS-CoV-2.
3.2. Three-Dimensional Cultures on Transwells
ALI cultures provide a more physiologically relevant environment compared to conventional 2D cell cultures. The main advantage of epithelial ALI cultures is the possibility to deliver viral particles through the airway route, thus allowing viral replication and transmission at the apical sides of the lung epithelium. Thanks to these research tools, the main mechanisms of SARS-CoV-2 viral entry, which involve the binding of the receptor binding domain (RBD) of the SARS-CoV-2 spike protein to ACE2, were identified soon after the onset of the pandemic. Zhang et al. developed recombinant human ACE2-Fc fusion protein (hACE2-Fc) and constructed an ALI model, consisting of lung epithelial cells, obtained by fiberoptic bronchoscopy and brushing of the airway walls, grown in ALI using transwells [70]. These investigators demonstrated that hACE2-Fc potently neutralized the SARS-CoV-2 virus as efficiently as neutralizing antibodies. Along these lines, Djidrovski et al. [71] obtained basal-like cells by differentiating iPSCs and used these cells to generate airway epithelial equivalents by ALI culture. They seeded the basal airway-like cells onto the apical side of 24-well plate cell culture inserts with a transparent membrane and fed them from the basal chamber to induce differentiation. The differentiated cell types included functional ciliated cells, capable of secreting mucus, which were readily infected by SARS-CoV-2. The infected cells secreted cytokines at levels comparable to those detected in the airway epithelium in vivo following SARS-CoV-2 infection. In another study, two models were constructed: ALI cultures of proximal airway epithelium and alveolarsphere of distal lung AT2 cells [52]. The distal lung epithelial cells were mixed with human lung fibroblast cells and resuspended in Matrigel. Both models were susceptible to SARS-CoV-2 infection, resulting in an autonomous pro-inflammatory response. Remdesivir strongly inhibited SARS-CoV-2 infection and/or replication in both models. However, a limitation of these constructs is the lack of immune and endothelial components. Notably, SARS-CoV-2 clinical isolates infected a 3D human respiratory epithelial cell model, which was developed using primary respiratory epithelial cells differentiated on transwells at ALI, with the highest expression of SARS-CoV-2 viral RNA at 24 h post infection. Interestingly, two long noncoding RNAs, LAS1 and TOSL were upregulated in both nasal swabs from COVID-19 patients and this 3D culture model [72], suggesting that these innate immune modulators may play a role in SARS-CoV-2-induced innate airway mucosal responses.
3.3. The Organ-on-a-Chip Technology
Dynamic models such as Lung-on-a-Chip have several advantages over static 3D models. First, some of them allow the application of mechanical forces that simulate alveolar contraction and expansion, which is crucial for the activation of innate immunity [29]. Furthermore, the possibility of perfusing leukocytes through the vascular channel allows the analysis of the anti-viral immune response [73]. A recent work used this model to monitor influenza virus evolution during multiple serial passages, identifying relevant clinical mutations and allowing the resistance to antiviral drugs to be studied [74]. Si et al. exploited the Airway-on-a-Chip, built with human-differentiated ciliated bronchial epithelium and lined with microvascular endothelial, to study SARS-COV-2 and the influenza virus infection as well as the neutrophilic responses to viral infection [14]. The use of Airway-on-a-Chip also demonstrated the ineffectiveness of hydroxychloroquine and chloroquine, contrary to what was seen in vitro [75], but consistent with the observations in non-human primates [76] and data from clinical trials [77,78,79]. In addition, Si et al. [14] revealed that clinically relevant doses of amodiaquine inhibited infection of human airway chips by pseudotyped SARS-CoV-2. The differences between amodiaquine and the other related antimalarial drugs, hydroxychloroquine and chloroquine, could be partially explained by their effects on the proteome of airway epithelial cells. In fact, quantitative proteomics analysis revealed that amodiaquine has different and broader effects on the host proteome, especially in relation to the proteins involved in the regulation of ciliary functions, compared with hydroxychloroquine and chloroquine. The in vivo prophylactic and therapeutic efficacies of amodiaquine were validated in hamsters challenged with native SARS-CoV-2. Artesunate-amodiaquine is being tested in a clinical trial for the treatment of COVID-19 in Africa [80].
The organ-on-chip has been used by several groups to study the response to SARS-CoV-2 infection in the distal lungs [29,81,82]. Epithelial cells are not the only cell types attacked by SARS-CoV-2. Indeed, microvascular thrombi and endotheliitis were found in lungs of patients who had died from COVID-19 [83,84,85,86]. Moreover, lung microvascular endothelial cells (LMVEC) express high levels of NRP1 [10], an alternative receptor for SARS-CoV-2 entry [13]. Thacker et al. [81] used the Lung-on-a-Chip model to study SARS-CoV-2 infection and its effects on endothelial cells (EC). They observed damage to the endothelial barrier integrity, confirming the pro-coagulant effects of SARS-CoV-2 observed in animal models and autoptic evidence from human subjects. Of note, ACE2 expression increased by ~10-fold in LMVEC on-chip co-culture conditions under shear stress, highlighting the relevance of a physiological microenvironment to studying viral infection, thus confirming on chip the alveolar-capillary injury during SARS-CoV-2 infection observed in a co-culture transwell model [30]. Finally, Bai et al. [29] examined tissue-level host responses of a human alveolus chip, including barrier injury, ATII cell death, tissue regeneration, and recruitment of B and T lymphocytes and monocytes, following infection with respiratory viruses such as H3N2, H5N1 and coronaviruses. This study revealed a critical role of mechanical forces in shaping lung innate immunity and identified the receptor for the glycation end product (RAGE) pathway as a major drive during mechanotransduction, in addition to being an amplifier of aberrant host responses in viral pneumonia. The antiviral properties of the RAGE inhibitor azeliragon and its synergist effect with molnupiravir were also uncovered by this study. A summary of the main findings obtained with these models is reported in Table 1.

Table 1.
Summary of 2D/3D in vitro cultures in COVID-19 research.
4. Discussion
In this review, we summarize the current knowledge on the use of respiratory 3D cultures, namely, organoids and organs-on-chips, for studies on the pathophysiology and pharmacology of viral infections. This field of investigation has become dramatically relevant with the outburst of the COVID-19 pandemic that has so far affected more than half a billion people causing almost six and half million deaths. A significant number of studies have consistently demonstrated that organoids and organs-on-chip constitute a more reliable system to model human respiratory viral infections, better than traditional 2D cell cultures. These 3D lung tissue models, whose characteristics are illustrated in Table 2, faithfully recapitulate human pathophysiology and host responses to the SARS-CoV-2 infection, each providing valuable information for the development of better treatment options against the COVID-19 pandemic, especially when the limitations of the available animal models are evident.

Table 2.
Comparison of the available in vitro lung models to study SARS-CoV-2 infection.
Indeed, mice, ferrets, hamsters and macaques [87,88,89] have been used as preclinical models of SARS-Co-2 infection; however, these models and even non-human primates often do not fully recapitulate the human disease, due to species-specific differences in receptors distribution, protease expression and host immune responses [18,19]. Thus, 3D cultures have been instrumental for the study of interactions among pathogens, tissues and the immune system, representing a significant step forward in in vitro studies of respiratory infections. Data from different groups, using different models have consistently confirmed that the more complex 3D cultures, namely, organoid and organ chips, have greatly expanded our toolbox to study virology in vitro and helped understand processes, such as viral entry, replication, and host innate and adaptive immunity, thus enabling the identification of more effective therapeutic targets and drugs [14,29]. In the specific case of COVID-19, the Lung and Airway-on-a-chip has provided a reliable platform to study how SARS-CoV-2 infects human cells and triggers the complex host-virus interplay and the immune system [14,29].
Studies with this model have proven clinical relevance. In fact, amodiaquine, which emerged as an effective anti-SARS-CoV-2 agent in the Lung-on-a-chip [14], has been approved for clinical trial [80], likewise, remdesivir [68], which is currently used to treat patients with COVID-19. Thus, the high predictive power of drug efficacy represents a strong indication for the use of the Airway and Lung-on-a-chip in preclinical studies.
However, these chips are not the only ones used for research on viral diseases. Given that COVID-19, as well as other coronaviruses, can affect several organs, including kidneys, and the gastrointestinal, cardiovascular and nervous systems [90,91,92,93], 3D models of other organs have been used. Bein et al. [94] recently modeled an immunocompetent human Intestine-on-a-Chip to study enteric NL63 coronavirus infection and treatment, whereas Helms et al. [95], using kidney organoids derived from pluripotent stem cells, showed that SARS-CoV-2 can directly infect and damage kidney tubular epithelial cells. They also demonstrated that kidney organoids can be used for drug testing.
In conclusion, even though a definitive cure for SARS-CoV-2 has not yet been discovered, 3D tissue models, such as lung organoids and lung-on-a-chip, have been extraordinarily useful in combating the COVID-19 pandemic by providing a vast amount of data on key clinical and therapeutic aspects of this disease. However, there are some limitations of this technology that need to be considered. Working with advanced cultures such as organoids or organ-chips requires extreme accuracy, particularly during the phase of cell differentiation and tissue assembly. Therefore, to obtain reliable results, an adequate number of replicates should be planned. On the other hand, primary cells are not always available, and, therefore, particularly in the perspective of personalized medicine, the use of iPSC-derived cells should be considered. Another limitation, particularly in the case of organ-on-chip technology, is the low yield of materials for conventional biological assays, such as Western blot or flow cytometry. This, however, can be circumvented by combining multiple chips or using high-throughput assay technologies, such as total RNA or single-cell sequencing [96,97].
5. Future Directions
Despite the indisputable utility of the current 3D models, the possibility of building more complex systems that include all tissue and immune components of an airway functional unit and to interconnect this unit with chips of other organs, affected by the same disease, remains a fascinating perspective. For instance, the current 3D technologies related to the respiratory system could be implemented by including fibroblasts and alveolar macrophages to study the inflammatory immune response. Moreover, the 3D culture can be maintained only for a few weeks. Thus, extending the culture duration will allow the study of chronic processes associated with viral infections, for example, lung fibrosis or the role of memory B- or T-cell responses, a crucial aspect in the field of virology [98].
Author Contributions
R.P., L.S. and H.B. conceived the manuscript. J.L. and C.Z. contributed to including significant sections in the main body of the manuscript. M.R. thoroughly revised the manuscript. R.P. coordinated the work from all contributors. All authors contributed to the final version of this review. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by funds from the Italian Ministry of the University and Research (ex 60% 2021 and 2022) to R.P.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- Ng, W.H.; Tipih, T.; Makoah, N.A.; Vermeulen, J.G.; Goedhals, D.; Sempa, J.B.; Burt, F.J.; Taylor, A.; Mahalingam, S. Comorbidities in SARS-CoV-2 Patients: A Systematic Review and Meta-Analysis. mBio 2021, 12, e03647-20. [Google Scholar] [CrossRef] [PubMed]
- Polack, F.P.; Thomas, S.J.; Kitchin, N.; Absalon, J.; Gurtman, A.; Lockhart, S.; Perez, J.L.; Perez Marc, G.; Moreira, E.D.; Zerbini, C.; et al. Safety and Efficacy of the BNT162b2 mRNA Covid-19 Vaccine. N. Engl. J. Med. 2020, 383, 2603–2615. [Google Scholar] [CrossRef] [PubMed]
- Baden, L.R.; El Sahly, H.M.; Essink, B.; Kotloff, K.; Frey, S.; Novak, R.; Diemert, D.; Spector, S.A.; Rouphael, N.; Creech, C.B.; et al. Efficacy and Safety of the mRNA-1273 SARS-CoV-2 Vaccine. N. Engl. J. Med. 2021, 384, 403–416. [Google Scholar] [CrossRef]
- Sadoff, J.C.; le Gars, M.; Shukarev, G.; Heerwegh, D.; Truyers, C.; de Groot, A.M.; Stoop, J.N.; Tete, S.M.; Van Damme, W.; Leroux-Roels, I.; et al. Interim Results of a Phase 1–2a Trial of Ad26.COV2.S Covid-19 Vaccine. N. Engl. J. Med. 2021, 384, 1824–1835. [Google Scholar] [CrossRef]
- Heath, P.T.; Galiza, E.P.; Baxter, D.N.; Boffito, M.; Browne, D.; Burns, F.; Chadwick, D.R.; Clark, R.; Cosgrove, C.; Galloway, J.; et al. Safety and Efficacy of NVX-CoV2373 Covid-19 Vaccine. N. Engl. J. Med. 2021, 385, 1172–1183. [Google Scholar] [CrossRef] [PubMed]
- Voysey, M.; Clemens, S.A.C.; Madhi, S.A.; Weckx, L.Y.; Folegatti, P.M.; Aley, P.K.; Angus, B.; Baillie, V.L.; Barnabas, S.L.; Bhorat, Q.E.; et al. Safety and efficacy of the ChAdOx1 nCoV-19 vaccine (AZD1222) against SARS-CoV-2: An interim analysis of four randomised controlled trials in Brazil, South Africa, and the UK. Lancet 2021, 397, 99–111. [Google Scholar] [CrossRef]
- WHO Solidarity Trial Consortium. Remdesivir and three other drugs for hospitalised patients with COVID-19: Final results of the WHO Solidarity randomised trial and updated meta-analyses. Lancet 2022, 399, 1941–1953. [Google Scholar]
- Williamson, B.N.; Feldmann, F.; Schwarz, B.; Meade-White, K.; Porter, D.P.; Schulz, J.; van Doremalen, N.; Leighton, I.; Yinda, C.K.; Perez-Perez, L.; et al. Clinical benefit of remdesivir in rhesus macaques infected with SARS-CoV-2. Nature 2020, 585, 273–276. [Google Scholar] [CrossRef]
- Takayama, K. In Vitro and Animal Models for SARS-CoV-2 research. Trends Pharmacol. Sci. 2020, 41, 513–517. [Google Scholar] [CrossRef]
- Cantuti-Castelvetri, L.; Ojha, R.; Pedro, L.D.; Djannatian, M.; Franz, J.; Kuivanen, S.; van der Meer, F.; Kallio, K.; Kaya, T.; Anastasina, M.; et al. Neuropilin-1 facilitates SARS-CoV-2 cell entry and infectivity. Science 2020, 370, 856–860. [Google Scholar] [CrossRef]
- Hoffmann, M.; Kleine-Weber, H.; Schroeder, S.; Krüger, N.; Herrler, T.; Erichsen, S.; Schiergens, T.S.; Herrler, G.; Wu, N.H.; Nitsche, A.; et al. SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor. Cell 2020, 181, 271–280.e8. [Google Scholar] [CrossRef] [PubMed]
- Lukassen, S.; Chua, R.L.; Trefzer, T.; Kahn, N.C.; Schneider, M.A.; Muley, T.; Winter, H.; Meister, M.; Veith, C.; Boots, A.W.; et al. SARS-CoV-2 receptor ACE2 and TMPRSS2 are primarily expressed in bronchial transient secretory cells. EMBO J. 2020, 39, e105114. [Google Scholar] [CrossRef] [PubMed]
- Daly, J.L.; Simonetti, B.; Klein, K.; Chen, K.-E.; Williamson, M.K.; Antón-Plágaro, C.; Shoemark, D.K.; Simón-Gracia, L.; Bauer, M.; Hollandi, R.; et al. Neuropilin-1 is a host factor for SARS-CoV-2 infection. Science 2020, 370, 861–865. [Google Scholar] [CrossRef] [PubMed]
- Si, L.; Bai, H.; Rodas, M.; Cao, W.; Oh, C.Y.; Jiang, A.; Moller, R.; Hoagland, D.; Oishi, K.; Horiuchi, S.; et al. A human-airway-on-a-chip for the rapid identification of candidate antiviral therapeutics and prophylactics. Nat. Biomed. Eng. 2021, 5, 815–829. [Google Scholar] [CrossRef]
- Wang, M.; Cao, R.; Zhang, L.; Yang, X.; Liu, J.; Xu, M.; Shi, Z.; Hu, Z.; Zhong, W.; Xiao, G. Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-nCoV) in vitro. Cell Res. 2020, 30, 269–271. [Google Scholar] [CrossRef]
- Liu, J.; Cao, R.; Xu, M.; Wang, X.; Zhang, H.; Hu, H.; Li, Y.; Hú, Z.; Zhong, W.; Wang, M. Hydroxychloroquine, a less toxic derivative of chloroquine, is effective in inhibiting SARS-CoV-2 infection in vitro. Cell Discov. 2020, 6, 16. [Google Scholar] [CrossRef]
- Hoffmann, M.; Mösbauer, K.; Hofmann-Winkler, H.; Kaul, A.; Kleine-Weber, H.; Krüger, N.; Gassen, N.C.; Müller, M.A.; Drosten, C.; Pöhlmann, S. Chloroquine does not inhibit infection of human lung cells with SARS-CoV-2. Nature 2020, 585, 588–590. [Google Scholar] [CrossRef] [PubMed]
- Rockx, B.; Kuiken, T.; Herfst, S.; Bestebroer, T.M.; Lamers, M.M.; Oude Munnink, B.B.; de Meulder, D.; van Amerongen, G.; van den Brand, J.; Okba, N.M.A.; et al. Comparative pathogenesis of COVID-19, MERS, and SARS in a nonhuman primate model. Science 2020, 368, 1012–1015. [Google Scholar] [CrossRef] [PubMed]
- Muñoz-Fontela, C.; Dowling, W.E.; Funnell, S.G.P.; Gsell, P.-S.; Balta, X.R.; Albrecht, R.A.; Andersen, H.; Baric, R.S.; Carroll, M.W.; Cavaleri, M.; et al. Animal models for COVID-19. Nature 2020, 586, 509–515. [Google Scholar] [CrossRef] [PubMed]
- Fulcher, M.L.; Gabriel, S.E.; Burns, K.A.; Yankaskas, J.R.; Randell, S.H. Well-differentiated human airway epithelial cell cultures. Methods Mol. Med. 2005, 107, 183–206. [Google Scholar]
- Kesimer, M.; Kirkham, S.; Pickles, R.J.; Henderson, A.G.; Alexis, N.E.; Demaria, G.; Knight, D.; Thornton, D.J.; Sheehan, J.K. Tracheobronchial air-liquid interface cell culture: A model for innate mucosal defense of the upper airways? Am. J. Physiol. Lung Cell Mol. Physiol. 2009, 296, L92–L100. [Google Scholar] [CrossRef] [PubMed]
- Pezzulo, A.A.; Starner, T.D.; Scheetz, T.E.; Traver, G.L.; Tilley, A.E.; Harvey, B.G.; Crystal, R.G.; McCray, P.B., Jr.; Zabner, J. The air-liquid interface and use of primary cell cultures are important to recapitulate the transcriptional profile of in vivo airway epithelia. Am. J. Physiol. Lung Cell Mol. Physiol. 2011, 300, L25–L31. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van der Vaart, J.; Clevers, H. Airway organoids as models of human disease. J. Intern. Med. 2021, 289, 604–613. [Google Scholar] [CrossRef]
- Laselva, O.; Conese, M. Three-Dimensional Airway Spheroids and Organoids for Cystic Fibrosis Research. J. Respir. 2021, 1, 229–247. [Google Scholar] [CrossRef]
- Hui, K.P.Y.; Ching, R.H.H.; Chan, S.K.H.; Nicholls, J.M.; Sachs, N.; Clevers, H.; Peiris, J.S.M.; Chan, M.C.W. Tropism, replication competence, and innate immune responses of influenza virus: An analysis of human airway organoids and ex-vivo bronchus cultures. Lancet Respir. Med. 2018, 6, 846–854. [Google Scholar] [CrossRef]
- Sachs, N.; Papaspyropoulos, A.; Zomer-van Ommen, D.D.; Heo, I.; Bottinger, L.; Klay, D.; Weeber, F.; Huelsz-Prince, G.; Iakobachvili, N.; Amatngalim, G.D.; et al. Long-term expanding human airway organoids for disease modeling. EMBO J. 2019, 38, e100300. [Google Scholar] [CrossRef]
- Ramani, S.; Crawford, S.E.; Blutt, S.E.; Estes, M.K. Human organoid cultures: Transformative new tools for human virus studies. Curr. Opin. Virol. 2018, 29, 79–86. [Google Scholar] [CrossRef]
- Liberti, D.C.; Morrisey, E.E. Organoid models: Assessing lung cell fate decisions and disease responses. Trends Mol. Med. 2021, 27, 1159–1174. [Google Scholar] [CrossRef]
- Bai, H.; Si, L.; Jiang, A.; Belgur, C.; Zhai, Y.; Plebani, R.; Oh, C.Y.; Rodas, M.; Patil, A.; Nurani, A.; et al. Mechanical control of innate immune responses against viral infection revealed in a human lung alveolus chip. Nat. Commun. 2022, 13, 1928. [Google Scholar] [CrossRef]
- Wang, P.-j.; Luo, R.; Zhang, M.; Wang, Y.; Song, T.; Tao, T.; Li, Z.; Jin, L.; Zheng, H.W.; Chen, W.; et al. A cross-talk between epithelium and endothelium mediates human alveolar–capillary injury during SARS-CoV-2 infection. Cell Death Dis 2020, 11, 1042. [Google Scholar] [CrossRef]
- Deng, Y.; Herbert, J.A.; Smith, C.M.; Smyth, R.L. An in vitro transepithelial migration assay to evaluate the role of neutrophils in Respiratory Syncytial Virus (RSV) induced epithelial damage. Sci Rep. 2018, 8, 6777. [Google Scholar] [CrossRef] [PubMed]
- Hurley, B.P.; Siccardi, D.; Mrsny, R.J.; McCormick, B.A. Polymorphonuclear cell transmigration induced by Pseudomonas aeruginosa requires the eicosanoid hepoxilin A3. J. Immunol. 2004, 173, 5712–5720. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hedstrom, U.; Oberg, L.; Vaarala, O.; Dellgren, G.; Silverborn, M.; Bjermer, L.; Westergren-Thorsson, G.; Hallgren, O.; Zhou, X. Impaired Differentiation of Chronic Obstructive Pulmonary Disease Bronchial Epithelial Cells Grown on Bronchial Scaffolds. Am. J. Respir. Cell Mol. Biol. 2021, 65, 201–213. [Google Scholar] [CrossRef]
- Pedemonte, N.; Bertozzi, F.; Caci, E.; Sorana, F.; Di Fruscia, P.; Tomati, V.; Ferrera, L.; Rodriguez-Gimeno, A.; Berti, F.; Pesce, E.; et al. Discovery of a picomolar potency pharmacological corrector of the mutant CFTR chloride channel. Sci. Adv. 2020, 6, eaay9669. [Google Scholar] [CrossRef]
- Braccia, C.; Tomati, V.; Caci, E.; Pedemonte, N.; Armirotti, A. SWATH label-free proteomics for cystic fibrosis research. J. Cyst. Fibros. 2019, 18, 501–506. [Google Scholar] [CrossRef] [PubMed]
- Mazio, C.; Scognamiglio, L.S.; De Cegli, R.; Galietta, L.J.V.; Bernardo, D.D.; Casale, C.; Urciuolo, F.; Imparato, G.; Netti, P.A. Intrinsic Abnormalities of Cystic Fibrosis Airway Connective Tissue Revealed by an In Vitro 3D Stromal Model. Cells 2020, 9, 1371. [Google Scholar] [CrossRef]
- Hiemstra, P.S.; Tetley, T.D.; Janes, S.M. Airway and alveolar epithelial cells in culture. Eur. Respir. J. 2019, 54, 1900742. [Google Scholar] [CrossRef]
- Ren, H.; Birch, N.P.; Suresh, V. An Optimised Human Cell Culture Model for Alveolar Epithelial Transport. PLoS ONE 2016, 11, e0165225. [Google Scholar] [CrossRef]
- Brookes, O.; Boland, S.; Kuen, R.L.; Miremont, D.; Movassat, J.; Baeza-Squiban, A. Co-culture of type I and type II pneumocytes as a model of alveolar epithelium. PLoS ONE 2021, 16, e0248798. [Google Scholar] [CrossRef]
- Abo, K.M.; de Aja, J.S.; Lindstrom-Vautrin, J.; Alysandratos, K.-D.; Richards, A.L.; Garcia-de-Alba, C.; Huang, J.; Hix, O.T.; Werder, R.B.; Bullitt, E.; et al. Air-liquid interface culture promotes maturation and allows environmental exposure of pluripotent stem cell–derived alveolar epithelium. JCI Insight 2022, 7, e155589. [Google Scholar] [CrossRef]
- Wang, J.; Edeen, K.E.; Manzer, R.; Chang, Y.; Wang, S.; Chen, X.; Funk, C.J.; Cosgrove, G.P.; Fang, X.; Mason, R.; et al. Differentiated human alveolar epithelial cells and reversibility of their phenotype in vitro. Am. J. Respir Cell Mol. Biol. 2007, 36, 661–668. [Google Scholar] [CrossRef] [PubMed]
- Hermanns, M.I.; Unger, R.E.; Kehe, K.; Peters, K.; Kirkpatrick, C.J. Lung epithelial cell lines in coculture with human pulmonary microvascular endothelial cells: Development of an alveolo-capillary barrier in vitro. Lab. Investig. 2004, 84, 736–752. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Short, K.R.; Kasper, J.; van der Aa, S.; Andeweg, A.C.; Zaaraoui-Boutahar, F.; Goeijenbier, M.; Richard, M.; Herold, S.; Becker, C.; Scott, D.P.; et al. Influenza virus damages the alveolar barrier by disrupting epithelial cell tight junctions. Eur. Respir. J. 2016, 47, 954–966. [Google Scholar] [CrossRef] [PubMed]
- Miller, A.J.; Spence, J.R. In Vitro Models to Study Human Lung Development, Disease and Homeostasis. Physiology 2017, 32, 246–260. [Google Scholar] [CrossRef] [PubMed]
- Fatehullah, A.; Tan, S.H.; Barker, N. Organoids as an in vitro model of human development and disease. Nat. Cell Biol 2016, 18, 246–254. [Google Scholar] [CrossRef]
- Clevers, H. Modeling Development and Disease with Organoids. Cell 2016, 165, 1586–1597. [Google Scholar] [CrossRef]
- Boecking, C.A.; Walentek, P.; Zlock, L.T.; Sun, D.I.; Wolters, P.J.; Ishikawa, H.; Jin, B.J.; Haggie, P.M.; Marshall, W.F.; Verkman, A.S.; et al. A simple method to generate human airway epithelial organoids with externally orientated apical membranes. Am. J. Physiol. Lung Cell Mol. Physiol. 2022, 322, L420–L437. [Google Scholar] [CrossRef]
- Salahudeen, A.A.; Choi, S.S.; Rustagi, A.; Zhu, J.; van Unen, V.; de la, O.S.; Flynn, R.A.; Margalef-Catala, M.; Santos, A.J.M.; Ju, J.; et al. Progenitor identification and SARS-CoV-2 infection in human distal lung organoids. Nature 2020, 588, 670–675. [Google Scholar] [CrossRef]
- Lamers, M.M.; van der Vaart, J.; Knoops, K.; Riesebosch, S.; Breugem, T.I.; Mykytyn, A.Z.; Beumer, J.; Schipper, D.; Bezstarosti, K.; Koopman, C.D.; et al. An organoid-derived bronchioalveolar model for SARS-CoV-2 infection of human alveolar type II-like cells. EMBO J. 2021, 40, e105912. [Google Scholar] [CrossRef]
- Tindle, C.; Fuller, M.; Fonseca, A.; Taheri, S.; Ibeawuchi, S.R.; Beutler, N.; Katkar, G.D.; Claire, A.; Castillo, V.; Hernandez, M.; et al. Adult stem cell-derived complete lung organoid models emulate lung disease in COVID-19. eLife 2021, 10, e66417. [Google Scholar] [CrossRef]
- Chen, J.; Lau, B.T.; Andor, N.; Grimes, S.M.; Handy, C.; Wood-Bouwens, C.; Ji, H.P. Single-cell transcriptome analysis identifies distinct cell types and niche signaling in a primary gastric organoid model. Sci. Rep. 2019, 9, 4536. [Google Scholar] [CrossRef] [PubMed]
- Mulay, A.; Konda, B.; Garcia, G.; Yao, C.; Beil, S.; Sen, C.; Purkayastha, A.; Kolls, J.K.; Pociask, D.A.; Pessina, P.; et al. SARS-CoV-2 infection of primary human lung epithelium for COVID-19 modeling and drug discovery. bioRxiv 2020. [Google Scholar] [CrossRef] [PubMed]
- Wörsdörfer, P.; Dalda, N.; Kern, A.; Krüger, S.; Wagner, N.; Kwok, C.K.; Henke, E.; Ergün, S. Generation of complex human organoid models including vascular networks by incorporation of mesodermal progenitor cells. Sci. Rep. 2019, 9, 15663. [Google Scholar] [CrossRef] [PubMed]
- Huh, D.; Matthews, B.D.; Mammoto, A.; Montoya-Zavala, M.; Hsin, H.Y.; Ingber, D.E. Reconstituting organ-level lung functions on a chip. Science 2010, 328, 1662–1668. [Google Scholar] [CrossRef]
- Benam, K.H.; Villenave, R.; Lucchesi, C.; Varone, A.; Hubeau, C.; Lee, H.H.; Alves, S.E.; Salmon, M.; Ferrante, T.C.; Weaver, J.C.; et al. Small airway-on-a-chip enables analysis of human lung inflammation and drug responses in vitro. Nat. Methods 2016, 13, 151–157. [Google Scholar] [CrossRef]
- Huh, D.; Leslie, D.C.; Matthews, B.D.; Fraser, J.P.; Jurek, S.; Hamilton, G.A.; Thorneloe, K.S.; McAlexander, M.A.; Ingber, D.E. A human disease model of drug toxicity-induced pulmonary edema in a lung-on-a-chip microdevice. Sci. Transl. Med. 2012, 4, 159ra147. [Google Scholar] [CrossRef]
- Plebani, R.; Potla, R.; Soong, M.; Bai, H.; Izadifar, Z.; Jiang, A.; Travis, R.N.; Belgur, C.; Dinis, A.; Cartwright, M.J.; et al. Modeling pulmonary cystic fibrosis in a human lung airway-on-a-chip. J. Cyst. Fibros. 2022, 21, 606–615. [Google Scholar] [CrossRef]
- Bai, H.; Ingber, D.E. What can an organ-on-a-chip teach us about human lung physiology? Physiology 2022, 37, 242–252. [Google Scholar] [CrossRef]
- Zhang, M.; Xu, C.; Jiang, L.; Qin, J. A 3D human lung-on-a-chip model for nanotoxicity testing. Toxicol. Res. 2018, 7, 1048–1060. [Google Scholar] [CrossRef]
- Kwak, B.S.; Ozcelikkale, A.; Shin, C.S.; Park, K.; Han, B. Simulation of complex transport of nanoparticles around a tumor using tumor-microenvironment-on-chip. J. Control. Release 2014, 194, 157–167. [Google Scholar] [CrossRef]
- Albanese, A.; Lam, A.K.; Sykes, E.A.; Rocheleau, J.V.; Chan, W.C.W. Tumour-on-a-chip provides an optical window into nanoparticle tissue transport. Nat. Commun. 2013, 4, 2718. [Google Scholar] [CrossRef] [PubMed]
- Huang, D.; Liu, T.; Liao, J.; Maharjan, S.; Xie, X.; Perez, M.; Anaya, I.; Wang, S.; Tirado Mayer, A.; Kang, Z.; et al. Reversed-engineered human alveolar lung-on-a-chip model. Proc. Natl. Acad. Sci. USA 2021, 118, e2016146118. [Google Scholar] [CrossRef] [PubMed]
- Ingber, D.E. Human organs-on-chips for disease modelling, drug development and personalized medicine. Nat. Rev. Genet. 2022, 23, 467–491. [Google Scholar] [CrossRef] [PubMed]
- Ekanger, C.T.; Zhou, F.; Bohan, D.; Lotsberg, M.L.; Ramnefjell, M.; Hoareau, L.; Rosland, G.V.; Lu, N.; Aanerud, M.; Gartner, F.; et al. Human Organotypic Airway and Lung Organoid Cells of Bronchiolar and Alveolar Differentiation Are Permissive to Infection by Influenza and SARS-CoV-2 Respiratory Virus. Front. Cell. Infect. Microbiol. 2022, 12, 841447. [Google Scholar] [CrossRef]
- Han, Y.; Yang, L.; Lacko, L.A.; Chen, S. Human organoid models to study SARS-CoV-2 infection. Nat. Methods 2022, 19, 418–428. [Google Scholar] [CrossRef]
- Han, Y.; Duan, X.; Yang, L.; Nilsson-Payant, B.E.; Wang, P.; Duan, F.; Tang, X.; Yaron, T.M.; Zhang, T.; Uhl, S.; et al. Identification of SARS-CoV-2 Inhibitors using Lung and Colonic Organoids. Nature 2020, 589, 270–275. [Google Scholar] [CrossRef]
- Aman, J.; Duijvelaar, E.; Botros, L.; Kianzad, A.; Schippers, J.R.; Smeele, P.J.; Azhang, S.; Bartelink, I.H.; Bayoumy, A.A.; Bet, P.M.; et al. Imatinib in patients with severe COVID-19: A randomised, double-blind, placebo-controlled, clinical trial. Lancet Respir. Med. 2021, 9, 957–968. [Google Scholar] [CrossRef]
- Sano, E.; Suzuki, T.; Hashimoto, R.; Itoh, Y.; Sakamoto, A.; Sakai, Y.; Saito, A.; Okuzaki, D.; Motooka, D.; Muramoto, Y.; et al. Cell response analysis in SARS-CoV-2 infected bronchial organoids. Commun. Biol. 2022, 5, 516. [Google Scholar] [CrossRef]
- Spitalieri, P.; Centofanti, F.; Murdocca, M.; Scioli, M.G.; Latini, A.; Di Cesare, S.; Citro, G.; Rossi, A.; Orlandi, A.; Miersch, S.; et al. Two Different Therapeutic Approaches for SARS-CoV-2 in hiPSCs-Derived Lung Organoids. Cells 2022, 11, 1235. [Google Scholar] [CrossRef]
- Zhang, Z.; Zeng, E.; Zhang, L.; Wang, W.; Jin, Y.; Sun, J.; Huang, S.; Yin, W.; Dai, J.; Zhuang, Z.; et al. Potent prophylactic and therapeutic efficacy of recombinant human ACE2-Fc against SARS-CoV-2 infection in vivo. Cell Discov. 2021, 7, 65. [Google Scholar] [CrossRef]
- Djidrovski, I.; Georgiou, M.; Hughes, G.L.; Patterson, E.I.; Casas-Sanchez, A.; Pennington, S.H.; Biagini, G.A.; Moya-Molina, M.; van den Bor, J.; Smit, M.J.; et al. SARS-CoV-2 infects an upper airway model derived from induced pluripotent stem cells. Stem Cells 2021, 39, 1310–1321. [Google Scholar] [CrossRef] [PubMed]
- Devadoss, D.; Acharya, A.; Manevski, M.; Pandey, K.; Thurman, M.; Nair, M.; Borchert, G.M.; Mirsaeidi, M.; Byrareddy, S.N.; Chand, H.S. Severe COVID19 Patients and a 3D Airway Tissue Model of SARS-CoV-2 Infection Express High Levels of Airway Mucins and Associated Immunomodulatory Long Noncoding RNAs. Am. J. Respir. Crit. Care Med. 2021, 203, A4183. [Google Scholar]
- Di Domizio, J.; Gulen, M.F.; Saidoune, F.; Thacker, V.V.; Yatim, A.; Sharma, K.; Nass, T.; Guenova, E.; Schaller, M.; Conrad, C.; et al. The cGAS–STING pathway drives type I IFN immunopathology in COVID-19. Nature 2022, 603, 145–151. [Google Scholar] [CrossRef]
- Si, L.; Bai, H.; Oh, C.Y.; Jin, L.; Prantil-Baun, R.; Ingber, D.E. Clinically Relevant Influenza Virus Evolution Reconstituted in a Human Lung Airway-on-a-Chip. Microbiol. Spectr. 2021, 9, e0025721. [Google Scholar] [CrossRef] [PubMed]
- Touret, F.; Gilles, M.; Barral, K.; Nougairede, A.; van Helden, J.; Decroly, E.; de Lamballerie, X.; Coutard, B. In vitro screening of a FDA approved chemical library reveals potential inhibitors of SARS-CoV-2 replication. Sci. Rep. 2020, 10, 13093. [Google Scholar] [CrossRef]
- Maisonnasse, P.; Guedj, J.; Contreras, V.; Behillil, S.; Solas, C.; Marlin, R.; Naninck, T.; Pizzorno, A.; Lemaitre, J.; Gonçalves, A.; et al. Hydroxychloroquine use against SARS-CoV-2 infection in non-human primates. Nature 2020, 585, 584–587. [Google Scholar] [CrossRef]
- Reis, G.; Moreira Silva, E.A.D.S.; Medeiros Silva, D.C.; Thabane, L.; Singh, G.; Park, J.J.H.; Forrest, J.I.; Harari, O.; Quirino dos Santos, C.V.; Guimarães de Almeida, A.P.F.; et al. Effect of Early Treatment With Hydroxychloroquine or Lopinavir and Ritonavir on Risk of Hospitalization Among Patients With COVID-19. JAMA Netw. Open 2021, 4, e216468. [Google Scholar] [CrossRef]
- Avezum, Á.; Oliveira, G.B.D.F.; Oliveira, H.; Lucchetta, R.C.; Pereira, V.F.A.; Dabarian, A.L.; D´O Vieira, R.; Silva, D.V.; Kormann, A.P.M.; Tognon, A.P.; et al. Hydroxychloroquine versus placebo in the treatment of non-hospitalised patients with COVID-19 (COPE—Coalition V): A double-blind, multicentre, randomised, controlled trial. Lancet Reg. Health-Am. 2022, 11, 100243. [Google Scholar] [CrossRef]
- Rebeaud, M.E.; Zorès, F. SARS-CoV-2 and the Use of Chloroquine as an Antiviral Treatment. Front. Med. 2020, 7, 184. [Google Scholar] [CrossRef]
- Shin Poong Pharmaceutical Co., Ltd.; Medicines for Malaria Venture. COVID-19 Treatment in South Africa. 2021. Available online: https://clinicaltrials.gov/ct2/results?pg=1&load=cart&id=NCT04532931 (accessed on 15 August 2022).
- Thacker, V.V.; Sharma, K.; Dhar, N.; Mancini, G.F.; Sordet-Dessimoz, J.; McKinney, J.D. Rapid endotheliitis and vascular damage characterize SARS-CoV-2 infection in a human lung-on-chip model. EMBO Rep. 2021, 22, e52744. [Google Scholar] [CrossRef]
- Wang, Y.; Wang, P.; Qin, J. Microfluidic Organs-on-a-Chip for Modeling Human Infectious Diseases. Acc. Chem. Res. 2021, 54, 3550–3562. [Google Scholar] [CrossRef] [PubMed]
- Ackermann, M.; Verleden, S.E.; Kuehnel, M.; Haverich, A.; Welte, T.; Laenger, F.; Vanstapel, A.; Werlein, C.; Stark, H.; Tzankov, A.; et al. Pulmonary Vascular Endothelialitis, Thrombosis, and Angiogenesis in Covid-19. N. Engl. J. Med. 2020, 383, 120–128. [Google Scholar] [CrossRef] [PubMed]
- Carsana, L.; Sonzogni, A.; Nasr, A.; Rossi, R.S.; Pellegrinelli, A.; Zerbi, P.; Rech, R.; Colombo, R.; Antinori, S.; Corbellino, M.; et al. Pulmonary post-mortem findings in a series of COVID-19 cases from northern Italy: A two-centre descriptive study. Lancet Infect. Dis. 2020, 20, 1135–1140. [Google Scholar] [CrossRef]
- Calabretta, E.; Moraleda, J.M.; Iacobelli, M.; Jara, R.; Vlodavsky, I.; O’Gorman, P.; Pagliuca, A.; Mo, C.C.; Baron, R.M.; Aghemo, A.; et al. COVID-19-induced endotheliitis: Emerging evidence and possible therapeutic strategies. Br. J. Haematol. 2021, 193, 43–51. [Google Scholar] [CrossRef]
- Varga, Z.; Flammer, A.J.; Steiger, P.; Haberecker, M.; Andermatt, R.; Zinkernagel, A.S.; Mehra, M.R.; Schuepbach, R.A.; Ruschitzka, F.; Moch, H.J.L. Endothelial cell infection and endotheliitis in COVID-19. Lancet 2020, 395, 1417–1418. [Google Scholar] [CrossRef]
- Kim, Y.I.; Kim, S.G.; Kim, S.M.; Kim, E.H.; Park, S.J.; Yu, K.M.; Chang, J.H.; Kim, E.J.; Lee, S.; Casel, M.A.B.; et al. Infection and Rapid Transmission of SARS-CoV-2 in Ferrets. Cell Host Microbe 2020, 27, 704–709.e2. [Google Scholar] [CrossRef]
- Chan, J.F.; Zhang, A.J.; Yuan, S.; Poon, V.K.; Chan, C.C.; Lee, A.C.; Chan, W.M.; Fan, Z.; Tsoi, H.W.; Wen, L.; et al. Simulation of the Clinical and Pathological Manifestations of Coronavirus Disease 2019 (COVID-19) in a Golden Syrian Hamster Model: Implications for Disease Pathogenesis and Transmissibility. Clin. Infect. Dis. 2020, 71, 2428–2446. [Google Scholar] [CrossRef]
- Bao, L.; Deng, W.; Gao, H.; Xiao, C.; Liu, J.; Xue, J.; Lv, Q.; Liu, J.; Yu, P.; Xu, Y.; et al. Reinfection could not occur in SARS-CoV-2 infected rhesus macaques. bioRxiv 2020. [Google Scholar] [CrossRef]
- Wu, X.; Jing, H.; Wang, C.; Wang, Y.; Zuo, N.; Jiang, T.; Novakovic, V.A.; Shi, J. Intestinal Damage in COVID-19: SARS-CoV-2 Infection and Intestinal Thrombosis. Front. Microbiol. 2022, 13, 860931. [Google Scholar] [CrossRef]
- Gabarre, P.; Dumas, G.; Dupont, T.; Darmon, M.; Azoulay, E.; Zafrani, L. Acute Kidney Injury in Critically Ill Patients with COVID-19. Intensive Care Med. 2020, 46, 1339–1348. [Google Scholar] [CrossRef]
- Keyhanian, K.; Umeton, R.P.; Mohit, B.; Davoudi, V.; Hajighasemi, F.; Ghasemi, M. SARS-CoV-2 and Nervous System: From Pathogenesis to Clinical Manifestation. J. Neuroimmunol. 2020, 350, 577436. [Google Scholar] [CrossRef] [PubMed]
- Koźlik, M.; Błahuszewska, A.; Kaźmierski, M. Cardiovascular System during SARS-CoV-2 Infection. Int. J. Environ. Res. Public Health 2022, 19, 1184. [Google Scholar] [CrossRef] [PubMed]
- Bein, A.; Kim, S.; Goyal, G.; Cao, W.; Fadel, C.; Naziripour, A.; Sharma, S.; Swenor, B.; LoGrande, N.; Nurani, A.; et al. Enteric Coronavirus Infection and Treatment Modeled With an Immunocompetent Human Intestine-On-A-Chip. Front. Pharmacol. 2021, 12, 718484. [Google Scholar] [CrossRef] [PubMed]
- Helms, L.; Marchiano, S.; Stanaway, I.B.; Hsiang, T.-Y.; Juliar, B.A.; Saini, S.; Zhao, Y.T.; Khanna, A.; Menon, R.; Alakwaa, F.; et al. Cross-Validation of SARS-CoV-2 Responses in Kidney Organoids and Clinical Populations. JCI Insight 2021, 6, e154882. [Google Scholar] [CrossRef]
- White, A.K.; VanInsberghe, M.; Petriv, O.I.; Hamidi, M.; Sikorski, D.; Marra, M.A.; Piret, J.; Aparicio, S.; Hansen, C.L. High-throughput microfluidic single-cell RT-qPCR. Proc. Natl. Acad. Sci. USA 2011, 108, 13999–14004. [Google Scholar] [CrossRef]
- Mertz, D.; Ahmed, T.; Takayama, S. Engineering cell heterogeneity into organs-on-a-chip. Lab Chip 2018, 18, 2378–2395. [Google Scholar] [CrossRef]
- Allie, S.R.; Bradley, J.E.; Mudunuru, U.; Schultz, M.D.; Graf, B.A.; Lund, F.E.; Randall, T.D. The establishment of resident memory B cells in the lung requires local antigen encounter. Nat. Immunol. 2018, 20, 97–108. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).