Nanoparticle Effects on Stress Response Pathways and Nanoparticle–Protein Interactions
Abstract
1. Introduction
1.1. Interactions of Nanoparticles with Cellular Components
1.2. Nanoparticles and Their Applications
2. Effects of Nanoparticles on Oxidative Stress and Stress Response Pathways
3. Nanoparticles and the Immune Response
3.1. Nanoparticle Effects on Immune Cell Receptors
3.2. Nanoparticle Effects on Oxidative Stress and the Immune Response
3.3. Summary
4. Inflammatory and Anti-Inflammatory Effects of Nanoparticles
4.1. Effects of Silver Nanoparticles on Inflammation
4.2. Pro-Inflammatory Effects of Titanium Dioxide Nanoparticles
4.3. Effects of Gold Nanoparticles on Inflammation
4.4. Pro-Inflammatory Effects of Silicon Dioxide Nanoparticles
4.5. Effects of Various Carbon Nanoparticles on Inflammation
4.6. Anti-Inflammatory Effects of Cerium Nanoparticles
4.7. Pro-Inflammatory Effects of Zinc Oxide Nanoparticles
4.8. Anti-Inflammatory Effects of Selenium Nanoparticles
4.9. Summary
5. Effects of Nanoparticles on Mitochondrial Function
5.1. Effects of Nanoparticles on Mitochondrial Fission and Fusion
5.2. Effects of Nanoparticles on Energy Production, Oxidative Phosphorylation, and Glycolysis
5.2.1. Effects of Nanoparticles on Energy Production In Vitro
5.2.2. Effects of Nanoparticles on Energy Production In Vivo
5.3. Summary
6. Effects of Nanoparticles on Insulin, Calcium, and Nitric Oxide Signaling Pathways
6.1. Effects of Nanoparticles on Insulin Signaling
6.2. Effects of Nanoparticles on Calcium Signaling
6.3. Effects of Nanoparticles on Nitric Oxide Signaling
7. Nanoparticle–Protein Interactions
7.1. Interactions of Nanoparticles with Zinc-Dependent Proteins
7.2. Interactions of Nanoparticles with Copper-Dependent Proteins
7.3. Interactions of Nanoparticles with Iron-Dependent Proteins
7.4. Interactions of Nanoparticles with Calcium-Dependent Proteins
8. Effects of Nanoparticles on Detoxification Enzymes
8.1. Effects of Nanoparticles on Phase I Detoxification Enzymes
8.2. Effects of Nanoparticles on Phase II Detoxification Enzymes
8.3. Effects of Nanoparticles on Metallothioneins
9. Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| 2D | Two-dimensional |
| 3D | Three-dimensional |
| 5-HETE | 5-Hydroxyicosatetraenoic acid |
| A-357 | Human skin melanoma cells |
| A498 | Human renal carcinoma cells |
| A549 | Human lung adenocarcinoma cells |
| AChE | Acetylcholinesterase |
| ADP | Adenosine diphosphate |
| Ag | Silver |
| AgNO3 | Silver nitrate |
| AIM2 | Absent in melanoma 2 |
| Al2O3 | Aluminum oxide |
| AlOOH | Boehmite |
| ALP | Alkaline phosphatase |
| ALT | Alanine aminotransferas |
| AMP | Adenosine monophosphate |
| AMPK | 5′ adenosine monophosphate-activated protein kinase |
| AP-1 | Activator protein-1 |
| Apaf-1 | Apoptotic protease-activating factor-1 |
| AS160 | 160 kDa Akt substrate |
| ASM | Airway smooth muscle cells |
| AST | Aspartate aminotransferase |
| ATP | Adenosine triphosphate |
| Au | Gold |
| Bak | Bcl-2 homologous antagonist/killer |
| Bax | Bcl-2 associated X protein |
| Bcl-2 | B cell lymphoma-2 |
| BMDMs | Bone marrow-derived macrophages |
| Ca2+ | Calcium |
| Ca2+-ATPase | Calcium ATPase |
| Ca2+/Mg2+-ATPase | Calcium-magnesium ATPase |
| CaF2 | Calcium fluoride |
| CaMKKβ | Calmodulin-dependent protein kinase kinase β |
| Cas9 | CRISPR-associated protein 9 |
| CAT | Catalase |
| CcO | Cytochrome c oxidase |
| CD | Circular dichroism |
| Cd | Cadmium |
| Ce | Cerium |
| CeO2 | Cerium dioxide |
| CGCs | Cerebellar granule cells |
| CICR | Calcium induced calcium release |
| COVID-19 | Coronavirus disease 2019 |
| COX-2 | Cyclooxygenase-2 |
| Cr | Chromium |
| CRISPR | Clustered regularly interspaced short palindromic repeats |
| CRL-2404 | Human epidermal keratinocytes |
| Cu | Copper |
| CuO | Copper oxide |
| Cu-Zn-SOD | Copper-zinc superoxide dismutase |
| CXCL8 | C-X-C motif chemokine ligand 8 |
| CYP450 | Cytochrome P450 |
| Cyt c | Cytochrome c |
| DAMPs | Damage-associated molecular patterns |
| dATP | Deoxyadenosine triphosphate |
| DEHP | Di(2-ethylhexyl) phthalate |
| DLS | Dynamic light scattering |
| DNA | Deoxyribonucleic acid |
| DPP-4 | Dipeptidyl peptidase-4 |
| Drp1 | Dynamin-related protein 1 |
| eNOS | Endothelial nitric oxide synthase |
| ER | Endoplasmic reticulum |
| ERK1/2 | Extracellular signal-regulated kinase (ERK) 1 and 2 |
| ETC | Electron transport chain |
| F10 | Melanoma cells |
| FAD | Flavin adenine dinucleotide |
| FADH2 | Reduced flavin adenine dinucleotide |
| Fe | Iron |
| Fe-SOD | Iron superoxide dismutase |
| Fis1 | Fission protein 1 |
| FMN | Flavin mononucleotide |
| FT-IR | Fourier transform infrared spectroscopy |
| GGT | Gamma-glutamyl transferase |
| GLUT | Glucose transporter |
| GPx | Glutathione peroxidase |
| GPx1 | Glutathione peroxidase 1 |
| GPx3 | Glutathione peroxidase 3 |
| GR | Glutathione reductase |
| GSH | Glutathione |
| GSK-3β | Glycogen synthase kinase-3β |
| GSSG | Glutathione disulfide |
| GST | Glutathione S-transferase |
| H2O | water |
| H2O2 | Hydrogen peroxide |
| H9 | Human embryonic stem cells |
| HaCaT | Human epidermal keratinocyte cells |
| HAECs | Human aortic endothelial cells |
| Hb | Hemoglobin |
| HCT116 | Human colon carcinoma cells |
| HDAC | Histone deacetylase |
| HeLa | Human cervical carcinoma cells |
| HEK293T | Human embryonic kidney 293T |
| HepG2 | Human hepatoma cells |
| hFOB1.19 | Human osteoblast cell line |
| Hg | Mercury |
| HL-60 | Human promyelocytic leukemia cells |
| HO-1 | Heme oxygenase-1 |
| HPAECs | Human pulmonary artery endothelial cells |
| HSC-3 | Human oral squamous cell carcinoma cells |
| HT22 | Murine hippocampal neuronal cells |
| HT-29 | Colon cancer cells |
| Huh7 | Human hepatoma cells |
| HUVECs | Human umbilical vein endothelial cells |
| IAPs | Inhibitor of apoptosis proteins |
| ICAM-1 | Intercellular adhesion molecule 1 |
| IFN-γ | Interferon gamma |
| IGF-1 | Insulin-like growth factor 1 |
| IGF-1R | Type 1 insulin-like growth factor receptor |
| IGFBP-3 | Insulin-like growth factor binding protein-3 |
| IgG | Immunoglobulin G |
| iGluRs | Ionotropic glutamate receptors |
| IL | Interleukin |
| iNOS | Inducible nitric oxide synthase |
| IP3 | Inositol 1,4,5-triphosphate |
| iPSCs | Human induced pluripotent stem cells |
| IRR | Orphan insulin receptor-related receptor |
| IRS | Insulin receptor substrate |
| J774 | Mouse macrophage cells |
| JAK-STAT | Janus kinase-signal transducer and activator of transcription |
| JNK | c-Jun N-terminal Kinase |
| K562 | Human chronic myeloid leukemia cells |
| Keap1 | Kelch-like ECH-associated protein 1 |
| KLF2 | Kruppel-like factor 2 |
| KLH | Keyhole limpet hemocyanin |
| LKB1 | Liver kinase B1 |
| LoVo | Human colon carcinoma cells |
| LPS | Lipopolysaccharide |
| Mac-1 | Macrophage-1 antigen |
| MAMs | Mitochondria-associated ER membranes |
| MAPK | Mitogen-activated protein kinase |
| MCF-7 | Breast adenocarcinoma cells |
| MCP-1 | Monocyte chemoattractant protein-1 |
| MD | Molecular dynamics |
| MEF | Murine embryonic fibroblast |
| Mfn1 | Mitofusions 1 |
| Mfn2 | Mitofusions 2 |
| MgO | Magnesium oxide |
| MLCK | Myosin light chain kinase |
| Mn | Manganese |
| Mn-SOD | Manganese superoxide dismutase |
| mRNA | Messenger ribonucleic acid |
| mTOR | Mammalian target of rapamycin |
| MT | Metallothionein |
| MTT | 3-(4, 5-dimethylthiazolyl-2)-2,5-diphenyltetraxolium bromide |
| NADH | Reduced nicotinamide adenine dinucleotide |
| NADPH | Nicotinamide adenine dinucleotide phosphate |
| Na+/K+-ATPase | Sodium-potassium ATPase |
| NB41A3 | Neuroblastoma cells |
| NCI-H292 | Human airway epithelial cells |
| NF-κB | Nuclear factor kappa B |
| Ni | Nickel |
| NiO | Nickel oxide |
| Ni-SOD | Nickel superoxide dismutase |
| NLRC4 | NLR family CARD domain containing 4 |
| NLRP1 | Nucleotide-binding oligomerization domain, leucine rich repeat and pyrin domain containing 1 |
| NMDA | N-methyl-D-aspartate receptors |
| NMRI | Naval medical research institute |
| nNOS | Neuronal nitric oxide synthase |
| ●NO | Nitric oxide |
| NOS | Nitric oxide synthase |
| NOSII | Nitric oxide synthase II |
| NOSIII | Nitric oxide synthase III |
| NPs | Nanoparticles |
| NQO1 | NADPH quinone dehydrogenase 1 |
| NR1 | NMDA receptor 1 |
| Nrf2 | Nuclear factor erythroid 2-related factor 2 |
| NSCLC | Non-small-cell lung cancer cells |
| O2 | Oxygen |
| O2− | Superoxide |
| ONOO− | Peroxynitrite |
| Opa1 | Optic atrophy 1 |
| OPG | Osteoprotegerin |
| PAK | p21-activated kinase |
| PAMPs | Pathogen-associated molecular patterns |
| PANC-1 | Pancreatic carcinoma cells |
| PASMCs | Pulmonary artery smooth muscle cells |
| Pb | Lead |
| PBMCs | Peripheral blood mononuclear cells |
| PC12 | Pheochromocytoma cells |
| PC3 | Prostate carcinoma cells |
| PDI | Protein disulfide isomerase |
| PDI-3 | Protein disulfide isomerase-3 |
| p-Drp1 | Phosphorylated dynamin-related protein 1 |
| PEG | Polyethylene glycol |
| PGC-1α | Peroxisome proliferator-activated receptor gamma coactivator 1-alpha |
| PI3K | Phosphatidylinositol 3-kinase |
| PKB | Protein kinase B |
| PLA | Polylactic acid |
| PLGA | Poly(lactice-co-glycolide) |
| PMF | Proton motive force |
| PRDX | Peroxiredoxin |
| PRR | Pattern recognition receptor |
| Pt | Platinum |
| PTEN | Phosphatase and tensin homolog deleted on chromosome ten |
| PVA | Polyvinyl alcohol |
| RANKL | Receptor activator of nuclear factor-kB ligand |
| RAW 264.7 | Murine macrophages |
| RIN-5F | Pancreatic cells |
| RNS | Reactive nitrogen species |
| ROS | Reactive oxygen species |
| RR spectroscopy | Resonance Raman spectroscopy |
| SAOS2 | Human bone osteosarcoma cells |
| Se | Selenium |
| SEIRAS | Surface enhanced infrared absorption spectroscopy |
| SERS | Surface-enhanced Raman scattering |
| SGLT2 | Sodium-dependent glucose transporter 2 |
| SH | Sulfhydryl |
| SH-SY5Y | Human neuroblastoma cells |
| Si | Silica |
| SiO2 | Silicon dioxide |
| SIRT1 | Silent mating type information regulation 2 homolog 1 |
| Smac | Second mitochondria-derived activator of caspase |
| SOD | Superoxide dismutase |
| SR-AI | Membrane type I class A scavenger receptor |
| SREBP-1c | Sterol regulatory element binding protein-1c |
| SV40 | Simian virus 40 |
| SVEC4-10 | mouse endothelial cells |
| TEM | Transmission electron microscopy |
| TGF-β | Transforming growth factor-beta |
| THP-1 | Tohoku Hospital Pediatrics-1 cells |
| TiO2 | Titanium dioxide |
| TLR | Toll-like receptor |
| TNF-α | Tumor necrosis factor alpha |
| TRAIL | Tumor necrosis factor-related apoptosis-inducing ligand |
| TRPV | Transient receptor potential vanilloid channels |
| TRX | Thioredoxin |
| TRX1 | Thioredoxin-1 |
| TRX2 | Thioredoxin-2 |
| TXNIP | Thioredoxin interacting protein |
| U2OS | Human bone osteosarcoma cells |
| U87 | Human astrocytoma cells |
| UV–vis | Ultraviolet–visible |
| VEGF | Vascular endothelial growth factor |
| WI-38 | Human lung fibroblast cells |
| WST-1 | 2-(4-Iodophenyl)-3-(4-nitrophenyl)-5-(2,4-disulfophenyl)-2H-tetrazolium |
| ZIP | Zinc-regulated, Iron-regulated transporter-like Protein |
| Zn | Zinc |
| ZnCL2 | Zinc chloride |
| ZnFe2O4 | Spinel zinc ferrite |
| ZnO | Zinc oxide |
| ZnT | Zinc Transporter |
| ZVFe | Zero valent iron |
References
- Rönkkö, T.; Pirjola, L.; Ntziachristos, L.; Heikkilä, J.; Karjalainen, P.; Hillamo, R.; Keskinen, J. Vehicle engines produce exhaust nanoparticles even when not fueled. Environ. Sci. Technol. 2014, 48, 2043–2050. [Google Scholar] [CrossRef]
- Evelyn, A.; Mannick, S.; Sermon, P.A. Unusual carbon-based nanofibers and chains among diesel-emitted particles. Nano Lett. 2003, 3, 63–64. [Google Scholar] [CrossRef]
- Van Dijk, W.D.; Gopal, S.; Scheepers, P.T.J. Nanoparticles in cigarette smoke; Real-time undiluted measurements by a scanning mobility particle sizer. Anal. Bioanal. Chem. 2011, 399, 3573–3578. [Google Scholar] [CrossRef]
- Williams, M.; Villarreal, A.; Bozhilov, K.; Lin, S.; Talbot, P. Metal and Silicate Particles Including Nanoparticles Are Present in Electronic Cigarette Cartomizer Fluid and Aerosol. PLoS ONE 2013, 8, e57987. [Google Scholar] [CrossRef]
- Wilson, M.D.; Prasad, K.A.; Kim, J.S.; Park, J.H. Characteristics of metallic nanoparticles emitted from heated Kanthal e-cigarette coils. J. Nanopart. Res. 2019, 21, 1–11. [Google Scholar] [CrossRef]
- Lai, B.; Cui, G.; Wang, H.; Song, Y.; Tan, M. Identification of fluorescent nanoparticles from roasted sweet potato (Ipomoea batatas) during normal cooking procedures. LWT 2020, 134, 109989. [Google Scholar] [CrossRef]
- Park, J.; Ham, S.; Jang, M.; Lee, J.; Kim, S.; Kim, S.; Lee, K.; Park, D.; Kwon, J.; Kim, H.; et al. Spatial-Temporal Dispersion of Aerosolized Nanoparticles during the Use of Consumer Spray Products and Estimates of Inhalation Exposure. Environ. Sci. Technol. 2017, 51, 7624–7638. [Google Scholar] [CrossRef]
- Hewitt, R.E.; Chappell, H.F.; Powell, J.J. Small and dangerous? Potential toxicity mechanisms of common exposure particles and nanoparticles. Curr. Opin. Toxicol. 2020, 19, 93–98. [Google Scholar] [CrossRef]
- Park, J.; Kwak, B.K.; Bae, E.; Lee, J.; Kim, Y.; Choi, K.; Yi, J. Characterization of exposure to silver nanoparticles in a manufacturing facility. J. Nanopart. Res. 2009, 11, 1705–1712. [Google Scholar] [CrossRef]
- Chenthamara, D.; Subramaniam, S.; Ramakrishnan, S.G.; Krishnaswamy, S.; Essa, M.M.; Lin, F.H.; Qoronfleh, M.W. Therapeutic efficacy of nanoparticles and routes of administration. Biomater. Res. 2019, 23, 1–29. [Google Scholar] [CrossRef]
- El-Sayed, A.; Kamel, M. Advances in nanomedical applications: Diagnostic, therapeutic, immunization, and vaccine production. Environ. Sci. Pollut. Res. 2020, 27, 19200–19213. [Google Scholar] [CrossRef]
- Fröhlich, E. Europe PMC Funders Group. Cellular Targets and Mechanisms in the Cytotoxic Action of Non-biodegradable Engineered Nanoparticles. Curr. Drug Metab. 2013, 14, 976–988. [Google Scholar] [CrossRef] [PubMed]
- Khanna, P.; Ong, C.; Bay, B.H.; Baeg, G.H. Nanotoxicity: An interplay of oxidative stress, inflammation and cell death. Nanomaterials 2015, 5, 1163–1180. [Google Scholar] [CrossRef] [PubMed]
- Nel, A.; Xia, T.; Mädler, L.; Li, N. Toxic potential of materials at the nanolevel. Science 2006, 311, 622–627. [Google Scholar] [CrossRef]
- Liu, L.; Zeng, L.; Wu, L.; Jiang, X. Revealing the Effect of Protein Weak Adsorption to Nanoparticles on the Interaction between the Desorbed Protein and its Binding Partner by Surface-Enhanced Infrared Spectroelectrochemistry. Anal. Chem. 2017, 89, 2724–2730. [Google Scholar] [CrossRef]
- Mariam, J.; Sivakami, S.; Dongre, P.M. Albumin corona on nanoparticles—A strategic approach in drug delivery. Drug Deliv. 2016, 23, 2668–2676. [Google Scholar] [CrossRef]
- Pan, Y.; Ong, C.E.; Pung, Y.F.; Chieng, J.Y. The current understanding of the interactions between nanoparticles and cytochrome P450 enzymes—A literature-based review. Xenobiotica 2019, 49, 863–876. [Google Scholar] [CrossRef]
- Vis, B.; Hewitt, R.E.; Faria, N.; Bastos, C.; Chappell, H.; Pele, L.; Jugdaohsingh, R.; Kinrade, S.D.; Powell, J.J. Non-Functionalized Ultrasmall Silica Nanoparticles Directly and Size-Selectively Activate T Cells. ACS Nano 2018, 12, 10843–10854. [Google Scholar] [CrossRef]
- Vis, B.; Hewitt, R.E.; Monie, T.P.; Fairbairn, C.; Turner, S.D.; Kinrade, S.D.; Powell, J.J. Ultrasmall silica nanoparticles directly ligate the T cell receptor complex. Proc. Natl. Acad. Sci. USA 2020, 117, 285–291. [Google Scholar] [CrossRef]
- Devineau, S.; Zargarian, L.; Renault, J.P.; Pin, S. Structure and Function of Adsorbed Hemoglobin on Silica Nanoparticles: Relationship between the Adsorption Process and the Oxygen Binding Properties. Langmuir 2017, 33, 3241–3252. [Google Scholar] [CrossRef]
- Pang, C.; Zhang, N.; Falahati, M. Acceleration of α-synuclein fibril formation and associated cytotoxicity stimulated by silica nanoparticles as a model of neurodegenerative diseases. Int. J. Biol. Macromol. 2021, 169, 532–540. [Google Scholar] [CrossRef] [PubMed]
- Bartels, T.; Ahlstrom, L.S.; Leftin, A.; Kamp, F.; Haass, C.; Brown, M.F.; Beyer, K. The N-terminus of the intrinsically disordered protein α-synuclein triggers membrane binding and helix folding. Biophys. J. 2010, 99, 2116–2124. [Google Scholar] [CrossRef] [PubMed]
- Verano-Braga, T.; Miethling-Graff, R.; Wojdyla, K.; Rogowska-Wrzesinska, A.; Brewer, J.R.; Erdmann, H.; Kjeldsen, F. Insights into the Cellular Response Triggered by Silver Nanoparticles Using Quantitative Proteomics. ACS Nano 2014, 8, 2161–2175. [Google Scholar] [CrossRef] [PubMed]
- Bahadar, H.; Maqbool, F.; Niaz, K.; Abdollahi, M. Toxicity of Nanoparticles and an Overview of Current Experimental Models. Iran. Biomed. J. 2016, 20, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Gurunathan, S.; Jeyaraj, M.; La, H.; Yoo, H.; Choi, Y.; Do, J.T.; Park, C.; Kim, J.-H.; Hong, K. Anisotropic Platinum Nanoparticle-Induced Cytotoxicity, Apoptosis, Inflammatory Response, and Transcriptomic and Molecular Pathways in Human Acute Monocytic Leukemia Cells. Int. J. Mol. Sci. 2020, 21, 440. [Google Scholar] [CrossRef]
- Labrador-Rached, C.J.; Browning, R.T.; Braydich-Stolle, L.K.; Comfort, K.K. Toxicological Implications of Platinum Nanoparticle Exposure: Stimulation of Intracellular Stress, Inflammatory Response, and Akt Signaling In Vitro. J. Toxicol. 2018, 2018, 1367801. [Google Scholar] [CrossRef]
- Vance, M.E.; Kuiken, T.; Vejerano, E.P.; McGinnis, S.P.; Hochella, M.F.; Hull, D.R. Nanotechnology in the real world: Redeveloping the nanomaterial consumer products inventory. Beilstein J. Nanotechnol. 2015, 6, 1769–1780. [Google Scholar] [CrossRef]
- Cameron, S.J.; Hosseinian, F.; Willmore, W.G. A Current Overview of the Biological and Cellular Effects of Nanosilver. Int. J. Mol. Sci. 2018, 19, 2030. [Google Scholar] [CrossRef]
- Mishra, S.; Singh, H.B. Biosynthesized silver nanoparticles as a nanoweapon against phytopathogens: Exploring their scope and potential in agriculture. Appl. Microbiol. Biotechnol. 2015, 99, 1097–1107. [Google Scholar] [CrossRef]
- Boisselier, E.; Astruc, D. Gold nanoparticles in nanomedicine: Preparations, imaging, diagnostics, therapies and toxicity. Chem. Soc. Rev. 2009, 38, 1759. [Google Scholar] [CrossRef]
- Dykman, L.A.; Khlebtsov, N.G. Gold nanoparticles in biology and medicine: Recent advances and prospects. Acta Nat. 2011, 3, 34–55. [Google Scholar] [CrossRef]
- Singh, P.; Pandit, S.; Mokkapati, V.R.S.S.; Garg, A.; Ravikumar, V.; Mijakovic, I. Gold Nanoparticles in Diagnostics and Therapeutics for Human Cancer. Int. J. Mol. Sci. 2018, 19, 1979. [Google Scholar] [CrossRef] [PubMed]
- Mohajerani, A.; Burnett, L.; Smith, J.V.; Kurmus, H.; Milas, J.; Arulrajah, A.; Horpibulsuk, S.; Kadir, A.A. Nanoparticles in construction materials and other applications, and implications of nanoparticle use. Materials 2019, 12, 3052. [Google Scholar] [CrossRef]
- Fytianos, G.; Rahdar, A.; Kyzas, G.Z. Nanomaterials in cosmetics: Recent updates. Nanomaterials 2020, 10, 979. [Google Scholar] [CrossRef] [PubMed]
- Minarchick, V.C.; Stapleton, P.A.; Fix, N.R.; Leonard, S.S.; Sabolsky, E.M.; Nurkiewicz, T.R. Intravenous and gastric cerium dioxide nanoparticle exposure disrupts microvascular smooth muscle signaling. Toxicol. Sci. 2015, 144, 77–89. [Google Scholar] [CrossRef] [PubMed]
- Asano, S.; Arvapalli, R.; Manne, N.D.; Maheshwari, M.; Ma, B.; Rice, K.M.; Selvaraj, V.; Blough, E.R. Cerium oxide nanoparticle treatment ameliorates peritonitis-induced diaphragm dysfunction. Int. J. Nanomed. 2015, 10, 6215–6226. [Google Scholar] [CrossRef]
- Burnett, M.; Abuetabh, Y.; Wronski, A.; Shen, F.; Persad, S.; Leng, R.; Eisenstat, D.; Sergi, C. Graphene oxide nanoparticles induce apoptosis in wild-type and CRISPR/Cas9-IGF/IGFBP3 knocked-out osteosarcoma cells. J. Cancer 2020, 11, 5007–5023. [Google Scholar] [CrossRef]
- Paul, M.B.; Stock, V.; Cara-Carmona, J.; Lisicki, E.; Shopova, S.; Fessard, V.; Braeuning, A.; Sieg, H.; Böhmert, L. Micro-and nanoplastics-current state of knowledge with the focus on oral uptake and toxicity. Nanoscale Adv. 2020, 2, 4350–4367. [Google Scholar] [CrossRef]
- Proquin, H.; Rodríguez-Ibarra, C.; Moonen, C.G.J.; Urrutia Ortega, I.M.; Briedé, J.J.; de Kok, T.M.; van Loveren, H.; Chirino, Y.I. Titanium dioxide food additive (E171) induces ROS formation and genotoxicity: Contribution of micro and nano-sized fractions. Mutagenesis 2017, 32, 139–149. [Google Scholar] [CrossRef]
- Rastogi, A.; Tripathi, D.K.; Yadav, S.; Chauhan, D.K.; Živčák, M.; Ghorbanpour, M.; El-Sheery, N.I.; Brestic, M. Application of silicon nanoparticles in agriculture. 3 Biotech 2019, 9, 1–11. [Google Scholar] [CrossRef]
- Wang, J.; Zhang, K.; Fei, G.; de Luna, M.S.; Lavorgna, M.; Xia, H. High silica content graphene/natural rubber composites prepared by a wet compounding and latex mixing process. Polymers 2020, 12, 2549. [Google Scholar] [CrossRef] [PubMed]
- Proquin, H.; Jonkhout, M.C.M.; Jetten, M.J.; van Loveren, H.; de Kok, T.M.; Briedé, J.J. Transcriptome changes in undifferentiated Caco-2 cells exposed to food-grade titanium dioxide (E171): Contribution of the nano- and micro- sized particles. Sci. Rep. 2019, 9, 18287. [Google Scholar] [CrossRef] [PubMed]
- Periasamy, V.S.; Athinarayanan, J.; Al-Hadi, A.M.; Juhaimi, F.A.; Mahmoud, M.H.; Alshatwi, A.A. Identification of titanium dioxide nanoparticles in food products: Induce intracellular oxidative stress mediated by TNF and CYP1A genes in human lung fibroblast cells. Environ. Toxicol. Pharmacol. 2015, 39, 176–186. [Google Scholar] [CrossRef] [PubMed]
- Weir, A.; Westerhoff, P.; Fabricius, L.; von Goetz, N. Titanium Dioxide Nanoparticles in Food and Personal Care Products. Environ. Sci. Technol. 2012, 46, 2242–2250. [Google Scholar] [CrossRef] [PubMed]
- Batt, J.; Milward, M.; Chapple, I.; Grant, M.; Roberts, H.; Addison, O. TiO(2) nanoparticles can selectively bind CXCL8 impacting on neutrophil chemotaxis. Eur. Cells Mater. 2018, 35, 13–24. [Google Scholar] [CrossRef]
- Jha, S.; Mathur, P.; Ramteke, S.; Jain, N.K. Pharmaceutical potential of quantum dots. Artif. Cells Nanomed. Biotechnol. 2018, 46, 57–65. [Google Scholar] [CrossRef]
- Guszpit, E.; Krejčová, L.; Křížková, S.; Kepinska, M.; Richtera, L.; Kopel, P.; Adam, V.; Milnerowicz, H. Kinetic analysis of human metallothionein and CdTe quantum dot complexes using fluorescence and voltammetry techniques. Colloids Surf. B Biointerfaces 2017, 160, 381–389. [Google Scholar] [CrossRef]
- Sabir, S.; Arshad, M.; Chaudhari, S.K. Zinc oxide nanoparticles for revolutionizing agriculture: Synthesis and applications. Sci. World J. 2014, 2014, 925494. [Google Scholar] [CrossRef]
- Deweirdt, J.; Quignard, J.F.; Lacomme, S.; Gontier, E.; Mornet, S.; Savineau, J.P.; Marthan, R.; Guibert, C.; Baudrimont, I. In vitro study of carbon black nanoparticles on human pulmonary artery endothelial cells: Effects on calcium signaling and mitochondrial alterations. Arch. Toxicol. 2020, 94, 2331–2348. [Google Scholar] [CrossRef]
- Gao, M.; Zheng, F.; Xu, J.; Zhang, S.; Bhosale, S.S.; Gu, J.; Hong, R. Surface modification of nano-sized carbon black for reinforcement of rubber. Nanotechnol. Rev. 2019, 8, 405–414. [Google Scholar] [CrossRef]
- Xu, Y.; Liu, H.; Song, L. Novel drug delivery systems targeting oxidative stress in chronic obstructive pulmonary disease: A review. J. Nanobiotechnol. 2020, 18, 1–25. [Google Scholar] [CrossRef] [PubMed]
- Xu, M.; Halimu, G.; Zhang, Q.; Song, Y.; Fu, X.; Li, Y.; Li, Y.; Zhang, H. Internalization and toxicity: A preliminary study of effects of nanoplastic particles on human lung epithelial cell. Sci. Total Environ. 2019, 694, 133794. [Google Scholar] [CrossRef]
- Manke, A.; Wang, L.; Rojanasakul, Y. Mechanisms of nanoparticle-induced oxidative stress and toxicity. Biomed Res. Int. 2013, 2013, 942916. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, D.; Bharali, D. Oxidative Stress and Nanotechnology; Humana: Totowa, NJ, USA, 2013; ISBN 9781627034746. [Google Scholar]
- Poljak-Blaži, M.; Jaganjac, M.; Žarković, N. Cell Oxidative Stress: Risk of Metal Nanoparticles. In Handbook of Nanophysics Nanomedicine and Nanorobotics; CRC Press: New York, NY, USA, 2010. [Google Scholar]
- Ju-Nam, Y.; Lead, J.R. Manufactured nanoparticles: An overview of their chemistry, interactions and potential environmental implications. Sci. Total Environ. 2008, 400, 396–414. [Google Scholar] [CrossRef]
- Li, N.; Xia, T.; Nel, A.E. The role of oxidative stress in ambient particulate matter-induced lung diseases and its implications in the toxicity of engineered nanoparticles. Free Radic. Biol. Med. 2008, 44, 1689–1699. [Google Scholar] [CrossRef] [PubMed]
- Stone, V.; Johnston, H.; Clift, M.J.D. Air pollution, ultrafine and nanoparticle toxicology: Cellular and molecular interactions. IEEE Trans. Nanobiosci. 2007, 6, 331–340. [Google Scholar] [CrossRef] [PubMed]
- Johnston, H.J.; Hutchison, G.; Christensen, F.M.; Peters, S.; Hankin, S.; Stone, V. A review of the in vivo and in vitro toxicity of silver and gold particulates: Particle attributes and biological mechanisms responsible for the observed toxicity. Crit. Rev. Toxicol. 2010, 40, 328–346. [Google Scholar] [CrossRef]
- Emerit, I. Reactive oxygen species, chromosome mutation, and cancer: Possible role of clastogenic factors in carcinogenesis. Free Radic. Biol. Med. 1994, 16, 99–109. [Google Scholar] [CrossRef]
- Waris, G.; Ahsan, H. Reactive oxygen species: Role in the development of cancer and various chronic conditions. J. Carcinog. 2006, 5, 14. [Google Scholar] [CrossRef]
- Harrison, D.; Griendling, K.K.; Landmesser, U.; Hornig, B.; Drexler, H. Role of Oxidative Stress in Atherosclerosis. Am. J. Cardiol. 2003, 91, 7A–11A. [Google Scholar] [CrossRef]
- Eberhardt, M.K. Reactive Oxygen Metabolites: Chemistry and Medical Consequences; CRC Press: Boca Raton, FL, USA, 2001. [Google Scholar]
- Simonian, N.A.; Coyle, J.T. Oxidative stress in neurodegenerative diseases. Annu. Rev. Pharmacol. Toxicol. 1996, 36, 83–106. [Google Scholar] [CrossRef] [PubMed]
- Griffiths, H.R. ROS as signalling molecules in T cells—Evidence for abnormal redox signalling in the autoimmune disease, rheumatoid arthritis. Redox Rep. 2005. [Google Scholar] [CrossRef] [PubMed]
- Namazi, M.R. Cytochrome-P450 enzymes and autoimmunity: Expansion of the relationship and introduction of free radicals as the link. J. Autoimmune Dis. 2009, 6, 4. [Google Scholar] [CrossRef]
- Houstis, N.; Rosen, E.D.; Lander, E.S. Reactive oxygen species have a causal role in multiple forms of insulin resistance. Nature 2006, 440, 944–948. [Google Scholar] [CrossRef] [PubMed]
- Nishikawa, T.; Araki, E. Impact of Mitochondrial ROS Production in the Pathogenesis of Diabetes Mellitus and Its Complications. Antioxid. Redox Signal. 2006, 9, 343–353. [Google Scholar] [CrossRef]
- Liu, W.; Worms, I.; Slaveykova, V.I. Interaction of silver nanoparticles with antioxidant enzymes. Environ. Sci. Nano 2020, 7, 1507–1517. [Google Scholar] [CrossRef]
- Srivastava, M.; Singh, S.; Self, W.T. Exposure to silver nanoparticles inhibits selenoprotein synthesis and the activity of thioredoxin reductase. Environ. Health Perspect. 2012, 120, 56–61. [Google Scholar] [CrossRef]
- Xu, M.; Yang, Q.; Xu, L.; Rao, Z.; Cao, D.; Gao, M.; Liu, S. Protein target identification and toxicological mechanism investigation of silver nanoparticles-induced hepatotoxicity by integrating proteomic and metallomic strategies. Part. Fibre Toxicol. 2019, 16, 46. [Google Scholar] [CrossRef]
- Zhao, L.; Zong, W.; Zhang, H.; Liu, R. Kidney Toxicity and Response of Selenium Containing Protein-glutathione Peroxidase (Gpx3) to CdTe QDs on Different Levels. Toxicol. Sci. 2019, 168, 201–208. [Google Scholar] [CrossRef]
- Congiu, L.; Chicca, M.; Pilastro, A.; Turchetto, M.; Tallandini, L. Effects of chronic dietary cadmium on hepatic glutathione levels and glutathione peroxidase activity in starlings (Sturnus vulgaris). Arch. Environ. Contam. Toxicol. 2000, 38, 357–361. [Google Scholar] [CrossRef]
- Triboulet, S.; Aude-Garcia, C.; Carrière, M.; Diemer, H.; Proamer, F.; Habert, A.; Chevallet, M.; Collin-Faure, V.; Strub, J.M.; Hanau, D.; et al. Molecular responses of mouse macrophages to copper and copper oxide nanoparticles inferred from proteomic analyses. Mol. Cell. Proteom. 2013, 12, 3108–3122. [Google Scholar] [CrossRef] [PubMed]
- Sund, J.; Alenius, H.; Vippola, M.; Savolainen, K.; Puustinen, A. Proteomic characterization of engineered nanomaterial-protein interactions in relation to surface reactivity. ACS Nano 2011, 5, 4300–4309. [Google Scholar] [CrossRef]
- El-Batal, A.I.; Thabet, N.M.; Mostafa, A.O.; Abdel Ghaffar, A.R.B.; Azab, K.S. Amelioration of oxidative damage induced in gamma irradiated rats by nano selenium and lovastatin mixture. World Appl. Sci. J. 2012, 19, 962–971. [Google Scholar] [CrossRef]
- Hao, X.; Zhang, L.; Zheng, X.; Zong, W.; Liu, C. Molecular mechanism of composite nanoparticles TiO2/WO3/GO-induced activity changes of catalase and superoxide dismutase. Chem. Biol. Interact. 2018, 292, 30–36. [Google Scholar] [CrossRef] [PubMed]
- Coban, T.; Senturk, M.; Ciftci, M.; Kufrevioglu, O. Effects of Some Metal Ions on Human Erythrocyte Glutathione Reductase: An In Vitro Study. Protein Pept. Lett. 2007, 14, 1027–1030. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.; Shao, H.; Liu, W.; Gu, W.; Shu, X.; Mo, Y.; Chen, X.; Zhang, Q.; Jiang, M. Endoplasmic reticulum stress and oxidative stress are involved in ZnO nanoparticle-induced hepatotoxicity. Toxicol. Lett. 2015, 234, 40–49. [Google Scholar] [CrossRef]
- Mirzaei, S.; Hadadi, Z.; Attar, F.; Mousavi, S.E.; Zargar, S.S.; Tajik, A.; Saboury, A.A.; Rezayat, S.M.; Falahati, M. ROS-mediated heme degradation and cytotoxicity induced by iron nanoparticles: Hemoglobin and lymphocyte cells as targets. J. Biomol. Struct. Dyn. 2018, 36, 4235–4245. [Google Scholar] [CrossRef]
- McCord, J.M.; Fridovich, I. Superoxide dismutase. An enzymic function for erythrocuprein (hemocuprein). J. Biol. Chem. 1969, 244, 6049–6055. [Google Scholar] [CrossRef]
- Maines, M.D.; Kappas, A. Regulation of cytochrome P-450-dependent microsomal drug-metabolizing enzymes by nickel, cobalt, and iron. Clin. Pharmacol. Ther. 1977, 5 Pt 2, 780–790. [Google Scholar] [CrossRef]
- Atli, G.; Alptekin, Ö.; Tükel, S.; Canli, M. Response of catalase activity to Ag+, Cd2+, Cr6+, Cu2+ and Zn2+ in five tissues of freshwater fish Oreochromis niloticus. Comp. Biochem. Physiol. C Toxicol. Pharmacol. 2006, 143, 218–224. [Google Scholar] [CrossRef]
- He, W.; Wamer, W.; Xia, Q.; Yin, J.J.; Fu, P.P. Enzyme-like activity of nanomaterials. J. Environ. Sci. Heal. Part C Environ. Carcinog. Ecotoxicol. Rev. 2014, 32, 186–211. [Google Scholar] [CrossRef] [PubMed]
- Singh, S. Zinc oxide nanoparticles impacts: Cytotoxicity, genotoxicity, developmental toxicity, and neurotoxicity. Toxicol. Mech. Methods 2019, 29, 300–311. [Google Scholar] [CrossRef] [PubMed]
- Heble, A.Y.; Santelli, J.; Armstrong, A.M.; Mattrey, R.F.; Lux, J. Catalase-Loaded Silica Nanoparticles Formulated via Direct Surface Modification as Potential Oxygen Generators for Hypoxia Relief. ACS Appl. Mater. Interfaces 2021, 13, 5945–5954. [Google Scholar] [CrossRef]
- Hossain, K.F.B.; Rahman, M.M.; Sikder, M.T.; Saito, T.; Hosokawa, T.; Kurasaki, M. Inhibitory effects of selenium on cadmium-induced cytotoxicity in PC12 cells via regulating oxidative stress and apoptosis. Food Chem. Toxicol. 2018, 114, 180–189. [Google Scholar] [CrossRef]
- Kuršvietienė, L.; Mongirdienė, A.; Bernatonienė, J.; Šulinskienė, J.; Stanevičienė, I. Selenium anticancer properties and impact on cellular redox status. Antioxidants 2020, 9, 80. [Google Scholar] [CrossRef] [PubMed]
- Dhanjal, S.; Cameotra, S.S. Aerobic biogenesis of selenium nanospheres by Bacillus cereus isolated from coalmine soil. Microb. Cell Fact. 2010, 9, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Berggren, M.M.; Mangin, J.F.; Gasdaska, J.R.; Powis, G. Effect of selenium on rat thioredoxin reductase activity: Increase by supranutritional selenium and decrease by selenium deficiency. Biochem. Pharmacol. 1999, 57, 187–193. [Google Scholar] [CrossRef]
- Azeh, E.G.; Udoka Ferdinand, P.; Nweke Nwalo, F.; Unachukwu, M.N. Mechanism and Health Effects of Heavy Metal Toxicity in Humans. In Poisoning in the Modern World-New Tricks for an Old Dog? IntechOpen: London, UK, 2019. [Google Scholar] [CrossRef]
- Duruibe, J.O.; Ogwuegbu, M.O.C.; Egwurugwu, J.N. Heavy metal pollution and human biotoxic effects. Int. J. Phys. Sci. 2007, 2, 112–118. [Google Scholar]
- Chrestensen, C.A.; Starke, D.W.; Mieyal, J.J. Acute cadmium exposure inactivates thioltransferase (Glutaredoxin), inhibits intracellular reduction of protein-glutathionyl-mixed disulfides, and initiates apoptosis. J. Biol. Chem. 2000, 275, 26556–26565. [Google Scholar] [CrossRef]
- Berkholz, D.S.; Faber, H.R.; Savvides, S.N.; Karplus, P.A. Catalytic Cycle of Human Glutathione Reductase Near 1 Å Resolution. J. Mol. Biol. 2008, 382, 371–384. [Google Scholar] [CrossRef]
- Shekhawat, K.; Chatterjee, S.; Joshi, B. Chromium Toxicity and its Health Hazards. Int. J. Adv. Res. 2015, 7, 167–172. [Google Scholar]
- Franco, J.L.; Posser, T.; Mattos, J.J.; Sánchez-Chardi, A.; Trevisan, R.; Oliveira, C.S.; Carvalho, P.S.M.; Leal, R.B.; Marques, M.R.F.; Bainy, A.C.D.; et al. Biochemical alterations in juvenile carp (Cyprinus carpio) exposed to zinc: Glutathione reductase as a target. Mar. Environ. Res. 2008, 66, 88–89. [Google Scholar] [CrossRef] [PubMed]
- Hansen, J.M.; Zhang, H.; Jones, D.P. Differential oxidation of thioredoxin-1, thioredoxin-2, and glutathione by metal ions. Free Radic. Biol. Med. 2006, 40, 138–145. [Google Scholar] [CrossRef] [PubMed]
- Syed, S.; Zubair, A.; Frieri, M. Immune response to nanomaterials: Implications for medicine and literature review. Curr. Allergy Asthma Rep. 2013, 13, 50–57. [Google Scholar] [CrossRef]
- Muhammad, Q.; Jang, Y.; Kang, S.H.; Moon, J.; Kim, W.J.; Park, H. Modulation of immune responses with nanoparticles and reduction of their immunotoxicity. Biomater. Sci. 2020, 8, 1490–1501. [Google Scholar] [CrossRef]
- Kononenko, V.; Narat, M.; Drobne, D. Nanoparticle interaction with the immune system. Arh. Hig. Rada Toksikol. 2015, 66, 97–108. [Google Scholar] [CrossRef]
- Roy, R.; Parashar, V.; Chauhan, L.K.S.; Shanker, R.; Das, M.; Tripathi, A.; Dwivedi, P.D. Mechanism of uptake of ZnO nanoparticles and inflammatory responses in macrophages require PI3K mediated MAPKs signaling. Toxicol. Vitr. 2014, 28, 457–467. [Google Scholar] [CrossRef]
- Dwivedi, P.D.; Misra, A.; Shanker, R.; Das, M. Are nanomaterials a threat to the immune system? Nanotoxicology 2009, 3, 19–26. [Google Scholar] [CrossRef]
- Małaczewska, J. The splenocyte proliferative response and cytokine secretion in mice after 28-day oral administration of silver nanocolloid. Pol. J. Vet. Sci. 2014, 17, 27–35. [Google Scholar] [CrossRef]
- Shi, G.; Chen, W.; Zhang, Y.; Dai, X.; Zhang, X.; Wu, Z. An Antifouling Hydrogel Containing Silver Nanoparticles for Modulating the Therapeutic Immune Response in Chronic Wound Healing. Langmuir 2019, 35, 1837–1845. [Google Scholar] [CrossRef]
- Njoroge, J.M.; Yourick, J.J.; Principato, M.A. A flow cytometric analysis of macrophage– nanoparticle interactions in vitro: Induction of altered Toll-like receptor expression. Int. J. Nanomed. 2018, 13, 8365–8378. [Google Scholar] [CrossRef] [PubMed]
- Vasilichin, V.A.; Tsymbal, S.A.; Fakhardo, A.F.; Anastasova, E.I.; Marchenko, A.S.; Shtil, A.A.; Vinogradov, V.V.; Koshel, E.I. Effects of metal oxide nanoparticles on toll-like receptor mRNAs in human monocytes. Nanomaterials 2020, 10, 127. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Huang, T.; Wang, Y.; Pan, B.; Zhang, L.; Zhang, Q.; Niu, Q. Toxicity of alumina nanoparticles in the immune system of mice. Nanomedicine 2020, 15, 927–946. [Google Scholar] [CrossRef] [PubMed]
- Tang, S.; Zhou, L.; Liu, Z.; Zou, L.; Xiao, M.; Huang, C.; Xie, Z.; He, H.; Guo, Y.; Cao, Y.; et al. Ceria nanoparticles promoted the cytotoxic activity of CD8(+) T cells by activating NF-κB signaling. Biomater. Sci. 2019, 7, 2533–2544. [Google Scholar] [CrossRef] [PubMed]
- Holan, V.; Javorkova, E.; Vrbova, K.; Vecera, Z.; Mikuska, P.; Coufalik, P.; Kulich, P.; Skoupy, R.; Machala, M.; Zajicova, A.; et al. A murine model of the effects of inhaled CuO nanoparticles on cells of innate and adaptive immunity–a kinetic study of a continuous three-month exposure. Nanotoxicology 2019, 13, 952–963. [Google Scholar] [CrossRef]
- Jin, R.; Liu, L.; Zhu, W.; Li, D.; Yang, L.; Duan, J.; Cai, Z.; Nie, Y.; Zhang, Y.; Gong, Q.; et al. Iron oxide nanoparticles promote macrophage autophagy and inflammatory response through activation of toll-like Receptor-4 signaling. Biomaterials 2019, 203, 23–30. [Google Scholar] [CrossRef]
- De Jong, W.H.; Van Der Ven, L.T.M.; Sleijffers, A.; Park, M.V.D.Z.; Jansen, E.H.J.M.; Van Loveren, H.; Vandebriel, R.J. Systemic and immunotoxicity of silver nanoparticles in an intravenous 28 days repeated dose toxicity study in rats. Biomaterials 2013, 34, 8333–8343. [Google Scholar] [CrossRef]
- Roach, K.A.; Anderson, S.E.; Stefaniak, A.B.; Shane, H.L.; Boyce, G.R.; Roberts, J.R. Evaluation of the skin-sensitizing potential of gold nanoparticles and the impact of established dermal sensitivity on the pulmonary immune response to various forms of gold. Nanotoxicology 2020, 14, 1096–1117. [Google Scholar] [CrossRef]
- Perez Ruiz De Garibay, A.; Spinato, C.; Klippstein, R.; Bourgognon, M.; Martincic, M.; Pach, E.; Ballesteros, B.; Ménard-Moyon, C.; Al-Jamal, K.T.; Tobias, G.; et al. Evaluation of the immunological profile of antibody-functionalized metal-filled single-walled carbon nanocapsules for targeted radiotherapy. Sci. Rep. 2017, 7, 1–12. [Google Scholar] [CrossRef]
- Lahiani, M.H.; Gokulan, K.; Williams, K.; Khodakovskaya, M.V.; Khare, S. Graphene and carbon nanotubes activate different cell surface receptors on macrophages before and after deactivation of endotoxins. J. Appl. Toxicol. 2017, 37, 1305–1316. [Google Scholar] [CrossRef]
- Vandebriel, R.J.; Tonk, E.C.M.; de la Fonteyne-Blankestijn, L.J.; Gremmer, E.R.; Verharen, H.W.; van der Ven, L.T.; van Loveren, H.; de Jong, W.H. Immunotoxicity of silver nanoparticles in an intravenous 28-day repeated-dose toxicity study in rats. Part. Fibre Toxicol. 2014, 11, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Devanabanda, M.; Latheef, S.A.; Madduri, R. Immunotoxic effects of gold and silver nanoparticles: Inhibition of mitogen-induced proliferative responses and viability of human and murine lymphocytes in vitro. J. Immunotoxicol. 2016, 13, 897–902. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Zeng, Z.; Ying, H.; Wu, C.; Chen, S. Superparamagnetic iron oxide nanoparticles attenuate lipopolysaccharide-induced inflammatory responses through modulation of toll-like receptor 4 expression. J. Appl. Toxicol. 2020, 40, 1067–1075. [Google Scholar] [CrossRef] [PubMed]
- Lim, K.-H.; Staudt, L.M. Toll-like receptor signaling. Cold Spring Harb. Perspect. Biol. 2013, 5, a011247. [Google Scholar] [CrossRef]
- Chen, L.; Deng, H.; Cui, H.; Fang, J.; Zuo, Z.; Deng, J.; Li, Y.; Wang, X.; Zhao, L. Inflammatory responses and inflammation-associated diseases in organs. Oncotarget 2018, 9, 7204–7218. [Google Scholar] [CrossRef]
- Lappas, C.M. The immunomodulatory effects of titanium dioxide and silver nanoparticles. Food Chem. Toxicol. Int. J. Publ. Br. Ind. Biol. Res. Assoc. 2015, 85, 78–83. [Google Scholar] [CrossRef]
- Luo, Y.-H.; Chang, L.W.; Lin, P. Metal-Based Nanoparticles and the Immune System: Activation, Inflammation, and Potential Applications. Biomed Res. Int. 2015, 2015, 143720. [Google Scholar] [CrossRef]
- Victor, V.M.; Rocha, M.; De La Fuente, M. Immune cells: Free radicals and antioxidants in sepsis. Int. Immunopharmacol. 2004, 4, 327–347. [Google Scholar] [CrossRef]
- Bryan, N.S.; Ka, B.; Murad, F. Discovery of the nitric oxide signaling pathway and targets for drug development Nathan. Front. Biosci. 2009, 14, 1–18. [Google Scholar] [CrossRef]
- Azimipour, S.; Ghaedi, S.; Mehrabi, Z.; Ghasemzadeh, S.A.; Heshmati, M.; Barikrow, N.; Attar, F.; Falahati, M. Heme degradation and iron release of hemoglobin and oxidative stress of lymphocyte cells in the presence of silica nanoparticles. Int. J. Biol. Macromol. 2018, 118, 800–807. [Google Scholar] [CrossRef]
- Barbasz, A.; Oćwieja, M.; Barbasz, J. Cytotoxic Activity of Highly Purified Silver Nanoparticles Sol against Cells of Human Immune System. Appl. Biochem. Biotechnol. 2015, 176, 817–834. [Google Scholar] [CrossRef] [PubMed]
- Gurunathan, S.; Kang, M.-H.; Jeyaraj, M.; Kim, J.-H. Differential Immunomodulatory Effect of Graphene Oxide and Vanillin-Functionalized Graphene Oxide Nanoparticles in Human Acute Monocytic Leukemia Cell Line (THP-1). Int. J. Mol. Sci. 2019, 20, 247. [Google Scholar] [CrossRef] [PubMed]
- Stevenson, R.; Hueber, A.J.; Hutton, A.; McInnes, I.B.; Graham, D. Nanoparticles and inflammation. ScientificWorldJournal 2011, 11, 1300–1312. [Google Scholar] [CrossRef] [PubMed]
- Boraschi, D.; Italiani, P.; Palomba, R.; Decuzzi, P.; Duschl, A.; Fadeel, B.; Moghimi, S.M. Nanoparticles and innate immunity: New perspectives on host defence. Semin. Immunol. 2017, 34, 33–51. [Google Scholar] [CrossRef] [PubMed]
- Di Cristo, L.; Movia, D.; Bianchi, M.G.; Allegri, M.; Mohamed, B.M.; Bell, A.P.; Moore, C.; Pinelli, S.; Rasmussen, K.; Riego-Sintes, J.; et al. Proinflammatory Effects of Pyrogenic and Precipitated Amorphous Silica Nanoparticles in Innate Immunity Cells. Toxicol. Sci. 2016, 150, 40–53. [Google Scholar] [CrossRef]
- Ko, J.-W.; Shin, N.-R.; Je-Oh, L.; Jung, T.-Y.; Moon, C.; Kim, T.-W.; Choi, J.; Shin, I.-S.; Heo, J.-D.; Kim, J.-C. Silica dioxide nanoparticles aggravate airway inflammation in an asthmatic mouse model via NLRP3 inflammasome activation. Regul. Toxicol. Pharmacol. 2020, 112, 104618. [Google Scholar] [CrossRef]
- Kumar, S.; Meena, R.; Paulraj, R. Role of Macrophage (M1 and M2) in Titanium-Dioxide Nanoparticle-Induced Oxidative Stress and Inflammatory Response in Rat. Appl. Biochem. Biotechnol. 2016, 180, 1257–1275. [Google Scholar] [CrossRef]
- Li, Y.; Monteiro-Riviere, N.A. Mechanisms of cell uptake, inflammatory potential and protein corona effects with gold nanoparticles. Nanomedicine 2016, 11, 3185–3203. [Google Scholar] [CrossRef]
- Lim, J.-O.; Shin, N.-R.; Seo, Y.-S.; Nam, H.-H.; Ko, J.-W.; Jung, T.-Y.; Lee, S.-J.; Kim, H.-J.; Cho, Y.-K.; Kim, J.-C.; et al. Silibinin Attenuates Silica Dioxide Nanoparticles-Induced Inflammation by Suppressing TXNIP/MAPKs/AP-1 Signaling. Cells 2020, 9, 678. [Google Scholar] [CrossRef]
- Liu, N.; Tang, M. Toxic effects and involved molecular pathways of nanoparticles on cells and subcellular organelles. J. Appl. Toxicol. 2020, 40, 16–36. [Google Scholar] [CrossRef]
- Murphy, F.A.; Schinwald, A.; Poland, C.A.; Donaldson, K. The mechanism of pleural inflammation by long carbon nanotubes: Interaction of long fibres with macrophages stimulates them to amplify pro-inflammatory responses in mesothelial cells. Part. Fibre Toxicol. 2012, 9, 8. [Google Scholar] [CrossRef]
- Schanen, B.C.; Das, S.; Reilly, C.M.; Warren, W.L.; Self, W.T.; Seal, S.; Drake, D.R. 3rd Immunomodulation and T helper TH1/TH2 response polarization by CeO2 and TiO2 nanoparticles. PLoS ONE 2013, 8, e62816. [Google Scholar] [CrossRef] [PubMed]
- Senapati, V.A.; Kumar, A.; Gupta, G.S.; Pandey, A.K.; Dhawan, A. ZnO nanoparticles induced inflammatory response and genotoxicity in human blood cells: A mechanistic approach. Food Chem. Toxicol. Int. J. Publ. Br. Ind. Biol. Res. Assoc. 2015, 85, 61–70. [Google Scholar] [CrossRef] [PubMed]
- Pandey, R.K.; Prajapati, V.K. Molecular and immunological toxic effects of nanoparticles. Int. J. Biol. Macromol. 2018, 107, 1278–1293. [Google Scholar] [CrossRef]
- Sharma, N.; Jha, S. Amorphous nanosilica induced toxicity, inflammation and innate immune responses: A critical review. Toxicology 2020, 441, 152519. [Google Scholar] [CrossRef]
- Mostafalou, S.; Mohammadi, H.; Ramazani, A.; Abdollahi, M. Different biokinetics of nanomedicines linking to their toxicity; an overview. Daru 2013, 21, 14. [Google Scholar] [CrossRef]
- Lacy, P.; Stow, J.L. Cytokine release from innate immune cells: Association with diverse membrane trafficking pathways. Blood 2011, 118, 9–18. [Google Scholar] [CrossRef] [PubMed]
- Åkerlund, E.; Islam, M.S.; McCarrick, S.; Alfaro-Moreno, E.; Karlsson, H.L. Inflammation and (secondary) genotoxicity of Ni and NiO nanoparticles. Nanotoxicology 2019, 13, 1060–1072. [Google Scholar] [CrossRef]
- Di Gioacchino, M.; Petrarca, C.; Lazzarin, F.; Di Giampaolo, L.; Sabbioni, E.; Boscolo, P.; Mariani-Costantini, R.; Bernardini, G. Immunotoxicity of nanoparticles. Int. J. Immunopathol. Pharmacol. 2011, 24, 75–94. [Google Scholar] [CrossRef]
- Zhao, F.; Wang, C.; Yang, Q.; Han, S.; Hu, Q.; Fu, Z. Titanium dioxide nanoparticle stimulating pro-inflammatory responses in vitro and in vivo for inhibited cancer metastasis. Life Sci. 2018, 202, 44–51. [Google Scholar] [CrossRef]
- Isoda, K.; Daibo, T.; Yushina, K.; Yoshioka, Y.; Tsutsumi, Y.; Akimoto, Y.; Kawakami, H.; Taira, Y.; Taira, I.; Yanoshita, R.; et al. Hepatotoxicity, nephrotoxicity, and drug/chemical interaction toxicity of platinum nanoparticles in mice. Pharmazie 2017, 72, 10–16. [Google Scholar] [CrossRef]
- Tian, L.; Lin, B.; Wu, L.; Li, K.; Liu, H.; Yan, J.; Liu, X.; Xi, Z. Neurotoxicity induced by zinc oxide nanoparticles: Age-related differences and interaction. Sci. Rep. 2015, 5, 16117. [Google Scholar] [CrossRef] [PubMed]
- You, D.J.; Lee, H.Y.; Taylor-Just, A.J.; Linder, K.E.; Bonner, J.C. Sex differences in the acute and subchronic lung inflammatory responses of mice to nickel nanoparticles. Nanotoxicology 2020, 14, 1058–1081. [Google Scholar] [CrossRef] [PubMed]
- Dakal, T.C.; Kumar, A.; Majumdar, R.S.; Yadav, V. Mechanistic Basis of Antimicrobial Actions of Silver Nanoparticles. Front. Microbiol. 2016, 7, 1831. [Google Scholar] [CrossRef] [PubMed]
- Paula, M.M.S.; Petronilho, F.; Vuolo, F.; Ferreira, G.K.; De Costa, L.; Santos, G.P.; Effting, P.S.; Dal-Pizzol, F.; Dal-Bó, A.G.; Frizon, T.E.; et al. Gold nanoparticles and/or N-acetylcysteine mediate carrageenan-induced inflammation and oxidative stress in a concentration-dependent manner. J. Biomed. Mater. Res. A 2015, 103, 3323–3330. [Google Scholar] [CrossRef]
- Liu, Y.; Kim, S.; Kim, Y.J.; Perumalsamy, H.; Lee, S.; Hwang, E.; Yi, T.H. Green synthesis of gold nanoparticles using Euphrasia officinalis leaf extract to inhibit lipopolysaccharide-induced inflammation through NF-κB and JAK/STAT pathways in RAW 264.7 macrophages. Int. J. Nanomed. 2019, 14, 2945–2959. [Google Scholar] [CrossRef]
- Zhang, Q.; Hitchins, V.M.; Schrand, A.M.; Hussain, S.M.; Goering, P.L. Uptake of gold nanoparticles in murine macrophage cells without cytotoxicity or production of pro-inflammatory mediators. Nanotoxicology 2011, 5, 284–295. [Google Scholar] [CrossRef]
- Xu, J.; Wang, J.; Qiu, J.; Liu, H.; Wang, Y.; Cui, Y.; Humphry, R.; Wang, N.; DurKan, C.; Chen, Y.; et al. Nanoparticles retard immune cells recruitment in vivo by inhibiting chemokine expression. Biomaterials 2021, 265, 120392. [Google Scholar] [CrossRef]
- Gonzalez-Carter, D.A.; Leo, B.F.; Ruenraroengsak, P.; Chen, S.; Goode, A.E.; Theodorou, I.G.; Chung, K.F.; Carzaniga, R.; Shaffer, M.S.P.; Dexter, D.T.; et al. Silver nanoparticles reduce brain inflammation and related neurotoxicity through induction of H(2)S-synthesizing enzymes. Sci. Rep. 2017, 7, 42871. [Google Scholar] [CrossRef]
- Li, X.; Zhen, M.; Zhou, C.; Deng, R.; Yu, T.; Wu, Y.; Shu, C.; Wang, C.; Bai, C. Gadofullerene Nanoparticles Reverse Dysfunctions of Pancreas and Improve Hepatic Insulin Resistance for Type 2 Diabetes Mellitus Treatment. ACS Nano 2019, 13, 8597–8608. [Google Scholar] [CrossRef]
- Abdulmalek, S.A.; Balbaa, M. Synergistic effect of nano-selenium and metformin on type 2 diabetic rat model: Diabetic complications alleviation through insulin sensitivity, oxidative mediators and inflammatory markers. PLoS ONE 2019, 14, e0220779. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Zhang, Y.; Yuan, Y.; Yue, T. Immunomodulatory of selenium nanoparticles decorated by sulfated Ganoderma lucidum polysaccharides. Food Chem. Toxicol. 2014, 68, 183–189. [Google Scholar] [CrossRef] [PubMed]
- Wu, T.; Tang, M. The inflammatory response to silver and titanium dioxide nanoparticles in the central nervous system. Nanomedicine 2018, 13, 233–249. [Google Scholar] [CrossRef] [PubMed]
- Christen, V.; Fent, K. Silica nanoparticles induce endoplasmic reticulum stress response and activate mitogen activated kinase (MAPK) signalling. Toxicol. Rep. 2016, 3, 832–840. [Google Scholar] [CrossRef]
- Nishanth, R.P.; Jyotsna, R.G.; Schlager, J.J.; Hussain, S.M.; Reddanna, P. Inflammatory responses of RAW 264.7 macrophages upon exposure to nanoparticles: Role of ROS-NFκB signaling pathway. Nanotoxicology 2011, 5, 502–516. [Google Scholar] [CrossRef]
- Park, S.Y.; Yi, E.H.; Kim, Y.; Park, G. Anti-neuroinflammatory effects of Ephedra sinica Stapf extract-capped gold nanoparticles in microglia. Int. J. Nanomed. 2019, 14, 2861–2877. [Google Scholar] [CrossRef]
- Romoser, A.A.; Chen, P.L.; Berg, J.M.; Seabury, C.; Ivanov, I.; Criscitiello, M.F.; Sayes, C.M. Quantum dots trigger immunomodulation of the NFκB pathway in human skin cells. Mol. Immunol. 2011, 48, 1349–1359. [Google Scholar] [CrossRef]
- Simón-Vázquez, R.; Lozano-Fernández, T.; Dávila-Grana, A.; González-Fernández, A. Metal oxide nanoparticles interact with immune cells and activate different cellular responses. Int. J. Nanomed. 2016, 11, 4657–4668. [Google Scholar] [CrossRef]
- Liang, H.; Chen, A.; Lai, X.; Liu, J.; Wu, J.; Kang, Y.; Wang, X.; Shao, L. Neuroinflammation is induced by tongue-instilled ZnO nanoparticles via the Ca(2+)-dependent NF-κB and MAPK pathways. Part. Fibre Toxicol. 2018, 15, 39. [Google Scholar] [CrossRef]
- Yang, Y.; Wang, H.; Kouadir, M.; Song, H.; Shi, F. Recent advances in the mechanisms of NLRP3 inflammasome activation and its inhibitors. Cell Death Dis. 2019, 10, 128. [Google Scholar] [CrossRef]
- Małaczewska, J. The in vitro effect of commercially available noble metal nanocolloids on the splenocyte proliferative response and cytokine production in mice. Pol. J. Vet. Sci. 2014, 17, 37–45. [Google Scholar] [CrossRef] [PubMed]
- Sasabe, E.; Tomomura, A.; Kitamura, N.; Yamamoto, T. Metal nanoparticles-induced activation of NLRP3 inflammasome in human oral keratinocytes is a possible mechanism of oral lichenoid lesions. Toxicol. Vitr. 2020, 62, 104663. [Google Scholar] [CrossRef] [PubMed]
- Deng, Z.J.; Liang, M.; Monteiro, M.; Toth, I.; Minchin, R.F. Nanoparticle-induced unfolding of fibrinogen promotes Mac-1 receptor activation and inflammation. Nat. Nanotechnol. 2011, 6, 39–44. [Google Scholar] [CrossRef] [PubMed]
- Singh, P.; Ahn, S.; Kang, J.P.; Veronika, S.; Huo, Y.; Singh, H.; Chokkaligam, M.; El-Agamy Farh, M.; Aceituno, V.C.; Kim, Y.J.; et al. In vitro anti-inflammatory activity of spherical silver nanoparticles and monodisperse hexagonal gold nanoparticles by fruit extract of Prunus serrulata: A green synthetic approach. Artif. Cells Nanomed. Biotechnol. 2018, 46, 2022–2032. [Google Scholar] [CrossRef]
- Fehaid, A.; Taniguchi, A. Silver nanoparticles reduce the apoptosis induced by tumor necrosis factor-α. Sci. Technol. Adv. Mater. 2018, 19, 526–534. [Google Scholar] [CrossRef]
- Park, M.V.D.Z.; Neigh, A.M.; Vermeulen, J.P.; de la Fonteyne, L.J.J.; Verharen, H.W.; Briedé, J.J.; van Loveren, H.; de Jong, W.H. The effect of particle size on the cytotoxicity, inflammation, developmental toxicity and genotoxicity of silver nanoparticles. Biomaterials 2011, 32, 9810–9817. [Google Scholar] [CrossRef]
- Li, L.; Bi, Z.; Hu, Y.; Sun, L.; Song, Y.; Chen, S.; Mo, F.; Yang, J.; Wei, Y.; Wei, X. Silver nanoparticles and silver ions cause inflammatory response through induction of cell necrosis and the release of mitochondria in vivo and in vitro. Cell Biol. Toxicol. 2020, 37, 177–191. [Google Scholar] [CrossRef]
- Jabir, M.S.; Saleh, Y.M.; Sulaiman, G.M.; Yaseen, N.Y.; Sahib, U.I.; Dewir, Y.H.; Alwahibi, M.S.; Soliman, D.A. Green Synthesis of Silver Nanoparticles Using Annona muricata Extract as an Inducer of Apoptosis in Cancer Cells and Inhibitor for NLRP3 Inflammasome via Enhanced Autophagy. Nanomaterials 2021, 11, 384. [Google Scholar] [CrossRef]
- De Astis, S.; Corradini, I.; Morini, R.; Rodighiero, S.; Tomasoni, R.; Lenardi, C.; Verderio, C.; Milani, P.; Matteoli, M. Nanostructured TiO2 surfaces promote polarized activation of microglia, but not astrocytes, toward a proinflammatory profile. Nanoscale 2013, 5, 10963–10974. [Google Scholar] [CrossRef]
- Lin, H.-C.; Huang, C.-L.; Huang, Y.-J.; Hsiao, I.-L.; Yang, C.-W.; Chuang, C.-Y. Transcriptomic gene-network analysis of exposure to silver nanoparticle reveals potentially neurodegenerative progression in mouse brain neural cells. Toxicol. Vitr. 2016, 34, 289–299. [Google Scholar] [CrossRef]
- Huang, C.-L.; Hsiao, I.-L.; Lin, H.-C.; Wang, C.-F.; Huang, Y.-J.; Chuang, C.-Y. Silver nanoparticles affect on gene expression of inflammatory and neurodegenerative responses in mouse brain neural cells. Environ. Res. 2015, 136, 253–263. [Google Scholar] [CrossRef]
- Murphy, A.; Casey, A.; Byrne, G.; Chambers, G.; Howe, O. Silver nanoparticles induce pro-inflammatory gene expression and inflammasome activation in human monocytes. J. Appl. Toxicol. 2016, 36, 1311–1320. [Google Scholar] [CrossRef]
- Mishra, A.R.; Zheng, J.; Tang, X.; Goering, P.L. Silver nanoparticle-induced autophagic-Lysosomal disruption and NLRP3-inflammasome activation in HepG2 cells is size-dependent. Toxicol. Sci. 2016, 150, 473–487. [Google Scholar] [CrossRef] [PubMed]
- Simard, J.C.; Vallieres, F.; De Liz, R.; Lavastre, V.; Girard, D. Silver nanoparticles induce degradation of the endoplasmic reticulum stress sensor activating transcription factor-6 Leading to activation of the NLRP-3 Inflammasome. J. Biol. Chem. 2015, 290, 5926–5939. [Google Scholar] [CrossRef] [PubMed]
- Yang, E.-J.; Kim, S.; Kim, J.S.; Choi, I.-H. Inflammasome formation and IL-1β release by human blood monocytes in response to silver nanoparticles. Biomaterials 2012, 33, 6858–6867. [Google Scholar] [CrossRef] [PubMed]
- Ramadi, K.B.; Mohamed, Y.A.; Al-Sbiei, A.; Almarzooqi, S.; Bashir, G.; Al Dhanhani, A.; Sarawathiamma, D.; Qadri, S.; Yasin, J.; Nemmar, A.; et al. Acute systemic exposure to silver-based nanoparticles induces hepatotoxicity and NLRP3-dependent inflammation. Nanotoxicology 2016, 10, 1061–1074. [Google Scholar] [CrossRef]
- Giovanni, M.; Yue, J.; Zhang, L.; Xie, J.; Ong, C.N.; Leong, D.T. Pro-inflammatory responses of RAW264.7 macrophages when treated with ultralow concentrations of silver, titanium dioxide, and zinc oxide nanoparticles. J. Hazard. Mater. 2015, 297, 146–152. [Google Scholar] [CrossRef]
- Hsin, Y.-H.; Chen, C.-F.; Huang, S.; Shih, T.-S.; Lai, P.-S.; Chueh, P.J. The apoptotic effect of nanosilver is mediated by a ROS- and JNK-dependent mechanism involving the mitochondrial pathway in NIH3T3 cells. Toxicol. Lett. 2008, 179, 130–139. [Google Scholar] [CrossRef]
- Poon, W.-L.; Lee, J.C.-Y.; Leung, K.S.; Alenius, H.; El-Nezami, H.; Karisola, P. Nanosized silver, but not titanium dioxide or zinc oxide, enhances oxidative stress and inflammatory response by inducing 5-HETE activation in THP-1 cells. Nanotoxicology 2020, 14, 453–467. [Google Scholar] [CrossRef]
- Hayashi, Y.; Engelmann, P.; Foldbjerg, R.; Szabó, M.; Somogyi, I.; Pollák, E.; Molnár, L.; Autrup, H.; Sutherland, D.S.; Scott-Fordsmand, J.; et al. Earthworms and humans in vitro: Characterizing evolutionarily conserved stress and immune responses to silver nanoparticles. Environ. Sci. Technol. 2012, 46, 4166–4173. [Google Scholar] [CrossRef]
- Shavandi, Z.; Ghazanfari, T.; Moghaddam, K.N. In vitro toxicity of silver nanoparticles on murine peritoneal macrophages. Immunopharmacol. Immunotoxicol. 2011, 33, 135–140. [Google Scholar] [CrossRef] [PubMed]
- Baron, L.; Gombault, A.; Fanny, M.; Villeret, B.; Savigny, F.; Guillou, N.; Panek, C.; Le Bert, M.; Lagente, V.; Rassendren, F.; et al. The NLRP3 inflammasome is activated by nanoparticles through ATP, ADP and adenosine. Cell Death Dis. 2015, 6, e1629. [Google Scholar] [CrossRef] [PubMed]
- Hong, J.; Wang, L.; Zhao, X.; Yu, X.; Sheng, L.; Xu, B.; Liu, D.; Zhu, Y.; Long, Y.; Hong, F. Th2 factors may be involved in TiO2; NP-induced hepatic inflammation. J. Agric. Food Chem. 2014, 62, 6871–6878. [Google Scholar] [CrossRef]
- Borgognoni, C.F.; Mormann, M.; Qu, Y.; Schäfer, M.; Langer, K.; Öztürk, C.; Wagner, S.; Chen, C.; Zhao, Y.; Fuchs, H.; et al. Reaction of human macrophages on protein corona covered TiO2; nanoparticles. Nanomedicine 2015, 11, 275–282. [Google Scholar] [CrossRef]
- Yazdi, A.S.; Guarda, G.; Riteau, N.; Drexler, S.K.; Tardivel, A.; Couillin, I.; Tschopp, J. Nanoparticles activate the NLR pyrin domain containing 3 (Nlrp3) inflammasome and cause pulmonary inflammation through release of IL-1α and IL-1β. Proc. Natl. Acad. Sci. USA 2010, 107, 19449–19454. [Google Scholar] [CrossRef] [PubMed]
- Ruiz, P.A.; Morón, B.; Becker, H.M.; Lang, S.; Atrott, K.; Spalinger, M.R.; Scharl, M.; Wojtal, K.A.; Fischbeck-Terhalle, A.; Frey-Wagner, I.; et al. Titanium dioxide nanoparticles exacerbate DSS-induced colitis: Role of the NLRP3 inflammasome. Gut 2017, 66, 1216–1224. [Google Scholar] [CrossRef]
- Trouiller, B.; Reliene, R.; Westbrook, A.; Solaimani, P.; Schiestl, R.H. Titanium dioxide nanoparticles induce DNA damage and genetic instability in vivo in mice. Cancer Res. 2009, 69, 8784–8789. [Google Scholar] [CrossRef] [PubMed]
- Leonoudakis, D.; Rane, A.; Angeli, S.; Lithgow, G.J.; Andersen, J.K.; Chinta, S.J. Anti-Inflammatory and Neuroprotective Role of Natural Product Securinine in Activated Glial Cells: Implications for Parkinson’s Disease. Mediat. Inflamm. 2017, 2017, 8302636. [Google Scholar] [CrossRef]
- Chen, P.; Kanehira, K.; Taniguchi, A. Role of toll-like receptors 3, 4 and 7 in cellular uptake and response to titanium dioxide nanoparticles. Sci. Technol. Adv. Mater. 2013, 14, 15008. [Google Scholar] [CrossRef]
- Montiel-Dávalos, A.; Ventura-Gallegos, J.L.; Alfaro-Moreno, E.; Soria-Castro, E.; García-Latorre, E.; Cabañas-Moreno, J.G.; del Pilar Ramos-Godinez, M.; López-Marure, R. TiO2 nanoparticles induce dysfunction and activation of human endothelial cells. Chem. Res. Toxicol. 2012, 25, 920–930. [Google Scholar] [CrossRef]
- Romoser, A.A.; Figueroa, D.E.; Sooresh, A.; Scribner, K.; Chen, P.L.; Porter, W.; Criscitiello, M.F.; Sayes, C.M. Distinct immunomodulatory effects of a panel of nanomaterials in human dermal fibroblasts. Toxicol. Lett. 2012, 210, 293–301. [Google Scholar] [CrossRef] [PubMed]
- Sun, B.; Wang, X.; Ji, Z.; Li, R.; Xia, T. NLRP3 inflammasome activation induced by engineered nanomaterials. Small 2013, 9, 1595–1607. [Google Scholar] [CrossRef] [PubMed]
- Winter, M.; Beer, H.-D.; Hornung, V.; Krämer, U.; Schins, R.P.F.; Förster, I. Activation of the inflammasome by amorphous silica and TiO2 nanoparticles in murine dendritic cells. Nanotoxicology 2011, 5, 326–340. [Google Scholar] [CrossRef] [PubMed]
- Muller, A.P.; Ferreira, G.K.; Pires, A.J.; de Bem Silveira, G.; de Souza, D.L.; de Abreu Brandolfi, J.; de Souza, C.T.; Paula, M.M.S.; Silveira, P.C.L. Gold nanoparticles prevent cognitive deficits, oxidative stress and inflammation in a rat model of sporadic dementia of Alzheimer’s type. Mater. Sci. Eng. C Mater. Biol. Appl. 2017, 77, 476–483. [Google Scholar] [CrossRef] [PubMed]
- Pedersen, M.O.; Larsen, A.; Pedersen, D.S.; Stoltenberg, M.; Penkowa, M. Metallic gold reduces TNFalpha expression, oxidative DNA damage and pro-apoptotic signals after experimental brain injury. Brain Res. 2009, 1271, 103–113. [Google Scholar] [CrossRef]
- Guo, C.; Yang, M.; Jing, L.; Wang, J.; Yu, Y.; Li, Y.; Duan, J.; Zhou, X.; Li, Y.; Sun, Z. Amorphous silica nanoparticles trigger vascular endothelial cell injury through apoptosis and autophagy via reactive oxygen species-mediated MAPK/Bcl-2 and PI3K/Akt/mTOR signaling. Int. J. Nanomed. 2016, 11, 5257–5276. [Google Scholar] [CrossRef]
- Ma, J.; Liu, R.; Wang, X.; Liu, Q.; Chen, Y.; Valle, R.P.; Zuo, Y.Y.; Xia, T.; Liu, S. Crucial Role of Lateral Size for Graphene Oxide in Activating Macrophages and Stimulating Pro-inflammatory Responses in Cells and Animals. ACS Nano 2015, 9, 10498–10515. [Google Scholar] [CrossRef]
- Duch, M.C.; Budinger, G.R.S.; Liang, Y.T.; Soberanes, S.; Urich, D.; Chiarella, S.E.; Campochiaro, L.A.; Gonzalez, A.; Chandel, N.S.; Hersam, M.C.; et al. Minimizing oxidation and stable nanoscale dispersion improves the biocompatibility of graphene in the lung. Nano Lett. 2011, 11, 5201–5207. [Google Scholar] [CrossRef]
- Schinwald, A.; Murphy, F.; Askounis, A.; Koutsos, V.; Sefiane, K.; Donaldson, K.; Campbell, C.J. Minimal oxidation and inflammogenicity of pristine graphene with residence in the lung. Nanotoxicology 2014, 8, 824–832. [Google Scholar] [CrossRef]
- Yue, H.; Wei, W.; Yue, Z.; Wang, B.; Luo, N.; Gao, Y.; Ma, D.; Ma, G.; Su, Z. The role of the lateral dimension of graphene oxide in the regulation of cellular responses. Biomaterials 2012, 33, 4013–4021. [Google Scholar] [CrossRef]
- Feito, M.J.; Vila, M.; Matesanz, M.C.; Linares, J.; Gonçalves, G.; Marques, P.A.A.P.; Vallet-Regí, M.; Rojo, J.M.; Portolés, M.T. In vitro evaluation of graphene oxide nanosheets on immune function. J. Colloid Interface Sci. 2014, 432, 221–228. [Google Scholar] [CrossRef] [PubMed]
- Orecchioni, M.; Ménard-Moyon, C.; Delogu, L.G.; Bianco, A. Graphene and the immune system: Challenges and potentiality. Adv. Drug Deliv. Rev. 2016, 105, 163–175. [Google Scholar] [CrossRef] [PubMed]
- Brown, D.M.; Dickson, C.; Duncan, P.; Al-Attili, F.; Stone, V. Interaction between nanoparticles and cytokine proteins: Impact on protein and particle functionality. Nanotechnology 2010, 21, 215104. [Google Scholar] [CrossRef] [PubMed]
- Lategan, K.; Alghadi, H.; Bayati, M.; de Cortalezzi, M.F.; Pool, E. Effects of Graphene Oxide Nanoparticles on the Immune System Biomarkers Produced by RAW 264.7 and Human Whole Blood Cell Cultures. Nanomaterials 2018, 8, 125. [Google Scholar] [CrossRef]
- Ding, D.-Q.; Matsuda, A.; Okamasa, K.; Nagahama, Y.; Haraguchi, T.; Hiraoka, Y. Meiotic cohesin-based chromosome structure is essential for homologous chromosome pairing in Schizosaccharomyces pombe. Chromosoma 2016, 125, 205–214. [Google Scholar] [CrossRef]
- Sun, P.; Wang, K.; Zhu, H. Recent Developments in Graphene-Based Membranes: Structure, Mass-Transport Mechanism and Potential Applications. Adv. Mater. 2016, 28, 2287–2310. [Google Scholar] [CrossRef]
- Russier, J.; Treossi, E.; Scarsi, A.; Perrozzi, F.; Dumortier, H.; Ottaviano, L.; Meneghetti, M.; Palermo, V.; Bianco, A. Evidencing the mask effect of graphene oxide: A comparative study on primary human and murine phagocytic cells. Nanoscale 2013, 5, 11234–11247. [Google Scholar] [CrossRef]
- Zhou, H.; Zhao, K.; Li, W.; Yang, N.; Liu, Y.; Chen, C.; Wei, T. The interactions between pristine graphene and macrophages and the production of cytokines/chemokines via TLR- and NF-κB-related signaling pathways. Biomaterials 2012, 33, 6933–6942. [Google Scholar] [CrossRef]
- Selvaraj, V.; Nepal, N.; Rogers, S.; Manne, N.D.P.K.; Arvapalli, R.; Rice, K.M.; Asano, S.; Fankhanel, E.; Ma, J.J.; Shokuhfar, T.; et al. Inhibition of MAP kinase/NF-kB mediated signaling and attenuation of lipopolysaccharide induced severe sepsis by cerium oxide nanoparticles. Biomaterials 2015, 59, 160–171. [Google Scholar] [CrossRef]
- Heng, B.C.; Zhao, X.; Tan, E.C.; Khamis, N.; Assodani, A.; Xiong, S.; Ruedl, C.; Ng, K.W.; Loo, J.S.C. Evaluation of the cytotoxic and inflammatory potential of differentially shaped zinc oxide nanoparticles. Arch. Toxicol. 2011, 85, 1517–1528. [Google Scholar] [CrossRef]
- Solovyev, N.D. Importance of selenium and selenoprotein for brain function: From antioxidant protection to neuronal signalling. J. Inorg. Biochem. 2015, 153, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Sadek, K.M.; Lebda, M.A.; Abouzed, T.K.; Nasr, S.M.; Shoukry, M. Neuro- and nephrotoxicity of subchronic cadmium chloride exposure and the potential chemoprotective effects of selenium nanoparticles. Metab. Brain Dis. 2017, 32, 1659–1673. [Google Scholar] [CrossRef] [PubMed]
- Guo, X.; Lie, Q.; Liu, Y.; Jia, Z.; Gong, Y.; Yuan, X.; Liu, J. Multifunctional Selenium Quantum Dots for the Treatment of Alzheimer’s Disease by Reducing Aβ-Neurotoxicity and Oxidative Stress and Alleviate Neuroinflammation. ACS Appl. Mater. Interfaces 2021, 13, 30261–30273. [Google Scholar] [CrossRef] [PubMed]
- Ahn, S.; Singh, P.; Jang, M.; Kim, Y.J.; Castro-Aceituno, V.; Simu, S.Y.; Kim, Y.J.; Yang, D.C. Gold nanoflowers synthesized using Acanthopanacis cortex extract inhibit inflammatory mediators in LPS-induced RAW264.7 macrophages via NF-κB and AP-1 pathways. Colloids Surf. B Biointerfaces 2018, 162, 398–404. [Google Scholar] [CrossRef] [PubMed]
- Simard, J.C.; Durocher, I.; Girard, D. Silver nanoparticles induce irremediable endoplasmic reticulum stress leading to unfolded protein response dependent apoptosis in breast cancer cells. Apoptosis 2016, 21, 1279–1290. [Google Scholar] [CrossRef]
- McGuire, P.J. Mitochondrial Dysfunction and the Aging Immune System. Biology 2019, 8, 26. [Google Scholar] [CrossRef]
- Vafai, S.B.; Mootha, V.K. Mitochondrial disorders as windows into an ancient organelle. Nature 2012, 491, 374–383. [Google Scholar] [CrossRef]
- Li, J.; Zhang, B.; Chang, X.; Gan, J.; Li, W.; Niu, S.; Kong, L.; Wu, T.; Zhang, T.; Tang, M.; et al. Silver nanoparticles modulate mitochondrial dynamics and biogenesis in HepG2 cells. Environ. Pollut. 2020, 256, 113430. [Google Scholar] [CrossRef]
- Galluzzi, L.; Kepp, O.; Kroemer, G. Mitochondria: Master regulators of danger signalling. Nat. Rev. Mol. Cell Biol. 2012, 13, 780–788. [Google Scholar] [CrossRef]
- Ma, W.; He, S.; Ma, H.; Jiang, H.; Yan, N.; Zhu, L.; Bang, J.J.; Li, P.A.; Jia, S. Silver nanoparticle exposure causes pulmonary structural damage and mitochondrial dynamic imbalance in the rat: Protective effects of sodium selenite. Int. J. Nanomed. 2020, 15, 633–645. [Google Scholar] [CrossRef]
- Wang, C.; Youle, R.J. The Role of Mitochondria in Apoptosis. Annu. Rev. Genet. 2009, 43, 95–118. [Google Scholar] [CrossRef] [PubMed]
- Endo, H.; Kamada, H.; Nito, C.; Nishi, T.; Chan, P.H. Mitochondrial translocation of p53 mediates release of cytochrome c and hippocampal CA1 neuronal death after transient global cerebral ischemia in rats. J. Neurosci. 2006, 26, 7974–7983. [Google Scholar] [CrossRef] [PubMed]
- Saito, Y.; Nishio, K.; Ogawa, Y.; Kimata, J.; Kinumi, T.; Yoshida, Y.; Noguchi, N.; Niki, E. Turning point in apoptosis/necrosis induced by hydrogen peroxide. Free Radic. Res. 2006, 40, 619–630. [Google Scholar] [CrossRef]
- Giampazolias, E.; Zunino, B.; Dhayade, S.; Bock, F.; Cloix, C.; Cao, K.; Roca, A.; Lopez, J.; Ichim, G.; Rubio-patiño, C.; et al. Europe PMC Funders Group Mitochondrial permeabilisation engages NF- κ B dependent anti- tumour activity under caspase deficiency. Nat. Cell Biol. 2018, 19, 1116–1129. [Google Scholar] [CrossRef]
- Chakraborty, R.; Basu, T. Metallic copper nanoparticles induce apoptosis in a human skin melanoma A-375 cell line. Nanotechnology 2017, 28, 105101. [Google Scholar] [CrossRef] [PubMed]
- Xue, Y.; Wang, J.; Huang, Y.; Gao, X.; Kong, L.; Zhang, T.; Tang, M. Comparative cytotoxicity and apoptotic pathways induced by nanosilver in human liver HepG2 and L02 cells. Hum. Exp. Toxicol. 2018, 37, 1298–1309. [Google Scholar] [CrossRef]
- Dasgupta, N.; Ranjan, S.; Mishra, D.; Ramalingam, C. Thermal Co-reduction engineered silver nanoparticles induce oxidative cell damage in human colon cancer cells through inhibition of reduced glutathione and induction of mitochondria-involved apoptosis. Chem. Biol. Interact. 2018, 295, 109–118. [Google Scholar] [CrossRef]
- Plackal Adimuriyil George, B.; Kumar, N.; Abrahamse, H.; Ray, S.S. Apoptotic efficacy of multifaceted biosynthesized silver nanoparticles on human adenocarcinoma cells. Sci. Rep. 2018, 8, 1–14. [Google Scholar] [CrossRef]
- Liu, Y.; Li, X.; Bao, S.; Lu, Z.; Li, Q.; Li, C.M. Plastic protein microarray to investigate the molecular pathways of magnetic nanoparticle-induced nanotoxicity. Nanotechnology 2013, 24, 175501. [Google Scholar] [CrossRef]
- Paesano, L.; Perotti, A.; Buschini, A.; Carubbi, C.; Marmiroli, M.; Maestri, E.; Iannotta, S.; Marmiroli, N. Markers for toxicity to HepG2 exposed to cadmium sulphide quantum dots; damage to mitochondria. Toxicology 2016, 374, 18–28. [Google Scholar] [CrossRef]
- Mariadoss, A.V.A.; Vinayagam, R.; Senthilkumar, V.; Paulpandi, M.; Murugan, K.; Xu, B.; Gothandam, K.M.; Kotakadi, V.S.; David, E. Phloretin loaded chitosan nanoparticles augments the pH-dependent mitochondrial-mediated intrinsic apoptosis in human oral cancer cells. Int. J. Biol. Macromol. 2019, 130, 997–1008. [Google Scholar] [CrossRef] [PubMed]
- Luo, H.; Su, H.; Wang, X.; Wang, L.; Li, J. N-Succinyl-chitosan nanoparticles induced mitochondria-dependent apoptosis in K562. Mol. Cell. Probes 2012, 26, 164–169. [Google Scholar] [CrossRef]
- Mata, R.; Nakkala, J.R.; Sadras, S.R. Polyphenol stabilized colloidal gold nanoparticles from Abutilon indicum leaf extract induce apoptosis in HT-29 colon cancer cells. Colloids Surf. B Biointerfaces 2016, 143, 499–510. [Google Scholar] [CrossRef] [PubMed]
- Xing, Y.; Cai, Z.; Xu, M.; Ju, W.; Luo, X.; Hu, Y.; Liu, X.; Kang, T.; Wu, P.; Cai, C.; et al. Raman observation of a molecular signaling pathway of apoptotic cells induced by photothermal therapy. Chem. Sci. 2019, 10, 10900–10910. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Hernández, M.; Del Pino, P.; Mitchell, S.G.; Moros, M.; Stepien, G.; Pelaz, B.; Parak, W.J.; Gálvez, E.M.; Pardo, J.; De La Fuente, J.M. Dissecting the molecular mechanism of apoptosis during photothermal therapy using gold nanoprisms. ACS Nano 2015, 9, 52–61. [Google Scholar] [CrossRef]
- Liang, S.; Sun, K.; Wang, Y.; Dong, S.; Wang, C.; Liu, L.; Wu, Y. Role of Cyt-C/caspases-9,3, Bax/Bcl-2 and the FAS death receptor pathway in apoptosis induced by zinc oxide nanoparticles in human aortic endothelial cells and the protective effect by alpha-lipoic acid. Chem. Biol. Interact. 2016, 258, 40–51. [Google Scholar] [CrossRef]
- Ma, W.; Jing, L.; Valladares, A.; Mehta, S.L.; Wang, Z.; Andy Li, P.; Bang, J.J. Silver nanoparticle exposure induced mitochondrial stress, caspase-3 activation and cell death: Amelioration by sodium selenite. Int. J. Biol. Sci. 2015, 11, 860–867. [Google Scholar] [CrossRef]
- Hu, S.; Yang, J.; Rao, M.; Wang, Y.; Zhou, F.; Cheng, G.; Xia, W.; Zhu, C. Copper nanoparticle-induced uterine injury in female rats. Environ. Toxicol. 2019, 34, 252–261. [Google Scholar] [CrossRef]
- Sarkar, A.; Das, J.; Manna, P.; Sil, P.C. Nano-copper induces oxidative stress and apoptosis in kidney via both extrinsic and intrinsic pathways. Toxicology 2011, 290, 208–217. [Google Scholar] [CrossRef]
- Li, W.; Zhao, L.; Wei, T.; Zhao, Y.; Chen, C. The inhibition of death receptor mediated apoptosis through lysosome stabilization following internalization of carboxyfullerene nanoparticles. Biomaterials 2011, 32, 4030–4041. [Google Scholar] [CrossRef]
- Yamada, S.; Yamazaki, D.; Kanda, Y. Silver nanoparticles inhibit neural induction in human induced pluripotent stem cells. Nanotoxicology 2018, 12, 836–846. [Google Scholar] [CrossRef] [PubMed]
- Ke, S.; Zhou, T.; Yang, P.; Wang, Y.; Zhang, P.; Chen, K.; Ren, L.; Ye, S. Gold nanoparticles enhance TRAIL sensitivity through Drp1-mediated apoptotic and autophagic mitochondrial fission in NSCLC cells. Int. J. Nanomed. 2017, 12, 2531–2551. [Google Scholar] [CrossRef]
- Guo, C.; Wang, J.; Jing, L.; Ma, R.; Liu, X.; Gao, L.; Cao, L.; Duan, J.; Zhou, X.; Li, Y.; et al. Mitochondrial dysfunction, perturbations of mitochondrial dynamics and biogenesis involved in endothelial injury induced by silica nanoparticles. Environ. Pollut. 2018, 236, 926–936. [Google Scholar] [CrossRef] [PubMed]
- Yetkin-Arik, B.; Vogels, I.M.C.; Nowak-Sliwinska, P.; Weiss, A.; Houtkooper, R.H.; Van Noorden, C.J.F.; Klaassen, I.; Schlingemann, R.O. The role of glycolysis and mitochondrial respiration in the formation and functioning of endothelial tip cells during angiogenesis. Sci. Rep. 2019, 9, 1–14. [Google Scholar] [CrossRef]
- Kim, H.H.; Kim, T.; Kim, E.; Park, J.K.; Park, S.-J.; Joo, H.; Kim, H.J. The Mitochondrial Warburg Effect: A Cancer Enigma. Interdiscip. Bio Cent. 2009, 1, 1–7. [Google Scholar] [CrossRef][Green Version]
- Luengo, A.; Li, Z.; Gui, D.Y.; Sullivan, L.B.; Zagorulya, M.; Do, B.T.; Ferreira, R.; Naamati, A.; Ali, A.; Lewis, C.A.; et al. Increased demand for NAD+ relative to ATP drives aerobic glycolysis. Mol. Cell 2021, 81, 691–707. [Google Scholar] [CrossRef] [PubMed]
- Seyfried, T.N.; Flores, R.E.; Poff, A.M.; D’Agostino, D.P. Cancer as a metabolic disease: Implications for novel therapeutics. Carcinogenesis 2014, 35, 515–527. [Google Scholar] [CrossRef]
- Zuberek, M.; Wojciechowska, D.; Krzyzanowski, D.; Meczynska-Wielgosz, S.; Kruszewski, M.; Grzelak, A. Glucose availability determines silver nanoparticles toxicity in HepG2. J. Nanobiotechnol. 2015, 13, 1. [Google Scholar] [CrossRef]
- Chen, Y.; Wang, Z.; Xu, M.; Wang, X.; Liu, R.; Liu, Q.; Zhang, Z.; Xia, T.; Zhao, J.; Jiang, G.; et al. Nanosilver incurs an adaptive shunt of energy metabolism mode to glycolysis in tumor and nontumor cells. ACS Nano 2014, 8, 5813–5825. [Google Scholar] [CrossRef]
- Ghosh, M.; Chakraborty, A.; Mukherjee, A. Cytotoxic, genotoxic and the hemolytic effect of titanium dioxide (TiO2) nanoparticles on human erythrocyte and lymphocyte cells in vitro. J. Appl. Toxicol. 2013, 33, 1097–1110. [Google Scholar] [CrossRef]
- Pereira, L.C.; Pazin, M.; Franco-Bernardes, M.F.; Martins, A.d.C.; Barcelos, G.R.M.; Pereira, M.C.; Mesquita, J.P.; Rodrigues, J.L.; Barbosa, F.; Dorta, D.J. A perspective of mitochondrial dysfunction in rats treated with silver and titanium nanoparticles (AgNPs and TiNPs). J. Trace Elem. Med. Biol. 2018, 47, 63–69. [Google Scholar] [CrossRef]
- Naserzadeh, P.; Ansari Esfeh, F.; Kaviani, M.; Ashtari, K.; Kheirbakhsh, R.; Salimi, A.; Pourahmad, J. Single-walled carbon nanotube, multi-walled carbon nanotube and Fe2O3 nanoparticles induced mitochondria mediated apoptosis in melanoma cells. Cutan. Ocul. Toxicol. 2018, 37, 157–166. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.; Jeon, W.B.; Kim, S.; Lee, S.-K. Decrease of reactive oxygen species-related biomarkers in the tissue-mimic 3D spheroid culture of human lung cells exposed to zinc oxide nanoparticles. J. Nanosci. Nanotechnol. 2014, 14, 3356–3365. [Google Scholar] [CrossRef]
- Lai, J.C.K.; Ananthakrishnan, G.; Jandhyam, S.; Dukhande, V.V.; Bhushan, A.; Gokhale, M.; Daniels, C.K.; Leung, S.W. Treatment of human astrocytoma U87 cells with silicon dioxide nanoparticles lowers their survival and alters their expression of mitochondrial and cell signaling proteins. Int. J. Nanomed. 2010, 5, 715–723. [Google Scholar] [CrossRef]
- Arab-Nozari, M.; Zamani, E.; Latifi, A.; Shaki, F. Mitochondrial toxicity of aluminium nanoparticles in comparison to its ionic form on isolated rat brain mitochondria. Bratisl. Lek. Listy 2019, 120, 516–522. [Google Scholar] [CrossRef] [PubMed]
- Majoumouo, M.S.; Sharma, J.R.; Sibuyi, N.R.S.; Tincho, M.B.; Boyom, F.F.; Meyer, M. Synthesis of biogenic gold nanoparticles from terminalia mantaly extracts and the evaluation of their in vitro cytotoxic effects in cancer cells. Molecules 2020, 25, 4469. [Google Scholar] [CrossRef] [PubMed]
- Barcińska, E.; Wierzbicka, J.; Zauszkiewicz-Pawlak, A.; Jacewicz, D.; Dabrowska, A.; Inkielewicz-Stepniak, I. Role of Oxidative and Nitro-Oxidative Damage in Silver Nanoparticles Cytotoxic Effect against Human Pancreatic Ductal Adenocarcinoma Cells. Oxidative Med. Cell. Longev. 2018, 2018, 8251961. [Google Scholar] [CrossRef] [PubMed]
- Teodoro, J.S.; Simões, A.M.; Duarte, F.V.; Rolo, A.P.; Murdoch, R.C.; Hussain, S.M.; Palmeira, C.M. Assessment of the toxicity of silver nanoparticles in vitro: A mitochondrial perspective. Toxicol. Vitr. 2011, 25, 664–670. [Google Scholar] [CrossRef] [PubMed]
- Manickam, V.; Periyasamy, M.; Dhakshinamoorthy, V.; Panneerselvam, L.; Perumal, E. Recurrent exposure to ferric oxide nanoparticles alters myocardial oxidative stress, apoptosis and necrotic markers in male mice. Chem. Biol. Interact. 2017, 278, 54–64. [Google Scholar] [CrossRef]
- Alphandéry, E. Bio-synthesized iron oxide nanoparticles for cancer treatment. Int. J. Pharm. 2020, 586, 119472. [Google Scholar] [CrossRef]
- Cabral-Romero, C.; Solís-Soto, J.M.; Sánchez-Pérez, Y.; Pineda-Aguilar, N.; Meester, I.; Pérez-Carrillo, E.; Nakagoshi-Cepeda, S.E.; Sánchez-Nájera, R.I.; Nakagoshi-Cepeda, M.A.A.; Hernandez-Delgadillo, R.; et al. Antitumor activity of a hydrogel loaded with lipophilic bismuth nanoparticles on cervical, prostate, and colon human cancer cells. Anticancer Drugs 2020, 31, 251–259. [Google Scholar] [CrossRef] [PubMed]
- Suma, P.R.; Padmanabhan, R.A.; Telukutla, S.R.; Ravindran, R.; Velikkakath, A.K.G.; Dekiwadia, C.D.; Paul, W.; Laloraya, M.; Srinivasula, S.M.; Bhosale, S.V.; et al. Vanadium pentoxide nanoparticle mediated perturbations in cellular redox balance and the paradigm of autophagy to apoptosis. Free Radic. Biol. Med. 2020, 161, 198–211. [Google Scholar] [CrossRef] [PubMed]
- Hernandez-Delgadillo, R.; García-Cuéllar, C.M.; Sánchez-Pérez, Y.; Pineda-Aguilar, N.; Martínez-Martínez, M.A.; Rangel-Padilla, E.E.; Nakagoshi-Cepeda, S.E.; Solís-Soto, J.M.; Sánchez-Nájera, R.I.; Nakagoshi-Cepeda, M.A.A.; et al. In vitro evaluation of the antitumor effect of bismuth lipophilic nanoparticles (BisBAL NPs) on breast cancer cells. Int. J. Nanomed. 2018, 13, 6089–6097. [Google Scholar] [CrossRef] [PubMed]
- Austin, L.A.; Ahmad, S.; Kang, B.; Rommel, K.R.; Mahmoud, M.; Peek, M.E.; El-Sayed, M.A. Cytotoxic effects of cytoplasmic-targeted and nuclear-targeted gold and silver nanoparticles in HSC-3 cells—A mechanistic study. Toxicol. Vitr. 2015, 29, 694–705. [Google Scholar] [CrossRef]
- De Meyts, P. The Insulin Receptor and Its Signal Transduction Network. In Endotext [Internet]; Feingold, K.R., Anawalt, B., Boyce, A., Chrousos, G., de Herder, W.W., Dhatariya, K., Dungan, K., Hershman, J.M., Hofland, J., Kalra, S., et al., Eds.; MDText.com, Inc.: South Dartmouth, UK, 2000. [Google Scholar]
- Xu, X.; Tang, Y.; Lang, Y.; Liu, Y.; Cheng, W.; Xu, H.; Liu, Y. Oral exposure to zno nanoparticles disrupt the structure of bone in young rats via the opg/ rank/rankl/igf-1 pathway. Int. J. Nanomed. 2020, 15, 9657–9668. [Google Scholar] [CrossRef]
- Rubin, J.; Ackert-Bicknell, C.L.; Zhu, L.; Fan, X.; Murphy, T.C.; Nanes, M.S.; Marcus, R.; Holloway, L.; Beamer, W.G.; Rosen, C.J. IGF-I regulates osteoprotegerin (OPG) and receptor activator of nuclear factor-κB ligand in vitro and OPG in vivo. J. Clin. Endocrinol. Metab. 2002, 87, 4273–4279. [Google Scholar] [CrossRef]
- Kong, L.; Hu, W.; Gao, X.; Wu, Y.; Xue, Y.; Cheng, K.; Tang, M. Molecular mechanisms underlying nickel nanoparticle induced rat Sertoli-germ cells apoptosis. Sci. Total Environ. 2019, 692, 240–248. [Google Scholar] [CrossRef]
- Mardilovich, K.; Pankratz, S.L.; Shaw, L.M. Expression and function of the insulin receptor substrate proteins in cancer. Cell Commun. Signal. 2009, 7, 1–15. [Google Scholar] [CrossRef]
- Yang, L.; Wang, H.; Liu, L.; Xie, A. The Role of Insulin / IGF-1 / PI3K / Akt / GSK3 β Signaling in Parkinson′s Disease Dementia. Front. Neurosci. 2018, 12, 1–8. [Google Scholar] [CrossRef]
- Ali, L.M.A.; Shaker, S.A.; Pinol, R.; Millan, A.; Hanafy, M.Y.; Helmy, M.H.; Kamel, M.A.; Mahmoud, S.A. Effect of superparamagnetic iron oxide nanoparticles on glucose homeostasis on type 2 diabetes experimental model. Life Sci. 2020, 245, 117361. [Google Scholar] [CrossRef]
- Rai, U.; Kosuru, R.; Prakash, S.; Singh, S.P.; Birla, H.; Tiwari, V.; Singh, S. Tetramethylpyrazine prevents diabetes by activating PI3K/Akt/GLUT-4 signalling in animal model of type-2 diabetes. Life Sci. 2019, 236, 116836. [Google Scholar] [CrossRef] [PubMed]
- Alkaladi, A.; Abdelazim, A.M.; Afifi, M. Antidiabetic activity of zinc oxide and silver nanoparticles on streptozotocin-induced diabetic rats. Int. J. Mol. Sci. 2014, 15, 2015–2023. [Google Scholar] [CrossRef] [PubMed]
- Jansen, J.; Karges, W.; Rink, L. Zinc and diabetes—Clinical links and molecular mechanisms. J. Nutr. Biochem. 2009, 20, 399–417. [Google Scholar] [CrossRef] [PubMed]
- Dogra, S.; Kar, A.K.; Girdhar, K.; Daniel, P.V.; Chatterjee, S.; Choubey, A.; Ghosh, S.; Patnaik, S.; Ghosh, D.; Mondal, P. Zinc oxide nanoparticles attenuate hepatic steatosis development in high-fat-diet fed mice through activated AMPK signaling axis. Nanomed. Nanotechnol. Biol. Med. 2019, 17, 210–222. [Google Scholar] [CrossRef] [PubMed]
- Stephenne, X.; Foretz, M.; Taleux, N.; Van Der Zon, G.C.; Sokal, E.; Hue, L.; Viollet, B.; Guigas, B. Metformin activates AMP-activated protein kinase in primary human hepatocytes by decreasing cellular energy status. Diabetologia 2011, 54, 3101–3110. [Google Scholar] [CrossRef]
- Brunmair, B.; Staniek, K.; Gras, F.; Scharf, N.; Althaym, A.; Clara, R.; Roden, M.; Gnaiger, E.; Nohl, H.; Waldhausl, W.; et al. Thiazolidinediones, Like Metformin, Inhibit Respiratory Complex I A Common Mechanism Contributing to Their Antidiabetic Actions? Diabetes 2004, 53, 1052–1059. [Google Scholar] [CrossRef]
- Guerrero-Romero, F.; Rodríguez-Morán, M. Complementary therapies for diabetes: The case for chromium, magnesium, and antioxidants. Arch. Med. Res. 2005, 36, 250–257. [Google Scholar] [CrossRef]
- Cunningham, J.J. Micronutrients as Nutriceutical Interventions in Diabetes Mellitus. J. Am. Coll. Nutr. 1998, 17, 7–10. [Google Scholar] [CrossRef]
- Ramachandran, V.; Anand, M.A.V.; David, E.; Venkatachalam, K.; Vijayakumar, S.; Sankaran, V.; Balupillai, A.; Sangeetha, C.C.; Gothandam, K.M.; Kotakadi, V.S.; et al. Antidiabetic activity of gold nanoparticles synthesized using wedelolactone in RIN-5F cell line. Antioxidants 2020, 9, 8. [Google Scholar] [CrossRef]
- Ebrahimpour, S.; Shahidi, S.B.; Abbasi, M.; Tavakoli, Z.; Esmaeili, A. Quercetin-conjugated superparamagnetic iron oxide nanoparticles (QCSPIONs) increases Nrf2 expression via miR-27a mediation to prevent memory dysfunction in diabetic rats. Sci. Rep. 2020, 10, 1–12. [Google Scholar] [CrossRef]
- Hussein, J.; El Naggar, M.E.; Latif, Y.A.; Medhat, D.; El Bana, M.; Refaat, E.; Morsy, S. Solvent-free and one pot synthesis of silver and zinc nanoparticles: Activity toward cell membrane component and insulin signaling pathway in experimental diabetes. Colloids Surf. B Biointerfaces 2018, 170, 76–84. [Google Scholar] [CrossRef] [PubMed]
- Hussein, J.; El-Banna, M.; Razik, T.A.; El-Naggar, M.E. Biocompatible zinc oxide nanocrystals stabilized via hydroxyethyl cellulose for mitigation of diabetic complications. Int. J. Biol. Macromol. 2018, 107, 748–754. [Google Scholar] [CrossRef] [PubMed]
- Blanco, J.; Tomás-Hernández, S.; García, T.; Mulero, M.; Gómez, M.; Domingo, J.L.; Sánchez, D.J. Oral exposure to silver nanoparticles increases oxidative stress markers in the liver of male rats and deregulates the insulin signalling pathway and p53 and cleaved caspase 3 protein expression. Food Chem. Toxicol. Int. J. Publ. Br. Ind. Biol. Res. Assoc. 2018, 115, 398–404. [Google Scholar] [CrossRef] [PubMed]
- Hu, H.; Guo, Q.; Wang, C.; Ma, X.; He, H.; Oh, Y.; Feng, Y.; Wu, Q.; Gu, N. Titanium dioxide nanoparticles increase plasma glucose via reactive oxygen species-induced insulin resistance in mice. J. Appl. Toxicol. 2015, 35, 1122–1132. [Google Scholar] [CrossRef]
- Proquin, H.; Jetten, M.J.; Jonkhout, M.C.M.; Garduño-Balderas, L.G.; Briedé, J.J.; de Kok, T.M.; Chirino, Y.I.; van Loveren, H. Time course gene expression data in colon of mice after exposure to food-grade E171. Data Br. 2018, 16, 531–600. [Google Scholar] [CrossRef]
- Kandimalla, R.; Thirumala, V.; Reddy, P.H. Is Alzheimer’s disease a Type 3 Diabetes? A critical appraisal. Biochim. Biophys. Acta-Mol. Basis Dis. 2017, 1863, 1078–1089. [Google Scholar] [CrossRef]
- Song, Z.; Wang, Y.; Zhang, F.; Yao, F.; Sun, C. Calcium Signaling Pathways: Key Pathways in the Regulation of Obesity. Int. J. Mol. Sci. 2019, 20, 2768. [Google Scholar] [CrossRef]
- Kim, S.; Park, J.W.; Kim, D.; Kim, D.; Lee, I.-H.; Jon, S. Bioinspired colorimetric detection of calcium (II) ions in serum using calsequestrin-functionalized gold nanoparticles. Angew. Chem. Int. Ed. Engl. 2009, 48, 4138–4141. [Google Scholar] [CrossRef]
- Weaver, C.M.; Peacock, M. Calcium. Adv. Nutr. 2019, 10, 546–548. [Google Scholar] [CrossRef]
- Li, L.; Cui, J.; Liu, Z.; Zhou, X.; Li, Z.; Yu, Y.; Jia, Y.; Zuo, D.; Wu, Y. Silver nanoparticles induce SH-SY5Y cell apoptosis via endoplasmic reticulum- and mitochondrial pathways that lengthen endoplasmic reticulum-mitochondria contact sites and alter inositol-3-phosphate receptor function. Toxicol. Lett. 2018, 285, 156–167. [Google Scholar] [CrossRef]
- Ziemińska, E.; Stafiej, A.; Struzyńska, L. The role of the glutamatergic NMDA receptor in nanosilver-evoked neurotoxicity in primary cultures of cerebellar granule cells. Toxicology 2014, 315, 38–48. [Google Scholar] [CrossRef] [PubMed]
- Dubes, V.; Parpaite, T.; Ducret, T.; Quignard, J.-F.; Mornet, S.; Reinhardt, N.; Baudrimont, I.; Dubois, M.; Freund-Michel, V.; Marthan, R.; et al. Calcium signalling induced by in vitro exposure to silicium dioxide nanoparticles in rat pulmonary artery smooth muscle cells. Toxicology 2017, 375, 37–47. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Li, L.; Zhou, X.; Yu, Y.; Li, Z.; Zuo, D.; Wu, Y. Silver nanoparticles induce protective autophagy via Ca(2+)/CaMKKβ/AMPK/mTOR pathway in SH-SY5Y cells and rat brains. Nanotoxicology 2019, 13, 369–391. [Google Scholar] [CrossRef] [PubMed]
- Yang, Q.; Wang, Y.; Yang, Q.; Gao, Y.; Duan, X.; Fu, Q.; Chu, C.; Pan, X.; Cui, X.; Sun, Y. Cuprous oxide nanoparticles trigger ER stress-induced apoptosis by regulating copper trafficking and overcoming resistance to sunitinib therapy in renal cancer. Biomaterials 2017, 146, 72–85. [Google Scholar] [CrossRef] [PubMed]
- Di Bucchianico, S.; Gliga, A.R.; Åkerlund, E.; Skoglund, S.; Wallinder, I.O.; Fadeel, B.; Karlsson, H.L. Calcium-dependent cyto- and genotoxicity of nickel metal and nickel oxide nanoparticles in human lung cells. Part. Fibre Toxicol. 2018, 15, 32. [Google Scholar] [CrossRef] [PubMed]
- Xu, Q.-H.; Guan, P.; Zhang, T.; Lu, C.; Li, G.; Liu, J.-X. Silver nanoparticles impair zebrafish skeletal and cardiac myofibrillogenesis and sarcomere formation. Aquat. Toxicol. 2018, 200, 102–113. [Google Scholar] [CrossRef] [PubMed]
- Hansen, K.B.; Yi, F.; Perszyk, R.E.; Furukawa, H.; Wollmuth, L.P.; Gibb, A.J.; Traynelis, S.F. Structure, function, and allosteric modulation of NMDA receptors. J. Gen. Physiol. 2018, 150, 1081–1105. [Google Scholar] [CrossRef]
- Torabi, M.; Kesmati, M.; Galehdari, H.; Varzi, H.N.; Pourreza, N. MgO and ZnO nanoparticles anti-nociceptive effect modulated by glutamate level and NMDA receptor expression in the hippocampus of stressed and non-stressed rats. Physiol. Behav. 2020, 214, 112727. [Google Scholar] [CrossRef]
- Ziemińska, E.; Strużyńska, L. Zinc Modulates Nanosilver-Induced Toxicity in Primary Neuronal Cultures. Neurotox. Res. 2016, 29, 325–343. [Google Scholar] [CrossRef]
- Begum, A.N.; Aguilar, J.S.; Elias, L.; Hong, Y. Silver nanoparticles exhibit coating and dose-dependent neurotoxicity in glutamatergic neurons derived from human embryonic stem cells. Neurotoxicology 2016, 57, 45–53. [Google Scholar] [CrossRef]
- Ahmed, M.M.; Hussein, M.M.A. Neurotoxic effects of silver nanoparticles and the protective role of rutin. Biomed. Pharmacother. 2017, 90, 731–739. [Google Scholar] [CrossRef] [PubMed]
- Maxwell, J.T.; Somasuntharam, I.; Gray, W.D.; Shen, M.; Singer, J.M.; Wang, B.; Saafir, T.; Crawford, B.H.; Jiang, R.; Murthy, N.; et al. Bioactive nanoparticles improve calcium handling in failing cardiac myocytes. Nanomedicine 2015, 10, 3343–3357. [Google Scholar] [CrossRef] [PubMed]
- Thomas, D.D. Breathing new life into nitric oxide signaling: A brief overview of the interplay between oxygen and nitric oxide. Redox Biol. 2015, 5, 225–233. [Google Scholar] [CrossRef]
- Alimoradi, H.; Greish, K.; Gamble, A.B.; Giles, G.I. Controlled Delivery of Nitric Oxide for Cancer Therapy. Pharm. Nanotechnol. 2019, 7, 279–303. [Google Scholar] [CrossRef] [PubMed]
- González, C.; Salazar-García, S.; Palestino, G.; Martínez-Cuevas, P.P.; Ramírez-Lee, M.A.; Jurado-Manzano, B.B.; Rosas-Hernández, H.; Gaytán-Pacheco, N.; Martel, G.; Espinosa-Tanguma, R.; et al. Effect of 45nm silver nanoparticles (AgNPs) upon the smooth muscle of rat trachea: Role of nitric oxide. Toxicol. Lett. 2011, 207, 306–313. [Google Scholar] [CrossRef]
- Ramírez-Lee, M.A.; Rosas-Hernández, H.; Salazar-García, S.; Gutiérrez-Hernández, J.M.; Espinosa-Tanguma, R.; González, F.J.; Ali, S.F.; González, C. Silver nanoparticles induce anti-proliferative effects on airway smooth muscle cells. Role of nitric oxide and muscarinic receptor signaling pathway. Toxicol. Lett. 2014, 224, 246–256. [Google Scholar] [CrossRef]
- Chan, C.M.; Hsiao, C.Y.; Li, H.J.; Fang, J.Y.; Chang, D.C.; Hung, C.F. The inhibitory effects of gold nanoparticles on VEGF-A-induced cell migration in choroid-retina endothelial cells. Int. J. Mol. Sci. 2020, 21, 109. [Google Scholar] [CrossRef]
- Zielinska, E.; Tukaj, C.; Radomski, M.W.; Inkielewicz-Stepniak, I. Molecular mechanism of silver nanoparticles-inducedhuman osteoblast cell death: Protective effect of inducible nitric oxide synthase inhibitor. PLoS ONE 2016, 11, e0164137. [Google Scholar] [CrossRef]
- Hassanpour, H.; Mirshokraei, P.; Khalili Sadrabad, E.; Esmailian Dehkordi, A.; Layeghi, S.; Afzali, A.; Mohebbi, A. In vitro effect of nanosilver on gene expression of superoxide dismutases and nitric oxide synthases in chicken sertoli cells. Animal 2014, 9, 295–300. [Google Scholar] [CrossRef]
- Ramirez-Lee, M.A.; Aguirre-Bañuelos, P.; Martinez-Cuevas, P.P.; Espinosa-Tanguma, R.; Chi-Ahumada, E.; Martinez-Castañon, G.A.; Gonzalez, C. Evaluation of cardiovascular responses to silver nanoparticles (AgNPs) in spontaneously hypertensive rats. Nanomed. Nanotechnol. Biol. Med. 2018, 14, 385–395. [Google Scholar] [CrossRef]
- Eroglu, E.; Saeedi Saravi, S.S.; Sorrentino, A.; Steinhorn, B.; Michel, T. Discordance between eNOS phosphorylation and activation revealed by multispectral imaging and chemogenetic methods. Proc. Natl. Acad. Sci. USA 2019, 116, 20210–20217. [Google Scholar] [CrossRef] [PubMed]
- Alqahtani, S.; Kobos, L.M.; Xia, L.; Ferreira, C.; Franco, J.; Du, X.; Shannahan, J.H. Exacerbation of Nanoparticle-Induced Acute Pulmonary Inflammation in a Mouse Model of Metabolic Syndrome. Front. Immunol. 2020, 11, 818. [Google Scholar] [CrossRef] [PubMed]
- Ahn, S.; Singh, P.; Castro-Aceituno, V.; Yesmin Simu, S.; Kim, Y.J.; Mathiyalagan, R.; Yang, D.C. Gold nanoparticles synthesized using Panax ginseng leaves suppress inflammatory—Mediators production via blockade of NF-κB activation in macrophages. Artif. Cells Nanomed. Biotechnol. 2017, 45, 270–276. [Google Scholar] [CrossRef] [PubMed]
- Dhupal, M.; Oh, J.M.; Tripathy, D.R.; Kim, S.K.; Koh, S.B.; Park, K.S. Immunotoxicity of titanium dioxide nanoparticles via simultaneous induction of apoptosis and multiple toll-like receptors signaling through ROS-dependent SAPK/JNK and p38 MAPK activation. Int. J. Nanomed. 2018, 13, 6735–6750. [Google Scholar] [CrossRef] [PubMed]
- Huang, K.T.; Wu, C.T.; Huang, K.H.; Lin, W.C.; Chen, C.M.; Guan, S.S.; Chiang, C.K.; Liu, S.H. Titanium nanoparticle inhalation induces renal fibrosis in mice via an oxidative stress upregulated transforming growth factor-β pathway. Chem. Res. Toxicol. 2015, 28, 354–364. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.F.; Tung, S.P.; Wang, D.; Yeh, D.Y.; Fong, Y.; Young, Y.C.; Leu, F.J. Lipoxygenase pathway mediates increases of airway resistance and lung inflation induced by exposure to nanotitanium dioxide in rats. Oxidative Med. Cell. Longev. 2014, 2014, 485604. [Google Scholar] [CrossRef] [PubMed]
- Hong, F.; Wang, L.; Yu, X.; Zhou, Y.; Hong, J.; Sheng, L. Toxicological effect of TiO2 nanoparticle-induced myocarditis in mice. Nanoscale Res. Lett. 2015, 10, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Knuckles, T.L.; Yi, J.; Frazer, D.G.; Leonard, H.D.; Chen, B.T.; Castranova, V.; Nurkiewicz, T.R. Nanoparticle inhalation alters systemic arteriolar vasoreactivity through sympathetic and cyclooxygenase-mediated pathways. Nanotoxicology 2012, 6, 724–735. [Google Scholar] [CrossRef]
- Gholinejad, Z.; Khadem Ansari, M.H.; Rasmi, Y. Titanium dioxide nanoparticles induce endothelial cell apoptosis via cell membrane oxidative damage and p38, PI3K/Akt, NF-κB signaling pathways modulation. J. Trace Elem. Med. Biol. 2019, 54, 27–35. [Google Scholar] [CrossRef]
- Li, S.; Liu, H.; Zhou, Z.; Cao, Y. Titanate nanotubes at non-cytotoxic concentrations affect NO signaling pathway in human umbilical vein endothelial cells. Toxicol. Vitr. 2019, 62, 104689. [Google Scholar] [CrossRef]
- Kim, M.H.; Jeong, H.J. Zinc oxide nanoparticles suppress LPS-Induced NF-κB activation by inducing A20, a negative regulator of NF-κB, in RAW 264.7 Macrophages. J. Nanosci. Nanotechnol. 2015, 15, 6509–6515. [Google Scholar] [CrossRef] [PubMed]
- Zhu, S.; Zeng, M.; Feng, G.; Wu, H. Platinum nanoparticles as a therapeutic agent against dextran sodium sulfate-induced colitis in mice. Int. J. Nanomed. 2019, 14, 8361–8378. [Google Scholar] [CrossRef] [PubMed]
- Chuang, K.J.; Lee, K.Y.; Pan, C.H.; Lai, C.H.; Lin, L.Y.; Ho, S.C.; Ho, K.F.; Chuang, H.C. Effects of zinc oxide nanoparticles on human coronary artery endothelial cells. Food Chem. Toxicol. 2016, 93, 138–144. [Google Scholar] [CrossRef] [PubMed]
- Roy, R.; Singh, S.K.; Das, M.; Tripathi, A.; Dwivedi, P.D. Toll-like receptor 6 mediated inflammatory and functional responses of zinc oxide nanoparticles primed macrophages. Immunology 2014, 142, 453–464. [Google Scholar] [CrossRef]
- Saquib, Q.; Al-Khedhairy, A.A.; Ahmad, J.; Siddiqui, M.A.; Dwivedi, S.; Khan, S.T.; Musarrat, J. Zinc ferrite nanoparticles activate IL-1b, NFKB1, CCL21 and NOS2 signaling to induce mitochondrial dependent intrinsic apoptotic pathway in WISH cells. Toxicol. Appl. Pharmacol. 2013, 273, 289–297. [Google Scholar] [CrossRef]
- Sharma, A.K.; Kumar, A.; Sahu, M.; Sharma, G.; Datusalia, A.K.; Rajput, S.K. Exercise preconditioning and low dose copper nanoparticles exhibits cardioprotection through targeting GSK-3β phosphorylation in ischemia/reperfusion induced myocardial infarction. Microvasc. Res. 2018, 120, 59–66. [Google Scholar] [CrossRef]
- Tang, H.; Xu, M.; Shi, F.; Ye, G.; Lv, C.; Luo, J.; Zhao, L.; Li, Y. Effects and mechanism of nano-copper exposure on hepatic cytochrome P450 enzymes in rats. Int. J. Mol. Sci. 2018, 19, 2140. [Google Scholar] [CrossRef]
- Arancibia, S.; Barrientos, A.; Torrejón, J.; Escobar, A.; Beltrán, C.J. Copper oxide nanoparticles recruit macrophages and modulate nitric oxide, proinflammatory cytokines and PGE2 production through arginase activation. Nanomedicine 2016, 11, 1237–1251. [Google Scholar] [CrossRef]
- Alawdi, S.H.; El-Denshary, E.S.; Safar, M.M.; Eidi, H.; David, M.O.; Abdel-Wahhab, M.A. Neuroprotective Effect of Nanodiamond in Alzheimer’s Disease Rat Model: A Pivotal Role for Modulating NF-κB and STAT3 Signaling. Mol. Neurobiol. 2017, 54, 1906–1918. [Google Scholar] [CrossRef]
- Volarevic, V.; Paunovic, V.; Markovic, Z.; Simovic Markovic, B.; Misirkic-Marjanovic, M.; Todorovic-Markovic, B.; Bojic, S.; Vucicevic, L.; Jovanovic, S.; Arsenijevic, N.; et al. Large graphene quantum dots alleviate immune-mediated liver damage. ACS Nano 2014, 8, 12098–12109. [Google Scholar] [CrossRef]
- Park, E.J.; Umh, H.N.; Kim, S.W.; Cho, M.H.; Kim, J.H.; Kim, Y. ERK pathway is activated in bare-FeNPs-induced autophagy. Arch. Toxicol. 2014, 88, 323–336. [Google Scholar] [CrossRef]
- Li, M.; Kim, H.S.; Tian, L.; Yu, M.K.; Jon, S.; Moon, W.K. Comparison of two ultrasmall superparamagnetic iron oxides on cyto-toxicity and MR imaging of tumors. Theranostics 2012, 2, 76–85. [Google Scholar] [CrossRef]
- Mahmoud, A.M.; Desouky, E.M.; Hozayen, W.G.; Bin-Jumah, M.; El-Nahass, E.S.; Soliman, H.A.; Farghali, A.A. Mesoporous silica nanoparticles trigger liver and kidney injury and fibrosis via altering tlr4/nf-ffb, jak2/stat3 and nrf2/ho-1 signaling in rats. Biomolecules 2019, 9, 528. [Google Scholar] [CrossRef] [PubMed]
- Guo, C.; Xia, Y.; Niu, P.; Jiang, L.; Duan, J.; Yu, Y.; Zhou, X.; Li, Y.; Sun, Z. Silica nanoparticles induce oxidative stress, inflammation, and endothelial dysfunction in vitro via activation of the MAPK/Nrf2 pathway and nuclear factor-κB signaling. Int. J. Nanomed. 2015, 10, 1463–1477. [Google Scholar] [CrossRef] [PubMed]
- Duan, J.; Yu, Y.; Yu, Y.; Li, Y.; Wang, J.; Geng, W.; Jiang, L.; Li, Q.; Zhou, X.; Sun, Z. Silica nanoparticles induce autophagy and endothelial dysfunction via the PI3K/Akt/mTOR signaling pathway. Int. J. Nanomed. 2014, 9, 5131–5141. [Google Scholar] [CrossRef] [PubMed]
- Kaur, R.; Verma, S.; Joshi, P.; Singh, S.P.; Singh, M. Cytotoxicity of Graphene Oxide (GO) and Graphene Oxide Conjugated Losartan Potassium (GO-LP) on Neuroblastoma (NB41A3) Cells. J. Nanosci. Nanotechnol. 2018, 18, 6765–6775. [Google Scholar] [CrossRef]
- Lee, J.K.; Sayers, B.C.; Chun, K.S.; Lao, H.C.; Shipley-Phillips, J.K.; Bonner, J.C.; Langenbach, R. Multi-walled carbon nanotubes induce COX-2 and iNOS expression via MAP Kinase-dependent and -independent mechanisms in mouse RAW264.7 macrophages. Part. Fibre Toxicol. 2012, 9, 1–11. [Google Scholar] [CrossRef]
- Kumar, S.; Adjei, I.M.; Brown, S.B.; Liseth, O.; Sharma, B. Manganese dioxide nanoparticles protect cartilage from inflammation-induced oxidative stress. Biomaterials 2019, 224, 1–39. [Google Scholar] [CrossRef]
- Kadry, M.O.; Abdel-Megeed, R.M.; El-Meliegy, E.; Abdel-Hamid, A.H.Z. Crosstalk between GSK-3, c-Fos, NFκB and TNF-α signaling pathways play an ambitious role in Chitosan Nanoparticles Cancer Therapy. Toxicol. Rep. 2018, 5, 723–727. [Google Scholar] [CrossRef]
- Shi, X.; Zhou, K.; Huang, F.; Wang, C. Interaction of hydroxyapatite nanoparticles with endothelial cells: Internalization and inhibition of angiogenesis in vitro through the PI3K/Akt pathway. Int. J. Nanomed. 2017, 12, 5781–5795. [Google Scholar] [CrossRef]
- Qiu, S.; Cai, L.; Zhao, W.; Pang, X. Effect of Propylene Glycol Alginate Sodium Sulfate Nanoparticles on Myocardial Injury in Diabetic Rats via Silent Information Regulator 1/Hypoxia-Inducible Factor-1 Alpha Pathway. J. Nanosci. Nanotechnol. 2020, 21, 1351–1356. [Google Scholar] [CrossRef]
- Guo, C.; Ma, R.; Liu, X.; Xia, Y.; Niu, P.; Ma, J.; Zhou, X.; Li, Y.; Sun, Z. Silica nanoparticles induced endothelial apoptosis via endoplasmic reticulum stress-mitochondrial apoptotic signaling pathway. Chemosphere 2018, 210, 183–192. [Google Scholar] [CrossRef] [PubMed]
- Kang, K.; Lim, D.H.; Choi, I.H.; Kang, T.; Lee, K.; Moon, E.Y.; Yang, Y.; Lee, M.S.; Lim, J.S. Vascular tube formation and angiogenesis induced by polyvinylpyrrolidone-coated silver nanoparticles. Toxicol. Lett. 2011, 205, 227–234. [Google Scholar] [CrossRef] [PubMed]
- Loan, T.T.; Do, L.T.; Yoo, H. Different Cellular Effects of Platinum Nanoparticles on RAW 264.7 Cells. J. Nanosci. Nanotechnol. 2018, 19, 709–712. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.D.; Kou, Y.Y.; Liao, C.Y.; Li, C.H.; Huang, S.P.; Cheng, Y.W.; Liao, W.C.; Chen, H.X.; Wu, P.L.; Kang, J.J.; et al. Zinc oxide nanoparticles impair bacterial clearance by macrophages. Nanomedicine 2014, 9, 1327–1339. [Google Scholar] [CrossRef]
- Baltaci, A.K.; Yuce, K.; Mogulkoc, R. Zinc Metabolism and Metallothioneins. Biol. Trace Elem. Res. 2018, 183, 22–31. [Google Scholar] [CrossRef]
- Gilbert, R.; Peto, T.; Lengyel, I.; Emri, E. Zinc Nutrition and Inflammation in the Aging Retina. Mol. Nutr. Food Res. 2019, 63, e1801049. [Google Scholar] [CrossRef]
- Hojyo, S.; Fukada, T. Roles of Zinc Signaling in the Immune System. J. Immunol. Res. 2016, 2016, 6762343. [Google Scholar] [CrossRef]
- Wessels, I.; Maywald, M.; Rink, L. Zinc as a Gatekeeper of Immune Function. Nutrients 2017, 9, 1286. [Google Scholar] [CrossRef]
- Maares, M.; Haase, H. Zinc and immunity: An essential interrelation. Arch. Biochem. Biophys. 2016, 611, 58–65. [Google Scholar] [CrossRef]
- Murphy, E.W.; Willis, B.W.; Watt, B.K. Provisional tables on the zinc content of foods. J. Am. Diet. Assoc. 1975, 66, 345–355. [Google Scholar] [CrossRef]
- Sanna, A.; Firinu, D.; Zavattari, P.; Valera, P. Zinc status and autoimmunity: A systematic review and meta-analysis. Nutrients 2018, 10, 68. [Google Scholar] [CrossRef] [PubMed]
- Glutsch, V.; Hamm, H.; Goebeler, M. Zinc and skin: An update. J. Dtsch. Dermatol. Ges. 2019, 17, 589–596. [Google Scholar] [CrossRef] [PubMed]
- Mayor-Ibarguren, A.; Busca-Arenzana, C.; Robles-Marhuenda, Á. A Hypothesis for the Possible Role of Zinc in the Immunological Pathways Related to COVID-19 Infection. Front. Immunol. 2020, 11, 1736. [Google Scholar] [CrossRef]
- Sabziparvar, N.; Saeedi, Y.; Nouri, M.; Najafi Bozorgi, A.S.; Alizadeh, E.; Attar, F.; Akhtari, K.; Mousavi, S.E.; Falahati, M. Investigating the Interaction of Silicon Dioxide Nanoparticles with Human Hemoglobin and Lymphocyte Cells by Biophysical, Computational, and Cellular Studies. J. Phys. Chem. B 2018, 122, 4278–4288. [Google Scholar] [CrossRef]
- Kalaiarasi, A.; Sankar, R.; Anusha, C.; Saravanan, K.; Aarthy, K.; Karthic, S.; Mathuram, T.L.; Ravikumar, V. Copper oxide nanoparticles induce anticancer activity in A549 lung cancer cells by inhibition of histone deacetylase. Biotechnol. Lett. 2018, 40, 249–256. [Google Scholar] [CrossRef]
- Chevallet, M.; Gallet, B.; Fuchs, A.; Jouneau, P.H.; Um, K.; Mintz, E.; Michaud-Soret, I. Metal homeostasis disruption and mitochondrial dysfunction in hepatocytes exposed to sub-toxic doses of zinc oxide nanoparticles. Nanoscale 2016, 8, 18495–18506. [Google Scholar] [CrossRef]
- Pan, C.-Y.; Lin, F.-Y.; Kao, L.-S.; Huang, C.-C.; Liu, P.-S. Zinc oxide nanoparticles modulate the gene expression of ZnT1 and ZIP8 to manipulate zinc homeostasis and stress-induced cytotoxicity in human neuroblastoma SH-SY5Y cells. PLoS ONE 2020, 15, e0232729. [Google Scholar] [CrossRef]
- Verma, S.K.; Panda, P.K.; Jha, E.; Suar, M.; Parashar, S.K.S. Altered physiochemical properties in industrially synthesized ZnO nanoparticles regulate oxidative stress; induce in vivo cytotoxicity in embryonic zebrafish by apoptosis. Sci. Rep. 2017, 7, 13909. [Google Scholar] [CrossRef]
- Myint, Z.W.; Oo, T.H.; Thein, K.Z.; Tun, A.M.; Saeed, H. Copper deficiency anemia: Review article. Ann. Hematol. 2018, 97, 1527–1534. [Google Scholar] [CrossRef]
- D’Ambrosi, N.; Rossi, L. Copper at synapse: Release, binding and modulation of neurotransmission. Neurochem. Int. 2015, 90, 36–45. [Google Scholar] [CrossRef] [PubMed]
- Ilyechova, E.Y.; Saveliev, A.N.; Skvortsov, A.N.; Babich, P.S.; Zatulovskaia, Y.A.; Pliss, M.G.; Korzhevskii, D.E.; Tsymbalenko, N.V.; Puchkova, L.V. The effects of silver ions on copper metabolism in rats. Metallomics 2014, 6, 1970–1987. [Google Scholar] [CrossRef] [PubMed]
- Pohanka, M. Copper and copper nanoparticles toxicity and their impact on basic functions in the body. Bratisl. Lek. Listy 2019, 120, 397–409. [Google Scholar] [CrossRef]
- Collins, J.F.; Klevay, L.M. Copper. Adv. Nutr. 2011, 2, 520–522. [Google Scholar] [CrossRef]
- Puchkova, L.V.; Broggini, M.; Polishchuk, E.V.; Ilyechova, E.Y.; Polishchuk, R.S. Silver Ions as a Tool for Understanding Different Aspects of Copper Metabolism. Nutrients 2019, 11, 1364. [Google Scholar] [CrossRef] [PubMed]
- Orlov, I.A.; Sankova, T.P.; Babich, P.S.; Sosnin, I.M.; Ilyechova, E.Y.; Kirilenko, D.A.; Brunkov, P.N.; Ataev, G.L.; Romanov, A.E.; Puchkova, L.V. New silver nanoparticles induce apoptosis-like process in E. coli and interfere with mammalian copper metabolism. Int. J. Nanomed. 2016, 11, 6561–6574. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, N.; Ramamoorthy, M.; Lyon, D.; Jones, K.; Duttaroy, A. Mechanism of Silver Nanoparticles Action on Insect Pigmentation Reveals Intervention of Copper Homeostasis. PLoS ONE 2013, 8, e0053186. [Google Scholar] [CrossRef]
- Wang, C.; Zhang, R.; Wei, X.; Lv, M.; Jiang, Z. Metalloimmunology: The metal ion-controlled immunity. Adv. Immunol. 2020, 145, 187–241. [Google Scholar] [CrossRef]
- Ganz, T.; Nemeth, E. Iron homeostasis in host defence and inflammation. Nat. Rev. Immunol. 2015, 15, 500–510. [Google Scholar] [CrossRef]
- McClung, J.P. Iron, Zinc, and Physical Performance. Biol. Trace Elem. Res. 2019, 188, 135–139. [Google Scholar] [CrossRef]
- Coad, J.; Pedley, K. Iron deficiency and iron deficiency anemia in women. Scand. J. Clin. Lab. Investig. Suppl. 2014, 244, 82–89. [Google Scholar] [CrossRef] [PubMed]
- Camaschella, C. Iron deficiency: New insights into diagnosis and treatment. Hematol. Am. Soc. Hematol. Educ. Progr. 2015, 2015, 8–13. [Google Scholar] [CrossRef] [PubMed]
- Grzelak, A.; Wojewódzka, M.; Meczynska-Wielgosz, S.; Zuberek, M.; Wojciechowska, D.; Kruszewski, M. Crucial role of chelatable iron in silver nanoparticles induced DNA damage and cytotoxicity. Redox Biol. 2018, 15, 435–440. [Google Scholar] [CrossRef]
- Doumandji, Z.; Safar, R.; Lovera-Leroux, M.; Nahle, S.; Cassidy, H.; Matallanas, D.; Rihn, B.; Ferrari, L.; Joubert, O. Protein and lipid homeostasis altered in rat macrophages after exposure to metallic oxide nanoparticles. Cell Biol. Toxicol. 2020, 36, 65–82. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Cao, F.; Yin, H.-L.; Huang, Z.-J.; Lin, Z.-T.; Mao, N.; Sun, B.; Wang, G. Ferroptosis: Past, present and future. Cell Death Dis. 2020, 11, 88. [Google Scholar] [CrossRef]
- Wang, S.; Luo, J.; Zhang, Z.; Dong, D.; Shen, Y.; Fang, Y.; Hu, L.; Liu, M.; Dai, C.; Peng, S.; et al. Iron and magnetic: New research direction of the ferroptosis-based cancer therapy. Am. J. Cancer Res. 2018, 8, 1933–1946. [Google Scholar]
- Zhang, H.; Zhabyeyev, P.; Wang, S.; Oudit, G.Y. Role of iron metabolism in heart failure: From iron deficiency to iron overload. Biochim. Biophys. Acta Mol. Basis Dis. 2019, 1865, 1925–1937. [Google Scholar] [CrossRef]
- Wang, X.; Wang, M.; Lei, R.; Zhu, S.F.; Zhao, Y.; Chen, C. Chiral Surface of Nanoparticles Determines the Orientation of Adsorbed Transferrin and Its Interaction with Receptors. ACS Nano 2017, 11, 4606–4616. [Google Scholar] [CrossRef]
- Ruiz, G.; Ryan, N.; Rutschke, K.; Awotunde, O.; Driskell, J.D. Antibodies Irreversibly Adsorb to Gold Nanoparticles and Resist Displacement by Common Blood Proteins. Langmuir 2019, 35, 10601–10609. [Google Scholar] [CrossRef]
- Zhang, J.L.; Di, W.; Gong, P.M.; Lin, K.; Lyu, L.Z.; Zhang, L.W.; Han, X.; Ma, Y. Direct and fast capture lactoferrin from cheese whey on nanoparticles of Fe3O4 combined with concanavalin A. Food Chem. 2019, 274, 314–318. [Google Scholar] [CrossRef]
- Hüttemann, M.; Pecina, P.; Rainbolt, M.; Sanderson, T.H.; Kagan, V.E.; Samavati, L.; Doan, J.W.; Lee, I. The multiple functions of cytochrome c and their regulation in life and death decisions of the mammalian cell: From respiration to apoptosis. Mitochondrion 2011, 11, 369–381. [Google Scholar] [CrossRef] [PubMed]
- Sun, X.; Feng, Z.; Zhang, L.; Hou, T.; Li, Y. The selective interaction between silica nanoparticles and enzymes from molecular dynamics simulations. PLoS ONE 2014, 9, e107696. [Google Scholar] [CrossRef] [PubMed]
- Tarpani, L.; Bellezza, F.; Sassi, P.; Gambucci, M.; Cipiciani, A.; Latterini, L. New Insights into the Effects of Surface Functionalization on the Peroxidase Activity of Cytochrome c Adsorbed on Silica Nanoparticles. J. Phys. Chem. B 2019, 123, 2567–2575. [Google Scholar] [CrossRef] [PubMed]
- Mukhopadhyay, A.; Joshi, N.; Chattopadhyay, K.; De, G. A facile synthesis of PEG-coated magnetite (Fe3O4) nanoparticles and their prevention of the reduction of cytochrome c. ACS Appl. Mater. Interfaces 2012, 4, 142–149. [Google Scholar] [CrossRef]
- Jafari Azad, V.; Kasravi, S.; Alizadeh Zeinabad, H.; Memar Bashi Aval, M.; Saboury, A.A.; Rahimi, A.; Falahati, M. Probing the conformational changes and peroxidase-like activity of cytochrome c upon interaction with iron nanoparticles. J. Biomol. Struct. Dyn. 2017, 35, 2565–2577. [Google Scholar] [CrossRef]
- Mansouri, A.; Mousavi, M.; Attar, F.; Saboury, A.A.; Falahati, M. Interaction of manganese nanoparticle with cytochrome c: A multi-spectroscopic study. Int. J. Biol. Macromol. 2018, 106, 78–86. [Google Scholar] [CrossRef]
- Ahmed, M.H.; Ghatge, M.S.; Safo, M.K. Hemoglobin: Structure, Function and Allostery. Subcell. Biochem. 2020, 94, 345–382. [Google Scholar] [CrossRef]
- Drescher, D.; Büchner, T.; McNaughton, D.; Kneipp, J. SERS reveals the specific interaction of silver and gold nanoparticles with hemoglobin and red blood cell components. Phys. Chem. Chem. Phys. 2013, 15, 5364–5373. [Google Scholar] [CrossRef]
- Devineau, S.; Kiger, L.; Galacteros, F.; Baudin-Creuza, V.; Marden, M.; Renault, J.P.; Pin, S. Manipulating hemoglobin oxygenation using silica nanoparticles: A novel prospect for artificial oxygen carriers. Blood Adv. 2018, 2, 90–94. [Google Scholar] [CrossRef]
- Yang, H.; Hao, C.; Nan, Z.; Sun, R. Bovine hemoglobin adsorption onto modified silica nanoparticles: Multi-spectroscopic measurements based on kinetics and protein conformation. Int. J. Biol. Macromol. 2020, 155, 208–215. [Google Scholar] [CrossRef]
- Aliakbari, F.; Haji Hosseinali, S.; Khalili Sarokhalil, Z.; Shahpasand, K.; Akbar Saboury, A.; Akhtari, K.; Falahati, M. Reactive oxygen species generated by titanium oxide nanoparticles stimulate the hemoglobin denaturation and cytotoxicity against human lymphocyte cell. J. Biomol. Struct. Dyn. 2019, 37, 4875–4881. [Google Scholar] [CrossRef] [PubMed]
- Abdolmajid, E.; Kharazi, H.; Chalaki, M.; Khojasteh, M.; Haghighat, S.; Attar, F.; Nemati, F.; Falahati, M. Titanium oxide nanoparticles fabrication, hemoglobin interaction, white blood cells cytotoxicity, and antibacterial studies. J. Biomol. Struct. Dyn. 2019, 37, 3007–3017. [Google Scholar] [CrossRef]
- Bhunia, A.K.; Saha, S.; Kamilya, T. Microscopic and spectroscopic study of the corona formation and unfolding of human haemoglobin in presence of ZnO nanoparticles. Luminescence 2020, 35, 144–155. [Google Scholar] [CrossRef] [PubMed]
- Beg, M.; Maji, A.; Mandal, A.K.; Das, S.; Jha, P.K.; Hossain, M. Spectroscopic investigation on interaction of biogenic, Croton bonplandianum leaves extract mediated potential bactericidal silver nanoparticles with human hemoglobin and human serum albumin. J. Biomol. Struct. Dyn. 2018, 36, 711–723. [Google Scholar] [CrossRef] [PubMed]
- Mahato, M.; Pal, P.; Tah, B.; Ghosh, M.; Talapatra, G.B. Study of silver nanoparticle-hemoglobin interaction and composite formation. Colloids Surf. B Biointerfaces 2011, 88, 141–149. [Google Scholar] [CrossRef]
- Zolghadri, S.; Saboury, A.A.; Atri, M.S.; Moosavi-Movahedi, A.A. Differential propensity of citrate- and polyethylene glycol-coated silver nanoparticles to bovine hemoglobin. Toxicol. Ind. Health 2015, 31, 721–726. [Google Scholar] [CrossRef]
- Wang, M.; Fu, C.; Liu, X.; Lin, Z.; Yang, N.; Yu, S. Probing the mechanism of plasma protein adsorption on Au and Ag nanoparticles with FT-IR spectroscopy. Nanoscale 2015, 7, 15191–15196. [Google Scholar] [CrossRef]
- Chakraborty, M.; Paul, S.; Mitra, I.; Bardhan, M.; Bose, M.; Saha, A.; Ganguly, T. To reveal the nature of interactions of human hemoglobin with gold nanoparticles having two different morphologies (sphere and star-shaped) by using various spectroscopic techniques. J. Photochem. Photobiol. B 2018, 178, 355–366. [Google Scholar] [CrossRef]
- Mobasherat Jajroud, S.Y.; Falahati, M.; Attar, F.; Khavari-Nejad, R.A. Human hemoglobin adsorption onto colloidal cerium oxide nanoparticles: A new model based on zeta potential and spectroscopy measurements. J. Biomol. Struct. Dyn. 2018, 36, 2908–2916. [Google Scholar] [CrossRef]
- Chetty, R.; Singh, M. In-vitro interaction of cerium oxide nanoparticles with hemoglobin, insulin, and dsDNA at 310.15 K: Physicochemical, spectroscopic and in-silico study. Int. J. Biol. Macromol. 2020, 156, 1022–1044. [Google Scholar] [CrossRef]
- Eskandari, N.; Nejadi Babadaei, M.M.; Nikpur, S.; Ghasrahmad, G.; Attar, F.; Heshmati, M.; Akhtari, K.; Rezayat Sorkhabadi, S.M.; Mousavi, S.E.; Falahati, M. Biophysical, docking, and cellular studies on the effects of cerium oxide nanoparticles on blood components: In vitro. Int. J. Nanomed. 2018, 13, 4575–4589. [Google Scholar] [CrossRef]
- Babadaei, M.M.N.; Moghaddam, M.F.; Solhvand, S.; Alizadehmollayaghoob, E.; Attar, F.; Rajabbeigi, E.; Akhtari, K.; Sari, S.; Falahati, M. Biophysical, bioinformatical, cellular, and molecular investigations on the effects of graphene oxide nanosheets on the hemoglobin structure and lymphocyte cell cytotoxicity. Int. J. Nanomed. 2018, 13, 6871–6884. [Google Scholar] [CrossRef] [PubMed]
- Karlsson, H.L.; Cronholm, P.; Hedberg, Y.; Tornberg, M.; De Battice, L.; Svedhem, S.; Wallinder, I.O. Cell membrane damage and protein interaction induced by copper containing nanoparticles—Importance of the metal release process. Toxicology 2013, 313, 59–69. [Google Scholar] [CrossRef] [PubMed]
- Kahbasi, S.; Samadbin, M.; Attar, F.; Heshmati, M.; Danaei, D.; Rasti, B.; Salihi, A.; Nanakali, N.M.Q.; Aziz, F.M.; Akhtari, K.; et al. The effect of aluminum oxide on red blood cell integrity and hemoglobin structure at nanoscale. Int. J. Biol. Macromol. 2019, 138, 800–809. [Google Scholar] [CrossRef] [PubMed]
- Gamasaee, N.A.; Muhammad, H.A.; Tadayon, E.; Ale-Ebrahim, M.; Mirpour, M.; Sharifi, M.; Salihi, A.; Shekha, M.S.; Alasady, A.A.B.; Aziz, F.M.; et al. The effects of nickel oxide nanoparticles on structural changes, heme degradation, aggregation of hemoglobin and expression of apoptotic genes in lymphocytes. J. Biomol. Struct. Dyn. 2020, 38, 3676–3686. [Google Scholar] [CrossRef]
- Tu, M.K.; Levin, J.B.; Hamilton, A.M.; Borodinsky, L.N. Calcium signaling in skeletal muscle development, maintenance and regeneration. Cell Calcium 2016, 59, 91–97. [Google Scholar] [CrossRef] [PubMed]
- Gelli, R.; Ridi, F.; Baglioni, P. The importance of being amorphous: Calcium and magnesium phosphates in the human body. Adv. Colloid Interface Sci. 2019, 269, 219–235. [Google Scholar] [CrossRef]
- Cormick, G.; Belizán, J.M. Calcium Intake and Health. Nutrients 2019, 11, 1606. [Google Scholar] [CrossRef]
- Beto, J.A. The role of calcium in human aging. Clin. Nutr. Res. 2015, 4, 1–8. [Google Scholar] [CrossRef]
- Fujita, T. Calcium paradox: Consequences of calcium deficiency manifested by a wide variety of diseases. J. Bone Miner. Metab. 2000, 18, 234–236. [Google Scholar] [CrossRef]
- Li, K.; Wang, X.-F.; Li, D.-Y.; Chen, Y.-C.; Zhao, L.-J.; Liu, X.-G.; Guo, Y.-F.; Shen, J.; Lin, X.; Deng, J.; et al. The good, the bad, and the ugly of calcium supplementation: A review of calcium intake on human health. Clin. Interv. Aging 2018, 13, 2443–2452. [Google Scholar] [CrossRef]
- Engin, A.B.; Engin, A. Nanoparticles and neurotoxicity: Dual response of glutamatergic receptors. Prog. Brain Res. 2019, 245, 281–303. [Google Scholar] [CrossRef] [PubMed]
- Astegno, A.; Maresi, E.; Marino, V.; Dominici, P.; Pedroni, M.; Piccinelli, F.; Dell’Orco, D. Structural plasticity of calmodulin on the surface of CaF2 nanoparticles preserves its biological function. Nanoscale 2014, 6, 15037–15047. [Google Scholar] [CrossRef]
- Mizuno, Y.; Isotani, E.; Huang, J.; Ding, H.; Stull, J.T.; Kamm, K.E. Myosin light chain kinase activation and calcium sensitization in smooth muscle in vivo. Am. J. Physiol. Cell Physiol. 2008, 295, 358–364. [Google Scholar] [CrossRef]
- Liu, Y.; Yoo, E.; Han, C.; Mahler, G.J.; Doiron, A.L. Endothelial barrier dysfunction induced by nanoparticle exposure through actin remodeling via caveolae/raft-regulated calcium signalling. NanoImpact 2018, 11, 82–91. [Google Scholar] [CrossRef] [PubMed]
- Mirzajani, F.; Motevalli, S.M.; Jabbari, S.; Ranaei Siadat, S.O.; Sefidbakht, Y. Recombinant Acetylcholinesterase purification and its interaction with silver nanoparticle. Protein Expr. Purif. 2017, 136, 58–65. [Google Scholar] [CrossRef]
- Cornu, R.; Béduneau, A.; Martin, H. Influence of nanoparticles on liver tissue and hepatic functions: A review. Toxicology 2020, 430, 152344. [Google Scholar] [CrossRef] [PubMed]
- Bao, H.; Zhang, Q.; Yan, Z. The impact of camptothecin-encapsulated poly(lactic-co-glycolic acid) nanoparticles on the activity of cytochrome P450 in vitro. Int. J. Nanomed. 2019, 14, 383–391. [Google Scholar] [CrossRef] [PubMed]
- Wasukan, N.; Kuno, M.; Maniratanachote, R. Molecular Docking as a Promising Predictive Model for Silver Nanoparticle-Mediated Inhibition of Cytochrome P450 Enzymes. J. Chem. Inf. Model. 2019, 59, 5126–5134. [Google Scholar] [CrossRef]
- Xu, M.; Tang, H.; Zhou, X.; Chen, H.; Dong, Q.; Zhang, Y.; Ye, G.; Shi, F.; Lv, C.; Jing, B.; et al. Effects and mechanisms of sub-chronic exposure to copper nanoparticles on renal cytochrome P450 enzymes in rats. Environ. Toxicol. Pharmacol. 2018, 63, 135–146. [Google Scholar] [CrossRef]
- Loh, J.W.; Yeoh, G.; Saunders, M.; Lim, L.-Y. Uptake and cytotoxicity of chitosan nanoparticles in human liver cells. Toxicol. Appl. Pharmacol. 2010, 249, 148–157. [Google Scholar] [CrossRef] [PubMed]
- Strojny, B.; Sawosz, E.; Grodzik, M.; Jaworski, S.; Szczepaniak, J.; Sosnowska, M.; Wierzbicki, M.; Kutwin, M.; Orlińska, S.; Chwalibog, A. Nanostructures of diamond, graphene oxide and graphite inhibit CYP1A2, CYP2D6 and CYP3A4 enzymes and downregulate their genes in liver cells. Int. J. Nanomed. 2018, 13, 8561–8575. [Google Scholar] [CrossRef]
- Lu, Z.; Ma, G.; Veinot, J.G.C.; Wong, C.S. Disruption of biomolecule function by nanoparticles: How do gold nanoparticles affect Phase I biotransformation of persistent organic pollutants? Chemosphere 2013, 93, 123–132. [Google Scholar] [CrossRef] [PubMed]
- Allocati, N.; Masulli, M.; Di Ilio, C.; Federici, L. Glutathione transferases: Substrates, inihibitors and pro-drugs in cancer and neurodegenerative diseases. Oncogenesis 2018, 7, 8. [Google Scholar] [CrossRef]
- Barman, U.; Mukhopadhyay, G.; Goswami, N.; Ghosh, S.S.; Paily, R.P. Detection of Glutathione by Glutathione-S-Transferase-Nanoconjugate Ensemble Electrochemical Device. IEEE Trans. Nanobiosci. 2017, 16, 271–279. [Google Scholar] [CrossRef]
- Prasannaraj, G.; Venkatachalam, P. Hepatoprotective effect of engineered silver nanoparticles coated bioactive compounds against diethylnitrosamine induced hepatocarcinogenesis in experimental mice. J. Photochem. Photobiol. B. 2017, 167, 309–320. [Google Scholar] [CrossRef]
- Afifi, M.; Almaghrabi, O.A.; Kadasa, N.M. Ameliorative Effect of Zinc Oxide Nanoparticles on Antioxidants and Sperm Characteristics in Streptozotocin-Induced Diabetic Rat Testes. Biomed Res. Int. 2015, 2015, 153573. [Google Scholar] [CrossRef]
- Chatterjee, N.; Jeong, J.; Yoon, D.; Kim, S.; Choi, J. Global metabolomics approach in in vitro and in vivo models reveals hepatic glutathione depletion induced by amorphous silica nanoparticles. Chem. Biol. Interact. 2018, 293, 100–106. [Google Scholar] [CrossRef]
- Ostrakhovitch, E.A.; Song, Y.P.; Cherian, M.G. Basal and copper-induced expression of metallothionein isoform 1,2 and 3 genes in epithelial cancer cells: The role of tumor suppressor p53. J. Trace Elem. Med. Biol. Organ Soc. Miner. Trace Elem. 2016, 35, 18–29. [Google Scholar] [CrossRef]
- Sharma, S.; Rais, A.; Sandhu, R.; Nel, W.; Ebadi, M. Clinical significance of metallothioneins in cell therapy and nanomedicine. Int. J. Nanomed. 2013, 8, 1477–1488. [Google Scholar] [CrossRef]
- Genchi, G.; Sinicropi, M.S.; Lauria, G.; Carocci, A.; Catalano, A. The Effects of Cadmium Toxicity. Int. J. Environ. Res. Public Health 2020, 17, 3782. [Google Scholar] [CrossRef]
- Thirumoorthy, N.; Manisenthil Kumar, K.-T.; Shyam Sundar, A.; Panayappan, L.; Chatterjee, M. Metallothionein: An overview. World J. Gastroenterol. 2007, 13, 993–996. [Google Scholar] [CrossRef] [PubMed]
- Bulcke, F.; Dringen, R. Copper oxide nanoparticles stimulate glycolytic flux and increase the cellular contents of glutathione and metallothioneins in cultured astrocytes. Neurochem. Res. 2015, 40, 15–26. [Google Scholar] [CrossRef] [PubMed]
- Falfushynska, H.; Gnatyshyna, L.; Horyn, O.; Sokolova, I.; Stoliar, O. Endocrine and cellular stress effects of zinc oxide nanoparticles and nifedipine in marsh frogs Pelophylax ridibundus. Aquat. Toxicol. 2017, 185, 171–182. [Google Scholar] [CrossRef] [PubMed]
- Jaskulak, M.; Rorat, A.; Grobelak, A.; Chaabene, Z.; Kacprzak, M.; Vandenbulcke, F. Bioaccumulation, antioxidative response, and metallothionein expression in Lupinus luteus L. exposed to heavy metals and silver nanoparticles. Environ. Sci. Pollut. Res. Int. 2019, 26, 16040–16052. [Google Scholar] [CrossRef] [PubMed]
- de Carvalho, T.G.; Garcia, V.B.; de Araújo, A.A.; da Silva Gasparotto, L.H.; Silva, H.; Guerra, G.C.B.; de Castro Miguel, E.; de Carvalho Leitão, R.F.; da Silva Costa, D.V.; Cruz, L.J.; et al. Spherical neutral gold nanoparticles improve anti-inflammatory response, oxidative stress and fibrosis in alcohol-methamphetamine-induced liver injury in rats. Int. J. Pharm. 2018, 548, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Liu, W.; Worms, I.A.M.; Herlin-Boime, N.; Truffier-Boutry, D.; Michaud-Soret, I.; Mintz, E.; Vidaud, C.; Rollin-Genetet, F. Interaction of silver nanoparticles with metallothionein and ceruloplasmin: Impact on metal substitution by Ag(i), corona formation and enzymatic activity. Nanoscale 2017, 9, 6581–6594. [Google Scholar] [CrossRef]
- Miyayama, T.; Arai, Y.; Suzuki, N.; Hirano, S. Cellular distribution and behavior of metallothionein in mammalian cells following exposure to silver nanoparticles and silver ions. Yakugaku Zasshi 2014, 134, 723–729. [Google Scholar] [CrossRef][Green Version]
- Rollin-Genetet, F.; Seidel, C.; Artells, E.; Auffan, M.; Thiéry, A.; Vidaud, C. Redox Reactivity of Cerium Oxide Nanoparticles Induces the Formation of Disulfide Bridges in Thiol-Containing Biomolecules. Chem. Res. Toxicol. 2015, 28, 2304–2312. [Google Scholar] [CrossRef]
- Cuillel, M.; Chevallet, M.; Charbonnier, P.; Fauquant, C.; Pignot-Paintrand, I.; Arnaud, J.; Cassio, D.; Michaud-Soret, I.; Mintz, E. Interference of CuO nanoparticles with metal homeostasis in hepatocytes under sub-toxic conditions. Nanoscale 2014, 6, 1707–1715. [Google Scholar] [CrossRef]
- Florianczyk, B. Metallothioneins and its role in metal regulation, binding of reactive oxygen species, apoptosis and cell differentiation. J. Pre-Clin. Clin. Res. 2007, 1, 16–18. [Google Scholar]
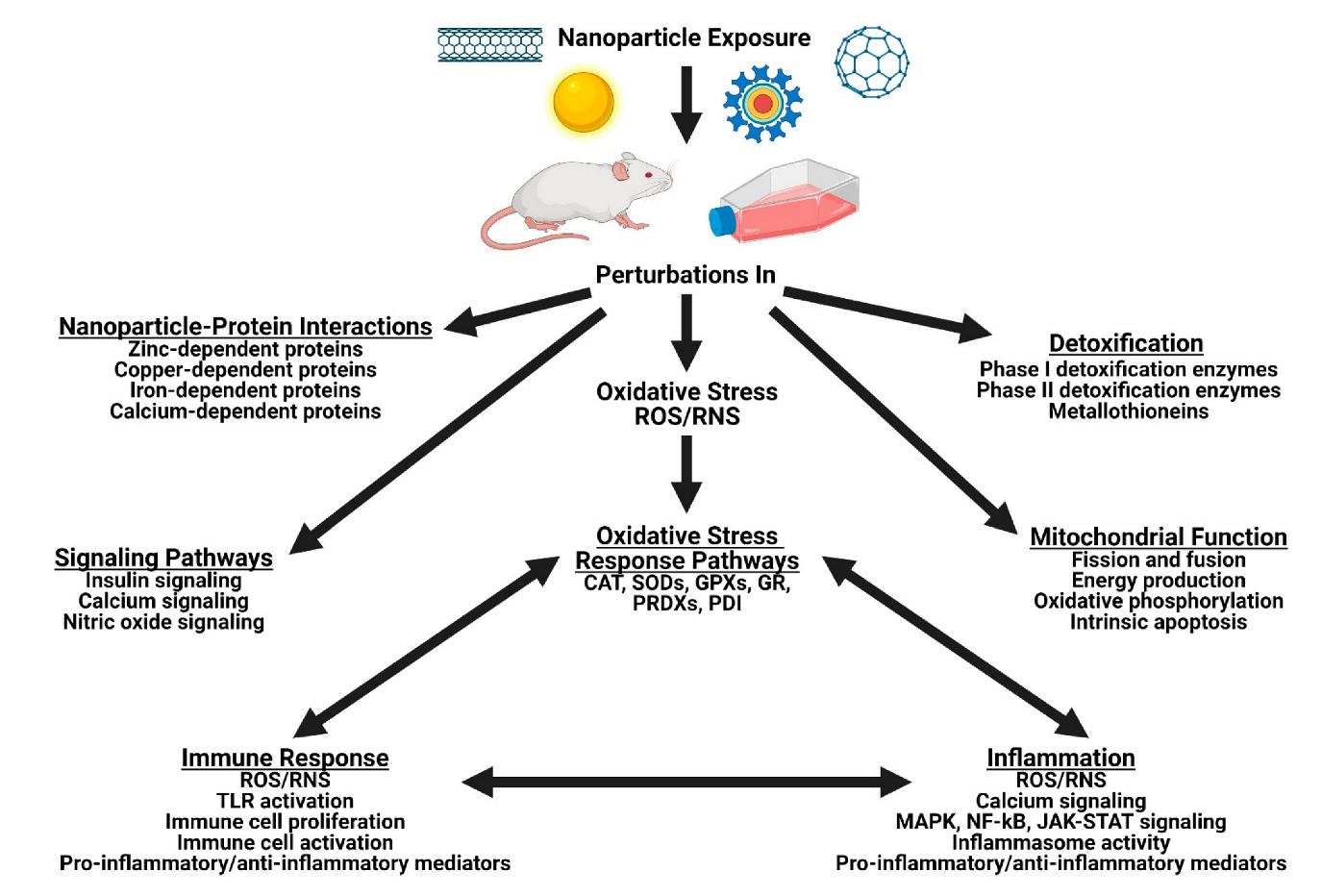
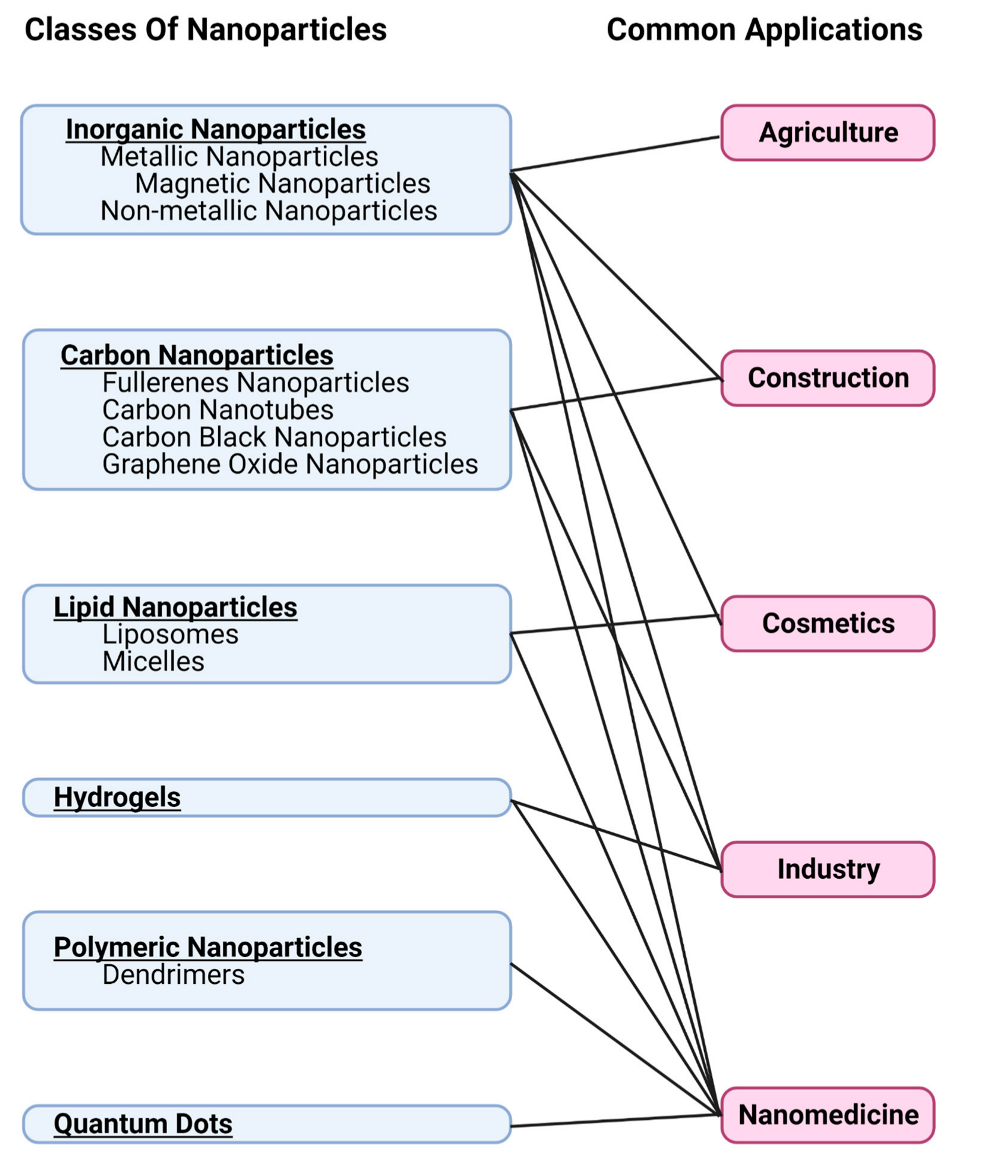
| Type of Nanoparticle | Common Applications | References |
|---|---|---|
| Ag | Industry, nanomedicine, cosmetics, agriculture | [24,25,26,27,28] |
| Al and Al2O3 | Industry, nanomedicine, construction | [13,24,33,34] |
| Au | Industry, nanomedicine | [11,13,24,30,31,32] |
| Carbon nanotubes | Industry, construction | [13,33,34] |
| Carbon black | Industry, cosmetics | 34,35,36] |
| CeO2 | Industry, nanomedicine | [35,36] |
| Cu and CuO | Industry, nanomedicine, construction | [24,33,34] |
| Dendrimers | Nanomedicine | [11,13] |
| Fullerenes | Nanomedicine | [13] |
| Graphene oxide | Nanomedicine | [37] |
| Iron oxide | Nanomedicine | [11,13,24] |
| Liposomes | Nanomedicine, cosmetics | [11,13,34] |
| Nanoplastics and microplastics | Industry | [38] |
| Pt | Industry, nanomedicine | [25,26] |
| Polymers | Nanomedicine | [10,39] |
| Si and SiO2 | Industry, nanomedicine, cosmetics, construction, agriculture | [13,17,24,27,28,38,40,41] |
| TiO2 | Industry, construction, cosmetics, nanomedicine | [13,17,27,28,39,42,43,44,45] |
| Quantum dots | Nanomedicine | [11,13,38,46,47] |
| Zinc oxide | Industry, cosmetics, agriculture | [24,28,48] |
| Type of Nanoparticle | Experimental Model | Protein(s) Affected | Main Findings | References |
|---|---|---|---|---|
| Ag | n/a | CAT and SOD | Conformational changes to CAT resulting in loss of catalytic activity, but minimal effects to SOD shape and activity | [69] |
| Ag | HaCaT and A549 | Thioredoxin reductase | Decreased expression of selenoproteins | [70] |
| Ag and Ag+ | HepG2 and human hepatocytes | PRDXs, GST, myosin, elongation fac-tor 1, 60S ribosomal protein, and 40S ribosomal protein | Direct binding | [71] |
| CdTe quantum dots | n/a | GPx3 | Direct binding through Van der Waals’ forces and hydrogen bonding, resulting in structural changes with increased alpha helical content | [72] |
| CdTe quantum dots | n/a | GPx3 | Interactions with glutamate 136, phenylalanine 132, proline 130, and valine 129 in the GPx3 active site | [73] |
| 4Cu and CuO | RAW264.7 | PRDX1, PRDX2, PRDX3, and PRDX6 | Increased protein levels of the oxidized form of PRDX1 and the native form of PRDX6, with no change in the levels of PRDX2 and PRDX3 | [74] |
| r/aTiO2, rTiO2 silica-coated, rTiO2 alumina-coated, aTiO2, and mwCNT | Human lung epithelial cells and human monocyte-derived macrophages | PRDXs | Association of the nanoparticles with PRDXs | [75] |
| Selenium-Lovastatin | Female albino rats | Se-dependent GPx | Increased enzyme activity | [76] |
| TiO2 | n/a | CAT and SOD | Conformational and functional changes with an increase in alpha helical content and increased exposure of hydrophobic regions | [77] |
| Pb2+, Hg2+, Cd2+, Fe3+, Cu2+, Al3+ | n/a | Human erythrocyte GR | Competitively inhibited by Pb2+, Hg2+, Cd2+, Fe3+; and non-competitively inhibited by Cu2+ and Al3+ | [78] |
| ZnO | Male C57BL/6 mouse liver | PDI-3 | Increased PDI-3 gene expression | [79] |
| ZVFe | Human lymphocytes | Hb | Heme displacement and degradation, and induction of protein carbonylation | [80] |
| Immune Response | Type of Nanoparticle | Experimental Model | Main Findings | References |
|---|---|---|---|---|
| Induced Immune Response | Ag | Male NMRI mice | Induced B-cell proliferation | [103] |
| Ag NP infused hydrogel | Diabetic rat model | Induced T-cell and macrophage proliferation and significantly decreased wound healing time | [104] | |
| Ag | RAW 264.7 | Increased the expression of TLR-3 with no change in expression of TLR-4 | [105] | |
| Ag2O | THP-1 | Increased TLR-6 gene expression | [106] | |
| Al | Male ICR mice | Oxidative damage, neutrophil dysfunction, and increased expression of TNF-α, IFN-γ, IL-1α, IL-1β, IL-2, IL-6, and IL-10 | [107] | |
| ALOOH | THP-1 | Increased TLR-4 and TLR-6 gene expression | [106] | |
| Ce | Cytotoxic T-cells | Activation of cytotoxic T-cells and increased killing activity through decreased ROS, increased NF-κB signaling, increased cytokine production (IL-2 and TNF-α), and increased production of granzyme B and perforin | [108] | |
| CuO | Female mice | Proliferation and cytokine production by the T-cells and B-cells that changed over time | [109] | |
| CuO | THP-1 | Increased TLR-4 and TLR-6 gene expression | [106] | |
| Iron oxide | THP-1 | Increased TLR-6 gene expression | [106] | |
| Superparamagnetic iron oxide | Mouse macrophages | Activated TLR-4 receptors, increased the expression of inflammatory cytokines, triggered the translocation of Nrf2 to the nucleus, stimulated autophagy, and increased the gene expression of SR-AI | [110] | |
| TiO2 | THP-1 | Increased TLR-4 and TLR-6 gene expression | [106] | |
| ZnO | THP-1 | Increased TLR-4 and TLR-6 gene expression | [106] | |
| No Change or Decreased Immune Response | Ag | Rats | Increased T-cell, B-cell, and natural killer cell proliferation; decreased natural killer cell activity; and decreased production of IFN-γ in the spleen | [111] |
| Au | Female C57BL/6J mice | No change in lymphocyte cell population, however, increased T-cell population was observed in mice that were pre-sensitized to Au | [112] | |
| Carbon nanotubes (amino-functionalized) | PBMCs and C57Bl/6 mice | Decreased monocyte and macrophage cell populations in PBMCs, but not in C57Bl/6 mice | [113] | |
| Graphene | J774 | Decreased the gene expression of TLR-5 and decreased the production of IL-1β and IL-6 | [114] | |
| Multi-wall carbon nanotubes | J774 | Decreased the gene expression of TLR-5 and decreased the production of IL-1β and IL-6 | [114] | |
| Attenuated an Induced Immune Response | Ag | Rats | Decreased the level of IgG induced by KLH | [115] |
| Ag and Au | Murine splenic lymphocytes and human blood lymphocytes | Decreased immune cell proliferation stimulated by LPS, Concanavalin A, phytohemagglutinin, or pokeweed mitogen. No change occurred in the unstimulated cells. | [116] | |
| Superparamagnetic iron oxide | RAW264.7 | Attenuated the immune response induced by LPS with decreased expression levels of TLR-4 and NOS, and decreased levels of IL-6 and TNF-α. | [117] |
| Anti-Inflammatory or Pro-Inflammatory | Type of Nanoparticle | Experimental Model | Main Findings | References |
|---|---|---|---|---|
| Anti-inflammatory | Ag | RAW264.7 cells | Inhibition of pro-inflammatory cytokines | [165,170] |
| Ag | BMDMs from C57/BL6 mice | Decrease of NLRP3 inflammasome levels | [172] | |
| Au | Rats | Inhibition of production of pro-inflammatory cytokines, induction of IL-10 | [149] | |
| Au | Mice | Decreased levels of NF-κB and IL-1β | [199] | |
| Au | RAW264.7 cells | Suppression of pro-inflammatory cytokines, inhibition of the activation of the JAK-STAT pathway | [150] | |
| Au | LPS-induced Mouse primary microglia | Decreased production of inflammatory cytokines, mediators, and downregulation of the LPS-induced NF-κB, MAPK, and JAK-STAT signaling pathways | [160] | |
| Au | LPS-induced RAW264.7 cells | Decreased LPS-induced inflammatory mediators, inhibition of LPS-induced activation of the MAPK and NF-κB signaling pathways | [218] | |
| Ce | Human dendritic cells | Increased production of anti-inflammatory cytokine IL-10 | [136] | |
| Gadofullerene | Diabetic mice | Decreased expression of pro-inflammatory cytokines (NF-κB, TNF-α, IL-6, and IL-1β) | [154] | |
| Gadofullerene | Kupffer cells | Decreased LPS-induced inflammatory cytokines | [213] | |
| Se | Type 2 diabetes rat | Decreased expression of pro-inflammatory cytokines (TNF-α, IL-6, and IL-1β) | [156] | |
| Se | RAW264.7 cells | Decreased gene expression of pro-inflammatory cytokines (IL-1 and TNF-α), increased gene expression of anti-inflammatory cytokine (IL-10), inhibition of NF-κB and MAPK pathways | [156] | |
| Pro-inflammatory | Ag | HepG2 | Activation of NLRP3 inflammasome | [177] |
| Ag | Human Monocytes | Activation of NLRP3 inflammasome | [176,179,219] | |
| Ag | Human keratinocytes | Activation of NLRP3 inflammasome | [166] | |
| Ag | RAW264.7 cells | Activation of NF-κB pathway | [181] | |
| Ag | THP-1 cells | Induce formation of pro-inflammatory chemoattractant, 5-HETE | [183] | |
| Au | Primary neonatal human epidermal keratinocytes | Increased production of pro-inflammatory cytokines, IL-1β, IL-1α, and IL-8 | [132] | |
| Carbon (graphene) | RAW264.7 cells | Increased secretion of TNF-α | [205] | |
| Carbon (graphene) | BALB/c mice (in vivo and in vitro) | Activation of NF-κB pathway, increased production of pro-inflammatory cytokines | [201] | |
| Carbon (graphene) | Primary mouse macrophages | Activation of NF-κB pathway | [212] | |
| SiO2 | NCI-H292 cells | Increase of production of pro-inflammatory cytokines (TNF-α, IL-6, and IL-8) | [130,133] | |
| SiO2 | HUVECs | Activation of MAPK signaling | [200] | |
| SiO2 | Huh7 cells | Induction of MAPK genes and increased expression of pro-inflammatory cytokines, TNF-α and IL-8 | [158] | |
| SiO2 | Ovalbumin-induced asthmatic mice | Activation of NLRP3 inflammasome, increased number of immune cells, inflammatory cytokine production (IL-1β, IL-6, and TNF-α), inflammation of airway | [130] | |
| SiO2 | NCI-H292 cells | Activation of NLRP3 inflammasome, increase in gene expression of pro-inflammatory cytokines (IL-1β, IL-6, and TNF-α) | [130] | |
| SiO2 | Mouse dendritic cells | Activation of NLRP3 inflammasome | [197] | |
| TiO2 | Male Wistar rats | Concentration dependent activation of M1 macrophages | [131] | |
| TiO2 | Human macrophages | Induction of IL-6 and high dose resulted in induction of IL-1β and IL-10 | [188] | |
| TiO2 | K562 cells | Activation of NF-κB pathway | [193] | |
| TiO2 | RAW264.7 | Activation of NF-κB pathway | [181] | |
| TiO2 | Human dermal fibroblasts | Activation of NF-κB pathway | [195] | |
| TiO2 | HUVECs | Activation of NF-κB pathway, increased ROS and ●NO production | [199] | |
| TiO2 | Human dendritic cells | Activation of NLRP3 inflammasome | [136] | |
| TiO2 | THP-1 cells | Activation of NLRP3 inflammasome | [186] | |
| TiO2 | Murine dendritic cells | Activation of NLRP3 inflammasome | [197] | |
| TiO2 | C57BL/6 mice | Induction of pro-inflammatory cytokine production | [202] | |
| ZnO | THP-1 cells | Activation of NF-κB and MAPK pathways | [137] | |
| ZnO | Macrophages from female BALB/c mice | Activation of MAPK and NF-κB pathways | [101] | |
| ZnO | Primary mice dendritic cells | Increased production of pro-inflammatory cytokines IL-6 and TNF-α | [214] |
| Mitochondrial Function | Type of Nanoparticle | Experimental Model | Main Findings | References |
|---|---|---|---|---|
| Intrinsic Apoptosis | Ag | HepG2 | Activation of intrinsic apoptosis | [230] |
| Ag | HCT116 | Activation of intrinsic apoptosis | [231] | |
| Ag | MCF-7 | Activation of intrinsic apoptosis | [232] | |
| Ag | HT22 | Intrinsic apoptosis alleviated with selenium | [241] | |
| Au | HT-29 | Activation of intrinsic apoptosis | [237] | |
| Au nanostars | MCF-7 | Activation of intrinsic apoptosis | [238] | |
| Au nanoprisms | MEFs transformed with SV40 | Activation of intrinsic apoptosis | [239] | |
| Cu | Female Sprague-Dawley rats | Intrinsic apoptosis in the uterine tissue | [242] | |
| Cu | Swiss albino male mice | Oxidative stress, intrinsic apoptosis, and extrinsic apoptosis in the kidney tissue | [243] | |
| Cu | A-357 | Activation of intrinsic apoptosis | [229] | |
| Fullerene derivative C60(C(COOH)2)2 | HeLa | Alleviated stimulated Cyt c release, intrinsic apoptosis, and mitochondrial membrane potential decrease | [244] | |
| Nanoplastic polystyrene | A549 | Activation of intrinsic apoptosis | [52] | |
| N-Succinyl-chitosan | K562 | Activation of intrinsic apoptosis | [236] | |
| Phloretin loaded chitosan | Human oral cancer cells | Activation of intrinsic apoptosis | [235] | |
| SiO2 | SH-SY5Y | Activation of intrinsic apoptosis | [21] | |
| Superparamagnetic iron oxide | PC12 | Activation of intrinsic apoptosis | [233] | |
| Quantum dots (cadmium sulphide) | HepG2 | Activation of intrinsic apoptosis | [234] | |
| ZnO | HAECs | Intrinsic apoptosis alleviated with alpha-lipoic acid | [240] | |
| Fission and Fusion | Ag | Sprague-Dawley rats | Increased fission (protein expression of Drp1, p-Drp1, and Fis1 increased) and decreased fusion (protein expression of Opa1 and Mfn2 decreased) | [224] |
| Ag | iPSCs | Increased fission and decreased fusion | [245] | |
| Ag | HepG2 | Increased fission, decreased fusion, and decreased mitochondrial biogenesis (protein expression of PGC-1α decreased) | [222] | |
| Au (combined with TRAIL) | NSCLC cells in female BALB/c mice | Increased fission (increased Drp1) | [246] | |
| Carbon black FW2 | HPAECs | Increased oxidative stress, fission, and intrinsic apoptosis | [49] | |
| Si | HUVECs | Increased oxidative stress, fission (increased Fis1, Drp1), and intrinsic apoptosis; decreased fusion (decreased Opa1) | [247] | |
| Energy Production | Ag | HepG2, HeLa, A498, PC3, HEK293T | Mitochondrial dysfunction, decreased ATP production, decrease in oxidative phosphorylation, and increase in glycolysis | [253] |
| Ag | HSC-3 | Mitochondrial depolarization | [268] | |
| Ag | PANC-1 | Decreased mitochondrial membrane potential | [261] | |
| Ag | Mitochondria from rat liver | Mitochondrial swelling, decreased mitochondrial membrane potential, and uncoupling of oxidative phosphorylation | [262] | |
| Ag | Male Wistar rats | Decrease in oxidative phosphorylation and increased ROS | [255] | |
| Al | Mitochondria from male Wistar rat brain tissue | Increased ROS mainly through inhibition of coenzyme Q-cytochrome c oxidoreductase (complex III) and induced intrinsic apoptosis | [259] | |
| Au | HSC-3 | Decreased ATP | [268] | |
| Carbon nanotubes (single walled and multiwalled) | F10 cells transplanted in a C57 mouse | Decreased mitochondrial membrane potential, decreased succinate dehydrogenase (complex II) activity, and increased intrinsic apoptosis | [256] | |
| Fe2O3 | Male albino mice | Cardiac dysfunction with damaged mitochondria, decreased ATP production, increased ROS, and intrinsic apoptosis | [263] | |
| Fe2O3 | F10 cells transplanted in a C57 mouse | Decreased mitochondrial membrane potential, decreased succinate dehydrogenase (complex II) activity, and increased intrinsic apoptosis | [256] | |
| SiO2 | U87 | Decreased cytochrome c oxidase (complex IV) subunit II protein expression | [258] | |
| Ti | Male Wistar rats | Decrease in oxidative phosphorylation and increased ROS | [255] | |
| TiO2 | Human lymphocytes | Decreased succinate dehydrogenase (complex II) activity | [254] | |
| TiO2 | WI-38 | Decreased mitochondrial membrane potential | [43] | |
| ZnO | A549 | Decreased cytochrome c oxidase (complex IV) and F1F0-ATPase (complex V) activity | [257] |
| Signaling Pathway | Type of Nanoparticle | Experimental Model | Main Findings | References |
|---|---|---|---|---|
| Insulin | Ag | Male Sprague Dawley rats | Increased levels of IRS-1, Akt, GSK3β | [288] |
| Ag | Male albino rats | Reduction of blood glucose, and increase in serum insulin, glucokinase activity, expression of insulin, insulin receptor, GLUT-2 and glucokinase genes | [277] | |
| Au | RIN-5F cells | Increased insulin secretion, decreased apoptosis, and increased gene and protein expression of IRS-1, GLUT2, and the insulin receptor | [284] | |
| Gadofullerene (functionalized with β-alanine) | Diabetic mice | Activated IRS2/PI3K/Akt signalling pathway, normalized blood sugar levels | [154] | |
| Ni | Rat testicular Sertoli-germ cells | Upregulation of the gene and protein expression of IGFBP-3 | [272] | |
| Platinum | HepG2 cells | Increased activation of Akt | [26] | |
| Se | Diabetic male Wistar rats | Normalized fasting blood glucose level, reduction of insulin level, normalized levels of phosphorylated: IRS-1, Akt, GSK-3β, and AMPK | [155] | |
| Superparamagnetic iron oxide | Diabetic male Wistar rats | Normalized fasting blood glucose levels, reduction of insulin level, increased levels of P13K and GSK-3β resulting in increased glucose uptake and decreased insulin resistance | [275] | |
| TiO2 | Male CD-1 mice | Increase in blood glucose level, increased IRS-1 phosphorylation, and decreased phosphorylation of Akt | [289] | |
| ZnO | Male Sprague-Dawley rats | Decreased serum level of IGF-1 | [270] | |
| ZnO | Streptozotocin-induced diabetic male albino rats | Normalized fasting blood glucose, insulin, and insulin resistance score levels, and improved diabetic vascular complications | [286,287] | |
| ZnO | Male albino rats | Reduction of blood glucose, and increase in serum insulin, glucokinase activity, expression of insulin, insulin receptor, GLUT-2 and glucokinase genes | [39] | |
| ZnO | Obese C57BL/6 mice | Decreased insulin resistance | [279] | |
| Calcium | Ag | SH-SY5Y | Induced release of calcium from ER | [295] |
| Ag | SH-SY5Y, Sprague-Dawley rats | Increased intracellular calcium level, activation of CaMKKβ and AMPK | [298] | |
| Ag | Zebrafish embryos | Downregulation of calcium signaling | [301] | |
| Ag | Rat CGCs | Increased intracellular calcium level | [296] | |
| Ag | Human embryonic stem cell-derived glutamatergic neurons | Decreased expression of NMDA receptor subunits | [305] | |
| Ag | Male Wistar rats | Increased gene expression of NMDA receptor subunits NR1, NR2A, and NR2B in the brain tissue | [306] | |
| Carbon | PASMCs | Increased intracellular calcium level | [297] | |
| Carbon black | Human pulmonary artery endothelial cells | Increased intracellular calcium level | [49] | |
| CuO | RCC | Increased intracellular calcium level | [299] | |
| NiO | BEAS-2B cells | Increased intracellular calcium level | [300] | |
| MgO | Male Wistar rats | Decreased level of glutamate, increased gene expression of NMDA subunit NR2B in the hippocampus | [303] | |
| Si | HUVECs | Increased intracellular calcium level, decreased activity of Ca2+-ATPase, Ca2+/Mg2+-ATPase, and Na+/K+-ATPase | [347] | |
| SiO2 | PASMCs | Increased intracellular calcium level | [52] | |
| TiO2 | PASMCs | Increased intracellular calcium level | [52] | |
| Nitric Oxide | Ag | Rat smooth muscle tracheal rings | Increased iNOS protein expression, ●NO production, activation of muscarinic receptors | [310] |
| Ag | ASM cells from male Wistar rats | Increased iNOS expression, ●NO production, and activation of muscarinic receptors | [311] | |
| Ag | SVEC4-10 mouse endothelial cells and hFOB 1.19 cells | Increased iNOS expression and ●NO production | [313,348] | |
| Ag | Human embryonic stem cell-derived glutamatergic neurons | Increased iNOS and nNOS expression | [305] | |
| Ag | Chicken sertoli cells | Increased gene expression of iNOS and eNOS | [314] | |
| Ag | LPS-induced RAW 264.7 cells | Decreased ●NO and iNOS expression | [168] | |
| Ag | Isolated perfused hearts from rats | Increased ROS, decreased ●NO production, decreased iNOS and eNOS expression, but increased expression of phosphorylated eNOS | [315] | |
| Ag | C57BL/6J male mice fed high-fat Western diet | Decreased iNOS gene expression | [317] | |
| Au | RAW 264.7 cells | Decreased ●NO and iNOS expression | [150,168,218,318] | |
| Au | Mouse BV-2 microglial cells | Decreased ●NO and iNOS expression | [160] | |
| Au | Rhesus macaque choroid-retinal endothelial RF/6A cells | Decreased VEGF-induced eNOS phosphorylation | [312] | |
| Carbon | Aluminum-induced Alzheimer’s male albino Wistar rats | Normalized iNOS expression | [334] | |
| Carbon (graphene QDs) | HepG2 cells | Decreased ●NO production | [335] | |
| Carbon (multi-walled nanotubes) | RAW 264.7 cells | Increased iNOS expression | [342] | |
| Chitosan | Male albino Wistar rats induced with carcinoma | Normalized ●NO level | [344] | |
| Se (capped with Ganoderma lucidum polysaccharides) | LPS-induced RAW 264.7 cells | Normalized ●NO level | [156] | |
| CeO2 | Male Sprague Dawley rats with LPS-induced sepsis and Kupffer cell macrophages | Decreased iNOS gene and protein expression and ●NO production | [36,213] | |
| CeO2 | Male Sprague Dawley rats | Decreased ●NO production | [35] | |
| Cu | Wistar albino rats with induced myocardial infarction | Normalized serum ●NO level | [331] | |
| Cu | Male Sprague-Dawley rats | Increased levels of ROS, iNOS, and ●NO in the liver tissue | [332] | |
| Cu | LPS-induced primary macrophages from C57BL/6 mice | Normalized ●NO level | [333] | |
| Cu | LPS-induced primary mouse macrophages | Normalized ●NO level | [74] | |
| Hydroxyapatite | HUVECs | Decreased ●NO production and phosphorylated eNOS expression | [345] | |
| MnO2 | Cytokine-challenged cartilage explants | Decreased ●NO level | [343] | |
| Propylene glycol alginate sodium sulfite | Streptozotocin-induced diabetic male Wistar rats | Inhibited diabetes-induced decrease in NOS activity and ●NO level | [346] | |
| Pt | LPS-induced RAW 264.7 cells | Decreased ●NO and iNOS expression | [327,349] | |
| Pt | THP-1 cells | Increased ●NO level | [25] | |
| TiO2 nanotubes | HUVECs | Downregulation of eNOS transcription factors (KLF2 and KLF4), and decreased ●NO level, resulting in decreased eNOS expression | [325] | |
| Si | Male Wistar rats | Increased ●NO level in the liver and kidneys | [338] | |
| Si | HUVECs | Increased ●NO levels, increased iNOS expression, and decreased eNOS expression | [339] | |
| Si | HUVECs | Decreased ●NO level, decreased expression of total NOS and eNOS, and increased iNOS expression | [340] | |
| Superparamagnetic FeO | LPS-induced RAW 264.7 cells | Increased ●NO level | [117] | |
| Superparamagnetic FeO | RAW 264.7 cells | Decreased iNOS expression | [336,337] | |
| ZnO | LPS-induced RAW 264.7 cells | Normalized iNOS expression and ●NO production | [326] | |
| ZnO | Streptozotocin-induced diabetic male albino rats | Normalized iNOS expression and ●NO production | [287] | |
| ZnO | Bacterial infection with nontypeable Haemophilus influenzae infected RAW 264.7 cells and C57BL/6 mice | Normalized iNOS expression and ●NO production | [350] | |
| ZnO | Human coronary artery endothelial cells | Increased iNOS and ●NO levels | [328] | |
| ZnO | BALB/c mice macrophages | Increased iNOS and ●NO levels | [101] | |
| ZnO | THP-1 cells | Increased iNOS and ●NO levels | [137] | |
| ZnFe2O4 | Human amnion epithelial cells | Increased iNOS expression | [330] |
| Protein Interaction | Type of Nanoparticle | Experimental Model | Protein(s) Affected | Main Findings | References |
|---|---|---|---|---|---|
| Zinc-dependent | CuO | A549 cells | HDAC | Inhibition of protein activity | [361] |
| ZnO | SH-SY5Y cells | ZnT1 and ZIPs | Increased protein expression | [363] | |
| Copper-dependent | Ag | n/a | AChE | Disruption of secondary structure, decrease of protein activity | [421] |
| CuO | Renal cell carcinoma cells | Copper chaperones | Regulates the chaperones, resulting in copper transportation disruption | [299] | |
| SiO2 | Drosophila melanogaster | Copper transporters | NPs competitively bound to proteins, resulting in copper deficiency | [372] | |
| Iron-dependent | Ag | n/a | Hb (human) | Induction of slight changes to secondary structure | [399] |
| Ag | n/a | Hb (human) | Induction of structural changes | [400] | |
| Ag | n/a | Hb (bovine) | Induction of changes to both secondary and tertiary structures | [401] | |
| Al2O3 | n/a | Hb (human) | Induction of changes to quaternary structure | [409] | |
| Au | n/a | Transferrin | Changes to secondary structure | [373,382] | |
| CeO2 | n/a | Hb (human) | Degradation of heme, structural changes | [404] | |
| CeO2 | n/a | Hb (human) | Induction of changes to secondary structure | [405] | |
| Fe (zero valent) | n/a | Hb (human) | Induction of changes to tertiary structure | [80] | |
| Graphene oxide | n/a | Hb (human) | Degradation of quaternary and secondary structure | [407] | |
| Iron oxide | n/a | Cyt c | Reduction of heme group in non-PEG coated NPs | [389] | |
| Magnetic NPs (Fe III and Fe II) | n/a | Lactoferrin | NPs absorbed onto protein | [385] | |
| NiO | n/a | Hb | Induction of changes to secondary and quaternary structure | [410] | |
| Manganese | n/a | Cyt c | Induction of conformational changes to tertiary structure | [391] | |
| Si | n/a | Cyt c | Adsorption of protein to NPs resulting in structural stabilization, however the active site became inaccessible to ligands | [387] | |
| Si | n/a | NPs absorbed onto Cyt c resulting in conformational changes and modifications to the active site | [388] | ||
| Si | n/a | Hb (porcine and human) | Loss of secondary structure | [20] | |
| Si | n/a | Hb (bovine) | Structural changes and heme degradation | [395] | |
| SiO2 | n/a | Hb (human) | Structural changes, heme degradation, release of iron from Hb | [124] | |
| SiO2 | n/a | Hb (human) | Adsorption of protein to NPs | [360] | |
| ZnO | n/a | Hb (human) | Induction of structural changes | [398] | |
| TiO2 | Human erythrocytes | Hb (human) | Induction of structural changes and degradation of heme group | [396] | |
| Calcium-dependent | CaF2 | n/a | Calmodulin | Irreversible binding | [418] |
| Protein Interaction | Type of Nanoparticle | Experimental Model | Protein(s) Affected | Main Findings | References |
|---|---|---|---|---|---|
| Phase I Detoxification Enzymes | Diamond and graphite | Microsomal based models | CYP1A2, CYP2D6, and CYP3A4 | Inhibition of activity | [427] |
| Camptothecin encapsulated PLGA | HepG2 cells | CYP3A4 | Dose-dependent decrease in activity | [423] | |
| Phase II Detoxification Enzymes | ZnO | Testicular tissue in diabetic rats | GST | Increase in activity | [432] |
| Ag | Mice with induced liver cancer | GST | Increase in levels | [431] | |
| Amorphous Si | HepG2 cells | GST | Decrease in activity | [433] | |
| Metallothioneins | Ag | n/a | MT-1 | Adsorbed to protein | [442] |
| Ag | J774.1 cells, UV-vis and CD | MT-1 | Ag+ ions released from NPs replaced native metals on MT-1 | [443] | |
| Ag | n/a | MT-1 | Ag+ ions released from NPs replaced native metals on MT-1 | [442] | |
| CeO2 | n/a | MT | Interaction with thiol groups | [444] | |
| CuO | HepG2 | MT-1 | Cu ions released from NPs replaced Zn bound to MT-1 | [445] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cameron, S.J.; Sheng, J.; Hosseinian, F.; Willmore, W.G. Nanoparticle Effects on Stress Response Pathways and Nanoparticle–Protein Interactions. Int. J. Mol. Sci. 2022, 23, 7962. https://doi.org/10.3390/ijms23147962
Cameron SJ, Sheng J, Hosseinian F, Willmore WG. Nanoparticle Effects on Stress Response Pathways and Nanoparticle–Protein Interactions. International Journal of Molecular Sciences. 2022; 23(14):7962. https://doi.org/10.3390/ijms23147962
Chicago/Turabian StyleCameron, Shana J., Jessica Sheng, Farah Hosseinian, and William G. Willmore. 2022. "Nanoparticle Effects on Stress Response Pathways and Nanoparticle–Protein Interactions" International Journal of Molecular Sciences 23, no. 14: 7962. https://doi.org/10.3390/ijms23147962
APA StyleCameron, S. J., Sheng, J., Hosseinian, F., & Willmore, W. G. (2022). Nanoparticle Effects on Stress Response Pathways and Nanoparticle–Protein Interactions. International Journal of Molecular Sciences, 23(14), 7962. https://doi.org/10.3390/ijms23147962






