Maternal Acetate Supplementation Reverses Blood Pressure Increase in Male Offspring Induced by Exposure to Minocycline during Pregnancy and Lactation
Abstract
:1. Introduction
2. Results
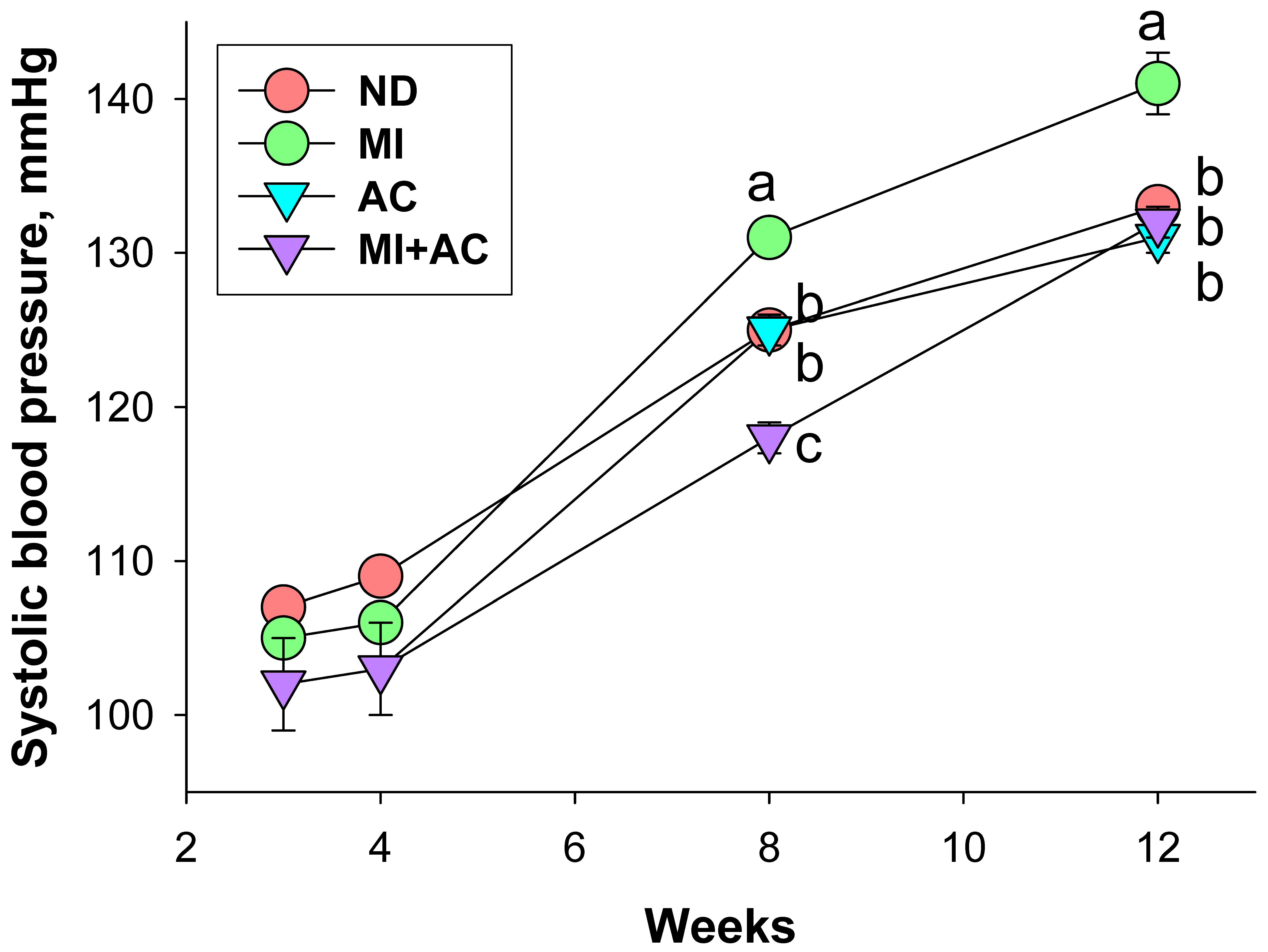
2.1. Body Weight and Blood Pressure
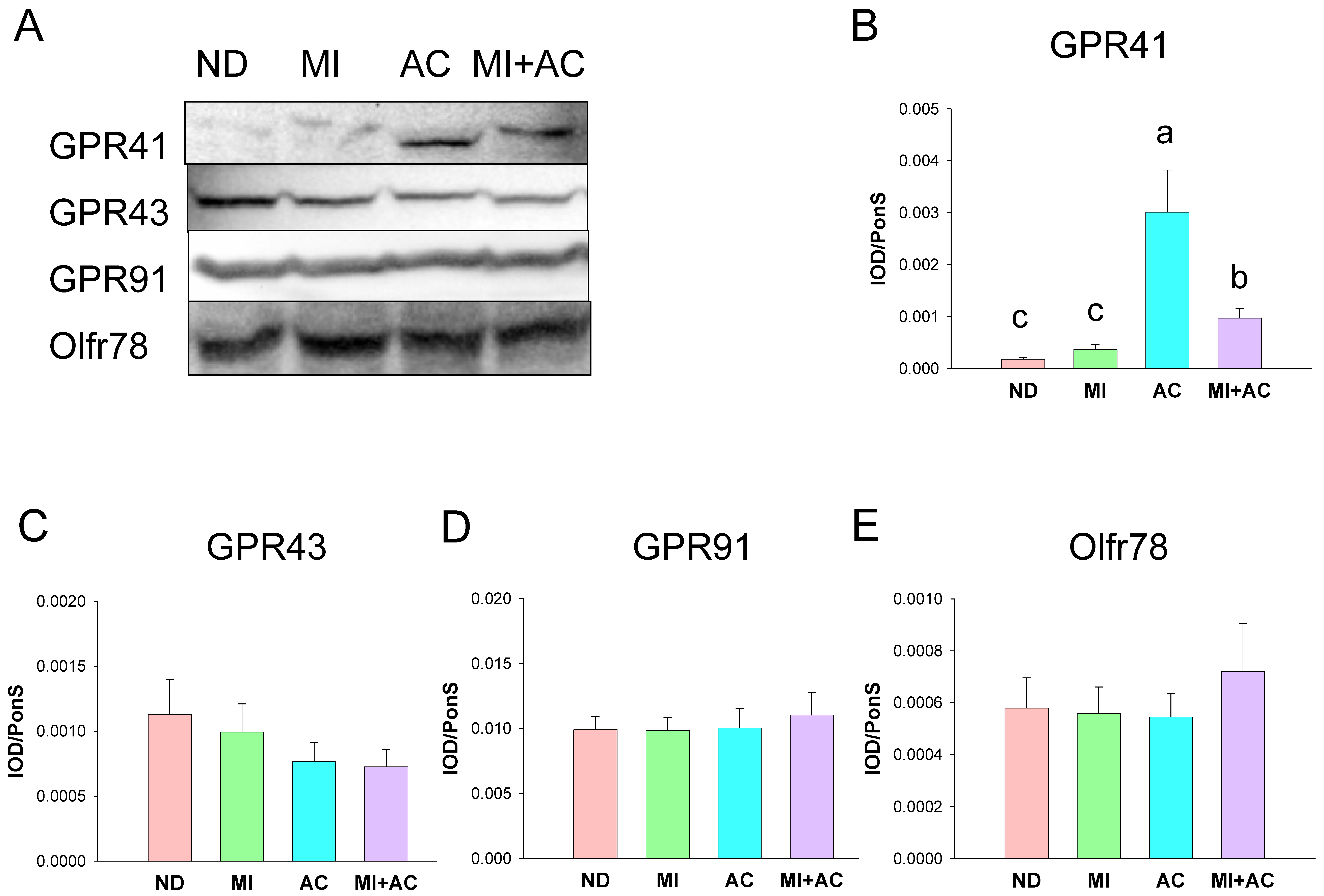
2.2. SCFA Levels and SCFA Receptors
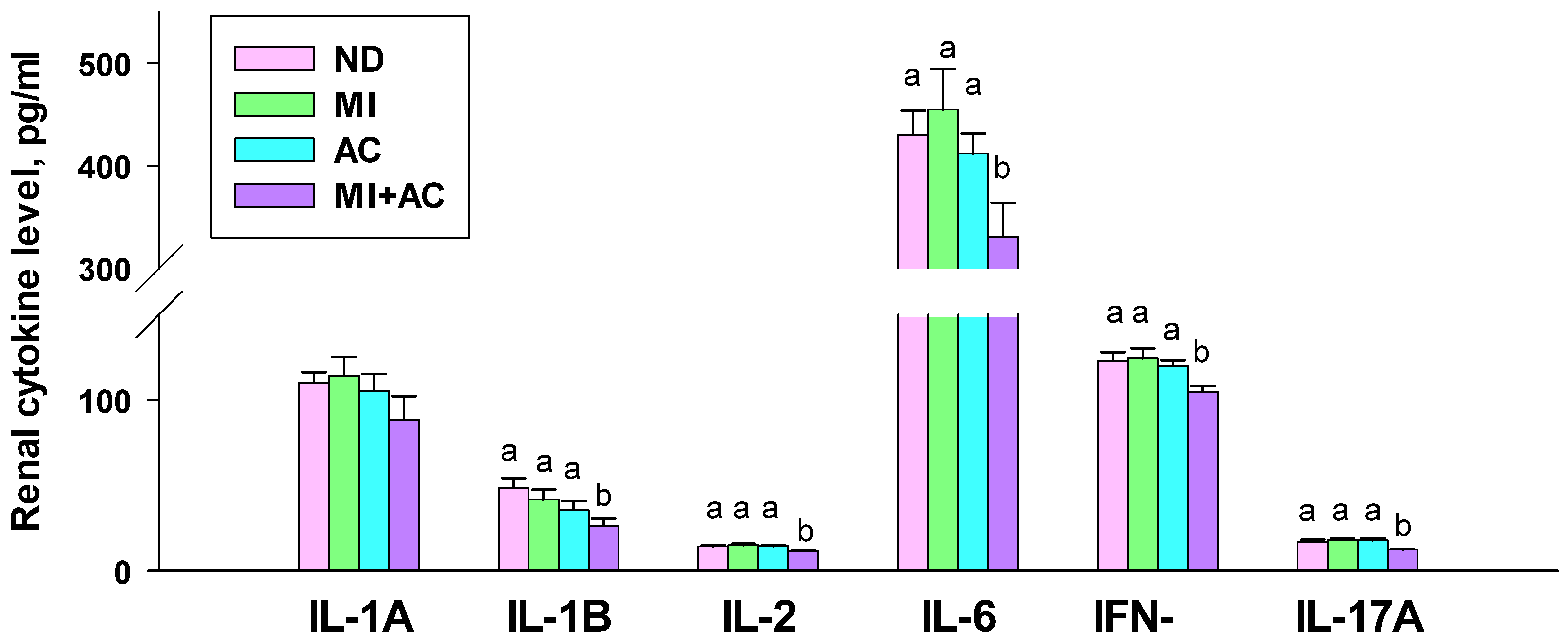
2.3. Cytokine Concentrations in the Kidneys
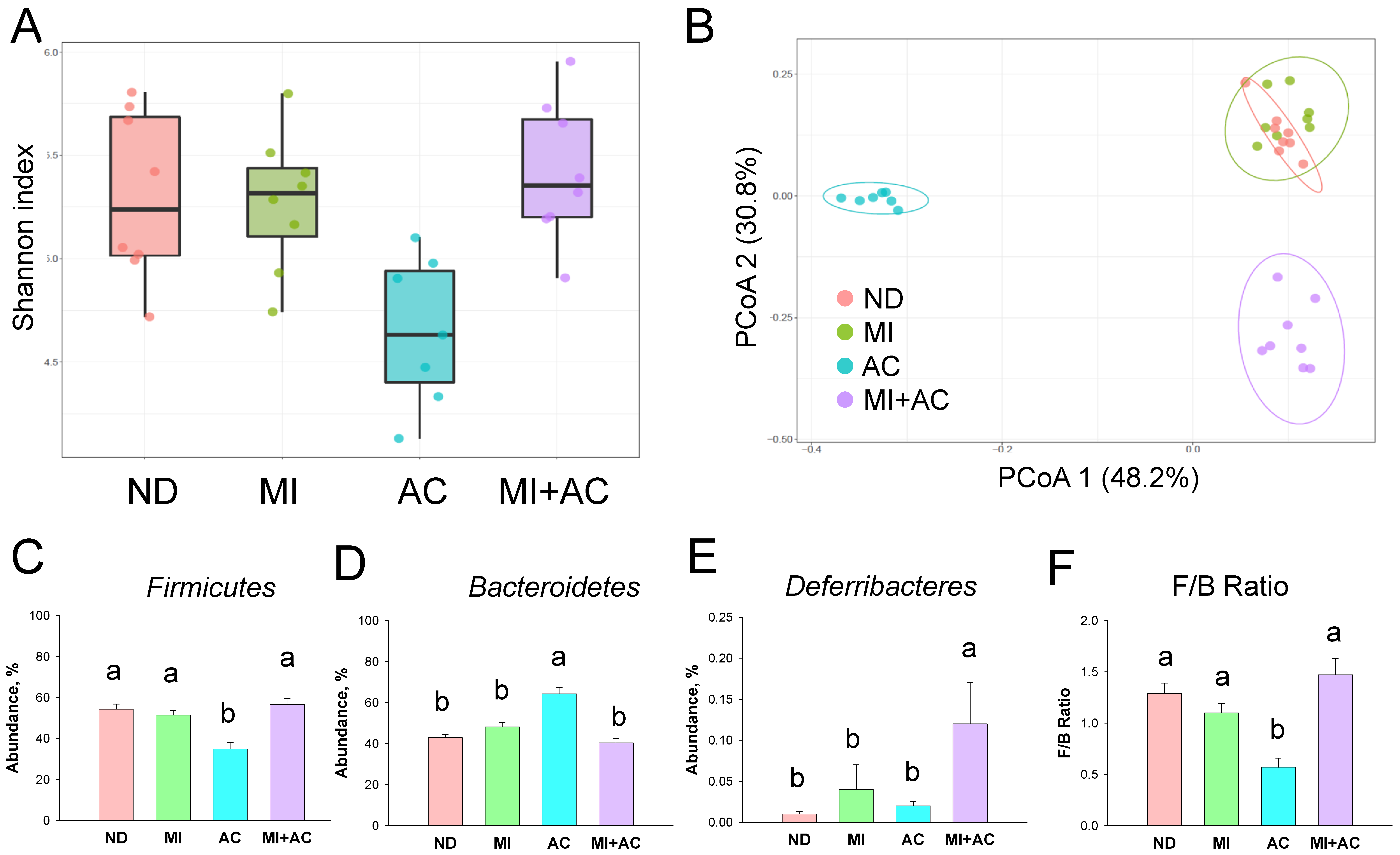
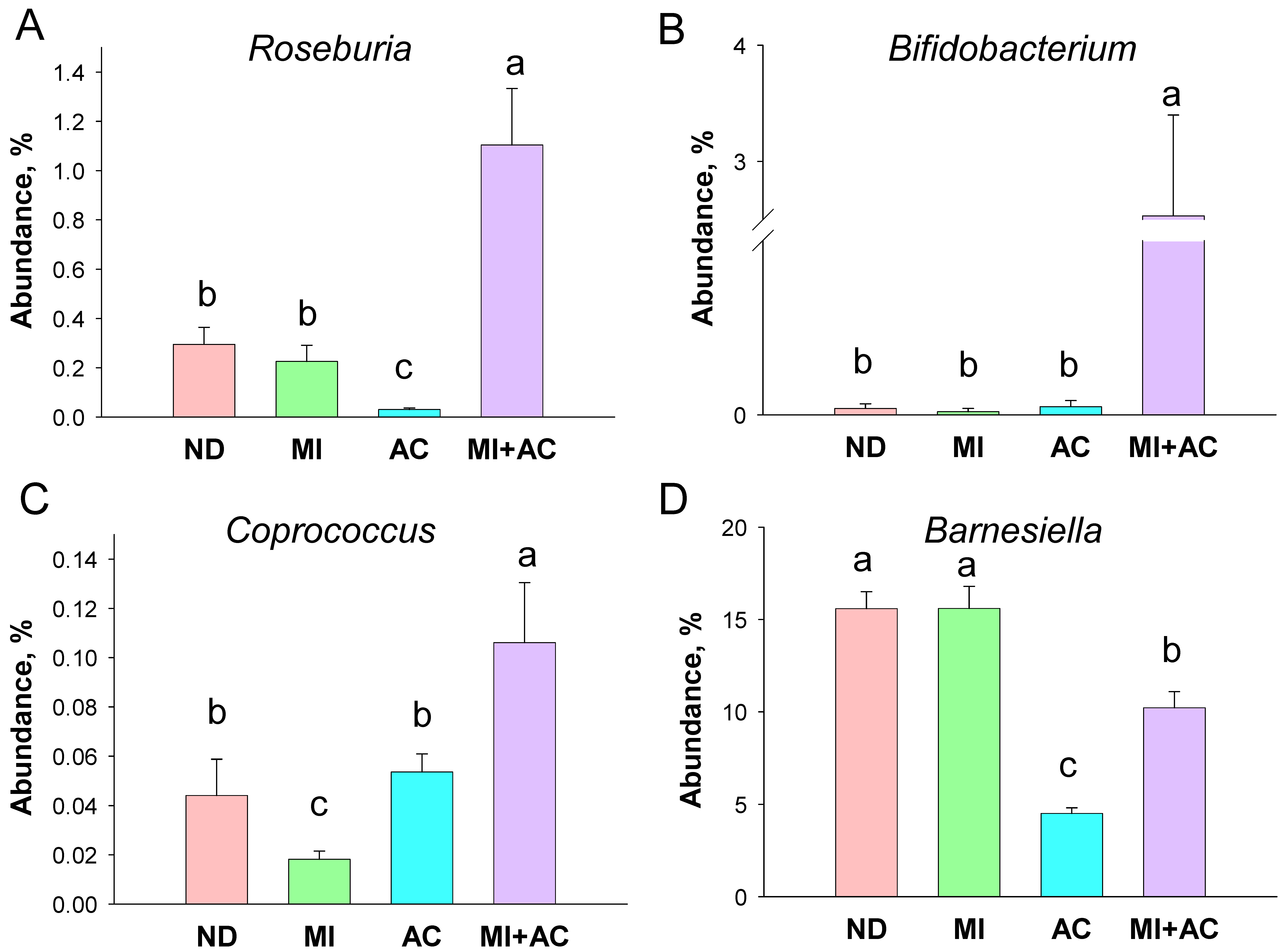
2.4. Gut Microbiota Composition
2.5. NO-Related Parameters
3. Discussion
4. Materials and Methods
4.1. Animal Experimental Research Design
4.2. Gas Chromatography-Mass Spectrometry (GC-MS)
4.3. Western Blot
4.4. Determination of Cytokines in the Kidneys
4.5. Nitric Oxide-Related Parameters
4.6. Gut Microbiota Composition
4.7. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hsu, C.N.; Tain, Y.L. The Good, the Bad, and the Ugly of Pregnancy Nutrients and Developmental Programming of Adult Disease. Nutrients 2019, 11, 894. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Suzuki, K. The developing world of DOHaD. J. Dev. Orig. Health Dis. 2018, 9, 266–269. [Google Scholar] [CrossRef]
- Paauw, N.D.; Van Rijn, B.B.; Lely, A.T.; Joles, J.A. Pregnancy as a critical window for blood pressure regulation in mother and child: Programming and reprogramming. Acta Physiol. 2016, 219, 241–259. [Google Scholar] [CrossRef] [Green Version]
- Hsu, C.N.; Tain, Y.L. The double-edged sword effects of maternal nutrition in the developmental programming of hypertension. Nutrients 2018, 10, 1917. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chu, D.M.; Meyer, K.M.; Prince, A.L.; Aagaard, K.M. Impact of maternal nutrition in pregnancy and lactation on offspring gut microbial composition and function. Gut Microbes 2016, 7, 459–470. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yang, T.; Santisteban, M.M.; Rodriguez, V.; Li, E.; Ahmari, N.; Carvajal, J.M.; Zadeh, M.; Gong, M.; Qi, Y.; Zubcevic, J.; et al. Gut dysbiosis is linked to hypertension. Hypertension 2015, 65, 1331–1340. [Google Scholar] [CrossRef] [Green Version]
- Sun, S.; Lulla, A.; Sioda, M.; Winglee, K.; Wu, M.C.; Jacobs, D.R., Jr.; Shikany, J.M.; LloydJones, D.M.; Launer, L.J.; Fodor, A.A.; et al. Gut microbiota composition and blood pressure. Hypertension 2019, 73, 998–1006. [Google Scholar] [CrossRef]
- Khodor, S.A.; Reichert, B.; Shatat, I.F. The microbiome and blood pressure: Can microbes regulate our blood pressure? Front. Pediatr. 2017, 5, 138. [Google Scholar] [CrossRef]
- Pluznick, J.L. Microbial short-chain fatty acids and blood pressure regulation. Curr. Hypertens. Rep. 2017, 19, 25. [Google Scholar] [CrossRef] [Green Version]
- Ziętek, M.; Celewicz, Z.; Szczuko, M. Short-Chain Fatty Acids, Maternal Microbiota and Metabolism in Pregnancy. Nutrients 2021, 13, 1244. [Google Scholar] [CrossRef]
- Pluznick, J.L.; Protzko, R.J.; Gevorgyan, H.; Peterlin, Z.; Sipos, A.; Han, J.; Brunet, I.; Wan, L.X.; Rey, F.; Wang, T.; et al. Olfactory receptor responding to gut microbiota-derived signals plays a role in renin secretion and blood pressure regulation. Proc. Natl. Acad. Sci. USA 2013, 110, 4410–4415. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ratajczak, W.; Rył, A.; Mizerski, A.; Walczakiewicz, K.; Sipak, O.; Laszczynska, M. Immunomodulatory potential of gut microbiome-derived short-chain fatty acids (SCFAs). Acta Biochim. Pol. 2019, 66, 1–12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Felizardo, R.J.F.; Watanabe, I.K.M.; Dardi, P.; Rossoni, L.V.; Câmara, N.O.S. The interplay among gut microbiota, hypertension and kidney diseases: The role of short-chain fatty acids. Pharmacol. Res. 2019, 141, 366–377. [Google Scholar] [CrossRef] [PubMed]
- Hsu, C.N.; Tain, Y.L. Animal Models for DOHaD Research: Focus on Hypertension of Developmental Origins. Biomedicines 2021, 9, 623. [Google Scholar] [CrossRef] [PubMed]
- Coker, M.O.; Hoen, A.G.; Dade, E.; Lundgren, S.; Li, Z.; Wong, A.D.; Zens, M.S.; Palys, T.J.; Morrison, H.G.; Sogin, M.L.; et al. Specific class of intrapartum antibiotics relates to maturation of the infant gut microbiota: A prospective cohort study. BJOG 2020, 127, 217–227. [Google Scholar] [CrossRef]
- Lange, K.; Buerger, M.; Stallmach, A.; Bruns, T. Effects of Antibiotics on Gut Microbiota. Dig. Dis. 2016, 34, 260–268. [Google Scholar] [CrossRef]
- Galla, S.; Chakraborty, S.; Cheng, X.; Yeo, J.; Mell, B.; Zhang, H.; Mathew, A.V.; Vijay-Kumar, M.; Joe, B. Disparate effects of antibiotics on hypertension. Physiol. Genom. 2018, 50, 837–845. [Google Scholar] [CrossRef]
- Hsu, C.N.; Chan, J.Y.H.; Wu, K.L.H.; Yu, H.R.; Lee, W.C.; Hou, C.Y.; Tain, Y.L. Altered Gut Microbiota and Its Metabolites in Hypertension of Developmental Origins: Exploring Differences between Fructose and Antibiotics Exposure. Int. J. Mol. Sci. 2021, 22, 2674. [Google Scholar] [CrossRef]
- Zółkiewicz, J.; Marzec, A.; Ruszczyn’ski, M.; Feleszko, W. Postbiotics—A step beyond pre- and probiotics. Nutrients 2020, 12, 2189. [Google Scholar] [CrossRef]
- Hsu, C.N.; Hou, C.Y.; Hsu, W.H.; Tain, Y.L. Cardiovascular diseases of developmental origins: Preventive aspects of gut microbiota-targeted therapy. Nutrients 2021, 13, 2290. [Google Scholar] [CrossRef]
- Soliman, M.L.; Smith, M.D.; Houdek, H.M.; Rosenberger, T.A. Acetate supplementation modulates brain histone acetylation and decreases interleukin1β expression in a rat model of neuroinflammation. J. Neuroinflamm. 2012, 9, 51. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marques, F.Z.; Nelson, E.; Chu, P.Y.; Horlock, D.; Fiedler, A.; Ziemann, M.; Tan, J.K.; Kuruppu, S.; Rajapakse, N.W.; El-Osta, A.; et al. High-Fiber Diet and Acetate Supplementation Change the Gut Microbiota and Prevent the Development of Hypertension and Heart Failure in Hypertensive Mice. Circulation 2017, 135, 964–977. [Google Scholar] [CrossRef] [PubMed]
- Hsu, C.N.; Chang-Chien, G.P.; Lin, S.; Hou, C.Y.; Tain, Y.L. Targeting on Gut Microbial Metabolite Trimethylamine-N-Oxide and Short-Chain Fatty Acid to Prevent Maternal High-Fructose-Diet-Induced Developmental Programming of Hypertension in Adult Male Offspring. Mol. Nutr. Food Res. 2019, 63, e1900073. [Google Scholar] [CrossRef] [PubMed]
- Hsu, C.N.; Tain, Y.L. Regulation of nitric oxide production in the developmental programming of hypertension and kidney disease. Int. J. Mol. Sci. 2019, 20, 681. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Galla, S.; Chakraborty, S.; Cheng, X.; Yeo, J.Y.; Mell, B.; Chiu, N.; Wenceslau, C.F.; Vijay-Kumar, M.; Joe, B. Exposure to Amoxicillin in Early Life Is Associated with Changes in Gut Microbiota and Reduction in Blood Pressure: Findings from a Study on Rat Dams and Offspring. J. Am. Heart Assoc. 2020, 9, e014373. [Google Scholar] [CrossRef] [PubMed]
- Azzam, O.; Kiuchi, M.G.; Ho, J.K.; Matthews, V.B.; Gavidia, L.M.L.; Nolde, J.M.; Carnagarin, R.; Schlaich, M.P. New Molecules for Treating Resistant Hypertension: A Clinical Perspective. Curr. Hypertens. Rep. 2019, 21, 80. [Google Scholar] [CrossRef] [PubMed]
- Natarajan, N.; Hori, D.; Flavahan, S.; Steppan, J.; Flavahan, N.A.; Berkowitz, D.E.; Pluznick, J.L. Microbial short chain fatty acid metabolites lower blood pressure via endothelial G protein-coupled receptor 41. Physiol. Genom. 2016, 48, 826–834. [Google Scholar] [CrossRef]
- Elijovich, F.; Laffer, C.L.; Sahinoz, M.; Pitzer, A.; Ferguson, J.F.; Kirabo, A. The Gut Microbiome, Inflammation, and Salt-Sensitive Hypertension. Curr. Hypertens. Rep. 2020, 22, 79. [Google Scholar] [CrossRef]
- López, P.; González-Rodríguez, I.; Gueimonde, M.; Margolles, A.; Suárez, A. Immune response to Bifidobacterium bifidum strains support Treg/Th17 plasticity. PLoS ONE 2011, 6, e24776. [Google Scholar] [CrossRef] [Green Version]
- Dan, X.; Mushi, Z.; Baili, W.; Han, L.; Enqi, W.; Huanhu, Z.; Shuchun, L. Differential Analysis of Hypertension-Associated Intestinal Microbiota. Int. J. Med. Sci. 2019, 16, 872–881. [Google Scholar] [CrossRef] [Green Version]
- Tamanai-Shacoori, Z.; Smida, I.; Bousarghin, L.; Loreal, O.; Meuric, V.; Fong, S.B.; Bonnaure-Mallet, M.; Jolivet-Gougeon, A. Roseburia spp.: A marker of health? Future Microbiol. 2017, 12, 157–170. [Google Scholar] [CrossRef] [PubMed]
- Ducatelle, R.; Eeckhaut, V.; Haesebrouck, F.; Van Immerseel, F. A review on prebiotics and probiotics for the control of dysbiosis: Present status and future perspectives. Animal 2015, 9, 43–48. [Google Scholar] [CrossRef] [PubMed]
- Altemani, F.; Barrett, H.L.; Gomez-Arango, L.; Josh, P.; David McIntyre, H.; Callaway, L.K.; Morrison, M.; Tyson, G.W.; Dekker Nitert, M. Pregnant women who develop preeclampsia have lower abundance of the butyrate-producer Coprococcus in their gut microbiota. Pregnancy Hypertens. 2021, 23, 211–219. [Google Scholar] [CrossRef]
- Adnan, S.; Nelson, J.W.; Ajami, N.J.; Venna, V.R.; Petrosino, J.F.; Bryan, R.M., Jr.; Durgan, D.J. Alterations in the gut microbiota can elicit hypertension in rats. Physiol. Genom. 2017, 49, 96–104. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Haj-Mirzaian, A.; Ramezanzadeh, K.; Tafazolimoghadam, A.; Kazemi, K.; Nikbakhsh, R.; Nikbakhsh, R.; Amini-Khoei, H.; Afshari, K.; Haddadi, N.S.; Shakiba, S.; et al. Protective effect of minocycline on LPS-induced mitochondrial dysfunction and decreased seizure threshold through nitric oxide pathway. Eur. J. Pharmacol. 2019, 858, 172446. [Google Scholar] [CrossRef]
- Reckelhoff, J.F. Gender differences in hypertension. Curr. Opin. Nephrol. Hypertens. 2018, 27, 176–181. [Google Scholar] [CrossRef] [PubMed]
- Hsu, C.N.; Hou, C.Y.; Chang-Chien, G.P.; Lin, S.; Tain, Y.L. Maternal garlic oil supplementation prevents high-fat diet-induced hypertension in adult rat offspring: Implications of H2S-generating pathway in the gut and kidneys. Mol. Nutr. Food Res. 2021, 65, e2001116. [Google Scholar] [CrossRef]
- Hsu, C.N.; Hung, C.H.; Hou, C.Y.; Chang, C.I.; Tain, Y.L. Perinatal Resveratrol Therapy to Dioxin-Exposed Dams Prevents the Programming of Hypertension in Adult Rat Offspring. Antioxidants 2021, 10, 1393. [Google Scholar] [CrossRef]

| Groups | ND | MI | AC | MI + AC |
|---|---|---|---|---|
| Mortality | 0% | 0% | 12.5% | 0% |
| Body weight (BW) (g) | 367 ± 12 a | 335 ± 6 a | 205 ± 7 b | 242 ± 9 b |
| Left kidney weight (g) | 1.71 ± 0.06 a | 1.64 ± 0.03 a | 0.94 ± 0.04 c | 1.36 ± 0.08 b |
| Left kidney weight/100 g BW | 0.47 ± 0.01 b | 0.49 ± 0.01 b | 0.46 ± 0.01 b | 0.56 ± 0.02 a |
| Systolic blood pressure (mmHg) | 133.1 ± 0.4 b | 141.3 ± 2.2 a | 131.1 ± 0.9 b | 131.9 ± 0.8 b |
| Diastolic blood pressure (mmHg) | 90.3 ± 2.2 a | 96.3 ± 3.1 a | 84.6 ± 1.2 b | 88.4 ± 1.1 b |
| Mean arterial pressure (mmHg) | 104.2 ± 0.9 b | 111.4 ± 3.3 a | 100.4 ± 0.8 b | 103.2 ± 0.8 b |
| Creatinine (μM) | 14.94 ± 1.36 b | 18.63 ± 0.53 a | 17.07 ± 1.12 a | 16.46 ± 0.7 b |
| Groups | ND | MI | AC | MI + AC |
|---|---|---|---|---|
| Acetic acid (μM) | 492.9 ± 8.11 b | 378.1 ± 12.39 c | 644.8 ± 27.23 a | 572.3 ± 20.93 a |
| Propionic acid (μM) | 8.44 ± 0.34 | 7.8 ± 0.37 | 8.63 ± 0.67 | 9.34 ± 0.6 |
| Isobutyric acid (μM) | 4.83 ± 0.15 | 3.94 ± 0.05 | 4.23 ± 0.05 | 3.99 ± 0.15 |
| Butyric acid (μM) | 5.6 ± 0.25 | 4.6 ± 0.56 | 4.09 ± 0.13 | 4.28 ± 0.22 |
| Isovaleric acid (μM) | 4.17 ± 0.17 | 3.4 ± 0.08 | 3.44 ± 0.05 | 3.33 ± 0.14 |
| Valeric acid (μM) | 4.82 ± 0.18 | 3.95 ± 0.12 | 4.39 ± 0.03 | 4.13 ± 0.06 |
| Groups | ND | MI | AC | MI + AC |
|---|---|---|---|---|
| l-Citrulline (μM) | 98.4 ± 8.8 a | 81.2 ± 3.5 b | 94 ± 6.7 a | 110.3 ± 5.7 a |
| l-Arginine (μM) | 255.4 ± 7.2 a | 231.7 ± 7.8 a | 215.6 ± 10.5 b | 256.6 ± 10.5 a |
| ADMA (μM) | 1.7 ± 0.2 b | 1.5 ± 0.1 b | 2.1 ± 0.3 a | 2.2 ± 0.2 a |
| SDMA (μM) | 1.2 ± 0.1 a | 1 ± 0.1 b | 1.5 ± 0.3 a | 1.3 ± 0.1 a |
| l-Arginine-to-ADMA ratio (μM/μM) | 153.3 ± 9.6 a | 156.6 ± 9.7 a | 120.9 ± 7 b | 126.6 ± 11 b |
| Antibody | Host | Source | Dilution |
|---|---|---|---|
| GPR41 | Rabbit | USBiological, Swampscott, MA, USA | 1:500 |
| GPR43 | Rabbit | Millipore, Burlington, MA, USA | 1:500 |
| GPR91 | Rabbit | Novus Biologicals, Centennial, CO, USA | 1:1000 |
| Olfr78 | Rabbit | Assay Biotech, San Francisco, CA, USA | 1:500 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hsu, C.-N.; Yu, H.-R.; Chan, J.Y.H.; Lee, W.-C.; Wu, K.L.H.; Hou, C.-Y.; Chang-Chien, G.-P.; Lin, S.; Tain, Y.-L. Maternal Acetate Supplementation Reverses Blood Pressure Increase in Male Offspring Induced by Exposure to Minocycline during Pregnancy and Lactation. Int. J. Mol. Sci. 2022, 23, 7924. https://doi.org/10.3390/ijms23147924
Hsu C-N, Yu H-R, Chan JYH, Lee W-C, Wu KLH, Hou C-Y, Chang-Chien G-P, Lin S, Tain Y-L. Maternal Acetate Supplementation Reverses Blood Pressure Increase in Male Offspring Induced by Exposure to Minocycline during Pregnancy and Lactation. International Journal of Molecular Sciences. 2022; 23(14):7924. https://doi.org/10.3390/ijms23147924
Chicago/Turabian StyleHsu, Chien-Ning, Hong-Ren Yu, Julie Y. H. Chan, Wei-Chia Lee, Kay L. H. Wu, Chih-Yao Hou, Guo-Ping Chang-Chien, Sufan Lin, and You-Lin Tain. 2022. "Maternal Acetate Supplementation Reverses Blood Pressure Increase in Male Offspring Induced by Exposure to Minocycline during Pregnancy and Lactation" International Journal of Molecular Sciences 23, no. 14: 7924. https://doi.org/10.3390/ijms23147924
APA StyleHsu, C.-N., Yu, H.-R., Chan, J. Y. H., Lee, W.-C., Wu, K. L. H., Hou, C.-Y., Chang-Chien, G.-P., Lin, S., & Tain, Y.-L. (2022). Maternal Acetate Supplementation Reverses Blood Pressure Increase in Male Offspring Induced by Exposure to Minocycline during Pregnancy and Lactation. International Journal of Molecular Sciences, 23(14), 7924. https://doi.org/10.3390/ijms23147924











