Specific Cerebrospinal Fluid SerpinA1 Isoform Pattern in Alzheimer’s Disease
Abstract
1. Introduction
2. Methods
2.1. Patients Selection
2.2. CSF Sampling and Analysis
2.3. CSF Serpina1 Analysis by CIEF Immunoassay
2.4. Statistical Analysis
3. Results
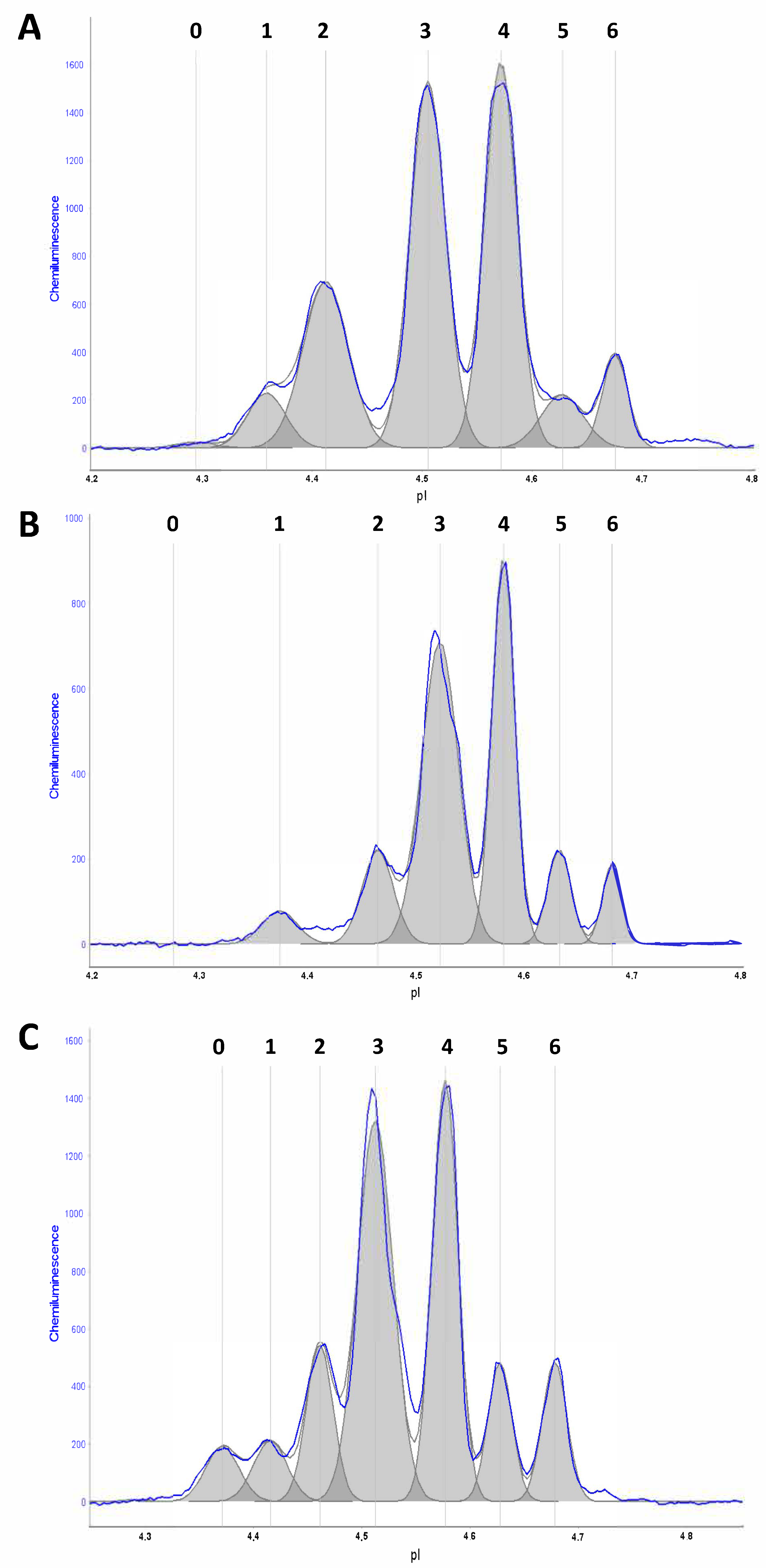
3.1. Distribution of CSF SerpinA1 Isoforms
3.2. CSF SerpinA1 Isoforms in Diagnostic Subgroups
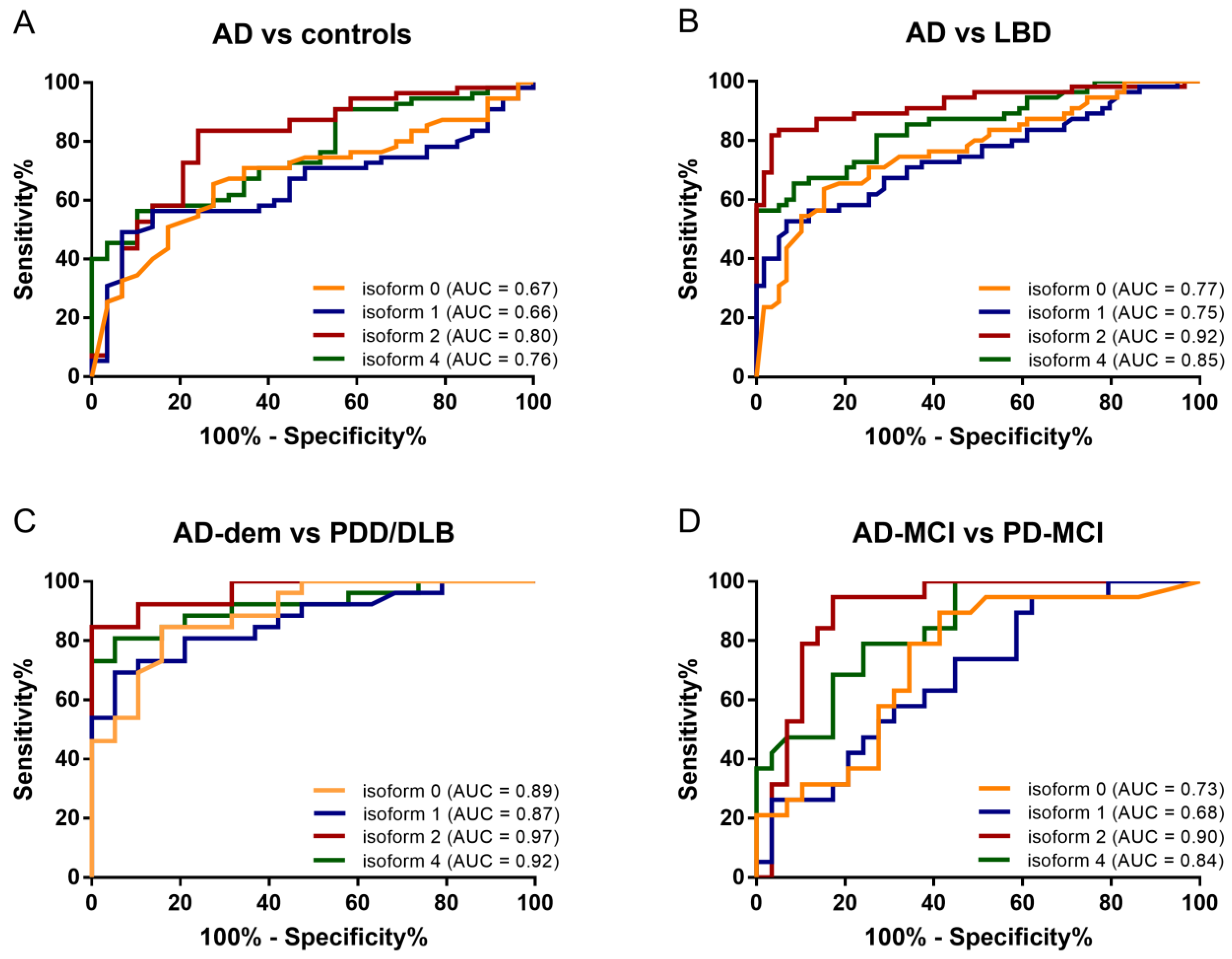
3.3. Receiver Operating Characteristic (ROC) Analysis
3.4. Correlations with AD Core Biomarkers
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- de Serres, F.; Blanco, I. Role of alpha-1 antitrypsin in human health and disease. J. Intern. Med. 2014, 276, 311–335. [Google Scholar] [CrossRef] [PubMed]
- Gold, M.; Dolga, A.M.; Koepke, J.; Mengel, D.; Culmsee, C.; Dodel, R.; Koczulla, A.R.; Bach, J.P. α1-antitrypsin modulates microglial-mediated neuroinflammation and protects microglial cells from amyloid-β-induced toxicity. J. Neuroinflamm. 2014, 11, 165. [Google Scholar] [CrossRef] [PubMed]
- Zhou, T.; Huang, Z.; Zhu, X.; Sun, X.; Liu, Y.; Cheng, B.; Li, M.; Liu, Y.; He, C.; Liu, X. Alpha-1 Antitrypsin Attenuates M1 Microglia-Mediated Neuroinflammation in Retinal Degeneration. Front. Immunol. 2018, 9, 1202. [Google Scholar] [CrossRef] [PubMed]
- Gollin, P.A.; Kalaria, R.N.; Eikelenboom, P.; Rozemuller, A.; Perry, G. Alpha 1-antitrypsin and alpha 1-antichymotrypsin are in the lesions of Alzheimer’s disease. Neuroreport 1992, 3, 201–203. [Google Scholar] [CrossRef] [PubMed]
- Ebbert, M.T.W.; Ross, C.A.; Pregent, L.J.; Lank, R.J.; Zhang, C.; Katzman, R.B.; Jansen-West, K.; Song, Y.; da Rocha, E.L.; Palmucci, C.; et al. Conserved DNA methylation combined with differential frontal cortex and cerebellar expression distinguishes C9orf72-associated and sporadic ALS, and implicates SERPINA1 in disease. Acta Neuropathol. 2017, 134, 715–728. [Google Scholar] [CrossRef]
- Devlin, G.L.; Chow, M.K.M.; Howlett, G.J.; Bottomley, S.P. Acid Denaturation of alpha1-antitrypsin: Characterization of a novel mechanism of serpin polymerization. J. Mol. Biol. 2002, 324, 859–870. [Google Scholar] [CrossRef]
- Jesse, S.; Lehnert, S.; Jahn, O.; Parnetti, L.; Soininen, H.; Herukka, S.K.; Steinacker, P.; Tawfik, S.; Tumani, H.; Von Arnim, C.A.; et al. Differential Sialylation of Serpin A1 in the Early Diagnosis of Parkinson’s Disease Dementia. PLoS ONE 2012, 7, e48783. [Google Scholar] [CrossRef]
- Nielsen, H.M.; Minthon, L.; Londos, E.; Blennow, K.; Miranda, E.; Perez, J.; Crowther, D.C.; Lomas, D.A.; Janciauskiene, S.M. Plasma and CSF serpins in Alzheimer disease and dementia with Lewy bodies. Neurology 2007, 69, 1569–1579. [Google Scholar] [CrossRef]
- Halbgebauer, S.; Nagl, M.; Klafki, H.; Haußmann, U.; Steinacker, P.; Oeckl, P.; Kassubek, J.; Pinkhardt, E.; Ludolph, A.C.; Soininen, H.; et al. Modified serpinA1 as risk marker for Parkinson’s disease dementia: Analysis of baseline data. Sci. Rep. 2016, 6, 26145. [Google Scholar] [CrossRef]
- Abu-Rumeileh, S.; Halbgebauer, S.; Steinacker, P.; Anderl-Straub, S.; Polischi, B.; Ludolph, A.C.; Capellari, S.; Parchi, P.; Otto, M. CSF SerpinA1 in Creutzfeldt-Jakob disease and frontotemporal lobar degeneration. Ann. Clin. Transl. Neurol. 2020, 7, 191–199. [Google Scholar] [CrossRef]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef]
- Gill, D.J.; Freshman, A.; Blender, J.A.; Ravina, B. The montreal cognitive assessment as a screening tool for cognitive impairment in Parkinson’s disease: Screening Tool for Cognitive Impairment. Mov Disord. 2008, 23, 1043–1046. [Google Scholar] [CrossRef] [PubMed]
- Morris, J.C. The Clinical Dementia Rating (CDR): Current version and scoring rules. Neurology 1993, 43, 2412–2414. [Google Scholar] [CrossRef] [PubMed]
- Jack, C.R.; Bennett, D.A.; Blennow, K.; Carrillo, M.C.; Dunn, B.; Haeberlein, S.B.; Holtzman, D.M.; Jagust, W.; Jessen, F.; Karlawish, J.; et al. NIA-AA Research Framework: Toward a biological definition of Alzheimer’s disease. Alzheimers Dement. 2018, 14, 535–562. [Google Scholar] [CrossRef] [PubMed]
- Albert, M.S.; DeKosky, S.T.; Dickson, D.; Dubois, B.; Feldman, H.H.; Fox, N.C.; Gamst, A.; Holtzman, D.M.; Jagust, W.J.; Petersen, R.C.; et al. The diagnosis of mild cognitive impairment due to Alzheimer’s disease: Recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011, 7, 270–279. [Google Scholar] [CrossRef]
- McKhann, G.M.; Knopman, D.S.; Chertkow, H.; Hyman, B.T.; Jack, C.R.; Kawas, C.H.; Klunk, W.E.; Koroshetz, W.J.; Manly, J.J.; Mayeux, R.; et al. The diagnosis of dementia due to Alzheimer’s disease: Recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011, 7, 263–269. [Google Scholar] [CrossRef]
- Postuma, R.B.; Berg, D.; Stern, M.; Poewe, W.; Olanow, C.W.; Oertel, W.; Obeso, J.; Marek, K.; Litvan, I.; Lang, A.E.; et al. MDS clinical diagnostic criteria for Parkinson’s disease: MDS-PD Clinical Diagnostic Criteria. Mov. Disord. 2015, 30, 1591–1601. [Google Scholar] [CrossRef]
- McKeith, I.G.; Boeve, B.F.; Dickson, D.W.; Halliday, G.; Taylor, J.P.; Weintraub, D.; Aarsland, D.; Galvin, J.; Attems, J.; Ballard, C.G.; et al. Diagnosis and management of dementia with Lewy bodies: Fourth consensus report of the DLB Consortium. Neurology 2017, 89, 88–100. [Google Scholar] [CrossRef]
- Litvan, I.; Goldman, J.G.; Tröster, A.I.; Weintraub, D.; Mollenhauer, B.; Adler, C.H.; Marder, K.; Williams-Gray, C.H.; Aarsland, D. Diagnostic Criteria for Mild Cognitive Impairment in Parkinson’s Disease: Movement Disorder Society Task Force Guidelines. Mov. Disord. 2012, 27, 349–356. [Google Scholar] [CrossRef]
- Emre, M.; Aarsland, D.; Brown, R.; Burn, D.J.; Duyckaerts, C.; Mizuno, Y.; Broe, G.A.; Cummings, J.; Dickson, D.W.; Gauthier, S.; et al. Clinical diagnostic criteria for dementia associated with Parkinson’s disease. Mov. Disord. 2007, 22, 1689–1707. [Google Scholar] [CrossRef]
- Petersen, R.C.; Knopman, D.S.; Boeve, B.F.; Geda, Y.E.; Ivnik, R.J.; Smith, G.E.; Jack, C.R. Mild Cognitive Impairment: Ten Years Later. Arch. Neurol. 2009, 66, 1447–1455. [Google Scholar] [CrossRef] [PubMed]
- Teunissen, C.E.; Petzold, A.; Bennett, J.L.; Berven, F.S.; Brundin, L.; Comabella, M.; Franciotta, D.; Frederiksen, J.L.; Fleming, J.O.; Furlan, R.; et al. A consensus protocol for the standardization of cerebrospinal fluid collection and biobanking. Neurology 2009, 73, 1914–1922. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Navarro, A.; González-Soria, I.; Caldiño-Bohn, R.; Bobadilla, N.A. An integrative view of serpins in health and disease: The contribution of SerpinA3. Am. J. Physiol. Cell Physiol. 2021, 320, C106–C118. [Google Scholar] [CrossRef] [PubMed]
- Gettins, P.G.W.; Olson, S.T. Inhibitory serpins. New insights into their folding, polymerization, regulation and clearance. Biochem. J. 2016, 473, 2273–2293. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Greene, C.M.; Marciniak, S.J.; Teckman, J.; Ferrarotti, I.; Brantly, M.L.; Lomas, D.A.; Stoller, J.K.; McElvaney, N.G. α1-Antitrypsin deficiency. Nat. Rev. Dis. Primers 2016, 2, 16051. [Google Scholar] [CrossRef]
- Yen, H.Y.; Liu, Y.C.; Chen, N.Y.; Tsai, C.F.; Wang, Y.T.; Chen, Y.J.; Hsu, T.-L.; Yang, P.-C.; Wong, C.-H. Effect of sialylation on EGFR phosphorylation and resistance to tyrosine kinase inhibition. Proc. Natl. Acad. Sci. USA 2015, 112, 6955–6960. [Google Scholar] [CrossRef]
- Yamasaki, M.; Li, W.; Johnson, D.J.D.; Huntington, J.A. Crystal structure of a stable dimer reveals the molecular basis of serpin polymerization. Nature 2008, 455, 1255–1258. [Google Scholar] [CrossRef]
- Bellomo, G.; Paolini Paoletti, F.; Chipi, E.; Petricciuolo, M.; Simoni, S.; Tambasco, N.; Parnetti, L. A/T/(N) Profile in Cerebrospinal Fluid of Parkinson’s Disease with/without Cognitive Impairment and Dementia with Lewy Bodies. Diagnostics 2020, 10, 1015. [Google Scholar] [CrossRef]
- Kantarci, K.; Lowe, V.J.; Chen, Q.; Przybelski, S.A.; Lesnick, T.G.; Schwarz, C.G.; Senjem, M.L.; Gunter, J.L.; Jack, C.R.; Graff-Radford, J.; et al. β-Amyloid PET and neuropathology in dementia with Lewy bodies. Neurology 2020, 94, e282–e291. [Google Scholar] [CrossRef]
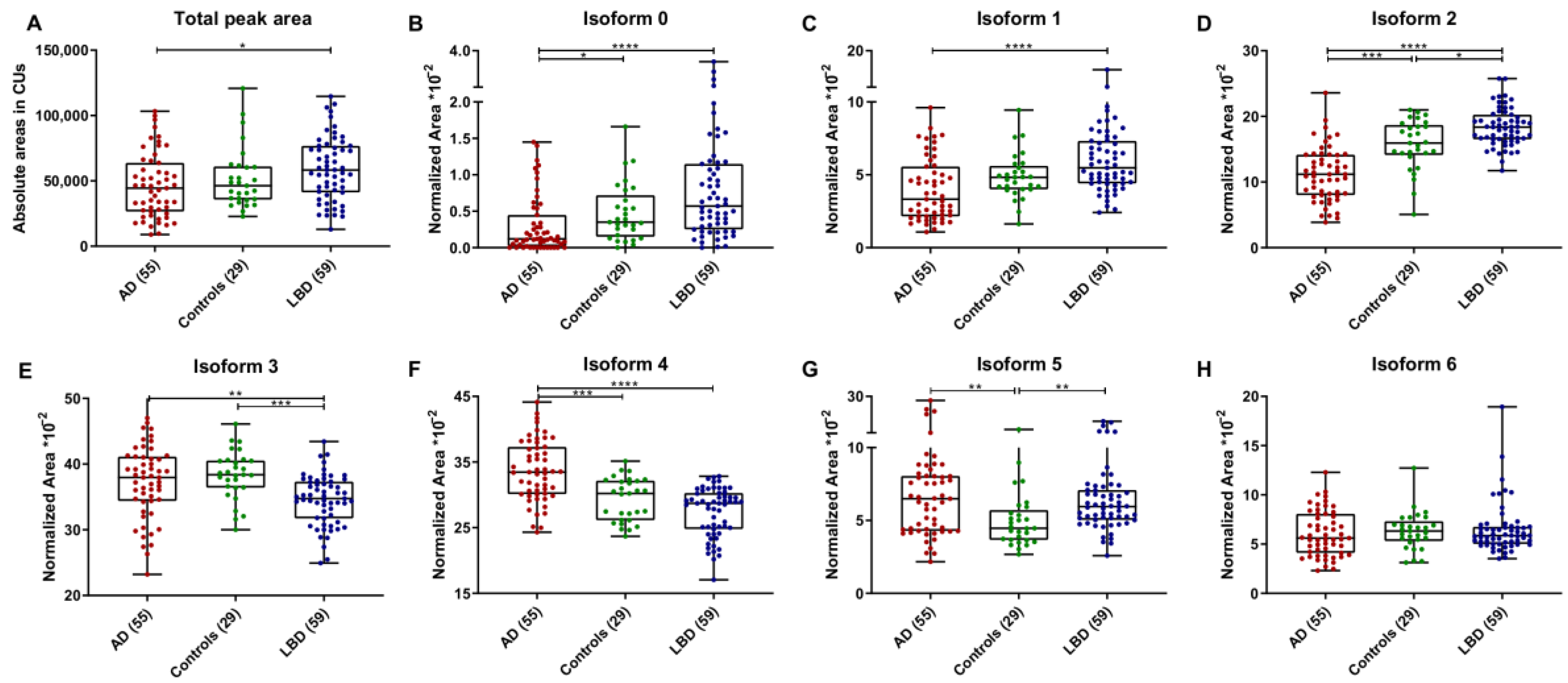
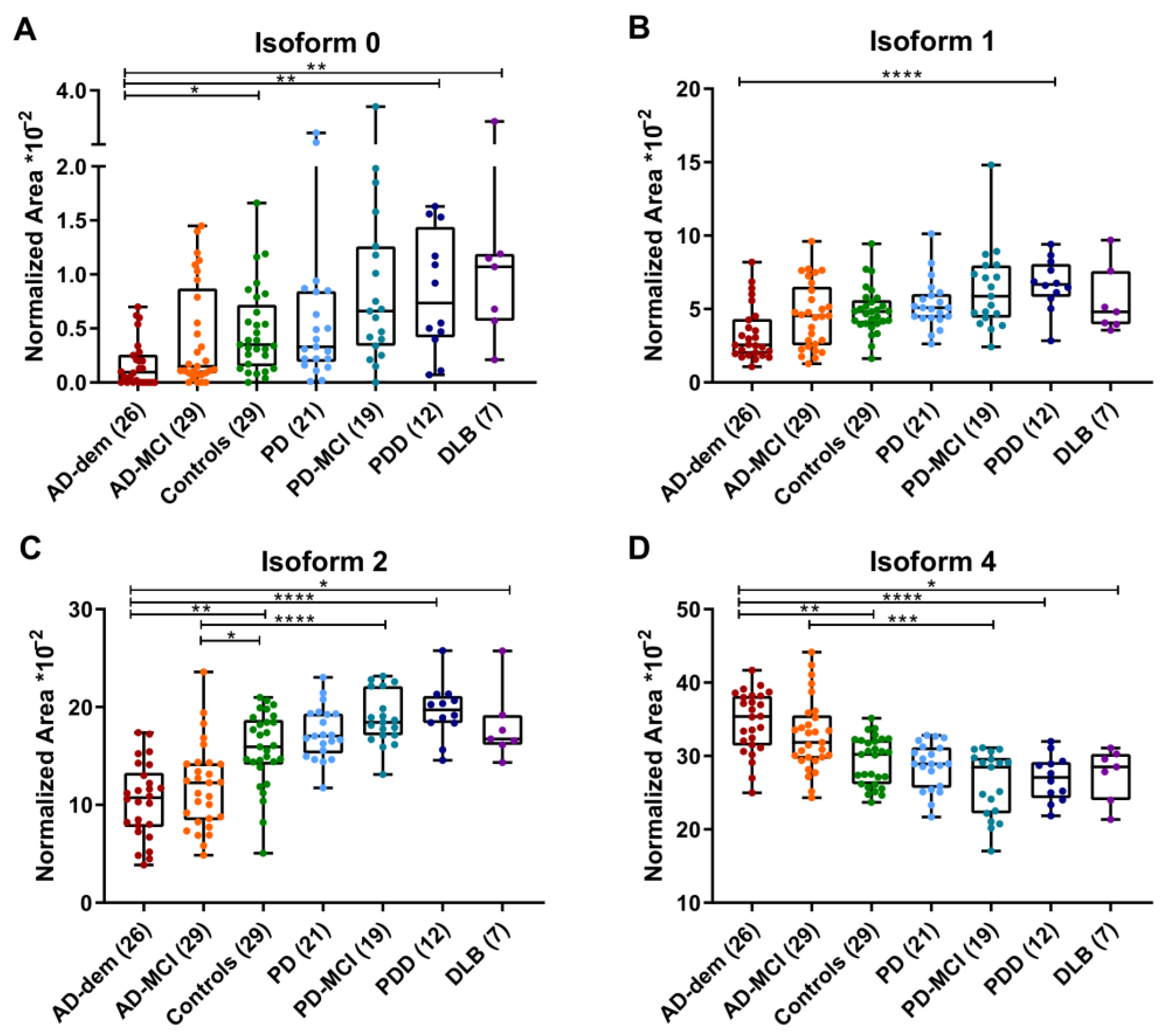
| AD | Controls | LBD | |||||||
| AD-dem | AD-MCI | Total | Total | PD | PD-MCI | PDD | DLB | Total | |
| N | 26 | 29 | 55 | 29 | 21 | 19 | 12 | 7 | 59 |
| Age * | 70.7 ± 7.8 | 73.7 ± 4.7 | 72.2 ± 6.5 | 59.7 ± 13.2 | 61.2 ± 9.5 | 67.9 ± 7.4 | 71.3 ± 9.5 | 71.7 ± 9.5 | 66.7 ± 9.7 |
| Females (%) ** | 17 (65.4%) | 16 (55.2%) | 33 (60.0%) | 12 (41.4%) | 7 (33.3%) | 4 (21.1%) | 1 (8.3%) | 2 (28.6%) | 14 (23.7%) |
| Aβ42/40 ratio | 0.052 ± 0.010 | 0.049 ± 0.012 | 0.051 ± 0.011 | 0.114 ± 0.024 *** | 0.105 ± 0.022 | 0.097 ± 0.030 | 0.079 ± 0.035 | 0.059 ± 0.019 | 0.095 ± 0.030 |
| p-tau (pg/mL) | 107.2 ± 54.2 | 99.5 ± 37.1 | 103.3 ± 46.2 | 44.1 ± 9.3 *** | 37.3 ± 14.3 | 40.6 ± 22.1 | 43.8 ± 18.8 | 55.13 ± 33.0 | 40.5 ± 19.9 |
| t-tau (pg/mL) | 814.7 ± 324.3 | 756.8 ± 322.0 | 785.7 ± 321.7 | 261.9 ± 74.9 *** | 248.4 ± 120.5 | 284.4 ± 172.0 | 274.2 ± 126.7 | 373.7 ± 188.0 | 273.8 ± 149.7 |
| Total peak area (CUs) | 42,791 ± 24,716 | 49,488 ± 24,654 | 46,322 ± 24,685 | 51,763 ± 23,350 | 50,894 ± 22,916 | 64,071 ± 23,332 | 64,759 ± 21,305 | 61,511 ± 33,844 | 59,217 ± 24,380 |
| isoform 0 (%) | 0.2 ± 0.2 | 0.4 ± 0.4 | 0.3 ± 0.3 | 0.5 ± 0.4 | 0.6 ± 0.6 | 0.9 ± 0.8 | 0.8 ± 0.8 | 1.1 ± 0.8 | 0.8 ± 0.7 |
| isoform 1 (%) | 3.3 ± 1.9 | 4.6 ± 2.2 | 4.0 ± 2.1 | 4.9 ± 1.6 | 5.3 ± 1.7 | 6.3 ± 2.8 | 6.7 ± 2.3 | 5.5 ± 2.3 | 6.0 ± 2.2 |
| isoform 2 (%) | 10.5 ± 3.8 | 11.9 ± 4.3 | 11.2 ± 4.1 | 15.7 ± 3.9 | 17.4 ± 2.7 | 18.8 ± 2.7 | 19.6 ± 3.7 | 18.1 ± 3.7 | 18.4 ± 2.9 |
| isoform 3 (%) | 37.2 ± 6.4 | 37.6 ± 5.2 | 37.4 ± 5.7 | 38.3 ± 3.7 | 35.8 ± 3.2 | 33.5 ± 3.4 | 32.6 ± 4.6 | 36.9 ± 4.6 | 34.5 ± 3.8 |
| isoform 4 (%) | 34.6 ± 4.2 | 32.8 ± 4.9 | 33.7 ± 4.7 | 29.3 ± 3.3 | 28.6 ± 3.1 | 26.1 ± 4.4 | 27.0 ± 3.6 | 27.5 ± 3.6 | 27.4 ± 3.7 |
| isoform 5 (%) | 8.3 ± 6.3 | 6.5 ± 3.3 | 7.3 ± 5.0 | 5.0 ± 2.0 | 6.4 ± 2.6 | 7.8 ± 3.2 | 5.2 ± 1.5 | 5.6 ± 1.5 | 6.5 ± 2.6 |
| isoform 6 (%) | 5.9 ± 2.2 | 6.2 ± 2.4 | 6.1 ± 2.3 | 6.3 ± 0.8 | 5.8 ± 1.0 | 6.6 ± 2.3 | 8.2 ± 0.9 | 5.3 ± 0.9 | 6.5 ± 2.6 |
| Mean Variation% | AUC (95% CI) | Best Cutoffs | Sensitivity% (95% CI) | Specificity% (95% CI) | LR+ | |
| AD vs. Controls | ||||||
| isoform 0 | −36.6 * | 0.67 (0.57–0.80) | 0.2 | 65.5 (51.4–77.8) | 72.4 (52.8–87.3) | 2.4 |
| isoform 1 | − | 0.66 (0.54–0.77) | 3.8 | 56.4 (42.3–69.7) | 86.2 (68.3–96.1) | 4.1 |
| isoform 2 | −28.6 *** | 0.80 (0.70–0.91) | 14.4 | 83.6 (71.2–92.2) | 75.9 (56.5–89.7) | 3.5 |
| isoform 3 | − | 0.54 (0.42–0.66) | 36.4 | 40.0 (27.0–54.1) | 79.3 (60.3–92.0) | 1.9 |
| isoform 4 | +14.9 *** | 0.76 (0.66–0.86) | 33.0 | 56.4 (42.3–69.7) | 89.7 (72.7–97.8) | 5.5 |
| isoform 5 | +46.2 ** | 0.69 (0.57–0.81) | 6.2 | 54.6 (40.6–68.0) | 86.2 (68.3–96.1) | 4.0 |
| isoform 6 | − | 0.55 (0.42–0.67) | 5.5 | 49.1 (35.4–62.9) | 72.4 (52.8–87.3) | 1.8 |
| AD vs. LBD | ||||||
| isoform 0 | −62.1 **** | 0.77 (0.65–0.86) | 0.2 | 63.6 (49.6–76.2) | 84.8 (73.0–92.8) | 4.2 |
| isoform 1 | −33.1 **** | 0.75 (0.66–0.84) | 3.5 | 52.7 (38.8–66.4) | 93.2 (83.5–98.1) | 7.8 |
| isoform 2 | −39.0 **** | 0.92 (0.87–0.98) | 14.3 | 81.8 (69.1–90.9) | 96.6 (88.3–99.6) | 24.1 |
| isoform 3 | +8.4 ** | 0.68 (0.58–0.78) | 38.6 | 45.5 (32.0–59.5) | 91.5 (81.3–97.2) | 5.4 |
| isoform 4 | +23.1 **** | 0.85 (0.78–0.92) | 31.4 | 65.5 (51.4–77.8) | 91.5 (81.3–97.2) | 7.7 |
| isoform 5 | +12.8 ** | 0.52 (0.41–0.63) | 7.5 | 41.8 (28.7–55.9) | 84.8 (73.0–92.8) | 2.7 |
| isoform 6 | − | 0.55 (0.44–0.66) | 4.2 | 27.3 (16.2–41.0) | 94.9 (85.9–98.9) | 5.4 |
| AD-dem vs. PDD/DLB | ||||||
| isoform 0 | −81.4 **** | 0.89 (0.80–0.99) | 0.4 | 84.6 (65.1–95.6) | 84.2 (60.4–96.6) | 5.4 |
| isoform 1 | −47.0 **** | 0.87 (0.76–0.97) | 3.6 | 69.2 (48.2–85.7) | 94.7 (74.0–99.9) | 13.2 |
| isoform 2 | −45.0 **** | 0.97 (0.93–1.00) | 14.3 | 84.6 (65.1–95.6) | 99.9 (82.4–100.0) | 84.6 |
| isoform 3 | − | 0.68 (0.52–0.84) | 38.5 | 50.0 (29.9–70.1) | 89.4 (66.9–98.7) | 4.8 |
| isoform 4 | +27.5 **** | 0.92 (0.84–0.99) | 31.1 | 80.8 (60.7–93.5) | 94.7 (74.0–99.9) | 15.4 |
| isoform 5 | − | 0.67 (0.52–0.83) | 7.5 | 46.2 (26.6–66.6) | 99.9 (82.4–100) | 84.6 |
| isoform 6 | − | 0.58 (0.41–0.75) | 10.1 | 96.2 (80.4–99.9) | 26.3 (9.1–51.2) | 1.3 |
| AD-MCI vs. PD-MCI | ||||||
| isoform 0 | − | 0.73 (0.59–0.88) | 0.2 | 89.5 (66.9–98.7) | 58.6 (38.9–76.5) | 2.2 |
| isoform 1 | − | 0.68 (0.53–0.83) | 3.5 | 94.7 (74.0–99.9) | 37.9 (20.7–57.7) | 1.5 |
| isoform 2 | −36.9 **** | 0.90 (0.81–0.99) | 14.4 | 94.7 (74.0–99.9) | 79.3 (60.3–92.0) | 4.6 |
| isoform 3 | +12.5 * | 0.75 (0.62–0.89) | 37.9 | 100.0 (82.4–100.0) | 48.3 (29.5–67.5) | 1.9 |
| isoform 4 | +25.5 *** | 0.84 (0.74–0.95) | 31.3 | 100.0 (82.4–100.0) | 55.2 (35.7–73.6) | 2.2 |
| isoform 5 | − | 0.65 (0.49–0.80) | 4.6 | 100.0 (82.4–100.0) | 37.9 (20.7–57.7) | 1.6 |
| isoform 6 | − | 0.54 (0.38–0.71) | 4.1 | 100.0 (82.4–100.0) | 24.1 (10.3–43.5) | 1.3 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barba, L.; Halbgebauer, S.; Paolini Paoletti, F.; Bellomo, G.; Abu-Rumeileh, S.; Steinacker, P.; Massa, F.; Parnetti, L.; Otto, M. Specific Cerebrospinal Fluid SerpinA1 Isoform Pattern in Alzheimer’s Disease. Int. J. Mol. Sci. 2022, 23, 6922. https://doi.org/10.3390/ijms23136922
Barba L, Halbgebauer S, Paolini Paoletti F, Bellomo G, Abu-Rumeileh S, Steinacker P, Massa F, Parnetti L, Otto M. Specific Cerebrospinal Fluid SerpinA1 Isoform Pattern in Alzheimer’s Disease. International Journal of Molecular Sciences. 2022; 23(13):6922. https://doi.org/10.3390/ijms23136922
Chicago/Turabian StyleBarba, Lorenzo, Steffen Halbgebauer, Federico Paolini Paoletti, Giovanni Bellomo, Samir Abu-Rumeileh, Petra Steinacker, Federico Massa, Lucilla Parnetti, and Markus Otto. 2022. "Specific Cerebrospinal Fluid SerpinA1 Isoform Pattern in Alzheimer’s Disease" International Journal of Molecular Sciences 23, no. 13: 6922. https://doi.org/10.3390/ijms23136922
APA StyleBarba, L., Halbgebauer, S., Paolini Paoletti, F., Bellomo, G., Abu-Rumeileh, S., Steinacker, P., Massa, F., Parnetti, L., & Otto, M. (2022). Specific Cerebrospinal Fluid SerpinA1 Isoform Pattern in Alzheimer’s Disease. International Journal of Molecular Sciences, 23(13), 6922. https://doi.org/10.3390/ijms23136922








