Importance of Matrix Cues on Intervertebral Disc Development, Degeneration, and Regeneration
Abstract
1. Introduction
2. IVD Physiology, Structure, and Function
2.1. The IVD
2.1.1. The NP
2.1.2. The AF
2.1.3. The CEPs
3. Changes to the ECM during IVD Development and Degeneration
3.1. IVD Development and Maturation
3.2. IVD Degeneration
4. Incorporation of Matrix Cues into Experimental Models Using Biomaterials
4.1. The Need for Regenerative Therapies
4.2. Cell-Based Regenerative Approaches
4.3. Development of Biomimetic Systems for the Delivery of Matrix Cues
| Matrix Cues(s) | Study Outcome | References |
|---|---|---|
| Type I collagen | Injectable collagen gel upregulates aggrecan and collagen type I production for in vitro AF repair. | [192] |
| Alginate-collagen porous scaffolds supported MSC proliferation and collagen type I production. | [193] | |
| Injectable high-density collagen gel partially repaired AF defect and remodelled by host fibroblasts into a fibrous cap. | [191] | |
| Injectable high-density collagen gel seeded with MSCs resulted in increased disc height, reduced Pfirrmann grade, and increased NP area. | [195] | |
| Injectable TGFβ1-supplemented collagen hydrogel resulted in production of collagen type I, CD146, MKX, and SM22α. | [194] | |
| Type I collagen and HA | Injectable collagen-HA hydrogel enabled growth factor delivery and supported growth and chondrogenic differentiation potential of MSCs and nasal chondrocytes. | [229] |
| Type II collagen | Injectable, crosslinked collagen hydrogel enriched with HA preserved NP cell morphology. | [230] |
| Collagen microspheres aided pre-differentiation of ADSCs in degenerate IVD-like conditions. | [189] | |
| Collagen scaffold activated the Shh pathway in ADSCs, promoting NP-like differentiation. | [187] | |
| Type II collagen and HA | Microgels influenced ADSCs to express high levels of collagen type II, aggrecan, and SOX9, and low levels of collagen type I. | [231] |
| Type I or II with HA hydrogels identified the role of SOCS in combating pro-inflammatory cytokine effects in degenerate NP. | [232] | |
| Type II collagen and CS | CS incorporation resulted in increased production of NP-like ECM, including sulphated GAGs. | [233] |
| Type II collagen and HA and CS | Cell-seeded scaffolds supported NP cell viability and resulted in maintenance of disc height. | [190] |
| Laminin | Injectable laminin-111 functionalized poly(ethylene glycol) (PEG) hydrogel resulted in significantly higher cell retention within NP. | [234] |
| Laminin mimic | Laminin-mimetic peptides resulted in cell signalling downstream of integrin and syndecan binding, promoted cell migration, and modulated NP behaviour similarly to full-length laminins. | [185] |
| Integrin- and syndecan-binding peptide-conjugated alginate hydrogel elicited NP-specific phenotype and re-expression of more juvenile-like phenotype in NP cells. | [186] | |
| Integrin- and syndecan-binding peptide-conjugated alginate hydrogel used to identify novel mechanosensitive targets in NP cells, including several G Protein-Coupled Receptor genes. | [132] | |
| HA | HA-pNIPAM hydrogel induced greater disc-like differentiation of MSCs compared to pre-differentiation, including collagen type II, SOX9, KR19, and CD24. | [235] |
| Eight different HA-PEG hydrogel formulations used to identify key parameters influencing IVD cell–material interactions. | [236] | |
| Treatment with HA-based hydrogel resulted in downregulation of NGF and BDNF, plus suppression of IL1R1 in an in vitro inflammation model of NP. | [237] | |
| HA and PRP hydrogel blended with batroxobin gelling agent resulted in heightened sulphated GAG production in MSCs and chondrocyte-like differentiation. | [218] | |
| Assessed the efficacy of HA hydrogel pain alleviation, demonstrating altered glycosylation plus modulation of inflammatory and regulatory signalling pathways. | [238] | |
| HA oligosaccharides shown to stimulate MMPs, ADAMTs, and anabolic matrix repair genes. | [239] | |
| Gelatine-HA hydrogel promoted NP-like differentiation of ADSCs. | [188] | |
| HA and GAG mimic | Used HA-PEG hydrogels to demonstrate the chondro-inductive potential of pentosan polysulphate, a sulphated semi-synthetic polysaccharide. | [240] |
| GAG mimic | Cytocompatible biomimetic aggrecan analogue comprising a polymeric core conjugated to CS ‘bristles’ was shown to have comparable osmotic pressure to natural aggrecan and increase intradiscal pressure upon injection. | [212] |
| Pentosan polysulphate embedded within a gelatine-fibrin scaffold with MSCs resulted in restored disc height, morphology, and NP proteoglycan content. | [241] | |
| Cytocompatible, large biomimetic aggrecan analogue comprising a polymeric core conjugated to CS was chemically, structurally, and mechanically characterised. Injection into ex vivo bovine NP showed localisation in the pericellular matrix. | [211] | |
| Co-polymerised naAMPS and KSPA GAG mimic provided intrinsic swelling pressure and restoration of stiffness within ex vivo NP. | [214] | |
| Elastin | Bioprinted silk fibronin hydrogel combined with elastin shown to support ADSC culture and enable creation of scaffolds with structural and mechanical properties similar to AF. | [242] |
| Matrilin-3 | Gelatine microparticles loaded with TGFβ3 and matrilin-3 promoted chondrogenic differentiation of ADSC spheroids while preventing hypertrophy and terminal differentiation of cells. | [243] |
| Decellularised AF ECM | Decellularised ECM and chitosan hydrogels increased production of collagen types I and II, and aggrecan, in AF-derived cells. | [196] |
4.4. Spatially Controlled Patterning of Matrix Cues Using Biofabrication Strategies
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Carvalho, M.S.; Alves, L.; Bogalho, I.; Cabral, J.M.S.; da Silva, C.L. Impact of Donor Age on the Osteogenic Supportive Capacity of Mesenchymal Stromal Cell-Derived Extracellular Matrix. Front. Cell Dev. Biol. 2021, 9, 747521. [Google Scholar] [CrossRef] [PubMed]
- Birch, H.L. Extracellular Matrix and Ageing. In Biochemistry and Cell Biology of Ageing: Part 1 Biomedical Science, 1st ed.; Harris, J.R., Korolchuk, V.I., Eds.; Springer: Singapore, 2018; pp. 169–190. [Google Scholar]
- Di Loreto, R.; Murphy, C.T. The cell biology of aging. Mol. Biol. Cell 2015, 26, 4524–4531. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.; Li, W.; Lu, Z.; Chen, R.; Ling, J.; Ran, Q.; Jilka, R.L.; Chen, X.D. Rescuing replication and osteogenesis of aged mesenchymal stem cells by exposure to a young extracellular matrix. FASEB J. 2011, 25, 1474–1485. [Google Scholar] [CrossRef] [PubMed]
- Kurtz, A.; Oh, S.J. Age related changes of the extracellular matrix and stem cell maintenance. Prev. Med. 2012, 54, S50–S56. [Google Scholar] [CrossRef]
- Hwang, P.Y.; Jing, L.; Michael, K.W.; Richardson, W.J.; Chen, J.; Setton, L.A. N-Cadherin-Mediated Signaling Regulates Cell Phenotype for Nucleus Pulposus Cells of the Intervertebral Disc. Cell. Mol. Bioeng. 2014, 8, 51–62. [Google Scholar] [CrossRef] [PubMed]
- Gilchrist, C.L.; Darling, E.M.; Chen, J.; Setton, L.A. Extracellular matrix ligand and stiffness modulate immature nucleus pulposus cell-cell interactions. PLoS ONE 2011, 6, 27170. [Google Scholar] [CrossRef]
- Newell, N.; Little, J.P.; Christou, A.; Adams, M.A.; Adam, C.J.; Masouros, S.D. Biomechanics of the human intervertebral disc: A review of testing techniques and results. J. Mech. Behav. Biomed. Mater. 2017, 69, 420–434. [Google Scholar] [CrossRef]
- Tam, V.; Chen, P.; Yee, A.; Solis, N.; Klein, T.; Kudelko, M.; Sharma, R.; Chan, W.C.W.; Overall, C.M.; Haglund, L.; et al. Dipper, a spatiotemporal proteomics atlas of human intervertebral discs for exploring ageing and degeneration dynamics. eLife 2020, 9, e64940. [Google Scholar] [CrossRef]
- Broberg, K.B. On the mechanical behaviour of intervertebral discs. Spine 1983, 8, 151–165. [Google Scholar] [CrossRef]
- Berg-Johansen, B.; Han, M.; Fields, A.J.; Liebenberg, E.C.; Lim, B.J.; Larson, P.E.Z.; Gunduz-Demir, C.; Kazakia, G.J.; Krug, R.; Lotz, J.C. Cartilage Endplate Thickness Variation Measured by Ultrashort Echo-Time MRI Is Associated with Adjacent Disc Degeneration. Spine 2018, 43, E592. [Google Scholar] [CrossRef]
- Grunhagen, T.; Shirazi-Adl, A.; Fairbank, J.C.T.; Urban, J.P.G. Intervertebral Disk Nutrition: A Review of Factors Influencing Concentrations of Nutrients and Metabolites. Orthop. Clin. N. Am. 2011, 42, 465–477. [Google Scholar] [CrossRef] [PubMed]
- Urban, J.P.G.; Smith, S.; Fairbank, J.C.T. Nutrition of the intervertebral disc. Spine 2004, 29, 2700–2709. [Google Scholar] [CrossRef] [PubMed]
- Grant, M.P.; Epure, L.M.; Bokhari, R.; Roughley, P.; Antoniou, J.; Mwale, F. Human cartilaginous endplate degeneration is induced by calcium and the extracellular calcium-sensing receptor in the intervertebral disc. Eur. Cells Mater. 2016, 32, 137–151. [Google Scholar] [CrossRef]
- Wills, C.R.; Foata, B.; González Ballester, M.; Karppinen, J.; Noailly, J. Theoretical explorations generate new hypotheses about the role of the cartilage endplate in early intervertebral disk degeneration. Front. Physiol. 2018, 9, 1210. [Google Scholar] [CrossRef] [PubMed]
- Iatridis, J.C.; Weidenbaum, M.; Setton, L.A.; Mow, C.V. Is the nucleus pulposus a solid or a fluid? Mechanical behaviors of the nucleus pulposus of the human intervertebral disc. Spine 1996, 15, 1174–1184. [Google Scholar] [CrossRef] [PubMed]
- Sakai, D.; Grad, S. Advancing the cellular and molecular therapy for intervertebral disc disease. Adv. Drug Deliv. Rev. 2015, 84, 159–171. [Google Scholar] [CrossRef]
- Mwale, F.; Roughley, P.; Antoniou, J.; Alini, M.; Hollander, A.; Kirsch, T.; Stokes, I. Distinction between the extracellular matrix of the nucleus pulposus and hyaline cartilage: A requisite for tissue engineering of intervertebral disc. Eur. Cells Mater. 2004, 8, 58–64. [Google Scholar] [CrossRef]
- Umehara, S.; Tadano, S.; Abumi, K.; Katagiri, K.; Kaneda, K.; Ukai, T. Effects of degeneration on the elastic modulus distribution in the lumbar intervertebral disc. Spine 1996, 21, 811–819. [Google Scholar] [CrossRef]
- Bron, J.L.; Koenderink, G.H.; Everts, V.; Smit, T.H. Rheological characterization of the nucleus pulposus and dense collagen scaffolds intended for functional replacement. J. Orthop. Res. 2009, 27, 620–626. [Google Scholar] [CrossRef]
- Iatridis, J.C.; Setton, L.A.; Weidenbaum, M.; Mow, V.C. The viscoelastic behavior of the non-degenerate human lumbar nucleus pulposus in shear. J. Biomech. 1997, 30, 1005–1013. [Google Scholar] [CrossRef]
- Race, A.; Broom, N.D.; Robertson, P. Effect of loading rate and hydration on the mechanical properties of the disc. Spine 2000, 25, 662–669. [Google Scholar] [CrossRef] [PubMed]
- Cloyd, J.M.; Malhotra, N.R.; Weng, L.; Chen, W.; Mauck, R.L.; Elliott, D.M. Material properties in unconfined compression of human nucleus pulposus, injectable hyaluronic acid-based hydrogels and tissue engineering scaffolds. Eur. Spine J. 2007, 16, 1892–1898. [Google Scholar] [CrossRef] [PubMed]
- Iatridis, J.C.; Kumar, S.; Foster, R.J.; Weidenbaum, M.; Mow, V.C. Shear mechanical properties of human lumbar annulus fibrosus. J. Orthop. Res. 1999, 17, 732–737. [Google Scholar] [CrossRef] [PubMed]
- Adams, M.A.; Roughley, P.J. What is intervertebral disc degeneration, and what causes it? Spine 2006, 31, 2151–2161. [Google Scholar] [CrossRef]
- Cortes, D.H.; Elliott, D.M. The intervertebral disc: Overview of disc mechanics. In The Intervertebral Disc: Molecular and Structural Studies of the Disc in Health and Disease, 1st ed.; Shapiro, I., Risbud, M., Eds.; Springer: Vienna, Austria, 2014; Volume 1, pp. 17–31. [Google Scholar]
- Maroudas, A.; Stockwell, R.A.; Nachemson, A.; Urban, J. Factors involved in the nutrition of the human lumbar intervertebral disc: Cellularity and diffusion of glucose in vitro. J. Anat. 1975, 120 Pt 1, 113–130. [Google Scholar]
- Roughley, P.J. Biology of intervertebral disc aging and degeneration: Involvement of the extracellular matrix. Spine 2004, 29, 2691–2699. [Google Scholar] [CrossRef]
- Risbud, M.V.; Schoepflin, Z.R.; Mwale, F.; Kandel, R.A.; Grad, S.; Iatridis, J.C.; Sakai, D.; Hoyland, J.A. Defining the phenotype of young healthy nucleus pulposus cells: Recommendations of the spine research interest group at the 2014 annual ORS meeting. J. Orthop. Res. 2015, 33, 283–293. [Google Scholar] [CrossRef]
- Bach, F.C.; Willems, N.; Penning, L.C.; Ito, K.; Meij, B.P.; Tryfonidou, M.A. Potential regenerative treatment strategies for intervertebral disc degeneration in dogs. BMC Vet. Res. 2014, 10, 3. [Google Scholar] [CrossRef]
- Neidlinger-Wilke, C.; Galbusera, F.; Pratsinis, H.; Mavrogonatou, E.; Mietsch, A.; Kletsas, D.; Wilke, H.J. Mechanical loading of the intervertebral disc: From the macroscopic to the cellular level. Eur. Spine J. 2014, 23 (Suppl. 3), S333–S343. [Google Scholar] [CrossRef]
- Marchand, F.; Ahmed, A.M. Investigation of the laminate structure of lumbar disc anulus fibrosus. Spine 1990, 15, 402–410. [Google Scholar] [CrossRef]
- Disney, C.M.; Madi, K.; Bodey, A.J.; Lee, P.D.; Hoyland, J.A.; Sherratt, M.J. Visualising the 3D microstructure of stained and native intervertebral discs using X-ray microtomography. Sci. Rep. 2017, 7, 16279. [Google Scholar] [CrossRef] [PubMed]
- Cassidy, J.J.; Hiltner, A.; Baer, E. Hierarchical structure of the intervertebral disc. Connect. Tissue Res. 1989, 23, 75–88. [Google Scholar] [CrossRef] [PubMed]
- Raza, A.; Michalek, A.J. Radial trend in murine annulus fibrosus fiber orientation is best explained by vertebral growth. Eur. Spine J. 2021, 30, 3450–3456. [Google Scholar] [CrossRef] [PubMed]
- Melrose, J.; Smith, S.M.; Appleyard, R.C.; Little, C.B. Aggrecan, versican and type VI collagen are components of annular translamellar crossbridges in the intervertebral disc. Eur. Spine J. 2008, 17, 314–324. [Google Scholar] [CrossRef]
- Smith, L.J.; Elliott, D.M. Formation of lamellar cross bridges in the annulus fibrosus of the intervertebral disc is a consequence of vascular regression. Matrix Biol. 2011, 30, 267–274. [Google Scholar] [CrossRef]
- Tavakoli, J.; Elliott, D.M.; Costi, J.J. Structure and mechanical function of the inter-lamellar matrix of the annulus fibrosus in the disc. J. Orthop. Res. 2016, 34, 1307–1315. [Google Scholar] [CrossRef]
- Disney, C.M.; Lee, P.D.; Hoyland, J.A.; Sherratt, M.J.; Bay, B.K. A review of techniques for visualising soft tissue microstructure deformation and quantifying strain Ex Vivo. J. Microsc. 2018, 272, 165–179. [Google Scholar] [CrossRef]
- Disney, C.M.; Eckersley, A.; McConnell, J.C.; Geng, H.; Bodey, A.J.; Hoyland, J.A.; Lee, P.D.; Sherratt, M.J.; Bay, B.K. Synchrotron tomography of intervertebral disc deformation quantified by digital volume correlation reveals microstructural influence on strain patterns. Acta Biomater. 2019, 92, 290–304. [Google Scholar] [CrossRef]
- Disney, C.M.; Mo, J.; Eckersley, A.; Bodey, A.J.; Hoyland, J.A.; Sherratt, M.J.; Pitsillides, A.A.; Lee, P.D.; Bay, B.K. Regional variations in discrete collagen fibre mechanics within intact intervertebral disc resolved using synchrotron computed tomography and digital volume correlation. Acta Biomater. 2022, 138, 361–374. [Google Scholar] [CrossRef]
- Pattappa, G.; Li, Z.; Peroglio, M.; Wismer, N.; Alini, M.; Grad, S. Diversity of intervertebral disc cells: Phenotype and function. J. Anat. 2012, 221, 480–496. [Google Scholar] [CrossRef]
- Singh, K.; Masuda, K.; Thonar, E.J.; An, H.S.; Cs-Szabo, G. Age-related changes in the extracellular matrix of nucleus pulposus and anulus fibrosus of human intervertebral disc. Spine 2009, 34, 10–16. [Google Scholar] [CrossRef] [PubMed]
- Oegema, T.R. Biochemistry of the Intervertebral Disc. Clin. Sports Med. 1993, 12, 419–438. [Google Scholar] [CrossRef]
- Urban, J.; Maroudas, A. The Chemistry of the Intervertebral Disc in Relation to its Physiological Function and Requirements. Clin. Rheum. Dis. 1980, 6, 51–76. [Google Scholar] [CrossRef]
- Eyre, D.R.; Matsui, Y.; Wu, J.J. Collagen polymorphisms of the intervertebral disc. Biochem. Soc. Trans. 2002, 30, 844–848. [Google Scholar] [CrossRef] [PubMed]
- Sivan, S.; Hayes, A.; Wachtel, E.; Merkher, Y.; Owen, S.; Caterson, B.; Maroudas, A.; Roberts, S. Biochemical composition and turnover of the extracellular matrix of the normal and degenerate intervertebral disc. Eur. Spine J. 2014, 23 (Suppl. 3), S344–S353. [Google Scholar] [CrossRef]
- Nakai, T.; Sakai, D.; Nakamura, Y.; Nukaga, T.; Grad, S.; Li, Z.; Alini, M.; Chan, D.; Masuda, K.; Ando, K.; et al. CD146 defines commitment of cultured annulus fibrosus cells to express a contractile phenotype. J. Orthop. Res. 2016, 34, 1361–1372. [Google Scholar] [CrossRef]
- Clouet, J.; Grimandi, G.; Pot-Vaucel, M.; Masson, M.; Fellah, H.B.; Guigand, L.; Cherel, Y.; Bord, E.; Rannou, F.; Weiss, P.; et al. Identification of phenotypic discriminating markers for intervertebral disc cells and articular chondrocytes. Rheumatology 2009, 48, 1447–1450. [Google Scholar] [CrossRef]
- van den Akker, G.G.H.; Eijssen, L.M.T.; Richardson, S.M.; Rhijn, L.W.v.; Hoyland, J.A.; Welting, T.J.M.; Voncken, J.W. A Membranome-Centered Approach Defines Novel Biomarkers for Cellular Subtypes in the Intervertebral Disc. Cartilage 2018, 11, 203–220. [Google Scholar] [CrossRef]
- Sharabi, M.; Wade, K.; Haj-Ali, R. The Mechanical Role of Collagen Fibers in the Intervertebral Disc. In Biomechanics of the Spine, 1st ed.; Galbusera, F., Wilke, H., Eds.; Academic Press: Cambridge, MN, USA, 2018; Volume 1, pp. 105–123. [Google Scholar]
- Roberts, S.; Menage, J.; Urban, J.P. Biochemical and structural properties of the cartilage end-plate and its relation to the intervertebral disc. Spine 1989, 14, 166–174. [Google Scholar] [CrossRef]
- Wu, Y.; Cisewski, S.E.; Sachs, B.L.; Pellegrini, V.D.; Kern, M.J.; Slate, E.H.; Yao, H. The Region-dependent Biomechanical and Biochemical Properties of Bovine Cartilaginous Endplate. J. Biomech. 2015, 48, 3185. [Google Scholar] [CrossRef]
- Giers, M.B.; Munter, B.T.; Eyster, K.J.; Ide, G.D.; Newcomb, A.G.U.S.; Lehrman, J.N.; Belykh, E.; Byvaltsev, V.A.; Kelly, B.P.; Preul, M.C.; et al. Biomechanical and Endplate Effects on Nutrient Transport in the Intervertebral Disc. World Neurosurg. 2017, 99, 395–402. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.C.; Urban, J.P.G.; Luk, K.D.K. Intervertebral disc regeneration: Do nutrients lead the way? Nat. Rev. Rheumatol. 2014, 10, 561–566. [Google Scholar] [CrossRef] [PubMed]
- Jackson, A.R.; Huang, C.Y.; Gua, W.Y. Effect of endplate calcification and mechanical deformation on the distribution of glucose in intervertebral disc: A 3D finite element study. Comput. Methods Biomech. Biomed. Eng. 2011, 14, 195–204. [Google Scholar] [CrossRef]
- St-Pierre, J.P.; Gan, L.; Wang, J.; Pilliar, R.M.; Grynpas, M.D.; Kandel, R.A. The incorporation of a zone of calcified cartilage improves the interfacial shear strength between in vitro-formed cartilage and the underlying substrate. Acta Biomater. 2012, 8, 1603–1615. [Google Scholar] [CrossRef]
- DeLucca, J.F.; Cortes, D.H.; Jacobs, N.T.; Vresilovic, E.J.; Duncan, R.L.; Elliott, D.M. Human cartilage endplate permeability varies with degeneration and intervertebral disc site. J. Biomech. 2016, 49, 550–557. [Google Scholar] [CrossRef] [PubMed]
- Naresh-Babu, J.; Neelima, G.; Reshma Begum, S.; Siva-Leela, V. Diffusion characteristics of human annulus fibrosus—a study documenting the dependence of annulus fibrosus on end plate for diffusion. Spine J. 2016, 16, 1007–1014. [Google Scholar] [CrossRef]
- Rajasekaran, S.; Venkatadass, K.; Naresh Babu, J.; Ganesh, K.; Shetty, A.P. Pharmacological enhancement of disc diffusion and differentiation of healthy, ageing and degenerated discs: Results from in-vivo serial post-contrast MRI studies in 365 human lumbar discs. Eur. Spine J. 2008, 17, 626–643. [Google Scholar] [CrossRef] [PubMed]
- Lakstins, K.; Arnold, L.; Gunsch, G.; Flanigan, D.; Khan, S.; Gadde, N.; Jones, B.; Agarwal, G.; Purmessur, D. Characterization of the human intervertebral disc cartilage endplate at the molecular, cell, and tissue levels. J. Orthop. Res. 2021, 39, 1898–1907. [Google Scholar] [CrossRef]
- Lakstins, K.; Arnold, L.; Gunsch, G.; Khan, S.; Moore, S.; Purmessur, D. Characterization of bovine and canine animal model cartilage endplates and comparison to human cartilage endplate structure, matrix composition, and cell phenotype. JOR Spine 2020, 3, e1116. [Google Scholar] [CrossRef]
- Smith, S.M.; Whitelock, J.M.; Iozzo, R.V.; Little, C.B.; Melrose, J. Topographical variation in the distributions of versican, aggrecan and perlecan in the foetal human spine reflects their diverse functional roles in spinal development. Histochem. Cell Biol. 2009, 132, 491–503. [Google Scholar] [CrossRef]
- Corallo, D.; Trapani, V.; Bonaldo, P. The notochord: Structure and functions. Cell. Mol. Life Sci. 2015, 72, 2989–3008. [Google Scholar] [CrossRef]
- Trapani, V.; Bonaldo, P.; Corallo, D. Role of the ECM in notochord formation, function and disease. J. Cell Sci. 2017, 130, 3203–3211. [Google Scholar] [CrossRef] [PubMed]
- Hwang, P.Y.; Chen, J.; Jing, L.; Hoffman, B.D.; Setton, L.A. The Role of Extracellular Matrix Elasticity and Composition In Regulating the Nucleus Pulposus Cell Phenotype in the Intervertebral Disc: A Narrative Review. J. Biomech. Eng. 2014, 136, 021010. [Google Scholar] [CrossRef] [PubMed]
- Matta, A.; Erwin, W.M. Current Status of the Instructional Cues Provided by Notochordal Cells in Novel Disc Repair Strategies. Int. J. Mol. Sci. 2021, 23, 427. [Google Scholar] [CrossRef] [PubMed]
- Ward, L.; Rodrigues-Pinto, R.; Humphreys, M.; Hoyland, J.; Richardson, S.M. Defining the phenotype of the human fetal notochordal cell: Implications for intervertebral disc regeneration. Osteoarthr. Cartil. 2018, 26, S39. [Google Scholar] [CrossRef]
- Richardson, S.M.; Ludwinski, F.E.; Gnanalingham, K.K.; Atkinson, R.A.; Freemont, A.J.; Hoyland, J.A. Notochordal and nucleus pulposus marker expression is maintained by sub-populations of adult human nucleus pulposus cells through aging and degeneration. Sci. Rep. 2017, 7, 1501. [Google Scholar] [CrossRef]
- van den Akker, G.; Welting, T.; Surtel, D.; Cremers, A.; Voncken, W.; van Rhijn, L. Cell lines for the human intervertebral disc: Nucleus pulposus and annulus fibrosis. Osteoarthr. Cartil. 2012, 20, S267–S268. [Google Scholar] [CrossRef][Green Version]
- van den Akker, G.G.H.; Surtel, D.A.M.; Cremers, A.; Rodrigues-Pinto, R.; Richardson, S.M.; Hoyland, J.A.; van Rhijn, L.W.; Welting, T.J.M.; Voncken, J.W. Novel immortal human cell lines reveal subpopulations in the nucleus pulposus. Arthritis Res. Ther. 2014, 16, R135. [Google Scholar] [CrossRef]
- Van Den Akker, G.G.H.; Surtel, D.A.M.; Cremers, A.; Richardson, S.M.; Hoyland, J.A.; Van Rhijn, L.W.; Voncken, J.W.; Welting, T.J.M. Novel immortal cell lines support cellular heterogeneity in the human annulus fibrosus. PLoS ONE 2016, 11, e0144497. [Google Scholar] [CrossRef]
- van den Akker, G.G.H.; Koenders, M.I.; van de Loo, F.A.J.; van Lent, P.L.E.M.; Blaney Davidson, E.; van der Kraan, P.M. Transcriptional profiling distinguishes inner and outer annulus fibrosus from nucleus pulposus in the bovine intervertebral disc. Eur. Spine J. 2017, 26, 2053–2062. [Google Scholar] [CrossRef]
- Aguiar, D.J.; Johnson, S.L.; Oegema, T.R. Notochordal cells interact with nucleus pulposus cells: Regulation of proteoglycan synthesis. Exp. Cell Res. 1999, 246, 129–137. [Google Scholar] [CrossRef] [PubMed]
- Erwin, W.M.; Islam, D.; Inman, R.D.; Fehlings, M.G.; Tsui, F.W.L. Notochordal cells protect nucleus pulposus cells from degradation and apoptosis: Implications for the mechanisms of intervertebral disc degeneration. Arthritis Res. Ther. 2011, 13, R215. [Google Scholar] [CrossRef] [PubMed]
- De Vries, S.A.H.; Potier, E.; Van Doeselaar, M.; Meij, B.P.; Tryfonidou, M.A.; Ito, K. Conditioned Medium Derived from Notochordal Cell-Rich Nucleus Pulposus Tissue Stimulates Matrix Production by Canine Nucleus Pulposus Cells and Bone Marrow-Derived Stromal Cells. Tissue Eng. Part A 2015, 21, 1077. [Google Scholar] [CrossRef] [PubMed]
- Alkhatib, B.; Ban, G.I.; Williams, S.; Serra, R. IVD Development: Nucleus pulposus development and sclerotome specification. Curr. Mol. Biol. Rep. 2018, 4, 132–141. [Google Scholar] [CrossRef]
- Gilchrist, C.L.; Francisco, A.T.; Plopper, G.E.; Chen, J.; Setton, L.A. Nucleus pulposus cell-matrix interactions with laminins. Eur. Cells Mater. 2011, 21, 523–532. [Google Scholar] [CrossRef]
- Bridgen, D.T.; Gilchrist, C.L.; Richardson, W.J.; Isaacs, R.E.; Brown, C.R.; Yang, K.L.; Chen, J.; Setton, L.A. Integrin-mediated interactions with extracellular matrix proteins for nucleus pulposus cells of the human intervertebral disc. J. Orthop. Res. 2013, 41, 793–810. [Google Scholar] [CrossRef]
- Gilchrist, C.L.; Chen, J.; Richardson, W.J.; Loeser, R.F.; Setton, L.A. Functional integrin subunits regulating cell-matrix interactions in the intervertebral disc. J. Orthop. Res. 2007, 25, 829–840. [Google Scholar] [CrossRef]
- Barcellona, M.N.; Speer, J.E.; Fearing, B.V.; Jing, L.; Pathak, A.; Gupta, M.C.; Buchowski, J.M.; Kelly, M.; Setton, L.A. Control of adhesive ligand density for modulation of nucleus pulposus cell phenotype. Biomaterials 2020, 250, 120057. [Google Scholar] [CrossRef]
- Choi, K.S.; Harfe, B.D. Hedgehog signaling is required for formation of the notochord sheath and patterning of nuclei pulposi within the intervertebral discs. Proc. Natl. Acad. Sci. USA 2011, 108, 9484–9489. [Google Scholar] [CrossRef]
- Rodrigues-Pinto, R.; Richardson, S.M.; Hoyland, J.A. An understanding of intervertebral disc development, maturation and cell phenotype provides clues to direct cell-based tissue regeneration therapies for disc degeneration. Eur. Spine J. 2014, 23, 1803–1814. [Google Scholar] [CrossRef]
- Hayes, A.J.; Lord, M.S.; Smith, S.M.; Smith, M.M.; Whitelock, J.M.; Weiss, A.S.; Melrose, J. Colocalization in vivo and association in vitro of perlecan and elastin. Histochem. Cell Biol. 2011, 136, 437–454. [Google Scholar] [CrossRef]
- Ghazanfari, S.; Werner, A.; Ghazanfari, S.; Weaver, J.C.; Smit, T.H. Morphogenesis of aligned collagen fibers in the annulus fibrosus: Mammals versus avians. Biochem. Biophys. Res. Commun. 2018, 503, 1168–1173. [Google Scholar] [CrossRef] [PubMed]
- Hayes, A.J.; Benjamin, M.; Ralphs, J.R. Role of Actin Stress Fibres in the Development of the Intervertebral Disc: Cytoskeletal Control of Extracellular Matrix Assembly. Dev. Dyn. 1999, 215, 179–189. [Google Scholar] [CrossRef]
- Rodrigues, S.A.; Thambyah, A.; Broom, N.D. How maturity influences annulus-endplate integration in the ovine intervertebral disc: A micro- and ultra-structural study. J. Anat. 2017, 230, 152–164. [Google Scholar] [CrossRef] [PubMed]
- Vergroesen, P.P.A.; Kingma, I.; Emanuel, K.S.; Hoogendoorn, R.J.W.; Welting, T.J.; van Royen, B.J.; van Dieën, J.H.; Smit, T.H. Mechanics and biology in intervertebral disc degeneration: A vicious circle. Osteoarthr. Cartil. 2015, 23, 1057–1070. [Google Scholar] [CrossRef]
- Sakai, D.; Nakamura, Y.; Nakai, T.; Mishima, T.; Kato, S.; Grad, S.; Alini, M.; Risbud, M.V.; Chan, D.; Cheah, K.S.E.; et al. Exhaustion of nucleus pulposus progenitor cells with ageing and degeneration of the intervertebral disc. Nat. Commun. 2012, 3, 1264. [Google Scholar] [CrossRef]
- Risbud, M.V.; Shapiro, I.M. Role of cytokines in intervertebral disc degeneration: Pain and disc content. Nat. Rev. Rheumatol. 2014, 10, 44–56. [Google Scholar] [CrossRef]
- Le Maitre, C.L.; Freemont, A.J.; Hoyland, J.A. The role of interleukin-1 in the pathogenesis of human intervertebral disc degeneration. Arthritis Res. Ther. 2005, 33, 255–262. [Google Scholar]
- Vo, N.V.; Hartman, R.A.; Yurube, T.; Jacobs, L.J.; Sowa, G.A.; Kang, J.D. Expression and regulation of metalloproteinases and their inhibitors in intervertebral disc aging and degeneration. Spine J. 2013, 13, 331–341. [Google Scholar] [CrossRef]
- Shiomi, T.; Lemaître, V.; D’Armiento, J.; Okada, Y. Matrix metalloproteinases, a disintegrin and metalloproteinases, and a disintegrin and metalloproteinases with thrombospondin motifs in non-neoplastic diseases: Review Article. Pathol. Int. 2010, 60, 477–496. [Google Scholar] [CrossRef]
- Jabłońska-Trypuć, A.; Matejczyk, M.; Rosochacki, S. Matrix metalloproteinases (MMPs), the main extracellular matrix (ECM) enzymes in collagen degradation, as a target for anticancer drugs. J. Enzym. Inhib. Med. Chem. 2016, 31, 177–183. [Google Scholar] [CrossRef]
- Fortelny, N.; Overall, C.M.; Pavlidis, P.; Freue, G.V.C. Can we predict protein from mRNA levels? Nature 2017, 547, E19–E20. [Google Scholar] [CrossRef] [PubMed]
- Allegri, M.; Montella, S.; Salici, F.; Valente, A.; Marchesini, M.; Compagnone, C.; Baciarello, M.; Manferdini, M.E.; Fanelli, G. Mechanisms of low back pain: A guide for diagnosis and therapy [version 2; peer review: 3 approved. F1000Research 2016, 5, F1000 Faculty Rev-1530. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Yang, M.; Liu, L.; Zhang, Y.; Zhu, Q.; Huang, C.; Wang, H.; Zhang, Y.; Li, H.; Li, C.; et al. Molecular basis of degenerative spinal disorders from a proteomic perspective (Review). Mol. Med. Rep. 2020, 21, 9–19. [Google Scholar] [CrossRef] [PubMed]
- Brown, S.; Melrose, J.; Caterson, B.; Roughley, P.; Eisenstein, S.M.; Roberts, S. A comparative evaluation of the small leucine-rich proteoglycans of pathological human intervertebral discs. Eur. Spine J. 2012, 21 (Suppl. 2), S154–S159. [Google Scholar] [CrossRef]
- Craddock, R.J.; Hodson, N.W.; Ozols, M.; Shearer, T.; Hoyland, J.A.; Sherratt, M.J. Extracellular matrix fragmentation in young, healthy cartilaginous tissues. Eur. Cells Mater. 2018, 35, 34–53. [Google Scholar] [CrossRef]
- Patel, K.P.; Sandy, J.D.; Akeda, K.; Miyamoto, K.; Chujo, T.; An, H.S.; Masuda, K. Aggrecanases and aggrecanase-generated fragments in the human intervertebral disc at early and advanced stages of disc degeneration. Spine 2007, 32, 2596–2603. [Google Scholar] [CrossRef]
- Sivan, S.S.; Wachtel, E.; Roughley, P. Structure, function, aging and turnover of aggrecan in the intervertebral disc. Biochim. Biophys. Acta 2014, 1840, 3181. [Google Scholar] [CrossRef]
- O’Connell, G.D.; Guerin, H.L.; Elliott, D.M. Theoretical and Uniaxial Experimental Evaluation of Human Annulus Fibrosus Degeneration. J. Biomech. Eng. 2010, 131, 111007. [Google Scholar] [CrossRef]
- Daly, C.; Ghosh, P.; Jenkin, G.; Oehme, D.; Goldschlager, T. A Review of Animal Models of Intervertebral Disc Degeneration: Pathophysiology, Regeneration, and Translation to the Clinic. BioMed Res. Int. 2016, 2016, 5952165. [Google Scholar] [CrossRef]
- Hwang, P.Y.; Jing, L.; Chen, J.; Lim, F.L.; Tang, R.; Choi, H.; Cheung, K.M.; Risbud, M.V.; Gersbach, C.A.; Guilak, F.; et al. N-cadherin is key to expression of the nucleus pulposus cell phenotype under selective substrate culture conditions. Sci. Rep. 2016, 6, 28038. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues-Pinto, R.; Ward, L.; Humphreys, M.; Zeef, L.A.H.; Berry, A.; Hanley, K.P.; Hanley, N.; Richardson, S.M.; Hoyland, J.A. Human notochordal cell transcriptome unveils potential regulators of cell function in the developing intervertebral disc. Sci. Rep. 2018, 8, 12866. [Google Scholar] [CrossRef] [PubMed]
- Risbud, M.V.; Shapiro, I.M. Notochordal Cells in the Adult Intervertebral Disc: New Perspective on an Old Question. Crit. Rev. Eukaryot. Gene Expr. 2012, 21, 29–41. [Google Scholar] [CrossRef] [PubMed]
- Li, D.; Zeng, Q.; Jiang, Z.; Ding, L.; Lu, W.; Bian, M.; Wu, J. Induction of notochordal differentiation of bone marrow mesenchymal-derived stem cells via the stimulation of notochordal cell-rich nucleus pulposus tissue. Mol. Med. Rep. 2021, 23, 1. [Google Scholar] [CrossRef]
- Li, X.C.; Wang, M.S.; Liu, W.; Zhong, C.F.; Deng, G.B.; Luo, S.J.; Huang, C.M. Co-culturing nucleus pulposus mesenchymal stem cells with notochordal cell-rich nucleus pulposus explants attenuates tumor necrosis factor-α-induced senescence. Stem Cell Res. Ther. 2018, 9, 171. [Google Scholar] [CrossRef]
- Diaz-Hernandez, M.E.; Khan, N.M.; Trochez, C.M.; Yoon, T.; Maye, P.; Presciutti, S.M.; Gibson, G.; Drissi, H. Derivation of notochordal cells from human embryonic stem cells reveals unique regulatory networks by single cell-transcriptomics. J. Cell. Physiol. 2020, 235, 5241–5255. [Google Scholar] [CrossRef]
- Rätsep, T.; Minajeva, A.; Asser, T. Relationship between neovascularization and degenerative changes in herniated lumbar intervertebral discs. Eur. Spine J. 2013, 22, 2474. [Google Scholar] [CrossRef]
- Patil, P.; Niedernhofer, L.J.; Robbins, P.D.; Lee, J.; Sowa, G.; Vo, N. Cellular senescence in intervertebral disc aging and degeneration. Curr. Mol. Biol. Rep. 2018, 4, 180. [Google Scholar] [CrossRef]
- Khan, A.N.; Jacobsen, H.E.; Khan, J.; Filippi, C.G.; Levine, M.; Lehman, R.A.; Riew, K.D.; Lenke, L.G.; Chahine, N.O. Inflammatory biomarkers of low back pain and disc degeneration: A review. Ann. N. Y. Acad. Sci. 2017, 1410, 68–84. [Google Scholar] [CrossRef]
- Pfirrmann, C.W.A.; Metzdorf, A.; Zanetti, M.; Hodler, J.; Boos, N. Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine 2001, 26, 1873–1878. [Google Scholar] [CrossRef]
- Cortes, D.H.; Jacobs, N.T.; DeLucca, J.F.; Elliott, D.M. Elastic, permeability and swelling properties of human intervertebral disc tissues: A benchmark for tissue engineering. J. Biomech. 2014, 47, 2088–2094. [Google Scholar] [CrossRef] [PubMed]
- Roberts, S.; Evans, E.H.; Kletsas, D.; Jaffray, D.C.; Eisenstein, S.M. Senescence in Human Intervertebral Discs. Eur. Spine J. 2006, 15 (Suppl. 3), S312–S316. [Google Scholar] [CrossRef] [PubMed]
- Horner, H.A.; Urban, J.P.G. 2001 Volvo award winner in basic science studies: Effect of nutrient supply on the viability of cells from the nucleus pulposus of the intervertebral disc. Spine 2001, 26, 2543–2549. [Google Scholar] [CrossRef] [PubMed]
- Li, F.C.; Zhang, N.; Chen, W.S.; Chen, Q.X. Endplate degeneration may be the origination of the vacuum phenomenon in intervertebral discs. Med. Hypotheses 2010, 75, 169–171. [Google Scholar] [CrossRef]
- Lu, K.; Li, H.Y.; Yang, K.; Wu, J.L.; Cai, X.W.; Zhou, Y.; Li, C.Q. Exosomes as potential alternatives to stem cell therapy for intervertebral disc degeneration: In-vitro study on exosomes in interaction of nucleus pulposus cells and bone marrow mesenchymal stem cells. Stem Cell Res. Ther. 2017, 8, 108. [Google Scholar] [CrossRef]
- Luo, L.; Jian, X.; Sun, H.; Qin, J.; Wang, Y.; Zhang, J.; Shen, Z.; Yang, D.; Li, C.; Zhao, P.; et al. Cartilage endplate stem cells inhibit intervertebral disc degeneration by releasing exosomes to nucleus pulposus cells to activate Akt/autophagy. Stem Cells 2021, 39, 467–481. [Google Scholar] [CrossRef]
- Johnson, W.E.B.; Caterson, B.; Eisenstein, S.M.; Hynds, D.L.; Snow, D.M.; Roberts, S. Human intervertebral disc aggrecan inhibits nerve growth in vitro. Arthritis Rheum. 2002, 46, 2658–2664. [Google Scholar] [CrossRef]
- Kudelko, M.; Chen, P.; Tam, V.; Zhang, Y.; Kong, O.Y.; Sharma, R.; Au, T.Y.K.; To, M.K.T.; Cheah, K.S.E.; Chan, W.C.W.; et al. PRIMUS: Comprehensive proteomics of mouse intervertebral discs that inform novel biology and relevance to human disease modelling. Matrix Biol. Plus 2021, 12, 100082. [Google Scholar] [CrossRef]
- Wang, H.; Wang, D.; Luo, B.; Wang, D.; Jia, H.; Peng, P.; Shang, Q.; Mao, J.; Gao, C.; Peng, Y.; et al. Decoding the annulus fibrosus cell atlas by scRNA-seq to develop an inducible composite hydrogel: A novel strategy for disc reconstruction. Bioact. Mater. 2022, 14, 350–363. [Google Scholar] [CrossRef]
- Li, K.; Kapper, D.; Mondal, S.; Lufkin, T.; Kraus, P. Quantitative Single-Cell Transcript Assessment of Biomarkers Supports Cellular Heterogeneity in the Bovine IVD. Vet. Sci. 2019, 6, 42. [Google Scholar] [CrossRef]
- Veras, M.A.; McCann, M.R.; Tenn, N.A.; Séguin, C.A. Transcriptional profiling of the murine intervertebral disc and age-associated changes in the nucleus pulposus. Connect. Tissue Res. 2020, 61, 63–81. [Google Scholar] [CrossRef] [PubMed]
- Caldeira, J.; Santa, C.; Osório, H.; Molinos, M.; Manadas, B.; Goncalves, R.; Barbosa, M. Matrisome Profiling during Intervertebral Disc Development and Ageing. Sci. Rep. 2017, 7, 11629. [Google Scholar] [CrossRef] [PubMed]
- Smolders, L.A.; Meij, B.P.; Onis, D.; Riemers, F.M.; Bergknut, N.; Wubbolts, R.; Grinwis, G.C.M.; Houweling, M.; Groot Koerkamp, M.J.A.; van Leenen, D.; et al. Gene expression profiling of early intervertebral disc degeneration reveals a down-regulation of canonical Wnt signaling and caveolin-1 expression: Implications for development of regenerative strategies. Arthritis Res. Ther. 2013, 15, R23. [Google Scholar] [CrossRef] [PubMed]
- Minogue, B.M.; Richardson, S.M.; Zeef, L.A.H.; Freemont, A.J.; Hoyland, J.A. Transcriptional profiling of bovine intervertebral disc cells: Implications for identification of normal and degenerate human intervertebral disc cell phenotypes. Arthritis Res. Ther. 2010, 12, R22. [Google Scholar] [CrossRef]
- Eckersley, A.; Ozols, M.; Chen, P.; Tam, V.; Hoyland, J.A.; Trafford, A.; Chan, D.; Sherratt, M.J. Peptide Location Fingerprinting Reveals Tissue Region-Specific Differences in Protein Structures in an Ageing Human Organ. Int. J. Mol. Sci. 2021, 22, 10408. [Google Scholar] [CrossRef]
- Minogue, B.M.; Richardson, S.M.; Zeef, L.A.H.; Freemont, A.J.; Hoyland, J.A. Characterization of the human nucleus pulposus cell phenotype and evaluation of novel marker gene expression to define adult stem cell differentiation. Arthritis Rheum. 2010, 62, 3695–3705. [Google Scholar] [CrossRef]
- Fernandes, L.M.; Khan, N.M.; Trochez, C.M.; Duan, M.; Diaz-Hernandez, M.E.; Presciutti, S.M.; Gibson, G.; Drissi, H. Single-cell RNA-seq identifies unique transcriptional landscapes of human nucleus pulposus and annulus fibrosus cells. Sci. Rep. 2020, 10, 15263. [Google Scholar] [CrossRef]
- Gan, Y.; He, J.; Zhu, J.; Xu, Z.; Wang, Z.; Yan, J.; Hu, O.; Bai, Z.; Chen, L.; Xie, Y.; et al. Spatially defined single-cell transcriptional profiling characterizes diverse chondrocyte subtypes and nucleus pulposus progenitors in human intervertebral discs. Bone Res. 2021, 9, 37. [Google Scholar] [CrossRef]
- Barcellona, M.N.; Speer, J.E.; Jing, L.; Gupta, M.C.; Buchowski, J.M.; Kelly, M.P.; Setton, L.A.; Lopata, S. Engineered Peptide-Functionalized Hydrogels Modulate the RNA Transcriptome of Human Nucleus Pulposus Cells In Vitro. bioRxiv 2021. [Google Scholar] [CrossRef]
- Riester, S.M.; Lin, Y.; Wang, W.; Cong, L.; Mohamed Ali, A.M.; Peck, S.H.; Smith, L.J.; Currier, B.L.; Clark, M.; Huddleston, P.; et al. RNA sequencing identifies gene regulatory networks controlling extracellular matrix synthesis in intervertebral disk tissues. J. Orthop. Res. Off. Publ. Orthop. Res. Soc. 2018, 36, 1356. [Google Scholar] [CrossRef]
- Rajasekaran, S.; Soundararajan, D.C.R.; Tangavel, C.; Sri Vijay Anand, K.S.; Nayagam, S.M.; Matchado, M.S.; Muthurajan, R.; Shetty, A.P.; Kanna, R.M.; Dharmalingam, K. Proteomic Signature of Nucleus Pulposus in Fetal Intervertebral Disc. Asian Spine J. 2020, 14, 409–420. [Google Scholar] [CrossRef] [PubMed]
- Qiu, C.; Wu, X.; Bian, J.; Ma, X.; Zhang, G.; Guo, Z.; Wang, Y.; Ci, Y.; Wang, Q.; Xiang, H.; et al. Differential proteomic analysis of fetal and geriatric lumbar nucleus pulposus: Immunoinflammation and age-related intervertebral disc degeneration. BMC Musculoskelet. Disord. 2020, 21, 339. [Google Scholar] [CrossRef] [PubMed]
- Rajasekaran, S.; Thangavel, C.; Djuric, N.; Raveendran, M.; Soundararajan, D.C.R.; Nayagam, S.M.; Matchado, M.S.; Sri Vijay Anand, K.S.; Venkateshwaran, K. Profiling extra cellular matrix associated proteome of human fetal nucleus pulposus in search for regenerative targets. Sci. Rep. 2021, 11, 19013. [Google Scholar] [CrossRef] [PubMed]
- Ye, D.; Liang, W.; Dai, L.; Zhou, L.; Yao, Y.; Zhong, X.; Chen, H.; Xu, J. Comparative and quantitative proteomic analysis of normal and degenerated human annulus fibrosus cells. Clin. Exp. Pharmacol. Physiol. 2015, 42, 530–536. [Google Scholar] [CrossRef] [PubMed]
- Önnerfjord, P.; Khabut, A.; Reinholt, F.P.; Svensson, O.; Heinegård, D. Quantitative Proteomic Analysis of Eight Cartilaginous Tissues Reveals Characteristic Differences as well as Similarities between Subgroups. J. Biol. Chem. 2012, 287, 18913. [Google Scholar] [CrossRef] [PubMed]
- Yee, A.; Lam, M.P.Y.; Tam, V.; Chan, W.C.W.; Chu, I.K.; Cheah, K.S.E.; Cheung, K.M.C.; Chan, D. Fibrotic-like changes in degenerate human intervertebral discs revealed by quantitative proteomic analysis. Osteoarthr. Cartil. 2016, 24, 503–513. [Google Scholar] [CrossRef]
- Rajasekaran, S.; Tangavel, C.; Sri Vijay Anand, K.S.; Soundararajan, D.C.R.; Nayagam, S.M.; Matchado, M.S.; Raveendran, M.; Shetty, A.P.; Kanna, R.M.; Dharmalingam, K. Inflammaging determines health and disease in lumbar discs-evidence from differing proteomic signatures of healthy, aging, and degenerating discs. Spine J. 2020, 20, 48–59. [Google Scholar] [CrossRef]
- Sarath Babu, N.; Krishnan, S.; Brahmendra Swamy, C.V.; Venkata Subbaiah, G.P.; Gurava Reddy, A.V.; Idris, M.M. Quantitative proteomic analysis of normal and degenerated human intervertebral disc. Spine J. 2016, 16, 989–1000. [Google Scholar] [CrossRef]
- Wangler, S.; Kamali, A.; Wapp, C.; Wuertz-Kozak, K.; Häckel, S.; Fortes, C.; Benneker, L.M.; Haglund, L.; Richards, R.G.; Alini, M.; et al. Uncovering the secretome of mesenchymal stromal cells exposed to healthy, traumatic, and degenerative intervertebral discs: A proteomic analysis. Stem Cell Res. Ther. 2021, 12, 11. [Google Scholar] [CrossRef]
- Radek, M.; Pacholczyk-Sienicka, B.; Jankowski, S.; Albrecht, Ł.; Grodzka, M.; Depta, A.; Radek, A. Assessing the correlation between the degree of disc degeneration on the Pfirrmann scale and the metabolites identified in HR-MAS NMR spectroscopy. Magn. Reson. Imaging 2016, 34, 376–380. [Google Scholar] [CrossRef]
- National Guideline Centre (UK). Low Back Pain and Sciatica in over 16s: Assessment and Management; National Institute for Health and Care Excellence (NICE): London, UK, 2016. [Google Scholar]
- Dagenais, S.; Caro, J.; Haldeman, S. A systematic review of low back pain cost of illness studies in the United States and internationally. Spine J. 2008, 8, 8–20. [Google Scholar] [CrossRef]
- Walker, B.F. The prevalence of low back pain: A systematic review of the literature from 1966 to 1998. J. Spinal Disord. 2000, 13, 205–217. [Google Scholar] [CrossRef]
- Vos, T.; Flaxman, A.D.; Naghavi, M.; Lozano, R.; Michaud, C.; Ezzati, M.; Shibuya, K.; Salomon, J.A.; Abdalla, S.; Aboyans, V.; et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012, 380, 2163–2196. [Google Scholar] [CrossRef]
- Foster, N.E.; Anema, J.R.; Cherkin, D.; Chou, R.; Cohen, S.P.; Gross, D.P.; Ferreira, P.H.; Fritz, J.M.; Koes, B.W.; Peul, W.; et al. Prevention and treatment of low back pain: Evidence, challenges, and promising directions. Lancet 2018, 391, 2368–2383. [Google Scholar] [CrossRef]
- Zigler, J.; Gornet, M.F.; Ferko, N.; Cameron, C.; Schranck, F.W.; Patel, L. Comparison of Lumbar Total Disc Replacement with Surgical Spinal Fusion for the Treatment of Single-Level Degenerative Disc Disease: A Meta-Analysis of 5-Year Outcomes from Randomized Controlled Trials. Glob. Spine J. 2017, 8, 413–423. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, T.H.; Randolph, D.C.; Talmage, J.; Succop, P.; Travis, R. Long-term outcomes of lumbar fusion among workers’ compensation subjects: A historical cohort study. Spine 2011, 36, 320–331. [Google Scholar] [CrossRef]
- Frost, B.A.; Camarero-Espinosa, S.; Johan Foster, E. Materials for the spine: Anatomy, problems, and solutions. Materials 2019, 12, 253. [Google Scholar] [CrossRef]
- Ruan, D.; He, Q.; Ding, Y.; Hou, L.; Li, J.; Luk, K.D.K. Intervertebral disc transplantation in the treatment of degenerative spine disease: A preliminary study. Lancet 2007, 369, 993–999. [Google Scholar] [CrossRef]
- Tarpada, S.P.; Morris, M.T.; Burton, D.A. Spinal fusion surgery: A historical perspective. J. Orthop. 2017, 14, 134–136. [Google Scholar] [CrossRef] [PubMed]
- Meng, B.; Bunch, J.; Burton, D.; Wang, J. Lumbar interbody fusion: Recent advances in surgical techniques and bone healing strategies. Eur. Spine J. 2021, 30, 22–33. [Google Scholar] [CrossRef]
- Iatridis, J.C.; Nicoll, S.B.; Michalek, A.J.; Walter, B.A.; Gupta, M.S. Role of biomechanics in intervertebral disc degeneration and regenerative therapies: What needs repairing in the disc and what are promising biomaterials for its repair? Spine J. 2013, 13, 243–262. [Google Scholar] [CrossRef] [PubMed]
- Sloan, S.R.; Lintz, M.; Hussain, I.; Hartl, R.; Bonassar, L.J. Biologic Annulus Fibrosus Repair: A Review of Preclinical in Vivo Investigations. Tissue Eng. Part B Rev. 2018, 24, 179–190. [Google Scholar] [CrossRef] [PubMed]
- Hom, W.W.; Tschopp, M.; Lin, H.A.; Nasser, P.; Laudier, D.M.; Hecht, A.C.; Nicoll, S.B.; Iatridis, J.C. Composite biomaterial repair strategy to restore biomechanical function and reduce herniation risk in an ex vivo large animal model of intervertebral disc herniation with varying injury severity. PLoS ONE 2019, 14, e0217357. [Google Scholar] [CrossRef] [PubMed]
- Iatridis, J.C. Structural and Functional Repair of the Annulus Fibrosus. Glob. Spine J. 2017, 6, s-1582578. [Google Scholar] [CrossRef]
- Tuakli-Wosornu, Y.A.; Terry, A.; Boachie-Adjei, K.; Harrison, J.R.; Gribbin, C.K.; LaSalle, E.E.; Nguyen, J.T.; Solomon, J.L.; Lutz, G.E. Lumbar Intradiskal Platelet-Rich Plasma (PRP) Injections: A Prospective, Double-Blind, Randomized Controlled Study. Phys. Med. Rehabil. 2016, 8, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Comella, K.; Silbert, R.; Parlo, M. Effects of the intradiscal implantation of stromal vascular fraction plus platelet rich plasma in patients with degenerative disc disease. J. Transl. Med. 2017, 15, 12. [Google Scholar] [CrossRef] [PubMed]
- Pirvu, T.N.; Schroeder, J.E.; Peroglio, M.; Verrier, S.; Kaplan, L.; Richards, R.G.; Alini, M.; Grad, S. Platelet-rich plasma induces annulus fibrosus cell proliferation and matrix production. Eur. Spine J. 2014, 23, 745–753. [Google Scholar] [CrossRef]
- Chen, W.H.; Liu, H.Y.; Lo, W.C.; Wu, S.C.; Chi, C.H.; Chang, H.Y.; Hsiao, S.H.; Wu, C.H.; Chiu, W.T.; Chen, B.J.; et al. Intervertebral disc regeneration in an ex vivo culture system using mesenchymal stem cells and platelet-rich plasma. Biomaterials 2009, 30, 5523–5533. [Google Scholar] [CrossRef]
- Gantenbein, B.; Illien-Jünger, S.; Chan, S.C.W.; Walser, J.; Haglund, L.; Ferguson, S.J.; Iatridis, J.C.; Grad, S. Organ culture bioreactors-platforms to study human intervertebral disc degeneration and regenerative therapy. Curr. Stem Cell Res. Ther. 2015, 10, 339–352. [Google Scholar] [CrossRef]
- Clouet, J.; Fusellier, M.; Camus, A.; Le Visage, C.; Guicheux, J. Intervertebral disc regeneration: From cell therapy to the development of novel bioinspired endogenous repair strategies. Adv. Drug Deliv. Rev. 2019, 146, 306–324. [Google Scholar] [CrossRef]
- Roh, E.J.; Darai, A.; Kyung, J.W.; Choi, H.; Kwon, S.Y.; Bhujel, B.; Kim, K.T.; Han, I. Genetic Therapy for Intervertebral Disc Degeneration. Int. J. Mol. Sci. 2021, 22, 1579. [Google Scholar] [CrossRef] [PubMed]
- Farhang, N.; Ginley-Hidinger, M.; Berrett, K.C.; Gertz, J.; Lawrence, B.; Bowles, R.D. Lentiviral CRISPR Epigenome Editing of Inflammatory Receptors as a Gene Therapy Strategy for Disc Degeneration. Hum. Gene Ther. 2019, 30, 1161–1175. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Zheng, Z.; Qi, J.; Wang, J.; Zhou, Q.; Hu, F.; Liang, J.; Li, C.; Zhang, W.; Zhang, X. CD24 identifies nucleus pulposus progenitors/notochordal cells for disc regeneration. J. Biol. Eng. 2018, 12, 35. [Google Scholar] [CrossRef]
- Williams, R.J.; Tryfonidou, M.A.; Snuggs, J.W.; Le Maitre, C.L. Cell sources proposed for nucleus pulposus regeneration. JOR Spine 2021, 4, e1175. [Google Scholar] [CrossRef] [PubMed]
- Gay, M.H.P.; Mehrkens, A.; Rittmann, M.; Haug, M.; Barbero, A.; Martin, I.; Schaeren, S. Nose to back: Compatibility of nasal chondrocytes with environmental conditions mimicking a degenerated intervertebral disc. Eur. Cells Mater. 2019, 37, 214–323. [Google Scholar] [CrossRef]
- Kuh, S.U.; Zhu, Y.; Li, J.; Tsai, K.J.; Fei, Q.; Hutton, W.C.; Yoon, T.S. A comparison of three cell types as potential candidates for intervertebral disc therapy: Annulus fibrosus cells, chondrocytes, and bone marrow derived cells. Jt. Bone Spine 2009, 76, 70–74. [Google Scholar] [CrossRef]
- Sakai, D.; Andersson, G.B.J. Stem cell therapy for intervertebral disc regeneration: Obstacles and solutions. Nat. Rev. Rheumatol. 2015, 11, 243–256. [Google Scholar] [CrossRef]
- Mobasheri, A.; Richardson, S.M. Cell and Gene Therapy for Spine Regeneration: Mammalian Protein Production Platforms for Overproduction of Therapeutic Proteins and Growth Factors. Neurosurg. Clin. N. Am. 2020, 31, 131. [Google Scholar] [CrossRef]
- Melrose, J. Strategies in regenerative medicine for intervertebral disc repair using mesenchymal stem cells and bioscaffolds. Regen. Med. 2016, 11, 705–724. [Google Scholar] [CrossRef]
- Clarke, L.E.; McConnell, J.C.; Sherratt, M.J.; Derby, B.; Richardson, S.M.; Hoyland, J.A. Growth differentiation factor 6 and transforming growth factor-beta differentially mediate mesenchymal stem cell differentiation, composition, and micromechanical properties of nucleus pulposus constructs. Arthritis Res. Ther. 2014, 16, R67. [Google Scholar] [CrossRef]
- Chujo, T.; An, H.S.; Akeda, K.; Miyamoto, K.; Muehleman, C.; Attawia, M.; Andersson, G.; Masuda, K. Effects of growth differentiation factor-5 on the intervertebral disc—In vitro bovine study and in vivo rabbit disc degeneration model study. Spine 2006, 31, 2909–2917. [Google Scholar] [CrossRef] [PubMed]
- Loibl, M.; Wuertz-Kozak, K.; Vadala, G.; Lang, S.; Fairbank, J.; Urban, J.P. Controversies in regenerative medicine: Should intervertebral disc degeneration be treated with mesenchymal stem cells? JOR Spine 2019, 2, e1043. [Google Scholar] [CrossRef] [PubMed]
- Migliorini, F.; Rath, B.; Tingart, M.; Baroncini, A.; Quack, V.; Eschweiler, J. Autogenic mesenchymal stem cells for intervertebral disc regeneration. Int. Orthop. 2018, 43, 1027–1036. [Google Scholar] [CrossRef] [PubMed]
- Stoyanov, J.V.; Gantenbein-Ritter, B.; Bertolo, A.; Aebli, N.; Baur, M.; Alini, M.; Grad, S. Role of hypoxia and growth and differentiation factor-5 on differentiation of human mesenchymal stem cells towards intervertebral nucleus pulposus-like cells. Eur. Cells Mater. 2011, 21, 533–547. [Google Scholar] [CrossRef] [PubMed]
- Zeckser, J.; Wolff, M.; Tucker, J.; Goodwin, J. Multipotent Mesenchymal Stem Cell Treatment for Discogenic Low Back Pain and Disc Degeneration. Stem Cells Int. 2016, 2016, 3908389. [Google Scholar] [CrossRef] [PubMed]
- Binch, A.L.A.; Fitzgerald, J.C.; Growney, E.A.; Barry, F. Cell-based strategies for IVD repair: Clinical progress and translational obstacles. Nat. Rev. Rheumatol. 2021, 17, 158–175. [Google Scholar] [CrossRef]
- Kennon, J.C.; Awad, M.E.; Chutkan, N.; Devine, J.; Fulzele, S. Current insights on use of growth factors as therapy for Intervertebral Disc Degeneration. Biomol. Concepts 2018, 9, 43–52. [Google Scholar] [CrossRef]
- Ho, G.; Leung, V.Y.L.; Cheung, K.M.C.; Chan, D. Effect of severity of intervertebral disc injury on mesenchymal stem cell-based regeneration. Connect. Tissue Res. 2008, 49, 15–21. [Google Scholar] [CrossRef]
- Wuertz, K.; Godburn, K.; Neidlinger-Wilke, C.; Urban, J.; Iatridis, J.C. Behavior of Mesenchymal Stem Cells in the Chemical Microenvironment of the Intervertebral Disc. Spine 2008, 33, 1843. [Google Scholar] [CrossRef]
- Kluba, T.; Niemeyer, T.; Gaissmaier, C.; Gründer, T. Human anulus fibrosis and nucleus pulposus cells of the intervertebral disc: Effect of degeneration and culture system on cell phenotype. Spine 2005, 30, 2743–2748. [Google Scholar] [CrossRef]
- Speer, J.E.; Barcellona, M.N.; Lu, M.Y.; Zha, Z.; Jing, L.; Gupta, M.C.; Buchowski, J.M.; Kelly, M.P.; Setton, L.A. Development of a library of laminin-mimetic peptide hydrogels for control of nucleus pulposus cell behaviors. J. Tissue Eng. 2021, 12, 20417314211021220. [Google Scholar] [CrossRef] [PubMed]
- Tan, X.; Jain, E.; Barcellona, M.N.; Morris, E.; Neal, S.; Gupta, M.C.; Buchowski, J.M.; Kelly, M.; Setton, L.A.; Huebsch, N. Integrin and syndecan binding peptide-conjugated alginate hydrogel for modulation of nucleus pulposus cell phenotype. Biomaterials 2021, 277, 121113. [Google Scholar] [CrossRef] [PubMed]
- Zhou, X.; Tao, Y.; Chen, E.; Wang, J.; Fang, W.; Zhao, T.; Liang, C.; Li, F.; Chen, Q. Genipin-cross-linked type II collagen scaffold promotes the differentiation of adipose-derived stem cells into nucleus pulposus-like cells. J. Biomed. Mater. Res. Part A 2018, 106, 1258–1268. [Google Scholar] [CrossRef]
- Chen, P.; Ning, L.; Qiu, P.; Mo, J.; Mei, S.; Xia, C.; Zhang, J.; Lin, X.; Fan, S. Photo-crosslinked gelatin-hyaluronic acid methacrylate hydrogel-committed nucleus pulposus-like differentiation of adipose stromal cells for intervertebral disc repair. J. Tissue Eng. Regen. Med. 2019, 13, 682–693. [Google Scholar] [CrossRef]
- Wang, J.; Tao, Y.; Zhou, X.; Li, H.; Liang, C.; Li, F.; Chen, Q.X. The potential of chondrogenic pre-differentiation of adipose-derived mesenchymal stem cells for regeneration in harsh nucleus pulposus microenvironment. Exp. Biol. Med. 2016, 241, 2104–2111. [Google Scholar] [CrossRef] [PubMed]
- Huang, B.; Zhuang, Y.; Li, C.Q.; Liu, L.T.; Zhou, Y. Regeneration of the intervertebral disc with nucleus pulposus cell-seeded collagen II/hyaluronan/chondroitin-6-sulfate tri-copolymer constructs in a rabbit disc degeneration model. Spine 2011, 36, 2252–2259. [Google Scholar] [CrossRef]
- Grunert, P.; Borde, B.H.; Towne, S.B.; Moriguchi, Y.; Hudson, K.D.; Bonassar, L.J.; Härtl, R. Riboflavin crosslinked high-density collagen gel for the repair of annular defects in intervertebral discs: An in vivo study. Acta Biomater. 2015, 26, 215–224. [Google Scholar] [CrossRef]
- Borde, B.; Grunert, P.; Härtl, R.; Bonassar, L.J. Injectable, high-density collagen gels for annulus fibrosus repair: An in vitro rat tail model. J. Biomed. Mater. Res. Part A 2015, 103, 2571–2581. [Google Scholar] [CrossRef]
- Guillaume, O.; Naqvi, S.M.; Lennon, K.; Buckley, C.T. Enhancing cell migration in shape-memory alginate-collagen composite scaffolds: In vitro and ex vivo assessment for intervertebral disc repair. J. Biomater. Appl. 2015, 29, 1230–1246. [Google Scholar] [CrossRef]
- Du, J.; Long, R.G.; Nakai, T.; Sakai, D.; Benneker, L.M.; Zhou, G.; Li, B.; Eglin, D.; Iatridis, J.C.; Alini, M.; et al. Functional cell phenotype induction with TGF-β1 and collagen-polyurethane scaffold for annulus fibrosus rupture repair. Eur. Cells Mater. 2020, 39, 1–17. [Google Scholar] [CrossRef]
- Hussain, I.; Sloan, S.R.; Wipplinger, C.; Navarro-Ramirez, R.; Zubkov, M.; Kim, E.; Kirnaz, S.; Bonassar, L.J.; Härtl, R. Mesenchymal Stem Cell-Seeded High-Density Collagen Gel for Annular Repair: 6-Week Results from in Vivo Sheep Models. Neurosurgery 2019, 85, E350–E359. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Jin, Z.; Ge, X.; Zhang, Y.; Xu, H. Decellularized Annulus Fibrosus Matrix/Chitosan Hybrid Hydrogels with Basic Fibroblast Growth Factor for Annulus Fibrosus Tissue Engineering. Tissue Eng. Part A 2019, 25, 1605–1613. [Google Scholar] [CrossRef] [PubMed]
- Kilmer, C.E.; Battistoni, C.M.; Cox, A.; Breur, G.J.; Panitch, A.; Liu, J.C. Collagen Type I and II Blend Hydrogel with Autologous Mesenchymal Stem Cells as a Scaffold for Articular Cartilage Defect Repair. ACS Biomater. Sci. Eng. 2020, 6, 3464–3476. [Google Scholar] [CrossRef] [PubMed]
- Kilmer, C.E.; Walimbe, T.; Panitch, A.; Liu, J.C. Incorporation of a Collagen-Binding Chondroitin Sulfate Molecule to a Collagen Type I and II Blend Hydrogel for Cartilage Tissue Engineering. ACS Biomater. Sci. Eng. 2022, 8, 1247–1257. [Google Scholar] [CrossRef] [PubMed]
- Walimbe, T.; Calve, S.; Panitch, A.; Sivasankar, M.P. Incorporation of types I and III collagen in tunable hyaluronan hydrogels for vocal fold tissue engineering. Acta Biomater. 2019, 87, 97–107. [Google Scholar] [CrossRef]
- Walimbe, T.; Panitch, A. Best of Both Hydrogel Worlds: Harnessing Bioactivity and Tunability by Incorporating Glycosaminoglycans in Collagen Hydrogels. Bioengineering 2020, 7, 156. [Google Scholar] [CrossRef]
- Sharma, S.; Panitch, A.; Neu, C.P. Incorporation of an aggrecan mimic prevents proteolytic degradation of anisotropic cartilage analogs. Acta Biomater. 2013, 9, 4618–4625. [Google Scholar] [CrossRef]
- Sarkar, S.; Moorehead, C.; Prudnikova, K.; Schauer, C.L.; Penn, L.S.; Marcolongo, M. Synthesis of macromolecular mimics of small leucine-rich proteoglycans with a poly(ethylene glycol) core and chondroitin sulphate bristles. Carbohydr. Polym. 2017, 166, 338–347. [Google Scholar] [CrossRef]
- Prudnikova, K.; Yucha, R.W.; Patel, P.; Kriete, A.S.; Han, L.; Penn, L.S.; Marcolongo, M.S. Biomimetic Proteoglycans Mimic Macromolecular Architecture and Water Uptake of Natural Proteoglycans. Biomacromolecules 2017, 18, 1713–1723. [Google Scholar] [CrossRef]
- Sarkar, S.; Lightfoot-Vidal, S.E.; Schauer, C.L.; Vresilovic, E.; Marcolongo, M. Terminal-end functionalization of chondroitin sulfate for the synthesis of biomimetic proteoglycans. Carbohydr. Polym. 2012, 90, 431–440. [Google Scholar] [CrossRef]
- Bernhard, J.C.; Panitch, A. Synthesis and characterization of an aggrecan mimic. Acta Biomater. 2012, 8, 1543–1550. [Google Scholar] [CrossRef] [PubMed]
- Sharma, S.; Lee, A.; Choi, K.; Kim, K.; Youn, I.; Trippel, S.B.; Panitch, A. Biomimetic Aggrecan Reduces Cartilage Extracellular Matrix from Degradation and Lowers Catabolic Activity in Ex Vivo and In Vivo Models. Macromol. Biosci. 2013, 13, 1228–1237. [Google Scholar] [CrossRef] [PubMed]
- Phillips, E.R.; Haislup, B.D.; Bertha, N.; Lefchak, M.; Sincavage, J.; Prudnikova, K.; Shallop, B.; Mulcahey, M.K.; Marcolongo, M.S. Biomimetic proteoglycans diffuse throughout articular cartilage and localize within the pericellular matrix. J. Biomed. Mater. Res. Part A 2019, 107, 1977–1987. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.; Shimmon, S.; Paton, S.; Daly, C.; Goldschlager, T.; Gronthos, S.; Zannettino, A.C.W.; Ghosh, P. Pentosan polysulfate binds to STRO-1+ mesenchymal progenitor cells, is internalized, and modifies gene expression: A novel approach of pre-programing stem cells for therapeutic application requiring their chondrogenesis. Stem Cell Res. Ther. 2017, 8, 278. [Google Scholar] [CrossRef]
- Hayes, A.J.; Melrose, J. Glycosaminoglycan and Proteoglycan Biotherapeutics in Articular Cartilage Protection and Repair Strategies: Novel Approaches to Visco-supplementation in Orthobiologics. Adv. Ther. 2019, 2, 1900034. [Google Scholar] [CrossRef]
- Farrugia, B.L.; Lord, M.S.; Whitelock, J.M.; Melrose, J. Harnessing chondroitin sulphate in composite scaffolds to direct progenitor and stem cell function for tissue repair. Biomater. Sci. 2018, 6, 947–957. [Google Scholar] [CrossRef]
- Prudnikova, K.; Lightfoot Vidal, S.E.; Sarkar, S.; Yu, T.; Yucha, R.W.; Ganesh, N.; Penn, L.S.; Han, L.; Schauer, C.L.; Vresilovic, E.J.; et al. Aggrecan-like biomimetic proteoglycans (BPGs) composed of natural chondroitin sulfate bristles grafted onto a poly(acrylic acid) core for molecular engineering of the extracellular matrix. Acta Biomater. 2018, 75, 93–104. [Google Scholar] [CrossRef]
- Madende, D.; Prudnikova, K.; Lightfoot, S.; Vresilovic, E.; Marcolongo, M. New biomimetic aggrecan for treatment of intervertebral disc degeneration. In Proceedings of the 2012 38th Annual Northeast Bioengineering Conference (NEBEC), Philadelphia, PA, USA, 16–18 March 2012; Volume 2012, pp. 213–214. [Google Scholar]
- Smith, M.M.; Hayes, A.J.; Melrose, J. Pentosan Polysulfate, a Semisynthetic Heparinoid Disease-Modifying Osteoarthritic Drug with Roles in Intervertebral Disc Repair Biology Emulating the Stem Cell Instructive and Tissue Reparative Properties of Heparan Sulfate. Stem Cells Dev. 2022; advance online publication. [Google Scholar] [CrossRef]
- Sivan, S.S.; Roberts, S.; Urban, J.P.G.; Menage, J.; Bramhill, J.; Campbell, D.; Franklin, V.J.; Lydon, F.; Merkher, Y.; Maroudas, A.; et al. Injectable hydrogels with high fixed charge density and swelling pressure for nucleus pulposus repair: Biomimetic glycosaminoglycan analogues. Acta Biomater. 2014, 10, 1124–1133. [Google Scholar] [CrossRef]
- Knani, D.; Eylon, M.; Sivan, S.S. Molecular modeling study of the swelling of glycosaminoglycan-analog biomimetics for intervertebral disc repair. Polym. Adv. Technol. 2020, 31, 2733–2741. [Google Scholar] [CrossRef]
- Farrugia, B.; Hayes, A.J.; Melrose, J. Use of Chondroitin Sulphate to Aid In Vitro Stem Cell Differentiation. In Proteoglycans in Stem Cells: From Development to Cancer, 1st ed.; Götte, M., Forsberg-Nilsson, K., Eds.; Springer: Cham, Switzerland, 2021; pp. 53–93. [Google Scholar]
- Place, L.W.; Kelly, S.M.; Kipper, M.J. Synthesis and characterization of proteoglycan-mimetic graft copolymers with tunable glycosaminoglycan density. Biomacromolecules 2014, 15, 3772–3780. [Google Scholar] [CrossRef]
- Vadalà, G.; Russo, F.; Musumeci, M.; D’Este, M.; Cattani, C.; Catanzaro, G.; Tirindelli, M.C.; Lazzari, L.; Alini, M.; Giordano, R.; et al. Clinically relevant hydrogel-based on hyaluronic acid and platelet rich plasma as a carrier for mesenchymal stem cells: Rheological and biological characterization. J. Orthop. Res. 2017, 35, 2109–2116. [Google Scholar] [CrossRef] [PubMed]
- Pati, F.; Jang, J.; Ha, D.H.; Won Kim, S.; Rhie, J.W.; Shim, J.H.; Kim, D.H.; Cho, D.W. Printing three-dimensional tissue analogues with decellularized extracellular matrix bioink. Nat. Commun. 2014, 5, 3935. [Google Scholar] [CrossRef] [PubMed]
- Fiordalisi, M.; Silva, A.J.; Barbosa, M.; Goncalves, R.; Caldeira, J. Decellularised Scaffolds for Intervertebral Disc Regeneration. Trends Biotechnol. 2020, 38, 947–951. [Google Scholar] [CrossRef]
- Hoshiba, T.; Chen, G.; Endo, C.; Maruyama, H.; Wakui, M.; Nemoto, E.; Kawazoe, N.; Tanaka, M. Decellularized Extracellular Matrix as an In Vitro Model to Study the Comprehensive Roles of the ECM in Stem Cell Differentiation. Stem Cells Int. 2016, 2016, 6397820. [Google Scholar] [CrossRef] [PubMed]
- Penolazzi, L.; Pozzobon, M.; Bergamin, L.S.; D’Agostino, S.; Francescato, R.; Bonaccorsi, G.; De Bonis, P.; Cavallo, M.; Lambertini, E.; Piva, R. Extracellular Matrix from Decellularized Wharton’s Jelly Improves the Behavior of Cells from Degenerated Intervertebral Disc. Front. Bioeng. Biotechnol. 2020, 8, 262. [Google Scholar] [CrossRef]
- Kim, B.S.; Kim, H.; Gao, G.; Jang, J.; Cho, D.W. Decellularized extracellular matrix: A step towards the next generation source for bioink manufacturing. Biofabrication 2017, 9, 034104. [Google Scholar] [CrossRef]
- Kim, B.S.; Das, S.; Jang, J.; Cho, D.W. Decellularized Extracellular Matrix-based Bioinks for Engineering Tissue- and Organ-specific Microenvironments. Chem. Rev. 2020, 120, 10608–10661. [Google Scholar] [CrossRef]
- Pina, S.; Ribeiro, V.P.; Marques, C.F.; Maia, F.R.; Silva, T.H.; Reis, R.L.; Oliveira, J.M. Scaffolding Strategies for Tissue Engineering and Regenerative Medicine Applications. Materials 2019, 12, 1824. [Google Scholar] [CrossRef]
- Taylor, D.A.; Sampaio, L.C.; Ferdous, Z.; Gobin, A.S.; Taite, L.J. Decellularized matrices in regenerative medicine. Acta Biomater. 2018, 74, 74–89. [Google Scholar] [CrossRef]
- Parmaksiz, M.; Dogan, A.; Odabas, S.; Elcin, A.E.; Elcin, Y.M. Clinical applications of decellularized extracellular matrices for tissue engineering and regenerative medicine. Biomed. Mater. 2016, 11, 022003. [Google Scholar] [CrossRef]
- Chae, S.; Cho, D.W. Three-dimensional bioprinting with decellularized extracellular matrix-based bioinks in translational regenerative medicine. MRS Bull. 2022, 47, 70–79. [Google Scholar] [CrossRef]
- Tsaryk, R.; Gloria, A.; Russo, T.; Anspach, L.; De Santis, R.; Ghanaati, S.; Unger, R.E.; Ambrosio, L.; Kirkpatrick, C.J. Collagen-low molecular weight hyaluronic acid semi-interpenetrating network loaded with gelatin microspheres for cell and growth factor delivery for nucleus pulposus regeneration. Acta Biomater. 2015, 20, 10–21. [Google Scholar] [CrossRef]
- Collin, E.C.; Grad, S.; Zeugolis, D.I.; Vinatier, C.S.; Clouet, J.R.; Guicheux, J.J.; Weiss, P.; Alini, M.; Pandit, A.S. An injectable vehicle for nucleus pulposus cell-based therapy. Biomaterials 2011, 32, 2862–2870. [Google Scholar] [CrossRef] [PubMed]
- Fontana, G.; Thomas, D.; Collin, E.; Pandit, A.; Fontana, G.; Thomas, D.; Collin, E.; Pandit, A. Microgel Microenvironment Primes Adipose-Derived Stem Cells Towards an NP Cells-Like Phenotype. Adv. Healthc. Mater. 2014, 3, 2012–2022. [Google Scholar] [CrossRef] [PubMed]
- Srivastava, A.; Isa, I.L.M.; Rooney, P.; Pandit, A. Bioengineered three-dimensional diseased intervertebral disc model revealed inflammatory crosstalk. Biomaterials 2017, 123, 127–141. [Google Scholar] [CrossRef] [PubMed]
- Borrelli, C.; Buckley, C.T. Injectable Disc-Derived ECM Hydrogel Functionalised with Chondroitin Sulfate for Intervertebral Disc Regeneration. Acta Biomater. 2020, 117, 142–155. [Google Scholar] [CrossRef]
- Francisco, A.T.; Mancino, R.J.; Bowles, R.D.; Brunger, J.M.; Tainter, D.M.; Chen, Y.T.; Richardson, W.J.; Guilak, F.; Setton, L.A. Injectable laminin-functionalized hydrogel for nucleus pulposus regeneration. Biomaterials 2013, 34, 7381–7388. [Google Scholar] [CrossRef]
- Peroglio, M.; Eglin, D.; Benneker, L.M.; Alini, M.; Grad, S. Thermoreversible hyaluronan-based hydrogel supports in vitro and ex vivo disc-like differentiation of human mesenchymal stem cells. Spine J. 2013, 13, 1627–1639. [Google Scholar] [CrossRef]
- Jeong, C.G.; Francisco, A.T.; Niu, Z.; Mancino, R.L.; Craig, S.L.; Setton, L.A. Screening of hyaluronic acid-poly(ethylene glycol) composite hydrogels to support intervertebral disc cell biosynthesis using artificial neural network analysis. Acta Biomater. 2014, 10, 3421–3430. [Google Scholar] [CrossRef]
- Isa, I.L.M.; Srivastava, A.; Tiernan, D.; Owens, P.; Rooney, P.; Dockery, P.; Pandit, A. Hyaluronic acid based hydrogels attenuate inflammatory receptors and neurotrophins in interleukin-1β induced inflammation model of nucleus pulposus cells. Biomacromolecules 2015, 16, 1714–1725. [Google Scholar] [CrossRef]
- Mohd Isa, I.L.; Abbah, S.A.; Kilcoyne, M.; Sakai, D.; Dockery, P.; Finn, D.P.; Pandit, A. Implantation of hyaluronic acid hydrogel prevents the pain phenotype in a rat model of intervertebral disc injury. Sci. Adv. 2018, 4, eaaq0597. [Google Scholar] [CrossRef] [PubMed]
- Fuller, E.S.; Shu, C.; Smith, M.M.; Little, C.B.; Melrose, J. Hyaluronan oligosaccharides stimulate matrix metalloproteinase and anabolic gene expression in vitro by intervertebral disc cells and annular repair in vivo. J. Tissue Eng. Regen. Med. 2018, 12, e216–e226. [Google Scholar] [CrossRef] [PubMed]
- Frith, J.E.; Menzies, D.J.; Cameron, A.R.; Ghosh, P.; Whitehead, D.L.; Gronthos, S.; Zannettino, A.C.W.; Cooper-White, J.J. Effects of bound versus soluble pentosan polysulphate in PEG/HA-based hydrogels tailored for intervertebral disc regeneration. Biomaterials 2014, 35, 1150–1162. [Google Scholar] [CrossRef] [PubMed]
- Oehme, D.; Ghosh, P.; Shimmon, S.; Wu, J.; McDonald, C.; Troupis, J.M.; Goldschlager, T.; Rosenfeld, J.V.; Jenkin, G. Mesenchymal progenitor cells combined with pentosan polysulfate mediating disc regeneration at the time of microdiscectomy: A preliminary study in an ovine model: Laboratory investigation. J. Neurosurg. Spine 2014, 20, 657–669. [Google Scholar] [CrossRef] [PubMed]
- Costa, J.B.; Silva-Correia, J.; Ribeiro, V.P.; da Silva Morais, A.; Oliveira, J.M.; Reis, R.L. Engineering patient-specific bioprinted constructs for treatment of degenerated intervertebral disc. Mater. Today Commun. 2019, 19, 506–512. [Google Scholar] [CrossRef]
- Bello, A.B.; Kim, Y.; Park, S.; Muttigi, M.S.; Kim, J.; Park, H.; Lee, S. Matrilin3/TGFβ3 gelatin microparticles promote chondrogenesis, prevent hypertrophy, and induce paracrine release in MSC spheroid for disc regeneration. NPJ Regen. Med. 2021, 6, 50. [Google Scholar] [CrossRef]
- Bridgen, D.T.; Fearing, B.V.; Jing, L.; Sanchez-Adams, J.; Cohan, M.C.; Guilak, F.; Chen, J.; Setton, L.A. Regulation of human nucleus pulposus cells by peptide-coupled substrates. Acta Biomater. 2017, 55, 100–108. [Google Scholar] [CrossRef]
- Barcellona, M.N.; Speer, J.E.; Jing, L.; Patil, D.S.; Gupta, M.C.; Buchowski, J.M.; Setton, L.A. Bioactive in situ crosslinkable polymer-peptide hydrogel for cell delivery to the intervertebral disc in a rat model. Acta Biomater. 2021, 131, 117–127. [Google Scholar] [CrossRef]
- Guilak, F.; Hayes, A.J.; Melrose, J. Perlecan in pericellular mechanosensory cell-matrix communication, extracellular matrix stabilisation and mechanoregulation of load-bearing connective tissues. Int. J. Mol. Sci. 2021, 22, 2716. [Google Scholar] [CrossRef]
- Smith, S.M.; Melrose, J. Type XI collagen-perlecan-HS interactions stabilise the pericellular matrix of annulus fibrosus cells and chondrocytes providing matrix stabilisation and homeostasis. J. Mol. Histol. 2019, 50, 285–294. [Google Scholar] [CrossRef]
- Hayes, A.J.; Melrose, J. What Are the Potential Roles of Nuclear Perlecan and Other Heparan Sulphate Proteoglycans in the Normal and Malignant Phenotype. Int. J. Mol. Sci. 2021, 22, 4415. [Google Scholar] [CrossRef] [PubMed]
- Melrose, J. Perlecan, a modular instructive proteoglycan with diverse functional properties. Int. J. Biochem. Cell Biol. 2020, 128, 105849. [Google Scholar] [CrossRef] [PubMed]
- Loebel, C.; Mauck, R.L.; Burdick, J.A. Local nascent protein deposition and remodelling guide mesenchymal stromal cell mechanosensing and fate in three-dimensional hydrogels. Nat. Mater. 2019, 18, 883–891. [Google Scholar] [CrossRef]
- Loebel, C.; Kwon, M.Y.; Wang, C.; Han, L.; Mauck, R.L.; Burdick, J.A. Metabolic Labeling to Probe the Spatiotemporal Accumulation of Matrix at the Chondrocyte-Hydrogel Interface. Adv. Funct. Mater. 2020, 30, 1909802. [Google Scholar] [CrossRef] [PubMed]
- Zhou, M.; Lozano, N.; Wychowaniec, J.K.; Hodgkinson, T.; Richardson, S.M.; Kostarelos, K.; Hoyland, J.A. Graphene oxide: A growth factor delivery carrier to enhance chondrogenic differentiation of human mesenchymal stem cells in 3D hydrogels. Acta Biomater. 2019, 96, 271–280. [Google Scholar] [CrossRef] [PubMed]
- Ligorio, C.; Zhou, M.; Wychowaniec, J.K.; Zhu, X.; Bartlam, C.; Miller, A.F.; Vijayaraghavan, A.; Hoyland, J.A.; Saiani, A. Graphene oxide containing self-assembling peptide hybrid hydrogels as a potential 3D injectable cell delivery platform for intervertebral disc repair applications. Acta Biomater. 2019, 92, 92–103. [Google Scholar] [CrossRef]
- Vyas, C.; Ates, G.; Aslan, E.; Hart, J.; Huang, B.; Bartolo, P. Three-Dimensional Printing and Electrospinning Dual-Scale Polycaprolactone Scaffolds with Low-Density and Oriented Fibers to Promote Cell Alignment. 3D Print. Addit. Manuf. 2020, 7, 105–113. [Google Scholar] [CrossRef] [PubMed]
- Chang, G.; Kim, H.J.; Vunjak-Novakovic, G.; Kaplan, D.L.; Kandel, R. Enhancing annulus fibrosus tissue formation in porous silk scaffolds. J. Biomed. Mater. Res. Part A 2010, 92, 43–51. [Google Scholar] [CrossRef]
- Kandel, R.; Santerre, P.; Massicotte, E.; Hurtig, M. Tissue engineering of the intervertebral disc. In The Intervertebral Disc: Molecular and Structural Studies of the Disc in Health and Disease, 1st ed.; Shapiro, I., Risbud, M., Eds.; Springer: Vienna, Austria, 2014; Volume 1, pp. 417–434. [Google Scholar]
- Attia, M.; Santerre, J.P.; Kandel, R.A. The response of annulus fibrosus cell to fibronectin-coated nanofibrous polyurethane-anionic dihydroxyoligomer scaffolds. Biomaterials 2011, 32, 450–460. [Google Scholar] [CrossRef]
- Pirvu, T.; Blanquer, S.B.G.; Benneker, L.M.; Grijpma, D.W.; Richards, R.G.; Alini, M.; Eglin, D.; Grad, S.; Li, Z. A combined biomaterial and cellular approach for annulus fibrosus rupture repair. Biomaterials 2015, 42, 11–19. [Google Scholar] [CrossRef]
- Shamsah, A.H.; Cartmell, S.H.; Richardson, S.M.; Bosworth, L.A. Mimicking the Annulus Fibrosus Using Electrospun Polyester Blended Scaffolds. Nanomaterials 2019, 9, 537. [Google Scholar] [CrossRef] [PubMed]
- Chong, J.E.; Santerre; Paul, J.; Kandel, R.A.; Mount, R.A.K.; Hospital, S. Generation of an in vitro model of the outer annulus fibrosus-cartilage interface. JOR Spine 2020, 3, e1089. [Google Scholar] [CrossRef] [PubMed]
- Turner, K.G.; Ahmed, N.; Santerre, J.P.; Kandel, R.A. Modulation of annulus fibrosus cell alignment and function on oriented nanofibrous polyurethane scaffolds under tension. Spine J. 2014, 14, 424–434. [Google Scholar] [CrossRef] [PubMed]
- Iu, J.; Santerre, J.P.; Kandel, R.A. Towards engineering distinct multi-lamellated outer and inner annulus fibrosus tissues. J. Orthop. Res. 2018, 36, 1346–1355. [Google Scholar] [CrossRef] [PubMed]
- Iu, J.; Santerre, J.P.; Kandel, R.A. Inner and outer annulus fibrosus cells exhibit differentiated phenotypes and yield changes in extracellular matrix protein composition in vitro on a polycarbonate urethane scaffold. Tissue Eng. Part A 2014, 20, 3261–3269. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Zhu, C.; Li, J.; Zhou, P.; Chen, M.; Yang, H.; Li, B. The effect of the fibre orientation of electrospun scaffolds on the matrix production of rabbit annulus fibrosus-derived stem cells. Bone Res. 2015, 3, 15012. [Google Scholar] [CrossRef] [PubMed]
- Zhou, P.; Chu, G.; Yuan, Z.; Wang, H.; Zhang, W.; Mao, Y.; Zhu, X.; Chen, W.; Yang, H.; Li, B. Regulation of differentiation of annulus fibrosus-derived stem cells using heterogeneous electrospun fibrous scaffolds. J. Orthop. Transl. 2021, 26, 171–180. [Google Scholar] [CrossRef]
- Zhu, C.; Li, J.; Liu, C.; Zhou, P.; Yang, H.; Li, B. Modulation of the gene expression of annulus fibrosus-derived stem cells using poly(ether carbonate urethane)urea scaffolds of tunable elasticity. Acta Biomater. 2016, 29, 228–238. [Google Scholar] [CrossRef]
- Zhu, C.; Li, J.; Liu, C.; Zhou, P.; Yang, H.; Li, B. Effect of scaffold elasticity on the gene expression of annulus fibrosus-derived stem cells. Data Brief 2015, 5, 1007. [Google Scholar] [CrossRef]
- Chu, G.; Yuan, Z.; Zhu, C.; Zhou, P.; Wang, H.; Zhang, W.; Cai, Y.; Zhu, X.; Yang, H.; Li, B. Substrate stiffness- and topography-dependent differentiation of annulus fibrosus-derived stem cells is regulated by Yes-associated protein. Acta Biomater. 2019, 92, 254–264. [Google Scholar] [CrossRef]
- Vernengo, A.J.; Grad, S.; Eglin, D.; Alini, M.; Li, Z. Bioprinting Tissue Analogues with Decellularized Extracellular Matrix Bioink for Regeneration and Tissue Models of Cartilage and Intervertebral Discs. Adv. Funct. Mater. 2020, 30, 1909044. [Google Scholar] [CrossRef]
- Vadalà, G.; Mozetic, P.; Rainer, A.; Centola, M.; Loppini, M.; Trombetta, M.; Denaro, V. Bioactive electrospun scaffold for annulus fibrosus repair and regeneration. Eur. Spine J. 2012, 21 (Suppl. 1), S20–S26. [Google Scholar] [CrossRef] [PubMed]
- Thorvaldsson, A.; Silva-Correia, J.; Oliveira, J.M.; Reis, R.L.; Gatenholm, P.; Walkenström, P. Development of nanofiber-reinforced hydrogel scaffolds for nucleus pulposus regeneration by a combination of electrospinning and spraying technique. J. Appl. Polym. Sci. 2013, 128, 1158–1163. [Google Scholar] [CrossRef]
- Choy, A.T.H.; Chan, B.P. A structurally and functionally biomimetic biphasic scaffold for intervertebral disc tissue engineering. PLoS ONE 2015, 10, e0131827. [Google Scholar] [CrossRef] [PubMed]
- Bowles, R.D.; Setton, L.A. Biomaterials for intervertebral disc regeneration and repair. Biomaterials 2017, 129, 54–67. [Google Scholar] [CrossRef] [PubMed]
- Moriguchi, Y.; Borde, B.; Grunert, P.; Khair, T.; Hudson, K.; Alimi, M.; Bonassar, L.; Hartl, R. Annular Repair Using High-Density Collagen Gels Seeded with Fibrochondrocytes: In Vivo Outcome in the Rodent Spine. Spine J. 2015, 15, S187–S188. [Google Scholar] [CrossRef]
- Moriguchi, Y.; Mojica-Santiago, J.; Grunert, P.; Pennicooke, B.; Berlin, C.; Khair, T.; Navarro-Ramirez, R.; Ricart Arbona, R.J.; Nguyen, J.; Härtl, R.; et al. Total disc replacement using tissue-engineered intervertebral discs in the canine cervical spine. PLoS ONE 2017, 12, e0185716. [Google Scholar] [CrossRef]
- Murphy, S.V.; Atala, A. 3D bioprinting of tissues and organs. Nat. Biotechnol. 2014, 32, 773–785. [Google Scholar] [CrossRef]
- Groll, J.; Burdick, J.A.; Cho, D.W.; Derby, B.; Gelinsky, M.; Heilshorn, S.C.; Jüngst, T.; Malda, J.; Mironov, V.A.; Nakayama, K.; et al. A definition of bioinks and their distinction from biomaterial inks. Biofabrication 2019, 11, 013001. [Google Scholar] [CrossRef]
- Hospodiuk, M.; Dey, M.; Sosnoski, D.; Ozbolat, I.T. The bioink: A comprehensive review on bioprintable materials. Biotechnol. Adv. 2017, 35, 217–239. [Google Scholar] [CrossRef]
- Vanaei, S.; Parizi, M.S.; Vanaei, S.; Salemizadehparizi, F.; Vanaei, H.R. An Overview on Materials and Techniques in 3D Bioprinting Toward Biomedical Application. Eng. Regen. 2021, 2, 1–18. [Google Scholar] [CrossRef]
- Shiwarski, D.J.; Hudson, A.R.; Tashman, J.W.; Feinberg, A.W. Emergence of FRESH 3D printing as a platform for advanced tissue biofabrication. APL Bioeng. 2021, 5, 10904. [Google Scholar] [CrossRef] [PubMed]
- Moxon, S.; Grover, L.M.; Smith, A. Bioprinting multilayered hydrogels using 3D suspended manufacturing. Front. Bioeng. Biotechnol. 2016, 2928. [Google Scholar] [CrossRef]
- Moxon, S.R.; Corbett, N.J.; Fisher, K.; Potjewyd, G.; Domingos, M.; Hooper, N.M. Blended alginate/collagen hydrogels promote neurogenesis and neuronal maturation. Mater. Sci. Eng. C 2019, 104, 109904. [Google Scholar] [CrossRef] [PubMed]
- Potjewyd, G.; Moxon, S.; Wang, T.; Domingos, M.; Hooper, N.M. Tissue Engineering 3D Neurovascular Units: A Biomaterials and Bioprinting Perspective. Trends Biotechnol. 2018, 36, 457–472. [Google Scholar] [CrossRef] [PubMed]
- Senior, J.J.; Cooke, M.E.; Grover, L.M.; Smith, A.M. Fabrication of Complex Hydrogel Structures Using Suspended Layer Additive Manufacturing (SLAM). Adv. Funct. Mater. 2019, 29, 1904845. [Google Scholar] [CrossRef]
- De Pieri, A.; Byerley, A.M.; Musumeci, C.R.; Salemizadehparizi, F.; Vanderhorst, M.A.; Wuertz-Kozak, K. Electrospinning and 3D bioprinting for intervertebral disc tissue engineering. JOR Spine 2020, 3, e1117. [Google Scholar] [CrossRef]
- Sun, B.; Lian, M.; Han, Y.; Mo, X.; Jiang, W.; Qiao, Z.; Dai, K. A 3D-Bioprinted dual growth factor-releasing intervertebral disc scaffold induces nucleus pulposus and annulus fibrosus reconstruction. Bioact. Mater. 2021, 6, 179–190. [Google Scholar] [CrossRef]
- Hu, D.; Wu, D.; Huang, L.; Jiao, Y.; Li, L.; Lu, L.; Zhou, C. 3D bioprinting of cell-laden scaffolds for intervertebral disc regeneration. Mater. Lett. 2018, 223, 219–222. [Google Scholar] [CrossRef]
- Zechuan, Y.; Chunde, L.I.; Haolin, S. Research advances of three-dimension printing technology in vertebrae and intervertebral disc tissue engineering. Zhejiang Da Xue Xue Bao Yi Xue Ban 2016, 45, 141–146. [Google Scholar]
- Zhang, F.; Liu, J.T.; Wang, R.; Lu, T.; Niu, B.B.; Qie, J.; Cai, X.; Zhang, T.; Ouyang, P.R.; He, X.J. Establishment of the model of goat lumbar spinal fusion by 3D printing technology and experimental perioperative management. Zhongguo Gu Shang = China J. Orthop. Traumatol. 2018, 31, 458–464. [Google Scholar]
- Zhu, M.; Tan, J.; Liu, L.; Tian, J.; Li, L.; Luo, B.; Zhou, C.; Lu, L. Construction of biomimetic artificial intervertebral disc scaffold via 3D printing and electrospinning. Mater. Sci. Eng. C 2021, 128, 112310. [Google Scholar] [CrossRef] [PubMed]
- Oner, T.; Cengiz, I.F.; Pitikakis, M.; Cesario, L.; Parascandolo, P.; Vosilla, L.; Viano, G.; Oliveira, J.M.; Reis, R.L.; Silva-Correia, J. 3D segmentation of intervertebral discs: From concept to the fabrication of patient-specific scaffolds. J. 3D Print. Med. 2017, 1, 91–101. [Google Scholar] [CrossRef]
- Wu, D.; Tan, J.; Yao, L.; Tian, J.; Luo, B.; Li, L.; Zhou, C.; Lu, L. Customized composite intervertebral disc scaffolds by integrated 3D bioprinting for therapeutic implantation. Compos. Part A Appl. Sci. Manuf. 2021, 147, 106468. [Google Scholar] [CrossRef]
- Rosenzweig, D.H.; Carelli, E.; Steffen, T.; Jarzem, P.; Haglund, L. 3D-printed ABS and PLA scaffolds for cartilage and nucleus pulposustissue regeneration. Int. J. Mol. Sci. 2015, 16, 15118–15135. [Google Scholar] [CrossRef] [PubMed]
- Cheng, H.W.; Luk, K.D.K.; Cheung, K.M.C.; Chan, B.P. In vitro generation of an osteochondral interface from mesenchymal stem cell–collagen microspheres. Biomaterials 2011, 32, 1526–1535. [Google Scholar] [CrossRef] [PubMed]
- Chik, T.K.; Chooi, W.H.; Li, Y.Y.; Ho, F.C.; Cheng, H.W.; Choy, T.H.; Sze, K.Y.; Luk, K.K.D.; Cheung, K.M.C.; Chan, B.P. Bioengineering a Multicomponent Spinal Motion Segment Construct—A 3D Model for Complex Tissue Engineering. Adv. Healthc. Mater. 2015, 4, 99–112. [Google Scholar] [CrossRef] [PubMed]
- Afghah, F.; Dikyol, C.; Altunbek, M.; Koc, B. Biomimicry in Bio-Manufacturing: Developments in Melt Electrospinning Writing Technology Towards Hybrid Biomanufacturing. Appl. Sci. 2019, 9, 3540. [Google Scholar] [CrossRef]
- de Ruijter, M.; Ribeiro, A.; Dokter, I.; Castilho, M.; Malda, J. Simultaneous Micropatterning of Fibrous Meshes and Bioinks for the Fabrication of Living Tissue Constructs. Adv. Healthc. Mater. 2019, 8, 1800418. [Google Scholar] [CrossRef]
- Hrynevich, A.; Haigh, J.N.; McMaster, R.; Youssef, A.; Blum, C.; Blunk, T.; Hochleitner, G.; Groll, J.; Dalton, P.D. Dimension-Based Design of Melt Electrowritten Scaffolds. Small 2018, 14, 1800232. [Google Scholar] [CrossRef]
- Bas, O.; Lucarotti, S.; Angella, D.D.; Castro, N.J.; Meinert, C.; Wunner, F.M.; Rank, E.; Vozzi, G.; Klein, T.J.; Catelas, I.; et al. Rational design and fabrication of multiphasic soft network composites for tissue engineering articular cartilage: A numerical model-based approach. Chem. Eng. J. 2018, 340, 15–23. [Google Scholar] [CrossRef]
- Castilho, M.; Mouser, V.; Chen, M.; Malda, J.; Ito, K. Bi-layered micro-fibre reinforced hydrogels for articular cartilage regeneration. Acta Biomater. 2019, 95, 297–306. [Google Scholar] [CrossRef] [PubMed]
- Visser, J.; Melchels, F.P.W.; Jeon, J.E.; Van Bussel, E.M.; Kimpton, L.S.; Byrne, H.M.; Dhert, W.J.A.; Dalton, P.D.; Hutmacher, D.W.; Malda, J. Reinforcement of hydrogels using three-dimensionally printed microfibres. Nat. Commun. 2015, 6, 6933. [Google Scholar] [CrossRef]
- Bas, O.; De-Juan-Pardo, E.M.; Meinert, C.; D’Angella, D.; Baldwin, J.G.; Bray, L.J.; Wellard, R.M.; Kollmannsberger, S.; Rank, E.; Werner, C.; et al. Biofabricated soft network composites for cartilage tissue engineering. Biofabrication 2017, 9, 025014. [Google Scholar] [CrossRef] [PubMed]
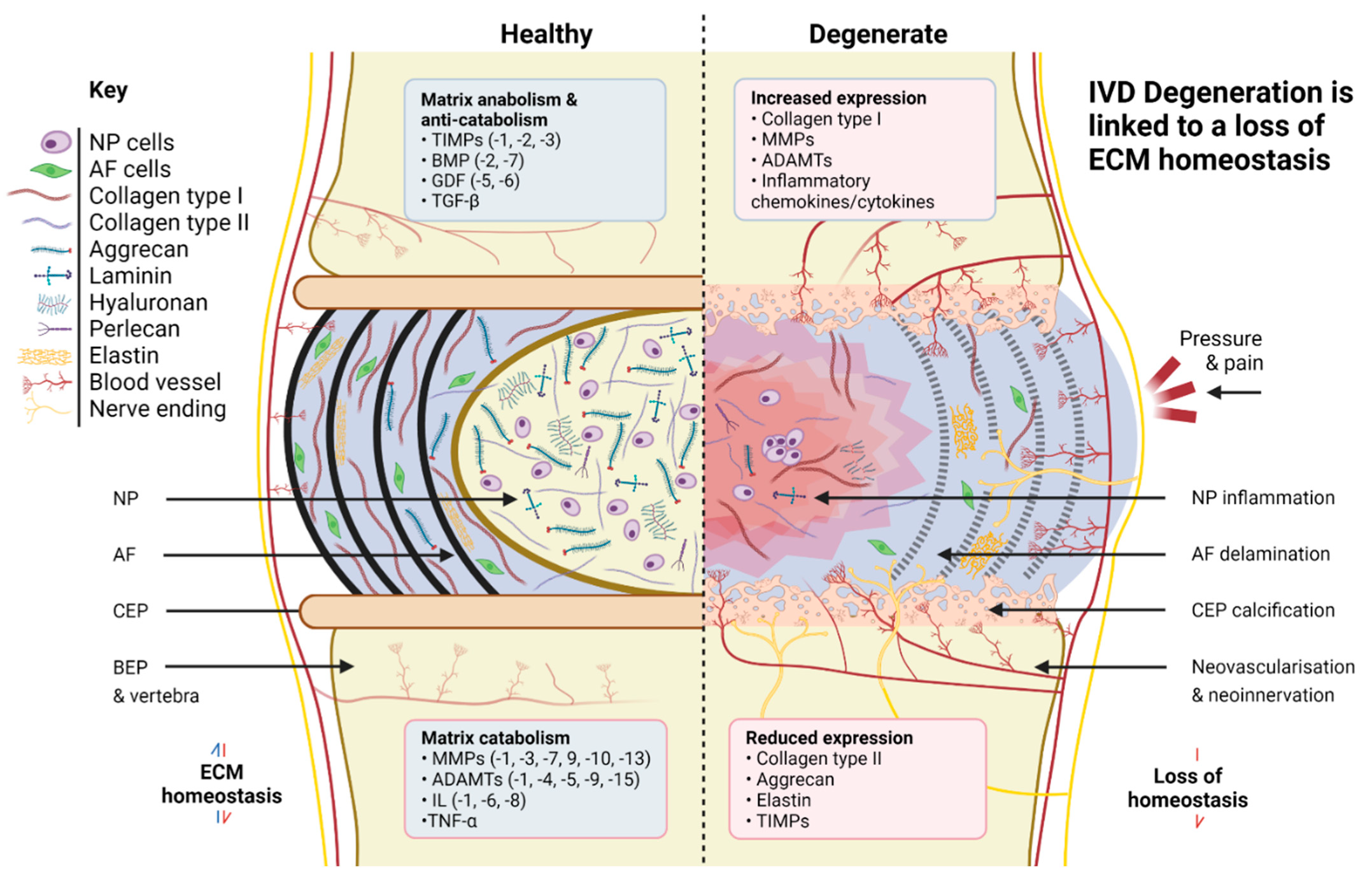
| Tissue | Matrix Component | Relative Composition (Dry Weight) | Structural/Biological Effects |
|---|---|---|---|
| NP | Collagen (esp. type II) | 5–20% | Confine hydrating proteoglycans within NP matrix. Modulation of cellular metabolism and extracellular signalling. |
| Proteoglycans (esp. aggrecan, versican, biglycan) | 35–65% | Generate swelling pressure; influence expression of NP cytoskeletal elements and matrix anabolism/catabolism during compression, particularly collagen fibrillogenesis. | |
| Non-collagenous proteins (esp. laminin) | 15–60% | Play a key role in matrix organisation through interaction with integrins. | |
| AF | Collagen (esp. type I) | 50–70% | Fibre orientation and composition ratio influences biomechanics and matrix production within IAF/OAF. |
| Proteoglycans (esp. aggrecan, versican, decorin) | 10–20% | Generate swelling pressure; influence expression of AF cytoskeletal elements and matrix anabolism/catabolism during tension and shear; regulate matrix assembly and repair following damage. | |
| Non-collagenous proteins (esp. elastin) | 10–40% | Support development of elastic matrix and enable collagen fibre recovery after deformation. |
| Source | Method | Matrix-Related Genes/Proteins Investigated | References |
|---|---|---|---|
| Transcriptomic | |||
| Foetal/notochord | Microarray analysis | Identified CD24, IGF1 and eight other notochord-specific markers, plus molecules involved in inhibiting vascularisation (WISP2, Noggin, and EDN2) and inflammation (IL1-RN). | [105] |
| Foetal/notochord | scRNA-seq | Identified eight drivers of notochordal differentiation: PAX6, GDF3, FOXD3, TDGF1, SOX5, LMX1A, LEFTY1, and LEFTY2. | [109] |
| Young/healthy NP | Microarray analysis | Identified marker genes including PAX1, FOXF1, HBB, CA12, and OVOS2 for NP; GDF10, CYTL1, IBSP, and FBLN1 for articular chondrocytes. | [129] |
| Young/healthy NP and AF | scRNA-seq | Higher expression of COL2A1, COL9A3, and COL11A1 in NP. Signature transcription factor for NP (KDM4E) and AF (FOXM1) identified. | [130] |
| Young/healthy NP, AF, and CEP | scRNA-seq | Identified progenitor IVD cell markers plus PDGF and TGFβ cascades important for regulating NP microenvironment. | [131] |
| Young/healthy and degenerate NP, IAF, and OAF | Microarray analysis | Overall, showed relative enrichment of COL5A1, SERPINA5, and MXRA5 in IAF; LAMB2, THBS1, and CTSD in OAF. Identified that clearest transition in proteomic signature is between ECM of OAF and IAF, not between IAF and NP. | [9] |
| Degenerate NP | RNA-seq | Used integrin- and syndecan-binding laminin-mimetic peptides to upregulate 148 genes, including NP markers (Noggin and ITGA6), and downregulate 277 genes, including known fibroblastic markers linked to matrix catabolism (CTGF). | [132] |
| Degenerate NP and AF | RNA-seq | High expression of genes encoding proteoglycan-rich ECM and TGF superfamily signalling pathways in NP (GPC6, INHBA, INHA); fibrous, vascular matrix and WNT/NOTCH signalling in AF (COL1/4/6, VEGFC, and JAG1/2). | [133] |
| Immortalised NP and AF cell lines | Microarray analysis | Identified membrane-associated genes for cellular subtypes, including CLDN11, TMEFF2, EFNA1 and NETO2 for NP; COLEC12, LPAR1, and CHIC1 for AF. Indicated that regulation of WNT signalling separates AF from NP cells. | [50] |
| Proteomic | |||
| Foetal NP | LC-MS/MS | Identified 1316 proteins, 1096 of them unique, and 10 significant protein clusters including collagens, SLRPs, and matrilins. Highly expressed COL14A1 identified for the first time. | [134] |
| Foetal/notochord and degenerate NP | LC-MS/MS | Identified 12 degeneration-linked proteins including interleukin-11, LTA, ECM1, and matrilin-3. | [135] |
| Foetal/notochord, young/healthy, and degenerate NP | ESI–LC–MS/MS | Identified ten ECM regulators and ECM affiliated proteins of interest, including four (P4HA1, PLOD1/2, and SERPINH1) involved in collagen biosynthesis. | [136] |
| Young/healthy and degenerate AF | MS and silver-stained 2-D electrophoresis gels | Degeneration led to decreases in three proteins and increases in seven, suggesting possible degenerative biomarkers and loss of cell adhesion ability. | [137] |
| Young/healthy NP and AF | LC-MS/MS and iTRAQ analysis | High level of lubricin and low levels of biglycan compared to seven other cartilaginous tissue types. | [138] |
| Young/healthy and degenerate NP and AF | LC-MS/MS and iTRAQ analysis | Increased levels of CILP and CILP2 in NP; HTRA, COMP, and CILP in AF with degeneration. | [139] |
| Young/healthy IVDs | Peptide location fingering | Indicated age-related structural differences in over one hundred ECM-associated proteins including COMP, CILP, CILP2, and LRP1. Regionally specific variations in collagen type II and type V, and aggrecan across ages. | [128] |
| Young/healthy and degenerate IVDs | LC-MS/MS | Observed reduction in structural and other matrix proteins including COL2A1, KRT, BGN, VCAN, and DCN with degeneration. | [140] |
| Degenerate NP and AF | FTMS/ITMSMS and iTRAQ analysis | Fifty-four and seventy-three proteins differentially regulated in NP and AF, including integrin-mediated cell adhesion pathways. | [141] |
| Bone marrow-derived stem cells (BMSCs) exposed to young/healthy and degenerate IVD environment | LC-MS/MS | Altered regulation of 224 and 223 proteins following exposure to healthy or degenerate IVD microenvironments compared to baseline secretome. Following trauma, MMP and IL production observed; however, CTGF, LTBP2, and TIMP1 were also recorded, indicating attempted inhibition of matrix degradation and inducement of NP cell growth and matrix production. | [142] |
| Metabolomic | |||
| DegeneraH HR MAS NMR te NP and AF | 1H HR MAS NMR spectroscopy | Correlation between degree of degeneration and metabolites including glycine and hydroxyproline, associated with significant collagen breakdown. Reduced abundance of CS observed in highly degenerate specimens. | [143] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kibble, M.J.; Domingos, M.; Hoyland, J.A.; Richardson, S.M. Importance of Matrix Cues on Intervertebral Disc Development, Degeneration, and Regeneration. Int. J. Mol. Sci. 2022, 23, 6915. https://doi.org/10.3390/ijms23136915
Kibble MJ, Domingos M, Hoyland JA, Richardson SM. Importance of Matrix Cues on Intervertebral Disc Development, Degeneration, and Regeneration. International Journal of Molecular Sciences. 2022; 23(13):6915. https://doi.org/10.3390/ijms23136915
Chicago/Turabian StyleKibble, Matthew J., Marco Domingos, Judith A. Hoyland, and Stephen M. Richardson. 2022. "Importance of Matrix Cues on Intervertebral Disc Development, Degeneration, and Regeneration" International Journal of Molecular Sciences 23, no. 13: 6915. https://doi.org/10.3390/ijms23136915
APA StyleKibble, M. J., Domingos, M., Hoyland, J. A., & Richardson, S. M. (2022). Importance of Matrix Cues on Intervertebral Disc Development, Degeneration, and Regeneration. International Journal of Molecular Sciences, 23(13), 6915. https://doi.org/10.3390/ijms23136915







