Signaling Pathways Used by the Specialized Pro-Resolving Mediator Maresin 2 Regulate Goblet Cell Function: Comparison with Maresin 1
Abstract
1. Introduction
2. Results
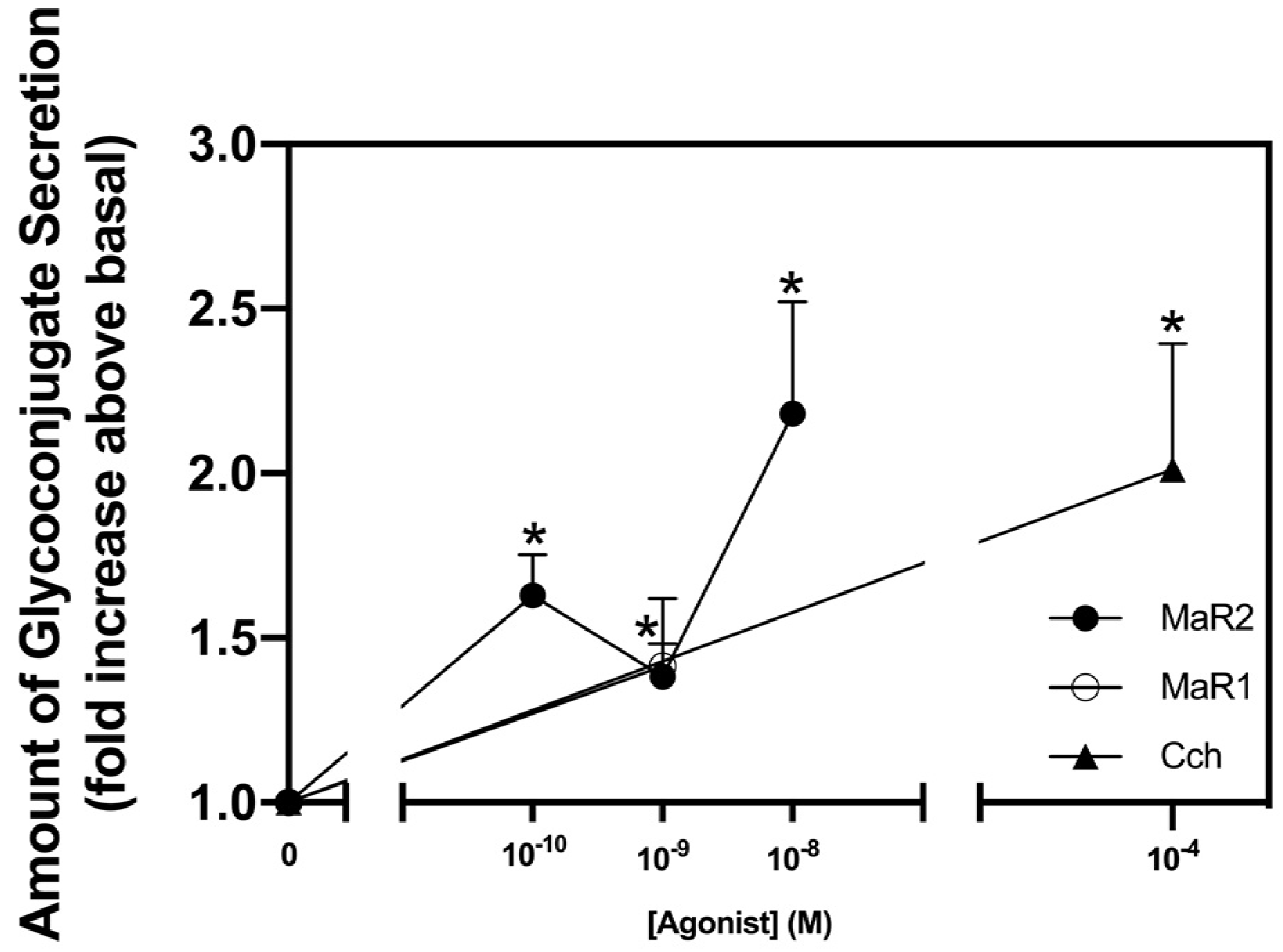
2.1. Maresin 2 Increases Secretion in Rat Conjunctival Goblet Cells
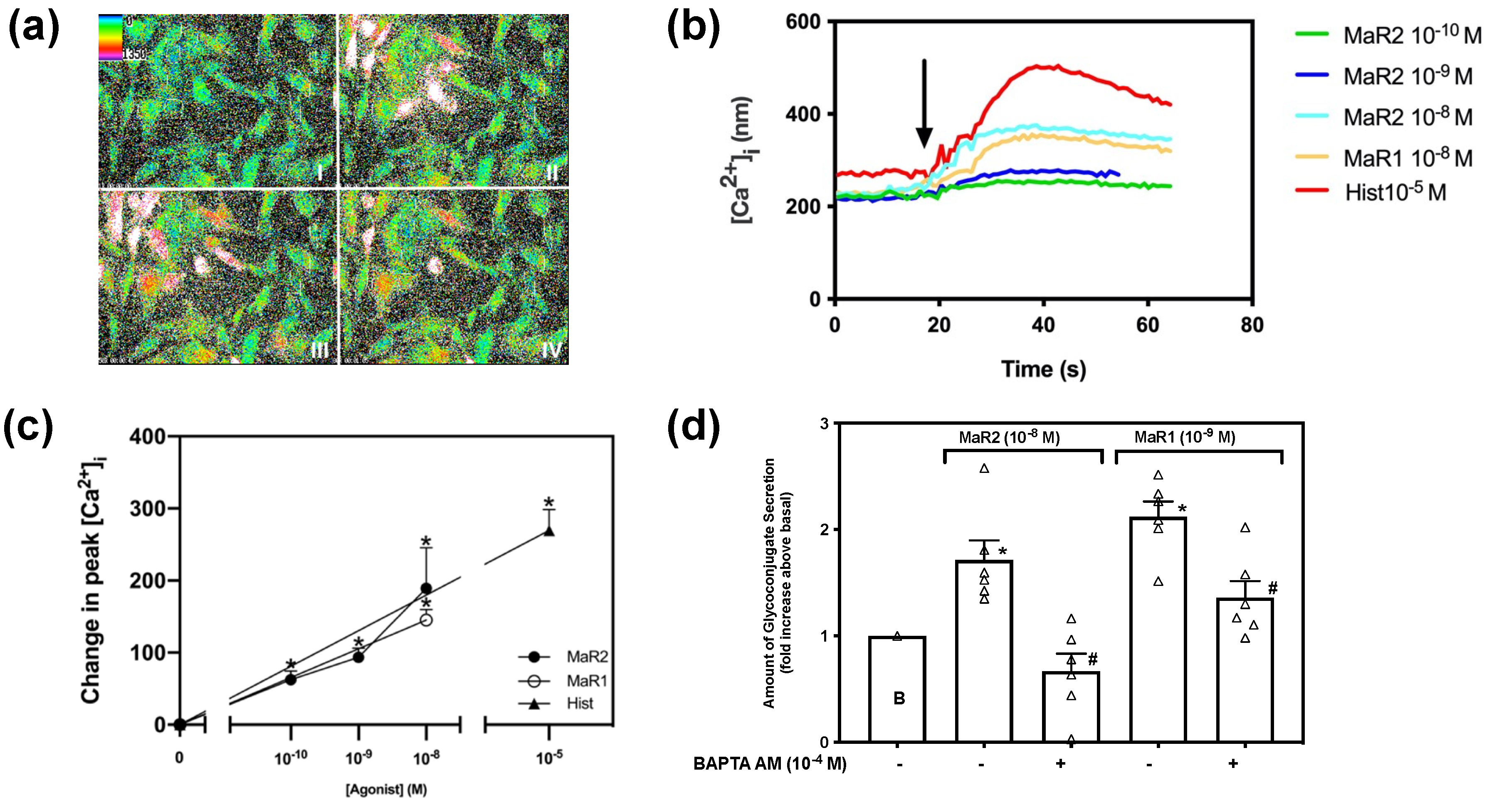
2.2. Maresin 2 Increases [Ca2+]i That Stimulates Secretion in Rat Conjunctival Goblet Cells
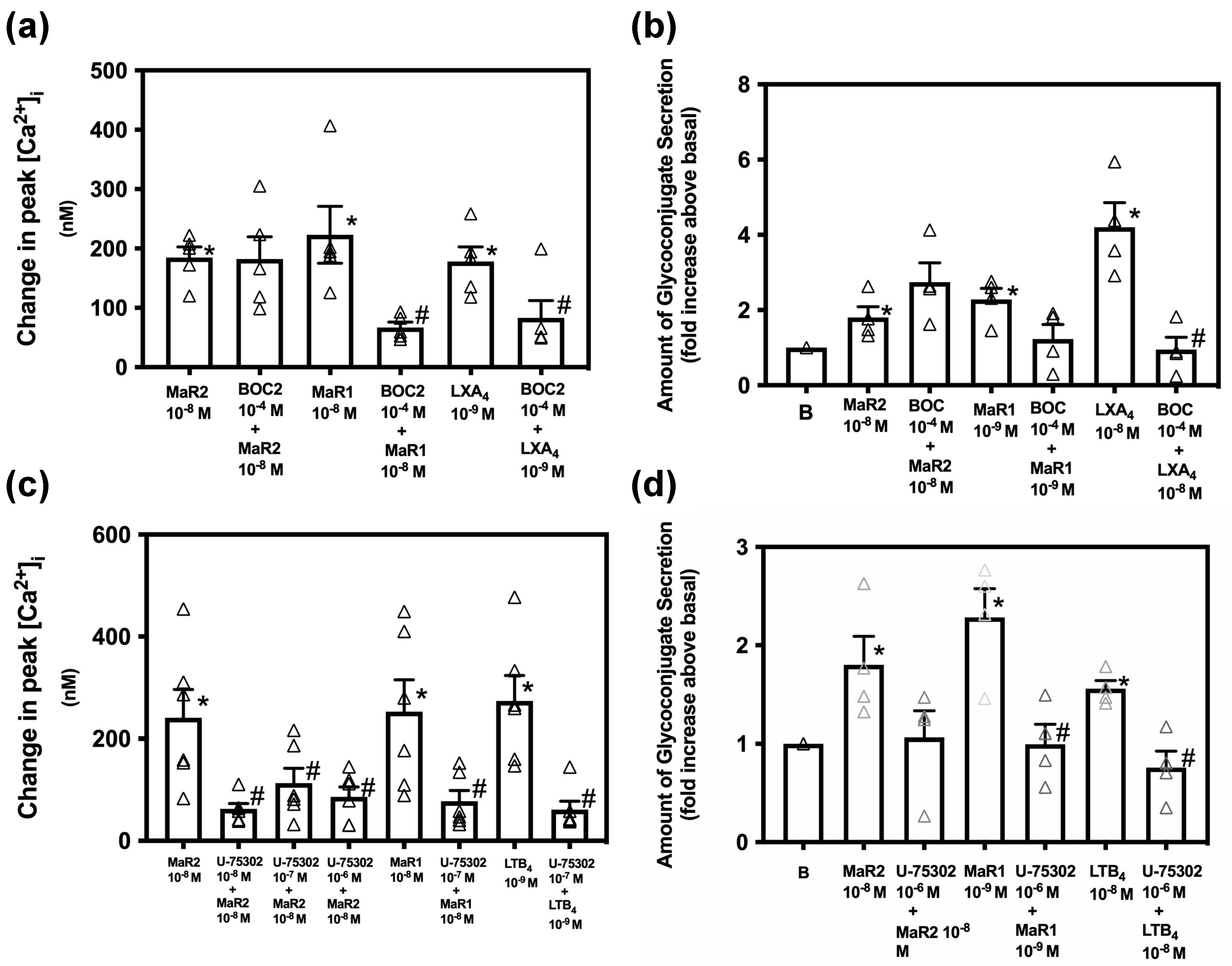
2.3. Maresin 2 Activates the BLT1 Receptor, but Not the ALX/FPR 2 Receptor to Increase [Ca2+]i
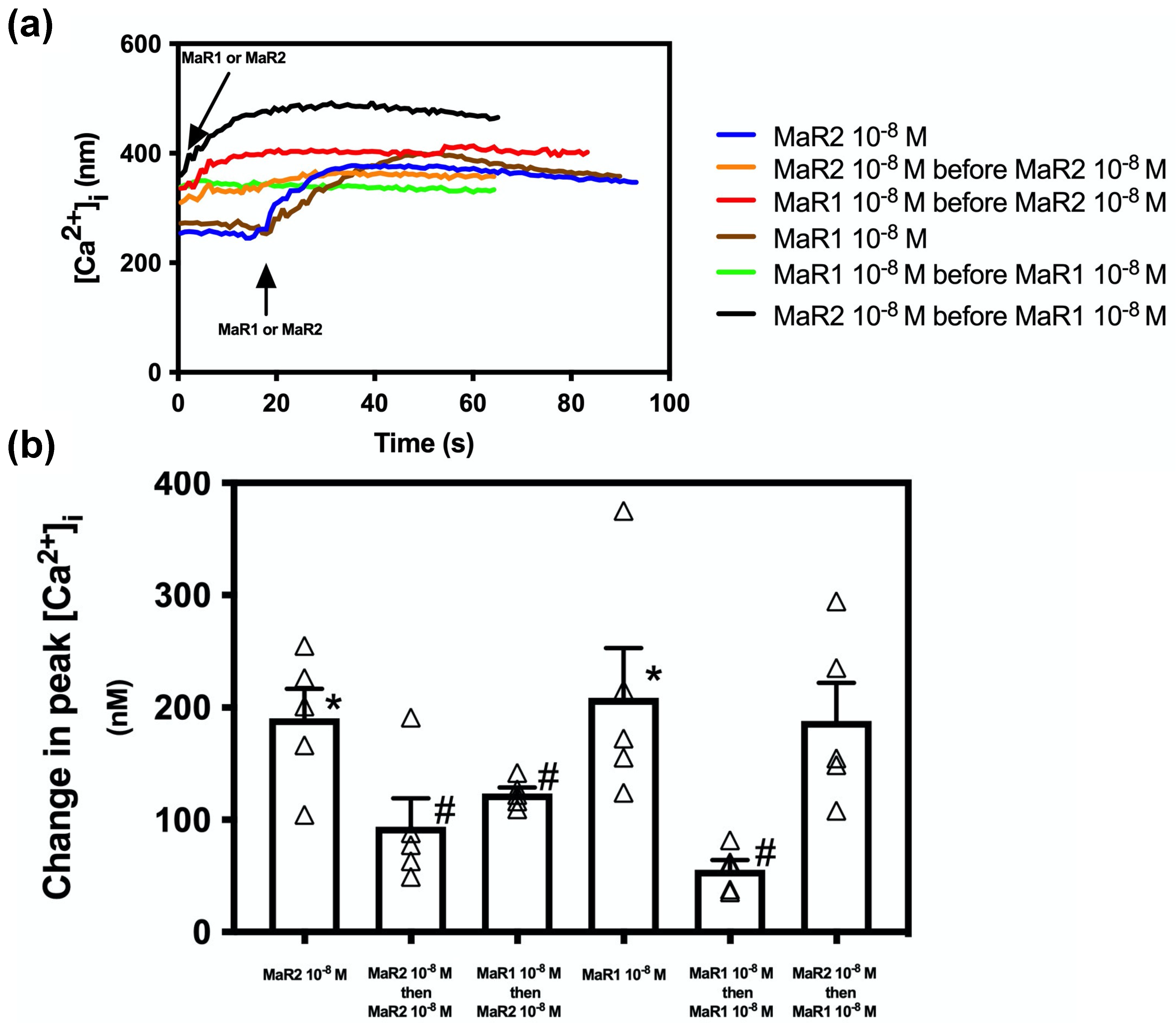
2.4. Maresin 2 Does Not Inhibit Maresin 1 Stimulated Increase in [Ca2+]i, but Maresin 1 Inhibits Maresin 2-Stimulated [Ca2+]i
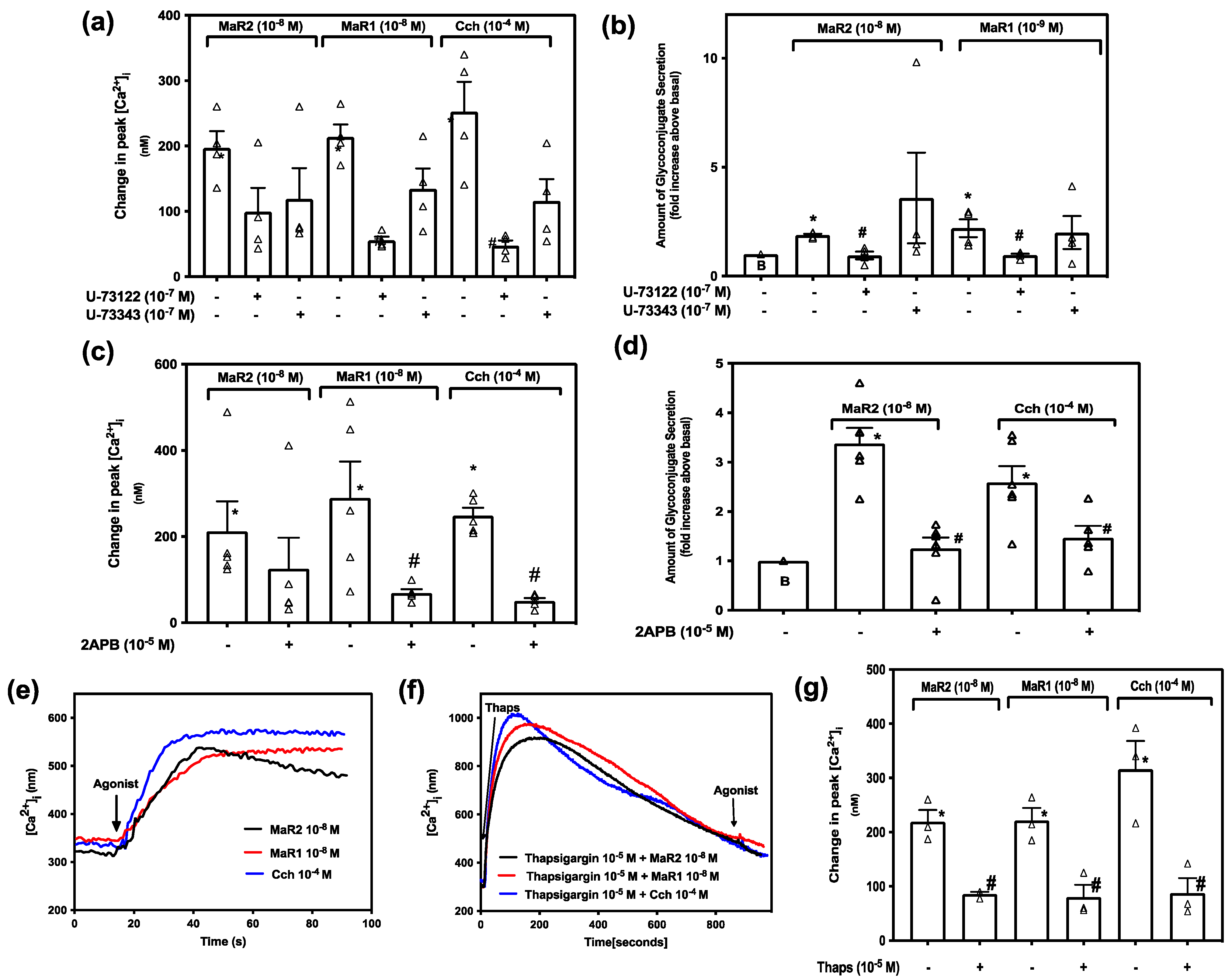
2.5. Maresin 2 Increase in [Ca2+]i, but Not Secretion, Is Independent of the PLC-Pathway in Rat Conjunctival Goblet Cells
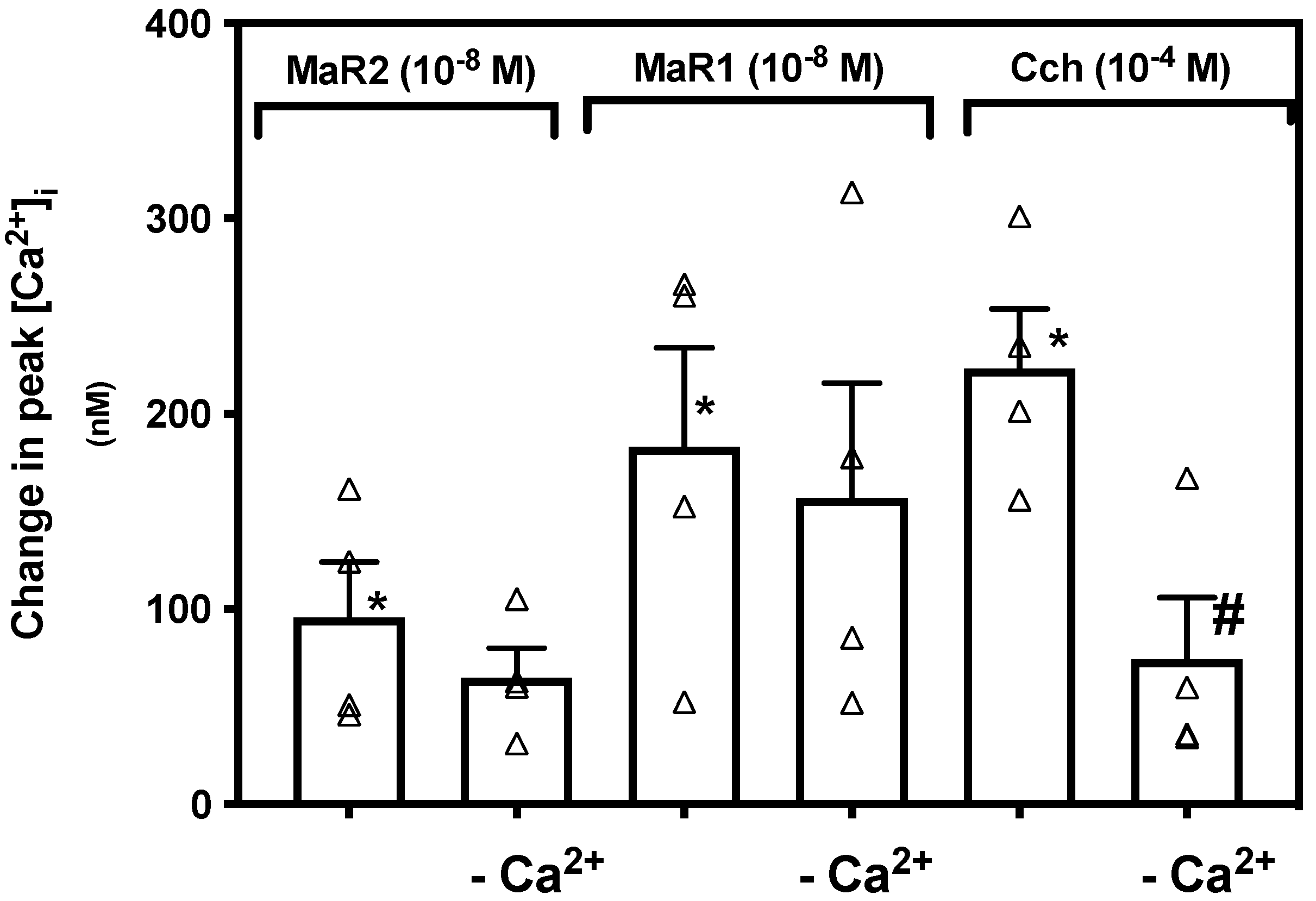
2.6. Maresin 2 Stimulated Increase in [Ca2+]i Is Independent of Extracellular Ca2+ in Rat Conjunctival Goblet Cells
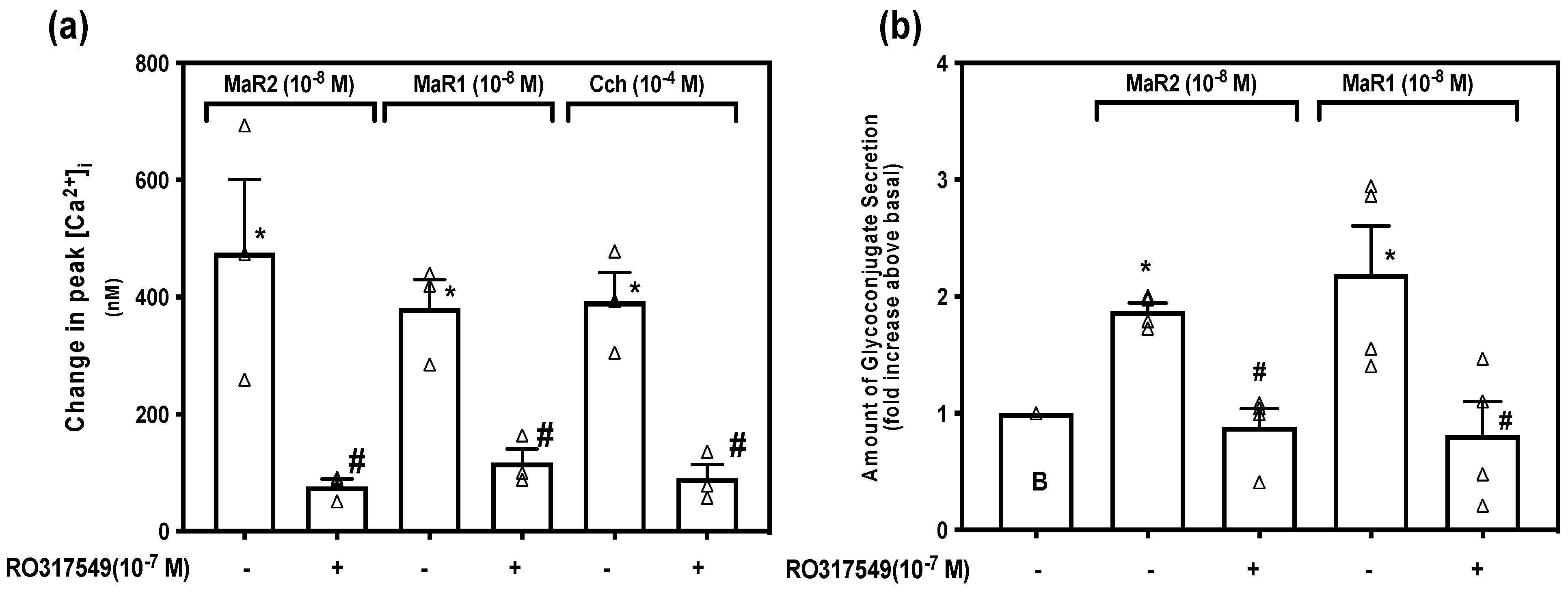
2.7. Maresin 2 Increases [Ca2+]i and Stimulates Secretion by Activation of Protein Kinase C
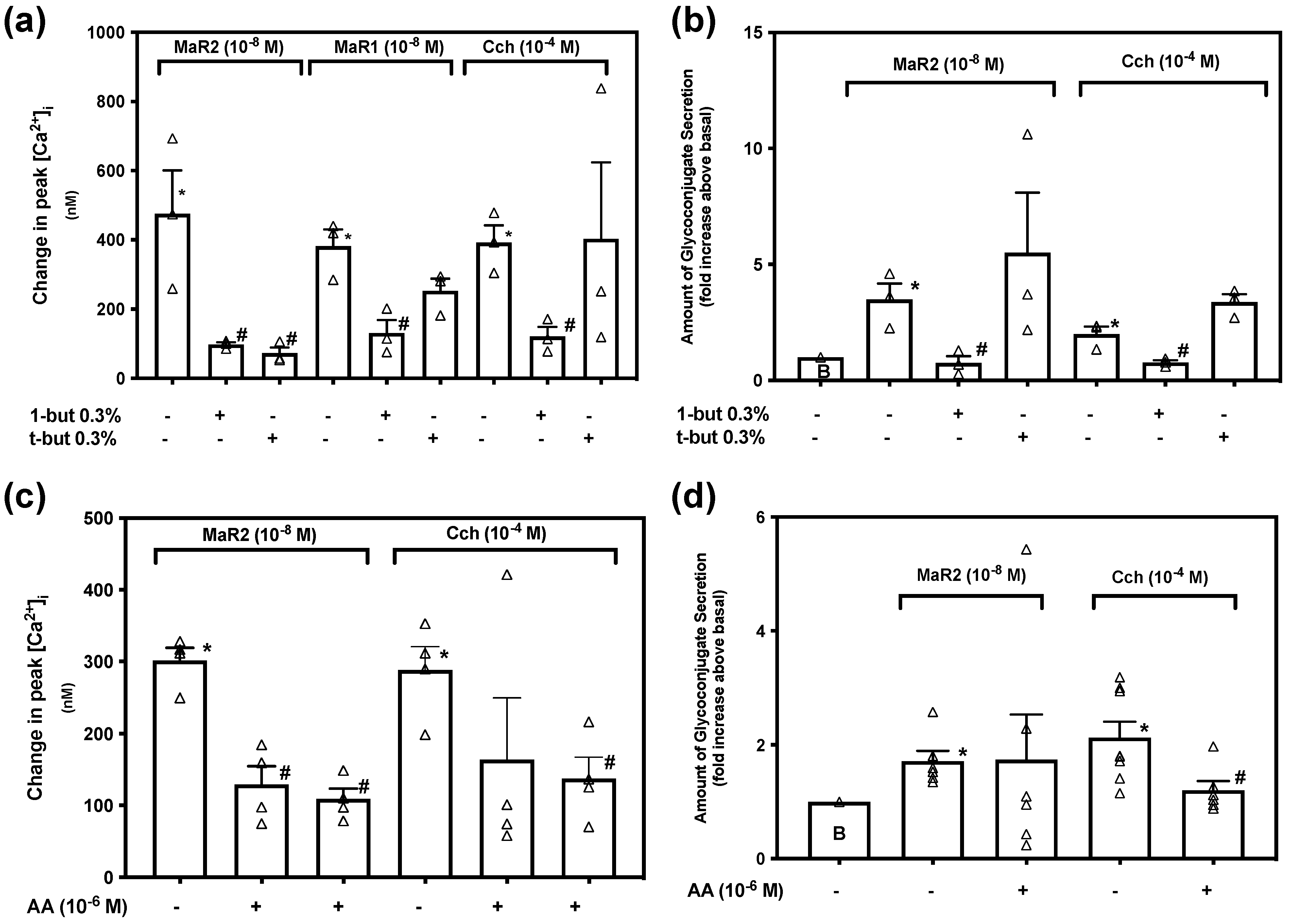
2.8. Maresin 2 Has Different Dependency on Phospholipase D (PLD) Compared to Phospholipase A2 (PLA2) to Increase [Ca2+]i and Stimulate Secretion in Rat Conjunctival Goblet Cells
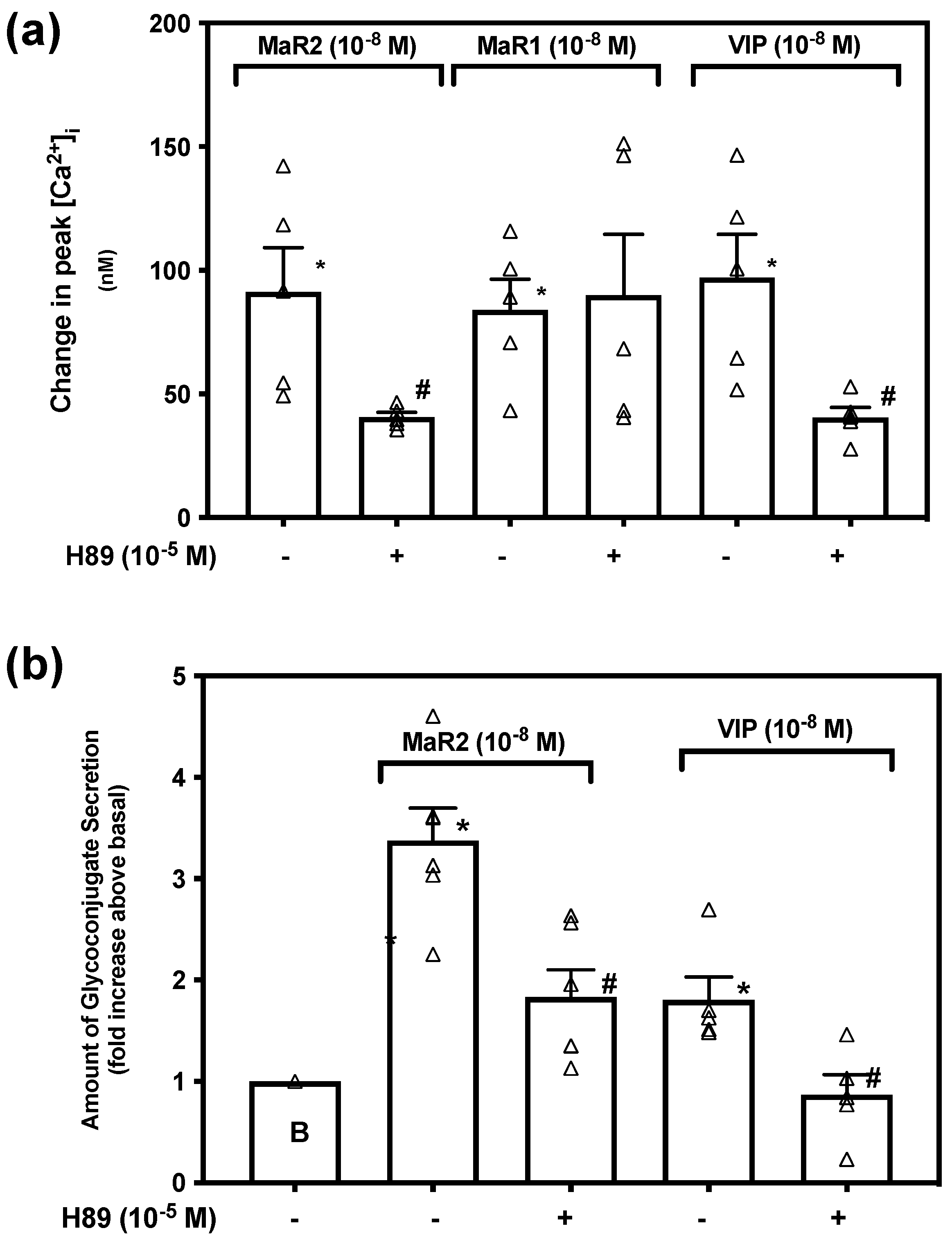
2.9. Maresin 2 Uses Protein Kinase A to Increase [Ca2+]i and Stimulate Secretion in Rat Conjunctival Goblet Cells
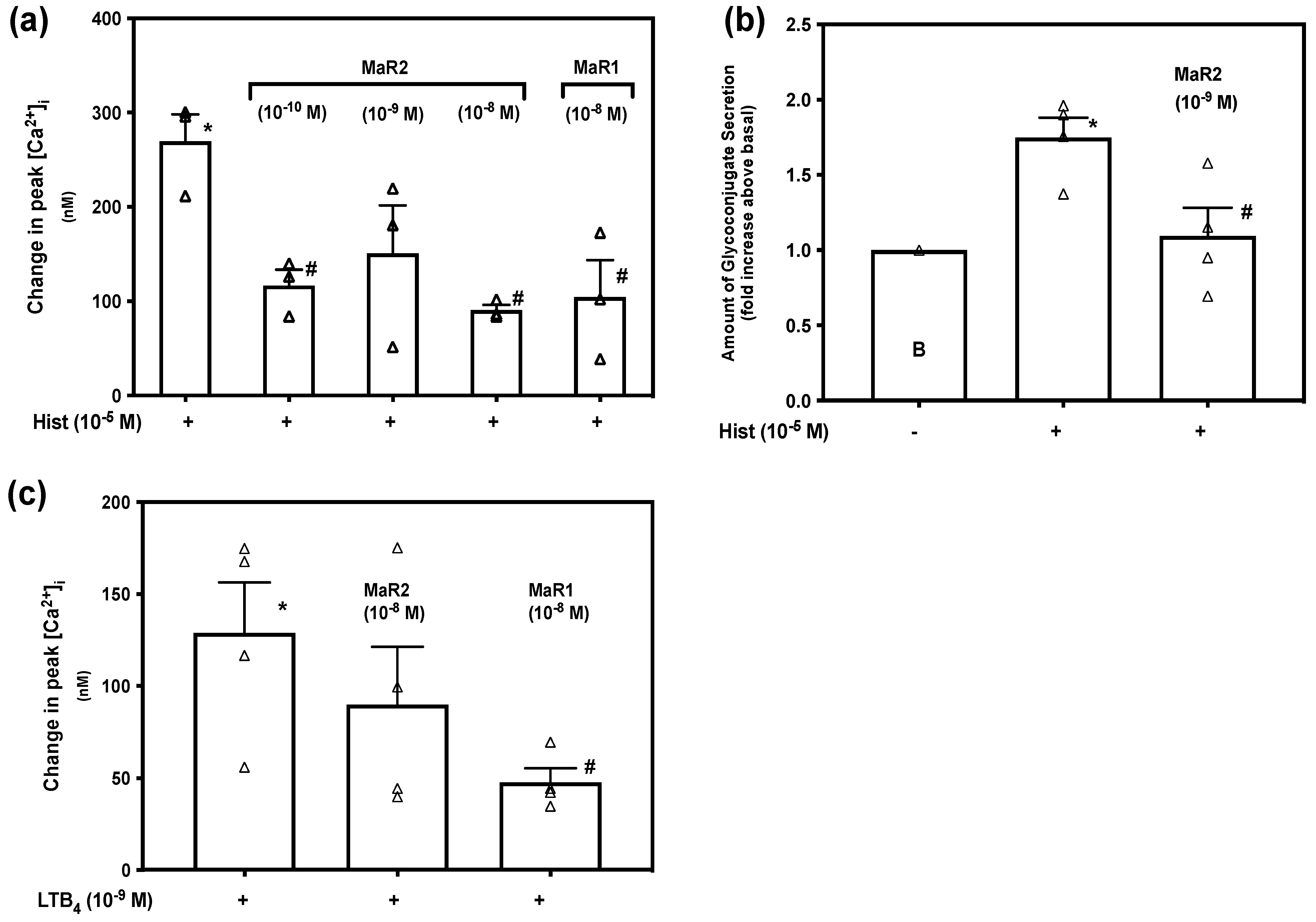
2.10. Maresin 2 Inhibits Histamine-, but Not LTB4-Stimulated Increase in [Ca2+]i and Histamine-Stimulated Glycoconjugate Secretion in Rat Conjunctival Goblet Cells
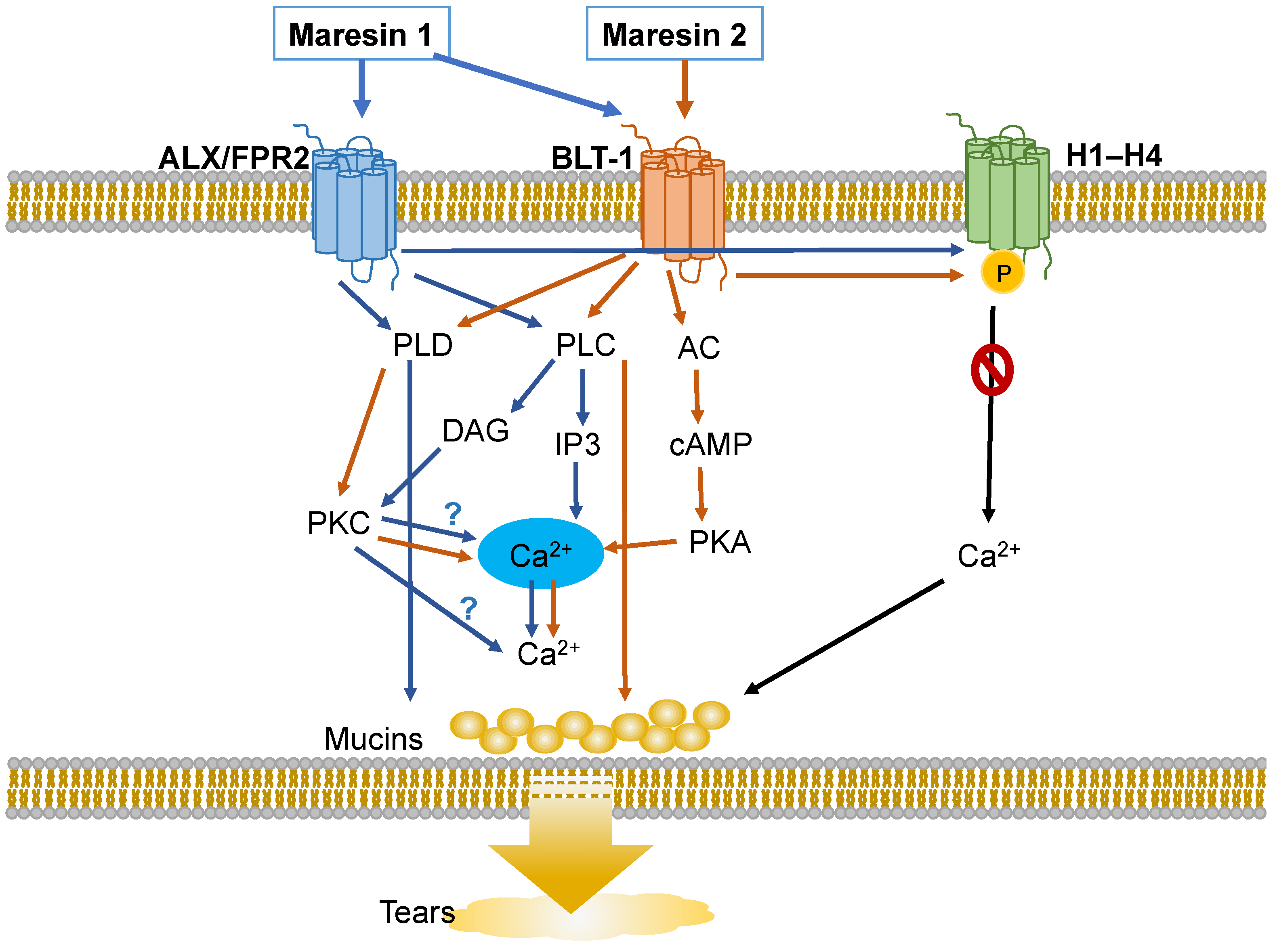
3. Discussion
4. Materials and Methods
4.1. Materials
4.2. Animals
4.3. Cell Culture
4.4. Measurement of [Ca2+]i
4.5. Measurement of High Molecular Weight Glycoconjugate Secretion
4.6. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hodges, R.R.; Dartt, D.A. Tear film mucins: Front line defenders of the ocular surface; comparison with airway and gastrointestinal tract mucins. Exp. Eye Res. 2013, 117, 62–78. [Google Scholar] [CrossRef]
- Dartt, D.A. Control of mucin production by ocular surface epithelial cells. Exp. Eye Res. 2004, 78, 173–185. [Google Scholar] [CrossRef]
- Argueso, P.; Balaram, M.; Spurr-Michaud, S.; Keutmann, H.T.; Dana, M.R.; Gipson, I.K. Decreased levels of the goblet cell mucin MUC5AC in tears of patients with Sjogren syndrome. Investig. Ophthalmol. Vis. Sci. 2002, 43, 1004–1011. [Google Scholar]
- Dogru, M.; Matsumoto, Y.; Okada, N.; Igarashi, A.; Fukagawa, K.; Shimazaki, J.; Tsubota, K.; Fujishima, H. Alterations of the ocular surface epithelial MUC16 and goblet cell MUC5AC in patients with atopic keratoconjunctivitis. Allergy 2008, 63, 1324–1334. [Google Scholar] [CrossRef]
- Zhao, H.; Jumblatt, J.E.; Wood, T.O.; Jumblatt, M.M. Quantification of MUC5AC protein in human tears. Cornea 2001, 20, 873–877. [Google Scholar] [CrossRef]
- Mantelli, F.; Argueso, P. Functions of ocular surface mucins in health and disease. Curr. Opin. Allergy Clin. Immunol. 2008, 8, 477–483. [Google Scholar] [CrossRef]
- Dartt, D.A.; Masli, S. Conjunctival epithelial and goblet cell function in chronic inflammation and ocular allergic inflammation. Curr. Opin. Allergy Clin. Immunol. 2014, 14, 464–470. [Google Scholar] [CrossRef]
- Serhan, C.N.; Petasis, N.A. Resolvins and protectins in inflammation resolution. Chem. Rev. 2011, 111, 5922–5943. [Google Scholar] [CrossRef]
- Serhan, C.N.; Dalli, J.; Colas, R.A.; Winkler, J.W.; Chiang, N. Protectins and maresins: New pro-resolving families of mediators in acute inflammation and resolution bioactive metabolome. Biochim. Biophys. Acta 2015, 1851, 397–413. [Google Scholar] [CrossRef]
- Serhan, C.N.; Krishnamoorthy, S.; Recchiuti, A.; Chiang, N. Novel anti-inflammatory—Pro-resolving mediators and their receptors. Curr. Top. Med. Chem. 2011, 11, 629–647. [Google Scholar] [CrossRef]
- Deng, B.; Wang, C.W.; Arnardottir, H.H.; Li, Y.; Cheng, C.Y.; Dalli, J.; Serhan, C.N. Maresin biosynthesis and identification of maresin 2, a new anti-inflammatory and pro-resolving mediator from human macrophages. PLoS ONE 2014, 9, e102362. [Google Scholar] [CrossRef]
- Serhan, C.N.; Yang, R.; Martinod, K.; Kasuga, K.; Pillai, P.S.; Porter, T.F.; Oh, S.F.; Spite, M. Maresins: Novel macrophage mediators with potent antiinflammatory and proresolving actions. J. Exp. Med. 2009, 206, 15–23. [Google Scholar] [CrossRef]
- Serhan, C.N.; Dalli, J.; Karamnov, S.; Choi, A.; Park, C.K.; Xu, Z.Z.; Ji, R.R.; Zhu, M.; Petasis, N.A. Macrophage proresolving mediator maresin 1 stimulates tissue regeneration and controls pain. FASEB J. Off. Publ. Fed. Am. Soc. Exp. Biol. 2012, 26, 1755–1765. [Google Scholar] [CrossRef]
- Colas, R.A.; Shinohara, M.; Dalli, J.; Chiang, N.; Serhan, C.N. Identification and signature profiles for pro-resolving and inflammatory lipid mediators in human tissue. Am. J. Physiol. Cell Physiol. 2014, 307, C39–C54. [Google Scholar] [CrossRef]
- Olsen, M.V.; Lyngstadaas, A.V.; Bair, J.A.; Hodges, R.R.; Utheim, T.P.; Serhan, C.N.; Dartt, D.A. Maresin 1, a specialized proresolving mediator, stimulates intracellular [Ca(2+)] and secretion in conjunctival goblet cells. J. Cell. Physiol. 2021, 236, 340–353. [Google Scholar] [CrossRef]
- Li, D.; Hodges, R.R.; Jiao, J.; Carozza, R.B.; Shatos, M.A.; Chiang, N.; Serhan, C.N.; Dartt, D.A. Resolvin D1 and aspirin-triggered resolvin D1 regulate histamine-stimulated conjunctival goblet cell secretion. Mucosal Immunol. 2013, 6, 1119–1130. [Google Scholar] [CrossRef]
- Lippestad, M.; Hodges, R.R.; Utheim, T.P.; Serhan, C.N.; Dartt, D.A. Signaling pathways activated by resolvin E1 to stimulate mucin secretion and increase intracellular Ca(2+) in cultured rat conjunctival goblet cells. Exp. Eye Res. 2018, 173, 64–72. [Google Scholar] [CrossRef]
- Lippestad, M.; Hodges, R.R.; Utheim, T.P.; Serhan, C.N.; Dartt, D.A. Resolvin D1 Increases Mucin Secretion in Cultured Rat Conjunctival Goblet Cells via Multiple Signaling Pathways. Investig. Ophthalmol. Vis. Sci. 2017, 58, 4530–4544. [Google Scholar] [CrossRef]
- Hodges, R.R.; Li, D.; Shatos, M.A.; Bair, J.A.; Lippestad, M.; Serhan, C.N.; Dartt, D.A. Lipoxin A4 activates ALX/FPR2 receptor to regulate conjunctival goblet cell secretion. Mucosal Immunol. 2017, 10, 46–57. [Google Scholar] [CrossRef]
- Rios, J.D.; Zoukhri, D.; Rawe, I.M.; Hodges, R.R.; Zieske, J.D.; Dartt, D.A. Immunolocalization of muscarinic and VIP receptor subtypes and their role in stimulating goblet cell secretion. Investig. Ophthalmol. Vis. Sci. 1999, 40, 1102–1111. [Google Scholar]
- Migeotte, I.; Communi, D.; Parmentier, M. Formyl peptide receptors: A promiscuous subfamily of G protein-coupled receptors controlling immune responses. Cytokine Growth Factor Rev. 2006, 17, 501–519. [Google Scholar] [CrossRef] [PubMed]
- Bena, S.; Brancaleone, V.; Wang, J.M.; Perretti, M.; Flower, R.J. Annexin A1 interaction with the FPR2/ALX receptor: Identification of distinct domains and downstream associated signaling. J. Biol. Chem. 2012, 287, 24690–24697. [Google Scholar] [CrossRef] [PubMed]
- Chiang, N.; Serhan, C.N.; Dahlén, S.-E.; Drazen, J.M.; Hay, D.W.P.; Rovati, G.E.; Shimizu, T.; Yokomizo, T.; Brink, C. The lipoxin receptor ALX: Potent ligand-specific and stereoselective actions in vivo. Pharmacol. Rev. 2006, 58, 463–487. [Google Scholar] [CrossRef] [PubMed]
- Scannell, M.; Maderna, P. Lipoxins and annexin-1: Resolution of inflammation and regulation of phagocytosis of apoptotic cells. Sci. World J. 2006, 6, 1555–1573. [Google Scholar] [CrossRef]
- Bae, Y.-S.; Yi, H.J.; Lee, H.-Y.; Jo, E.J.; Kim, J.I.; Lee, T.G.; Ye, R.D.; Kwak, J.-Y.; Ryu, S.H. Differential activation of formyl peptide receptor-like 1 by peptide ligands. J. Immunol. 2003, 171, 6807–6813. [Google Scholar] [CrossRef]
- Lyngstadaas, A.V.; Olsen, M.V.; Bair, J.A.; Hodges, R.R.; Utheim, T.P.; Serhan, C.N.; Dartt, D.A. Pro-Resolving Mediator Annexin A1 Regulates Intracellular Ca(2+) and Mucin Secretion in Cultured Goblet Cells Suggesting a New Use in Inflammatory Conjunctival Diseases. Front. Immunol. 2021, 12, 618653. [Google Scholar] [CrossRef]
- Dartt, D.A.; Hodges, R.R.; Serhan, C.N. Immunoresolvent Resolvin D1 Maintains the Health of the Ocular Surface. Adv. Exp. Med. Biol. 2019, 1161, 13–25. [Google Scholar]
- Yokomizo, T.; Izumi, T.; Chang, K.; Takuwa, Y.; Shimizu, T. A G-protein-coupled receptor for leukotriene B4 that mediates chemotaxis. Nature 1997, 387, 620–624. [Google Scholar] [CrossRef]
- Arita, M.; Ohira, T.; Sun, Y.P.; Elangovan, S.; Chiang, N.; Serhan, C.N. Resolvin E1 selectively interacts with leukotriene B4 receptor BLT1 and ChemR23 to regulate inflammation. J. Immunol. 2007, 178, 3912–3917. [Google Scholar] [CrossRef]
- Berridge, M.J. Inositol trisphosphate and calcium signalling mechanisms. Biochim. Biophys. Acta 2009, 1793, 933–940. [Google Scholar] [CrossRef]
- Billah, M.M. Phospholipase D and cell signaling. Curr. Opin. Immunol. 1993, 5, 114–123. [Google Scholar] [CrossRef]
- Billington, C.K.; Hall, I.P. Novel cAMP signalling paradigms: Therapeutic implications for airway disease. Br. J. Pharmacol. 2012, 166, 401–410. [Google Scholar] [CrossRef] [PubMed]
- Thurmond, R.L.; Gelfand, E.W.; Dunford, P.J. The role of histamine H1 and H4 receptors in allergic inflammation: The search for new antihistamines. Nat. Rev. Drug Discov. 2008, 7, 41–53. [Google Scholar] [CrossRef] [PubMed]
- Li, D.; Carozza, R.B.; Shatos, M.A.; Hodges, R.R.; Dartt, D.A. Effect of histamine on Ca(2+)-dependent signaling pathways in rat conjunctival goblet cells. Investig. Ophthalmol. Vis. Sci. 2012, 53, 6928–6938. [Google Scholar] [CrossRef]
- Alexander, S.P.; Mathie, A.; Peters, J.A. Guide to Receptors and Channels (GRAC), 5th edition. Br. J. Pharmacol. 2011, 164 (Suppl. 1), S1–S2. [Google Scholar] [CrossRef]
- Botten, N.; Hodges, R.R.; Li, D.; Bair, J.A.; Shatos, M.A.; Utheim, T.P.; Serhan, C.N.; Dartt, D.A. Resolvin D2 elevates cAMP to increase intracellular [Ca(2+)] and stimulate secretion from conjunctival goblet cells. FASEB J. Off. Publ. Fed. Am. Soc. Exp. Biol. 2019, 33, 8468–8478. [Google Scholar] [CrossRef]
- Chiang, N.; Libreros, S.; Norris, P.C.; de la Rosa, X.; Serhan, C.N. Maresin 1 activates LGR6 receptor promoting phagocyte immunoresolvent functions. J. Clin. Invest. 2019, 129, 5294–5311. [Google Scholar] [CrossRef]
- Samuelsson, B. Leukotrienes: Mediators of immediate hypersensitivity reactions and inflammation. Science 1983, 220, 568–575. [Google Scholar] [CrossRef]
- Cooray, S.N.; Gobbetti, T.; Montero-Melendez, T.; McArthur, S.; Thompson, D.; Clark, A.J.L.; Flower, R.J.; Perretti, M. Ligand-specific conformational change of the G-protein-coupled receptor ALX/FPR2 determines proresolving functional responses. Proc. Natl. Acad. Sci. USA 2013, 110, 18232–18237. [Google Scholar] [CrossRef]
- Yokomizo, T. Leukotriene B4 receptors: Novel roles in immunological regulations. Adv. Enzym. Regul. 2011, 51, 59–64. [Google Scholar] [CrossRef]
- Li, D.; Jiao, J.; Shatos, M.A.; Hodges, R.R.; Dartt, D.A. Effect of VIP on intracellular [Ca2+], extracellular regulated kinase 1/2, and secretion in cultured rat conjunctival goblet cells. Investig. Ophthalmol. Vis. Sci. 2013, 54, 2872–2884. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Shatos, M.A.; Hodges, R.R.; Oshi, Y.; Bair, J.A.; Zoukhri, D.; Kublin, C.; Lashkari, K.; Dartt, D.A. Role of cPKCalpha and nPKCepsilon in EGF-stimulated goblet cell proliferation. Investig. Ophthalmol. Vis. Sci. 2009, 50, 614–620. [Google Scholar] [CrossRef] [PubMed]
- Yang, M.; Bair, J.A.; Hodges, R.R.; Serhan, C.N.; Dartt, D.A. Resolvin E1 Reduces Leukotriene B4-Induced Intracellular Calcium Increase and Mucin Secretion in Rat Conjunctival Goblet Cells. Am. J. Pathol. 2020, 190, 1823–1832. [Google Scholar] [CrossRef] [PubMed]
- Hodges, R.R.; Li, D.; Shatos, M.A.; Serhan, C.N.; Dartt, D.A. Lipoxin A(4) Counter-regulates Histamine-stimulated Glycoconjugate Secretion in Conjunctival Goblet Cells. Sci. Rep. 2016, 6, 36124. [Google Scholar] [CrossRef]
- Jadapalli, J.K.; Halade, G.V. Unified nexus of macrophages and maresins in cardiac reparative mechanisms. FASEB J. Off. Publ. Fed. Am. Soc. Exp. Biol. 2018, 32, 5227–5237. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Olsen, M.V.; Lyngstadaas, A.V.; Bair, J.A.; Hodges, R.R.; Utheim, T.P.; Serhan, C.N.; Dartt, D.A. Signaling Pathways Used by the Specialized Pro-Resolving Mediator Maresin 2 Regulate Goblet Cell Function: Comparison with Maresin 1. Int. J. Mol. Sci. 2022, 23, 6233. https://doi.org/10.3390/ijms23116233
Olsen MV, Lyngstadaas AV, Bair JA, Hodges RR, Utheim TP, Serhan CN, Dartt DA. Signaling Pathways Used by the Specialized Pro-Resolving Mediator Maresin 2 Regulate Goblet Cell Function: Comparison with Maresin 1. International Journal of Molecular Sciences. 2022; 23(11):6233. https://doi.org/10.3390/ijms23116233
Chicago/Turabian StyleOlsen, Markus V., Anne V. Lyngstadaas, Jeffrey A. Bair, Robin R. Hodges, Tor P. Utheim, Charles N. Serhan, and Darlene A. Dartt. 2022. "Signaling Pathways Used by the Specialized Pro-Resolving Mediator Maresin 2 Regulate Goblet Cell Function: Comparison with Maresin 1" International Journal of Molecular Sciences 23, no. 11: 6233. https://doi.org/10.3390/ijms23116233
APA StyleOlsen, M. V., Lyngstadaas, A. V., Bair, J. A., Hodges, R. R., Utheim, T. P., Serhan, C. N., & Dartt, D. A. (2022). Signaling Pathways Used by the Specialized Pro-Resolving Mediator Maresin 2 Regulate Goblet Cell Function: Comparison with Maresin 1. International Journal of Molecular Sciences, 23(11), 6233. https://doi.org/10.3390/ijms23116233





