Tyrosine Kinase Src Is a Regulatory Factor of Bone Homeostasis
Abstract
1. Introduction
2. Src Function in Osteoclasts and Functional Domains
3. Regulation of Src Activity in Osteoclasts
4. Downstream Proteins of Src in Actin Regulation
4.1. Cortactin
4.2. p130Cas
4.3. Proline-Rich Tyrosine Kinase 2 (Pyk2)
4.4. Casitas B-Lineage Lymphoma Proto-Oncogene (Cbl)
4.5. Vav Guanine Nucleotide Exchange Factor 3 (Vav3)
4.6. Kinesin Family Member 1C (Kif1c)
4.7. Plectin
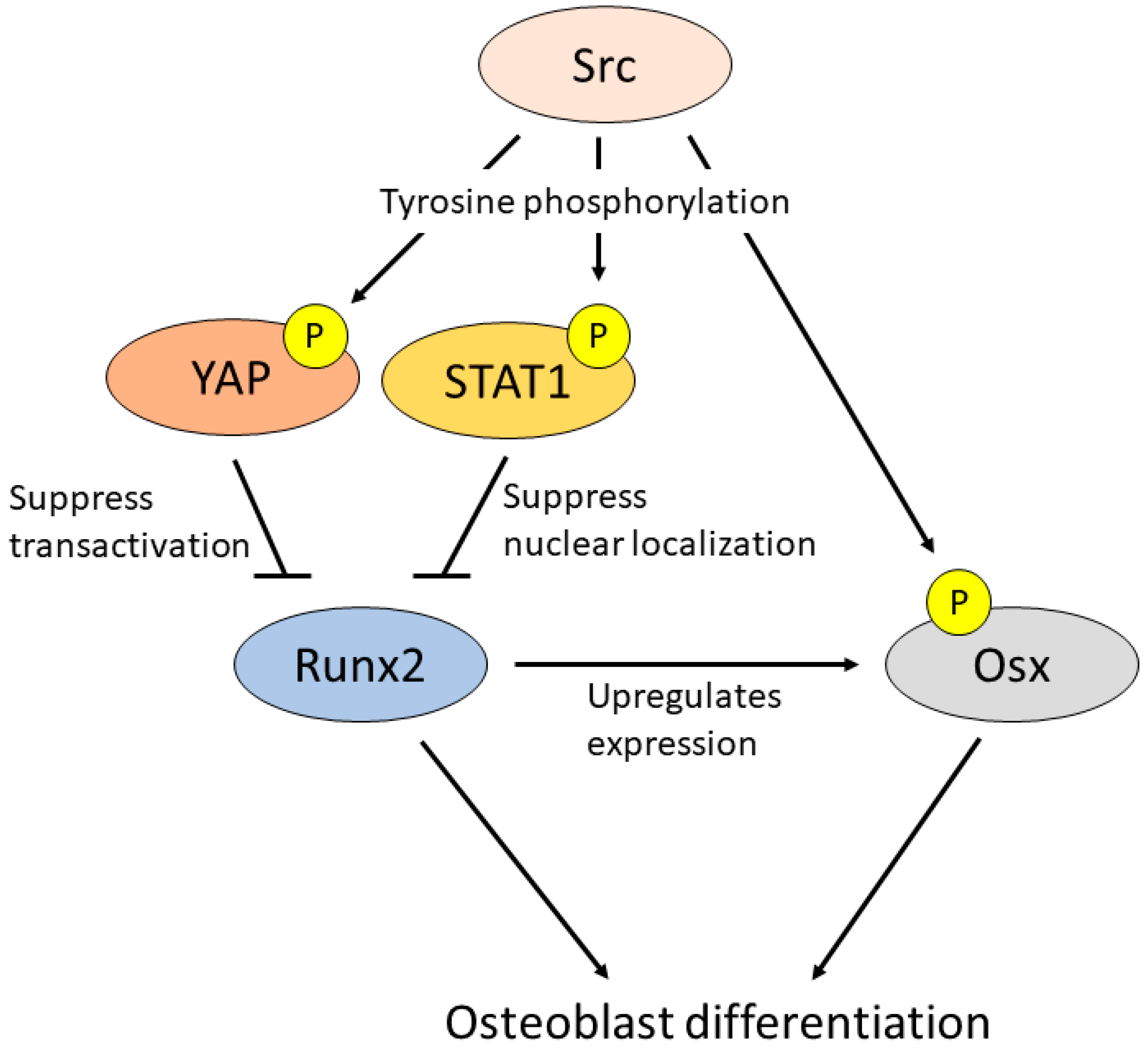
5. Src in Osteoblasts
6. Other Src Family Kinases in Bone Metabolism
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Raggatt, L.J.; Partridge, N.C. Cellular and Molecular Mechanisms of Bone Remodeling. J. Biol. Chem. 2010, 285, 25103–25108. [Google Scholar] [CrossRef] [PubMed]
- Baron, R.; Kneissel, M. WNT Signaling in Bone Homeostasis and Disease: From Human Mutations to Treatments. Nat. Med. 2013, 19, 179–192. [Google Scholar] [CrossRef] [PubMed]
- Boyce, B.; Xing, L. Src Inhibitors in the Treatment of Metastatic Bone Disease: Rationale and Clinical Data. Clin. Investig. 2011, 1, 1695–1706. [Google Scholar] [CrossRef] [PubMed]
- Rachner, T.D.; Khosla, S.; Hofbauer, L.C. Osteoporosis: Now and the Future. Lancet 2011, 377, 1276–1287. [Google Scholar] [CrossRef]
- Takayanagi, H. Osteoimmunology: Shared Mechanisms and Crosstalk between the Immune and Bone Systems. Nat. Rev. Immunol. 2007, 7, 292–304. [Google Scholar] [CrossRef]
- Takahashi, N.; Ejiri, S.; Yanagisawa, S.; Ozawa, H. Regulation of Osteoclast Polarization. Odontology 2007, 95, 1–9. [Google Scholar] [CrossRef]
- Ikeda, F.; Nishimura, R.; Matsubara, T.; Tanaka, S.; Inoue, J.-I.; Reddy, S.V.; Hata, K.; Yamashita, K.; Hiraga, T.; Watanabe, T.; et al. Critical Roles of C-Jun Signaling in Regulation of NFAT Family and RANKL-Regulated Osteoclast Differentiation. J. Clin. Investig. 2004, 114, 475–484. [Google Scholar] [CrossRef]
- Jimi, E.; Takakura, N.; Hiura, F.; Nakamura, I.; Hirata-Tsuchiya, S. The Role of NF-ΚB in Physiological Bone Development and Inflammatory Bone Diseases: Is NF-ΚB Inhibition “Killing Two Birds with One Stone”? Cells 2019, 8, 1636. [Google Scholar] [CrossRef]
- Yasuda, K.; Matsubara, T.; Shirakawa, T.; Kawamoto, T.; Kokabu, S. Protein Phosphatase 1 Regulatory Subunit 18 Suppresses the Transcriptional Activity of NFATc1 via Regulation of C-Fos. Bone Rep. 2021, 15, 101114. [Google Scholar] [CrossRef]
- Takayanagi, H.; Kim, S.; Koga, T.; Nishina, H.; Isshiki, M.; Yoshida, H.; Saiura, A.; Isobe, M.; Yokochi, T.; Inoue, J.-I.; et al. Induction and Activation of the Transcription Factor NFATc1 (NFAT2) Integrate RANKL Signaling in Terminal Differentiation of Osteoclasts. Dev. Cell 2002, 3, 889–901. [Google Scholar] [CrossRef]
- Ikeda, F.; Nishimura, R.; Matsubara, T.; Hata, K.; Reddy, S.V.; Yoneda, T. Activation of NFAT Signal in Vivo Leads to Osteopenia Associated with Increased Osteoclastogenesis and Bone-Resorbing Activity. J. Immunol. 2006, 177, 2384–2390. [Google Scholar] [CrossRef] [PubMed]
- Soriano, P.; Montgomery, C.; Geske, R.; Bradley, A. Targeted Disruption of the C-Src Proto-Oncogene Leads to Osteopetrosis in Mice. Cell 1991, 64, 693–702. [Google Scholar] [CrossRef]
- Jurdic, P.; Saltel, F.; Chabadel, A.; Destaing, O. Podosome and Sealing Zone: Specificity of the Osteoclast Model. Eur. J. Cell Biol. 2006, 85, 195–202. [Google Scholar] [CrossRef] [PubMed]
- Blair, H.C.; Teitelbaum, S.L.; Ghiselli, R.; Gluck, S. Osteoclastic Bone Resorption by a Polarized Vacuolar Proton Pump. Science 1989, 245, 855–857. [Google Scholar] [CrossRef]
- Tezuka, K.; Tezuka, Y.; Maejima, A.; Sato, T.; Nemoto, K.; Kamioka, H.; Hakeda, Y.; Kumegawa, M. Molecular Cloning of a Possible Cysteine Proteinase Predominantly Expressed in Osteoclasts. J. Biol. Chem. 1994, 269, 1106–1109. [Google Scholar] [CrossRef]
- Rosen, V.; Thies, R.S. The BMP Proteins in Bone Formation and Repair. Trends Genet. 1992, 8, 97–102. [Google Scholar] [CrossRef]
- Komori, T.; Yagi, H.; Nomura, S.; Yamaguchi, A.; Sasaki, K.; Deguchi, K.; Shimizu, Y.; Bronson, R.T.; Gao, Y.H.; Inada, M.; et al. Targeted Disruption of Cbfa1 Results in a Complete Lack of Bone Formation Owing to Maturational Arrest of Osteoblasts. Cell 1997, 89, 755–764. [Google Scholar] [CrossRef]
- Nakashima, K.; Zhou, X.; Kunkel, G.; Zhang, Z.; Deng, J.M.; Behringer, R.R.; de Crombrugghe, B. The Novel Zinc Finger-Containing Transcription Factor Osterix Is Required for Osteoblast Differentiation and Bone Formation. Cell 2002, 108, 17–29. [Google Scholar] [CrossRef]
- Matsubara, T.; Kida, K.; Yamaguchi, A.; Hata, K.; Ichida, F.; Meguro, H.; Aburatani, H.; Nishimura, R.; Yoneda, T. BMP2 Regulates Osterix through Msx2 and Runx2 during Osteoblast Differentiation. J. Biol. Chem. 2008, 283, 29119–29125. [Google Scholar] [CrossRef]
- Boyce, B.F.; Yoneda, T.; Lowe, C.; Soriano, P.; Mundy, G.R. Requirement of Pp60c-Src Expression for Osteoclasts to Form Ruffled Borders and Resorb Bone in Mice. J. Clin. Investig. 1992, 90, 1622–1627. [Google Scholar] [CrossRef]
- Marzia, M.; Sims, N.A.; Voit, S.; Migliaccio, S.; Taranta, A.; Bernardini, S.; Faraggiana, T.; Yoneda, T.; Mundy, G.R.; Boyce, B.F.; et al. Decreased C-Src Expression Enhances Osteoblast Differentiation and Bone Formation. J. Cell Biol. 2000, 151, 311–320. [Google Scholar] [CrossRef] [PubMed]
- Brown, M.T.; Cooper, J.A. Regulation, Substrates and Functions of Src. Biochim. Biophys. Acta Rev. Cancer 1996, 1287, 121–149. [Google Scholar] [CrossRef]
- Garcia-Gomez, A.; Ocio, E.M.; Crusoe, E.; Santamaria, C.; Hernández-Campo, P.; Blanco, J.F.; Sanchez-Guijo, F.M.; Hernández-Iglesias, T.; Briñón, J.G.; Fisac-Herrero, R.M.; et al. Dasatinib as a Bone-Modifying Agent: Anabolic and Anti-Resorptive Effects. PLoS ONE 2012, 7, e34914. [Google Scholar] [CrossRef]
- Horne, W.C.; Neff, L.; Chatterjee, D.; Lomri, A.; Levy, J.B.; Baron, R. Osteoclasts Express High Levels of Pp60c-Src in Association with Intracellular Membranes. J. Cell Biol. 1992, 119, 1003–1013. [Google Scholar] [CrossRef]
- Schwartzberg, P.L.; Xing, L.; Hoffmann, O.; Lowell, C.A.; Garrett, L.; Boyce, B.F.; Varmus, H.E. Rescue of Osteoclast Function by Transgenic Expression of Kinase-Deficient Src in Src-/- Mutant Mice. Genes Dev. 1997, 11, 2835–2844. [Google Scholar] [CrossRef] [PubMed]
- Xing, L.; Venegas, A.M.; Chen, A.; Garrett-Beal, L.; Boyce, B.F.; Varmus, H.E.; Schwartzberg, P.L. Genetic Evidence for a Role for Src Family Kinases in TNF Family Receptor Signaling and Cell Survival. Genes Dev. 2001, 15, 241–253. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, S.; Nakamura, I.; Inoue, J.-I.; Oda, H.; Nakamura, K. Signal Transduction Pathways Regulating Osteoclast Differentiation and Function. J. Bone Miner. Metab. 2003, 21, 123–133. [Google Scholar] [CrossRef] [PubMed]
- Destaing, O.; Sanjay, A.; Itzstein, C.; Horne, W.C.; Toomre, D.; De Camilli, P.; Baron, R. The Tyrosine Kinase Activity of C-Src Regulates Actin Dynamics and Organization of Podosomes in Osteoclasts. Mol. Biol. Cell 2008, 19, 394–404. [Google Scholar] [CrossRef]
- Yoneda, T.; Lowe, C.; Lee, C.H.; Gutierrez, G.; Niewolna, M.; Williams, P.J.; Izbicka, E.; Uehara, Y.; Mundy, G.R. Herbimycin A, a Pp60c-Src Tyrosine Kinase Inhibitor, Inhibits Osteoclastic Bone Resorption in Vitro and Hypercalcemia in Vivo. J. Clin. Investig. 1993, 91, 2791–2795. [Google Scholar] [CrossRef]
- Resh, M.D. Myristylation and Palmitylation of Src Family Members: The Fats of the Matter. Cell 1994, 76, 411–413. [Google Scholar] [CrossRef]
- Okada, M. Regulation of the SRC Family Kinases by Csk. Int. J. Biol. Sci. 2012, 8, 1385–1397. [Google Scholar] [CrossRef] [PubMed]
- Arcaro, A.; Aubert, M.; Espinosa del Hierro, M.E.; Khanzada, U.K.; Angelidou, S.; Tetley, T.D.; Bittermann, A.G.; Frame, M.C.; Seckl, M.J. Critical Role for Lipid Raft-Associated Src Kinases in Activation of PI3K-Akt Signalling. Cell. Signal. 2007, 19, 1081–1092. [Google Scholar] [CrossRef] [PubMed]
- Oneyama, C.; Hikita, T.; Enya, K.; Dobenecker, M.-W.; Saito, K.; Nada, S.; Tarakhovsky, A.; Okada, M. The Lipid Raft-Anchored Adaptor Protein Cbp Controls the Oncogenic Potential of c-Src. Mol. Cell 2008, 30, 426–436. [Google Scholar] [CrossRef]
- Head, B.P.; Patel, H.H.; Insel, P.A. Interaction of Membrane/Lipid Rafts with the Cytoskeleton: Impact on Signaling and Function: Membrane/Lipid Rafts, Mediators of Cytoskeletal Arrangement and Cell Signaling. Biochim. Biophys. Acta 2014, 1838, 532–545. [Google Scholar] [CrossRef] [PubMed]
- Pawson, T.; Gish, G.D. SH2 and SH3 Domains: From Structure to Function. Cell 1992, 71, 359–362. [Google Scholar] [CrossRef]
- Shvartsman, D.E.; Donaldson, J.C.; Diaz, B.; Gutman, O.; Martin, G.S.; Henis, Y.I. Src Kinase Activity and SH2 Domain Regulate the Dynamics of Src Association with Lipid and Protein Targets. J. Cell Biol. 2007, 178, 675–686. [Google Scholar] [CrossRef] [PubMed]
- Matsubara, T.; Ikeda, F.; Hata, K.; Nakanishi, M.; Okada, M.; Yasuda, H.; Nishimura, R.; Yoneda, T. Cbp Recruitment of Csk into Lipid Rafts Is Critical to C-Src Kinase Activity and Bone Resorption in Osteoclasts. J. Bone Miner. Res. 2010, 25, 1068–1076. [Google Scholar] [CrossRef]
- Lau, K.-H.W.; Wu, L.-W.; Sheng, M.H.-C.; Amoui, M.; Suhr, S.M.; Baylink, D.J. An Osteoclastic Protein-Tyrosine Phosphatase Is a Potential Positive Regulator of the c-Src Protein-Tyrosine Kinase Activity: A Mediator of Osteoclast Activity. J. Cell. Biochem. 2006, 97, 940–955. [Google Scholar] [CrossRef]
- Irtegun, S.; Wood, R.J.; Ormsby, A.R.; Mulhern, T.D.; Hatters, D.M. Tyrosine 416 Is Phosphorylated in the Closed, Repressed Conformation of c-Src. PLoS ONE 2013, 8, e71035. [Google Scholar] [CrossRef]
- Kong, L.; Deng, Z.; Shen, H.; Zhang, Y. Src Family Kinase Inhibitor PP2 Efficiently Inhibits Cervical Cancer Cell Proliferation through Down-Regulating Phospho-Src-Y416 and Phospho-EGFR-Y1173. Mol. Cell. Biochem. 2011, 348, 11–19. [Google Scholar] [CrossRef]
- Saltel, F.; Destaing, O.; Bard, F.; Eichert, D.; Jurdic, P. Apatite-Mediated Actin Dynamics in Resorbing Osteoclasts. Mol. Biol. Cell 2004, 15, 5231–5241. [Google Scholar] [CrossRef] [PubMed]
- Obara, Y.; Labudda, K.; Dillon, T.J.; Stork, P.J.S. PKA Phosphorylation of Src Mediates Rap1 Activation in NGF and CAMP Signaling in PC12 Cells. J. Cell Sci. 2004, 117, 6085–6094. [Google Scholar] [CrossRef] [PubMed]
- Matsubara, T.; Kokabu, S.; Nakatomi, C.; Kinbara, M.; Maeda, T.; Yoshizawa, M.; Yasuda, H.; Takano-Yamamoto, T.; Baron, R.; Jimi, E. The Actin-Binding Protein PPP1r18 Regulates Maturation, Actin Organization, and Bone Resorption Activity of Osteoclasts. Mol. Cell. Biol. 2018, 38, e00425-17. [Google Scholar] [CrossRef] [PubMed]
- Rao, A.; Luo, C.; Hogan, P.G. Transcription Factors of the NFAT Family: Regulation and Function. Annu. Rev. Immunol. 1997, 15, 707–747. [Google Scholar] [CrossRef]
- Peng, S.L.; Gerth, A.J.; Ranger, A.M.; Glimcher, L.H. NFATc1 and NFATc2 Together Control Both T and B Cell Activation and Differentiation. Immunity 2001, 14, 13–20. [Google Scholar] [CrossRef]
- Matsubara, T.; Myoui, A.; Ikeda, F.; Hata, K.; Yoshikawa, H.; Nishimura, R.; Yoneda, T. Critical Role of Cortactin in Actin Ring Formation and Osteoclastic Bone Resorption. J. Bone Miner. Metab. 2006, 24, 368–372. [Google Scholar] [CrossRef]
- Biosse Duplan, M.; Zalli, D.; Stephens, S.; Zenger, S.; Neff, L.; Oelkers, J.M.; Lai, F.P.L.; Horne, W.; Rottner, K.; Baron, R. Microtubule Dynamic Instability Controls Podosome Patterning in Osteoclasts through EB1, Cortactin, and Src. Mol. Cell. Biol. 2014, 34, 16–29. [Google Scholar] [CrossRef]
- Tehrani, S.; Faccio, R.; Chandrasekar, I.; Ross, F.P.; Cooper, J.A. Cortactin Has an Essential and Specific Role in Osteoclast Actin Assembly. Mol. Biol. Cell 2006, 17, 2882–2895. [Google Scholar] [CrossRef]
- Nakamura, I.; Jimi, E.; Duong, L.T.; Sasaki, T.; Takahashi, N.; Rodan, G.A.; Suda, T. Tyrosine Phosphorylation of P130Cas Is Involved in Actin Organization in Osteoclasts. J. Biol. Chem. 1998, 273, 11144–11149. [Google Scholar] [CrossRef]
- Nagai, Y.; Osawa, K.; Fukushima, H.; Tamura, Y.; Aoki, K.; Ohya, K.; Yasuda, H.; Hikiji, H.; Takahashi, M.; Seta, Y.; et al. P130Cas, Crk-Associated Substrate, Plays Important Roles in Osteoclastic Bone Resorption. J. Bone Miner. Res. 2013, 28, 2449–2462. [Google Scholar] [CrossRef]
- Duong, L.T.; Lakkakorpi, P.T.; Nakamura, I.; Machwate, M.; Nagy, R.M.; Rodan, G.A. PYK2 in Osteoclasts Is an Adhesion Kinase, Localized in the Sealing Zone, Activated by Ligation of Alpha(v)Beta3 Integrin, and Phosphorylated by Src Kinase. J. Clin. Investig. 1998, 102, 881–892. [Google Scholar] [CrossRef] [PubMed]
- Gil-Henn, H.; Destaing, O.; Sims, N.A.; Aoki, K.; Alles, N.; Neff, L.; Sanjay, A.; Bruzzaniti, A.; De Camilli, P.; Baron, R.; et al. Defective Microtubule-Dependent Podosome Organization in Osteoclasts Leads to Increased Bone Density in Pyk2−/− Mice. J. Cell Biol. 2007, 178, 1053–1064. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, S.; Amling, M.; Neff, L.; Peyman, A.; Uhlmann, E.; Levy, J.B.; Baron, R. C-Cbl Is Downstream of c-Src in a Signalling Pathway Necessary for Bone Resorption. Nature 1996, 383, 528–531. [Google Scholar] [CrossRef] [PubMed]
- Faccio, R.; Teitelbaum, S.L.; Fujikawa, K.; Chappel, J.; Zallone, A.; Tybulewicz, V.L.; Ross, F.P.; Swat, W. Vav3 Regulates Osteoclast Function and Bone Mass. Nat. Med. 2005, 11, 284–290. [Google Scholar] [CrossRef]
- Kobayakawa, M.; Matsubara, T.; Mizokami, A.; Hiura, F.; Takakura, N.; Kokabu, S.; Matsuda, M.; Yasuda, H.; Nakamura, I.; Takei, Y.; et al. Kif1c Regulates Osteoclastic Bone Resorption as a Downstream Molecule of P130Cas. Cell Biochem. Funct. 2020, 38, 300–308. [Google Scholar] [CrossRef]
- Matsubara, T.; Kinbara, M.; Maeda, T.; Yoshizawa, M.; Kokabu, S.; Takano Yamamoto, T. Regulation of Osteoclast Differentiation and Actin Ring Formation by the Cytolinker Protein Plectin. Biochem. Biophys. Res. Commun. 2017, 489, 472–476. [Google Scholar] [CrossRef]
- Matsubara, T.; Yaginuma, T.; Addison, W.N.; Fujita, Y.; Watanabe, K.; Yoshioka, I.; Hikiji, H.; Maki, K.; Baron, R.; Kokabu, S. Plectin Stabilizes Microtubules during Osteoclastic Bone Resorption by Acting as a Scaffold for Src and Pyk2. Bone 2020, 132, 115209. [Google Scholar] [CrossRef]
- Blangy, A.; Bompard, G.; Guerit, D.; Marie, P.; Maurin, J.; Morel, A.; Vives, V. The Osteoclast Cytoskeleton—Current Understanding and Therapeutic Perspectives for Osteoporosis. J. Cell Sci. 2020, 133, jcs244794. [Google Scholar] [CrossRef]
- Thomas, S.G.; Poulter, N.S.; Bem, D.; Finney, B.; Machesky, L.M.; Watson, S.P. The Actin Binding Proteins Cortactin and HS1 Are Dispensable for Platelet Actin Nodule and Megakaryocyte Podosome Formation. Platelets 2017, 28, 372–379. [Google Scholar] [CrossRef]
- Horne, W.C.; Sanjay, A.; Bruzzaniti, A.; Baron, R. The Role(s) of Src Kinase and Cbl Proteins in the Regulation of Osteoclast Differentiation and Function. Immunol. Rev. 2005, 208, 106–125. [Google Scholar] [CrossRef]
- Lakkakorpi, P.T.; Nakamura, I.; Nagy, R.M.; Parsons, J.T.; Rodan, G.A.; Duong, L.T. Stable Association of PYK2 and P130Cas in Osteoclasts and Their Co-Localization in the Sealing Zone. J. Biol. Chem. 1999, 274, 4900–4907. [Google Scholar] [CrossRef] [PubMed]
- Buckbinder, L.; Crawford, D.T.; Qi, H.; Ke, H.Z.; Olson, L.M.; Long, K.R.; Bonnette, P.C.; Baumann, A.P.; Hambor, J.E.; Grasser, W.A., III; et al. Proline-Rich Tyrosine Kinase 2 Regulates Osteoprogenitor Cells and Bone Formation, and Offers an Anabolic Treatment Approach for Osteoporosis. Proc. Natl. Acad. Sci. USA 2007, 104, 10619–10624. [Google Scholar] [CrossRef] [PubMed]
- Chiusaroli, R.; Sanjay, A.; Henriksen, K.; Engsig, M.T.; Horne, W.C.; Gu, H.; Baron, R. Deletion of the Gene Encoding C-Cbl Alters the Ability of Osteoclasts to Migrate, Delaying Resorption and Ossification of Cartilage during the Development of Long Bones. Dev. Biol. 2003, 261, 537–547. [Google Scholar] [CrossRef]
- Nakajima, A.; Sanjay, A.; Chiusaroli, R.; Adapala, N.S.; Neff, L.; Itzsteink, C.; Horne, W.C.; Baron, R. Loss of Cbl-b Increases Osteoclast Bone-Resorbing Activity and Induces Osteopenia. J. Bone Miner. Res. 2009, 24, 1162–1172. [Google Scholar] [CrossRef]
- Jang, J.S.; Kang, I.S.; Cha, Y.-N.; Lee, Z.H.; Dinauer, M.C.; Kim, Y.-J.; Kim, C. Vav1 Inhibits RANKL-Induced Osteoclast Differentiation and Bone Resorption. BMB Rep. 2019, 52, 659–664. [Google Scholar] [CrossRef]
- Efimova, N.; Grimaldi, A.; Bachmann, A.; Frye, K.; Zhu, X.; Feoktistov, A.; Straube, A.; Kaverina, I. Podosome-Regulating Kinesin KIF1C Translocates to the Cell Periphery in a CLASP-Dependent Manner. J. Cell Sci. 2014, 127, 5179–5188. [Google Scholar] [CrossRef]
- Wiche, G.; Osmanagic-Myers, S.; Castañón, M.J. Networking and Anchoring through Plectin: A Key to IF Functionality and Mechanotransduction. Curr. Opin. Cell Biol. 2015, 32, 21–29. [Google Scholar] [CrossRef]
- Meier, S.M.; Kreutz, D.; Winter, L.; Klose, M.H.M.; Cseh, K.; Weiss, T.; Bileck, A.; Alte, B.; Mader, J.C.; Jana, S.; et al. An Organoruthenium Anticancer Agent Shows Unexpected Target Selectivity For Plectin. Angew. Chem. Int. Ed. 2017, 56, 8267–8271. [Google Scholar] [CrossRef]
- Zaidi, S.K.; Sullivan, A.J.; Medina, R.; Ito, Y.; van Wijnen, A.J.; Stein, J.L.; Lian, J.B.; Stein, G.S. Tyrosine Phosphorylation Controls Runx2-Mediated Subnuclear Targeting of YAP to Repress Transcription. EMBO J. 2004, 23, 790–799. [Google Scholar] [CrossRef]
- Xiong, J.; Almeida, M.; O’Brien, C.A. The YAP/TAZ Transcriptional Co-Activators Have Opposing Effects at Different Stages of Osteoblast Differentiation. Bone 2018, 112, 1–9. [Google Scholar] [CrossRef]
- Kim, S.; Koga, T.; Isobe, M.; Kern, B.E.; Yokochi, T.; Chin, Y.E.; Karsenty, G.; Taniguchi, T.; Takayanagi, H. Stat1 Functions as a Cytoplasmic Attenuator of Runx2 in the Transcriptional Program of Osteoblast Differentiation. Genes Dev. 2003, 17, 1979–1991. [Google Scholar] [CrossRef] [PubMed]
- Alvandi, Z.; Opas, M. C-Src Kinase Inhibits Osteogenic Differentiation via Enhancing STAT1 Stability. PLoS ONE 2020, 15, e0241646. [Google Scholar] [CrossRef] [PubMed]
- Id Boufker, H.; Lagneaux, L.; Najar, M.; Piccart, M.; Ghanem, G.; Body, J.-J.; Journé, F. The Src Inhibitor Dasatinib Accelerates the Differentiation of Human Bone Marrow-Derived Mesenchymal Stromal Cells into Osteoblasts. BMC Cancer 2010, 10, 298. [Google Scholar] [CrossRef] [PubMed]
- Choi, Y.H.; Han, Y.; Lee, S.H.; Cheong, H.; Chun, K.-H.; Yeo, C.-Y.; Lee, K.Y. Src Enhances Osteogenic Differentiation through Phosphorylation of Osterix. Mol. Cell. Endocrinol. 2015, 407, 85–97. [Google Scholar] [CrossRef]
- Sawada, Y.; Tamada, M.; Dubin-Thaler, B.J.; Cherniavskaya, O.; Sakai, R.; Tanaka, S.; Sheetz, M.P. Force Sensing by Mechanical Extension of the Src Family Kinase Substrate P130Cas. Cell 2006, 127, 1015–1026. [Google Scholar] [CrossRef]
- Kaneko, K.; Ito, M.; Naoe, Y.; Lacy-Hulbert, A.; Ikeda, K. Integrin Av in the Mechanical Response of Osteoblast Lineage Cells. Biochem. Biophys. Res. Commun. 2014, 447, 352–357. [Google Scholar] [CrossRef]
- Borer, K.T. Physical Activity in the Prevention and Amelioration of Osteoporosis in Women. Sports Med. 2005, 35, 779–830. [Google Scholar] [CrossRef]
- Sibonga, J.D. Spaceflight-Induced Bone Loss: Is There an Osteoporosis Risk? Curr. Osteoporos. Rep. 2013, 11, 92–98. [Google Scholar] [CrossRef]
- Huang, W.-C.; Chen, J.-J.; Inoue, H.; Chen, C.-C. Tyrosine Phosphorylation of I-ΚB Kinase α/β by Protein Kinase C-Dependent c-Src Activation Is Involved in TNF-α-Induced Cyclooxygenase-2 Expression. J. Immunol. 2003, 170, 4767–4775. [Google Scholar] [CrossRef]
- Zaric, J.; Rüegg, C. Integrin-Mediated Adhesion and Soluble Ligand Binding Stabilize COX-2 Protein Levels in Endothelial Cells by Inducing Expression and Preventing Degradation. J. Biol. Chem. 2005, 280, 1077–1085. [Google Scholar] [CrossRef]
- Zhang, X.; Schwarz, E.M.; Young, D.A.; Puzas, J.E.; Rosier, R.N.; O’Keefe, R.J. Cyclooxygenase-2 Regulates Mesenchymal Cell Differentiation into the Osteoblast Lineage and Is Critically Involved in Bone Repair. J. Clin. Investig. 2002, 109, 1405–1415. [Google Scholar] [CrossRef] [PubMed]
- Yao, Z.; Li, Y.; Yin, X.; Dong, Y.; Xing, L.; Boyce, B.F. NF-ΚB RelB Negatively Regulates Osteoblast Differentiation and Bone Formation. J. Bone Miner. Res. 2014, 29, 866–877. [Google Scholar] [CrossRef] [PubMed]
- Matsubara, T.; Addison, W.N.; Kokabu, S.; Neff, L.; Horne, W.; Gori, F.; Baron, R. Characterization of Unique Functionalities in C-Src Domains Required for Osteoclast Podosome Belt Formation. J. Biol. Chem. 2021, 296, 100790. [Google Scholar] [CrossRef] [PubMed]
- Stein, P.L.; Vogel, H.; Soriano, P. Combined Deficiencies of Src, Fyn, and Yes Tyrosine Kinases in Mutant Mice. Genes Dev. 1994, 8, 1999–2007. [Google Scholar] [CrossRef] [PubMed]
- Kaabeche, K.; Lemonnier, J.; Le Mée, S.; Caverzasio, J.; Marie, P.J. Cbl-Mediated Degradation of Lyn and Fyn Induced by Constitutive Fibroblast Growth Factor Receptor-2 Activation Supports Osteoblast Differentiation. J. Biol. Chem. 2004, 279, 36259–36267. [Google Scholar] [CrossRef]
- Kim, H.-J.; Zhang, K.; Zhang, L.; Ross, F.P.; Teitelbaum, S.L.; Faccio, R. The Src Family Kinase, Lyn, Suppresses Osteoclastogenesis in Vitro and in Vivo. Proc. Natl. Acad. Sci. USA 2009, 106, 2325–2330. [Google Scholar] [CrossRef]
- Lowell, C.A.; Soriano, P.; Varmus, H.E. Functional Overlap in the Src Gene Family: Inactivation of Hck and Fgr Impairs Natural Immunity. Genes Dev. 1994, 8, 387–398. [Google Scholar] [CrossRef]
- Lowell, C.A.; Niwa, M.; Soriano, P.; Varmus, H.E. Deficiency of the Hck and Src Tyrosine Kinases Results in Extreme Levels of Extramedullary Hematopoiesis. Blood 1996, 87, 1780–1792. [Google Scholar] [CrossRef]
- Kim, Y.; Hayashi, M.; Ono, T.; Yoda, T.; Takayanagi, H.; Nakashima, T. Suppression of Hematopoietic Cell Kinase Ameliorates the Bone Destruction Associated with Inflammation. Mod. Rheumatol. 2020, 30, 85–92. [Google Scholar] [CrossRef]
- Matsuura, V.K.S.K.; Yoshida, C.A.; Komori, H.; Sakane, C.; Yamana, K.; Jiang, Q.; Komori, T. Expression of a Constitutively Active Form of Hck in Chondrocytes Activates Wnt and Hedgehog Signaling Pathways, and Induces Chondrocyte Proliferation in Mice. Int. J. Mol. Sci. 2020, 21, 2682. [Google Scholar] [CrossRef]


| Src Family | Bone Resorption | Bone Formation |
|---|---|---|
| Src | Essential for osteoclastic bone resorption [12] | Suppress osteoblast differentiation [72,73] |
| Fyn | Promote osteoclastic bone resorption [83] | Suppress osteoblast differentiation [85] |
| Lyn | Suppress osteoclast differentiation [86] | Suppress osteoblast differentiation [85] |
| Hck | Promote osteoclastic bone resorption [87,88] | Upregulate chondrocyte proliferation [90] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Matsubara, T.; Yasuda, K.; Mizuta, K.; Kawaue, H.; Kokabu, S. Tyrosine Kinase Src Is a Regulatory Factor of Bone Homeostasis. Int. J. Mol. Sci. 2022, 23, 5508. https://doi.org/10.3390/ijms23105508
Matsubara T, Yasuda K, Mizuta K, Kawaue H, Kokabu S. Tyrosine Kinase Src Is a Regulatory Factor of Bone Homeostasis. International Journal of Molecular Sciences. 2022; 23(10):5508. https://doi.org/10.3390/ijms23105508
Chicago/Turabian StyleMatsubara, Takuma, Kazuma Yasuda, Kana Mizuta, Hiroka Kawaue, and Shoichiro Kokabu. 2022. "Tyrosine Kinase Src Is a Regulatory Factor of Bone Homeostasis" International Journal of Molecular Sciences 23, no. 10: 5508. https://doi.org/10.3390/ijms23105508
APA StyleMatsubara, T., Yasuda, K., Mizuta, K., Kawaue, H., & Kokabu, S. (2022). Tyrosine Kinase Src Is a Regulatory Factor of Bone Homeostasis. International Journal of Molecular Sciences, 23(10), 5508. https://doi.org/10.3390/ijms23105508






