KCNK3 Mutation Causes Altered Immune Function in Pulmonary Arterial Hypertension Patients and Mouse Models
Abstract
1. Introduction
2. Results
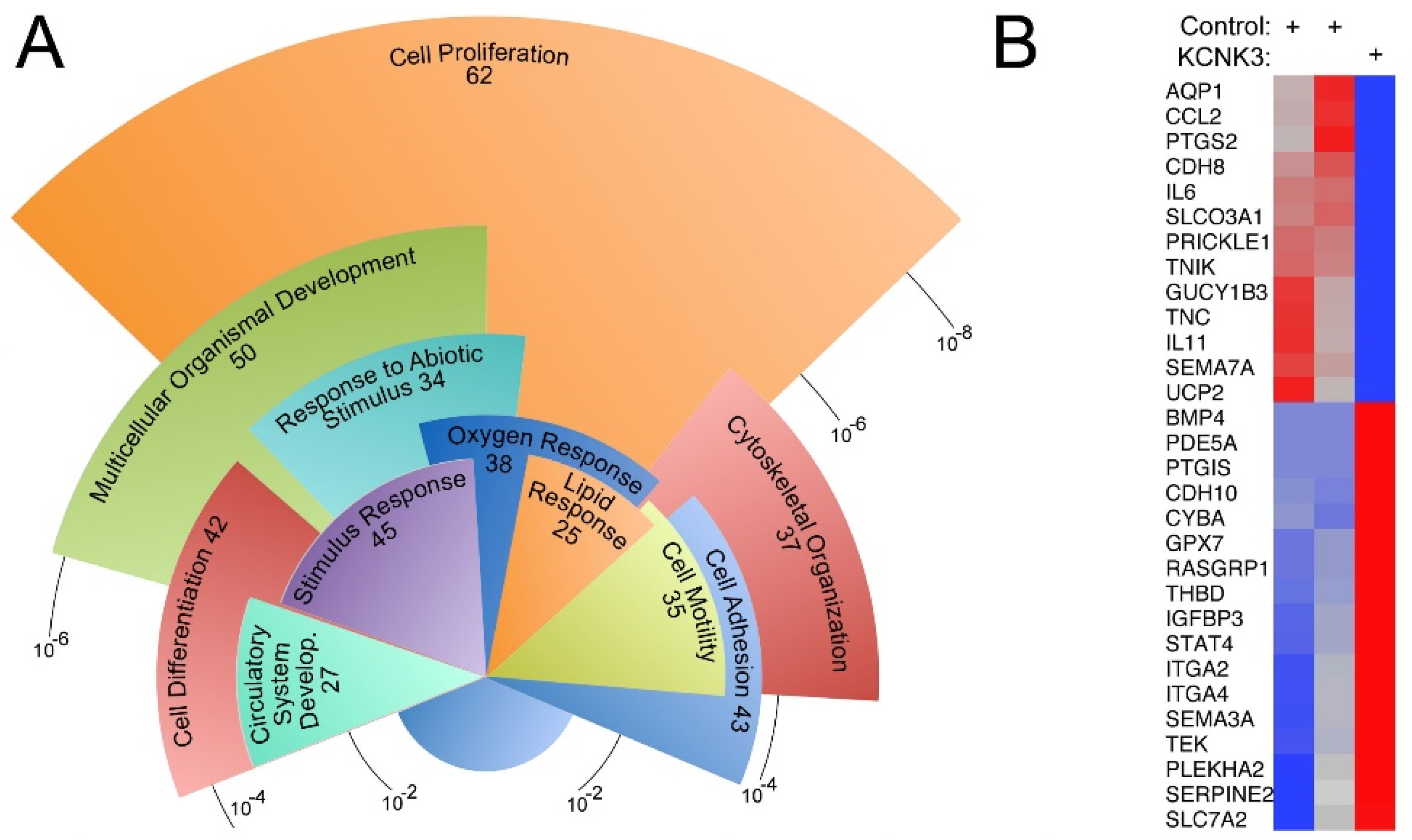
2.1. Gene Expression Differences in iPS-Derived Mesenchyme from a PAH Patient with KCNK3 Mutation Compared to Controls
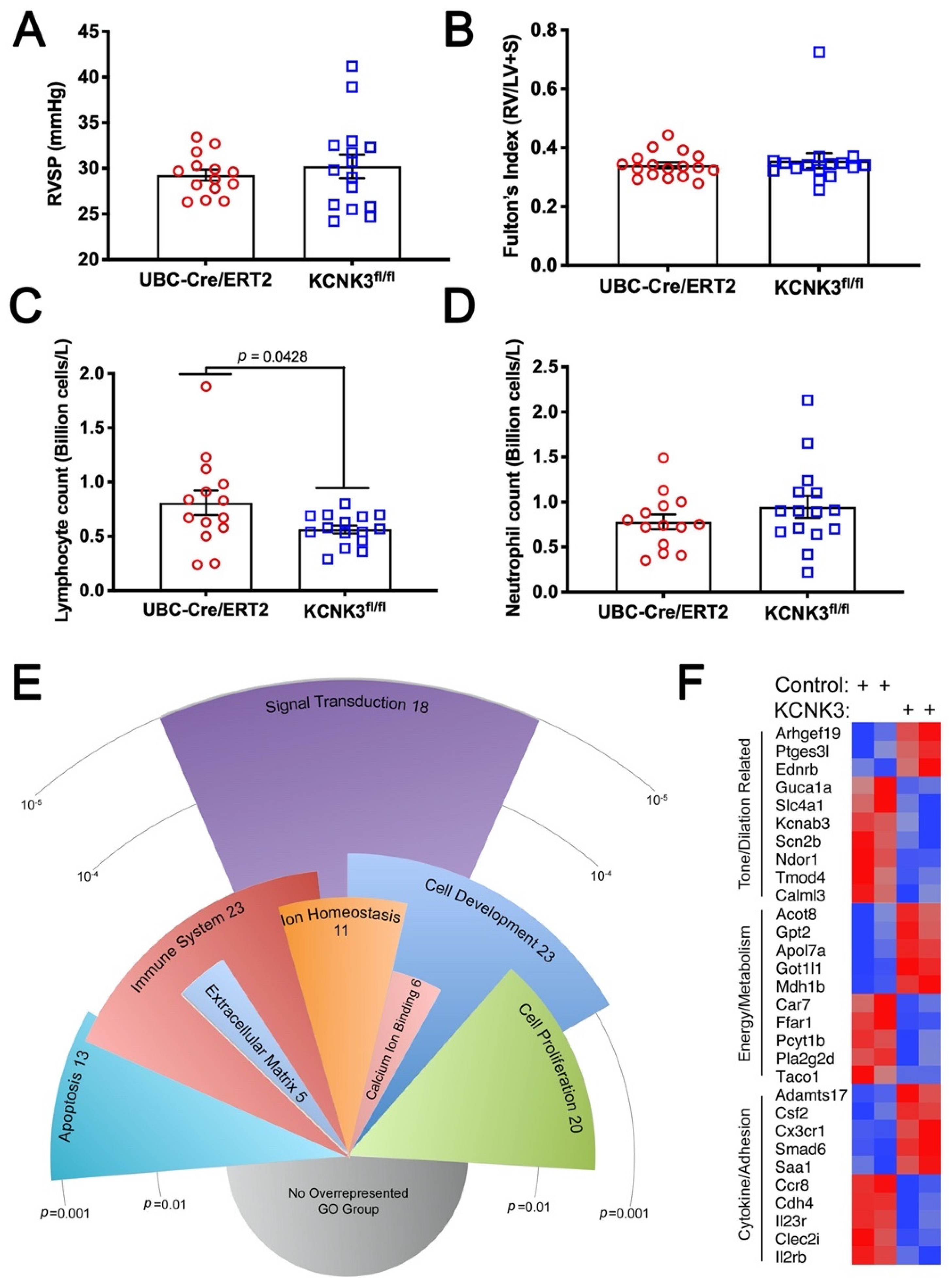
2.2. Mice with KCNK3 Knocked Out as Adults Lack Increased Susceptibility to Hypoxia
2.3. Gene Expression Differences in KCNK3 Mouse Lung by RNA-Seq
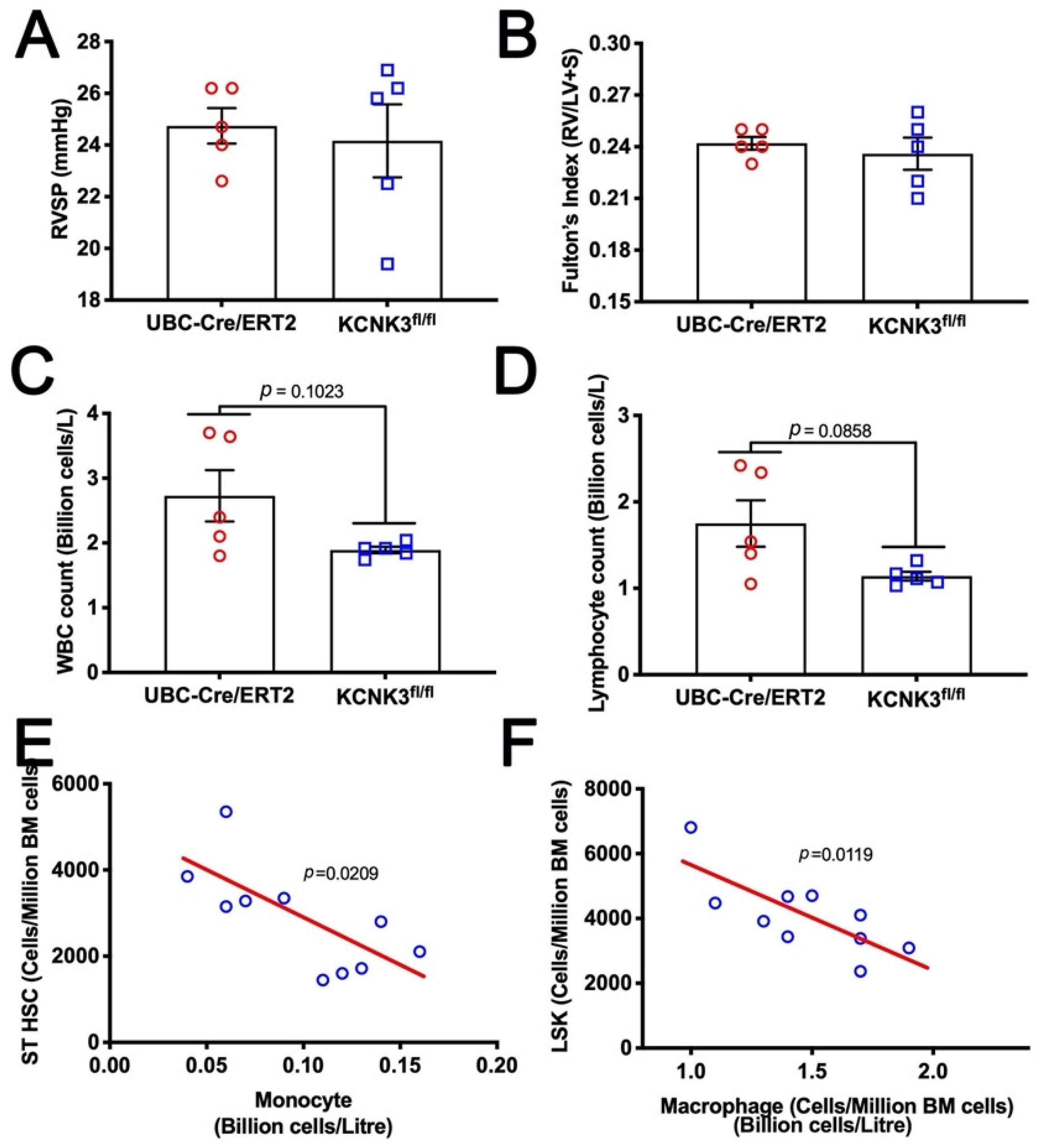
2.4. Mice with kcnk3 Knocked Out as Adults Lack Susceptibility to Western Diet, but Show Signs of Increased Production and Margination of Lymphocytes
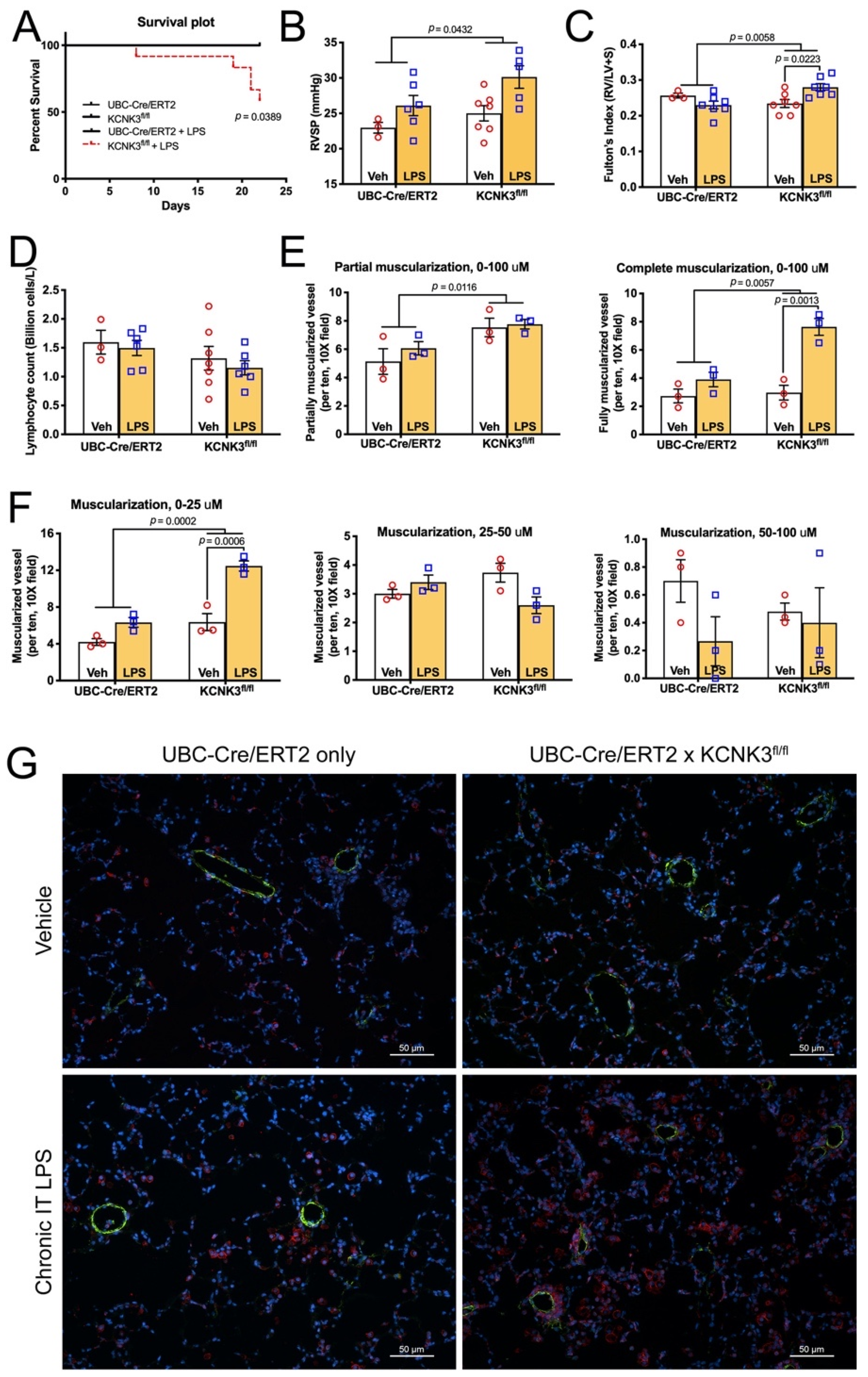
2.5. Mice with kcnk3 Knocked Out as Adults Have High Mortality and Develop Pulmonary Hypertension in Response to Low Dose Lipopolysaccharide
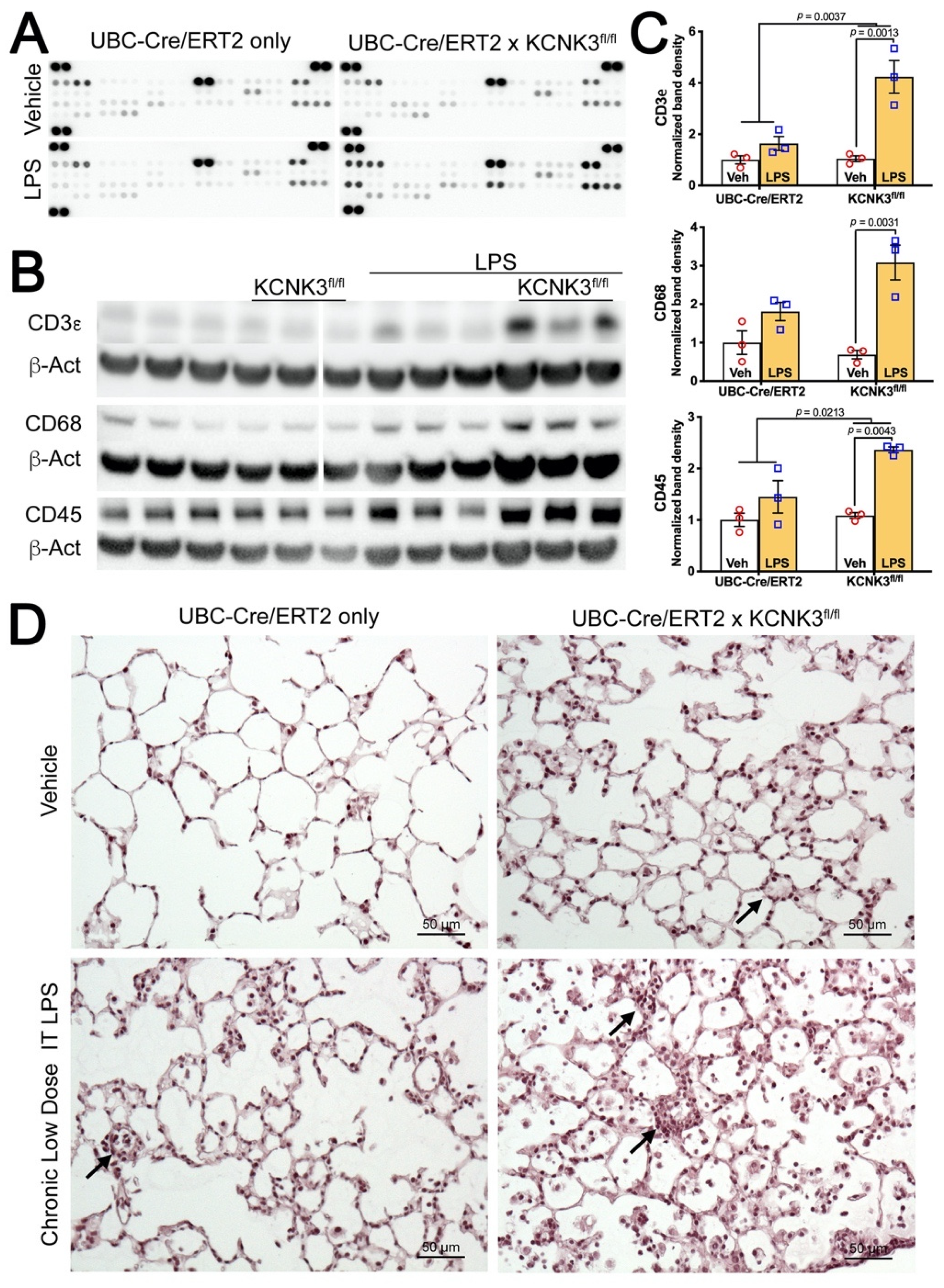
2.6. Kcnk3fl/fl Mice Have Striking Increases in Pulmonary Inflammatory Cells, Multiple Cytokines
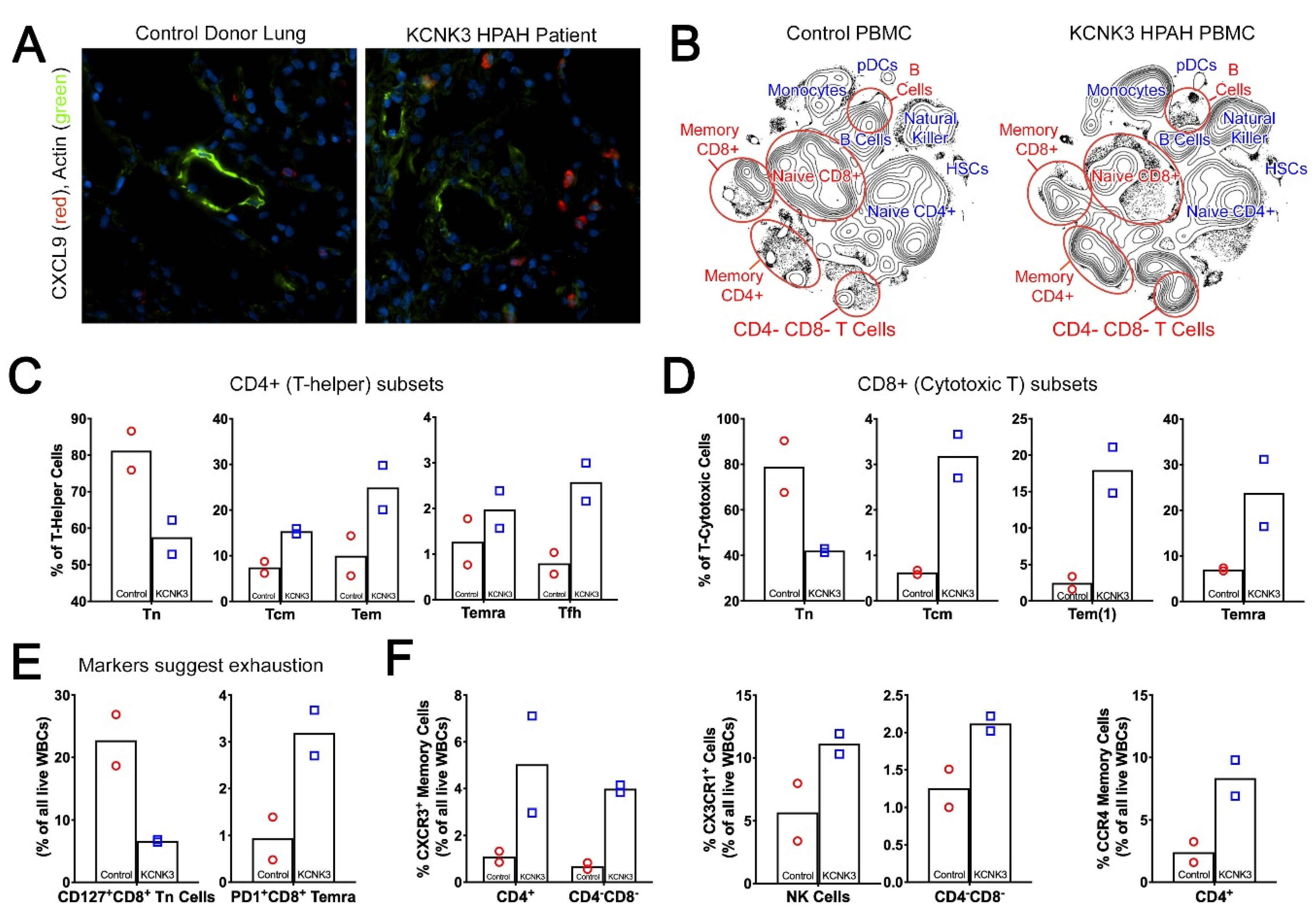
2.7. Human PAH Patients with KCNK3 Mutation Show Increased Cytokines and Chronic Immune Cell Activation
3. Discussion
4. Materials and Methods
4.1. Reagents, Chemicals and Kits
4.2. Animal Study Design
4.2.1. Hypoxia Study
4.2.2. Diet Study
4.2.3. LPS Study
4.3. Hemodynamic and Right Ventricular Hypertrophy Assessment
4.4. Western and Dot Blot Analysis
4.5. Immunohistochemical Analysis (IHC)
4.6. Human Samples and Study Design
4.6.1. Induced Pluripotent Stem Cells (iPS)
4.6.2. Lungs
4.6.3. Blood
4.7. Mass Immunophenotyping of Human PBMCs (CyTOF)
4.7.1. PBMC Staining Protocol
4.7.2. Data Acquisition and Analysis
4.8. Statistics
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ma, L.; Roman-Campos, D.; Austin, E.D.; Eyries, M.; Sampson, K.S.; Soubrier, F.; Germain, M.; Trégouët, D.-A.; Borczuk, A.; Rosenzweig, E.B.; et al. A Novel Channelopathy in Pulmonary Arterial Hypertension. N. Engl. J. Med. 2013, 369, 351–361. [Google Scholar] [CrossRef] [PubMed]
- Tejedor, P.N.; Castano, J.T.; Doza, J.P.; Lajara, P.A.; Trujillo, G.G.; Meseguer, M.L.; Broto, A.R.; Abadia, P.L.; Subia, P.E. An homozygous mutation in KCNK3 is associated with an aggressive form of hereditary pulmonary arterial hypertension. Clin. Genet. 2017, 91, 453–457. [Google Scholar] [CrossRef] [PubMed]
- Navas, P.; Tenorio, J.; Quezada, C.A.; Barrios, E.; Gordo, G.; Arias, P.; Meseguer, M.L.; Santos-Lozano, A.; Doza, J.P.; Lapunzina, P.; et al. Molecular Analysis of BMPR2, TBX4, and KCNK3 and Genotype-Phenotype Correlations in Spanish Patients and Families With Idiopathic and Hereditary Pulmonary Arterial Hypertension. Rev. Esp. Cardiol. 2016, 69, 1011–1019. [Google Scholar] [CrossRef]
- Higasa, K.; Ogawa, A.; Terao, C.; Shimizu, M.; Kosugi, S.; Yamada, R.; Date, H.; Matsubara, H.; Matsuda, F. A burden of rare variants in BMPR2 and KCNK3 contributes to a risk of familial pulmonary arterial hypertension. BMC Pulm. Med. 2017, 17, 1–8. [Google Scholar] [CrossRef]
- Le Ribeuz, H.; Dumont, F.; Ruellou, G.; Lambert, M.; Balliau, T.; Quatredeniers, M.; Girerd, B.; Cohen-Kaminsky, S.; Mercier, O.; Yen-Nicolay, S.; et al. Proteomic Analysis of KCNK3 Loss of Expression Identified Dysregulated Pathways in Pulmonary Vascular Cells. Int. J. Mol. Sci. 2020, 21, 7400. [Google Scholar] [CrossRef] [PubMed]
- Egnatchik, R.A.; Brittain, E.L.; Shah, A.T.; Fares, W.H.; Ford, H.J.; Monahan, K.; Kang, C.J.; Kocurek, E.G.; Zhu, S.; Luong, T.; et al. Dysfunctional BMPR2 signaling drives an abnormal endothelial requirement for glutamine in pulmonary arterial hypertension. Pulm. Circ. 2017, 7, 186–199. [Google Scholar] [CrossRef]
- Antigny, F.; Hautefort, A.; Meloche, J.; Belacel-Ouari, M.; Manoury, B.; Rucker-Martin, C.; Pechoux, C.; Potus, F.; Nadeau, V.; Tremblay, E.; et al. Potassium Channel Subfamily K Member 3 (KCNK3) Contributes to the Development of Pulmonary Arterial Hypertension. Circulation 2016, 133, 1371–1385. [Google Scholar] [CrossRef] [PubMed]
- Boucherat, O.; Chabot, S.; Antigny, F.; Perros, F.; Provencher, S.; Bonnet, S. Potassium channels in pulmonary arterial hypertension. Eur. Respir. J. 2015, 46, 1167–1177. [Google Scholar] [CrossRef] [PubMed]
- Murtaza, G.; Mermer, P.; Goldenberg, A.; Pfeil, U.; Paddenberg, R.; Weissmann, N.; Lochnit, G.; Kummer, W. TASK-1 potassium channel is not critically involved in mediating hypoxic pulmonary vasoconstriction of murine intra-pulmonary arteries. PLoS ONE 2017, 12, e0174071. [Google Scholar] [CrossRef] [PubMed]
- Kitagawa, M.G.; Reynolds, J.O.; Wehrens, X.H.T.; Bryan, R.M., Jr.; Pandit, L.M. Hemodynamic and Pathologic Characterization of the TASK-1(-/-) Mouse Does Not Demonstrate Pulmonary Hypertension. Front. Med. 2017, 4, 177. [Google Scholar] [CrossRef]
- Manoury, B.; Lamalle, C.; Oliveira, R.; Reid, J.; Gurney, A.M. Contractile and electrophysiological properties of pulmonary artery smooth muscle are not altered in TASK-1 knockout mice. J. Physiol. 2011, 589, 3231–3246. [Google Scholar] [CrossRef] [PubMed]
- Lambert, M.; Capuano, V.; Boet, A.; Tesson, L.; Bertero, T.; Nakhleh, M.K.; Remy, S.; Anegon, I.; Pechoux, C.; Hautefort, A.; et al. Characterization of Kcnk3 -Mutated Rat, a Novel Model of Pulmonary Hypertension. Circ. Res. 2019, 125, 678–695. [Google Scholar] [CrossRef]
- Bohnen, M.S.; Roman-Campos, D.; Terrenoire, C.; Jnani, J.; Sampson, K.J.; Chung, W.K.; Kass, R.S. The Impact of Heterozygous KCNK3 Mutations Associated With Pulmonary Arterial Hypertension on Channel Function and Pharmacological Recovery. J. Am. Hear. Assoc. 2017, 6, e006465. [Google Scholar] [CrossRef] [PubMed]
- Lambert, M.; Boet, A.; Rucker-Martin, C.; Mendes-Ferreira, P.; Capuano, V.; Hatem, S.; Adão, R.; Brás-Silva, C.; Hautefort, A.; Michel, J.-B.; et al. Loss of KCNK3 is a hallmark of RV hypertrophy/dysfunction associated with pulmonary hypertension. Cardiovasc. Res. 2018, 114, 880–893. [Google Scholar] [CrossRef]
- Schmidt, C.; Wiedmann, F.; Voigt, N.; Zhou, X.B.; Heijman, J.; Lang, S.; Albert, V.; Kallenberger, S.; Ruhparwar, A.; Szabo, G.; et al. Upregulation of K(2P)3.1 K+ Current Causes Action Potential Shortening in Patients with Chronic Atrial Fibrillation. Circulation 2015, 132, 82–92. [Google Scholar] [CrossRef] [PubMed]
- Chen, A.X.; Nishimoto, K.; Nanba, K.; Rainey, W.E. Potassium channels related to primary aldosteronism: Expression similarities and differences between human and rat adrenals. Mol. Cell. Endocrinol. 2015, 417, 141–148. [Google Scholar] [CrossRef]
- Chen, Y.; Zeng, X.; Huang, X.; Serag, S.; Woolf, C.J.; Spiegelman, B.M. Crosstalk between KCNK3-Mediated Ion Current and Adrenergic Signaling Regulates Adipose Thermogenesis and Obesity. Cell 2017, 171, 836–848. [Google Scholar] [CrossRef]
- Kanjhan, R.; Pow, D.V.; Noakes, P.G.; Bellingham, M.C. The two-pore domain K+ channel TASK-1 is closely associated with brain barriers and meninges. J. Mol. Histol. 2010, 41, 315–323. [Google Scholar] [CrossRef]
- Bittner, S.; Bauer, M.A.; Ehling, P.; Bobak, N.; Breuer, J.; Herrmann, A.M.; Golfels, M.; Wiendl, H.; Budde, T.; Meuth, S.G. The TASK1 channel inhibitor A293 shows efficacy in a mouse model of multiple sclerosis. Exp. Neurol. 2012, 238, 149–155. [Google Scholar] [CrossRef]
- Dadi, P.K.; Vierra, N.C.; Jacobson, D.A. Pancreatic beta-cell-specific ablation of TASK-1 channels augments glucose-stimulated calcium entry and insulin secretion, improving glucose tolerance. Endocrinology 2014, 155, 3757–3768. [Google Scholar] [CrossRef] [PubMed]
- Turner, P.J.; Buckler, K.J. Oxygen and mitochondrial inhibitors modulate both monomeric and heteromeric TASK-1 and TASK-3 channels in mouse carotid body type-1 cells. J. Physiol. 2013, 591, 5977–5998. [Google Scholar] [CrossRef] [PubMed]
- Park, S.J.; Chun, Y.-S.; Park, K.S.; Kim, S.J.; Choi, S.-O.; Kim, H.-L.; Park, J.-W. Identification of subdomains in NADPH oxidase-4 critical for the oxygen-dependent regulation of TASK-1 K+ channels. Am. J. Physiol. Physiol. 2009, 297, C855–C864. [Google Scholar] [CrossRef]
- Trapp, S.; Aller, M.I.; Wisden, W.; Gourine, A.V. A Role for TASK-1 (KCNK3) Channels in the Chemosensory Control of Breathing. J. Neurosci. 2008, 28, 8844–8850. [Google Scholar] [CrossRef] [PubMed]
- Michelakis, E.D.; Gurtu, V.; Webster, L.; Barnes, G.; Watson, G.; Howard, L.; Cupitt, J.; Paterson, I.; Thompson, R.B.; Chow, K.; et al. Inhibition of pyruvate dehydrogenase kinase improves pulmonary arterial hypertension in genetically susceptible patients. Sci. Transl. Med. 2017, 9, 413. [Google Scholar] [CrossRef]
- Prior, K.-K.; Leisegang, M.S.; Josipovic, I.; Löwe, O.; Shah, A.M.; Weissmann, N.; Schröder, K.; Brandes, R.P. CRISPR/Cas9-mediated knockout of p22phox leads to loss of Nox1 and Nox4, but not Nox5 activity. Redox Biol. 2016, 9, 287–295. [Google Scholar] [CrossRef]
- Chen, Y.-I.; Wei, P.-C.; Hsu, J.-L.; Su, F.-Y.; Lee, W.-H. NPGPx (GPx7): A novel oxidative stress sensor/transmitter with multiple roles in redox homeostasis. Am. J. Transl. Res. 2016, 8, 1626–1640. [Google Scholar]
- Tokunaga, R.; Zhang, W.; Naseem, M.; Puccini, A.; Berger, M.D.; Soni, S.; McSkane, M.; Baba, H.; Lenz, H.-J. CXCL9, CXCL10, CXCL11/CXCR3 axis for immune activation–a target for novel cancer therapy. Cancer Treat. Rev. 2018, 63, 40–47. [Google Scholar] [CrossRef] [PubMed]
- Sponaas, A.-M.; Yang, R.; Rustad, E.H.; Standal, T.; Thoresen, A.S.; Vo, C.D.; Waage, A.; Slørdahl, T.S.; Børset, M.; Sundan, A. PD1 is expressed on exhausted T cells as well as virus specific memory CD8+ T cells in the bone marrow of myeloma patients. Oncotarget 2018, 9, 32024–32035. [Google Scholar] [CrossRef]
- Lang, K.S.; Recher, M.; Navarini, A.A.; Harris, N.L.; Löhning, M.; Junt, T.; Probst, H.C.; Hengartner, H.; Zinkernagel, R.M. Inverse correlation between IL-7 receptor expression and CD8 T cell exhaustion during persistent antigen stimulation. Eur. J. Immunol. 2005, 35, 738–745. [Google Scholar] [CrossRef] [PubMed]
- Austin, E.; Rock, M.; Mosse, C.; Vnencak-Jones, C.; Yoder, S.; Robbins, I.; Loyd, J.; Meyrick, B. T lymphocyte subset abnormalities in the blood and lung in pulmonary arterial hypertension. Respir. Med. 2010, 104, 454–462. [Google Scholar] [CrossRef]
- Bryant, A.J.; Fu, C.; Lu, Y.; Brantly, M.L.; Mehrad, B.; Moldawer, L.L.; Brusko, T.M.; Brittain, E.L.; West, J.D.; Austin, E.D.; et al. A checkpoint on innate myeloid cells in pulmonary arterial hypertension. Pulm. Circ. 2018, 9. [Google Scholar] [CrossRef]
- Ross, D.J.; Strieter, R.M.; Fishbein, M.C.; Ardehali, A.; Belperio, J.A. Type I immune response cytokine–chemokine cascade is associated with pulmonary arterial hypertension. J. Hear. Lung Transplant. 2012, 31, 865–873. [Google Scholar] [CrossRef] [PubMed]
- Groom, J.R.; Luster, A.D. CXCR3 in T cell function. Exp. Cell Res. 2011, 317, 620–631. [Google Scholar] [CrossRef]
- Gerlach, C.; Moseman, E.A.; Loughhead, S.M.; Alvarez, D.; Zwijnenburg, A.J.; Waanders, L.; Garg, R.; Juan, C.; von Andrian, U.H. The chemokine receptor CX3CR1 defines three antigen-experienced CD8 T cell subsets with distinct roles in immune surveillance and homeostasis. Immunity 2016, 45, 1270–1284. [Google Scholar] [CrossRef]
- Fraticelli, P.; Sironi, M.; Bianchi, G.; D’Ambrosio, D.; Albanesi, C.; Stoppacciaro, A.; Chieppa, M.; Allavena, P.; Ruco, L.; Girolomoni, G.; et al. Fractalkine (CX3CL1) as an amplification circuit of polarized Th1 responses. J. Clin. Investig. 2001, 107, 1173–1181. [Google Scholar] [CrossRef]
- Balabanian, K.; Foussat, A.; Dorfmüller, P.; Durand-Gasselin, I.; Capel, F.; Bouchet-Delbos, L.; Portier, A.; Marfaing-Koka, A.; Krzysiek, R.; Rimaniol, A.-C.; et al. CX3C Chemokine Fractalkine in Pulmonary Arterial Hypertension. Am. J. Respir. Crit. Care Med. 2002, 165, 1419–1425. [Google Scholar] [CrossRef]
- Hirata, H.; Yukawa, T.; Tanaka, A.; Miyao, T.; Fukuda, T.; Fukushima, Y.; Kurasawa, K.; Arima, M. Th2 cell differentiation from naive CD 4+ T cells is enhanced by autocrine CC chemokines in atopic diseases. Clin. Exp. Allergy 2019, 49, 474–483. [Google Scholar] [CrossRef]
- Yoshie, O.; Matsushima, K. CCR4 and its ligands: From bench to bedside. Int. Immunol. 2015, 27, 11–20. [Google Scholar] [CrossRef]
- Daley, E.; Emson, C.; Guignabert, C.; Malefyt, R.D.W.; Louten, J.; Kurup, V.P.; Hogaboam, C.; Taraseviciene-Stewart, L.; Voelkel, N.F.; Rabinovitch, M.; et al. Pulmonary arterial remodeling induced by a Th2 immune response. J. Exp. Med. 2008, 205, 361–372. [Google Scholar] [CrossRef] [PubMed]
- Meng, Q.; Lai, Y.-C.; Kelly, N.J.; Bueno, M.; Baust, J.J.; Bachman, T.N.; Goncharov, D.; Vanderpool, R.R.; Radder, J.E.; Hu, J.; et al. Development of a Mouse Model of Metabolic Syndrome, Pulmonary Hypertension, and Heart Failure with Preserved Ejection Fraction. Am. J. Respir. Cell Mol. Biol. 2017, 56, 497–505. [Google Scholar] [CrossRef] [PubMed]
- West, J.; Niswender, K.D.; Johnson, J.A.; Pugh, M.E.; Gleaves, L.; Fessel, J.P.; Hemnes, A.R. A potential role for insulin resistance in experimental pulmonary hypertension. Eur. Respir. J. 2013, 41, 861–871. [Google Scholar] [CrossRef] [PubMed]
- Stenmark, K.R.; Morganroth, M.L.; Remigio, L.K.; Voelkel, N.F.; Murphy, R.C.; Henson, P.M.; Mathias, M.M.; Reeves, J.T. Alveolar inflammation and arachidonate metabolism in monocrotaline-induced pulmonary hypertension. Am. J. Physiol. Circ. Physiol. 1985, 248, H859–H866. [Google Scholar] [CrossRef]
- Cool, C.D.; Rai, P.R.; Yeager, M.E.; Hernandez-Saavedra, D.; Serls, A.E.; Bull, T.M.; Geraci, M.W.; Brown, K.K.; Routes, J.M.; Tuder, R.M.; et al. Expression of Human Herpesvirus 8 in Primary Pulmonary Hypertension. N. Engl. J. Med. 2003, 349, 1113–1122. [Google Scholar] [CrossRef] [PubMed]
- Liao, J.K. Linking endothelial dysfunction with endothelial cell activation. J. Clin. Investig. 2013, 123, 540–541. [Google Scholar] [CrossRef] [PubMed]
- Jacobson, D.A.; Shyng, S.-L. Ion channels of the islets in type 2 diabetes. J. Mol. Biol. 2020, 432, 1326–1346. [Google Scholar] [CrossRef]
- Li, W.; Dunmore, B.J.; Morrell, N.W. Bone Morphogenetic Protein Type II Receptor Mutations Causing Protein Misfolding in Heritable Pulmonary Arterial Hypertension. Proc. Am. Thorac. Soc. 2010, 7, 395–398. [Google Scholar] [CrossRef]
- Austin, E.D.; Menon, S.; Hemnes, A.R.; Robinson, L.R.; Talati, M.; Fox, K.L.; Cogan, J.D.; Hamid, R.; Hedges, L.K.; Robbins, I.; et al. Idiopathic and Heritable PAH Perturb Common Molecular Pathways, Correlated with Increased MSX1 Expression. Pulm. Circ. 2011, 1, 389–398. [Google Scholar] [CrossRef]
- Young, K.A.; Ivester, C.; West, J.; Carr, M.; Rodman, D.M. BMP signaling controls PASMC KV channel expression in vitro and in vivo. Am. J. Physiol. Cell. Mol. Physiol. 2006, 290, L841–L848. [Google Scholar] [CrossRef]
- Dromparis, P.; Paulin, R.; Stenson, T.H.; Haromy, A.; Sutendra, G.; Michelakis, E.D. Attenuating Endoplasmic Reticulum Stress as a Novel Therapeutic Strategy in Pulmonary Hypertension. Circulation 2013, 127, 115–125. [Google Scholar] [CrossRef]
- Dromparis, P.; Paulin, R.; Sutendra, G.; Qi, A.C.; Bonnet, S.; Michelakis, E.D.; Konstandin, M.H.; Toko, H.; Gastelum, G.M.; Quijada, P.; et al. Uncoupling Protein 2 Deficiency Mimics the Effects of Hypoxia and Endoplasmic Reticulum Stress on Mitochondria and Triggers Pseudohypoxic Pulmonary Vascular Remodeling and Pulmonary Hypertension. Circ. Res. 2013, 113, 126–136. [Google Scholar] [CrossRef]
- Salminen, A.; Kaarniranta, K.; Kauppinen, A. ER stress activates immunosuppressive network: Implications for aging and Alzheimer’s disease. J. Mol. Med. 2020, 98, 633–650. [Google Scholar] [CrossRef]
- Díaz-Bulnes, P.; Saiz, M.L.; López-Larrea, C.; Rodríguez, R.M. Crosstalk Between Hypoxia and ER Stress Response: A Key Regulator of Macrophage Polarization. Front. Immunol. 2020, 10, 2951. [Google Scholar] [CrossRef]
- Bantug, G.R.; Fischer, M.; Grählert, J.; Balmer, M.L.; Unterstab, G.; Develioglu, L.; Steiner, R.; Zhang, L.; Costa, A.S.; Gubser, P.M. Mitochondria-endoplasmic reticulum contact sites function as immunometabolic hubs that orchestrate the rapid recall response of memory CD8+ T cells. Immunity 2018, 48, 542–555. [Google Scholar] [CrossRef] [PubMed]
- Rabinovitch, M.; Guignabert, C.; Humbert, M.; Nicolls, M.R. Inflammation and Immunity in the Pathogenesis of Pulmonary Arterial Hypertension. Circ. Res. 2014, 115, 165–175. [Google Scholar] [CrossRef]
- Fisher, D.T.; Appenheimer, M.M.; Evans, S.S. The two faces of IL-6 in the tumor microenvironment. Semin. Immunol. 2014, 26, 38–47. [Google Scholar] [CrossRef]
- Graham, B.B.; Chabon, J.; Kumar, R.; Kolosionek, E.; Gebreab, L.; Debella, E.; Edwards, M.; Diener, K.; Shade, T.; Bifeng, G.; et al. Protective role of IL-6 in vascular remodeling in Schistosoma pulmonary hypertension. Am. J. Respir. Cell. Mol. Biol. 2013, 49, 951–959. [Google Scholar] [CrossRef] [PubMed]
- Bittner, S.; Meuth, S.G.; Göbel, K.; Melzer, N.; Herrmann, A.M.; Simon, O.J.; Weishaupt, A.; Budde, T.; Bayliss, D.A.; Bendszus, M.; et al. TASK1 modulates inflammation and neurodegeneration in autoimmune inflammation of the central nervous system. Brain 2009, 132, 2501–2516. [Google Scholar] [CrossRef] [PubMed]
- Meuth, S.G.; Bittner, S.; Meuth, P.; Simon, O.J.; Budde, T.; Wiendl, H. TWIK-related Acid-sensitive K+ Channel 1 (TASK1) and TASK3 Critically Influence T Lymphocyte Effector Functions. J. Biol. Chem. 2008, 283, 14559–14570. [Google Scholar] [CrossRef]
- Zhuang, Q.; Ou, J.; Zhang, S.; Ming, Y. Crosstalk between the CX3CL1/CX3CR1 Axis and Inflammatory Signaling Pathways in Tissue Injury. Curr. Protein Pept. Sci. 2019, 20, 844–854. [Google Scholar] [CrossRef] [PubMed]
- Zabini, D.; Nagaraj, C.; Stacher, E.; Lang, I.M.; Nierlich, P.; Klepetko, W.; Heinemann, A.; Olschewski, H.; Balint, Z.; Olschewski, A. Angiostatic factors in the pulmonary endarterectomy material from chronic thromboembolic pulmonary hypertension patients cause endothelial dysfunction. PLoS ONE. 2012, 7, e43793. [Google Scholar] [CrossRef]
- Zhang, J.; Hu, H.; Palma, N.L.; Harrison, J.K.; Mubarak, K.K.; Carrie, R.D.; Alnuaimat, H.; Shen, X.; Luo, D.; Patel, J.M. Hypoxia-induced endothelial CX3CL1 triggers lung smooth muscle cell phenotypic switching and proliferative expansion. Am. J. Physiol. Lung Cell. Mol. Physiol. 2012. [CrossRef]
- Arger, N.K.; Machiraju, S.; Allen, I.E.; Woodruff, P.G.; Koth, L.L. T-bet Expression in Peripheral Th17.0 Cells Is Associated with Pulmonary Function Changes in Sarcoidosis. Front. Immunol. 2020, 11, 1129. [Google Scholar] [CrossRef] [PubMed]
- Hemnes, A.R.; Rathinasabapathy, A.; Austin, E.A.; Brittain, E.L.; Carrier, E.J.; Chen, X.; Fessel, J.P.; Fike, C.D.; Fong, P.; Fortune, N.; et al. A potential therapeutic role for angiotensin-converting enzyme 2 in human pulmonary arterial hypertension. Eur. Respir. J. 2018, 51, 1702638. [Google Scholar] [CrossRef]
- Yan, L.; Chen, X.; Talati, M.; Nunley, B.W.; Gladson, S.; Blackwell, T.; Cogan, J.; Austin, E.; Wheeler, F.; Loyd, J.; et al. Bone Marrow–derived Cells Contribute to the Pathogenesis of Pulmonary Arterial Hypertension. Am. J. Respir. Crit. Care Med. 2016, 193, 898–909. [Google Scholar] [CrossRef]
- Rathinasabapathy, A.; Copeland, C.; Crabtree, A.L.; Carrier, E.J.; Moore, C.S.; Shay, S.D.; Gladson, S.; Austin, E.D.; Kenworthy, A.K.; Loyd, J.E. Expression of a Human Caveolin-1 Mutation in Mice Drives Inflammatory and Metabolic Defect-Associated Pulmonary Arterial Hypertension. Front. Med. 2020, 7, 540. [Google Scholar] [CrossRef]
- Rathinasabapathy, A.; Horowitz, A.; Horton, K.; Kumar, A.; Gladson, S.; Unger, T.; Martinez, D.; Bedse, G.; West, J.; Raizada, M.K.; et al. The Selective Angiotensin II Type 2 Receptor Agonist, Compound 21, Attenuates the Progression of Lung Fibrosis and Pulmonary Hypertension in an Experimental Model of Bleomycin-Induced Lung Injury. Front. Physiol. 2018, 9, 180. [Google Scholar] [CrossRef] [PubMed]
- West, J.D.; Austin, E.D.; Gaskill, C.; Marriott, S.; Baskir, R.; Bilousova, G.; Jean, J.-C.; Hemnes, A.R.; Menon, S.; Bloodworth, N.C.; et al. Identification of a common Wnt-associated genetic signature across multiple cell types in pulmonary arterial hypertension. Am. J. Physiol. Physiol. 2014, 307, C415–C430. [Google Scholar] [CrossRef] [PubMed]
- Leelatian, N.; Diggins, K.E.; Irish, J.M. Characterizing phenotypes and signaling networks of single human cells by mass cytometry. Methods Mol. Biol. 2015, 1346, 99–113. [Google Scholar] [CrossRef] [PubMed]

| Control-1 | Control-2 | KCNK3 | |
|---|---|---|---|
| CD73 (%) | 100 | 100 | 99.9 |
| CD44 (%) | 99.9 | 100 | 99.8 |
| ABCG2 (%) | 1.59 | 0.032 | 1.41 |
| CD45 (%) | 0.096 | 0.13 | 0.19 |
| CD144 (%) | 1.00 | 0.026 | 0.15 |
| CD105 (%) | 99.4 | 99.9 | 99.9 |
| CD14 (%) | 0.069 | 0.13 | 0.03 |
| CD31 (%) | 0.00 | 0.16 | 0.00 |
| CD34 (%) | 1.00 | 0.00 | 0.076 |
| CD146 (%) | 84.00 | 99.7 | 99.5 |
| CD146a (%) | 0.014 | 0.00 | 0.032 |
| Cell Type | UBC-Cre/ERT2 | kcnk3fl/fl | p Value |
|---|---|---|---|
| LT HSC | 228 | 300 | |
| ST HSC | 2007 | 3727 | 0.0089 |
| MPP | 1039 | 1701 | |
| LSK | 3397 | 4799 | 0.0498 |
| MEP% | 0.5 | 0.3 | |
| CMP% | 45.1 | 50.2 | |
| GMP% | 47.5 | 42.4 | |
| B220% | 15.9 | 14.0 | |
| Mac-1% | 1.6 | 1.3 | 0.0308 |
| Mac+Gr1% | 62.0 | 60.9 | |
| Gr1% | 6.6 | 6.7 | |
| CD4+% | 1.4 | 1.6 | |
| CD8+% | 1.3 | 1.3 | |
| CD4+CD+8% | 0.1 | 0.1 |
| Control | +LPS | Ratio fl/fl:Control | ||||
|---|---|---|---|---|---|---|
| UBC-Cre/ERT2 | kcnk3fl/fl | UBC-Cre/ERT2 | kcnk3fl/fl | Control | +LPS | |
| C4/C5a | 1148 | 911 | 826 | 1145 | 0.8 | 1.4 |
| CCL12/MCP-5 | 157 | 124 | 152 | 590 | 0.8 | 3.9 |
| CCL2/MCP-1 | 1370 | 1158 | 489 | 1917 | 0.8 | 3.9 |
| CCL3/MIP-1a | 341 | 217 | 248 | 557 | 0.6 | 2.3 |
| CCL4/MIP-1b | 140 | 181 | 120 | 72 | 1.3 | 0.6 |
| CXCL1 | 781 | 1370 | 495 | 1010 | 1.8 | 2.0 |
| CXCL10/CRG-2 | 1050 | 526 | 770 | 8381 | 0.5 | 10.9 |
| CXCL11/I-TAC | 496 | 230 | 230 | 398 | 0.5 | 1.7 |
| CXCL12/MIP-2 | 163 | 165 | 130 | 194 | 1.0 | 1.5 |
| CXCL13/BCA-1/BLC | 489 | 267 | 254 | 1470 | 0.5 | 5.8 |
| CXCL9/MIG | 389 | 240 | 454 | 4791 | 0.6 | 10.6 |
| IL-10 | 813 | 312 | 677 | 674 | 0.4 | 1.0 |
| IL-13 | 6830 | 7231 | 5083 | 1938 | 1.1 | 0.4 |
| IL-16 | 5305 | 5922 | 3640 | 5415 | 1.1 | 1.5 |
| IL-17 | 463 | 251 | 356 | 1209 | 0.5 | 3.4 |
| IL-1ra/IL-1F3 | 709 | 701 | 1101 | 4138 | 1.0 | 3.8 |
| IL-23 | 557 | 328 | 536 | 1308 | 0.6 | 2.4 |
| IL-27 | 934 | 488 | 697 | 1132 | 0.5 | 1.6 |
| IL-3 | 3269 | 2358 | 2533 | 5727 | 0.7 | 2.3 |
| IL-4 | 3880 | 3133 | 3464 | 5065 | 0.8 | 1.5 |
| IL-5 | 837 | 95 | 529 | 535 | 0.1 | 1.0 |
| IL-6 | 1420 | 106 | 374 | 317 | 0.1 | 0.8 |
| IL-7 | 4281 | 2131 | 2610 | 2610 | 0.5 | 1.0 |
| M-CSF | 1212 | 623 | 506 | 453 | 0.5 | 0.9 |
| RANTES/CCL5 | 2587 | 2735 | 3020 | 7692 | 1.1 | 2.5 |
| SDF-1 | 2605 | 2161 | 1930 | 4607 | 0.8 | 2.4 |
| sICAM-1 | 8730 | 7482 | 8075 | 7720 | 0.9 | 1.0 |
| TIMP-1 | 4639 | 3397 | 3444 | 13,502 | 0.7 | 3.9 |
| TNFa | 1932 | 2628 | 2699 | 3094 | 1.4 | 1.1 |
| TREM-1 | 10,167 | 11,872 | 6342 | 8302 | 1.2 | 1.3 |
| Target | Healthy Volunteers | KCNK3 HPAH Patients | p Value |
|---|---|---|---|
| ITAC | 21.0 ± 6.6 | 35.3 ± 4.6 | 0.31 |
| Fractalkine (CX3CL1) | 52.7 ± 4.6 | 118.3 ± 13.1 | <0.01 |
| IFNγ | 5.4 ± 0.7 | 11.8 ± 3.1 | 0.01 |
| IL10 | 3.3 ± 1.9 | 10.0 ± 0.7 | 0.12 |
| IL13 | 4.0 ± 1.7 | 12.3 ± 9.9 | 0.17 |
| IL17 | 4.8 ± 0.5 | 9.5 ± 3.4 | 0.03 |
| IL1β | 0.5 ± 0.0 | 1.1 ± 0.0 | <0.01 |
| IL6 | 1.0 ± 0.4 | 2.8 ± 0.5 | 0.05 |
| MIP1α | 2.6 ± 0.8 | 11.3 ± 9.5 | 0.08 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
West, J.D.; Austin, E.D.; Rizzi, E.M.; Yan, L.; Tanjore, H.; Crabtree, A.L.; Moore, C.S.; Muthian, G.; Carrier, E.J.; Jacobson, D.A.; et al. KCNK3 Mutation Causes Altered Immune Function in Pulmonary Arterial Hypertension Patients and Mouse Models. Int. J. Mol. Sci. 2021, 22, 5014. https://doi.org/10.3390/ijms22095014
West JD, Austin ED, Rizzi EM, Yan L, Tanjore H, Crabtree AL, Moore CS, Muthian G, Carrier EJ, Jacobson DA, et al. KCNK3 Mutation Causes Altered Immune Function in Pulmonary Arterial Hypertension Patients and Mouse Models. International Journal of Molecular Sciences. 2021; 22(9):5014. https://doi.org/10.3390/ijms22095014
Chicago/Turabian StyleWest, James D., Eric D. Austin, Elise M. Rizzi, Ling Yan, Harikrishna Tanjore, Amber L. Crabtree, Christy S. Moore, Gladson Muthian, Erica J. Carrier, David A. Jacobson, and et al. 2021. "KCNK3 Mutation Causes Altered Immune Function in Pulmonary Arterial Hypertension Patients and Mouse Models" International Journal of Molecular Sciences 22, no. 9: 5014. https://doi.org/10.3390/ijms22095014
APA StyleWest, J. D., Austin, E. D., Rizzi, E. M., Yan, L., Tanjore, H., Crabtree, A. L., Moore, C. S., Muthian, G., Carrier, E. J., Jacobson, D. A., Hamid, R., Kendall, P. L., Majka, S., & Rathinasabapathy, A. (2021). KCNK3 Mutation Causes Altered Immune Function in Pulmonary Arterial Hypertension Patients and Mouse Models. International Journal of Molecular Sciences, 22(9), 5014. https://doi.org/10.3390/ijms22095014







