(Pro)renin Receptor Is Present in Human Sperm and It Adversely Affects Sperm Fertility Ability
Abstract
1. Introduction
2. Results
2.1. Patients and Seminal Samples
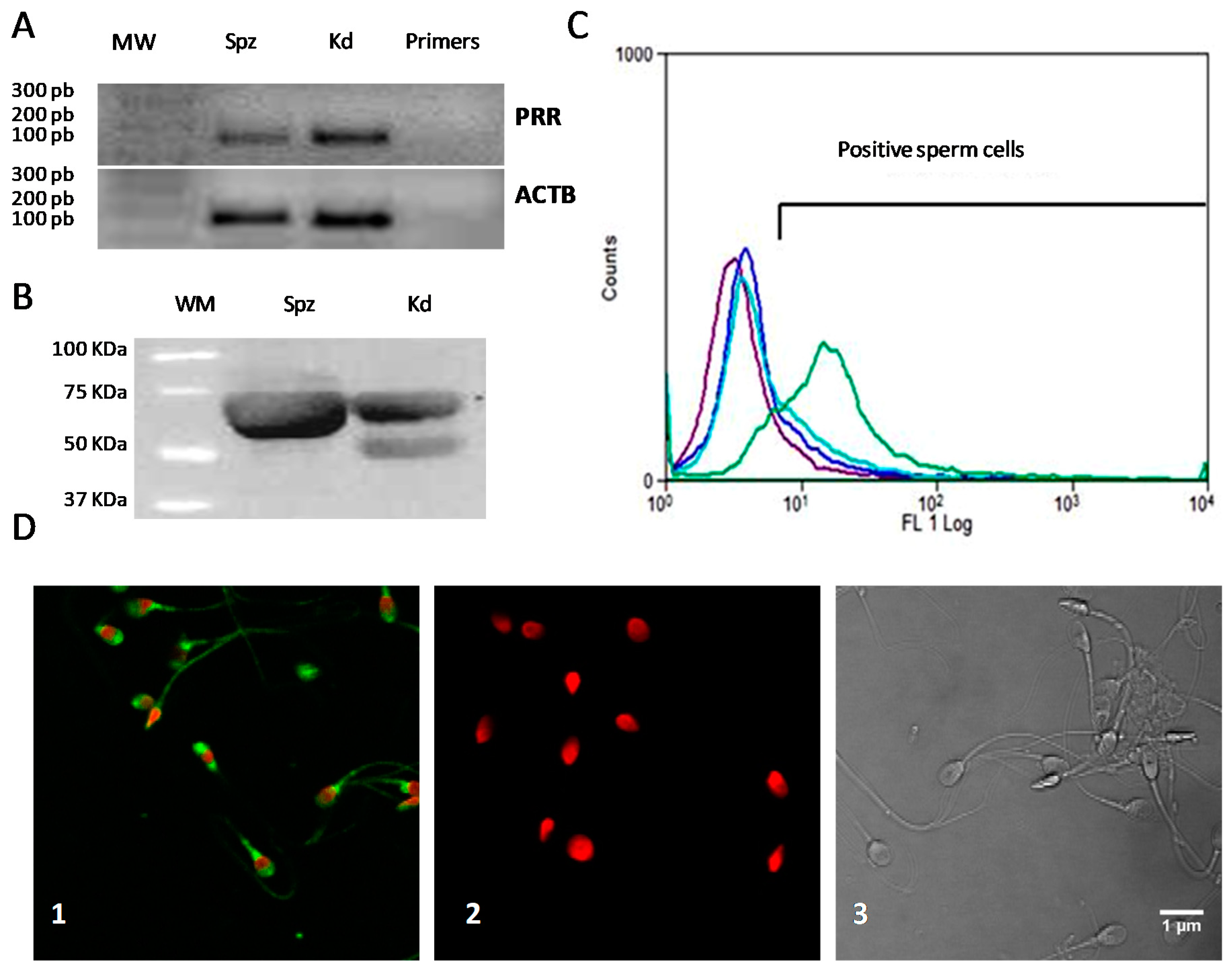
2.2. Expression and Localization of PRR in Human Sperm
2.3. Correlation between PRR with Basic Sperm Parameters
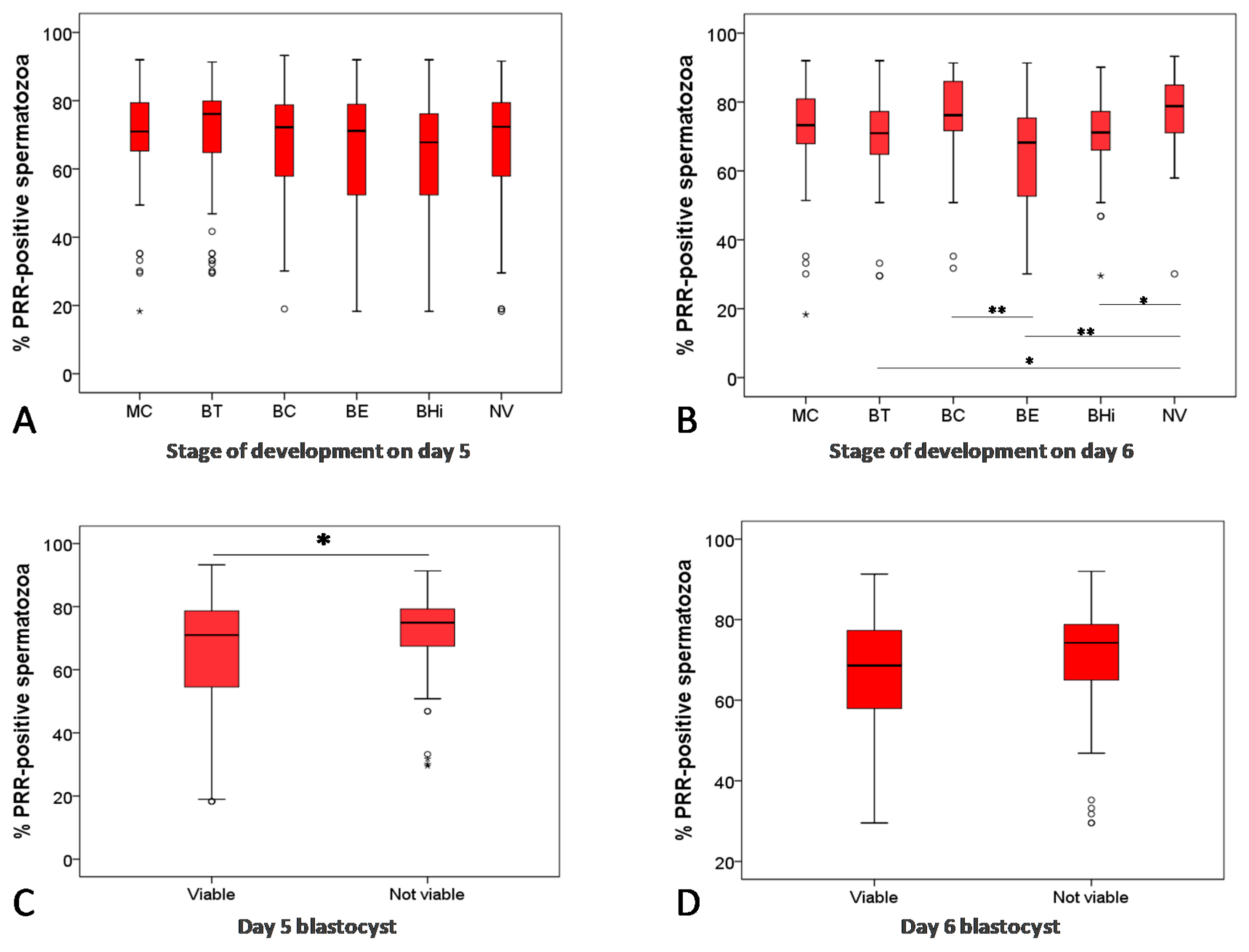
2.4. Percentage of PRR-Positive Sperm Cells and Fertilization and Embryo Quality
2.5. Percentage of PRR-Positive Sperm Cells and Embryo Transfer, Clinical Pregnancy and Live-Birth Outcomes
3. Discussion
4. Materials and Methods
4.1. Ethical Approval
4.2. Patients and Semen Analysis
4.3. Reverse Transcription-Polymerase Chain Reaction Analysis
4.4. Western Blotting
4.5. Flow Cytometry
4.6. Immunofluorescence
4.7. Assisted Reproductive Technology Procedures
4.8. Fertilization Rates, Embryo Quality, Transference, Biochemical and Clinical Pregnancy and Live-Birth Outcome
4.9. Statistical Analysis
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ACE | Angiotensin Converting Enzyme |
| ACTB | Beta-actin |
| ART | Assisted Reproductive Techniques |
| ASEBIR | Spanish Association of Reproduction Biology Studies |
| BC | Expanding blastocysts |
| BD | Blocked or degenerated blastocysts |
| BE | Expanded blastocysts |
| BHi | Hatching or hatched blastocysts |
| BT | Early blastocysts |
| ICSI | Intracitoplasmatic sperm injection |
| IM | Non-motile spermatozoa |
| IVF | In vitro fertilization |
| MC | Morula stage |
| NP | Spermatozoa with non-progressive motility |
| NV | Non-viable blastocysts |
| PR | Spermatozoa with progressive motility |
| PRR | (Pro)renin receptor |
| RAS | Renin-angiotensin system |
| V | Viable blastocysts |
| WHO | World Health Organization |
References
- Inhorn, M.C.; Patrizio, P. Infertility around the globe: New thinking on gender, reproductive technologies and global movements in the 21st century. Hum. Reprod. Updat. 2015, 21, 411–426. [Google Scholar] [CrossRef] [PubMed]
- Larson-Cook, K.L.; Brannian, J.D.; Hansen, K.A.; Kasperson, K.M.; Aamold, E.T.; Evenson, D.P. Relationship between the outcomes of assisted reproductive techniques and sperm DNA fragmentation as measured by the sperm chromatin structure assay. Fertil. Steril. 2003, 80, 895–902. [Google Scholar] [CrossRef]
- Janny, L.; Menezo, Y.J.R. Evidence for a strong paternal effect on human preimplantation embryo development and blastocyst formation. Mol. Reprod. Dev. 1994, 38, 36–42. [Google Scholar] [CrossRef]
- Liu, D.Y.; Baker, H.W.G. Disordered zona pellucida–induced acrosome reaction and failure of in vitro fertilization in patients with unexplained infertility. Fertil. Steril. 2003, 79, 74–80. [Google Scholar] [CrossRef]
- Meseguer, M.; Pellicer, A.; Garrido, N.; Martínez-Conejero, J.A.; Simón, C.; Remohí, J. Relationship Between Standard Semen Parameters, Calcium, Cholesterol Contents, and Mitochondrial Activity in Ejaculated Spermatozoa From Fertile and Infertile Males. J. Assist. Reprod. Genet. 2004, 21, 445–451. [Google Scholar] [CrossRef]
- Krawetz, S.A. Paternal contribution: New insights and future challenges. Nat. Rev. Genet. 2005, 6, 633–642. [Google Scholar] [CrossRef] [PubMed]
- Barroso, G.; Valdespin, C.; Vega, E.; Kershenovich, R.; Avila, R.; Avendaño, C.; Oehninger, S. Developmental sperm contributions: Fertilization and beyond. Fertil. Steril. 2009, 92, 835–848. [Google Scholar] [CrossRef] [PubMed]
- Govindaraju, A.; Dogan, S.; Rodriguez-Osorio, N.; Grant, K.; Kaya, A.; Memili, E. Delivering value from sperm proteomics for fertility. Cell Tissue Res. 2012, 349, 783–793. [Google Scholar] [CrossRef] [PubMed]
- Sakkas, D.; Ramalingam, M.; Garrido, N.; Barratt, C.L. Sperm selection in natural conception: What can we learn from Mother Nature to improve assisted reproduction outcomes? Hum. Reprod. Updat. 2015, 21, 711–726. [Google Scholar] [CrossRef]
- Subirán, N.; Casis, L.; Irazusta, J. Regulation of Male Fertility by the Opioid System. Mol. Med. 2011, 17, 846–853. [Google Scholar] [CrossRef] [PubMed]
- Pinto, F.M.; Ravina, C.G.; Subiran, N.; Cejudo-Román, A.; Fernández-Sánchez, M.; Irazusta, J.; Garrido, N.; Candenas, M.L. Autocrine regulation of human sperm motility by tachykinins. Reprod. Biol. Endocrinol. 2010, 8, 104. [Google Scholar] [CrossRef]
- Gianzo, M.; Muñoa-Hoyos, I.; Urizar-Arenaza, I.; Larreategui, Z.; Quintana, F.; Garrido, N.; Subirán, N.; Irazusta, J. Angiotensin II type 2 receptor is expressed in human sperm cells and is involved in sperm motility. Fertil. Steril. 2016, 105, 608–616. [Google Scholar] [CrossRef] [PubMed]
- Subirán, N.; Gianzo, M.; Urizar-Arenaza, I.; Muñoa-Hoyos, I.; Larreategui, Z.; Garrido, N.; Casis, L.; Irazusta, J. Human sperm testicular angiotensin-converting enzyme helps determine human embryo quality. Asian J. Androl. 2018, 20, 498–504. [Google Scholar] [CrossRef] [PubMed]
- Gianzo, M.; Subirán, N. Regulation of Male Fertility by the Renin-Angiotensin System. Int. J. Mol. Sci. 2020, 21, 7943. [Google Scholar] [CrossRef] [PubMed]
- Paul, M.; Mehr, A.P.; Kreutz, R. Physiology of Local Renin-Angiotensin Systems. Physiol. Rev. 2006, 86, 747–803. [Google Scholar] [CrossRef] [PubMed]
- Pandey, K.N.; Misono, K.S.; Inagami, T. Evidence for intracellular formation of angiotensins: Coexistence of renin and angiotensin-converting enzyme in Leydig cells of rat testis. Biochem. Biophys. Res. Commun. 1984, 122, 1337–1343. [Google Scholar] [CrossRef]
- Tumova, L.; Zigo, M.; Sutovsky, P.; Sedmikova, M.; Postlerova, P. Ligands and Receptors Involved in the Sperm-Zona Pellucida Interactions in Mammals. Cells 2021, 10, 133. [Google Scholar] [CrossRef] [PubMed]
- Fyhrquist, F.; Saijonmaa, O. Renin-angiotensin system revisited. J. Intern. Med. 2008, 264, 224–236. [Google Scholar] [CrossRef] [PubMed]
- Re, R.N. Intracellular Renin and the Nature of Intracrine Enzymes. Hypertension 2003, 42, 117–122. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, G.; Delarue, F.; Burckle, C.; Bouzhir, L.; Giller, T.; Sraer, J.D. Pivotal Role of the renin/prorenin Receptor in Angiotensin II Production and Cellular Responses to Renin. J. Clin. Investig. 2002, 109, 1417–1427. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, G. Renin, (pro)renin and receptor: An update. Clin. Sci. 2010, 120, 169–178. [Google Scholar] [CrossRef] [PubMed]
- Speth, R.C.; Daubert, D.L.; Grove, K.L. Angiotensin II: A Reproductive Hormone Too? Regul. Pept. 1999, 79, 25–40. [Google Scholar] [CrossRef]
- Craven, D.J.; Warren, A.Y.; Symonds, E.M. Active and Inactive Renin in Human Seminal Plasma. Arch. Androl. 1981, 7, 63–67. [Google Scholar] [CrossRef] [PubMed]
- Mukhopadhyay, A.K.; Cobilanschi, J.; Schulze, W.; Brunswig-Spickenheier, B.; Leidenberger, F.A. Human seminal fluid contains significant quantities of prorenin: Its correlation with the sperm density. Mol. Cell. Endocrinol. 1995, 109, 219–224. [Google Scholar] [CrossRef]
- WHO. WHO Laboratory Manual for the Examination and Processing of Human Semen, 5th ed.; World Health Organization: Geneva, Switzerland, 2010; Available online: https://www.who.int/publications/i/item/9789241547789 (accessed on 15 February 2021).
- Ostermeier, G.C.; Goodrich, R.J.; Diamond, M.P.; Dix, D.J.; Krawetz, S.A. Toward using stable spermatozoal RNAs for prognostic assessment of male factor fertility. Fertil. Steril. 2005, 83, 1687–1694. [Google Scholar] [CrossRef]
- Miller, D.; Ostermeier, G.C. Spermatozoal RNA: Why is it there and what does it do? Gynecol. Obstet. Fertil. 2006, 34, 840–846. [Google Scholar] [CrossRef] [PubMed]
- Boerke, A.; Dieleman, S.; Gadella, B. A possible role for sperm RNA in early embryo development. Theriogenology 2007, 68, S147–S155. [Google Scholar] [CrossRef]
- Ostermeier, G.C.; Miller, D.; Huntriss, J.D.; Diamond, M.P.; Krawetz, S.A. Reproductive Biology: Delivering Spermatozoan RNA to the Oocyte. Nature 2004, 429, 154. [Google Scholar] [CrossRef]
- Miller, D.; Ostermeier, G.C.; Krawetz, S.A. The controversy, potential and roles of spermatozoal RNA. Trends Mol. Med. 2005, 11, 156–163. [Google Scholar] [CrossRef]
- Yoshikawa, A.; Aizaki, Y.; Kusano, K.-I.; Kishi, F.; Susumu, T.; Iida, S.; Ishiura, S.; Nishimura, S.; Shichiri, M.; Senbonmatsu, T. The (pro)renin receptor is cleaved by ADAM19 in the Golgi leading to its secretion into extracellular space. Hypertens. Res. 2011, 34, 599–605. [Google Scholar] [CrossRef]
- Clavreul, N.; Sansilvestri-Morel, P.; Magard, D.; Verbeuren, T.J.; Rupin, A. (Pro)renin promotes fibrosis gene expression in HEK cells through a Nox4-dependent mechanism. Am. J. Physiol. Physiol. 2011, 300, F1310–F1318. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, H.; Kaneko, K.; Ohba, K.; Morimoto, R.; Hirose, T.; Satoh, F.; Totsune, K.; Takahashi, K. Increased expression of (pro)renin receptor in aldosterone-producing adenomas. Peptide 2013, 49, 68–73. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, G.; Muller, D.N. The Biology of the (Pro)Renin Receptor. J. Am. Soc. Nephrol. 2009, 21, 18–23. [Google Scholar] [CrossRef] [PubMed]
- Naz, R.K.; Sellamuthu, R. Receptors in Spermatozoa: Are They Real? J. Androl. 2006, 27, 627–636. [Google Scholar] [CrossRef]
- Meseguer, M.; de los Santos, M.J.; Simón, C.; Pellicer, A.; Remohí, J.; Garrido, N. Effect of sperm glutathione peroxidases 1 and 4 on embryo asymmetry and blastocyst quality in oocyte donation cycles. Fertil. Steril. 2006, 86, 1376–1385. [Google Scholar] [CrossRef] [PubMed]
- Aboutorabi, R.; Mazani, F.; Rafiee, L. Evaluation of CD52 Positive Sperms in Subfertile Human Semen Samples: Is there any Relationship with Main Semen Parameters? Adv. Biomed. Res. 2014, 3, 124–9175. [Google Scholar] [CrossRef] [PubMed]
- Subirán, N.; Pinto, F.M.; Agirregoitia, E.; Candenas, L.; Irazusta, J. Control of APN/CD13 and NEP/CD10 on sperm motility. Asian J. Androl. 2010, 12, 899–902. [Google Scholar] [CrossRef] [PubMed]
- Agirregoitia, E.; Valdivia, A.; Carracedo, A.; Casis, L.; Gil, J.; Subiran, N.; Ochoa, C.; Irazusta, J. Expression and Localization of Delta-, Kappa-, and Mu-Opioid Receptors in Human Spermatozoa and Implications for Sperm Motility. J. Clin. Endocrinol. Metab. 2006, 91, 4969–4975. [Google Scholar] [CrossRef] [PubMed]
- Bhilawadikar, R.; Zaveri, K.; Mukadam, L.; Naik, S.; Kamble, K.; Modi, D.; Hinduja, I. Levels of Tektin 2 and CatSper 2 in normozoospermic and oligoasthenozoospermic men and its association with motility, fertilization rate, embryo quality and pregnancy rate. J. Assist. Reprod. Genet. 2013, 30, 513–523. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Machtinger, R.; Racowsky, C. Morphological systems of human embryo assessment and clinical evidence. Reprod. Biomed. Online 2013, 26, 210–221. [Google Scholar] [CrossRef] [PubMed]
- Balakumar, P.; Jagadeesh, G. Potential cross-talk between (pro)renin receptors and Wnt/frizzled receptors in cardiovascular and renal disorders. Hypertens. Res. 2011, 34, 1161–1170. [Google Scholar] [CrossRef] [PubMed]
- Binger, K.J.; Muller, D.N. Autophagy and the (Pro)renin Receptor. Front. Endocrinol. 2013, 4, 155. [Google Scholar] [CrossRef] [PubMed]
- Aarabi, M.; Balakier, H.; Bashar, S.; Moskovtsev, S.I.; Sutovsky, P.; Librach, C.L.; Oko, R. Sperm content of postacrosomal WW binding protein is related to fertilization outcomes in patients undergoing assisted reproductive technology. Fertil. Steril. 2014, 102, 440–447. [Google Scholar] [CrossRef]
- Ferri, N.; Greco, C.M.; Maiocchi, G.; Corsini, A. Aliskiren reduces prorenin receptor expression and activity in cultured human aortic smooth muscle cells. J. Renin Angiotensin Aldosterone Syst. 2011, 12, 469–474. [Google Scholar] [CrossRef] [PubMed]
- Muñoz, E.; Fernandez, I.; Martinez, M.; Tocino, A.; Portela, S.; Pellicer, A.; García-Velasco, J.A.; Garrido, N. Oocyte donation outcome after oncological treatment in cancer survivors. Fertil. Steril. 2015, 103, 205–213. [Google Scholar] [CrossRef] [PubMed]
- Palermo, G.; Joris, H.; Devroey, P.; Van Steirteghem, A.C. Pregnancies after Intracytoplasmic Injection of Single Spermatozoon into an Oocyte. Lancet 1992, 340, 17–18. [Google Scholar] [CrossRef]
- ASEBIR. Cuadernos De Embriología Clínica II. In Criterios ASEBIR De Valoración Morfológica De Oocitos, Embriones Tempranos y Blastocistos Humanos, 2nd ed.; Góbalo: Madrid, Spain, 2008. [Google Scholar]
- Alpha Scientists in Reproductive Medicine and ESHRE Special Interest Group of Embryology. The Istanbul Consensus Workshop on Embryo Assessment: Proceedings of an Expert Meeting. Hum. Reprod. 2011, 26, 1270–1283. [Google Scholar] [CrossRef]
| Seminal Parameters | Fresh Samples | Processed Samples |
|---|---|---|
| Volume (mL) | 2.99 ± 0.15 | 0.76 ± 0.02 |
| Sperm concentration (×106 spz/mL) | 75.31 ± 4.05 | 14.86 ± 1.19 |
| Total sperm count (×106 spz) | 205.94 ± 13.45 | 11.99 ± 1.13 |
| Progressive motility (%) | 54.42 ± 1.75 | 94.67 ± 0.49 |
| Non-motile spermatozoa (%) | 37.87 ± 1.49 | 4.54 ± 0.49 |
| Fresh Samples | Processed Samples | |||
|---|---|---|---|---|
| Total sperm count | Correlation coefficient | 0.043 | −0.257 * | |
| p value | 0.676 | 0.011 | ||
| Concentration | Correlation coefficient | −0.091 | −0.259 * | |
| p value | 0.373 | 0.010 | ||
| Motility | Progressive motility (PR) | Correlation coefficient | 0.087 | −0.081 |
| p value | 0.399 | 0.428 | ||
| Non-progressive motility (NP) | Correlation coefficient | 0.035 | 0.274 ** | |
| p value | 0.736 | 0.007 | ||
| Immotility (IM) | Correlation coefficient | −0.089 | −0.025 | |
| p value | 0.384 | 0.811 | ||
| Correlation Coefficient | p Value | |
|---|---|---|
| Fertilization Rate | −0.130 | 0.204 |
| Day 2 embryo | ||
| Embryo quality | 0.061 | 0.558 |
| Number of blastomeres | 0.084 | 0.423 |
| Embryo fragmentation | 0.071 | 0.490 |
| Embryo symmetry | 0.050 | 0.627 |
| Day 3 embryo | ||
| Embryo quality | 0.010 | 0.920 |
| Number of blastomeres | 0.053 | 0.605 |
| Embryo fragmentation | 0.118 | 0.257 |
| Embryo symmetry | 0.050 | 0.627 |
| Yes | No | p(UMW) | |
|---|---|---|---|
| Embryo transfer | 72.26 (n = 89) | 69.71 (n = 8) | 0.704 |
| Biochemical pregnancy | 71.93 (n = 63) | 74.22 (n = 26) | 0.427 |
| Clinical pregnancy | 71.46 (n = 55) | 75.00 (n = 34) | 0.303 |
| Live-birth outcome | 71.46 (n = 49) | 74.22 (n = 40) | 0.453 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gianzo, M.; Urizar-Arenaza, I.; Muñoa-Hoyos, I.; Larreategui, Z.; Garrido, N.; Irazusta, J.; Subirán, N. (Pro)renin Receptor Is Present in Human Sperm and It Adversely Affects Sperm Fertility Ability. Int. J. Mol. Sci. 2021, 22, 3215. https://doi.org/10.3390/ijms22063215
Gianzo M, Urizar-Arenaza I, Muñoa-Hoyos I, Larreategui Z, Garrido N, Irazusta J, Subirán N. (Pro)renin Receptor Is Present in Human Sperm and It Adversely Affects Sperm Fertility Ability. International Journal of Molecular Sciences. 2021; 22(6):3215. https://doi.org/10.3390/ijms22063215
Chicago/Turabian StyleGianzo, Marta, Itziar Urizar-Arenaza, Iraia Muñoa-Hoyos, Zaloa Larreategui, Nicolás Garrido, Jon Irazusta, and Nerea Subirán. 2021. "(Pro)renin Receptor Is Present in Human Sperm and It Adversely Affects Sperm Fertility Ability" International Journal of Molecular Sciences 22, no. 6: 3215. https://doi.org/10.3390/ijms22063215
APA StyleGianzo, M., Urizar-Arenaza, I., Muñoa-Hoyos, I., Larreategui, Z., Garrido, N., Irazusta, J., & Subirán, N. (2021). (Pro)renin Receptor Is Present in Human Sperm and It Adversely Affects Sperm Fertility Ability. International Journal of Molecular Sciences, 22(6), 3215. https://doi.org/10.3390/ijms22063215







