Exogenous Transforming Growth Factor-β in Brain-Induced Symptoms of Central Fatigue and Suppressed Dopamine Production in Mice
Abstract
1. Introduction
2. Results
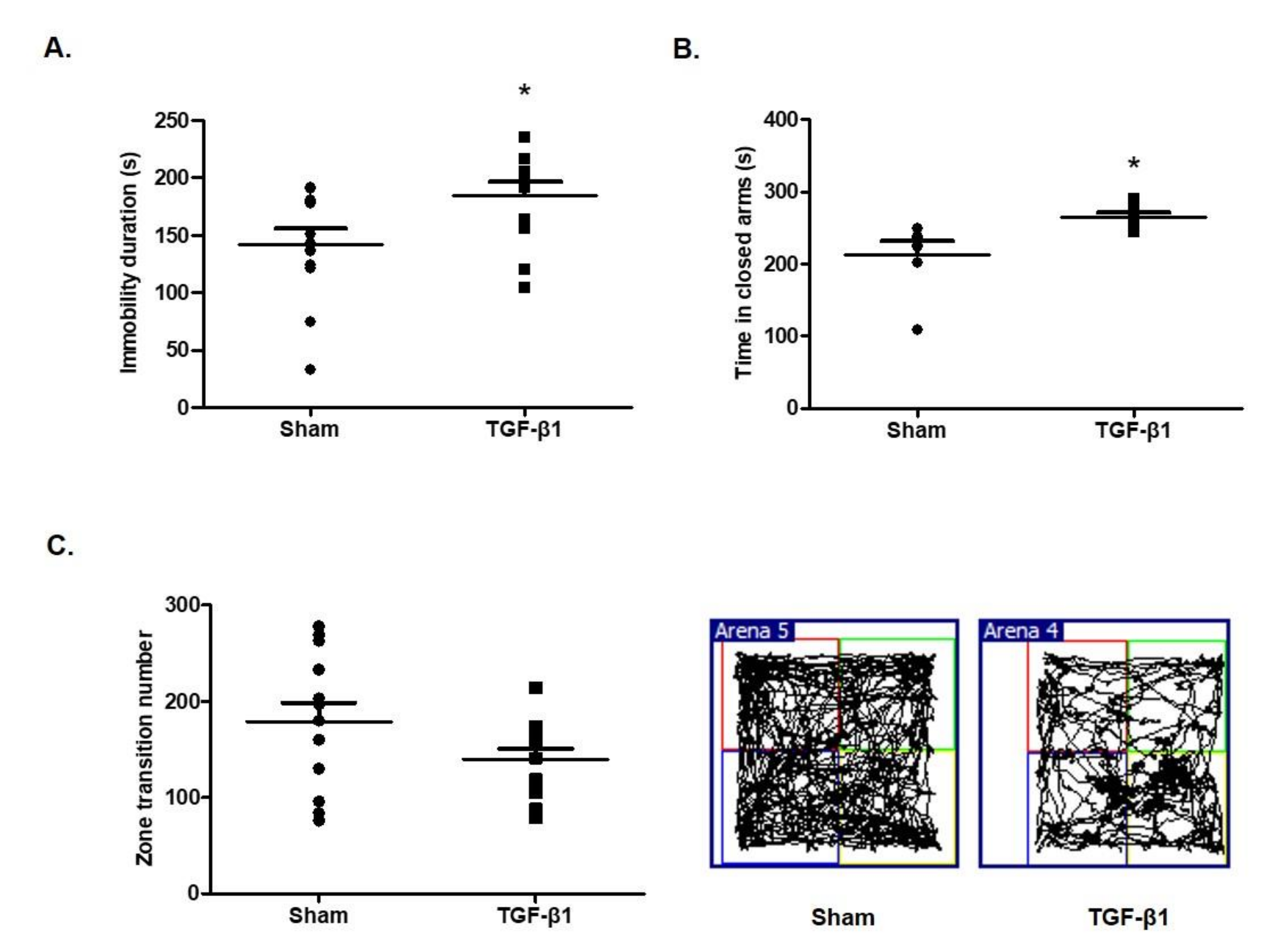
2.1. Effects of TGF-β1 on Depressive and Anxious Behaviors
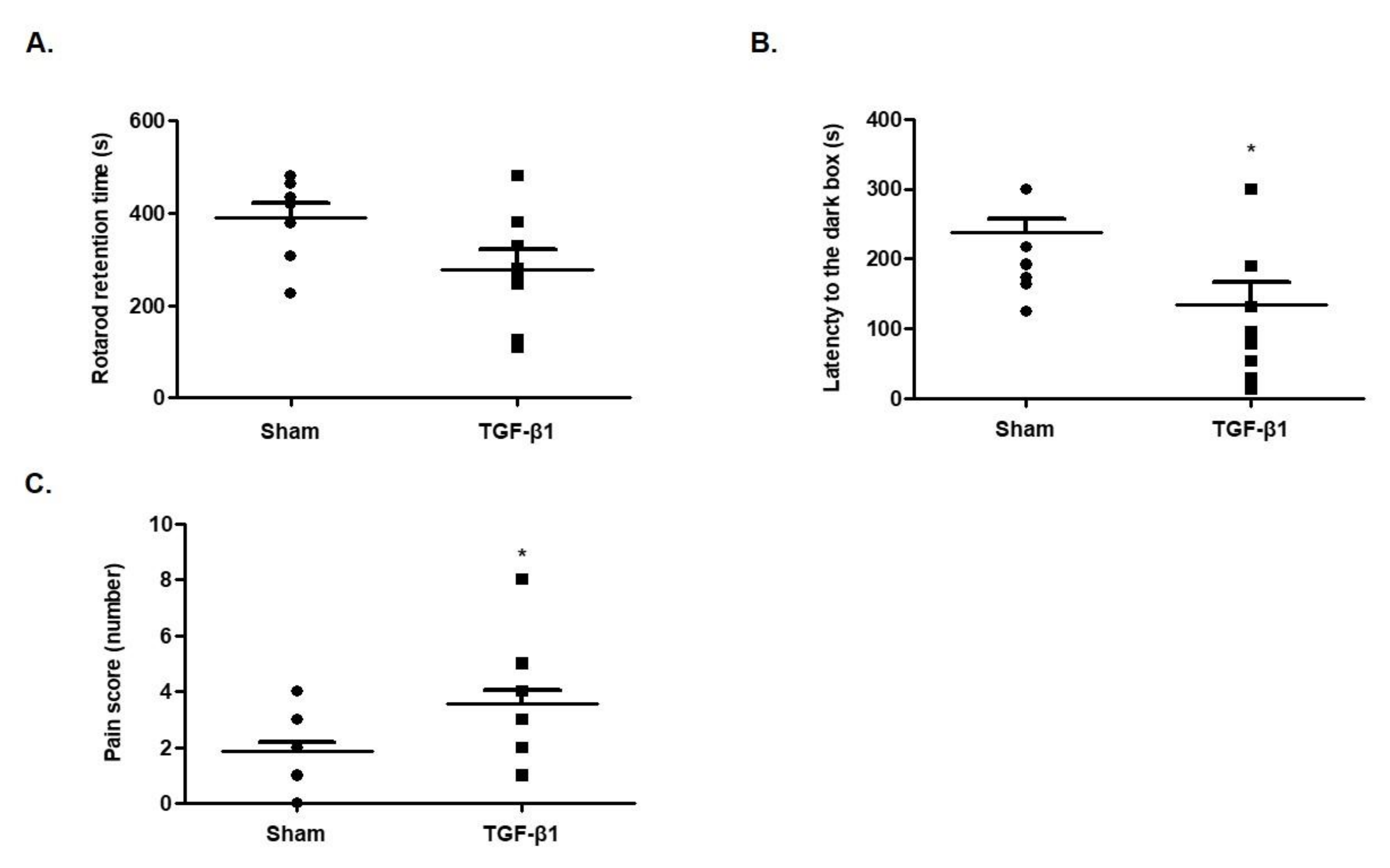
2.2. Effects of TGF-β1 on Fatigue-Like Behaviors
2.3. Effects of TGF-β1 on Learning Memory
2.4. Effects of TGF-β1 on Allodynia
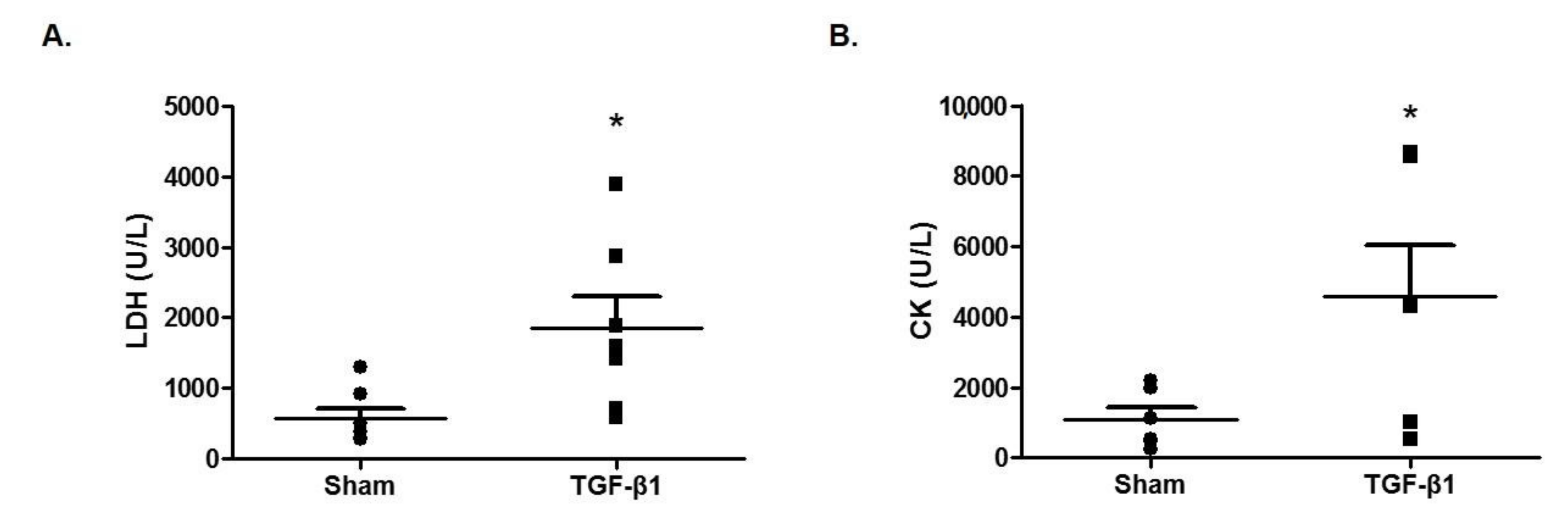
2.5. Effects of TGF-β1 on Enzyme Markers of Fatigue in Serum
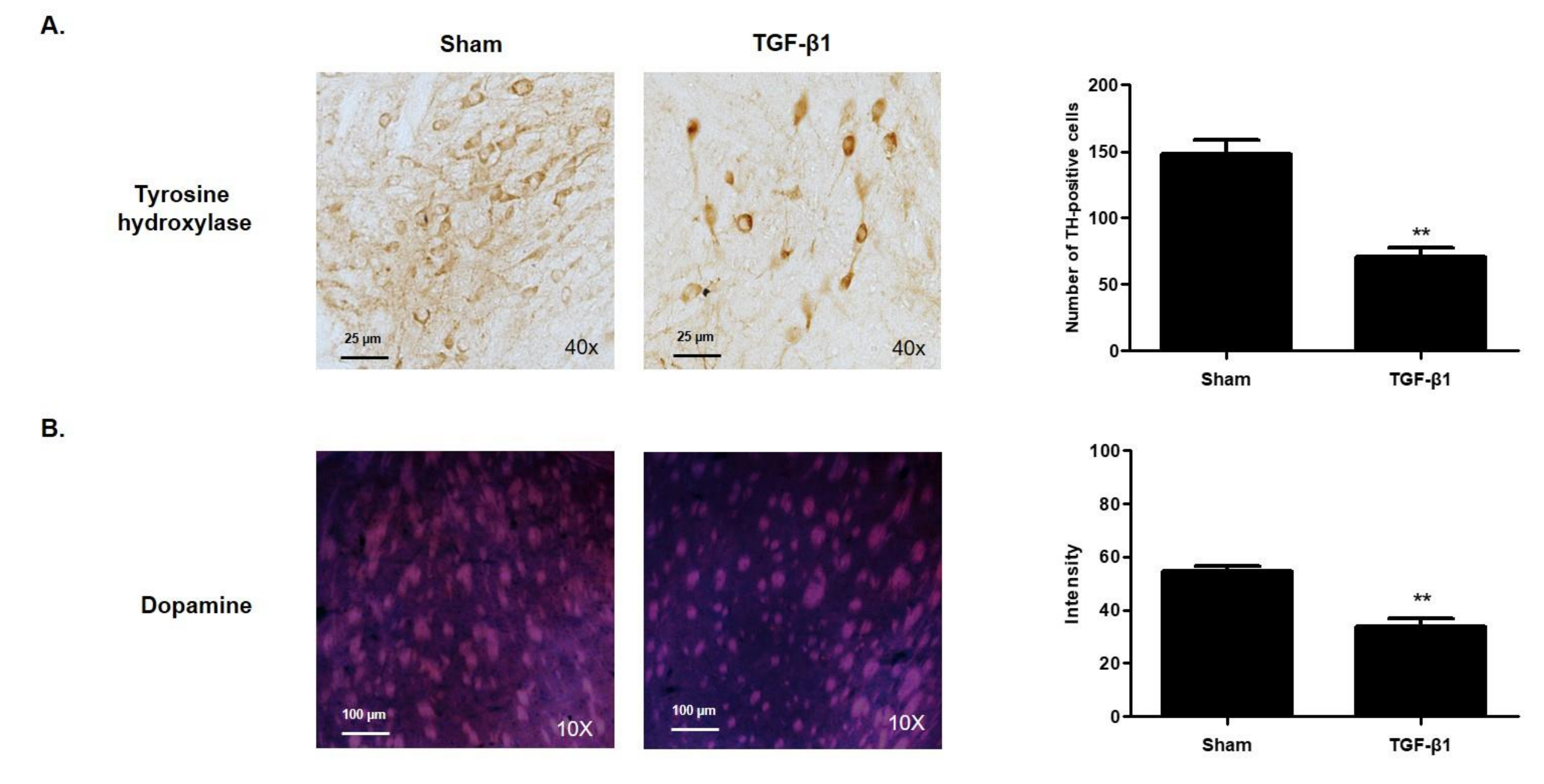
2.6. Effects of TGF-β1 on Dopaminergic System
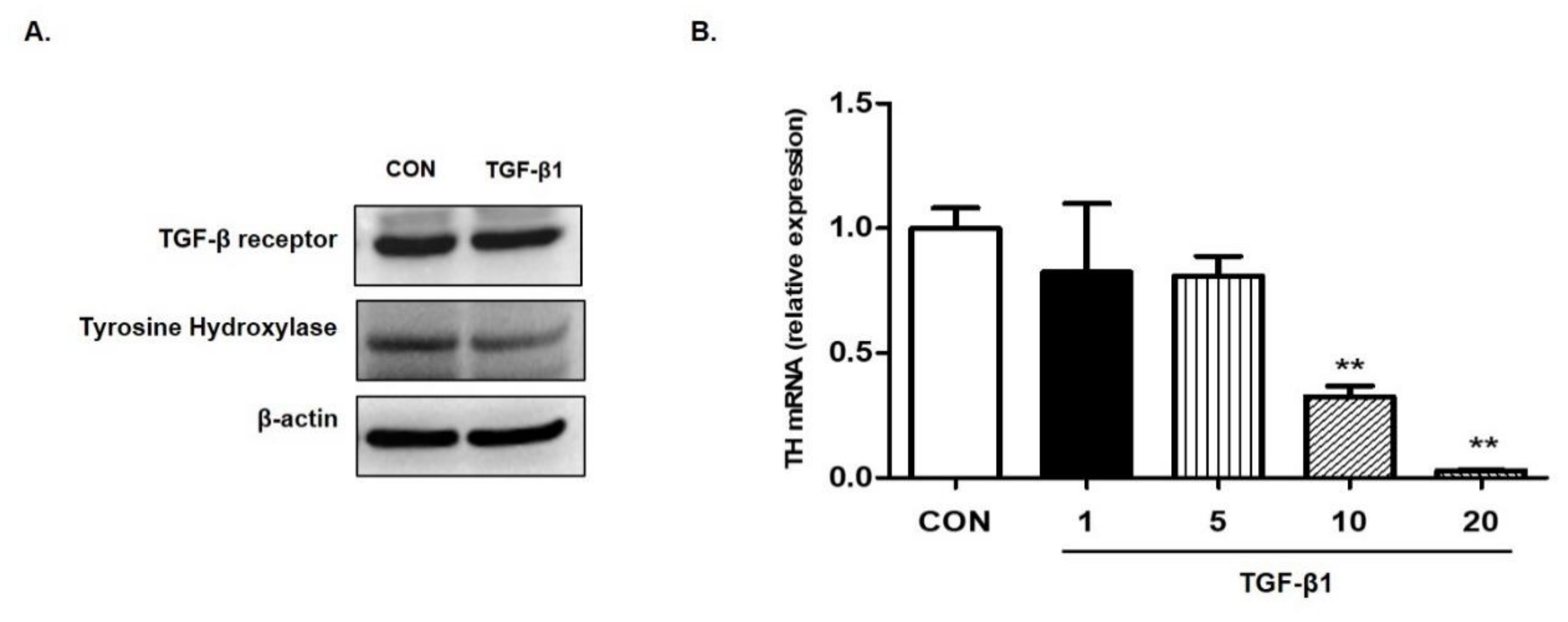
2.7. Effects of TGF-β1 on the Expression of TH in SH-SY5Y Cells
3. Discussion
4. Materials and Methods
4.1. Animals
4.2. Intracerebroventricular Injection of TGF-β1
4.3. Open Field Test
4.4. Rotarod Test
4.5. Passive Avoidance Test
4.6. Von Frey Test
4.7. Sacrifice
4.8. Blood Biochemical Examination
4.9. Immunofluorescence Staining
4.10. Immunohistochemistry Staining
4.11. Cell Culture
4.12. Western Blotting Analysis
4.13. Real-Time PCR
4.14. Statistical Analysis
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lim, E.J.; Ahn, Y.C.; Jang, E.S.; Lee, S.W.; Lee, S.H.; Son, C.G. Systematic review and meta-analysis of the prevalence of chronic fatigue syndrome/myalgic encephalomyelitis (CFS/ME). J. Transl. Med. 2020, 18, 100. [Google Scholar] [CrossRef]
- Cortes Rivera, M.; Mastronardi, C.; Silva-Aldana, C.T.; Arcos-Burgos, M.; Lidbury, B.A. Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: A Comprehensive Review. Diagnostics 2019, 9, 91. [Google Scholar] [CrossRef] [PubMed]
- Joo, J.H.; Park, S.H. Chronic fatigue syndrome. Korean J. Med. 2006, 70, 469–473. [Google Scholar]
- Mensah, F.K.F.; Bansal, A.S.; Ford, B.; Cambridge, G. Chronic fatigue syndrome and the immune system: Where are we now? Neurophysiol. Clin. 2017, 47, 131–138. [Google Scholar] [CrossRef]
- Lim, E.J.; Jang, E.S.; Son, C.G. Characteristics of Chronic Fatigue Syndrome (CFS): Based on Qualitative Content-Analysis of Patient Description. Korean Public Health Res. 2020, 46, 107–116. [Google Scholar]
- Muller, A.E.; Tveito, K.; Bakken, I.J.; Flottorp, S.A.; Mjaaland, S.; Larun, L. Potential causal factors of CFS/ME: A concise and systematic scoping review of factors researched. J. Transl. Med. 2020, 18, 484. [Google Scholar] [CrossRef] [PubMed]
- Brenu, E.W.; van Driel, M.L.; Staines, D.R.; Ashton, K.J.; Ramos, S.B.; Keane, J.; Klimas, N.G.; Marshall-Gradisnik, S.M. Immunological abnormalities as potential biomarkers in Chronic Fatigue Syndrome/Myalgic Encephalomyelitis. J. Transl. Med. 2011, 9, 81. [Google Scholar] [CrossRef] [PubMed]
- Skowera, A.; Cleare, A.; Blair, D.; Bevis, L.; Wessely, S.C.; Peakman, M. High levels of type 2 cytokine-producing cells in chronic fatigue syndrome. Clin. Exp. Immunol. 2004, 135, 294–302. [Google Scholar] [CrossRef]
- Morris, G.; Maes, M. Mitochondrial dysfunctions in myalgic encephalomyelitis/chronic fatigue syndrome explained by activated immuno-inflammatory, oxidative and nitrosative stress pathways. Metab. Brain Dis. 2014, 29, 19–36. [Google Scholar] [CrossRef] [PubMed]
- Nakatomi, Y.; Mizuno, K.; Ishii, A.; Wada, Y.; Tanaka, M.; Tazawa, S.; Onoe, K.; Fukuda, S.; Kawabe, J.; Takahashi, K.; et al. Neuroinflammation in Patients with Chronic Fatigue Syndrome/Myalgic Encephalomyelitis: An (1)(1)C-(R)-PK11195 PET Study. J. Nucl. Med. 2014, 55, 945–950. [Google Scholar] [CrossRef]
- Clark, L.V.; Buckland, M.; Murphy, G.; Taylor, N.; Vleck, V.; Mein, C.; Wozniak, E.; Smuk, M.; White, P.D. Cytokine responses to exercise and activity in patients with chronic fatigue syndrome: Case-control study. Clin. Exp. Immunol. 2017, 190, 360–371. [Google Scholar] [CrossRef] [PubMed]
- Montoya, J.G.; Holmes, T.H.; Anderson, J.N.; Maecker, H.T.; Rosenberg-Hasson, Y.; Valencia, I.J.; Chu, L.; Younger, J.W.; Tato, C.M.; Davis, M.M. Cytokine signature associated with disease severity in chronic fatigue syndrome patients. Proc. Natl. Acad. Sci. USA 2017, 114, E7150–E7158. [Google Scholar] [CrossRef] [PubMed]
- Bennett, A.L.; Chao, C.C.; Hu, S.; Buchwald, D.; Fagioli, L.R.; Schur, P.H.; Peterson, P.K.; Komaroff, A.L. Elevation of bioactive transforming growth factor-beta in serum from patients with chronic fatigue syndrome. J. Clin. Immunol. 1997, 17, 160–166. [Google Scholar] [CrossRef] [PubMed]
- Strawbridge, R.; Sartor, M.L.; Scott, F.; Cleare, A.J. Inflammatory proteins are altered in chronic fatigue syndrome-A systematic review and meta-analysis. Neurosci. Biobehav. Rev. 2019, 107, 69–83. [Google Scholar] [CrossRef]
- Connolly, E.C.; Akhurst, R.J. The complexities of TGF-beta action during mammary and squamous cell carcinogenesis. Curr. Pharm. Biotechnol. 2011, 12, 2138–2149. [Google Scholar] [CrossRef]
- Korpal, M.; Kang, Y. Targeting the transforming growth factor-beta signalling pathway in metastatic cancer. Eur. J. Cancer 2010, 46, 1232–1240. [Google Scholar] [CrossRef]
- Massague, J. TGFbeta signalling in context. Nat. Rev. Mol. Cell Biol. 2012, 13, 616–630. [Google Scholar] [CrossRef]
- Broughton, G., 2nd; Janis, J.E.; Attinger, C.E. The basic science of wound healing. Plast. Reconstr. Surg. 2006, 117 (Suppl. 7), 12S–34S. [Google Scholar] [CrossRef]
- Faler, B.J.; Macsata, R.A.; Plummer, D.; Mishra, L.; Sidawy, A.N. Transforming growth factor-beta and wound healing. Perspect. Vasc. Surg. Endovasc. Ther. 2006, 18, 55–62. [Google Scholar] [CrossRef]
- Kristjansson, R.P.; Oddsson, A.; Helgason, H.; Sveinbjornsson, G.; Arnadottir, G.A.; Jensson, B.O.; Jonasdottir, A.; Jonasdottir, A.; Bragi Walters, G.; Sulem, G.; et al. Common and rare variants associating with serum levels of creatine kinase and lactate dehydrogenase. Nat. Commun. 2016, 7, 10572. [Google Scholar] [CrossRef]
- Shimwe, D.N.; Praveen, K.; Paul, X.; Jessy, M.; Paul, D.K.; Elodie, B.; Mounir, B.; Amine, M. A review of neurotransmitters sensing methods for neuro-engineering research. Appl. Sci. 2019, 9, 4719. [Google Scholar]
- Krupinski, J.; Kumar, P.; Kumar, S.; Kaluza, J. Increased expression of TGF-beta 1 in brain tissue after ischemic stroke in humans. Stroke 1996, 27, 852–857. [Google Scholar] [CrossRef]
- Lindholm, D.; Castren, E.; Kiefer, R.; Zafra, F.; Thoenen, H. Transforming growth factor-beta 1 in the rat brain: Increase after injury and inhibition of astrocyte proliferation. J. Cell Biol. 1992, 117, 395–400. [Google Scholar] [CrossRef]
- Carmeliet, P. Mechanisms of angiogenesis and arteriogenesis. Nat. Med. 2000, 6, 389–395. [Google Scholar] [CrossRef] [PubMed]
- Lesne, S.; Docagne, F.; Gabriel, C.; Liot, G.; Lahiri, D.K.; Buee, L.; Plawinski, L.; Delacourte, A.; MacKenzie, E.T.; Buisson, A.; et al. Transforming growth factor-beta 1 potentiates amyloid-beta generation in astrocytes and in transgenic mice. J. Biol. Chem. 2003, 278, 18408–18418. [Google Scholar] [CrossRef]
- Wachs, F.P.; Winner, B.; Couillard-Despres, S.; Schiller, T.; Aigner, R.; Winkler, J.; Bogdahn, U.; Aigner, L. Transforming growth factor-beta1 is a negative modulator of adult neurogenesis. J. Neuropathol. Exp. Neurol. 2006, 65, 358–370. [Google Scholar] [CrossRef] [PubMed]
- Hamada, Y.; Ikata, T.; Katoh, S.; Katoh, K.; Niwa, M.; Tsutsumishita, Y.; Fukuzawa, K. Effects of exogenous transforming growth factor-beta 1 on spinal cord injury in rats. Neurosci. Lett. 1996, 203, 97–100. [Google Scholar] [CrossRef]
- Matsumura, S.; Shibakusa, T.; Fujikawa, T.; Yamada, H.; Inoue, K.; Fushiki, T. Increase in transforming growth factor-beta in the brain during infection is related to fever, not depression of spontaneous motor activity. Neuroscience 2007, 144, 1133–1140. [Google Scholar] [CrossRef]
- Fujikawa, T.; Fujita, R.; Iwaki, Y.; Matsumura, S.; Fushiki, T.; Inoue, K. Inhibition of fatty acid oxidation activates transforming growth factor-beta in cerebrospinal fluid and decreases spontaneous motor activity. Physiol. Behav. 2010, 101, 370–375. [Google Scholar] [CrossRef]
- Lee, J.S.; Jeon, Y.J.; Park, S.Y.; Son, C.G. An Adrenalectomy Mouse Model Reflecting Clinical Features for Chronic Fatigue Syndrome. Biomolecules 2020, 10, 71. [Google Scholar] [CrossRef] [PubMed]
- Nakazato, F.; Tada, T.; Sekiguchi, Y.; Murakami, K.; Yanagisawa, S.; Tanaka, Y.; Hongo, K. Disturbed spatial learning of rats after intraventricular administration of transforming growth factor-beta 1. Neurol. Med. Chir. 2002, 42, 151–156. [Google Scholar] [CrossRef][Green Version]
- Calabresi, P.; Picconi, B.; Tozzi, A.; Di Filippo, M. Dopamine-mediated regulation of corticostriatal synaptic plasticity. Trends Neurosci. 2007, 30, 211–219. [Google Scholar] [CrossRef] [PubMed]
- Padua, D.; Massague, J. Roles of TGFbeta in metastasis. Cell Res. 2009, 19, 89–102. [Google Scholar] [CrossRef] [PubMed]
- Georgiades, E.; Behan, W.M.; Kilduff, L.P.; Hadjicharalambous, M.; Mackie, E.E.; Wilson, J.; Ward, S.A.; Pitsiladis, Y.P. Chronic fatigue syndrome: New evidence for a central fatigue disorder. Clin. Sci. 2003, 105, 213–218. [Google Scholar] [CrossRef]
- Miller, A.H.; Jones, J.F.; Drake, D.F.; Tian, H.; Unger, E.R.; Pagnoni, G. Decreased basal ganglia activation in subjects with chronic fatigue syndrome: Association with symptoms of fatigue. PLoS ONE 2014, 9, e98156. [Google Scholar] [CrossRef] [PubMed]
- Sanjabi, S.; Zenewicz, L.A.; Kamanaka, M.; Flavell, R.A. Anti-inflammatory and pro-inflammatory roles of TGF-beta, IL-10, and IL-22 in immunity and autoimmunity. Curr. Opin. Pharmacol. 2009, 9, 447–453. [Google Scholar] [CrossRef]
- Ieraci, A.; Herrera, D.G. Nicotinamide protects against ethanol-induced apoptotic neurodegeneration in the developing mouse brain. PLoS Med. 2006, 3, e101. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, W.K.; Kim, Y.; Jang, H.; Sim, J.H.; Choi, H.J.; Shin, Y.; Choi, J.J. Exogenous Transforming Growth Factor-β in Brain-Induced Symptoms of Central Fatigue and Suppressed Dopamine Production in Mice. Int. J. Mol. Sci. 2021, 22, 2580. https://doi.org/10.3390/ijms22052580
Lee WK, Kim Y, Jang H, Sim JH, Choi HJ, Shin Y, Choi JJ. Exogenous Transforming Growth Factor-β in Brain-Induced Symptoms of Central Fatigue and Suppressed Dopamine Production in Mice. International Journal of Molecular Sciences. 2021; 22(5):2580. https://doi.org/10.3390/ijms22052580
Chicago/Turabian StyleLee, Won Kil, Yeongyeong Kim, Heejin Jang, Joo Hye Sim, Hye Jin Choi, Younmin Shin, and Jeong June Choi. 2021. "Exogenous Transforming Growth Factor-β in Brain-Induced Symptoms of Central Fatigue and Suppressed Dopamine Production in Mice" International Journal of Molecular Sciences 22, no. 5: 2580. https://doi.org/10.3390/ijms22052580
APA StyleLee, W. K., Kim, Y., Jang, H., Sim, J. H., Choi, H. J., Shin, Y., & Choi, J. J. (2021). Exogenous Transforming Growth Factor-β in Brain-Induced Symptoms of Central Fatigue and Suppressed Dopamine Production in Mice. International Journal of Molecular Sciences, 22(5), 2580. https://doi.org/10.3390/ijms22052580





