Role of Nociceptin/Orphanin FQ-NOP Receptor System in the Regulation of Stress-Related Disorders
Abstract
1. Introduction
2. Neurobiology of the N/OFQ-NOP Receptor System
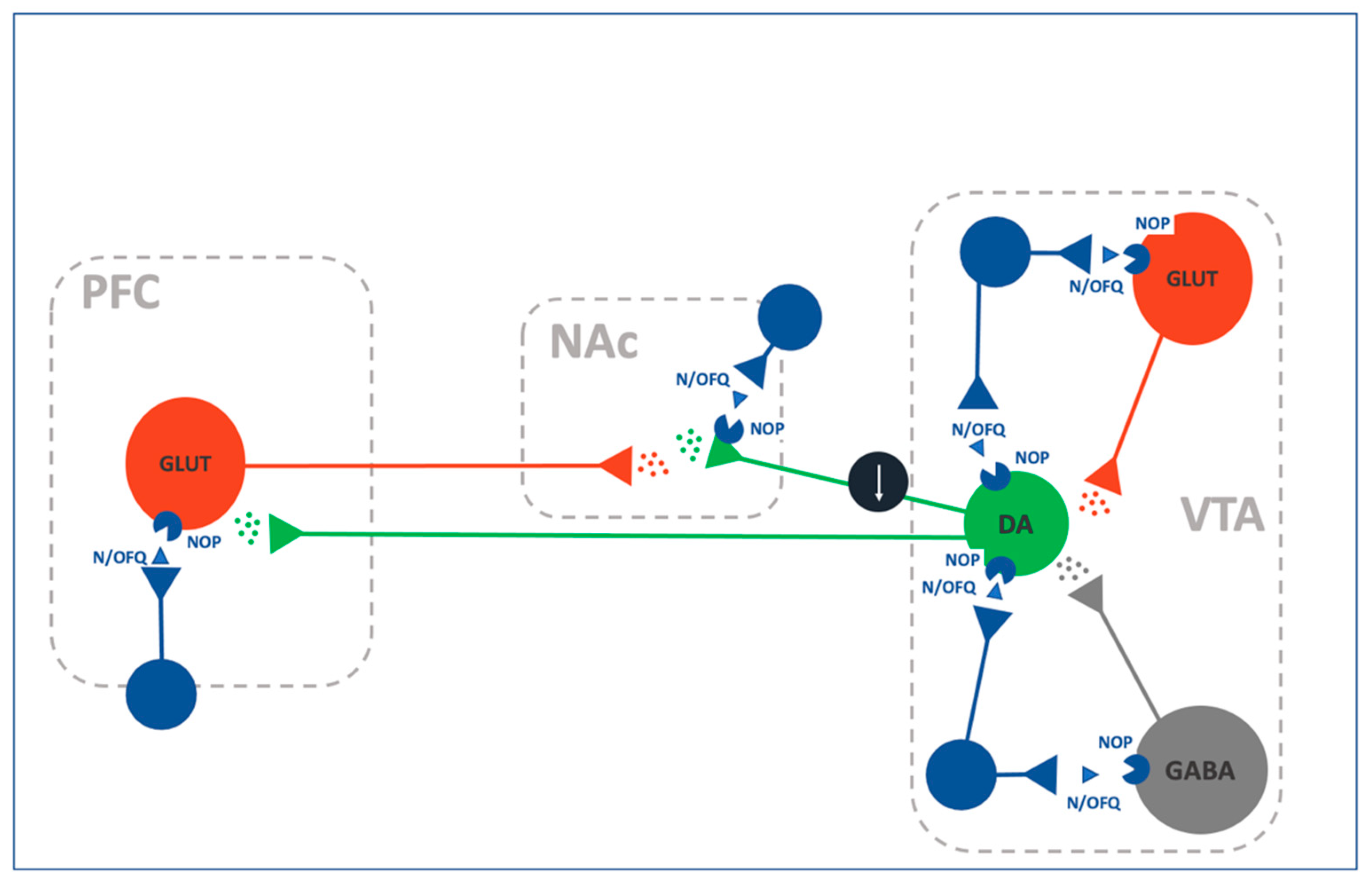
2.1. N/OFQ-NOP and the Mesocorticolimbic Reward System
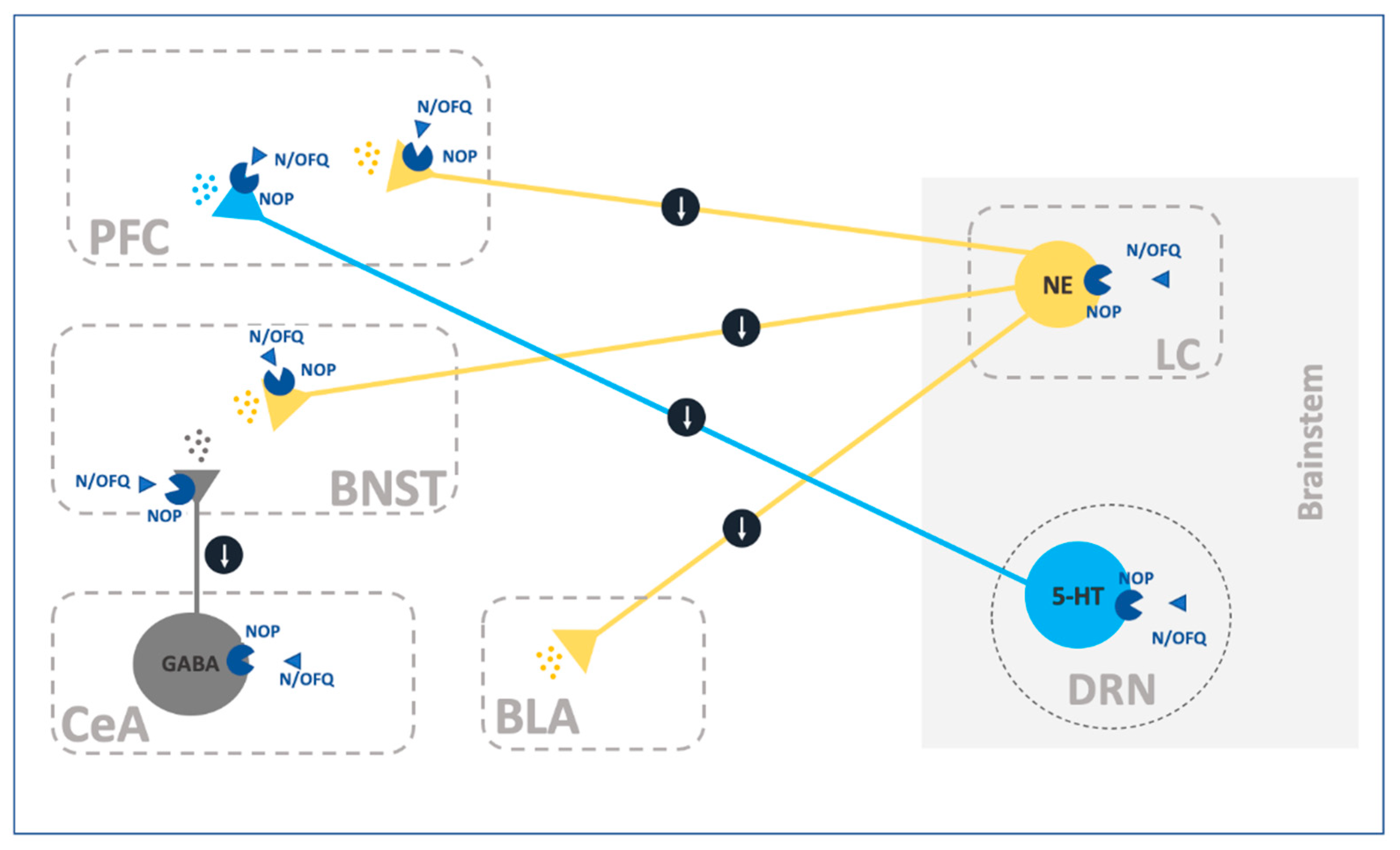
2.2. N/OFQ and the Extrahypothalamic Stress System
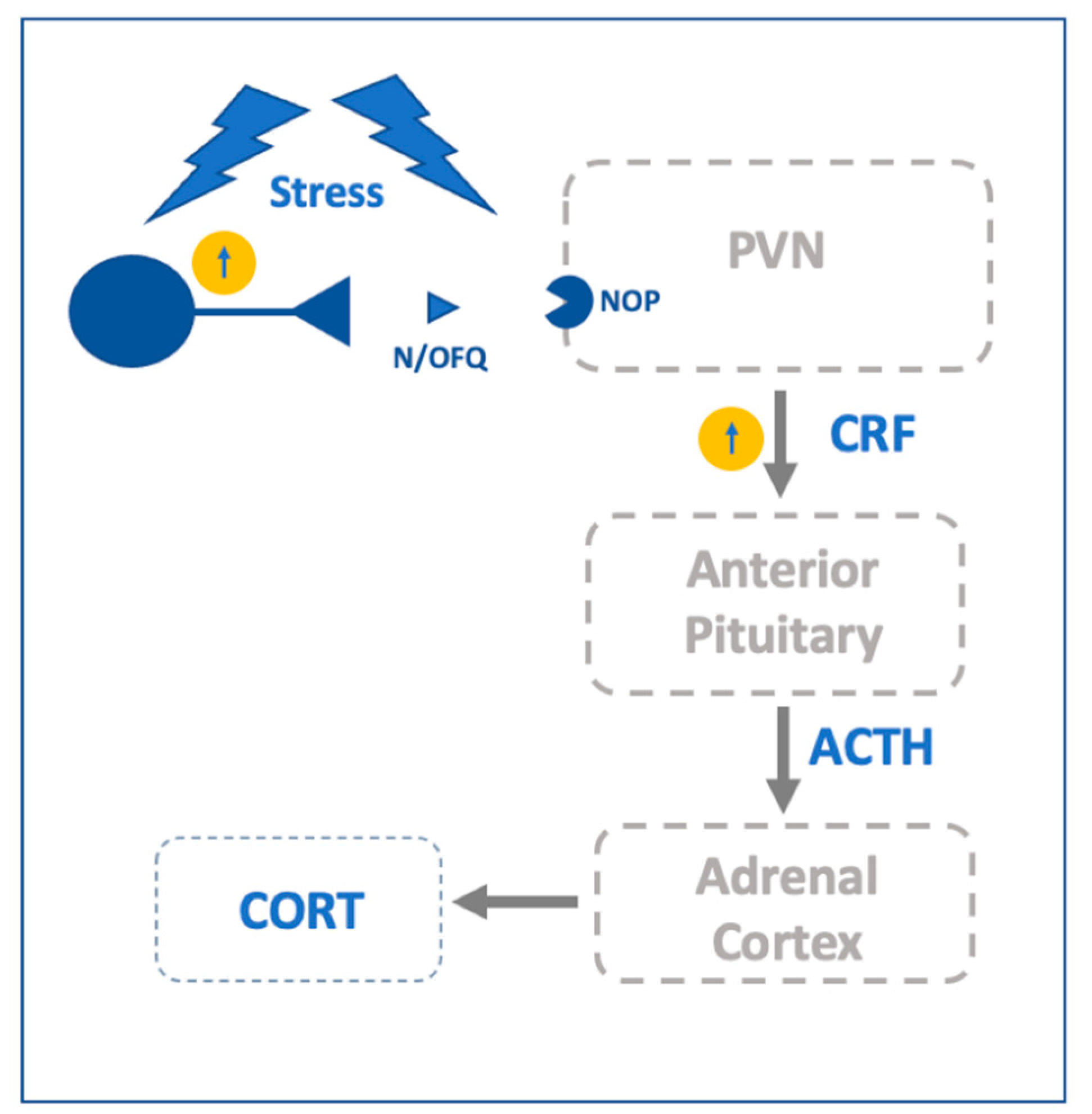
2.3. N/OFQ-NOP and the Hypothalamic Stress System
3. Role of the N/OFQ-NOP Receptor System in Anxiety and Mood Disorders
4. Role of N/OFQ-NOP Receptor System in the Interaction between Stress and Drug Addiction
5. Role of the N/OFQ-NOP System in the Regulation of Feeding and Food-Related Disorders
6. Conclusive Remarks
Author Contributions
Funding
Conflicts of Interest
References
- Meunier, J.C.; Mollereau, C.; Toll, L.; Suaudeau, C.; Moisand, C.; Alvinerie, P.; Butour, J.L.; Guillemot, J.C.; Ferrara, P.; Monsarrat, B.; et al. Isolation and structure of the endogenous agonist of opioid receptor-like ORL1 receptor. Nature 1995, 377, 532–535. [Google Scholar] [CrossRef] [PubMed]
- Reinscheid, R.K.; Nothacker, H.P.; Bourson, A.; Ardati, A.; Henningsen, R.A.; Bunzow, J.R.; Grandy, D.K.; Langen, H.; Monsma, F.J., Jr.; Civelli, O. Orphanin FQ: A neuropeptide that activates an opioidlike G protein-coupled receptor. Science 1995, 270, 792–794. [Google Scholar] [CrossRef] [PubMed]
- Mollereau, C.; Parmentier, M.; Mailleux, P.; Butour, J.L.; Moisand, C.; Chalon, P.; Caput, D.; Vassart, G.; Meunier, J.C. ORL1, a novel member of the opioid receptor family. Cloning, functional expression and localization. FEBS Lett. 1994, 341, 33–38. [Google Scholar] [CrossRef]
- Civelli, O. The orphanin FQ/nociceptin (OFQ/N) system. Results Probl. Cell Differ. 2008, 46, 1–25. [Google Scholar]
- Mollereau, C.; Simons, M.J.; Soularue, P.; Liners, F.; Vassart, G.; Meunier, J.C.; Parmentier, M. Structure, tissue distribution, and chromosomal localization of the prepronociceptin gene. Proc. Natl. Acad. Sci. USA 1996, 93, 8666–8670. [Google Scholar] [CrossRef] [PubMed]
- Morgan, M.M.; Grisel, J.E.; Robbins, C.S.; Grandy, D.K. Antinociception mediated by the periaqueductal gray is attenuated by orphanin FQ. Neuroreport 1997, 8, 3431–3434. [Google Scholar] [CrossRef] [PubMed]
- Pan, Z.; Hirakawa, N.; Fields, H.L. A cellular mechanism for the bidirectional pain-modulating actions of orphanin FQ/nociceptin. Neuron 2000, 26, 515–522. [Google Scholar] [CrossRef]
- Ciccocioppo, R.; Angeletti, S.; Sanna, P.P.; Weiss, F.; Massi, M. Effect of nociceptin/orphanin FQ on the rewarding properties of morphine. Eur. J. Pharmacol. 2000, 404, 153–159. [Google Scholar] [CrossRef]
- Sakoori, K.; Murphy, N.P. Central administration of nociceptin/orphanin FQ blocks the acquisition of conditioned place preference to morphine and cocaine, but not conditioned place aversion to naloxone in mice. Psychopharmacology (Berlin) 2004, 172, 129–136. [Google Scholar] [CrossRef]
- Murphy, N.P.; Maidment, N.T. Orphanin FQ/nociceptin modulation of mesolimbic dopamine transmission determined by microdialysis. J. Neurochem. 1999, 73, 179–186. [Google Scholar] [CrossRef]
- Mogil, J.S.; Grisel, J.E.; Reinscheid, R.K.; Civelli, O.; Belknap, J.K.; Grandy, D.K. Orphanin FQ is a functional anti-opioid peptide. Neuroscience 1996, 75, 333–337. [Google Scholar] [CrossRef]
- Chiou, L.C.; Liao, Y.Y.; Fan, P.C.; Kuo, P.H.; Wang, C.H.; Riemer, C.; Prinssen, E.P. Nociceptin/orphanin FQ peptide receptors: Pharmacology and clinical implications. Curr. Drug Targets 2007, 8, 117–135. [Google Scholar] [CrossRef]
- Fioravanti, B.; Vanderah, T.W. The ORL-1 receptor system: Are there opportunities for antagonists in pain therapy? Curr. Top. Med. Chem. 2008, 8, 1442–1451. [Google Scholar] [CrossRef]
- Mika, J.; Obara, I.; Przewlocka, B. The role of nociceptin and dynorphin in chronic pain: Implications of neuro-glial interaction. Neuropeptides 2011, 45, 247–261. [Google Scholar] [CrossRef] [PubMed]
- Sukhtankar, D.D.; Lee, H.; Rice, K.C.; Ko, M.C. Differential effects of opioid-related ligands and NSAIDs in nonhuman primate models of acute and inflammatory pain. Psychopharmacology (Berlin) 2014, 231, 1377–1387. [Google Scholar] [CrossRef] [PubMed]
- Rizzi, A.; Sukhtankar, D.D.; Ding, H.; Hayashida, K.; Ruzza, C.; Guerrini, R.; Calo, G.; Ko, M.C. Spinal antinociceptive effects of the novel NOP receptor agonist PWT2-nociceptin/orphanin FQ in mice and monkeys. Br. J. Pharmacol. 2015, 172, 3661–3670. [Google Scholar] [CrossRef]
- Neal, C.R., Jr.; Mansour, A.; Reinscheid, R.; Nothacker, H.P.; Civelli, O.; Akil, H.; Watson, S.J., Jr. Opioid receptor-like (ORL1) receptor distribution in the rat central nervous system: Comparison of ORL1 receptor mRNA expression with (125)I-[(14)Tyr]-orphanin FQ binding. J. Comp. Neurol. 1999, 412, 563–605. [Google Scholar] [CrossRef]
- Neal, C.R., Jr.; Mansour, A.; Reinscheid, R.; Nothacker, H.P.; Civelli, O.; Watson, S.J., Jr. Localization of orphanin FQ (nociceptin) peptide and messenger RNA in the central nervous system of the rat. J. Comp. Neurol. 1999, 406, 503–547. [Google Scholar] [CrossRef]
- Sandin, J.; Ogren, S.O.; Terenius, L. Nociceptin/orphanin FQ modulates spatial learning via ORL-1 receptors in the dorsal hippocampus of the rat. Brain Res. 2004, 997, 222–233. [Google Scholar] [CrossRef]
- Jenck, F.; Moreau, J.L.; Martin, J.R.; Kilpatrick, G.J.; Reinscheid, R.K.; Monsma, F.J., Jr.; Nothacker, H.P.; Civelli, O. Orphanin FQ acts as an anxiolytic to attenuate behavioral responses to stress. Proc. Natl. Acad. Sci. USA 1997, 94, 14854–14858. [Google Scholar] [CrossRef] [PubMed]
- Pomonis, J.D.; Billington, C.J.; Levine, A.S. Orphanin FQ, agonist of orphan opioid receptor ORL1, stimulates feeding in rats. Neuroreport 1996, 8, 369–371. [Google Scholar] [CrossRef] [PubMed]
- Rodi, D.; Polidori, C.; Bregola, G.; Zucchini, S.; Simonato, M.; Massi, M. Pro-nociceptin/orphanin FQ and NOP receptor mRNA levels in the forebrain of food deprived rats. Brain Res. 2002, 957, 354–361. [Google Scholar] [CrossRef]
- Economidou, D.; Policani, F.; Angellotti, T.; Massi, M.; Terada, T.; Ciccocioppo, R. Effect of novel NOP receptor ligands on food intake in rats. Peptides 2006, 27, 775–783. [Google Scholar] [CrossRef]
- Wang, J.B.; Johnson, P.S.; Imai, Y.; Persico, A.M.; Ozenberger, B.A.; Eppler, C.M.; Uhl, G.R. cDNA cloning of an orphan opiate receptor gene family member and its splice variant. FEBS Lett. 1994, 348, 75–79. [Google Scholar] [CrossRef]
- Lambert, D.G. The nociceptin/orphanin FQ receptor: A target with broad therapeutic potential. Nat. Rev. Drug Discov. 2008, 7, 694–710. [Google Scholar] [CrossRef]
- Leggett, J.D.; Dawe, K.L.; Jessop, D.S.; Fulford, A.J. Endogenous nociceptin/orphanin FQ system involvement in hypothalamic-pituitary-adrenal axis responses: Relevance to models of inflammation. J. Neuroendocr. 2009, 21, 888–897. [Google Scholar] [CrossRef]
- Armstead, W.M. Nociceptin/orphanin phenylalanine glutamine (FQ) receptor and cardiovascular disease. Cardiovasc. Ther. 2011, 29, 23–28. [Google Scholar] [CrossRef]
- Gavioli, E.C.; Romao, P.R. NOP Receptor Ligands as Potential Agents for Inflammatory and Autoimmune Diseases. J. Amino Acids 2011, 2011, 836569. [Google Scholar] [CrossRef]
- Serrano-Gomez, A.; Thompson, J.P.; Lambert, D.G. Nociceptin/orphanin FQ in inflammation and sepsis. Br. J. Anaesth. 2011, 106, 6–12. [Google Scholar] [CrossRef] [PubMed]
- Woodcock, A.; McLeod, R.L.; Sadeh, J.; Smith, J.A. The efficacy of a NOP1 agonist (SCH486757) in subacute cough. Lung 2010, 188 (Suppl. 1), 47–52. [Google Scholar] [CrossRef]
- McLeod, R.L.; Tulshian, D.B.; Bolser, D.C.; Varty, G.B.; Baptista, M.; Fernandez, X.; Parra, L.E.; Zimmer, J.C.; Erickson, C.H.; Ho, G.D.; et al. Pharmacological profile of the NOP agonist and cough suppressing agent SCH 486757 (8-[Bis(2-Chlorophenyl)Methyl]-3-(2-Pyrimidinyl)-8-Azabicyclo[3.2.1]Octan-3-Ol) in preclinical models. Eur. J. Pharmacol. 2010, 630, 112–120. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Varty, G.B.; Hyde, L.A.; Hodgson, R.A.; Lu, S.X.; McCool, M.F.; Kazdoba, T.M.; Del Vecchio, R.A.; Guthrie, D.H.; Pond, A.J.; Grzelak, M.E.; et al. Characterization of the nociceptin receptor (ORL-1) agonist, Ro64-6198, in tests of anxiety across multiple species. Psychopharmacology (Berlin) 2005, 182, 132–143. [Google Scholar] [CrossRef] [PubMed]
- Reiss, D.; Wichmann, J.; Tekeshima, H.; Kieffer, B.L.; Ouagazzal, A.M. Effects of nociceptin/orphanin FQ receptor (NOP) agonist, Ro64-6198, on reactivity to acute pain in mice: Comparison to morphine. Eur. J. Pharmacol. 2008, 579, 141–148. [Google Scholar] [CrossRef]
- Ko, M.C.; Woods, J.H.; Fantegrossi, W.E.; Galuska, C.M.; Wichmann, J.; Prinssen, E.P. Behavioral effects of a synthetic agonist selective for nociceptin/orphanin FQ peptide receptors in monkeys. Neuropsychopharmacology 2009, 34, 2088–2096. [Google Scholar] [CrossRef]
- Shoblock, J.R.; Wichmann, J.; Maidment, N.T. The effect of a systemically active ORL-1 agonist, Ro 64-6198, on the acquisition, expression, extinction, and reinstatement of morphine conditioned place preference. Neuropharmacology 2005, 49, 439–446. [Google Scholar] [CrossRef]
- Heinig, K.; Kratochwil, N.; Bucheli, F.; Thomae, A. Bioanalytics and pharmacokinetics of the nociceptin/orphanin FQ peptide receptor agonist RO0646198 in Wistar rats and Cynomolgus monkeys. J. Chromatogr. B Anal. Technol. Biomed. Life Sci. 2010, 878, 2101–2105. [Google Scholar] [CrossRef]
- Jenck, F.; Wichmann, J.; Dautzenberg, F.M.; Moreau, J.L.; Ouagazzal, A.M.; Martin, J.R.; Lundstrom, K.; Cesura, A.M.; Poli, S.M.; Roever, S.; et al. A synthetic agonist at the orphanin FQ/nociceptin receptor ORL1: Anxiolytic profile in the rat. Proc. Natl. Acad. Sci. USA 2000, 97, 4938–4943. [Google Scholar] [CrossRef]
- Toledo, M.A.; Pedregal, C.; Lafuente, C.; Diaz, N.; Martinez-Grau, M.A.; Jimenez, A.; Benito, A.; Torrado, A.; Mateos, C.; Joshi, E.M.; et al. Discovery of a novel series of orally active nociceptin/orphanin FQ (NOP) receptor antagonists based on a dihydrospiro(piperidine-4,7′-thieno[2,3-c]pyran) scaffold. J. Med. Chem. 2014, 57, 3418–3429. [Google Scholar] [CrossRef] [PubMed]
- Zaveri, N.T. Nociceptin Opioid Receptor (NOP) as a Therapeutic Target: Progress in Translation from Preclinical Research to Clinical Utility. J. Med. Chem. 2016, 59, 7011–7028. [Google Scholar] [CrossRef] [PubMed]
- Pike, V.W.; Rash, K.S.; Chen, Z.; Pedregal, C.; Statnick, M.A.; Kimura, Y.; Hong, J.; Zoghbi, S.S.; Fujita, M.; Toledo, M.A.; et al. Synthesis and evaluation of radioligands for imaging brain nociceptin/orphanin FQ peptide (NOP) receptors with positron emission tomography. J. Med. Chem. 2011, 54, 2687–2700. [Google Scholar] [CrossRef]
- Lohith, T.G.; Zoghbi, S.S.; Morse, C.L.; Araneta, M.F.; Barth, V.N.; Goebl, N.A.; Tauscher, J.T.; Pike, V.W.; Innis, R.B.; Fujita, M. Brain and whole-body imaging of nociceptin/orphanin FQ peptide receptor in humans using the PET ligand 11C-NOP-1A. J. Nucl. Med. 2012, 53, 385–392. [Google Scholar] [CrossRef]
- Ulrich-Lai, Y.M.; Herman, J.P. Neural regulation of endocrine and autonomic stress responses. Nat. Rev. Neurosci. 2009, 10, 397–409. [Google Scholar] [CrossRef]
- Kiguchi, N.; Ding, H.; Ko, M.C. Therapeutic potentials of NOP and MOP receptor coactivation for the treatment of pain and opioid abuse. J. Neurosci. Res. 2020. [Google Scholar] [CrossRef]
- Dumitrascuta, M.; Bermudez, M.; Trovato, O.; De Neve, J.; Ballet, S.; Wolber, G.; Spetea, M. Antinociceptive Efficacy of the micro-Opioid/Nociceptin Peptide-Based Hybrid KGNOP1 in Inflammatory Pain without Rewarding Effects in Mice: An Experimental Assessment and Molecular Docking. Molecules 2021, 26, 3267. [Google Scholar] [CrossRef]
- Bloms-Funke, P.; Gillen, C.; Schuettler, A.J.; Wnendt, S. Agonistic effects of the opioid buprenorphine on the nociceptin/OFQ receptor. Peptides 2000, 21, 1141–1146. [Google Scholar] [CrossRef]
- Huang, P.; Kehner, G.B.; Cowan, A.; Liu-Chen, L.Y. Comparison of pharmacological activities of buprenorphine and norbuprenorphine: Norbuprenorphine is a potent opioid agonist. J. Pharmacol. Exp. Ther. 2001, 297, 688–695. [Google Scholar]
- Kallupi, M.; Shen, Q.; de Guglielmo, G.; Yasuda, D.; Journigan, V.B.; Zaveri, N.T.; Ciccocioppo, R. Buprenorphine requires concomitant activation of NOP and MOP receptors to reduce cocaine consumption. Addict. Biol. 2018, 23, 585–595. [Google Scholar] [CrossRef]
- Sorge, R.E.; Stewart, J. The effects of chronic buprenorphine on intake of heroin and cocaine in rats and its effects on nucleus accumbens dopamine levels during self-administration. Psychopharmacology (Berlin) 2006, 188, 28–41. [Google Scholar] [CrossRef]
- Mello, N.K.; Lukas, S.E.; Kamien, J.B.; Mendelson, J.H.; Drieze, J.; Cone, E.J. The effects of chronic buprenorphine treatment on cocaine and food self-administration by rhesus monkeys. J. Pharmacol. Exp. Ther. 1992, 260, 1185–1193. [Google Scholar]
- Montoya, I.D.; Gorelick, D.A.; Preston, K.L.; Schroeder, J.R.; Umbricht, A.; Cheskin, L.J.; Lange, W.R.; Contoreggi, C.; Johnson, R.E.; Fudala, P.J. Randomized trial of buprenorphine for treatment of concurrent opiate and cocaine dependence. Clin. Pharm. Ther. 2004, 75, 34–48. [Google Scholar] [CrossRef]
- Ciccocioppo, R.; Economidou, D.; Rimondini, R.; Sommer, W.; Massi, M.; Heilig, M. Buprenorphine reduces alcohol drinking through activation of the nociceptin/orphanin FQ-NOP receptor system. Biol. Psychiatry 2007, 61, 4–12. [Google Scholar] [CrossRef]
- Nava, F.; Manzato, E.; Leonardi, C.; Lucchini, A. Opioid maintenance therapy suppresses alcohol intake in heroin addicts with alcohol dependence: Preliminary results of an open randomized study. Prog. Neuropsychopharmacol. Biol. Psychiatry 2008, 32, 1867–1872. [Google Scholar] [CrossRef]
- Linz, K.; Christoph, T.; Tzschentke, T.M.; Koch, T.; Schiene, K.; Gautrois, M.; Schroder, W.; Kogel, B.Y.; Beier, H.; Englberger, W.; et al. Cebranopadol: A novel potent analgesic nociceptin/orphanin FQ peptide and opioid receptor agonist. J. Pharmacol. Exp. Ther. 2014, 349, 535–548. [Google Scholar] [CrossRef]
- Rizzi, A.; Cerlesi, M.C.; Ruzza, C.; Malfacini, D.; Ferrari, F.; Bianco, S.; Costa, T.; Guerrini, R.; Trapella, C.; Calo, G. Pharmacological characterization of cebranopadol a novel analgesic acting as mixed nociceptin/orphanin FQ and opioid receptor agonist. Pharm. Res. Perspect. 2016, 4, e00247. [Google Scholar] [CrossRef]
- Shen, Q.; Deng, Y.; Ciccocioppo, R.; Cannella, N. Cebranopadol, a Mixed Opioid Agonist, Reduces Cocaine Self-administration through Nociceptin Opioid and Mu Opioid Receptors. Front. Psychiatry 2017, 8, 234. [Google Scholar] [CrossRef] [PubMed]
- Gavioli, E.C.; Calo, G. Antidepressant- and anxiolytic-like effects of nociceptin/orphanin FQ receptor ligands. Naunyn-Schmiedebergs Arch. Pharmacol. 2006, 372, 319–330. [Google Scholar] [CrossRef]
- Toll, L.; Bruchas, M.R.; Calo, G.; Cox, B.M.; Zaveri, N.T. Nociceptin/Orphanin FQ Receptor Structure, Signaling, Ligands, Functions, and Interactions with Opioid Systems. Pharmacol. Rev. 2016, 68, 419–457. [Google Scholar] [CrossRef]
- Winters, B.L.; Christie, M.J.; Vaughan, C.W. Electrophysiological Actions of N/OFQ. Handb. Exp. Pharm. 2019, 254, 91–130. [Google Scholar]
- Park, J.Y.; Chae, S.; Kim, C.S.; Kim, Y.J.; Yi, H.J.; Han, E.; Joo, Y.; Hong, S.; Yun, J.W.; Kim, H.; et al. Role of nociceptin/orphanin FQ and nociceptin opioid peptide receptor in depression and antidepressant effects of nociceptin opioid peptide receptor antagonists. Korean J. Physiol. Pharm. 2019, 23, 427–448. [Google Scholar] [CrossRef]
- Norton, C.S.; Neal, C.R.; Kumar, S.; Akil, H.; Watson, S.J. Nociceptin/orphanin FQ and opioid receptor-like receptor mRNA expression in dopamine systems. J. Comp. Neurol. 2002, 444, 358–368. [Google Scholar] [CrossRef]
- Maidment, N.T.; Chen, Y.; Tan, A.M.; Murphy, N.P.; Leslie, F.M. Rat ventral midbrain dopamine neurons express the orphanin FQ/nociceptin receptor ORL-1. Neuroreport 2002, 13, 1137–1140. [Google Scholar] [CrossRef]
- Parker, K.E.; Pedersen, C.E.; Gomez, A.M.; Spangler, S.M.; Walicki, M.C.; Feng, S.Y.; Stewart, S.L.; Otis, J.M.; Al-Hasani, R.; McCall, J.G.; et al. A Paranigral VTA Nociceptin Circuit that Constrains Motivation for Reward. Cell 2019, 178, 653–671.e19. [Google Scholar] [CrossRef]
- Wise, R.A. Role of brain dopamine in food reward and reinforcement. Philos. Trans. R. Soc. Lond. B Biol. Sci. 2006, 361, 1149–1158. [Google Scholar] [CrossRef]
- Di Chiara, G.; Tanda, G.; Bassareo, V.; Pontieri, F.; Acquas, E.; Fenu, S.; Cadoni, C.; Carboni, E. Drug addiction as a disorder of associative learning. Role of nucleus accumbens shell/extended amygdala dopamine. Ann. N. Y. Acad. Sci. 1999, 877, 461–485. [Google Scholar] [CrossRef] [PubMed]
- Murphy, N.P.; Ly, H.T.; Maidment, N.T. Intracerebroventricular orphanin FQ/nociceptin suppresses dopamine release in the nucleus accumbens of anaesthetized rats. Neuroscience 1996, 75, 1–4. [Google Scholar] [CrossRef]
- Zheng, F.; Grandy, D.K.; Johnson, S.W. Actions of orphanin FQ/nociceptin on rat ventral tegmental area neurons in vitro. Br. J. Pharmacol. 2002, 136, 1065–1071. [Google Scholar] [CrossRef]
- Hernandez, J.; Perez, L.; Soto, R.; Le, N.; Gastelum, C.; Wagner, E.J. Nociceptin/orphanin FQ neurons in the Arcuate Nucleus and Ventral Tegmental Area Act via Nociceptin Opioid Peptide Receptor Signaling to Inhibit Proopiomelanocortin and A10 Dopamine Neurons and Thereby Modulate Ingestion of Palatable Food. Physiol. Behav. 2020, 228, 113183. [Google Scholar] [CrossRef]
- Driscoll, J.R.; Wallace, T.L.; Mansourian, K.A.; Martin, W.J.; Margolis, E.B. Differential modulation of ventral tegmental area circuits by the nociceptin/orphanin FQ system. eNeuro 2020, 7. [Google Scholar] [CrossRef]
- Olianas, M.C.; Dedoni, S.; Boi, M.; Onali, P. Activation of nociceptin/orphanin FQ-NOP receptor system inhibits tyrosine hydroxylase phosphorylation, dopamine synthesis, and dopamine D(1) receptor signaling in rat nucleus accumbens and dorsal striatum. J. Neurochem. 2008, 107, 544–556. [Google Scholar] [CrossRef]
- Vazquez-DeRose, J.; Stauber, G.; Khroyan, T.V.; Xie, X.S.; Zaveri, N.T.; Toll, L. Retrodialysis of N/OFQ into the nucleus accumbens shell blocks cocaine-induced increases in extracellular dopamine and locomotor activity. Eur. J. Pharmacol. 2013, 699, 200–206. [Google Scholar] [CrossRef] [PubMed]
- Murphy, N.P.; Tan, A.M.; Lam, H.A.; Maidment, N.T. Nociceptin/orphanin FQ modulation of rat midbrain dopamine neurons in primary culture. Neuroscience 2004, 127, 929–940. [Google Scholar] [CrossRef]
- Okawa, H.; Kudo, M.; Kudo, T.; Guerrini, R.; Lambert, D.G.; Kushikata, T.; Yoshida, H.; Matsuki, A. Effects of nociceptinNH2 and [Nphe1]nociceptin(1-13)NH2 on rat brain noradrenaline release in vivo and in vitro. Neurosci. Lett. 2001, 303, 173–176. [Google Scholar] [CrossRef]
- Koizumi, M.; Midorikawa, N.; Takeshima, H.; Murphy, N.P. Exogenous, but not endogenous nociceptin modulates mesolimbic dopamine release in mice. J. Neurochem. 2004, 89, 257–263. [Google Scholar] [CrossRef]
- Koizumi, M.; Sakoori, K.; Midorikawa, N.; Murphy, N.P. The NOP (ORL1) receptor antagonist Compound B stimulates mesolimbic dopamine release and is rewarding in mice by a non-NOP-receptor-mediated mechanism. Br. J. Pharmacol. 2004, 143, 53–62. [Google Scholar] [CrossRef]
- Volta, M.; Marti, M.; McDonald, J.; Molinari, S.; Camarda, V.; Pela, M.; Trapella, C.; Morari, M. Pharmacological profile and antiparkinsonian properties of the novel nociceptin/orphanin FQ receptor antagonist 1-[1-cyclooctylmethyl-5-(1-hydroxy-1-methyl-ethyl)-1,2,3,6-tetrahydro-pyridin-4-y l]-3-ethyl-1,3-dihydro-benzoimidazol-2-one (GF-4). Peptides 2010, 31, 1194–1204. [Google Scholar] [CrossRef] [PubMed]
- Marti, M.; Trapella, C.; Viaro, R.; Morari, M. The nociceptin/orphanin FQ receptor antagonist J-113397 and L-DOPA additively attenuate experimental parkinsonism through overinhibition of the nigrothalamic pathway. J. Neurosci. 2007, 27, 1297–1307. [Google Scholar] [CrossRef]
- Marti, M.; Trapella, C.; Morari, M. The novel nociceptin/orphanin FQ receptor antagonist Trap-101 alleviates experimental parkinsonism through inhibition of the nigro-thalamic pathway: Positive interaction with L-DOPA. J. Neurochem. 2008, 107, 1683–1696. [Google Scholar] [CrossRef] [PubMed]
- Mabrouk, O.S.; Marti, M.; Morari, M. Endogenous nociceptin/orphanin FQ (N/OFQ) contributes to haloperidol-induced changes of nigral amino acid transmission and parkinsonism: A combined microdialysis and behavioral study in naive and nociceptin/orphanin FQ receptor knockout mice. Neuroscience 2010, 166, 40–48. [Google Scholar] [CrossRef] [PubMed]
- Spiess, J.; Rivier, J.; Rivier, C.; Vale, W. Primary structure of corticotropin-releasing factor from ovine hypothalamus. Proc. Natl. Acad. Sci. USA 1981, 78, 6517–6521. [Google Scholar] [CrossRef]
- Herman, J.P.; Cullinan, W.E. Neurocircuitry of stress: Central control of the hypothalamo-pituitary-adrenocortical axis. Trends Neurosci. 1997, 20, 78–84. [Google Scholar] [CrossRef]
- Schank, J.R.; Ryabinin, A.E.; Giardino, W.J.; Ciccocioppo, R.; Heilig, M. Stress-related neuropeptides and addictive behaviors: Beyond the usual suspects. Neuron 2012, 76, 192–208. [Google Scholar] [CrossRef] [PubMed]
- Witkin, J.M.; Statnick, M.A.; Rorick-Kehn, L.M.; Pintar, J.E.; Ansonoff, M.; Chen, Y.; Tucker, R.C.; Ciccocioppo, R. The biology of Nociceptin/Orphanin FQ (N/OFQ) related to obesity, stress, anxiety, mood, and drug dependence. Pharmacol. Ther. 2014, 141, 283–299. [Google Scholar] [CrossRef]
- Charlton, B.G.; Ferrier, I.N.; Perry, R.H. Distribution of corticotropin-releasing factor-like immunoreactivity in human brain. Neuropeptides 1987, 10, 329–334. [Google Scholar] [CrossRef]
- Swanson, L.W.; Sawchenko, P.E.; Rivier, J.; Vale, W.W. Organization of ovine corticotropin-releasing factor immunoreactive cells and fibers in the rat brain: An immunohistochemical study. Neuroendocrinology 1983, 36, 165–186. [Google Scholar] [CrossRef] [PubMed]
- Heimer, L.; Alheid, G.F. Piecing together the puzzle of basal forebrain anatomy. Adv. Exp. Med. Biol. 1991, 295, 1–42. [Google Scholar]
- Day, H.E.; Nebel, S.; Sasse, S.; Campeau, S. Inhibition of the central extended amygdala by loud noise and restraint stress. Eur. J. Neurosci. 2005, 21, 441–454. [Google Scholar] [CrossRef]
- Hammack, S.E.; Richey, K.J.; Watkins, L.R.; Maier, S.F. Chemical lesion of the bed nucleus of the stria terminalis blocks the behavioral consequences of uncontrollable stress. Behav. Neurosci. 2004, 118, 443–448. [Google Scholar] [CrossRef]
- Heinrichs, S.C.; Menzaghi, F.; Merlo Pich, E.; Britton, K.T.; Koob, G.F. The role of CRF in behavioral aspects of stress. Ann. N. Y. Acad. Sci. 1995, 771, 92–104. [Google Scholar] [CrossRef]
- Devine, D.P.; Watson, S.J.; Akil, H. Nociceptin/orphanin FQ regulates neuroendocrine function of the limbic-hypothalamic-pituitary-adrenal axis. Neuroscience 2001, 102, 541–553. [Google Scholar] [CrossRef]
- Ciccocioppo, R.; Fedeli, A.; Economidou, D.; Policani, F.; Weiss, F.; Massi, M. The bed nucleus is a neuroanatomical substrate for the anorectic effect of corticotropin-releasing factor and for its reversal by nociceptin/orphanin FQ. J. Neurosci. 2003, 23, 9445–9451. [Google Scholar] [CrossRef] [PubMed]
- Rodi, D.; Zucchini, S.; Simonato, M.; Cifani, C.; Massi, M.; Polidori, C. Functional antagonism between nociceptin/orphanin FQ (N/OFQ) and corticotropin-releasing factor (CRF) in the rat brain: Evidence for involvement of the bed nucleus of the stria terminalis. Psychopharmacology (Berlin) 2008, 196, 523–531. [Google Scholar] [CrossRef]
- Uchiyama, H.; Toda, A.; Hiranita, T.; Watanabe, S.; Eyanagi, R. Role of amygdaloid nuclei in the anxiolytic-like effect of nociceptin/orphanin FQ in rats. Neurosci. Lett. 2008, 431, 66–70. [Google Scholar] [CrossRef]
- Ciccocioppo, R.; de Guglielmo, G.; Hansson, A.C.; Ubaldi, M.; Kallupi, M.; Cruz, M.T.; Oleata, C.S.; Heilig, M.; Roberto, M. Restraint stress alters nociceptin/orphanin FQ and CRF systems in the rat central amygdala: Significance for anxiety-like behaviors. J. Neurosci. 2014, 34, 363–372. [Google Scholar] [CrossRef] [PubMed]
- Roberto, M.; Siggins, G.R. Nociceptin/orphanin FQ presynaptically decreases GABAergic transmission and blocks the ethanol-induced increase of GABA release in central amygdala. Proc. Natl. Acad. Sci. USA 2006, 103, 9715–9720. [Google Scholar] [CrossRef] [PubMed]
- Kallupi, M.; Varodayan, F.P.; Oleata, C.S.; Correia, D.; Luu, G.; Roberto, M. Nociceptin/orphanin FQ decreases glutamate transmission and blocks ethanol-induced effects in the central amygdala of naive and ethanol-dependent rats. Neuropsychopharmacology 2014, 39, 1081–1092. [Google Scholar] [CrossRef]
- Meis, S.; Pape, H.C. Postsynaptic mechanisms underlying responsiveness of amygdaloid neurons to nociceptin/orphanin FQ. J. Neurosci. 1998, 18, 8133–8144. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.L.; Li, A.H.; Yeh, T.H.; Chou, A.H.; Wang, H.L. Nocistatin and nociceptin exert opposite effects on the excitability of central amygdala nucleus-periaqueductal gray projection neurons. Mol. Cell. Neurosci. 2009, 40, 76–88. [Google Scholar] [CrossRef] [PubMed]
- Chieng, B.; Christie, M.J. Somatostatin and nociceptin inhibit neurons in the central nucleus of amygdala that project to the periaqueductal grey. Neuropharmacology 2010, 59, 425–430. [Google Scholar] [CrossRef]
- Green, M.K.; Devine, D.P. Nociceptin/orphanin FQ and NOP receptor gene regulation after acute or repeated social defeat stress. Neuropeptides 2009, 43, 507–514. [Google Scholar] [CrossRef]
- Ciccocioppo, R.; Cippitelli, A.; Economidou, D.; Fedeli, A.; Massi, M. Nociceptin/orphanin FQ acts as a functional antagonist of corticotropin-releasing factor to inhibit its anorectic effect. Physiol. Behav. 2004, 82, 63–68. [Google Scholar] [CrossRef]
- Cruz, M.T.; Herman, M.A.; Kallupi, M.; Roberto, M. Nociceptin/orphanin FQ blockade of corticotropin-releasing factor-induced gamma-aminobutyric acid release in central amygdala is enhanced after chronic ethanol exposure. Biol. Psychiatry 2012, 71, 666–676. [Google Scholar] [CrossRef]
- Dawe, K.L.; Wakerley, J.B.; Fulford, A.J. Nociceptin/orphanin FQ and the regulation of neuronal excitability in the rat bed nucleus of the stria terminalis: Interaction with glucocorticoids. Stress 2010, 13, 516–527. [Google Scholar] [CrossRef]
- Prager, E.M.; Bergstrom, H.C.; Wynn, G.H.; Braga, M.F. The basolateral amygdala gamma-aminobutyric acidergic system in health and disease. J. Neurosci. Res. 2016, 94, 548–567. [Google Scholar] [CrossRef]
- Economidou, D.; Hansson, A.C.; Weiss, F.; Terasmaa, A.; Sommer, W.H.; Cippitelli, A.; Fedeli, A.; Martin-Fardon, R.; Massi, M.; Ciccocioppo, R.; et al. Dysregulation of nociceptin/orphanin FQ activity in the amygdala is linked to excessive alcohol drinking in the rat. Biol. Psychiatry 2008, 64, 211–218. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Meis, S.; Pape, H.C. Control of glutamate and GABA release by nociceptin/orphanin FQ in the rat lateral amygdala. J. Physiol. 2001, 532 Pt 3, 701–712. [Google Scholar] [CrossRef] [PubMed]
- Schlicker, E.; Werthwein, S.; Kathmann, M.; Bauer, U. Nociceptin inhibits noradrenaline release in the mouse brain cortex via presynaptic ORL1 receptors. Naunyn-Schmiedebergs Arch. Pharm. 1998, 358, 418–422. [Google Scholar] [CrossRef]
- Werthwein, S.; Bauer, U.; Nakazi, M.; Kathmann, M.; Schlicker, E. Further characterization of the ORL1 receptor-mediated inhibition of noradrenaline release in the mouse brain in vitro. Br. J. Pharmacol. 1999, 127, 300–308. [Google Scholar] [CrossRef] [PubMed]
- Siniscalchi, A.; Rodi, D.; Morari, M.; Marti, M.; Cavallini, S.; Marino, S.; Beani, L.; Bianchi, C. Direct and indirect inhibition by nociceptin/orphanin FQ on noradrenaline release from rodent cerebral cortex in vitro. Br. J. Pharmacol. 2002, 136, 1178–1184. [Google Scholar] [CrossRef] [PubMed]
- Marti, M.; Stocchi, S.; Paganini, F.; Mela, F.; De Risi, C.; Calo, G.; Guerrini, R.; Barnes, T.A.; Lambert, D.G.; Beani, L.; et al. Pharmacological profiles of presynaptic nociceptin/orphanin FQ receptors modulating 5-hydroxytryptamine and noradrenaline release in the rat neocortex. Br. J. Pharmacol. 2003, 138, 91–98. [Google Scholar] [CrossRef] [PubMed]
- Connor, M.; Vaughan, C.W.; Chieng, B.; Christie, M.J. Nociceptin receptor coupling to a potassium conductance in rat locus coeruleus neurones in vitro. Br. J. Pharmacol. 1996, 119, 1614–1618. [Google Scholar] [CrossRef] [PubMed]
- Gavioli, E.C.; Vaughan, C.W.; Marzola, G.; Guerrini, R.; Mitchell, V.A.; Zucchini, S.; De Lima, T.C.; Rae, G.A.; Salvadori, S.; Regoli, D.; et al. Antidepressant-like effects of the nociceptin/orphanin FQ receptor antagonist UFP-101: New evidence from rats and mice. Naunyn-Schmiedebergs Arch. Pharm. 2004, 369, 547–553. [Google Scholar] [CrossRef] [PubMed]
- Yoshitake, S.; Ijiri, S.; Kehr, J.; Yoshitake, T. Concurrent modulation of extracellular levels of noradrenaline and cAMP during stress and by anxiogenic- or anxiolytic-like neuropeptides in the prefrontal cortex of awake rats. Neurochem. Int. 2013, 62, 314–323. [Google Scholar] [CrossRef]
- Kawahara, Y.; Hesselink, M.B.; van Scharrenburg, G.; Westerink, B.H. Tonic inhibition by orphanin FQ/nociceptin of noradrenaline neurotransmission in the amygdala. Eur. J. Pharmacol. 2004, 485, 197–200. [Google Scholar] [CrossRef]
- Siniscalchi, A.; Rodi, D.; Beani, L.; Bianchi, C. Inhibitory effect of nociceptin on [3H]-5-HT release from rat cerebral cortex slices. Br. J. Pharmacol. 1999, 128, 119–123. [Google Scholar] [CrossRef] [PubMed]
- Sbrenna, S.; Marti, M.; Morari, M.; Calo, G.; Guerrini, R.; Beani, L.; Bianchi, C. Modulation of 5-hydroxytryptamine efflux from rat cortical synaptosomes by opioids and nociceptin. Br. J. Pharmacol. 2000, 130, 425–433. [Google Scholar] [CrossRef][Green Version]
- Tao, R.; Ma, Z.; Thakkar, M.M.; McCarley, R.W.; Auerbach, S.B. Nociceptin/orphanin FQ decreases serotonin efflux in the rat brain but in contrast to a kappa-opioid has no antagonistic effect on mu-opioid-induced increases in serotonin efflux. Neuroscience 2007, 147, 106–116. [Google Scholar] [CrossRef]
- Vaughan, C.W.; Christie, M.J. Increase by the ORL1 receptor (opioid receptor-like1) ligand, nociceptin, of inwardly rectifying K conductance in dorsal raphe nucleus neurones. Br. J. Pharmacol. 1996, 117, 1609–1611. [Google Scholar] [CrossRef] [PubMed]
- Nazzaro, C.; Marino, S.; Barbieri, M.; Siniscalchi, A. Inhibition of serotonin outflow by nociceptin/orphaninFQ in dorsal raphe nucleus slices from normal and stressed rats: Role of corticotropin releasing factor. Neurochem. Int. 2009, 54, 378–384. [Google Scholar] [CrossRef]
- Nazzaro, C.; Barbieri, M.; Varani, K.; Beani, L.; Valentino, R.J.; Siniscalchi, A. Swim stress enhances nociceptin/orphanin FQ-induced inhibition of rat dorsal raphe nucleus activity in vivo and in vitro: Role of corticotropin releasing factor. Neuropharmacology 2010, 58, 457–464. [Google Scholar] [CrossRef][Green Version]
- Rorick-Kehn, L.M.; Ciccocioppo, R.; Wong, C.J.; Witkin, J.M.; Martinez-Grau, M.A.; Stopponi, S.; Adams, B.L.; Katner, J.S.; Perry, K.W.; Toledo, M.A.; et al. A Novel, Orally Bioavailable Nociceptin Receptor Antagonist, LY2940094, Reduces Ethanol Self-Administration and Ethanol Seeking in Animal Models. Alcohol. Clin. Exp. Res. 2016, 40, 945–954. [Google Scholar] [CrossRef]
- Olszewski, P.K.; Billington, C.J.; Levine, A.S. Fos expression in feeding-related brain areas following intracerebroventricular administration of orphanin FQ in rats. Brain Res. 2000, 855, 171–175. [Google Scholar] [CrossRef]
- Fernandez, F.; Misilmeri, M.A.; Felger, J.C.; Devine, D.P. Nociceptin/orphanin FQ increases anxiety-related behavior and circulating levels of corticosterone during neophobic tests of anxiety. Neuropsychopharmacology 2004, 29, 59–71. [Google Scholar] [CrossRef]
- Leggett, J.D.; Harbuz, M.S.; Jessop, D.S.; Fulford, A.J. The nociceptin receptor antagonist [Nphe1,Arg14,Lys15]nociceptin/orphanin FQ-NH2 blocks the stimulatory effects of nociceptin/orphanin FQ on the HPA axis in rats. Neuroscience 2006, 141, 2051–2057. [Google Scholar] [CrossRef]
- Vitale, G.; Ruggieri, V.; Filaferro, M.; Frigeri, C.; Alboni, S.; Tascedda, F.; Brunello, N.; Guerrini, R.; Cifani, C.; Massi, M. Chronic treatment with the selective NOP receptor antagonist [Nphe 1, Arg 14, Lys 15]N/OFQ-NH 2 (UFP-101) reverses the behavioural and biochemical effects of unpredictable chronic mild stress in rats. Psychopharmacology 2009, 207, 173–189. [Google Scholar] [CrossRef] [PubMed]
- Devine, D.P.; Hoversten, M.T.; Ueda, Y.; Akil, H. Nociceptin/orphanin FQ content is decreased in forebrain neurones during acute stress. J. Neuroendocr. 2003, 15, 69–74. [Google Scholar] [CrossRef] [PubMed]
- Leggett, J.D.; Jessop, D.S.; Fulford, A.J. The nociceptin/orphanin FQ antagonist UFP-101 differentially modulates the glucocorticoid response to restraint stress in rats during the peak and nadir phases of the hypothalamo-pituitary-adrenal axis circadian rhythm. Neuroscience 2007, 147, 757–764. [Google Scholar] [CrossRef] [PubMed]
- Green, M.K.; Barbieri, E.V.; Brown, B.D.; Chen, K.W.; Devine, D.P. Roles of the bed nucleus of stria terminalis and of the amygdala in N/OFQ-mediated anxiety and HPA axis activation. Neuropeptides 2007, 41, 399–410. [Google Scholar] [CrossRef]
- Allen, C.N.; Jiang, Z.G.; Teshima, K.; Darland, T.; Ikeda, M.; Nelson, C.S.; Quigley, D.I.; Yoshioka, T.; Allen, R.G.; Rea, M.A.; et al. Orphanin-FQ/nociceptin (OFQ/N) modulates the activity of suprachiasmatic nucleus neurons. J. Neurosci. 1999, 19, 2152–2160. [Google Scholar] [CrossRef]
- Mollereau, C.; Mouledous, L. Tissue distribution of the opioid receptor-like (ORL1) receptor. Peptides 2000, 21, 907–917. [Google Scholar] [CrossRef]
- Gillette, M.U.; Tischkau, S.A. Suprachiasmatic nucleus: The brain’s circadian clock. Recent Prog. Horm. Res. 1999, 54, 33–58; discussion 58–59. [Google Scholar]
- Dibner, C.; Schibler, U.; Albrecht, U. The mammalian circadian timing system: Organization and coordination of central and peripheral clocks. Annu. Rev. Physiol. 2010, 72, 517–549. [Google Scholar] [CrossRef] [PubMed]
- Koch, C.E.; Leinweber, B.; Drengberg, B.C.; Blaum, C.; Oster, H. Interaction between circadian rhythms and stress. Neurobiol. Stress 2017, 6, 57–67. [Google Scholar] [CrossRef] [PubMed]
- Gompf, H.S.; Moldavan, M.G.; Irwin, R.P.; Allen, C.N. Nociceptin/orphanin FQ (N/OFQ) inhibits excitatory and inhibitory synaptic signaling in the suprachiasmatic nucleus (SCN). Neuroscience 2005, 132, 955–965. [Google Scholar] [CrossRef] [PubMed]
- Teshima, K.; Minoguchi, M.; Tounai, S.; Ashimori, A.; Eguchi, J.; Allen, C.N.; Shibata, S. Nonphotic entrainment of the circadian body temperature rhythm by the selective ORL1 receptor agonist W-212393 in rats. Br. J. Pharmacol. 2005, 146, 33–40. [Google Scholar] [CrossRef] [PubMed]
- Sugino, T.; Shimazoe, T.; Ikeda, M.; Watanabe, S. Role of nociceptin and opioid receptor like 1 on entrainment function in the rat suprachiasmatic nucleus. Neuroscience 2006, 137, 537–544. [Google Scholar] [CrossRef]
- Griebel, G.; Perrault, G.; Sanger, D.J. Orphanin FQ, a novel neuropeptide with anti-stress-like activity. Brain Res. 1999, 836, 221–224. [Google Scholar] [CrossRef]
- Gavioli, E.C.; Rae, G.A.; Calo, G.; Guerrini, R.; De Lima, T.C. Central injections of nocistatin or its C-terminal hexapeptide exert anxiogenic-like effect on behaviour of mice in the plus-maze test. Br. J. Pharmacol. 2002, 136, 764–772. [Google Scholar] [CrossRef]
- Kamei, J.; Matsunawa, Y.; Miyata, S.; Tanaka, S.; Saitoh, A. Effects of nociceptin on the exploratory behavior of mice in the hole-board test. Eur. J. Pharmacol. 2004, 489, 77–87. [Google Scholar] [CrossRef]
- Vitale, G.; Arletti, R.; Ruggieri, V.; Cifani, C.; Massi, M. Anxiolytic-like effects of nociceptin/orphanin FQ in the elevated plus maze and in the conditioned defensive burying test in rats. Peptides 2006, 27, 2193–2200. [Google Scholar] [CrossRef]
- Aujla, H.; Cannarsa, R.; Romualdi, P.; Ciccocioppo, R.; Martin-Fardon, R.; Weiss, F. Modification of anxiety-like behaviors by nociceptin/orphanin FQ (N/OFQ) and time-dependent changes in N/OFQ-NOP gene expression following ethanol withdrawal. Addict. Biol. 2013, 18, 467–479. [Google Scholar] [CrossRef]
- Filaferro, M.; Ruggieri, V.; Novi, C.; Calo, G.; Cifani, C.; Micioni Di Bonaventura, M.V.; Sandrini, M.; Vitale, G. Functional antagonism between nociceptin/orphanin FQ and corticotropin-releasing factor in rat anxiety-related behaviors: Involvement of the serotonergic system. Neuropeptides 2014, 48, 189–197. [Google Scholar] [CrossRef]
- Asth, L.; Correia, N.; Lobao-Soares, B.; De Lima, T.C.; Guerrini, R.; Calo, G.; Soares-Rachetti, V.P.; Gavioli, E.C. Nociceptin/orphanin FQ induces simultaneously anxiolytic and amnesic effects in the mouse elevated T-maze task. Naunyn-Schmiedebergs Arch. Pharm. 2015, 388, 33–41. [Google Scholar] [CrossRef]
- Goeldner, C.; Spooren, W.; Wichmann, J.; Prinssen, E.P. Further characterization of the prototypical nociceptin/orphanin FQ peptide receptor agonist Ro 64-6198 in rodent models of conflict anxiety and despair. Psychopharmacology (Berlin) 2012, 222, 203–214. [Google Scholar] [CrossRef] [PubMed]
- Aziz, A.M.; Brothers, S.; Sartor, G.; Holm, L.; Heilig, M.; Wahlestedt, C.; Thorsell, A. The nociceptin/orphanin FQ receptor agonist SR-8993 as a candidate therapeutic for alcohol use disorders: Validation in rat models. Psychopharmacology (Berlin) 2016, 233, 3553–3563. [Google Scholar] [CrossRef]
- Dautzenberg, F.M.; Wichmann, J.; Higelin, J.; Py-Lang, G.; Kratzeisen, C.; Malherbe, P.; Kilpatrick, G.J.; Jenck, F. Pharmacological characterization of the novel nonpeptide orphanin FQ/nociceptin receptor agonist Ro 64-6198: Rapid and reversible desensitization of the ORL1 receptor in vitro and lack of tolerance in vivo. J. Pharmacol. Exp. Ther. 2001, 298, 812–819. [Google Scholar] [PubMed]
- Varty, G.B.; Lu, S.X.; Morgan, C.A.; Cohen-Williams, M.E.; Hodgson, R.A.; Smith-Torhan, A.; Zhang, H.; Fawzi, A.B.; Graziano, M.P.; Ho, G.D.; et al. The anxiolytic-like effects of the novel, orally active nociceptin opioid receptor agonist 8-[bis(2-methylphenyl)methyl]-3-phenyl-8-azabicyclo[3.2.1]octan-3-ol (SCH 221510). J. Pharmacol. Exp. Ther. 2008, 326, 672–682. [Google Scholar] [CrossRef] [PubMed]
- Nicolas, L.B.; Kolb, Y.; Prinssen, E.P. A combined marble burying-locomotor activity test in mice: A practical screening test with sensitivity to different classes of anxiolytics and antidepressants. Eur. J. Pharmacol. 2006, 547, 106–115. [Google Scholar] [CrossRef]
- Hirao, A.; Imai, A.; Sugie, Y.; Yamada, Y.; Hayashi, S.; Toide, K. Pharmacological characterization of the newly synthesized nociceptin/orphanin FQ-receptor agonist 1-[1-(1-methylcyclooctyl)-4-piperidinyl]-2-[(3R)-3-piperidinyl]-1H-benzimidazole as an anxiolytic agent. J. Pharm. Sci. 2008, 106, 361–368. [Google Scholar] [CrossRef]
- Hayashi, S.; Hirao, A.; Imai, A.; Nakamura, H.; Murata, Y.; Ohashi, K.; Nakata, E. Novel non-peptide nociceptin/orphanin FQ receptor agonist, 1-[1-(1-Methylcyclooctyl)-4-piperidinyl]-2-[(3R)-3-piperidinyl]-1H-benzimidazole: Design, synthesis, and structure-activity relationship of oral receptor occupancy in the brain for orally potent antianxiety drug. J. Med. Chem. 2009, 52, 610–625. [Google Scholar] [PubMed]
- Asth, L.; Ruzza, C.; Malfacini, D.; Medeiros, I.; Guerrini, R.; Zaveri, N.T.; Gavioli, E.C.; Calo, G. Beta-arrestin 2 rather than G protein efficacy determines the anxiolytic-versus antidepressant-like effects of nociceptin/orphanin FQ receptor ligands. Neuropharmacology 2016, 105, 434–442. [Google Scholar] [CrossRef]
- Wichmann, J.; Adam, G.; Rover, S.; Hennig, M.; Scalone, M.; Cesura, A.M.; Dautzenberg, F.M.; Jenck, F. Synthesis of (1S,3aS)-8-(2,3,3a,4,5, 6-hexahydro-1H-phenalen-1-yl)-1-phenyl-1,3,8-triaza-spiro[4. 5]decan-4-one, a potent and selective orphanin FQ (OFQ) receptor agonist with anxiolytic-like properties. Eur. J. Med. Chem. 2000, 35, 839–851. [Google Scholar] [CrossRef]
- Wichmann, J.; Adam, G.; Rover, S.; Cesura, A.M.; Dautzenberg, F.M.; Jenck, F. 8-acenaphthen-1-yl-1-phenyl-1,3,8-triaza-spiro[4.5]decan-4-one derivatives as orphanin FQ receptor agonists. Bioorg. Med. Chem. Lett. 1999, 9, 2343–2348. [Google Scholar] [CrossRef]
- Marti, M.; Viaro, R.; Guerrini, R.; Franchi, G.; Morari, M. Nociceptin/orphanin FQ modulates motor behavior and primary motor cortex output through receptors located in substantia nigra reticulata. Neuropsychopharmacology 2009, 34, 341–355. [Google Scholar] [CrossRef]
- Devine, D.P.; Taylor, L.; Reinscheid, R.K.; Monsma, F.J., Jr.; Civelli, O.; Akil, H. Rats rapidly develop tolerance to the locomotor-inhibiting effects of the novel neuropeptide orphanin FQ. Neurochem. Res. 1996, 21, 1387–1396. [Google Scholar] [CrossRef]
- Andero, R.; Brothers, S.P.; Jovanovic, T.; Chen, Y.T.; Salah-Uddin, H.; Cameron, M.; Bannister, T.D.; Almli, L.; Stevens, J.S.; Bradley, B.; et al. Amygdala-dependent fear is regulated by Oprl1 in mice and humans with PTSD. Sci. Transl. Med. 2013, 5, 188ra73. [Google Scholar] [CrossRef] [PubMed]
- Narendran, R.; Tollefson, S.; Fasenmyer, K.; Paris, J.; Himes, M.L.; Lopresti, B.; Ciccocioppo, R.; Mason, N.S. Decreased Nociceptin Receptors Are Related to Resilience and Recovery in College Women Who Have Experienced Sexual Violence: Therapeutic Implications for Posttraumatic Stress Disorder. Biol. Psychiatry 2019, 85, 1056–1064. [Google Scholar] [CrossRef]
- Reiss, D.; Wolter-Sutter, A.; Krezel, W.; Ouagazzal, A.M. Effects of social crowding on emotionality and expression of hippocampal nociceptin/orphanin FQ system transcripts in mice. Behav. Brain Res. 2007, 184, 167–173. [Google Scholar] [CrossRef] [PubMed]
- Nativio, P.; Pascale, E.; Maffei, A.; Scaccianoce, S.; Passarelli, F. Effect of stress on hippocampal nociceptin expression in the rat. Stress 2012, 15, 378–384. [Google Scholar] [CrossRef]
- Koster, A.; Montkowski, A.; Schulz, S.; Stube, E.M.; Knaudt, K.; Jenck, F.; Moreau, J.L.; Nothacker, H.P.; Civelli, O.; Reinscheid, R.K. Targeted disruption of the orphanin FQ/nociceptin gene increases stress susceptibility and impairs stress adaptation in mice. Proc. Natl. Acad. Sci. USA 1999, 96, 10444–10449. [Google Scholar] [CrossRef]
- Gavioli, E.C.; Rizzi, A.; Marzola, G.; Zucchini, S.; Regoli, D.; Calo, G. Altered anxiety-related behavior in nociceptin/orphanin FQ receptor gene knockout mice. Peptides 2007, 28, 1229–1239. [Google Scholar] [CrossRef]
- Rizzi, A.; Molinari, S.; Marti, M.; Marzola, G.; Calo, G. Nociceptin/orphanin FQ receptor knockout rats: In vitro and in vivo studies. Neuropharmacology 2011, 60, 572–579. [Google Scholar] [CrossRef]
- Duzzioni, M.; Duarte, F.S.; Leme, L.R.; Gavioli, E.C.; De Lima, T.C. Anxiolytic-like effect of central administration of NOP receptor antagonist UFP-101 in rats submitted to the elevated T-maze. Behav. Brain Res. 2011, 222, 206–211. [Google Scholar] [CrossRef] [PubMed]
- Witkin, J.M.; Rorick-Kehn, L.M.; Benvenga, M.J.; Adams, B.L.; Gleason, S.D.; Knitowski, K.M.; Li, X.; Chaney, S.; Falcone, J.F.; Smith, J.W.; et al. Preclinical findings predicting efficacy and side-effect profile of LY2940094, an antagonist of nociceptin receptors. Pharm. Res. Perspect. 2016, 4, e00275. [Google Scholar] [CrossRef]
- Post, A.; Smart, T.S.; Krikke-Workel, J.; Dawson, G.R.; Harmer, C.J.; Browning, M.; Jackson, K.; Kakar, R.; Mohs, R.; Statnick, M.; et al. A Selective Nociceptin Receptor Antagonist to Treat Depression: Evidence from Preclinical and Clinical Studies. Neuropsychopharmacology 2016, 41, 1803–1812. [Google Scholar] [CrossRef]
- Silva, A.I.; Holanda, V.A.D.; Azevedo Neto, J.G.; Silva Junior, E.D.; Soares-Rachetti, V.P.; Calo, G.; Ruzza, C.; Gavioli, E.C. Blockade of NOP receptor modulates anxiety-related behaviors in mice exposed to inescapable stress. Psychopharmacology (Berlin) 2020, 237, 1633–1642. [Google Scholar] [CrossRef]
- Genovese, R.F.; Dobre, S. Mitigation of adverse behavioral impact from predator exposure by the nociceptin/orphanin FQ peptide antagonist J-113397 in rats. Behav. Pharm. 2017, 28, 521–530. [Google Scholar] [CrossRef] [PubMed]
- Witkin, J.M.; Wallace, T.L.; Martin, W.J. Therapeutic Approaches for NOP Receptor Antagonists in Neurobehavioral Disorders: Clinical Studies in Major Depressive Disorder and Alcohol Use Disorder with BTRX-246040 (LY2940094). Handb. Exp. Pharm. 2019, 254, 399–415. [Google Scholar]
- Redrobe, J.P.; Calo, G.; Regoli, D.; Quirion, R. Nociceptin receptor antagonists display antidepressant-like properties in the mouse forced swimming test. Naunyn-Schmiedebergs Arch. Pharm. 2002, 365, 164–167. [Google Scholar] [CrossRef] [PubMed]
- Rizzi, A.; Gavioli, E.C.; Marzola, G.; Spagnolo, B.; Zucchini, S.; Ciccocioppo, R.; Trapella, C.; Regoli, D.; Calo, G. Pharmacological characterization of the nociceptin/orphanin FQ receptor antagonist SB-612111 [(-)-cis-1-methyl-7-[[4-(2,6-dichlorophenyl)piperidin-1-yl]methyl]-6,7,8,9-tetrah ydro-5H-benzocyclohepten-5-ol]: In vivo studies. J. Pharmacol. Exp. Ther. 2007, 321, 968–974. [Google Scholar] [CrossRef]
- Holanda, V.A.D.; Santos, W.B.; Asth, L.; Guerrini, R.; Calo, G.; Ruzza, C.; Gavioli, E.C. NOP agonists prevent the antidepressant-like effects of nortriptyline and fluoxetine but not R-ketamine. Psychopharmacology (Berlin) 2018, 235, 3093–3102. [Google Scholar] [CrossRef]
- Holanda, V.A.D.; Pacifico, S.; Azevedo Neto, J.; Finetti, L.; Lobao-Soares, B.; Calo, G.; Gavioli, E.C.; Ruzza, C. Modulation of the NOP receptor signaling affects resilience to acute stress. J. Psychopharmacol. 2019, 33, 1540–1549. [Google Scholar] [CrossRef] [PubMed]
- Gavioli, E.C.; Marzola, G.; Guerrini, R.; Bertorelli, R.; Zucchini, S.; De Lima, T.C.; Rae, G.A.; Salvadori, S.; Regoli, D.; Calo, G. Blockade of nociceptin/orphanin FQ-NOP receptor signalling produces antidepressant-like effects: Pharmacological and genetic evidences from the mouse forced swimming test. Eur. J. Neurosci. 2003, 17, 1987–1990. [Google Scholar] [CrossRef] [PubMed]
- Vitale, G.; Filaferro, M.; Micioni Di Bonaventura, M.V.; Ruggieri, V.; Cifani, C.; Guerrini, R.; Simonato, M.; Zucchini, S. Effects of [Nphe(1), Arg(14), Lys(15)] N/OFQ-NH2 (UFP-101), a potent NOP receptor antagonist, on molecular, cellular and behavioural alterations associated with chronic mild stress. J. Psychopharmacol. 2017, 31, 691–703. [Google Scholar] [CrossRef]
- Holanda, V.A.; Medeiros, I.U.; Asth, L.; Guerrini, R.; Calo, G.; Gavioli, E.C. Antidepressant activity of nociceptin/orphanin FQ receptor antagonists in the mouse learned helplessness. Psychopharmacology (Berlin) 2016, 233, 2525–2532. [Google Scholar] [CrossRef]
- Gavioli, E.C.; Holanda, V.A.D.; Ruzza, C. NOP Ligands for the Treatment of Anxiety and Mood Disorders. Handb. Exp. Pharm. 2019, 254, 233–257. [Google Scholar]
- Medeiros, I.U.; Ruzza, C.; Asth, L.; Guerrini, R.; Romao, P.R.; Gavioli, E.C.; Calo, G. Blockade of nociceptin/orphanin FQ receptor signaling reverses LPS-induced depressive-like behavior in mice. Peptides 2015, 72, 95–103. [Google Scholar] [CrossRef]
- Santos, J.M.; Martinez, R.C.; Brandao, M.L. Effects of acute and subchronic treatments with fluoxetine and desipramine on the memory of fear in moderate and high-intensity contextual conditioning. Eur. J. Pharmacol. 2006, 542, 121–128. [Google Scholar] [CrossRef]
- Jorge, S.D.; Pobbe, R.L.; de Paula Soares, V.; de Oliveira, A.M.; Zangrossi, H., Jr. Effects of sibutramine on anxiety-related behaviours in rats. Pharm. Res. 2004, 50, 517–522. [Google Scholar] [CrossRef] [PubMed]
- Narendran, R.; Tollefson, S.; Himes, M.L.; Paris, J.; Lopresti, B.; Ciccocioppo, R.; Mason, N.S. Nociceptin Receptors Upregulated in Cocaine Use Disorder: A Positron Emission Tomography Imaging Study Using [(11)C]NOP-1A. Am. J. Psychiatry 2019, 176, 468–476. [Google Scholar] [CrossRef]
- Narendran, R.; Ciccocioppo, R.; Lopresti, B.; Paris, J.; Himes, M.L.; Mason, N.S. Nociceptin Receptors in Alcohol Use Disorders: A Positron Emission Tomography Study Using [(11)C]NOP-1A. Biol. Psychiatry 2018, 84, 708–714. [Google Scholar] [CrossRef]
- Ruggeri, B.; Macare, C.; Stopponi, S.; Jia, T.; Carvalho, F.M.; Robert, G.; Banaschewski, T.; Bokde, A.L.W.; Bromberg, U.; Buchel, C.; et al. Methylation of OPRL1 mediates the effect of psychosocial stress on binge drinking in adolescents. J. Child Psychol. Psychiatry 2018, 59, 650–658. [Google Scholar] [CrossRef]
- Kuzmin, A.; Bazov, I.; Sheedy, D.; Garrick, T.; Harper, C.; Bakalkin, G. Expression of pronociceptin and its receptor is downregulated in the brain of human alcoholics. Brain Res. 2009, 1305, S80–S85. [Google Scholar] [CrossRef]
- Lutfy, K.; Zaveri, N.T. The Nociceptin Receptor as an Emerging Molecular Target for Cocaine Addiction. Prog. Mol. Biol. Transl. Sci. 2016, 137, 149–181. [Google Scholar]
- Zaveri, N.T. The nociceptin/orphanin FQ receptor (NOP) as a target for drug abuse medications. Curr. Top. Med. Chem. 2011, 11, 1151–1156. [Google Scholar] [CrossRef]
- Sinha, R. Chronic stress, drug use, and vulnerability to addiction. Ann. N. Y. Acad. Sci. 2008, 1141, 105–130. [Google Scholar] [CrossRef]
- Ciccocioppo, R.; Economidou, D.; Fedeli, A.; Angeletti, S.; Weiss, F.; Heilig, M.; Massi, M. Attenuation of ethanol self-administration and of conditioned reinstatement of alcohol-seeking behaviour by the antiopioid peptide nociceptin/orphanin FQ in alcohol-preferring rats. Psychopharmacology (Berlin) 2004, 172, 170–178. [Google Scholar] [CrossRef] [PubMed]
- Ciccocioppo, R.; Economidou, D.; Cippitelli, A.; Cucculelli, M.; Ubaldi, M.; Soverchia, L.; Lourdusamy, A.; Massi, M. Genetically selected Marchigian Sardinian alcohol-preferring (msP) rats: An animal model to study the neurobiology of alcoholism. Addict. Biol. 2006, 11, 339–355. [Google Scholar] [CrossRef] [PubMed]
- Borruto, A.M.; Stopponi, S.; Li, H.; Weiss, F.; Roberto, M.; Ciccocioppo, R. Genetically selected alcohol-preferring msP rats to study alcohol use disorder: Anything lost in translation? Neuropharmacology 2021, 186, 108446. [Google Scholar] [CrossRef]
- Caputi, F.F.; Stopponi, S.; Rullo, L.; Palmisano, M.; Ubaldi, M.; Candeletti, S.; Ciccocioppo, R.; Romualdi, P. Dysregulation of Nociceptin/Orphanin FQ and Dynorphin Systems in the Extended Amygdala of Alcohol Preferring Marchigian Sardinian (msP) Rats. Int. J. Mol. Sci. 2021, 22, 2448. [Google Scholar] [CrossRef]
- Aujla, H.; Nedjadrasul, D. Low-dose Nociceptin/Orphanin FQ reduces anxiety-like performance in alcohol-withdrawn, but not alcohol-naive, Male Wistar rats. Neuropharmacology 2015, 93, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Economidou, D.; Cippitelli, A.; Stopponi, S.; Braconi, S.; Clementi, S.; Ubaldi, M.; Martin-Fardon, R.; Weiss, F.; Massi, M.; Ciccocioppo, R. Activation of brain NOP receptors attenuates acute and protracted alcohol withdrawal symptoms in the rat. Alcohol. Clin. Exp. Res. 2011, 35, 747–755. [Google Scholar] [CrossRef][Green Version]
- Koob, G.F.; Volkow, N.D. Neurocircuitry of addiction. Neuropsychopharmacology 2010, 35, 217–238. [Google Scholar] [CrossRef]
- Ciccocioppo, R.; Stopponi, S.; Economidou, D.; Kuriyama, M.; Kinoshita, H.; Heilig, M.; Roberto, M.; Weiss, F.; Teshima, K. Chronic treatment with novel brain-penetrating selective NOP receptor agonist MT-7716 reduces alcohol drinking and seeking in the rat. Neuropsychopharmacology 2014, 39, 2601–2610. [Google Scholar] [CrossRef] [PubMed]
- De Guglielmo, G.; Martin-Fardon, R.; Teshima, K.; Ciccocioppo, R.; Weiss, F. MT-7716, a potent NOP receptor agonist, preferentially reduces ethanol seeking and reinforcement in post-dependent rats. Addict. Biol. 2015, 20, 643–651. [Google Scholar] [CrossRef]
- Li, H.; Scuppa, G.; Shen, Q.; Masi, A.; Nasuti, C.; Cannella, N.; Ciccocioppo, R. NOP Receptor Agonist Ro 64-6198 Decreases Escalation of Cocaine Self-Administration in Rats Genetically Selected for Alcohol Preference. Front. Psychiatry 2019, 10, 176. [Google Scholar] [CrossRef] [PubMed]
- Cippitelli, A.; Barnes, M.; Zaveri, N.T.; Toll, L. Potent and selective NOP receptor activation reduces cocaine self-administration in rats by lowering hedonic set point. Addict. Biol. 2019, 25, e12844. [Google Scholar] [CrossRef] [PubMed]
- Mantsch, J.R.; Baker, D.A.; Funk, D.; Le, A.D.; Shaham, Y. Stress-Induced Reinstatement of Drug Seeking: 20 Years of Progress. Neuropsychopharmacology 2016, 41, 335–356. [Google Scholar] [CrossRef]
- Martin-Fardon, R.; Ciccocioppo, R.; Massi, M.; Weiss, F. Nociceptin prevents stress-induced ethanol- but not cocaine-seeking behavior in rats. Neuroreport 2000, 11, 1939–1943. [Google Scholar] [CrossRef] [PubMed]
- Kallupi, M.; Scuppa, G.; de Guglielmo, G.; Calo, G.; Weiss, F.; Statnick, M.A.; Rorick-Kehn, L.M.; Ciccocioppo, R. Genetic Deletion of the Nociceptin/Orphanin FQ Receptor in the Rat Confers Resilience to the Development of Drug Addiction. Neuropsychopharmacology 2017, 42, 695–706. [Google Scholar] [CrossRef] [PubMed]
- Borruto, A.M.; Fotio, Y.; Stopponi, S.; Brunori, G.; Petrella, M.; Caputi, F.F.; Romualdi, P.; Candeletti, S.; Narendran, R.; Rorick-Kehn, L.M.; et al. NOP receptor antagonism reduces alcohol drinking in male and female rats through mechanisms involving the central amygdala and ventral tegmental area. Br. J. Pharmacol. 2020, 177, 1525–1537. [Google Scholar] [CrossRef]
- Malfacini, D.; Ambrosio, C.; Gro, M.C.; Sbraccia, M.; Trapella, C.; Guerrini, R.; Bonora, M.; Pinton, P.; Costa, T.; Calo, G. Pharmacological Profile of Nociceptin/Orphanin FQ Receptors Interacting with G-Proteins and beta-Arrestins 2. PLoS ONE 2015, 10, e0132865. [Google Scholar] [CrossRef] [PubMed]
- Di Bonaventura, M.V.M.; Di Bonaventura, E.M.; Cifani, C.; Polidori, C. N/OFQ-NOP System in Food Intake. Handb. Exp. Pharmacol. 2019, 254, 279–295. [Google Scholar]
- Avena, N.M. Food and addiction: Implications and relevance to eating disorders and obesity. Curr. Drug Abus. Rev. 2011, 4, 131–132. [Google Scholar] [CrossRef]
- Avena, N.M.; Bocarsly, M.E.; Hoebel, B.G.; Gold, M.S. Overlaps in the nosology of substance abuse and overeating: The translational implications of “food addiction”. Curr. Drug Abus. Rev. 2011, 4, 133–139. [Google Scholar] [CrossRef]
- D’Addario, C.; Di Bonaventura, M.V.M.; Pucci, M.; Romano, A.; Gaetani, S.; Ciccocioppo, R.; Cifani, C.; Maccarrone, M. Endocannabinoid signaling and food addiction. Neurosci. Biobehav. Rev. 2014, 47, 203–224. [Google Scholar] [CrossRef] [PubMed]
- Adeghate, E.; D’Souza, C.M.; Saeed, Z.; Al Jaberi, S.; Tariq, S.; Kalasz, H.; Tekes, K.; Adeghate, E.A. Nociceptin Increases Antioxidant Expression in the Kidney, Liver and Brain of Diabetic Rats. Biology 2021, 10, 621. [Google Scholar] [CrossRef]
- Polidori, C.; de Caro, G.; Massi, M. The hyperphagic effect of nociceptin/orphanin FQ in rats. Peptides 2000, 21, 1051–1062. [Google Scholar] [CrossRef]
- Cifani, C.; Guerrini, R.; Massi, M.; Polidori, C. Chronic intracerebroventricular infusion of nociceptin/orphanin FQ increases food and ethanol intake in alcohol-preferring rats. Peptides 2006, 27, 2803–2810. [Google Scholar] [CrossRef] [PubMed]
- Calo, G.; Rizzi, A.; Cifani, C.; Di Bonaventura, M.V.M.; Regoli, D.; Massi, M.; Salvadori, S.; Lambert, D.G.; Guerrini, R. UFP-112 a potent and long-lasting agonist selective for the Nociceptin/Orphanin FQ receptor. CNS Neurosci. Ther. 2011, 17, 178–198. [Google Scholar] [CrossRef]
- Matsushita, H.; Ishihara, A.; Mashiko, S.; Tanaka, T.; Kanno, T.; Iwaasa, H.; Ohta, H.; Kanatani, A. Chronic intracerebroventricular infusion of nociceptin/orphanin FQ produces body weight gain by affecting both feeding and energy metabolism in mice. Endocrinology 2009, 150, 2668–2673. [Google Scholar] [CrossRef]
- Chee, M.J.; Price, C.J.; Statnick, M.A.; Colmers, W.F. Nociceptin/orphanin FQ suppresses the excitability of neurons in the ventromedial nucleus of the hypothalamus. J. Physiol. 2011, 589 Pt 13, 3103–3114. [Google Scholar] [CrossRef] [PubMed]
- Borgquist, A.; Kachani, M.; Tavitian, N.; Sinchak, K.; Wagner, E.J. Estradiol negatively modulates the pleiotropic actions of orphanin FQ/nociceptin at proopiomelanocortin synapses. Neuroendocrinology 2013, 98, 60–72. [Google Scholar] [CrossRef]
- Hernandez, J.; Fabelo, C.; Perez, L.; Moore, C.; Chang, R.; Wagner, E.J. Nociceptin/orphanin FQ modulates energy homeostasis through inhibition of neurotransmission at VMN SF-1/ARC POMC synapses in a sex- and diet-dependent manner. Biol. Sex Differ. 2019, 10, 9. [Google Scholar] [CrossRef] [PubMed]
- Gastelum, C.; Perez, L.; Hernandez, J.; Le, N.; Vahrson, I.; Sayers, S.; Wagner, E.J. Adaptive Changes in the Central Control of Energy Homeostasis Occur in Response to Variations in Energy Status. Int. J. Mol. Sci. 2021, 22, 2728. [Google Scholar] [CrossRef]
- Sternson, S.M.; Shepherd, G.M.; Friedman, J.M. Topographic mapping of VMH→Arcuate nucleus microcircuits and their reorganization by fasting. Nat. Neurosci. 2005, 8, 1356–1363. [Google Scholar] [CrossRef] [PubMed]
- Krashes, M.J.; Shah, B.P.; Madara, J.C.; Olson, D.P.; Strochlic, D.E.; Garfield, A.S.; Vong, L.; Pei, H.; Watabe-Uchida, M.; Uchida, N.; et al. An excitatory paraventricular nucleus to AgRP neuron circuit that drives hunger. Nature 2014, 507, 238–242. [Google Scholar] [CrossRef]
- Chang, R.; Hernandez, J.; Gastelum, C.; Guadagno, K.; Perez, L.; Wagner, E.J. Pituitary Adenylate Cyclase-Activating Polypeptide Excites Proopiomelanocortin Neurons: Implications for the Regulation of Energy Homeostasis. Neuroendocrinology 2021, 111, 45–69. [Google Scholar] [CrossRef]
- Fabelo, C.; Hernandez, J.; Chang, R.; Seng, S.; Alicea, N.; Tian, S.; Conde, K.; Wagner, E.J. Endocannabinoid Signaling at Hypothalamic Steroidogenic Factor-1/Proopiomelanocortin Synapses Is Sex- and Diet-Sensitive. Front. Mol. Neurosci. 2018, 11, 214. [Google Scholar] [CrossRef]
- Jais, A.; Paeger, L.; Sotelo-Hitschfeld, T.; Bremser, S.; Prinzensteiner, M.; Klemm, P.; Mykytiuk, V.; Widdershooven, P.J.M.; Vesting, A.J.; Grzelka, K.; et al. PNOC(ARC) Neurons Promote Hyperphagia and Obesity upon High-Fat-Diet Feeding. Neuron 2020, 106, 1009–1025.e10. [Google Scholar] [CrossRef]
- Yakimova, K.S.; Pierau, F.K. Nociceptin/orphanin FQ: Effects on thermoregulation in rats. Methods Find. Exp. Clin. Pharmacol. 1999, 21, 345–352. [Google Scholar] [CrossRef]
- Baiula, M.; Bedini, A.; Spampinato, S.M. Role of nociceptin/orphanin FQ in thermoregulation. Neuropeptides 2015, 50, 51–56. [Google Scholar] [CrossRef] [PubMed]
- Di Bonaventura, M.V.M.; Ubaldi, M.; Liberati, S.; Ciccocioppo, R.; Massi, M.; Cifani, C. Caloric restriction increases the sensitivity to the hyperphagic effect of nociceptin/orphanin FQ limiting its ability to reduce binge eating in female rats. Psychopharmacology 2013, 228, 53–63. [Google Scholar] [CrossRef]
- Olszewski, P.K.; Grace, M.K.; Billington, C.J.; Levine, A.S. The effect of [Phe(1)psi(CH(2)-NH)Gly(2)]-nociceptin(1-13)NH(2) on feeding and c-Fos immunoreactivity in selected brain sites. Brain Res. 2000, 876, 95–102. [Google Scholar] [CrossRef]
- Olszewski, P.K.; Grace, M.K.; Sanders, J.B.; Billington, C.J.; Levine, A.S. Effect of nociceptin/orphanin FQ on food intake in rats that differ in diet preference. Pharm. Biochem. Behav. 2002, 73, 529–535. [Google Scholar] [CrossRef]
- Bomberg, E.M.; Grace, M.K.; Levine, A.S.; Olszewski, P.K. Functional interaction between nociceptin/orphanin FQ and alpha-melanocyte-stimulating hormone in the regulation of feeding. Peptides 2006, 27, 1827–1834. [Google Scholar] [CrossRef] [PubMed]
- Olszewski, P.K.; Levine, A.S. Minireview: Characterization of influence of central nociceptin/orphanin FQ on consummatory behavior. Endocrinology 2004, 145, 2627–2632. [Google Scholar] [CrossRef]
- Romano, A.; Di Bonaventura, M.V.M.; Gallelli, C.A.; Koczwara, J.B.; Smeets, D.; Giusepponi, M.E.; De Ceglia, M.; Friuli, M.; Di Bonaventura, E.M.; Scuderi, C.; et al. Oleoylethanolamide decreases frustration stress-induced binge-like eating in female rats: A novel potential treatment for binge eating disorder. Neuropsychopharmacol. Off. Publ. Am. Coll. Neuropsychopharmacol. 2020, 45, 1931–1941. [Google Scholar] [CrossRef]
- Romano, A.; Tempesta, B.; Di Bonaventura, M.V.M.; Gaetani, S. From Autism to Eating Disorders and More: The Role of Oxytocin in Neuropsychiatric Disorders. Front. Neurosci. 2015, 9, 497. [Google Scholar] [CrossRef]
- Baltatzi, M.; Hatzitolios, A.; Tziomalos, K.; Iliadis, F.; Zamboulis, C. Neuropeptide Y and alpha-melanocyte-stimulating hormone: Interaction in obesity and possible role in the development of hypertension. Int. J. Clin. Pract. 2008, 62, 1432–1440. [Google Scholar] [CrossRef]
- Di Bonaventura, E.M.; Botticelli, L.; Tomassoni, D.; Tayebati, S.K.; Di Bonaventura, M.V.M.; Cifani, C. The Melanocortin System behind the Dysfunctional Eating Behaviors. Nutrients 2020, 12, 3502. [Google Scholar] [CrossRef]
- Battistoni, S.; Kloting, I.; Cifani, C.; Massi, M.; Polidori, C. Gender differences in Nociceptin/Orphanin FQ-induced food intake in strains derived from rats prone (WOKW) and resistant (Dark Agouti) to metabolic syndrome: A possible involvement of the cocaine- and amphetamine-regulated transcript system. Genes Nutr. 2011, 6, 197–202. [Google Scholar] [CrossRef][Green Version]
- Cifani, C.; Kloting, I.; Morini, G.; Grandi, D.; Massi, M.; Polidori, C. Nociceptin/orphanin FQ-induced food intake and cocaine amphetamine regulated transcript gene expression in strains derived from rats prone (WOKW) and resistant (Dark Agouti) to metabolic syndrome. Peptides 2009, 30, 727–734. [Google Scholar] [CrossRef]
- Filippetti, R.; Kloting, I.; Massi, M.; Cifani, C.; Polidori, C. Involvement of cocaine-amphetamine regulated transcript in the differential feeding responses to nociceptin/orphanin FQ in dark agouti and Wistar Ottawa Karlsburg W rats. Peptides 2007, 28, 1966–1973. [Google Scholar] [CrossRef]
- Kristensen, P.; Judge, M.E.; Thim, L.; Ribel, U.; Christjansen, K.N.; Wulff, B.S.; Clausen, J.T.; Jensen, P.B.; Madsen, O.D.; Vrang, N.; et al. Hypothalamic CART is a new anorectic peptide regulated by leptin. Nature 1998, 393, 72–76. [Google Scholar] [CrossRef]
- Da Silva, R.A.; de Oliveira, S.T.; Hackl, L.P.; Spilere, C.I.; Faria, M.S.; Marino-Neto, J.; Paschoalini, M.A. Ingestive behaviors and metabolic fuels after central injections of 5-HT1A and 5-HT1D/1B receptors agonists in the pigeon. Brain Res. 2004, 1026, 275–283. [Google Scholar] [CrossRef] [PubMed]
- De Vry, J.; Schreiber, R. Effects of selected serotonin 5-HT(1) and 5-HT(2) receptor agonists on feeding behavior: Possible mechanisms of action. Neurosci. Biobehav. Rev. 2000, 24, 341–353. [Google Scholar] [CrossRef]
- Simansky, K.J. Serotonergic control of the organization of feeding and satiety. Behav. Brain Res. 1996, 73, 37–42. [Google Scholar] [CrossRef]
- Halford, J.C.; Harrold, J.A.; Boyland, E.J.; Lawton, C.L.; Blundell, J.E. Serotonergic drugs: Effects on appetite expression and use for the treatment of obesity. Drugs 2007, 67, 27–55. [Google Scholar] [CrossRef]
- Hardaway, J.A.; Halladay, L.R.; Mazzone, C.M.; Pati, D.; Bloodgood, D.W.; Kim, M.; Jensen, J.; DiBerto, J.F.; Boyt, K.M.; Shiddapur, A.; et al. Central Amygdala Prepronociceptin-Expressing Neurons Mediate Palatable Food Consumption and Reward. Neuron 2019, 102, 1037–1052.e7. [Google Scholar] [CrossRef] [PubMed]
- Cifani, C.; Polidori, C.; Melotto, S.; Ciccocioppo, R.; Massi, M. A preclinical model of binge eating elicited by yo-yo dieting and stressful exposure to food: Effect of sibutramine, fluoxetine, topiramate, and midazolam. Psychopharmacology 2009, 204, 113–125. [Google Scholar] [CrossRef] [PubMed]
- Pucci, M.; Di Bonaventura, M.V.M.; Giusepponi, M.E.; Romano, A.; Filaferro, M.; Maccarrone, M.; Ciccocioppo, R.; Cifani, C.; D’Addario, C. Epigenetic regulation of nociceptin/orphanin FQ and corticotropin-releasing factor system genes in frustration stress-induced binge-like palatable food consumption. Addict. Biol. 2016, 21, 1168–1185. [Google Scholar] [CrossRef] [PubMed]
- Hardaway, J.A.; Jensen, J.; Kim, M.; Mazzone, C.M.; Sugam, J.A.; Diberto, J.F.; Lowery-Gionta, E.G.; Hwa, L.S.; Pleil, K.E.; Bulik, C.M.; et al. Nociceptin receptor antagonist SB 612111 decreases high fat diet binge eating. Behav. Brain Res. 2016, 307, 25–34. [Google Scholar] [CrossRef] [PubMed]
- Statnick, M.A.; Chen, Y.; Ansonoff, M.; Witkin, J.M.; Rorick-Kehn, L.; Suter, T.M.; Song, M.; Hu, C.; Lafuente, C.; Jimenez, A.; et al. A Novel Nociceptin Receptor Antagonist LY2940094 Inhibits Excessive Feeding Behavior in Rodents: A Possible Mechanism for the Treatment of Binge Eating Disorder. J. Pharm. Exp. Ther. 2016, 356, 493–502. [Google Scholar] [CrossRef]
- Kania, A.; Szlaga, A.; Sambak, P.; Gugula, A.; Blasiak, E.; Di Bonaventura, M.V.M.; Hossain, M.A.; Cifani, C.; Hess, G.; Gundlach, A.L.; et al. RLN3/RXFP3 Signaling in the PVN Inhibits Magnocellular Neurons via M-like Current Activation and Contributes to Binge Eating Behavior. J. Neurosci. 2020, 40, 5362–5375. [Google Scholar] [CrossRef] [PubMed]
- De Avila, C.; Chometton, S.; Calvez, J.; Guevremont, G.; Kania, A.; Torz, L.; Lenglos, C.; Blasiak, A.; Rosenkilde, M.M.; Holst, B.; et al. Estrous Cycle Modulation of Feeding and Relaxin-3/Rxfp3 mRNA Expression: Implications for Estradiol Action. Neuroendocrinology 2021, 111, 1201–1218. [Google Scholar] [CrossRef]
- Freeman, L.R.; Bentzley, B.S.; James, M.H.; Aston-Jones, G. Sex Differences in Demand for Highly Palatable Foods: Role of the Orexin System. Int. J. Neuropsychopharmacol./Off. Sci. J. Coll. Int. Neuropsychopharmacol. 2021, 24, 54–63. [Google Scholar] [CrossRef]
- Piccoli, L.; Micioni Di Bonaventura, M.V.; Cifani, C.; Costantini, V.J.; Massagrande, M.; Montanari, D.; Martinelli, P.; Antolini, M.; Ciccocioppo, R.; Massi, M.; et al. Role of orexin-1 receptor mechanisms on compulsive food consumption in a model of binge eating in female rats. Neuropsychopharmacology 2012, 37, 1999–2011. [Google Scholar] [CrossRef]
- Buczek, L.; Migliaccio, J.; Petrovich, G.D. Hedonic Eating: Sex Differences and Characterization of Orexin Activation and Signaling. Neuroscience 2020, 436, 34–45. [Google Scholar] [CrossRef]
- Mikhail, M.E.; Anaya, C.; Culbert, K.M.; Sisk, C.L.; Johnson, A.; Klump, K.L. Gonadal Hormone Influences on Sex Differences in Binge Eating Across Development. Curr. Psychiatry Rep. 2021, 23, 74. [Google Scholar] [CrossRef]
- Ma, R.; Mikhail, M.E.; Culbert, K.M.; Johnson, A.W.; Sisk, C.L.; Klump, K.L. Ovarian Hormones and Reward Processes in Palatable Food Intake and Binge Eating. Physiology (Bethesda) 2020, 35, 69–78. [Google Scholar] [CrossRef]
- Anversa, R.G.; Muthmainah, M.; Sketriene, D.; Gogos, A.; Sumithran, P.; Brown, R.M. A review of sex differences in the mechanisms and drivers of overeating. Front. Neuroendocr. 2021, 63, 100941. [Google Scholar] [CrossRef]
- Klump, K.L.; Racine, S.; Hildebrandt, B.; Sisk, C.L. Sex differences in binge eating patterns in male and female adult rats. Int. J. Eat. Disord. 2013, 46, 729–736. [Google Scholar] [CrossRef] [PubMed]
- Hildebrandt, B.A.; Klump, K.L.; Racine, S.E.; Sisk, C.L. Differential strain vulnerability to binge eating behaviors in rats. Physiol. Behav. 2014, 127, 81–86. [Google Scholar] [CrossRef] [PubMed]
- Di Bonaventura, M.V.M.; Lutz, T.A.; Romano, A.; Pucci, M.; Geary, N.; Asarian, L.; Cifani, C. Estrogenic suppression of binge-like eating elicited by cyclic food restriction and frustrative-nonreward stress in female rats. Int. J. Eat. Disord. 2017, 50, 624–635. [Google Scholar] [CrossRef]
- Alboni, S.; Di Bonaventura, M.V.M.; Benatti, C.; Giusepponi, M.E.; Brunello, N.; Cifani, C. Hypothalamic expression of inflammatory mediators in an animal model of binge eating. Behav. Brain Res. 2017, 320, 420–430. [Google Scholar] [CrossRef]
- Brutman, J.N.; Sirohi, S.; Davis, J.F. Examining the Impact of Estrogen on Binge Feeding, Food-Motivated Behavior, and Body Weight in Female Rats. Obesity (Silver Spring) 2019, 27, 1617–1626. [Google Scholar] [CrossRef] [PubMed]
- De Wit, L.M.; van Straten, A.; van Herten, M.; Penninx, B.W.; Cuijpers, P. Depression and body mass index, a u-shaped association. BMC Public Health 2009, 9, 14. [Google Scholar] [CrossRef]
- Scott, K.M.; McGee, M.A.; Wells, J.E.; Oakley Browne, M.A. Obesity and mental disorders in the adult general population. J. Psychosom. Res. 2008, 64, 97–105. [Google Scholar] [CrossRef]
- Polidori, C.; Calo, G.; Ciccocioppo, R.; Guerrini, R.; Regoli, D.; Massi, M. Pharmacological characterization of the nociceptin receptor mediating hyperphagia: Identification of a selective antagonist. Psychopharmacology 2000, 148, 430–437. [Google Scholar] [CrossRef]
- Gavioli, E.C.; Calo, G. Nociceptin/orphanin FQ receptor antagonists as innovative antidepressant drugs. Pharmacol. Ther. 2013, 140, 10–25. [Google Scholar] [CrossRef]
- Romano, S.J.; Halmi, K.A.; Sarkar, N.P.; Koke, S.C.; Lee, J.S. A placebo-controlled study of fluoxetine in continued treatment of bulimia nervosa after successful acute fluoxetine treatment. Am. J. Psychiatry 2002, 159, 96–102. [Google Scholar] [CrossRef] [PubMed]
- Fluoxetine Bulimia Nervosa Collaborative Study Group. Fluoxetine in the treatment of bulimia nervosa. A multicenter, placebo-controlled, double-blind trial. Fluoxetine Bulimia Nervosa Collaborative Study Group. Arch. Gen. Psychiatry 1992, 49, 139–147. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ubaldi, M.; Cannella, N.; Borruto, A.M.; Petrella, M.; Micioni Di Bonaventura, M.V.; Soverchia, L.; Stopponi, S.; Weiss, F.; Cifani, C.; Ciccocioppo, R. Role of Nociceptin/Orphanin FQ-NOP Receptor System in the Regulation of Stress-Related Disorders. Int. J. Mol. Sci. 2021, 22, 12956. https://doi.org/10.3390/ijms222312956
Ubaldi M, Cannella N, Borruto AM, Petrella M, Micioni Di Bonaventura MV, Soverchia L, Stopponi S, Weiss F, Cifani C, Ciccocioppo R. Role of Nociceptin/Orphanin FQ-NOP Receptor System in the Regulation of Stress-Related Disorders. International Journal of Molecular Sciences. 2021; 22(23):12956. https://doi.org/10.3390/ijms222312956
Chicago/Turabian StyleUbaldi, Massimo, Nazzareno Cannella, Anna Maria Borruto, Michele Petrella, Maria Vittoria Micioni Di Bonaventura, Laura Soverchia, Serena Stopponi, Friedbert Weiss, Carlo Cifani, and Roberto Ciccocioppo. 2021. "Role of Nociceptin/Orphanin FQ-NOP Receptor System in the Regulation of Stress-Related Disorders" International Journal of Molecular Sciences 22, no. 23: 12956. https://doi.org/10.3390/ijms222312956
APA StyleUbaldi, M., Cannella, N., Borruto, A. M., Petrella, M., Micioni Di Bonaventura, M. V., Soverchia, L., Stopponi, S., Weiss, F., Cifani, C., & Ciccocioppo, R. (2021). Role of Nociceptin/Orphanin FQ-NOP Receptor System in the Regulation of Stress-Related Disorders. International Journal of Molecular Sciences, 22(23), 12956. https://doi.org/10.3390/ijms222312956






