Abstract
Arachidonic acid (AA) is an essential fatty acid that is released by phospholipids in cell membranes and metabolized by cyclooxygenase (COX), cytochrome P450 (CYP) enzymes, and lipid oxygenase (LOX) pathways to regulate complex cardiovascular function under physiological and pathological conditions. Various AA metabolites include prostaglandins, prostacyclin, thromboxanes, hydroxyeicosatetraenoic acids, leukotrienes, lipoxins, and epoxyeicosatrienoic acids. The AA metabolites play important and differential roles in the modulation of vascular tone, and cardiovascular complications including atherosclerosis, hypertension, and myocardial infarction upon actions to different receptors and vascular beds. This article reviews the roles of AA metabolism in cardiovascular health and disease as well as their potential therapeutic implication.
1. Introduction
Polyunsaturated fatty acids (PUFAs) have long been considered to have positive effects on cardiovascular health [1]. A meta-analysis study demonstrated a reduction in the risk of cardiovascular events by increasing PUFAs intake [2]. It is noteworthy that arachidonic acid (AA), one of the most abundant PUFAs in the human body, is a long-chain polyunsaturated omega-6 fatty acid containing 20 carbon atoms and 4 double bonds (20:4, n-6), and its role in cardiovascular function has been revealed in recent studies [3,4,5,6]. AA has several physiological functions: as a constituent in the phospholipid bilayer of cell membranes, as a precursor for a crucial group of biologically active compounds known as eicosanoids (C20 unsaturated lipids), as a regulator of gene expression, as inflammatory intermediator, and as vasodilator/vasoconstrictor [7,8,9]. Its mobility and flexibility are attributed to its four cis double bonds that maintain the fluidity of cell membranes at physiological temperatures, and the double bonds can react with oxygen to form eicosanoids and isoprostanes through enzymatic and non-enzymatic mechanisms, respectively [10,11]. Endogenous AA is mainly released through cell membrane phospholipids to produce a myriad of bioactive derivatives, eicosanoids, which can be metabolized by three different enzyme systems, including cyclooxygenase (COX), cytochrome P450 (CYP) enzymes, and lipid oxygenase (LOX) [12]. The oxidized lipid molecules participate in a variety of physiological and pathological functions. Upon binding to corresponding receptors and triggering the downstream signaling pathways in different tissues, AA metabolites play differential roles to control important cellular processes, such as cell apoptosis, cell proliferation, metabolism, and vascular function [7,13], and they are also related to many chronic diseases, especially cardiovascular diseases (CVD) [14,15].
CVD is a disease with high mortality and recurrence rate worldwide [16]. CVD is a hemorrhagic or ischemic disease of blood vessels caused by atherosclerosis and encompasses several entities such as hypertension, pulmonary arterial hypertension (PAH), cardiac hypertrophy, and heart failure [17]. The main risk factor for CVD is metabolic disorder including obesity and diabetes [18]. Despite the recent advances in drug and surgical treatment [19], CVD is still a common and progressive disease that threatens human health. Studies have shown that AA metabolites play an important role in cardiovascular health and disease mechanism, especially related to inflammation and atherosclerosis [15]. AA metabolites regulate the complex vascular functions in the human body and also play a role in the treatment of CVD. The current article reviews the comprehensive involvement of AA metabolites in cardiovascular function, from the differential signaling pathways mediated to their potential therapeutic implications.
2. Food Sources of Arachidonic Acid
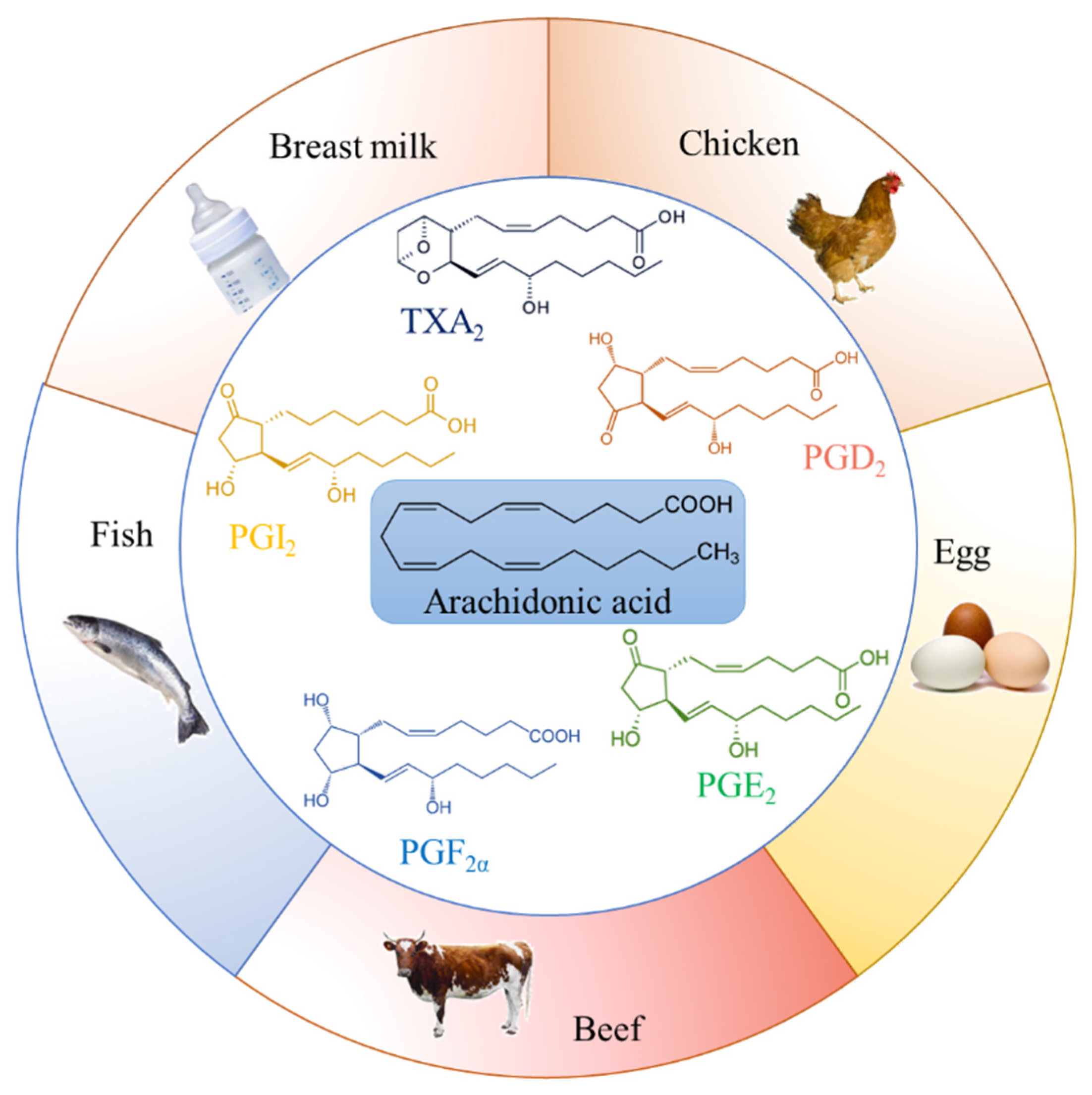
As an important fatty acid for human growth and development, AA can be obtained from various types of food, especially meat and fish products. Food items rich in AA can be seen in Figure 1. According to previous investigations, chicken and chicken-mixed dishes provide the most AA intake to Americans, while eggs, beef and beef products, as well as pork and pork products, are other major contributors of AA from the American diet [20]. Pork provides the most abundant AA intake to South Korea diet, accounting for 70%, followed by eggs [21]. Moreover, invertebrates and fish are rich sources of omega-3 fatty acids and also rich in AA [22]. These PUFAs play important roles in their growth and reproduction, especially in fish; therefore, AA is highly retained in phospholipids of all species [23,24]. The intake of pre-formed AA in food is an important cause of circulating AA [25]. However, previous studies mainly show the dietary content and human intake of AA in America and South Korea. Data on dietary AA from other countries are lacking, and further studies are needed to explore and provide new insights into the relationship between dietary AA with cardiovascular health.
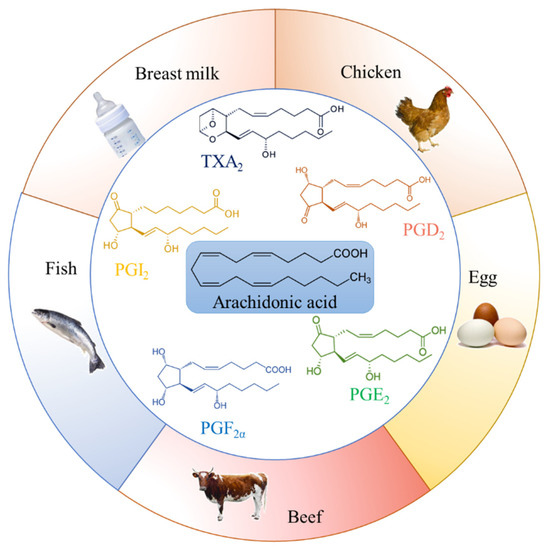
Figure 1.
Food items rich in arachidonic acid. Chicken and chicken-mixed dishes, eggs, beef and beef products, pork and pork products, invertebrates and fish, breast milk and infant formula milk powder provide the most arachidonic acid intake to humans. Prostaglandin (PG)D2, PGE2, PGF2α, prostacyclin (PGI2), and thromboxanes (TX)A2 are major arachidonic acid metabolites. These polyunsaturated fatty acids play an important role in their growth and reproduction.
On the other hand, AA can be converted from linoleic acid even though such endogenous conversion from linoleic acid to AA is generally poor [26]. Linoleic acid and gamma-linolenic acid are the major dietary PUFAs in common diets, and when we consume large amounts of them in our diet, our body can make AA from them [27]. Linoleic acid is broken down into gamma-linolenic acid, which is converted to AA subsequently. Linoleic acid is present in nuts, seeds, and vegetable oils including canola, corn, safflower, and sunflower oils, whereas gamma-linolenic acid is found in black current seed oil, borage oil, evening primrose oil, oats, and spirulina [28]. Around 5% to 10% of linoleic acid is taken up in phospholipid membranes and then converted to AA and bioactive lipid products [29]. Notably, improper intake of PUFAs can lead to chronic diseases such as CVD and metabolic diseases [30]. Notably, AA is a natural component found in breast milk, produced by the conversion of linoleic acid and alpha-linolenic acid of PUFAs [31], having a positive effect on growth and development, such as the brain, retina, and other nervous systems; AA is also added to infant formula milk powder [32]. Compared with European and American countries, the level of AA in Chinese mothers’ breast milk is significantly higher even though the intake of AA is lower [33]. The World Health Organization (WHO) recommends that the AA content should be at least 0.66% of the total fatty acids [34,35] based on the global average level of breast milk, while the French Food Safety Agency proposed a minimum AA intake of 0.5% of total fatty acids [36]. These results indicate that AA is abundant in various food items. The intake of pre-formed AA in food rather than conversion from linoleic acid appears to be a more important source of circulating AA. Thus, the impact of AA on cardiovascular functions is discussed further in the following sections.
3. Pathways Involved in Arachidonic Acid Metabolism
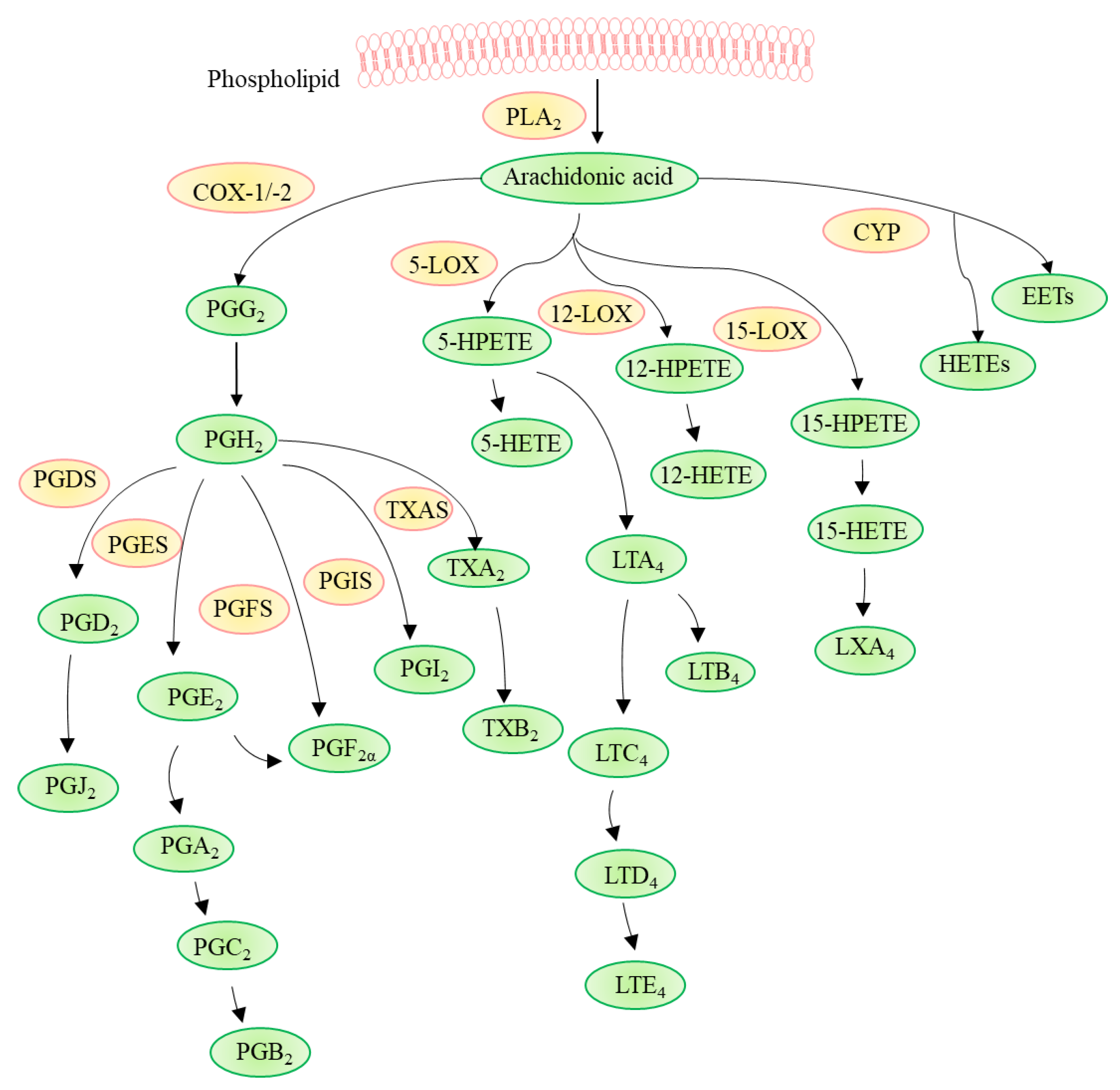
AA is released from cell membrane phospholipids primarily by phospholipase A2 (PLA2) and, in turn, metabolized through three different pathways involving cyclooxygenase (COX), cytochrome P450 (CYP) enzymes (ω-hydroxylases and epoxygenases), or lipoxygenase (LOX) (Figure 2) [37,38]. Various substances such as acetylcholine and shear stress can activate PLA2 and trigger the downstream mechanism in vascular endothelial cells (ECs). AA metabolism takes place in several organs including the brain, heart, kidney, liver, lung, and vasculature [12].
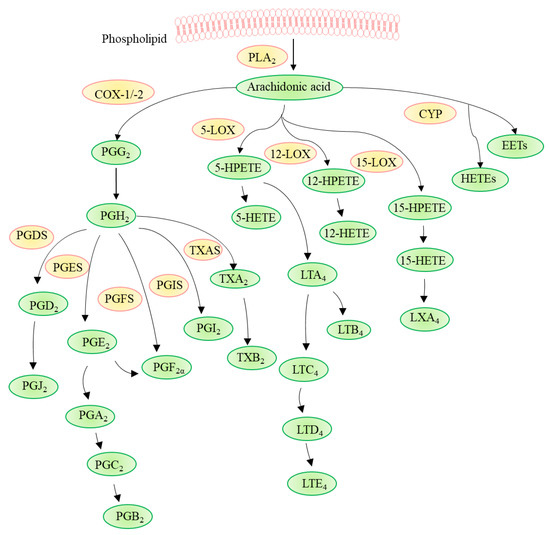
Figure 2.
Arachidonic acid metabolism. Arachidonic acid is released from phospholipid by phospholipase A2 (PLA2) and, in turn, is metabolized through three different pathways involving cyclooxygenase (COX), cytochrome P450 (CYP) enzymes, or lipoxygenase (LOX). COX-1 and COX-2 convert arachidonic acid to prostaglandin (PG)G2 and PGH2, which are further metabolized to various prostaglandins (PGs) such as PGD2, PGE2, PGF2α, prostacyclin (PGI2), and thromboxanes (TX)A2 by corresponding synthases, i.e., PGD2 synthase (PGDS), PGE2 synthase (PGES), PGF2α synthase (PGFS), PGI2 synthase (PGIS), and TXA2 synthase (TXAS). LOXs catalyze the dioxygenation of polyunsaturated fatty acids to their corresponding hydroperoxyeicosatetraenoic acids (HPETEs), which are subsequently converted to hydroxyeicosatetraenoic acids (HETEs), leukotrienes (LTs), and lipoxins (LXs). CYP generates HETEs and epoxyeicosatrienoic acids (EETs).
In the first pathway, COX, also known as prostaglandin G/H synthases (PGHS), which is present in macrophages and ECs, contributes to the production of autoregulatory and homeostatic prostanoids [13]. There are two subtypes of COX: COX-1 exists in most cells and is the primary source of prostanoids with protective functions, while COX-2 is induced by pro-inflammatory factors, growth factors, and hormones to produce prostanoids in pathological conditions such as CVD, cancer, and inflammation [39]. COX-1 and COX-2 convert AA to prostaglandin (PG)G2 and PGH2, which are further metabolized to various PGs (including PGD2, PGE2, and PGF2α), prostacyclin (PGI2), and thromboxane (TX)A2 via their respective synthases [40]. The expressions of various enzymes in different inflammatory cells determine distinct AA metabolism. For example, macrophages convert AA into PGE2 and TXA2 mainly through COX, which is involved in the development of atherosclerosis and thrombosis [41,42]. PGE2 is further hydrolyzed to produce PGA2, PGC2, and PGB2 sequentially, and TXA2 is hydrolyzed to produce TXB2 [43], whereas mast cells produce PGD2, which is hydrolyzed to PGJ2 [44]. PGD2 plays an important protective role in cardiovascular diseases by increasing vascular permeability and blood flow, thereby resisting atherosclerosis and thrombosis [45].
In the second pathway, LOXs, including 5-LOX, 12-LOX, and 15-LOX catalyze the dioxygenation of AA to their corresponding hydroperoxyeicosatetraenoic acids (HPETEs), i.e., 5-HPETE, 12-HPETE, 15-HPETE, which are subsequently converted to hydroxyeicosatetraenoic acids (HETEs), leukotrienes (LTs), and lipoxins (LXs) [46,47]. Notably, the metabolic pathway of LOXs is associated with the progression of CVD, such as atherosclerosis [48]. In addition, 5-LOX can be expressed by different types of white blood cells to insert molecular oxygen at a specific position of AA to form 5-HPETE and LTA4, which are further hydrolyzed to generate LTB4, LTC4, LTD4, and LTE4 [49], and these LTs aggravate the risk of atherosclerosis or myocardial infarction [50]. The 15-LOX pathway has anti-inflammatory and pro-inflammatory effects and is also involved in the process of atherosclerosis [51]. AA generates 15-HPETE under the catalysis of this enzyme, followed by 15-HETE and LXA4 [52,53].
Thirdly, the CYP pathway contributes mainly to the metabolism of lipophilic xenobiotics, including drugs, fatty acids, and fat-soluble vitamins, and its expression is affected by various growth factors and hormones [54,55]. CYP is easily affected by external factors, generating various HETEs and epoxyeicosatrienoic acids (EETs) from AA [56,57]. Among them, 20-HETE and various EETs are related to the regulation of vascular tone and have cardioprotective effects [58]. The AA metabolites obtained through these three pathways are fully involved in the process of CVD, especially atherosclerosis.
AA metabolites bind to different G-protein-coupled receptors (GPCRs), mediating distinct signaling pathways. There are two PGD2 receptors—namely, DP1 and DP2 [59]. PGE2 binds to EP1, EP2, EP3, and EP4 receptors, which mediate diverse functions [60]. Furthermore, there is one receptor each for PGF2α, PGI2, and TXA2 to activate FP, IP, and TP, respectively [61]. Two TP subtypes are available: TPα is present in platelets and smooth muscle cells (SMCs), whereas TPβ is present in ECs and SMCs [62,63]. Notably, cross binding of lipid mediators derived from AA to different receptors results in the versatility of signaling [64], as for example, TP can be activated by PGH2, PGD2, PGE2, PGF2α, and 20-HETE [65,66]. Additionally, LTs act on BLT1 and BLT2, which modulate chemotaxis [67]. Cysteinyl LTs (LTs having the amino acid cysteine in their structure) bind to CysLT1 and CysLT2 receptors, modulating vascular tone. Activation of CysLT2 results in relaxation of pulmonary arteries and increases the expression of inflammatory proteins in ECs [68]. LXs bind to formyl peptide receptor 2 (ALX/FPR2) present in leukocytes for the regulation of inflammatory responses [69].
Apart from the enzymatic actions to generate eicosanoids, AA can undergo oxidative modification to form isoprostanes through a non-enzymatic, free radical-catalyzed mechanism. These isoprostanes can serve as markers of oxidative stress and are linked to CVD, where the 8-iso-PGF2α level shows a positive correlation with the presence and extent of coronary stenosis [70]. Notably, 8-iso-PGF2α produced in a COX-dependent manner is associated with hypoxia-induced hyperreactivity of pulmonary arteries by activating TP receptors [71]. These AA metabolites regulate different signaling pathways by binding different receptors, thereby affecting cardiovascular functions. The upregulation and/or downregulation of the three AA metabolic pathways lead to or protect against CVDs, and such connections are evaluated in the subsequent sections.
4. Contribution of AA Metabolites to the Regulation of Vascular Tone
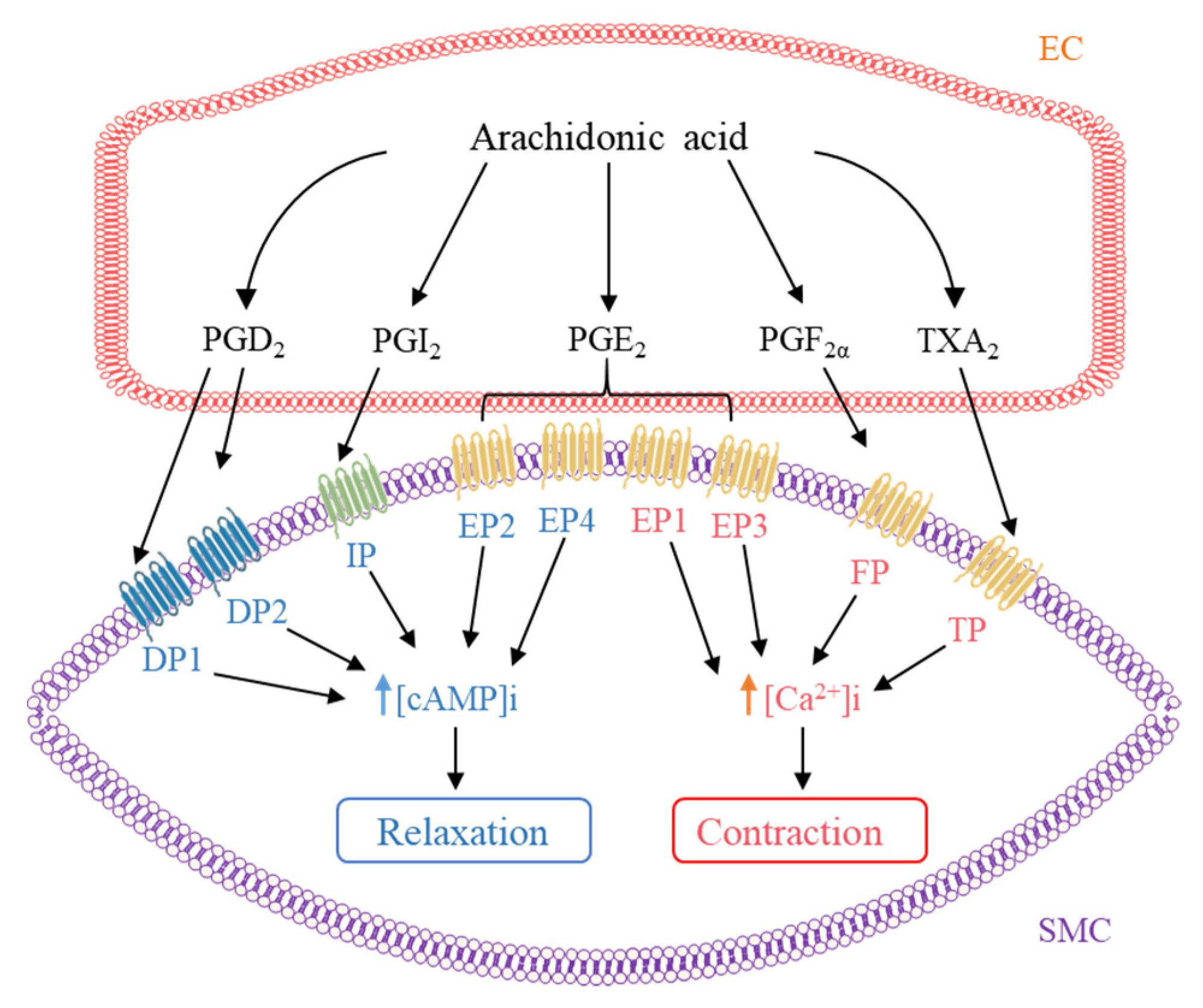
Various AA metabolites such as PGs and TX can act as vasodilators or vasoconstrictors to modulate vascular tone in both physiological and pathophysiological conditions (Figure 3) [72]. The same PG may induce opposite effects depending on the type of receptor it binds to in different tissues.
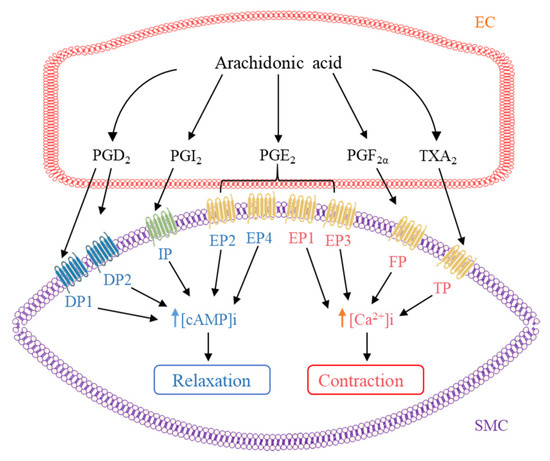
Figure 3.
Regulation of vascular tone by arachidonic acid metabolites. Arachidonic acid metabolites produced in endothelial cell (EC) including prostaglandin (PG)D2, PGE2, PGF2α, prostacyclin (PGI2), and thromboxanes (TX)A2 target to their corresponding receptor in smooth muscle cell (SMC), increasing intracellular cAMP level [cAMP]i to induce relaxation or decreasing intracellular calcium level [Ca2+]i to induce contraction.
PGI2, the principal AA metabolite, is mainly produced by platelets and vascular ECs and affects cardiovascular health, inducing vasodilatation through activation of IP receptors [73]. Activation of muscarinic receptors by agonists such as acetylcholine or bradykinin triggers the production of inositol 1,4,5-triphosphate (IP3) and diacylglycerol (DAG) and thereby increases endothelial intracellular calcium level [Ca2+]i. Elevation of endothelial [Ca2+]i activates PLA2 to release free AA from cell membrane, while DAG is converted to 2-arachidonoylglycerol, which is further metabolized to generate free AA. Free AA is metabolized by COX to PGI2, which exerts vasodilatory responses [74]. In contrast, PGI2 evokes vasoconstriction when acting through TP and EP3 receptors [75]. In mice, inhibition of COX-2-dependent PGI2 biosynthesis results in depression of endothelial nitric oxide synthase (eNOS) and thereby reduces nitric oxide (NO) bioavailability, resulting in high blood pressure and thrombus formation [76]. On the other hand, controversial findings are observed for COX-2 inhibition in humans. Treatment with celecoxib for 1–2 weeks improves endothelial function in hypertensive patients [77], as well as in patients with coronary artery disease [78], while aspirin relieves acute myocardial infarction (AMI) and stroke by inhibiting blood clots [79]; nevertheless, treatment with indomethacin or rofecoxib for 2 weeks failed to improve endothelial function in patients with rheumatoid arthritis [80]. However, other studies show that increased risk of major vascular events is associated with COX-2 inhibitors such as celecoxib and rofecoxib [81,82].
Activation of DP receptors by PGD2 induces endothelium- and NO-dependent relaxations in choroidal vessels and increases blood flow, as well as vascular permeability [83]. Importantly, PGH2, PGD2, PGE2, PGF2α, PGI2, TXA2 analog U46619, and 8-isoprostane all induce endothelium-independent contractions in aortas from hypertensive rats through activation of TP receptors [84].
PGE2 can act as both vasodilator and vasoconstrictor depending on the receptor subtypes activated: stimulation of EP1 increases intracellular calcium concentration; EP2 and EP4 increase cAMP level, whereas EP3 decrease cAMP level [85]. A previous study has shown that PGE2 increases renal vascular tone by stimulating EP1 and EP3, and vice versa, PGE2 decreases it by stimulating EP2 and EP4 [86]. PGE2 has a relaxing effect in some vascular beds such as human middle cerebral arteries [87] and human pulmonary veins [88] through action on EP4 receptors. On the other hand, PGE2 can cause vasoconstriction in some circumstances. PGE2 induces contraction in rat mesenteric arteries [89] and human internal mammary arteries [90] via EP3 receptor, and it triggers contraction through concomitant activation of EP1 and EP3 receptors in porcine cerebral arteries [91]. Moreover, the EP1 receptor is involved in the vasoconstriction induced by angiotensin II (Ang II), endothelin-1, and TXA2 [92].
PGF2α is a potent vasoconstrictor, increasing blood pressure and atherosclerosis through activation of the FP receptor [93]. Furthermore, PGF2α is shown to trigger endothelium-dependent, TP-receptor-mediated contractions in hamster aortae and human renal arteries; in particular, the impact is increased during aging [94].
TXA2 is a potent vasoconstrictor and aggregating factor produced mainly from platelet but also from ECs. The preferential ligand of TP receptors is TXA2; nevertheless, TP receptors can be activated to induce contraction by other PGs, isoprostanes, and HETEs at higher concentrations as aforementioned [95].
As aforementioned, free AA is generated upon activation of agonists, such as acetylcholine, and then forms LOX metabolites, such as 12-HETE and 15-HETE, which function as endothelium-derived relaxing factors (EDRFs) in arteries of rodents, rabbits, pigs, dogs, and humans, contributing to relaxation [96]. In addition, 20-HETE mediates contractile response through activation of Rho-kinase [97] and sensitizes vascular SMCs to constrictors such as Ang II, phenylephrine, and endothelin [98]. By contrast, 20-HETE produced by vascular endothelium induces relaxation in pulmonary arteries through activation of eNOS [99].
Extensive evidence supports that EETs formed from AA by CYP enzymes function as EDRF in vascular beds from different species to relax bovine and human coronary arteries [100,101]. Shear stress also activates cytosolic PLA2 to liberate AA, which is metabolized to EETs through CYP, and EETs activate TRPV4 channels to increase intracellular Ca2+ and subsequently trigger K+ efflux from ECs, leading to vasodilation [102].
5. Preventing and Managing Vascular Complications in Metabolic Disorders
In long-term streptozocin-induced diabetes, reduced vasodilators PGI2 and PGE2 and increased vasoconstrictor TXA2 contribute to endothelial dysfunction in rat aortas and mesenteric arteries [103]. Accelerated atherogenesis caused by diabetes is associated with increased TXA2, and hence, antagonizing the TP receptor by S18886 prevents endothelial dysfunction and atherosclerosis associated with diabetes [104]. Upregulation of COX-2 expression has been linked to impaired cardiovascular function in diabetes and obesity [105]. For instance, palmitate induces endothelial dysfunction through upregulation of COX-2 and the resultant oxidative stress in mouse aortas [106]. Expression of miRNA-200c is found to be elevated in arteries from diabetic mice and patients with diabetes, causing endothelial dysfunction through upregulated COX-2 in ECs and increased generation of PGE2 [107]. Downregulation of COX-2 and TP receptor is attributed to the improved renovascular function in estrogen-deficient rats by long-term calcitriol treatment [108].
Notably, 20-HETE is associated with adipogenesis, increasing adiposity and adipocyte differentiation [109], and is elevated in patients with obesity and CVD [110], whereas 12- and 15-HETEs are associated with microvascular dysfunction during diabetic retinopathy [111]. Levels of 12-HETE, 20-HETE, and LTB are increased and closely related to endothelial progenitor cells dysfunction in diabetic patients with cardiac ischemia [112]. Furthermore, inhibition of 20-HETE generation and decreased inactivation of EETs alleviate cardiac dysfunction following ischemic reperfusion injury in diabetes [113]. EET can prevent diabetic cardiomyopathy by maintaining vascular tension, improving myocardial glucose uptake, and reducing related complications caused by diabetes [114]. These findings imply a close linkage between AA metabolites, particularly COX-2 activity, and vascular complications associated with diabetes and obesity.
6. Regulation of Blood Pressure
PGE2 plays a diverse role in the regulation of blood pressure, determined by the balance between the pressor action of EP1/EP3 receptors and the depressor action of EP2/EP4 receptors. Centrally administered PGE2 elevates blood pressure by modulating renal hemodynamics, renin release, and salt and water transport in the nephron, while systemic administration of PGE2 generates a hypotensive effect by the diuretic and natriuretic roles in kidney and the depressor action of EP receptors [115,116]. Activation of EP1 receptor by PGE2 or the selective agonist increases vascular tone and is responsible for the development of hypertension in diabetic db/db mice [117]. In line with the vasoconstrictive/prohypertensive property of EP1 receptor, EP1 antagonist SC51322 reduces blood pressure in spontaneous hypertensive rats (SHR), whereas genetic disruption of EP1 receptor in mice attenuates AngII-induced hypertension [118]. Both pharmacological inhibition and knockdown of EP3 receptors attenuate pulmonary hypertension [119]. On the other hand, mice lacking EP2 receptors exhibit hypertensive phenotype at baseline and follow a high-salt diet [120]. PGE2 relaxes aortic rings and lowers blood pressure in mice by EP4 receptor-mediated stimulation of eNOS activity [121].
In addition to PGE2, PGI2 also plays a significant role in the regulation of blood pressure. Reduced PGI2 level contributes to vasoconstriction and platelet aggregation in PAH. Inhalation of PGI2 reduces pulmonary artery pressure and pulmonary vascular resistance in patients with residual pulmonary hypertension [122]. Epoprostenol, synthetic PGI2 sodium under the name of Flolan® or in the new formulation of Veletri® was the first available drug for treating PAH [123]. The PGI2 analogs developed afterward include beraprost, iloprost, treprostinil, and selexipag administered by oral, intravenous, subcutaneous, or inhalation route, improving survival in patients with PAH [124].
COX-2-derived PGF2α impairs endothelial function in renovascular hypertension which can be reversed by treatment with celecoxib (COX-2 inhibitor) [125]. Renal arteries from hypertensive rats and humans show higher expressions of COX-2 and bone morphogenic protein 4 (BMP4). Pharmacological inhibition with COX-2 inhibitor or TP receptor antagonist prevents BMP4-induced endothelial dysfunction in hypertension [126]. Antidiabetic drug sitagliptin has been illustrated to restore endothelial function in SHR and Ang-II-induced hypertensive mice through downregulation of COX-2 and upregulation of uncoupling protein 2 expression in arteries [127]. Studies using several animal models show that 20-HETE mediates eNOS uncoupling and reduces NO production, leading to endothelial dysfunction and hypertension [128,129,130]. These AA metabolites have different functions in regulating blood pressure.
7. Antiatherosclerosis Effect
COX-2 inhibitors contribute to atherogenesis owning to favoring the synthesis of TXA2 and PGE2 while reducing PGI2 [131]. Deletion of COX-2 in mice shows accelerated atherogenesis [132]. However, osteocalcin, a skeletal hormone highly expressed in human atherosclerotic lesions, promotes fibroblast transformation through stimulating COX-2 signaling cascade [133]. Ang-II induces COX-2 expression in ECs, which, in turn, increases the generation of proatherosclerotic cytokine monocyte chemoattractant protein-1 [134]. Low-dose aspirin also shows an antithrombotic effect [135]. Inhibition of TXA2 by synthetic compound I4 decreases platelet aggregation [136]. Increasing EETs generation inhibits Ang II-induced inflammation and protects against abdominal aortic aneurysms in mice [137].
Similar to the case of hypertension, PGE2 plays a crucial role in developing atherosclerosis with diverse actions via different types of EP receptors involved in the formation and stabilization of atherosclerotic lesions. EP4 is the most abundant PGE2 receptor expressed in human atherosclerotic lesions, and EP4 overexpression contributes to the deteriorated inflammatory reaction in atherosclerotic plaques [138]. Both genetic and pharmacological inhibitions of EP4 reduce abdominal aortic aneurism formation in mice and humans [139,140]. In contrast to these observations, deficiency of EP4 on bone marrow-derived cells enhances inflammation in atherosclerotic lesions [141] and abdominal aortic aneurism formation [142]. EP2 also implies differential effects in atherosclerosis: its activation promotes the adhesion of monocytes to vascular ECs involved during atherosclerogenesis [143], but genetic disruption of EP2 exacerbates neointimal hyperplasia after arterial injury [144]. Activation of EP3 facilitates atherothrombosis [145], while genetic deletion of EP3 reduces susceptibility to thrombus formation [146] and suppresses neointimal hyperplasia response to injury [147]. Atorvastatin, which suppresses the expression of EP1, EP3, and EP4, effectively protects against thrombotic events [148].
LTB4 and LXA4, produced by the metabolism of LOXs, are associated with the progression of atherosclerotic lesions. The activation of LTB4 via the 5-LOX pathway can increase the recruitment of neutrophils to atherosclerotic plaques destabilization [149]. LTB4 increases vascular permeability by activating the CysLT2 receptor in blood vessels, mediating myocardial ischemia and reperfusion injury, and thus, blocking this receptor can alleviate these damages and prevent atherosclerosis [150]. Blocking the binding of LTB4 with CysLT receptors helps to stabilize plaque and prevents atherosclerotic lesions [151]. Montelukast (CysLT1 receptor antagonist) has been shown to protect heart function and ameliorate atherosclerosis [152]. LXA4 is produced by the activation of 15-LOX and has a positive effect on atherosclerosis, in contrast to the destructive effect of LTs [153]. LXA4 has effective anti-inflammatory and pro-decomposition abilities, protecting against atherosclerosis [154] and achieving the therapeutic effects of drugs such as aspirin and statins. Aspirin can effectively reduce the plasma level of LXA4 in patients with peripheral artery disease and eliminate inflammation [155]. Moreover, lipophilic statins, including simvastatin and atorvastatin, possess strong anti-inflammatory properties, upregulate LXA4 expression in the body, and protect the heart function [156].
8. Modulating Heart Function and Protecting against Myocardial Infarction
The amount of AA in adipose tissue is found to be associated with the risk of myocardial infarction [157]. Deletion of PGE2 synthase-1 accomplished with decreased PGE2 level leads to impaired left ventricular contractile function after myocardial infarction [158]. Previous studies have demonstrated the cardioprotective effect of EP3 activation against ischemia/reperfusion (I/R) injury [159,160]. EP3 is necessary for maintaining the normal growth and development of the heart and knockout of EP3 causes eccentric cardiac hypertrophy and fibrosis [161]. Moreover, EP4 is abundantly expressed in the heart with acute myocardial infarction, and activation of EP4 by PGE2 or pharmacologically protects the heart from I/R injury [162,163]. Both PGD2 [164] and PGI2 [165] exert a protective effect on cardiac I/R injury. Low-dose aspirin reduces the risk of myocardial infarction and ischemic stroke [166]. On the other hand, TXA2 induces cardiac arrhythmias, and such impairment can be blocked by inhibition of the inositol triphosphate pathway [167]. Receiving combination treatment of aspirin plus atorvastatin, patients with AMI show reduced persistent platelet TXA2 production [168].
In addition to PGs, HETEs and EETs affect heart function. Cardioprotective effects of EETs toward acute myocardial I/R injury and cardiac fibrosis have been well reported [169,170,171]. A recent study has shown that AMI patients have a higher baseline level of 20-HETE, which may play a role in the clinical prevention of coronary artery disease [172].
9. Clinical Significance of AA Metabolites
AA metabolites have complex modulatory effects upon normal vascular function [9]; therefore, cardiovascular complications may be resulted due to drug treatment-induced alteration of AA metabolism. Aspirin (non-selective COX inhibitor) and celecoxib (selective COX-2 inhibitor) are common nonsteroidal anti-inflammatory drugs (NSAIDs) for treating pain and inflammation [173,174]. Aspirin has been demonstrated to be an effective preventive therapy among patients at risk of developing or suffering from CVD [175,176]. According to American data, aspirin prevents 28% of the risk of coronary heart diseases and 5% of the risk of heart attacks in patients [177]. Although aspirin is cardioprotective, elevated risk of cardiovascular events including myocardial infarction, stroke, hypertension, and congestive heart failure has been reported after using COX-2 inhibitor; in particular, the more COX-2 selective the drug is, the higher is the risk [178]. Therefore, rofecoxib and valdecoxib were withdrawn from the US market [179,180]. Further development of new COX-2 inhibitors is greatly delayed or halted. Celecoxib is still marketed in the US, but individual cardiovascular risk profiles should be evaluated prior to obtaining a prescription [181]. TP antagonists might offset the cardiovascular toxicity of COX-2 inhibitors by blocking TXA2 signaling. In turn, inhibitors of TXA2 synthase or TP receptors are under development, but no inhibitor has become clinically useful, likely due to the alternative activation of TP by PGH2, PGD2, PGE2, PGF2α, or 20-HETE. Evidence from animal studies supports that TP inhibitor terutroban (S18886) slows down the progression of atherosclerosis [182,183]. Despite having no advantage over aspirin, terutroban has similar cardioprotective effects to ischemic stroke, myocardial infarction, or vascular deaths in patients with cerebral ischemic events [184]. Terutroban treatment in patients with a history of ischemic stroke or transient ischemic attack also has a similar protective effect against the progression of carotid atherosclerosis, as compared with aspirin [185]. A dual TXA2 synthase inhibitor/TP antagonist EV-077 is better than aspirin to inhibit platelet aggregation in type-2 diabetes [186]. Another possible way to impose a cardiovascular risk of COX-2 inhibitors is to combine with NO or hydrogen sulfide (HS) donors for the provision of additional vasodilatory activity [187]. All these lines of evidence indicate the clinical significance of AA metabolites and that a therapeutic approach targeting AA metabolism can ameliorate the risk factors associated with CVD.
10. Potential Health Concerns of Dietary AA
Although our body requires AA, consuming too much of it could be problematic. Israel, one of the countries with the highest level of AA intake, has high prevalence rates of atherosclerosis, diabetes, obesity, and hypertension [188]. This may be, however, confounded by saturated fat and heme iron contained in AA-rich red meat leading to a higher risk of dyslipidemia, thereby an increased risk of CVD [189]. According to a recent survey in Korea, among the highest and lowest consumption of red meat, the risk of dyslipidemia in men increased by 58% and 32%, respectively [190]. A recent Mendelian randomized study has shown that genetically predicted plasma phospholipid AA is positively correlated with atherosclerosis [15]. Moderate consumption of red meat will not increase the risk of CVD, and the nutrients from red meat including AA possess a positive impact on cardiovascular health [191]. Studies have shown that excessive intake of linoleic acid can increase susceptibility to lipid oxidation due to increased plasma low-density lipoprotein (LDL) and diminished high-density lipoprotein (HDL), which may be a major cause of the increased risk of CVD [192]. Moreover, lipid peroxidation alters platelet function and increases the risk of atherosclerosis [193,194]. In fact, replacing saturated fat with omega-6 PUFA has been a cornerstone of dietary recommendations aimed at lowering CVD risk [195]. No upper limit is set for dietary linoleic acid or AA because omega-6 and omega-3 fatty acids counteract the effect of each other and there is a lack of a defined intake found to cause adverse effects [196]. The experimental studies are difficult to translate into clinical research, which involves long-term follow-up investigation of the diet of the individuals and complicated criteria for evaluating dietary intake and timing. In general, AA is beneficial to human health, but excessive intake may cause side effects. Consuming a balanced diet, rather than considering only a single nutrient, is the best choice for human health.
11. Conclusions
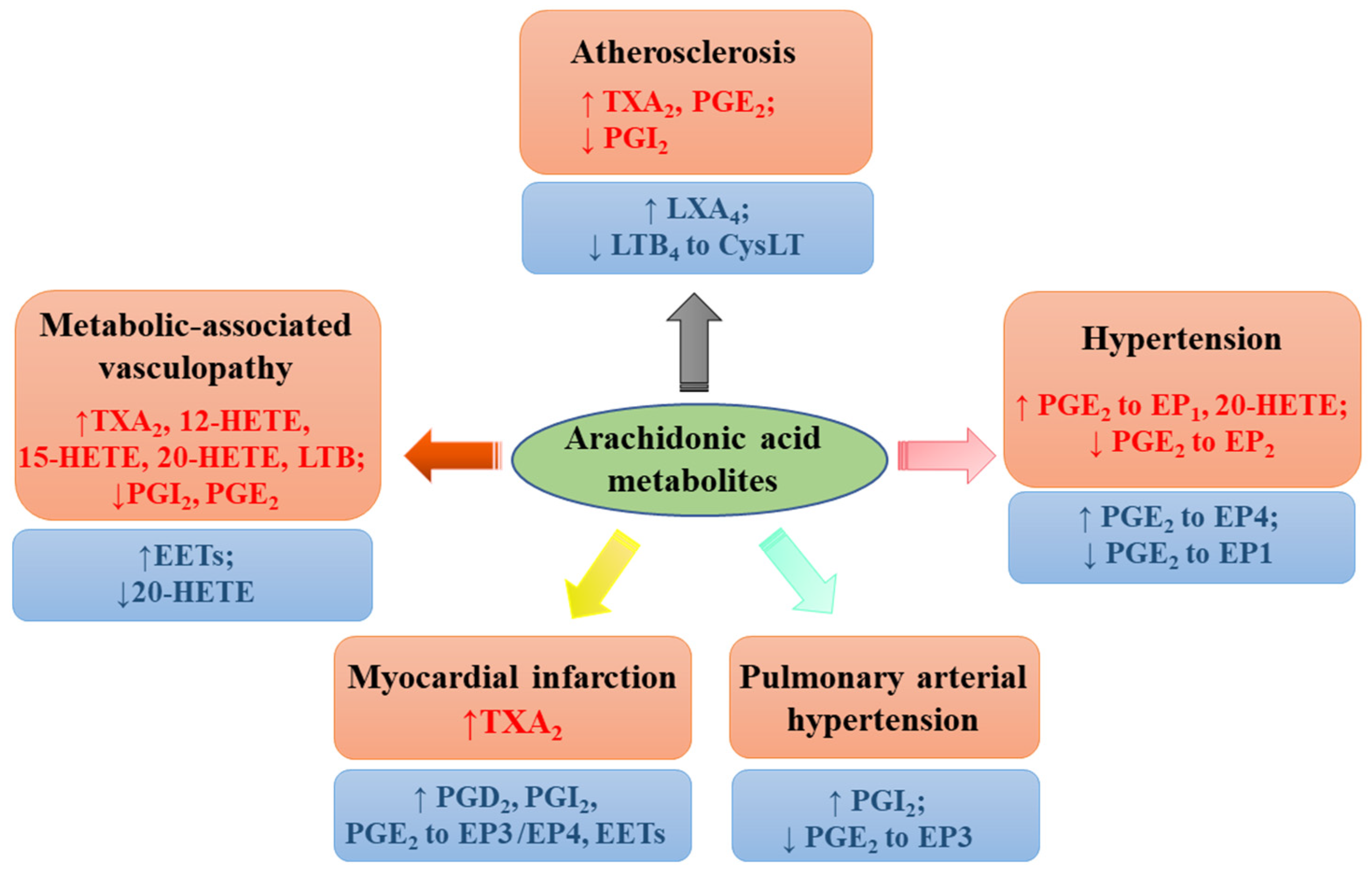
Taken together, extensive lines of evidence imply a diverse and disease-specific contribution of individual AA metabolites to cardiovascular health and complications (Figure 4). More concerted research efforts, especially clinical studies, are required to clarify the controversies and to gain insight into the precise contribution of each AA metabolite targeting specific receptor, aiming at increasing the cardiovascular efficacy of currently available drugs or developing a new class of drugs to overcome CVD.
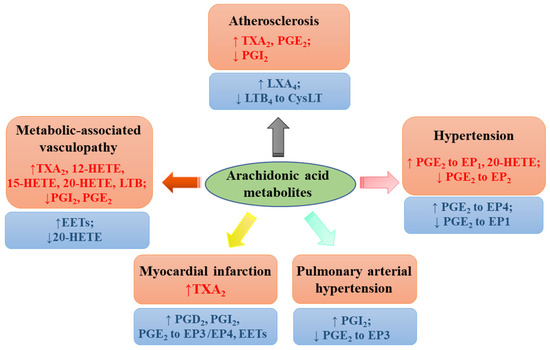
Figure 4.
Effects of arachidonic acid metabolites on cardiovascular diseases. Various metabolites including prostaglandin (PG)D2 and PGE2 (to EP1, EP2, EP3 or EP4 receptor), prostacyclin (PGI2), thromboxane (TX)A2, leukotrienes B4 (LTB4) (to CysLT receptors), lipoxin A4 (LXA4), hydroxyeicosatetraenoic acids (HETEs), and epoxyeicosatrienoic acids (EETs) exert vasoprotective (labeled with blue color) and deteriorative effects (labeled with red color).
Author Contributions
Writing—original draft preparation, Y.Z. and W.S.C.; writing—review and editing, H.K. and J.X.; supervision, W.S.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Research Committee of the University of Macau (SRG2019-00154-ICMS and MYRG2019-00157-ICMS) and the Operation Fund of State Key Laboratory of Quality Research in Chinese Medicine of University of Macau (SKL-QRCM(UM)-2020-2022). The APC was funded by MYRG2019-00157-ICMS.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Acknowledgments
The authors thank the technical team of the Institute of Chinese Medical Sciences at the University of Macau for their valuable assistance.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Picard, F.; Steg, P.G. Cardiovascular Disease Risk Reduction in Mild-Moderate Hypertriglyceridemia: Integrating Prescription of Omega-3 with Standard Treatment. Curr. Atheroscler. Rep. 2021, 23, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Abdelhamid, A.S.; Martin, N.; Bridges, C.; Brainard, J.S.; Wang, X.; Brown, T.J.; Hanson, S.; Jimoh, O.F.; Ajabnoor, S.M.; Deane, K.H.O.; et al. Polyunsaturated fatty acids for the primary and secondary prevention of cardiovascular disease. Cochrane Database Syst. Rev. 2018, 11, CD012345. [Google Scholar] [CrossRef]
- Yuan, S.; Back, M.; Bruzelius, M.; Mason, A.M.; Burgess, S.; Larsson, S. Plasma Phospholipid Fatty Acids, FADS1 and Risk of 15 Cardiovascular Diseases: A Mendelian Randomisation Study. Nutrients 2019, 11, 3001. [Google Scholar] [CrossRef] [PubMed]
- Yuan, T.H.; Si, S.C.; Li, Y.X.; Li, W.C.; Chen, X.L.; Liu, C.C.; Li, J.Q.; Wang, B.J.; Hou, L.; Liu, Y.X.; et al. Roles for circulating polyunsaturated fatty acids in ischemic stroke and modifiable factors: A Mendelian randomization study. Nutr. J. 2020, 19, 1–11. [Google Scholar] [CrossRef]
- Hikita, H.; Shigeta, T.; Kimura, S.; Takahashi, A.; Isobe, M. Coronary Artery Disease Severity and Cardiovascular Biomarkers in Patients with Peripheral Artery Disease. Int. J. Angiol. 2015, 24, 278–282. [Google Scholar] [CrossRef]
- Narverud, I.; Bogsrud, M.P.; Ril, L.; Ulven, S.M.; Retterstøl, K.; Ueland, T.; Mulder, M.; van Lennep, J.R.; Halvorsen, B.; Aukrust, P.; et al. Lipoprotein (a) concentration is associated with plasma arachidonic acid in subjects with familial hypercholesterolemia. Br. J. Nutr. 2019, 122, 1–24. [Google Scholar] [CrossRef] [PubMed]
- Badimon, L.; Vilahur, G.; Rocca, B.; Patrono, C. The Key Contribution Of Platelet And Vascular Arachidonic Acid Metabolism To The Pathophysiology Of Atherothrombosis. Cardiovasc. Res. 2021, 117, 2001–2015. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.H.; Hsiao, G.; Al-Shabrawey, M. Eicosanoids and Oxidative Stress in Diabetic Retinopathy. Antioxidants 2020, 9, 520. [Google Scholar] [CrossRef]
- Imig, J.D. Eicosanoid blood vessel regulation in physiological and pathological states. Clin. Sci. 2020, 134, 2707–2727. [Google Scholar] [CrossRef] [PubMed]
- Hayashi, S.; Satoh, Y.; Ogasawara, Y.; Maruyama, C.; Hamano, Y.; Ujihara, T.; Dairi, T. Control Mechanism for cis Double-Bond Formation by Polyunsaturated Fatty-Acid Synthases. Angew. Chem. Int. Ed. 2019, 58, 2326–2330. [Google Scholar] [CrossRef]
- Kratzsch, S.; Drossler, K.; Sprinz, H.; Brede, O. Thiyl radicals in biosystems: Inhibition of the prostaglandin metabolism by the cis-trans-isomerization of arachidonic acid double bonds. Arch. Biochem. Biophys. 2003, 416, 238–248. [Google Scholar] [CrossRef]
- Wang, T.Q.; Fu, X.J.; Chen, Q.F.; Patra, J.K.; Wang, D.D.; Wang, Z.G.; Gai, Z.B. Arachidonic Acid Metabolism and Kidney Inflammation. Int. J. Mol. Sci. 2019, 20, 3683. [Google Scholar] [CrossRef]
- Wang, B.; Wu, L.J.; Chen, J.; Dong, L.L.; Chen, C.; Wen, Z.; Hu, J.; Fleming, I.; Wang, D.W. Metabolism pathways of arachidonic acids: Mechanisms and potential therapeutic targets. Signal Transduct. Tar. 2021, 6, 94. [Google Scholar] [CrossRef]
- Zhang, T.; Yeung, S.L.A.; Schooling, C.M. Associations of Arachidonic Acid Synthesis with Cardiovascular Risk Factors and Relation to Ischemic Heart Disease and Stroke: A Univariable and Multivariable Mendelian Randomization Study. Nutrients 2021, 13, 1489. [Google Scholar] [CrossRef] [PubMed]
- Zhang, T.; Zhao, J.V.; Schooling, C.M. The associations of plasma phospholipid arachidonic acid with cardiovascular diseases: A Mendelian randomization study. EBioMedicine 2021, 63, 103189. [Google Scholar] [CrossRef]
- Wang, W.; Liu, Y.; Liu, J.; Yin, P.; Wang, L.; Qi, J.; You, J.; Lin, L.; Meng, S.; Wang, F.; et al. Mortality and years of life lost of cardiovascular diseases in China, 2005–2020: Empirical evidence from national mortality surveillance system. Int. J. Cardiol. 2021, 340, 105–112. [Google Scholar] [CrossRef] [PubMed]
- Afzal, M. Recent updates on novel therapeutic targets of cardiovascular diseases. Mol. Cell. Biochem. 2021, 476, 145–155. [Google Scholar] [CrossRef] [PubMed]
- Itoh, H.; Kaneko, H.; Kiriyama, H.; Kamon, T.; Fujiu, K.; Morita, K.; Michihata, N.; Jo, T.; Takeda, N.; Morita, H.; et al. Metabolically Healthy Obesity and the Risk of Cardiovascular Disease in the General Population-Analysis of a Nationwide Epidemiological Database. Circ. J. 2021, 85, 914–920. [Google Scholar] [CrossRef]
- Groenland, E.H.; Bots, M.L.; Asselbergs, F.W.; de Borst, G.J.; Kappelle, L.J.; Visseren, F.L.J.; Spiering, W.; Grp, U.-S.S. Apparent treatment resistant hypertension and the risk of recurrent cardiovascular events and mortality in patients with established vascular disease. Int. J. Cardiol. 2021, 334, 135–141. [Google Scholar] [CrossRef]
- Taber, L.; Chiu, C.H.; Whelan, J. Assessment of the arachidonic acid content in foods commonly consumed in the American diet. Lipids 1998, 33, 1151–1157. [Google Scholar] [CrossRef]
- Ha, A.W.; Kim, W.K. Intake ratio and major food sources of n-3 and n-6 fatty acids in Korea: A study based on the sixth Korea national health and nutrition examination survey (2013–2014). Asia Pac. J. Clin. Nutr. 2018, 27, 433–440. [Google Scholar] [CrossRef]
- Tani, S.; Matsuo, R.; Matsumoto, N. A longitudinal study of the association of the eicosapentaenoic acid/arachidonic acid ratio derived from fish consumption with the serum lipid levels: A pilot study. Heart Vessel. 2019, 34, 189–196. [Google Scholar] [CrossRef]
- Asil, S.M.; Kenari, A.A.; Mianji, G.R.; Van der Kraak, G. Estimation of Arachidonic Acid Requirement for Improvement of Pre-maturation Growth and Egg and Larval Quality in the Female Blue Gourami (Trichopodus trichopterus; Pallas, 1770): A Model for the Anabantidae Family. J. World Aquacult Soc. 2019, 50, 359–373. [Google Scholar] [CrossRef]
- Arts, M.T.; Ackman, R.G.; Holub, B.J. “Essential fatty acids” in aquatic ecosystems: A crucial link between diet and human health and evolution. Can. J. Fish Aquat. Sci. 2001, 58, 122–137. [Google Scholar] [CrossRef]
- Seah, J.Y.; Gay, G.M.; Su, J.; Tai, E.S.; Yuan, J.M.; Koh, W.P.; Ong, C.N.; van Dam, R.M. Consumption of Red Meat, but Not Cooking Oils High in Polyunsaturated Fat, Is Associated with Higher Arachidonic Acid Status in Singapore Chinese Adults. Nutrients 2017, 9, 101. [Google Scholar] [CrossRef] [PubMed]
- Rett, B.S.; Whelan, J. Increasing dietary linoleic acid does not increase tissue arachidonic acid content in adults consuming Western-type diets: A systematic review. Nutr. Metab. 2011, 8, 36. [Google Scholar] [CrossRef]
- Markworth, J.F.; Mitchell, C.J.; D’Souza, R.F.; Aasen, K.M.M.; Durainayagam, B.R.; Mitchell, S.M.; Chan, A.H.C.; Sinclair, A.J.; Garg, M.; Cameron-Smith, D. Arachidonic acid supplementation modulates blood and skeletal muscle lipid profile with no effect on basal inflammation in resistance exercise trained men. Prostaglandins Leukot. Essent. Fat. Acids 2018, 128, 74–86. [Google Scholar] [CrossRef]
- Bermudez Menendez de la Granda, M.; Sinclair, A.J. Fatty acids and obesity. Curr. Pharm. Des. 2009, 15, 4117–4125. [Google Scholar] [CrossRef] [PubMed]
- Burns, J.L.; Nakamura, M.T.; Ma, D.W.L. Differentiating the biological effects of linoleic acid from arachidonic acid in health and disease. Prostaglandins Leukot. Essent. Fat. Acids 2018, 135, 1–4. [Google Scholar] [CrossRef]
- Das, U.N. Arachidonic acid in health and disease with focus on hypertension and diabetes mellitus: A review. J. Adv. Res. 2018, 11, 43–55. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, A.T.; Anthony, J.C.; Diersen-Schade, D.A.; Rumsey, S.C.; Lawrence, P.; Li, C.; Nathanielsz, P.W.; Brenna, J.T. The influence of moderate and high dietary long chain polyunsaturated fatty acids (LCPUFA) on baboon neonate tissue fatty acids. Pediatr. Res. 2007, 61, 537–545. [Google Scholar] [CrossRef]
- Tyburczy, C.; Brenna, M.E.; DeMari, J.A.; Kothapalli, K.S.D.; Blank, B.S.; Valentine, H.; McDonough, S.P.; Banavara, D.; Diersen-Schade, D.A.; Brenna, J.T. Evaluation of bioequivalency and toxicological effects of three sources of arachidonic acid (ARA) in domestic piglets. Food Chem. Toxicol. 2011, 49, 2320–2327. [Google Scholar] [CrossRef]
- Steinberg, D.; Parthasarathy, S.; Ca Rew, T.E.; Khoo, J.C.; Witztum, J.L. Beyond cholesterol. Modifications of low-density lipoprotein that increase its atherogenicity. N. Engl. J. Med. 1989, 320, 915–924. [Google Scholar] [CrossRef]
- FAO/WHO. Fats and oils in human nutrition. Report of a joint expert consultation. FAO Food Nutr. Pap. 1994, i–xix, 1–147. [Google Scholar]
- Huang, M.C.; Brenna, J.T.; Chao, A.C.; Tschanz, C.; Diersen-Schade, D.A.; Hung, H.C. Differential tissue dose responses of (n-3) and (n-6) PUFA in neonatal piglets fed docosahexaenoate and arachidonoate. J. Nutr. 2007, 137, 2049–2055. [Google Scholar] [CrossRef] [PubMed]
- AFSSA. Opinion of the French Food Safety Agency on the Update of French Population Reference Intakes (ANCs) for Fatty Acids; AFSSA: Maisons-Alfort, France, 2010; Available online: http://www.anses.fr/en/content/opinion-french-food-safety-agency-update-french-population-reference-intakes-ancs-fatty (accessed on 8 October 2021).
- Tunctan, B.; Senol, S.P.; Temiz-Resitoglu, M.; Guden, D.S.; Sahan-Firat, S.; Falck, J.R.; Malik, K.U. Eicosanoids derived from cytochrome P450 pathway of arachidonic acid and inflammatory shock. Prostaglandins Other Lipid Mediat. 2019, 145, 106377. [Google Scholar] [CrossRef] [PubMed]
- Trostchansky, A.; Moore-Carrasco, R.; Fuentes, E. Oxidative pathways of arachidonic acid as targets for regulation of platelet activation. Prostaglandins Other Lipid Mediat. 2019, 145, 106382. [Google Scholar] [CrossRef]
- Marnett, L.J.; Rowlinson, S.W.; Goodwin, D.C.; Kalgutkar, A.S.; Lanzo, C.A. Arachidonic acid oxygenation by COX-1 and COX-2-Mechanisms of catalysis and inhibition. J. Biol. Chem. 1999, 274, 22903–22906. [Google Scholar] [CrossRef]
- Simmons, D.L.; Botting, R.M.; Hla, T. Cyclooxygenase isozymes: The biology of prostaglandin synthesis and inhibition. Pharmacol. Rev. 2004, 56, 387–437. [Google Scholar] [CrossRef] [PubMed]
- Wu, D.Y.; Hayek, M.G.; Meydani, S.N. Vitamin E and macrophage cyclooxygenase regulation in the aged. J. Nutr. 2001, 131, 382S–388S. [Google Scholar] [CrossRef]
- Tirsan, T. Analysis of prostaglandins induced by spontaneous platelet aggregation in patients with primary thrombocythemia. Jpn. J. Thromb. Hemost. 2010, 16, 169–171. [Google Scholar] [CrossRef]
- Moreira, V.; Gutierrez, J.M.; Lomonte, B.; Vinolo, M.A.R.; Curi, R.; Lambeau, G.; Teixeira, C. 12-HETE is a regulator of PGE(2) production via COX-2 expression induced by a snake venom group IIA phospholipase A(2) in isolated peritoneal macrophages. Chem.-Biol. Interact. 2020, 317, 108903. [Google Scholar] [CrossRef]
- Dichlberger, A.; Schlager, S.; Kovanen, P.T.; Schneider, W.J. Lipid droplets in activated mast cells-a significant source of triglyceride-derived arachidonic acid for eicosanoid production. Eur. J. Pharmacol. 2016, 785, 59–69. [Google Scholar] [CrossRef] [PubMed]
- Miwa, Y.; Oda, H.; Shiina, Y.; Shikata, K.; Tsushima, M.; Nakano, S.; Maruyama, T.; Kyotani, S.; Eguchi, N.; Urade, Y.; et al. Association of serum lipocalin-type prostaglandin D synthase levels with subclinical atherosclerosis in untreated asymptomatic subjects. Hypertens Res. 2008, 31, 1931–1939. [Google Scholar] [CrossRef][Green Version]
- Jansen, C.; Hofheinz, K.; Vogel, R.; Roffeis, J.; Anton, M.; Reddanna, P.; Kuhn, H.; Walther, M. Stereocontrol of arachidonic acid oxygenation by vertebrate lipoxygenases: Newly cloned zebrafish lipoxygenase 1 does not follow the Ala-versus-Gly concept. J. Biol. Chem. 2011, 286, 37804–37812. [Google Scholar] [CrossRef]
- Reddy, K.K.; Vidya Rajan, V.K.; Gupta, A.; Aparoy, P.; Reddanna, P. Exploration of binding site pattern in arachidonic acid metabolizing enzymes, Cyclooxygenases and Lipoxygenases. BMC Res. Notes 2015, 8, 152. [Google Scholar] [CrossRef] [PubMed]
- Wittwer, J.; Hersberger, M. The two faces of the 15-lipoxygenase in atherosclerosis. Prostaglandins Leukot. Essent. Fat. Acids 2007, 77, 67–77. [Google Scholar] [CrossRef]
- Mittal, M.; Kumar, R.B.; Balagunaseelan, N.; Hamberg, M.; Jegerschold, C.; Radmark, O.; Haeggstrom, J.Z.; Rinaldo-Matthis, A. Kinetic investigation of human 5-lipoxygenase with arachidonic acid. Bioorg Med. Chem. Lett. 2016, 26, 3547–3551. [Google Scholar] [CrossRef]
- Lotzer, K.; Funk, C.D.; Habenicht, A.J.R. The 5-lipoxygenase pathway in arterial wall biology and atherosclerosis. BBA-Mol. Cell Biol. Lipids 2005, 1736, 30–37. [Google Scholar] [CrossRef] [PubMed]
- Bender, G.; Schexnaydre, E.E.; Murphy, R.C.; Uhlson, C.; Newcomer, M.E. Membrane-dependent Activities of Human 15-LOX-2 and Its Murine Counterpart Implications for Murine Models of Atherosclerosis. J. Biol. Chem. 2016, 291, 19413–19424. [Google Scholar] [CrossRef]
- Suardiaz, R.; Jambrina, P.G.; Masgrau, L.; Gonzalez-Lafont, A.; Rosta, E.; Lluch, J.M. Understanding the Mechanism of the Hydrogen Abstraction from Arachidonic Acid Catalyzed by the Human Enzyme 15-Lipoxygenase-2. A Quantum Mechanics/Molecular Mechanics Free Energy Simulation. J. Chem. Theory Comput. 2016, 12, 2079–2090. [Google Scholar] [CrossRef] [PubMed]
- Jiang, W.G.; Watkins, G.; Douglas-Jones, A.; Mansel, R.E. Reduction of isoforms of 15-lipoxygenase (15-LOX)-1 and 15-LOX-2 in human breast cancer. Prostaglandins Leukot. Essent. Fat. Acids 2006, 74, 235–245. [Google Scholar] [CrossRef]
- Gervasini, G.; Garcia-Cerrada, M.; Vergara, E.; Garcia-Pino, G.; Alvarado, R.; Fernandez-Cavada, M.J.; Barroso, S.; Doblare, E.; Cubero, J.J. Polymorphisms in CYP-mediated arachidonic acid routes affect the outcome of renal transplantation. Eur. J. Clin. Investig. 2015, 45, 1060–1068. [Google Scholar] [CrossRef]
- Capdevila, J.H.; Falck, J.R. The CYP P450 arachidonic acid monooxygenases: From cell signaling to blood pressure regulation. Biochem. Biophys. Res. Commun. 2001, 285, 571–576. [Google Scholar] [CrossRef]
- Gu, R.M.; Yang, L.; Zhang, Y.; Wang, L.; Kong, S.; Zhang, C.; Zhai, Y.; Wang, M.; Wu, P.; Liu, L.; et al. CYP-omega-hydroxylation-dependent metabolites of arachidonic acid inhibit the basolateral 10 pS chloride channel in the rat thick ascending limb. Kidney Int. 2009, 76, 849–856. [Google Scholar] [CrossRef] [PubMed]
- Colombero, C.; Cardenas, S.; Venara, M.; Martin, A.; Pennisi, P.; Barontini, M.; Nowicki, S. Cytochrome 450 metabolites of arachidonic acid (20-HETE, 11,12-EET and 14,15-EET) promote pheochromocytoma cell growth and tumor associated angiogenesis. Biochimie 2020, 171–172, 147–157. [Google Scholar] [CrossRef]
- Al-Lawati, H.; Vakili, M.R.; Lavasanifar, A.; Ahmed, S.; Jamali, F. Reduced Heart Exposure of Diclofenac by Its Polymeric Micellar Formulation Normalizes CYP-Mediated Metabolism of Arachidonic Acid Imbalance in An Adjuvant Arthritis Rat Model: Implications in Reduced Cardiovascular Side Effects of Diclofenac by Nanodrug Delivery. Mol. Pharm. 2020, 17, 1377–1386. [Google Scholar] [CrossRef] [PubMed]
- Ulven, T.; Kostenis, E. Targeting the Prostaglandin D-2 Receptors DP1 and CRTH2 for Treatment of Inflammation. Front. Med. Chem. 2010, 5, 350–380. [Google Scholar] [CrossRef]
- Mawhin, M.A.; Tilly, P.; Fabre, J.E. The receptor EP3 to PGE2: A rational target to prevent atherothrombosis without inducing bleeding. Prostaglandins Other Lipid Mediat. 2015, 121, 4–16. [Google Scholar] [CrossRef]
- Leng, X.; Jiang, H. Effects of arachidonic acid and its major prostaglandin derivatives on bovine myoblast proliferation, differentiation, and fusion. Domest. Anim. Endocrin. 2019, 67, 28–36. [Google Scholar] [CrossRef]
- Siangjong, L.; Goldman, D.H.; Kriska, T.; Gauthier, K.M.; Smyth, E.M.; Puli, N.; Kumar, G.; Falck, J.R.; Campbell, W.B. Vascular hepoxilin and trioxilins mediate vasorelaxation through TP receptor inhibition in mouse arteries. Acta Physiol. 2017, 219, 188–201. [Google Scholar] [CrossRef] [PubMed]
- Kurahashi, K.; Nishihashi, T.; Trandafir, C.C.; Wang, A.M.; Murakami, S.; Ji, X. Diversity of endothelium-derived vasocontracting factors-arachidonic acid metabolites. Acta Pharmacol. Sin. 2003, 24, 1065–1069. [Google Scholar] [CrossRef]
- Trostchansky, A.; Wood, I.; Rubbo, H. Regulation of arachidonic acid oxidation and metabolism by lipid electrophiles. Prostaglandins Other Lipid Mediat. 2021, 152, 106482. [Google Scholar] [CrossRef]
- Bauer, J.; Ripperger, A.; Frantz, S.; Ergun, S.; Schwedhelm, E.; Benndorf, R.A. Pathophysiology of isoprostanes in the cardiovascular system: Implications of isoprostane-mediated thromboxane A2 receptor activation. Br. J. Pharmacol. 2014, 171, 3115–3131. [Google Scholar] [CrossRef] [PubMed]
- Trostchansky, A.; Rubbo, H. Anti-inflammatory signaling actions of electrophilic nitro-arachidonic acid in vascular cells and astrocytes. Arch. Biochem. Biophys. 2017, 617, 155–161. [Google Scholar] [CrossRef]
- Yokomizo, T. Two distinct leukotriene B4 receptors, BLT1 and BLT2. J. Biochem. 2015, 157, 65–71. [Google Scholar] [CrossRef]
- Duah, E.; Adapala, R.K.; Al-Azzam, N.; Kondeti, V.; Gombedza, F.; Thodeti, C.K.; Paruchuri, S. Cysteinyl leukotrienes regulate endothelial cell inflammatory and proliferative signals through CysLT(2) and CysLT(1) receptors. Sci. Rep.-UK 2013, 3, 3274. [Google Scholar] [CrossRef]
- Nunes, V.S.; Rogerio, A.P.; Abrahao, O. Insights into the Activation Mechanism of the ALX/FPR2 Receptor. J. Phys. Chem. Lett. 2020, 11, 8952–8957. [Google Scholar] [CrossRef] [PubMed]
- Wang, B.; Pan, J.; Wang, L.; Zhu, H.; Yu, R.; Zou, Y. Associations of plasma 8-isoprostane levels with the presence and extent of coronary stenosis in patients with coronary artery disease. Atherosclerosis 2006, 184, 425–430. [Google Scholar] [CrossRef]
- Delannoy, E.; Courtois, A.; Freund-Michel, V.; Leblais, V.; Marthan, R.; Muller, B. Hypoxia-induced hyperreactivity of pulmonary arteries: Role of cyclooxygenase-2, isoprostanes, and thromboxane receptors. Cardiovasc. Res. 2010, 85, 582–592. [Google Scholar] [CrossRef]
- Feletou, M.; Huang, Y.; Vanhoutte, P.M. Endothelium-mediated control of vascular tone: COX-1 and COX-2 products. Br. J. Pharmacol. 2011, 164, 894–912. [Google Scholar] [CrossRef] [PubMed]
- Ozen, G.; Gomez, I.; Daci, A.; Deschildre, C.; Boubaya, L.; Teskin, O.; Uydes-Dogan, B.S.; Jakobsson, P.J.; Longrois, D.; Topal, G.; et al. Inhibition of microsomal PGE synthase-1 reduces human vascular tone by increasing PGI2: A safer alternative to COX-2 inhibition. Br. J. Pharmacol. 2017, 174, 4087–4098. [Google Scholar] [CrossRef]
- Tang, X.; Edwards, E.M.; Holmes, B.B.; Falck, J.R.; Campbell, W.B. Role of phospholipase C and diacylglyceride lipase pathway in arachidonic acid release and acetylcholine-induced vascular relaxation in rabbit aorta. Am. J. Physiol. Heart Circ. Physiol. 2006, 290, H37–H45. [Google Scholar] [CrossRef]
- Li, Z.; Zhang, Y.; Liu, B.; Luo, W.; Li, H.; Zhou, Y. Role of E-type prostaglandin receptor EP3 in the vasoconstrictor activity evoked by prostacyclin in thromboxane-prostanoid receptor deficient mice. Sci. Rep. 2017, 7, 42167. [Google Scholar] [CrossRef]
- Yu, Y.; Ricciotti, E.; Scalia, R.; Tang, S.Y.; Grant, G.; Yu, Z.; Landesberg, G.; Crichton, I.; Wu, W.; Pure, E.; et al. Vascular COX-2 modulates blood pressure and thrombosis in mice. Sci. Transl. Med. 2012, 4, 132ra154. [Google Scholar] [CrossRef]
- Widlansky, M.E.; Price, D.T.; Gokce, N.; Eberhardt, R.T.; Duffy, S.J.; Holbrook, M.; Maxwell, C.; Palmisano, J.; Keaney, J.F., Jr.; Morrow, J.D.; et al. Short- and long-term COX-2 inhibition reverses endothelial dysfunction in patients with hypertension. Hypertension 2003, 42, 310–315. [Google Scholar] [CrossRef] [PubMed]
- Chenevard, R.; Hurlimann, D.; Bechir, M.; Enseleit, F.; Spieker, L.; Hermann, M.; Riesen, W.; Gay, S.; Gay, R.E.; Neidhart, M.; et al. Selective COX-2 inhibition improves endothelial function in coronary artery disease. Circulation 2003, 107, 405–409. [Google Scholar] [CrossRef]
- Howes, L.G.; Krum, H. Selective cyclo-oxygenase-2 inhibitors and myocardial infarction-How strong is the link? Drug Safety 2002, 25, 829–835. [Google Scholar] [CrossRef] [PubMed]
- Wong, M.; Jiang, B.Y.; McNeill, K.; Farish, S.; Kirkham, B.; Chowienczyk, P. Effects of selective and non-selective cyclo-oxygenase inhibition on endothelial function in patients with rheumatoid arthritis. Scand. J. Rheumatol. 2007, 36, 265–269. [Google Scholar] [CrossRef]
- Coxib and Traditional NSAID Trialists’ (CNT) Collaboration; Bhala, N.; Emberson, J.; Merhi, A.; Abramson, S.; Arber, N.; Baron, J.A.; Bombardier, C.; Cannon, C.; Farkouh, M.E.; et al. Vascular and upper gastrointestinal effects of non-steroidal anti-inflammatory drugs: Meta-analyses of individual participant data from randomised trials. Lancet 2013, 382, 769–779. [Google Scholar] [CrossRef]
- Ross, S.J.; Elgendy, I.Y.; Bavry, A.A. Cardiovascular Safety and Bleeding Risk Associated with Nonsteroidal Anti-Inflammatory Medications in Patients with Cardiovascular Disease. Curr. Cardiol. Rep. 2017, 19, 8. [Google Scholar] [CrossRef] [PubMed]
- Smyth, E.M.; Grosser, T.; Wang, M.; Yu, Y.; FitzGerald, G.A. Prostanoids in health and disease. J. Lipid Res. 2009, 50, S423–S428. [Google Scholar] [CrossRef] [PubMed]
- Gluais, P.; Lonchampt, M.; Morrow, J.D.; Vanhoutte, P.M.; Feletou, M. Acetylcholine-induced endothelium-dependent contractions in the SHR aorta: The Janus face of prostacyclin. Br. J. Pharmacol. 2005, 146, 834–845. [Google Scholar] [CrossRef]
- Legler, D.F.; Bruckner, M.; Uetz-von Allmen, E.; Krause, P. Prostaglandin E-2 at new glance: Novel insights in functional diversity offer therapeutic chances. Int. J. Biochem. Cell B 2010, 42, 198–201. [Google Scholar] [CrossRef] [PubMed]
- Schweda, F.; Klar, J.; Narumiya, S.; Nusing, R.M.; Kurtz, A. Stimulation of renin release by prostaglandin E2 is mediated by EP2 and EP4 receptors in mouse kidneys. Am. J. Physiol. Renal. Physiol. 2004, 287, F427–F433. [Google Scholar] [CrossRef]
- Davis, R.J.; Murdoch, C.E.; Ali, M.; Purbrick, S.; Ravid, R.; Baxter, G.S.; Tilford, N.; Sheldrick, R.L.; Clark, K.L.; Coleman, R.A. EP4 prostanoid receptor-mediated vasodilatation of human middle cerebral arteries. Br. J. Pharmacol. 2004, 141, 580–585. [Google Scholar] [CrossRef]
- Foudi, N.; Kotelevets, L.; Louedec, L.; Leseche, G.; Henin, D.; Chastre, E.; Norel, X. Vasorelaxation induced by prostaglandin E2 in human pulmonary vein: Role of the EP4 receptor subtype. Br. J. Pharmacol. 2008, 154, 1631–1639. [Google Scholar] [CrossRef]
- Kobayashi, K.; Murata, T.; Hori, M.; Ozaki, H. Prostaglandin E2-prostanoid EP3 signal induces vascular contraction via nPKC and ROCK activation in rat mesenteric artery. Eur. J. Pharmacol. 2011, 660, 375–380. [Google Scholar] [CrossRef]
- Foudi, N.; Kotelevets, L.; Gomez, I.; Louedec, L.; Longrois, D.; Chastre, E.; Norel, X. Differential reactivity of human mammary artery and saphenous vein to prostaglandin E(2): Implication for cardiovascular grafts. Br. J. Pharmacol. 2011, 163, 826–834. [Google Scholar] [CrossRef]
- Jadhav, V.; Jabre, A.; Lin, S.Z.; Lee, T.J. EP1- and EP3-receptors mediate prostaglandin E2-induced constriction of porcine large cerebral arteries. J. Cereb. Blood Flow Metab. 2004, 24, 1305–1316. [Google Scholar] [CrossRef]
- Pan, X.F.; Grigoryeva, L.; Seyrantepe, V.; Peng, J.Z.; Kollmann, K.; Tremblay, J.; Lavoie, J.L.; Hinek, A.; Lubke, T.; Pshezhetsky, A.V. Serine Carboxypeptidase SCPEP1 and Cathepsin A Play Complementary Roles in Regulation of Vasoconstriction via Inactivation of Endothelin-1. PLoS Genet. 2014, 10, e1004146. [Google Scholar] [CrossRef]
- Yu, Y.; Lucitt, M.B.; Stubbe, J.; Cheng, Y.; Friis, U.G.; Hansen, P.B.; Jensen, B.L.; Smyth, E.M.; FitzGerald, G.A. Prostaglandin F2alpha elevates blood pressure and promotes atherosclerosis. Proc. Natl. Acad. Sci. USA 2009, 106, 7985–7990. [Google Scholar] [CrossRef]
- Wong, S.L.; Leung, F.P.; Lau, C.W.; Au, C.L.; Yung, L.M.; Yao, X.; Chen, Z.Y.; Vanhoutte, P.M.; Gollasch, M.; Huang, Y. Cyclooxygenase-2-derived prostaglandin F2alpha mediates endothelium-dependent contractions in the aortae of hamsters with increased impact during aging. Circ. Res. 2009, 104, 228–235. [Google Scholar] [CrossRef]
- Feletou, M.; Vanhoutte, P.M.; Verbeuren, T.J. The thromboxane/endoperoxide receptor (TP): The common villain. J. Cardiovasc. Pharmacol. 2010, 55, 317–332. [Google Scholar] [CrossRef]
- Chawengsub, Y.; Gauthier, K.M.; Campbell, W.B. Role of arachidonic acid lipoxygenase metabolites in the regulation of vascular tone. Am. J. Physiol. Heart Circ. Physiol. 2009, 297, H495–H507. [Google Scholar] [CrossRef] [PubMed]
- Randriamboavonjy, V.; Busse, R.; Fleming, I. 20-HETE-induced contraction of small coronary arteries depends on the activation of Rho-kinase. Hypertension 2003, 41, 801–806. [Google Scholar] [CrossRef] [PubMed]
- Miyata, N.; Roman, R.J. Role of 20-hydroxyeicosatetraenoic acid (20-HETE) in vascular system. J. Smooth Muscle Res. 2005, 41, 175–193. [Google Scholar] [CrossRef]
- Chen, Y.; Medhora, M.; Falck, J.R.; Pritchard, K.A., Jr.; Jacobs, E.R. Mechanisms of activation of eNOS by 20-HETE and VEGF in bovine pulmonary artery endothelial cells. Am. J. Physiol. Lung Cell Mol. Physiol. 2006, 291, L378–L385. [Google Scholar] [CrossRef]
- Campbell, W.B.; Falck, J.R.; Gauthier, K. Role of epoxyeicosatrienoic acids as endothelium-derived hyperpolarizing factor in bovine coronary arteries. Med. Sci. Monit. 2001, 7, 578–584. [Google Scholar] [PubMed]
- Larsen, B.T.; Miura, H.; Hatoum, O.A.; Campbell, W.B.; Hammock, B.D.; Zeldin, D.C.; Falck, J.R.; Gutterman, D.D. Epoxyeicosatrienoic and dihydroxyeicosatrienoic acids dilate human coronary arterioles via BK(Ca) channels: Implications for soluble epoxide hydrolase inhibition. Am. J. Physiol. Heart Circ. Physiol. 2006, 290, H491–H499. [Google Scholar] [CrossRef] [PubMed]
- Randhawa, P.K.; Jaggi, A.S. TRPV4 channels: Physiological and pathological role in cardiovascular system. Basic Res. Cardiol. 2015, 110, 54. [Google Scholar] [CrossRef] [PubMed]
- Peredo, H.A.; Rodriguez, R.; Susemihl, M.C.; Villarreal, I.; Filinger, E. Long-term streptozotocin-induced diabetes alters prostanoid production in rat aorta and mesenteric bed. Auton. Autacoid Pharmacol. 2006, 26, 355–360. [Google Scholar] [CrossRef] [PubMed]
- Zuccollo, A.; Shi, C.; Mastroianni, R.; Maitland-Toolan, K.A.; Weisbrod, R.M.; Zang, M.; Xu, S.; Jiang, B.; Oliver-Krasinski, J.M.; Cayatte, A.J.; et al. The thromboxane A2 receptor antagonist S18886 prevents enhanced atherogenesis caused by diabetes mellitus. Circulation 2005, 112, 3001–3008. [Google Scholar] [CrossRef]
- Chan, P.C.; Liao, M.T.; Hsieh, P.S. The Dualistic Effect of COX-2-Mediated Signaling in Obesity and Insulin Resistance. Int. J. Mol. Sci. 2019, 20, 3115. [Google Scholar] [CrossRef]
- Gao, Z.; Zhang, H.; Liu, J.; Lau, C.W.; Liu, P.; Chen, Z.Y.; Lee, H.K.; Tipoe, G.L.; Ho, H.M.; Yao, X.; et al. Cyclooxygenase-2-dependent oxidative stress mediates palmitate-induced impairment of endothelium-dependent relaxations in mouse arteries. Biochem. Pharmacol. 2014, 91, 474–482. [Google Scholar] [CrossRef]
- Zhang, H.; Liu, J.; Qu, D.; Wang, L.; Luo, J.Y.; Lau, C.W.; Liu, P.; Gao, Z.; Tipoe, G.L.; Lee, H.K.; et al. Inhibition of miR-200c Restores Endothelial Function in Diabetic Mice Through Suppression of COX-2. Diabetes 2016, 65, 1196–1207. [Google Scholar] [CrossRef] [PubMed]
- Dong, J.; Wong, S.L.; Lau, C.W.; Liu, J.; Wang, Y.X.; Dan He, Z.; Fai Ng, C.; Yu Chen, Z.; Yao, X.; Xu, A.; et al. Calcitriol restores renovascular function in estrogen-deficient rats through downregulation of cyclooxygenase-2 and the thromboxane-prostanoid receptor. Kidney Int. 2013, 84, 54–63. [Google Scholar] [CrossRef]
- Kim, D.H.; Puri, N.; Sodhi, K.; Falck, J.R.; Abraham, N.G.; Shapiro, J.; Schwartzman, M.L. Cyclooxygenase-2 dependent metabolism of 20-HETE increases adiposity and adipocyte enlargement in mesenchymal stem cell-derived adipocytes. J. Lipid Res. 2013, 54, 786–793. [Google Scholar] [CrossRef]
- Peterson, L.R. To Lose Weight or Not to Lose Weight, That Is the Big Question--in Obesity-Related Heart Failure. Diabetes 2015, 64, 1509–1510. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ibrahim, A.S.; Elshafey, S.; Sellak, H.; Hussein, K.A.; El-Sherbiny, M.; Abdelsaid, M.; Rizk, N.; Beasley, S.; Tawfik, A.M.; Smith, S.B.; et al. A lipidomic screen of hyperglycemia-treated HRECs links 12/15-Lipoxygenase to microvascular dysfunction during diabetic retinopathy via NADPH oxidase. J. Lipid Res. 2015, 56, 599–611. [Google Scholar] [CrossRef]
- Issan, Y.; Hochhauser, E.; Guo, A.; Gotlinger, K.H.; Kornowski, R.; Leshem-Lev, D.; Lev, E.; Porat, E.; Snir, E.; Thompson, C.I.; et al. Elevated level of pro-inflammatory eicosanoids and EPC dysfunction in diabetic patients with cardiac ischemia. Prostaglandins Other Lipid Mediat. 2013, 100–101, 15–21. [Google Scholar] [CrossRef]
- Yousif, M.H.; Benter, I.F.; Roman, R.J. Cytochrome P450 metabolites of arachidonic acid play a role in the enhanced cardiac dysfunction in diabetic rats following ischaemic reperfusion injury. Auton. Autacoid Pharmacol. 2009, 29, 33–41. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.P.; McClung, J.A.; Bellner, L.; Cao, J.; Waldman, M.; Schragenheim, J.; Arad, M.; Hochhauser, E.; Falck, J.R.; Weingarten, J.A.; et al. CYP-450 Epoxygenase Derived Epoxyeicosatrienoic Acid Contribute To Reversal of Heart Failure in Obesity-Induced Diabetic Cardiomyopathy via PGC-1 alpha Activation. Cardiovasc. Pharm. Open Access. 2018, 7, 233. [Google Scholar] [CrossRef] [PubMed]
- Yang, T.; Du, Y. Distinct roles of central and peripheral prostaglandin E2 and EP subtypes in blood pressure regulation. Am. J. Hypertens 2012, 25, 1042–1049. [Google Scholar] [CrossRef]
- Nasrallah, R.; Hassouneh, R.; Hebert, R.L. PGE2, Kidney Disease, and Cardiovascular Risk: Beyond Hypertension and Diabetes. J. Am. Soc. Nephrol. 2016, 27, 666–676. [Google Scholar] [CrossRef]
- Rutkai, I.; Feher, A.; Erdei, N.; Henrion, D.; Papp, Z.; Edes, I.; Koller, A.; Kaley, G.; Bagi, Z. Activation of prostaglandin E2 EP1 receptor increases arteriolar tone and blood pressure in mice with type 2 diabetes. Cardiovasc. Res. 2009, 83, 148–154. [Google Scholar] [CrossRef]
- Guan, Y.; Zhang, Y.; Wu, J.; Qi, Z.; Yang, G.; Dou, D.; Gao, Y.; Chen, L.; Zhang, X.; Davis, L.S.; et al. Antihypertensive effects of selective prostaglandin E2 receptor subtype 1 targeting. J. Clin. Investig. 2007, 117, 2496–2505. [Google Scholar] [CrossRef]
- Lu, A.; Zuo, C.; He, Y.; Chen, G.; Piao, L.; Zhang, J.; Xiao, B.; Shen, Y.; Tang, J.; Kong, D.; et al. EP3 receptor deficiency attenuates pulmonary hypertension through suppression of Rho/TGF-beta1 signaling. J. Clin. Investig. 2015, 125, 1228–1242. [Google Scholar] [CrossRef]
- Kennedy, C.R.; Zhang, Y.; Brandon, S.; Guan, Y.; Coffee, K.; Funk, C.D.; Magnuson, M.A.; Oates, J.A.; Breyer, M.D.; Breyer, R.M. Salt-sensitive hypertension and reduced fertility in mice lacking the prostaglandin EP2 receptor. Nat. Med. 1999, 5, 217–220. [Google Scholar] [CrossRef] [PubMed]
- Hristovska, A.M.; Rasmussen, L.E.; Hansen, P.B.; Nielsen, S.S.; Nusing, R.M.; Narumiya, S.; Vanhoutte, P.; Skott, O.; Jensen, B.L. Prostaglandin E2 induces vascular relaxation by E-prostanoid 4 receptor-mediated activation of endothelial nitric oxide synthase. Hypertension 2007, 50, 525–530. [Google Scholar] [CrossRef]
- Abe, S.; Ishida, K.; Masuda, M.; Ueda, H.; Kohno, H.; Matsuura, K.; Tamura, Y.; Watanabe, M.; Matsumiya, G. A prospective, randomized study of inhaled prostacyclin versus nitric oxide in patients with residual pulmonary hypertension after pulmonary endarterectomy. Gen. Thorac. Cardiovasc. Surg. 2016, 65, 153–159. [Google Scholar] [CrossRef]
- Jacobs, W.; Vonk-Noordegraaf, A. Epoprostenol in pulmonary arterial hypertension. Expert Opin. Drug Metab. Toxicol. 2009, 5, 83–90. [Google Scholar] [CrossRef]
- Menon, A.A.; Sahay, S.; Braverman, L.E.; Farber, H.W. Thyroid Dysfunction in Patients with Pulmonary Artery Hypertension (PAH): The Effect of Therapies Affecting the Prostanoid Pathway. Lung 2019, 197, 761–768. [Google Scholar] [CrossRef] [PubMed]
- Tian, X.Y.; Wong, W.T.; Leung, F.P.; Zhang, Y.; Wang, Y.X.; Lee, H.K.; Ng, C.F.; Chen, Z.Y.; Yao, X.; Au, C.L.; et al. Oxidative stress-dependent cyclooxygenase-2-derived prostaglandin f(2alpha) impairs endothelial function in renovascular hypertensive rats. Antioxid. Redox Signal. 2012, 16, 363–373. [Google Scholar] [CrossRef]
- Wong, W.T.; Tian, X.Y.; Chen, Y.; Leung, F.P.; Liu, L.; Lee, H.K.; Ng, C.F.; Xu, A.; Yao, X.; Vanhoutte, P.M.; et al. Bone morphogenic protein-4 impairs endothelial function through oxidative stress-dependent cyclooxygenase-2 upregulation: Implications on hypertension. Circ. Res. 2010, 107, 984–991. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.; Liu, J.; Tian, X.Y.; Wong, W.T.; Lau, C.W.; Xu, A.; Xu, G.; Ng, C.F.; Yao, X.; Gao, Y.; et al. Uncoupling protein-2 mediates DPP-4 inhibitor-induced restoration of endothelial function in hypertension through reducing oxidative stress. Antioxid. Redox Signal. 2014, 21, 1571–1581. [Google Scholar] [CrossRef] [PubMed]
- Singh, H.; Cheng, J.; Deng, H.; Kemp, R.; Ishizuka, T.; Nasjletti, A.; Schwartzman, M.L. Vascular cytochrome P450 4A expression and 20-hydroxyeicosatetraenoic acid synthesis contribute to endothelial dysfunction in androgen-induced hypertension. Hypertension 2007, 50, 123–129. [Google Scholar] [CrossRef]
- Cheng, J.; Wu, C.C.; Gotlinger, K.H.; Zhang, F.; Falck, J.R.; Narsimhaswamy, D.; Schwartzman, M.L. 20-hydroxy-5,8,11,14-eicosatetraenoic acid mediates endothelial dysfunction via IkappaB kinase-dependent endothelial nitric-oxide synthase uncoupling. J. Pharmacol. Exp. Ther. 2010, 332, 57–65. [Google Scholar] [CrossRef]
- Inoue, K.; Sodhi, K.; Puri, N.; Gotlinger, K.H.; Cao, J.; Rezzani, R.; Falck, J.R.; Abraham, N.G.; Laniado-Schwartzman, M. Endothelial-specific CYP4A2 overexpression leads to renal injury and hypertension via increased production of 20-HETE. Am. J. Physiol. Renal. Physiol. 2009, 297, F875–F884. [Google Scholar] [CrossRef] [PubMed]
- Narasimha, A.; Watanabe, J.; Lin, J.A.; Hama, S.; Langenbach, R.; Navab, M.; Fogelman, A.M.; Reddy, S.T. A novel anti-atherogenic role for COX-2--potential mechanism for the cardiovascular side effects of COX-2 inhibitors. Prostaglandins Other Lipid Mediat. 2007, 84, 24–33. [Google Scholar] [CrossRef]
- Yu, Z.; Crichton, I.; Tang, S.Y.; Hui, Y.; Ricciotti, E.; Levin, M.D.; Lawson, J.A.; Pure, E.; FitzGerald, G.A. Disruption of the 5-lipoxygenase pathway attenuates atherogenesis consequent to COX-2 deletion in mice. Proc. Natl. Acad. Sci. USA 2012, 109, 6727–6732. [Google Scholar] [CrossRef]
- Yuen, C.Y.; Wong, S.L.; Lau, C.W.; Tsang, S.Y.; Xu, A.; Zhu, Z.; Ng, C.F.; Yao, X.; Kong, S.K.; Lee, H.K.; et al. From skeleton to cytoskeleton: Osteocalcin transforms vascular fibroblasts to myofibroblasts via angiotensin II and Toll-like receptor 4. Circ. Res. 2012, 111, e55–e66. [Google Scholar] [CrossRef]
- Wong, S.L.; Lau, C.W.; Wong, W.T.; Xu, A.; Au, C.L.; Ng, C.F.; Ng, S.S.; Gollasch, M.; Yao, X.; Huang, Y. Pivotal role of protein kinase Cdelta in angiotensin II-induced endothelial cyclooxygenase-2 expression: A link to vascular inflammation. Arter. Thromb. Vasc. Biol. 2011, 31, 1169–1176. [Google Scholar] [CrossRef]
- Patrono, C. Low-dose aspirin in primary prevention: Cardioprotection, chemoprevention, both, or neither? Eur. Heart J. 2013, 34, 3403–3411. [Google Scholar] [CrossRef] [PubMed]
- Lu, N.; Zhan, M.; Gao, C.; Wu, G.; Zhang, H. I4, a new synthetic sulfonylurea compound, inhibits the action of TXA2 in vivo and in vitro on platelets and aorta vascular smooth muscle. Thromb. Res. 2012, 130, e209–e215. [Google Scholar] [CrossRef]
- Cai, Z.; Zhao, G.; Yan, J.; Liu, W.; Feng, W.; Ma, B.; Yang, L.; Wang, J.A.; Tu, L.; Wang, D.W. CYP2J2 overexpression increases EETs and protects against angiotensin II-induced abdominal aortic aneurysm in mice. J. Lipid Res. 2013, 54, 1448–1456. [Google Scholar] [CrossRef]
- Cipollone, F.; Fazia, M.L.; Iezzi, A.; Cuccurullo, C.; De Cesare, D.; Ucchino, S.; Spigonardo, F.; Marchetti, A.; Buttitta, F.; Paloscia, L.; et al. Association between prostaglandin E receptor subtype EP4 overexpression and unstable phenotype in atherosclerotic plaques in human. Arterioscler. Thromb. Vasc. Biol. 2005, 25, 1925–1931. [Google Scholar] [CrossRef] [PubMed]
- Cao, R.Y.; St Amand, T.; Li, X.; Yoon, S.H.; Wang, C.P.; Song, H.; Maruyama, T.; Brown, P.M.; Zelt, D.T.; Funk, C.D. Prostaglandin receptor EP4 in abdominal aortic aneurysms. Am. J. Pathol. 2012, 181, 313–321. [Google Scholar] [CrossRef] [PubMed]
- Camacho, M.; Dilme, J.; Sola-Villa, D.; Rodriguez, C.; Bellmunt, S.; Siguero, L.; Alcolea, S.; Romero, J.M.; Escudero, J.R.; Martinez-Gonzalez, J.; et al. Microvascular COX-2/mPGES-1/EP-4 axis in human abdominal aortic aneurysm. J. Lipid Res. 2013, 54, 3506–3515. [Google Scholar] [CrossRef]
- Tang, E.H.; Shimizu, K.; Christen, T.; Rocha, V.Z.; Shvartz, E.; Tesmenitsky, Y.; Sukhova, G.; Shi, G.P.; Libby, P. Lack of EP4 receptors on bone marrow-derived cells enhances inflammation in atherosclerotic lesions. Cardiovasc. Res. 2011, 89, 234–243. [Google Scholar] [CrossRef]
- Tang, E.H.; Shvartz, E.; Shimizu, K.; Rocha, V.Z.; Zheng, C.; Fukuda, D.; Shi, G.P.; Sukhova, G.; Libby, P. Deletion of EP4 on bone marrow-derived cells enhances inflammation and angiotensin II-induced abdominal aortic aneurysm formation. Arterioscler. Thromb. Vasc. Biol. 2011, 31, 261–269. [Google Scholar] [CrossRef] [PubMed]
- Li, R.; Mouillesseaux, K.P.; Montoya, D.; Cruz, D.; Gharavi, N.; Dun, M.; Koroniak, L.; Berliner, J.A. Identification of prostaglandin E2 receptor subtype 2 as a receptor activated by OxPAPC. Circ. Res. 2006, 98, 642–650. [Google Scholar] [CrossRef]
- Zhu, S.; Xue, R.; Zhao, P.; Fan, F.L.; Kong, X.; Zheng, S.; Han, Q.; Zhu, Y.; Wang, N.; Yang, J.; et al. Targeted disruption of the prostaglandin E2 E-prostanoid 2 receptor exacerbates vascular neointimal formation in mice. Arterioscler. Thromb. Vasc. Biol. 2011, 31, 1739–1747. [Google Scholar] [CrossRef]
- Gross, S.; Tilly, P.; Hentsch, D.; Vonesch, J.L.; Fabre, J.E. Vascular wall-produced prostaglandin E2 exacerbates arterial thrombosis and atherothrombosis through platelet EP3 receptors. J. Exp. Med. 2007, 204, 311–320. [Google Scholar] [CrossRef] [PubMed]
- Ma, H.; Hara, A.; Xiao, C.Y.; Okada, Y.; Takahata, O.; Nakaya, K.; Sugimoto, Y.; Ichikawa, A.; Narumiya, S.; Ushikubi, F. Increased bleeding tendency and decreased susceptibility to thromboembolism in mice lacking the prostaglandin E receptor subtype EP(3). Circulation 2001, 104, 1176–1180. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Zou, F.; Tang, J.; Zhang, Q.; Gong, Y.; Wang, Q.; Shen, Y.; Xiong, L.; Breyer, R.M.; Lazarus, M.; et al. Cyclooxygenase-2-derived prostaglandin E(2) promotes injury-induced vascular neointimal hyperplasia through the E-prostanoid 3 receptor. Circ. Res. 2013, 113, 104–114. [Google Scholar] [CrossRef]
- Gomez-Hernandez, A.; Sanchez-Galan, E.; Martin-Ventura, J.L.; Vidal, C.; Blanco-Colio, L.M.; Ortego, M.; Vega, M.; Serrano, J.; Ortega, L.; Hernandez, G.; et al. Atorvastatin reduces the expression of prostaglandin E2 receptors in human carotid atherosclerotic plaques and monocytic cells: Potential implications for plaque stabilization. J. Cardiovasc. Pharmacol. 2006, 47, 60–69. [Google Scholar] [CrossRef]
- Mawhin, M.A.; Tilly, P.; Zirka, G.; Charles, A.L.; Slimani, F.; Vonesch, J.L.; Michel, J.B.; Back, M.; Norel, X.; Fabre, J.E. Neutrophils recruited by leukotriene B4 induce features of plaque destabilization during endotoxaemia. Cardiovasc. Res. 2018, 114, 1656–1666. [Google Scholar] [CrossRef] [PubMed]
- Jiang, W.; Hall, S.R.; Moos, M.P.; Cao, R.Y.; Ishii, S.; Ogunyankin, K.O.; Melo, L.G.; Funk, C.D. Endothelial cysteinyl leukotriene 2 receptor expression mediates myocardial ischemia-reperfusion injury. Am. J. Pathol. 2008, 172, 592–602. [Google Scholar] [CrossRef] [PubMed]
- Qiu, H.; Gabrielsen, A.; Agardh, H.E.; Wan, M.; Wetterholm, A.; Wong, C.H.; Hedin, U.; Swedenborg, J.; Hansson, G.K.; Samuelsson, B.; et al. Expression of 5-lipoxygenase and leukotriene A4 hydrolase in human atherosclerotic lesions correlates with symptoms of plaque instability. Proc. Natl. Acad. Sci. USA 2006, 103, 8161–8166. [Google Scholar] [CrossRef]
- Hoxha, M.; Capra, V.; Malaj, V.; Sala, A.; Rovati, G. The Role of Montelukast in Cardiovascular Events. Atherosclerosis 2017, 263, E150. [Google Scholar] [CrossRef]
- Leedom, A.J.; Sullivan, A.B.; Dong, B.; Lau, D.; Gronert, K. Endogenous LXA4 circuits are determinants of pathological angiogenesis in response to chronic injury. Am. J. Pathol. 2010, 176, 74–84. [Google Scholar] [CrossRef] [PubMed]
- Mei, H.X.; Ye, Y.; Xu, H.R.; Xiang, S.Y.; Yang, Q.; Ma, H.Y.; Jin, S.W.; Wang, Q. LXA4 Inhibits Lipopolysaccharide-Induced Inflammatory Cell Accumulation by Resident Macrophages in Mice. J. Inflamm. Res. 2021, 14, 1375–1385. [Google Scholar] [CrossRef]
- Romano, M.; Cianci, E.; Simiele, F.; Recchiuti, A. Lipoxins and aspirin-triggered lipoxins in resolution of inflammation. Eur. J. Pharmacol. 2015, 760, 49–63. [Google Scholar] [CrossRef] [PubMed]
- Das, U.N. Bioactive Lipids as Mediators of the Beneficial Actions of Statins. J. Cardiovasc. Pharm. 2019, 74, 4–8. [Google Scholar] [CrossRef]
- Nielsen, M.S.; Schmidt, E.B.; Stegger, J.; Gorst-Rasmussen, A.; Tjonneland, A.; Overvad, K. Adipose tissue arachidonic acid content is associated with the risk of myocardial infarction: A Danish case-cohort study. Atherosclerosis 2013, 227, 386–390. [Google Scholar] [CrossRef]
- Degousee, N.; Fazel, S.; Angoulvant, D.; Stefanski, E.; Pawelzik, S.C.; Korotkova, M.; Arab, S.; Liu, P.; Lindsay, T.F.; Zhuo, S.; et al. Microsomal prostaglandin E2 synthase-1 deletion leads to adverse left ventricular remodeling after myocardial infarction. Circulation 2008, 117, 1701–1710. [Google Scholar] [CrossRef]
- Martin, M.; Meyer-Kirchrath, J.; Kaber, G.; Jacoby, C.; Flogel, U.; Schrader, J.; Ruther, U.; Schror, K.; Hohlfeld, T. Cardiospecific overexpression of the prostaglandin EP3 receptor attenuates ischemia-induced myocardial injury. Circulation 2005, 112, 400–406. [Google Scholar] [CrossRef]
- Zacharowski, K.; Olbrich, A.; Piper, J.; Hafner, G.; Kondo, K.; Thiemermann, C. Selective activation of the prostanoid EP(3) receptor reduces myocardial infarct size in rodents. Arterioscler. Thromb. Vasc. Biol. 1999, 19, 2141–2147. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Ji, Y.; Yao, J.; Zhao, X.; Xu, H.; Guan, Y.; Breyer, R.M.; Sheng, H.; Zhu, J. Knockout of the Prostaglandin E2 Receptor Subtype 3 Promotes Eccentric Cardiac Hypertrophy and Fibrosis in Mice. J. Cardiovasc. Pharmacol. Ther. 2016, 22, 71–82. [Google Scholar] [CrossRef] [PubMed]
- Xiao, C.Y.; Yuhki, K.; Hara, A.; Fujino, T.; Kuriyama, S.; Yamada, T.; Takayama, K.; Takahata, O.; Karibe, H.; Taniguchi, T.; et al. Prostaglandin E2 protects the heart from ischemia-reperfusion injury via its receptor subtype EP4. Circulation 2004, 109, 2462–2468. [Google Scholar] [CrossRef]
- Hishikari, K.; Suzuki, J.; Ogawa, M.; Isobe, K.; Takahashi, T.; Onishi, M.; Takayama, K.; Isobe, M. Pharmacological activation of the prostaglandin E2 receptor EP4 improves cardiac function after myocardial ischaemia/reperfusion injury. Cardiovasc. Res. 2009, 81, 123–132. [Google Scholar] [CrossRef]
- Katsumata, Y.; Shinmura, K.; Sugiura, Y.; Tohyama, S.; Matsuhashi, T.; Ito, H.; Yan, X.; Ito, K.; Yuasa, S.; Ieda, M.; et al. Endogenous prostaglandin D2 and its metabolites protect the heart against ischemia-reperfusion injury by activating Nrf2. Hypertension 2014, 63, 80–87. [Google Scholar] [CrossRef] [PubMed]
- Xiao, C.Y.; Hara, A.; Yuhki, K.; Fujino, T.; Ma, H.; Okada, Y.; Takahata, O.; Yamada, T.; Murata, T.; Narumiya, S.; et al. Roles of prostaglandin I(2) and thromboxane A(2) in cardiac ischemia-reperfusion injury: A study using mice lacking their respective receptors. Circulation 2001, 104, 2210–2215. [Google Scholar] [CrossRef] [PubMed]
- Antithrombotic Trialists’ Collaboration. Collaborative meta-analysis of randomised trials of antiplatelet therapy for prevention of death, myocardial infarction, and stroke in high risk patients. BMJ 2002, 324, 71–86. [Google Scholar]
- Wacker, M.J.; Kosloski, L.M.; Gilbert, W.J.; Touchberry, C.D.; Moore, D.S.; Kelly, J.K.; Brotto, M.; Orr, J.A. Inhibition of thromboxane A2-induced arrhythmias and intracellular calcium changes in cardiac myocytes by blockade of the inositol trisphosphate pathway. J. Pharmacol. Exp. Ther. 2009, 331, 917–924. [Google Scholar] [CrossRef]
- Santos, M.T.; Fuset, M.P.; Ruano, M.; Moscardo, A.; Valles, J. Effect of Atorvastatin on Platelet Thromboxane A(2) Synthesis in Aspirin-Treated Patients with Acute Myocardial Infarction. Am. J. Cardiol. 2009, 104, 1618–1623. [Google Scholar] [CrossRef]
- Yang, L.; Ni, L.; Duan, Q.; Wang, X.; Chen, C.; Chen, S.; Chaugai, S.; Zeldin, D.C.; Tang, J.R.; Wang, D.W. CYP epoxygenase 2J2 prevents cardiac fibrosis by suppression of transmission of pro-inflammation from cardiomyocytes to macrophages. Prostaglandins Other Lipid Mediat. 2015, 116-117, 64–75. [Google Scholar] [CrossRef]
- Batchu, S.N.; Lee, S.B.; Qadhi, R.S.; Chaudhary, K.R.; El-Sikhry, H.; Kodela, R.; Falck, J.R.; Seubert, J.M. Cardioprotective effect of a dual acting epoxyeicosatrienoic acid analogue towards ischaemia reperfusion injury. Br. J. Pharmacol. 2011, 162, 897–907. [Google Scholar] [CrossRef]
- Nithipatikom, K.; Moore, J.M.; Isbell, M.A.; Falck, J.R.; Gross, G.J. Epoxyeicosatrienoic acids in cardioprotection: Ischemic versus reperfusion injury. Am. J. Physiol. Heart Circ. Physiol. 2006, 291, H537–H542. [Google Scholar] [CrossRef]
- Huang, C.C.; Chang, M.T.; Leu, H.B.; Yin, W.H.; Tseng, W.K.; Wu, Y.W.; Lin, T.H.; Yeh, H.I.; Chang, K.C.; Wang, J.H.; et al. Association of Arachidonic Acid-derived Lipid Mediators with Subsequent Onset of Acute Myocardial Infarction in Patients with Coronary Artery Disease. Sci. Rep. 2020, 10, 8105. [Google Scholar] [CrossRef]
- Wang, C.H.; Ouyang, Q.; Tang, C.W.; Huang, M.H.; Li, X. [Effects of selective and non-selective cyclooxygenase-2 inhibitor on the growth of colon cancer cells]. Sichuan Da Xue Xue Bao Yi Xue Ban 2006, 37, 547–550. [Google Scholar]
- Martin-Garcia, C.; Hinojosa, M.; Berges, P.; Camacho, E.; Garcia-Rodriguez, R.; Alfaya, T. Celecoxib, a highly selective COX-2 inhibitor, is safe in aspirin-induced asthma patients. J. Investig. Allergol. Clin. Immunol. 2003, 13, 20–25. [Google Scholar]
- Stuntz, M.; Bernstein, B. Recent trends in the prevalence of low-dose aspirin use for primary and secondary prevention of cardiovascular disease in the United States, 2012–2015. Prev. Med. Rep. 2017, 5, 183–186. [Google Scholar] [CrossRef]
- Antithrombotic Trialists’ Collaboration; Baigent, C.; Blackwell, L.; Collins, R.; Emberson, J.; Godwin, J.; Peto, R.; Buring, J.; Hennekens, C.; Kearney, P.; et al. Aspirin in the primary and secondary prevention of vascular disease: Collaborative meta-analysis of individual participant data from randomised trials. Lancet 2009, 373, 1849–1860. [Google Scholar] [CrossRef]
- Rodondi, N.; Bauer, D.C. Assessing the risk/benefit profile before recommending aspirin for the primary prevention of cardiovascular events. Am. J. Med. 2004, 117, 528–530. [Google Scholar] [CrossRef] [PubMed]
- Grosser, T.; Fries, S.; FitzGerald, G.A. Biological basis for the cardiovascular consequences of COX-2 inhibition: Therapeutic challenges and opportunities. J. Clin. Investig. 2006, 116, 4–15. [Google Scholar] [CrossRef]
- Sun, S.X.; Lee, K.Y.; Bertram, C.T.; Goldstein, J.L. Withdrawal of COX-2 selective inhibitors rofecoxib and valdecoxib: Impact on NSAID and gastroprotective drug prescribing and utilization. Curr. Med. Res. Opin. 2007, 23, 1859–1866. [Google Scholar] [CrossRef] [PubMed]
- Bolten, W.W.; Reiter, S.; Kommission Pharmakotherapie und des Vorstandes der Deutschen Gesellschaft für Rheumatologie. Cardiovascular risks of Cox-2-antagonists. Opinion on the marketed name rofecoxib, and its market-withdrawn valdecoxib and the actual therapeutic restrictions. Z. Rheumatol. 2005, 64, 286–289. [Google Scholar] [CrossRef]
- Howes, L.G. Selective COX-2 inhibitors, NSAIDs and cardiovascular events-is celecoxib the safest choice? Ther. Clin. Risk. Manag. 2007, 3, 831–845. [Google Scholar] [PubMed]
- Cayatte, A.J.; Du, Y.; Oliver-Krasinski, J.; Lavielle, G.; Verbeuren, T.J.; Cohen, R.A. The thromboxane receptor antagonist S18886 but not aspirin inhibits atherogenesis in apo E-deficient mice: Evidence that eicosanoids other than thromboxane contribute to atherosclerosis. Arterioscler. Thromb. Vasc. Biol. 2000, 20, 1724–1728. [Google Scholar] [CrossRef]
- Viles-Gonzalez, J.F.; Fuster, V.; Corti, R.; Valdiviezo, C.; Hutter, R.; Corda, S.; Anand, S.X.; Badimon, J.J. Atherosclerosis regression and TP receptor inhibition: Effect of S18886 on plaque size and composition--a magnetic resonance imaging study. Eur. Heart J. 2005, 26, 1557–1561. [Google Scholar] [CrossRef]
- Bousser, M.G.; Amarenco, P.; Chamorro, A.; Fisher, M.; Ford, I.; Fox, K.M.; Hennerici, M.G.; Mattle, H.P.; Rothwell, P.M.; de Cordoue, A.; et al. Terutroban versus aspirin in patients with cerebral ischaemic events (PERFORM): A randomised, double-blind, parallel-group trial. Lancet 2011, 377, 2013–2022. [Google Scholar] [CrossRef]
- Bots, M.L.; Ford, I.; Lloyd, S.M.; Laurent, S.; Touboul, P.J.; Hennerici, M.G.; Prevention of Cerebrovascular and Cardiovascular Events of Ischemic Origin with Terutroban in Patients with a History of Ischemic Stroke or Transient Ischemic Attack Vascular Ultrasound Study Investigators. Thromboxane prostaglandin receptor antagonist and carotid atherosclerosis progression in patients with cerebrovascular disease of ischemic origin: A randomized controlled trial. Stroke 2014, 45, 2348–2353. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Sakariassen, K.S.; Femia, E.A.; Daray, F.M.; Podda, G.M.; Razzari, C.; Pugliano, M.; Errasti, A.E.; Armesto, A.R.; Nowak, W.; Alberts, P.; et al. EV-077 in vitro inhibits platelet aggregation in type-2 diabetics on aspirin. Thromb. Res. 2012, 130, 746–752. [Google Scholar] [CrossRef]
- McCarberg, B.H.; Cryer, B. Evolving therapeutic strategies to improve nonsteroidal anti-inflammatory drug safety. Am. J. Ther. 2015, 22, e167–e178. [Google Scholar] [CrossRef] [PubMed]
- Yam, D.; Eliraz, A.; Berry, E.M. Diet and disease--the Israeli paradox: Possible dangers of a high omega-6 polyunsaturated fatty acid diet. Isr. J. Med. Sci. 1996, 32, 1134–1143. [Google Scholar]
- Zhong, V.W.; Van Horn, L.; Greenland, P.; Carnethon, M.R.; Ning, H.; Wilkins, J.T.; Lloyd-Jones, D.M.; Allen, N.B. Associations of Processed Meat, Unprocessed Red Meat, Poultry, or Fish Intake with Incident Cardiovascular Disease and All-Cause Mortality. JAMA Intern. Med. 2020, 180, 503–512. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.A.; Shin, S. Red meat and processed meat consumption and the risk of dyslipidemia in Korean adults: A prospective cohort study based on the Health Examinees (HEXA) study. Nutr. Metab. Cardiovasc. Dis. 2021, 31, 1714–1727. [Google Scholar] [CrossRef] [PubMed]
- McAfee, A.J.; McSorley, E.M.; Cuskelly, G.J.; Moss, B.W.; Wallace, J.M.; Bonham, M.; Fearon, A.M. Red meat consumption: An overview of the risks and benefits. Meat Sci. 2010, 84, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Hodgson, J.M.; Wahlqvist, M.L.; Boxall, J.A.; Balazs, N.D. Can linoleic acid contribute to coronary artery disease? Am. J. Clin. Nutr. 1993, 58, 228–234. [Google Scholar] [CrossRef]
- Loeper, J.; Goy, J.; Emerit, J. Lipid peroxidation in human and experimental atherosclerosis. Bull. Acad. Natl. Med. 1984, 168, 91–97. [Google Scholar] [PubMed]
- Loeper, J.; Goy, J.; Emerit, J.; Rozensztajn, L.; Jeny, C.; Bedu, O. Fatty acid and lipid peroxidation in human atherosclerosis. Sem. Hop. 1983, 59, 1657–1660. [Google Scholar] [PubMed]
- DiNicolantonio, J.J.; O’Keefe, J.H. Effects of dietary fats on blood lipids: A review of direct comparison trials. Open Heart 2018, 5, e000871. [Google Scholar] [CrossRef] [PubMed]
- Berry, E.M. Are diets high in omega-6 polyunsaturated fatty acids unhealthy? Eur. Heart J. Suppl. 2001, 3, D37–D41. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).