Left Axis Deviation in Brugada Syndrome: Vectorcardiographic Evaluation during Ajmaline Provocation Testing Reveals Additional Depolarization Abnormalities
Abstract
1. Introduction
2. Results
2.1. Baseline Characteristics
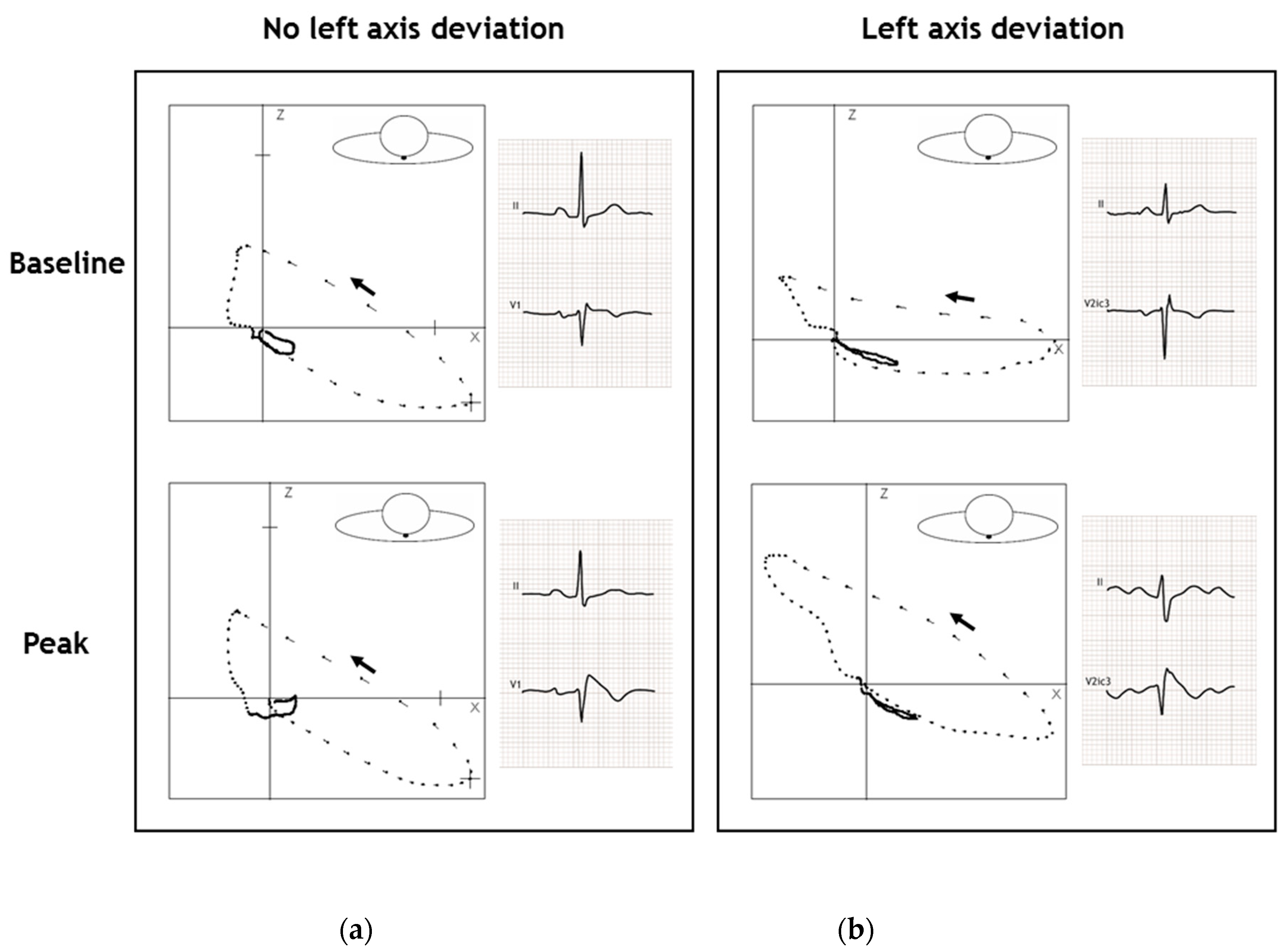
2.2. Baseline Vectorcardiogram Parameters
2.3. Vectorcardiogram Parameters at Peak Ajmaline Dose
2.3.1. Depolarization Abnormalities
2.3.2. Repolarization Abnormalities
3. Discussion
3.1. Main Findings
3.2. Future Perspective
3.3. Limitations
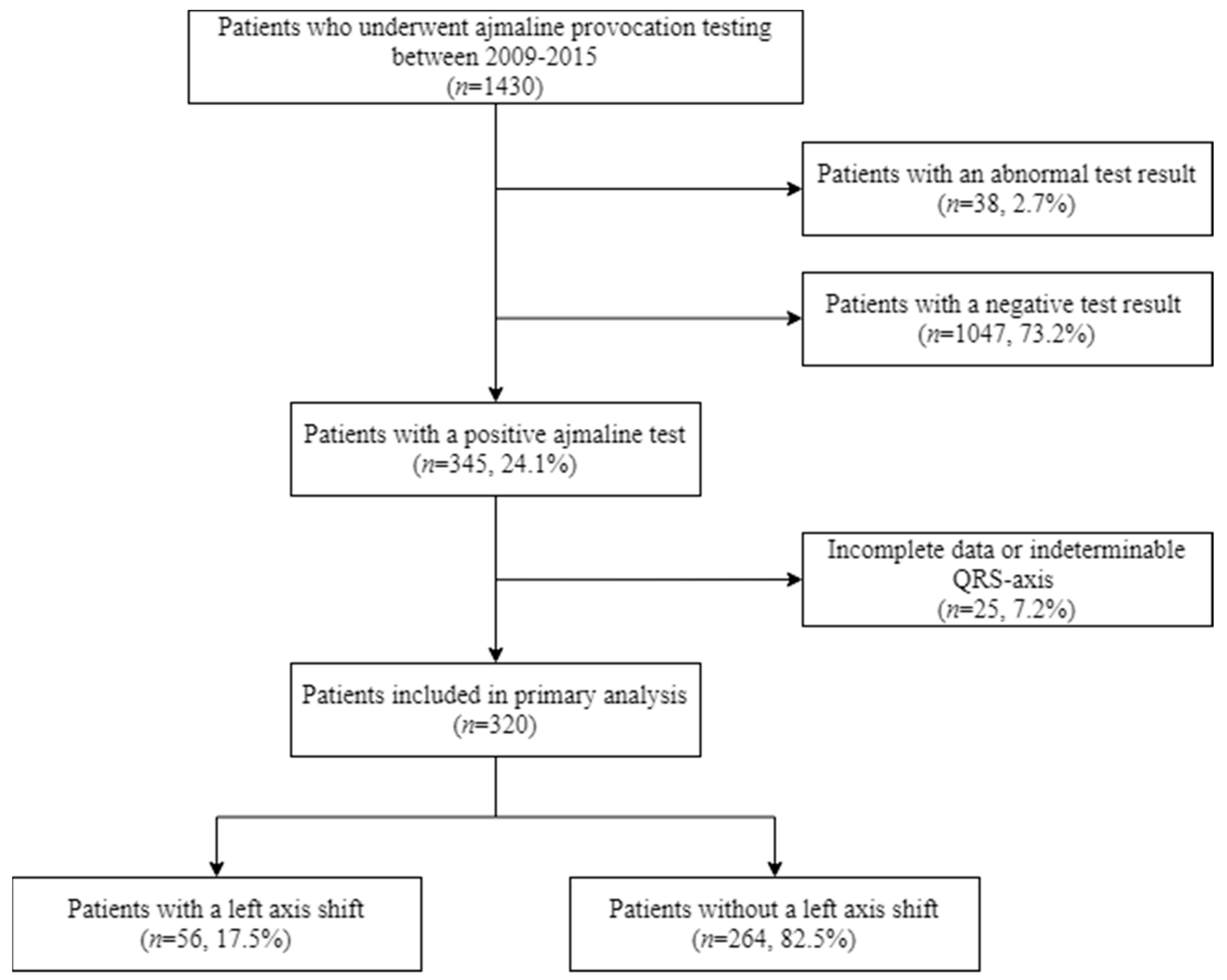
4. Materials and Methods
4.1. Patients and Sodium Channel Provocation Testing
4.2. Electrocardiographic Recordings, Analysis and Definitions
4.2.1. Electrocardiographic Recordings
4.2.2. Electrocardiographic Analysis
4.2.3. Electrocardiographic Definitions
4.3. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| BrS | Brugada Syndrome |
| ECG | Electrocardiogram |
References
- Antzelevitch, C.; Yan, G.-X.; Ackerman, M.J.; Borggrefe, M.; Corrado, D.; Guo, J.; Gussak, I.; Hasdemir, C.; Horie, M.; Huikuri, H.; et al. J-Wave syndromes expert consensus conference report: Emerging concepts and gaps in knowledge. Europace 2016, 13, 665–694. [Google Scholar] [CrossRef]
- Morita, H.; Morita, S.T.; Nagase, S.; Banba, K.; Nishii, N.; Tani, Y.; Watanabe, A.; Nakamura, K.; Kusano, K.F.; Emori, T.; et al. Ventricular Arrhythmia Induced by Sodium Channel Blocker in Patients with Brugada Syndrome. J. Am. Coll. Cardiol. 2003, 42, 1624–1631. [Google Scholar] [CrossRef] [PubMed]
- Wilde, A.A.M.; Antzelevitch, C.; Borggrefe, M.; Brugada, J.; Brugada, R.; Brugada, P.; Corrado, D.; Hauer, R.N.W.; Kass, R.S.; Nademanee, K.; et al. Proposed diagnostic criteria for the Brugada syndrome: Consensus report. Circulation 2002, 106, 2514–2519. [Google Scholar] [CrossRef] [PubMed]
- Postema, P.G.; van Dessel, P.F.H.M.; Kors, J.A.; Linnenbank, A.C.; van Herpen, G.; Ritsema van Eck, H.J.; van Geloven, N.; de Bakker, J.M.T.; Wilde, A.A.M.; Tan, H.L. Local Depolarization Abnormalities Are the Dominant Pathophysiologic Mechanism for Type 1 Electrocardiogram in Brugada Syndrome. A Study of Electrocardiograms, Vectorcardiograms, and Body Surface Potential Maps During Ajmaline Provocation. J. Am. Coll. Cardiol. 2010, 55, 789–797. [Google Scholar] [CrossRef] [PubMed]
- Pappone, C.; Mecarocci, V.; Manguso, F.; Ciconte, G.; Vicedomini, G.; Sturla, F.; Votta, E.; Mazza, B.; Pozzi, P.; Borrelli, V.; et al. New electromechanical substrate abnormalities in high-risk patients with Brugada syndrome. Heart Rhythm 2020, 17, 637–645. [Google Scholar] [CrossRef] [PubMed]
- Pérez Riera, A.R.; Uchida, A.H.; Filho, C.F.; Meneghini, A.; Ferreira, C.; Schapacknik, E.; Dubner, S.; Moffa, P. Significance of Vectorcardiogram in the Cardiological Diagnosis of the 21st Century. Clin. Cardiol. 2007, 30, 319–323. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Riera, A.R.; Ferreira Filho, C.; de Abreu, L.C.; Ferreira, C.; Yanowitz, F.G.; Femenia, F.; Brugada, P.; Baranchuk, A. Do patients with electrocardiographic Brugada type 1 pattern have associated right bundle branch block? A comparative vectorcardiographic study. Europace 2012, 14, 889–897. [Google Scholar] [CrossRef] [PubMed]
- Kardys, I.; Kors, J.A.; Van der Meer, I.M.; Hofman, A.; Van der Kuip, D.A.M.; Witteman, J.C.M. Spatial QRS-T angle predicts cardiac death in a general population. Eur. Heart J. 2003, 24, 1357–1364. [Google Scholar] [CrossRef]
- Draisma, H.H.M.; Schalij, M.J.; van der Wall, E.E.; Swenne, C.A. Elucidation of the spatial ventricular gradient and its link with dispersion of repolarization. Heart Rhythm 2006, 3, 1092–1099. [Google Scholar] [CrossRef] [PubMed]
- Durrer, D.; van Dam, R.T.; Freud, G.E.; Janse, M.J.; Meijler, F.L.; Arzbaecher, R.C. Total excitation of the isolated human heart. Circulation 1970, 41, 899–912. [Google Scholar] [CrossRef]
- Lambiase, P.D.; Rinaldi, A.; Hauck, J.; Mobb, M.; Elliott, D.; Mohammad, S.; Gill, J.S.; Bucknall, C.A. Non-contact left ventricular endocardial mapping in cardiac resynchronisation therapy. Heart 2004, 90, 44–51. [Google Scholar] [CrossRef] [PubMed]
- Postema, P.G.; van Dessel, P.F.H.M.; de Bakker, J.M.T.; Dekker, L.R.C.; Linnenbank, A.C.; Hoogendijk, M.G.; Coronel, R.; Tijssen, J.G.P.; Wilde, A.A.M.; Tan, H.L. Slow and discontinuous conduction conspire in Brugada syndrome: A right ventricular mapping and stimulation study. Circ. Arrhythm. Electrophysiol. 2008, 1, 379–386. [Google Scholar] [CrossRef] [PubMed]
- Hoogendijk, M.G.; Potse, M.; Vinet, A.; de Bakker, J.M.T.; Coronel, R. ST segment elevation by current-to-load mismatch: An experimental and computational study. Heart Rhythm 2011, 8, 111–118. [Google Scholar] [CrossRef] [PubMed]
- Hoogendijk, M.G.; Opthof, T.; Postema, P.G.; Wilde, A.A.M.; De Bakker, J.M.T.; Coronel, R. The Brugada ECG pattern a marker of channelopathy, structural heart disease, or neither? Toward a unifying mechanism of the Brugada syndrome. Circ. Arrhythmia Electrophysiol. 2010, 3, 283–290. [Google Scholar] [CrossRef] [PubMed]
- Kors, J.A.; Van Herpen, G.; Sittig, A.C.; Van Bemmel, J.H. Reconstruction of the frank vectorcardiogram from standard electrocardiographic leads: Diagnostic comparison of different methods. Eur. Heart J. 1990, 11, 1083–1092. [Google Scholar] [CrossRef] [PubMed]
- Van Bemmel, J.H.; Kors, J.A.; van Herpen, G. Methodology of the modular ECG analysis system MEANS. Methods Inf. Med. 1990, 29, 346–353. [Google Scholar] [PubMed]

| Characteristic | Left Axis Deviation (n = 56) | No Left Axis Deviation (n = 264) |
|---|---|---|
| Age, years | 46 ± 13 | 45 ± 13 |
| Male sex | 20 (35.7) * | 143 (54.2) |
| Length, cm | 171 ± 10 * | 175 ± 11 |
| Weight, kg | 71 ± 16 * | 78 ± 14 |
| BMI, kg/m2 | 24 ± 4 | 26 ± 4 |
| History of SVT, n (%) | 0 (0.0) | 6 (2.6) |
| History of VT/VF, n (%) | 1 (2.2) | 11 (4.8) |
| History of Syncope, n (%) | 13 (28.9) | 45 (20.4) |
| Family history of SCD/ SUD, n (%) | 25 (47.2) | 134 (52.3) |
| Family history of BrS, n (%) | 31 (55.4) | 135 (51.1) |
| Genetic testing, n (%) | 35 (62.5) | 154 (58.3) |
| Likely pathogenic or pathogenic SCN5A variant, n (%) | 9 (25.7 ‡) | 18 (11.7 ‡) |
| Indication for Test | ||
| ECG suspicious for BrS, n (%) | 7 (12.5) | 56 (21.2) |
| Symptoms (Syncope, VT/VF or AF), n (%) | 6 (10.7) | 18 (6.8) |
| Family screening BrS, n (%) | 32 (57.1) | 134 (50.8) |
| Family screening SCD/ SUD, n (%) | 11 (19.6) | 56 (21.2) |
| Ajmaline administered (mg) | 72 ± 19 | 74 ± 24 |
| Percentage of maximum ajmaline target dose administered (%) | 100 ± 22 | 95 ± 28 |
| ECG Parameters | ||
| Heart rate (bpm) | 66 ± 10 | 68 ± 1 |
| PR-interval | 168 ± 30 | 168 ± 29 |
| QRS-duration (ms) | 100 ± 14 * | 105 ± 15 |
| QTc-interval (ms) | 425 ± 22 | 424 ± 28 |
| Normal QRS-axis, n (%) | 53 (94.6) | 224 (84.8) |
| Left QRS-axis, n (%) | 3 (5.4) | 23 (8.7) |
| Characteristic | Baseline | Peak | Change in Vectorcardiographic Parameters between the Baseline and Ajmaline Peak | |||
|---|---|---|---|---|---|---|
| Left Axis Deviation (n = 56) | No Left Axis Deviation (n = 264) | Left Axis Deviation (n = 56) | No Left Axis Deviation (n = 264) | Left Axis Deviation (n = 56) | No Left Axis Deviation (n = 264) | |
| QRS duration, ms | 100 ± 14 * | 105 ± 15 | 143 ± 21 * | 136 ± 20 | +43 ± 16 † | +31 ± 21 |
| Duration of q1, ms | 33 ± 4 | 33 ± 5 | 45 ± 8 * | 42 ± 8 | +12[8;18] † | +8[4;12] |
| Duration of q2, ms | 15 ± 3 | 15 ± 3 | 18 ± 6 * | 20 ± 5 | +2[–2;6] † | +6[2;8] |
| Duration of q3, ms | 10[8;12] * | 12[10;14] | 22[14;30] † | 14[10;20] | +12 ± 10 † | +5 ± 7 |
| Duration of q4, ms | 42 ± 10 | 44 ± 11 | 58 ± 16 | 57 ± 14 | +17 ± 14 | +13 ± 15 |
| Frontal axis QRS-loop, ° | 29 ± 24 | 29 ± 36 | –74[–107;3] † | 29[0;40] | –98[–128;–24] † | –6[–27;–1] |
| Spatial QRS T angle, ° | 67 ± 27 | 62 ± 34 | 122[59;147] † | 44[25;91] | 39 ± 46 † | –1 ± 43 |
| Ventricular gradient, mV.ms | 37 ± 16 | 41 ± 17 | 35 ± 13 | 38 ± 14 | –1 ± 7 | –3 ± 7 |
| Max. J-amplitude in V1-V2ic3 (µV) | 98.5[59;129] | 89[52;142] | 311[220;397] | 342[245;440] | 236 ± 185 | 246 ± 165 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
van der Ree, M.H.; Vendrik, J.; Kors, J.A.; Amin, A.S.; Wilde, A.A.M.; Tan, H.L.; Postema, P.G. Left Axis Deviation in Brugada Syndrome: Vectorcardiographic Evaluation during Ajmaline Provocation Testing Reveals Additional Depolarization Abnormalities. Int. J. Mol. Sci. 2021, 22, 484. https://doi.org/10.3390/ijms22020484
van der Ree MH, Vendrik J, Kors JA, Amin AS, Wilde AAM, Tan HL, Postema PG. Left Axis Deviation in Brugada Syndrome: Vectorcardiographic Evaluation during Ajmaline Provocation Testing Reveals Additional Depolarization Abnormalities. International Journal of Molecular Sciences. 2021; 22(2):484. https://doi.org/10.3390/ijms22020484
Chicago/Turabian Stylevan der Ree, Martijn H., Jeroen Vendrik, Jan A. Kors, Ahmad S. Amin, Arthur A. M. Wilde, Hanno L. Tan, and Pieter G. Postema. 2021. "Left Axis Deviation in Brugada Syndrome: Vectorcardiographic Evaluation during Ajmaline Provocation Testing Reveals Additional Depolarization Abnormalities" International Journal of Molecular Sciences 22, no. 2: 484. https://doi.org/10.3390/ijms22020484
APA Stylevan der Ree, M. H., Vendrik, J., Kors, J. A., Amin, A. S., Wilde, A. A. M., Tan, H. L., & Postema, P. G. (2021). Left Axis Deviation in Brugada Syndrome: Vectorcardiographic Evaluation during Ajmaline Provocation Testing Reveals Additional Depolarization Abnormalities. International Journal of Molecular Sciences, 22(2), 484. https://doi.org/10.3390/ijms22020484





