Air-Spun Silk-Based Micro-/Nanofibers and Thin Films for Drug Delivery
Abstract
:1. Introduction
2. Results and Discussion
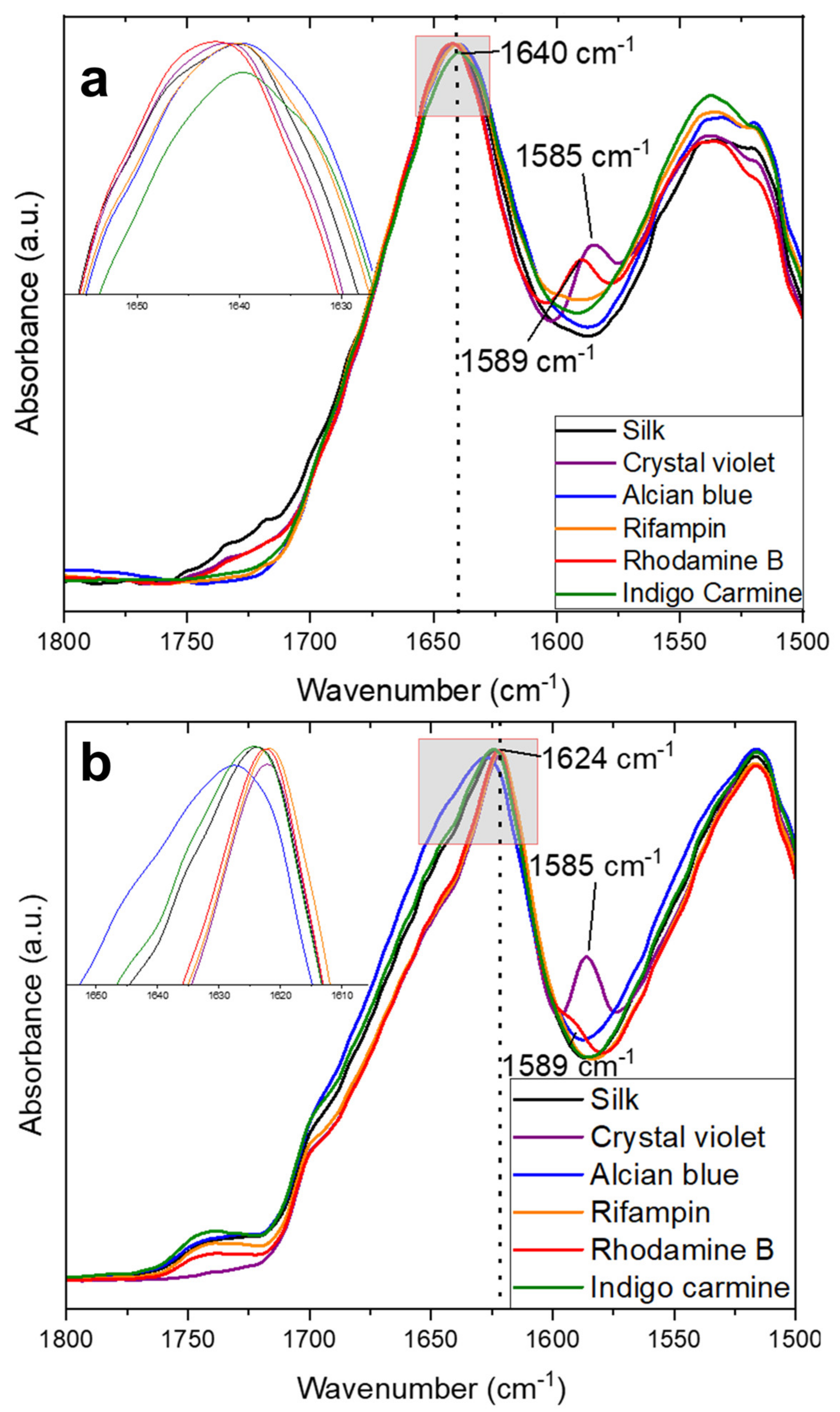
2.1. Structural Characterization
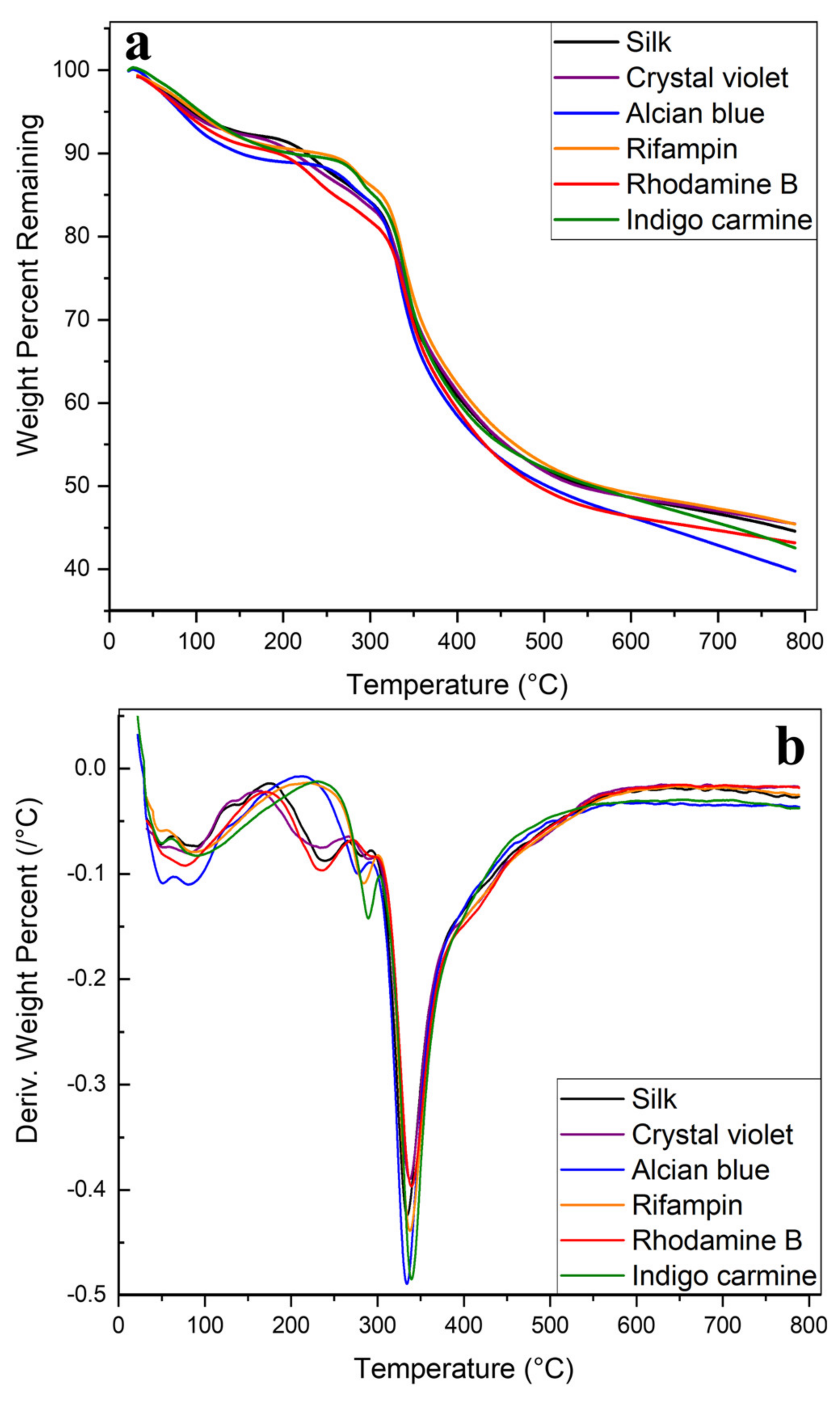
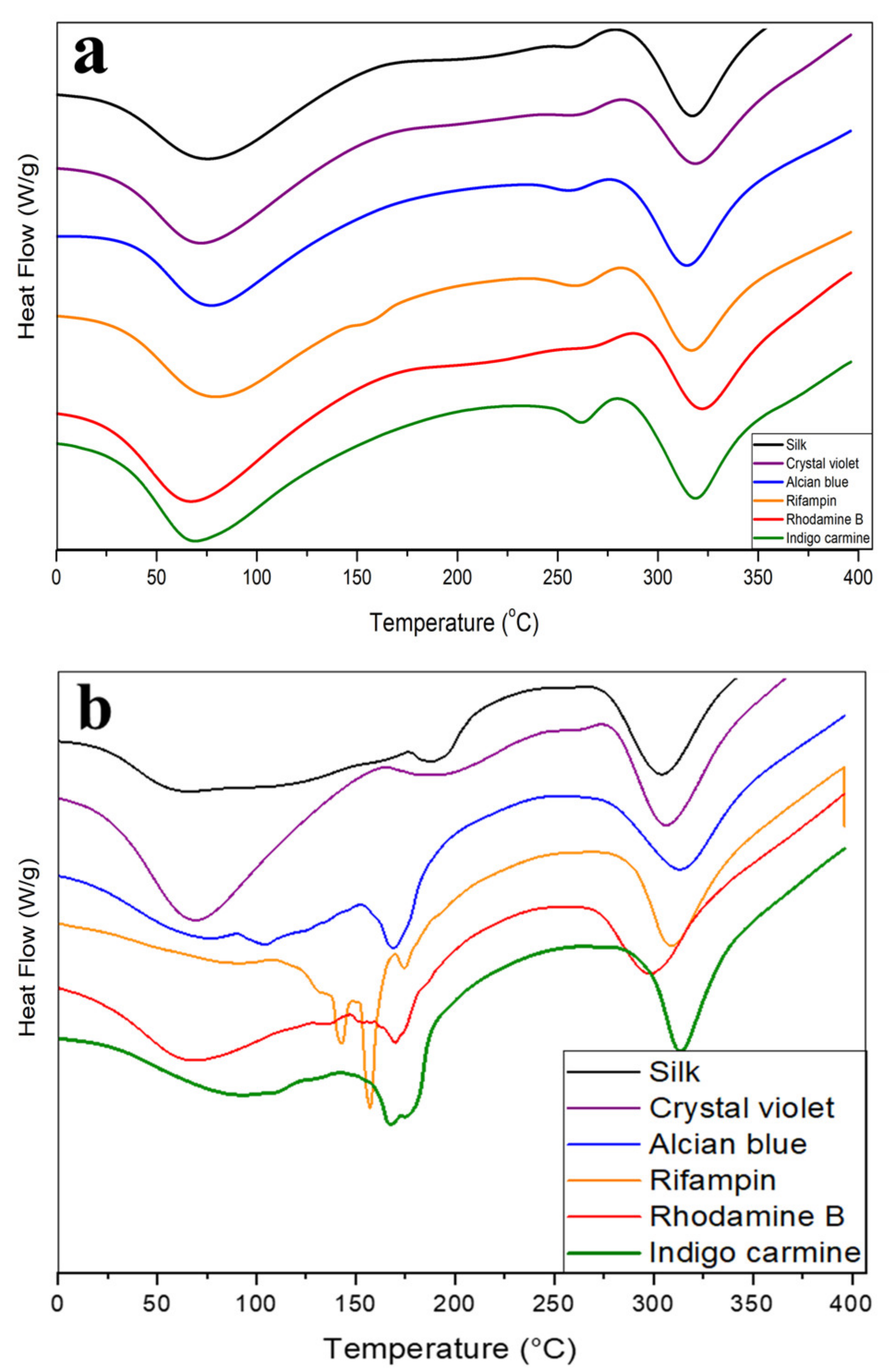
2.2. Thermal Analysis
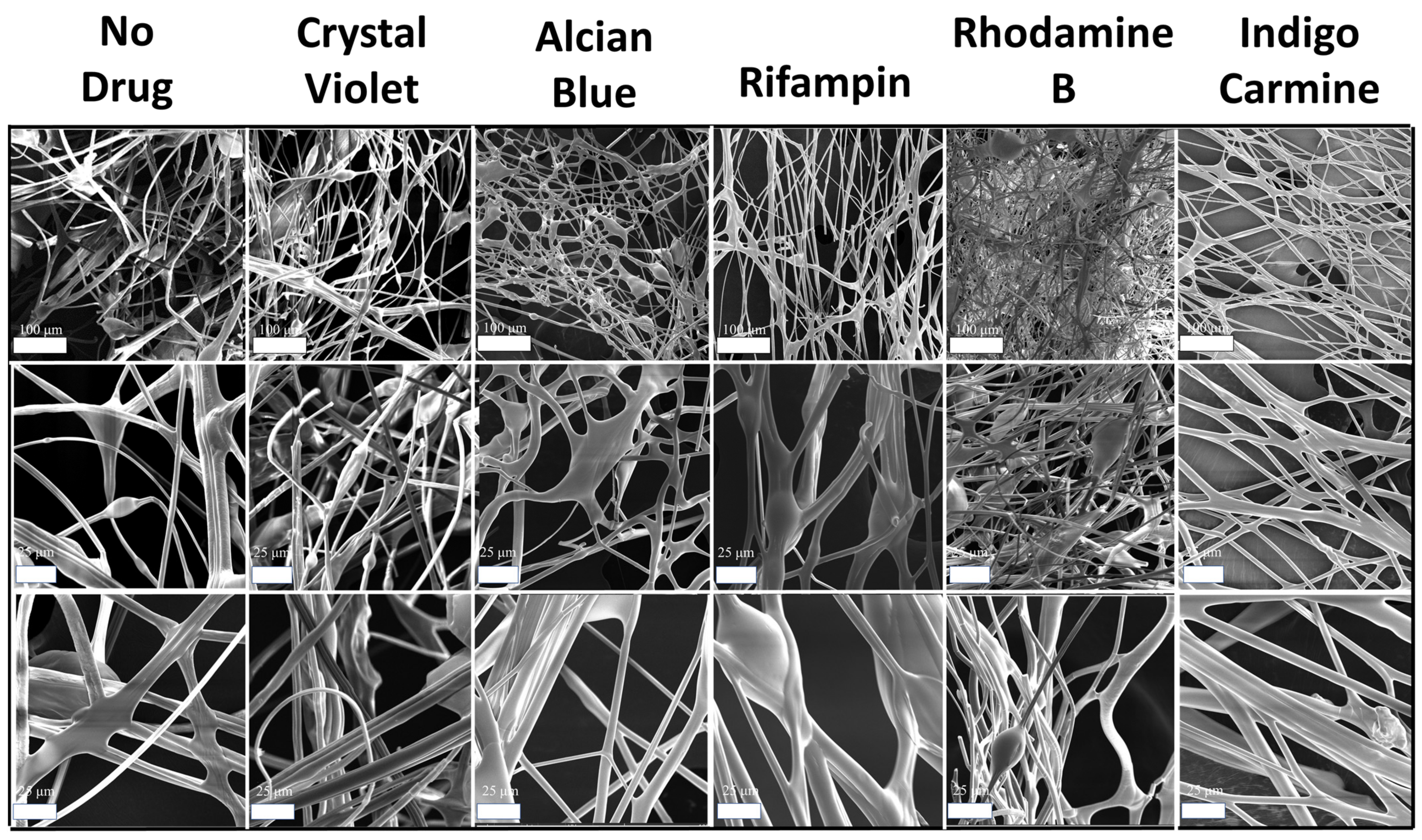
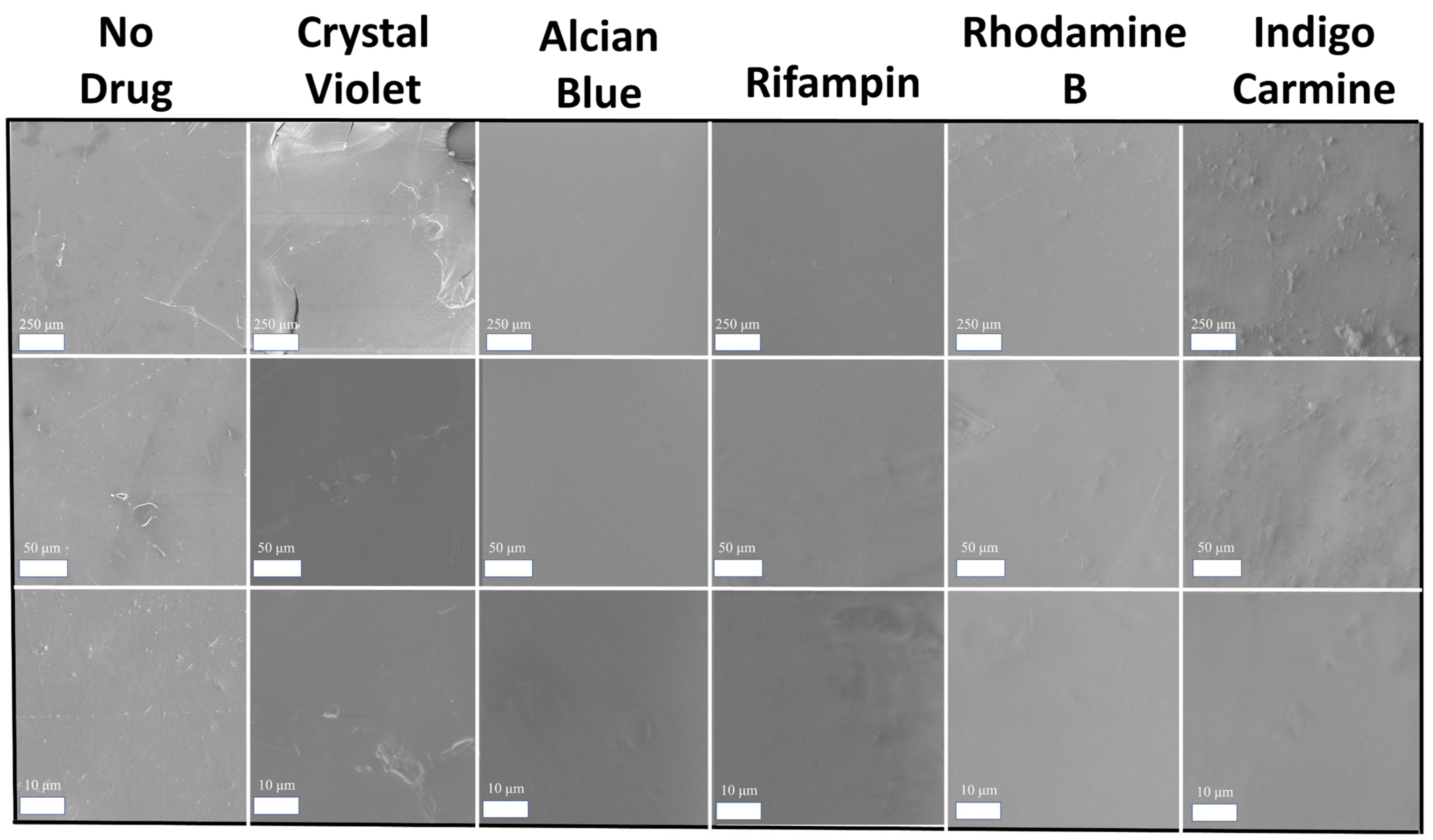
2.3. Morphology Discussion
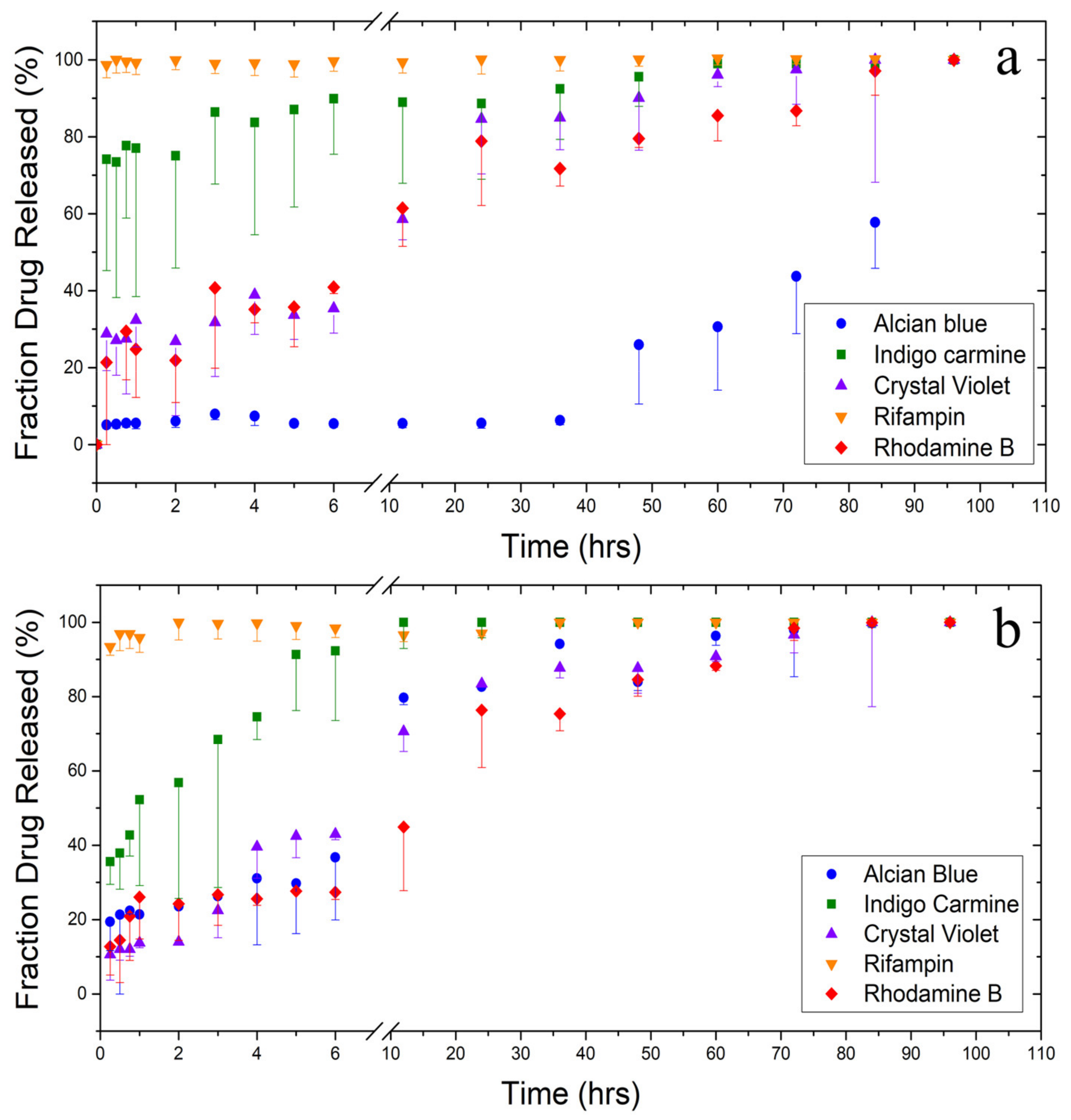
2.4. Drug Release Testing
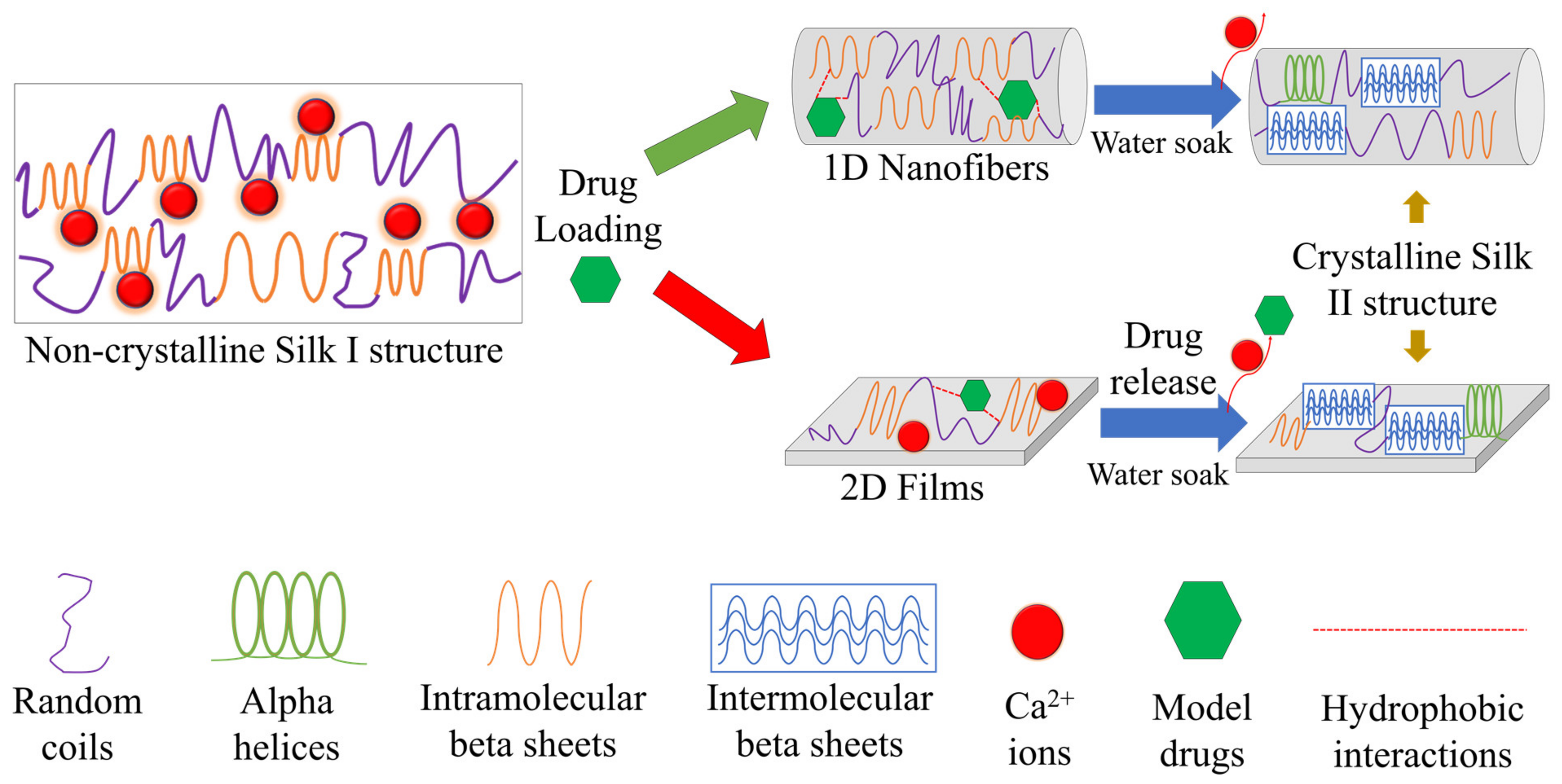
2.5. Concept of Interaction
3. Materials and Methods
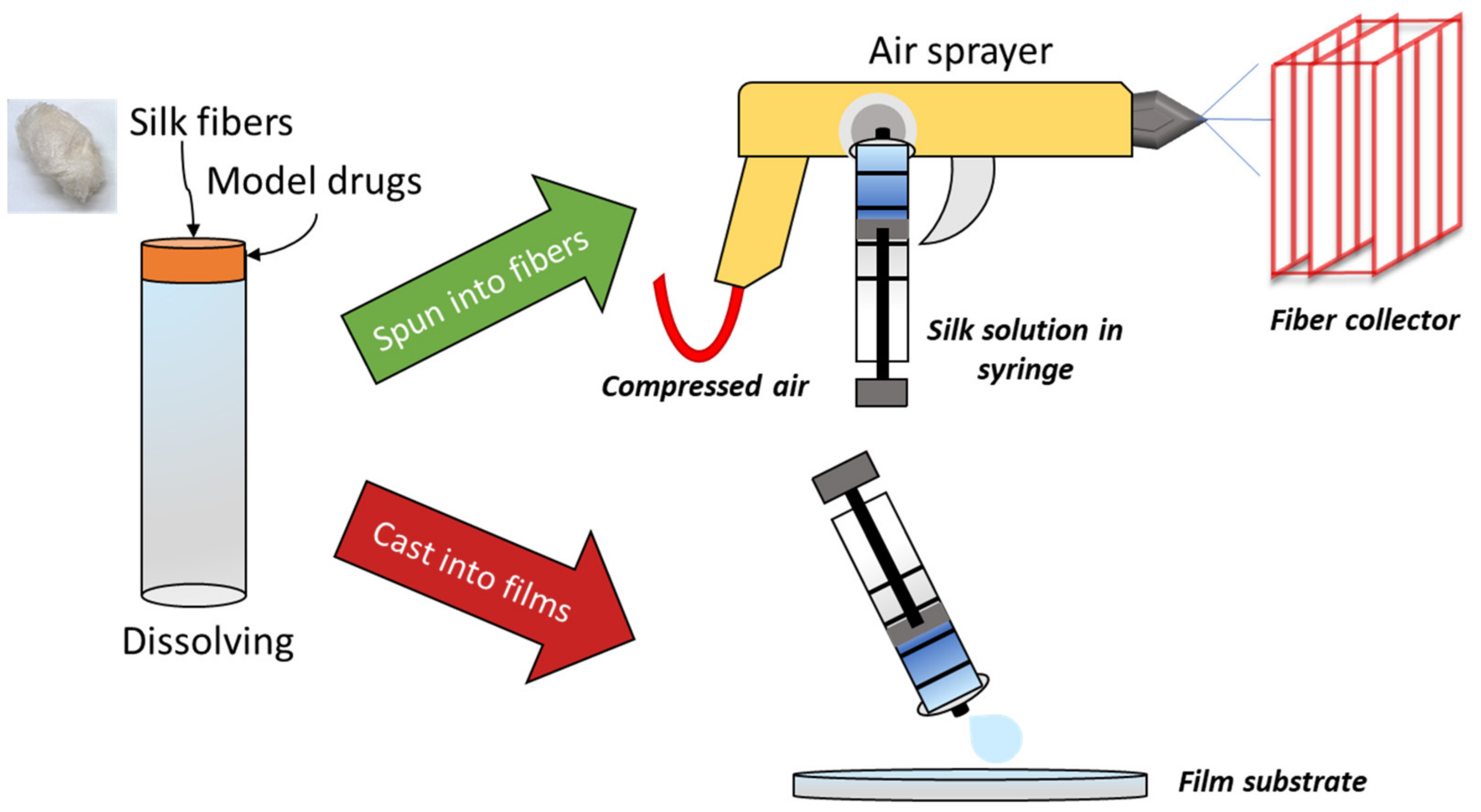
3.1. Materials Preparation
3.2. Silk Fibers
3.3. Silk Films
3.4. Morphology Characterization
3.5. Fourier Transform Infrared Spectrometry (FTIR)
3.6. Differential Scanning Calorimetry (DSC)
3.7. Thermal Gravimetric Analysis (TGA)
3.8. Drug Release Study
3.9. Statistical Analysis
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Jao, D.; Xue, Y.; Medina, J.; Hu, X. Protein-based drug-delivery materials. Materials 2017, 10, 517. [Google Scholar] [CrossRef]
- Wenk, E.; Merkle, H.P.; Meinel, L. Silk fibroin as a vehicle for drug delivery applications. J. Control. Release 2011, 150, 128–141. [Google Scholar] [CrossRef]
- Yewale, C.; Baradia, D.; Vhora, I.; Misra, A. Proteins: Emerging carrier for delivery of cancer therapeutics. Expert Opin. Drug Deliv. 2013, 10, 1429–1448. [Google Scholar] [CrossRef] [PubMed]
- Hu, X.; Liu, S.; Zhou, G.; Huang, Y.; Xie, Z.; Jing, X. Electrospinning of polymeric nanofibers for drug delivery applications. J. Control. Release 2014, 185, 12–21. [Google Scholar] [CrossRef] [PubMed]
- Paliwal, R.; Palakurthi, S. Zein in controlled drug delivery and tissue engineering. J. Control. Release 2014, 189, 108–122. [Google Scholar] [CrossRef]
- DeFrates, K.; Markiewicz, T.; Xue, Y.; Callaway, K.; Gough, C.; Moore, R.; Bessette, K.; Mou, X.; Hu, X. Air-jet spinning corn zein protein nanofibers for drug delivery: Effect of biomaterial structure and shape on release properties. Mater. Sci. Eng. C 2021, 118, 111419. [Google Scholar] [CrossRef]
- Kenawy, E.-R.; Abdel-Hay, F.I.; El-Newehy, M.H.; Wnek, G.E. Processing of polymer nanofibers through electrospinning as drug delivery systems. Mater. Chem. Phys. 2009, 113, 296–302. [Google Scholar] [CrossRef]
- Wendorff, J.H.; Agarwal, S.; Greiner, A. Medicinal Applications for Electrospun Nanofibers. Electrospinning 2012, 217–236. [Google Scholar] [CrossRef]
- Karki, S.; Kim, H.; Na, S.-J.; Shin, D.; Jo, K.; Lee, J. Thin films as an emerging platform for drug delivery. Asian J. Pharmceutical Sci. 2016, 11, 559–574. [Google Scholar] [CrossRef] [Green Version]
- Goyal, R.; Macri, L.K.; Kaplan, H.M.; Kohn, J. Nanoparticles and nanofibers for topical drug delivery. J. Control. Release 2016, 240, 77–92. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gough, C.R.; Bessette, K.; Xue, Y.; Mou, X.; Hu, X. Air-Jet Spun Corn Zein Nanofibers and Thin Films with Topical Drug for Medical Applications. Int. J. Mol. Sci. 2020, 21, 5780. [Google Scholar] [CrossRef]
- Huang, W.; Zou, T.; Li, S.; Jing, J.; Xia, X.; Liu, X. Drug-Loaded Zein Nanofibers Prepared Using a Modified Coaxial Electrospinning Process. AAPS PharmSciTech 2013, 14, 675–681. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tonglairoum, P.; Ngawhirunpat, T.; Rojanarata, T.; Kaomongkolgit, R.; Opanasopit, P. Fabrication of a novel scaffold of clotrimazole-microemulsion-containing nanofibers using an electrospinning process for oral candidiasis applications. Colloids Surf. B Biointerfaces 2015, 126, 18–25. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Dunne, F.O.; Fan, X.; Fu, X.; Zhong, W.H. A protein-functionalized microfiber/protein nanofiber Bi-layered air filter with synergistically enhanced filtration performance by a viable method. Sep. Purif. Technol. 2019, 229, 115837. [Google Scholar] [CrossRef]
- Aluigi, A.; Corbellini, A.; Rombaldoni, F.; Mazzuchetti, G. Wool-derived keratin nanofiber membranes for dynamic adsorption of heavy-metal ions from aqueous solutions. Text. Res. J. 2013, 83, 1574–1586. [Google Scholar] [CrossRef]
- Goh, Y.-F.; Shakir, I.; Hussain, R. Electrospun fibers for tissue engineering, drug delivery, and wound dressing. J. Mater. Sci. 2013, 48, 3027–3054. [Google Scholar] [CrossRef]
- Xue, Y.; Hu, X. Electrospun silk-boron nitride nanofibers with tunable structure and properties. Polymers 2020, 12, 1093. [Google Scholar] [CrossRef]
- Bambole, V.; Yakhmi, J.V. Chapter 14—Tissue engineering: Use of electrospinning technique for recreating physiological functions. In Nanobiomaterials in Soft Tissue Engineering; Grumezescu, A.M., Ed.; William Andrew Publishing: Norwich, NY, USA, 2016; pp. 387–455. [Google Scholar] [CrossRef]
- Grimmelsmann, N.; Grothe, T.; Homburg, S.V.; Ehrmann, A. Electrospinning and Stabilization of Chitosan Nanofiber MATS; Institute of Physics Publishing: Bristol, UK, 2017; Volume 254. [Google Scholar]
- Kishimoto, Y.; Morikawa, H.; Yamanaka, S.; Tamada, Y. Electrospinning of silk fibroin from all aqueous solution at low concentration. Mater. Sci. Eng. C 2017, 73, 498–506. [Google Scholar] [CrossRef]
- Shamshina, J.L.; Zavgorodnya, O.; Bonner, J.R.; Gurau, G.; Di Nardo, T.; Rogers, R.D. “Practical” Electrospinning of Biopolymers in Ionic Liquids. ChemSusChem 2017, 10, 106–111. [Google Scholar] [CrossRef]
- Zhang, F.; Lu, Q.; Yue, X.; Zuo, B.; Qin, M.; Li, F.; Kaplan, D.L.; Zhang, X. Regeneration of high-quality silk fibroin fiber by wet spinning from CaCl2–formic acid solvent. Acta Biomater. 2015, 12, 139–145. [Google Scholar] [CrossRef]
- Kolbasov, A.; Sinha-Ray, S.; Joijode, A.; Hassan, M.A.; Brown, D.; Maze, B.; Pourdeyhimi, B.; Yarin, A.L. Industrial-Scale Solution Blowing of Soy Protein Nanofibers. Ind. Eng. Chem. Res. 2016, 55, 323–333. [Google Scholar] [CrossRef]
- Sinha-Ray, S.; Sinha-Ray, S.; Yarin, A.L.; Pourdeyhimi, B. Theoretical and experimental investigation of physical mechanisms responsible for polymer nanofiber formation in solution blowing. Polymer 2015, 56, 452–463. [Google Scholar] [CrossRef]
- Xue, Y.; Jao, D.; Hu, W.; Hu, X. Silk-silk blend materials: A comparative study of Mori-Tussah, Mori-Muga, Mori-Eri, and Mori-Thai silk films. J. Therm. Anal. Calorim. 2017, 127, 915–921. [Google Scholar] [CrossRef]
- Mottaghitalab, F.; Farokhi, M.; Shokrgozar, M.A.; Atyabi, F.; Hosseinkhani, H. Silk fibroin nanoparticle as a novel drug delivery system. J. Control. Release 2015, 206, 161–176. [Google Scholar] [CrossRef]
- Magaz, A.n.; Roberts, A.D.; Faraji, S.; Nascimento, T.R.L.; Medeiros, E.S.; Zhang, W.; Greenhalgh, R.D.; Mautner, A.; Li, X.; Blaker, J.J. Porous, Aligned, and Biomimetic Fibers of Regenerated Silk Fibroin Produced by Solution Blow Spinning. Biomacromolecules 2018, 19, 4542–4553. [Google Scholar] [CrossRef] [Green Version]
- Pereira, R.F.P.; Brito-Pereira, R.; Goncalves, R.; Silva, M.P.; Costa, C.M.; Silva, M.M.; de Zea Bermudez, V.; Lanceros-Mendez, S. Silk Fibroin Separators: A Step Toward Lithium-Ion Batteries with Enhanced Sustainability. ACS Appl. Mater. Interfaces 2018, 10, 5385–5394. [Google Scholar] [CrossRef]
- Ying-ying, L.I.; Fang, W.; Qi-chun, L.I.U.; Dong-min, Z.; Xue, Z.; Qing-yu, M.A.; Zheng-gui, G.U. Research Progress in Silk Fibroin and Its Composite Materials. J. Mater. Eng. 2018, 46, 14–26. [Google Scholar] [CrossRef]
- Liu, Q.; Wang, F.; Li, Y.; Yu, H.; Gu, Z. Comparative studies of structure, thermal decomposition mechanism and thermodynamic parameters of two kinds of silk fibroin films. Sci. Sin. Chim. 2019, 49, 1014–1029. [Google Scholar] [CrossRef]
- Xue, Y.; Wang, F.; Torculas, M.; Lofland, S.; Hu, X. Formic Acid Regenerated Mori, Tussah, Eri, Thai, and Muga Silk Materials: Mechanism of Self-Assembly. ACS Biomater. Sci. Eng. 2019, 5, 6361–6373. [Google Scholar] [CrossRef]
- Jiang, F.; Liu, K.; Zhao, M.; Tao, X.; Hu, X.; Lu, S. Tunable High-Molecular-Weight Silk Fibroin Polypeptide Materials: Fabrication and Self-Assembly Mechanism. ACS Appl. Bio Mater. 2020, 3, 3248–3259. [Google Scholar] [CrossRef]
- Xia, X.-X.; Xu, Q.; Hu, X.; Qin, G.; Kaplan, D.L. Tunable Self-Assembly of Genetically Engineered Silk–Elastin-like Protein Polymers. Biomacromolecules 2011, 12, 3844–3850. [Google Scholar] [CrossRef] [Green Version]
- Wei, Q.N.; Huang, A.M.; Ma, L.; Huang, Z.; Huang, X.; Qiang, P.P.; Gong, Z.P.; Zhang, L. Structure regulation of silk fibroin films for controlled drug release. J. Appl. Polym. Sci. 2012, 125, E477–E484. [Google Scholar] [CrossRef]
- Hines, D.J.; Kaplan, D.L. Characterization of Small Molecule Controlled Release From Silk Films. Macromol. Chem. Phys. 2013, 214, 280–294. [Google Scholar] [CrossRef]
- Wang, F.; Wolf, N.; Rocks, E.-M.; Vuong, T.; Hu, X. Comparative studies of regenerated water-based Mori, Thai, Eri, Muga and Tussah silk fibroin films. J. Therm. Anal. Calorim. 2015, 122, 1069–1076. [Google Scholar] [CrossRef]
- Hu, X.; Kaplan, D.; Cebe, P. Determining Beta-Sheet Crystallinity in Fibrous Proteins by Thermal Analysis and Infrared Spectroscopy. Macromolecules 2006, 39, 6161–6170. [Google Scholar] [CrossRef]
- Goormaghtigh, E.; Cabiaux, V.; Ruysschaert, J.M. Secondary structure and dosage of soluble and membrane proteins by attenuated total reflection Fourier-transform infrared spectroscopy on hydrated films. Eur. J. Biochem. 1990, 193, 409–420. [Google Scholar] [CrossRef]
- Dong, A.; Huang, P.; Caughey, W.S. Protein secondary structures in water from second-derivative amide I infrared spectra. Biochemistry 1990, 29, 3303–3308. [Google Scholar] [CrossRef]
- Mouro, C.; Jung, C.; Bondon, A.; Simonneaux, G. Comparative Fourier transform infrared studies of the secondary structure and the CO heme ligand environment in cytochrome P-450cam and cytochrome P-420cam. Biochemistry 1997, 36, 8125–8134. [Google Scholar] [CrossRef]
- Tretinnikov, O.N.; Tamada, Y. Influence of casting temperature on the near-surface structure and wettability of cast silk fibroin films. Langmuir 2001, 17, 7406–7413. [Google Scholar] [CrossRef]
- Teramoto, H.; Miyazawa, M. Molecular orientation behavior of silk sericin film as revealed by ATR infrared spectroscopy. Biomacromolecules 2005, 6, 2049–2057. [Google Scholar] [CrossRef]
- Defrates, K.; Markiewicz, T.; Callaway, K.; Xue, Y.; Stanton, J.; Salas-de La Cruz, D.; Hu, X. Structure–property relationships of Thai silk–microcrystalline cellulose biocomposite materials fabricated from ionic liquid. Int. J. Biol. Macromol. 2017, 104, 919–928. [Google Scholar] [CrossRef]
- Díez-Pascual, A.M.; Díez-Vicente, A.L. Development of linseed oil–TiO 2 green nanocomposites as antimicrobial coatings. J. Mater. Chem. B 2015, 3, 4458–4471. [Google Scholar] [CrossRef]
- Arakawa, T.; Ejima, D.; Tsumoto, K.; Obeyama, N.; Tanaka, Y.; Kita, Y.; Timasheff, S.N. Suppression of protein interactions by arginine: A proposed mechanism of the arginine effects. Biophys. Chem. 2007, 127, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Wang, F.; Yu, H.-y.; Gu, Z.-G.; Si, L.; Liu, Q.-c.; Hu, X. Impact of calcium chloride concentration on structure and thermal property of Thai silk fibroin films. J. Therm. Anal. Calorim. 2017, 130, 851–859. [Google Scholar] [CrossRef]
- O’Neil, M.J.; Smith, A.; Heckelman, P.E.; Budavari, S. The Merck Index-An Encyclopedia of Chemicals, Drugs, and Biologicals; Merck and Co. Inc.: Whitehouse Station, NJ, USA, 2001; p. 4342. [Google Scholar]
- Nagiah, N.; Murdock, C.J.; Bhattacharjee, M.; Nair, L.; Laurencin, C.T. Development of Tripolymeric Triaxial Electrospun Fibrous Matrices for Dual Drug Delivery Applications. Sci. Rep. 2020, 10, 609. [Google Scholar] [CrossRef] [Green Version]
- Luciani-Giacobbe, L.C.; Lorenzutti, A.M.; Litterio, N.J.; Ramirez-Rigo, M.V.; Olivera, M.E. Anti-tuberculosis site-specific oral delivery system that enhances rifampicin bioavailability in a fixed-dose combination with isoniazid. Drug Deliv. Transl. Res. 2021, 11, 894–908. [Google Scholar] [CrossRef]
- Kim, S.H.; Lee, K.M.; Lee, G.S.; Seong, J.-W.; Kang, T.J. Rifampicin alleviates atopic dermatitis-like response in vivo and in vitro. Biomol. Ther. 2017, 25, 634. [Google Scholar] [CrossRef] [Green Version]
- Maley, A.M.; Arbiser, J.L. Gentian Violet: A 19th century drug re-emerges in the 21st century. Exp. Dermatol. 2013, 22, 775–780. [Google Scholar] [CrossRef] [Green Version]
- Loeffler, A.M. Uses of rifampin for infections other than tuberculosis. Pediatric Infect. Dis. J. 1999, 18, 631–632. [Google Scholar] [CrossRef] [PubMed]
- Shui, T.; Shi, C.; Jing, Z.; Yang, D.; Zhu, J. Case Report: Rifampicin-Induced Thrombocytopenia in a Patient with Borderline Lepromatous Leprosy. Am. J. Trop. Med. Hyg. 2020, 103, 1441–1442. [Google Scholar] [CrossRef] [PubMed]
- Sousa, G.; Carreiro, A.; Duarte, P. Rifampicin-induced disseminated intravascular coagulation: An antibody-mediated side effect. Pulmonology 2021, 27, 269–272. [Google Scholar] [CrossRef] [PubMed]
- Su, Q.; Kuang, W.; Hao, W.; Liang, J.; Wu, L.; Tang, C.; Wang, Y.; Liu, T. Antituberculosis Drugs (Rifampicin and Isoniazid) Induce Liver Injury by Regulating NLRP3 Inflammasomes. Mediat. Inflamm. 2021, 2021, 8086253. [Google Scholar] [CrossRef] [PubMed]



| Sample | Fiber | Film | ||
|---|---|---|---|---|
| Glass Transition Tg/°C | Major Degradation Td/°C | Glass Transition Tg/°C | Major Degradation Td/°C | |
| Pure Silk | 175 | 299 | 182 | 286 |
| Alcian Blue | N/A | 298 | N/A | 292 |
| Indigo Carmine | N/A | 302 | N/A | 302 |
| Rifampin | N/A | 301 | N/A | 297 |
| Crystal Violet | 179 | 299 | 177 | 291 |
| Rhodamine B | 183 | 306 | N/A | 283 |
| Silk with Drugs | Pearson Correlation | T-Stat | p (T ≤ t) |
|---|---|---|---|
| Alcian Blue | 0.645 | −5.781 | 0.00 |
| Indigo Carmine | 0.914 | 1.929 | 0.072 |
| Rifampin | 0.488 | 2.792 | 0.013 |
| Crystal Violet | 0.971 | 1.740 | 0.101 |
| Rhodamine B | 0.979 | 1.839 | 0.085 |
| Model Drug | Molecular Weight (g/mol) | Solubility in Water at 25 ℃ (g/L) | Log P | Melting Point (°C) |
|---|---|---|---|---|
Crystal violet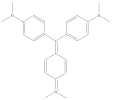 | 407.98 | 50 | 1.4 | 205 |
Indigo carmine | 466.36 | 10 | 1.01 | >300 |
Rhodamine B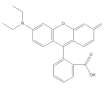 | 497.02 | 8 | 1.95 | ~210–211 |
Rifampin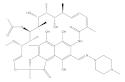 | 822.94 | 2.5 | 2.77 | ~183–188 |
Alcian blue (8gx) | 1298.9 | 1 | −9.7 | 148 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gough, C.R.; Hu, X. Air-Spun Silk-Based Micro-/Nanofibers and Thin Films for Drug Delivery. Int. J. Mol. Sci. 2021, 22, 9588. https://doi.org/10.3390/ijms22179588
Gough CR, Hu X. Air-Spun Silk-Based Micro-/Nanofibers and Thin Films for Drug Delivery. International Journal of Molecular Sciences. 2021; 22(17):9588. https://doi.org/10.3390/ijms22179588
Chicago/Turabian StyleGough, Christopher R., and Xiao Hu. 2021. "Air-Spun Silk-Based Micro-/Nanofibers and Thin Films for Drug Delivery" International Journal of Molecular Sciences 22, no. 17: 9588. https://doi.org/10.3390/ijms22179588
APA StyleGough, C. R., & Hu, X. (2021). Air-Spun Silk-Based Micro-/Nanofibers and Thin Films for Drug Delivery. International Journal of Molecular Sciences, 22(17), 9588. https://doi.org/10.3390/ijms22179588








