IGF-1 and IGFBP-3 in Inflammatory Cachexia
Abstract
1. Introduction
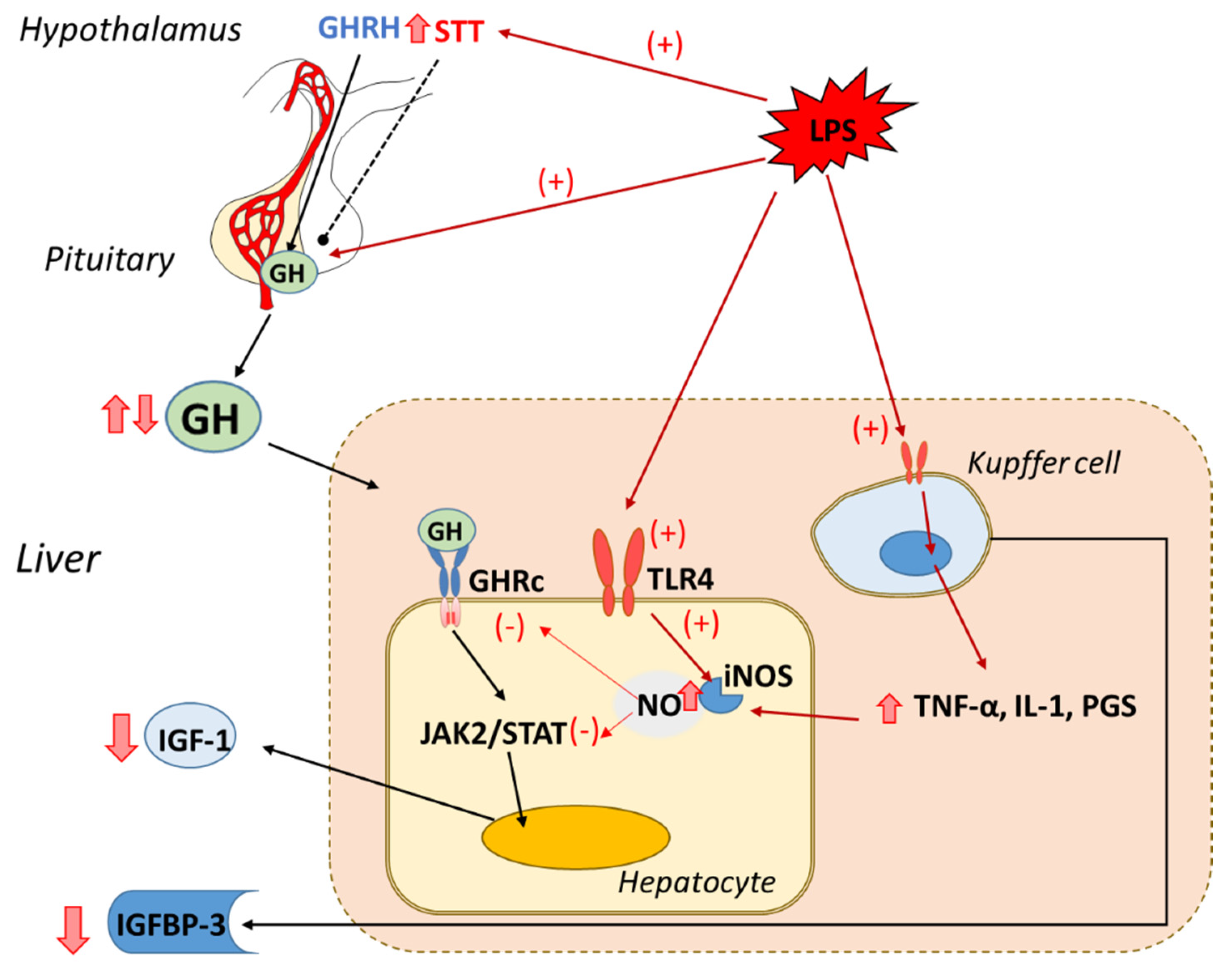
2. The Hypothalamic–GH–IGF-1 Axis in Inflammation
2.1. Inflammation Induces GH Resistance
2.2. Inflammation Modifies Circulating IGF-Binding Protein-3
2.3. Inflammation Decreases IGF-1 and IGFBP-3 Synthesis in the Liver
3. The Essential Role of Inflammation and IGF-1 on Muscle Mass
3.1. Inflammation-Induced Muscle Wasting
3.2. The Antagonistic Effects of IGF-1 and IGFBP-3 on Skeletal Muscle Mass during Inflammation
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Straub, R.H. Interaction of the endocrine system with inflammation: A function of energy and volume regulation. Arthritis Res. 2014, 16, 203. [Google Scholar] [CrossRef]
- Soto, L.; Martin, A.I.; Millan, S.; Vara, E.; Lopez-Calderon, A. Effects of endotoxin lipopolysaccharide administration on the somatotropic axis. J. Endocrinol. 1998, 159, 239–246. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Priego, T.; Granado, M.; Ibanez de Caceres, I.; Martin, A.I.; Villanua, M.A.; Lopez-Calderon, A. Endotoxin at low doses stimulates pituitary GH whereas it decreases IGF-I and IGF-binding protein-3 in rats. J. Endocrinol. 2003, 179, 107–117. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Priego, T.; de Caceres, I.I.; Martin, A.I.; Villanua, M.A.; Lopez-Calderon, A. Endotoxin administration increases hypothalamic somatostatin mRNA through nitric oxide release. Regul. Pept. 2005, 124, 113–118. [Google Scholar] [CrossRef]
- Kasting, N.W.; Martin, J.B. Altered release of growth hormone and thyrotropin induced by endotoxin in the rat. Am. J. Physiol. 1982, 243, E332–E337. [Google Scholar] [CrossRef]
- Lang, C.H.; Pollard, V.; Fan, J.; Traber, L.D.; Traber, D.L.; Frost, R.A.; Gelato, M.C.; Prough, D.S. Acute alterations in growth hormone-insulin-like growth factor axis in humans injected with endotoxin. Am. J. Physiol. 1997, 273, R371–R378. [Google Scholar] [CrossRef] [PubMed]
- Lopez-Calderon, A.; Soto, L.; Martin, A.I. Chronic inflammation inhibits GH secretion and alters the serum insulin-like growth factor system in rats. Life Sci. 1999, 65, 2049–2060. [Google Scholar] [CrossRef]
- Neidhart, M.; Fluckiger, E.W. Hyperprolactinaemia in hypophysectomized or intact male rats and the development of adjuvant arthritis. Immunology 1992, 77, 449–455. [Google Scholar]
- Cirillo, F.; Lazzeroni, P.; Catellani, C.; Sartori, C.; Amarri, S.; Street, M.E. MicroRNAs link chronic inflammation in childhood to growth impairment and insulin-resistance. Cytokine Growth Factor Rev. 2018, 39, 1–18. [Google Scholar] [CrossRef]
- Maleta, K.; Fan, Y.M.; Luoma, J.; Ashorn, U.; Bendabenda, J.; Dewey, K.G.; Hyoty, H.; Knip, M.; Kortekangas, E.; Lehto, K.M.; et al. Infections and systemic inflammation are associated with lower plasma concentration of insulin-like growth factor I among Malawian children. Am. J. Clin. Nutr. 2021, 113, 380–390. [Google Scholar] [CrossRef] [PubMed]
- Van den Berghe, G.; de Zegher, F.; Bouillon, R. Clinical review 95: Acute and prolonged critical illness as different neuroendocrine paradigms. J. Clin. Endocrinol. Metab. 1998, 83, 1827–1834. [Google Scholar] [CrossRef][Green Version]
- Faim, F.; Passaglia, P.; Batalhao, M.; Lacchini, R.; Stabile, A.M.; Carnio, E.C. Role of ghrelin on growth hormone/insulin-like growth factor-1 axis during endotoxemia. Growth Horm. IGF Res. 2019, 48–49, 36–44. [Google Scholar] [CrossRef]
- Wang, X.; Jiang, J.; Warram, J.; Baumann, G.; Gan, Y.; Menon, R.K.; Denson, L.A.; Zinn, K.R.; Frank, S.J. Endotoxin-induced proteolytic reduction in hepatic growth hormone (GH) receptor: A novel mechanism for GH insensitivity. Mol. Endocrinol. 2008, 22, 1427–1437. [Google Scholar] [CrossRef]
- Ross, R.; Miell, J.; Freeman, E.; Jones, J.; Matthews, D.; Preece, M.; Buchanan, C. Critically ill patients have high basal growth hormone levels with attenuated oscillatory activity associated with low levels of insulin-like growth factor-I. Clin. Endocrinol. 1991, 35, 47–54. [Google Scholar] [CrossRef] [PubMed]
- Xu, L.; Zhang, W.; Sun, R.; Liu, J.; Hong, J.; Li, Q.; Hu, B.; Gong, F. IGF-1 may predict the severity and outcome of patients with sepsis and be associated with microRNA-1 level changes. Exp. Ther. Med. 2017, 14, 797–804. [Google Scholar] [CrossRef] [PubMed]
- Priego, T.; de Caceres, I.I.; Martin, A.I.; Villanua, M.A.; Lopez-Calderon, A. Endotoxin decreases serum IGFBP-3 and liver IGFBP-3 mRNA: Comparison between Lewis and Wistar rats. Mol. Cell Endocrinol. 2003, 199, 23–28. [Google Scholar] [CrossRef]
- Mak, R.H.; Cheung, W.W.; Roberts, C.T., Jr. The growth hormone-insulin-like growth factor-I axis in chronic kidney disease. Growth Horm. IGF Res. 2008, 18, 17–25. [Google Scholar] [CrossRef][Green Version]
- Soendergaard, C.; Kvist, P.H.; Thygesen, P.; Reslow, M.; Nielsen, O.H.; Kopchick, J.J.; Holm, T.L. Characterization of Growth Hormone Resistance in Experimental and Ulcerative Colitis. Int. J. Mol. Sci. 2017, 18, 2046. [Google Scholar] [CrossRef]
- Yumet, G.; Shumate, M.L.; Bryant, D.P.; Lang, C.H.; Cooney, R.N. Hepatic growth hormone resistance during sepsis is associated with increased suppressors of cytokine signaling expression and impaired growth hormone signaling. Crit. Care Med. 2006, 34, 1420–1427. [Google Scholar] [CrossRef] [PubMed]
- Jeschke, M.G.; Herndon, D.N. Effect of growth factors as therapeutic drugs on hepatic metabolism during the systemic inflammatory response syndrome. Curr. Drug Metab. 2004, 5, 399–413. [Google Scholar] [CrossRef] [PubMed]
- Priego, T.; Granado, M.; Martin, A.I.; Lopez-Calderon, A.; Villanua, M.A. Dexamethasone administration attenuates the inhibitory effect of lipopolysaccharide on IGF-I and IGF-binding protein-3 in adult rats. J. Endocrinol. 2005, 185, 467–476. [Google Scholar] [CrossRef] [PubMed]
- Strous, G.J.; Almeida, A.D.S.; Putters, J.; Schantl, J.; Sedek, M.; Slotman, J.A.; Nespital, T.; Hassink, G.C.; Mol, J.A. Growth Hormone Receptor Regulation in Cancer and Chronic Diseases. Front. Endocrinol. 2020, 11, 597573. [Google Scholar] [CrossRef] [PubMed]
- Linossi, E.M.; Nicholson, S.E. Kinase inhibition, competitive binding and proteasomal degradation: Resolving the molecular function of the suppressor of cytokine signaling (SOCS) proteins. Immunol. Rev. 2015, 266, 123–133. [Google Scholar] [CrossRef] [PubMed]
- Cavaillon, J.M. Exotoxins and endotoxins: Inducers of inflammatory cytokines. Toxicon 2018, 149, 45–53. [Google Scholar] [CrossRef]
- Cooney, R.N.; Shumate, M. The inhibitory effects of interleukin-1 on growth hormone action during catabolic illness. Vitam. Horm. 2006, 74, 317–340. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Xiao, X.; Frank, S.J.; Lin, H.Y.; Xia, Y. Distinct mechanisms of induction of hepatic growth hormone resistance by endogenous IL-6, TNF-alpha, and IL-1beta. Am. J. Physiol. Endocrinol. Metab. 2014, 307, E186–E198. [Google Scholar] [CrossRef]
- Hawkes, C.P.; Grimberg, A. Insulin-Like Growth Factor-I is a Marker for the Nutritional State. Pediatric Endocrinol. Rev. 2015, 13, 499–511. [Google Scholar] [PubMed]
- Granado, M.; Martin, A.I.; Lopez-Menduina, M.; Lopez-Calderon, A.; Villanua, M.A. GH-releasing peptide-2 administration prevents liver inflammatory response in endotoxemia. Am. J. Physiol. Endocrinol. Metab. 2008, 294, E131–E141. [Google Scholar] [CrossRef]
- Xu, J.; Zhu, C.; Zhang, M.; Tong, Q.; Wan, X.; Liao, Z.; Cai, X.; Xu, Y.; Yuan, Y.; Wang, L.; et al. Arginine reverses growth hormone resistance through the inhibition of toll-like receptor 4-mediated inflammatory pathway. Metabolism 2018, 79, 10–23. [Google Scholar] [CrossRef]
- Wong, S.C.; Dobie, R.; Altowati, M.A.; Werther, G.A.; Farquharson, C.; Ahmed, S.F. Growth and the Growth Hormone-Insulin Like Growth Factor 1 Axis in Children with Chronic Inflammation: Current Evidence, Gaps in Knowledge, and Future Directions. Endocr. Rev. 2016, 37, 62–110. [Google Scholar] [CrossRef]
- Bechtold, S.; Ripperger, P.; Pozza, R.D.; Bonfig, W.; Hafner, R.; Michels, H.; Schwarz, H.P. Growth hormone increases final height in patients with juvenile idiopathic arthritis: Data from a randomized controlled study. J. Clin. Endocrinol. Metab. 2007, 92, 3013–3018. [Google Scholar] [CrossRef] [PubMed]
- De Caceres, I.I.; Villanua, M.A.; Soto, L.; Martin, A.I.; Lopez-Calderon, A. IGF-I and IGF-I-binding proteins in rats with adjuvant-induced arthritis given recombinant human growth hormone. J. Endocrinol. 2000, 165, 537–544. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Allard, J.B.; Duan, C. IGF-Binding Proteins: Why Do They Exist and Why Are There So Many? Front. Endocrinol. 2018, 9, 117. [Google Scholar] [CrossRef] [PubMed]
- Varma Shrivastav, S.; Bhardwaj, A.; Pathak, K.A.; Shrivastav, A. Insulin-Like Growth Factor Binding Protein-3 (IGFBP-3): Unraveling the Role in Mediating IGF-Independent Effects within the Cell. Front. Cell Dev. Biol. 2020, 8, 286. [Google Scholar] [CrossRef] [PubMed]
- Papastathi, C.; Mavrommatis, A.; Mentzelopoulos, S.; Konstandelou, E.; Alevizaki, M.; Zakynthinos, S. Insulin-like Growth Factor I and its binding protein 3 in sepsis. Growth Horm. IGF Res. 2013, 23, 98–104. [Google Scholar] [CrossRef]
- Ahasic, A.M.; Tejera, P.; Wei, Y.; Su, L.; Mantzoros, C.S.; Bajwa, E.K.; Thompson, B.T.; Christiani, D.C. Predictors of Circulating Insulin-Like Growth Factor-1 and Insulin-Like Growth Factor-Binding Protein-3 in Critical Illness. Crit. Care Med. 2015, 43, 2651–2659. [Google Scholar] [CrossRef] [PubMed]
- DeBoer, M.D.; Scharf, R.J.; Leite, A.M.; Ferrer, A.; Havt, A.; Pinkerton, R.; Lima, A.A.; Guerrant, R.L. Systemic inflammation, growth factors, and linear growth in the setting of infection and malnutrition. Nutrition 2017, 33, 248–253. [Google Scholar] [CrossRef] [PubMed]
- Gupta, N.; Lustig, R.H.; Kohn, M.A.; McCracken, M.; Vittinghoff, E. Sex differences in statural growth impairment in Crohn’s disease: Role of IGF-1. Inflamm. Bowel Dis. 2011, 17, 2318–2325. [Google Scholar] [CrossRef] [PubMed]
- Sheng, X.; Sun, X.; Li, F.; Wang, J.; Ma, J. Linear growth failure induced by systemic inflammation inhibiting IGF-1/IGFBP axis in rats with asymptomatic colitis. BMC Gastroenterol. 2019, 19, 96. [Google Scholar] [CrossRef] [PubMed]
- Zelazowska-Rutkowska, B.; Trusiak, M.; Bossowski, A.; Cylwik, B. Diagnostic Usefulness of Insulin-Like Growth Factor 1 and Insulin-Like Growth Factor Binding Protein 3 in Children with Suspected Pituitary Dwarfism. Clin. Lab. 2018, 64, 759–765. [Google Scholar] [CrossRef]
- Bang, P.; Thorell, A.; Carlsson-Skwirut, C.; Ljungqvist, O.; Brismar, K.; Nygren, J. Free dissociable IGF-I: Association with changes in IGFBP-3 proteolysis and insulin sensitivity after surgery. Clin. Nutr. 2016, 35, 408–413. [Google Scholar] [CrossRef]
- Frost, V.J.; Macaulay, V.M.; Wass, J.A.; Holly, J.M. Proteolytic modification of insulin-like growth factor-binding proteins: Comparison of conditioned media from human cell lines, circulating proteases and characterized enzymes. J. Endocrinol. 1993, 138, 545–554. [Google Scholar] [CrossRef] [PubMed]
- Skjaerbaek, C.; Frystyk, J.; Orskov, H.; Kissmeyer-Nielsen, P.; Jensen, M.B.; Laurberg, S.; Moller, N.; Flyvbjerg, A. Differential changes in free and total insulin-like growth factor I after major, elective abdominal surgery: The possible role of insulin-like growth factor-binding protein-3 proteolysis. J. Clin. Endocrinol. Metab. 1998, 83, 2445–2449. [Google Scholar] [CrossRef][Green Version]
- Priego, T.; Granado, M.; Castillero, E.; Martin, A.I.; Villanua, M.A.; Lopez-Calderon, A. Nitric oxide production by hepatocytes contributes to the inhibitory effect of endotoxin on insulin-like growth factor I gene expression. J. Endocrinol. 2006, 190, 847–856. [Google Scholar] [CrossRef] [PubMed]
- Thissen, J.P.; Verniers, J. Inhibition by interleukin-1 beta and tumor necrosis factor-alpha of the insulin-like growth factor I messenger ribonucleic acid response to growth hormone in rat hepatocyte primary culture. Endocrinology 1997, 138, 1078–1084. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Gallo, D.J.; Green, A.M.; Williams, D.L.; Gong, X.; Shapiro, R.A.; Gambotto, A.A.; Humphris, E.L.; Vodovotz, Y.; Billiar, T.R. Role of toll-like receptors in changes in gene expression and NF-kappa B activation in mouse hepatocytes stimulated with lipopolysaccharide. Infect. Immun. 2002, 70, 3433–3442. [Google Scholar] [CrossRef] [PubMed]
- Priego, T.; de Caceres, I.I.; Martin, A.I.; Villanua, M.A.; Lopez-Calderon, A. NO plays a role in LPS-induced decreases in circulating IGF-I and IGFBP-3 and their gene expression in the liver. Am. J. Physiol. Endocrinol. Metab. 2004, 286, E50–E56. [Google Scholar] [CrossRef]
- Granado, M.; Martin, A.I.; Priego, T.; Villanua, M.A.; Lopez-Calderon, A. Inactivation of Kupffer cells by gadolinium administration prevents lipopolysaccharide-induced decrease in liver insulin-like growth factor-I and IGF-binding protein-3 gene expression. J. Endocrinol. 2006, 188, 503–511. [Google Scholar] [CrossRef] [PubMed]
- Arany, E.; Afford, S.; Strain, A.J.; Winwood, P.J.; Arthur, M.J.; Hill, D.J. Differential cellular synthesis of insulin-like growth factor binding protein-1 (IGFBP-1) and IGFBP-3 within human liver. J. Clin. Endocrinol. Metab. 1994, 79, 1871–1876. [Google Scholar] [CrossRef] [PubMed]
- Lelbach, A.; Scharf, J.G.; Ramadori, G. Regulation of insulin-like growth factor-I and of insulin-like growth factor binding protein-1, -3 and -4 in cocultures of rat hepatocytes and Kupffer cells by interleukin-6. J. Hepatol. 2001, 35, 558–567. [Google Scholar] [CrossRef]
- Murton, A.; Bohanon, F.J.; Ogunbileje, J.O.; Capek, K.D.; Tran, E.A.; Chao, T.; Sidossis, L.S.; Porter, C.; Herndon, D.N. Sepsis Increases Muscle Proteolysis in Severely Burned Adults, but Does not Impact Whole-Body Lipid or Carbohydrate Kinetics. Shock 2019, 52, 353–361. [Google Scholar] [CrossRef]
- Poulsen, J.B.; Moller, K.; Jensen, C.V.; Weisdorf, S.; Kehlet, H.; Perner, A. Effect of transcutaneous electrical muscle stimulation on muscle volume in patients with septic shock. Crit. Care Med. 2011, 39, 456–461. [Google Scholar] [CrossRef] [PubMed]
- Schefold, J.C.; Wollersheim, T.; Grunow, J.J.; Luedi, M.M.; Z’Graggen, W.J.; Weber-Carstens, S. Muscular weakness and muscle wasting in the critically ill. J. Cachexia Sarcopenia Muscle 2020, 11, 1399–1412. [Google Scholar] [CrossRef]
- Buhl, M.; Bosnjak, E.; Vendelbo, M.H.; Gjedsted, J.; Nielsen, R.R.; Hafstrøm, T.K.; Vestergaard, E.T.; Jessen, N.; Tonnesen, E.; Moller, A.B.; et al. Direct effects of locally administered lipopolysaccharide on glucose, lipid, and protein metabolism in the placebo-controlled, bilaterally infused human leg. J. Clin. Endocrinol. Metab. 2013, 98, 2090–2099. [Google Scholar] [CrossRef] [PubMed]
- Stana, F.; Vujovic, M.; Mayaki, D.; Leduc-Gaudet, J.P.; Leblanc, P.; Huck, L.; Hussain, S.N.A. Differential Regulation of the Autophagy and Proteasome Pathways in Skeletal Muscles in Sepsis. Crit. Care Med. 2017, 45, e971–e979. [Google Scholar] [CrossRef]
- Gómez-SanMiguel, A.B.; Gomez-Moreira, C.; Nieto-Bona, M.P.; Fernández-Galaz, C.; Villanúa, M.Á.; Martín, A.I.; López-Calderón, A. Formoterol decreases muscle wasting as well as inflammation in the rat model of rheumatoid arthritis. Am. J. Physiol. -Endocrinol. Metab. 2016, 310, E925–E937. [Google Scholar] [CrossRef] [PubMed]
- Gomez-SanMiguel, A.B.; Villanua, M.A.; Martin, A.I.; Lopez-Calderon, A. D-TRP(8)-gammaMSH Prevents the Effects of Endotoxin in Rat Skeletal Muscle Cells through TNFalpha/NF-KB Signalling Pathway. PLoS ONE 2016, 11, e0155645. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Rittig, N.; Bach, E.; Thomsen, H.H.; Johannsen, M.; Jorgensen, J.O.; Richelsen, B.; Jessen, N.; Moller, N. Amino acid supplementation is anabolic during the acute phase of endotoxin-induced inflammation: A human randomized crossover trial. Clin. Nutr. 2016, 35, 322–330. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, S.S.; Ahmad, K.; Lee, E.J.; Lee, Y.H.; Choi, I. Implications of Insulin-Like Growth Factor-1 in Skeletal Muscle and Various Diseases. Cells 2020, 9, 1773. [Google Scholar] [CrossRef] [PubMed]
- Martin, A.I.; Priego, T.; Lopez-Calderon, A. Hormones and Muscle Atrophy. Adv. Exp. Med. Biol. 2018, 1088, 207–233. [Google Scholar] [CrossRef]
- Yoshida, T.; Delafontaine, P. Mechanisms of IGF-1-Mediated Regulation of Skeletal Muscle Hypertrophy and Atrophy. Cells 2020, 9, 1970. [Google Scholar] [CrossRef]
- Lopez-Menduina, M.; Martin, A.I.; Castillero, E.; Villanua, M.A.; Lopez-Calderon, A. Systemic IGF-I administration attenuates the inhibitory effect of chronic arthritis on gastrocnemius mass and decreases atrogin-1 and IGFBP-3. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2010, 299, R541–R551. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Yakar, S.; Liu, J.L.; Stannard, B.; Butler, A.; Accili, D.; Sauer, B.; LeRoith, D. Normal growth and development in the absence of hepatic insulin-like growth factor I. Proc. Natl. Acad. Sci. USA 1999, 96, 7324–7329. [Google Scholar] [CrossRef]
- Yakar, S.; Werner, H.; Rosen, C.J. Insulin-like growth factors: Actions on the skeleton. J. Mol. Endocrinol. 2018, 61, T115–T137. [Google Scholar] [CrossRef]
- Lang, C.H.; Frost, R.A.; Jefferson, L.S.; Kimball, S.R.; Vary, T.C. Endotoxin-induced decrease in muscle protein synthesis is associated with changes in eIF2B, eIF4E, and IGF-I. Am. J. Physiol. Endocrinol. Metab. 2000, 278, E1133–E1143. [Google Scholar] [CrossRef] [PubMed]
- Martin, A.I.; Gomez-SanMiguel, A.B.; Priego, T.; Lopez-Calderon, A. Formoterol treatment prevents the effects of endotoxin on muscle TNF/NF-kB, Akt/mTOR, and proteolytic pathways in a rat model. Role of IGF-I and miRNA 29b. Am. J. Physiol. Endocrinol. Metab. 2018, 315, E705–E714. [Google Scholar] [CrossRef]
- Nystrom, G.; Pruznak, A.; Huber, D.; Frost, R.A.; Lang, C.H. Local insulin-like growth factor I prevents sepsis-induced muscle atrophy. Metabolism 2009, 58, 787–797. [Google Scholar] [CrossRef] [PubMed]
- Castillero, E.; Martin, A.I.; Lopez-Menduina, M.; Granado, M.; Villanua, M.A.; Lopez-Calderon, A. IGF-I system, atrogenes and myogenic regulatory factors in arthritis induced muscle wasting. Mol. Cell Endocrinol. 2009, 309, 8–16. [Google Scholar] [CrossRef]
- Martin, A.I.; Gomez-SanMiguel, A.B.; Gomez-Moreira, C.; Villanua, M.A.; Lopez-Calderon, A. alphaMSH blunts endotoxin-induced MuRF1 and atrogin-1 upregulation in skeletal muscle by modulating NF-kappaB and Akt/FoxO1 pathway. Mediat. Inflamm. 2014, 2014, 179368. [Google Scholar] [CrossRef]
- Blum, W.F.; Albertsson-Wikland, K.; Rosberg, S.; Ranke, M.B. Serum levels of insulin-like growth factor I (IGF-I) and IGF binding protein 3 reflect spontaneous growth hormone secretion. J. Clin. Endocrinol. Metab. 1993, 76, 1610–1616. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Frankel, W.L.; Adamson, W.T.; Roth, J.A.; Mantell, M.P.; Bain, A.; Ziegler, T.R.; Smith, R.J.; Rombeau, J.L. Insulin-like growth factor-I improves mucosal structure and function in transplanted rat small intestine. Transplantation 1995, 59, 755–761. [Google Scholar] [CrossRef] [PubMed]
- Lopez-Menduina, M.; Martin, A.I.; Castillero, E.; Villanua, M.A.; Lopez-Calderon, A. Short-term growth hormone or IGF-I administration improves the IGF-IGFBP system in arthritic rats. Growth Horm. IGF Res. 2012, 22, 22–29. [Google Scholar] [CrossRef] [PubMed]
- Oufattole, M.; Lin, S.W.; Liu, B.; Mascarenhas, D.; Cohen, P.; Rodgers, B.D. Ribonucleic acid polymerase II binding subunit 3 (Rpb3), a potential nuclear target of insulin-like growth factor binding protein-3. Endocrinology 2006, 147, 2138–2146. [Google Scholar] [CrossRef] [PubMed]
- Poreba, E.; Durzynska, J. Nuclear localization and actions of the insulin-like growth factor 1 (IGF-1) system components: Transcriptional regulation and DNA damage response. Mutat. Res. 2020, 784, 108307. [Google Scholar] [CrossRef] [PubMed]
- Huang, X.Y.; Huang, Z.L.; Yang, J.H.; Xu, Y.H.; Sun, J.S.; Zheng, Q.; Wei, C.; Song, W.; Yuan, Z. Pancreatic cancer cell-derived IGFBP-3 contributes to muscle wasting. J. Exp. Clin. Cancer Res. 2016, 35, 46. [Google Scholar] [CrossRef] [PubMed]
- Pampusch, M.S.; Kamanga-Sollo, E.; White, M.E.; Hathaway, M.R.; Dayton, W.R. Effect of recombinant porcine IGF-binding protein-3 on proliferation of embryonic porcine myogenic cell cultures in the presence and absence of IGF-I. J. Endocrinol. 2003, 176, 227–235. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kamanga-Sollo, E.; Pampusch, M.S.; White, M.E.; Hathaway, M.R.; Dayton, W.R. Insulin-like growth factor binding protein (IGFBP)-3 and IGFBP-5 mediate TGF-beta- and myostatin-induced suppression of proliferation in porcine embryonic myogenic cell cultures. Exp. Cell Res. 2005, 311, 167–176. [Google Scholar] [CrossRef]
- Jogie-Brahim, S.; Feldman, D.; Oh, Y. Unraveling insulin-like growth factor binding protein-3 actions in human disease. Endocr. Rev. 2009, 30, 417–437. [Google Scholar] [CrossRef]
- Dodson, S.; Baracos, V.E.; Jatoi, A.; Evans, W.J.; Cella, D.; Dalton, J.T.; Steiner, M.S. Muscle wasting in cancer cachexia: Clinical implications, diagnosis, and emerging treatment strategies. Annu. Rev. Med. 2011, 62, 265–279. [Google Scholar] [CrossRef]

| Reference | Inflammatory Stimuli | Specie/Cell Culture | Pituitary GH Secretion (↑/↓) |
|---|---|---|---|
| [3] | Low LPS doses (5, 10, 50 and 100 µg/kg, i.p.) | Rodents | ↑ |
| [2,3,12,13] | High LPS doses (100, 250, 500 and 1000 microg/kg, i.p.) | Rodents | ↓ |
| [6] | LPS (4 ng/kg, i.v.) | Humans | ↑ |
| [3] | LPS (0.1 and 10 ng/mL) | Pituitary cell culture (rodents) | ↑ |
| [2,7,8] | Experimental arthritis | Rodents | ↓ |
| [9,10] | Cystic fibrosis, inflammatory bowel disease | Humans | ↓ |
| [11] | Critical ill patients: | Humans | |
| acute phase | ↑ | ||
| chronic phase | ↓ |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Martín, A.I.; Priego, T.; Moreno-Ruperez, Á.; González-Hedström, D.; Granado, M.; López-Calderón, A. IGF-1 and IGFBP-3 in Inflammatory Cachexia. Int. J. Mol. Sci. 2021, 22, 9469. https://doi.org/10.3390/ijms22179469
Martín AI, Priego T, Moreno-Ruperez Á, González-Hedström D, Granado M, López-Calderón A. IGF-1 and IGFBP-3 in Inflammatory Cachexia. International Journal of Molecular Sciences. 2021; 22(17):9469. https://doi.org/10.3390/ijms22179469
Chicago/Turabian StyleMartín, Ana Isabel, Teresa Priego, Álvaro Moreno-Ruperez, Daniel González-Hedström, Miriam Granado, and Asunción López-Calderón. 2021. "IGF-1 and IGFBP-3 in Inflammatory Cachexia" International Journal of Molecular Sciences 22, no. 17: 9469. https://doi.org/10.3390/ijms22179469
APA StyleMartín, A. I., Priego, T., Moreno-Ruperez, Á., González-Hedström, D., Granado, M., & López-Calderón, A. (2021). IGF-1 and IGFBP-3 in Inflammatory Cachexia. International Journal of Molecular Sciences, 22(17), 9469. https://doi.org/10.3390/ijms22179469








