The Second-Generation PIM Kinase Inhibitor TP-3654 Resensitizes ABCG2-Overexpressing Multidrug-Resistant Cancer Cells to Cytotoxic Anticancer Drugs
Abstract
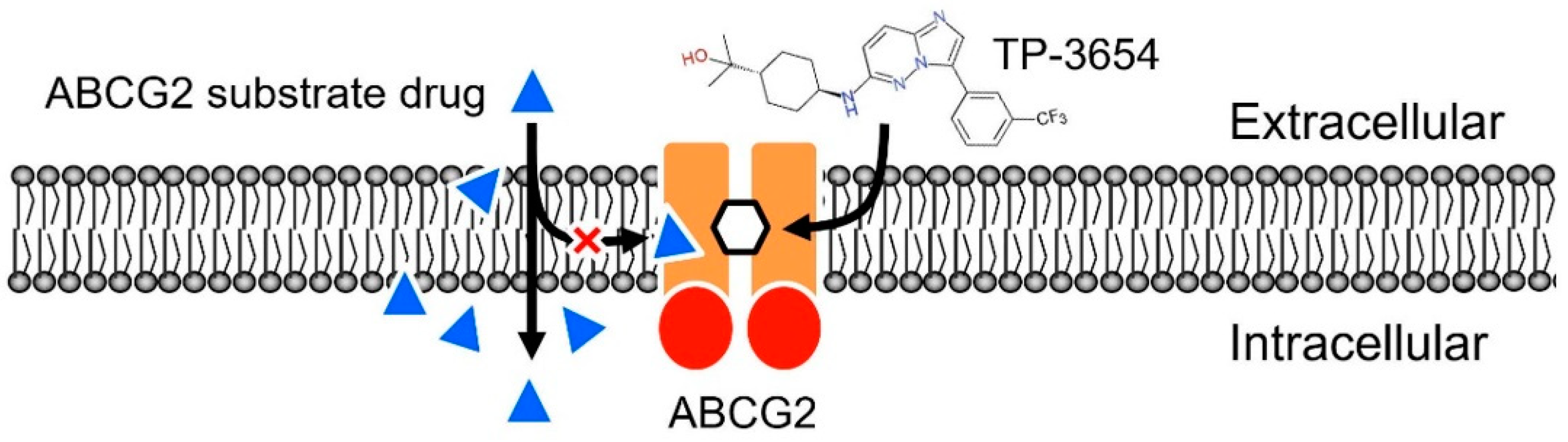
:1. Introduction
2. Results
2.1. TP-3654 Is Equally Cytotoxic to ABCB1- and ABCG2-Overexpressing Multidrug-Resistant Cancer Cells as to Drug-Sensitive Cancer Cells
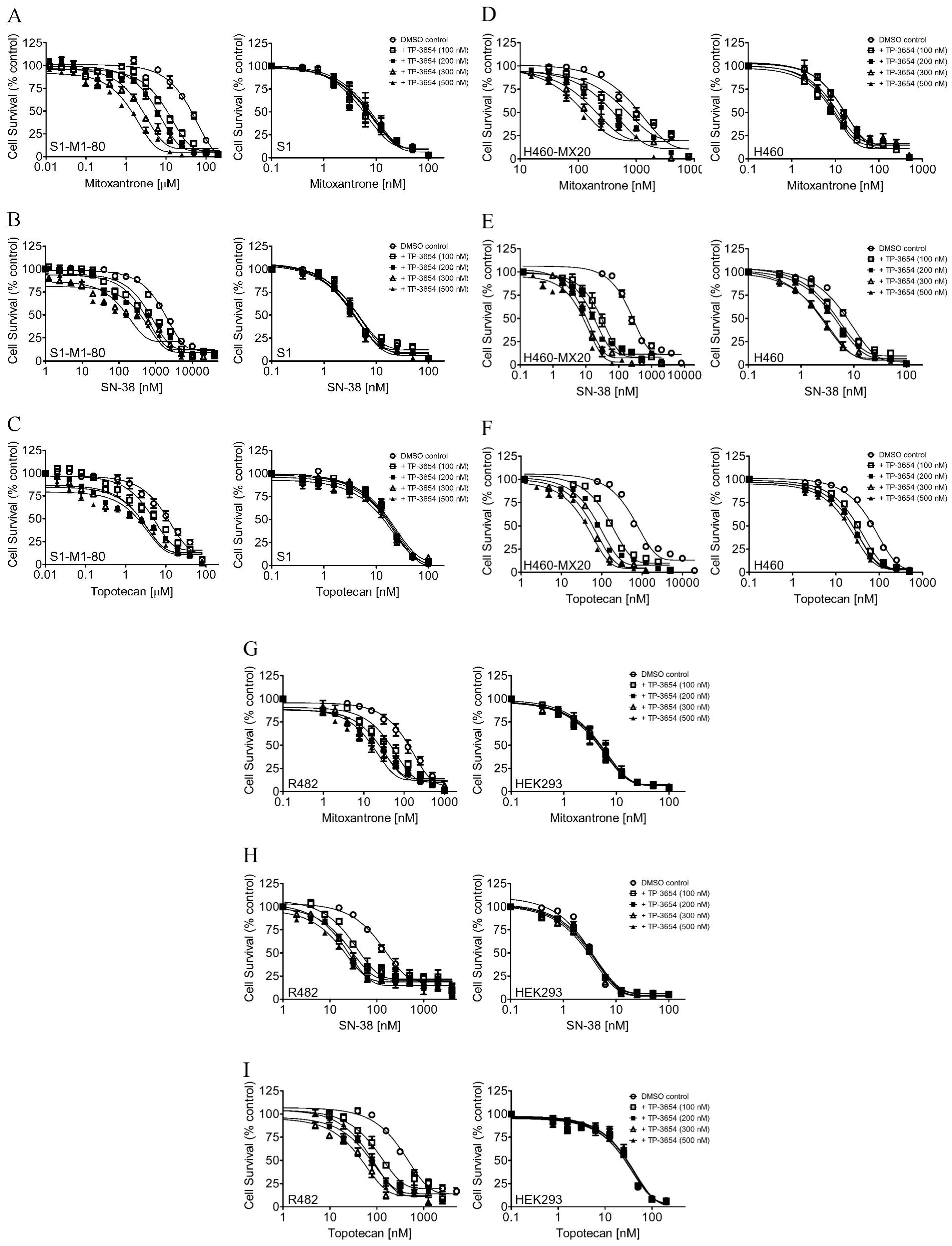
2.2. TP-3654 Selectively Reverses Multidrug Resistance in ABCG2-Overexpressing Cancer Cells
2.3. TP-3654 Selectively Inhibits the Drug Efflux Function of ABCG2
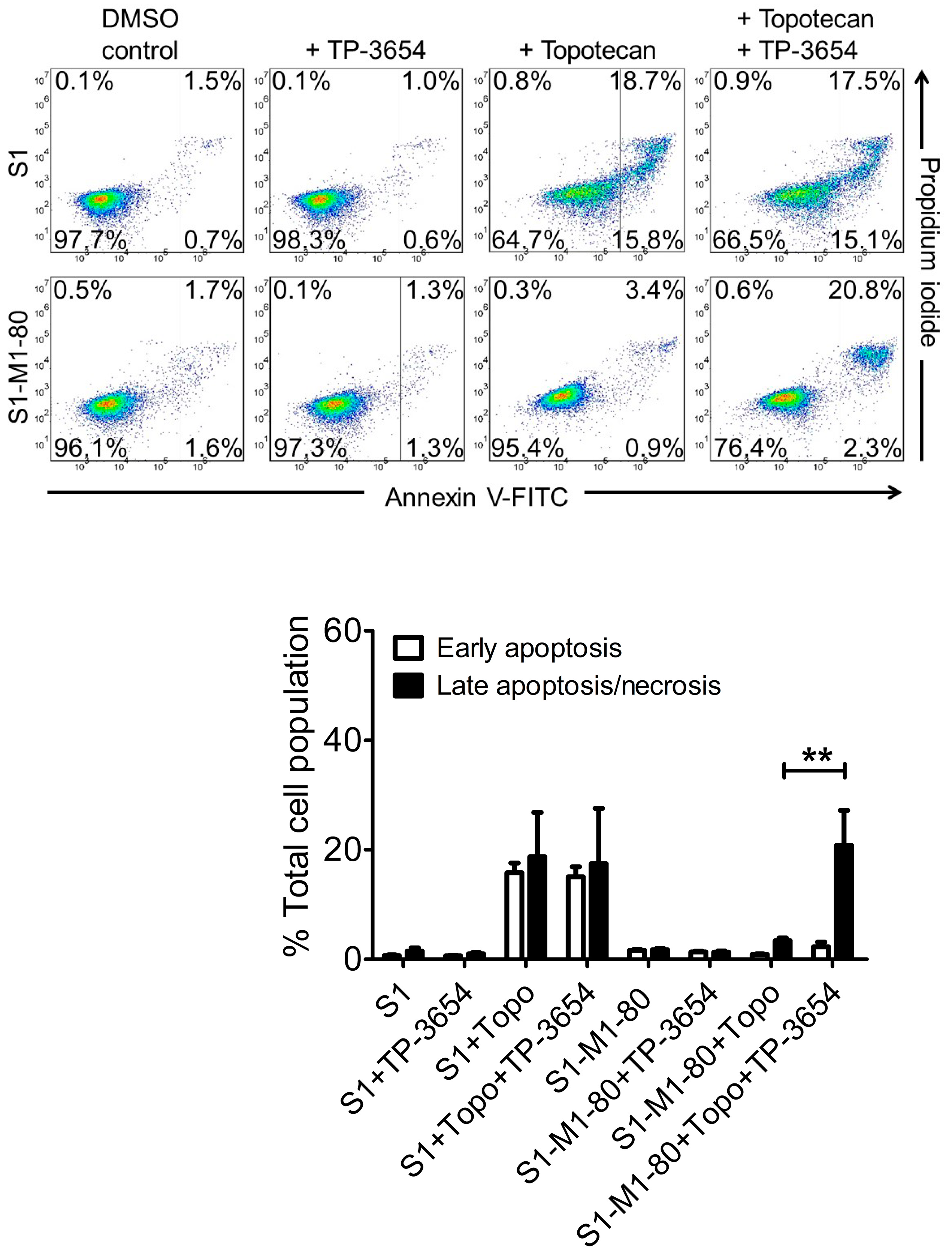
2.4. TP-3654 Enhances Drug-Induced Apoptosis in ABCG2-Overexpressing Cancer Cells
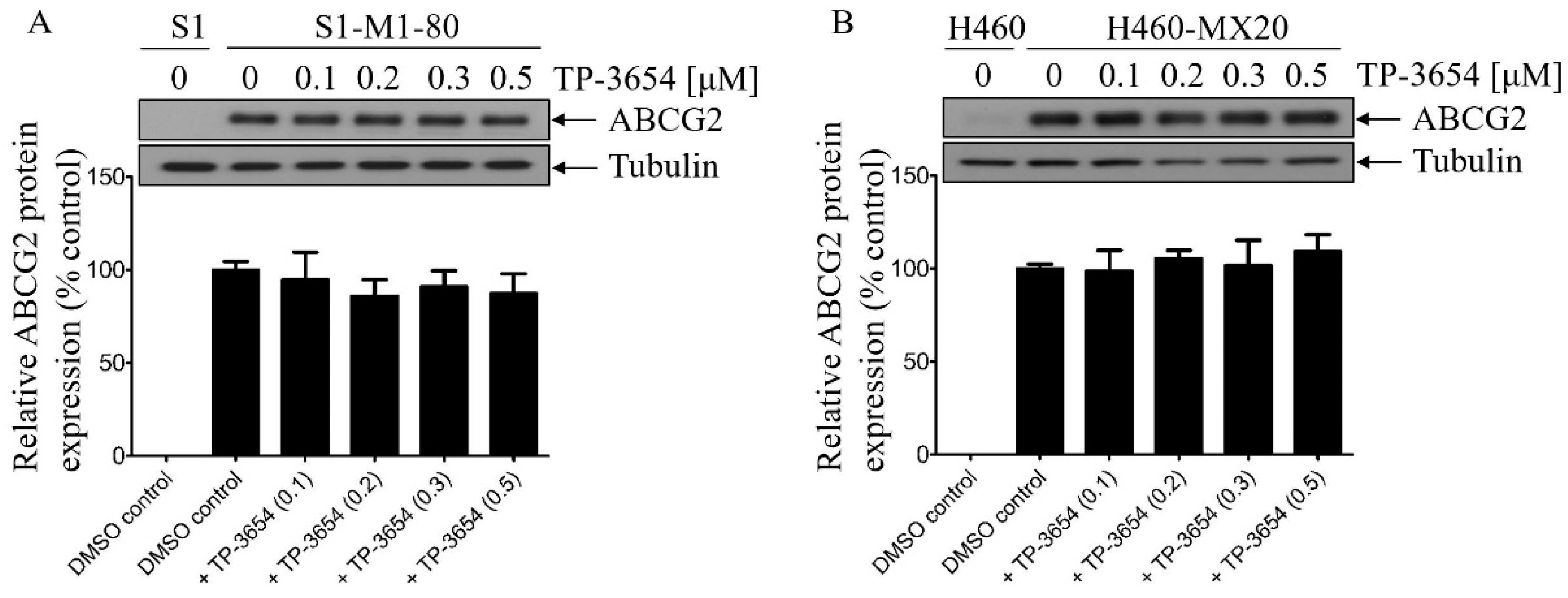
2.5. TP-3654 Treatment Does Not Affect the Protein Expression of ABCG2 in ABCG2-Overexpressing Cancer Cells
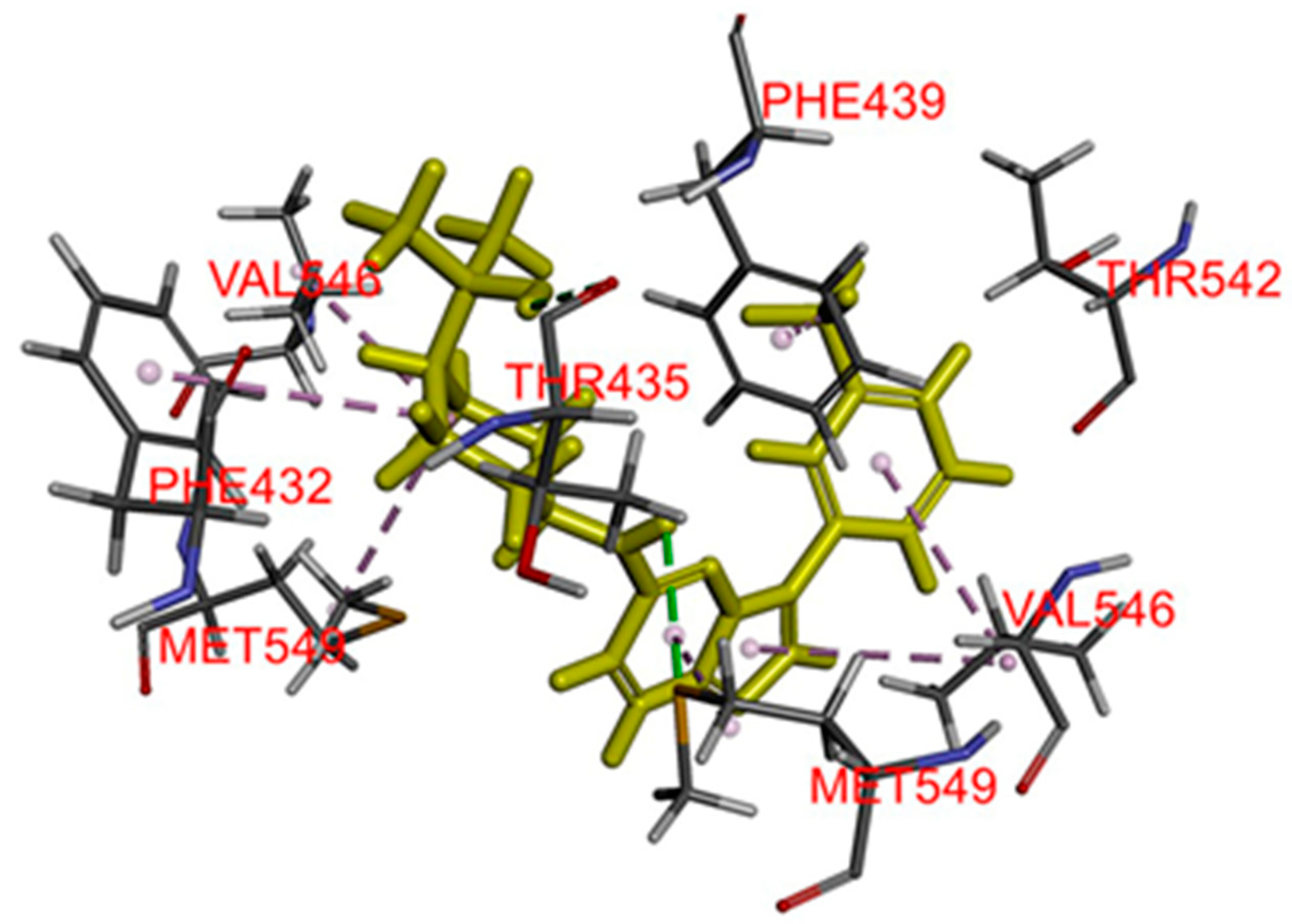
2.6. Docking of TP-3654 in the Drug-Binding Pocket of ABCG2
3. Discussion
4. Materials and Methods
4.1. Chemicals
4.2. Cell Lines
4.3. Cytotoxicity Assay
4.4. Apoptosis Assay
4.5. Flow Cytometry
4.6. Immunoblot
4.7. Docking Analysis of TP-3654 with ABCG2
4.8. Quantification and Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Szakacs, G.; Paterson, J.K.; Ludwig, J.A.; Booth-Genthe, C.; Gottesman, M.M. Targeting multidrug resistance in cancer. Nat. Rev. 2006, 5, 219–234. [Google Scholar] [CrossRef]
- Wu, C.-P.; Hsieh, C.-H.; Wu, Y.-S. The Emergence of Drug Transporter-Mediated Multidrug Resistance to Cancer Chemotherapy. Mol. Pharm. 2011, 8, 1996–2011. [Google Scholar] [CrossRef]
- Robey, R.W.; Pluchino, K.M.; Hall, M.D.; Fojo, A.T.; Bates, S.E.; Gottesman, M.M. Revisiting the role of ABC transporters in multidrug-resistant cancer. Nat. Rev. Cancer 2018, 18, 452–464. [Google Scholar] [CrossRef]
- Gottesman, M.; Ambudkar, S.V. Overview: ABC transporters and human disease. J. Bioenerg. Biomembr. 2001, 33, 453–458. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, S.; Sane, R.; Gallardo, J.L.; Ohlfest, J.R.; Elmquist, W.F. Distribution of gefitinib to the brain is limited by P-glycoprotein (ABCB1) and breast cancer resistance protein (ABCG2)-mediated active efflux. J. Pharmacol. Exp. Ther. 2010, 334, 147–155. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shukla, S.; Skoumbourdis, A.P.; Walsh, M.J.; Hartz, A.M.; Fung, K.L.; Wu, C.P.; Gottesman, M.M.; Bauer, B.; Thomas, C.J.; Ambudkar, S.V. Synthesis and characterization of a BODIPY conjugate of the BCR-ABL kinase inhibitor Tasigna (nilotinib): Evidence for transport of Tasigna and its fluorescent derivative by ABC drug transporters. Mol. Pharm. 2011, 8, 1292–1302. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brozik, A.; Hegedus, C.; Erdei, Z.; Hegedus, T.; Ozvegy-Laczka, C.; Szakacs, G.; Sarkadi, B. Tyrosine kinase inhibitors as modulators of ATP binding cassette multidrug transporters: Substrates, chemosensitizers or inducers of acquired multidrug resistance? Expert Opin. Drug Metab. Toxicol. 2011, 7, 623–642. [Google Scholar] [CrossRef]
- Wu, C.P.; Hsieh, Y.J.; Hsiao, S.H.; Su, C.Y.; Li, Y.Q.; Huang, Y.H.; Huang, C.W.; Hsieh, C.H.; Yu, J.S.; Wu, Y.S. Human ATP-Binding Cassette Transporter ABCG2 Confers Resistance to CUDC-907, a Dual Inhibitor of Histone Deacetylase and Phosphatidylinositol 3-Kinase. Mol. Pharm. 2016, 13, 784–794. [Google Scholar] [CrossRef]
- Wu, C.P.; Hsieh, Y.J.; Murakami, M.; Vahedi, S.; Hsiao, S.H.; Yeh, N.; Chou, A.W.; Li, Y.Q.; Wu, Y.S.; Yu, J.S.; et al. Human ATP-binding cassette transporters ABCB1 and ABCG2 confer resistance to histone deacetylase 6 inhibitor ricolinostat (ACY-1215) in cancer cell lines. Biochem. Pharmacol. 2018, 155, 316–325. [Google Scholar] [CrossRef] [PubMed]
- Kovalev, A.A.; Tsvetaeva, D.A.; Grudinskaja, T.V. Role of ABC-cassette transporters (MDR1, MRP1, BCRP) in the development of primary and acquired multiple drug resistance in patients with early and metastatic breast cancer. Exp. Oncol. 2013, 35, 287–290. [Google Scholar] [PubMed]
- Ross, D.D.; Karp, J.E.; Chen, T.T.; Doyle, L.A. Expression of breast cancer resistance protein in blast cells from patients with acute leukemia. Blood 2000, 96, 365–368. [Google Scholar] [CrossRef]
- Steinbach, D.; Sell, W.; Voigt, A.; Hermann, J.; Zintl, F.; Sauerbrey, A. BCRP gene expression is associated with a poor response to remission induction therapy in childhood acute myeloid leukemia. Leukemia 2002, 16, 1443–1447. [Google Scholar] [CrossRef]
- Uggla, B.; Stahl, E.; Wagsater, D.; Paul, C.; Karlsson, M.G.; Sirsjo, A.; Tidefelt, U. BCRP mRNA expression v. clinical outcome in 40 adult AML patients. Leuk. Res. 2005, 29, 141–146. [Google Scholar] [CrossRef]
- Matthews, C.; Catherwood, M.A.; Larkin, A.M.; Clynes, M.; Morris, T.C.; Alexander, H.D. MDR-1, but not MDR-3 gene expression, is associated with unmutated IgVH genes and poor prognosis chromosomal aberrations in chronic lymphocytic leukemia. Leuk. Lymphoma 2006, 47, 2308–2313. [Google Scholar] [CrossRef]
- Turner, J.G.; Gump, J.L.; Zhang, C.; Cook, J.M.; Marchion, D.; Hazlehurst, L.; Munster, P.; Schell, M.J.; Dalton, W.S.; Sullivan, D.M. ABCG2 expression, function, and promoter methylation in human multiple myeloma. Blood 2006, 108, 3881–3889. [Google Scholar] [CrossRef] [PubMed]
- Dai, C.L.; Tiwari, A.K.; Wu, C.P.; Su, X.D.; Wang, S.R.; Liu, D.G.; Ashby, C.R., Jr.; Huang, Y.; Robey, R.W.; Liang, Y.J.; et al. Lapatinib (Tykerb, GW572016) reverses multidrug resistance in cancer cells by inhibiting the activity of ATP-binding cassette subfamily B member 1 and G member 2. Cancer Res. 2008, 68, 7905–7914. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mi, Y.J.; Liang, Y.J.; Huang, H.B.; Zhao, H.Y.; Wu, C.P.; Wang, F.; Tao, L.Y.; Zhang, C.Z.; Dai, C.L.; Tiwari, A.K.; et al. Apatinib (YN968D1) reverses multidrug resistance by inhibiting the efflux function of multiple ATP-binding cassette transporters. Cancer Res. 2010, 70, 7981–7991. [Google Scholar] [CrossRef] [Green Version]
- Kuang, Y.H.; Patel, J.P.; Sodani, K.; Wu, C.P.; Liao, L.Q.; Patel, A.; Tiwari, A.K.; Dai, C.L.; Chen, X.; Fu, L.W.; et al. OSI-930 analogues as novel reversal agents for ABCG2-mediated multidrug resistance. Biochem. Pharmacol. 2012, 84, 766–774. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hsiao, S.H.; Lu, Y.J.; Li, Y.Q.; Huang, Y.H.; Hsieh, C.H.; Wu, C.P. Osimertinib (AZD9291) Attenuates the Function of Multidrug Resistance-Linked ATP-Binding Cassette Transporter ABCB1 In Vitro. Mol. Pharm. 2016. [Google Scholar] [CrossRef]
- Wu, C.P.; Hsiao, S.H.; Murakami, M.; Lu, M.J.; Li, Y.Q.; Hsieh, C.H.; Ambudkar, S.V.; Wu, Y.S. Tyrphostin RG14620 selectively reverses ABCG2-mediated multidrug resistance in cancer cell lines. Cancer Lett. 2017, 409, 56–65. [Google Scholar] [CrossRef] [PubMed]
- Beretta, G.L.; Cassinelli, G.; Pennati, M.; Zuco, V.; Gatti, L. Overcoming ABC transporter-mediated multidrug resistance: The dual role of tyrosine kinase inhibitors as multitargeting agents. Eur. J. Med. Chem. 2017, 142, 271–289. [Google Scholar] [CrossRef] [PubMed]
- Wu, S.; Fu, L. Tyrosine kinase inhibitors enhanced the efficacy of conventional chemotherapeutic agent in multidrug resistant cancer cells. Mol. Cancer 2018, 17, 25. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.P.; Hung, T.H.; Hsiao, S.H.; Huang, Y.H.; Hung, L.C.; Yu, Y.J.; Chang, Y.T.; Wang, S.P.; Wu, Y.S. Erdafitinib Resensitizes ABCB1-Overexpressing Multidrug-Resistant Cancer Cells to Cytotoxic Anticancer Drugs. Cancers 2020, 12, 1366. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.P.; Hung, T.H.; Lusvarghi, S.; Chu, Y.H.; Hsiao, S.H.; Huang, Y.H.; Chang, Y.T.; Ambudkar, S.V. The third-generation EGFR inhibitor almonertinib (HS-10296) resensitizes ABCB1-overexpressing multidrug-resistant cancer cells to chemotherapeutic drugs. Biochem. Pharmacol. 2021, 188, 114516. [Google Scholar] [CrossRef]
- Foulks, J.M.; Carpenter, K.J.; Luo, B.; Xu, Y.; Senina, A.; Nix, R.; Chan, A.; Clifford, A.; Wilkes, M.; Vollmer, D.; et al. A small-molecule inhibitor of PIM kinases as a potential treatment for urothelial carcinomas. Neoplasia 2014, 16, 403–412. [Google Scholar] [CrossRef] [Green Version]
- Mondello, P.; Cuzzocrea, S.; Mian, M. Pim kinases in hematological malignancies: Where are we now and where are we going? J. Hematol. Oncol. 2014, 7, 95. [Google Scholar] [CrossRef] [Green Version]
- Beier, U.H.; Weise, J.B.; Laudien, M.; Sauerwein, H.; Gorogh, T. Overexpression of Pim-1 in head and neck squamous cell carcinomas. Int. J. Oncol. 2007, 30, 1381–1387. [Google Scholar] [CrossRef] [Green Version]
- Guo, S.; Mao, X.; Chen, J.; Huang, B.; Jin, C.; Xu, Z.; Qiu, S. Overexpression of Pim-1 in bladder cancer. J. Exp. Clin. Cancer Res. 2010, 29, 161. [Google Scholar] [CrossRef] [Green Version]
- Wang, J.; Anderson, P.D.; Luo, W.; Gius, D.; Roh, M.; Abdulkadir, S.A. Pim1 kinase is required to maintain tumorigenicity in MYC-expressing prostate cancer cells. Oncogene 2012, 31, 1794–1803. [Google Scholar] [CrossRef] [Green Version]
- Fathi, A.T.; Arowojolu, O.; Swinnen, I.; Sato, T.; Rajkhowa, T.; Small, D.; Marmsater, F.; Robinson, J.E.; Gross, S.D.; Martinson, M.; et al. A potential therapeutic target for FLT3-ITD AML: PIM1 kinase. Leuk. Res. 2012, 36, 224–231. [Google Scholar] [CrossRef] [Green Version]
- Decker, S.; Finter, J.; Forde, A.J.; Kissel, S.; Schwaller, J.; Mack, T.S.; Kuhn, A.; Gray, N.; Follo, M.; Jumaa, H.; et al. PIM kinases are essential for chronic lymphocytic leukemia cell survival (PIM2/3) and CXCR4-mediated microenvironmental interactions (PIM1). Mol. Cancer Ther. 2014, 13, 1231–1245. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gomez-Abad, C.; Pisonero, H.; Blanco-Aparicio, C.; Roncador, G.; Gonzalez-Menchen, A.; Martinez-Climent, J.A.; Mata, E.; Rodriguez, M.E.; Munoz-Gonzalez, G.; Sanchez-Beato, M.; et al. PIM2 inhibition as a rational therapeutic approach in B-cell lymphoma. Blood 2011, 118, 5517–5527. [Google Scholar] [CrossRef] [Green Version]
- Alnabulsi, S.; Al-Hurani, E.A. Pim kinase inhibitors in cancer: Medicinal chemistry insights into their activity and selectivity. Drug Discov. Today 2020. [Google Scholar] [CrossRef] [PubMed]
- Panchal, N.K.; Sabina, E.P. A serine/threonine protein PIM kinase as a biomarker of cancer and a target for anti-tumor therapy. Life Sci. 2020, 255, 117866. [Google Scholar] [CrossRef]
- Toth, R.K.; Warfel, N.A. Targeting PIM Kinases to Overcome Therapeutic Resistance in Cancer. Mol. Cancer Ther. 2021, 20, 3–10. [Google Scholar] [CrossRef]
- Robey, R.W.; Shukla, S.; Steadman, K.; Obrzut, T.; Finley, E.M.; Ambudkar, S.V.; Bates, S.E. Inhibition of ABCG2-mediated transport by protein kinase inhibitors with a bisindolylmaleimide or indolocarbazole structure. Mol. Cancer Ther. 2007, 6, 1877–1885. [Google Scholar] [CrossRef] [Green Version]
- Shukla, S.; Chen, Z.S.; Ambudkar, S.V. Tyrosine kinase inhibitors as modulators of ABC transporter-mediated drug resistance. Drug Resist. Updat. 2012, 15, 70–80. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wu, C.P.; Hsiao, S.H.; Sim, H.M.; Luo, S.Y.; Tuo, W.C.; Cheng, H.W.; Li, Y.Q.; Huang, Y.H.; Ambudkar, S.V. Human ABCB1 (P-glycoprotein) and ABCG2 mediate resistance to BI 2536, a potent and selective inhibitor of Polo-like kinase 1. Biochem. Pharmacol. 2013, 86, 904–913. [Google Scholar] [CrossRef] [Green Version]
- Wu, C.P.; Hsiao, S.H.; Luo, S.Y.; Tuo, W.C.; Su, C.Y.; Li, Y.Q.; Huang, Y.H.; Hsieh, C.H. Overexpression of human ABCB1 in cancer cells leads to reduced activity of GSK461364, a specific inhibitor of polo-like kinase 1. Mol. Pharm. 2014, 11, 3727–3736. [Google Scholar] [CrossRef]
- Wu, C.P.; Hsieh, C.H.; Hsiao, S.H.; Luo, S.Y.; Su, C.Y.; Li, Y.Q.; Huang, Y.H.; Huang, C.W.; Hsu, S.C. Human ATP-Binding Cassette Transporter ABCB1 Confers Resistance to Volasertib (BI 6727), a Selective Inhibitor of Polo-like Kinase 1. Mol. Pharm. 2015, 12, 3885–3895. [Google Scholar] [CrossRef]
- Natarajan, K.; Bhullar, J.; Shukla, S.; Burcu, M.; Chen, Z.S.; Ambudkar, S.V.; Baer, M.R. The Pim kinase inhibitor SGI-1776 decreases cell surface expression of P-glycoprotein (ABCB1) and breast cancer resistance protein (ABCG2) and drug transport by Pim-1-dependent and -independent mechanisms. Biochem. Pharmacol. 2013, 85, 514–524. [Google Scholar] [CrossRef] [Green Version]
- Kartner, N.; Riordan, J.R.; Ling, V. Cell surface P-glycoprotein associated with multidrug resistance in mammalian cell lines. Science 1983, 221, 1285–1288. [Google Scholar] [CrossRef]
- Bates, S.E.; Medina-Perez, W.Y.; Kohlhagen, G.; Antony, S.; Nadjem, T.; Robey, R.W.; Pommier, Y. ABCG2 mediates differential resistance to SN-38 (7-ethyl-10-hydroxycamptothecin) and homocamptothecins. J. Pharmacol. Exp. Ther. 2004, 310, 836–842. [Google Scholar] [CrossRef] [Green Version]
- Maliepaard, M.; van Gastelen, M.A.; de Jong, L.A.; Pluim, D.; van Waardenburg, R.C.; Ruevekamp-Helmers, M.C.; Floot, B.G.; Schellens, J.H. Overexpression of the BCRP/MXR/ABCP gene in a topotecan-selected ovarian tumor cell line. Cancer Res. 1999, 59, 4559–4563. [Google Scholar]
- Wu, C.P.; Lusvarghi, S.; Wang, J.C.; Hsiao, S.H.; Huang, Y.H.; Hung, T.H.; Ambudkar, S.V. Avapritinib: A Selective Inhibitor of KIT and PDGFRalpha that Reverses ABCB1 and ABCG2-Mediated Multidrug Resistance in Cancer Cell Lines. Mol. Pharm. 2019, 16, 3040–3052. [Google Scholar] [CrossRef]
- Galetti, M.; Petronini, P.G.; Fumarola, C.; Cretella, D.; La Monica, S.; Bonelli, M.; Cavazzoni, A.; Saccani, F.; Caffarra, C.; Andreoli, R.; et al. Effect of ABCG2/BCRP Expression on Efflux and Uptake of Gefitinib in NSCLC Cell Lines. PLoS ONE 2015, 10, e0141795. [Google Scholar] [CrossRef]
- Kannan, P.; Telu, S.; Shukla, S.; Ambudkar, S.V.; Pike, V.W.; Halldin, C.; Gottesman, M.M.; Innis, R.B.; Hall, M.D. The “specific” P-glycoprotein inhibitor Tariquidar is also a substrate and an inhibitor for breast cancer resistance protein (BCRP/ABCG2). ACS Chem. Neurosci. 2011, 2, 82–89. [Google Scholar] [CrossRef] [Green Version]
- Weidner, L.D.; Zoghbi, S.S.; Lu, S.; Shukla, S.; Ambudkar, S.V.; Pike, V.W.; Mulder, J.; Gottesman, M.M.; Innis, R.B.; Hall, M.D. The Inhibitor Ko143 Is Not Specific for ABCG2. J. Pharmacol. Exp. Ther. 2015, 354, 384–393. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Toyoda, Y.; Takada, T.; Suzuki, H. Inhibitors of Human ABCG2: From Technical Background to Recent Updates With Clinical Implications. Front. Pharmacol. 2019, 10, 208. [Google Scholar] [CrossRef] [Green Version]
- Dong, J.; Qin, Z.; Zhang, W.D.; Cheng, G.; Yehuda, A.G.; Ashby, C.R., Jr.; Chen, Z.S.; Cheng, X.D.; Qin, J.J. Medicinal chemistry strategies to discover P-glycoprotein inhibitors: An update. Drug Resist. Updat. 2020, 49, 100681. [Google Scholar] [CrossRef]
- Wu, C.P.; Hsiao, S.H.; Huang, Y.H.; Hung, L.C.; Yu, Y.J.; Chang, Y.T.; Hung, T.H.; Wu, Y.S. Sitravatinib Sensitizes ABCB1- and ABCG2-Overexpressing Multidrug-Resistant Cancer Cells to Chemotherapeutic Drugs. Cancers 2020, 12, 195. [Google Scholar] [CrossRef] [Green Version]
- Hsiao, S.H.; Lusvarghi, S.; Huang, Y.H.; Ambudkar, S.V.; Hsu, S.C.; Wu, C.P. The FLT3 inhibitor midostaurin selectively resensitizes ABCB1-overexpressing multidrug-resistant cancer cells to conventional chemotherapeutic agents. Cancer Lett. 2019, 445, 34–44. [Google Scholar] [CrossRef] [PubMed]
- Van Hoppe, S.; Jamalpoor, A.; Rood, J.J.M.; Wagenaar, E.; Sparidans, R.W.; Beijnen, J.H.; Schinkel, A.H. Brain accumulation of osimertinib and its active metabolite AZ5104 is restricted by ABCB1 (P-glycoprotein) and ABCG2 (breast cancer resistance protein). Pharmacol. Res. 2019, 146, 104297. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Gan, C.; Sparidans, R.W.; Wagenaar, E.; van Hoppe, S.; Beijnen, J.H.; Schinkel, A.H. P-glycoprotein (MDR1/ABCB1) and Breast Cancer Resistance Protein (BCRP/ABCG2) affect brain accumulation and intestinal disposition of encorafenib in mice. Pharmacol. Res. 2018, 129, 414–423. [Google Scholar] [CrossRef] [PubMed]
- Van Hoppe, S.; Rood, J.J.M.; Buil, L.; Wagenaar, E.; Sparidans, R.W.; Beijnen, J.H.; Schinkel, A.H. P-Glycoprotein (MDR1/ABCB1) Restricts Brain Penetration of the Bruton’s Tyrosine Kinase Inhibitor Ibrutinib, While Cytochrome P450-3A (CYP3A) Limits Its Oral Bioavailability. Mol. Pharm. 2018, 15, 5124–5134. [Google Scholar] [CrossRef]
- Wu, C.P.; Sim, H.M.; Huang, Y.H.; Liu, Y.C.; Hsiao, S.H.; Cheng, H.W.; Li, Y.Q.; Ambudkar, S.V.; Hsu, S.C. Overexpression of ATP-binding cassette transporter ABCG2 as a potential mechanism of acquired resistance to vemurafenib in BRAF(V600E) mutant cancer cells. Biochem. Pharmacol. 2013, 85, 325–334. [Google Scholar] [CrossRef] [Green Version]
- Moore, M.J.; Goldstein, D.; Hamm, J.; Figer, A.; Hecht, J.R.; Gallinger, S.; Au, H.J.; Murawa, P.; Walde, D.; Wolff, R.A.; et al. Erlotinib plus gemcitabine compared with gemcitabine alone in patients with advanced pancreatic cancer: A phase III trial of the National Cancer Institute of Canada Clinical Trials Group. J. Clin. Oncol. 2007, 25, 1960–1966. [Google Scholar] [CrossRef]
- Yang, Z.Y.; Yuan, J.Q.; Di, M.Y.; Zheng, D.Y.; Chen, J.Z.; Ding, H.; Wu, X.Y.; Huang, Y.F.; Mao, C.; Tang, J.L. Gemcitabine plus erlotinib for advanced pancreatic cancer: A systematic review with meta-analysis. PLoS ONE 2013, 8, e57528. [Google Scholar] [CrossRef] [Green Version]
- Geyer, C.E.; Forster, J.; Lindquist, D.; Chan, S.; Romieu, C.G.; Pienkowski, T.; Jagiello-Gruszfeld, A.; Crown, J.; Chan, A.; Kaufman, B.; et al. Lapatinib plus capecitabine for HER2-positive advanced breast cancer. N. Engl. J. Med. 2006, 355, 2733–2743. [Google Scholar] [CrossRef] [Green Version]
- Cetin, B.; Benekli, M.; Turker, I.; Koral, L.; Ulas, A.; Dane, F.; Oksuzoglu, B.; Kaplan, M.A.; Koca, D.; Boruban, C.; et al. Lapatinib plus capecitabine for HER2-positive advanced breast cancer: A multicentre study of Anatolian Society of Medical Oncology (ASMO). J. Chemother. 2014, 26, 300–305. [Google Scholar] [CrossRef]
- Alemany, R.; Moura, D.S.; Redondo, A.; Martinez-Trufero, J.; Calabuig, S.; Saus, C.; Obrador-Hevia, A.; Ramos, R.F.; Villar, V.H.; Valverde, C.; et al. Nilotinib as co-adjuvant treatment with doxorubicin in patients with sarcomas: A phase I trial of the Spanish Group for Research on Sarcoma. Clin. Cancer Res. 2018. [Google Scholar] [CrossRef] [Green Version]
- Chen, L.S.; Redkar, S.; Bearss, D.; Wierda, W.G.; Gandhi, V. Pim kinase inhibitor, SGI-1776, induces apoptosis in chronic lymphocytic leukemia cells. Blood 2009, 114, 4150–4157. [Google Scholar] [CrossRef]
- Shen, D.W.; Cardarelli, C.; Hwang, J.; Cornwell, M.; Richert, N.; Ishii, S.; Pastan, I.; Gottesman, M.M. Multiple drug-resistant human KB carcinoma cells independently selected for high-level resistance to colchicine, adriamycin, or vinblastine show changes in expression of specific proteins. J. Biol. Chem. 1986, 261, 7762–7770. [Google Scholar] [CrossRef]
- Robey, R.W.; Shukla, S.; Finley, E.M.; Oldham, R.K.; Barnett, D.; Ambudkar, S.V.; Fojo, T.; Bates, S.E. Inhibition of P-glycoprotein (ABCB1)- and multidrug resistance-associated protein 1 (ABCC1)-mediated transport by the orally administered inhibitor, CBT-1((R)). Biochem. Pharmacol. 2008, 75, 1302–1312. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Robey, R.W.; Honjo, Y.; Morisaki, K.; Nadjem, T.A.; Runge, S.; Risbood, M.; Poruchynsky, M.S.; Bates, S.E. Mutations at amino-acid 482 in the ABCG2 gene affect substrate and antagonist specificity. Br. J. Cancer 2003, 89, 1971–1978. [Google Scholar] [CrossRef] [PubMed]
- Roschke, A.V.; Tonon, G.; Gehlhaus, K.S.; McTyre, N.; Bussey, K.J.; Lababidi, S.; Scudiero, D.A.; Weinstein, J.N.; Kirsch, I.R. Karyotypic complexity of the NCI-60 drug-screening panel. Cancer Res. 2003, 63, 8634–8647. [Google Scholar]
- Shen, D.W.; Fojo, A.; Chin, J.E.; Roninson, I.B.; Richert, N.; Pastan, I.; Gottesman, M.M. Human multidrug-resistant cell lines: Increased mdr1 expression can precede gene amplification. Science 1986, 232, 643–645. [Google Scholar] [CrossRef]
- Henrich, C.J.; Robey, R.W.; Bokesch, H.R.; Bates, S.E.; Shukla, S.; Ambudkar, S.V.; Dean, M.; McMahon, J.B. New inhibitors of ABCG2 identified by high-throughput screening. Mol. Cancer Ther. 2007, 6, 3271–3278. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Honjo, Y.; Hrycyna, C.A.; Yan, Q.W.; Medina-Perez, W.Y.; Robey, R.W.; van de Laar, A.; Litman, T.; Dean, M.; Bates, S.E. Acquired mutations in the MXR/BCRP/ABCP gene alter substrate specificity in MXR/BCRP/ABCP-overexpressing cells. Cancer Res. 2001, 61, 6635–6639. [Google Scholar]
- Henrich, C.J.; Bokesch, H.R.; Dean, M.; Bates, S.E.; Robey, R.W.; Goncharova, E.I.; Wilson, J.A.; McMahon, J.B. A high-throughput cell-based assay for inhibitors of ABCG2 activity. J. Biomol. Screen. 2006, 11, 176–183. [Google Scholar] [CrossRef] [Green Version]
- Wu, C.P.; Shukla, S.; Calcagno, A.M.; Hall, M.D.; Gottesman, M.M.; Ambudkar, S.V. Evidence for dual mode of action of a thiosemicarbazone, NSC73306: A potent substrate of the multidrug resistance linked ABCG2 transporter. Mol. Cancer Ther. 2007, 6, 3287–3296. [Google Scholar] [CrossRef] [Green Version]
- Ishiyama, M.; Tominaga, H.; Shiga, M.; Sasamoto, K.; Ohkura, Y.; Ueno, K. A combined assay of cell viability and in vitro cytotoxicity with a highly water-soluble tetrazolium salt, neutral red and crystal violet. Biol. Pharm. Bull. 1996, 19, 1518–1520. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Robey, R.W.; Steadman, K.; Polgar, O.; Morisaki, K.; Blayney, M.; Mistry, P.; Bates, S.E. Pheophorbide a is a specific probe for ABCG2 function and inhibition. Cancer Res. 2004, 64, 1242–1246. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Orlando, B.J.; Liao, M. ABCG2 transports anticancer drugs via a closed-to-open switch. Nat. Commun. 2020, 11, 2264. [Google Scholar] [CrossRef] [PubMed]

| Cell Line | Type | Transporter Expressed | IC50 (μM) † |
|---|---|---|---|
| KB-3-1 | Epidermal | - | 19.07 ± 1.59 |
| KB-V-1 | Epidermal | ABCB1 | 24.50 ± 3.24 |
| OVCAR-8 | Ovarian | - | 34.33 ± 5.92 |
| NCI-ADR-RES | Ovarian | ABCB1 | 28.00 ± 3.38 |
| S1 | Colon | - | 4.10 ± 1.17 |
| S1-M1-80 | Colon | ABCG2 | 3.39 ± 0.39 |
| H460 | Lung | - | 22.26 ± 3.35 |
| H460-MX20 | Lung | ABCG2 | 22.05 ± 3.87 |
| pcDNA3.1-HEK293 | - | - | 2.76 ± 0.79 |
| MDR19-HEK293 | - | ABCB1 | 3.03 ± 0.59 |
| R482-HEK293 | - | ABCG2 | 2.55 ± 0.53 |
| Treatment | Concentration (nM) | Mean IC50 † ± SD and (FR ‡) | |
|---|---|---|---|
| OVCAR-8 (Parental) (nM) | NCI-ADR-RES (Resistant) (μM) | ||
| Paclitaxel | - | 3.82 ± 0.62 (1.0) | 9.37 ± 1.47 (1.0) |
| +TP-3654 | 100 | 4.47 ± 0.65 (0.9) | 10.12 ± 1.20 (0.9) |
| +TP-3654 | 200 | 4.18 ± 0.61 (0.9) | 9.34 ± 1.24 (1.0) |
| +TP-3654 | 300 | 4.46 ± 0.66 (0.9) | 9.17 ± 1.15 (1.0) |
| +TP-3654 | 500 | 4.12 ± 0.47 (0.9) | 7.36 ± 0.84 (1.3) |
| +tariquidar | 1000 | 3.56 ± 0.59 (1.1) | 12.74 ± 1.32 (nM) *** (735) |
| (nM) | (μM) | ||
| Doxorubicin | - | 248.55 ± 52.08 (1.0) | 6.30 ± 0.67 (1.0) |
| +TP-3654 | 100 | 242.57 ± 41.55 (1.0) | 7.26 ± 1.11 (0.9) |
| +TP-3654 | 200 | 226.91 ± 51.04 (1.1) | 8.35 ± 1.15 (0.8) |
| +TP-3654 | 300 | 190.94 ± 35.52 (1.3) | 7.63 ± 1.12 (0.8) |
| +TP-3654 | 500 | 201.04 ± 48.62 (1.2) | 6.86 ± 0.87 (0.9) |
| +tariquidar | 1000 | 216.42 ± 50.37 (1.1) | 0.36 ± 0.07 *** (17.5) |
| (nM) | (nM) | ||
| Colchicine | - | 33.25 ± 11.26 (1.0) | 1827.27 ± 229.42 (1.0) |
| +TP-3654 | 100 | 34.30 ± 13.08 (1.0) | 2300.41 ± 525.88 (0.8) |
| +TP-3654 | 200 | 35.92 ± 13.87 (0.9) | 2185.00 ± 387.82 (0.8) |
| +TP-3654 | 300 | 35.99 ± 12.62 (0.9) | 2135.46 ± 235.40 (0.9) |
| +TP-3654 | 500 | 32.94 ± 12.25 (1.0) | 2672.43 ± 581.86 (0.7) |
| +tariquidar | 1000 | 34.98 ± 12.35 (0.9) | 65.29 ± 23.07 *** (28.0) |
| Treatment | Concentration (nM) | KB-3-1 (Parental) (nM) | KB-V-1 (Resistant) (nM) |
| Paclitaxel | - | 2.31 ± 0.75 (1.0) | 2083.57 ± 250.53 (1.0) |
| +TP-3654 | 100 | 2.46 ± 0.64 (0.9) | 2269.00 ± 245.85 (0.9) |
| +TP-3654 | 200 | 2.26 ± 0.52 (1.0) | 2171.55 ± 290.13 (1.0) |
| +TP-3654 | 300 | 2.07 ± 0.48 (1.1) | 2263.61 ± 271.75 (0.9) |
| +TP-3654 | 500 | 2.15 ± 0.42 (1.1) | 1648.56 ± 187.39 (1.3) |
| +tariquidar | 1000 | 2.24 ± 0.59 (1.0) | 2.16 ± 0.59 *** (964.6) |
| (nM) | (μM) | ||
| Doxorubicin | - | 174.34 ± 41.49 (1.0) | 2.27 ± 0.21 (1.0) |
| +TP-3654 | 100 | 153.79 ± 43.44 (1.1) | 2.66 ± 0.21 (0.9) |
| +TP-3654 | 200 | 161.07 ± 44.68 (1.1) | 2.33 ± 0.20 (1.0) |
| +TP-3654 | 300 | 209.34 ± 59.06 (0.8) | 1.85 ± 0.19 (1.2) |
| +TP-3654 | 500 | 153.50 ± 43.54 (1.1) | 1.95 ± 0.18 (1.1) |
| +tariquidar | 1000 | 185.90 ± 73.46 (0.9) | 79.29 ± 23.05 (nM) *** (28.6) |
| (nM) | (nM) | ||
| Colchicine | - | 20.59 ± 8.45 (1.0) | 854.44 ± 71.42 (1.0) |
| +TP-3654 | 100 | 20.55 ± 8.10 (1.0) | 921.75 ± 113.96 (0.9) |
| +TP-3654 | 200 | 20.98 ± 7.97 (1.0) | 808.36 ± 79.91 (1.1) |
| +TP-3654 | 300 | 19.43 ± 7.17 (1.1) | 947.28 ± 98.51 (0.9) |
| +TP-3654 | 500 | 20.56 ± 7.12 (1.0) | 914.81 ± 109.63 (0.9) |
| +tariquidar | 1000 | 19.00 ± 7.23 (1.1) | 20.36 ± 6.30 *** (42.0) |
| Treatment | Concentration (nM) | pcDNA3.1-HEK293 (Parental) (nM) | MDR19-HEK293 (Resistant) (nM) |
| Paclitaxel | - | 3.47 ± 0.67 (1.0) | 737.62 ± 126.44 (1.0) |
| +TP-3654 | 100 | 4.11 ± 0.97 (0.8) | 743.54 ± 146.73 (1.0) |
| +TP-3654 | 200 | 4.02 ± 0.74 (0.9) | 581.71 ± 90.37 (1.3) |
| +TP-3654 | 300 | 4.14 ± 0.75 (0.8) | 738.96 ± 108.01 (1.0) |
| +TP-3654 | 500 | 3.68 ± 0.63 (0.9) | 642.38 ± 132.50 (1.1) |
| +tariquidar | 1000 | 2.74 ± 0.43 (1.3) | 2.05 ± 0.39 *** (359.8) |
| (nM) | (nM) | ||
| Doxorubicin | - | 25.55 ± 6.31 (1.0) | 297.78 ± 51.34 (1.0) |
| +TP-3654 | 100 | 28.60 ± 7.10 (0.9) | 294.19 ± 52.47 (1.0) |
| +TP-3654 | 200 | 28.77 ± 7.62 (0.9) | 237.93 ± 46.90 (1.3) |
| +TP-3654 | 300 | 27.38 ± 7.99 (0.9) | 273.57 ± 78.20 (1.1) |
| +TP-3654 | 500 | 28.61 ± 9.59 (0.9) | 272.00 ± 69.14 (1.1) |
| +tariquidar | 1000 | 22.26 ± 5.37 (1.1) | 16.59 ± 2.33 *** (18.0) |
| (nM) | (nM) | ||
| Colchicine | - | 13.02 ± 2.79 (1.0) | 100.07 ± 21.01 (1.0) |
| +TP-3654 | 100 | 15.98 ± 4.05 (0.8) | 107.28 ± 21.50 (0.9) |
| +TP-3654 | 200 | 14.95 ± 3.73 (0.9) | 78.54 ± 15.95 (1.3) |
| +TP-3654 | 300 | 14.11 ± 3.10 (0.9) | 98.65 ± 20.29 (1.0) |
| +TP-3654 | 500 | 14.91 ± 3.50 (0.9) | 89.50 ± 22.14 (1.1) |
| +tariquidar | 1000 | 14.12 ± 3.29 (0.9) | 8.46 ± 2.66 ** (11.8) |
| Treatment | Concentration (nM) | Mean IC50 † ± SD and (FR ‡) | |
|---|---|---|---|
| S1 (Parental) (nM) | S1-M1-80 (Resistant) (μM) | ||
| Topotecan | - | 12.82 ± 3.16 (1.0) | 10.81 ± 0.91 (1.0) |
| +TP-3654 | 100 | 14.43 ± 3.06 (0.9) | 5.09 ± 0.76 ** (2.1) |
| +TP-3654 | 200 | 13.66 ± 3.22 (0.9) | 2.90 ± 0.64 *** (3.7) |
| +TP-3654 | 300 | 15.93 ± 3.49 (0.8) | 2.94 ± 0.70 *** (3.7) |
| +TP-3654 | 500 | 12.94 ± 2.63 (1.0) | 2.75 ± 0.73 *** (3.9) |
| +Ko143 | 1000 | 13.23 ± 2.63 (1.0) | 1.13 ± 0.24 *** (9.6) |
| (nM) | (nM) | ||
| SN-38 | - | 3.22 ± 0.54 (1.0) | 1804.90 ± 112.67 (1.0) |
| +TP-3654 | 100 | 4.14 ± 0.74 (0.8) | 706.84 ± 106.11 *** (2.6) |
| +TP-3654 | 200 | 3.32 ± 0.54 (1.0) | 517.32 ± 100.26 *** (3.5) |
| +TP-3654 | 300 | 3.67 ± 0.64 (0.9) | 443.73 ± 101.80 *** (4.1) |
| +TP-3654 | 500 | 3.14 ± 0.62 (1.0) | 304.09 ± 81.75 *** (5.9) |
| +Ko143 | 1000 | 2.69 ± 0.47 (1.2) | 104.36 ± 22.88 *** (17.3) |
| (nM) | (μM) | ||
| Mitoxantrone | - | 5.65 ± 0.48 (1.0) | 35.04 ± 6.71 (1.0) |
| +TP-3654 | 100 | 5.10 ± 0.34 (1.1) | 10.50 ± 1.03 ** (3.3) |
| +TP-3654 | 200 | 5.94 ± 0.42 (1.0) | 5.42 ± 0.57 ** (6.5) |
| +TP-3654 | 300 | 5.92 ± 0.36 (1.0) | 2.53 ± 0.25 ** (13.8) |
| +TP-3654 | 500 | 6.22 ± 0.44 (0.9) | 1.30 ± 0.11 *** (27.0) |
| +Ko143 | 1000 | 5.34 ± 0.61 (1.1) | 0.36 ± 0.04 *** (58.4) |
| Treatment | Concentration (nM) | H460 (Parental) (nM) | H460-MX20 (Resistant) (nM) |
| Topotecan | - | 60.21 ± 10.05 (1.0) | 737.60 ± 145.43 (1.0) |
| +TP-3654 | 100 | 26.93 ± 4.35 ** (2.2) | 161.36 ± 26.08 ** (4.6) |
| +TP-3654 | 200 | 20.54 ± 3.24** (2.9) | 76.96 ± 12.29 ** (9.6) |
| +TP-3654 | 300 | 21.23 ± 2.99 ** (2.8) | 51.10 ± 10.63 ** (14.4) |
| +TP-3654 | 500 | 16.81 ± 2.34 ** (3.6) | 37.09 ± 6.65 ** (19.9) |
| +Ko143 | 1000 | 21.53 ± 3.25 ** (2.8) | 25.10 ± 5.50 ** (29.4) |
| (nM) | (nM) | ||
| SN-38 | - | 6.10 ± 1.21 (1.0) | 246.21 ± 44.64 (1.0) |
| +TP-3654 | 100 | 4.29 ± 0.66 (1.4) | 27.87 ± 2.58 ** (8.8) |
| +TP-3654 | 200 | 3.61 ± 0.33 * (1.7) | 18.00 ± 2.98 *** (13.7) |
| +TP-3654 | 300 | 1.98 ± 0.22 ** (3.1) | 9.20 ± 1.33 *** (26.8) |
| +TP-3654 | 500 | 2.05 ± 0.19 ** (3.0) | 7.72 ± 1.92 *** (31.9) |
| +Ko143 | 1000 | 2.10 ± 0.27 ** (2.9) | 2.57 ± 0.66 *** (95.8) |
| (nM) | (nM) | ||
| Mitoxantrone | - | 15.42 ± 1.83 (1.0) | 996.71 ± 127.75 (1.0) |
| +TP-3654 | 100 | 8.83 ± 0.99 ** (1.7) | 841.73 ± 187.29 (1.2) |
| +TP-3654 | 200 | 10.45 ± 1.95 * (1.5) | 388.45 ± 40.35 ** (2.6) |
| +TP-3654 | 300 | 13.19 ± 2.74 (1.2) | 261.46 ± 55.67 *** (3.8) |
| +TP-3654 | 500 | 16.46 ± 2.58 (0.9) | 153.79 ± 28.65 *** (6.5) |
| +Ko143 | 1000 | 10.28 ± 1.78 * (1.5) | 208.89 ± 29.46 *** (4.8) |
| Treatment | Concentration (nM) | pcDNA3.1-HEK293 (Parental) (nM) | R482-HEK293 (Resistant) (nM) |
| Topotecan | - | 24.19 ± 4.95 (1.0) | 430.30 ± 67.85 (1.0) |
| +TP-3654 | 100 | 24.72 ± 5.60 (1.0) | 149.56 ± 31.21 ** (2.9) |
| +TP-3654 | 200 | 26.34 ± 6.76 (0.9) | 81.88 ± 14.13 *** (5.3) |
| +TP-3654 | 300 | 24.80 ± 5.40 (1.0) | 73.56 ± 11.35 *** (5.8) |
| +TP-3654 | 500 | 27.06 ± 6.68 (0.9) | 49.04 ± 8.91 *** (8.8) |
| +Ko143 | 1000 | 26.34 ± 5.49 (0.9) | 41.75 ± 8.49 *** (10.3) |
| (nM) | (nM) | ||
| SN-38 | - | 2.61 ± 0.80 (1.0) | 177.87 ± 31.96 (1.0) |
| +TP-3654 | 100 | 2.67 ± 0.48 (1.0) | 53.98 ± 17.04 ** (3.3) |
| +TP-3654 | 200 | 2.83 ± 0.55 (0.9) | 27.40 ± 7.04 ** (6.5) |
| +TP-3654 | 300 | 2.34 ± 0.50 (1.1) | 34.31 ± 5.22 ** (5.2) |
| +TP-3654 | 500 | 2.55 ± 0.55 (1.0) | 25.26 ± 4.19 ** (7.0) |
| +Ko143 | 1000 | 2.73 ± 0.76 (1.0) | 9.35 ± 1.76 *** (19.0) |
| (nM) | (nM) | ||
| Mitoxantrone | - | 4.28 ± 0.39 (1.0) | 114.49 ± 9.59 (1.0) |
| +TP-3654 | 100 | 3.88 ± 0.29 (1.1) | 45.56 ± 5.97 *** (2.5) |
| +TP-3654 | 200 | 4.02 ± 0.33 (1.1) | 28.76 ± 4.28 *** (4.0) |
| +TP-3654 | 300 | 3.98 ± 0.38 (1.1) | 29.92 ± 5.17 *** (3.8) |
| +TP-3654 | 500 | 4.20 ± 0.36 (1.0) | 19.06 ± 3.83 *** (6.0) |
| +Ko143 | 1000 | 4.15 ± 0.48 (1.0) | 12.88 ± 1.79 *** (8.9) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wu, C.-P.; Li, Y.-Q.; Chi, Y.-C.; Huang, Y.-H.; Hung, T.-H.; Wu, Y.-S. The Second-Generation PIM Kinase Inhibitor TP-3654 Resensitizes ABCG2-Overexpressing Multidrug-Resistant Cancer Cells to Cytotoxic Anticancer Drugs. Int. J. Mol. Sci. 2021, 22, 9440. https://doi.org/10.3390/ijms22179440
Wu C-P, Li Y-Q, Chi Y-C, Huang Y-H, Hung T-H, Wu Y-S. The Second-Generation PIM Kinase Inhibitor TP-3654 Resensitizes ABCG2-Overexpressing Multidrug-Resistant Cancer Cells to Cytotoxic Anticancer Drugs. International Journal of Molecular Sciences. 2021; 22(17):9440. https://doi.org/10.3390/ijms22179440
Chicago/Turabian StyleWu, Chung-Pu, Yan-Qing Li, Ya-Chen Chi, Yang-Hui Huang, Tai-Ho Hung, and Yu-Shan Wu. 2021. "The Second-Generation PIM Kinase Inhibitor TP-3654 Resensitizes ABCG2-Overexpressing Multidrug-Resistant Cancer Cells to Cytotoxic Anticancer Drugs" International Journal of Molecular Sciences 22, no. 17: 9440. https://doi.org/10.3390/ijms22179440
APA StyleWu, C.-P., Li, Y.-Q., Chi, Y.-C., Huang, Y.-H., Hung, T.-H., & Wu, Y.-S. (2021). The Second-Generation PIM Kinase Inhibitor TP-3654 Resensitizes ABCG2-Overexpressing Multidrug-Resistant Cancer Cells to Cytotoxic Anticancer Drugs. International Journal of Molecular Sciences, 22(17), 9440. https://doi.org/10.3390/ijms22179440







