Cross-Talks between the Cardiovascular Disease-Sarcopenia-Osteoporosis Triad and Magnesium in Humans
Abstract
:1. Introduction
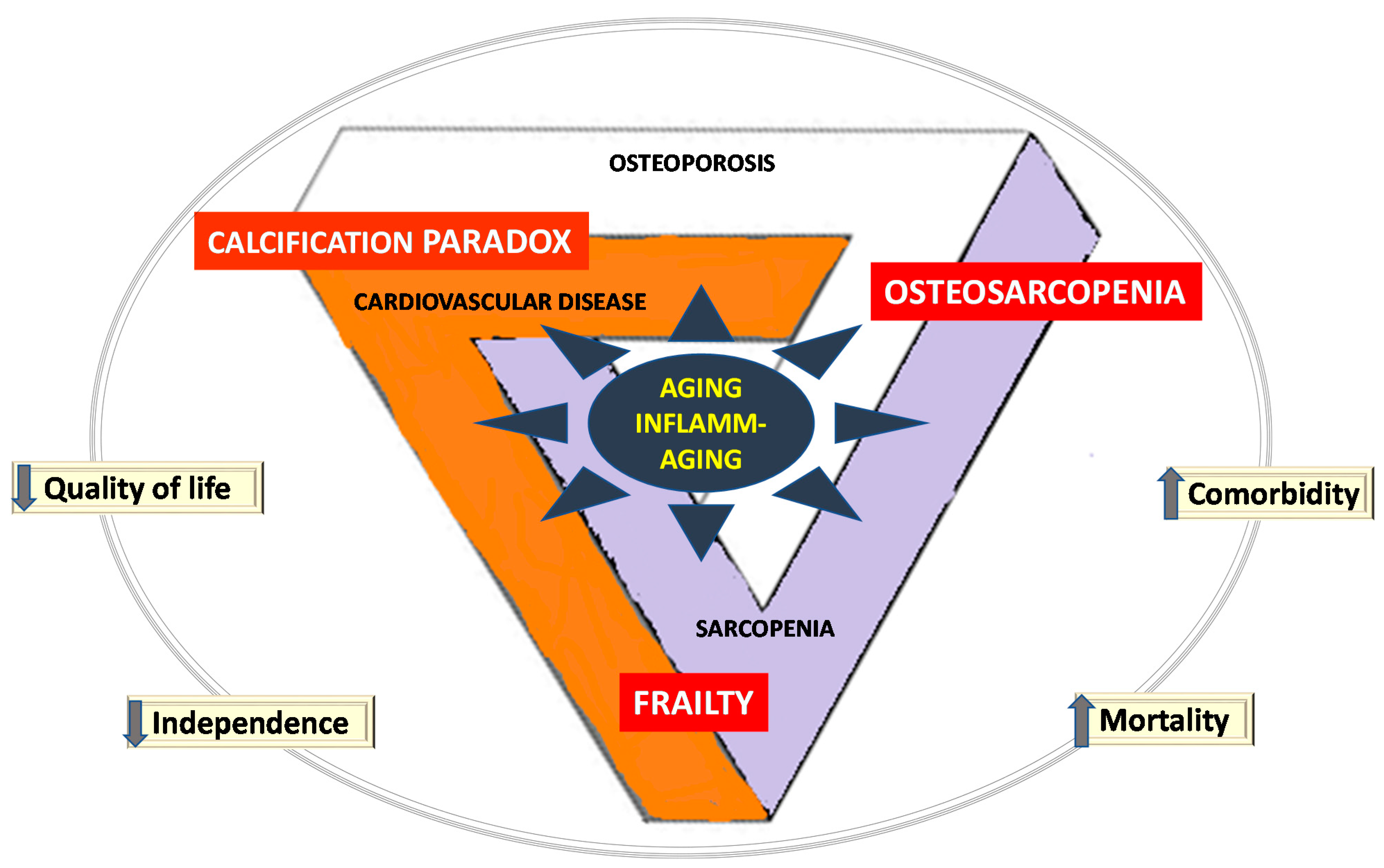
2. The Cardiovascular Disease-Sarcopenia-Osteoporosis Triad
2.1. Cardiovascular Disease
2.2. Sarcopenia
2.3. Osteoporosis
3. Cross Talks in the Cardiovascular Disease-Sarcopenia-Osteoporosis Triad
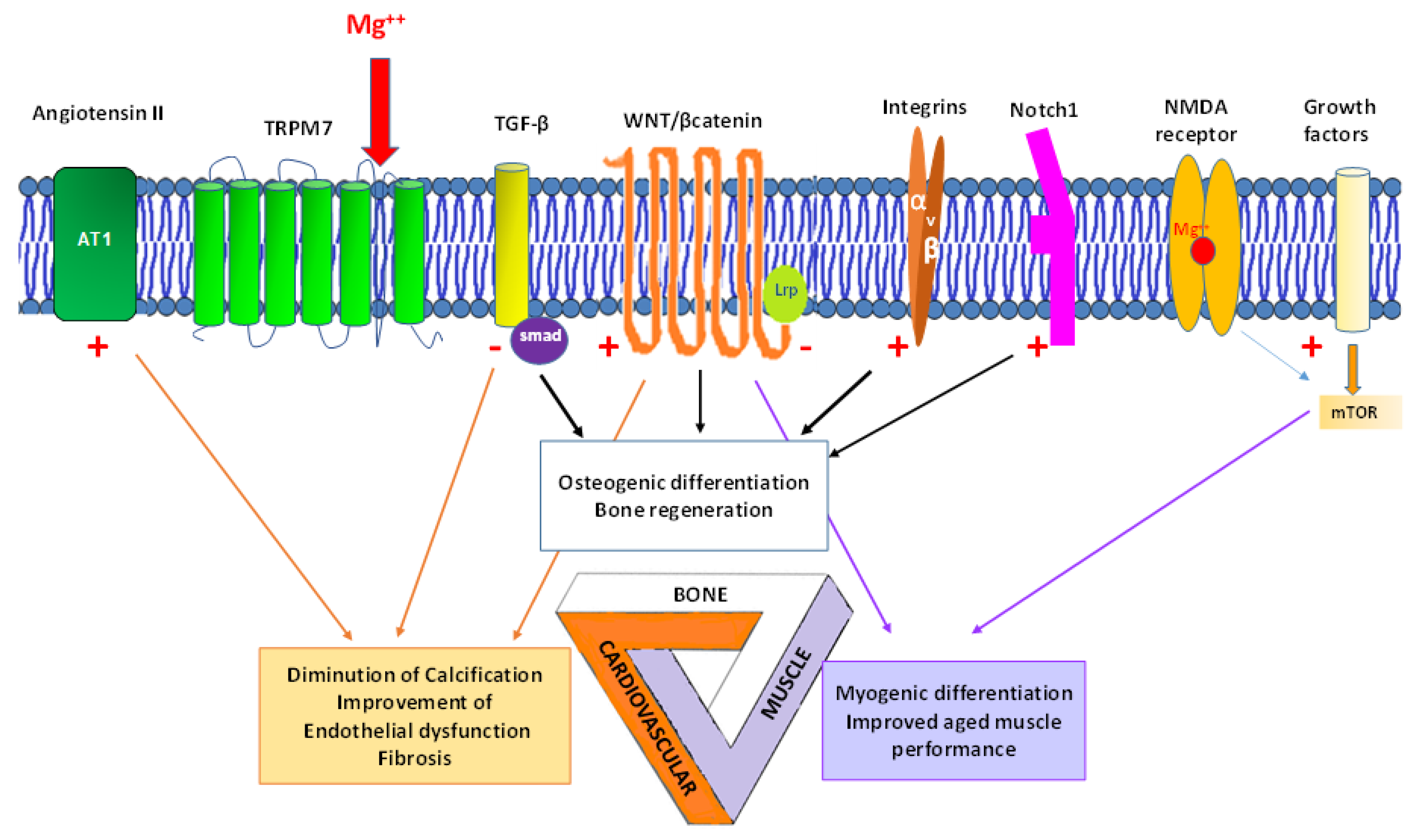
4. Magnesium and the Triad
4.1. Magnesium and Cardiovascular Function
4.2. Magnesium and Muscle
4.3. Magnesium and Bone
5. Prospects of Mg in the Cardiovascular Disease-Sarcopenia-Osteoporosis Triad
6. Perspectives for Future Trials on the Triad
7. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Franceschi, C.; Garagnani, P.; Morsiani, C.; Conte, M.; Santoro, A.; Grignolio, A.; Monti, D.; Capri, M.; Salvioli, S. The Continuum of Aging and Age-Related Diseases: Common Mechanisms but Different Rates. Front. Med. 2018, 5, 61. [Google Scholar] [CrossRef] [Green Version]
- Rodriguez, A.J.; Scott, D.; Ebeling, P.R. Exploring the Links Between Common Diseases of Ageing—Osteoporosis, Sarcopenia and Vascular Calcification. Clinic. Rev. Bone Miner. Metab. 2019, 17, 1–23. [Google Scholar] [CrossRef]
- Porter, J.L.; Varacallo, M. Osteoporosis. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2021. [Google Scholar]
- Compston, J.E.; McClung, M.R.; Leslie, W.D. Osteoporosis. Lancet 2019, 393, 364–376. [Google Scholar] [CrossRef]
- Castiglioni, S.; Cazzaniga, A.; Albisetti, W.; Maier, J.A.M. Magnesium and Osteoporosis: Current State of Knowledge and Future Research Directions. Nutrients 2013, 5, 3022–3033. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cruz-Jentoft, A.J.; Baeyens, J.P.; Bauer, J.M.; Boirie, Y.; Cederholm, T.; Landi, F.; Martin, F.C.; Michel, J.-P.; Rolland, Y.; Schneider, S.M.; et al. Sarcopenia: European Consensus on Definition and Diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing 2010, 39, 412–423. [Google Scholar] [CrossRef] [Green Version]
- Cruz-Jentoft, A.J.; Bahat, G.; Bauer, J.; Boirie, Y.; Bruyère, O.; Cederholm, T.; Cooper, C.; Landi, F.; Rolland, Y.; Sayer, A.A.; et al. Sarcopenia: Revised European Consensus on Definition and Diagnosis. Age Ageing 2019, 48, 16–31. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ganapathy, A.; Nieves, J.W. Nutrition and Sarcopenia-What Do We Know? Nutrients 2020, 12, 1755. [Google Scholar] [CrossRef]
- Welch, A.A.; Skinner, J.; Hickson, M. Dietary Magnesium May Be Protective for Aging of Bone and Skeletal Muscle in Middle and Younger Older Age Men and Women: Cross-Sectional Findings from the UK Biobank Cohort. Nutrients 2017, 9, 1189. [Google Scholar] [CrossRef] [Green Version]
- Dominguez, L.J.; Barbagallo, M. The Biology of the Metabolic Syndrome and Aging. Curr. Opin. Clin. Nutr. Metab. Care 2016, 19, 5–11. [Google Scholar] [CrossRef]
- Szulc, P.; Samelson, E.J.; Sornay-Rendu, E.; Chapurlat, R.; Kiel, D.P. Severity of Aortic Calcification Is Positively Associated with Vertebral Fracture in Older Men--a Densitometry Study in the STRAMBO Cohort. Osteoporos. Int. 2013, 24, 1177–1184. [Google Scholar] [CrossRef] [Green Version]
- Thompson, B.; Towler, D.A. Arterial Calcification and Bone Physiology: Role of the Bone-Vascular Axis. Nat. Rev. Endocrinol. 2012, 8, 529–543. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Szulc, P.; Maurice, C.; Marchand, F.; Delmas, P.D. Increased Bone Resorption Is Associated with Higher Mortality in Community-Dwelling Men >or=50 Years of Age: The MINOS Study. J. Bone Miner. Res. 2009, 24, 1116–1124. [Google Scholar] [CrossRef] [PubMed]
- Wiklund, P.; Nordström, A.; Jansson, J.-H.; Weinehall, L.; Nordström, P. Low Bone Mineral Density Is Associated with Increased Risk for Myocardial Infarction in Men and Women. Osteoporos. Int. 2012, 23, 963–970. [Google Scholar] [CrossRef] [Green Version]
- Muñoz-Garach, A.; García-Fontana, B.; Muñoz-Torres, M. Nutrients and Dietary Patterns Related to Osteoporosis. Nutrients 2020, 12, 1986. [Google Scholar] [CrossRef]
- Pickering, G.; Mazur, A.; Trousselard, M.; Bienkowski, P.; Yaltsewa, N.; Amessou, M.; Noah, L.; Pouteau, E. Magnesium Status and Stress: The Vicious Circle Concept Revisited. Nutrients 2020, 12, 3672. [Google Scholar] [CrossRef]
- Office of Dietary Supplements-Magnesium. Available online: https://ods.od.nih.gov/factsheets/Magnesium-HealthProfessional/ (accessed on 23 August 2021).
- Veronese, N.; Barbagallo, M. Magnesium and Micro-Elements in Older Persons. Nutrients 2021, 13, 847. [Google Scholar] [CrossRef]
- Barbagallo, M.; Veronese, N.; Dominguez, L.J. Magnesium in Aging, Health and Diseases. Nutrients 2021, 13, 463. [Google Scholar] [CrossRef]
- Franceschi, C.; Garagnani, P.; Parini, P.; Giuliani, C.; Santoro, A. Inflammaging: A New Immune-Metabolic Viewpoint for Age-Related Diseases. Nat. Rev. Endocrinol. 2018, 14, 576–590. [Google Scholar] [CrossRef] [PubMed]
- Hirschfeld, H.P.; Kinsella, R.; Duque, G. Osteosarcopenia: Where Bone, Muscle, and Fat Collide. Osteoporos. Int. 2017, 28, 2781–2790. [Google Scholar] [CrossRef]
- Wang, Y.; Xiao, X.; Zhou, T.; Han, D.; Dong, N. Novel Mechanisms for Osteogenic Differentiation of Human Aortic Valve Interstitial Cells. J. Thorac. Cardiovasc. Surg. 2020, 159, 1742–1753.e7. [Google Scholar] [CrossRef]
- Nadruz, W.; Kitzman, D.; Windham, B.G.; Kucharska-Newton, A.; Butler, K.; Palta, P.; Griswold, M.E.; Wagenknecht, L.E.; Heiss, G.; Solomon, S.D.; et al. Cardiovascular Dysfunction and Frailty Among Older Adults in the Community: The ARIC Study. J. Gerontol. A Biol. Sci. Med. Sci. 2017, 72, 958–964. [Google Scholar] [CrossRef] [Green Version]
- Lind, L.; Sundström, J.; Ärnlöv, J.; Lampa, E. Impact of Aging on the Strength of Cardiovascular Risk Factors: A Longitudinal Study Over 40 Years. J. Am. Heart Assoc. 2018, 7, e007061. [Google Scholar] [CrossRef] [Green Version]
- Hypertension. Available online: https://www.who.int/westernpacific/health-topics/hypertension (accessed on 23 August 2021).
- Saheera, S.; Krishnamurthy, P. Cardiovascular Changes Associated with Hypertensive Heart Disease and Aging. Cell Transplant. 2020, 29, 963689720920830. [Google Scholar] [CrossRef] [PubMed]
- Godo, S.; Shimokawa, H. Endothelial Functions. Arterioscler. Thromb. Vasc. Biol. 2017, 37, e108–e114. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Leite, A.R.; Borges-Canha, M.; Cardoso, R.; Neves, J.S.; Castro-Ferreira, R.; Leite-Moreira, A. Novel Biomarkers for Evaluation of Endothelial Dysfunction. Angiology 2020, 71, 397–410. [Google Scholar] [CrossRef]
- Mikael, L.D.R.; Paiva, A.M.G.D.; Gomes, M.M.; Sousa, A.L.L.; Jardim, P.C.B.V.; Vitorino, P.V.D.O.; Euzébio, M.B.; Sousa, W.D.M.; Barroso, W.K.S. Vascular Aging and Arterial Stiffness. Arq. Bras. Cardiol. 2017, 109, 253–258. [Google Scholar] [CrossRef] [PubMed]
- Nishiga, M.; Wang, D.W.; Han, Y.; Lewis, D.B.; Wu, J.C. COVID-19 and Cardiovascular Disease: From Basic Mechanisms to Clinical Perspectives. Nat. Rev. Cardiol. 2020, 17, 543–558. [Google Scholar] [CrossRef]
- Rizzoli, R.; Reginster, J.-Y.; Arnal, J.-F.; Bautmans, I.; Beaudart, C.; Bischoff-Ferrari, H.; Biver, E.; Boonen, S.; Brandi, M.-L.; Chines, A.; et al. Quality of Life in Sarcopenia and Frailty. Calcif. Tissue Int. 2013, 93, 101–120. [Google Scholar] [CrossRef]
- Pickering, M.-E.; Chapurlat, R. Where Two Common Conditions of Aging Meet: Osteoarthritis and Sarcopenia. Calcif. Tissue Int. 2020, 107, 203–211. [Google Scholar] [CrossRef]
- Cruz-Jentoft, A.J.; Landi, F.; Schneider, S.M.; Zúñiga, C.; Arai, H.; Boirie, Y.; Chen, L.-K.; Fielding, R.A.; Martin, F.C.; Michel, J.-P.; et al. Prevalence of and Interventions for Sarcopenia in Ageing Adults: A Systematic Review. Report of the International Sarcopenia Initiative (EWGSOP and IWGS). Age Ageing 2014, 43, 748–759. [Google Scholar] [CrossRef]
- Jeon, Y.K.; Shin, M.J.; Saini, S.K.; Custodero, C.; Aggarwal, M.; Anton, S.D.; Leeuwenburgh, C.; Mankowski, R.T. Vascular Dysfunction as a Potential Culprit of Sarcopenia. Exp. Gerontol. 2021, 145, 111220. [Google Scholar] [CrossRef]
- Wang, P.-Y.; Li, Y.; Wang, Q. Sarcopenia: An Underlying Treatment Target during the COVID-19 Pandemic. Nutrition 2021, 84, 111104. [Google Scholar] [CrossRef]
- Bellanti, F.; Lo Buglio, A.; Vendemiale, G. Mitochondrial Impairment in Sarcopenia. Biology 2021, 10, 31. [Google Scholar] [CrossRef]
- Reginster, J.-Y.; Beaudart, C.; Al-Daghri, N.; Avouac, B.; Bauer, J.; Bere, N.; Bruyère, O.; Cerreta, F.; Cesari, M.; Rosa, M.M.; et al. Update on the ESCEO Recommendation for the Conduct of Clinical Trials for Drugs Aiming at the Treatment of Sarcopenia in Older Adults. Aging Clin. Exp. Res. 2021, 33, 3–17. [Google Scholar] [CrossRef]
- Marrinan, S.; Pearce, M.S.; Jiang, X.Y.; Waters, S.; Shanshal, Y. Admission for Osteoporotic Pelvic Fractures and Predictors of Length of Hospital Stay, Mortality and Loss of Independence. Age Ageing 2015, 44, 258–261. [Google Scholar] [CrossRef] [Green Version]
- Reginster, J.-Y. Antifracture Efficacy of Currently Available Therapies for Postmenopausal Osteoporosis. Drugs 2011, 71, 65–78. [Google Scholar] [CrossRef] [PubMed]
- Yu, E.W.; Tsourdi, E.; Clarke, B.L.; Bauer, D.C.; Drake, M.T. Osteoporosis Management in the Era of COVID-19. J. Bone Miner. Res. 2020, 35, 1009–1013. [Google Scholar] [CrossRef]
- Lampropoulos, C.E.; Papaioannou, I.; D’Cruz, D.P. Osteoporosis—A Risk Factor for Cardiovascular Disease? Nat. Rev. Rheumatol. 2012, 8, 587–598. [Google Scholar] [CrossRef] [PubMed]
- Deligiorgi, M.V.; Panayiotidis, M.I.; Siasos, G.; Trafalis, D.T. Osteoporosis Entwined with Cardiovascular Disease: The Implication of Osteoprotegerin and the Example of Statins. Curr. Med. Chem. 2021, 28, 1443–1467. [Google Scholar] [CrossRef]
- Rodríguez, A.J.; Lewis, J.R.; Scott, D.S.; Kiel, D.P.; Schousboe, J.T.; Ebeling, P.R.; Prince, R.L. Aortic Calcification Is Associated with Five-Year Decline in Handgrip Strength in Older Women. Calcif. Tissue Int. 2018, 103, 589–598. [Google Scholar] [CrossRef]
- Lena, A.; Anker, M.S.; Springer, J. Muscle Wasting and Sarcopenia in Heart Failure-The Current State of Science. Int. J. Mol. Sci. 2020, 21, 6549. [Google Scholar] [CrossRef] [PubMed]
- Clynes, M.A.; Gregson, C.L.; Bruyère, O.; Cooper, C.; Dennison, E.M. Osteosarcopenia: Where Osteoporosis and Sarcopenia Collide. Rheumatology 2021, 60, 529–537. [Google Scholar] [CrossRef] [PubMed]
- Soysal, P.; Arik, F.; Smith, L.; Jackson, S.E.; Isik, A.T. Inflammation, Frailty and Cardiovascular Disease. Adv. Exp. Med. Biol. 2020, 1216, 55–64. [Google Scholar] [CrossRef] [Green Version]
- Greco, E.A.; Pietschmann, P.; Migliaccio, S. Osteoporosis and Sarcopenia Increase Frailty Syndrome in the Elderly. Front. Endocrinol. 2019, 10, 255. [Google Scholar] [CrossRef]
- Thompson, M.Q.; Yu, S.; Tucker, G.R.; Adams, R.J.; Cesari, M.; Theou, O.; Visvanathan, R. Frailty and Sarcopenia in Combination Are More Predictive of Mortality than Either Condition Alone. Maturitas 2021, 144, 102–107. [Google Scholar] [CrossRef]
- Liberale, L.; Montecucco, F.; Tardif, J.-C.; Libby, P.; Camici, G.G. Inflamm-Ageing: The Role of Inflammation in Age-Dependent Cardiovascular Disease. Eur. Heart J. 2020, 41, 2974–2982. [Google Scholar] [CrossRef]
- Hung, C.-C.; Chaya, A.; Liu, K.; Verdelis, K.; Sfeir, C. The Role of Magnesium Ions in Bone Regeneration Involves the Canonical Wnt Signaling Pathway. Acta Biomater. 2019, 98, 246–255. [Google Scholar] [CrossRef]
- Nie, X.; Sun, X.; Wang, C.; Yang, J. Effect of Magnesium Ions/Type I Collagen Promote the Biological Behavior of Osteoblasts and Its Mechanism. Regen. Biomater. 2020, 7, 53–61. [Google Scholar] [CrossRef]
- Díaz-Tocados, J.M.; Herencia, C.; Martínez-Moreno, J.M.; Montes de Oca, A.; Rodríguez-Ortiz, M.E.; Vergara, N.; Blanco, A.; Steppan, S.; Almadén, Y.; Rodríguez, M.; et al. Magnesium Chloride Promotes Osteogenesis through Notch Signaling Activation and Expansion of Mesenchymal Stem Cells. Sci. Rep. 2017, 7, 7839. [Google Scholar] [CrossRef] [Green Version]
- Lin, Z.; Shen, D.; Zhou, W.; Zheng, Y.; Kong, T.; Liu, X.; Wu, S.; Chu, P.K.; Zhao, Y.; Wu, J.; et al. Regulation of Extracellular Bioactive Cations in Bone Tissue Microenvironment Induces Favorable Osteoimmune Conditions to Accelerate in Situ Bone Regeneration. Bioact. Mater. 2021, 6, 2315–2330. [Google Scholar] [CrossRef]
- Herencia, C.; Rodríguez-Ortiz, M.E.; Muñoz-Castañeda, J.R.; Martinez-Moreno, J.M.; Canalejo, R.; Montes de Oca, A.; Díaz-Tocados, J.M.; Peralbo-Santaella, E.; Marín, C.; Canalejo, A.; et al. Angiotensin II Prevents Calcification in Vascular Smooth Muscle Cells by Enhancing Magnesium Influx. Eur. J. Clin. Investig. 2015, 45, 1129–1144. [Google Scholar] [CrossRef]
- Montes de Oca, A.; Guerrero, F.; Martinez-Moreno, J.M.; Madueño, J.A.; Herencia, C.; Peralta, A.; Almaden, Y.; Lopez, I.; Aguilera-Tejero, E.; Gundlach, K.; et al. Magnesium Inhibits Wnt/β-Catenin Activity and Reverses the Osteogenic Transformation of Vascular Smooth Muscle Cells. PLoS ONE 2014, 9, e89525. [Google Scholar] [CrossRef]
- Gifford, C.C.; Tang, J.; Costello, A.; Khakoo, N.S.; Nguyen, T.Q.; Goldschmeding, R.; Higgins, P.J.; Samarakoon, R. Negative Regulators of TGF-Β1 Signaling in Renal Fibrosis; Pathological Mechanisms and Novel Therapeutic Opportunities. Clin. Sci. 2021, 135, 275–303. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Wang, Q.; Zhang, Z.; Fu, R.; Zhou, T.; Long, C.; He, T.; Yang, D.; Li, Z.; Peng, S. Magnesium Supplementation Enhances MTOR Signalling to Facilitate Myogenic Differentiation and Improve Aged Muscle Performance. Bone 2021, 146, 115886. [Google Scholar] [CrossRef]
- Pendón-Ruiz de Mier, M.V.; Rodelo-Haad, C.; Díaz-Tocados, J.M.; Muñoz-Castañeda, J.R.; Rodríguez, M. Magnesium: An Old Player Revisited in the Context of CKD-MBD. Clin. Chim. Acta 2020, 501, 53–59. [Google Scholar] [CrossRef]
- Rosique-Esteban, N.; Guasch-Ferré, M.; Hernández-Alonso, P.; Salas-Salvadó, J. Dietary Magnesium and Cardiovascular Disease: A Review with Emphasis in Epidemiological Studies. Nutrients 2018, 10, 168. [Google Scholar] [CrossRef] [Green Version]
- Rosanoff, A.; Costello, R.B.; Johnson, G.H. Effectively Prescribing Oral Magnesium Therapy for Hypertension: A Categorized Systematic Review of 49 Clinical Trials. Nutrients 2021, 13, 195. [Google Scholar] [CrossRef]
- Dibaba, D.T.; Xun, P.; Song, Y.; Rosanoff, A.; Shechter, M.; He, K. The Effect of Magnesium Supplementation on Blood Pressure in Individuals with Insulin Resistance, Prediabetes, or Noncommunicable Chronic Diseases: A Meta-Analysis of Randomized Controlled Trials. Am. J. Clin. Nutr. 2017, 106, 921–929. [Google Scholar] [CrossRef] [Green Version]
- Darooghegi Mofrad, M.; Djafarian, K.; Mozaffari, H.; Shab-Bidar, S. Effect of Magnesium Supplementation on Endothelial Function: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Atherosclerosis 2018, 273, 98–105. [Google Scholar] [CrossRef]
- Montezano, A.C.; Zimmerman, D.; Yusuf, H.; Burger, D.; Chignalia, A.Z.; Wadhera, V.; van Leeuwen, F.N.; Touyz, R.M. Vascular Smooth Muscle Cell Differentiation to an Osteogenic Phenotype Involves TRPM7 Modulation by Magnesium. Hypertension 2010, 56, 453–462. [Google Scholar] [CrossRef] [Green Version]
- Del Gobbo, L.C.; Imamura, F.; Wu, J.H.Y.; de Oliveira Otto, M.C.; Chiuve, S.E.; Mozaffarian, D. Circulating and Dietary Magnesium and Risk of Cardiovascular Disease: A Systematic Review and Meta-Analysis of Prospective Studies. Am. J. Clin. Nutr. 2013, 98, 160–173. [Google Scholar] [CrossRef] [Green Version]
- Zhao, B.; Hu, L.; Dong, Y.; Xu, J.; Wei, Y.; Yu, D.; Xu, J.; Zhang, W. The Effect of Magnesium Intake on Stroke Incidence: A Systematic Review and Meta-Analysis With Trial Sequential Analysis. Front. Neurol. 2019, 10, 852. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Salaminia, S.; Sayehmiri, F.; Angha, P.; Sayehmiri, K.; Motedayen, M. Evaluating the Effect of Magnesium Supplementation and Cardiac Arrhythmias after Acute Coronary Syndrome: A Systematic Review and Meta-Analysis. BMC Cardiovasc. Disord. 2018, 18, 129. [Google Scholar] [CrossRef] [PubMed]
- Bagheri, A.; Naghshi, S.; Sadeghi, O.; Larijani, B.; Esmaillzadeh, A. Total, Dietary, and Supplemental Magnesium Intakes and Risk of All-Cause, Cardiovascular, and Cancer Mortality: A Systematic Review and Dose-Response Meta-Analysis of Prospective Cohort Studies. Adv. Nutr. 2021, 12, 1196–1210. [Google Scholar] [CrossRef]
- Malinowska, J.; Małecka, M.; Ciepiela, O. Variations in Magnesium Concentration Are Associated with Increased Mortality: Study in an Unselected Population of Hospitalized Patients. Nutrients 2020, 12, 1836. [Google Scholar] [CrossRef] [PubMed]
- Fang, X.; Liang, C.; Li, M.; Montgomery, S.; Fall, K.; Aaseth, J.; Cao, Y. Dose-Response Relationship between Dietary Magnesium Intake and Cardiovascular Mortality: A Systematic Review and Dose-Based Meta-Regression Analysis of Prospective Studies. J. Trace Elem. Med. Biol. 2016, 38, 64–73. [Google Scholar] [CrossRef]
- Jiang, L.; He, P.; Chen, J.; Liu, Y.; Liu, D.; Qin, G.; Tan, N. Magnesium Levels in Drinking Water and Coronary Heart Disease Mortality Risk: A Meta-Analysis. Nutrients 2016, 8, 5. [Google Scholar] [CrossRef] [Green Version]
- Massy, Z.A.; Drüeke, T.B. Magnesium and Cardiovascular Complications of Chronic Kidney Disease. Nat. Rev. Nephrol. 2015, 11, 432–442. [Google Scholar] [CrossRef]
- Ye, H.; Cao, P.; Zhang, X.; Lin, J.; Guo, Q.; Mao, H.; Yu, X.; Yang, X. Serum Magnesium and Cardiovascular Mortality in Peritoneal Dialysis Patients: A 5-Year Prospective Cohort Study. Br. J. Nutr. 2018, 120, 415–423. [Google Scholar] [CrossRef] [Green Version]
- Azem, R.; Daou, R.; Bassil, E.; Anvari, E.M.; Taliercio, J.J.; Arrigain, S.; Schold, J.D.; Vachharajani, T.; Nally, J.; Na Khoul, G.N. Serum Magnesium, Mortality and Disease Progression in Chronic Kidney Disease. BMC Nephrol. 2020, 21, 49. [Google Scholar] [CrossRef] [Green Version]
- Cheungpasitporn, W.; Thongprayoon, C.; Bathini, T.; Hansrivijit, P.; Vaitla, P.; Medaura, J.; Vallabhajosyula, S.; Chewcharat, A.; Mao, M.A.; Erickson, S.B. Impact of Admission Serum Magnesium Levels on Long-Term Mortality in Hospitalized Patients. Hosp. Pract. (1995) 2020, 48, 80–85. [Google Scholar] [CrossRef] [PubMed]
- Leenders, N.H.J.; Vermeulen, E.A.; van Ballegooijen, A.J.; Hoekstra, T.; de Vries, R.; Beulens, J.W.; Vervloet, M.G. The Association between Circulating Magnesium and Clinically Relevant Outcomes in Patients with Chronic Kidney Disease: A Systematic Review and Meta-Analysis. Clin. Nutr. 2021, 40, 3133–3147. [Google Scholar] [CrossRef]
- Fan, L.; Zhu, X.; Rosanoff, A.; Costello, R.B.; Yu, C.; Ness, R.; Seidner, D.L.; Murff, H.J.; Roumie, C.L.; Shrubsole, M.J.; et al. Magnesium Depletion Score (MDS) Predicts Risk of Systemic Inflammation and Cardiovascular Mortality among US Adults. J. Nutr. 2021, 151, 2226–2235. [Google Scholar] [CrossRef] [PubMed]
- Gyamlani, G.; Parikh, C.; Kulkarni, A.G. Benefits of Magnesium in Acute Myocardial Infarction: Timing Is Crucial. Am. Heart J. 2000, 139, 703. [Google Scholar] [CrossRef]
- Bechler, K.; Shkirkova, K.; Saver, J.L.; Starkman, S.; Hamilton, S.; Liebeskind, D.S.; Eckstein, M.; Stratton, S.; Pratt, F.; Conwit, R.; et al. The Effect of Early Treatment with Intravenous Magnesium Sulfate on the Incidence of Cardiac Comorbidities in Hospitalized Stroke Patients. Cardiovasc. Ther. 2020, 2020, 1494506. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, F.H.; Milne, D.B.; Klevay, L.M.; Gallagher, S.; Johnson, L. Dietary Magnesium Deficiency Induces Heart Rhythm Changes, Impairs Glucose Tolerance, and Decreases Serum Cholesterol in Post Menopausal Women. J. Am. Coll. Nutr. 2007, 26, 121–132. [Google Scholar] [CrossRef] [PubMed]
- Cunha, A.R.; D’El-Rei, J.; Medeiros, F.; Umbelino, B.; Oigman, W.; Touyz, R.M.; Neves, M.F. Oral Magnesium Supplementation Improves Endothelial Function and Attenuates Subclinical Atherosclerosis in Thiazide-Treated Hypertensive Women. J. Hypertens. 2017, 35, 89–97. [Google Scholar] [CrossRef] [Green Version]
- Onalan, O.; Crystal, E.; Daoulah, A.; Lau, C.; Crystal, A.; Lashevsky, I. Meta-Analysis of Magnesium Therapy for the Acute Management of Rapid Atrial Fibrillation. Am. J. Cardiol. 2007, 99, 1726–1732. [Google Scholar] [CrossRef] [PubMed]
- Chiuve, S.E.; Sun, Q.; Curhan, G.C.; Taylor, E.N.; Spiegelman, D.; Willett, W.C.; Manson, J.E.; Rexrode, K.M.; Albert, C.M. Dietary and Plasma Magnesium and Risk of Coronary Heart Disease among Women. J. Am. Heart Assoc. 2013, 2, e000114. [Google Scholar] [CrossRef] [Green Version]
- Gupta, A.; Lawrence, A.T.; Krishnan, K.; Kavinsky, C.J.; Trohman, R.G. Current Concepts in the Mechanisms and Management of Drug-Induced QT Prolongation and Torsade de Pointes. Am. Heart J. 2007, 153, 891–899. [Google Scholar] [CrossRef]
- Stepura, O.B.; Martynow, A.I. Magnesium Orotate in Severe Congestive Heart Failure (MACH). Int. J. Cardiol. 2009, 131, 293–295. [Google Scholar] [CrossRef]
- Antman, E.M. Magnesium in Coronaries (MAGIC) Trial Investigators Early Administration of Intravenous Magnesium to High-Risk Patients with Acute Myocardial Infarction in the Magnesium in Coronaries (MAGIC) Trial: A Randomised Controlled Trial. Lancet 2002, 360, 1189–1196. [Google Scholar] [CrossRef]
- Collins, R.; Peto, R.; Flather, M.; Parish, S.; Sleight, P.; Conway, M.; Pipilis, A.; Baigent, C.; Barnett, D.; Boissel, J.P.; et al. ISIS-4: A Randomised Factorial Trial Assessing Early Oral Captopril, Oral Mononitrate, and Intravenous Magnesium Sulphate in 58,050 Patients with Suspected Acute Myocardial Infarction. ISIS-4 (Fourth International Study of Infarct Survival) Collaborative Group. Lancet 1995, 345, 669–685. [Google Scholar]
- Ziegelstein, R.C.; Hilbe, J.M.; French, W.J.; Antman, E.M.; Chandra-Strobos, N. Magnesium Use in the Treatment of Acute Myocardial Infarction in the United States (Observations from the Second National Registry of Myocardial Infarction). Am. J. Cardiol. 2001, 87, 7–10. [Google Scholar] [CrossRef]
- Lee, S.Y.; Hyun, Y.Y.; Lee, K.B.; Kim, H. Low Serum Magnesium Is Associated with Coronary Artery Calcification in a Korean Population at Low Risk for Cardiovascular Disease. Nutr. Metab. Cardiovasc. Dis. 2015, 25, 1056–1061. [Google Scholar] [CrossRef]
- Costello, R.B.; Moser-Veillon, P.B. A Review of Magnesium Intake in the Elderly. A Cause for Concern? Magnes. Res. 1992, 5, 61–67. [Google Scholar] [PubMed]
- Pickering, R.T.; Bradlee, M.L.; Singer, M.R.; Moore, L.L. Higher Intakes of Potassium and Magnesium, but Not Lower Sodium, Reduce Cardiovascular Risk in the Framingham Offspring Study. Nutrients 2021, 13, 269. [Google Scholar] [CrossRef] [PubMed]
- Sakaguchi, Y.; Hamano, T.; Obi, Y.; Monden, C.; Oka, T.; Yamaguchi, S.; Matsui, I.; Hashimoto, N.; Matsumoto, A.; Shimada, K.; et al. A Randomized Trial of Magnesium Oxide and Oral Carbon Adsorbent for Coronary Artery Calcification in Predialysis CKD. J. Am. Soc. Nephrol. 2019, 30, 1073–1085. [Google Scholar] [CrossRef]
- Rosanoff, A. Perspective: US Adult Magnesium Requirements Need Updating: Impacts of Rising Body Weights and Data-Derived Variance. Adv. Nutr. 2021, 12, 298–304. [Google Scholar] [CrossRef]
- Marques, B.C.A.A.; Klein, M.R.S.T.; da Cunha, M.R.; de Souza Mattos, S.; de Paula Nogueira, L.; de Paula, T.; Corrêa, F.M.; Oigman, W.; Neves, M.F. Effects of Oral Magnesium Supplementation on Vascular Function: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. High Blood Press Cardiovasc. Prev. 2020, 27, 19–28. [Google Scholar] [CrossRef]
- Song, Y.; Li, T.Y.; van Dam, R.M.; Manson, J.E.; Hu, F.B. Magnesium Intake and Plasma Concentrations of Markers of Systemic Inflammation and Endothelial Dysfunction in Women. Am. J. Clin. Nutr. 2007, 85, 1068–1074. [Google Scholar] [CrossRef]
- Shechter, M.; Sharir, M.; Labrador, M.J.; Forrester, J.; Silver, B.; Bairey Merz, C.N. Oral Magnesium Therapy Improves Endothelial Function in Patients with Coronary Artery Disease. Circulation 2000, 102, 2353–2358. [Google Scholar] [CrossRef] [Green Version]
- Joris, P.J.; Plat, J.; Bakker, S.J.L.; Mensink, R.P. Effects of Long-Term Magnesium Supplementation on Endothelial Function and Cardiometabolic Risk Markers: A Randomized Controlled Trial in Overweight/Obese Adults. Sci. Rep. 2017, 7, 106. [Google Scholar] [CrossRef]
- Barbagallo, M.; Dominguez, L.J.; Galioto, A.; Pineo, A.; Belvedere, M. Oral Magnesium Supplementation Improves Vascular Function in Elderly Diabetic Patients. Magnes. Res. 2010, 23, 131–137. [Google Scholar] [CrossRef]
- Turgut, F.; Kanbay, M.; Metin, M.R.; Uz, E.; Akcay, A.; Covic, A. Magnesium Supplementation Helps to Improve Carotid Intima Media Thickness in Patients on Hemodialysis. Int. Urol. Nephrol. 2008, 40, 1075–1082. [Google Scholar] [CrossRef]
- Mortazavi, M.; Moeinzadeh, F.; Saadatnia, M.; Shahidi, S.; McGee, J.C.; Minagar, A. Effect of Magnesium Supplementation on Carotid Intima-Media Thickness and Flow-Mediated Dilatation among Hemodialysis Patients: A Double-Blind, Randomized, Placebo-Controlled Trial. Eur. Neurol. 2013, 69, 309–316. [Google Scholar] [CrossRef]
- Guerrera, M.P.; Volpe, S.L.; Mao, J.J. Therapeutic Uses of Magnesium. Am. Fam. Physician 2009, 80, 157–162. [Google Scholar]
- Adebamowo, S.N.; Spiegelman, D.; Flint, A.J.; Willett, W.C.; Rexrode, K.M. Intakes of Magnesium, Potassium, and Calcium and the Risk of Stroke among Men. Int. J. Stroke 2015, 10, 1093–1100. [Google Scholar] [CrossRef] [PubMed]
- Veronese, N.; Demurtas, J.; Pesolillo, G.; Celotto, S.; Barnini, T.; Calusi, G.; Caruso, M.G.; Notarnicola, M.; Reddavide, R.; Stubbs, B.; et al. Magnesium and Health Outcomes: An Umbrella Review of Systematic Reviews and Meta-Analyses of Observational and Intervention Studies. Eur. J. Nutr. 2020, 59, 263–272. [Google Scholar] [CrossRef] [PubMed]
- Zhu, H.-L.; Liu, Y.; Zhang, J.; Wang, M.-X.; Jiang, H.; Guo, F.; Li, M.; Qi, F.-F.; Liu, X.-H.; Ma, L. Dietary Calcium, Magnesium, and Phosphorus Intakes and Risk of Stroke in Chinese Adults. Sci. Rep. 2021, 11, 11270. [Google Scholar] [CrossRef] [PubMed]
- Xu, R.; Wang, L.; Sun, L.; Dong, J. Neuroprotective Effect of Magnesium Supplementation on Cerebral Ischemic Diseases. Life Sci. 2021, 272, 119257. [Google Scholar] [CrossRef]
- Muir, K.W.; Lees, K.R.; Ford, I.; Davis, S. Intravenous Magnesium Efficacy in Stroke (IMAGES) Study Investigators Magnesium for Acute Stroke (Intravenous Magnesium Efficacy in Stroke Trial): Randomised Controlled Trial. Lancet 2004, 363, 439–445. [Google Scholar] [CrossRef]
- Saver, J.L.; Starkman, S.; Eckstein, M.; Stratton, S.J.; Pratt, F.D.; Hamilton, S.; Conwit, R.; Liebeskind, D.S.; Sung, G.; Kramer, I.; et al. Prehospital Use of Magnesium Sulfate as Neuroprotection in Acute Stroke. N. Engl. J. Med. 2015, 372, 528–536. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Takeuchi, S.; Kumagai, K.; Toyooka, T.; Otani, N.; Wada, K.; Mori, K. Intravenous Hydrogen Therapy With Intracisternal Magnesium Sulfate Infusion in Severe Aneurysmal Subarachnoid Hemorrhage. Stroke 2021, 52, 20–27. [Google Scholar] [CrossRef] [PubMed]
- Tournadre, A.; Vial, G.; Capel, F.; Soubrier, M.; Boirie, Y. Sarcopenia. Jt. Bone Spine 2019, 86, 309–314. [Google Scholar] [CrossRef] [PubMed]
- Cruz-Jentoft, A.J.; Dawson Hughes, B.; Scott, D.; Sanders, K.M.; Rizzoli, R. Nutritional Strategies for Maintaining Muscle Mass and Strength from Middle Age to Later Life: A Narrative Review. Maturitas 2020, 132, 57–64. [Google Scholar] [CrossRef]
- Kaiser, M.J.; Bauer, J.M.; Rämsch, C.; Uter, W.; Guigoz, Y.; Cederholm, T.; Thomas, D.R.; Anthony, P.S.; Charlton, K.E.; Maggio, M.; et al. Frequency of Malnutrition in Older Adults: A Multinational Perspective Using the Mini Nutritional Assessment. J. Am. Geriatr. Soc. 2010, 58, 1734–1738. [Google Scholar] [CrossRef] [PubMed]
- Bayle, D.; Coudy-Gandilhon, C.; Gueugneau, M.; Castiglioni, S.; Zocchi, M.; Maj-Zurawska, M.; Palinska-Saadi, A.; Mazur, A.; Béchet, D.; Maier, J.A. Magnesium Deficiency Alters Expression of Genes Critical for Muscle Magnesium Homeostasis and Physiology in Mice. Nutrients 2021, 13, 2169. [Google Scholar] [CrossRef]
- Dominguez, L.J.; Barbagallo, M.; Lauretani, F.; Bandinelli, S.; Bos, A.; Corsi, A.M.; Simonsick, E.M.; Ferrucci, L. Magnesium and Muscle Performance in Older Persons: The InCHIANTI Study. Am. J. Clin. Nutr. 2006, 84, 419–426. [Google Scholar] [CrossRef]
- Petermann-Rocha, F.; Chen, M.; Gray, S.R.; Ho, F.K.; Pell, J.P.; Celis-Morales, C. Factors Associated with Sarcopenia: A Cross-Sectional Analysis Using UK Biobank. Maturitas 2020, 133, 60–67. [Google Scholar] [CrossRef] [PubMed]
- Verlaan, S.; Aspray, T.J.; Bauer, J.M.; Cederholm, T.; Hemsworth, J.; Hill, T.R.; McPhee, J.S.; Piasecki, M.; Seal, C.; Sieber, C.C.; et al. Nutritional Status, Body Composition, and Quality of Life in Community-Dwelling Sarcopenic and Non-Sarcopenic Older Adults: A Case-Control Study. Clin. Nutr. 2017, 36, 267–274. [Google Scholar] [CrossRef] [Green Version]
- Welch, A.A.; Kelaiditi, E.; Jennings, A.; Steves, C.J.; Spector, T.D.; MacGregor, A. Dietary Magnesium Is Positively Associated With Skeletal Muscle Power and Indices of Muscle Mass and May Attenuate the Association Between Circulating C-Reactive Protein and Muscle Mass in Women. J. Bone Miner. Res. 2016, 31, 317–325. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Veronese, N.; Berton, L.; Carraro, S.; Bolzetta, F.; De Rui, M.; Perissinotto, E.; Toffanello, E.D.; Bano, G.; Pizzato, S.; Miotto, F.; et al. Effect of Oral Magnesium Supplementation on Physical Performance in Healthy Elderly Women Involved in a Weekly Exercise Program: A Randomized Controlled Trial. Am. J. Clin. Nutr. 2014, 100, 974–981. [Google Scholar] [CrossRef] [Green Version]
- Hayhoe, R.P.G.; Lentjes, M.A.H.; Mulligan, A.A.; Luben, R.N.; Khaw, K.-T.; Welch, A.A. Cross-Sectional Associations of Dietary and Circulating Magnesium with Skeletal Muscle Mass in the EPIC-Norfolk Cohort. Clin. Nutr. 2019, 38, 317–323. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Scott, D.; Blizzard, L.; Fell, J.; Giles, G.; Jones, G. Associations between Dietary Nutrient Intake and Muscle Mass and Strength in Community-Dwelling Older Adults: The Tasmanian Older Adult Cohort Study. J. Am. Geriatr. Soc. 2010, 58, 2129–2134. [Google Scholar] [CrossRef]
- Moradell, A.; Fernández-García, Á.I.; Navarrete-Villanueva, D.; Sagarra-Romero, L.; Gesteiro, E.; Pérez-Gómez, J.; Rodríguez-Gómez, I.; Ara, I.; Casajús, J.A.; Vicente-Rodríguez, G.; et al. Functional Frailty, Dietary Intake, and Risk of Malnutrition. Are Nutrients Involved in Muscle Synthesis the Key for Frailty Prevention? Nutrients 2021, 13, 1231. [Google Scholar] [CrossRef]
- Ter Borg, S.; de Groot, L.C.P.G.M.; Mijnarends, D.M.; de Vries, J.H.M.; Verlaan, S.; Meijboom, S.; Luiking, Y.C.; Schols, J.M.G.A. Differences in Nutrient Intake and Biochemical Nutrient Status Between Sarcopenic and Nonsarcopenic Older Adults-Results From the Maastricht Sarcopenia Study. J. Am. Med. Dir. Assoc. 2016, 17, 393–401. [Google Scholar] [CrossRef] [Green Version]
- Jahnen-Dechent, W.; Ketteler, M. Magnesium Basics. Clin. Kidney J. 2012, 5, i3–i14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Farsinejad-Marj, M.; Saneei, P.; Esmaillzadeh, A. Dietary Magnesium Intake, Bone Mineral Density and Risk of Fracture: A Systematic Review and Meta-Analysis. Osteoporos. Int. 2016, 27, 1389–1399. [Google Scholar] [CrossRef]
- Mederle, O.A.; Balas, M.; Ioanoviciu, S.D.; Gurban, C.-V.; Tudor, A.; Borza, C. Correlations between Bone Turnover Markers, Serum Magnesium and Bone Mass Density in Postmenopausal Osteoporosis. Clin. Interv. Aging 2018, 13, 1383–1389. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Creedon, A.; Flynn, A.; Cashman, K. The Effect of Moderately and Severely Restricted Dietary Magnesium Intakes on Bone Composition and Bone Metabolism in the Rat. Br. J. Nutr. 1999, 82, 63–71. [Google Scholar] [CrossRef] [Green Version]
- Cohen, L.; Kitzes, R. Infrared Spectroscopy and Magnesium Content of Bone Mineral in Osteoporotic Women. Isr. J. Med. Sci. 1981, 17, 1123–1125. [Google Scholar]
- Rude, R.K.; Gruber, H.E.; Wei, L.Y.; Frausto, A.; Mills, B.G. Magnesium Deficiency: Effect on Bone and Mineral Metabolism in the Mouse. Calcif. Tissue Int. 2003, 72, 32–41. [Google Scholar] [CrossRef] [PubMed]
- Rude, R.K.; Kirchen, M.E.; Gruber, H.E.; Meyer, M.H.; Luck, J.S.; Crawford, D.L. Magnesium Deficiency-Induced Osteoporosis in the Rat: Uncoupling of Bone Formation and Bone Resorption. Magnes. Res. 1999, 12, 257–267. [Google Scholar] [PubMed]
- Qi, T.; Weng, J.; Yu, F.; Zhang, W.; Li, G.; Qin, H.; Tan, Z.; Zeng, H. Insights into the Role of Magnesium Ions in Affecting Osteogenic Differentiation of Mesenchymal Stem Cells. Biol. Trace Elem. Res. 2021, 199, 559–567. [Google Scholar] [CrossRef]
- Tsao, Y.-T.; Shih, Y.-Y.; Liu, Y.-A.; Liu, Y.-S.; Lee, O.K. Knockdown of SLC41A1 Magnesium Transporter Promotes Mineralization and Attenuates Magnesium Inhibition during Osteogenesis of Mesenchymal Stromal Cells. Stem Cell Res. Ther. 2017, 8, 39. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Duan, P.; Bonewald, L.F. The Role of the Wnt/β-Catenin Signaling Pathway in Formation and Maintenance of Bone and Teeth. Int. J. Biochem. Cell Biol. 2016, 77, 23–29. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Belluci, M.M.; de Molon, R.S.; Rossa, C.; Tetradis, S.; Giro, G.; Cerri, P.S.; Marcantonio, E.; Orrico, S.R.P. Severe Magnesium Deficiency Compromises Systemic Bone Mineral Density and Aggravates Inflammatory Bone Resorption. J. Nutr. Biochem. 2020, 77, 108301. [Google Scholar] [CrossRef] [PubMed]
- Ciosek, Ż.; Kot, K.; Kosik-Bogacka, D.; Łanocha-Arendarczyk, N.; Rotter, I. The Effects of Calcium, Magnesium, Phosphorus, Fluoride, and Lead on Bone Tissue. Biomolecules 2021, 11, 506. [Google Scholar] [CrossRef] [PubMed]
- Rondanelli, M.; Faliva, M.A.; Tartara, A.; Gasparri, C.; Perna, S.; Infantino, V.; Riva, A.; Petrangolini, G.; Peroni, G. An Update on Magnesium and Bone Health. Biometals 2021, 34, 715–736. [Google Scholar] [CrossRef]
- Okyay, E.; Ertugrul, C.; Acar, B.; Sisman, A.R.; Onvural, B.; Ozaksoy, D. Comparative Evaluation of Serum Levels of Main Minerals and Postmenopausal Osteoporosis. Maturitas 2013, 76, 320–325. [Google Scholar] [CrossRef]
- Mokhtari, Z.; Hekmatdoost, A.; Nourian, M. Antioxidant Efficacy of Vitamin D. J. Parathyr. Dis. 2016, 5, 11–16. [Google Scholar]
- Sharma, R.; Sharma, P.; Kumar, P.; Gupta, G. Role of Magnesium in Post-Menopausal Women with Osteoporosis and Osteopenia. Asian J. Pharm. Clin. Res. 2016, 9, 198–199. [Google Scholar]
- Hayhoe, R.P.G.; Lentjes, M.A.H.; Luben, R.N.; Khaw, K.-T.; Welch, A.A. Dietary Magnesium and Potassium Intakes and Circulating Magnesium Are Associated with Heel Bone Ultrasound Attenuation and Osteoporotic Fracture Risk in the EPIC-Norfolk Cohort Study. Am. J. Clin. Nutr. 2015, 102, 376–384. [Google Scholar] [CrossRef] [Green Version]
- Kunutsor, S.K.; Whitehouse, M.R.; Blom, A.W.; Laukkanen, J.A. Low Serum Magnesium Levels Are Associated with Increased Risk of Fractures: A Long-Term Prospective Cohort Study. Eur. J. Epidemiol. 2017, 32, 593–603. [Google Scholar] [CrossRef] [Green Version]
- Rai, S.P.; Sharma, R. Magnesium as an important marker in post-menopausal women with osteoporosis and osteopenia. Int. J. Pharm. Sci. Invent. ISSN 2016, 5, 1–3. [Google Scholar]
- Wright, H.H.; Kruger, M.C.; Schutte, W.D.; Wentzel-Viljoen, E.; Kruger, I.M.; Kruger, H.S. Magnesium Intake Predicts Bone Turnover in Postmenopausal Black South African Women. Nutrients 2019, 11, 2519. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Orchard, T.S.; Larson, J.C.; Alghothani, N.; Bout-Tabaku, S.; Cauley, J.A.; Chen, Z.; LaCroix, A.Z.; Wactawski-Wende, J.; Jackson, R.D. Magnesium Intake, Bone Mineral Density, and Fractures: Results from the Women’s Health Initiative Observational Study. Am. J. Clin. Nutr. 2014, 99, 926–933. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Veronese, N.; Stubbs, B.; Solmi, M.; Noale, M.; Vaona, A.; Demurtas, J.; Maggi, S. Dietary Magnesium Intake and Fracture Risk: Data from a Large Prospective Study. Br. J. Nutr. 2017, 117, 1570–1576. [Google Scholar] [CrossRef] [Green Version]
- Farrell, V.A.; Harris, M.; Lohman, T.G.; Going, S.B.; Thomson, C.A.; Weber, J.L.; Houtkooper, L.B. Comparison between Dietary Assessment Methods for Determining Associations between Nutrient Intakes and Bone Mineral Density in Postmenopausal Women. J. Am. Diet. Assoc. 2009, 109, 899–904. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gunn, C.A.; Weber, J.L.; Kruger, M.C. Diet, Weight, Cytokines and Bone Health in Postmenopausal Women. J. Nutr. Health Aging 2014, 18, 479–486. [Google Scholar] [CrossRef] [PubMed]
- Stendig-Lindberg, G.; Tepper, R.; Leichter, I. Trabecular Bone Density in a Two Year Controlled Trial of Peroral Magnesium in Osteoporosis. Magnes. Res. 1993, 6, 155–163. [Google Scholar] [PubMed]
- Abraham, G.E.; Grewal, H. A Total Dietary Program Emphasizing Magnesium Instead of Calcium. Effect on the Mineral Density of Calcaneous Bone in Postmenopausal Women on Hormonal Therapy. J. Reprod Med. 1990, 35, 503–507. [Google Scholar] [PubMed]
- Eisinger, J.; Clairet, D. Effects of Silicon, Fluoride, Etidronate and Magnesium on Bone Mineral Density: A Retrospective Study. Magnes. Res. 1993, 6, 247–249. [Google Scholar]
- Aydin, H.; Deyneli, O.; Yavuz, D.; Gözü, H.; Mutlu, N.; Kaygusuz, I.; Akalin, S. Short-Term Oral Magnesium Supplementation Suppresses Bone Turnover in Postmenopausal Osteoporotic Women. Biol. Trace Elem. Res. 2010, 133, 136–143. [Google Scholar] [CrossRef]
- Yeung, S.S.Y.; Reijnierse, E.M.; Pham, V.K.; Trappenburg, M.C.; Lim, W.K.; Meskers, C.G.M.; Maier, A.B. Sarcopenia and Its Association with Falls and Fractures in Older Adults: A Systematic Review and Meta-Analysis. J. Cachexia Sarcopenia Muscle 2019, 10, 485–500. [Google Scholar] [CrossRef] [Green Version]
- Severino, P.; Netti, L.; Mariani, M.V.; Maraone, A.; D’Amato, A.; Scarpati, R.; Infusino, F.; Pucci, M.; Lavalle, C.; Maestrini, V.; et al. Prevention of Cardiovascular Disease: Screening for Magnesium Deficiency. Cardiol. Res. Pract. 2019, 2019, 4874921. [Google Scholar] [CrossRef] [Green Version]
- Morel, V.; Pickering, M.-E.; Goubayon, J.; Djobo, M.; Macian, N.; Pickering, G. Magnesium for Pain Treatment in 2021? State of the Art. Nutrients 2021, 13, 1397. [Google Scholar] [CrossRef]
- Roy, M.E.; Nishimoto, S.K. Matrix Gla Protein Binding to Hydroxyapatite Is Dependent on the Ionic Environment: Calcium Enhances Binding Affinity but Phosphate and Magnesium Decrease Affinity. Bone 2002, 31, 296–302. [Google Scholar] [CrossRef]
- Esses, G.; Deiner, S.; Ko, F.; Khelemsky, Y. Chronic Post-Surgical Pain in the Frail Older Adult. Drugs Aging 2020, 37, 321–329. [Google Scholar] [CrossRef] [PubMed]
- Pickering, M.-E.; Chapurlat, R.; Kocher, L.; Peter-Derex, L. Sleep Disturbances and Osteoarthritis. Pain Pract. 2016, 16, 237–244. [Google Scholar] [CrossRef] [PubMed]
- Bani Younes, M.N. Magnesium Sulfate Extended Infusion as an Adjunctive Treatment for Complicated Covid-19 Infected Critically Ill Patients. EAS J. Anesthesiol. Crti. Care 2020, 2, 97–101. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pickering, M.-E. Cross-Talks between the Cardiovascular Disease-Sarcopenia-Osteoporosis Triad and Magnesium in Humans. Int. J. Mol. Sci. 2021, 22, 9102. https://doi.org/10.3390/ijms22169102
Pickering M-E. Cross-Talks between the Cardiovascular Disease-Sarcopenia-Osteoporosis Triad and Magnesium in Humans. International Journal of Molecular Sciences. 2021; 22(16):9102. https://doi.org/10.3390/ijms22169102
Chicago/Turabian StylePickering, Marie-Eva. 2021. "Cross-Talks between the Cardiovascular Disease-Sarcopenia-Osteoporosis Triad and Magnesium in Humans" International Journal of Molecular Sciences 22, no. 16: 9102. https://doi.org/10.3390/ijms22169102
APA StylePickering, M.-E. (2021). Cross-Talks between the Cardiovascular Disease-Sarcopenia-Osteoporosis Triad and Magnesium in Humans. International Journal of Molecular Sciences, 22(16), 9102. https://doi.org/10.3390/ijms22169102




