Dextran-Curcumin Nanosystems Inhibit Cell Growth and Migration Regulating the Epithelial to Mesenchymal Transition in Prostate Cancer Cells
Abstract
1. Introduction
2. Results
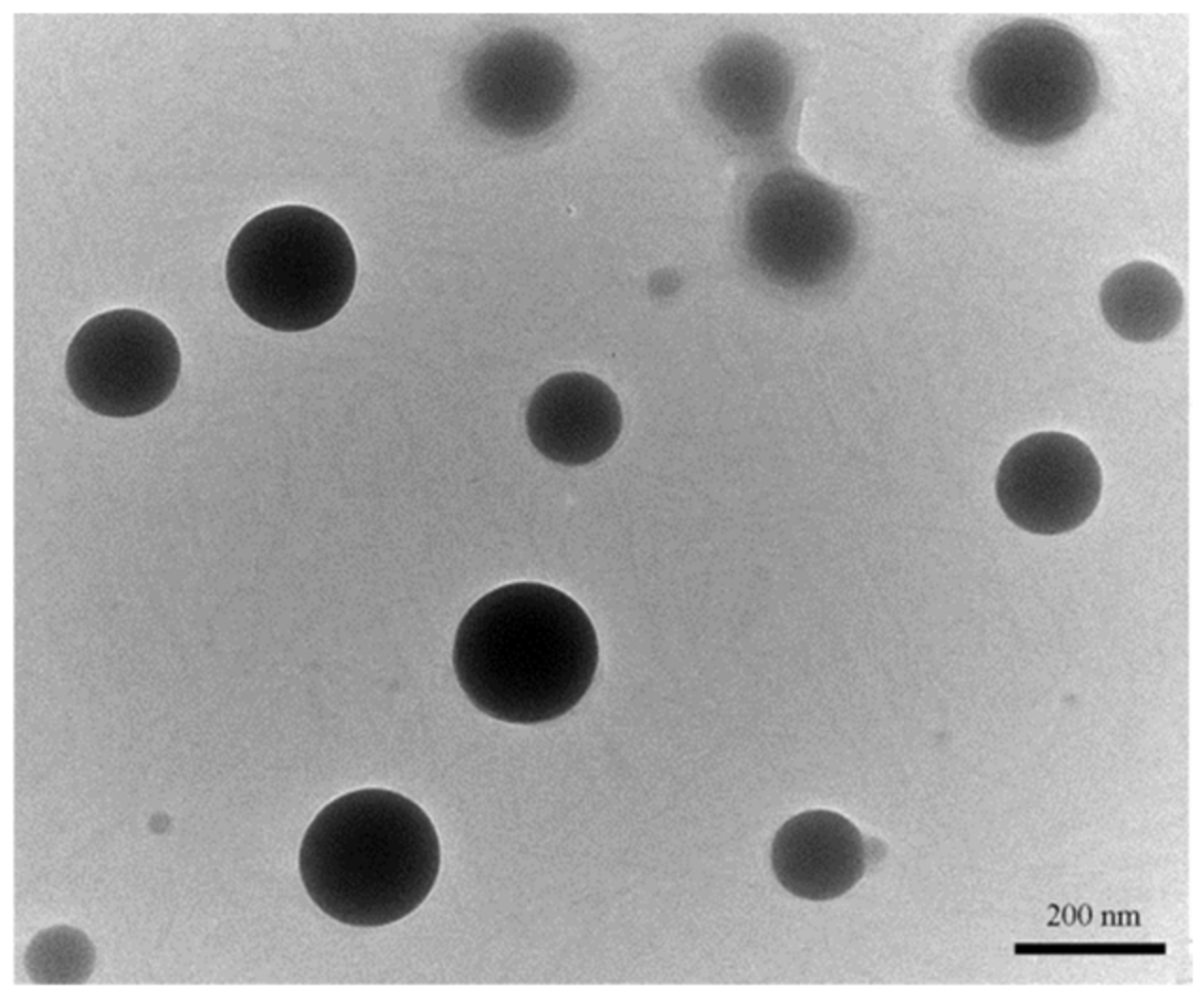
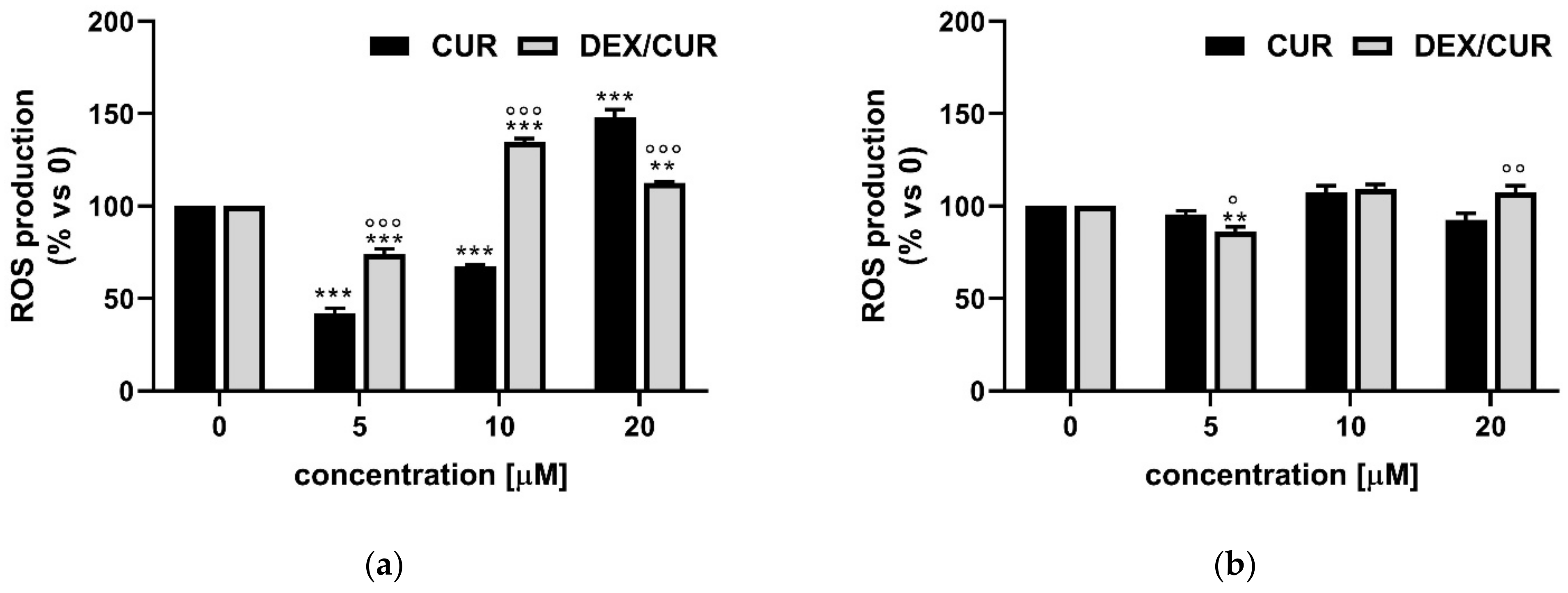
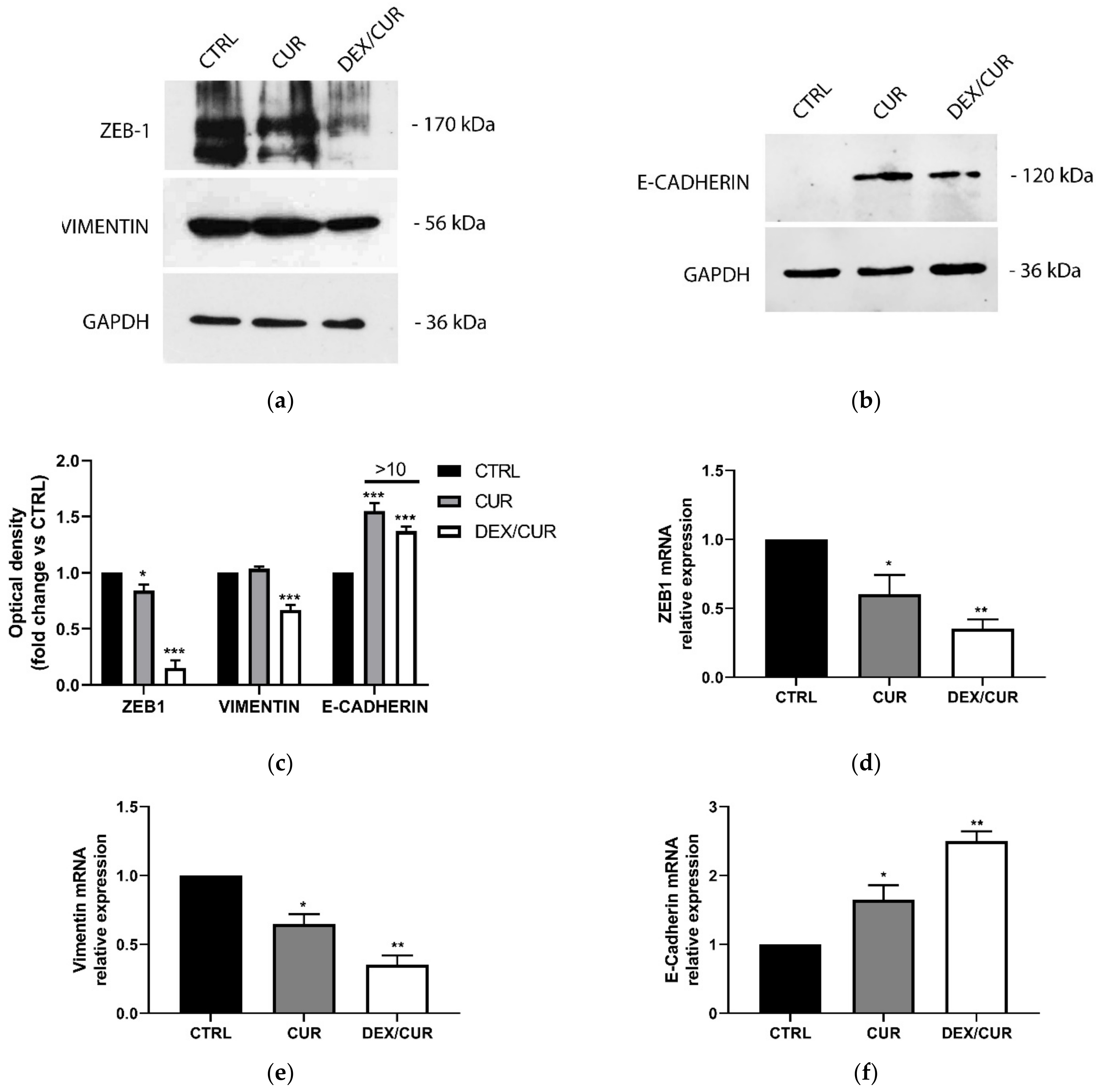
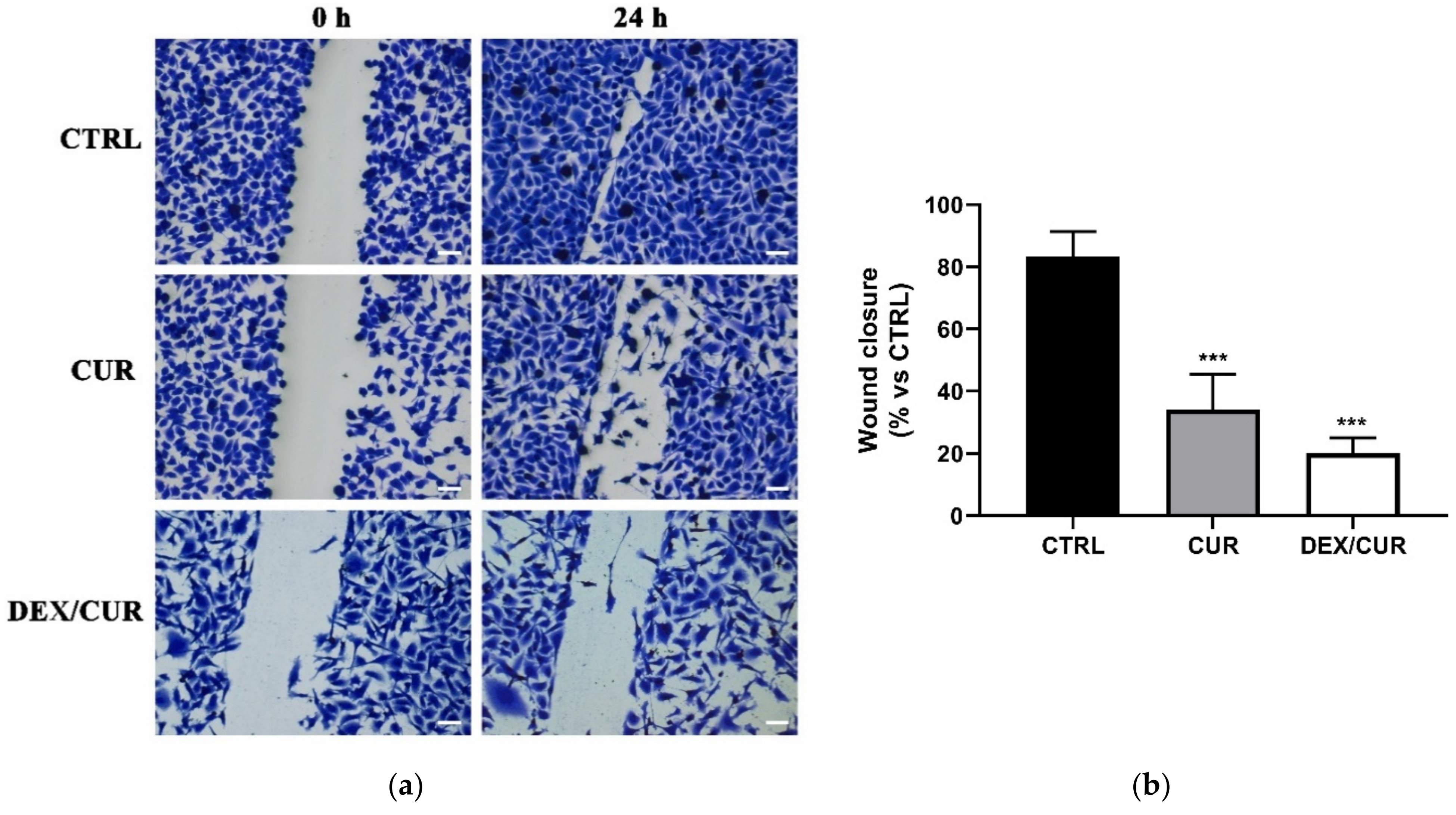
2.1. Biological Characterization of DEX/CUR Conjugate
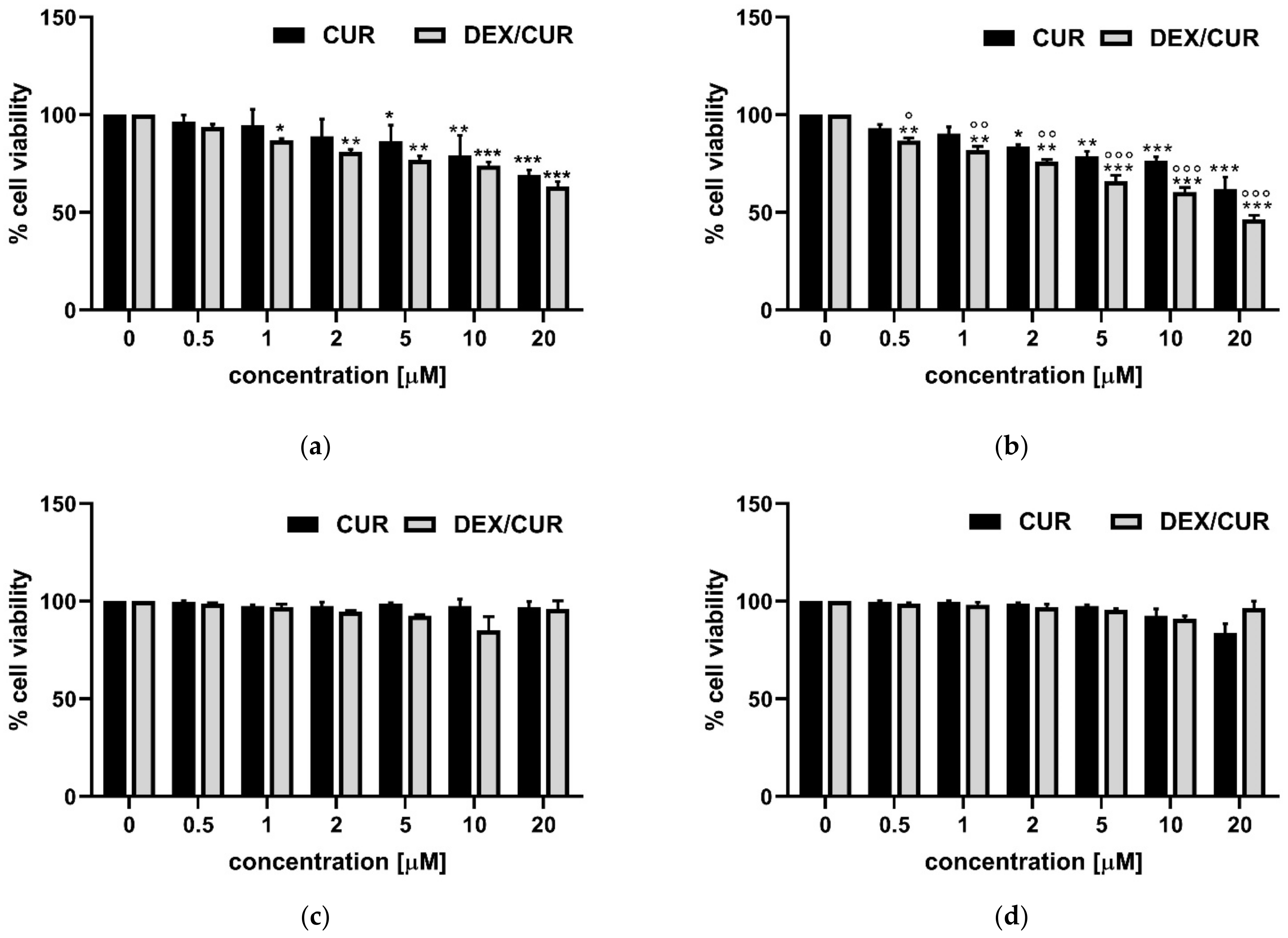
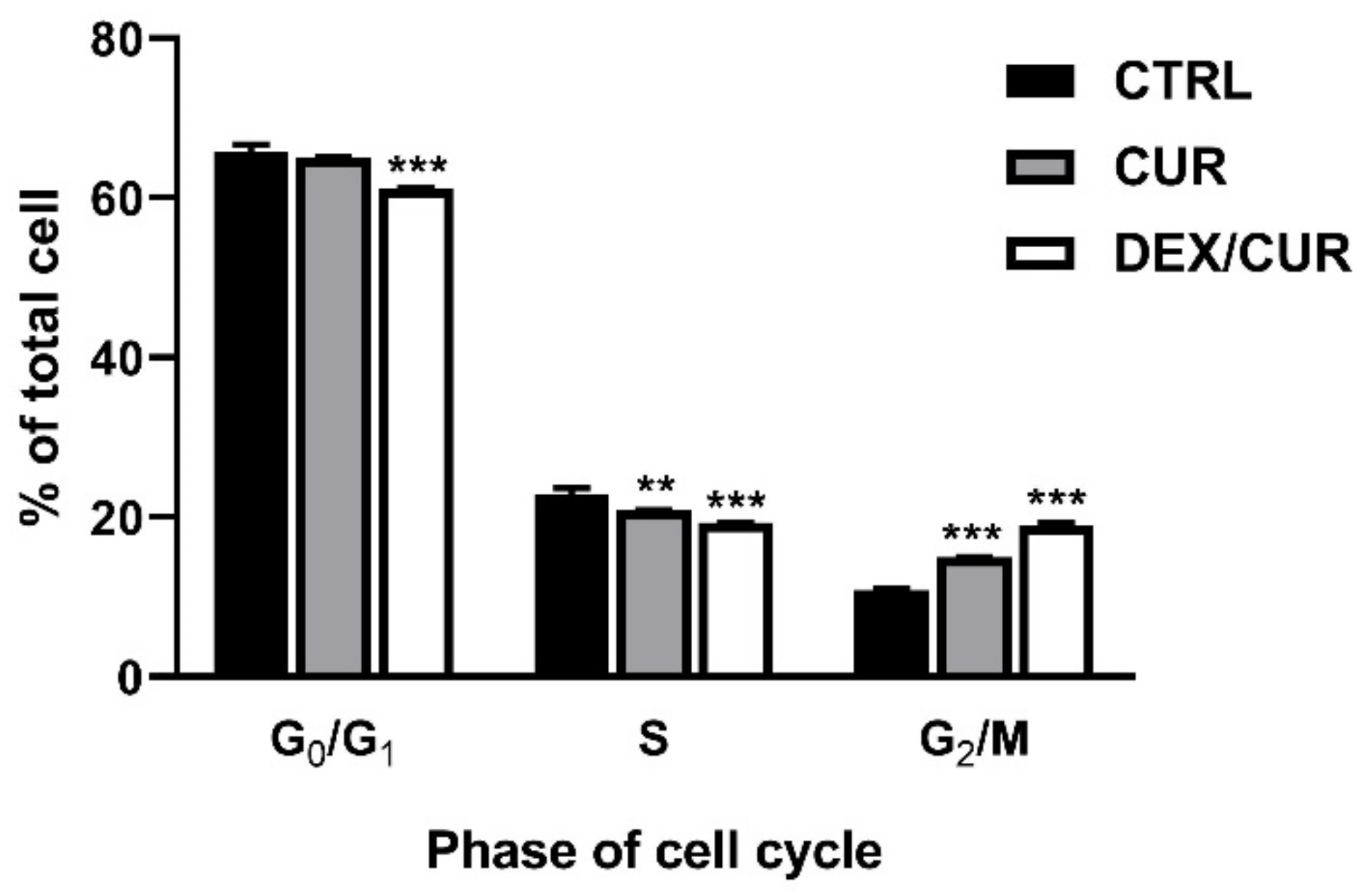
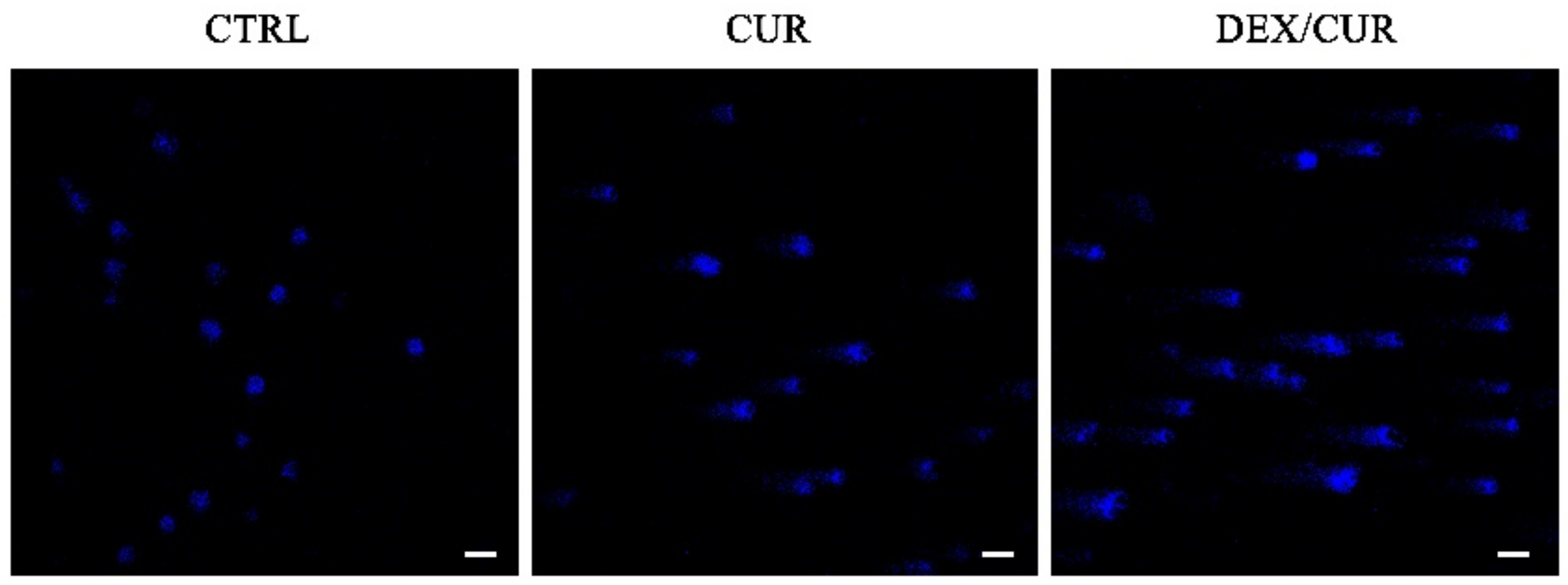
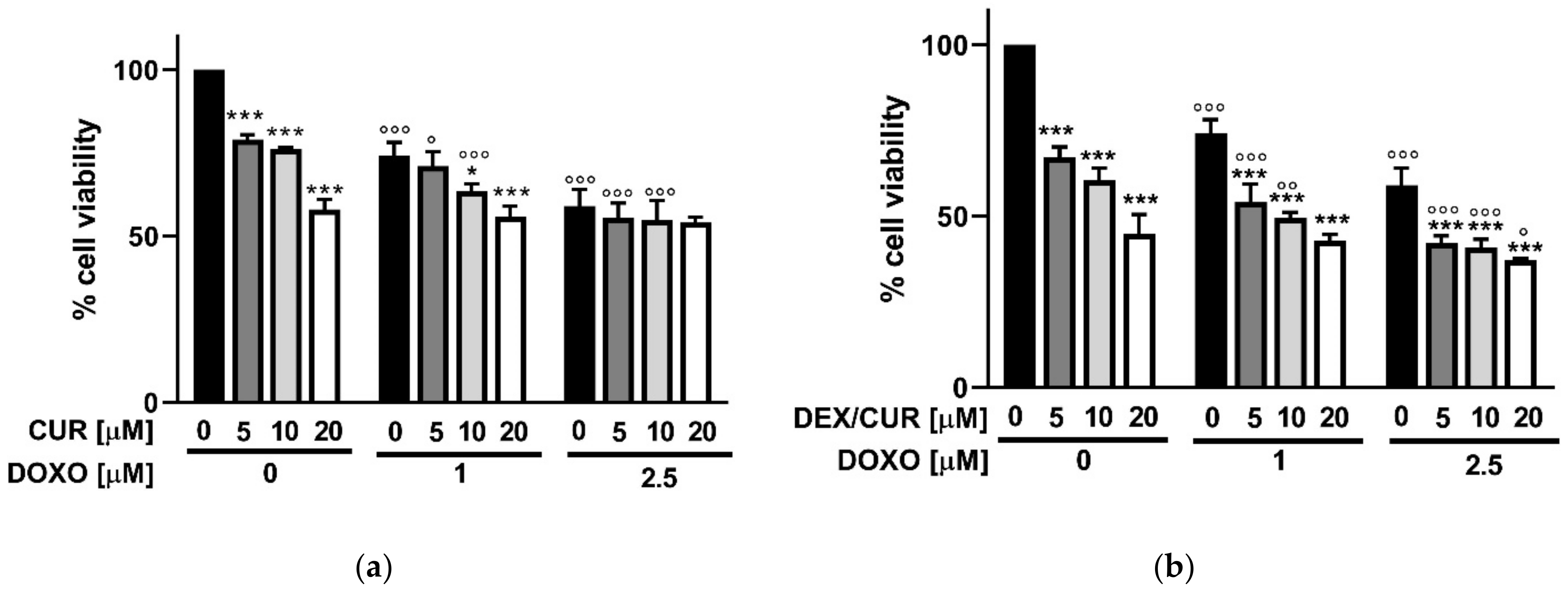
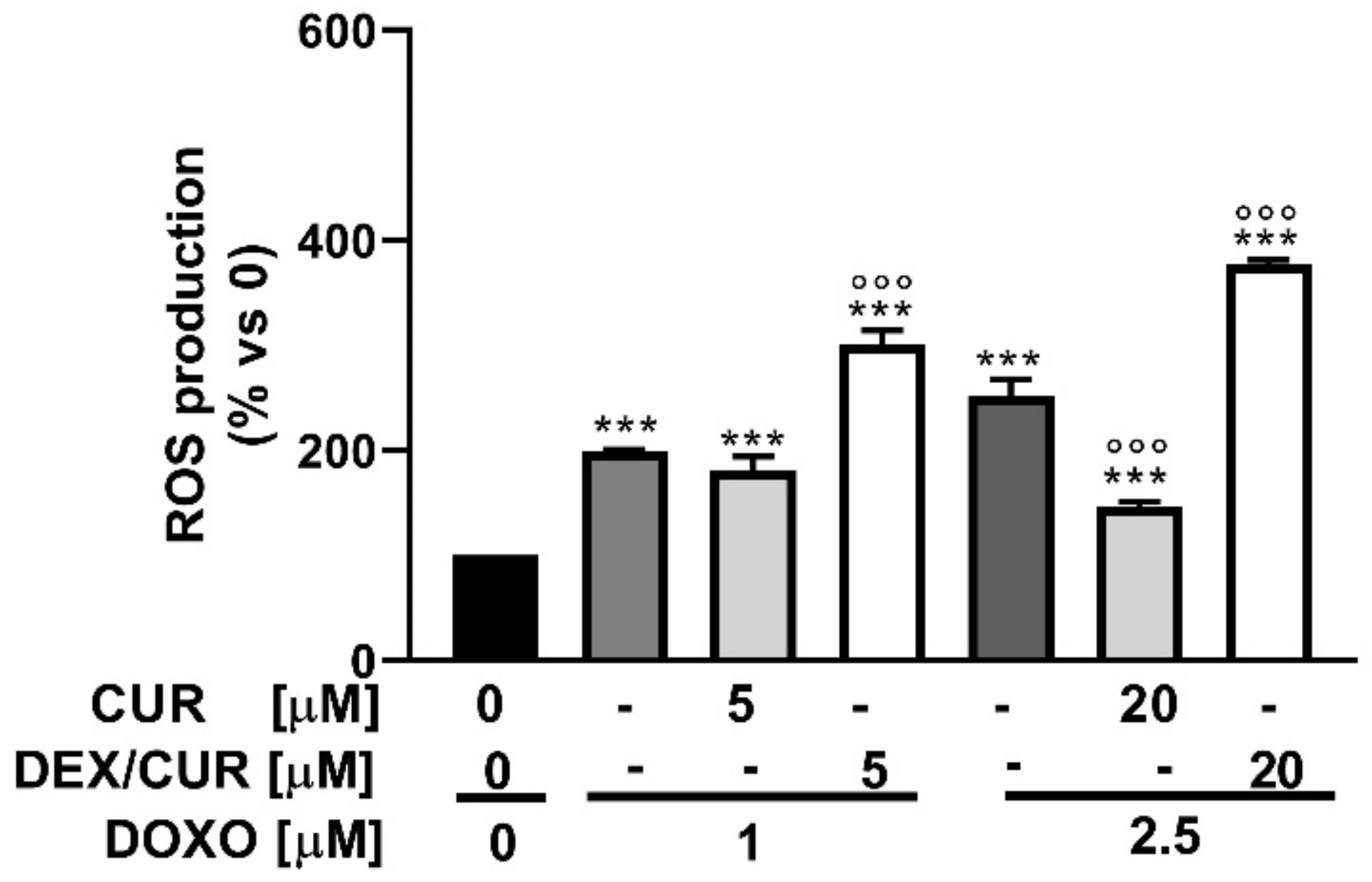
2.2. Curcumin Nanoparticles Increases Sensitivity to Chemotherapy
3. Discussion
4. Materials and Methods
4.1. Cell Culture and Treatments
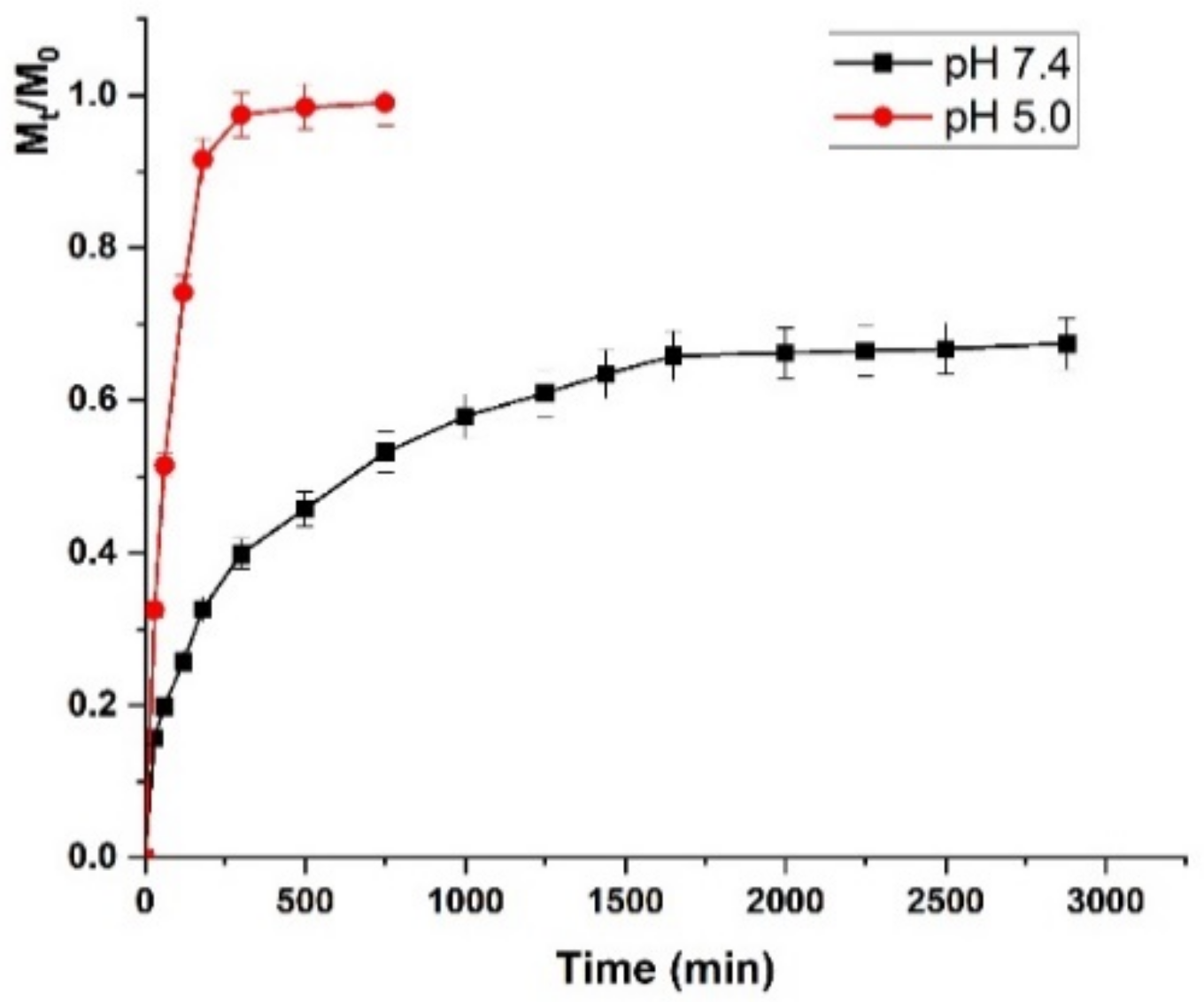
4.2. Synthesis of Doxorubicin Loaded Nanoparticles and Evaluation of Release Profiles
4.3. Cell Viability Assay
4.4. Staining for Confocal Microscopy
4.5. Cell Cycle Analysis
4.6. Comet Assay
4.7. ROS Detection Assay
4.8. Western Blotting Analysis
4.9. RNA Extraction, cDNA Synthesis and qRT-PCR
4.10. Wound Healing Assay
4.11. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer Statistics. CA Cancer J. Clin. 2019, 69, 7–34. [Google Scholar] [CrossRef] [PubMed]
- Hu, H.; Xu, D.F. Co-Delivery of Docetaxel and Retinoic Acid by Poly (Ethylene Glycol)-Retinoic Acid Conjugates Based Micelles for Synergistic Prostate Cancer Therapy. Micro Nano Lett. 2021, 16, 336–343. [Google Scholar] [CrossRef]
- Teo, M.Y.; Rathkopf, D.E.; Kantoff, P. Treatment of Advanced Prostate Cancer. Annu. Rev. Med. 2019, 70, 479–499. [Google Scholar] [CrossRef] [PubMed]
- Dubrovska, A.; Tyutyunnykova, A.; Chen, O.; Linge, A.; Lock, S.; Telychko, V.; Richter, S.; Hein, L.; Toma, M.; Zschaeck, S.; et al. Glutamine Metabolism as Potential Biomarker and Target for Prostate Cancer Radiosensitization. Radiother. Oncol. 2018, 127, S76–S77. [Google Scholar] [CrossRef]
- Liu, Y.; Long, W.; Zhang, Z.T.; Mai, L.X.; Huang, S.J.; Liu, B.J.; Cao, W.F.; Wu, J.H.; Zhou, F.J.; Li, Y.H.; et al. Cytoreductive Radiotherapy Combined with Abiraterone in Metastatic Castration-Resistance Prostate Cancer: A Single Center Experience. Radiat. Oncol. 2021, 16, 5. [Google Scholar] [CrossRef]
- Yamazaki, H.; Masui, K.; Suzuki, G.; Aibe, N.; Shimizu, D.; Kimoto, T.; Yamada, K.; Ueno, A.; Matsugasumi, T.; Yamada, Y.; et al. High-Dose-Rate Brachytherapy with External Beam Radiotherapy Versus Low-Dose-Rate Brachytherapy with or without External Beam Radiotherapy for Clinically Localized Prostate Cancer. Sci. Rep. 2021, 1, 11. [Google Scholar] [CrossRef]
- Dostalova, S.; Polanska, H.; Svobodova, M.; Balvan, J.; Krystofova, O.; Haddad, Y.; Krizkova, S.; Masarik, M.; Eckschlager, T.; Stiborova, M.; et al. Prostate-Specific Membrane Antigen-Targeted Site-Directed Antibody-Conjugated Apoferritin Nanovehicle Favorably Influences in Vivo Side Effects of Doxorubicin. Sci. Rep. 2018, 8, 8867. [Google Scholar] [CrossRef]
- Feng, C.X.; Xiong, Z.Y.; Wang, C.; Xiao, W.; Xiao, H.B.; Xie, K.R.; Chen, K.; Liang, H.G.; Zhang, X.P.; Yang, H.M. Folic Acid-Modified Exosome-Ph20 Enhances the Efficiency of Therapy Via Modulation of the Tumor Microenvironment and Directly Inhibits Tumor Cell Metastasis. Bioact. Mater. 2021, 6, 963–974. [Google Scholar] [CrossRef]
- Negrette-Guzman, M. Combinations of the Antioxidants Sulforaphane or Curcumin and the Conventional Antineoplastics Cisplatin or Doxorubicin as Prospects for Anticancer Chemotherapy. Eur. J. Pharmacol. 2019, 859, 172513. [Google Scholar] [CrossRef]
- Octavia, Y.; Tocchetti, C.G.; Gabrielson, K.L.; Janssens, S.; Crijns, H.J.; Moens, A.L. Doxorubicin-Induced Cardiomyopathy: From Molecular Mechanisms to Therapeutic Strategies. J. Mol. Cell. Cardiol. 2012, 52, 1213–1225. [Google Scholar] [CrossRef]
- Fan, C.M.; Su, Y.W.; Howe, P.R.; Xian, C.J. Long Chain Omega-3 Polyunsaturated Fatty Acid Supplementation Protects against Adriamycin and Cyclophosphamide Chemotherapy-Induced Bone Marrow Damage in Female Rats. Int. J. Mol. Sci. 2018, 19, 484. [Google Scholar] [CrossRef]
- Bai, T.L.; Liu, Y.B.; Li, B.H. Lncrna Loxl1-As1/Mir-Let-7a-5p/Egfr-Related Pathway Regulates the Doxorubicin Resistance of Prostate Cancer Du-145 Cells. IUBMB Life 2019, 71, 1537–1551. [Google Scholar] [CrossRef]
- Cheteh, E.H.; Sarne, V.; Ceder, S.; Bianchi, J.; Augsten, M.; Rundqvist, H.; Egevad, L.; Ostman, A.; Wiman, K.G. Interleukin-6 Derived from Cancer-Associated Fibroblasts Attenuates the P53 Response to Doxorubicin in Prostate Cancer Cells. Cell Death Discov. 2020, 6, 42. [Google Scholar] [CrossRef]
- Vittorio, O.M.; Le Grand, S.A.; Makharza, M.; Curcio, P.; Tucci, F.; Iemma, F.; Nicoletta, P.; Hampel, S.; Cirillo, G. Doxorubicin Synergism and Resistance Reversal in Human Neuroblastoma Be(2)C Cell Lines: An in Vitro Study with Dextran-Catechin Nanohybrids. Eur. J. Pharm. Biopharm. 2018, 122, 176–185. [Google Scholar] [CrossRef]
- Zhao, W.C.; Ning, L.; Wang, L.H.; Ouyang, T.; Qi, L.; Yang, R.H.; Wu, Y.L. Mir-21 Inhibition Reverses Doxorubicin-Resistance and Inhibits Pc3 Human Prostate Cancer Cells Proliferation. Andrologia 2021, 53, e14016. [Google Scholar] [CrossRef]
- Wadhawan, A.; Chatterjee, M.; Singh, G. Present Scenario of Bioconjugates in Cancer Therapy: A Review. Int. J. Mol. Sci. 2019, 20, 5243. [Google Scholar] [CrossRef]
- Zhang, L.H.; Zhang, S.Q.; Li, M.X.; Li, Y.M.; Xiong, H.Y.; Jiang, D.G.; Li, L.J.; Huang, H.; Kang, Y.; Pang, J. Reactive Oxygen Species and Glutathione Dual Responsive Nanoparticles for Enhanced Prostate Cancer Therapy. Mater. Sci. Eng. C Mater. Biol. Appl. 2021, 123, 111956. [Google Scholar] [CrossRef]
- Clyburn, R.D.; Reid, P.; Evans, C.A.; Lefley, D.V.; Holen, I. Increased Anti-Tumour Effects of Doxorubicin and Zoledronic Acid in Prostate Cancer Cells in Vitro: Supporting the Benefits of Combination Therapy. Cancer Chemother. Pharmacol. 2010, 65, 969–978. [Google Scholar] [CrossRef]
- Abedi, F.; Davaran, S.; Hekmati, M.; Akbarzadeh, A.; Baradaran, B.; Moghaddam, V.S. An Improved Method in Fabrication of Smart Dual-Responsive Nanogels for Controlled Release of Doxorubicin and Curcumin in Ht-29 Colon Cancer Cells. J. Nanobiotechnol. 2021, 19, 18. [Google Scholar] [CrossRef]
- Li, Q.; Fu, D.S.; Zhang, J.; Yan, H.; Wang, H.F.; Niu, B.L.; Guo, R.J.; Liu, Y.M. Dual Stimuli-Responsive Polypeptide-Calcium Phosphate Hybrid Nanoparticles for Co-Delivery of Multiple Drugs in Cancer Therapy. Colloids Surf. B Biointerfaces 2021, 200, 111586. [Google Scholar] [CrossRef]
- Kashyap, D.; Tuli, H.S.; Yerer, M.B.; Sharma, A.; Sak, K.; Srivastava, S.; Pandey, A.; Garg, V.K.; Sethi, G.; Bishayee, A. Natural Product-Based Nanoformulations for Cancer Therapy: Opportunities and Challenges. Semin. Cancer Biol. 2021, 69, 5–23. [Google Scholar] [CrossRef]
- Costa, R.; Azevedo, D.; Barata, P.; Soares, R.; Guido, L.F.; Carvalho, D.O. Antiangiogenic and Antioxidant in Vitro Properties of Hydroethanolic Extract from Acai (Euterpe Oleracea) Dietary Powder Supplement. Molecules 2021, 26, 2011. [Google Scholar] [CrossRef]
- Kluska, M.; Juszczak, M.; Zuchowski, J.; Stochmal, A.; Wozniak, K. Kaempferol and Its Glycoside Derivatives as Modulators of Etoposide Activity in Hl-60 Cells. Int. J. Mol. Sci. 2021, 22, 3520. [Google Scholar] [CrossRef]
- Cacciola, N.A.; Cerrato, A.; Capriotti, A.L.; Cavaliere, C.; D’Apolito, M.; Montone, C.M.; Piovesana, S.; Squillaci, G.; Peluso, G.; Lagana, A. Untargeted Characterization of Chestnut (Castanea Sativa Mill.) Shell Polyphenol Extract: A Valued Bioresource for Prostate Cancer Cell Growth Inhibition. Molecules 2020, 25, 2730. [Google Scholar] [CrossRef]
- Figarol, A.; Gibot, L.; Golzio, M.; Lonetti, B.; Mingotaud, A.F.; Rols, M.P. A Journey from the Endothelium to the Tumor Tissue: Distinct Behavior between Peo-Pcl Micelles and Polymersomes Nanocarriers. Drug Deliv. 2018, 25, 1766–1778. [Google Scholar] [CrossRef]
- Chen, B.H.; Hsieh, C.H.; Tsai, S.Y.; Wang, C.Y.; Wang, C.C. Anticancer Effects of Epigallocatechin-3-Gallate Nanoemulsion on Lung Cancer Cells through the Activation of Amp-Activated Protein Kinase Signaling Pathway. Sci. Rep. 2020, 10, 5163. [Google Scholar] [CrossRef]
- Zhang, F.; Lu, G.H.; Wen, X.L.; Li, F.; Ji, X.Y.; Li, Q.Q.; Wu, M.Y.; Cheng, Q.Z.; Yu, Y.K.; Tang, J.; et al. Magnetic Nanoparticles Coated with Polyphenols for Spatio-Temporally Controlled Cancer Photothermal/Immunotherapy. J. Control. Release 2020, 326, 131–139. [Google Scholar] [CrossRef]
- Lerra, L.; Farfalla, A.; Sanz, B.; Cirillo, G.; Vittorio, O.; Voli, F.; le Grand, M.; Curcio, M.; Nicoletta, F.P.; Dubrovska, A.; et al. Graphene Oxide Functional Nanohybrids with Magnetic Nanoparticles for Improved Vectorization of Doxorubicin to Neuroblastoma Cells. Pharmaceutics 2019, 11, 3. [Google Scholar] [CrossRef]
- Wang, W.L.; Zhang, L.; Le, Y.; Chen, J.F.; Wang, J.X.; Yun, J. Synergistic Effect of Pegylated Resveratrol on Delivery of Anticancer Drugs. Int. J. Pharm. 2016, 498, 134–141. [Google Scholar] [CrossRef]
- Rai, S.; Kureel, A.K.; Dutta, P.K.; Mehrotra, G.K. Phenolic Compounds Based Conjugates from Dextran Aldehyde and Bsa: Preparation, Characterization and Evaluation of Their Anti-Cancer Efficacy for Therapeutic Applications. Int. J. Biol. Macromol. 2018, 110, 425–436. [Google Scholar] [CrossRef]
- Karabasz, A.; Lachowicz, D.; Karewicz, A.; Mezyk-Kopec, R.; Stalinska, K.; Werner, E.; Cierniak, A.; Dyduch, G.; Bereta, J.; Bzowska, M. Analysis of Toxicity and Anticancer Activity of Micelles of Sodium Alginate-Curcumin. Int. J. Nanomed. 2019, 14, 7249–7262. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Tan, W.Q.; Zhang, J.J.; Guo, Z.Y. Phenolic-Containing Chitosan Quaternary Ammonium Derivatives and Their Significantly Enhanced Antioxidant and Antitumor Properties. Carbohydr. Res. 2020, 498, 108169. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.H.; Jang, H.; Roh, J.L. A Novel Polyphenol Conjugate Sensitizes Cisplatin-Resistant Head and Neck Cancer Cells to Cisplatin Via Nrf2 Inhibition. Mol. Cancer Ther. 2016, 15, 2620–2629. [Google Scholar] [CrossRef] [PubMed]
- Shah, K.N.; Ditto, A.J.; Crowder, D.C.; Overmeyer, J.H.; Tavana, H.; Maltese, W.A.; Yun, Y.H. Receptor-Mediated Attachment and Uptake of Hyaluronan Conjugates by Breast Cancer Cells. Mol. Pharm. 2017, 14, 3968–3977. [Google Scholar] [CrossRef]
- Shin, S.Y.; Lee, J.M.; Lee, M.S.; Koh, D.; Jung, H.; Lim, Y.; Lee, Y.H. Targeting Cancer Cells Via the Reactive Oxygen Species-Mediated Unfolded Protein Response with a Novel Synthetic Polyphenol Conjugate. Clin. Cancer Res. 2014, 20, 4302–4313. [Google Scholar] [CrossRef]
- Su, J.; Chen, F.; Cryns, V.L.; Messersmith, P.B. Catechol Polymers for Ph-Responsive, Targeted Drug Delivery to Cancer Cells. J. Am. Chem. Soc. 2011, 133, 11850–11853. [Google Scholar] [CrossRef]
- Vittorio, O.; Cojoc, M.; Curcio, M.; Spizzirri, U.G.; Hampel, S.; Nicoletta, F.P.; Iemma, F.; Dubrovska, A.; Kavallaris, M.; Cirillo, G. Polyphenol Conjugates by Immobilized Laccase: The Green Synthesis of Dextran-Catechin. Macromol. Chem. Phys. 2016, 217, 1488–1492. [Google Scholar] [CrossRef]
- Cirillo, G.; Pantuso, E.; Curcio, M.; Vittorio, O.; Leggio, A.; Iemma, F.; de Filpo, G.; Nicoletta, F.P. Alginate Bioconjugate and Graphene Oxide in Multifunctional Hydrogels for Versatile Biomedical Applications. Molecules 2021, 26, 1355. [Google Scholar] [CrossRef]
- Vittorio, O.; Brandl, M.; Cirillo, G.; Kimpton, K.; Hinde, E.; Gaus, K.; Yee, E.; Kumar, N.; Duong, H.; Fleming, C.; et al. Dextran-Catechin: An Anticancer Chemically-Modified Natural Compound Targeting Copper That Attenuates Neuroblastoma Growth. Oncotarget 2016, 7, 47479–47493. [Google Scholar] [CrossRef]
- Curcio, M.; Cirillo, G.; Tucci, P.; Farfalla, A.; Bevacqua, E.; Vittorio, O.; Iemma, F.; Nicoletta, F.P. Dextran-Curcumin Nanoparticles as a Methotrexate Delivery Vehicle: A Step Forward in Breast Cancer Combination Therapy. Pharmaceuticals 2020, 13, 2. [Google Scholar] [CrossRef]
- Rivera, M.; Ramos, Y.; Rodriguez-Valentin, M.; Lopez-Acevedo, S.; Cubano, L.A.; Zou, J.; Zhang, Q.; Wang, G.D.; Boukli, N.M. Targeting Multiple Pro-Apoptotic Signaling Pathways with Curcumin in Prostate Cancer Cells. PLoS ONE 2017, 12, e0179587. [Google Scholar] [CrossRef]
- Tanaudommongkon, I.; Tanaudommongkon, A.; Prathipati, P.; Nguyen, J.T.; Keller, E.T.; Dong, X.W. Curcumin Nanoparticles and Their Cytotoxicity in Docetaxel-Resistant Castration-Resistant Prostate Cancer Cells. Biomedicines 2020, 8, 253. [Google Scholar] [CrossRef]
- Zhang, P.J.; Sun, Y.T.; Ma, L. Zeb1: At the Crossroads of Epithelial-Mesenchymal Transition, Metastasis and Therapy Resistance. Cell Cycle 2015, 14, 481–487. [Google Scholar] [CrossRef]
- Keklikoglou, I.; Cianciaruso, C.; Guc, E.; Squadrito, M.L.; Spring, L.M.; Tazzyman, S.; Lambein, L.; Poissonnier, A.; Ferraro, G.B.; Baer, C.; et al. Chemotherapy Elicits Pro-Metastatic Extracellular Vesicles in Breast Cancer Models. Nat. Cell Biol. 2019, 21, 190–202. [Google Scholar] [CrossRef]
- Liang, Y.P.; Zhao, X.; Ma, P.X.; Guo, B.L.; Du, Y.P.; Han, X.Z. Ph-Responsive Injectable Hydrogels with Mucosal Adhesiveness Based on Chitosan-Grafted-Dihydrocaffeic Acid and Oxidized Pullulan for Localized Drug Delivery. J. Colloid Interface Sci. 2019, 536, 224–234. [Google Scholar] [CrossRef]
- Singh, N.; Sallem, F.; Mirjolet, C.; Nury, T.; Sahoo, S.K.; Millot, N.; Kumar, R. Polydopamine Modified Superparamagnetic Iron Oxide Nanoparticles as Multifunctional Nanocarrier for Targeted Prostate Cancer Treatment. Nanomaterials 2019, 9, 138. [Google Scholar] [CrossRef]
- Dey, S.; Ambattu, L.A.; Hari, P.R.; Rekha, M.R.; Sreenivasan, K. Glutathione-Bearing Fluorescent Polymer-Curcumin Conjugate Enables Simultaneous Drug Delivery and Label-Free Cellular Imaging. Polymer 2015, 75, 25–33. [Google Scholar] [CrossRef]
- Ghasemi, F.; Shafiee, M.; Banikazemi, Z.; Pourhanifeh, M.H.; Khanbabaei, H.; Shamshirian, A.; Moghadam, S.A.; ArefNezhad, R.; Sahebkar, A.; Avan, A.; et al. Curcumin Inhibits Nf-Kb and Wnt/Beta-Catenin Pathways in Cervical Cancer Cells. Pathol. Res. Pract. 2019, 215, 152556. [Google Scholar] [CrossRef]
- Hassan, F.-U.; Rehman, M.S.U.; Khan, M.S.; Ali, M.A.; Javed, A.; Nawaz, A.; Yang, C.J. Curcumin as an Alternative Epigenetic Modulator: Mechanism of Action and Potential Effects. Front. Genet. 2019, 10, 514. [Google Scholar] [CrossRef]
- Hassanzadeh, K.; Buccarello, L.; Dragotto, J.; Mohammadi, A.; Corbo, M.; Feligioni, M. Obstacles against the Marketing of Curcumin as a Drug. Int. J. Mol. Sci. 2020, 21, 6619. [Google Scholar] [CrossRef]
- Ghayour, N.; Hosseini, S.M.H.; Eskandari, M.H.; Esteghlal, S.; Nekoei, A.R.; Gahruie, H.H.; Tatar, M.; Naghibalhossaini, F. Nanoencapsulation of Quercetin and Curcumin in Casein-Based Delivery Systems. Food Hydrocoll. 2019, 87, 394–403. [Google Scholar] [CrossRef]
- Chen, F.; Huang, G.L.; Huang, H.L. Preparation and Application of Dextran and Its Derivatives as Carriers. Int. J. Biol. Macromol. 2020, 145, 827–834. [Google Scholar] [CrossRef]
- Shen, M.Y.; Liu, T.I.; Yu, T.W.; Kv, R.; Chiang, W.H.; Tsai, Y.C.; Chen, H.H.; Lin, S.C.; Chiu, H.C. Hierarchically Targetable Polysaccharide-Coated Solid Lipid Nanoparticles as an Oral Chemo/Thermotherapy Delivery System for Local Treatment of Colon Cancer. Biomaterials 2019, 197, 86–100. [Google Scholar] [CrossRef]
- Chen, Y.; Gao, Y.J.; Li, Y.C.; Wang, K.; Zhu, J.T. Synergistic Chemo-Photodynamic Therapy Mediated by Light-Activated Ros-Degradable Nanocarriers. J. Mater. Chem. B 2019, 7, 460–468. [Google Scholar] [CrossRef]
- Sadreddini, S.; Safaralizadeh, R.; Baradaran, B.; Aghebati-Maleki, L.; Hosseinpour-Feizi, M.A.; Shanehbandi, D.; Jadidi-Niaragh, F.; Sadreddini, S.; Kafil, H.S.; Younesi, V.; et al. Chitosan Nanoparticles as a Dual Drug/Sirna Delivery System for Treatment of Colorectal Cancer. Immunol. Lett. 2017, 181, 79–86. [Google Scholar] [CrossRef]
- Afkham, A.; Aghebati-Maleki, L.; Siahmansouri, H.; Sadreddini, S.; Ahmadi, M.; Dolati, S.; Afkham, N.M.; Akbarzadeh, P.; Jadidi-Niaragh, F.; Younesi, V.; et al. Chitosan (Cmd)-Mediated Co-Delivery of Sn38 and Snail-Specific Sirna as a Useful Anticancer Approach against Prostate Cancer. Pharmacol. Rep. 2018, 70, 418–425. [Google Scholar] [CrossRef]
- Deryugina, E.I.; Kiosses, W.B. Intratumoral Cancer Cell Intravasation Can Occur Independent of Invasion into the Adjacent Stroma. Cell Rep. 2017, 19, 601–616. [Google Scholar] [CrossRef]
- Chen, A.C.; Donovan, A.; Ned-Sykes, R.; Andrews, N.C. Noncanonical Role of Transferrin Receptor 1 Is Essential for Intestinal Homeostasis. Proc. Natl. Acad. Sci. USA 2015, 112, 11714–11719. [Google Scholar] [CrossRef] [PubMed]
- Shenoy, A.K.; Jin, Y.; Luo, H.C.; Tang, M.; Pampo, C.; Shao, R.; Siemann, D.W.; Wu, L.Z.; Heldermon, C.D.; Law, B.K.; et al. Epithelial-to-Mesenchymal Transition Confers Pericyte Properties on Cancer Cells. J. Clin. Investig. 2016, 126, 4174–4186. [Google Scholar] [CrossRef]
- Liu, J.; Yong, H.M.; Yao, X.Y.; Hu, H.X.; Yun, D.W.; Xiao, L.X. Recent Advances in Phenolic-Protein Conjugates: Synthesis, Characterization, Biological Activities and Potential Applications. RSC Adv. 2019, 9, 35825–35840. [Google Scholar] [CrossRef]
- Yang, B.Y.; Dong, Y.X.; Wang, F.; Zhang, Y. Nanoformulations to Enhance the Bioavailability and Physiological Functions of Polyphenols. Molecules 2020, 25, 4613. [Google Scholar] [CrossRef] [PubMed]
- Zhou, H.; Ning, Y.C.; Zeng, G.R.; Zhou, C.; Ding, X.F. Curcumin Promotes Cell Cycle Arrest and Apoptosis of Acute Myeloid Leukemia Cells by Inactivating Akt. Oncol. Rep. 2021, 45, 11. [Google Scholar] [CrossRef] [PubMed]
- Li, W.F.; Gong, Y.X.; Li, H.F.; Sun, F.L.; Li, W.L.; Chen, D.Q.; Xie, D.P.; Ren, C.X.; Guo, X.Y.; Wang, Z.Y.; et al. Curcumin Activates Ros Signaling to Promote Pyroptosis in Hepatocellular Carcinoma Hepg2 Cells. In Vivo 2021, 35, 249–257. [Google Scholar]
- Gupta, N.; Verma, K.; Nalla, S.; Kulshreshtha, A.; Lall, R.; Prasad, S. Free Radicals as a Double-Edged Sword: The Cancer Preventive and Therapeutic Roles of Curcumin. Molecules 2020, 25, 5390. [Google Scholar] [CrossRef]
- Redza-Dutordoir, M.; Averill-Bates, D.A. Activation of Apoptosis Signalling Pathways by Reactive Oxygen Species. Biochim. Biophys. Acta Mol. Cell Res. 2016, 1863, 2977–2992. [Google Scholar] [CrossRef]
- Piktel, E.; Oscilowska, I.; Suprewicz, L.; Depciuch, J.; Marcinczyk, N.; Chabielska, E.; Wolak, P.; Wollny, T.; Janion, M.; Parlinska-Wojtan, M.; et al. Ros-Mediated Apoptosis and Autophagy in Ovarian Cancer Cells Treated with Peanut-Shaped Gold Nanoparticles. Int. J. Nanomed. 2021, 16, 1993–2011. [Google Scholar] [CrossRef]
- Feng, Z.J.; Guo, J.X.; Liu, X.; Song, H.J.; Zhang, C.N.; Huang, P.S.; Dong, A.J.; Kong, D.L.; Wang, W.W. Cascade of Reactive Oxygen Species Generation by Polyprodrug for Combinational Photodynamic Therapy. Biomaterials 2020, 255, 120210. [Google Scholar] [CrossRef]
- Halliwell, B. The Antioxidant Paradox: Less Paradoxical Now? Br. J. Clin. Pharmacol. 2013, 75, 637–644. [Google Scholar] [CrossRef]
- Bonner, M.Y.; Arbiser, J.L.; Halliwell, B. The antioxidant paradox: What are antioxidants and how should they be used in a therapeutic context for cancer. Future Med. Chem. 2014, 6, 1413–1422. [Google Scholar] [CrossRef]
- Reed, I.K.G. Mechanism and Regulation of Epithelial-Mesenchymal Transition in Cancer. Cell Health Cytoskelet. 2015, 7, 155–165. [Google Scholar] [CrossRef]
- Zhang, N.; Fu, J.N.; Chou, T.C. Synergistic Combination of Microtubule Targeting Anticancer Fludelone with Cytoprotective Panaxytriol Derived from Panax Ginseng against Mx-1 Cells in Vitro: Experimental Design and Data Analysis Using the Combination Index Method. Am. J. Cancer Res. 2016, 6, 97–104. [Google Scholar]
- Foca, A.; Gasperlin, M.; Kristl, J. Investigation of Liposomes as Carriers of Sodium Ascorbyl Phosphate for Cutaneous Photoprotection. Int. J. Pharm. 2005, 291, 21–29. [Google Scholar] [CrossRef]
- Tucci, P.; Agostini, M.; Grespi, F.; Markert, E.K.; Terrinoni, A.; Vousden, K.H.; Muller, P.A.J.; Dotsch, V.; Kehrloesser, S.; Sayan, B.S.; et al. Loss of P63 and Its Microrna-205 Target Results in Enhanced Cell Migration and Metastasis in Prostate Cancer. Proc. Natl. Acad. Sci. USA 2012, 109, 15312–15317. [Google Scholar] [CrossRef]
- Frattaruolo, L.; Fiorillo, M.; Brindisi, M.; Curcio, R.; Dolce, V.; Lacret, R.; Truman, A.W.; Sotgia, F.; Lisanti, M.P.; Cappello, A.R. Thioalbamide, a Thioamidated Peptide from Amycolatopsis Alba, Affects Tumor Growth and Stemness by Inducing Metabolic Dysfunction and Oxidative Stress. Cells 2019, 8, 1408. [Google Scholar] [CrossRef]

| Model | R2 | K | ||
|---|---|---|---|---|
| pH 5.0 | pH 7.4 | pH 5.0 | pH 7.4 | |
| Equation (1) | 0.9978 | 0.5855 | 0.0122 | 0.0007 |
| Equation (2) | 0.9575 | 0.9985 | 0.0868 1 0.0019 2 | 0.0271 1 0.0003 2 |
| Treatment | [µM] 1 | DOXO [µM] | |
|---|---|---|---|
| 1.0 | 2.5 | ||
| CUR | 5 | 0.91 | 1.04 |
| 10 | 1.02 | 1.17 | |
| 20 | 1.35 | 1.48 | |
| DEX/CUR | 5 | 0.72 | 0.90 |
| 10 | 0.81 | 0.95 | |
| 20 | 0.95 | 1.31 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bevacqua, E.; Curcio, M.; Saletta, F.; Vittorio, O.; Cirillo, G.; Tucci, P. Dextran-Curcumin Nanosystems Inhibit Cell Growth and Migration Regulating the Epithelial to Mesenchymal Transition in Prostate Cancer Cells. Int. J. Mol. Sci. 2021, 22, 7013. https://doi.org/10.3390/ijms22137013
Bevacqua E, Curcio M, Saletta F, Vittorio O, Cirillo G, Tucci P. Dextran-Curcumin Nanosystems Inhibit Cell Growth and Migration Regulating the Epithelial to Mesenchymal Transition in Prostate Cancer Cells. International Journal of Molecular Sciences. 2021; 22(13):7013. https://doi.org/10.3390/ijms22137013
Chicago/Turabian StyleBevacqua, Emilia, Manuela Curcio, Federica Saletta, Orazio Vittorio, Giuseppe Cirillo, and Paola Tucci. 2021. "Dextran-Curcumin Nanosystems Inhibit Cell Growth and Migration Regulating the Epithelial to Mesenchymal Transition in Prostate Cancer Cells" International Journal of Molecular Sciences 22, no. 13: 7013. https://doi.org/10.3390/ijms22137013
APA StyleBevacqua, E., Curcio, M., Saletta, F., Vittorio, O., Cirillo, G., & Tucci, P. (2021). Dextran-Curcumin Nanosystems Inhibit Cell Growth and Migration Regulating the Epithelial to Mesenchymal Transition in Prostate Cancer Cells. International Journal of Molecular Sciences, 22(13), 7013. https://doi.org/10.3390/ijms22137013









